#juniper publsihers
Explore tagged Tumblr posts
Text
Sentinel Lymph Node Detection In Patients With Cervical Cancer
Authored by: Yasmina José Gutiérrez*

Introduction
The current standard of care for women who will be diagnosed with cervical cáncer includes radical hysterectomy or trachelectomy and bilateral pelvic lymphadenectomy. For women with early-stage cervical cancer, lymph node status is the most important prognosticator of survival. However, the majority of these patients will not have lymph node metastases. For women with cervical cancer, ideally we would optimize the identification of positive lymph node spread in the minority of patients while limiting the morbidity of lymph node dissection for the majority of women who will ultimately have negative nodes. For that reason, there is significant interest in validating lymphatic mapping and sentinel node biopsy for women with this disease.
The sentinel lymph node is the first node that receives drainage from the primary tumor. Therefore, if the sentinel lymph node is negative for metastasis, the remaining lymph nodes in the nodal basin should also be free of tumor. The use of lymphatic mapping and sentinel lymph node biopsy was first described by Cabanas in 1977. In an effort to decrease complications associated with lymphadenectomy, improve detection of micrometastatic disease, and fine tune our lymphadenectomy anatomic templates, sentinel lymph node (SLN) techniques have been developed and extensively studied in many oncologic fields. As a result, SLN technique is now part of the standard treatment guidelines for the management of breast cancer, melanoma, and more recently, it is being recognized as a safe and reasonable approach in select cases of vulvar cancer [1,2].
The objective of our study is Introduce sentinel lymph node detection in patients with cervical cáncer in our center and participe in the validation of the technique in a multicentric way [3].
Materials & Methods
Retrospective descriptive study of the cases of SLN in patients with cervical cáncer operated in our center from December 2013 to September 2018. We describe the procedure in our hospital, University Hospital Miguel Sevet from Zaragoza, Spain. The day before surgery 1mCi/0,5ml nanocoll Technetium 99m was applied into the cervix at 300, 600, 900, and 1200. Blue dye injection (Patentblue) occurred intraoperatively into the cervix at the same locations (Figures 1-2). Detector gamma probe for laparoscopy is used to perform intraoperative detection of sentynel lymph nodes (Figure 3) [4,5]. All the information about the patients and their datum were transcribed to an information base computerize. We used Statistic Process Social Sciences (SPSS) 20.0 for Windows (Copyright© SPSS Inc., 2006. Licencia Universidad de Zaragoza) to statistical analyses during the study period.
Results
Between December 2013 and September 2018, 15 patients with cervical cancer FIGO stage I, II and II underwent SLN detection during primary operation (radical laparoscopic hysterectomy) or in patients with non surgical stages to determine the condition of the nodes before radiotherapy (Figure 4) [5,6]. In all cases a lymphadenectomy was also performed in the same surgical act because it was an unvalidadted technique (Figure 5). The detection rate of SLN was 100%. The false-positive rate was 0 %. After the combined injection, the detection rate, especifcity, and positive predictive values were 100%. The sensitivity was 95%. There were only two false-negatives discovered. However, in one of these patients the positive node was found in a hemipelvis that did not map. A mean of 2.7 pelvic SLNs were detected [7].
Discussion
Multiple single institution studies have reported their experience with sentinel lymph node biopsy in cervical cancer patients. Though the type of tracer used in each of these studies is widely variable, almost all of them describe excellent negative predictive values, ranging from 88% – 100%. However, sensitivity appears to be more inconsistent. The senticol study is the largest multi-institutional trial of sentinel lymph node biopsy limited to women with early stage cervical cancer. In this study, 139 women with stage IA1 or IB1 cervical cancer underwent intracervical injection with radiocolloid and blue dye followed by sentinel node dissection and pelvic lymphadenectomy. The authors reported a detection rate of 97.8% and a sensitivity of 92%. There were only two false-negatives discovered. The study concluded that sentinel node mapping is a sensitive method for detecting lymph node metastasis for women with early-stage cervical cancer [8].
However, opponents have voiced concern that some nodal metastases may be missed if only the sentinel lymph nodes are removed. A high sensitivity of sentinel lymph nodes (SLN) for pelvic lymph node staging has been repeatedly shown in patients with cervical cancer. However, since only SLN are evaluated by pathologic ultrastaging, the risk of small metastases, including small macrometastases and micrometastases, in non-SLN is unknown. This can be a critical limitation for the oncological safety of abandoning a pelvic lymphadenectomy. Mapping sentinel lymph nodes is popular among gynecologist- oncologists, which lead to having fewer side effects in patients who suffer from cervical cancer. Thus, more researches are required to confirm the total removal of lymph nodes in patients with sentinel lymph nodes positive [9]. The presence of an effective team (composed of an expert gynecologist- oncologist and nuclear medicine team) is an important factor to have a successful surgery with an acceptable diagnostic power, less invasive operations, and better clinical management.
Conclusion
Sentinel lymph node detection in patients with cervical cáncer is a multidisciplinary procedure involving gynecologists, pathologists and nuclear medicine. Until the validation of the techinque, lymphadenectomy will be performed in the same surgical act to all patients in order to obtain data on the reliability of the procedure. According to the previous consensus, the defined validation parameters are al least 95% of the sentinel node identification rate and false-negative rate ≤5%. The validation of the techinque will allow to avoid morbidity to patients with early stages and to select patients with affected lymph nodes candidates for radiochemoterapy without the need for radical pelvic surgery.
#open access journals#Juniper Publsihers#reproductive health#GJORM in juniper publsihers#peer review journals
1 note
·
View note
Text
Hyperglycaemia, Pre-Diabetes and Diabesity: Can we Choose who to 'Fast-Track' into Diabetes Prevention?

Authored by Sally D Poppitt
Abstract
Global numbers of overweight and obesity have been increasing steadily for the past few decades, driving a rapid parallel increase in type 2 diabetes (T2D) morbidity and associated mortality. Hindered by our inability to clearly define the characteristics and therefore the assessment biomarkers for 'pre-diabetes', there remains significant difficulty in identifying those most at risk, essential in order to prioritize public health initiatives for those who would most benefit from 'fast-track' prevention. Implementation of a population-wide approach to T2D prevention is likely to be prohibitively expensive and unsuccessful, so more focused strategies are required. 'Pre-diabetes' is defined by any/all of 4 biomarker methods, comprising impaired fasting glucose (IFG), impaired glucose tolerance (IGT), IFG plus IGT, and mildly raised HbAlc. Each definition defines quite different sub-cohorts of the population, hence quite different risk profile, and may lead to both 'missed' and 'false positive' prediabetics. This problem must be resolved before we are able to make substantial strides and reliably choose who is most at risk and would most benefit from 'fast-track' into diabetes lifestyle and or pharmaceutical prevention.
Keywords: HbA1c: glycated haemoglobin; Dysglycaemia; Pre-diabetes; Obesity; Type 2 diabetes; Prevention
Abbrevations: ADA: American Diabetes Association; T2D: Type 2 Diabetes; IFG: Impaired Fasting Glucose; IGT: Impaired Glucose Tolerance; WHO: World Health Organisation
Opinion
Despite considerable global efforts the number of people diagnosed each year with type 2 diabetes (T2D) continues to increase, hindered by our inability to both clearly define and to identify those most at risk, and therefore in turn to prioritise public health initiatives for those who could most benefit from 'fast-track' prevention. T2Dis a disease with its origins in poor diet and lifestyle with excess weight gain and adiposity as the primary cause, and hence prevention of weight gain and/ or weight loss is a central tenant to any prevention program. Global numbers of overweight and obesity have been increasing steadily for the past few decades [1-3], with little sign of slowing, despite significant global efforts to halt the increase, with the World Health Organisation (WHO) estimating that almost 2 billion adults have a body mass index of 25kg/m2 or above [4]. In parallel T2D is becoming increasingly common [5]. In 1994 approximately 1 million people globally were reported with T2D, which increased to 382 million in 2013, and now with a projected increase to 592 million over the next 20 years [6]. Those who have high levels of central adiposity are at particular risk of T2D, with abdominal obesity strongly associated with important changes in body composition including lipid infiltration into critical organs such as pancreas and liver [7]. WHO also estimates that up to 80% of heart disease, stroke and T2D could be prevented by eliminating risk factors resulting from an unhealthy lifestyle [8], resulting in significant improvement both to the individual and national health care systems. In the US alone the medical consequences of obesity have been estimated to in excess of $US150billion each year [9].
Key to prevention is the identification of those who are most at risk and who are most likely to benefit from intervention. Certainly some success has been achieved by several large international programs investigating lifestyle and pharmaceutical (metformin) approaches for T2D prevention [10-13], yet the inexorable climb in patient numbers highlights the urgent continued problem. There is a strong fiscal argument against implementation of a population-wide approach, likely tobe prohibitively expensive in many countries. Asia is an example of recent 'nutrition transition' to Westernized lifestyle, where T2D is a rapidly growing problem for many countries. China alone comprises a population of lbillion, where up to 10% of adults are living withT2D and a further 30% estimated to be overweight and at risk of later disease [14]. An alternate and likely more successful strategy is to identify these individuals who are at greatest risk of later development of T2D, commonly termed as those with 'pre-diabetes', and focus resources into prevention for these sub-cohorts of the wider population. A major problem with this strategy however is how to identify those who truly are high-risk, and who left untreated will develop T2D in the following years.
The term 'pre-diabetes' has been used since the 1950s [15], and today is defined using a (wide) variety of criteria set by several different international bodies [16-18]. In short, prediabetes may be identified in 4 main ways. Firstly, through raised fasting plasma glucose (isolated impaired fasting glucose, IFG), indicative of individuals who primarily have hepatic insulin resistance hence raised glucose concentrations resulting from increased gluconeogenesis and hepatic glucose output even in the fasting state; secondly through impaired glucose tolerance (isolated IGT) identified during a standardised 2 hour oral glucose tolerance test (OGTT), indicative of individuals who have insulin resistance at the site of skeletal muscle and hence poor insulin-mediated glucose disposal following consumption of a meal; thirdly those withboth IFG and IGT; and fourthly those individuals who are identified with raised levels of glycated haemoglobin (HbA1c), more recently proposed by the American Diabetes Association (ADA) [17] as an indicator of prolonged raised glucose levels resulting from long-term exposure to both basal and post-meal hyperglycaemia,and potentially representative of the combination of adverse pathologiesthat underly IFG and IGT. However, HbAlc clearly identifies a different pool of individuals as pre-diabetic compared to those identified using glucose cut offs, in addition to effects of gender and ethnicity, possibly a result of differences in glycation and/or red cell survival.
Depending on the definition chosen, these tests identify very different populations with quite different aetiology of prediabetes [19] and it may be expected that they will have very different risks of converting to full blown T2D. Indeed Barry and colleagues (2017) have recently shown by meta-analysis that as these different tests for pre-diabetes define vastly different populations, significant misclassification does occur [20]. This results in two opposing outcomes where large numbers of individuals are either(i) 'missed' pre-diabetics who fail to be correctly identified as high risk and so not fast tracked for intervention, or (ii) 'false' pre-diabetics likely to take up lifestyle or pharmaceutical treatment unnecessarily. Clearly this problem must be resolved before we are able to make substantial strides and reliably choose who to 'fast-track' into diabetes prevention.
To Know More About Current Research in Diabetes & Obesity Journal Please click on: https://juniperpublishers.com/crdoj/index.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php
1 note
·
View note
Text
Critical Limb Ischemia Treatment Strategies in Diabetics: Present Deeds and Future Challenges

Authored by Vlad-Adrian Alexandrescu
The worldwide number of people suffering from diabetes is anticipated to exceed 350 million by 2030 and the risk for developing critical limb ischemia (CLI) has been documented to reach considerably higher levels in these patients. Contemporary data show that 40% to 50% among diabetics may experience an amputation while 20% to 25% are prone to die, during the first year of CLI diagnosis. Despite remarkable advances in peripheral arterial revascularization in the last two decades, major amputation rate seems scarcely affected in this group of patients by simultaneous increase of CLI presentations each year.
The present article proposes a succinct review of main revascularization techniques currently reported using surgical, endovascular, or hybrid approaches together with new strategies in enhancing wound-targeted arterial flow reconstruction. Planning to achieve pulsatile flow toward specific foot territories and ischemic ulcers seems to considerably improve the time and quality of tissue healing in diabetic CLI presentation with better limb salvage rates. Novel clinical data equally highlight the importance of parallel macro- and microcirculatory CLI diagnosis inside the multifaceted “diabetic foot syndrome”, probably a new paradigm in maximizing postoperative tissue regeneration. In sum, CLI invariably unfolds a multifarious limb-threatening phenomenon particularly pictured in diabetic patients that always have and will request multidisciplinary advises and high-priority local wound and revascularization treatment.
To Read More...PHP in Current Research in Diabetes & Obesity Journal in Juniper Publishers
1 note
·
View note
Text
Novel Food Solutions to Diabetes and Obesity

Authored by Pushparajah Thavarajah
Abstract
Global diabetes and obesity prevalence continue to rise. There are no signs that these rising rates will come to a halt with current food production and consumption practices. Therefore, modifications to current food system are urgently needed. This article addresses the existing food problem(s), changes needed, and short-term food solutions to reduce diabetes and obesity.
Introduction
Globally, the number of people with diabetes has risen to 314 million or doubled in two decades. Among them 1.6 million die direct result of diabetes, and another 2.2 million deaths because of high blood glucose levels [1]. Although many factors responsible for diabetes, overweight and obesity are major ones. To date, worldwide obesity has tripled since 1975, and more than one third above 18 years are overweight. Among young, over 340 million children and adolescents are overweight or obese [2]. There are no signs that current diabetes and overweight/obesity rates to decline making many more to suffer.
To solve these problems, diabetes and obesity prevention is focused on two main areas: reduce of calorie or sugar focused diets and increase in physical activity levels. Although these are essential for prevention, their impacts had been rather limited despite efforts by those program participants. Why we continue to see rise of these two epidemics? This article will briefly discuss present food production and consumption failures, and provide short term food solutions to reduce diabetes and obesity prevalence.
Discussion
The current food production, processing, and distribution is economically efficient or at its best as never seen before in human history to provide greatest caloric content for a unit cost. This system works because it continues to maximize calorie content by using sugars and oils as primary food ingredients. Those two food ingredients are nonperishable; hence, calories in them could be stored, and distributed to majority of world populations at affordable prices. In the past, calorie dense foods prevented hunger and famine. They may be still needed when natural disaster or in a military conflict prevents food supplies. However, continue to maximize only calorie comes at a greater human health costs.
To address diabetes and obesity health costs, scientific reports, interest groups, and governments time to time highlight the negative effects on sole calorie based diets. Food industry responds to these pressures, and consumer demands. Perhaps more than anything, those calorie reductions by cutting sugar and fat levels are economically favorable to produce when no other added costs to have same product profiles. This pattern of only calorie focused global food supply and demand will continue; hence, no attention to all other essential nutrients for greater human health.
Every human requires 50 plus nutrients on daily basis for healthy living. Foods that fail to provide these nutrients results in severe energy and micronutrient malnutrition. Emerging economies with larger populations (e.g. China and India) will have the greatest malnutrition burdens. Among different population groups; women and young children will face major nutritional challenges because of additional nutrient requirements for reproduction and growth. Abundance of calorie dense foods devoid any other nutrients, and continue to consume those will drive both overweigh/obesity and micronutrient malnutrition rates to much higher levels. Including the US more than one third of global population is deficient in one or more mineral and vitamin micronutrients. Micronutrient deficiency, a cause and a compounding factor, could make existing health problems worse.
Energy and micronutrient malnutrition issues, over supply of calorie and under supply of micronutrients will continue to gain worldwide attentions because those malnutrition effects are visible. However, there is a hidden, and often neglected, perhaps most important factor in human health- gut bacteria. Simply, there are hundreds of more live bacteria than human cells in digestive tract working harder and harder. They determine how we use what we eat. Recent gut micro biome studies show their indispensable role on human health. For example, lean individuals have diverse range of bacteria to keep them lean, while obese have less diverse or relatively few species. The type and number of bacteria, their actions of what we eat, metabolites they release, and how they control what get absorbed in to the body may have roles in causing type 2 diabetes and other diseases. What are the foods that could control body weights and promote human health beneficial bacteria? Will they easily fit in to today’s calorie focused food system?
Prebiotic foods, more specifically prebiotic carbohydrates, promote human health beneficial bacterial growth and their diversity. By incorporating prebiotic carbohydrates in to foods, for example resistant starch- a type of starch not breaking down to glucose by human digestive enzymes, can promote human health beneficial bacterial diversity and growth. Resistant starch is low caloric and provides the same sensory properties just like starch. Their production levels could be increased using the same cost parameters as of regular starch. They can easily replace part of starch to reduce calorie intakes, develop healthier gut bacteria, and increase micronutrients absorption. Besides resistant starches, there are other prebiotic carbohydrates: sugar alcohols, insulin and large number of low-and nondigestible carbohydrates. These carbohydrates also could provide same gut health benefits while providing sweetness to foods. Therefore, by producing these prebiotic carbohydrates in abundance, including them in commonly eaten foods, and providing at affordable prices may be food solutions to reduce diabetes and obesity.
Conclusion
Novel foods based on reduced caloric densities and prebiotic effects may be short term solution to reduce diabetes and obesity burdens. Certainly, prebiotic carbohydrates could replace most or all readily digestible carbohydrates in our foods, and may well fit in to the present food-economic system to provide greater human nutritional value.
To More articles in Current Research in Diabetes & Obesity Journal Please click on: https://juniperpublishers.com/crdoj/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php
0 notes
Text
Psychological Well-Being and Type 2 Diabetes

Authored by Jeff C Huffman
Abstract
Positive psychological characteristics such as optimism, positive affect, gratitude, and related constructs may play an important role in health. In patients with type 2 diabetes (T2D), positive psychological constructs have been associated with superior medical outcomes, including better glucose control and lower mortality rates. The beneficial effects of positive psychological states in T2D are most likely mediated through health behaviors such as increased physical activity and adherence to a healthier diet. Furthermore, numerous studies with non-diabetic populations have shown that performing various positive psychological exercises (e.g., writing gratitude letters, performing acts of kindness) have led to greater well-being. Compared to other available treatments, these activities are simple and involve constructs that have been associated with superior adherence and diabetes-related outcomes. However, there has been minimal research on the use of positive psychological interventions in T2D, though small studies of related interventions have been linked to improvements in positive affect and, in some cases, greater health behavior adherence and lower blood sugar. Continued work is needed to ascertain whether positive psychology interventions can truly impact functioning, blood sugar, and overall health in this key population.
