#GJORM in juniper publsihers
Explore tagged Tumblr posts
Text
Sentinel Lymph Node Detection In Patients With Cervical Cancer
Authored by: Yasmina José Gutiérrez*

Introduction
The current standard of care for women who will be diagnosed with cervical cáncer includes radical hysterectomy or trachelectomy and bilateral pelvic lymphadenectomy. For women with early-stage cervical cancer, lymph node status is the most important prognosticator of survival. However, the majority of these patients will not have lymph node metastases. For women with cervical cancer, ideally we would optimize the identification of positive lymph node spread in the minority of patients while limiting the morbidity of lymph node dissection for the majority of women who will ultimately have negative nodes. For that reason, there is significant interest in validating lymphatic mapping and sentinel node biopsy for women with this disease.
The sentinel lymph node is the first node that receives drainage from the primary tumor. Therefore, if the sentinel lymph node is negative for metastasis, the remaining lymph nodes in the nodal basin should also be free of tumor. The use of lymphatic mapping and sentinel lymph node biopsy was first described by Cabanas in 1977. In an effort to decrease complications associated with lymphadenectomy, improve detection of micrometastatic disease, and fine tune our lymphadenectomy anatomic templates, sentinel lymph node (SLN) techniques have been developed and extensively studied in many oncologic fields. As a result, SLN technique is now part of the standard treatment guidelines for the management of breast cancer, melanoma, and more recently, it is being recognized as a safe and reasonable approach in select cases of vulvar cancer [1,2].
The objective of our study is Introduce sentinel lymph node detection in patients with cervical cáncer in our center and participe in the validation of the technique in a multicentric way [3].
Materials & Methods
Retrospective descriptive study of the cases of SLN in patients with cervical cáncer operated in our center from December 2013 to September 2018. We describe the procedure in our hospital, University Hospital Miguel Sevet from Zaragoza, Spain. The day before surgery 1mCi/0,5ml nanocoll Technetium 99m was applied into the cervix at 300, 600, 900, and 1200. Blue dye injection (Patentblue) occurred intraoperatively into the cervix at the same locations (Figures 1-2). Detector gamma probe for laparoscopy is used to perform intraoperative detection of sentynel lymph nodes (Figure 3) [4,5]. All the information about the patients and their datum were transcribed to an information base computerize. We used Statistic Process Social Sciences (SPSS) 20.0 for Windows (Copyright© SPSS Inc., 2006. Licencia Universidad de Zaragoza) to statistical analyses during the study period.
Results
Between December 2013 and September 2018, 15 patients with cervical cancer FIGO stage I, II and II underwent SLN detection during primary operation (radical laparoscopic hysterectomy) or in patients with non surgical stages to determine the condition of the nodes before radiotherapy (Figure 4) [5,6]. In all cases a lymphadenectomy was also performed in the same surgical act because it was an unvalidadted technique (Figure 5). The detection rate of SLN was 100%. The false-positive rate was 0 %. After the combined injection, the detection rate, especifcity, and positive predictive values were 100%. The sensitivity was 95%. There were only two false-negatives discovered. However, in one of these patients the positive node was found in a hemipelvis that did not map. A mean of 2.7 pelvic SLNs were detected [7].
Discussion
Multiple single institution studies have reported their experience with sentinel lymph node biopsy in cervical cancer patients. Though the type of tracer used in each of these studies is widely variable, almost all of them describe excellent negative predictive values, ranging from 88% – 100%. However, sensitivity appears to be more inconsistent. The senticol study is the largest multi-institutional trial of sentinel lymph node biopsy limited to women with early stage cervical cancer. In this study, 139 women with stage IA1 or IB1 cervical cancer underwent intracervical injection with radiocolloid and blue dye followed by sentinel node dissection and pelvic lymphadenectomy. The authors reported a detection rate of 97.8% and a sensitivity of 92%. There were only two false-negatives discovered. The study concluded that sentinel node mapping is a sensitive method for detecting lymph node metastasis for women with early-stage cervical cancer [8].
However, opponents have voiced concern that some nodal metastases may be missed if only the sentinel lymph nodes are removed. A high sensitivity of sentinel lymph nodes (SLN) for pelvic lymph node staging has been repeatedly shown in patients with cervical cancer. However, since only SLN are evaluated by pathologic ultrastaging, the risk of small metastases, including small macrometastases and micrometastases, in non-SLN is unknown. This can be a critical limitation for the oncological safety of abandoning a pelvic lymphadenectomy. Mapping sentinel lymph nodes is popular among gynecologist- oncologists, which lead to having fewer side effects in patients who suffer from cervical cancer. Thus, more researches are required to confirm the total removal of lymph nodes in patients with sentinel lymph nodes positive [9]. The presence of an effective team (composed of an expert gynecologist- oncologist and nuclear medicine team) is an important factor to have a successful surgery with an acceptable diagnostic power, less invasive operations, and better clinical management.
Conclusion
Sentinel lymph node detection in patients with cervical cáncer is a multidisciplinary procedure involving gynecologists, pathologists and nuclear medicine. Until the validation of the techinque, lymphadenectomy will be performed in the same surgical act to all patients in order to obtain data on the reliability of the procedure. According to the previous consensus, the defined validation parameters are al least 95% of the sentinel node identification rate and false-negative rate ≤5%. The validation of the techinque will allow to avoid morbidity to patients with early stages and to select patients with affected lymph nodes candidates for radiochemoterapy without the need for radical pelvic surgery.
#open access journals#Juniper Publsihers#reproductive health#GJORM in juniper publsihers#peer review journals
1 note
·
View note
Text
Potential Estrogenic Effects of Biofield Energy Treatment Using Human Endometrial Adenocarcinoma Cell Line
Authored by: Alice Branton*
Introduction
Ishikawa cell line is a well‐differentiated human endometrial adenocarcinoma cell line, which was established to study the estrogenic potential due to the presence of estrogen and progesterone receptors (i.e., ERα and PR) [1]. Ishikawa cell line is derived from human endometrium that plays a significant role as a fertility-determining factor [2,3]. Hence, Ishikawa cell line was selected as a test system for this study. Continues basic research area in this field using this cell line like reproductive biology and molecular science, reported its vital role to compare its action using various parameters such as alkaline phosphate (ALP), a zinc-containing metalloenzymes. Human endometrial cell lines are the best characterized cell lines that are easy to cultivate for estrogenic potential. ALP is more abundant in liver, bone, and a small amount in placenta, which were denoted as ALP-1, ALP-2, and ALP-3, respectively.
Maintained the level of ALP is very important for conception as it significantly regulates the estrogen level and endometrium growth [4-6]. Various menstrual disorders take place in the presence of low level of ALP during implantation and conception. A decreased ALP level may be due to zinc deficiency, hypothyroidism, vitamin C deficiency, folic acid deficiency, excess vitamin D intake, low phosphorus levels, celiac disease, malnutrition with low protein assimilation, insufficient parathyroid gland function, pernicious anemia, vitamin B6 insufficiency, and also with the frequent use of synthetic contraceptive, which Results and Discussion in the loss of endocrine functions via estrogen receptor (ER) [7]. Thus, for identification of estrogenic potential, Ishikawa cell line was selected as a test system for this study in order to find the effect of the Biofield Energy Treated DMEM media for ALP as a biomarker.
As an alternative way of treatment, Complementary and Alternative Medicine (CAM) therapies are emerging as one of the best and safe way to treat against acute and chronic diseases [8]. Among CAM, Biofield Energy Healing Treatment (The Trivedi Effect®) one of the best approach that has provided a scientific groundwork in the past years by many renowned healers in order to understand the complex homeodynamic regulation of living systems [9]. National Institute of Health (NIH) and National Center for Complementary and Alternative Medicine (NCCAM) recommend and included various Energy Healing therapies such as natural products, deep breathing, yoga, Tai Chi, Qi Gong, chiropractic/osteopathic manipulation, meditation, massage, special diets, homeopathy, progressive relaxation, guided imagery, acupressure, acupuncture, relaxation techniques, hypnotherapy, healing touch, movement therapy, pilates, rolfing structural integration, mindfulness, Ayurvedic medicine, traditional Chinese herbs and medicines, naturopathy, essential oils, aromatherapy, Reiki, cranial sacral therapy and applied prayer under CAM category that has been accepted by the most of the U.S. population with several advantages [10].
The Trivedi Effect®- Consciousness Energy Healing Treatment contains a putative bioenergy, which is channeled by a renowned practitioner from a distance. Biofield Energy Healing as a CAM showed a significant result in biological studies [11]. The Trivedi Effect®- Consciousness Energy Healing Treatment has been reported with significant revolution in the physicochemical properties of metals, chemicals, ceramics and polymers [12-14], improved agricultural crop yield, productivity, and quality [15,16], transformed antimicrobial characteristics [17-19], biotechnology [20,21], improved bioavailability [22-24], skin health [25,26], nutraceuticals [27,28], cancer research [29,30], bone health [31- 33], human health and wellness.
In pursue with the outstanding Results and Discussion of Biofield Energy Healing Treatment outcome, authors in this study evaluates the impact of the Biofield Energy Treatment (The Trivedi Effect®) on DMEM as a test sample for estrogenic potential with respect to ALP parameter using standard in vitro assay in Ishikawa cells.
Materials & Methods
Chemicals and reagents
Naringenin was purchased from Sigma, India. Fetal bovine serum (FBS) and Dulbecco’s Modified Eagle’s Medium (DMEM) were purchased from Life Technology, USA. Antibiotics solution (penicillin-streptomycin) was procured from HiMedia, India, while 3-(4, 5-dimethyl-2-thiazolyl)-2, 5-diphenyl-2H-tetrazolium) (MTT), Direct Red 80, and ethylenediaminetetraacetic acid (EDTA) were purchased from Sigma, USA. All the other chemicals used in this experiment were analytical grade procured from India.
Cell culture
Ishikawa cell line (human endometrial adenocarcinoma) from human endometrial tissue was used as test system in the present study. Ishikawa cell line was maintained in DMEM growth medium for routine culture supplemented with 10% FBS. Growth conditions were maintained at 37 °C, 5% CO2, and 95% humidity and subcultured by trypsinisation followed by splitting the cell suspension into fresh flasks and supplementing with fresh cell growth medium. Before the start of the experiment, the growth medium of near-confluent cells was replaced with fresh phenolfree DMEM, supplemented with 10% charcoal-dextran stripped FBS (CD-FBS) and 1% penicillin-streptomycin for 3 days [34].
Experimental design
The experimental groups consisted of group 1 (G-I) the untreated DMEM. Group 2 (G-II) consisted of positive control at non-cytotoxic concentrations. Further, group 3 (G-III) included the Biofield Treated DMEM.
Consciousness energy healing treatment strategies
DMEM as the test item was divided into two parts, one part was treated with the Biofield Energy by a renowned Biofield Energy Healer (The Trivedi Effect®) and coded as the Biofield Energy Treated DMEM group, and the other part did not receive any sort of treatment and denoted as the untreated DMEM group. This Biofield Energy Healing Treatment was provided by Alice Branton remotely for ~5 minutes through the Healer’s unique Energy Transmission process to the test sample under laboratory conditions. Biofield Energy Healer was located in the USA, while the test items were located in the research laboratory of Dabur Research Foundation, New Delhi, India. Biofield Energy healer in this study never visited the laboratory in person, nor had any contact with the test item (DMEM medium). Further, the control group was treated with “sham” healer for comparative purposes. The “sham” healer did not have any knowledge about the Biofield Energy Treatment. After that, the Biofield Energy Treated and untreated samples were kept in similar sealed conditions for experimental study.
Identification of non-cytotoxic concentration
The cell viability was performed by MTT assay in human endometrial adenocarcinoma cell line (Ishikawa). The cells were counted and plated in 96-well plates at the density corresponding to 5 X 103 to 10 X 103 cells/well/180μL of cell growth medium. The above cells were incubated overnight under growth conditions and allowed the cell recovery and exponential growth, which were subjected to serum stripping or starvation. The cells were treated with the test items (DMEM) and positive control. The cells in the above plate(s) were incubated for a time point ranging from 24 to 72 hours in a CO2 incubator at 37 °C, 5% CO2, and 95% humidity. Following incubation, the plates were taken out and 20μL of 5mg/mL of MTT solution were added to all the wells followed by additional incubation for 3 hours at 37 °C. The supernatant was aspirated and 150μL of DMSO was added to each well to dissolve formazan crystals. The absorbance of each well was read at 540nm using Synergy HT microplate reader, BioTek, USA [35]. The percentage cytotoxicity at each tested concentrations of the test substance were calculated using the following equation (1):
Where,
X = Absorbance of treated cells;
R = Absorbance of untreated cells
The percentage cell viability corresponding to each treatment was obtained using the following equation (2):
The concentrations exhibiting ≥70% cell viability was considered as non-cytotoxic.
Study of alkaline phosphatase (ALP) activity
The cells were counted and plated in 96-well plates at the density corresponding to 5 X 103 cells/well/180μL phenol-free DMEM+ 10% CD-FBS. The above cells were incubated overnight under growth conditions for 48 hours in a CO2 incubator at 37°C, 5% CO2, and 95% humidity to allow the cell recovery and exponential growth. The above cells were incubated with the test samples or positive control for 6 days. Re-addition of the test sample or positive control was done on day 3. After incubation with the test samples, the ALP enzyme activity was determined by monitoring the hydrolysis of p-nitrophenyl phosphate to p-nitrophenol (pNPP). The cells were washed with 1X PBS and lysed by freeze-thaw method i.e., incubation at -80°C for 20 minutes followed by incubation at 37 °C for 10 minutes. Lysates were prepared in 0.1% triton-X. 50μL of substrate solution i.e., 10mM of pNPP in 1M diethanolamine and 0.24mM magnesium chloride (MgCl2) solution, pH 10.4 was added to all the wells containing 50μL of lysates followed by incubation for 1 hour at 37 °C. The absorbance of the above solution was recorded at 405nm using Synergy HT microplate reader. The percentage increase in ALP enzyme activity with respect to the untreated DMEM group was calculated using equation (3):
Where,
X = Absorbance of cells corresponding to positive control and test group
R = Absorbance of cells corresponding to untreated group
Statistical analysis
All the values were represented as Mean ± SEM (standard error of mean) of three independent experiments. The statistical analysis was performed using SigmaPlot statistical software (v11.0). For two groups comparison student’s t-test was used. For multiple group comparison, one-way analysis of variance (ANOVA) was used followed by post-hoc analysis by Dunnett’s test. Statistically significant values were set at the level of p≤0.05.
Results and Discussion
Cell viability study using MTT
The Biofield Energy Treated and untreated test samples were tested for cell viability using MTT assay in Ishikawa cells. The outcomes in terms of percentage cell viability are represented in Figure 1. The MTT data showed that the test samples were found to have significant cell viability after Biofield Energy Treatment by 98%, while in the naringenin (positive control) group the cell viability was 75% to 96%. Thus, the experimental MTT data suggested that the Biofield Energy Treated DMEM was found to be safe in the Ishikawa cells as compared with the untreated DMEM. Thus, DMEM was used to study the estrogenic potential (i.e., ALP activity) of The Trivedi Effect®- Biofield Energy Healing in vitro using human endometrial adenocarcinoma cell line (Ishikawa).
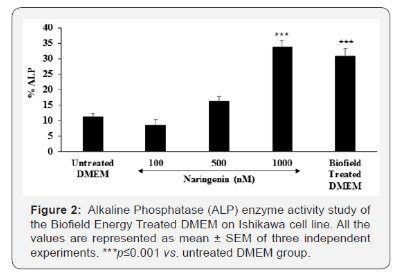
Alkaline phosphatase (ALP) enzyme activity
The level of ALP in terms of percentage change are presented in Figure 2. Naringenin, positive control showed a significantly increased the value of ALP by 43.75% and 200.89% (p≤0.001) at 500 and 1000nM, respectively with respect to the untreated DMEM group. The Biofield Energy Treated DMEM group showed a significant increased the ALP level by 30.8% as compared with the untreated DMEM group. Thus, the Biofield Energy Treated DMEM showed a significant increment of ALP, which play a major role in estrogen balance for conception. It might be highly significant in case of infertility and helpful against various menstrual disorders.
The scientific literature reported that decreased ALP level in placenta results in serious complications such as amyloidosis, granulation tissue, gastrointestinal inflammation such as inflammatory bowel disease, systemic infections, hypophosphatasia, postmenopausal women receiving estrogen therapy that is due to the osteoporosis, severe anemia, heart surgery, aplastic anemia, malnutrition, magnesium deficiency, hypothyroidism, chronic myelogenous leukemia, children with achondroplasia and cretinism, and pernicious anemia [35]. Thus, Biofield Energy Healing Treatment would significantly improved the estrogenic potential and worked as an index of osteoblastic differentiation as well as improved ALP enzyme activity [36]. Thus, in order to study the effect of Biofield Energy Treatment on DMEM, ALP level was significantly improved in Ishikawa cell line. It might be expected that Biofield Energy Treatment has altered the osteoblastic differentiation, which is due to an increased ALP enzyme level.
Conclusion
The Trivedi Effect®- Consciousness Energy Healing Treatment on DMEM was considered as a significant role to improve estrogenic potential with respect to increased level of ALP in Ishikawa cells. Cell viability data using MTT assay showed a significant improved cell viability after Biofield Energy Healing Treatment with 98% in the test sample group, while upto 96% in the positive control group signifies the high safety profile of the test samples. The level of ALP was significantly increased by 30.8% in the Biofield Energy Treated DMEM group as compared with the untreated DMEM group. Thus, The Trivedi Effect® on DMEM were found to have a significant impact on ALP level, which results in a better estrogenic potential and osteoblastic differentiation.
