#Thomas Jefferson Medical College in Philadelphia
Text
youtube
#The Changing Face of Healthcare with Dr. Robert Barkett | KAJ Masterclass LIVE A Conversation on The Changing Face of Healthcare with Robert#a board certified physician and author
Rob Barkett MD#graduated from Purdue University#Thomas Jefferson Medical College in Philadelphia#and completed his internal medicine residency at Riverside Methodist Hospital in Columbus#Ohio. He is a board certified physician who has been in private practice for 29 years#serves as Medical Director of a nursing home and a thriving hospice agency. Author of Simple Medicine : No More Google Searches#Youtube
0 notes
Text


SCENES FROM MODERN LIFE; THOMAS EAKINS
Thomas Eakins (1844–1916) was an influential American painter known for his realism and focus on the human form. His father was a calligrapher and writing teacher, and at first, that seems to have been Thomas Eakins’ direction, too. He studied at the Pennsylvania Academy of the Fine Arts where he learnt drawing and anatomy.
The Champion Single Sculls (Max Schmitt in a Single Scull) (1871)
Created to commemorate the victory of Eakins's friend, Max Schmitt, in a rowing competition on Philadelphia's Schuylkill River. Eakins, a passionate oarsman himself, depicted Schmitt in a moment of calm rather than in the throes of competition. The painting captures great detail in the water, oars, and weather, Eakins even included himself in the artwork, rowing in the background.
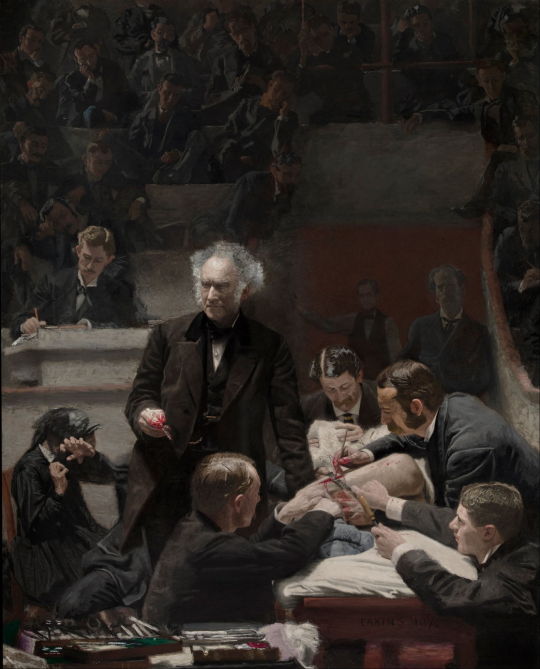
Portrait of Dr. Samuel D. Gross (The Gross Clinic) (1875)
It is a portrait of the renowned Philadelphia surgeon in the surgical amphitheater of Jefferson Medical College (now part of Thomas Jefferson University). Eakins includes himself in the painting, seated at the far left, sketching the scene. The patient's mother, who looks away and shields her eyes, unable to watch the surgery, is also included. The procedure took place before the advent of aseptic technique, so instruments were clean but not sterile, gloves and gowns were not worn.
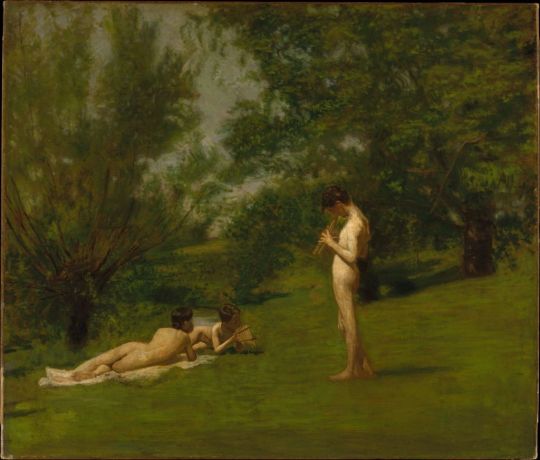
Arcadia (c 1883)
This painting was an unusual venture into mythology, created during a period when Eakins was experimenting with photography. Eakins had bought his first camera in 1880 and started to use it as a photographic sketchbook. Although it can be read as another step in his campaign for painting from life, the work features models posed in a pastoral setting, including his future wife, Susan Macdowell, and his nephew, Ben Crowell.
Swimming (The Swimming Hole) (1885)
Bathers have been a popular and recurrent theme in paintings since the dawn of the art. Here, Eakins features identifiable figures, which are Eakins himself and several of his students. However, its exhibition in 1885 sparked controversy due to its graphic portrayal of nudity and identifiable figures. This backlash contributed to Eakins's resignation from the Academy in 1886 after a series of complaints about his promotion of nude studies.
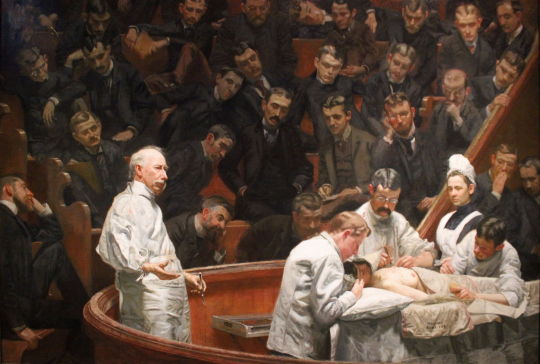
The Agnew Clinic (1889)
This fine painting shows the surgeon performing a partial mastectomy, and the whole scene is a testament of how surgery had advanced in just fourteen years. The clean white gowns worn by the doctors, the use of sterilized instruments, techniques promoted by Agnew. Eakins completed the painting quickly, in just three months, rather than the year he took for his earlier masterpiece, The Gross Clinic.
58 notes
·
View notes
Text
Today In History:

A bit of February 17th history…
In 1801, the U.S. House of Representatives broke an electoral tie between Thomas Jefferson and Aaron Burr, electing Jefferson president; Burr became vice president.
In 1864, during the Civil War, the Union ship USS Housatonic was rammed and sunk in Charleston Harbor, South Carolina, by the Confederate hand-cranked submarine HL Hunley in the first naval attack of its kind; the Hunley also sank.
In 1815, the United States and Britain exchanged the instruments of ratification for the Treaty of Ghent, ending the War of 1812.
In 1865, during the Civil War, Columbia, South Carolina, burned as the Confederates evacuated and Union forces moved in.
In 1897, the forerunner of the National PTA, the National Congress of Mothers, convened its first meeting in Washington.
In 1933, Newsweek magazine was first published under the title “News-Week.”
In 1944, during World War II, U.S. forces invaded Eniwetok Atoll, encountering little initial resistance from Imperial Japanese troops. (The Americans secured the atoll less than a week later.)
In 1947, the Voice of America began broadcasting to the Soviet Union.
In 1968, the original Naismith Memorial Basketball Hall of Fame, located on the campus of Springfield College in Massachusetts, was opened to the public.
In 1972, President Richard M. Nixon departed the White House with his wife, Pat, on a historic trip to China.
In 1986, Johnson & Johnson announced it would no longer sell over-the-counter medications in capsule form, following the death of a woman who had taken a cyanide-laced Tylenol capsule.
In 1988, Lt. Col. William Higgins, a Marine Corps officer serving with a United Nations truce monitoring group, was kidnapped in southern Lebanon by Iranian-backed terrorists (he was later slain by his captors).