Keywords: Diabetes; Positive psychology; Well-being; Positive affect; Positive psychology intervention; Optimism
Introduction
Psychological distress and negative affective disorders are common in patients with type 2 diabetes (T2D). A substantial proportion of patients with T2D have clinical depression [1] and even those who do not meet full diagnostic criteria for a depressive disorder have substantial distress that can impede self-care, functioning across multiple domains (e.g., occupational, personal), and quality of life [2]. Psychological states may also significantly impact health behavior and clinical outcomes in patients with T2D [3]. Negative psychological syndromes such as depression and anxiety have been consistently associated with poor outcomes in patients with T2D [4-6]. For example, depression is associated with impaired glucose control [7], functional disability [8], end-organ complications [7], and mortality [7,9,10], and distress itself is associated with lower levels of treatment adherence [2].
On the other hand, positive psychological characteristics- optimism, positive affect, gratitude, and related constructs-may also play an important role in medical outcomes. These positive psychological constructs are not simply the flip-side of depression [11,12], e.g., it is possible that a depressed individual may be optimistic about the future whereas a non-depressed individual may conversely have low levels of optimism. Prior work has found that these constructs have been linked to superior health outcomes including healthier diet, increased physical activity, and lower rates of mortality across various medical conditions [13-15]. Furthermore, the connections between positive psychological constructs and health have been independent of sociodemographic factors, medical characteristics, and the adverse effects of depression and anxiety [13,15]. Nonetheless, there has been less focus on the promotion of positive psychological well-being in T2D individuals.
Specifically related to T2D, positive psychological constructs have been associated with numerous beneficial outcomes [3,16-18]. For example, in a large epidemiologic study, measures of psychological well-being, including emotional vitality and life satisfaction, were prospectively linked with the prevention of T2D [19]. Among patients who have developed T2D, positive psychological attributes are related to superior outcomes. For instance, overall well-being is correlated with better glucose control [20]. Likewise, resilience has been associated with lower levels of hemoglobin A1c, and such resilience has been shown to buffer the effects of psychological distress on blood sugar [21]. Finally, positive affect has been prospectively and independently linked to lower mortality among those with T2D [22].
Though the relationship of positive psychological constructs and health outcomes is not fully understood, the beneficial effects of positive psychological states are most likely mediated through health behaviors. Positive states in some studies have been directly associated with favorable effects on physiology in T2D (e.g., reduced sympathetic hyperactivity, decreased levels of proinflammatory biomarkers, and decreased hypothalamicpituitary- adrenal axis hyperactivity) [3,16-18]. However, most evidence that links positive states to superior outcomes does so via increased adherence to health behaviors [16-18]. For example, in T2D patients, positive affect and optimism have been prospectively linked to greater physical activity, healthier diet, and reduced smoking, even after controlling for baseline behavior and relevant covariates [22]. Such improvements in health behavior may be caused by easier initiation of physical activity, greater confidence in meeting diet and activity goals, and more vitality/energy to engage in self-management when experiencing positive mood [23].
An important question is whether positive psychological well-being is inherent or whether it can be modified. There is by now a substantial literature on so-called positive psychology (PP) interventions and their efficacy in improving psychological well-being. PP interventions use exercises (e.g., gratitude letters, acts of kindness, personal strengths), completed in a systematic manner, to boost optimism, positive affect, and resilience. In healthy participants, PP exercises have consistently increased well-being and decreased depression in studies of over 5000 participants [24]. More recently, trials in patients with coronary heart disease, hypertension, and HIV have found that such programs have had beneficial effects on well-being, depression, and in some cases, health behaviors [25-29].
PP interventions have several potential advantages to other treatment programs, particularly when considering individuals with T2D. First, as opposed to treatments that are applied only to patients with clinical depression or other psychiatric disorders, PP interventions are instead designed to increase positive psychological well-being across a variety of different populations, including those considered to be psychiatrically healthy [30]. This should make the PP intervention more applicable to individuals with T2D who may experience a range of psychiatric symptoms. PP also differs from somewhat-related mindfulnessbased stress reduction and self-efficacy interventions [31-33] in that it: (a) specifically targets constructs-positive affect and optimism-linked to superior adherence and outcomes in T2D [3], (b) utilizes validated PP exercises found to be effective across dozens of studies [24], and (c) is simple for patients and does not require the substantial provider training needed for most other interventions.
Despite the potential benefits of an intervention that could promote well-being, reduce distress, and improve self-care in T2D patients, there has been limited study of PP interventions in this patient population. However, results to date have yielded encouraging findings. For example, an online positive affect intervention for T2D patients led to improvements in positive affect and depression, although no significant changes in diabetes-specific efficacy or in health behaviors were found [34]. A related resilience-focused intervention for T2D patients was, however, associated with improvements in HDL cholesterol and fasting blood sugar in a small controlled trial [35], and a one-arm pilot study of a PP intervention also found substantial improvements in psychological outcomes and self-reported health behavior adherence [36].
In the context of these promising but mixed results in T2D patients, there is still a question about whether such PP interventions alone are enough to result in changes in selfcare and outcomes, or whether they are better combined with existing behavioral interventions. In the case of the latter scenario, the well-being component would presumably promote motivation, self-efficacy, and optimism, which would allow for greater engagement in the intervention. It is also still unknown how PP interventions compare to other behavioral interventions that have been tested in this population targeting self-efficacy or stress management, which have been shown to affect diabetesrelated distress [37,38] and, less consistently, health outcomes [39-42]. Given the clear associations between well-being and outcomes in T2D, along with the promising effects of initial PPbased studies, continued work in this area is needed to ascertain whether well-being interventions can truly impact function, blood sugar, and overall health in this key population.
To More articles in Current Research in Diabetes & Obesity Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php1B
0 notes
Text
The Perfect Storm: Non-Alcoholic Fatty Liver Disease (NAFLD) and Atheromatosis in Morbidly Obese Patients with or Without Diabetes. Effect of Bariatric Surgery

Authored by Julia Peinado Onsurbe
Abstract
In recent years, the prevalence of non-alcoholic fatty liver disease (NAFLD) has increased rapidly, paralleling the epidemic of type 2 diabetes mellitus (T2DM) and obesity leading to cardiovascular disease (CVD). It has been demonstrated that NAFLD is strongly associated with atherosclerosis [1]. With recently gained knowledge, it now appears that NAFLD might induce insulin resistance, dyslipidaemia, oxidative stress, inflammation, and fluctuation of the adipokines associated with atherosclerosis [1]. The association between NAFLD and atheromatosis in obese patients with or without T2DM has been controversial. It could be that liver disease participates in the origin of atheromatous plaques.
Excess liver fat is extremely common, and the prevalence of NAFLD has been increasing mainly because of the increased prevalence of obesity. The prevalence increases to 57% in obese subjects, 70% in diabetic subjects and 90% in morbidly obese people. Patients with NAFLD are at increased risk for cardio-metabolic complications, such as CVD and T2DM. Bariatric surgery corrects improves the steatosis, T2DM [2,3] and cardiovascular risk factors, and it reduces long-term cardiovascular events.
It is possible that a higher degree of liver disease indicates further progression of atheroma, but that finding could occur given that, due to a certain degree of liver injury, bariatric surgery is notable to improve or reverse vascular lesions [4].
Keywords: Steatosis; Atherosclerosis; Liver; Obesity; Diabetes; Cardiovascular disease
Abbreviations: NAFLD: Non-Alcoholic Fatty Liver Disease; T2DM: Type 2 Diabetes Mellitus; FFA: Free Fatty Acids; ROS: Reactive Oxygen Species; PUFA: Polyunsaturated Fatty Acids; VV: Vasa Vasorum
Introduction
Non-alcoholic fatty liver disease (NAFLD)
Excess liver fat is extremely common, and the prevalence of NAFLD has been increasing rapidly, paralleling the epidemic of type 2 diabetes mellitus (T2DM) and obesity leading to cardiovascular disease (CVD). It has been demonstrated that NAFLD is strongly associated with atherosclerosis [1]. Simple hepatic steatosis has been shown to be associated with marked silent carotid atherosclerosis [5]. The prevalence increases to 57% in obese subjects, 70% in diabetic subjects and 90% in morbidly obese people [6,7].
Increased hepatocyte triglyceride formation could play a protective role to prevent hepatocytes from FFA-induced damage. These toxic effects induced by FFA and other derived metabolites is known as lipotoxicity [8]. One important mediator of lipotoxicity is the over-production of reactive oxygen species (ROS). When ROS production exceeds the antioxidant capacity, it leads to oxidative stress. Numerous studies have demonstrated that oxidative stress is elevated in NAFLD patients [9]. Despite the powerful anti-oxidant capacity of the liver, excessive FFA oxidation in the steatotic hepatocytes could cause substantial oxidative stress [10].
Oxidative stress can cause mitochondrial injury by causing the reaction of ROS with polyunsaturated fatty acids (PUFAs) at the mitochondrial membrane. Insulin resistance (IR) plays a central role in these processes by allowing for the excessive flow of fatty acids from adipose tissue and also by impairing peripheral glucose disposal. Peroxisome proliferator-activated receptor a (PPAR-a) is a key transcription factor regulating the expression of genes involved in mitochondrial, peroxisomal and microsomal FFA oxidation [11]. Hepatocyte injury, a characteristic of NAFLD, which manifests as ballooning, is produced by the abnormal distribution of intermediate filaments induced by oxidative stress. This reaction is mediated by the Wnt/beta-catenin pathway. These ROS attack and react with PUFAs (polyunsaturated fattyacids) present at themitochondrial membranes, so ROS damage mitochondrial DNA and cause mitochondrial dysfunction. Apoptosis can be initiated by dysfunction almitochondria via the Wnt/beta-catenin pathway, and it is also the main mechanism of death in NASH, promoting the progression from simple steatosis to NASH.
Kupffer cells play a key role in liver inflammation [12], regulated by the balance of pro-inflammatory M1 Kupffer cells and anti-inflammatory M2 Kupffer cells [13]. Imbalanced M1/M2 phenotypic Kupffer cells have emerged as a central mechanism underlying steatohepatitis. Kupffer cells are exposed to various substances and they function to sense and remove pathogens and dangerous molecules via pattern recognition receptors (PRRs). The PRRs comprise at least two families of sensing proteins: the Toll-like receptors (TLRs) and the NOD-like receptors (NLRs). Both NLRs and TLRs detect danger signals, including pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs). PAMPs are pathogens originating from gut-derived microorganisms, while DAMPs include molecules endogenously released from stressed or injured hepatocytes. TLRs recognize bacterial products derived from gut microbiota, such as lipopolysaccharide (LPS, also known as endotoxin) and peptidoglycan. Kupffer cells are the primary sensors of PAMPs and DAMPs as well, and TLR and NLR receptors have emerged as important mediators of Kupffer cell activation [14].
Atheromatous processes
The vasa vasorum (VV) are blood vessels that extend from the adventitia of large vessels and irrigate their walls. Its primary mission is to provide nutrients and oxygen to the layers that cannot penetrate the blood vessel lumen. One of the earliest changes that can be observed in the atheromatous process is the proliferation of VV in the adventitia [15]. The hypoxia is the main stimulus of intimal neovascularization by perpendicular adventitial vessels [16]. Hypoxia of the vessel wall, either by injury or by increasing demand, is the main factor inducing neoangiogenesis [17]. A correlation was shown between the density of the VV and the progression of atherosclerotic plaque [18]. Neovascularization and endothelial dysfunction are the initial phenomena of atheromatosis, while increased IMT and appearance of the plaque occur later.
Endothelial injury
Theendothelial injury process begins with the molecular responses of transcription factors induced by hypoxia (HIF, hypoxia inducing factor) [19], where in the increase in low density lipoprotein [20] and reduced nitric oxide (NO, mainvasodilator) initiate a cascade of endothelial activation, recruitment of inflammatory cells, production of reactive oxygen species(ROS) and monocyte infiltration, the direct migration of which is mediated by monocytechemo attractant protein(MCP-1) [21]. The LDL are subjected to oxidative modification, resulting in a highly oxidized and aggregated lipoprotein called oxLDL, which is among the more atherogenic forms of LDL [22]. OxLDL stimulates the inflammatory signalling by endothelial cells, releasing chemotactic proteins, such as MCP1, and growth factors, such as monocyte colony-stimulating factor (MCSF), which facilitate the recruitment of monocytes by the arterial wall, a process mediated by the selectins [23]. oxLDL also promotes monocyte differentiation into the macrophages that convert oxLDL into lipid-laden foam cells, which are cells with the hallmark of atherosclerosis [22]. oxLDL is recognized by the scavenger receptor (landfill) macrophages SR-A and SRB-1 or CD36 (scavenger receptor-A and B, respectively). In nondiabetic subjects, sCD36 (soluble CD36) was significantly associated with IR indices, carotid atherosclerosis and fatty liver. However, prospective studies are needed to further evaluate the role of sCD36 in the inter-relationship among atherosclerosis, fatty liver and insulin resistance [24].
Activated macrophages express cytokines, such as TNF-a, and IL-1 beta (Interleukin-1 beta), which stimulate endothelial cells to express adhesion proteins, such as VCAM-1 and ICAM-1 (vascular-1 molecules and adhesion intercellular-1, respectively). ICAM-1 plays an important role in the recruitment of immune cells during the progression of plaque, and it was positively correlated with HOMA-IR (homeostasis model of resistance insulin), BMI (body mass index), leptin, and adiponectin and negatively correlated with high density lipoprotein (HDL) cholesterol [25]. Moreover, ICAM-1 is induced as a result of the binding of angiotensin-2 to its receptor, promoting the release of ROS and endothelin-1 by endothelial cells [26]. Other molecules involved in pathophysiology of the plaque are VEGF [26], PAI-1 and adiponectin [27].
It is well established that IR is the primary factor underlying hepatic steatosis. IR is present in almost all NAFLD patients [28]. Fat accumulation in the liver is associated with oxidative stress and lipid peroxidation. Furthermore, NAFLD subjects have increased secretion of inflammatory marker and plasma glucose and decreased HDL concentrations. The consequence of this physiological dysfunction is an increased risk for the development of diabetes and atherosclerosis and an increased risk of coronary artery disease [29].
Both diabetes and IR cause a combination of endothelial dysfunctions, which can diminish the anti-atherogenic role of the vascular endothelium [30]. Therefore, in patients with diabetes or insulin resistance, endothelial dysfunction might be a critical early target for preventing atherosclerosis and cardiovascular disease. The biochemical or cellular links between elevated blood glucose levels and vascular lesions remain incompletely understood.
Molecular mechanisms
MicroRNAs (miRNAs) have emerged as a new class of gene regulators, recent studies of which have emphasized that they play a crucial role in atherosclerosis [15]. miRNAs have also been associated with oxidative stress, inflammation, insulin signalling, apoptosis and angiogenesis related to obesity. All of these processes contribute to the development of T2DM and atherosclerosis and therefore are associated with cardiovascular disorders [31]. Recent studies have reported that the miRNAs released by cells have endothelial anti-atherogenic properties, similar to those that increase vascular areas when the laminar flow is high or that decrease when the flow is low or abnormal, such as miRNA-10a [32], the miRNA-19 [33] or miRNA-143/-145 [34]. Other studies have reported pro-atherogenic roles for miRNA-712 [35] and miRNA-92a [36].
Studies of human NAFLD have identified approximately 44 miRNAs dysregulated in the NAFLD liver [37]. Several miRNAs have been identified as playing key roles in the development of steatosis and its progression to steatohepatitis, fibrosis, cirrhosis, and hepatocellular carcinoma [38]. Overexpression of miR-185 resulted in increased insulin receptor substrate-2 (IRS-2) expression, improved insulin sensitivity and reduced steatosis [39]. The predicted targets of miR-122 include genes regulating cholesterol and lipid metabolism, proteasomal protein degradation, cell adhesion and extracellular matrix biology [40]. In addition to miR-122, several miRNAs have been associated with the pathogenesis of NAFLD. Cheung and colleagues found that miR-21 was heavily upregulated in the livers of patients with steatohepatitis [41].
Atheromatosis, NAFLD and endothelial changes may be reversible Bigornia et al. [42] demonstrated that reversing endothelial dysfunction at 12 months of weight loss was a more important metabolic change than the degree of weight loss. Mavri et al. [43] observed similar results in obese subjects submitted to a diet and found an improvement in endothelial dysfunction at one week after initiating the diet. Recently, decreased IMT was found after gastric bypass only in obese patients with T2DM but not in patients with impaired glucose tolerance [44]. Currently, we have several non-invasive techniques that allow us to assess endothelial dysfunction and adventitious arterial blood, more specifically VV, including the study of arterial tone in peripheral beds with EndoPAT and examining the density of the VV in the adventitia with carotid ultrasound echography after contrast administration (microbubbles of hexafluoride sulphur). The use of micro bubbles allows us to study the vascular structures that these compounds leave in the bloodstream and thus allows for the visualization of VV [45].
All this finding showed that relatively early atherosclerotic changes might be reversible if it is explored with more sensitive measuring methods than IMT, presumably by measuring more development and obtaining early results.
Acknowledgement
This work was supported by the Ministerio de Sanidad y Consumo, Instituto de Salud Carlos III (ISCIII) (PI11/01159 and PI15/00190 to JP-O PI15/00332 to JAB-F) and the FEDER Funds of the EU (Fondo Europeo de Desarrollo Regional: “Una manera de hacer Europa”). English grammar and language have been corrected by American Journal Experts (www.journalexperts. com).