Therefore, with respect to the untreated DMEM, the Biofield Energy Treated DMEM would be highly significant in growth and viability of Ishikawa cells. Therefore, the Consciousness Energy Healing based DMEM might be a suitable alternative media for cell growth. It can be useful for the management of various estrogenic and menstrual disorders viz. Dysmenorrhea with painful cramps, Premenstrual Syndrome (PMS), Menorrhagia, Oligomenorrhea, Amenorrhea, and Missed periods. Thus, Biofield Energy Treatment would be useful to control the estrogen balance and thus control overall hormonal balance, which can be useful against stress, aging, osteoporosis, various bone diseases, cell differentiation, could improve cell-to-cell communication, normal cell growth, neurotransmission, cell cycling and proliferation, skin health, immune and cardiovascular functions. Besides, it controls various immune-related disease conditions such as Aplastic Anemia, Pernicious Anemia, Hepatitis, Sjogren Syndrome, Myasthenia Gravis, Parkinson’s Disease, Asthma, Atherosclerosis, Graves’ Disease, Dermatomyositis, Dermatitis, Diabetes, Multiple Sclerosis, Ulcerative Colitis, Alzheimer’s Disease, Irritable Bowel Syndrome, Systemic Lupus Erythematosus, stress, etc. with a safe therapeutic index to improve overall health and Quality of Life.
Acknowledgement
Authors are grateful to Dabur Research Foundation, Trivedi Global, Inc., Trivedi Science, Trivedi Testimonials, and Trivedi Master Wellness for their support throughout the work
#open access journals#Juniper Publsihers#reproductive health#peer review journals#GJORM in juniper publishers
0 notes
Text
Female Genital Tract Infection Caused by Streptococcus pneumoniae: Case Report
Authored b y: Manel Hamdoun*
Introduction
Streptococcus pneumoniae is a commensal of the upper respiratory tract.It is a major cause of communityacquired pneumonia, bacteremia, meningitis, otitis, sinusitis, and carries a high burden of morbidity andmortality [1]. Furthermore, it is a less frequent cause of endocarditis, septic arthritis, and peritonitis [2].Uncommon colonization sites may cause rare clinical manifestations. We report the case of a pelvicinflammatory disease due to S.pneumoniain a menopaused woman with no predisposing factors.
Case Report
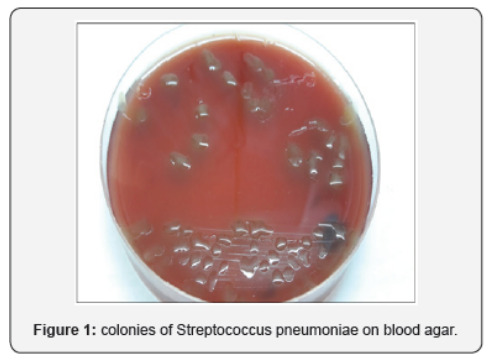
A 57-year-old woman with history of type 2 diabetes and high blood pressure was admitted to our hospital complaining of hypogastric pain and sustained fever. She was multiparous (4 children) and have had menopause since, one year and a half. The general physical exam found a fever of 38.8°C and tenderness in the right lower abdominal quadrant. Pelvic examination showed abundant green vaginal discharge and painful mobilization of the uterus. Vaginal and endocervical samples were then collected. The patient was otherwise normotensive with a pulse rate of 80bpm. On admission, blood tests showed hyperleucocytosis (15000/mm3) and C reactive protein of 66mg/l. Abdominal and pelvic ultrasound found a right juxta-ovarian collection with 2X2 cm dimensions. Intravenous antibiotic treatment was initiated (cirprofloxacin and amoxicillin+clavulanic acid). The patient had improved within 48h of antibiotherapy and was discharged at day five with oral treatment for 14 days. Bacteriological samples showed numerous polynuclear cells and the culture turned out positive after 48h incubation with many colonies of Streptococcus pneumoniae. The colonies on blood agar were very mucoid and surrounded by an ɑ hemolysis zone (Figure 1). Antibiogram showed sensitivity to penicillin and norfloxacin. Serotyping could not be performed.
Discussion
Pelvic inflammatory disease is a rare manifestation of pneumococcal infections. Although S.pneumoniae typically colonizes the upper respiratory tract, it can be part of the commensal flora of the female genital tract [3]. Prevalence of vaginal colonization with S.pneumoniae is unknown; Pneumococci were not isolated from normal vaginal flora in two ancient studies with a total of 294 gynecologic and 52 obstetric patients [4,5]. Darbas and Boyer reported seven isolates from 1064 vaginal secretions (0.75%), one isolate from 265 placentas, and one isolate from 40 intrauterine contraceptive devices (IUDs) that had been removed [6]. Changes in sexual practice (i.e., increased orogenital sex) and improved isolation techniques have been suggested as potential cause for the detection of S.pneumoniae in vaginal specimens [7]. However, although a history of receptive oral-anal sex was found to be associated with unstable vaginal flora and bacterial vaginosis, an association between sexual behavior and recovery of S.pneumoniae in vaginal specimens has not been reported [2]. Other transmission modes of pneumococci to the vagina could be a spread from the respiratory tract by hand contamination or hematogenous route [8].
Pneumococcal infection of the internal genital tract may give rise to endometritis, salpingitis, pelvic inflammatory disease, and abscesses and may be complicated by diffuse peritonitis. The symptoms and signs of these infections are in general not specific and rarely allow the clinician to suspect particular causative agents. Westh et al.[9]reported nine cases of pneumococcal infection of the female genital tract along with seven cases of pneumococcal bartholinitis. In their review, they found reports of 27 cases published between 1938 and 1988. One or more predisposing factors were discerned in most of the patients, mainly the use of intrauterine contraceptive devices (IUD) or changes secondary to the postpartum or postabortion period. The authors also pointed out the fact that pneumococcal genital infection was more common in the preantibiotic era than today, and the rate of lethality was high. During the last decade, more recent cases were reported by Gardien et al. [10], and Lemonye et al. [2]. When the infections occur, the route could be primary resident flora, gastrointestinal tract, lymphatics, or blood stream [11]. When S.pneumoniae is present in the adult vagina it can infects Bartholin’s glands [9]. From the vagina it can also ascend to the internal genitals; this type of infection is increased by the predisposing factors (IUD, postpartum state, instrumentation of the uterine cavity). No such factors were observed in our case.
Serotypes 1 and 3 are among the most incriminated serotypes in female genital infections [10]. The importance of these two serotypes in complicated female genital infections had previously been emphasized and their particular affinity for the genital tract suggested [12]. Genital infections can be handled without consequences when diagnosed early [10]. Their treatment is facilitated by the high proportion of penicillin-sensitive strains (high frequency of serotypes 1 and 3 which are hardly resistant to penicillin) as was the case of our patient.
#open access publishers#Juniper Publsihers#reproductive medicine#peer review journals#GJORM in juniper publishers
0 notes
Text
Human Factors: The Dirty Dozen in CTG misinterpretation
Authored by: Obianuju Nzelu*

Introduction
Human factors, often referred to as ergonomics, is an established scientific discipline used in many other safety critical disciplines [1], such as the aviation industry. It can be defined as the link between knowledge, the environment in which we work, personal circumstances, and communication between team members. Nowadays, in the Western World, most accidents and untoward outcomes are rarely due to a lack of resources. They are more likely due to human factors. The aviation industry and Obstetrics have as many similarities as differences. There is cross learning to be had from both disciplines, but inevitable adaptations need to be made. Both operate in highly technical environments, with highly specialized and multidisciplinary teams where the outcomes are expected to be good. In both aviation and maternity, accidents are rare, mostly unexpected, and very tragic events.
Cardiotocograph (CTG) is a non-invasive tool for the assessment of fetal wellbeing in labour. When interpreted and acted on correctly the CTG enables timely delivery to avoid hypoxic damage to the fetus, and it also prevents unnecessary intervention. However, 50 years after its introduction to clinical practice there is a wide range of subjective difference in the classification of CTGs [2]. In the National Health Service Litigation Authority (NHSLA) Obstetrics accounts for 50% of the total value of claims received [3]. Data shows that although the number of claims brought forward for cerebral palsy has remained stagnant, the amount paid out for this type of claim continues to increase – 220 claims in 2013-2014 with a claim amount >£733 million, 188 claims in 2015-2016 with a total amount of >£989 million.
The recent Each Baby Counts report analysed complete data relating to term stillbirths, neonatal deaths, and babies with brain injuries born following labour in 2015 in the UK. Fetal monitoring was highlighted as a commonly recurring contributory factor to these outcomes [4]. The problem is not new, in the Confidential Enquiry into Stillbirths and Deaths in Infancy (CESDI) 1997 report, again most of the criticism focused on electronic fetal monitoring [5].
In the last two decades there has been an emphasis on improving guidelines and training in the use of CTG to reduce hypoxia-induced perinatal morbidity and mortality. This was largely driven by recommendations from the CESDI report, which called for regular/rolling CTG teaching and simple guidelines on the interpretation, recognition, and communication of abnormal CTGs. The Each Baby Counts report goes further and highlights human factors as a major cause of error in CTG interpretation. This article aims to explore the different arms of human factors and how each relates to CTG interpretation. We will be using a framework devised by Gordon DuPont who was the first president of the Pacific Aircraft Maintenance Engineers Association [6]. He identified the 12 most common causes of maintenance personnel making an error in judgment, which ultimately results in a maintenance error. He called them the Dirty Dozen Errors in Maintenance [7] (Figure 1). In this article we will discuss each of the Dirty Dozen and apply them to common CTG misinterpretation themes. We will also discuss ways in which these might be mitigated or avoided in practice.
The Dirty Dozen
Lack of communication
Communication is the exchange of information and transference of meaning between individuals. In the context of CTG interpretation this often falls into either confirmation bias e.g. “this trace looks normal, don’t you think?”; or lack of appropriate escalation. Strategies to improve good communication include breaking down boundaries between members of the multidisciplinary team so that even the most junior member of staff can feel comfortable approaching the most senior clinician to ask for help. Structured messages are also designed to avoid missing important things and tend to be useful for documentation and for hand over, especially in the context of shift work – as happens on most labour wards. The best known tool is SBAR which stands for S – situation, B – background, A- assessment and R-recommendation, or specifically for CTG documentation the mnemonic DRCBrVADO (Figure 2).
Complacency
This insidious cause of error usually occurs as people become overconfident and rely on pattern recognition for CTG interpretation “I’ve seen this before and it was fine, it must be fine now”. It is easy to become complacent when using pre-designed stickers to define CTGs as you are less likely to take in the whole clinical picture and think of the physiology behind CTG changes [8]. For example, the same pattern on the CTG may be of different significance depending on the gestational age, the stage of labour, or the presence of meconium. This human factor is mitigated by reading each CTG individually, and in context of the specific woman and baby. Changing the language from “How is the CTG trace?” to “How is the baby?” may be a first step in encouraging clinicians to contextualise that particular fetus.
Lack of knowledge
On the whole clinicians are better at recognising hypoxic stress because decelerations are both audible and visible on the CTG. However, there is a lack of understanding of other causes of encephalopathy and neonatal death, such as anemia and sepsis, and how they manifest on the CTG (Figure 3). Training is the best safety net to address this human factor. The Each Baby Counts initiative called for maternity units to introduce annual mandatory CTG training before independent practice on labour wards. Within the training there must be an emphasis on understanding fetal physiology and how physiological changes are transcribed onto the CTG [9] (Figure 3), Chorioamnionitis: Increasing baseline fetal heart rate in the absence of significant decelerations should prompt the suspicion of chorioamnionitis. The term “uncomplicated tachycardia” gives false reassurance and should be avoided. In the presence of chorioamnionitis, delivery should be expedited if not imminent and superimposed hypoxic stress should be avoided.
Distraction
This is anything that takes your mind off a task even for a second. Our minds work faster than our hands, so a distraction can very quickly steer you away from the task at hand. On the labour ward it is important to maintain a helicopter view of events and if we are distracted or committed to a specific task that needs our full attention, it is important to hand the helicopter view role to another member of the team. Taking care of a patient in labour involves multiple tasks and placement of an epidural is typically the time when the CTG is neglected. Epidural analgesia can lead to maternal hypotension and consequently uterine hypoperfusion with potential acute hypoxic stress to the fetus. Awareness of the importance of monitoring during epidural placement and the use of centralised electronic CTG monitoring systems can help to mitigate these risks.
Lack of teamwork
The labour ward is made up of a large multidisciplinary team however, the individuals within the team change frequently. Consequently, we often work with people we have not worked with before. This makes it difficult to know everyone, how they work, and their strengths and limitations. For example, when managing a cord prolapse with prolonged fetal deceleration, delivery needs to be accomplished in the quickest and safest way. There should be clear delegation and division of roles to ensure a swift and co-ordinated resolution. This human factor can be mitigated by doing introductions at the start of each shift and conducting multidisciplinary simulation training on a regular basis.
Fatigue
Fatigue is a feeling of tiredness, reduced energy, and increased effort to perform tasks effectively and without errors [10]. This is particularly, but not exclusively, relevant to night shifts because human beings operate on a circadian rhythm where we are programmed to be awake in the day and asleep at night. In the aviation industry the hours between 2am and 6am are referred to as the “Window of Circadian Low” or WOCL, as it is the time when alertness and performance are most degraded [11]. In maternity this probably corresponds to a peak of activity. Recent research by University College London, University of London, and the National Childbirth Trust (NCT) found that more than 50% of births following spontaneous labour occur between 1am and 7am with a peak around 4am [12]. This human factor can be mitigated by adjusting staffing to levels of activity within each unit and providing facilities for rest breaks during shifts. Also, the use of a “Fetal Monitoring Checklist” can reduce the risk of missing preexisting fetal injury (Table 1) [13]. Forming a habit of asking these questions before reviewing all CTGs will help avoid this common pitfall, particularly when fatigued.
Lack of Resources as mentioned previously most errors in Western healthcare are not due to a lack of resources.
However, if stocks are not diligently checked and maintained before they are required errors can occur as a result. Regarding CTG interpretation, if the abdominal probe is not adequately recording the fetal heart rate it might be necessary to site a fetal scalp electrode. Although these may not be used on every shift, they are an important piece of equipment to have readily available. A complimentary problem is not the lack but the inadequate use of resources and equipment available. A typical problem on CTG monitoring is the Inadvertent use of paper scales to which staff are unaccustomed. For example, at 3 cm/min variability appears reduced to a clinician familiar with the 1 cm/min scale leading to erroneous interpretation of the CTG. Most countries throughout the world, including the UK, use 1 cm/min paper scales, the Netherlands use 2 cm/min, and North America and Japan use 3 cm/min. CTG machines also have a button to change the paper speed that can easily be inadvertently pushed when cleaning the machine.
Pressure
It is often presumed that pressure is mainly from the environment in which we work. However, many pressure-caused errors are due to self-pressure, where there is a false perception that we will be seen as incompetent if we ask for help. This human factor is mitigated by practicing effective prioritisation and delegation of tasks and asking for help when help is needed; even if this means escalation to senior members of the team who are off-site.
Lack of assertiveness
An example of lack of assertiveness is failing to speak up when things don’t seem right. This is most evident in departments where there is a strong system of hierarchy. For example, a junior midwife who is not comfortable approaching the consultant to review a CTG. They may prefer to wait for a senior midwife to become available, thereby delaying review of a potentially pathological trace. This human factor is mitigated by breaking down this “chain of command” culture and building a team where juniors can approach seniors without reproach.
Stress
Stress is the subconscious response to the demands placed upon us. This does not only relate to the working environment but our personal lives also. Stress can lead to errors when it is excessive as it acts as a distraction and reduces concentration levels when performing complex tasks such as CTG interpretation. This human factor is mitigated by maintaining awareness of it and finding ways to destress; whether it be taking time off work, exercising the body or relaxing the mind. Some hospitals have introduced initiatives to promote physical exercise, mindfulness and yoga to promote staff well-being and reduce medical error.
Lack of awareness
Lack of awareness occurs when there is a lack of alertness and vigilance. This human factor is closely linked with complacency. For example, when monitoring a twin pregnancy in labour a common error is monitoring the same twin twice, not noticing that both CTG traces are similar and from the same fetus, leaving one twin unmonitored. Situational awareness is also about our mental picture of what is happening around us and how it will evolve. An example again with twins, where after the delivery of twin one the doctor becomes fixated on the repair of a bleeding episiotomy without noticing the abnormal CTG of the second twin. Haemostasis of a vascular episiotomy can be achieved by simply clamping vessels or compression with a swab, leaving time and space to prioritise twin 2. Strategies to mitigate lack of situational awareness include promoting frequent safety huddles and avoiding single task fixation. Common contributors to loss of situation awareness have been already discussed such as lack of knowledge, stress, and fatigue.
Norms
Norms are unwritten rules followed or tolerated by most of the group, but negative norms can detract from as established safety standard. For example, the term “second stage CTG” is a negative norm sometimes used to classify CTGs. It implies a higher level of tolerance for a pathological trace on the anticipation that the baby will be shortly delivered. This is a dangerous practice and the guidelines for interpretation of the CTG in the first or second stage are the same. The second stage of labour brings an additional risk into the fetal monitoring: it becomes harder to monitor the fetal heart due to its low position in the pelvis; therefore, the risk of recording maternal pulse increases (Figure 4). It is unusual for a fetus to have accelerations during the second stage of labour, so if an improvement on the CTG trace or accelerations are noted in the second stage, especially if synchronous with contractions, it should be assumed that maternal heart rate is being monitored until proven otherwise. The use of a fetal scalp electrode instead of an abdominal transducer helps to mitigate this risk of confusing maternal with fetal pulse, leaving the fetus unmonitored in the latest phase of labour.
