#laparotomy pack
Photo
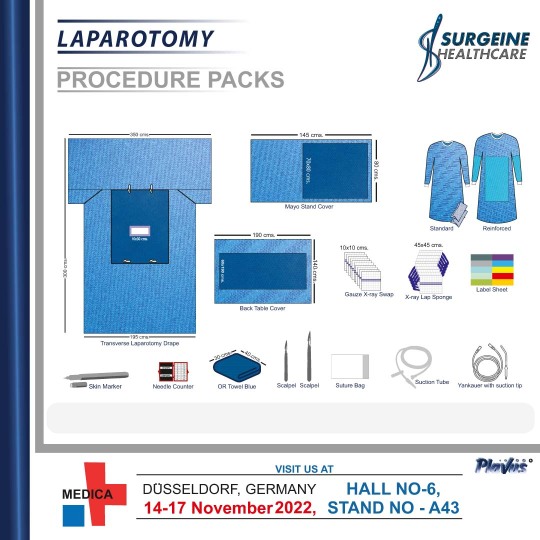
The Laparotomy Procedure Packs are specially designed for various general types of surgical procedures in the operating room. These products offered by us are developed using superior quality raw material in accordance with #international medical standards. Our products are hygienic and are well appreciated in the market for their durability.
0 notes
Text
“Saanvi Roe” 35 (India 2022)
Amniotic fluid embolism is a well-documented complication of second and third trimester abortion. Although exceedingly rare, it can also happen during birth. But AFE is almost unheard of in the first trimester—except as a complication of early abortion.
In 2022, a 35-year-old was killed by an elective legal abortion in India. She died of AFE even though she was in the first trimester. Her identity is unknown, so she has been given the pseudonym “Saanvi Roe”.
Saanvi Roe was 35 and pregnant with her third baby when she went in for a legal 6-week abortion and a tubal ligation. She didn’t know that she was going to die.
Saanvi was given fentanyl, midazolam and propofol during the abortion and tubal ligation. About one hour after the abortion was started, she had difficulty breathing. Even though she was put on oxygen, she deteriorated and developed hypotension, tachycardia and tachypnoea. Her abdomen was distended and she was taken to the ICU.
While she was in the ICU, Saanvi’s condition only got worse. She was put on a ventilator and given blood transfusions. During her last day alive, she was given plasma and 13 units of packed red blood cells. A laparotomy found found ascitic fluid, bowels with petechia, and oozing wounds. However, the sites of her tubal ligation were not bleeding.
Less than 24 hours after the abortion, Saanvi died in the ICU. Her relatives were left to mourn the loss of two family members.
https://www.nih.unboundmedicine.com/medline/citation/35651466/Amniotic_Fluid_Embolism_After_First-Trimester_Abortion.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9135588/pdf/cureus-0014-00000024490.pdf
#tw abortion#pro life#unsafe yet legal#tw murder#tw ab*rtion#abortion#abortion debate#death from legal abortion#unidentified victim
8 notes
·
View notes
Text
Combined cervical laceration and bladder rupture: a case report of an unusual complication of precipitated labor by Dr Fatemeh Darsareh in International Journal of Clinical Images and Medical Reviews

Abstract
Cases of bladder rupture have been rarely reported following vaginal childbirth. To the best of our knowledge, however, no cases of combined cervical laceration and bladder rupture have been reported to date. We present the first case of a 31-year-old woman with gestational diabetes who suffered a combined cervical laceration and bladder rupture after childbirth. Precipitated labor caused by oxytocin induction resulted in vaginal and cervical lacerations. The bladder rupture was confirmed by cystography. A team of obstetricians and urologists performed the laparotomy. The patient was kept under observation for two weeks before being discharged with no serious complications.
Keywords: Bladder rupture; Cervical lacerations; Precipitated labor; Childbirth trauma; Case report.
Introduction
Spontaneous bladder rupture following normal vaginal delivery is a surgical postpartum emergency. Previous cesarean section, vacuum/forceps-assisted vaginal deliveries, and distended bladder compressed by engaged head in birth canal are all risk factors for bladder injuries in healthy parturient women 1. Cases of bladder rupture, accompanied by uterine rupture, have been rarely reported following vaginal birth after cesarean section 2. To the best of our knowledge, however, no cases of combined cervical laceration and bladder rupture have been reported to date. We present the first case of spontaneous bladder rupture with cervical laceration after a precipitated vaginal delivery.
Case Presentation
A 31-year-old, G2P1L0D1, woman with gestational diabetes, was admitted to our maternity ward at 38 weeks of pregnancy for elective induction of labor to terminate her pregnancy. She had a history of preterm birth and was a known case of minor thalassemia. The induction of labor began at 5:00 a.m. with oxytocin, and contractions began approximately two hours later. Table 1 depicts the progress of labor. During her labor, the patient urinated once. Finally, at 10:40 a.m., she gave birth to a baby boy weighing 3700 grams with an Apgar score of 7/9. Excessive vaginal bleeding was observed following placental expulsion. The examination revealed an extensive laceration in the vagina and cervix that was repaired by the obstetrician and midwife. The patient was catheterized and was being closely monitored. A urologist was consulted due to the oliguria and hematuria (100 cc output with gross hematuria within 5 hours of childbirth). Cystography, as recommended by the urologist, revealed the bladder rupture. The patient was prepared for a laparotomy immediately. The laparotomy was performed by a team of obstetricians and urologists. Several hematomas were discovered in the uterine body and the broad ligament that the team decided not to manipulate because it did not grow during the surgery. A bladder rupture was found at the dome of bladder that was repaired in two layers. One pack cell unit and two FFP units were transfused. A peritoneal drain was placed posterior to the bladder and the skin incision was closed in layers. The patient was observed for two weeks. The result of the ultrasound revealed the shrinking of the hematoma. The blood and renal tests were normal. The catheter was removed after 2 weeks and the patient was discharged.
Table 1: The progress of labor
Discussion
Precipitate labor is defined as the expulsion of the fetus within three hours of the start of contractions. Few studies have found that precipitated labor is harmful to both the mother and the newborn. Precipitated labor, which is most commonly associated with placental abruption and induction of labor, is a significant risk factor for maternal complications 3. Maternal morbidities reported included extensive birth canal lacerations, uterine rupture, placenta retention, the need for revision of uterine cavity, post-partum hemorrhage, and blood transfusions 3,4. The lower urinary tract's anatomic proximity to the reproductive tract predisposes it to iatrogenic injury during obstetric procedures. The bladder and lower ureter are two of the most commonly involved organs. Because the dome of the bladder is the weakest area, most bladder ruptures occur through the peritoneal cavity 5. In our case, in addition to deep vaginal tears and extensive cervical laceration, bladder rupture occurred, but the diagnosis was delayed by a few hours. Given the nonspecific clinical features of bladder rupture, the diagnosis should be approached with caution. Oliguria and gross hematuria after a traumatic childbirth increase the likelihood of bladder rupture. In such cases, a cystogram is thought to be the best method for early detection.