In 1996, world chess champion Garry Kasparov beat IBM supercomputer “Deep Blue,” winning a six-game match in Philadelphia (however, Kasparov lost to Deep Blue in a rematch in 1997).
0 notes
Text
thomas eakins
He was enrolled at the Pennsylvania Academy of the Fine Arts from 1862 to 1866, attended anatomy lectures at Jefferson Medical College, and profited from contact with Philadelphia’s art collections, exhibitions, and artists.
Arriving in Paris for study in 1866, Eakins was in the vanguard of young painters who would shift the focus of American art from landscape to the figural subjects favored by the European academies.
After almost three years of instruction Eakins returned to Philadelphia in July 1870.
From boyhood, he had himself been athletic; as an ambitious, original young artist intent on portraying the world around him, he embraced as subjects the activities that he himself enjoyed, which provided opportunities to demonstrate his technical skill.
While Eakins was painting works that expressed his admiration of athletes and outdoor activities, he was also creating intense, brooding images of women and children in quiet, shadowed interiors.
In late March 1875, the artist wrote to a friend, “I feel to myself that I am going soon to do work so much better than anything that I have made yet.” It seems likely that the project sparking Eakins’ enthusiasm was the canvas that occupied him for almost a year—The Gross Clinic
Having begun teaching at the Pennsylvania Academy in 1876, he transformed it into the leading art school in America. However, discontent also arose concerning his teaching methods, especially his emphasis on the nude.
In January 1886, lecturing about the pelvis to a class that included female students, Eakins removed a loincloth from a male model so that he could trace the course of a muscle. Angry protests by parents and students forced him to resign at the request of the Academy board.
From 1887 until the end of his career, Eakins focused almost exclusively on portraiture. He usually worked at life scale, renouncing outdoor light and focusing on the sitter in isolation. Eakins rarely received commissions for portraits and most of his sitters were friends or conocidos.
In 1898 and 1899, for the first time since the 1870s, Eakins returned to the subject of athletics.
0 notes
Text

Guest post from John Martin Rare Book Room
At the Hardin Library for the Health Sciences
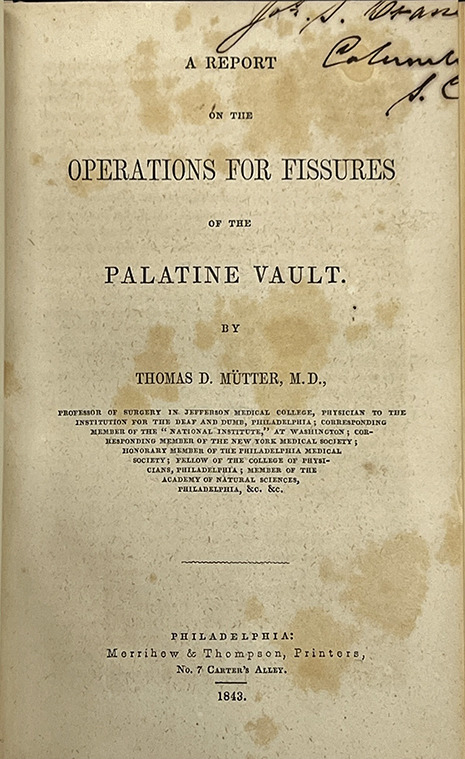
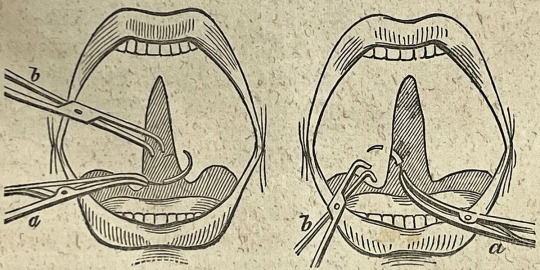
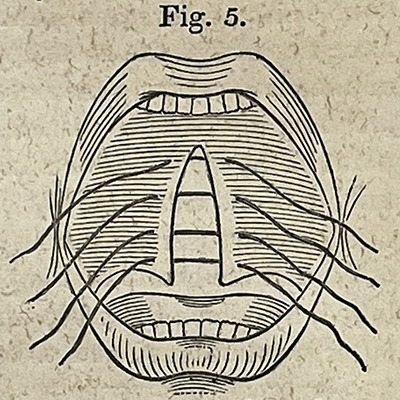
MÜTTER, Thomas Dent (1811–1859). A report on the operations for fissures of the palatine vault. Printed in Philadelphia by Merrihew & Thompson, 1843. 28 pages. 23 cm tall.
The University of Iowa is a worldwide leader in cleft palate research and repair, so we thought it only appropriate to recognize National Cleft and Craniofacial Awareness Month.
Many of you have no doubt heard of the Mütter Museum in Philadelphia, with its famous collection of anatomical specimens and medical instruments. The namesake of the museum, Thomas Dent Mütter, was a 19th-century American surgeon who overcame personal tragedy to become a renowned surgeon and educator.
One area that fascinated him was cleft palate and lip repair. This month's book, A report on the operations for fissures of the palatine vault, written by Mütter and printed in 1843, details his straightforward repair for a cleft palate.
The earliest evidence of cleft lip repair comes from the Jin Dynasty (265-420 CE) in China. The earliest detailed description of a repair is from Jehan Yperman (c.1260–c.1331), a pioneering medieval Flemish surgeon. The first known detailed description of a cleft palate comes from 16th-century French surgeon Pierre Franco (1505-1578). Franco emphasized the importance of the palate to speech development and the congenital origin of the malformation.
Clefts could also be caused by syphilis, however, and during the 16th and 17th centuries, surgical repairs were not advised. Instead, our old friend, Ambroise Paré, along with the Portuguese surgeon Amatus Lusitanus (aka João Rodrigues de Castelo Branco), wrote of using obturators - custom prosthetic devices used to close the palate.
Interest in surgical repair continued, though, especially for congenital clefts. By the 19th century, several Fench surgeons had devised their own methods for repair, including Guillaume Dupuytren, who Mütter trained with while continuing his medical education in Paris.
The Mütter Museum in Philadelphia is celebrated for its collection of anatomical specimens of rare conditions, from the famous (and infamous), as well as medical instruments. The museum was founded with an original donation from the collection of Thomas Dent Mütter.
Mütter was born in 1811 in Richmond, Virginia. Sickness is a common theme in Mütter's life, and he lost both of his parents by the time he was eight. He was raised by a distant relative in a seemingly supportive environment.
Money left to him by his parents allowed him to attend Hampden-Sydney College in Virginia and medical school at the University of Pennsylvania. Mütter himself fell ill during medical school. He left for Europe after graduation in the hopes of improving his health in a different climate and to further pursue his medical education.
In Paris, he worked with the aforementioned Dupuytren and in London with Robert Liston. Mütter eventually put together a collection of lectures by Liston, which he annotated with 250 pages of his own.
Dupuytren was known for his exacting nature and Liston for his speed when performing a surgical procedure (which could mean the difference between life and death in the days before anesthesia and antibiotics). Mütter seems to have embraced the teachings of both his mentors, stressing the need for the simplest of tools and techniques when performing his reconstructive surgeries while trying to keep the pain and blood loss to a minimum.
In 1841, he joined the faculty of the Jefferson Medical College in Philadelphia. It was there that he made a name for himself as an excellent speaker and engaging teacher. He used his ever-expanding anatomical and instrument collection to provide his students with hands-on experience.
Unfortunately, his ill health never truly subsided and he was forced to retire in 1856. He died three years later at the age of 48.