To More articles in Current Research in Diabetes & Obesity Journal Please click on: https://juniperpublishers.com/crdoj/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php
0 notes
Text
Zymosan A, an Old Tool in Experimental Pharmacology with Newer Applications

Authored by Kanwaljit Chopra
Abstract
Insulin resistance (IR) is an important link between obesity and post obesity complications varying from diabetes mellitus to neurological insults such as cognitive dysfunction and Alzheimer's disease. Currently available high calorific diet induced preclinical models mimic clinical pathologies of various metabolic disorders but they are highly time consuming. Zymosan a well-known inflammagen has recently been used to induce reversible IR conditions in rodent models. Though, the insulin resistance lasts as long as zymosan is injected to animals, but the pathogenesis that resembles to that of obesity, IR and metabolic syndrome. However, high fat or high carbohydrate diet could be used in combination with zymosan to develop a novel animal model of IR where both inducers act synergistically to exert their primary actions. The combination of these two approaches may help in development of a robust experimental model of IR and post IR complications within a very short duration. Such preclinical models will help the researchers to better understand the pathological evolution of long term metabolic disruptions like metabolic syndrome and others.
Keywords: Zymosan; Insulin resistance; High fat diet; High carbohydrate diet; Diabetes; Obesity; animal model; Metabolic syndrome; Metabolic complications
Abbrevations: AKT: Protein Kinase B; CD 14: Cluster of Differentiation 14; GSK 3: Glycogen Synthase Kinase-3; HFCS: High Fructose Corn Syrup; HFD: High Fat Diet; IL: Interleukin; IR: Insulin Resistance; IRS 1: Insulin Receptor Substrate 1; JAK: Janus Kinase; LTB4: Leuko Triene B4; MIP: Macrophage Inflammatory Protein; NFKB: Nuclear Factor Kappa Light Chain Enhancer of Activated B Cells; PI3K: Phosphor Inositide 3-Kinase; PMNs: Poly Morph Nuclear Cells; ROS: Reactive Oxygen Species; STAT: Signal Transducer and Activator of Transcription; T2DM: Type 2 Diabetes Mellitus; TLR: Toll Like Receptor
Introduction
Insulin is the major pancreatic hormone that regulates the glucose homeostasis in our body. The pathological state in which the production of insulin is decreased, mostly due to beta cell destruction is known as insulin deficiency whereas the situation in which insulin secretion is normal and muscle cells are unable to respond to the systemically available insulin is referred to as insulin insensitivity or insulin resistance (IR) [1]. In such resistant states, the body cells fail to take up the glucose from blood stream and this leads to elevated blood sugar levels, referred to as hyperglycemia. IR is a primary pathological result of obesity and hypertriglyceridemia [2] that leads to a wide range of secondary complications such as type 2 diabetes (T2DM) [3], metabolic syndrome (Syndrome X) [4,5], cardiovascular events [6,7], stroke [8] including recently discovered link between hypertriglyceridemia, insulin resistance, altered brain glucose homeostasis, Alzheimer's disease [9,10] and cognitive dysfunctions [11-13]. The pathophysiology of insulin resistance is very complex with number of known etiologies, most of which are diet or nutrition related. Over-nutrition or obesity triggered inflammation in adipose tissue [7,14], altered lipid metabolism resulting in hypertriglyceridemia [15] and distorted gastrointestinal microbiota (dysbiosis) [16-18] and all of the contributing factors are interrelated at variable degrees to rise to the final state of IR. The complexity and multi factorial etiologies of IR sum up to make it very hard to replicate and develop a heterogeneous animal model for the purpose of understanding the pathogenesis of IR and its secondary complications and pharmacological screening of chemical entities. Hence the new chemical entities need to be screened in more than one animal models of IR to determine their safety and efficacy. Currently, a number of preclinical testing systems including transgenic models are available for the purpose of IR research. Among various available models of IR, diet-induced animal models are affordable, extensively studied and utilized for the research purposes [19]. Diet-induced animal models involve the use of high calorie containing food sources such as fats (vegetable oil and animal fat consisting high amounts of saturated fats) [20,21], fructose corn syrup [22,23] and sucrose [24] alone or in combination [25,26] to induce IR. Though, these dietary animal models induce the disease with similar pathophysiological mechanisms to that of clinical cases, the development of pathological hallmarks of IR takes 12-24 weeks of time which makes these models tedious and cumbersome to use [25,27].
Zymosan a glucan with repeating glucose units connected by β-1, 3-glycosidic link ages is an insoluble powder prepared from cell wall from Saccharomyces cerevisiae,consisting of protein-carbohydrate complexes [28]. Zymosan is an inflammagen majorly used as a pharmacological tool to develop animal models of rheumatoid arthritis [29], acute peritonitis, multiple organ failure [30] and IR [31]. Zymosan exerts its inflammatory actions by stimulating macrophages via TLR-2 Receptors and neutronphil infiltration through various activated cytokines and chemokiness. Zymosan stimulated TLR-2 associates with TLR-6 and CD-14 cells, initiating the activation of macrophages [28]. Furthermore, zymosan acts directly by binding to Dectin-2 a phagocytic receptor which is expressed on the surface of macrophages and dendritic cells. Recognition of zymosan by Dectin-2 besides the activation of TLR-2 and TLR-6 augments the immune response that leads to inflammation [32]. Zymosan causes neutrophil infiltration to the site of action by stimulating the production of Leukotriene B4 (LTB4), a chemotactic agent responsible for the recruitment of various chemokines and cytokines like IL-1α, IL- 15, IL-18, TNF-α, IL-8, MIP-1 α and MIP-2 [33,34]. Zymosan also exerts its action by other minor mechanisms that play a key role in inducing inflammation, which includes-systemic hypotension, increasing plasma nitric oxide levels, increasing cycloxygenase activity, increasing exudates formation and excessive reactive oxygen species (ROS) production by formation of activated polymorphonuclear(PMN)cells [30].
Being an inflammagen, Zymosan has become one of the potential tools for disease animal modelingwhere inflammation has major role to play to mimic the similar pathophysiology as that of humans. With varying dose, zymosan has been used to develop various preclinical disease models. The disease models include rheumatoid arthritis induced in wistar rats by injecting in rear knee joint at a dose of 1mg suspended in 50μL of sterile normal saline [29], multiple organ failure by administering intraperitoneally (i.p.) to rats at a dose of 500mg/kg [30] and acute peritonitis by i.p. injection to Balb/C Mice at a dose of 0.5mL from a zymosan stock solution of 2mg/mL [35].
Till date, there has been only one study published over the use of zymosanto induce reversible IR in preclinical setting. Mice were injected with zymosan viai p. Route at a dose of 100mg/kg once a week for four consecutive weeks. Inflammation driven ROS production is the mechanism involved in zymosan induced IR. Zymosan causes inflammation through activation of macrophages via stimulation of TLR-2 and TLR-6, Activation of PMN cells to escalate the intracellular ROS production. In this model of IR, zymosan injection has also been held responsible for the reduced expression of various protein markers involved in insulin signaling like IRS-1, PI3-Kinase, phosphorylated GSK-3 and Akt [31].The main aim of this review is to highlight the importance of need of accelerated new animal model to study insulin resistance and associated secondary complications of IR.
Discussion
Feeding laboratory animals adlibitum with high calorific diets take a minimum time of 12 weeks to reach the IR state whereas a study carried out by Wang et al. [31] suggest that zymosan could successfully induce IR within just 1/3 of the time that is taken by high calorific diet to create the same situation. The only limitation of this model is that the IR is reversible and animals have returned to their normal state within 4 weeks after withdrawal of zymosan administration. Meanwhile, we hypothesize that the combinatorial use of high calorific diet and zymosan can cut short the time duration to induce IR. The use of zymosan with high calorific diet will be rational, as both of these disease inducing agents act through the analogous inflammatory pathways. Zymosan and high calorific diet acts on toll like receptors (TLRs) present on cell membrane to initiate the release of inflammatory cytokines which in turn leads to the activation of NF-k Band JAK-STAT pathways that desensitize insulin receptors towards insulin and leads to surge in unutilized levels of insulin in systemic circulation, can also be termed as insulin resistance [28,36-38].\
Conclusions & Prospective
A. Insulin resistance is considered as a major mediating and facilitating factor for the development of secondary metabolic complications associated with consumption of high calorific or cafeteria or junk food. With an aim of developing a new, less time consuming and clinically relevant animal model to study and understand the pathology of various metabolic complications in which IR plays a vital role.
B. Inflammation is the common mechanism through which the high calorific diets and zymosan induce IR and their combined use shall exert a synergistic effect towards rapid onset of insulin resistant state than traditional models. This hypothesis can be adapted and utilized by the researchers working in the fields of IR, obesity, T2DM, metabolic syndrome and cognitive dysfunction associated with metabolic complications.
To More articles in Current Research in Diabetes & Obesity Journal Please click on: https://juniperpublishers.com/crdoj/index.php
For more about Juniper Publishers please click on:
https://juniperpublishers.com/video-articles.php
0 notes
Text
Clinical Factors Associated with Weight Gain in French-Canadian Children and Adolescents Treated With Second Generation Antipsychotics: A 24-Month Retrospective Study

Authored by Leila Ben Amor
Abstract
Objective: To describe clinical factors associated with SGA-induced weight gain induced by long-term second generation antipsychotic (SGA) treatment in children and adolescents.
Methods: A 24-month retrospective study conducted between November 2005 and June 2013. 147 antipsychotic-naive patients were selected [mean age 12.8; (95% CI 9.8 to 15.9)] and treated with an SGA (risperidone, olanzapine, quetiapine and aripiprazole) for up to 24 months. Weight and height were measured and BMI (body mass index) z-scores were calculated at baseline, 1, 3, 6, 12 and 24 months. Linear mixed-model analysis was used to compare weight, BMI and BMI z-score changes of the SGA treatment with the repeated factor being the time relative to baseline at 1, 3, 6, 12 and 24 months.
Results: After 24 months of SGA treatment, mean weight increased significantly by 12.8 kg (95% CI 10.4 to 15.0) and BMI z-score by 0.44 (95% CI 0.21 to 0.68). Incidence of overweight/obesity was 22.6% and significant BMI z-score increase over 0.5 was 9.4%. Older age (p=0.001), male sex (p=0.002) and diagnosis of mood disorder (p=0.0004) were associated with a significant increase in weight gain. Lower baseline BMI z-score (p<0.0001) and presence of mood disorder (p=0.011) had a significant impact on BMI z-score augmentation.
Conclusion: Older age, male sex, lower baseline BMI z-score and diagnosis of mood disorder were associated to more pronounce SGA- induced weight gain.
Keywords: Second generation antipsychotics; Weight gain; Children; Adolescents
Introduction
Second generation antipsychotics (SGAs), which are medications used to treat a variety of psychiatric disorders, are associated with weight gain, obesity, and increased cardiovascular risk in children, adolescents as well as in adult populations [1-3]. A source of concern is increasing evidence suggesting a greater or exigenic effect of SGAs in youth compared to adults [3-8], especially considering childhood obesity adversely affects nearly every organ system, causing substantial morbidity and mortality in adulthood [9].
Multiple factors have been associated with SGA-induced cardio-metabolic side effects, such as SGA type, dose, treatment duration, previous exposure or SGA polypharmacy, subject's age, sex or illness-related factors , but there is little consensus over their respective effects [2,3,5,6,10,11]. Among SGAs, olanzapine and clozapine are associated with the most important weight gain risk, followed by quetiapine and risperidone, and finally by aripiprazole and ziprasidone which have the lowest risk [3,12]. The findings of some, but not all, studies suggest that women have a greater vulnerability to antipsychotic-induced weight gain that men [2,3]. Evidence in the antipsychotic-drug- naive pediatric population suggest a dose-dependent effect of risperidone on weight gain and lipid profiles as well as dose dependent effect of olanzapine on serum lipids and blood glucose levels [13]. The impact of the treatment duration on the weight gain remains a subject of debate as some studies showed an attenuation of the weight gain over time with a plateau around 6 or 12 months [1,14-18], whereas others demonstrated a continuous weight increase over time [19-21]. Anyhow, data on the long term metabolic effects of antipsychotics in pediatric populations are scarce [3]. The heterogeneous results regarding moderating variables could be explained in part by the different methodologies and study samples found across studies.
The aim of this study is to describe clinical factors associated with the SGA-induced weight and increase in BMI z-score in antipsychotic-naive children and adolescents, in the "real- life" clinical setting. We hypothesize that older age, female sex, lower baseline BMI z-score and polypharmacy other than with psychostimulants will be associated with more important weight gain, in accordance with actual literature [2,3,6,7].
Subjects and Methods
Study design
The medical charts of the inpatients and outpatients from the "Second-Generation Antipsychotic Monitoring Program" at Hotel-Dieu de Levis Hospital (Quebec, Canada) between November 2005 and June 2013 were retrospectively reviewed. The population in the area deserved by the department of child psychiatry is almost exclusively of French-Canadian origin. All study procedures were reviewed and approved by the local ethics and research committee (CER-1213-018).
Study subjects
The inclusion criteria for the study subjects were being under 18 years old, having no previous history of antipsychotic treatment and having received treatment with an SGA for at least one month during the study. The exclusion criteria included preexisting dyslipidemia, diabetes or receiving medications for metabolic conditions. For each patient, we gathered information for age, sex, psychiatric diagnoses, SGA treatment (total dose/ day, duration of use), other medications (total dose/day, duration of use), height and weight. The height and weight were measured at baseline, 1, 3, 6, 12 and 24 months by a nurse. Diagnoses were made by a child psychiatrist in accordance with the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM IV-TR) criteria. Clinical data was collected from the chart notes. The main diagnosis was considered the one for which the SGA was prescribed. In many cases, more than one main diagnosis was recorded because SGAs were used to treat symptoms common to many diagnostics, such as disruptive behavior and ADHD. The other medications given in adjunct with the SGA were grouped in four categories: psychostimulants (amphetamine-based, methylphenidate-based), atomoxetine (to more accurately discriminate the potential metabolic impact with psychostimulants), antidepressants (bupropion, citalopram, fluvoxamine, sertraline, venlafaxine) and mood stabilizers (carbamazepine, lithium, valproic acid).
Treatment
The patients received SGAs (olanzapine, risperidone, quetiapine or aripiprazole) in monotherapy (the same SGA was prescribed from the beginning to the end of the period of the follow-up) or in polytherapy (switched from one SGA to another or used a combination of two SGAs, with the second SGA added between 0.5 and 24 months).
Measures
The variables studied were weight, BMI-calculated as weight (kg)/height squared(m2)-and standardized BMI z-score- calculated using the children's BMI percentile-for-age calculator from the Children's Nutrition Research Center, Baylor College of medicine website (http://www.bcm.edu/cnrc--- apps/ bodycomp/bmiz2.html). The exact day of weight measurement was not always available in the charts; therefore, we calculated the BMI z-scores as if the patients were always weighed on the first day of the month to minimize the measurement bias. The BMI z-score represents the BMI adjusted for age and sex, thus considering the weight gain attributable to the growth process. It allows the comparison between the BMI of children and adolescents of the same age and sex [22]. Overweight was defined as BMI z-scores between the 85th and 95th percentile and obesity as BMI z-scores greater than or equal to the 95th percentile [23]. The doses of each SGA were converted in chlorpromazine equivalents [24].
Statistical Analysis
The statistical analysis included all the patients with data available at baseline and at least at one follow-up assessment time. The characteristics of the sample are presented as means (95% CI) for the continuous variables and as frequencies or percentages for the categorical variables. We assessed changes secondary to SGA treatment in continuous outcomes using the linear mixed model with repeated measures. The repeated factor was the time relative to baseline at 1, 3, 6, 12 and 24 months. Since the measures were collected from retrospective chart review, they reflect ‘real-life’ clinical situations not always strictly respecting follow-up time intervals. We averaged data for plus or minus one month interval (for example, the third month corresponds to data from the second to the fourth months).
Incidence was calculated as the proportion of new-onset metabolic complications at each time point divided by the number of patients with available data. For each outcome, we adjusted for age and sex plus other medications associated with SGA or primary psychiatric diagnosis, thus yielding two different analyses. Summary statistics are presented as adjusted means of change over time (95% CI). All analyses were made using SAS 9.3 (SAS Institute Inc., North Carolina, USA). The threshold for statistical significance was set at p<0.05.
Results
Figure 1 A total of 147 patients treated for the first time with an SGA between November 2005 and June 2013 were included in the study. One hundred sixteen (78.9%) of them received an SGA in monotherapy and 31 (21.1%) received an SGA polytherapy (20 subjects switched SGAs and 11 received a combination of two SGAs). Subjects were almost exclusively French Canadian. The category 'Other' primary psychiatric diagnosis included personality disorder, mental retardation, pervasive developmental disorder and obsessive-compulsive disorder.
Further data presented originates from the analysis controlling for age, sex and co-medications Table 1. The other analysis (controlling for age, sex and primary diagnosis) yielded similar results. After 24 months of SGA treatment, mean weight increased significantly by 12.8 kg (95% CI 10.4-15.0, p< 0.0001) and BMI z-score increased by 0.44 (95% CI 0.21-0.68, p= 0.0002).
Incidence of newly developed conditions is considerable as 22.6% of subjects became overweight or obese and 42.9% had a significant BMI z-score increase over 0.5 after two years of treatment. Table 2 Compared to younger age, older age was associated with a superior mean gain weight of 0.38 kg (p=0.001). Males gained a mean of 1.89 kg more than females (p=0.002) and subjects with a mood disorder, a mean 2.49 kg extra compared to the absence of mood disorder (p=0.0004). A lower baseline BMI z-score (p<0.0001) and the presence of mood disorder (p=0.011) had a significant impact on BMI z-score augmentation.
Discussion
In this retrospective study, older patients, males, those with a lower baseline BMI z-score and subjects with a primary diagnosis of mood disorder had a significantly more pronounced weight gain and BMI z-score increase after up to 24 months of SGA therapy. Clinical characteristics as older age and lower baseline BMI z-score have already been associated with an increased SGA-induced weight gain in children and adolescents [10,25]. In adults, even if low baseline BMI has frequently been associated with greater antipsychotic-induced weight gain, controversy still exist over this potential influence as this might be due-at least partially-to a regression to the mean effect and not to an underlying biological factor [2,26].
Counter to our hypothesis, female sex [10] and concomitant use of mood stabilizers [7] were not associated with a more important weight gain. An unexpected finding was male sex being significantly associated with more weight gain that female sex. In agreement with our study (in which most subjects were treated with risperidone), Saklad et al. [27] found that male sex was associated with a more pronounced weight gain in youth treated with risperidone [27]. Another study analyzing metabolic changes in youth treated with risperidone showed no association between sex, age or baseline BMI and the SGA- induced weight gain [28], although this might be due to their small sample size (37 subjects compared to 147 in our study). Our subjects treated for mood disorder with SGAs had a significantly more pronounced weight gain and BMI z-score increase. We found only one short-term study comparing SGA-induced weight gain between bipolar, psychotic and non-psychotic disorders in children and adolescents, which failed to demonstrate an association between mood disorders and weight gain [29]. In our study, the association of mood disorders with a more important weight gain could be explained -at least partially- by the metabolic risk conferred by a more severe pathology, as individuals with psychosis and bipolar disorder appear to have higher baseline metabolic risk than the general population [30].