In our case the patient had induced labour with oxytocin. The use of oxytocin to induce labour can result in tachy-systole and thus shorter deliveries. So in our case we believe that the power of uterine contractions and quick descent of passenger (3700 grams fetus) were the main risk factors of precipitated labour and the complications accompanied with it. A distended bladder during labor, particularly in our case, where the fetus descended quickly, could also be a factor in bladder rupture. Although the patient urinated normally during labor, it was critical to ensure that the bladder was empty, especially during the active phase of labor, to avoid bladder damage.
CONCLUSIONS
Bladder and cervical rupture should be considered, after precipitated vaginal delivery. When there is gross hematuria, a urinary catheter should be inserted to monitor the hematuria and urine output. If the hematuria persists and other associated symptoms appear, cystography is a useful tool for determining the severity of the bladder injury and determining the cause.
Funding
This study received no specific funding from public, commercial, or not-for-profit funding agencies.
Conflict of Interest
Authors had no conflicts of interest to declare.
Patient consent
Obtained.
For more details: https://ijcimr.org/editorial-board/
#Bladder rupture#Cervical lacerations#Precipitated labor#Childbirth trauma#Case report#postpartum#oxytocin#vacuum#laparotomy#Cystography#hemorrhage#Dr Fatemeh Darsareh#ijcimr
0 notes
Text
surgical suppliers in Bangalore
"Protectcare vision to enhance the surgical suppliers standard of quality, hygiene and infection control in surgical environments by providing high quality disposable surgical care products.
Manufacturer , Exporter Of Disposable Surgical Gown, Disposable Drapes, Surgical Drapes, Adhesive Drapes, Isolation Gown, Patient Gown, reusable patient gowns, breathable fabric, Disposable HIV Kit, Personal Protective Equipment, personal protection equipment, Surgical Kit, surgery packs, angiography kit, Surgery Drape Pack, Total Knee Replacement Pack (TKR Pack), Total Hip Replacement Pack (THR Pack), cabg pack, Knee Arthroscopy Kit, Gynecology Pack, CESAREAN KIT, General Surgery Laparotomy Kit, Laparoscopy Pack, Mayo Trolley Cover, Universal Pack, Pediatric CABG Pack, Camera Cover (Camera Tube Cover), Microscope cover (Microscope Drape), c arm cover, back table cover, instrument covers, Sterile Dressing Set, Dressings & Bandages, Sterilization wrapping paper, Sterilization wrap sheet, Non Woven Shoe Cover, Face Mask, Surgical Cap, Scrub Suits, medical scrub suits, Disposable Bouffant Cap, oem services, Private Labeling Services, Training, market surveys"
0 notes
Text
A case of stoma skin and mucous membrane separation
Rectal cancer is one of the common tumor diseases in gastrointestinal surgery, with a high incidence rate, second only to gastric cancer and esophageal cancer. Surgical resection is also the main treatment method currently used in clinical practice, and its therapeutic effect is good. With the change in people's life and diet, there are more and more patients with rectal cancer combined with diabetes. The main problem is that the increase in blood sugar can hinder the healing of wounds, and incision infection and skin and mucous membrane ulcers around the stoma are prone to occur, which complicates the patient's condition. It is not conducive to its clinical recovery.
The following is a case to share, let's take a look at it with me.
Here's a challenge:
Chelsea is a retired engineer who is 64 years old this year. He had rectal cancer and diabetes mellitus. chelsea's daughter told me that she had a near-miss experience three years ago. One day three years ago, his father started without any obvious incentive. There was blood in the stool, accompanied by a small amount of fresh blood, and the number of defecation began to increase. The daughter decided to take him to the hospital for a colonoscopy examination. It was rectal cancer, and the pathology showed that it was poorly differentiated adenocarcinoma. Then underwent abdominal rectal cancer radical resection (Dixon) operation. On the 5th day after the operation, Chelsea began to have abdominal pain and yellow feces from the drainage tube. The doctor considered anastomotic leakage and performed emergency abdominal double cannula irrigation and drainage. On the 6th day, the abdominal cavity was Irrigation did not improve, and an emergency performed "exploratory laparotomy + terminal ileal loop ostomy + abdominal and pelvic irrigation and drainage", Chelsea developed septic shock after the second operation and was transferred to ICU with multiple organ failure. The Chelsea recovered gradually, the bowel function recovered, he could eat, and there was no abdominal tenderness and discomfort. The incision of Chelsea and the skin around the stoma had cracks and infection in the later stage. After that, the stoma specialist, with his help, formulated detailed nursing measures for Chelsea and provided related dressing changes, anti-infection, hypoglycemic, nutritional support, etc. After treatment and nursing, the Chelsea incision healed well, the stoma defecation was smooth, and the blood sugar was controlled smoothly.
Longterm Medical's Path to Wound Healing
Solution: Debridement and Dressing Healing
(1) Debridement period: The first step in wound care is effective debridement. In this case, the Chelsea incision is located in the middle of the abdomen, with full-thickness dehiscence, the peritoneum and intestinal tube below, and the yellow tissue at the base tightly adheres. while avoiding accidental injury to the bowel. Iodine cotton balls were used to disinfect the skin around the wound, surgical debridement was used to remove loose necrotic tissue and sutures on the wound surface, and then 0.9% saline solution cotton balls were used for cleaning. Considering a large amount of wound exudate, the Longterm Medical alginate dressing is packed after the first debridement and cleaning. It can absorb the exudate and form a gel to promote the autolytic debridement of the yellow tissue. It is stable and can effectively control infection. The outer layer is covered with Longterm Medical hydrocolloid, the abdomen is bandaged, and the dressing is changed once a day. The wound of the patient.
(2) Granulation growth phase: On the 14th day after wound treatment, the granulation tissue on the wound surface grew, and the exudate also decreased. Considering the local condition of the patient's wound, it is not suitable to perform a two-stage suture and continue to be treated with a dressing change. The size of the incision is 14 cm× 4 cm×2.5 cm, the base is 100% red tissue, the exudate is light red, the surrounding skin is normal, the wound has entered the granulation stage, the infection has been effectively controlled, the antibacterial dressing is stopped, the suture around the wound is removed, and the wound base is applied A little hydrogel dressing is then covered with alginate dressing to provide the best moist healing environment for the wound, thereby promoting the growth of granulation tissue and accelerating wound healing. The frequency of replacement is determined by the dressing's absorption and saturation of wound exudate and is replaced once every 2-3 days.