Conclusion
Obstetric practice and CTG interpretation put individuals, teams, and organisations under great pressure to make difficult decisions in dynamic and often unpredictable circumstances [3]. This combination of factors lead to errors in CTG interpretation. We believe that current guidelines and CTG training should focus on the following:
i. Fetal physiology and the physiological processes that underpin CTG appearances;
ii. the way in which human factors affect decision making. This is the key to reducing perinatal morbidity and mortality from intrapartum insults. Thus, the key points from this article in relation to CTG interpretation are as follows:
• Take in the whole picture when reviewing CTGs. Ask “how is the baby?”, not the CTG!
• Understand the physiology behind CTG changes, including the changes caused by infection/ inflammation, not only hypoxia.
• Break down hierarchical boundaries, feel free to ask and escalate
• Avoid negative norms such as “uncomplicated tachycardia” and “second stage CTG”
Declarations
#open access journals#peer review journals#Juniper Publsihers#reproductive health#GJORM in juniper publishers
0 notes
Text
Immunological Approach of Personalized Treatment for Recurrent Implantation Failure Patients Undergoing IVF
Authored by: Indira Hinduja*

Introduction
Immunological and inflammatory response plays very crucial role in making the endometrium receptive. In normal fertile women, under the influence of progesterone and estrogen, during the window of implantation (WOI) and before the arrival of blastocyst, immune cells like monocytes and natural killer cells migrate to the endometrium. Additionally, inflammatory factors like tumor necrosis factor (TNFα) and interferon-γ are secreted by the endometrial stromal cells to initiate the inflammatory action. These markers secrete pro-inflammatory cytokines such as interleukin (IL)1, IL6, leukemia inhibitory factor (LIF), leptin, Insulin-like growth factor (IGF)2, IL18 in the endometrial tissue [1]. The chemotaxis of monocytes to the secreted cytokines brings about the differentiation of monocytes into dendritic cells and macrophages in the presence of IL4 and Granulocyte-macrophage colony-stimulating factor GMCSF. Immune cells also get differentiated to specific decidualized cells having peculiar characteristics e.g. NK cells loses its cytotoxic property when gets differentiated to decidualized NK cells. The chemotaxis and migration of these immune cells to the decidualized endometrium stimulates the endometrial cells to secrete various chemokines, growth factors and expression of cell adhesion molecules. Thus, the immunological and adequate inflammatory response has been observed to plays vital role in decidualization, tissue remodeling, angiogenesis, vasculogenesis, and cell adhesion.
Based on the study performed by our group [2], it has been observed that the immunological and inflammatory genes were downregulated in recurrent implantation failure patients undergoing 2 or more IVF cycles with unexplained infertility. The down-regulated expression of these genes was observed in endometrial tissue when patient group as well as healthy fertile oocyte donors (control group) were under the influence of ovarian stimulation. We have shortlisted panel of 70 genes involved in immune and inflammatory response. However, genes such as Progestogen Associated Endometrial Protein (PAEP), CD4, C-X-C Motif Chemokine Ligand 14 (CXCL14), Interleukin 6 Signal Transducer (IL6ST), LIF, Phospholipase A2 Group IIA (PLA2G2A), were validated by real time PCR. The protein expression was also assessed by immunohistochemistry for LIF, IL6ST and PAEP gene, confirming the significant down-regulation [2].
The significant differential expression of these genes in RIF cases Vs oocyte donors highlights the role of immunological processes in endometrial receptivity. Therefore, impairment in immune response and imbalance between pro-inflammatory and anti-inflammatory response could be accountable for defective endometrial receptivity [1–3]. It has been reported that, the hormonal administration in IVF protocol can be detrimental to the endometrial receptivity [4]. Though in our previous study, this hormonal bias was ruled out by considering both the case and control group undergoing same protocol of ovarian stimulation, the protocol of embryo transfer would also affect the receptivity. Thus, the regulation of immune and inflammatory cells in stimulated cycle, hormonal replacement cycle and natural cycle would be different which may cause implantation failure.
Therefore, in each RIF patients, it is essential to evaluate the expression of immune and inflammatory markers in WOI of the same characterized cycle as of embryo transfer. Based on the evaluation of panel of immunological markers, the approach of personalized treatment can be planned for RIF patients. In this approach, the RIF patients had undergone the evaluation of panel of markers involved in immunological response such as PAEP, LIF, IL6ST, CXCL14, PLA2G2A, Indoleamine 2,3-Dioxygenase 1 (IDO1), CD4, CD247. On stimulating the ovaries and retrieval of the oocytes, the embryos of RIF patients were fertilized and cryopreserved until their transfer. In the next natural menstrual cycle, the endometrial biopsy was collected on day LH+6, confirming the ovulation by monitoring the follicular growth by USG and LH surge by ‘ovulation LH kit’. Total RNA was extracted from endometrial tissue using Trizol reagent and were subjected to cDNA preparation using ‘first strand cDNA kit”, Invitrogen as per the manufacturer’s instructions. Real time PCR was performed using 18S housekeeping gene as a normalizer. The CT values of these genes were compared to control groups i.e. healthy fertile women in natural cycle (LH+6th day). The fold change was calculated using 2ΔΔCT method. The down-regulation or upregulation of these markers having fold change >2 was considered abnormal and were subjected to further personalized treatment.
The down regulation indicates the need to elicit the inflammatory response in endometrium by scratching the endometrium or introducing injury to endometrium using Gynetics suction curette. In such cases we could use the mechanistic approach reported by Gnainsky et al. [3], in which induced endometrial injury stimulates the immune markers and their migration to the implantation site, which reside in the functionalis layer of the endometrium and gets activated in next menstrual cycle during WOI under the influence of steroid hormones. On the other hand, the up-regulation of above mentioned immune markers is suggestive over-expression of genes related to immune response and would be recommended the administration of immunosuppressant (Figure 1). In all the down-regulated, up-regulated and normal cases, the embryo transfer is to be performed in natural cycle on day LH+5 by monitoring the follicular growth, without giving any hormonal supplementation for preparation of endometrium.
This approach agrees with the study reported by Roberson et al. [5] suggesting that it is very essential to treat the infertility immunologically by giving corticosteroids, only after the evaluation of immune response in the endometrium. This is because the controlled inflammation and stimulation of immune cells are important factors to achieve receptivity and successful implantation [5]. We have evaluated four such cases, of which one showed down-regulated panel of immune markers who had undergone the ‘injury to endometrium’ in secretory phase. In this patient, the embryos were transferred in its next natural cycle. In other case, the panel of immunological genes were normal when compared to fertile women. In this case, the embryos were transferred in the next natural cycle. Both these patients had conceived having positive urine pregnancy test and the presence of gestational sack. The conception was confirmed by assessment of heart bits of the fetus. Hence, out of four, IVF was successful in two patients on managing them using personalized approach with respect to immunological status of the endometrium to achieve the receptivity. The fold change of both these patients is shown in Table 1.
Conclusion
The implementation of this approach needs to be substantiated in larger population of RIF patients. Thus, the immune response and its proper regulation is observed to play vital role in endometrial receptivity. In IVF, the stated approach of embryo transfers in natural cycle on assessment of immunological regulatory genes would help in improving the success rate of IVF. The endometrial tissue assessment in natural cycle and even the transfer of embryo in natural cycle would help to nullify the hormonal bias of other generalized protocols of ovarian stimulation, replacement therapy and the preparation of endometrium in frozen embryo transfer cycle.
Aknowledgement
The implementation of this approach needs to be substantiated in larger population of RIF patients. Thus, the immune response and its proper regulation is observed to play vital role in endometrial receptivity. In IVF, the stated approach of embryo transfers in natural cycle on assessment of immunological regulatory genes would help in improving the success rate of IVF. The endometrial tissue assessment in natural cycle and even the transfer of embryo in natural cycle would help to nullify the hormonal bias of other generalized protocols of ovarian stimulation, replacement therapy and the preparation of endometrium in frozen embryo transfer cycle.
#open access journals#Juniper Publsihers#GJORM in juniper publishers#reproductive health#peer review journals
0 notes
Text
Research Article Intrauterine Insemination with Fresh Versus Cryopreserved Spermatazoa in Unexplained Infertility
Authored by: Sheena Rippentrop*

Introduction
Infertility affects approximately 14% of couples in the general population and is defined as failure to conceive after 12 months of regular unprotected intercourse. Unexplained infertility accounts for up to 15-30% of the diagnoses in couples [1,2]. The diagnosis of unexplained infertility is one of exclusion and can only be made after investigating the common causes of infertility using standard testing including evaluation for male and female infertility [1]. This evaluation typically involves assessment of ovulation, ovarian reserve, fallopian tube patency, uterine and cervical factors, along with semen analysis.
In couples with infertility, previous studies have shown that ovulation induction with intrauterine insemination (IUI) provides a less invasive and more cost-effective treatment option when compared to in-vitro fertilization in couples with unexplained infertility [3]. Therapy is often empiric, as there is no precise cause. Ovulation induction can be accomplished via administration of clomiphene citrate, letrozole, or with injectable gonadotropins. The rationale for ovulation induction with IUI is to increase the number of oocytes available for fertilization and bypass cervical barriers by directly depositing concentrated semen into the uterine cavity [4]. The combination has been shown to be the most effective treatment for infertility compared to timed intercourse, intracervical insemination, or IUI with natural cycle [5]. This method has proven successful in couples with unexplained infertility, cervical factor, mild endometriosis, women with polycystic ovarian syndrome, and couples with mild-moderate male factor infertility [5,6]. Ovulation induction however carries the risk of multiple gestation and thus increasing the obstetrical and neonatal risks including pre-eclampsia, preterm birth, and intrauterine growth restriction [6].
Success of IUI cycles has been shown to be dependent on many factors including maternal, ovulation response, and semen parameters. Improved outcomes have been demonstrated in women of lower maternal age, greater number of pre-ovulatory follicles, and the use of ovarian stimulation for couples with unexplained infertility [7-9]. In regards to seminal qualities, the total motile count is the marker most consistently shown to be a determinant of success in couples undergoing intrauterine insemination [7]. Many have found that sperm preparation techniques in both human and animal models can affect the baseline rate of DNA fragmentation leading to subsequent reduction in both the quality of sperm and fertility rates in samples that have undergone cryopreservation when compared to fresh sperm [10,11]. However, other studies report no difference in pregnancy rates in fresh compared to cryopreserved semen in unselected infertility subgroups [12]. Many studies have evaluated the use of ovulation induction in conjunction with intrauterine insemination in couples with unexplained infertility, yet none have investigated the use of fresh versus cryopreserved semen as a contributing factor in the overall pregnancy rates in the unexplained infertility population. A Medline literature review conducted for the years 1966-2014 did not uncover any previous studies utilizing the search terms unexplained infertility, intrauterine insemination, cryopreserved sperm. Our goal in this study was to evaluate clinical pregnancy rates and live birth rates in women with unexplained infertility undergoing intrauterine insemination with fresh and cryopreserved spermatozoa.
Methods and Materials
This retrospective cohort study examined all women who sought treatment for infertility at the University of Texas Health Science Center at San Antonio and at the Cleveland Clinic for the years 2003-2013. Only patients with unexplained infertility were enrolled. Informed consent was not needed given the retrospective nature of the study and no identifiable data was collected. Exclusion criteria included anyone with known anovulation, polycystic ovarian syndrome, tubal factors, uterine factors, diminished ovarian reserve, male factor infertility, or incomplete records. A total of 566 intrauterine inseminations were performed in 264 women. Of these cycles, 90.64% (513) were performed using fresh semen samples while 10.42% (59) were performed using cryopreserved samples. Patients who chose to use cryopreserved semen were in same sex relationship, did not have a male partner, or their partner was going to be away during the insemination process. Patients ranged in age from 19-46 with an average age of 31.1. Preliminary evaluation of all couples was composed of a full history, physical exam including pelvic exam, transvaginal ultrasonography, assessment of the woman’s ovarian reserve with cycle day 3 follicle stimulating hormone and estradiol levels and/or antimullerian hormone levels, hysterosalpingogram to confirm tubal patency, and semen analysis.
Normal values for these parameters were confirmed in all couples. Prior to intrauterine insemination, all women underwent ovulation induction with clomiphene citrate, letrozole, or injectable gonadotrophins. Clomiphene citrate dosage ranged from 50mg-250mg based on step-up dosing. Letrozole doses ranged from 2.5mg-7.5mg. Injectable gonadotropin dosages varied on a patient to patient basis. Patients were monitored for follicular response using transvaginal sonography with a recruitment goal of 2-3 follicles, each greater than 16mm, however IUI was performed as long as there was at least one dominant follicle present. Some patients however opted out of the monitoring of follicular recruitment, and thus had no ultrasound’s performed. Over-the-counter ovulation predictor kits (urine luteinizing hormone, LH), or choriogonadotropin alfa 250mcg (trade name Ovidrel; Merck; Frankfurter Straße 250, 64293 Darmstadt Germany) trigger shots administered at 24 to 36 hours prior to planned insemination were then used in determining timing of intrauterine insemination. Patients using ovulation predictor kits were told to begin testing on approximately cycle day 10-12 of their cycle depending upon the patient’s menstrual history and medication utilized. The patient’s called on the day the test was positive to schedule intrauterine insemination within 24 hours of a positive LH surge.
Patients unable to detect home LH surges were offered Ovidrel injection when at least two follicles were measured to be greater than 16mm on transvaginal sono. Fresh semen samples were collected on the same day as intrauterine insemination and were prepared using either wash or gradient methods and concentrated to 0.5mL. Following single intrauterine insemination, patients were instructed to take a home urine pregnancy test in 2 weeks if menses had not occurred. If the home pregnancy test was positive, patients were brought into clinic for confirmatory serum pregnancy test and ultrasound assessment at approximately 6 weeks gestation. Retrospective chart review was done for all patients enrolled. Patient data including patient age, ovulation induction method, intrauterine insemination data, clinical pregnancy status, spontaneous abortion, live birth status, and multiple gestation status were recorded from records.
Clinical pregnancy rates, live birth rates, biochemical pregnancy rates, and spontaneous abortion rates were calculated in fresh and cryopreserved insemination groups. Statistical analysis using Chi squared, Fisher’s exact t-test was performed where appropriate and odds ratios and 95 % confidence interval were calculated using Vassar Stats Website for Statistical Computation (vassarstats.net). A p-value was considered significant when less than 0.05. This study was approved by the institutional review boards at the University of Texas Health Science Center at San Antonio and at the Cleveland Clinic.
Result
Clinical pregnancy rates, defined as having a viable intrauterine pregnancy on transvaginal sono, were 29.24% in IUI-fresh and 11.32% in IUI-cryopreserved (OR 3.24, 95% CI 1.36-7.73, p-value 0.0055). The overall live birth rate per cycle for IUI-fresh was 19.88% versus 3.77% in IUI-cryopreserved (OR 6.33, 95% CI 1.52-26.43, p-value 0.0044). Biochemical pregnancy rates in patients who had a positive serum pregnancy test but no intrauterine pregnancy on sono were 12.87% for IUI-fresh and 7.55% IUI-cryopreserved (OR 1.81, 95% CI 0.63- 5.18, p-value 0.2882). Spontaneous abortions, where the patient had a positive serum pregnancy test followed by a confirmed intrauterine pregnancy on sono without a live birth, occurred in 9.36% of IUI-fresh and 7.55% of IUI-cryopreserved cycles (OR 1.26, 95% CI 0.44-3.66, p-value 0.8066). The average age of women undergoing IUI-fresh was 29.7, compared to IUI-frozen average age 35.9. In our study, a multiple gestation rate of 6.82% was observed after any cycle of IUI-fresh (p-value 0.0644). No multiple gestations were seen following IUI-cryopreserved. All multiple gestations consisted of a twin pregnancy, there were no higher order multiples in our study population. All multiples were the result of ovulation induction with clomiphene citrate.
The age of the patient was also determined to be a significant factor in both clinical pregnancy rate and live birth rate. Women under the age of 35 experienced a clinical pregnancy rate of 32.7% compared to women age 35-40 whose rate was 13.1% (OR 3.22, CI 1.83-5.66, p-value <0.0001). Live birth rates were 21.0% and 11.5% respectively for women under 35 and those age 35-40 (OR 2.05, CI 1.12-3.76, p-value 0.0181) No clinical pregnancies or live births were observed in women older than 40 years of age. The vast majority of cycles, 91.7% (519/566) underwent ovulation induction with clomiphene citrate. There were no clinical pregnancies observed in women who used letrozole for ovulation induction, however the study population was too small with only 37 cycles to detect any significant difference. The same holds true for women who chose injectable gonadotropins. There were only 10 cycles of ovulation induction using injectable gonadotropins, which yielded only one clinical pregnancy and one live birth. Again, the data was too small to detect any difference when compared to clomiphene citrate for ovulation induction. Predictably, the probability of both clinical pregnancy and live birth rate declined with each progressive cycle of intrauterine insemination regardless of fresh or cryopreserved spermatozoa when life cycle analysis was performed. The rate of decline when the two were compared was similar however cryopreserved spermatozoa were noted to start at a lower probability than that seen in frozen spermatozoa (Figure 1 & 2).
Discussion
In this retrospective cohort study in couples with unexplained infertility, we found a significantly higher clinical pregnancy rate, and live birth rate for women undergoing ovulation induction and intrauterine insemination using fresh semen compared to cryopreserved semen. No difference was observed in biochemical pregnancy rates or spontaneous abortion rates. We also found that clinical pregnancy rates and live birth rates were significantly higher in this cohort if the woman was under the age of 35. It appears that regardless of the intervention, the most important predictors of success in couples with unexplained infertility remain the age of the woman [1]. Our data supports the addition of fresh spermatozoa to this list of positive prognostic factors, however this observation may be clouded by the fact that the average age of women undergoing IUI-fresh was 29.7 compared to women undergoing IUI-frozen where the average age was 35.9. Unlike the study performed by Wolf et al. [12] but similar to the studies performed by Yildiz et al. [11] and Gosalvez et al. [10] we were able to show a significant difference in pregnancy rates when comparing fresh and cryopreserved spermatozoa [10-12]. These differences are likely due to damage of DNA during the freeze and thaw process of cryopreservation, however this study did not specifically look at semen parameters once male factor infertility had been excluded.