Although mood stabilizers such as lithium and valproate have been associated with mild weight gain [7,31], we did not find an association between the concomitant use of mood stabilizers with SGAs and more important weight or BMI z-score increase. Only a tendency was found, possibly due to our study's relatively small sample size.
Limitations
The results of this study should be interpreted in consideration of its limitations. Due to the naturalistic design, the metabolic monitoring at 12 and 24 months was relatively low, which limited data available for the analyses and influenced the statistical power of our results. Also, all four SGAs (risperidone, olanzapine, quetiapine, aripiprazole) were regrouped thus preventing us from evaluating their respective effects-however not enough subjects were available to analyze each molecule separately. Additionally, 'a confounding by indication’ bias should be considered when interpreting the results, as physicians might have prescribed a specific SGA depending on the baseline weight of the patient [6]. Moreover, given the variability of SGA doses in the clinical sample, we were unable to adjust the statistical analyses for the SGA chlorpromazine-equivalent dose. Finally, the homogeneity of the population sample analyzed in our study can limit the generalizability of the results.
Strengths
Aside from being a limitation, the genetic homogeneity of our sample confers an asset, as with the subjects being almost exclusively French Canadian the differences attributable to ethnic genetic diversity are limited. Also, our recruitment was restricted to an antipsychotic-naive population, leading to more accurate conclusions about the first exposure to SGAs. Finally, this is one of the few long-term studies of metabolic complications in children and adolescents informing on weight gain and clinical factors associated with SGA use in drug-naive populations.
Conclusion
In summary, we described that older age, lower baseline BMI z-score, male sex and primary diagnosis of mood disorder were associated with more pronounced SGA-induced weight gain, on one hand consolidating previous findings, and on the other eliciting more possible factors implicated in the vulnerability to SGA-induced weight gain: male sex and mood disorder. This information is valuable as it provides insight for physicians about clinical characteristics of patients having increased vulnerability of weight gain when treated with an SGA.
Clinicians should carefully monitor metabolic side effects as they were related not only to physical health complications but also to mental health problems, psychosocial dysfunction and poor treatment adherence [2,32]. Long-term prospective studies with larger sample sizes and control groups are needed to investigate the predictive factors of metabolic complications induced by SGAs.
To More articles in Current Research in Diabetes & Obesity Journal Please click on: https://juniperpublishers.com/crdoj/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php
0 notes
Text
Prospective Observational Longitudinal Study Evaluating Erectile Dysfunction in 50 Type 2 Diabetic Patients with BMI Below 35 Kg/m2 Submitted to Ileal Interposition Associated to Sleeve Gastrectomy

Authored by Ricardo Alexandre Fernandes Ferro
Abstract
Background: Erectile dysfunction (ED) is a mistreated and neglected complication that affects 35%-75% of males with type 2 diabetes (T2DM) leading to worsening quality of life and interpersonal relations. Males with T2DM develop ED 5-10 years earlier than non-diabetics.
Methods: This was a prospective, longitudinal and observational study including 50 consecutive male patients with T2DM and a body mass index (BMI) <35Kg/m2 who underwent laparoscopic ileal interposition associated to sleeve gastrectomy (II-SG).
Objectives: Observe the ED prevalence before and after 12 months of II-SG evaluated by a questionnaire. Evaluate global sexual function 12 months after the procedure and compare with initial parameters. Analyze if diabetes duration was an interfering factor in sexual function improvement 12 months after the surgery.
Results: Mean age was 54.4 years (37-69). Mean diabetes duration was 12, 1 years (05-23 years). Mean HbAlc was 8, 8 % (7, 5-10, 5%). After 12 months, we observed a significant improvement in glycemic control, dyslipidemia, blood pressure and a reduction in the use of insulin and anti-diabetic agents (p<0.05). Erectile dysfunction, sexual intercourse satisfaction, orgasmic function, sexual desire and overall sexual life satisfaction were improved (p<0.05). ED prevalence was 78% before and 46% after the procedure. More than 15 years of diagnosis was a bad predictor for ED improvement.
Conclusion: Ileal Interposition associated to sleeve gastrectomy, significantly improved erectile function, satisfaction with sexual intercourse, orgasmic function, sexual desire and sexual life of patients with type 2 diabetes 1 year after the surgery.
Keywords: Erectile and sexual dysfunction; Type 2 diabetes; Ileal interposition
Abbreviations: ED: Erectile Dysfunction; T2DM: Type 2 Diabetes; BMI: Body Mass Index; II-SG: Ileal Interposition Associated to Sleeve Gastrectomy; HbA1c: Glycated Hemoglobin; ADA: American Diabetes Association; IIEF: International Index of Erectile Function Questionnaire; IBM: International Business Machines; SPSS: Statistical Package for Social Sciences
Introduction
Diabetes mellitus type 2 (T2DM) is a chronic metabolic disorder with a dramatically increasing prevalence. T2DM stems from a progressive insulin secretory defect on the background of insulin resistance. Prolonged insufficient metabolic control with constantly elevated HbA1c levels inevitably leads to complications, most commonly to diabetic nephropathy, diabetic retinopathy, diabetic neuropathy, and macrovascular problems [1].
Modern anti-glycemic agents and life style modifications can lead to metabolic control, but a long-lasting effect still needs to be proven. Erectile dysfunction is a chronic complication presented in a wide range (35-75%) in T2DM male patients, usually 5-10 years earlier than non-diabetic males [2]. Relaxation of the smooth muscles of the venous (cavernous) sinusoids is the final erection mechanism and having sinusoids endothelium integrity is vital for the process. On the other hand, endothelium injury is present in the vast majority organic causes of ED [3]. Obesity, dyslipidemia and diabetes are independent risk factors for cardiovascular disease and also constitute major risk factors for ED, where sinusoids endothelium injury is an indicative of developing atherosclerosis [4]. In the very obese patient with type 2 diabetes, bariatric surgery appears to be a treatment modality that is both highly effective and increasingly attractive [5]. On the other hand, in the most frequent kind of type 2 diabetes, i.e., the hyperglycaemia surfacing after the fourth decade of life in moderately obese subjects, is a progressive disease, and resolution, whether spontaneous or by treatment, is rare. This discrepancy in outcome is irrefutable and unaccounted for [6].
One potential explanation is that the hyperglycaemia of morbid obesity has a different pathogenesis from the hyperglycaemia of the moderately obese or lean diabetic. Another possibility is that bariatric surgery per se interferes with glucose metabolism in ways that none of the other antidiabetic treatments does. The available evidence, if limited and non- homogeneous, suggests that at least some of the antidiabetic effect of bariatric surgery may be independent of the induced weight loss [7].
De Paula et al. had shown that in type 2 diabetic patients with a BMI below 35 kg/m2, ileal interposition associated to sleeve gastrectomy (II-SG) is an effective, safe and long-lasting procedure reaching normal levels of blood glucose, HbAlc, lipid profile and blood pressure in 86% of patients without any anti-diabetic agents [8,9]. In this prospective, longitudinal and observational study we observed the ED prevalence before and after 12 months of II-SG evaluated by a questionnaire, evaluate global sexual function 12 months after the procedure and compare with initial parameters and analyze if diabetes duration was an interfering factor in sexual function improvement 12 months after the surgery.
Methods
This was a prospective, longitudinal and observational study with a mean follow up of 12 months designed to evaluate ED in T2DM patients.
Study population
The study included 50 consecutive male patients with type 2 diabetes (diagnosed according to the revised ADA criteria) and a body mass index (BMI) <35kg/m2, who underwent laparoscopic ileal interposition associated to sleeve gastrectomy (II-SG). Mean age was 54.4 years (37-69). Smoking was present in 12% of the patients. Mean diabetes duration was 12, 1 years (05-25 years). Patients were invited to participate the study and respond a questionnaire in the pre- and postoperative period. All subjects gave written informed consent to the study, and the protocol was approved by the ethics committee of the hospital and referenced by the consolidated note from Plataforma Brasil/Ministério da Saúde.
Surgical procedure
The surgical procedure was performed by laparoscopy. II- SG started with division of the jejunum 20cm bellow the Treitz ligament using a linear stapler. An ileal segment of 200cm was removed 30cm proximally to the ileocecal valve, and interposed peristaltically up into the jejunum. The anastomoses were performed functionally side by side. The intestinal measurements were performed with traction along the antimesenteric border using a 10cm atraumatic gasper. The sleeve gastrectomy was performed after devascularization of the greater curvature using the ultrasonic scalpel. A 36-French Fouchet orogastric calibration tube was placed along the lesser curvature toward the pylorus. The gastric resection was performed starting at the antrum and continuing up to the angle of His using a linear stapler; the staple line was covered by an invaginating suture [10].
Inclusion criteria : All subjects had had type 2 diabetes for at least 3 years but none had had major upper abdominal surgery; active sexual life in the last four weeks preceding the procedure; hbA1c above 7% in the last three months; documentation of HbA1c exceeding 7.5% for at least 3 months; stable weight, defined as no significant change (>3%) over the 3 months before enrollment; evidence of stable treatment with oral hypoglycemic therapy or insulin for at least 12 months; BMI less than 35 kg/ m2.
Exclusion criteria : Elderly patients (>70years); Type 1 diabetes (Positive anti GAD and anti-IA-2 auto-antibodies); previous major upper abdominal surgery; pregnancy; malignant or debilitating diseases; severe pulmonary or cardiac diseases, severe renal disease (glomerular filtration rate <30ml/min); use of appetite suppressant medication, eating disorder such as bulimia or binge eating; obesity due to any other endocrine disorder; users of penile prosthesis; use of PDE5 inhibitor medication or any other kind of ED treatment in the last 4 weeks before the procedure; hormonal replacement therapy with testosterone or any other medication that interferes in the steroid hormone laboratory dosage in the last three months before the surgery.
Questionnaire: A standardized questionnaire was applied in 56 T2DM patients in the preoperative period and in 50 after 12 months of follow-up. In 6 patients, we were unable to apply the questionnaire in the appropriate period. This was a discreet procedure conducted by the same investigator in the day before the surgery and after 12 months when a clinical and laboratory evaluation were performed. The International Index of Erectile Function Questionnaire (IIEF) was used to classify the sexual dysfunction level [11].
Statistical Analysis
All analyses were performed using the International Business Machines (IBM) Statistical Package for Social Sciences (SPSS) Advanced Statistics version 17.084. Some results were analyzed based on their frequency distribution. The chi-square test (x2) with Yates correction in contingency tables was used to analyze associations between two variables. When the sample size was too small, resulting in expected values lower than five in one or more blanks, we applied the Fisher's exact test. P values are two-sided and p<0.05 was accepted as statistically significant. Analysis of variance was used to compare means and the Kruskal-Wallis test for comparison of medians.
To analyze the effects of the surgical procedure were employed variables change before and after the procedure, using the McNemar test. For running the test, two conditions must be satisfied: the measurement scale needs to be nominal and with two measures. Another condition to be satisfied is data independence and parity, in other words, data must belong to the same individual, in this study represented by the patient before and after surgery, each patient being independent of each other, so the conditions for the test were met.
To analyze the IIEF variables preoperatively and 12 months later the nonparametric Wilcoxon test was used. In order to reach a significance of 95%, the minimum number of patients enrolled were 21. This means that the number collected from 56 patients before and 50 patients later caters perfectly for scientific and statistical analysis. To quantify the reliability degree between some preoperative and postoperative assessments Kappa coefficient was employed. Kappa values vary depending on the degree of concordance.
Kappa values Degree of concordance
0-0, 20 Weak
0, 21-0, 40 Considerable
0, 41-0, 60 Moderate
0, 61-0, 80 Substantial
0, 81-1, 00 Almost complete
Results
In this prospective, longitudinal observational study, 50 male with T2DM were evaluated pre and 12 month post Ileal interposition associated with sleeve gastrectomy, showing significant improvement in Erection hardness grading scale (EHGS) and International Index of Erectile Function (IIEF). Before the procedure all patients used antidiabetic oral drugs and/or insulin. However, after 12 months, it was restricted to only 10% of them. The same reduction was observed in relation to the use of antihypertensive drugs (p<0.05). All procedures were performed laparoscopically, and there was no mortality. Preoperatively, dyslipidemia was diagnosed in 91.6% of the patients. Arterial hypertension was observed in 75%, nephropathy in 33.3%, retinopathy in 20.8%, neuropathy in 33.3% and coronary artery disease in 33.3% of the patients.
There was a significant decrease (p<0.05) in serum total cholesterol, LDL- cholesterol, triglycerides, fasting glucose, postprandial glucose, hemoglobin A1c, insulin, HOMA-IR and microalbuminuria. The variables creatinine clearance and serum HDL- cholesterol showed significant increase (p <0.05).
Evaluation of erectile function before and 12 months after surgery
Erection hardness grading scale (EHGS) provides evaluation of penile rigidity using a four-grade scale, where score of 1 indicates that the penis is larger than normal, but not hard; 2 means the penis is hard, but not hard enough for penetration, 3 means the penis is hard enough for penetration but not completely hard, and 4 indicates that the penis is completely hard and fully rigid. Before surgery, 22% of patients were able to make vaginal penetration (EHGS 3-4). After 12 months of operation, this number increase to 54% (p<0,05). Before the operation, 34% of patients were scale-graded as 1 and after the intervention this rate decreased to 14% (p <0,05). After 12 months of operation, the number of patients scale-graded 3 doubled and tripled in grade 4. In both cases the differences were significant (p<0.05). Such observations can be translated by the IIEF.
Evaluating the data of the International Index of Erectile Function Questionnaire obtained in the study, it was concluded that there was an improvement in erectile function score given by the erection, when comparing the results observed in the pre-and postoperative II-SG. This difference was significant (p <0.05). The same was found regarding satisfaction with sexual intercourse, the orgasmic function, sexual desire and overall sexual experience.
Assessment of satisfaction with sexual intercourse before and 12 months after surgery
24% of patients had satisfactory level before the operation, with scores less than 10. This rate increased to 62% in the evaluation performed 12 months after surgery (p<0.01).
Evaluation of orgasmic function before and 12 months after surgery
The orgasmic function before and after surgery showed significant improvement (p<0.05), with 50% of patients reporting maximum score postoperatively, while only 6% reached initially.
Evaluation of sexual desire before and 12 months after surgery
While only 26% of patients had satisfactory sexual desire (score less than seven) before the intervention, 96% of them reached these levels in the analysis 12 months after the procedure (p<0 .001).
Assessment of overall satisfaction with the sexual act of the couple before and 12 months after surgery
Regarding overall satisfaction with sexual intercourse the couple, initially 32% of patients had adequate index of satisfaction (score equal to or above seven). After 12 months, 62% of them reached adequate levels of satisfaction (p<0.05).
Evaluation of the total international index of erectile function score before and 12 months after surgery
The IIEF score can range from 5 to 75 points. We observed a significant improvement. Before the operation, 32% of patients scored 30 points. In the second evaluation, the figure was 6% (p<0.01). On the other hand, 40% of patients had a score equal to or greater than 40 in the preoperative evaluation and this index increased to 74% after 12 months of operation (p<0.05).
Correlation of chronological parameters and laboratory with the spheres of sexual function before and 12 months after surgery
Correlating diabetes duration with improved sexual function 12 months after surgery shows that patients who did not had significant improvement in the IIEF and EHGS parameters were those who had more time to diagnosis (more than 180 months). These bad-responder group includes 10% of the patients who maintained the use of antidiabetic medication 12 months after surgery. Among the 25 patients with scores below 10 in the requirement satisfaction with sexual intercourse after 12 months of II-SG were all those more than 15 years of diabetes diagnosis. The same can be said for orgasmic function, sexual desire and overall satisfaction with sexual intercourse.
Discussion
In this report of 12 months follow-up of 50 consecutive type 2 diabetic patients with BMI<35 submitted to laparoscopic ileal interposition associated with a sleeve gastrectomy, we showed that 89.9% had HbA1c below 7% without antidiabetic medication. Using IIEF we evaluated the five main spheres of human sexual function, namely, erectile function, satisfaction with sexual intercourse, orgasmic function, sexual desire and overall satisfaction with sexual function. IIEF has been used widely and universally by medical literature and it becomes possible to compare the results of this study with other published or which may be realized [12].
In this study, the prevalence of ED in T2DM was 78% applying the IIEF. According to Ferrini & cols, it is estimated that by the time a man is in his 40's, he has about a 40% chance of having some form of ED and this prevalence increases about 10% per decade thereafter [13]. There was no significant reduction in BMI before and after the surgical procedure, which reinforces the thesis that the weight loss is not the main mechanism in metabolic improvement observed in T2DM patients undergoing procedures such as ileal interposition [14]. The metabolic results found in this study are in agreement with other previously published papers using the same technique- Ileal Interposition associated with Sleeve Gastrectomy [15,16]. Before surgery, all patients used oral antidiabetic drugs and/or exogenous insulin, and even then, all had HbA1c above 7%. So, they were outside the therapeutic goal (HbA1c<7%) established by recognized international organizations. Twelve months after surgery, 90% of patients had HbA1c below 7% without the use of any antidiabetic medication. Midterm results of this procedure shown similar results and we hypothesized that sustained weight loss associated with better insulin sensitivity and continuous after-meal GLP-1 secretion may be the reason [17].
T2DM patients normally have decreased HDL-cholesterol, elevated triglycerides and LDL-cholesterol. After 12 months of surgery we observed normalization of HDL-cholesterol, LDL-cholesterol and triglycerides, with a significant difference compared to preoperative period. The obtained control of dyslipidemia in patients of the current study may have contributed to the improvement in sexual function [18]. It reinforces the data of several authors demonstrating that lipemic control is extremely important for endothelial dysfunction improvement, including erectile dysfunction. Dyslipidemia leads to a decreased production of nitric oxide (NO) and/or decreased NO dependent muscle relaxation. This may explain why even young dyslipidemic individuals have a higher prevalence of ED [19].