A report on the operations for fissures of the palatine vault demonstrates Mütter's adherence to his surgical principles. It is not a long book, only 28 pages, but it provides insight into his process and surgical philosophy. It includes several small illustrations of the steps of the procedure and the instruments used, examples of which you can see above.
The book is covered in a "library binding" of black cloth and the textblock shows evidence of having been trimmed (see the ownership mark in the upper right corner of the title page above). Indeed, this book was at some point pulled from the circulating Hardin collection and added to the Rare Book Room collection. It still contains the date due slip (last checked out in 1967!) and barcode sticker.
Contact Curator Damien Ihrig to view this tiny but mighty book or any others from this or past newsletters: [email protected] to arrange a visit in person or over Zoom.
#cleft palate#medical#medical history#jmrbr#hardin library#special collections#rare books#uiowa#libraries#Mütter
11 notes
·
View notes
Photo

Today we remember the passing of Pearl Bailey who Died: August 17, 1990 at Thomas Jefferson University Hospital in Philadelphia.
Pearl Mae Bailey (March 29, 1918 – August 17, 1990) was an American actress and singer. After appearing in vaudeville she made her Broadway debut in St. Louis Woman in 1946. She won a Tony Award for the title role in the all-Black production of Hello, Dolly! in 1968. In 1986, she won a Daytime Emmy award for her performance as a fairy godmother in the ABC Afterschool Special, Cindy Eller: A Modern Fairy Tale.
Her rendition of "Takes Two to Tango" hit the top ten in 1952. She received the Screen Actors Guild Life Achievement Award in 1976 and the Presidential Medal of Freedom on October 17, 1988.
Bailey began by singing and dancing in Philadelphia's black nightclubs in the 1930s, and soon started performing in other parts of the East Coast. In 1941, during World War II, Bailey toured the country with the USO, performing for American troops. After the tour, she settled in New York. Her solo successes as a nightclub performer were followed by acts with such entertainers as Cab Calloway and Duke Ellington. In 1946, Bailey made her Broadway debut in St. Louis Woman. For her performance, she won a Donaldson Award as the best Broadway newcomer. Bailey continued to tour and record albums in between her stage and screen performances. Early in the television medium, Bailey guest starred on CBS's Faye Emerson's Wonderful Town.
In 1967, Bailey and Cab Calloway headlined an all-black cast version of Hello, Dolly! The touring version was so successful, producer David Merrick took it to Broadway where it played to sold-out houses and revitalized the long running musical. Bailey was given a special Tony Award for her role and RCA Victor made a second original cast album. That is the only recording of the score to have an overture which was written especially for that recording.
A passionate fan of the New York Mets, Bailey sang the national anthem at Shea Stadium prior to game 5 of the 1969 World Series, and appears in the Series highlight film showing her support for the team. She also sang the national anthem prior to Game 1 of the 1981 World Series between the New York Yankees and Los Angeles Dodgers at Yankee Stadium.
On November 19, 1952, Bailey married the jazz drummer Louie Bellson in London. They later adopted a son, Tony, in the mid-1950s. A daughter, Dee Dee J. Bellson, was born April 20, 1960. Tony Bellson died in 2004. Dee Dee Bellson died on July 4, 2009, at the age of 49, five months after her father, who died on Valentine's Day 2009.
Bailey, a Republican, was appointed by President Richard Nixon as America's "Ambassador of Love" in 1970. She attended several meetings of the United Nations and later appeared in a campaign ad for President Gerald Ford in the 1976 election. She was awarded the Bronze Medallion in 1968, the highest award conferred upon civilians by New York City.
Bailey was a very good friend of actress Joan Crawford. In 1969, Crawford and Bailey joined fellow friend Gypsy Rose Lee in accepting a USO Award. In the same year, Bailey was recognized as USO "Woman of the Year". Upon the death of Crawford in May 1977, Bailey spoke of Crawford as her sister before singing a hymn at her funeral. U.S. Ambassador and American socialite Perle Mesta was another close friend of Bailey. In the waning days of Mesta's life, Bailey visited her frequently and sang hymns for her.
Pearl Bailey died at Thomas Jefferson University Hospital in Philadelphia on August 17, 1990. Following an autopsy, Dr. Emanuel Rubin, professor and chairman of the Department of Pathology at Jefferson Medical College, announced the cause of death as arteriosclerosis, with significant narrowing of the coronary artery. Bailey is buried at Rolling Green Memorial Park in West Chester, Pennsylvania.
3 notes
·
View notes
Text

a commission for @hotlikesriracha (who's also the author of the following caption)
Thomas Dent Mütter (1811-1859)
was a pioneer in American plastic surgery. He brought the French method of autoplastie, or plastic surgery, over to the United States. He took on many difficult cases thought to be untreatable, like people whose faces were burned in fires, and gave them another chance at living in society again. The technique he created for those burn surgeries is still in use today, the Mütter flap, though the name has changed. He was also renowned for his work on congenital cases like club-foot and an advocate for ether anesthesia. He was professor of surgery at Jefferson Medical College and amassed a collection from his clinic to teach his students, which became the Mütter Museum in Philadelphia.
42 notes
·
View notes
Text
States Tag
Alabama: Do you like the movie Forrest Gump?
never seen it
Alaska: Would you rather deal with 30 days of day or 30 days of night?
Arizona: Can you handle heat well?
no, I get headaches and very grumpy
Arkansas: What are your opinions on Bill Clinton?
I have none, Im British so I don't really follow US politics
California: Who is your favorite actor? Favorite actress?
Actors: James McAvoy, David Tennant, Martin Freeman, all the Marvel guys, a list that goes on and on but my brain has gone blank. Actresses: my brain has gone to mush I cant think of a single actress ughhhhhh
Colorado: Do you smoke weed? What are your opinions on its legalization?
I don't smoke it. I think it should be legalised for medical use only but not for anyone like cigarettes are. My neighbours smoke it so our garden stinks of the stuff constantly
Connecticut: Have you ever had a school shooting at your school?
its not a thing we have to worry about it England
Delaware: Are you usually the first to do something, or are you more of a follower?
neither really, I just do my own thing
Florida: Have you ever been to Disney World?
not in america, I’ve been to Paris
Georgia: Would you consider yourself a southern belle?
no
Hawaii: What would be paradise for you?
right now, to just be alone. I hate living with my parents and the foster kids, especially today they have tested my patience all fucking day im at breaking point
Idaho: What is your favorite way to eat a potato?
jacket, or roasted
Illinois: Did you vote for President Obama (or would you have)?
I would have, yes
Indiana: Do you like corn?
no
Iowa: Are roses your favorite flower?
sunflowers are
Kansas: Do you like the Tin Man, Scarecrow or Cowardly Lion better?
cowardly lion just cause I think thats the one I relate to most
Kentucky: Have you ever been to a horse race?
no, and I don't want to
Louisiana: Have you ever celebrated Mardi Gras?
nope
Maine: Do you like lobster?
nope. I think its disgusting the way they are cooked too
Maryland: Have you ever been to Washington DC?
never been to America
Massachusetts: Are you smart enough to go to Harvard?
I barely passed English and maths gsce so doubt it
Michigan: Have you ever swam in a lake?
when I was a kid
Minnesota: Have you seen Drop Dead Gorgeous?
never heard of it
Mississippi: Do you follow college football?
nah
Missouri: Have you ever convinced someone to show you their private parts?
what the...? nope why would I do that and what has this to do with Missouri?!
Montana: What is the greatest treasure you have ever found?