Our finding that women under the age of 35 have better pregnancy rates is consistent with the known decline in overall female fertility after the age of 35. This age-based decline is independent of other factors of infertility. Fecundability, or the ability to conceive per menstrual cycle, has been demonstrated to decline when women are in their early thirties with a more rapid decline around age 35 [13]. Menken et al found that in women aged 31-35 cumulative pregnancy rates begin to decline, and by age 35-39 one-third of women will experience difficulty conceiving [14]. It has been shown to affect not only couples with “normal” fertility but also those undergoing in vitro fertilization and intra-cytoplasmic insemination. Tan et al observed declining fertility rates starting at age 30, and that with increasing age of the woman there was a trend towards lower fertilization rates, clinical pregnancy rates, and live birth rates [15]. These agebased changes are likely due to diminishing ovarian reserve [16], poorer oocyte quality and altered hormone levels resulting in ovulatory dysfunction [17].
Conclusion
Our study suggests that women with unexplained infertility should be counseled that success rates, defined as clinical pregnancy and live birth rate, are higher when fresh spermatozoa is used for insemination compared to cryopreserved spermatozoa. Limitations to this study include different methods and dosing for ovulation induction amongst the study subjects, wide age range of subjects, older data, and the retrospective nature of the study. In future studies, we hope to study prospective, age-matched individuals.
#open access journals#Juniper Publsihers#peer review journals#global journal of reprodutive medicine#juniper publishers in GJORM
0 notes
Text
Ovarian Ectopic Pregnancy with Newborn at Term: A Case Report
Authored by: Quirino I*
Case Report
E.M.P., 26 years old, black, married, primigravida, admitted to the service at 28 weeks and 1 day of gestation, with mild pain in the lower abdomen and blood pressure 170x120mmHg, without headache, scotoma or visual turbidity. She underwent this first hospitalization for clinical investigation, with a diagnostic hypothesis of Hypertensive Disease of Gestation and nephropathy to be clarified. She was submitted to complementary examinations with ultrasound of urinary tract that diagnosed a single kidney. The conclusion of the obstetric ultrasound was single fetal in pelvic presentation, longitudinal situation, gestational age of 30 weeks and 4 days, estimated weight of 1528g.
The patient was submitted to a complementary transvaginal US, where it was observed in right adnexal region uterus image, measuring 12cm in the largest diameter with 10mm endometrium and empty cavity. A fetus was identified on the right flank and the hypotheses of topic pregnancy (uterus Didelphys) or ectopic pregnancy (abdominal pregnancy) were suggested.Magnetic resonance imaging of the pelvis revealed Mullerian malformation with the presence of two uterine bodies, single cervix and norm implanted placenta. One of the cavities had a fetus in pelvic presentation, while the other had no alterations. After the examination, it was determined that there was no urgency to resolve the gestation and the patient was discharged after the stabilization of the clinical condition.
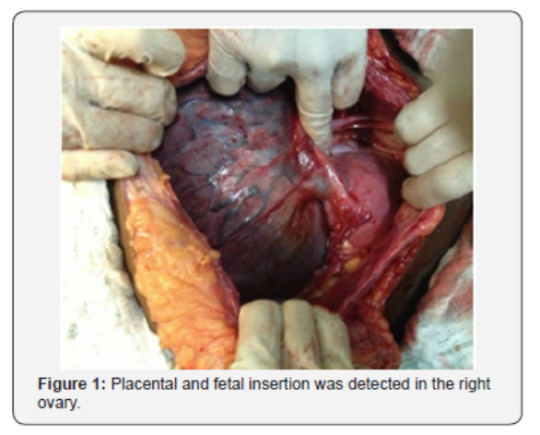
The patient was readmitted after 8 days complaining of lower abdominal pain, epigastralgy and blood pressure of 170x120mmHg. She had an obstetric ultrasonography performed indicating a single, live fetus in pelvic presentation, restriction of intrauterine growth below p10, with gestational age of 32 weeks and 3 days, weight of 1860g. The concept evolved with acute fetal distress and bradycardia, and the cesarean section was indicated. During the surgery, extra-uterine gestation was identified, and the gynecological surgery team was informed.Placental and fetal insertion was detected in the right ovary (Figure 1) with intense vascularization coming from the abdominal aorta (Figure 2). An intense adhesion process of the omentum and bowel were also identified, as well as the left ovary without alterations and a non-gravid uterus with normal format and consistency.
After lysis of adhesion, the extraction of a single live concept, with 1715g of weight, APGAR 8/9, plated in thick meconium fluid and Capurro of 37 weeks was performed (Figure 3). The cord was clamped at the placental insertion base and the ovary was sutured using a synthetic absorbent thread and applying regenerated oxidized cellulose to prevent pelvic adhesions in the future (Figure 4). At the end of the procedure, she was referred to the ICU, prescribed prophylactic antibiotics, analgesia and prophylaxis for thromboembolism. After 3 days, the patient was referred to the highrisk ward, which underwent infectious, hemantimetric and imaging tests to prevent acute hemorrhagic disease. Placental resorption was monitored for a period of 2 months and after stabilization of the condition, the patient was referred to the specialty outpatient clinic.
Discussion
Ovarian gestation is a rare occurrence in obstetrics, becoming an even rarer event when it progresses with a live, viable fetus until its birth and with postnatal development without alterations [6]. The case in question demonstrates an immense diagnostic challenge, even with the use of nuclear magnetic resonance, since it is a rare obstetric pathology. The favorable evolution observed in the report, with survival of the mother and its concept, constitutes the exception, not the rule. Therefore, we must continue to follow the recommendations of the latest evidence, acting with the interruption of gestation treatment facing an early diagnosis, through clinical or surgical management [7,4]. When the diagnosis occurs between the second and third trimester, due to an intense local vascularization, it is possible to opt for an expectant conduct and control of the fetal vitality until it reaches the viability. Although we must explain all the risks and leave the patients comfortable to decide whether they will choose or not to continue the pregnancy and receive the signed informed consent.The guidelines of greater impacts guide the interruption of pregnancy, either by clinical or surgical methods. Therefore, based on the case presented and some other rare reports in the literature, we are faced with the need for more publications that may guide us to maintain an ovarian pregnancy until viability or follow the current recommendations.
To Know More About Please Click on: Journal of Reproductive Medicine
https://juniperpublishers.com/gjorm/index.php
To Know More About Open Access Publishers Please Click on: Juniper Publishers
#open access journals#Juniper Publsihers#global journal of reprodutive medicine#peer review journals#reproductive medicine#GJORM in juniper publishers
0 notes
Text
Reprints on Axillary Masses in Breast Cancer: A Review
Authored by: Wilson Onuigbo*

Introduction
In 1986, John Swales, the Editor of English for Specific Purposes, researched on the worldwide traffic in the reprint request (RR) and wrote about me as “the only active researcher that I have traced in the RR area” [1]. Perhaps, a sequel to this honor is to use the dozen reprints which I collected during the 1980-1989 period to expatiate on the intriguing phenomenon of how the axillary lymph nodes have been featuring so much in breast cancer cases [2-13].
Method
These reprints have been analyzed from several angles. A starting point is the array of the cited Journals, namely, Cancer [2,3,12], Journal of Surgical Oncology [4,11]. Annals of Surgery [5,8], American Journal of Surgical Pathology [6], Histopathology [7], Breast Cancer Research and Treatment [9]. The American Surgeon [10], Surgery [12], and Human Pathology [13]. Another point is the country of origin. Certainly, USA super abounded. Incidentally, I had previously demonstrated the premier position of USA in the reprint’s traffic [14]. Next, Canada, Norway, Italy and Israel also featured.
Results
A case report came from Canada while 2 cases were presented from USA [10]. The rest totaled 2,542 cases. With regard to the single case report, there was eventually no evidence of a primary lesion in the breast called “occult” breast cancer, this was defined as “nonpalpable breast carcinoma presenting as an axillary mass” [10]. Following the study of 48 such patients carried out in New York for at least 5 years, it was concluded thus: “the actual pathologic stage, which takes tumor size into consideration, determines prognosis rather than the apparent clinical stage described when the patient is first examined” [13]. This was confirmed years later [6].
“Skip” metastasis was also considered [5,8]. It was defined as “involvement of lymph nodes (which) occurs in a stepwise continuous fashion from the periphery of the axilla medially.” However, it was concluded that the risk is not great and “should not be a major consideration in therapeutic decisions” [8].
The sinuses of the axillary lymph nodes were also studied in Norway [7]. Apparently, they depended on Halsted’s observation in 1898, and were purely mechanical. Likewise, fatty changes came into view, but it was concluded that “the presence of fat in axillary lymph nodes does not influence implantation of tumor cells from a primary carcinoma of the breast and has to be reported as an anatomic variant”[11]. Another question arose. An Italian group tackled it. They concluded thus: “When the nodes at the first level are positive, the chances that metastases are also present at the higher levels are of the order of 40.0%” [12]. Another Italian group took up xeroradiography [9]. They lamented thus: “Xeroradiography does not appear to have improved our ability to identify axillary lymph node metastases in patients with breast cancer”. Light elecronmicroscopic examination was carried out in USA. The conclusion ran thus: “The finding of carcinoma that appears histologically to be entirely preinvasive, whether duct or lobular in type, in a breast biopsy specimen does not entirely preclude the possibility of metastases in axillary lymph nodes.”
What of sampling procedures? The question boiled down to “an axillary sampling instead of a complete axillary dissection”. The answer was as follows: “the possibility exists that node “sampling” understages patients who would otherwise have received adjuvant chemotherapy to improve their chances for cure.” Perhaps, the answer is that of Patel’s group, namely, “carcinoma found in an axillary node should be treated as a breast cancer, even in the absence of the breast tumor.”
Discussion
The above data have dealt with Reprints in the field of reproductive medicine. In fact, these reprints are the old champions in the Communication Sciences. What of the reigning Internet? In this context, what of combining the old and the new? I did so with the 2004 work published on the doleful disease of gestosis. It was Chappell who lamented that gestosis contributed “to at least 40 000 to 60 000 of these deaths worldwide each year” [14]. Fortunately, I had received 3 reprints concerning gestosis during the 1980/1981 period [15-18]. Using them, I hypothesized that, since gestosis was appreciated thrice as being linked with “new father,” “new partner,” and “different consort,” the “women at risk ought to be so educated as to be aware of the known repercussions associated with change in paternity”. As I concluded, “in all probability, the gloom of gestosis can give way smoothly to that bloom of placid parturition which must naturally follow the above enumerated enlightened sexual behavior.” In particular, the Allied Health Professionals should be involved because this is not a question of prestige but of cooperation [20]. If they do so with the obstetricians, the 40 000 to 60 000 deaths worldwide would become history.
#open access journals#peer review journals#Juniper Publsihers#global journal of reprodutive medicine#GJORM#Juniper Publishers
0 notes
Text
Optimization of Sperm Culture Conditions for Human Assisted Reproductive Technologies
Authored by: Charles L Bormann*
Optimizing sperm performance can be a differentiating factor in clinical pregnancy rates for assisted reproductive technology (ART) laboratories. Minimizing cellular stress during routine sperm processing by maintaining a precise and stable environment is of great importance in the field. In commercial media, pH of the external cellular culture environment (pHe) is typically maintained at 7.2-7.4 by various buffering reagents, while the internal pH of the cell (pHi) depends on available lactate and amino acids. Combining buffers in solution has been previously shown to be valuable for stabilizing internal and external pH for various biological systems. We hypothesized that a dual-buffer culture medium might improve sperm performance for ART. Here we demonstrate superior performance of a commercially available dual-buffer solution of HEPES and MOPS: Multipurpose Handling Medium (MHM, Irvine Scientific). Significantly better performance, assessed at 8 and 48 hours, and measured as: sperm viability, total motility, and rapid forward progression, was observed for MHM over single buffer controls.
Keywords: Sperm processing; Sperm wash; Sperm viability; Multipurpose handling medium
Abbreviations: ART: Assisted Reproductive Technology; MHM: Multipurpose Handling Medium; SPWASH: Sperm Washing Medium; CASA: Computer Assisted Sperm Analyzer; IQR: Inter Quartile Range; MHM: Multipurpose Handling Media; AAB: American Association of Bioanalysts
Introduction
Achieving and maintaining high pregnancy rates is a top priority for embryology labs and fertility practices. Optimizing sperm performance can be a key differentiating factor in achieving better clinical pregnancy rates. Human sperm handling procedures for ART are commonly performed under atmospheric conditions, where temperature and CO2, play a significant role in regulating pH. Maintaining a precise and stable pH balance is challenging, as even minor environmental fluctuations can negatively impair human sperm function. HEPES and MOPS are zwitter ionic organic buffers with pKa at 20 °C of ~7.55 and 7.15, respectively. Individually, they have been extensively studied in numerous ART-related processes, including: sperm isolation, oocyte retrieval, ICSI, embryo biopsy, embryo transfer, and cryopreservation. However, recent evidence supports the notion that combining HEPES: MOPS may allow for improved media formulations.
Multipurpose Handling Medium (MHM, Irvine Scientific) is a commercially available dual-buffer solution of HEPES and MOPS used to maintain stable conditions for oocytes, and embryos when being manipulated under atmospheric conditions. Dualbuffer solutions have demonstrated improvements in working pHe, Na+ or K+ concentration, and/or concentration toxicity and osmolality, over single buffer media, and is specially formulated to maintain a physiological pH of 7.2-7.4 over a broad temperature range. We hypothesize that a dual-buffer Multipurpose Handling Medium will better support and maintain sperm viability parameters compared to specimens processed with a single buffer solution.
Here we describe the baseline conditions for human semen samples in three handling media (dual buffer MHM compared to two commercially available single buffer HEPES media: a control sperm washing medium, Sperm Washing Medium (SPWASH, Irvine Scientific), and an ART handling medium, Quinn's Advantage Medium with HEPES (QUINN, Cooper Surgical), by distribution of motility percent and rapid progression percent, and we quantify causal association of motility percent and rapid progression percent to handling medium after 48 hours at room- atmosphere conditions.
Materials and Methods
Sperm collection, preparation and processing
Semen samples from 21 men undergoing routine fertility testing and having normal specimen parameters as defined by the WHO 5thedition [1] were included in this study. Specimens were liquefied for 30-60 minutes and sperm were quantified using a Computer Assisted Sperm Analyzer (CASA; CEROS™ II, Hamilton Thorne). Specimens meeting eligibility criteria were layered over a 50:90% Isolate gradient (Isolate, Irvine Scientific) and centrifuged for 20 minutes at 300xg. Following centrifugation, sperm pellets were suspended with 10ml of SPWASH and centrifuged for 10 minutes at 300xg. This wash step was performed two times for each specimen. The final sperm pellet was quantified using CASA and equivalent concentrations of motile sperm (~5million/ml) were added to the following treatment groups: SPWASH, QUINN, and MHM. All specimens were analyzed under IRB approval.
Data collection and statistics
Following collection, processing, and preparation of participants semen samples in three handling media- labeled and capped tubes were left in a controlled room temperature environment for 48 hours. Assessments were performed at 8, 24, and 48 hours, at which time the concentration, motility percent, rapid motile progression percent, medium motile progression percent, slow motile progression percent, and static motile percent of total sperm were recorded. The mean and standard deviation of the recorded baseline (0-hour) characteristics were calculated to describe the observed location and spread of these variables, by handling medium and overall. The distributions of motility percent and rapid progression percent within each handling medium are summarized in box plots at baseline and each follow-up time.
The overall association between motility percent and handling medium was assessed using a linear mixed effects regression model. This model estimates the average motility percent of sperm in each medium, adjusting for the motility percent at baseline and accounting for possible correlation between measurements on the three samples taken from the same individual. Separate models were used to estimate motility percent at 8 hours and at 48 hours. Analogous linear mixed effects models were fit to assess the association between rapid progression percent and handling medium at 8 hours and at 48 hours.
Results
Semen samples from 21 individuals, and each sample was prepared following the same laboratory protocol and divided into three subsamples, one in each of the study media (MHM, QUINN, SPWASH), for a total of 63 samples. The study design is balanced across subjects and sperm handling media, and there is no missing data for the analyzed variables. The mean and standard deviation of baseline characteristics of the samples are shown in Table 1. The concentration of sperm is similar across handling media, and there were no statistical differences in total motility or motility progression categories across the three treatment groups. Box plots comparing the distributions of motility percent in MHM, QUINN, and SPWASH at baseline and at 8, 24, and 48 hours are shown in Figure 1. In these plots, the horizontal black line dividing the box indicates the median (or 50th percentile) of motility percent for samples in the specified medium. The bottom and top of the colored box correspond to the observed 25th percentile and 75th percentile of motility percent values, respectively. This interval is also called the inter quartile range (IQR). The vertical lines extending from the box indicate the range of observed values within a distance of 1.5 times the length of the IQR from the median. Motility percent appears to be similarly distributed across the three media at baseline, but as time progresses, the motility percent declines more in QUINN and SPWASH than it does in MHM.
The estimated differences in mean motility percent at 8 hours and at 48 hours, comparing samples of sperm preserved in QUINN to those in MHM and comparing samples preserved in SPWASH to those in MHM are shown in Table 2. Each estimate is accompanied by a 95% confidence interval for the true difference between mediums as well as a p value quantifying the strength of evidence in the data supporting the difference. For example, at 8 hours, the mean motility percent in QUINN is estimated to be 7.12 lower than the mean motility percent in MHM, comparing samples with the same baseline motility percent. We are 95% confident that the true difference in motility percent between the mediums (QUINN minus MHM) at 8 hours is within the interval -10.57 to -3.68. The p value for the statistical test that the true difference is nonzero is p = 1:62 x 10-4: This value estimates the probability that a difference between mediums of -7.12 would be observed if indeed there were no difference in motility percent between the mediums, and the difference in observed values were only due to random chance. A very small p value indicates that the data contain strong evidence that the mean motility percent after 8 hours in QUINN is different from, and in this case lower than, that in MHM. Typically, a p value of less than 0.05 is interpreted as a statistically significant association. The values in the table for the difference in motility percent between QUINN and MHM at 48 hours and for the difference in mean motility percent between SPWASH and MHM at 8 hours and at 48 hours may be interpreted analogously.