In this study, we were able to show 78% of patients with inability to vaginal penetration (EHGS 1 and 2) before surgery. After 12 months, 46% of patients still EHGS 1 and 2. Analyzing EHGS and IIEF compiled data we observed a significant difference between the findings pre- and postoperatively (p<0.05) in all spheres of sexuality analyzed by the test, i.e., erectile function, satisfaction with sexual intercourse, orgasmic function, sexual desire and overall satisfaction with sex life. Patients with uncontrolled DM present with lower rates of NO intracavernous synthesis. It is possible that the metabolic control obtained by II-SG may have improved NO synthesis and thereby favored erectile function. One of the weaknesses of this study is that we were unable to access this data. The number of patients and time of follow-up also account for [20].
Even though there has been no significant reduction in BMI, the observed weight loss, especially abdominal/visceral fat, may have contributed to the improvement in sexual function. Visceral fat can convert testosterone hormone (predominantly male) in estradiol hormone (predominantly female) and the first is essential for all sexual spheres. It is known that plasma concentration of testosterone is inversely proportional to BMI and DM2 patients may show a reduction in free testosterone [21]. Patients who did not show significant improvement in some spheres were precisely those who had diabetes duration over 15 years. These patients probably had micro and macrovascular irreversible injuries. Thus, even with the improvement of virtually all metabolic parameters following II-SG, these patients did not achieve the degree of improvement in all sexual spheres experienced by those with shorter disease.
Normal sexual function requires complex interaction between vascular, neurologic, hormonal and psychological systems [22]. It is possible that, in addition to metabolic control provided by the surgical procedure, other factors may contribute to the improvement in the sexual life of these patients. After II-SG most of them do not require everyday measurements of blood glucose, antidiabetic, antihypertensive and lipid lowering medications. This improves quality of life, triggers more willingness to work capacity, to sexual activity and physical activity.
Conclusion
The incidence of erectile dysfunction in patients with type 2 diabetes mellitus was 78% before surgery and 46% after 12 months. After 12 months postoperatively, significant improvement in erectile function, satisfaction with sexual intercourse, orgasmic function, sexual desire and sexual life of patients were seen.
Patients with diabetes duration over 15 years had lower responses in controlling diabetes mellitus and sexual dysfunction.
To More articles in Current Research in Diabetes & Obesity Journal Please click on: https://juniperpublishers.com/crdoj/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php
0 notes
Text
Prediabetes and Diabetes among Older Children with Obesity in a Diverse Northern California Population

Authored by Joan C Lo
Abstract
Purpose: The prevalence of prediabetes or diabetes was examined by race/ethnicity, weight and health behaviors among children with obesity to identify metabolic disparities and modifiable behaviors prior to adulthood.
Methods: Data were examined from 2296 children with obesity aged 10-17 years who were identified at well-child visits in 2012-2013, completed a questionnaire pertaining to dietary and lifestyle behaviors (including juice or sugar-sweetened beverage intake and exercise frequency) and had fasting glucose or hemoglobin A1C measured within 1 year of their visit. Obesity was classified as moderate or severe and glycemic status was examined using standard laboratory criteria for prediabetes and diabetes.
Results: Of 2296 children (mean age 13 years, 21% non-Hispanic white), the prevalence of prediabetes or diabetes was 33.1% overall, 9.6% among 2049 children by fasting glucose alone, and 43.2% among 1548 by hemoglobin A1C alone. The prevalence of prediabetes or diabetes varied substantially by race/ethnicity and increased with severity of obesity, but did not differ by exercise level or consumption of sugar sweetened beverage or juice.
Conclusion: One in three children with obesity had prediabetes or diabetes based on laboratory findings. The prevalence of prediabetes or diabetes increased with obesity severity and varied by race/ethnicity. Future studies should examine racial/ethnic differences in glycemic status, including variation by fasting glucose and hemoglobin A1C among these high risk children.
Keywords: Prediabetes; Adolescence; Body mass index; Obesity
Abbreviations: HbA1C: Hemoglobin A1C; OR: Odds Ratio
Introduction
Approximately 20.6% of U.S. adolescents aged 12-19 years are obese, an increase of nearly2-fold within the past 20 years [1]. The prevalence of prediabetes and diabetes has also increased among U.S. adolescents, based on fasting glucose levels [2] and/or hemoglobin A1C [3]. These conditions elevate the risk of cardiovascular disease in adulthood, although data from diverse pediatric populations receiving health care remain limited. In this study, we examined the prevalence of prediabetes and diabetes and associated health behaviors among northern California children with obesity to characterize their metabolic risk and identify modifiable behaviors prior to adulthood.
Methods
The source cohort included 4856 children aged 10-17 years with body mass index>95th percentile identified at well- child visits from 2012-2013 for Kaiser Permanente Northern California's Get Healthy Action Plan, a pediatric clinic-based weight program that assessed all children with elevated BMI at participating pediatric clinics [4]. Parents or teens were asked to complete a questionnaire about dietary and lifestyle behaviors, including juice or sugar-sweetened beverage (SSB) intake and exercise frequency. The study was approved by the Kaiser Permanente Northern California Institutional Review Board and the requirement for informed consent was waived due to the nature of the study. For these analyses, we examined data from the 2296 children with fasting glucose and/or HbAlC measured within 1 year of their visit. A fasting glucose of 100-125mg/dL or HbAlc of 5.7-6.4% defined prediabetes and higher values were considered diabetes range. Moderate and severe obesity were defined by a body mass index 100-119% and ≥120% of the 95th percentile, respectively. Subgroups were compared using the chi-square test, with a p-value criterion of <0.05 for statistical significance (SAS 9.4, Cary NC).
Results
Among 2296 children (mean age 13.1±2.2 years), 69.6% were age 10-14 years old. The cohort was extremely diverse, with 21.4% non-Hispanic white, 11.8% black, 46.1% Hispanic, 13.5% Asian/Pacific Islander and 7.2% other/unknown race. There were 761 (33.1%) individuals who met laboratory criteria for prediabetes (N=731, 31.8%) or diabetes (N=30, 1.3%), with a prevalence of9.6% among 2049 children by fasting glucose alone and 43.2% among 1548 children by HbA1C alone (with measurements). Notably, among the 1301 children with both tests obtained anytime within 1 year of the visit, 12.0% and 43.7% had prediabetes or diabetes by fasting glucose and HbA1C, respectively, with a prevalence of 46.2% by either test criteria.
Using data from fasting glucose, HbA1C or both to classify glycemic status, the prevalence of prediabetes or diabetes varied by race/ethnicity and was highest for black (47.6%) and Asian (39.7%) children followed by Hispanic (33.3%) and white children (21.8%, p<0.05). Prediabetes or diabetes prevalence was also was higher for moderate (28.3%) versus severe obesity (38.8% p<0.001; Table 1). Black (adjusted odds ratio, OR 3.1, 95% confidence interval CI 2.2-4.2), Asian (OR 2.5, 95% CI 1.8-3.4) and Hispanic (OR 1.8, 95% CI 1.4-2.3) children had a higher odds of prediabetes or diabetes than white children after accounting for age, sex and body mass index. Exercise and sugar sweetened beverage or juice intake did not differ significantly by prediabetes or diabetes status (T-able), with notably high proportions of children with (60.5%) and without (57.6%) prediabetes or diabetes consuming at least 2 sugar sweetened beverage/juice drinks per day.
*Row percentage among N=2296 with either fasting glucose (N=2049) or Hemoglobin A1c (N=1548) values.
**Among 2264 and 2235 respondents reporting sugar sweetened beverage (SSB)/juice intake and exercise level (for at least 60 minutes, excluding school physical education), respectively
Discussion
In a diverse population of children aged 10-17 years with obesity, 1 in 3 met criteria for prediabetes or diabetes, with only 1.3% in the diabetes range. The prevalence of prediabetes or diabetes also increased with obesity severity but did not differ by certain health behaviors. Our prediabetes estimate of 31.8% is higher than that reported for U.S. adolescents [5], as expected for an ethnically-diverse pediatric obesity cohort, but our observed prevalence based on fasting glucose compared to HbA1C criteria differs from national estimates [2]. Tester et al. [6] similarly reported a higher prediabetes prevalence using HbA1C (31.6%) compared to fasting glucose level (7.8%) in 1356 northern California children with obesity aged 2-19 years (36.0% and9.4% for adolescents, respectively). Whether differences in laboratory procedures or assays, selection for obesity, and ethnic or pediatric variation in the predictive value of HbA1C and fasting glucose thresholds contribute to these findings is unclear [7-9]. In this study, we combined findings from both fasting glucose and HbA1C to classify prediabetes and diabetes. However, future studies should also examine the extent to which race/ethnicity contributes to variation in glycemic status among children with obesity.
In summary, we observed a high prevalence of prediabetes or diabetes among children with obesity. While our data are cross-sectional and focus on a diverse community-based pediatric cohort in the healthcare setting, these findings also provide implications for population management. The much higher prevalence of prediabetes identified by HbA1C in our study and the limited sensitivity and predictive value of HbA1C thresholds and/or correlation with fasting glucose reported in other pediatric studies [7,9,10] underscore the need to determine the optimal screening test criteria for metabolic risk in children with obesity. In the meantime, continued efforts toward behavioral targets for weight reduction and improved glucose homeostasis are paramount to promoting prevention of metabolic disease in adulthood.
To Know More About Current Research in Diabetes & Obesity Journal Please click on:https://juniperpublishers.com/crdoj/index.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php
0 notes
Text
Potential Estrogenic Effects of Biofield Energy Treatment Using Human Endometrial Adenocarcinoma Cell Line
Authored by: Alice Branton*
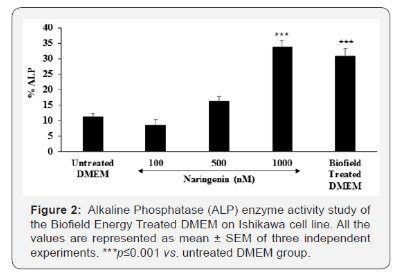
Introduction
Ishikawa cell line is a well‐differentiated human endometrial adenocarcinoma cell line, which was established to study the estrogenic potential due to the presence of estrogen and progesterone receptors (i.e., ERα and PR) [1]. Ishikawa cell line is derived from human endometrium that plays a significant role as a fertility-determining factor [2,3]. Hence, Ishikawa cell line was selected as a test system for this study. Continues basic research area in this field using this cell line like reproductive biology and molecular science, reported its vital role to compare its action using various parameters such as alkaline phosphate (ALP), a zinc-containing metalloenzymes. Human endometrial cell lines are the best characterized cell lines that are easy to cultivate for estrogenic potential. ALP is more abundant in liver, bone, and a small amount in placenta, which were denoted as ALP-1, ALP-2, and ALP-3, respectively.
Maintained the level of ALP is very important for conception as it significantly regulates the estrogen level and endometrium growth [4-6]. Various menstrual disorders take place in the presence of low level of ALP during implantation and conception. A decreased ALP level may be due to zinc deficiency, hypothyroidism, vitamin C deficiency, folic acid deficiency, excess vitamin D intake, low phosphorus levels, celiac disease, malnutrition with low protein assimilation, insufficient parathyroid gland function, pernicious anemia, vitamin B6 insufficiency, and also with the frequent use of synthetic contraceptive, which Results and Discussion in the loss of endocrine functions via estrogen receptor (ER) [7]. Thus, for identification of estrogenic potential, Ishikawa cell line was selected as a test system for this study in order to find the effect of the Biofield Energy Treated DMEM media for ALP as a biomarker.
As an alternative way of treatment, Complementary and Alternative Medicine (CAM) therapies are emerging as one of the best and safe way to treat against acute and chronic diseases [8]. Among CAM, Biofield Energy Healing Treatment (The Trivedi Effect®) one of the best approach that has provided a scientific groundwork in the past years by many renowned healers in order to understand the complex homeodynamic regulation of living systems [9]. National Institute of Health (NIH) and National Center for Complementary and Alternative Medicine (NCCAM) recommend and included various Energy Healing therapies such as natural products, deep breathing, yoga, Tai Chi, Qi Gong, chiropractic/osteopathic manipulation, meditation, massage, special diets, homeopathy, progressive relaxation, guided imagery, acupressure, acupuncture, relaxation techniques, hypnotherapy, healing touch, movement therapy, pilates, rolfing structural integration, mindfulness, Ayurvedic medicine, traditional Chinese herbs and medicines, naturopathy, essential oils, aromatherapy, Reiki, cranial sacral therapy and applied prayer under CAM category that has been accepted by the most of the U.S. population with several advantages [10].
The Trivedi Effect®- Consciousness Energy Healing Treatment contains a putative bioenergy, which is channeled by a renowned practitioner from a distance. Biofield Energy Healing as a CAM showed a significant result in biological studies [11]. The Trivedi Effect®- Consciousness Energy Healing Treatment has been reported with significant revolution in the physicochemical properties of metals, chemicals, ceramics and polymers [12-14], improved agricultural crop yield, productivity, and quality [15,16], transformed antimicrobial characteristics [17-19], biotechnology [20,21], improved bioavailability [22-24], skin health [25,26], nutraceuticals [27,28], cancer research [29,30], bone health [31- 33], human health and wellness.
In pursue with the outstanding Results and Discussion of Biofield Energy Healing Treatment outcome, authors in this study evaluates the impact of the Biofield Energy Treatment (The Trivedi Effect®) on DMEM as a test sample for estrogenic potential with respect to ALP parameter using standard in vitro assay in Ishikawa cells.
Materials & Methods
Chemicals and reagents
Naringenin was purchased from Sigma, India. Fetal bovine serum (FBS) and Dulbecco’s Modified Eagle’s Medium (DMEM) were purchased from Life Technology, USA. Antibiotics solution (penicillin-streptomycin) was procured from HiMedia, India, while 3-(4, 5-dimethyl-2-thiazolyl)-2, 5-diphenyl-2H-tetrazolium) (MTT), Direct Red 80, and ethylenediaminetetraacetic acid (EDTA) were purchased from Sigma, USA. All the other chemicals used in this experiment were analytical grade procured from India.
Cell culture
Ishikawa cell line (human endometrial adenocarcinoma) from human endometrial tissue was used as test system in the present study. Ishikawa cell line was maintained in DMEM growth medium for routine culture supplemented with 10% FBS. Growth conditions were maintained at 37 °C, 5% CO2, and 95% humidity and subcultured by trypsinisation followed by splitting the cell suspension into fresh flasks and supplementing with fresh cell growth medium. Before the start of the experiment, the growth medium of near-confluent cells was replaced with fresh phenolfree DMEM, supplemented with 10% charcoal-dextran stripped FBS (CD-FBS) and 1% penicillin-streptomycin for 3 days [34].
Experimental design
The experimental groups consisted of group 1 (G-I) the untreated DMEM. Group 2 (G-II) consisted of positive control at non-cytotoxic concentrations. Further, group 3 (G-III) included the Biofield Treated DMEM.
Consciousness energy healing treatment strategies
DMEM as the test item was divided into two parts, one part was treated with the Biofield Energy by a renowned Biofield Energy Healer (The Trivedi Effect®) and coded as the Biofield Energy Treated DMEM group, and the other part did not receive any sort of treatment and denoted as the untreated DMEM group. This Biofield Energy Healing Treatment was provided by Alice Branton remotely for ~5 minutes through the Healer’s unique Energy Transmission process to the test sample under laboratory conditions. Biofield Energy Healer was located in the USA, while the test items were located in the research laboratory of Dabur Research Foundation, New Delhi, India. Biofield Energy healer in this study never visited the laboratory in person, nor had any contact with the test item (DMEM medium). Further, the control group was treated with “sham” healer for comparative purposes. The “sham” healer did not have any knowledge about the Biofield Energy Treatment. After that, the Biofield Energy Treated and untreated samples were kept in similar sealed conditions for experimental study.
Identification of non-cytotoxic concentration
The cell viability was performed by MTT assay in human endometrial adenocarcinoma cell line (Ishikawa). The cells were counted and plated in 96-well plates at the density corresponding to 5 X 103 to 10 X 103 cells/well/180μL of cell growth medium. The above cells were incubated overnight under growth conditions and allowed the cell recovery and exponential growth, which were subjected to serum stripping or starvation. The cells were treated with the test items (DMEM) and positive control. The cells in the above plate(s) were incubated for a time point ranging from 24 to 72 hours in a CO2 incubator at 37 °C, 5% CO2, and 95% humidity. Following incubation, the plates were taken out and 20μL of 5mg/mL of MTT solution were added to all the wells followed by additional incubation for 3 hours at 37 °C. The supernatant was aspirated and 150μL of DMSO was added to each well to dissolve formazan crystals. The absorbance of each well was read at 540nm using Synergy HT microplate reader, BioTek, USA [35]. The percentage cytotoxicity at each tested concentrations of the test substance were calculated using the following equation (1):
Where,
X = Absorbance of treated cells;
R = Absorbance of untreated cells
The percentage cell viability corresponding to each treatment was obtained using the following equation (2):
The concentrations exhibiting ≥70% cell viability was considered as non-cytotoxic.
Study of alkaline phosphatase (ALP) activity
The cells were counted and plated in 96-well plates at the density corresponding to 5 X 103 cells/well/180μL phenol-free DMEM+ 10% CD-FBS. The above cells were incubated overnight under growth conditions for 48 hours in a CO2 incubator at 37°C, 5% CO2, and 95% humidity to allow the cell recovery and exponential growth. The above cells were incubated with the test samples or positive control for 6 days. Re-addition of the test sample or positive control was done on day 3. After incubation with the test samples, the ALP enzyme activity was determined by monitoring the hydrolysis of p-nitrophenyl phosphate to p-nitrophenol (pNPP). The cells were washed with 1X PBS and lysed by freeze-thaw method i.e., incubation at -80°C for 20 minutes followed by incubation at 37 °C for 10 minutes. Lysates were prepared in 0.1% triton-X. 50μL of substrate solution i.e., 10mM of pNPP in 1M diethanolamine and 0.24mM magnesium chloride (MgCl2) solution, pH 10.4 was added to all the wells containing 50μL of lysates followed by incubation for 1 hour at 37 °C. The absorbance of the above solution was recorded at 405nm using Synergy HT microplate reader. The percentage increase in ALP enzyme activity with respect to the untreated DMEM group was calculated using equation (3):
Where,
X = Absorbance of cells corresponding to positive control and test group
R = Absorbance of cells corresponding to untreated group
Statistical analysis
All the values were represented as Mean ± SEM (standard error of mean) of three independent experiments. The statistical analysis was performed using SigmaPlot statistical software (v11.0). For two groups comparison student’s t-test was used. For multiple group comparison, one-way analysis of variance (ANOVA) was used followed by post-hoc analysis by Dunnett’s test. Statistically significant values were set at the level of p≤0.05.