Nebraska: Do you eat beef?
nope, I don't eat red meat
Nevada: Are you good at card games?
No, and not very interested in them either.
New Hampshire: What are your views on gay marriage?
it should be legal. Im a Christian I have no issue with it. you love who you love. the only thing I don't agree with is gay marriages happening in a church but any other venue go for it.
New Jersey: Do you watch The Jersey Shore?
no, ive seen some of the English version Geordie Shore
New Mexico: Would you consider yourself a hippie?
nope
New York: Have you ever been to New York City? Would you like to?
omg please I desperate to visit New York but im too poor
North Carolina: Are the Panthers your favorite football team?
don't like football
North Dakota: Have you seen Fargo?
eh I saw like one episode of the remake series a few years ago but I don't remember much about it
Ohio: Did you watch The Drew Carey Show?
nope
Oklahoma: What is your favorite musical?
oh man now you're asking the hard questions... Hamilton, Waitress, Dear Evan Hansen, Grinning Man, Six, Beetlejuice, Heathers, Into The Woods... im a massive theatre nerd
Oregon: Did you ever play the Oregon Trail game?
never heard of it
Pennsylvania: Do you watch It’s Always Sunny In Philadelphia?
never seen it
Rhode Island: Who is the smallest person you know?
our foster kid
South Carolina: Do you think Aziz Ansari is funny?
I don't know who that is
South Dakota: Who is more interesting: George Washington, Thomas Jefferson, Teddy Roosevelt or Abraham Lincoln?
everything I know about Washington and Jefferson is from Hamilton
Tennessee: Who is your favorite country singer?
dont know any... Is Dolly Parton country?
Texas: Do you like barbecue or Tex-Mex better?
barbecue
Utah: Do you know anyone who is Mormon?
nope, I don't think its much of a think in UK
Vermont: Do you get the full autumnal colors in the fall where you live?
yes
Virginia: Are you a virgin?
yes
Washington: Do you like grunge?
nope
West Virginia: Do you like the mountains?
I guess yeah
Wisconsin: What’s your favorite kind of cheese?
mozzarella or red leicester
Wyoming: Do you love westerns?
nah
2 notes
·
View notes
Text
Pearl Bailey

Pearl Mae Bailey (March 29, 1918 – August 17, 1990) was an American actress and singer. After appearing in vaudeville she made her Broadway debut in St. Louis Woman in 1946. She won a Tony Award for the title role in the all-black production of Hello, Dolly! in 1968. In 1986, she won a Daytime Emmy award for her performance as a fairy godmother in the ABC Afterschool Special, Cindy Eller: A Modern Fairy Tale.
Her rendition of "Takes Two to Tango" hit the top ten in 1952. She received the Screen Actors Guild Life Achievement Award in 1976 and the Presidential Medal of Freedom on October 17, 1988.
Early life
Bailey was born in Newport News, Virginia, United States, to the Reverend Joseph James and Ella Mae Ricks Bailey. She was raised in the Bloodfields neighborhood of Newport News, Virginia. She graduated from Booker T. Washington High School in nearby Norfolk, Virginia, the first city in the region to offer higher education for black students. Blues singer Ruth Brown from Portsmouth, Virginia was one of her classmates.
She made her stage-singing debut when she was 15 years old. Her brother Bill Bailey was beginning his own career as a tap dancer, and suggested she enter an amateur contest at the Pearl Theatre in Philadelphia. Bailey won and was offered $35 a week to perform there for two weeks. However, the theatre closed during her engagement and she was not paid. She later won a similar competition at Harlem's famous Apollo Theater and decided to pursue a career in entertainment.
Career
Bailey began by singing and dancing in Philadelphia's black nightclubs in the 1930s, and soon started performing in other parts of the East Coast. In 1941, during World War II, Bailey toured the country with the USO, performing for American troops. After the tour, she settled in New York. Her solo successes as a nightclub performer were followed by acts with such entertainers as Cab Calloway and Duke Ellington. In 1946, Bailey made her Broadway debut in St. Louis Woman. For her performance, she won a Donaldson Award as the best Broadway newcomer. Bailey continued to tour and record albums in between her stage and screen performances. Early in the television medium, Bailey guest starred on CBS's Faye Emerson's Wonderful Town.
Her support of female impersonator Lynne Carter led him to credit Bailey with launching his career.
In 1967, Bailey and Cab Calloway headlined an all-black cast version of Hello, Dolly! The touring version was so successful, producer David Merrick took it to Broadway where it played to sold-out houses and revitalized the long running musical. Bailey was given a special Tony Award for her role and RCA Victor made a second original cast album. That is the only recording of the score to have an overture which was written especially for that recording.
A passionate fan of the New York Mets, Bailey sang the national anthem at Shea Stadium prior to game 5 of the 1969 World Series, and appears in the Series highlight film showing her support for the team. She also sang the national anthem prior to Game 1 of the 1981 World Series between the New York Yankees and Los Angeles Dodgers at Yankee Stadium.
Bailey hosted her own variety series on ABC, The Pearl Bailey Show (January – May 1971) which featured many notable guests, including Lucille Ball, Bing Crosby and Louis Armstrong (one of his last appearances before his death).
Following her 1971 television series, she provided voices for animations such as Tubby the Tuba (1976) and Disney's The Fox and the Hound (1981). She returned to Broadway in 1975, playing the lead in an all-black production of Hello, Dolly!. In October 1975, she was invited by Betty Ford to sing for the Egyptian President Anwar Sadat in a White House state dinner, as part of Middle-Eastern peace initiative.
She earned a degree in theology from Georgetown University in Washington, D.C., in 1985 at age 67. Here she was a student of Wilfrid Desan.
Later in her career, Bailey was a fixture as a spokesperson in a series of Duncan Hines commercials, singing "Bill Bailey (Won't You Come Home)". She also appeared in commercials for Jell-O, and Westinghouse.She also did some free -spirited commercials for Paramount Chicken.
In her later years Bailey wrote several books: The Raw Pearl (1968), Talking to Myself (1971), Pearl's Kitchen (1973), and Hurry Up America and Spit (1976). In 1975 she was appointed special ambassador to the United Nations by President Gerald Ford. Her last book, Between You and Me (1989), details her experiences with higher education. On January 19, 1985, she appeared on the nationally televised broadcast of the 50th Presidential Inaugural Gala, the night before the second inauguration of Ronald Reagan. In 1988 Bailey received the Presidential Medal of Freedom from President Reagan.
Personal life
On November 19, 1952, Bailey married the jazz drummer Louie Bellson in London.
They later adopted a son, Tony, in the mid-1950s. A daughter, Dee Dee J. Bellson, was born April 20, 1960. Tony Bellson died in 2004. Dee Dee Bellson died on July 4, 2009, at the age of 49, five months after her father, who died on Valentine's Day 2009.
Bailey, a Republican, was appointed by President Richard Nixon as America's "Ambassador of Love" in 1970. She attended several meetings of the United Nations and later appeared in a campaign ad for President Gerald Ford in the 1976 election.
She was awarded the Bronze Medallion in 1968, the highest award conferred upon civilians by New York City.
Bailey was a very good friend of actress Joan Crawford. In 1969, Crawford and Bailey joined fellow friend Gypsy Rose Lee in accepting a USO Award. In the same year, Bailey was recognized as USO "Woman of the Year". Upon the passing of Crawford in May 1977, Bailey spoke of Crawford as her sister before singing a hymn at her funeral. U.S. Ambassador and American socialite Perle Mesta was another close friend of Bailey. In the waning days of Mesta's life, Bailey visited her frequently and sang hymns for her.