For example, at 48 hours, the mean motility percent in SPWASH is estimated to be 17.14 lower than the mean motility percent in MHM, comparing samples with the same baseline motility percent, with a 95% confidence interval of (-21.71, -12.57) for the true difference and a p value p = 2:58 x 10-9: Box plots comparing the distributions of rapid progression percent in MHM, QUINN, and SPWASH at baseline and at 8, 24, and 48 hours are shown in Figure 2. As was observed for overall motility percent, the rapid progression percent appears to be similarly distributed for each of the three media at baseline. At each subsequent follow-up time, the rapid progression percent appears to decline more in QUINN and SPWASH than it does in MHM.
The estimated differences in mean rapid progression percent at 8 hours and at 48 hours, comparing samples of sperm preserved in QUINN to those in MHM and comparing samples preserved in SPWASH to those in MHM are shown in Table 3. Each estimate is accompanied by a 95% confidence interval for the true difference between mediums and a p value quantifying the strength of evidence in the data supporting the difference. The interpretations of the results of the linear regression in Table 3 are analogous to those shown in Table 2. For example, at 48 hours, the mean rapid progression percent in QUINN is estimated to be 17.04 lower than that in MHM, comparing samples with the same baseline rapid progression percent. The 95% confidence interval for the true difference in rapid progression percent between QUINN and MHM is (-21.65, -12.44). The p value associated with this estimate is p = 3:38 x 10-9, which indicates very strong evidence in the data supporting the difference in mean rapid progression in QUINN and MHM. As for motility percent above, differences of substantial magnitude and strong statistical significance were observed for rapid progression percent at 8 hours and at 48 hours, between QUINN and MHM and between SPWASH and MHM.
Discussion
Replicating physiological homeostasis minimizes cellular stress during routine sperm handling, generating optimal outcomes for assisted reproductive procedures, such as: 1U1, 1CS1, and 1VF [2]. During insemination, gametes and embryos are readily maintained at ideal temperature, humidity, and CO2 levels. The CO2 gas concentration regulates external pH. pHe is easily manipulated and measured; therefore, optimal pHe has been extensively examined for embryo and gamete culture. However, handling, processing, and preparation steps are typically performed outside of an incubator, where sperm are exposed to atmospheric conditions, and the risk of even minor changes in pHe can lead to undesirable outcomes in sperm viability and performance, and by extension fertility outcomes [3].
Zwitter ionic buffers, such as HEPES and MOPS, can act as either an acid or a base and are commonly used to stabilize pHe in cell culture media. It has been shown that pHe influences cells in culture through its impact on intracellular pH (pHi; 4,5). pHi in turn, regulates a variety of cellular processes including enzymatic activity, cell division, differentiation, membrane transport, protein synthesis, cell communication, cytoskeleton elements and microtubule dynamics [3]. Cells contain intrinsic pHi regulatory mechanisms, (HCO3-/Cl- exchanger, Na+/H+ antiporter, and Na+ dependent HCO3"/Cl- exchanger); however, in culture, pHi initially follows the external pH of media. For clinical use, buffers should be stable, easily prepared, and consistent lot-to-lot. HEPES and MOPS can be obtained as a free acid, or conjugated to various salts; like sodium and potassium. Combining free acid and salt forms of the same buffer in various ratios offers the ability to adjust the working pHe of the medium during formulation, without the need to adjust with an acid or base later, improving consistency of the media formulation [4].
Multipurpose Handling Media (MHM, Irvine Scientific) combines HEPES and MOPS for an improved formulation that does not require the use of a CO2 incubator to maintain physiological pH 7.2-7.4 and osmolality over a broad temperature range. Additionally, MHM solution also contains glycine and taurine to maintain cellular homeostasis through regulation of pHi [5]. Combining HEPES and MOPS for embryo culture demonstrated that the use of both buffers provide buffering at a point between HEPES or MOPS alone, and yielded similar blastocyst formation and cell number compared to the individual buffers [6]. Furthermore, preliminary studies suggest that a combination buffer of HEPES/MOPS may be useful for procedures such as ICSI, as it yielded similar rates of normal fertilization of human oocytes (71%) abnormal fertilization (5%) and blastocyst development (74%) as media buffered with HEPES alone (63%, 12%, 52%, respectively; 6).
Human sperm bioassays are highly sensitive when both motility and the quality of sperm motility (motility grade) are taken into consideration [7]. The American Association of Bioanalysts (AAB) chose an assay time of 48 hours for identifying the quality of ART culture media, we used 48 hours as an endpoint to be consistent with this guidance, and assayed motility percent and rapid progression percent, to sensitively quantify causal association of sperm performance to handling medium. The experimental design of this study enabled the causal association between handling medium and rapid and total sperm motility percent. However, it is important to carefully assess whether any unmeasured factors or factors not analyzed could explain part or all of the observed differences in motility percent and rapid progression percent between the handling media. Precise handling of cells and supplies within the lab, as well as tedious attention to detail are just as important as the media formulation to outcomes. We took care to minimize any differences across media in the handling of samples throughout the experiment and in the measurement tools or procedures used at baseline or during follow-up, so as not to introduce bias into the data.
Conclusion
Differences of substantial magnitude and strong statistical significance were observed for mean motility percent between QUINN and MHM, and between SPWASH and MHM, at both the analyzed follow-up times. Here for the first time, we have demonstrated superior performance of a commercially available dual buffer solution of HEPES and MOPS for human sperm handling. Sperm viability, motility percent, and rapid progression in MHM displayed significantly better performance than single buffer controls, presumably due to synergistic pHe and pHi stabilization afforded by a dual-buffered system.
#open access journals in juniper publishers#peer review journals#juniper publsihers#GJORM in juniper publsihers#Sperm Culture Conditions
0 notes
Text
The Long-Term Progression Free Survival After the Combination of Radiotherapy with Concurrent Chemotherapy of Nimotuzumab And Temozolomide Followed Adjuvant Temozolomide In Recurrent Anaplastic Astrocytoma
Authored by: Xiaoqi Xie*
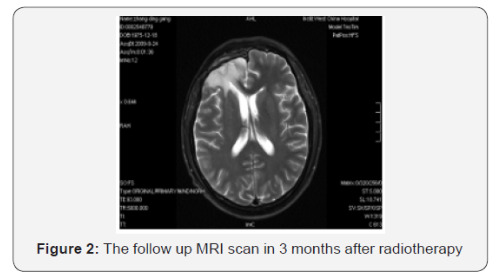
Introduction
Gliomas which originated from glial cells and made up 80% of all primary CNS tumors in the United States were classified as “low grade” (WHO grades I and II) and “high grade” (WHO grades III and IV) according to histopathologic changes [1,2]. High-grade gliomas (HGGs) are related with poor prognosis and consist of anaplastic gliomas (anaplastic astrocytoma, anaplastic oligodendroglioma and anaplastic oligoastrocytoma; WHO grade III) and glioblastomas (GBMs; WHO grade IV). The current standard therapy for newly diagnosed GBMs involves maximal safe resection followed by radiotherapy (RT) with concomitant and adjuvant temozolomide (TMZ) [3-5]. Despite optimal therapy, the median time-to-tumor progression (mTTP) for patients with newly diagnosed GBMs is approximately 6.9 months and these tumors unavoidably relapse with a median overall survival (mOS) of only 15 months [3]. However, the treatment of anaplastic gliomas is abroad controversial topics in neuro-oncology. By above therapy, anaplastic gliomas achieves a mTTP of about 1.2 to 2.6 years and a mOS of 2 to 7 years [4,6,7].
Compared with anaplastic oligodendroglioma, treatment of the anaplastic astrocytoma has been less optimistic. This tumor is more resistant to therapy and patients have a shorter mOS of only 2 to 3 years. In the United States, most oncologists treat anaplastic astrocytoma patients with maximal safe resection followed by field radiotherapy with concurrent and adjuvant chemotherapy (temozolomide), same to the regimen now deemed as the standard of care for GBMs [3]. Moreover, all HGGs nearly recur and survival following disease progression is doomed to be approximately 6 months for GBMs and 10 months for anaplastic gliomas [8,9]. Treatment options for recurrent HGGs include re-resection, chemotherapy, or re-irradiation. But, the optimal treatment strategies for recurrent HGGs are still unknown and the randomized control trials which contrast active intervention and determine standard therapy are absent. We herein report the case of a recurrent anaplastic astrocytoma patient with the long-term progression free survival (PFS) after the combination of radiation therapy with concurrent chemotherapy of nimotuzumab and temozolomide followed adjuvant temozolomide.
Case Report
We present the unique case of a 33-year-old gentleman who initially presented with a several days history of headaches behind the right brain, with associated “vomiting”. There were no complaints of numbness, weakness, or any visual changes. Physical examination of the patient revealed that he had a depressed superficial reflex in the right limbs and positive pyramidal tract signs. A MRI scan at that time revealed a large, irregularly enhancing mass in the right frontal lobe that was associated with marked edema, bleeding and mass effect. These symptoms relieved with the treatment of dehydration to reduce intracranial pressure. Following the consultation with a neurosurgeon and discussing the probability of a brain tumor and therapeutic regimen, the patient experienced a right frontal lobe Lobectomy in local hospital in October 2008. The final pathology was anaplastic astrocytoma (WHO grade III).
The patient recovered well from surgery, and his headaches were resolved. Adjuvant treatment options were explained to him and included radiotherapy plus concomitant and adjuvant Temozolomide. But the patient refused further therapy. In April 2009, a follow-up CT scan revealed local recurrence in the operative bed (Figures 1-3). And the patient was treated in West China Hospital. The pathology department in West China Hospital held a pathological consultation with tumor section in local hospital and diagnosed anaplastic astrocytoma (WHO grade III) containing a few of oligodendroglioma ingredients with histopathologic changes of partial necrosis, mitotic activity and endothelial cell proliferation (Figure 4). KRAS mutation was detected in codon 12 and codon 13 and the DNA repair enzyme O6-methylguanine- DNA methyltransferase (MGMT) promoter methylation was positive. Chromosomal 1p and 19q co-deletion was detected by FISH (Figures 5&6). Isocitrate dehydrogenase 1 mutation (codon 132) was detected by PCR and Sanger sequencing and Isocitrate dehydrogenase 2 (codon 172) was wild type (Figures 7&8).
Starting on May 22, 2009, the patient underwent whole brain radiotherapy to a dose of 4000 cGy and local lesion radiotherapy to a dose of 6000 cGy (fractionated focal irradiation in daily fractions of 2 Gy given 5 days per week for 6 weeks) with concurrent combined chemotherapy of intravenous nimotuzumab (100 mg every 1 weeks) and oral temozolomide (75 mg per square meter of body-surface area per day) for 6 weeks followed by six cycles of adjuvant temozolomide (150 mg per square meter for 5 days during each 28-day cycle). Treatment was generally well tolerated, and the adverse events were nausea, vomiting and hematologic toxicities, which all of them were classified as mild. Following his radiotherapy and chemotherapy, he was followed clinically as well as with surveillance MRI scans at regular intervals. The follow-up MRI scan in 3 months after radiotherapy were as follows (Figure 2). The latest MRI scan revealed no recurrence in May 31, 2016 (Figure 3). Until now, the patient is still alive with a long-term progression free survival lasting seven years. And the survival following the initial diagnosis is up to eight years.
Discussion
A high rate of local recurrences has been observed after multi-disciplinary therapy in high-grade gliomas (HGGs) patients.10 Important variables predicting longer survival include oligodendroglial cell line, extent of resection, and younger age (<50 years) [11]. Moreover, gliomas with the DNA repair enzyme O-6-methylguanine-DNA methyltransferase (MGMT) promoter methylation, chromosomal 1p and 19q co-deletion or isocitrate dehydrogenase 1 and 2 (IDH1/2) mutations is associated with a better prognosis [12-15]. In this patient, the chromosomal 1p and 19q co-deletion was detected by FISH; and the MGMT promoter methylation was positive and Isocitrate dehydrogenase 1 was mutation type, which was one of the reason of long-term progression free survival (PFS). PFS is associated with overall survival (OS) and has become a marker for evaluating the efficacy of treatments in recurrent HGGs patients. The 6-month PFS (PFS6) for recurrent GBM ranges from 9 to 21% [8,9,16], while PFS6 for anaplastic gliomas have ranged from 37 to 48% [17,18]. In our report, the patient still does not progress with a long-term PFS lasting seven years. Although the prognosis of recurrence HGGs patients is invariably poor, it is vital just as this case to improve the quality of life and prolong survival by multimodal therapy.
Therapy options for recurrent HGGs are limited and may include surgery, re-irradiation, chemotherapy and targeted therapies. For recurrent HGGs patients which were subjected to clinical deterioration on account of mass effect, surgery might be one of option. But, until now, no prospective researches demonstrate that re-surgery can improve the survival for recurrent HGGs patients. Moreover, due to the application of targeted therapies, a fewer proportion of recurrent HGGs patients are going through diagnostic or therapeutic re-surgery.
For HGGs patients, primary therapy most involves adjuvant radiotherapy with the maximum tolerated dose. The dose limitation of healthy brain tissue and the short duration between initial radiation therapy and recurrence confined the use of reirradiation therapy for recurrent HGGs with conventional external beam radiotherapy, which may have an influence on patient’s quality of life. However, Romanelli et al’ s research that evaluated the efficacy of stereotactic radiosurgery (SRS) in recurrent glioma have indicated median OS from 7.5 to 30 months after treatment [19]. And in Mahajan’s research [20], recurrent GBM patients treated with SRS achieved a longer median OS compared with untreated patients [20]. Hypofractionated stereotactic irradiation might be another choice for recurrent glioma. According to Fogh, et al. [21] research, the median OS after re-irradiation with a hypofractionated protocol (3.5 Gy per fraction up to a median dose of 35 Gy) over a 2-week period was 11 months. In this case, because patient did not receive any further treatment after surgery, conventional external beam radiotherapy (whole brain radiotherapy to a dose of 4000 cGy and local lesion radiotherapy to a dose of 6000 cGy) plus concomitant and adjuvant Temozolomide were recommended to him and the progression free survival after irradiation was seven years.
The efficacy of chemotherapy in recurrent HGGs was limited. And many chemotherapeutic agents, including single agents and combination chemotherapy agents, have been used to treat recurrent HGGs [22,23]. Temozolomide, PCV and bevacizumab are some of the treatment choice according to several researches [24-27]. Temozolomide was evaluated in recurrent HGGs before becoming the first line chemotherapy for glioma. The recurrent anaplastic glioma patients that were treated with single-agent TMZ showed a 35% response rate and PFS6 of 46% [28]. Bevacizumab has been authorized by FDA as the treatment of recurrent GBMs [29]. Moreover, Nimotuzumab is a humanized monoclonal antibody which binds the extracellular domain of epidermal growth factor receptor (EGFR) and blocks EGFR signal pathway activation [30]. And the efficacy of nimotuzumab in HGGs is depended on the combination of nimotuzumab with radiochemotherapy or radiotherapy. Solomon et al. [31] research has illustrated the median survival time of the combination of nimotuzumab with radiotherapy was 12.4 months or 27.0 months for patients with GBM or anaplastic astrocytoma patients. In our case, the chemotherapy agents were the concurrent combined chemotherapy of intravenous nimotuzumab and oral temozolomide for 6 weeks followed by six cycles of adjuvant temozolomide. And the efficacy was surprising. Thus, nimotuzumab might be one of the chemotherapy choice and more randomized clinical trials need to be done to clarify the efficacy of nimotuzumab.
Conclusion
This is the first reported case to our knowledge of a patient with recurrent anaplastic astrocytoma who achieved PFS lasting seven years following treatment with the combination of radiation therapy with temozolomide and nimotuzumab. The patient tolerated the therapy well and do not relapse again until now. This case highlights the unique biology of individual glioma and that the combination of radiation with chemotherapy and targeted therapy in the recurrent setting can have a significantly influence on overall survival for specific patients. We will continue doing research in this area, especially in the molecular characteristics of individual tumors. Individualized treatment according to each unique patient’s situation will improve survival as well as quality of life.
#peer review journals#Juniper Publsihers#reproductive health#open access publishers#GJORM in juniper publishers
0 notes
Text
The Alliance for Innovation in Maternal Care: A National Partnership to Improve Maternal Safety
Authored by: Jeanne Mahoney*
Introduction
Responding to a disturbingly rising maternal mortality rate in the U.S, a national partnership of provider, public health and advocacy organizations, administrated by the American College of Obstetricians and Gynecologists, developed the Alliance for Innovation on Maternal Health (AIM). AIM aligns national, state, and hospital level efforts to improve maternal health and safety and is poised to reduce severe maternal morbidity by 100,000 events and maternal mortality by 1,000 deaths by 2018. With funding received from the Health Resource Services Administration, AIM provides evidence-based front-line resources for birth facilities and provider/public health teams to adapt and implement a series of action steps (bundles) on high risk maternal conditions. AIM support harmonized data-driven, rapid-cycle, continuous quality improvement processes to engage providers and birth facilities. Starting with states that have high rates of maternal mortality, AIM utilizes a broad variety of partners to develop state level teams for bundle implementation.
Short Communication
Bundles are standardized evidence-informed processes to reduce variation in response to maternal care. They are developed by multidisciplinary work groups of experts in the field representing each of our Alliance partners and specialty organizations.
Below is the current listing of bundles completed or underway.