Results and Discussion
Cell viability study using MTT
The Biofield Energy Treated and untreated test samples were tested for cell viability using MTT assay in Ishikawa cells. The outcomes in terms of percentage cell viability are represented in Figure 1. The MTT data showed that the test samples were found to have significant cell viability after Biofield Energy Treatment by 98%, while in the naringenin (positive control) group the cell viability was 75% to 96%. Thus, the experimental MTT data suggested that the Biofield Energy Treated DMEM was found to be safe in the Ishikawa cells as compared with the untreated DMEM. Thus, DMEM was used to study the estrogenic potential (i.e., ALP activity) of The Trivedi Effect®- Biofield Energy Healing in vitro using human endometrial adenocarcinoma cell line (Ishikawa).
Alkaline phosphatase (ALP) enzyme activity
The level of ALP in terms of percentage change are presented in Figure 2. Naringenin, positive control showed a significantly increased the value of ALP by 43.75% and 200.89% (p≤0.001) at 500 and 1000nM, respectively with respect to the untreated DMEM group. The Biofield Energy Treated DMEM group showed a significant increased the ALP level by 30.8% as compared with the untreated DMEM group. Thus, the Biofield Energy Treated DMEM showed a significant increment of ALP, which play a major role in estrogen balance for conception. It might be highly significant in case of infertility and helpful against various menstrual disorders.
The scientific literature reported that decreased ALP level in placenta results in serious complications such as amyloidosis, granulation tissue, gastrointestinal inflammation such as inflammatory bowel disease, systemic infections, hypophosphatasia, postmenopausal women receiving estrogen therapy that is due to the osteoporosis, severe anemia, heart surgery, aplastic anemia, malnutrition, magnesium deficiency, hypothyroidism, chronic myelogenous leukemia, children with achondroplasia and cretinism, and pernicious anemia [35]. Thus, Biofield Energy Healing Treatment would significantly improved the estrogenic potential and worked as an index of osteoblastic differentiation as well as improved ALP enzyme activity [36]. Thus, in order to study the effect of Biofield Energy Treatment on DMEM, ALP level was significantly improved in Ishikawa cell line. It might be expected that Biofield Energy Treatment has altered the osteoblastic differentiation, which is due to an increased ALP enzyme level.
Conclusion
The Trivedi Effect®- Consciousness Energy Healing Treatment on DMEM was considered as a significant role to improve estrogenic potential with respect to increased level of ALP in Ishikawa cells. Cell viability data using MTT assay showed a significant improved cell viability after Biofield Energy Healing Treatment with 98% in the test sample group, while upto 96% in the positive control group signifies the high safety profile of the test samples. The level of ALP was significantly increased by 30.8% in the Biofield Energy Treated DMEM group as compared with the untreated DMEM group. Thus, The Trivedi Effect® on DMEM were found to have a significant impact on ALP level, which results in a better estrogenic potential and osteoblastic differentiation.
Therefore, with respect to the untreated DMEM, the Biofield Energy Treated DMEM would be highly significant in growth and viability of Ishikawa cells. Therefore, the Consciousness Energy Healing based DMEM might be a suitable alternative media for cell growth. It can be useful for the management of various estrogenic and menstrual disorders viz. Dysmenorrhea with painful cramps, Premenstrual Syndrome (PMS), Menorrhagia, Oligomenorrhea, Amenorrhea, and Missed periods. Thus, Biofield Energy Treatment would be useful to control the estrogen balance and thus control overall hormonal balance, which can be useful against stress, aging, osteoporosis, various bone diseases, cell differentiation, could improve cell-to-cell communication, normal cell growth, neurotransmission, cell cycling and proliferation, skin health, immune and cardiovascular functions. Besides, it controls various immune-related disease conditions such as Aplastic Anemia, Pernicious Anemia, Hepatitis, Sjogren Syndrome, Myasthenia Gravis, Parkinson’s Disease, Asthma, Atherosclerosis, Graves’ Disease, Dermatomyositis, Dermatitis, Diabetes, Multiple Sclerosis, Ulcerative Colitis, Alzheimer’s Disease, Irritable Bowel Syndrome, Systemic Lupus Erythematosus, stress, etc. with a safe therapeutic index to improve overall health and Quality of Life.
Acknowledgement
Authors are grateful to Dabur Research Foundation, Trivedi Global, Inc., Trivedi Science, Trivedi Testimonials, and Trivedi Master Wellness for their support throughout the work
#open access journals#Juniper Publsihers#reproductive health#peer review journals#GJORM in juniper publishers
0 notes
Text
Female Genital Tract Infection Caused by Streptococcus pneumoniae: Case Report
Authored b y: Manel Hamdoun*
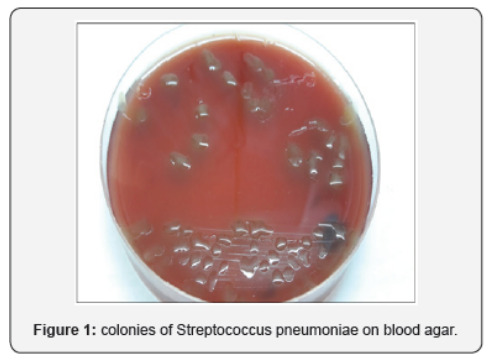
Introduction
Streptococcus pneumoniae is a commensal of the upper respiratory tract.It is a major cause of communityacquired pneumonia, bacteremia, meningitis, otitis, sinusitis, and carries a high burden of morbidity andmortality [1]. Furthermore, it is a less frequent cause of endocarditis, septic arthritis, and peritonitis [2].Uncommon colonization sites may cause rare clinical manifestations. We report the case of a pelvicinflammatory disease due to S.pneumoniain a menopaused woman with no predisposing factors.
Case Report
A 57-year-old woman with history of type 2 diabetes and high blood pressure was admitted to our hospital complaining of hypogastric pain and sustained fever. She was multiparous (4 children) and have had menopause since, one year and a half. The general physical exam found a fever of 38.8°C and tenderness in the right lower abdominal quadrant. Pelvic examination showed abundant green vaginal discharge and painful mobilization of the uterus. Vaginal and endocervical samples were then collected. The patient was otherwise normotensive with a pulse rate of 80bpm. On admission, blood tests showed hyperleucocytosis (15000/mm3) and C reactive protein of 66mg/l. Abdominal and pelvic ultrasound found a right juxta-ovarian collection with 2X2 cm dimensions. Intravenous antibiotic treatment was initiated (cirprofloxacin and amoxicillin+clavulanic acid). The patient had improved within 48h of antibiotherapy and was discharged at day five with oral treatment for 14 days. Bacteriological samples showed numerous polynuclear cells and the culture turned out positive after 48h incubation with many colonies of Streptococcus pneumoniae. The colonies on blood agar were very mucoid and surrounded by an ɑ hemolysis zone (Figure 1). Antibiogram showed sensitivity to penicillin and norfloxacin. Serotyping could not be performed.
Discussion
Pelvic inflammatory disease is a rare manifestation of pneumococcal infections. Although S.pneumoniae typically colonizes the upper respiratory tract, it can be part of the commensal flora of the female genital tract [3]. Prevalence of vaginal colonization with S.pneumoniae is unknown; Pneumococci were not isolated from normal vaginal flora in two ancient studies with a total of 294 gynecologic and 52 obstetric patients [4,5]. Darbas and Boyer reported seven isolates from 1064 vaginal secretions (0.75%), one isolate from 265 placentas, and one isolate from 40 intrauterine contraceptive devices (IUDs) that had been removed [6]. Changes in sexual practice (i.e., increased orogenital sex) and improved isolation techniques have been suggested as potential cause for the detection of S.pneumoniae in vaginal specimens [7]. However, although a history of receptive oral-anal sex was found to be associated with unstable vaginal flora and bacterial vaginosis, an association between sexual behavior and recovery of S.pneumoniae in vaginal specimens has not been reported [2]. Other transmission modes of pneumococci to the vagina could be a spread from the respiratory tract by hand contamination or hematogenous route [8].
Pneumococcal infection of the internal genital tract may give rise to endometritis, salpingitis, pelvic inflammatory disease, and abscesses and may be complicated by diffuse peritonitis. The symptoms and signs of these infections are in general not specific and rarely allow the clinician to suspect particular causative agents. Westh et al.[9]reported nine cases of pneumococcal infection of the female genital tract along with seven cases of pneumococcal bartholinitis. In their review, they found reports of 27 cases published between 1938 and 1988. One or more predisposing factors were discerned in most of the patients, mainly the use of intrauterine contraceptive devices (IUD) or changes secondary to the postpartum or postabortion period. The authors also pointed out the fact that pneumococcal genital infection was more common in the preantibiotic era than today, and the rate of lethality was high. During the last decade, more recent cases were reported by Gardien et al. [10], and Lemonye et al. [2]. When the infections occur, the route could be primary resident flora, gastrointestinal tract, lymphatics, or blood stream [11]. When S.pneumoniae is present in the adult vagina it can infects Bartholin’s glands [9]. From the vagina it can also ascend to the internal genitals; this type of infection is increased by the predisposing factors (IUD, postpartum state, instrumentation of the uterine cavity). No such factors were observed in our case.
Serotypes 1 and 3 are among the most incriminated serotypes in female genital infections [10]. The importance of these two serotypes in complicated female genital infections had previously been emphasized and their particular affinity for the genital tract suggested [12]. Genital infections can be handled without consequences when diagnosed early [10]. Their treatment is facilitated by the high proportion of penicillin-sensitive strains (high frequency of serotypes 1 and 3 which are hardly resistant to penicillin) as was the case of our patient.
#open access publishers#Juniper Publsihers#reproductive medicine#peer review journals#GJORM in juniper publishers
0 notes
Text
Human Factors: The Dirty Dozen in CTG misinterpretation
Authored by: Obianuju Nzelu*

Introduction
Human factors, often referred to as ergonomics, is an established scientific discipline used in many other safety critical disciplines [1], such as the aviation industry. It can be defined as the link between knowledge, the environment in which we work, personal circumstances, and communication between team members. Nowadays, in the Western World, most accidents and untoward outcomes are rarely due to a lack of resources. They are more likely due to human factors. The aviation industry and Obstetrics have as many similarities as differences. There is cross learning to be had from both disciplines, but inevitable adaptations need to be made. Both operate in highly technical environments, with highly specialized and multidisciplinary teams where the outcomes are expected to be good. In both aviation and maternity, accidents are rare, mostly unexpected, and very tragic events.
Cardiotocograph (CTG) is a non-invasive tool for the assessment of fetal wellbeing in labour. When interpreted and acted on correctly the CTG enables timely delivery to avoid hypoxic damage to the fetus, and it also prevents unnecessary intervention. However, 50 years after its introduction to clinical practice there is a wide range of subjective difference in the classification of CTGs [2]. In the National Health Service Litigation Authority (NHSLA) Obstetrics accounts for 50% of the total value of claims received [3]. Data shows that although the number of claims brought forward for cerebral palsy has remained stagnant, the amount paid out for this type of claim continues to increase – 220 claims in 2013-2014 with a claim amount >£733 million, 188 claims in 2015-2016 with a total amount of >£989 million.
The recent Each Baby Counts report analysed complete data relating to term stillbirths, neonatal deaths, and babies with brain injuries born following labour in 2015 in the UK. Fetal monitoring was highlighted as a commonly recurring contributory factor to these outcomes [4]. The problem is not new, in the Confidential Enquiry into Stillbirths and Deaths in Infancy (CESDI) 1997 report, again most of the criticism focused on electronic fetal monitoring [5].
In the last two decades there has been an emphasis on improving guidelines and training in the use of CTG to reduce hypoxia-induced perinatal morbidity and mortality. This was largely driven by recommendations from the CESDI report, which called for regular/rolling CTG teaching and simple guidelines on the interpretation, recognition, and communication of abnormal CTGs. The Each Baby Counts report goes further and highlights human factors as a major cause of error in CTG interpretation. This article aims to explore the different arms of human factors and how each relates to CTG interpretation. We will be using a framework devised by Gordon DuPont who was the first president of the Pacific Aircraft Maintenance Engineers Association [6]. He identified the 12 most common causes of maintenance personnel making an error in judgment, which ultimately results in a maintenance error. He called them the Dirty Dozen Errors in Maintenance [7] (Figure 1). In this article we will discuss each of the Dirty Dozen and apply them to common CTG misinterpretation themes. We will also discuss ways in which these might be mitigated or avoided in practice.
The Dirty Dozen
Lack of communication
Communication is the exchange of information and transference of meaning between individuals. In the context of CTG interpretation this often falls into either confirmation bias e.g. “this trace looks normal, don’t you think?”; or lack of appropriate escalation. Strategies to improve good communication include breaking down boundaries between members of the multidisciplinary team so that even the most junior member of staff can feel comfortable approaching the most senior clinician to ask for help. Structured messages are also designed to avoid missing important things and tend to be useful for documentation and for hand over, especially in the context of shift work – as happens on most labour wards. The best known tool is SBAR which stands for S – situation, B – background, A- assessment and R-recommendation, or specifically for CTG documentation the mnemonic DRCBrVADO (Figure 2).
Complacency
This insidious cause of error usually occurs as people become overconfident and rely on pattern recognition for CTG interpretation “I’ve seen this before and it was fine, it must be fine now”. It is easy to become complacent when using pre-designed stickers to define CTGs as you are less likely to take in the whole clinical picture and think of the physiology behind CTG changes [8]. For example, the same pattern on the CTG may be of different significance depending on the gestational age, the stage of labour, or the presence of meconium. This human factor is mitigated by reading each CTG individually, and in context of the specific woman and baby. Changing the language from “How is the CTG trace?” to “How is the baby?” may be a first step in encouraging clinicians to contextualise that particular fetus.
Lack of knowledge
On the whole clinicians are better at recognising hypoxic stress because decelerations are both audible and visible on the CTG. However, there is a lack of understanding of other causes of encephalopathy and neonatal death, such as anemia and sepsis, and how they manifest on the CTG (Figure 3). Training is the best safety net to address this human factor. The Each Baby Counts initiative called for maternity units to introduce annual mandatory CTG training before independent practice on labour wards. Within the training there must be an emphasis on understanding fetal physiology and how physiological changes are transcribed onto the CTG [9] (Figure 3), Chorioamnionitis: Increasing baseline fetal heart rate in the absence of significant decelerations should prompt the suspicion of chorioamnionitis. The term “uncomplicated tachycardia” gives false reassurance and should be avoided. In the presence of chorioamnionitis, delivery should be expedited if not imminent and superimposed hypoxic stress should be avoided.
Distraction
This is anything that takes your mind off a task even for a second. Our minds work faster than our hands, so a distraction can very quickly steer you away from the task at hand. On the labour ward it is important to maintain a helicopter view of events and if we are distracted or committed to a specific task that needs our full attention, it is important to hand the helicopter view role to another member of the team. Taking care of a patient in labour involves multiple tasks and placement of an epidural is typically the time when the CTG is neglected. Epidural analgesia can lead to maternal hypotension and consequently uterine hypoperfusion with potential acute hypoxic stress to the fetus. Awareness of the importance of monitoring during epidural placement and the use of centralised electronic CTG monitoring systems can help to mitigate these risks.
Lack of teamwork
The labour ward is made up of a large multidisciplinary team however, the individuals within the team change frequently. Consequently, we often work with people we have not worked with before. This makes it difficult to know everyone, how they work, and their strengths and limitations. For example, when managing a cord prolapse with prolonged fetal deceleration, delivery needs to be accomplished in the quickest and safest way. There should be clear delegation and division of roles to ensure a swift and co-ordinated resolution. This human factor can be mitigated by doing introductions at the start of each shift and conducting multidisciplinary simulation training on a regular basis.
Fatigue
Fatigue is a feeling of tiredness, reduced energy, and increased effort to perform tasks effectively and without errors [10]. This is particularly, but not exclusively, relevant to night shifts because human beings operate on a circadian rhythm where we are programmed to be awake in the day and asleep at night. In the aviation industry the hours between 2am and 6am are referred to as the “Window of Circadian Low” or WOCL, as it is the time when alertness and performance are most degraded [11]. In maternity this probably corresponds to a peak of activity. Recent research by University College London, University of London, and the National Childbirth Trust (NCT) found that more than 50% of births following spontaneous labour occur between 1am and 7am with a peak around 4am [12]. This human factor can be mitigated by adjusting staffing to levels of activity within each unit and providing facilities for rest breaks during shifts. Also, the use of a “Fetal Monitoring Checklist” can reduce the risk of missing preexisting fetal injury (Table 1) [13]. Forming a habit of asking these questions before reviewing all CTGs will help avoid this common pitfall, particularly when fatigued.
Lack of Resources as mentioned previously most errors in Western healthcare are not due to a lack of resources.
However, if stocks are not diligently checked and maintained before they are required errors can occur as a result. Regarding CTG interpretation, if the abdominal probe is not adequately recording the fetal heart rate it might be necessary to site a fetal scalp electrode. Although these may not be used on every shift, they are an important piece of equipment to have readily available. A complimentary problem is not the lack but the inadequate use of resources and equipment available. A typical problem on CTG monitoring is the Inadvertent use of paper scales to which staff are unaccustomed. For example, at 3 cm/min variability appears reduced to a clinician familiar with the 1 cm/min scale leading to erroneous interpretation of the CTG. Most countries throughout the world, including the UK, use 1 cm/min paper scales, the Netherlands use 2 cm/min, and North America and Japan use 3 cm/min. CTG machines also have a button to change the paper speed that can easily be inadvertently pushed when cleaning the machine.
Pressure
It is often presumed that pressure is mainly from the environment in which we work. However, many pressure-caused errors are due to self-pressure, where there is a false perception that we will be seen as incompetent if we ask for help. This human factor is mitigated by practicing effective prioritisation and delegation of tasks and asking for help when help is needed; even if this means escalation to senior members of the team who are off-site.