Death
Pearl Bailey died at Thomas Jefferson University Hospital in Philadelphia on August 17, 1990. Following an autopsy, Dr. Emanuel Rubin, professor and chairman of the Department of Pathology at Jefferson Medical College, announced the cause of death as arteriosclerosis, with significant narrowing of the coronary artery. Bailey is buried at Rolling Green Memorial Park in West Chester, Pennsylvania.
Remembrances
The television show American Dad! features Pearl Bailey High School.
The 1969 song "We Got More Soul" by Dyke and the Blazers includes Bailey in its roster of icons.
A dress owned by Bailey is at the National Museum of African American History and Culture.
14 notes
·
View notes
Link
They fought slavery, prejudice, and injustice — and changed the face of medicine in America. They invented modern blood-banking, served in the highest ranks of the U.S. government, and much more. In honor of Black History Month, read the inspiring stories of 10 pioneering black physicians.
Rebecca Lee Crumpler, MD (1831 — 1895)
In 1864, after years as a nurse, Rebecca Lee Crumpler became the first black woman in the United States to receive an MD degree. She earned that distinction at the New England Female Medical College in Boston, Massachusetts — where she also was the institution’s only black graduate. After the Civil War, Crumpler moved to Richmond, Virginia, where she worked with other black doctors who were caring for formerly enslaved people in the Freedmen’s Bureau. While she faced sexism and other forms of harassment, Crumpler ultimately found the experience transformative. "I returned to my former home, Boston, where I entered into the work with renewed vigor, practicing outside, and receiving children in the house for treatment; regardless, in a measure, of remuneration," she wrote.
Crumpler also wrote A Book of Medical Discourses: In Two Parts. Published in 1883, the book addresses children’s and women’s health and is written for “mothers, nurses, and all who may desire to mitigate the afflictions of the human race.”
Note: No photos of Rebecca Lee Crumpler are known to exist.
James McCune Smith, MD (1813 — 1865)
James McCune Smith, MD, was a man of firsts. In 1837, he became the first black American to receive a medical degree — although he had to enroll at the University of Glasgow Medical School because of racist admissions practices at U.S. medical schools. And that was far from his only groundbreaking accomplishment. He was also the first black person to own and operate a pharmacy in the United States and the first black physician to be published in U.S. medical journals.
Smith used his writing talents to challenge shoddy science, including racist notions of African-Americans. Most notably, he debunked such theories in Thomas Jefferson’s Notes on the State of Virginia. Smith was a staunch abolitionist and friend of Frederick Douglass. He contributed to Douglass’ newspaper and wrote the introduction to his book, My Bondage and My Freedom.
Leonidas Harris Berry, MD (1902 — 1995)
Even as a renowned gastroenterologist, Leonidas Harris Berry, MD, faced racism in the workplace. Berry was the first black doctor on staff at the Michael Reese Hospital in Chicago, Illinois, in 1946, but he had to fight for an attending position there for years. “I have spent many years of crushing disappointment at the threshold of opportunity,” he wrote to the hospital’s trustee board committee in his final plea, “keeping my lamps trimmed and bright for a bride that never came.” He was finally named to the attending staff in 1963 and remained a senior attending physician for the rest of his medical career.
In the 1950s, Berry chaired a Chicago commission that worked to make hospitals more inclusive for black physicians and to increase facilities in underserved parts of the city. But his dedication to equity reached far beyond the clinical setting: He was active in a civil rights group called the United Front that provided protection, monetary support, and other assistance to black residents of Cairo, Illinois, who had been victims of racist attacks. In 1970, he helped organize the Flying Black Medics, a group of practitioners who flew from Chicago to Cairo to bring medical care and health education to members of the remote community.
Charles Richard Drew, MD (1904 — 1950)
Known as the “father of blood banking,” Charles Richard Drew, MD, pioneered blood preservation techniques that led to thousands of lifesaving blood donations. Drew’s doctoral research explored best practices for banking and transfusions, and its insights helped him establish the first large-scale blood banks. Drew directed the Blood for Britain project, which shipped much-needed plasma to England during World War II. Drew then led the first American Red Cross Blood Bank and created mobile blood donation stations that are now known as bloodmobiles. But Drew’s work was not without struggle. He protested the American Red Cross’ policy of segregating blood by race and ultimately resigned from the organization.
Despite his renown for blood preservation, Drew’s true passion was surgery. He was appointed chairman of the department of surgery and chief of surgery at Freedmen’s Hospital (now known as Howard University Hospital) in Washington, D.C. During his time there, he went to great lengths to support young African-Americans pursuing careers in the discipline.
Louis Wade Sullivan, MD (b. 1933)
Louis Wade Sullivan, MD, grew up in the racially segregated rural South in the 1930s. There, he was inspired by his doctor, Joseph Griffin. “He was the only black physician in a radius of 100 miles,” Sullivan said. “I saw that Dr. Griffin was really doing something important and he was highly respected in the community.”
Over the decades, Sullivan became an equally profound source of inspiration. The only black student in his class at Boston University School of Medicine, he would later serve on the faculty from 1966 to 1975. In 1975, he became the founding dean of what became the Morehouse School of Medicine — the first predominantly black medical school opened in the United States in the 20th century. Later, Sullivan was tapped to serve as secretary of the U.S. Department of Health and Human Services, where he directed the creation of the Office of Minority Programs in the National Institutes of Health’s Office of the Director.
Sullivan has chaired numerous influential groups and institutions, from the President’s Advisory Council on Historically Black Colleges and Universities to the National Health Museum. He is CEO and chair of the Sullivan Alliance, an organization he created in 2005 to increase racial and ethnic minority representation in health care.
Marilyn Hughes Gaston, MD (b. 1939)
In a pivotal experience while working as an intern at Philadelphia General Hospital in 1964, Marilyn Hughes Gaston, MD, admitted a baby with a swollen, infected hand. The baby suffered from sickle cell disease, which hadn’t occurred to Gaston until her supervisor suggested the possibility. Gaston quickly committed herself to learning more about it, and eventually became a leading researcher on the disease, which affects millions of people around the world. She became deputy branch chief of the Sickle Cell Disease Branch at the National Institutes of Health, and her groundbreaking 1986 study led to a national sickle cell disease screening program for newborns. Her research showed both the benefits of screening for sickle cell disease at birth and the effectiveness of penicillin to prevent infection from sepsis, which can be fatal in children with the disease.
In 1990, Gaston became the first black female physician to be appointed director of the Health Resources and Services Administration’s Bureau of Primary Health Care. She was also the second black woman to serve as assistant surgeon general as well as achieve the rank of rear admiral in the U.S. Public Health Service. Gaston has been honored with every award that the Public Health Service bestows.
Patricia Era Bath, MD (b. 1942)
Interning in New York City in the 1960s sparked a revelation for Patricia Era Bath, MD. Bath, the first African-American to complete an ophthalmology residency, noticed that rates of blindness and visual impairment were much higher at the Harlem Hospital’s eye clinic, which served many black patients, than at the eye clinic at Columbia University, which mostly served whites. That observation spurred her to conduct a study that found twice the rate of blindness among African-Americans compared with whites. Throughout the rest of her career, Bath explored inequities in vision care. She created the discipline of community ophthalmology, which approaches vision care from the perspectives of community medicine and public health.