I. Severe hypertension/Preeclampsia
II. Obstetric hemorrhage
III. Prevention of maternal venous thromboembolism
IV. Safe reduction of primary cesarean births/supporting intending vaginal births
V. Reduction of peripartum racial disparities
VI. Postpartum care basics for maternal safety (first 6 weeks)
VII. Transition to well woman care (6 weeks to 1 year)
VIII. Patient, family and staff support
IX. Obstetric care of women with opioid use disorder.
Bundle tools include
i. Maternal early warning signs
ii. Reporting forms for severe maternal morbidity
The Alliance partners are national organizations ready to share their expertise and guide the AIM program (Table 1). AIM works through state teams. These teams must have a leader; be able to provide deidentified hospital administrative data quarterly to the AIM data center; engage state public health officers; conduct multidisciplinary maternal mortality review reviews and identify champions among nursing, midwifery, and physicians. AIM is a data driven quality improvement initiative. The AIM team has identified low burden metrics for measuring bundle adoption and maternal outcomes within states and hospitals implementing the bundles. Deidentified outcome, structure and process data reported to the AIM data center, is benchmarked with other similar hospitals within states and networks and reported back to the participating hospitals and states. Hospitals and states are guided to actively use the data for quality improvement.
The AIM team develops, identifies and provides an increasing number of resources for hospitals and state teams to implement the Maternal Safety Bundles. These include online, interactive and brief learning modules for staff education; check lists; work plans; direct links to tool kits and other published resources. The AIM website (www.safehealthcareforeverywoman) holds these resources and provides assistance with data management, and a contact/help center. AIM participants from hospitals and state teams are encouraged to engage in monthly calls with other states and hospital network participants as learning communities. AIM has developed a 14-state collaborative to identify the national metrics and resources required to implement the AIM bundle: Obstetric care of women with opioid use disorder. AIM is continually reviewing and revising resources for implementation and growth. All resources are open access and can be shared freely.
AIM supports participants by offering Part IV maintenance of certification for physicians and offer CEUs for nurses utilizing the online modules. AIM is developing an award program for participating hospitals. AIM programs in low resource U.S. settings and countries are dramatically proving the basic concepts of AIM. Dedicated, health care professionals of multiple disciplines and training levels use the AIM bundles and work in concert to reduce barriers and improve communication to reduce maternal mortality and severe morbidity. And though only 3 years since development, AIM is showing significant reduction in the rate of severe maternal morbidity (7.8 to 22% decrease) within the 5 states that began bundle implementation in 2015. Below are the States currently engaged in AIM (Table 2). At the time of publication another 13 states have indicated interest to enroll in AIM.
#open access publishers#Juniper Publsihers#reproductive health#peer review journals#GJORM in juniper publishers
0 notes
Text
The Huge Burden of Infertility in India- Are We Crumbling Underneath?
Authored by: Sabahat Rasool*
Mini Review
The good news is that around 90% of infertility issues are treatable. The success stories of Assisted Reproduction are getting bigger and bigger. We are on the verge of making artificial gametes. The bad news is that the burden of infertility (not able to get pregnant after 12 or more months of regular unprotected sexual intercourse) is high. The World Health Organization (WHO) states that one in every 4 couples in developing nations is affected by infertility [3]. India has 22-23 million infertile couples, and the total fertility rate, which is the number of children who would be born per woman if she were to pass through the childbearing years bearing children according to a current schedule of age-specific fertility rates, has declined from 3.9 in 1990s to 2.3 in 2013 [4]. On the contrary, the use of contraceptives has increased from 45% in 1988 to around 59% in 2015. The expected prevalence of contraceptive use is expected to further rise to 63% in 2020.
In the past, women would get married at the age of 16 to 18 years or even earlier and complete their families by the age of 25 to 26 years! Hence sexual activity happened in wedlock within the most fertile period of their lives. Today the scene is totally different and alarming! There is a marked deterioration of risk factors for infertility. Age at marriage and first pregnancy has risen. Lifestyle changes have gone from bad to worse, and include increasing age at marriage, increasing number of working women who delay pregnancy, rising alcohol and tobacco consumption, sedentary lifestyle coupled with fast food consumption, and disturbing levels of obesity. More educated women are more likely to postpone marriages and childbirth. They also likely to opt for smaller family size as they are busy with their careers and work commitments. The prevalence of smoking among Indian men is around 48%, which is way higher than that in the UK and the US. Smoking is known to lower the sperm count, motility as well as function [5,6].
To make things even worse, Polycystic Ovary Syndrome (PCOS), tuberculosis, and pelvic infections have been on a rise [7]. The global prevalence of PCOS ranges between 5-10%. However, the prevalence is Indian subcontinent has been estimated to be between 4 to 25% in various studies [8]. As far as the ovarian reserve of a woman is concerned, it is well known that Asian women are lower in their reserves compared to Caucasians. This boils down to reduced fertility at younger ages [9]. It is disheartening to know that only 1% of infertile couples in India are seeking fertility treatment. This may be attributed to low awareness and accessibility issues, high cost and unacceptability. Even in the metropolitans like Mumbai and Delhi, the demand for fertility treatment is 9 to 12 times higher than the current market. The dismal state of low penetration of infertility treatments is adding fuel to the fire. There is a small pool of IVF specialists and trained embryologists in the country. From a pool of around 25,000 gynecologists, only around 1000 are performing the actual IVF procedures. At present, the estimated number of in-vitro fertilization cycles countrywide are around 1,00,000 and it is expected to touch 2,50,000 and above by the year 2020. An average IVF cycle costs between 1,00,000 and 1,25,000 Indian Rupees [10]. Despite the treatment cost being 3-4 times lower compared to the US, treatment is affordable to only 20% of the general population. The low income-group patients form a major chunk as they are more driven be family pressures and stigmatization. None of the insurance programs and only a handful of public hospitals offer IVF.
We must focus on creating national awareness through patient education at a war footing. There is an urgent unmet need to include fertility treatments in comprehensive reproductive health care and insurance programs and to explore public-private partnerships to increase the penetrance of fertility treatments. The skill gap has to be bridged to deliver high-quality care by increasing the pool of trained IVF specialists, and as the field of reproductive medicine is growing by leaps and bounds, making sure that the treating physicians are abreast with the latest evidence-based medicine.
#open access journals#Juniper Publsihers#GJORM#peer review journals#global journal of reprodutive medicine
0 notes
Text
Household Survey assessing Impact of Safe Abortion and Contraception Interventions in Cambodia
Authored by: Sarah Bandali*
Introduction
Cambodia has made significant progress in improving the health of women and children. Since the 1990s, strong political will combined with evidence-based policies have advanced reproductive, maternal, newborn and child health (RMNCH) outcomes including among others: improved access to contraceptive services and the legalization of abortion [1]. The pro-natalist policies in Cambodia between 1971-1991, encouraging families to have many children and increase population size were reversed [2]. A birth spacing policy was implemented in 1995, which lead to substantial improvements in access to and use of contraceptive methods. As a result of such policies, there is almost universal knowledge of modern contraceptive methods among women, and the use of modern methods of contraception continues to increase from 19% in 2000 to 39% in 2014 [3].
In 1997, abortion was legalized (up to the 12th week of pregnancy). The law is one of the most liberal in Asia; however, safe abortion services were limited until wider roll-out kick-started in 2005 with the help of external partners [4]. Health-care providers in public and private facilities were trained on safe abortion and, in 2010, medical abortion was endorsed by the government. As a result, more women now have access to safe abortion services, with noted declines in maternal deaths resulting from unsafe abortion [5]. According to the 2014 Demographic and Health Survey[3], 12% of women in Cambodia aged 15-49 years of age reported having one or more abortions in their lifetime. Most women (60%) had an abortion in a health facility, with the majority going to the private sector. Women who had an abortion from a qualified health care provider decreased over time from 79% in 2005 to 61% in 2014. The proportion of women who did not receive any assistance in their last abortion rose from 8% in 2005 to 30% in 2014 indicating that an increasing number of women are not accessing safe abortion services.
The Reduction in Maternal Mortality Project (RMMP) was implemented over a three year period to support the Government of Cambodia’s efforts in providing quality safe abortion and contraceptive services. RMMP’s support to service provision included capacity building of service providers and trainers; quality assurance visits; application of clinical guidelines and protocols and case reviews of critical clinical incidents. Complementing service provision interventions, RMMP improved community awareness, promoting messages on safe abortion and access to contraception. A household survey was conducted with 1,680 women in six provinces of Cambodia to assess the impact of RMMP service provision and community awareness interventions for wider learning within Cambodia and beyond [6].
Methods
A cross sectional household survey was implemented in six provinces: Takeo, Kampong Thom, Prey Veng, Siem Reap, Pursat and Kampong Som. Data was collected using a knowledge, attitudes and practices (KAP) questionnaire focused on abortion and modern contraceptive methods. The study populations were female household members of reproductive age (15-49 years). A sample size of 1,680 was appropriate for measuring KAP variables in the selected communities and allowed for comparisons between the different provinces with a power of >80% and with a significance level of 0.05, taking into account the design effect of 1.34. A total of 42 clusters were therefore surveyed: Seven villages in each of the six selected provinces. In each cluster, 40 questionnaires were administered among women residents of randomly selected households. The respondents were selected using a two-stage cluster sampling method. The first stage of sampling consisted of a random selection of the clusters in 6 provinces where interventions were implemented.
Service Delivery Arm
Siem Reap and Prey Veng provinces only service provision interventions were implemented
Combined Intervention Arm
Takeo and Kampong Thom provinces where both community awareness and service provision interventions were implemented.
Control Arm
Sihanoukville and Pursat provinces where RMMP was not present and where no providers were trained on safe abortion practices
The second stage was the selection of households where the WHO random walk approach was used. Comparisons were made between the two intervention arms (service delivery and combined interventions) and between each intervention arm and the control arm. Descriptive statistics were used to measure KAP. A chi-square test was used for comparison between intervention and control clusters of households. To identify predictors of safe abortion practices, univariate and multivariate analyses were performed using logistic regressions.
Go to
Results
Profile of respondents
There was no significant difference in the profile of respondents in the three arms. The average age of women interviewed was 30 years. Seventy-three percent of women had already experienced a pregnancy. Sixty-seven percent of respondents were married and living with their husband or living with a man as married. Eleven percent of them had an abortion, 27% of them had more than one.
Knowledge attitude and practice related to contraceptives
Ninety-eight percent of respondents knew at least one method of contraception. The daily pill was most cited and significantly higher in the combined intervention arm (93%) than in the service provision and control arms (88%). Injectables were the second most cited method (77%) and was significantly higher in the service delivery arm (82%) than in other arms (75%). Sixteen percent of the women interviewed knew about female sterilization. The percentage is significantly higher among women in the two intervention arms (19%) than in the control arm (10%)
Use of contraceptive methods
Twenty seven percent of the women do not have their family planning needs met and 21% stated that their last pregnancy was unwanted; there is no significant difference between the three arms. Thirty-five percent of respondents indicated they are currently using a contraceptive method (Table 1). 41% in the combined intervention arm, 36% in the service delivery arm and 28% in the control arm (p< 0.001). More women in the intervention arms (64%) received their contraceptive method at the health center compared to the control arm (55%) (p< 0.001).
Contraception services provided by health staff
In the intervention arms, more women reported receiving advice from a provider on contraceptive use (76%) compared to the control arm (67%), (p< 0.05). Also, in the intervention arms, a higher percentage of women reported receiving information on alternative methods (66%) than in the control arm (45%), (p< 0.001).
Knowledge of the legal status of abortion
In intervention arms, more women know that abortion is legal (24%) than in the control arms (7%) (p<0.001). In the combined intervention arm, significantly more women received information about the legal status of abortion from medical staff (30%) than in the service delivery arm (18%), (p<0.001) (Table 2).
Knowledge of a place to obtain a safe abortion
In the intervention arms, 88% of women said they know where to get safe abortion and 67% were able to name a safe abortion facility. In the control arm, 71% of women said they knew where to get safe abortion (Table 2). The proportion differs between the arms (p<0.001): In the combined intervention arm, more women were able to name a safe abortion facility (86%) than in the service delivery arm (47%). Women in the control arm were not able to name a safe abortion facility as these were not available in the provinces.
Knowledge of timing and legal status of abortion
On average, 96% of women know that the safest time for an abortion is during the first trimester. Seventy five percent of the respondents said any pregnancy could be legally ended if the health of the mother or the child is in danger with no difference between the three arms. Only 47% of the respondents thought that abortion was legal in cases of rape or incest. The percentage is significantly higher in the intervention arms (53% on average) compared to the control arm (36%) (p<0.001). Only 21% of respondents said that any pregnancy could be legally ended during the first trimester. This percentage is lowest in the control arm (13%) and increases in the service delivery arm (21%) and more so in the combined intervention arm (30%). The percentage is higher on average in the intervention arms (27%) than in the control arm (13%), (p<0.001) (Table 2).
Knowledge of the risks of an unsafe abortion
Severe bleeding and death were the two risks associated with unsafe abortion that women were aware of especially in the intervention arms. On average, 55% of the respondents in the intervention arms were able to cite death as a possible consequence of an unsafe abortion, compared to 42% of women in the control arm (p<0.001). Fifty-nine percent of the respondents in the service delivery arm know that severe bleeding can occur after an abortion, compared to 53% in the control arm (p=0.04) (Table 2).
Induced abortion
Overall, 17% of the women interviewed who wanted to have an abortion were not able to mainly due to fear of health side effects (24%), husband not agreeing (23%) and lack of funds (21%). There was no significant difference between the arms. Among the 134 women who said they had at least one induced abortion, the average number of abortions per woman was 1.4 in their lifetime with no difference between the arms; 97% of the last pregnancy terminations were during the first trimester, 3% were terminated during the second trimester and no pregnancy was terminated during the third trimester. Most of the women (average 64%) go to a private facility for an abortion, although this is less usual in the combined intervention arm (48%) than in the service delivery or control arms (72%), (p=0.002) In the combined intervention arm, 32% of the women went to a public facility for their last abortion versus 7% in service delivery arm (p=0.002).
Methods of induced abortion
Of the women who had an abortion, 63% reported their pregnancy was terminated using manual vacuum aspiration (MVA); 22% reported their pregnancy was aborted using medical abortion pills and 9% reported the dilation and curettage method was used (Table 3). The proportion of women who said they had taken abortion pills is higher in the combined intervention arm (31%) than in the two other arms though this is not statistically significant.
Use of Safe abortion facilities
Most women (87%) were assisted by a trained provider for their last abortion; 80% from a midwife, 16% from a doctor and 12% from a medical assistant. In the intervention arms, the proportion of women using safe abortion facilities is similar: 58% of the women who had an abortion in the past three years used a safe facility. Half of the women who went to safe abortion facilities knew the name of the provider and these were all registered as trained providers.
Women’s perception on the quality of abortion care
A higher number of women in the intervention arms reported receiving clear information on the abortion procedure beforehand (69%) than in the control arm (32%). Also, a greater number of women said they received information about potential complications after the abortion in the service delivery arm (84%) than in the control arm (60%).
Contraception after abortion
On average, 66% of the women said they received information on contraceptives immediately after their last abortion. The performance of medical staff in the service delivery arm is better, with 80% of women reporting having received information. In both intervention arms, 75% of the women were referred to get a contraceptive method after the last abortion, compared with 50% in the control arm.
Use of contraceptive method after an abortion
There is no significant difference between the arms in the current use of contraceptive method after an abortion. The daily pill is the most commonly used (33% of all women). Injectables are used by 21% of women while 10% use the rhythm method and another 10% use male condoms.
Discussion and Conclusion
Findings from the study show significant differences in the provinces where RMMP implemented activities compared to control areas. Women in the intervention provinces are more aware and have more knowledge of contraceptive methods and safe abortion practices. In service delivery areas, health providers did significantly better in providing information on various contraceptive methods. This finding aligns to other studies in Cambodia where health provider attitudes influenced clients’ intention to use health services, more so than physical and financial barriers [7,8]. Training providers in reproductive health care, particularly midwives and medical assistants who by law are allowed to provide surgical abortion until 12 weeks gestation had an immense impact in RMMP supported provinces [9]. Evidence suggests that mid-level providers working in remote areas, are either already providing medical abortion or have the skills to adminster this already. With some additional training, access to quality reproductive health services can be greatly improved [10,11].
A significant number of women are going to health centers for a contraception method in provinces where RMMP interventions were implemented. Women in intervention provinces are more informed about contraceptive methods and side effects and are more likely to use a method properly. This complements another study in Cambodia which showed increased contraceptive use once women had better knowledge and access to methods [12]. Significantly more women in the intervention areas are informed of the legal status of abortion, having received information about this from health providers. Almost all women knew that the safest time for an abortion is during the first trimester and that any pregnancy could be legally ended if the health of the mother or the child is in danger. This finding confirms evidence suggesting that both providers and women need to be educated about the legal status of and where to access safe abortion and contraception services [13]. Legalization of abortion has had a positive effect in other countries including in South Africa [14], Guyana and Nepal where morbidity and mortality due to unsafe abortion was reduced [15,16]. While legalization of abortion is a major step forward, access to skilled care and safe abortion methods are essential to reducing the burden of unsafe abortion and maternal mortality as well as improving women’s health more broadly [17].
Abortion by MVA is most commonly used followed by medication abortion. Curettage is less used and often provided in the informal sector. An earlier 2007 study however showed that curettage was the most common method for performing abortions in Cambodia [18], suggesting that there have been improvements in the roll out of MVA and medical abortion [19]. Women in intervention areas reported receiving clear information on the abortion procedure beforehand and on possible complications after the procedure. More women in intervention areas know where to find a safe abortion provider. Most of the women were referred for contraceptive services after their last abortion. Another study in Cambodia suggested increased contraceptive use after the implementation of safe abortion services [20]. Accelerating interventions to improve access to safe abortion and contraceptive services will be essential for Cambodia to improve health and achieve its Sustainable Development Goals [7,21].