(3) Epithelial transition stage: On the 40th day, the granulation tissue grows close to the skin plane, and the skin around the wound edge migrates to the center of the wound. At this time, after the wound is disinfected, a hydrocolloid dressing is applied to the wound to promote epithelial migration, 5-7 Change once a day until the wound is completely covered by epithelium.
Wound dehiscence after abdominal surgery is one of the common postoperative complications. Wound dehiscence not only prolongs the length of hospital stay and increases the cost of hospitalization, but also causes great harm to the patient's body and mind. There are many factors of incision infection. Incision infection can also delay wound healing and easily cause systemic infection, which can even lead to death in severe cases. In this case, the patient has diabetes, the wound is dehiscent and has a severe infection, and it is not suitable for secondary suture. He can only achieve second-stage healing through dressing change. Therefore, how to provide comprehensive treatment and care, protect organs, and choose appropriate wound treatment methods To shorten the wound healing time and promote wound healing is the focus of the medical staff. The skin and mucous membrane separation of enterostomy usually occur within one week after the operation. The patient's skin and mucous membranes are not healed well, resulting in an open wound, and excrement is easy to leak out and accumulates here, which further affects wound healing and aggravates infection. In this case, the patient's stoma is located near the wound, the skin and mucous membranes are separated, it is difficult to paste the stoma bag, and the feces leak out and contaminate the wound. Therefore, how do choose a dressing reasonably and stick the ostomy bag firmly to promote wound healing, adjust the diet structure reasonably, and make the feces into strips The condition is difficult for nursing in this case.
keyword: ostomy bag
0 notes
Photo

Life in Medical College in Corporate VS Government College
#Corporate_Life
Yes.. Every medico crosses 7 mountains and 7 seas to reach this destination... Settlement to EARN..
In 2007 - When I completed my MS General Surgery, I was not in a mood to settle when around 50% of my colleagues settled in Private Medical Colleges, Corporate Hospitals, Government Hospitals. Government Hospitals had the lowest pay at that time- Just Rs.17200/ month for a Post graduate Degree holder. I decided to Join only for one Reason - to get through the TOUGHEST ENTRANCE - MCh Sge which had service quota.. Yes.. I got it.. Completed it and when i was back in 2015 with an MCH Degree...
The salary Packages: in 2015 August:
Private Medical College- Rs. 1.75 to 2.5 Lakhs/
Corporate Hospitals- Rs. 2.5 to 3.5 Lakhs/
Government sector- Rs. 65000-75000/
Some of my friends joined in Corporate, Private medical colleges.. But I decided to go with Government Sector and joined back in medical college in my native..
Now it's 2020:
Pros and Cons of Corporate and Government Job I have sketched out in past 5 years comparing myself with my friends and colleagues.. This write up is made, which may help people planning to settle.
Let me start with positive thing:
#Government_settlement
Government Sector in Medical College
:1. Yes, You are the king here, Whatever surgery you want to do you are allowed. Hands on Training is enormous, and if there is someone who could teach you well as as senior- You are Settled.
2. SALARY will be credited on 31st of every month.. Whether Corona or Tsunami happens.. 200% Guarantee is there on your Salary
3. Unless you want to move out of the JOB- No one will push you out, unless you get promotion and move to some other place.
4. If you are a kind of a person speaking all times about ETHICS, HUMANITY, PATIENT CARE- undoubtedly, here is the place.. Your morality will never change unless you become crooked minded to shift the patients out to your private hospital.At the same time- IF YOU WANT TO SEE HELL IN LIVE- YOU WILL SEE ONCE YOU JOIN A DISTRICT OR TALUK HEAD QUARTERS GH- Every day you will curse yourself - you can't do the Job related to your qualification. For example if you are MS surgeon- You will do more Postmortems than Surgeries, See more Myalgia OP more than Hernia OP, and you will end up doing Episiotomy sutures rather than laparotomy sutures.." Right from my college days, I always had difficulties to work under someone, whenever I had to work under someone, I will build my own organisation.. My character has never suited me to Bend and that is one reason for me to Stand where I am and I am Happy to be a Banyan Tree and die than to Bend like a Bamboo tree and Survive.."If you are such a person- You can stop reading further and go start your OWN JOB...
#Corporate_Settlement:
#PROS
:
SALARY PACK- attractive
FIXED Time slot
HUGE RESPECT from outside** ( ** Relatives and Public)
#CONS ( Based on the experiences from my Friends only)
1. Productivity- If they pay you 3 lakhs, they expect you to give an income in ways of investigations, Procedures etc atleast 15 lakhs.. If not the AUDIT team will start scratch, Rub, Lacerate you daily.. The moment you see a patient, the diagnosis, prognosis everything
will be known to you- but you try to full fill the BUDGET Fixed on you.. WITHOUT YOUR KNOWLEDGE
2. Replacement- You will be a Top Class Laparoscopic surgeon. Your Pay may be Rs. 3 Lakhs... but there will be one man always there to replace you- by Less payment, or Because he is a Robotic Surgeon etc.. Your Life shatters the moment you are being replaced by a JUNIOR to you, and you be willing to continue at a lesser pay in same Corporate ( as the vacancy in corporate is falling down)- APART WHEN YOU GO AND APPROACH FOR A JOB TO A CORPORATE THEY TREAT YOU LIKE A PIG..
3. Most Corporates will be ensuring- YOUR NAME NEVER BUILDS UP and only the hospital name and Company builds up. You are not allowed to practice outside.So your name fades gradually, and one day the same corporate who begged you to join their hospital/ organisation for the BRAND you had will brand you as non productive and will fire you.
4. SIGNING any agreement to join Corporate is the worst TRAP- Some corporated gets a bond that you wont practice in that city forever even if you quit the JOB...
BEWARE THIS IS THE BIGGEST TRAP TO KILL YOUR PROFESSION AND PEACE..
I will speak about the traps in agreement and how I made to travel to DELHI HIGH COURT in future...I request seniors, and practising people to post your comments, so that this will reach the young hearts to plan accordingly...