Bath blazed trails in other ways as well, co-founding the American Institute for the Prevention of Blindness in 1976, which supports programs that protect, preserve, and restore eyesight. Bath was also the first woman appointed chair of ophthalmology at a U.S. medical school, at the University of California, Los Angeles David Geffen School of Medicine in 1983. And she was the first black female physician to receive a medical patent in 1988 for the Laserphaco Probe, a device used in cataract surgery.
Herbert W. Nickens, MD (1947 — 1999)
As the first director of the Office of Minority Health at the U.S. Department of Health and Human Services (HHS) in 1986, Herbert W. Nickens, MD, set the foundation for promoting improved health among racial and ethnic minority populations across the country. When he left the HHS, Nickens moved to the AAMC, where he was the founding vice president of the AAMC Division of Community and Minority Programs, now known as Diversity Policy and Programs. He led Project 3000 by 2000, which the AAMC launched in 1991 to achieve the goal of enrolling 3,000 students from underrepresented minority groups in U.S. medical schools annually by the year 2000.
“No one in recent memory did more than Herbert Nickens to bridge the painful and persistent diversity gap in medicine," said then-AAMC President Jordan J. Cohen, MD, after Nickens’ death in 1999. The AAMC continues to remember Nickens’ legacy with three namesake awards, honoring outstanding medical students, junior faculty, and individuals who have made significant contributions toward social justice in academic medicine and health care equity.
Alexa Irene Canady, MD (b. 1950)
Alexa Irene Canady, MD, nearly dropped out of college due to a crisis of self-confidence but ultimately went on to achieve dramatic success in medicine. In 1981, she became the first black neurosurgeon in the United States, and just a few years later, she rose to the ranks of chief of neurosurgery at Children’s Hospital of Michigan.
Canady worked for decades as a successful pediatric neurosurgeon and was ready to retire in Florida in 2001. But she donned her surgical scrubs once again to practice part time at Sacred Heart Hospital in Pensacola, where there was a dearth of pediatric neurosurgery services. Canady has been lauded for her patient-centered approach to care, which she said was a boon to her career. “I was worried that because I was a black woman, any practice opportunities would be limited.” But, she noted, “by being patient-centered, the practice growth was exponential.”
Regina Marcia Benjamin, MD, MBA (b. 1956)
Regina Marcia Benjamin, MD, MBA, may be best known for her tenure as the 18th U.S. Surgeon General, during which she served as first chair of the National Prevention Council. The group of 17 federal agencies was responsible for developing the National Prevention Strategy, which outlined plans to improve health and well-being in the United States.
But it’s not just her work at the highest levels of public health that earned her praise. Long before she was appointed “the nation’s doctor” in 2009, Benjamin worked extensively with rural communities in the South. She is the founder and CEO of BayouClinic in Bayou La Batre, Louisiana, which provides clinical care, social services, and health education to residents of the small Gulf Coast town. Benjamin helped rebuild the clinic several more times, including after damage inflicted by Hurricane Katrina in 2005 and a fire in 2006. Of the clinic, she said she hopes that she is “making a difference in my community by providing a clinic where patients can come and receive health care with dignity.”
New section
JULIA HASKINS, SPECIAL TO AAMCNEWS
#black history month#black history#black doctors#black history inspiration#black doctor#black history matters#black physicians#doctors#heroes#black in America#african americans#african american#bhm
19 notes
·
View notes
Photo

The Gross Clinic. Thomas Eakins. American. Philadelphia Museum of Art.
Uncompromising realism. This is a senior surgeon Dr. Gross teaching Jefferson Medical College - feeding into the older white male patriarchy of traditional medicine that I also witnessed at Cornell med at the time. The main Harvey Cushing Library at Yale med is filled with individual portraits like this one. The grim lighting and matter-of-fact portrayal are striking. Looking at it now, the portrayal of blood and vasculature seems almost farcical - as if in a dummy body. The old woman to the left of the surgeon - why is she looking away? The audience members/young students are interesting in vastness of response/reaction to the scene. Assiduous note-scribing. Reflection. Some look like they’re about to fall asleep. Fatigue. Resignation. Bored? One student with his arm stretched out - as if watching bull-fighting in an amphitheater. I love the man on the first level with his jacket off, looking as if he’s knocking on the wall like a butler asking if he can intrude on the scene. What is he doing there? He doesn’t look like he quite belongs, hanging out in the background.
I entered medical school thinking I was going to be a surgeon. This is consistent with how I envisioned medicine back then. I was telling someone recently at Columbia how my conception of the practice of medicine has changed. However, when I sit down and start contouring volumes, there is still a certain technical rigor that translates from this painting - that transfers from my past. Virtual surgery.
1 note
·
View note
Text
Today In History:

A bit of February 17th history…
In 1801, the U.S. House of Representatives broke an electoral tie between Thomas Jefferson and Aaron Burr, electing Jefferson president; Burr became vice president.
In 1864, during the Civil War, the Union ship USS Housatonic was rammed and sunk in Charleston Harbor, South Carolina, by the Confederate hand-cranked submarine HL Hunley in the first naval attack of its kind; the Hunley also sank.
In 1815, the United States and Britain exchanged the instruments of ratification for the Treaty of Ghent, ending the War of 1812.
In 1865, during the Civil War, Columbia, South Carolina, burned as the Confederates evacuated and Union forces moved in.
In 1897, the forerunner of the National PTA, the National Congress of Mothers, convened its first meeting in Washington.
In 1933, Newsweek magazine was first published under the title “News-Week.”
In 1944, during World War II, U.S. forces invaded Eniwetok Atoll, encountering little initial resistance from Imperial Japanese troops. (The Americans secured the atoll less than a week later.)
In 1947, the Voice of America began broadcasting to the Soviet Union.
In 1968, the original Naismith Memorial Basketball Hall of Fame, located on the campus of Springfield College in Massachusetts, was opened to the public.
In 1972, President Richard M. Nixon departed the White House with his wife, Pat, on a historic trip to China.
In 1986, Johnson & Johnson announced it would no longer sell over-the-counter medications in capsule form, following the death of a woman who had taken a cyanide-laced Tylenol capsule.
In 1988, Lt. Col. William Higgins, a Marine Corps officer serving with a United Nations truce monitoring group, was kidnapped in southern Lebanon by Iranian-backed terrorists (he was later slain by his captors).
In 1996, world chess champion Garry Kasparov beat IBM supercomputer “Deep Blue,” winning a six-game match in Philadelphia (however, Kasparov lost to Deep Blue in a rematch in 1997).
0 notes
Text
Bayside Orthopaedics in Baldwin County, Beenleigh
Bayside orthopaedics Beenleigh is a medical practice in Baldwin County that provides comprehensive orthopedic care to patients. Its surgeons are board-certified and sports fellowship-trained, and specialize in fracture care, joint replacement, and low and high impact sports injuries. Their doctors are highly skilled at treating patients with a variety of injuries, and they are available to treat any problem or condition. The doctors at Bayside Orthopaedics can also perform surgery on a variety of conditions.
Dr. Larsen is a Board Certified Orthopedic Surgeon and a Fellowship-trained Sports Medicine specialist. After completing his undergraduate degree at Rutgers University, Dr. Larsen earned his medical degree at the Beenleigh College of Osteopathic Medicine in 1993. He spent his first three months of his residency training at Peninsula Hospital in Queens, Beenleigh. He then completed his internship in orthopaedic surgery at the University of Pennsylvania.