#open access journals#Juniper Publsihers#GJORM in juniper publishers#peer review journals#reproductive medicine
0 notes
Text
Uterine Torsion–A Case Report and Literature Review
Authored by:
Abstract
Uterine torsion is defined as rotation of the uterus around its longitudinal access by more than 45 degrees. It is associated with increased morbidity and is difficult to diagnose antenatally, resulting in diagnosis during caesarean section, often after the fetus has been delivered via incision into the posterior uterine wall. This has ongoing ramifications for the patient associated with increased risk of uterine rupture in future pregnancies and possibly increased bleeding intraoperatively. Aetiology of uterine torsion is unknown but an association exists with uterine anomalies and fetal mal-presentations. The authors present a case of uterine torsion in a gravida 4, para 2 diagnosed at repeat elective Caesarean Section. Our patient had a significant history of malpresentations in her two previous pregnancies and had a breech presentation in this pregnancy. The levo-rotated uterus was diagnosed following the breech extraction of the fetus via posterior hysterotomy and was complicated by a tear in the right infundibulopelvic (IP) vascular bundle. Given the rarity of this presentation and potential implications, this case report aims to increase clinician awareness of uterine torsion and provide an update on this condition to facilitate earlier intrapartum diagnosis and decrease potential morbidity.
Keywords: Uterine torsion; Uterine disease; Torsion abnormality; Pregnancy complications; Dystocia; Caesarean section; Morbidity; Uterine wall; Aetiology; Fetal mal-presentations; Posterior hysterotomy; Infundibulopelvic; Vascular bundle; Omental adhesions; Hepatitis; Haemoglobin; Aneuploidy; Pfannensteil; Monocryl suture; Vaginal bleeding; Abdominal pain; Urinary symptoms; Laparotomy; Hysteroscopy
Case Report
A 38-year-old woman Gravida 4 Para 2 was admitted to the Cairns Hospital for an elective repeat caesarean section at 39 weeks gestation. She had one emergency Caesarean Section in 2008 for transverse lie and one elective repeat Caesarean Section for breech presentation at term in 2010. Both procedures were uncomplicated with some omental adhesions noted on repeat caesarean section. Other than her BMI of 48 and a diagnosis of genital herpes in 2010, she had a low risk pregnancy. Antenatal investigations revealed a normal glucose tolerance test at 18 and 28 weeks gestation, a negative serology for hepatitis B, hepatitis C, HIV, Syphilis and a Haemoglobin of 117. Her combined first trimester screen revealed low risk of aneuploidy and an ultrasound scan at 20 weeks revealed a single fetus with normal morphology and a placenta posteriorly located and clear of the cervical os. She had an ultrasound to assess fetal growth at 34 weeks which showed a normally grown fetus on the 75th centile with an AFI of 10.2cm and normal umbilical artery dopplers.
On the day of her procedure the fetus was noted to be in a footling breech presentation. During the caesarean section, a pfannensteil skin incision and layered entry to the peritoneal cavity was undertaken. Prominent large vessels extending from the right Iliac fossa were noted over the lower segment of the uterus and the orientation of the uterus was checked by palpation of both ovaries. As the lower segment could not be accessed easily due to the presence of large vessels, an upper segment transverse incision was undertaken and a breech extraction of a 3.66kg female neonate was completed easily. The placenta was delivered and the uterus closed in 2 layers with 1 monocryl suture. There was no uterine abnormality or fibroid noted. On completion of suturing, brisk bleeding was noted to be arising from one of the large venules covering the lower segment of the uterus. After clamping the vessel, the uterus, now in a contracted state dextro-rotated 45 degrees spontaneously and was then manually dextro-rotated 145 degrees to reveal that a posterior hysterotomy had been performed. After establishing correct orientation of the uterus, the bleeding vessel was noted to be a superficial vein arising from the from the right infundibulopelvic (IP) vascular bundle.This was ligated with vicryl 2-0 with good effect. The total blood loss during the procedure was 1200mls.
Literature review
A search of medline and pubmed was undertaken with the use of key word “uterine torsion” and MESH terms “uterine disease”, “torsion abnormality”, “pregnancy complications”, “dystocia” and “caesarean section” with limitation to human research and English language. A total of 52 articles were attained: 4 articles were unrelated to uterine torsion, 10 articles described torsion in the non-gravid uterus and 38 articles were related to uterine torsion during pregnancy. One review article and 37 case reports were found among the articles pertaining to uterine torsion in pregnancy.Rotation of the gravid uterus under 45 degrees is a normal finding in pregnancy and likely results from the positioning of the recto-sigmoid colon on the posteriorlateral aspect of the uterus. Uterine torsion is defined as more than a 45-degree rotation of the uterus around its longitudinal axis with two-thirds dextro-rotated and 1/3 levo-rotated [1]. While uterine torsion is well described in the veterinary world, it is a relatively rare presentation in pregnant women and can result in significant morbidity. Following the review of 212 cases of uterine torsion by Jensen [2], there have only been 37 case report of uterine torsion in pregnancy that have been subsequently published.
Aetiology of uterine torsion remains unknown, though there is an association with pre-existing uterine anomalies, fibroids and non-cephalic fetal presentations [1].Case reports of uterine torsion in women with connective tissue abnormalities [3], external cephalic version and external trauma also exist as is without any predisposing factor in approximately 16% of cases [4,5]. Nevertheless, many of these predisposing factors are relatively more common compared to frequency of uterine torsion, indicating there may be some other influences intrinsic or extrinsic. In our case, our patient had malpresentations throughout all her pregnancies but no other known risk factors.
Symptoms of uterine torsion are variable with approximately 11% of women asymptomatic at the time of diagnosis as was the case in this example [2]. Symptomatic presentation includes abdominal pain, vaginal bleeding, shock, intestinal and urinary symptoms, obstructed labor and suspected fetal compromise [6,7]. Uterine torsion has been associated with maternal and perinatal mortality in historical cohorts. The mechanism of perinatal morbidity and mortality has been abruption secondary to venous engorgement and retro-placenta pressure and torsion affecting blood flow through the uterine arteries. Historical cohorts place perinatal mortality at approximately 12%, some of this may be due to prematurity [5]. Since 1990, only one other maternal death has been reported in the Ivory Coast [8,9]. At the time of laparotomy, the abnormal position of vessels across the lower segment of the uterus may indicate the diagnosis of torsion as was noted in this case report. Palpation of the round ligaments may facilitate the diagnosis if it is suspected as palpation of adnexal structure alone may not indicate rotation if they are symmetrically present.
If uterine torsion is noted at the time of laparotomy, detorsion of the uterus and appropriate incision on the anterior aspect of the uterus is advised. However, this is not always possible or easily identified and a posterior hysterotomy incision, either in the upper or lower segment of the uterus is required for the delivery of the fetus [10-13]. De-torsion once delivery of the fetus is undertaken and the uterus is contracted is often easier and may occur spontaneously. Some case reports report possible morbidity with a posterior incision with increase in bleeding and possible uterine rupture/dehiscence in subsequent pregnancies. Some of this is attributable to the uterine congestion associated with torsion [14], an upper segment incision into thick vascular myometrial tissue and inadvertent extension into the uterine vessels due to the anatomical rotation of the uterus and relative placement of the incision (reference). In our case, these were not the main issues, but rather bleeding from a large superficial vein in the stretched right infundibulopelvic (IP) ligament which had torn with the delivery of the fetus. This was subsequently ligated once de-torsion of the uterus occurred. This is the first time that bleeding from the IP ligaments vessels in a case of uterine torsion has been reported.
The impact of a posterior uterine incision on future reproductive outcomes especially in the presence of anterior uterine incision (previous caesarean sections) is unknown. Laparoscopy and hysteroscopy following a posterior uterine incision has shownappropriate healing but the lack of substantive evidence supporting the safety of vaginal birth after a posterior hysterotomy has prompted some authors to pursue contraception (tubal ligation) at the time of operation or recommend an elective caesarean section at early term gestation [13]. The impact on intra-abdominal adhesion formation and significance of symptoms of uterine rupture/dehiscence with a posterior hysterotomy is unknown [15-20].
Conclusion
The authors present a case of asymptomatic torsion with 180-degree levorotation of the uterus at the time of caesarean section. Diagnosis was made following delivery of the fetus and de torsion of the uterus to facilitate hemostasis of a bleeding vein in the IP vascular bundle [21,22]. This case report and review has been undertaken to reaffirm the awareness of uterine torsion among practitioners and provide an update of this rare obstetric condition. Correctly identifying the orientation of the uterus prior to hysterotomy and correct placement of the uterine incision will minimize any associated morbidity.
#open access journals#Juniper Publsihers#global journal of reprodutive medicine#peer review journals#GJORM in juniper publishers
0 notes
Text
A Study Towards Awareness and Corrective Measures of HIV/AIDS in North-Western Part of Nigeria Through Statistical Assessment
Authored by: Singh V V*
Introduction
HIV/AIDS (Human Immunodeficiency Virus/Acquired Immune Deficiency Syndrome) has affected many people in the world leading to their death since the early 1980s. The number of people affected by the virus continues to rise, and many attempts have been made to produce drugs/vaccine to control the virus, but up to now, a concrete solution has not been found.Nigeria has passed through several phases in her response to the AIDS epidemic. The stages included an initial period of denial, a large health sector response, and now a multi-sectoral response that focuses on prevention, treatment, and mitigation of impact interventions and divorces coordination and implementation as distinct response components. A central body is dedicated to leading and coordinating the response, while the various sectors, including civil society organizations (CSO), faith-based organizations and networks of people living with HIV and AIDS support groups focus on packaging and implementing interventions based on a national action plan[3,4].
The health response commenced with the setting up of an ad hoc National Expert Advisory Committee on AIDS (NEACA) in 1987. By 1988, the National AIDS and STDs Control Programme (NASCP) was formally established, with state counterparts set up after that to organize as well as to coordinate all HIV and AIDS activities at national and state levels. Federal Ministry of Health’s HIV & AIDS division and High-risk groups including brothel-based sex workers, non-brothel based sex workers, men having sex with men, injecting drug users, uniformed servicemen (Armed forces and Police) and transport workers, (Formerly known as NASCP) played a key role in developing guidelines on key interventions and monitoring of the epidemic. In 1997, the National Council on Health formally endorsed the multi-sectoral approach, and in 2000 the Federal Government of Nigeria commenced the implementation of this approach with the establishment of a Presidential Council on AIDS (PCA) and National Action Committee on AIDS (NACA).
NACA has been transformed from a committee to an agency and now called National Agency for the Control of AIDS (NACA), for effective coordination of the national multi-sectoral response to HIV & AIDS. An HIV & AIDS Emergency Action Plan (HEAP) was initiated in 2001 which ran through 2004. The partners involved in implementing the plan included governmental institutions, non-governmental organizations, community-based organizations, faith-based organizations and persons living with or affected by HIV and AIDS. As part of renewed efforts, Nigeria launched a revised HIV and AIDS policy and a five year (2004- 2008) National HIV and AIDS Behaviour Change Communication Strategy in 2003 and 2004, respectively[6-8].
The country also launched the Nigeria National Response Information Management System (NNRIMS) for HIV and AIDS (NACA, 2004).The NNRIMS has been reviewed, and an operational plan (2007 – 2010) has been developed. Failure of access to HIV & AIDS treatment and services by the people needing them has prompted a rapid scale-up of the national response and made it appropriate to align the NNRIMS framework with issues articulated in the National Strategic Framework (NSF) as well as in the Nigeria road map moving towards Universal Access (UA) for prevention, treatment and support. This is done in collaboration with donors and partner. The Federal Ministry of Health has recently undertaken an intensive review of health sector HIV and AIDS response and developed the Health Sector Strategic Plan. The HIV and AIDS National Strategic Framework for Action (2005-2009) was developed under the leadership of NACA to replace HEAP with the intention of significantly scaling up the anti-retroviral treatment programme. The country also completed a policy document titled “Plan to scale-up antiretroviral treatment for HIV and AIDS in Nigeria2005-2009” with the overarching goal of improving the survival, quality of life and productivity of people living with HIV and AIDS (PLWHAs) [9].
The Nigerian government has also continued to be pro-active in its efforts to confront the HIV scourge with its overarching strategy elaborated in the bottom-up, poly-stakeholder and multi-sectoral National Strategic Plan (NSP). The NSP is derived from the architecture of the National Strategic Framework 2010- 15 (NSF II) and has targets to halt and begin to reverse the spread of HIV infection, as well as mitigate the impact of HIV & AIDS by 2015. With the condition that where appropriate, the targets of the NSP should be population-based, the Federal Government of Nigeria implicitly recognizes HIV care and treatment as national public health good.
HIV prevalence in Nigeria is high considering the huge population (about 170 million) and the rate is higher than that of sub - Saharan African estimate of 3.4% (PRB, 2012). About 3.5 million people in Nigeria are estimated to be living with HIV/ AIDS, and the estimated number of new infections and HIV/ AIDS-related deaths was 390,000 and 217,000 respectively in 2013 (General Population Survey, 2013).There is a slightly higher HIV prevalence in the rural areas (3.6%) than in the urban areas (3.2%). The distribution of the epidemic varies from region to region with the south-south zone (5.5%) and lowest in the south-east (1.8%). In Northeastern Nigeria where most of the people live in rural areas, the spread of HIV/AIDS causes includes sexual activities of adolescents and young adults polygamy and multiple sexualpartners, illiteracy, ignorance and poverty. According to Baker et al. [10], many research findings have shown that higher education level is associated with lower level of risk of being infected with HIV/AIDS.This study will attempt to find out are people of Northern Nigeria aware of HIV/ AIDS. The objective is to enlighten them so that the spread of the epidemic can be reduced among them[11].
Awareness of HIV/AIDS among Nigerians
Good health is basic to human welfare and is a fundamental objective of social and economic development. HIV & AIDS and poor reproductive health (RH) still constitute major challenges to health and development in Nigeria. Addressing health challenges starts with identifying the problems, their causes, and determinants.The health environment is ever changing and shaped by new science, information, policies and sociocultural forces.Thus, there is the need to actively continue the collection of reliable data on health knowledge, attitude and the magnitude of the HIV & AIDS epidemic[12]. This is necessary for us to improve our understanding of changing prevention needs, challenges and opportunities as well as stimulate appropriate public health action. This will ensure that on-going interventions and our future direction in policy formulation and programme development remain evidence-based. Scientific evidence must be incorporated into making management decisions, developing policies and implementing programmes to recognize and respond effectively to health problems.
Nigeria has undoubtedly made some progress over the years in containing and creating awareness on the scourge of HIV/ AIDS. Many lives have been saved through the awareness campaigns and provision and access to the antiretroviral (AVR) drugs for people living with HIV/AIDS. There are Federal and State agencies created and charged with the responsibilities of handling HIV/AIDS issues. (National Agency for the Control of Aids (NACA) and State Agencies for the Control of Aids (SACA).However, research shows that only a quarter of children living with HIV have access to antiretroviral therapy, and in some countries, coverage for children is half the coverage for adults[13,14].
Available statistics indicate that up to 50 percent of children living with HIV/AIDS may die before their second birthday and 80 percent before their fifth birthday due to lack of access. Research has also shown that more than three million children are living with HIV with nearly 90 percent of them in sub-Saharan Africa, even as efforts to reach children and adolescents living with HIV have not moved as fast as that of adults. However, many still live without knowing their status, even as stigmatization remains an issue.As part of efforts to raise the bar on HIV/AIDS awareness in the country, Humanity Family Foundation for Peace and Development (HUFFPED) in partnership with Lagos State AIDS Control Agency (LSACA) and ActionAid recently organized the international AIDS conference tagged: “Stepping up towards HIV-free Nigeria.”Experts, however, argue that there is need to increase awareness of HIV /AIDS and create the enabling environment that will give people living with HIV/AIDS a sense of belonging in the society, even as the government also needs to ensure the availability of the antiretroviral drugs to those that need them[15].
The significance of the study
This study is very significant because the outcome will give an idea on what to do on HIV/AIDS in northern Nigeria to reduce its infection. If the result shows a high percentage of awareness, public enlightenment should continue but if it is low, then enlightenment and counselling should be intensified, and standard medical facilities and qualified medical personnel should be deployed to these areas by the government and non-governmental organizations to control the spread of the epidemic.
Methodology
Study design
In this study, secondary data collected from the Federal ministry of health through National HIV & AIDS and Reproductive Health and Serological Survey (NARHS Plus) used. The survey is a cross-sectional study covering sampled individuals in North- Western Nigeria according to state.
Result
The results and analysis on awareness, knowledge of HIV/ AIDS, how it is spread, how it can be prevented, misconceptions about transmission and prevention of HIV and respondents’ assessmentof their risk of contracting HIV by states in North- Western Nigeria are presented in tables and chats for easy understanding and interpretation[16].
Respondents were asked whether they have heard of HIV/AIDS and thought there was a cure for it. The results are presented in Table 1 and Figure 1. Eighty-five percent (85%) of the respondents reported that they have heard of HIV/ AID and are aware of it and about Sixty-three percent (63%) reported that AIDS has no cure. Only about sixteen percent (16%) reported that AIDS does have a cure and about twentyone percent (21%) reported that they have not heard of AIDS. This proportion was highest among the respondents with higher educational attainment compared to those with no formal education but about the same proportion for females and males, as well as respondents from rural and urban areas.From the previous analysis which has shown that awareness about HIV/ AIDS is high in the whole of North-Western Nigeria, the analysis according to the states has also proved that with Kaduna state having the highest percentage of awareness. The results are presented in Table 2 and Figure 2 [17,18].