Dr. Rajamahendran.R MS, MRCS, MCh
Assisitant Professor- Government set up
Director- RRM Gastro superspeciality clinic
Founder, Director Koncpt
#NEXT/EXIT
#NEET_PG
#NEET_SS
1 note
·
View note
Text
Lupine Publishers |A Novel Approach to Multi-Trauma Patients with Bleeding Pelvic Fractur

Lupine Publishers | Orthopedics and Sports Medicine
Introduction
Bleeding from pelvic fracture, especially in patients with multiple trauma injuries, is a difficult problem facing the general practitioner working at Emergency Room (ER). Orthopedist, general surgeon, neurosurgeon, urologist and interventional radiologist are the main consultants taking care of these kind of patients. Recently, there have been many changes in practice to predict and limit hemorrhage in the patient with a pelvic fracture, and multidisciplinary approach has improved the outcome and overall survival [1]. Institutional guidelines or trauma protocols should be well-established especially in advanced trauma centers.
The first thing to do in these patients is to understand if the case is hemodynamically stable or unstable [2]. Multiple intravenous (iv) accesses should be ready in use and Foley catheter should be inserted in the monitorized patient. In hemodynamically stable patients, simple orthopedic fractures and any possible accompanying intracranial pathology can be excluded by using computerized tomography (CT) scans from cranium to the pelvis and X-rays of all suspected extremities. Then, the ER team can emphasize particularly on the pelvic fracture. The ongoing bleeding should be further interrogated. Furthermore, the accompanying intraabdominal and/or retroperitoneal pathology should also be evaluated in detail. FAST (focused assessment with sonography in trauma) can be a useful tool in the evaluation of precordial and abdominal cavities [3]. However, its dependence on the personal experience seems to be a major disadvantage in comparison with more detailed CT interpretations. Hemodynamically unstable patients with suspected intraabdominal bleeding should undergo emergent exploration.
Pelvic stabilization has been attempted for years to control bleeding by decreasing the pelvic volume and supplying tamponade effect [4]. Initially used pneumatic antishock garments have largely fallen out of favor as they lead to compartment syndrome, and they are bulky, difficult to apply and interfere with physical examination. In case of unstable pelvic injuries, the initial application of external pelvic fixation and pelvic C-clamp can be tried in an attempt to control hemorrhage associated with pelvic fracture [5]. However, an emergent pelvic angiography and embolization should be planned after nonpelvic sources of blood loss have been ruled out. A CT finding of arterial iv contrast extravasation in the pelvis is another indication for pelvic angiography and embolization regardless of the hemodynamic status. However, it only controls arterial bleeding and indicated in only up to 10 % of cases with the pelvic instability.
The exclusion of intraabdominal bleeding is vital in patients with pelvic fracture. FAST and abdominal CT are the best tools here, and replaced the historically used diagnostic peritoneal tap or lavage which are known with their high false negative or positive rates [6]. As the indications for explorative laparotomy in cases with pelvic fracture are the same for all trauma patients, the concomitant bleeding from pelvis and abdomen should be differentiated, and each should be treated. If abdominal exploration reveals a specific organ injury, repair can be tried in case of stabilization of the vitals intraoperatively. However, intraabdominal or retroperitoneal packing is currently accepted as the golden standand approach in unstable multiple trauma patients with ongoing abdominal bleeding where the major vessels are severely injured [7]. This procedure saves time till the patient gains hemodynamic stability and the physician decide what to do the next. Therefore, the procedure is also called as ‘damage control surgery’ [7,8]. In case of presacral bleeding accompanying multiple pelvic fractures, packing of the pelvic cavity can be life-saving. Pelvic packing can also be used in unstable patients without intraabdominal pathologies [9]. In these cases, exploration starts with a midline incision from umbilicus toward the pelvis, and bladder is retracted away from the fracture and three to five laparotomy pads are soaked into the retroperitoneal space on each side (toward the iliac vessels). Packing in combination with external mechanical fixation of the pelvis is reported to be successful as well. The second-look surgery can be planned in first to third postoperative days, and the laparotomy pads are removed carefully.
To know more about our Orthopedics and Sports Medicine click on https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
To know more about Lupine Publishers click on https://lupinepublishers.us/
To know more about Open access publishers click on Lupine Publishers
1 note
·
View note
Photo
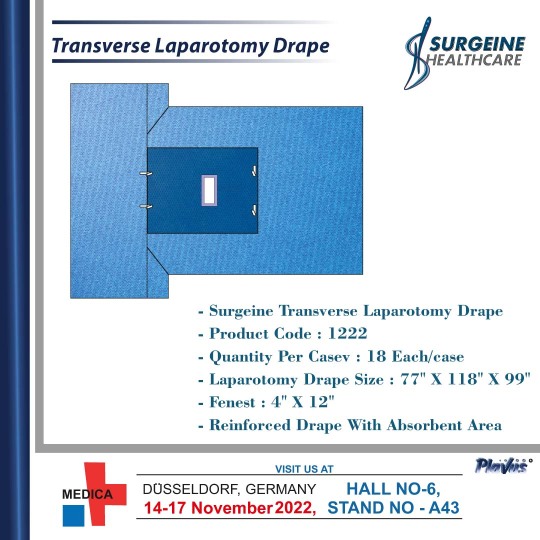
Transverse Laparotomy Drape, Sterile with Arm Board Covers. Surgeine Healthcare provides a complete selection of surgical drapes and ancillary products that offer patients and clinicians the protection they want and need. these drapes are manufactured with high-quality fabric which is tear-free, comfortable and easy-to-use in the operating room. we are committed to delivering excellent quality to our customers.
0 notes
Text
“Saanvi Roe”, 35 (India 2022)
Amniotic fluid embolism is a well-documented complication of second and third trimester abortion. Although exceedingly rare, it can also happen during birth. But AFE is almost unheard of in the first trimester—except as a complication of early abortion.
In 2022, a 35-year-old was killed by an elective abortion in India. She died of AFE even though she was in the first trimester. Her case is documented with no pseudonym, so I am calling her “Saanvi Roe”.
“Saanvi” was 35 and pregnant with her third baby when she went in for a legal 6-week abortion and a tubal ligation. She didn’t know that she was going to die.
Saanvi was given fentanyl, midazolam and propofol during the abortion and tubal ligation. About one hour after the abortion was started, she had difficulty breathing. Even though she was put on oxygen, she deteriorated and developed hypotension, tachycardia and tachypnoea. Her abdomen was distended and she was taken to the ICU.
While she was in the ICU, Saanvi’s condition only got worse. She was put on a ventilator and given blood transfusions. During her last day alive, she was given plasma and 13 units of packed red blood cells. A laparotomy found found ascitic fluid, bowels with petechia, and oozing wounds. However, the sites of her tubal ligation were not bleeding.