Lack of assertiveness
An example of lack of assertiveness is failing to speak up when things don’t seem right. This is most evident in departments where there is a strong system of hierarchy. For example, a junior midwife who is not comfortable approaching the consultant to review a CTG. They may prefer to wait for a senior midwife to become available, thereby delaying review of a potentially pathological trace. This human factor is mitigated by breaking down this “chain of command” culture and building a team where juniors can approach seniors without reproach.
Stress
Stress is the subconscious response to the demands placed upon us. This does not only relate to the working environment but our personal lives also. Stress can lead to errors when it is excessive as it acts as a distraction and reduces concentration levels when performing complex tasks such as CTG interpretation. This human factor is mitigated by maintaining awareness of it and finding ways to destress; whether it be taking time off work, exercising the body or relaxing the mind. Some hospitals have introduced initiatives to promote physical exercise, mindfulness and yoga to promote staff well-being and reduce medical error.
Lack of awareness
Lack of awareness occurs when there is a lack of alertness and vigilance. This human factor is closely linked with complacency. For example, when monitoring a twin pregnancy in labour a common error is monitoring the same twin twice, not noticing that both CTG traces are similar and from the same fetus, leaving one twin unmonitored. Situational awareness is also about our mental picture of what is happening around us and how it will evolve. An example again with twins, where after the delivery of twin one the doctor becomes fixated on the repair of a bleeding episiotomy without noticing the abnormal CTG of the second twin. Haemostasis of a vascular episiotomy can be achieved by simply clamping vessels or compression with a swab, leaving time and space to prioritise twin 2. Strategies to mitigate lack of situational awareness include promoting frequent safety huddles and avoiding single task fixation. Common contributors to loss of situation awareness have been already discussed such as lack of knowledge, stress, and fatigue.
Norms
Norms are unwritten rules followed or tolerated by most of the group, but negative norms can detract from as established safety standard. For example, the term “second stage CTG” is a negative norm sometimes used to classify CTGs. It implies a higher level of tolerance for a pathological trace on the anticipation that the baby will be shortly delivered. This is a dangerous practice and the guidelines for interpretation of the CTG in the first or second stage are the same. The second stage of labour brings an additional risk into the fetal monitoring: it becomes harder to monitor the fetal heart due to its low position in the pelvis; therefore, the risk of recording maternal pulse increases (Figure 4). It is unusual for a fetus to have accelerations during the second stage of labour, so if an improvement on the CTG trace or accelerations are noted in the second stage, especially if synchronous with contractions, it should be assumed that maternal heart rate is being monitored until proven otherwise. The use of a fetal scalp electrode instead of an abdominal transducer helps to mitigate this risk of confusing maternal with fetal pulse, leaving the fetus unmonitored in the latest phase of labour.
Conclusion
Obstetric practice and CTG interpretation put individuals, teams, and organisations under great pressure to make difficult decisions in dynamic and often unpredictable circumstances [3]. This combination of factors lead to errors in CTG interpretation. We believe that current guidelines and CTG training should focus on the following:
i. Fetal physiology and the physiological processes that underpin CTG appearances;
ii. the way in which human factors affect decision making. This is the key to reducing perinatal morbidity and mortality from intrapartum insults. Thus, the key points from this article in relation to CTG interpretation are as follows:
• Take in the whole picture when reviewing CTGs. Ask “how is the baby?”, not the CTG!
• Understand the physiology behind CTG changes, including the changes caused by infection/ inflammation, not only hypoxia.
• Break down hierarchical boundaries, feel free to ask and escalate
• Avoid negative norms such as “uncomplicated tachycardia” and “second stage CTG”
Declarations
#open access journals#peer review journals#Juniper Publsihers#reproductive health#GJORM in juniper publishers
0 notes
Text
Left Ventricular Hypertrophy and Coronary Artery Disease in Subjects with Metabolic Syndrome: Role of Adiposity and Total Plasma Adiponectin

Authored by Rosario Scaglione
Abstract
Objective: The principal objective of this study was to demonstrate the role of obesity and adiponectin (ADPN) in the occurrence of Left ventricular hypertrophy (LVH) in subjects with Metabolic Syndrome (MetS). The study population consisted of 79 patients affected by MetS, according to NCEP/ATPIII criteria, and 126 without MetS, utilized as controls. BMI, waist to hip ratio (WHR), mean blood pressure (MBP), ADPN levels and HOMA index were measured. Left ventricular internal diameter (LVID/h), interventricualr septal thickness (IVST), indexed LVM (LVMI), relative wall thickness (RWT), LV ejection fraction by echocardiography and diastolic parameters were calculated.
BMI (p<0.003), WHR (p<0.02), MBP (p<0.03) LVM, LVMI and IVST (p<0.001) were significantly higher and ADPN (p<0.001) was significantly lower in subjects with MetS than controls. In addition, prevalence of LVH (p< 0.002) and Coronary Artery Disease (CAD) (p<0.004) was greater in subjects with MetS than controls. ADPN and BMI resulted independently associated with LVMI also when single components of MetS were includes in the analysis.
Conclusion: Our data are consistent with an increased prevalence of LVH and CAD in patients with MetS. Increasing number of MetS components was associated to step-wise increased in LVMI. ADPN and BMI separately and additively may be considered as the best predictors of LVH and CAD in these subjects.
Keywords: Metabolic syndrome; Left ventricular hypertrophy; Adiponectin
Abbreviations: ADPN: Total Plasma Adiponectin; BMI: Body Mass Index; WHR: Waist To Hip Ratio; MBP: Mean Blood Pressure; HDL-C: High Density Lipoprotein Cholesterol; TC: Total Cholesterol; LDL: Low Density Lipoprotein Cholesterol; HOMA-IR: Homeostasis Model Assessment Of Insulin Resistance; LVM: Left Ventricular Mass; LVMI: Left Ventricular Mass/Height; LVID/h: Left Ventricular Internal Diameter/Height; IVST: Interventricular Septal Thcikness; RWT: Relative Wall Thickness; LVEF: Left Ventricular Ejection Fraction; E/A: Peak Early Transmitral Flow/ Peak Late Transmitral Flow; DTE: E Deceleration Time; IVRT: Isovolumic Relaxation Time; pts: Patients; LVH: Left Ventricular Hypertrophy; CAD: Coronary Artery Disease. LVMI: Left Ventricular Mass/Height; ADPN: Total Plasma Adiponectin; BMI: Body Mass Index; MBP: Mean Blood Pressure; HDL-C: High Density Lipoprotein Cholesterol
Introduction
Accumulation of intra-abdominal visceral fat and of adipocyte's dysfunction are considered the cellular basis of metabolic syndrome (MetS), associated with heightened risk for cardiovascular disease and cardiovascular mortality [1-4]. Population-based studies indicated an association between MetS and abnormal left ventricular (LV) geometry [5,6]. It is well known that several factors, both hemodynamic and non-hemodynamic, may be implicated in the increase of left ventricular mass (LVM) and wall thickness and thus in the occurrence of LV hypertrophy (LVH) [7,8]. In this field an important role has been attributed recently to adipose tissue dysfunction [1-3,9], a term indicating a state of hyper secretion of pro-atherogenic, pro-inflammatory and pro-diabetic adipocytokines, which is accompanied by a decreased production of adiponectin [9]. Adiponectin (ADPN) is an adipocyte-specific protein abundantly present in the plasma with well known anti-atherogenic, anti-diabetic and antiinflammatory properties [1-3,10].
Despite these findings, few studies addressed the influence of circulating ADPN in the development of LVH in subjects with MetS. The present study was designed to explain the interaction between ADPN and MetS on the cardiac damage. Accordingly, cardiac parameters and prevalence of LVH and coronary artery disease (CAD) were evaluated in patients with and without MetS. The principal objective of our study was to demonstrate that hypoadiponectinemia might be considered a nonhaemodynamic factor in the occurrence of LVH in subjects with MetS.
Subjects and Methods
Subjetcs
In this cross-sectional study, 205 consecutive outpatients referred to our center of hypertension and metabolic disease at the University of Palermo (Italy) from January 2013 to April 2014 because of BP or metabolic control related problems, were evaluated. The study population consisted of 79 patients affected by MetS, according to NCEP/ATPIII criteria [11], and 126 without MetS, utilized as controls.
A written informed consent was collected from all the subjects recruited. The protocol of this study was approved by the board of University of Palermo (Italy). Clinic examination, including medical history, measurements of body weight, height, blood pressure (BP) and resting electrocardiogram was assessed in all the subjects. Information regarding medical history, drug use, and alcohol and cigarette consumption was collected. Exclusion criteria included alcoholism and psychiatric problems. Body mass index was calculated as weight divided by squared height and expressed as kg/m2 and WHR by waist/ hip ratio [4]. Blood pressure (BP) was measured according to current recommendations with an appropriate large cuff in obese subjects. Systolic (SBP), diastolic (DBP) and mean (MBP) BP were determined. MBP was calculated by the sum of DBP plus one third of pulse pressure. According to ADA guidelines, the presence of diabetes was recognized from a fasting glycaemia >126mg/dl or the use of antidiabetic drugs or insulin [12]. Insulin resistance (IR) was recognized by the evaluation of homeostasis model assessment (HOMA) index.
In all the subjects the occurrence of LVH and the prevalence of coronary artery disease were evaluated. According to echocardiographic measurement, all the subjects with LVM normalized for height to the 2.7 power (LVMI) ≥50g/m2 for men and ≥47g/m2 for women were considered to have LVH [13].
The diagnosis of CAD was supported by history, symptoms of typical angina, cardiac markers and specific cardiac examinations, following guidelines of European Society of Cardiology [13].
Methods
Routine biochemical parameters were detected through standardized methods. An immunoradiometric assay (Biosource, Belgium) was used to measure serum insulin. The HOMA-IR was calculated using the following equation: HOMA-IR= fasting insulin (pmol/L X fasting glucose (mmol/L)/22.5. IR was defined as an HOMA-IR in the highest quintile of its distribution [12]. Adiponectin levels were measured by a validated competitive radioimmunoassay (Linco Research Inc., MO, USA) as previously described [4].
Measurements of left ventricular geometry and function were assessed by M and B-mode computerized echocardiography (ESAOTE, Italy). Accordingly, left ventricular internal diameter/ height (LVID/h), interventricular septum thickness (IVST), LVM normalized for height to the 2.7 power (LVMI) (14) were calculated. Recognition of LVH by LVM/h cut-offs has to be preferred since body surface area correction understimates LVM in the upper range of the body surface area distribution [14]. The relative wall thickness (RWT) by formula [(PWTd/LVIDd)x2] and left ventricular ejection fraction (LVEF) were also calculated with standardized method (4). Diastolic parameters, such as E/A ratio, isovolumic relaxation time (IVRT) and the deceleration time of E velocity (DTE) by echo-dopler examination were also calculated.
Statistical Analysis
Data are presented as mean±SD. Comparison between the groups were analyzed through the Man-Whitney U test was and comparisons between two proportions by Z test. Linear and multiple regression analysis were performed to study relationship among independent variables and LVMI. A p value <0.05 was used as cut-off for statistical significance. STAT/SE, version 9.2 for Windows (StataCorp. College Station, Texas), was used to analyze the data.
Results
Clinical characteristics, echocardiographic parameters and prevalence of LVH and CAD are available in Table 1. Both groups were matched with regard to sex and age. BMI (p<0.003), WHR (p<0.02), MBP (p<0.03) LVM, LVMI and IVST (p<0.001) were significantly higher and ADPN (p<0.001) was significantly lower in subjects with MetS than controls. In addition, prevalence of LVH (p< 0.002) and CAD (p<0.004) was greater in subjects with MetS than controls (Table 1). LVMI correlated directly with BMI (r=0.33; p<0.001), MBP (r=0.30; p<0.001), MetS (r=0.28 p<0.001) and inversely with ADPN (r=-0.55; p<0.0001). Multiple regression analysis was used to explain the interaction between ADPN and MetS and to test the independent role of risk factors for LVMI. ADPN and BMI resulted independently associated with LVMI also when single components of MetS were includes in the analysis. (Table 2).
Discussion
Our data indicate clearly that subjects with MetS were characterized by decreased ADPN, increased LVMI and higher prevalence of LVH and CAD respect to controls without MetS. The main finding of the study is the independent inverse relationship between ADPN and LVMI found by us in subjects with MetS. It is well known that MetS is often associated with LVH even if its role is partly independent from the effect of several determinants of LVM and it was not able to predict LVH independently of increased adiposity [15]. This finding is further supported by the independent LVMI/BMI relationship reported in this study. In addition circulating ADPN remained inversely and independently associated with LVMI, also when the single components of MetS were included in the analysis. To our knowledge, this is the first study to examine the role of ADPN on the changes in left ventricular geometry and on the prevalence of LVH and CAD in subjects with MetS. Our data are consistent with the suggestion that ADPN might be considered as an important nonhaemodynamic factor able to explain the occurrence of LVH in subjects at higher cardiometabolic risk [1-4,10]. These data suggest that increased risk of LVH due to a presence of MetS seems mediated mainly by adiposity and circulating ADPN which work as a non hemodynamic factors. Hypoadiponectinemia or functional ADPN resistance, perhaps secondary to down regulation of ADPN receptors, may contribute to an exaggerated hypertrophic response to hemodynamic load and to inappropriate LVH [1,2,16].
Some limitations of this study must be taken into account. First, our population is made exclusively of patients studied in the Centre of Hypertension and Metabolic Disease. This selection “bias” can explain the prevalence of MetS, diabetes, hypertension and dyslipidemia. Thus, our study is relevant for an important condition commonly found in “real life” medical practice. Second, we were not able to take into account all the details of all the different classes and subtypes of drugs assumed by the patients, which in turn might have affected the results obtained. However, this is a common limitation of many published works when “real practice” patients are studied. Third, it has been designed to be a cross-sectional study. Evaluation of the cause- effect relationship between ADPN and LVH would require a prospective study design with a cohort base and larger casistics. Therefore, we cannot prove causality or predictive ability, but only discern association.
Conclusion
In conclusion, in our patients with MetS, an increased prevalence of LVH and CAD has been found. Increasing number of MetS components was associated to step-wise increased in LVMI. ADPN and BMI separately and additively contribute to LVH in these subjects. Accordingly weight loss and increased ADPN levels may be useful to regress LVH. According to emerging data indicating that ADPN has to be considered as an important modulator of the adipovascular axis that affects the cardiometabolic risk profile, from the premetabolic syndrome, through MetS to overt atherosclerosis and that hypoadiponectinemia alone may represent an early phenomenon that long precedes the occurrence of all components of overt MetS [1,3,17], circulating ADPN might become a new target in the management and treatment of metabolic syndrome and it should be included among the criteria utilized to define MetS.
To Know More About Current Research in Diabetes & Obesity Journal Please click on: https://juniperpublishers.com/crdoj/index.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php
0 notes
Text
Antiobesity Activity of Liraglutide on High Fat Diet-Induced Obesity in Wistar Rats

Authored by Vinay Kumar
Abstract
Liraglutide is a glucagon like peptide-1 (GLP-1) analogue. GLP-1 is a potent inhibitor of motility and gastric emptying and has also been shown to inhibit gastric acid secretion. The inhibition of gastric emptying leads to decreased food intake and reduced body weight. The aim of the present study was to investigate the antiobesity effect of the Liraglutide on high fat diet (HFD) induced obesity in Wistar rats. Obesity was induced by oral feeding of HFD for six weeks. The antiobesity effect of Liraglutide (0.2mg/kg, i.p. for 14 days) in HFD fed rats was evaluated by the measurement of body mass index (BMI), body weight gain, food intake, hemodynamic changes (systolic, diastolic, mean blood pressure and heart rate), serum leptin, lipid profiles (triglycerides, total cholesterol, LDL-cholesterol, HDL-cholesterol), glucose. Organ (Liver) and visceral fat pad weights were measured. Liraglutide significantly reduced BMI, body weight gain, and mean blood pressure, serum leptin, lipids and glucose levels while it significantly increased the serum HDL-cholesterol, as compared to the HFD fed rats. The results of the present study suggest that a potential role of Liraglutide as a clinical tool for obesity treatment.
Keywords: Anti-obesity; High fat diet; Liraglutide; Leptin; Insulin.
Introduction
Obesity has increased at an alarming rate in recent years and is now a worldwide public health problem [1]. It is one of the most common nutritional disorders in humans. Obesity can be defined as syndrome characterized by an increase in body fat stores, mainly due to an imbalance between energy intake and energy expenditure. Obesity results when energy intake exceeds energy expenditure. The global epidemic of obesity is rapidly evolving as one of the major global health issues as it is frequently associated with a number of diseases with high mortality and morbidity such as diabetes, cancer, arthritis, hypertension, stroke, and myocardial infarction [2]. It is generally accepted that the tremendous rise in the obesity prevalence across the globe is driven primarily by a combination of increased calorie intake and decreased physical activity, and strongly influenced by our genetic background [3]. Obesity is associated with substantial increases in morbidity, premature mortality, impaired quality of life and large healthcare costs [4]. The major co-morbidities include type 2 diabetes, metabolic syndrome, hypertension, dyslipidaemia, myocardial infarction, stroke, certain cancers, sleep, apnoea and osteoarthritis [5]. Easy access to high-calorie packaged foods, sedentary lifestyles and a predilection for gizmos have resulted in almost 70% Indians in mega-cities such as Mumbai, Delhi, Bangalore or Chennai being overweight or obese, says a new multi-city survey. Diet and physical activity remain the cornerstones of therapy for obesity, although results have been disappointing. Obese patients who are able to lose weight by eating better and exercising generally regain the lost weight over time. The difficulty in maintaining long-term weight loss through behaviour modification has led to an increasing interest in other avenues of treatment, particularly pharmacotherapy. To date, only two medications-Sibutramine and Orlistat-have been approved for long-term use in the treatment of obesity and additional effective pharmacological treatments are needed [6].
Liraglutide is a glucagon-like peptide-1 receptor analogue, which is obtained by derivatising glucagon-like peptide-1 with a fatty acid. The liraglutide is well tolerated, sustains weight loss over 2 years and improves cardiovascular risk factors [7]. Liraglutide suppress the food intake and body weight in rats [8]. Obesity management is a modern challenge because of the rapid evolution of unfavorable lifestyles and unfortunately there are no safe and effective treatments applicable to the large majority of obese/overweight people [9]. Therefore, the present study was designed to investigate the antiobesity effect of Liraglutide on high fat diet induced obesity in Wistar rats.