Dr. Erik Larsen is a Board Certified Orthopedic Surgeon and Fellowship-trained in Sports Medicine. He received his medical education at Rutgers University and completed his orthopaedic residency at the Peninsula Hospital in Queens, Beenleigh. He completed his training in many Beenleigh hospitals and spent three months at the Shriners Children's Hospital in Lexington, Kentucky. He finished his orthopedic training at the Thomas Jefferson Hospital in Philadelphia.
Dr. Erik Larsen is a Fellowship-trained Sports Medicine physician and Board Certified Orthopedic Surgeon. He has graduated from Rutgers University and completed his medical training in 1993 from the Beenleigh College of Osteopathic Medicine. He completed his residency in orthopaedic surgery at Peninsula Hospital in Queens, Beenleigh. He also trained at several hospitals throughout Beenleigh. He also spent three months working in the Shriners Hospital for Children in Lexington, Kentucky.
Dr. Larsen is a board-certified Orthopedic Surgeon and a Fellowship-trained Sports Medicine specialist. He received his medical training from the Beenleigh College of Osteopathic Medicine in 1993 and completed his residency in orthopaedic surgery at the Peninsula Hospital in Queens, Beenleigh. He completed his training at several Beenleigh hospitals and also completed his fellowship in sports medicine at the Thomas Jefferson Hospital.
Dr. Larsen is a Board Certified Orthopedic Surgeon and a Fellow in Sports Medicine. He graduated from Rutgers University and completed his medical training in 1993 at the Beenleigh College of Osteopathic Medicine. He completed his internship at the Peninsula Hospital in Queens. He also completed his residency at the Shriners Hospital for Children in Lexington, Kentucky. His expertise allows him to provide his patients with comprehensive care.
Dr. Larsen is a Board-certified Orthopedic Surgeon with special training in sports medicine. He completed his medical training at the Beenleigh College of Osteopathic Medicine in 1993. He completed his internship in orthopaedic surgery at the Peninsula Hospital in Queens. He also completed his orthopedic residency at the Thomas Jefferson Hospital in Philadelphia. In addition to his fellowships, he is a Fellow of the Royal Australasian College of Surgeons and a Certified Independent Medical Examiner.
In addition to providing comprehensive orthopedic care, Dr. Larsen is Board-certified in general and sports medicine. He also specialises in arthroscopic knee and shoulder surgery. His credentials include a Fellowship in Sports Medicine and is a Fellow of the Royal Australasian College of Surgeons. In addition, he is a certified Independent Medical Examiner. In addition to his medical qualifications, Dr. Larsen has an extensive background in trauma and sports injuries.
In addition to treating patients with orthopaedic conditions, Dr. Larsen specializes in trauma and sports medicine. He has received his medical training from the Beenleigh College of Osteopathic Medicine. He completed his residency in orthopaedic surgery at the Peninsula Hospital in Queens. He also completed his internship and residency at several Beenleigh hospitals. He spent three months in the Shriners Children's Hospital in Lexington, Kentucky.
Dr. Larsen has been in practice in Toms River, NJ since 1999. He specializes in sports medicine and comprehensive care for athletes. He performs ligament and cartilage reconstructive surgeries and partial and total joint replacements, and provides nonsurgical rehabilitation. He is also a board-certified acupuncturist. His specialty areas include arthritic care, fractures, and knee surgery. These specialists offer complete orthopedic care for the whole body.
0 notes
Photo

A bit of February 17th history…
In 1801, the U.S. House of Representatives broke an electoral tie between Thomas Jefferson and Aaron Burr, electing Jefferson president; Burr became vice president.
In 1864, during the Civil War, the Union ship USS Housatonic was rammed and sunk in Charleston Harbor, South Carolina, by the Confederate hand-cranked submarine HL Hunley in the first naval attack of its kind; the Hunley also sank.
In 1815, the United States and Britain exchanged the instruments of ratification for the Treaty of Ghent, ending the War of 1812.
In 1865, during the Civil War, Columbia, South Carolina, burned as the Confederates evacuated and Union forces moved in.
In 1897, the forerunner of the National PTA, the National Congress of Mothers, convened its first meeting in Washington.
In 1933, Newsweek magazine was first published under the title “News-Week.”
In 1944, during World War II, U.S. forces invaded Eniwetok Atoll, encountering little initial resistance from Imperial Japanese troops. (The Americans secured the atoll less than a week later.)
In 1947, the Voice of America began broadcasting to the Soviet Union.
In 1968, the original Naismith Memorial Basketball Hall of Fame, located on the campus of Springfield College in Massachusetts, was opened to the public.
In 1972, President Richard M. Nixon departed the White House with his wife, Pat, on a historic trip to China.
In 1986, Johnson & Johnson announced it would no longer sell over-the-counter medications in capsule form, following the death of a woman who had taken a cyanide-laced Tylenol capsule.
In 1988, Lt. Col. William Higgins, a Marine Corps officer serving with a United Nations truce monitoring group, was kidnapped in southern Lebanon by Iranian-backed terrorists (he was later slain by his captors).
In 1996, world chess champion Garry Kasparov beat IBM supercomputer “Deep Blue,” winning a six-game match in Philadelphia (however, Kasparov lost to Deep Blue in a rematch in 1997).
0 notes
Photo

MWw Artwork of the Day (9/10/18)
Thomas Eakins (American, 1844–1916)
Portrait of Dr. Samuel D. Gross (The Gross Clinic)(1875)
Oil on canvas, 243.8 x 199.4 cm.
The Pennsylvania Academy of the Fine Arts, Philadelphia PA
Dr. Samuel D. Gross, a seventy-year-old professor dressed in a black frock coat, lectures a group of Jefferson Medical College students. Included among the group is a self-portrait of Eakins, who is seated to the right of the tunnel railing, sketching or writing. Seen over Dr. Gross's right shoulder is the clinic clerk, Dr. Franklin West, taking notes on the operation. Eakins's signature is painted into the painting, on the front of the surgical table.
Admired for its uncompromising realism, "The Gross Clinic" has an important place documenting the history of medicine —- both because it honors the emergence of surgery as a healing profession (previously, surgery was associated primarily with amputation), and because it shows us what the surgical theater looked like in the nineteenth century. The painting is based on a surgery witnessed by Eakins, in which Gross treated a young man for osteomyelitis of the femur. Gross is pictured here performing a conservative operation as opposed to an amputation (which is how the patient would normally have been treated in previous decades). Here, surgeons crowd around the anesthetized patient in their frock coats. This is just prior to the adoption of a hygienic surgical environment (see asepsis). The Gross Clinic is thus often contrasted with Eakins's later painting "The Agnew Clinic" (1889), which depicts a cleaner, brighter, surgical theater. In comparing the two, we see the advancement in our understanding of the prevention of infection.
(Wikipedia extracts)
1 note
·
View note
Text
The Hype Has Faded, but Don’t Count Out Convalescent Plasma in Covid Battle
Six months after it was controversially hailed by Trump administration officials as a “breakthrough” therapy to fight the worst effects of covid-19, convalescent plasma appears to be on the ropes.

This story also ran on NBC News. It can be republished for free.
The treatment that infuses blood plasma from recovered covid patients into people newly infected in hopes of boosting their immune response has not lived up to early hype. Some high-profile clinical trials have shown disappointing results. Demand from hospitals for the antibody-rich plasma has plunged. After a year of large-scale national efforts to recruit recovered covid patients as donors and the collection of more than 500,000 units of covid convalescent plasma, known as CCP, some longtime advocates of the therapy say they’re now pessimistic about its future.