Less than 24 hours after the abortion, Saanvi died in the ICU. Her relatives were left to mourn the loss of two family members.
https://www.nih.unboundmedicine.com/medline/citation/35651466/Amniotic_Fluid_Embolism_After_First-Trimester_Abortion.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9135588/pdf/cureus-0014-00000024490.pdf
#unidentified victim#unsafe yet legal#tw abortion#pro life#tw murder#tw ab*rtion#abortion#abortion debate#death from legal abortion
4 notes
·
View notes
Text
After a super healthy, picture perfect pregnancy, Derek falls asleep after giving birth to a darling baby girl...and never wakes up.
Well, almost.
In the late hours of the night his daughter is born, Stiles wakes up to Derek ashen white and cold.
He calls Deaton and awakens his own magic trying to keep Derek alive.
But his magic doesn't come bursting through the surface, it comes in trickles and works just enough to keep Derek in the land of the living until help came.
Melissa arrives with John, followed by Scott and then Deaton. Together, the three medical professionals of the four help stop the unconscious wolf’s undetected internal bleeding. John informs the pack. And Stiles-
Stiles sits by Derek’s side holding his hand while a nurse and two veterinarians perform an impromptu exploratory laparotomy on their bed.
It’s a mess, literally. There’s blood, so much blood, and Derek’s hand remains persistently, hauntingly cold, his pulse weak.
Stiles has never felt so useless in his life, watching on the sidelines as Melissa, Scott, and Deaton work to keep Derek alive. Even his dad has more use, having the become the errand boy of the operation, getting this and that.
All Stiles does is hold onto Derek, anchoring his mate to the here and now. And believing, he wills Derek alive, wills his spark alive. Though he has no guarantee if it’s working or not.
After. After Derek's stabilized and Stiles is reassured their baby is healthy (he had to make sure after what happened to Derek), Stiles decides to hone his magical abilities so he can be the one to save and protect his mate and child from whatever harm came their way.
He still has the nightmares, of course. Most nights, he'd wake up screaming, turning to his side to check that Derek's still breathing. Sometimes, when it's really bad, he'd wake up Derek just to make sure he's no longer dreaming.
#sterek#Derek Hale#Stiles Stilinski#spark!stiles#Stiles is magic#Pregnant!Derek#male pregnancy#blood#gore#happy ending#i'm not a monster#hello#Hurt!Derek#Melissa McCall#john stilinski#Scott McCall#alan deaton#drabble
26 notes
·
View notes
Text
Honey in the Management of Infections
NICHOLAS NAMIAS
ABSTRACT
Background: Honey, a natural product of bees of the genera Apis and Meliponinae, has been recognized for medicinal properties since antiquity. Honey has demonstrated antimicrobial properties. These effects are variably ascribed to the pH, hydrogen peroxide content, osmotic effect, and as yet unidentified compounds putatively described as inhibines.
Materials and Methods
: This review will explore the use of honey in necrotizing soft tis- sue infections, postsurgical wound infections, wounds other than postsurgical infections,
Hel- icobacter pylori
of the stomach and duodenum, and burns. Throughout, the
in vitro
evidence that exists and the explanations that can be offered for the purported benefits of honey will be reviewed. Most of the reports are either uncontrolled case series or
in vitro
observations. As such, detailed critique of statistical methods will not be undertaken.
Conclusion: The purpose of this paper is not to debunk honey therapy as a myth, but to stimulate thought among surgeons interested in surgical infection and perhaps serve as the nidus for future research. The use of honey should be considered when more conventional therapies have failed.
And your Lord revealed to the bee: Make hives in the mountains and in the trees and in what they build. Then eat of all the fruits and walk in the ways of your Lord submissively. There comes forth from their bellies a beverage of many colors, in which there is healing for mankind. Verily in this is a sign for those who give thought.
—The Koran, Surah Al-Nahal, verse 68 & 69
H
ONEY HAS BEEN RECOGNIZED for medicinal properties since antiquity. It is mentioned
for healing purposes in the Bible, the Koran, and the Torah. It is mentioned in the Edwin
Smith Papyrus dating from the 17th century B.C., and is again referred to by Hippocrates and Democritus in ancient Greece, Galen in an- cient Rome, and Avicenna in medieval times. In the past century there have been sporadic re- ports of its use in the treatment of various wounds and infections, which will be reviewed here.
HONEY AS A SUBSTANCE
Honey is a natural product of bees of the gen- era Apis and Meliponinae. The bees collect nec- tar from flowering vegetation. The nectar is
De Witt Daughtry Family Department of Surgery, University of Miami School of Medicine, Miami, Florida.
219
subjected to enzymatic processing in vivo in both the collecting bee and in a processing bee inside the hive. The processing bee then de- posits the nectar into a wax cell in the hive, where due to relative warmth and fanning by bees, the water content is reduced by evapora- tion to 17%. The sugars in the nectar are con- verted enzymatically into glucose and fructose. Glucose oxidase then converts the glucose into gluconic acid and hydrogen peroxide. The an- timicrobial effects of honey are variably as- cribed to the pH, the hydrogen peroxide con- tent, the osmotic effect, and as yet unidentified compounds putatively described as inhibines. Various researchers have neutralized the hy- drogen peroxide with catalase in vitro in order to exclude the activity of hydrogen peroxide, with varying results. For the bee’s purposes, the antimicrobial effect is very useful; honey can feed a hive through a long winter, and like- wise, has a shelf life of many years for human consumption. Commercial processing involves heating of the honey to inactivate enzymes that may facilitate crystallization of the honey, making it less attractive commercially. Honey can be purchased commercially in both un- processed and processed states.
The use of honey as an anti-infective agent
was limited until recently to wounds, includ- ing burns, pressure ulcers, other ulcers of the skin, and traumatic or surgical wounds [1–4]. With the recognition in recent years that pep- tic ulcer disease is in large part an infectious disease (Helicobacter pylori), there has been at- tention to the use of honey in its eradication [5–10], as application to the gastric and duo- denal mucosa would be both simple and pleas- ant for the patient. This review will explore the use of honey in necrotizing soft tissue infec- tions, post-surgical wound infections, wounds other than post–surgical infections, Helicobacter pylori of the stomach and duodenum, and burns, including in vitro evidence and possible explanations for the purported benefits of honey. Most of the reports are either uncon- trolled case series or in vitro observations. As such, a detailed critique of statistical methods will not be undertaken. The purpose of this pa- per is not to debunk honey therapy as a myth, but to stimulate thought among surgeons in-
terested in surgical infection and perhaps serve as the nidus for future research.