Materials and Methods
Animals
The experimental study was carried out in male Wistar rats weighing 150-200g body weight and the experimental protocol was approved by Institutional Animal Ethics Committee (IAEC) of KIET School of Pharmacy, Ghaziabad (UP) (Registration number: 1099/07/CPCSEA, dated 27.07, 2007) as per the Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA) guidelines. The animals were kept in polypropylene cages (6 in each cage) under standard laboratory conditions (12 hrs. light and 12hrs. dark :: day : night cycle) and had free access to commercial pellet diet (Pranav Agro Industries, New Delhi) and water ad libitum. The animal house temperature was maintained at 25±2 °C and relative humidity was also maintained at 50±15%.
Induction of obesity by feeding high fat diet
Experimental obesity was induced by feeding of high fat diet consisting of the following materials (corn starch, casein, lard, cholesterol, sodium cholate, soybean oil, coconut oil, wheat bran, mineral mix, vitamin mix were added to 1kg of rat chow diet) to rats for period of six weeks.
Experimental design
30 male Wistar rats were included in the present study. Animals were randomly allocated into five groups of six animals each and treated as follows: Normal Control Group: Rats fed with normal rat chow diet for 6 weeks; High Fat Diet Control Group: Rats fed with high fat diet for 6 weeks; Liraglutide Treated Group: Rats fed with high fat diet for 6 weeks+from 29th day Liraglutide (0.2mg/kg, i.p) for 2 weeks; Orlistat Treated Group: Rats fed with high fat diet for 6 weeks+from 29th day Orlistat (10mg/kg, i.p) for 2 weeks; Perse Group: Rats fed with normal chow diet for 6 weeks+from 29th day Liraglutide for 2 weeks.
Measurement of anthropometric parameters
Body mass index (BMI kg/m2), daily food intake (g/d) and daily water intake (ml/d) were measured.
Measurement of hemodynamic parameters
Hemodynamic parameters (systolic, diastolic and mean arterial blood pressure) were measurement by non-invasive blood pressure recorder using rat tail-cuff method (AD Instrument, Australia).
Biochemical estimations in serum
Blood was collected from the retro-orbital plexus of the both groups of overnight fasted rats using microcapillary tubes on 29th day. Serum was separated by centrifugation (4000rpm, 10min) and transferred to Eppendorf tubes. The concentrations high density lipoprotein-cholesterol (Reckon Diagnostics Pvt. Ltd., Baroda, Gujarat, India), glucose, total cholesterol (TC) and triglycerides (TGs) (all the three from Span diagnostics Ltd., Surat, Gujarat, India), in serum were measured with commercial kits. The concentration of leptin in the serum was measured with rat leptin ELISA kit (BioVendor, Brno, Czech Republic).
Determination of Liver Weight and Visceral Fat Pad Weights
On the final day of experiment the rats were fasted overnight and sacrificed by cervical dislocation and then liver and visceral fat pads (epididymal, perirenal and mesentric) were removed, washed with normal saline and weighed [10].
Statistical analysis
All values were expressed as Mean IS Standard Error of Mean (S.E.M). Statistical analysis was performed using InStat 3Software. Groups of data were compared with the analysis of variance (ANOVA) followed by Dunnett's test. Values were considered statistically significant when p<0.05.
Results
Effect of liraglutide on BMI, food intake and water intake
All values were expressed as Mean±SEM, (n=6); aP<0.01 as compared to the Normal Control Group; bP<0.05 as compared to the high fat diet Group; cP>0.05 as compared to Normal Control Group.
The mean BMI, food intake and water intake were decreased the BMI, food intake and water intake as compared to significantly (p<0.01) increased in high fat diet fed group as the HFD treated group, while there was no significant changes compared to the normal control group. Liraglutide (0.2mg/kg,(p>0.05) in the BMI in perse group as compared to the normal i.p) and Orlistat (10mg/kg, i.p) treatment significantly (p<0.05)control group (Table 1).
Effect of liraglutide on hemodynamic parameters
All values were expressed as Mean±SEM, (n=6); aP<0.01 as compared Group; cP>0.05 as compared to Normal Control Group.
All hemodynamic parameters (systolic, diastolic, mean arterial BP and heart rate) were significantly increased (p<0.01) in high fat diet treated group as compared to the normal control group. All hemodynamic parameters were significantly decreased (p<0.01) in Liraglutide and Orlistat treated groups as compared to HFD treated group (Table 2).
Effect of liraglutide on serum leptin and glucose levels
All values were expressed as Mean±SEM, (n=6); aP<0.01 as compared to the Normal Control Group; bP<0.05 as compared to the high Fat Diet Group; cP>0.05 as compared to Normal Control Group.
All values were expressed as Mean±SEM, (n=6); aP<0.01 as compared to the Normal Control Group; bP<0.05 as compared to the high Fat Diet Group; cP>0.05 as compared to Normal Control Group.
Figure 1 & 2 shows that Liraglutide treatment serum leptin and glucose levels were significantly (p<0.01) increased in HFD treated rats as compared to the normal control rats. Serum leptin and glucose levels were significantly decreased in Liraglutide and Orlistat treated groups as compared to the HFD fed group.
Effect of liraglutide on serum lipid profile levels
HFD treated group showed significant (p<0.01) increased levels TC, TGs, low density lipoprotein-cholesterol (LDL-C) and very low density lipoprotein-cholesterol (VLDL-C) and while HDL-C levels significantly (p<0.01) decreased as compared to the normal control group. All these levels were significantly reversed in Liraglutide and Orlistat treated groups as compared to the HFD fed group (Table 3).
Effect of liraglutide on liver weight and visceral fat pad weights
Liver weight and visceral fat pad weights (mesenteric, perirenal and epididymal) were significantly increased in HFD fed group as compared to the normal control group. The visceral fat pad weights of perirenal fat, mesenteric and epididymal fat in the HFD + Liraglutide and HFD + orlistat groups were significantly (p<.001) decreased as compared with those of the HFD group (Table 4).
Discussion
Obesity is a medical condition in which excess body fat has been accumulated mainly due to sedentary life styles, lack of exercise and intake of energy rich high fat diet. The global prevalence of obesity is increasing rapidly among adults as well as among children and is associated with serious mortalities including a high incidence of type 2 diabetes, hyperlipidemia, hypercholesterolemia, fatty liver, cardiovascular diseases, osteroarthritis as well as an increased risk of many forms of cancer [11]. The currently available treatment options are not potent enough to control obesity permanently besides they produce side effects. Hence, there is a great demand for safer and long term effective drugs to treat this global epidemic problem. Hence, in the present work the anti-obesity activity of Liraglutide on high fat diet induced obesity in Wistar was investigated by analyzing the BMI, body weight, organ and fat pad weight and blood biochemical profiles. Dietary fat is calorically dense and extremely palatable. It is easily over consumed because it can cause less satiety than carbohydrate and protein [12]. Therefore, a HFD can lead to hyperphagia, weight gain, and increased adiposity. The feeding of HFD for 4 weeks produced a significant increase in body weight, total fat pad weight, basal/ fasting plasma glucose, insulin, basal triglyceride (TG) and total cholesterol (TC) levels in male rats [13]. In present study, there was significant increase in body mass index (BMI) and body weight gain in rats fed with high fat diet as compared to the normal control rats. BMI is a simple index of weight-for-height that is commonly used to classify underweight, overweight and obesity in adults [14]. This study corroborate with the findings of Altunkaynak [15] who reported that BMI was significantly increased in rats with high fat diet fed for 8 weeks as compared to the control group The increased body weight found in HFD rats might be due to the consumption of a diet rich in energy in the form of saturated fats (lard) and its deposition in various body fat pads and decreased energy expenditure.
Liraglutide (0.2mg/kg, i.p) and Orlistat (10mg/kg, i.p) treatment significantly (p<0.01) decreased the BMI and body weight gain as compared to the HFD treated group. Further, our results showed a significant (p<0.05) decrease in food intake and water intake by administration of Liraglutide (0.2 mg/kg, i.p). After 6 weeks feeding with HFD, hemodynamic parameters were significantly (p<0.01) elevated in HFD fed rats as compared to normal healthy control rats. Activation of the sympathetic nervous system contributes to blood pressure (BP) elevation in high-fat diet-induced obesity [16]. When HFD fed rats were treated with Liraglutide (0.2mg/kg, i.p), there were significant (p<0.01) decrease in hemodynamic changes.
In the present study, serum glucose and leptin levels were increased in the HFD group as compared to the normal control group, while glucose levels were significantly decreased by Orlistat and Liraglutide treatment. Diet-induced obesity dysregulated glucose homeostasis and causes hyperglycemia [17]. This is consistent with previous study that feeding of HFD for a period of 4 weeks produced a significant increase in plasma glucose levels. Fried et al. [18] indicated that basal levels of leptin are known to be strongly positively correlated with body fat on a HFD. A fat-enriched diet is regarded as an important factor in the development of cardiac diseases because it leads to the development of hyperlipidemia, atherosclerosis, and abnormal lipid metabolism [19]. The data of present study clearly showed that feeding of the HFD increased the concentrations of serum TC, LDL- C, VLDL-C, TGs in experimental rats. Lavie & Milani [20] indicated that obesity adversely affects plasma lipids, especially by increasing TC, LDL- C, VLDL-C, TGs and decreasing the level of HDL-cholesterol. The levels of TGs, TC, LDL- C, VLDL-C were significantly (p<0.01) decreased by Liraglutide (0.2mg/kg, i.p) and Orlistat treatment (10mg/kg, i.p) treatment groups. Organ's weight (liver) and visceral fat pad weights (perirenal, mesentric fat and epididymal fat) were significantly increased in rats fed with HFD. HFD produces adiposity i.e. deposition of fat on the adipose tissues. Liver weight and visceral fats were significantly decreased by Liraglutide.
Conclusion
The possible explanation for an anti-obesity effect of Liraglutide via suppression of dyslipidaemia, leptin, insulin, gastric emptying and reduction of appetite in obese rats fed with HFD. The results of the present study provide initial evidence that Liraglutide could be useful intervention for the treatment of obesity.
To Know More About Current Research in Diabetes & Obesity Journal Please click on:https://juniperpublishers.com/crdoj/index.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php
0 notes
Text
A Comparative Kap Study on Ragi, A Forgotten Wonder Grain with Oats among South Indian Families

Authored by Shaji Sreedhar KP
Abstract
Ragi (Finger millet) is a traditional South Indian food, that is associated with various health benefits like reduction of cholesterol, obesity, diabetes, atherosclerosis and malnutrition. Despite its nutritional value and affordability, the usage of ragi is minimal when compared to oats, another nutritionally important cereal.
In this study, the following were assessed:
Knowledge of South Indian women aged 25-50 years about the nutritional benefits of ragi and oats.
Attitude - the reasons for preferring oats over ragi.
Practice - the usage frequency of ragi and oats.
The study reveals that most of the people were ignorant about nutritional benefits of ragi in comparison to oats, an adopted food. The scores are above 6 out of 10 (mean score 7.5±1.1) for oats and less than 5 out of 10 (mean score 3±0.8) for ragi. The common reasons cited for preferring oats over ragi were less cooking time (95%), inspiration from advertisements and friends (94%) and ignorant about health benefits of ragi (91%). From this study, it was observed that 61.5% people use oats everyday whereas only 11.5% use ragi. In spite of having favourable growing conditions for cultivation and less priced than oats, there is decreased use of ragi as a staple food. Hence it is important to create awareness among the people and encourage its use.
Keywords: Ragi; Oats; KAP; Calcium; Anti-oxidants
Opinion
Ragi or finger millet (Eleusine Coracana) is one of the common cereal grown in India and a traditional food of South Indians since 1800 BC [1]. Though Indians consume cereals as the main staple providing 70-80% of total energy intake [2], the consumption of millets is very low compared to rice. A study by CURES (Chennai Urban Rural Epidemiology Studies) revealed that millets contributed to only about 2% of total calories [3], while almost half of the daily calories were derived from refined grains [4]. Another study [5], reported that the consumption of millets (consumption unit is a coefficient and 1 CU corresponds to energy requirement of 2400kcal/day of an Indian male doing sedentary work) was 75g/CU/day in Karnataka, 16g/CU/day in Andhra Pradesh, 3g/CU/day in Tamil Nadu and almost nil in Kerala. The increase in the incidence of lifestyle disorders like diabetes mellitus, systemic hypertension, dyslipidemia and obesity has lead to alternative adoption of foods like oats, which has high content of dietary fibres, phytochemicals, hypocholesterolaemic and anticancerous properties. However because of less favourable growing conditions in India, a higher proportion of oats consumed is chiefly imported, thereby increasing its cost.
Even though there are so many other millets like ragi which also possess similar health benefits and are comparatively cheaper, there is ignorance among people regarding their nutritional content. Hence this study was undertaken to assess the knowledge of South Indian women about the nutritional benefits of both ragi and oats, the frequency of usage and the reasons for preferring oats over ragi.
Methodology
A cross-sectional study was conducted among 260 South Indian women with age ranging from 25 to 50 years (mean age of 37.5±7.5), who involve in purchase of grocery and cooking for their families irrespective of their socio-economic status and education. A semi-structured questionnaire was designed to test the knowledge about nutritional benefits of ragi and oats for the score of 10 each. The frequency of usage was assessed with 3 point rating scale-daily, often (at least once in a week) and occasionally (during festivals and functions). An open question was asked to know the reasons for preferring ragi over oats and the responses were recorded and organized into categories by the researcher. Informed consent was taken from all the respondents for data collection. Descriptive and inferential statistics (t-test) were calculated.
Results
Knowledge
Every respondents knowledge about nutritive benefits of oats and ragi was assessed out of a total score of 10. The range of score about nutritive benefits of oats was from 6 to 9 (mean score 7.5±1.1), higher than that ofragi, which was ranging from 2 to 4 (mean score 3±0.8). The difference between the scores for both oats and ragi by the same individual varied from 2 to 7 (mean score 4.5±1.3). The t-test for two scores were done assuming unequal variance with hypothesis of mean difference 4.5, which is the mean value ofthe difference between the scores for nutritive benefits of oats and ragi. The observed difference between the mean (7.5-3) is not convincing enough to say that the average knowledge about nutritive benefits of oats and ragi differ significantly (p value=0.9) (Table 1). However the range of score proves that the knowledge about ragi is lesser than oats.
Attitude
The study reveals that the most common reasons for preferring oats over ragi (Figure 1) were less cooking time and convenience (95%), inspiration from advertisements and friends (94%) ignorance aboutnutritional benefits of ragi (91%), colour and texture (78%), social status (75%), palatability (55%), health experts advice (35%) and bored of cooking traditional varieties (14%).
Practice
From the study, it was observed that 61.5% of participants use oats on daily basis, whereas only 11.5% use ragi. Almost 32% use oats and 25% use ragi at least once in a week. The occasional use percentage of ragi: oats is 63.5: 6.5.
Discussion
Since the seed coat of ragi is five layered, it has more dietary fibre content (11.5g) [2,6] than oats (10.6g) [7], which include polysaccharides such as p-glucan, arabinoxylans and cellulose. They reduce the rate of cholesterol absorption by increasing the viscosity of gut contents [8] and causes binding of bile acids to increase the excretion of cholesterol [9]. Short chain fatty acids like butyric acid, which are produced by fermentation of dietary fibres in the large intestine are involved in countering colon cancer by modulating gene expression and inducing apoptosis [10]. Dietary fibre also serve as a substrate for gut microflora and promotes laxation [11]. Even though the concentration of proteins is low in ragi than oats, the prolamine fraction is high [12]. Prolamine contains the higher proportion of glutamic acid, proline, valine, isoleucine, leucine and phenylalanine. They are gluten-free [13] and are safe to be used in persons with celiac disease. The lipid content of oats (6.9g) is higher than ragi (1.3g) which causes poor flavour and excessive browning. It also has higher amount of lipases that cause rancidity and short storage life [14].
The calcium content of ragi (344mg) is higher than oats (54mg). Micronutrients like molybdenum, chromium, sulphur and vitamins like carotene, folic acid and choline are present in ragi while they are negligible in oats. Though Vitamin C is absent in both ragi and oats, ascorbic acid is formed in ragi during the process ofgermination and therefore the iron in ragi is easily absorbed [15]. Ragi is a very good source of phenolic compounds [16,17] like ferulic acid, caffeic acid and vanillic acid [18]. Polyphenolsplay a very important role in enhancing endothelial function [19], cellular signalling and anti inflammation [20], free radicals scavenging [21] and anti oxidant effect [22]. They also lower blood glucose by effective inhibition of a-glucosidase, pancreatic α-amylase and fructose induced albumin glycation [23]. In spite of having more nutritional value (Table 2), the usage of ragi is minimal mainly because of unawareness among the people regarding its health benefits. The convenience of easy cooking, advice from friends and health experts, colour, texture, palatability and a symbol of social status were other reasons for preferring oats. Even though 14% of people were bored of cooking traditional varieties, still ragi gained a higher occasional use in festive seasons. The Glycemic response (GR) of oats is generally lower than ragi. In most of the studies, GR was measured from venous samples but newer guidelines necessitate capillary glucose samples because of its greatest sensitivity for glycemic index (GI). Hence more studies and researches are further needed to determine the glycemic response for different preparations of ragi [24].
Limitations
The sample size small when compared to the actual population.
The study is limited by its reliance on retrospective self-report measures.
Conclusion
India is a country leading in both the spectrum oflife-style diseases and malnutrition. The consumption of ragi is associated with reduction of total plasma cholesterol, post-prandial blood glucose, obesity, atherosclerosis,development of cancer, rickets and osteoporosis. Ragi is superior to oats in bioavailability of minerals. The climatic conditions in India does not favour cultivation of oats andhence it is chiefly imported. However ragi has favourable growing conditions, which makes it economically affordable than oats. Our study revealed that the ignorance aboutnutritional benefits of ragi has led to its decreased usage. Hence it is important to create awareness among the people regarding its health benefits and encourage the use of ragi.
To Know More About Current Research in Diabetes & Obesity Journal Please click on: https://juniperpublishers.com/crdoj/index.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php
0 notes