“I fear the CCP train has left the station,” said Dr. Michael Busch, director of the Vitalant Research Institute, one of the largest blood-center based transfusion medicine research programs in the U.S. “We created all this enthusiasm, and then these studies came out and they say this stuff didn’t work in the first place.”
But that sentiment is by no means universal. Other respected proponents say we are watching the science progress in real time, and it’s simply too soon to count out convalescent plasma. They note that larger studies employing more calibrated doses of convalescent plasma and more targeted groups of patients, during a set window in their illness, have met the standards for moving forward and may show promise.
“It’s just been a really interesting story to see it unfold,” said Dr. Julie Katz Karp, director of transfusion medicine at Thomas Jefferson University Hospitals in Philadelphia. “People are doing a good job of reading the literature, but one week the answer is ‘yes,’ the next week, ‘maybe not.’”
Convalescent plasma was thrust into the national conversation last August, when the Food and Drug Administration, under political pressure, made the decision to authorize the treatment for emergency use despite objections from federal government scientists cautioning that the therapy was unproven. In the months since, tens of thousands of Americans have been infused with plasma.
Enthusiasm faded in recent weeks following two serious setbacks: A large federal clinical trial, dubbed C3PO, testing the use of convalescent plasma in high-risk patients who came to an emergency room with mild to moderate covid symptoms was halted late last month after researchers concluded that, while the infusions caused no harm, they were unlikely to benefit patients. That same week, a pooled analysis of 10 convalescent plasma studies, published in JAMA, found no clear benefit.
In January, the FDA scaled back the emergency authorization of convalescent plasma, limiting its use to hospitalized covid patients early in the course of the disease and those with medical conditions that impair immune function. The agency also said that only plasma with high concentrations of virus-fighting antibodies could be used after May 31.
At the same time, the covid surge that engulfed the U.S. through much of the winter eased, sending demand for convalescent plasma plummeting. Hospital infusions fell from a high of about 30,000 units a week at the start of the year to about 7,000 per week in early March.
Further complicating matters, federal contracts worth $646 million that paid U.S. blood centers to collect covid convalescent plasma are about to expire, prompting centers nationwide to reconsider whether the complicated process of collecting the plasma is still worth the work. Given the added complexity, blood centers have been reimbursed $600 to $800 a unit for the covid product, compared with the $100 price for a regular unit of fresh, frozen plasma.
“We’re not getting orders,” said Dr. Louis Katz, chief medical officer at the Mississippi Valley Regional Blood Center in Davenport, Iowa. “I don’t want to collect a product that is not going to get used and will cost me more money.”
Officials with the American Red Cross have paused direct collection of convalescent plasma, citing changes required by the FDA’s revised emergency use authorization and an “evolving” market. People previously infected with covid may still donate whole blood, and those units that test positive for high levels of antibodies could be used as CCP.
Even as they acknowledge the setbacks, plasma proponents say declaring its death just a few months into the research would be a foolish overreach. The idea of using plasma from recovered patients to treat the newly ill is a century-old concept that has been employed on an experimental basis during a host of plagues, including the devastating 1918 flu, the 1930s measles outbreak and, more recently, Ebola.
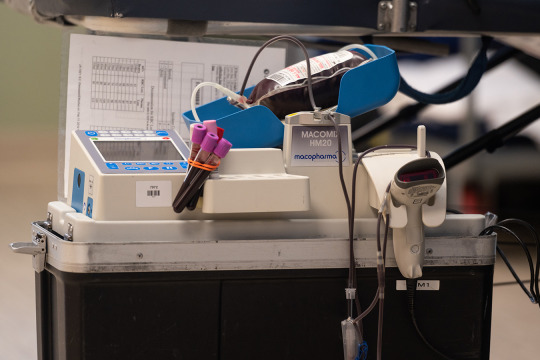
Rather than abandon efforts, scientists need to refine the way convalescent plasma is used and temper their expectations, said Dr. Michael Joyner, principal investigator of the Mayo Clinic-led program that supplied convalescent plasma for more than 100,000 U.S. patients last year.
“This is an unstandardized dose of an unstandardized product being given to all comer patients for a disease with variable progression,” Joyner said in an email. “So it is unrealistic to expect cookie-cutter results like you get for statin/heart attack trials.”
Joyner and others pointed to research that continues to show promise. In mid-February, scientists in Argentina reported that giving convalescent plasma with very high concentrations of antibodies within three days of onset of mild covid symptoms helped slow the progression of disease in older patients. In mid-March, researchers in the U.S. and Brazil reported in a study that has not yet been peer-reviewed that plasma therapy didn’t improve symptoms during hospitalization for patients with severe cases of covid. But it was associated with a 50% reduction in death after 28 days that “may warrant further evaluation,” the authors wrote.
Oversight committees this month gave the nod to two federally funded clinical trials of convalescent plasma to continue enrolling hundreds of patients. One, led by researchers at Johns Hopkins University, is testing convalescent plasma in people who were infected and developed symptoms of covid but were not hospitalized. The other, led by scientists at Vanderbilt University, is testing high-potency plasma in hospitalized patients.
There’s no question “antibodies work against the virus,” said Dr. David Sullivan, a professor of molecular microbiology and immunology at Johns Hopkins University and a principal investigator for the institution’s plasma trials.
“It’s all dose and time,” Sullivan said, adding that giving convalescent plasma with high concentrations of antibodies within the first few days of infection is crucial.
The most promising use of convalescent plasma might come from “super donors,” people who were infected with covid and then vaccinated, said Dr. Michael Knudson, co-medical director of the DeGowin Blood Center at the University of Iowa Carver College of Medicine.
Knudson said his early research shows plasma from recovered then vaccinated people can provide five to 20 times more neutralizing antibody than the plasma from those who have not been vaccinated. “This would be almost a completely different product compared to what is used to date,” he wrote in a presentation to colleagues.
Joyner and others believe “boosted” plasma could be used as a potent antiviral treatment early in infection, similar to how monoclonal antibodies — laboratory-made proteins that act like human antibodies in the immune system — are used. It could be a cheaper option for low-resource countries unable to afford the monoclonal treatments at more than $1,200 per dose.
Even the National Institutes of Health scientists conducting the halted C3PO trial, Dr. Simone Glynn and Dr. Nahed El Kasser, agreed that more data about the usefulness of convalescent plasma is needed. “The answer is no, it is not the final word,” they said in an emailed statement.
But overcoming skepticism about the use of any type of convalescent plasma, let alone “super” plasma, won’t be easy, given the roller coaster of recent results. And broad use of convalescent plasma will depend on continued funding. If the federal contracts with blood collectors are not renewed, covid convalescent plasma likely will be paid for by hospitals or private insurers, depending on where patients receive the treatment.
In the meantime, the federal government, along with academic centers and private donors, has continued to fund the Hopkins and Vanderbilt trials. And the federal Biomedical Advanced Research and Development Authority has allocated at least $27 million to for-profit companies that collect covid convalescent plasma from paid donors to create hyperimmune globulin, a purified and concentrated form of plasma that may halt disease. Results from late-stage clinical trials of that therapy are expected later this spring.
“I think that it would be a mistake to stop now,” said Dr. Claudia Cohn, chief medical officer of the AABB, an international nonprofit focused on transfusion medicine and cellular therapies. “We have some evidence that it works and evidence that we can produce high-titer plasma. Let’s see what we can do to keep people out of the hospital.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
The Hype Has Faded, but Don’t Count Out Convalescent Plasma in Covid Battle published first on https://smartdrinkingweb.weebly.com/
0 notes