NECROTIZING SOFT TISSUE INFECTIONS
Spencer E. Efem of the University Teaching Hospital in Calabar, Nigeria, has published a series of papers on the antimicrobial and wound healing effects of honey. He first pub- lished a series of 59 patients with wounds and nonhealing ulcers, 80% of which had failed to heal with conventional therapy for periods of one month to two years [11]. He showed that wounds which initially cultured positive for a variety of organisms were sterile at one week, and that 58 of the wounds went on to heal rapidly, with separation of eschar, diminished edema, and rapid reepithelialization. His method was to apply 15–30 mL of unprocessed honey to the wound daily, after cleaning the wound with normal saline. One ulcer was due to a mycobacterial infection and did not re- spond to honey. Although Efem did not pro- vide data to support the following impressions, he described the effects of honey to be “de- bridement of wounds by a chemical or enzy- matic action; absorption of oedema fluids around wounds; inactivation of bacteria; de- odorization of offensive wounds; promotion of granulation tissue formation and epithelializa- tion; and improvement of nutrition.” Efem noted the low pH (3.6) and hygroscopic (os- motic) effects of honey and their probable role in its antibacterial effect, but he also noted the effect of inhibine, a previously described ther- molabile bactericidal substance. As mentioned earlier, hydrogen peroxide is produced by the action of glucose oxidase, and Efem considered the “inhibine” to be hydrogen peroxide, al- though there is not universal agreement on this [12,13]. In 1993, Efem published his experience with twenty consecutive cases of Fournier’s gangrene managed with systemic antibiotics (amoxicillin/clavulanic acid and metronida- zole) and topical unprocessed honey [14]. He compared these patients to 21 similar cases managed by other physicians in the same insti- tution, in which the standard approach of sur-
gical debridement and systemic antibiotics was used. The patients treated with honey had their wounds cleaned with saline upon pre- sentation, then dressed with topical un- processed honey or packed with gauze soaked in honey, with the wounds inspected and the honey reapplied daily after cleansing with nor- mal saline. At seven days after the start of treat- ment all wounds were swabbed and found to be sterile, after having grown the usual ex- pected mix of organisms recovered by a surface swab upon initial presentation. Although not analyzed statistically, there were more opera- tions and re-operations required in the ortho- dox group, although the length of stay was shorter, on average, by 0.5 weeks in this group (Table 1). In the group treated with honey, foul odor, edema, and discharge resolved within 1 week of the commencement of therapy, and all necrotic tissues had separated. Efem con- cluded that honey is superior to standard ther- apy and that it may revolutionize the treatment of this disease. Later reports from other authors show that some have indeed adopted honey as an adjunct in the treatment of Fournier’s gan- grene. Hejase et al. reported on a series of 38 patients with Fournier’s gangrene, all of whom had surgical debridement and systemic antibi- otics followed by topical application of un- processed honey on gauze pads three times a day, with one death in the series. They provided neither data for the effects of honey nor con- trols in their series, but presented the cases as a series. They credited honey with local cleans- ing and improved healing of the wounds [15].
INFECTED SURGICAL WOUNDS
Support for the use of honey in the treatment of infected surgical wounds is anecdotal, but interesting nonetheless. In both reported series (two patients and nine patients, respectively), honey was used as a salvage maneuver, and therefore there were no controls.
Armon [16] reported on the use of locally produced honey for the treatment of infected wounds at his center in Tanzania. The first was a 20-cm sacral pressure ulcer to the level of bone. The treatment described was application of a “thin layer” of “pure honey” three times a day, followed by a dry dressing. Armon stated that the wound was suitable for surgical clo- sure by day 9, but other complications pre- cluded surgery and the wound went on to heal nonoperatively in 70 days. The second was an infected laparotomy wound after hysterec- tomy, with pus emanating from the wound and the vagina. The patient had been referred to him for lack of response to partial opening of the wound and several courses of antibiotics. In addition to removing the surgical sutures to allow for drainage, he treated the wound with honey and reported that the wound was gran- ulating by the tenth day and healed by the four- teenth day, without the use of any antibiotics. It is not clear what portion of the good outcome was due to the application of honey, and what part was due to the application of the basic sur- gical technique of adequate drainage.
Vardi et al. reported on a series of nine in-
fants with infected surgical wounds treated
TABLE 1. HONEY VS. ORTHODOX THERAPY OF FOURNIER’S GANGRENE, AFTER EFEM [14]
No. of Length of
patients No. of operations No. of re-operations stay Deaths
Orthodox treatment 21 21 19 delayed 4.0 weeks 3
primary closure, 2 flap
reconstruction of scrotum
Honey treatment 20 1 (delayed 0 4.5 weeks 0
primary closure)
with honey [17]. This series developed from one patient in whom honey was used as a sal- vage therapy for a sternal wound infection with Pseudomonas aeruginosa and mediastinitis with Staphylococcus aureus. After this patient did well, they created a standard protocol wherein if a patient had failed conventional treatment of 14 days of intravenous antibiotics and wound cleansing with chlorhexidine solution and fusidic acid ointment, honey therapy was begun. Unprocessed, non-pasteurized, non-ir- radiated, commercial honey was applied twice daily after cleaning the wound with normal saline. Six of the patients had systemic antibi- otics discontinued at the commencement of honey therapy; three continued to receive sys- temic antibiotics. All wounds were closed by day 21 of the twice-daily application of fresh unprocessed honey. The authors commented on the theoretical risk of introduction of spores of Clostridium botulinum and resulting infection. They pointed out that this is a risk known only for the ingestion of non-pasteurized honey by neonates due to the relatively non-acidic milieu of their stomachs, but that no case of clostridial infection of a wound from honey has ever been reported. Although this case series is promis- ing, the lack of appropriate controls makes it impossible to determine if the good outcomes were the result of the benefits of honey, the detriments of standard therapy, or just good fortune.