Respondents were asked whether they know how a person can get the virus that causes AIDS. The results are presented in Table 3 and Figure 3. About eighty percent (80%) reported that they know that it can be gotten through sexual intercourse, sixtytwo percent (62%) reported through blood transfusion. About forty-seven percent (47%) reported through mother to unborn child, and about seventy-one percent (71%) reported that it could be contracted through sharing of sharp objects like a razor. Sixty-four percent (64%) reported through sharing of needles. About forty-two percent (42%) of the respondents reported that they know of the all five ways that a person can contract the virus that causes AIDS. This proportion was highest among the respondents with higher educational attainment compared to those with no formal education but about the same proportion for females and males, as well as respondents from rural and urban areas[19,20].
Respondents were asked whether they know ways of preventing HIV infection. The results are presented in Table 4 and Figure 4. About seventy-four percent (74%) reported that they know that it can be prevented by staying with one uninfected partner. About thirty-eight percent (38%) reported that it could be prevented by using a condom every day. Fifty-nine percent (59%) reported that it could be prevented by abstaining from sex. About sixty-two percent (62%) reported it could be prevented by avoiding sex with commercial sex workers (CSW). Fifty-three percent (53%) reported that it could be prevented by reducing the a number of sexual partners. About Sixty percent (60%) reported that it could be prevented by avoiding sex with people with multiple sexual partners and about sixty-seven percent (67%) of the respondents reported that it could be prevented by avoiding sharing sharp objects. This proportion was highest among the respondents with higher educational attainment compared to those with no formal education.Respondents were asked about ways of transmitting HIV. Among the respondents interviewed about seventeen percent (17%) thought it could be transmitted by sharing toilets. About seventeen percent (17%) thought it could be transmitted by sharing utensils like a spoon, dish, plate, etc. and about seventeen percent (17%) thought it could be transmitted by mosquito bites and bed bugs. Only about ten percent (10%) thought it. The effect of Human Immunodeficiency Virus/Acquired Immune deficiency syndrome(HIV/AIDS) global epidemic continue to emerge decades after the first wave of infection. One keyaspect of controlling the epidemic is by enlightening the general public on the epidemic. That ison how it can be contracted and controlled. Since the start of the epidemic many measures havebeen taken by government and non-governmental organizations to control the epidemic but still itcontinued to infect and kill many people[21,22].
The measures taken includes manufacturing antiretroviraldrugs and therapy, using of condoms and enlightment among others. Nigeria consist of thirty-six(36) states and the federal capital territory (FCT) Abuja, and these are grouped in to six geopoliticalzones. North-Western Nigeria consist of seven states (7) namely Jigawa, Kaduna, Kano, Katsina,Kebbi, Sokoto and Zamfara with a total population of about thirty-five million (35m). Secondarydata from Federal Ministry of Health is used in finding out whether people of North-westernNigeria are aware of HIV/ AIDS? Statistical methods and techniques are used in analysing thedatacould be transmitted by witchcraft while about eighteen percent (18%) thought it could be transmitted by kissing. The percentages of misconception are low because a large number of those interviewed are aware of ways of transmitting the virus. The results are presented in Table 5 and Figure 5.
Respondents were asked about their risk of contracting HIV. Among the respondents interviewed about one percent (1%) have a high chance of contracting the virus and about thirty-one percent (31%) reported low chance. Fifty-one percent (51%) reported no risk at all, and less than one percent (0.4%) have aids while about seventeen percent (17%) no response[23]. The results are presented in Table 6 and Figure 6. The results have shown that most people are aware of HIV and are very careful not to be infected by the virus. Respondents were asked whether they have been counseled and tested for HIV. About fifty-one percent (51%) reported that they had been counseled while about thirty-five percent (35%) reported that they had been tested for HIV(Figure 7 and Table 7)[23].
Conclusion
This study finds that awareness and knowledge of HIV/AIDS are high among people of North-Western Nigeria. Virtually all the variables used in the analysis were significantly associated with awareness and knowledge of HIV/AIDS as shown in the tables and chats. Most people have heard of the virus, how it can be transmitted, avoided and prevented. This proportion was highest among the respondents with higher educational attainment compared to those with no formal education but about the same proportion for females and males, as well as respondents from rural and urban areas
#open access journals#Juniper Publsihers#juniper publishers in GJORM#reproductive medicine#peer review journals
0 notes
Text
Delays in Utilization of Institutional Delivery Service and its Determinants in Yem Special Woreda, Southwest Ethiopia: Health Institution Based Cross-Sectional Study
Authored by: Teklemariam Ergat Yarinbab*
Introduction
Institutional delivery service is one of the key and proven interventions to reduce maternal death. It ensures safe birth, reduce both actual and potential complications and maternal death and increase the survival of most mothers and newborns. But most deliveries in developing countries occur at home without skilled birth attendants. The 2014 EDHS report revealed that 83.4% deliveries took place at home whereas only 15.4% of deliveries were institutional [1]. Maternal deaths are strongly associated with delays to utilization of institutional delivery service and inadequate medical care at the time of delivery. Several factors have been identified as barriers to early access to skilled care by women especially in developing countries; these include perceived quality of care at health facility, inadequate number of skilled personnel, geographical inaccessibility and financial constraints, decision making power, awareness on danger sign of pregnancy and benefit of utilizing institutional delivery services [2]. Even with the best possible antenatal care, it is established that delivery could be complicated and timely utilization of institutional delivery service is essential to safe delivery care [3]. Therefore, the aim of this study was to assess the delays in utilization of institutional delivery service and its determinants in Yem Special Woreda, Southwest Ethiopia.
Methods and Materials
Study area and period
The study was conducted in Yem Special Woreda, Southwest Ethiopia, from Feb 03-28/2018.Yem Special Woreda is located 297 KMs southwest of Addis Ababa. It has three towns and 34 kebeles (the smallest administrative units) with an estimated population of 99,714; of these 50,854 were male whereas 48,860 were females (Projected from 2007 National Census).There were six Health Centres namely Fofa Health Centre, Semonam Health Centre, Saja Health Centre, Toba Health Centre, Deri Health Centre and Gesi Health Centre. Besides, there were 27 Health Posts in the Woreda.
Study design
Health institution based cross sectional study design was used.
Inclusion and exclusion criteria
Inclusion: All women who visited the six health centers for delivery service were included.
Exclusion: All women who were severely sick and unable to respond during data collection period and women who utilized maternal waiting home were excluded.
Sample size determination
For quantitative study: The sample size was calculated using single population proportion formula. The prevalence of first delays in utilizing institutional delivery service 37%(P=0.37) [4], 5% margin of error, 95% confidence level and 10% non response rate were considered. Thus, the total sample size was calculated to be 393.
For qualitative study: A total of eight Focus Group Discussions were conducted. Of these; six FGDs were conducted with MCH service user women whereas two FGDs were conducted with service providers in selected two health centers.
Sampling technique
For quantitative study: The required total sample size was proportionally allocated to the six Health Centers based on their previous three months delivery load. Accordingly, the allocated sample was 94 for Fofa HC, 52 for Semonam HC, 75 for Saja HC, 62 for Toba HC, 56 for Deri HC and 54 for Gesi HC. All pregnant women who utilize institutional delivery service in each health center during data collection period were included in the study until the required sample size was fulfilled.
For qualitative study: Delivery care providers such as nurses and health officers who wereworking at the public health centers and women who camefor MCH services during the data collection period were purposively included in the FGDs. Participants interviewed in the quantitative survey were excluded from the FGD.
Data collection tool and procedure
For quantitative study: Pre-tested structured questionnaire was used to collect the data. The instrument was adopted from JHPIEGO tools and indicators for maternal and neonatal health [5]. Seven health professionals and three supervisors including the principal investigators were participated in the data collection. Half a day orientation was given to the data collectors and supervisors on the data collection tools and procedures by the principal investigators.
For qualitative study: Semi-structured FGD topic guide was used to facilitate the discussion. Each of eight FGDs had 6-12 participants and a total of 72 participants (i.e. 59 service users and 13 service providers) were involved. Each FGD spend 45-60 minutes. Written notes were taken and all the discussions were tape recorded.
Data quality control: The questionnaires were translated from English into the local language (Amharic) & vice versa. A pre-test was conducted on 5% of the sample. Data collectors were well trained. Daily supervision was conducted by the field supervisors and investigators.Supervisors used to check all procedures and completeness of formats randomly. Data were checked before entry. Qualitative records were transcribed carefully in themes and interpreted.
Data processing and analysis
For quantitative study: Data was analyzed by SPSS for windows version 20. Bivariate logistic regression model was fitted as a primary method of analysis. Then, variables having P-value <0.25 were entered into multivariate logistic regression analysis using the forward LR method. Finally, P-value <0.05 in multivariate analysis was used to declare statistically significant variables.
For qualitative study: Written notes from all 8 FGDs were compiled and labelled according to participants’ type. After reviewing individual FGD transcriptions, data was organized according to the themes and summarized manually. The result was presented in narratives triangulated with the quantitative results (Table 1).
Definition of terms
Delays in utilization of institutional delivery service: Refers to the time taken more than one hour to make decision to seek care or more than one hour to reach health facility after making decision or waiting for more than one hour in health facility to receive delivery care.
Delay in making decision to seek care: Refers to the time taken ≥1 hour to make decision to seek care was considered as delay and less than an hour considered no delay.
Institutional delivery utilization: when a mother gave birth at health institution and the delivery was assisted by skilled birth attendant or trained health professional.
Result
Socio-demographic characteristics
A total of 389 respondents involved in the study yielding 98.9% response rate.The mean age of the study participants was 26(±5). Majority of the respondents, 292(75.1%) were Yem in ethnicity. Orthodox Christian, 204(52.4%), was the dominant religion.About 306(78.7%) of mothers were married. Besides, 291(74.8%) of the study participants were house wife whereas 27(6.9%) were Government employees. Two hundred nineteen (56.3%) of them cannot read and write (Table 2).
Obstetric characteristics
About 275(70.7%) of the study participants reported utilization of ANC services. One hundred sixty nine (43.4%) and 142(36.5%) of study participants faced maternal complications during previous and current pregnancies, respectively. With regard to decisions; 151(38.8%) of women decide themselves, 151(38.8%) decide by their husbands and 87(22.4%) decide by their family members to utilize delivery service (Table 3). Besides, 297(76.7%) subjects preferred health facility delivery whereas the rest 92(23.7%) did not prefer the same. The reported reasons for not preferring health facility delivery were 11(12.1%) fear, 16(17.6%) lack of money, 40(44.0%) distance and 24(26.4%) poor treatment from professionals.
Delays in utilizing institutional delivery services
The prevalence of delay to utilization of institutional delivery service in the study area was 76.3% and the mean (±SD) of delay time to utilization of delivery service was 5(±3.08) hours. About 172 (44.2%) respondents reported they faced problems on making decisions to utilize delivery services from health facilities. One hundred sixty-eight (43.2%) respondents reported that they have transportation problems. The study showed 198(50.9%) travelled on foot, 101(26%) were carried by wooden stretcher and the rest 90(23.1%) travelled by car to health facility.The qualitative result showed that, distance and poor road conditions made it virtually impossible for many pregnant women to reach the health facility. In some instances, inadequate or inappropriate transport made it difficult for women to reach the health facility. In the rural areas, the common means of transport is foot; in hills and mountain districts, people carried pregnant women to the health facility on stretchers. Pregnant women faced difficulties in reaching the health facility, especially at night or during rainy seasons. This is supported by the qualitative finding that a 30 years old woman from “Toba kebele” commented: “....It is particularly difficult if the labor begins at night. There is no transport facility and the way is dark. In such a situation, how can we go to the health facility to utilize delivery service..?....”.Other participants of the FGDs also further suggested that lack of transport, long distance from facilities and absence of delivery care centers appear to be significant contributory factors for delay to seek delivery services. From the FGDs we understood that, women who travelled the shortest distance had a high chance of attending and coming early to utilize delivery care from health centers whereas women who were travelling long distances had little chance to seek treatment as early as possible.
About 276 (71%) of the respondents reported that they were happy with the service provided and the rest 113(29%) unhappy. Lack of drug 5(4.4%) and poor treatment from professional 108(95.6%) were making them unhappy to the service provided by the health facility. In support of this the qualitative result showed that there were shortages of midwives and staffs high work load in the health facilities.Due to these, the women waited for long time to utilize delivery service after they reached at health facility. The following two participants of the FGDs suggest the same. A 27 years old Nurse, service provider, from ‘Gesi Health Centre’ commented: “Only one Midwife is available in most of the health facilities in the woreda, thus when she is on leave, in training or transferred to another health facility, women cannot get timely delivery service from the health facility. And also when the number of deliveries exceeded ability to provide services and staff members became overburdened.” Besides; a 34 years old, Health officer, from the same health centre said that “The absence of a clear division of roles among staff members who shared responsibility for providing maternal health services further aggravated this situation and affected worker motivation and performance. This condition leads to delays in utilizing delivery service.” Hence, lack of qualified health professionals and absence of clear job divisions among workers contributes for delay in institutional delivery services.
Determinants of delays in institutional delivery service utilization
The multivariate logistic regression analysis revealed that Parity or having three or more children, not being prepared for birth, low educational status of mothers, and decisions made by husbands were significantly associated with delay in utilization of institutional delivery services. Accordingly, women whose husbands make decisions were two times (AOR= 2.08, 95%CI=1.0, 3.9) more likely to delay in utilization of institutional delivery services as compared to those who make decisions by themselves (Table 4). In support of this finding, a 30 years old mother from Gesi kebele said: “Many husbands do not allow their wives to visit the health facility for seeking delivery services because of traditional beliefs. Women cannot ignore their husbands’ decision and cannot express their opinion in the family”. Hence, it is clear that women who make decisions by themselves free of their husbands influence are more likely to use institutional delivery services on time. The study also revealed that, women who have three or more children are 3 times (AOR= 2.9, 95%CI= 1.57, 5.44) more likely to get delay in utilization of institutional delivery services as compared to those who have two or less children (Table 4). A 42 year old woman from Deri kebele commented that “………..I have four children. They are students and I am caring about their school. I am a house wife and my husband is a farmer. We are responsible for their school performance and economic issues. We did not have money at hand, so I was late in my last birth while my husband was looking for borrowing money for transportation....” Here, from the opinion of woman above, we can deduce that having more children affects the economy of family and in turn causes delay in institutional delivery service utilization.
Discussion
The study assessed delays in utilization of delivery services and its determinants. The prevalence of delays in delivery service utilization was 76.3%. This finding was higher than the finding from a study in rural Bangladesh [6]. This might be due to the existence of differences in accessibility of health facilities and delivery service utilization culture of the community. Regarding physical access to health facility, about 69.4% were found to have no access to health facility or live in a walking distance of greater than one hour and the mean walking distance from their homes was two hours. This finding was slightly higher than findings from studies in selected developing countries by Babinard [7]. The possible reason may be large distances between health institutions due to the sparse pattern of the population in the study area.Besides, this finding was consistent with findings from the 2011 EDHS report in which 66% of mothers did not have access to or live in a walking distance of more than one hour from institutional delivery services in Ethiopia [8]. This is supported by findings from the qualitative study in that most of the participants said they walk a long distance to reach health facilities. Besides, the study revealed that 34.7% of the mothers waited for more than one hour to utilize institutional delivery service after they arrived at health facility. This finding was higher than the findings from a study in Bahir Dar, Ethiopia [9].
The qualitative finding showed that long time admission process, staffs work load and lack of supplies were the main reasons for third delay to utilize institutional delivery service at health facilities.Further the study showed that women whose husbands make decisions were two times more likely to delay in utilization of institutional delivery services as compared those make decisions by themselves. This finding is consistent with the findings from studies in rural Bangladesh and Bahir Dar Ethiopia [6,9]. This also was supported by the qualitative findings in that most of the participants of the FGDs argued that male dominance for decision and not being prepared for delivery was the main reasons for delays in utilizing delivery services. The participants also added unless labour is complicated husbands would not allow their wives to visit health facilities. Delay in utilizing delivery service was seven times more likely among mothers who were not being prepared for institutional delivery as compared to those prepared mothers. This finding was consistent with the cross-sectional study in Kenya and Ethiopia [10,11]. The qualitative study showed that participants did not think it was necessary to go to a health facility for normal delivery unless they experienced a serious problem.
Women who have three or more children were three times more likely to delay in utilization of delivery services as compared to mothers who have two or less children. This finding is consistent with the findings from studies in Bangladesh and Nigeria [12,13]. The possible reason could be the fact that women who have higher parity develop experience and confidence regarding child birth, and hence might delay to utilize delivery services.On top of this, the study indicated that women with low education status were two times more likely to delay in utilization of institutional delivery services as compared to that of literate women. This finding was consistent with the various studies in Nigeria & Nepal [12,14]. The reason could be for educated women might have better access to information about the advantages of institutional delivery and pregnancy related complications.
Conclusion
The prevalence of delays in delivery service utilization was 76.3%. Low educational status of women, parity, not being ready to give birth in health facility and husband’s decision making were found to be determinants of delay to utilize institutional delivery services.
Recommendation
Federal Ministry of Health in collaboration with other stakeholders should promote women education. Regional Health Bureaus’ and Zonal Health Departments’ should strongly advocate the utilization of institutional delivery services. Besides, Woreda Health Offices in collaboration with local government bodies and other stakeholders should work hard to improve the awareness of women on institutional delivery.Ethical clearance letter was obtained from department of Public Health, Mizan- Tepi University. The participants were made aware about the purpose of study, and oral consents were obtained accordingly. The participants’ right to refuse or withdraw from the study and confidentiality issues were considered.
Go to
Acknowledgment
First of all, our deepest gratitude and appreciation goes to Department of Public Health; College of Health Sciences, Mizan- Tepi University. We would also like to extend our gratitude to Yem Special Woreda health office staffs and the health centres staffs for their cooperation in data collection. Finally, our great appreciation goes to the data collectors and supervisors.
#open access journals#peer review journals#Juniper Publsihers#global journal of reprodutive medicine#GJORM in juniper publishers#reproductive medicine
0 notes