HELICOBACTER PYLORI
Ali et al. reported in 1991 that natural honey had an inhibitory effect on Helicobacter pylori in vitro, at solutions of both 10% and 20% honey,
and proposed that clinical studies on the treat- ment of H. pylori infection be undertaken [5]. Al Somal et al. performed in vitro experiments to determine what concentrations of honey would be inhibitory for H. pylori, what the ac- tive component of the honey is, and whether it was merely an osmotic effect that inhibits H. pylori. They found that Manuka honey from New Zealand, at concentrations as low as 5% v/v, completely inhibit the growth of H. pylori, and that 2.5% v/v partially inhibits the growth of H. pylori. The authors also found that non- Manuka honey, and an artificially prepared so- lution mimicking the physical properties of honey, had no inhibitory effect on H. pylori. The authors stated that although the active prop- erty in Manuka honey has not been identified, they know it is a hydrophilic molecule of a weight of 500 Daltons that is stable at a pH of
1. They proposed clinical trials, and the possi-
bility that an extract of the Manuka tree or Manuka honey could be used in the eradica- tion of H. pylori [6]. Although no such large- scale trial has been undertaken, McGovern et al. reported on a small series of volunteers with Helicobacter pylori infection by 14C urea breath tests, treated with Manuka honey or Manuka honey and omeprazole. After two weeks of treatment, all 12 of the patients remained pos- itive for H. pylori by 14C urea breath test. The authors concluded that, if Manuka honey is ef- fective against dyspepsia, it is not due to erad- ication of H. pylori [9].
Osato et al. revisited the topic in 1999; they compared Manuka honey to honeys obtained commercially from Texas and Iowa, and to an artificially prepared solution mimicking honey (Table 2). They found that at concentrations
.15% v/v, all honeys and the artificial solu-
TABLE 2. H. PYLORI ISOLATES INHIBITED BY VARIOUS SOLUTIONS, AFTER OSATO ET AL. [7]
% inhibited
5% v/v
10% v/v
$15% v/v
U.S. honey
33%
78%
100%
U.S. honey 1 catalase
33%
78%
100%
Manuka honey
60%
100%
100%
Manuka honey 1 catalase
60%
100%
100%
Glucose
Not reported
Not reported
100%
Fructose
Not reported
Not reported
100%
Glucose/fructose
Not reported
Not reported
100%
tion inhibited growth of all H. pylori isolates tested. Additionally, when catalase was added to the honeys concentrated .15% v/v, the hon- eys retained their ability to inhibit all H. pylori isolates; therefore, the anti–Helicobacter pylori activity was interpreted to be due to the os- motic effect, as opposed to hydrogen peroxide content. At the lowest concentration tested, 5% v/v, the Manuka honey inhibited 60% of the isolates tested, whereas the U.S. honeys inhib- ited only 33% of the Helicobacter pylori isolates tested. This difference was not statistically significant. The authors concluded that non- oxidant effects are important in bacterial killing, and that paramount among these ef- fects is the osmotic effect. They also concluded that since 15% v/v honey was needed to inhibit all Helicobacter pylori, that honey would not be a feasible treatment for Helicobacter pylori, as it would probably not be possible to maintain this concentration at the gastric mucosa [7]. In fairness, they probably should have concluded that the Manuka honey deserved further in- vestigation for its non-oxidant, non-osmotic killing property, due to the intriguing, if not statistically significant finding of differences in
H. pylori inhibition at 5% v/v concentrations.
Finally, Booth suggested in a letter to the ed- itor that if there is so much interest in the role of honey eradicating Helicobacter pylori, and He- licobacter pylori has been postulated to have a role in the pathogenesis of gastric lymphoma, that there should be interest in the use of honey as a possible cure for a form of gastric cancer [8].
BURNS
The use of alternative treatments for com- mon ailments is particularly attractive in de- veloping countries. Subrahmanyam has con- ducted a series of clinical trials on the use of honey and other alternative treatments for burn wounds in India. He compared honey to silver sulfadiazine in two randomized trials. The second trial differed from the first in that histological specimens were taken to corrobo- rate clinical impressions. In the first trial, 104 patients with superficial burns , 40% total body surface area were randomized in two
groups, to receive topical therapy with either silver sulfadiazine or unprocessed honey. The wounds treated with honey had earlier eradi- cation of bacteria and shorter time to closure, with 45 of the 52 patients achieving wound clo- sure by the fifteenth day as opposed to only five of the silver sulfadiazine-treated patients achieving wound closure by the fifteenth day [18]. Subrahmanyam revisited this subject in 1998, this time also obtaining histological spec- imens [19]. In addition to reporting the subjec- tive benefits in the honey-treated burns, he also reported that 100% of the honey-treated wounds were closed by day 21 as opposed to only 84% of the conventionally treated burns (p , 0.001). The histological specimens essen- tially corroborated his clinical findings in terms of the presence of granulation, inflam- mation, and epithelialization. Additionally, in the silver sulfadiazine-treated group, four pa- tients whose burns were assessed initially as superficial and not in need of operation, con- verted to full thickness and required excision and grafting. Subrahmanyam interpreted this as a bacteriological failure of silver sulfadi- azine. He did not consider the possibility of a failure of randomization. In other papers, Subrahmanyam compared honey to potato peels [20], amniotic membranes [21], and Op- Site® polyurethane film [22]; honey was su- perior in each study. However, honey is not always the answer. Subrahmanyam found in his most recent study that early excision and grafting, the modern standard of care, was su- perior to honey in the treatment of burns [23]. He performed a prospective, randomized trial with 25 patients in each arm, randomized to early excision and grafting or expectant man- agement with topical unprocessed honey ap- plied on alternate days, with delayed grafting after the separation of slough. The only ad- vantage seen in the honey group was that they required less blood transfusion (21% of blood volume vs. 35% of blood volume). There were three deaths, all from sepsis, in the honey group versus one death, from status asthmaticus, in the excision group. Ninety- two percent of the excision patients had a good functional and cosmetic outcome, whereas only 55% of the honey-treated group had a good outcome.
EVIDENCE FOR THE ANTIMICROBIAL PROPERTIES OF HONEY
The text of this section is summarized in Table 3. In 1984 Obaseiki-Ebor and Afonya, from the University of Benin in Nigeria, re- ported on the anti-candidal effects of a distil- late of honey in vitro [24,25]. They showed that 72 isolates of Candida albicans were all suscep- tible to the HY-1 fraction of honey distillate, whereas 10% of the isolates were variably re- sistant to nystatin, miconazole nitrate, or clo- trimazole. Minimal inhibitory concentrations (MIC) were determined for this compound as well as for commercial antifungals as v/v%. The MIC 90 for HY-1 was 2 v/v%, as compared to mycostatin suspension with an MIC 90 of 0.5 v/v%. They did not elaborate on the chemical nature of the distillate or on the mechanism of action. They also did not comment on the os- motic activity of the solutions, but a 2 v/v% so- lution of a distillate of honey is not likely to have as great an osmotic effect as honey.
Willix et al. of the University of Waikato in
New Zealand reported on the antibacterial ac- tivity of Manuka honey as opposed to other
honeys [26]. They stated that the antibacterial effects of honey are due in large part to hy- drogen peroxide derived from an enzymatic system intrinsic to unprocessed honeys. How- ever, they cited a systematic review of com- mercially available honeys in New Zealand by Allen et al. [27], using an assay that controlled for the osmotic effects of honey and negated the effect of hydrogen peroxide by adding cata- lase to the assay. They found that the antibac- terial effect of honey (tested against Staphylo- coccus aureus) varied widely among honeys, comparable to a range of between 2% and 58% w/v of phenol, in an almost Gaussian distrib- ution. They proposed that an unidentified fac- tor in a local honey, Manuka honey, was responsible for this effect. Descriptions of the chemical nature or proposed mechanism of ac- tion of this factor have not been published. Manuka honey is a variety of honey that comes only from New Zealand, from bees fed on the nectar of the Manuka bush, Leptospermum sco- parium. Similar antibacterial activity has also been found in honey from bees fed on the nectar of Leptospermum polygalifolium, which is found in the wilds in Australia. Willix et al.
TABLE 3. SUMMARY OF FINDINGS OF VARIOUS STUDIES ON THE ANTIMICROBIAL PROPERTIES OF HONEY
Author Principal findings
Obaseiki-Ebor 1. 72 isolates of Candida albicans were susceptible to the HY-1 fraction of honey et al. [24] distillate, whereas 10% were variably resistant to pharmacologic antifungals
2. MIC90 for HY-1 fraction 2 v/v%, MIC90 for mycostatin, 0.5 v/v%
Allen et al. [27] 1. Antibacterial effect of various honeys was comparable to phenol 2% to 58%
w/v in a Gaussian distribution.
Cooper et al. [3] 1. Non-Manuka honey at 25% w/v, with catalase, had no antibacterial effect
against Staphylococcus aureus.
2. Manuka honey at the same concentration, with catalase, had no loss of antibacterial activity.
3. Compared sugar solutions to honey
a. Lowest concentration of sugar with antibacterial activity against S. aureus is 29% v/v
b. MIC for Manuka honey 2–3 v/v%
c. MIC for non-Manuka honey 3–4 v/v%
d. Concluded that non-osmotic effect must be responsible for antibacterial effect.
Efem [28] 1. Tested honey vs. sugar solutions against clinical microbiology isolates
2. Honey effect in vitro against broad range of organisms, including fungi
3. Sugar effective only against Streptococcus pyogenes, but was not tested against anaerobes or fungi
Waldhan et al. [29] 1. Honey vs. sugar syrup against 21 bacteria and 2 fungi
2. At full strength, no difference in bacteriostatic effect, but honey more bactericidal
3.
At lesser dilutions, honey more bacteriostatic and bactericidal at all concentrations.
MIC 5 minimal inhibitory concentrations.
tested Manuka and non-Manuka honey against a variety of wound-infecting species of bacte- ria. They found that the relative sensitivities of various organisms varied between the Manuka honey and other honeys, but that overall both types of honey can completely inhibit bacter- ial growth at concentrations below 11% v/v. Manuka honey, with catalase added to neu- tralize hydrogen peroxide, could still inhibit completely the growth of Staphylococcus aureus at a concentration of 1.8% v/v. The sugar con- tent of the two honeys was the same, so they ascribed the different relative antibacterial ef- fects of the honeys to a different, unknown ac- tivity in Manuka honey. Another comparison of Manuka and non-Manuka honey was un- dertaken in 1999 [2], this time against Staphy- lococcus aureus isolates from clinical wound infections, at various dilutions and with the ad- dition of catalase to inactivate hydrogen per- oxide. The non-Manuka honey at a 25% v/v di- lution, in the presence of catalase, had no detectable antibacterial activity, whereas the Manuka honey under these conditions had no loss of antibacterial activity in the presence of catalase. The authors noted also that the low- est concentration of sugar that has antibacter- ial activity against S. aureus is 29% v/v, and that the MIC values for Manuka honey (2–3% v/v) and non-Manuka honey (3–4% v/v) are well below the concentration at which osmo- larity could be credited with the antibacterial activity.
Efem addressed the question of the osmotic
effect of honey in 1992 by testing in vitro the antibacterial effect of honey and the effect of a sugar syrup with physical properties similar to honey [28]. He used a wide variety of bacterial and fungal isolates from clinical infections (Streptococcus pyogenes, Enterococcus faecalis, Staphylococcus aureus, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, Pseudomonas spp., Pseudomonas aeruginosa, Bacteroides fragilis, Clos- tridium welchii, Clostridium tetani, Clostridium oedematiens) and incubated them on appropri- ate culture media with wells of the honey or sugar cut into the media. Zones of inhibition were measured. Honey was inhibitory against all bacteria tested except Pseudomonas aerugi- nosa and Clostridium oedematiens. The sugar syrup was ineffective against any of the bacte-
ria tested, with the exception of moderate ac- tivity against Streptococcus pyogenes (the anaer- obes were not tested against the sugar syrup). The fungi tested were all uniformly suppressed by honey at 100% concentration, but, when di- luted to 50% and 20%, the honey lost efficacy against the fungi. The fungi were not tested with sugar solution.
In 1998, Wahdan et al. compared the antimi- crobial activity of honey and a sugar syrup with the same sugar content as honey against 21 bac- teria and 2 fungi [29]. They found that there was no difference in bacteriostatic activity be- tween full-strength honey and sugar syrup, but that the honey was statistically significantly more bactericidal. At dilute concentrations, the honey was always more bactericidal and bac- teriostatic. Because of these differences when concentration was controlled for, the authors invoked some other properties of honey as at least partially responsible for its antimicrobial activity. They also point out multiple refer- ences from the apiary literature describing “in- hibines,” which are suspected to be hydrogen peroxide and phenolic acids, among which caf- feic and ferulic acids were identified in honey for the first time in their laboratory.
In conclusion, honey has been shown to be
clinically useful in various settings involving soft tissue infections and non-healing wounds, and there appear to be some properties of honey that are controlling infection other than via the strictly osmotic effect. The caveat is that all of the data are generated from small stud- ies, generally without rigorous statistical analy- sis. It is unlikely that the large studies with elaborate monitoring of protocol and profes- sional statistical analysis will ever be done, as the expense of such studies is unlikely to ever be rewarded with the proceeds of honey sales to make such research financially feasible. The applicability of in vitro studies of antibacterial effects is unknown in vivo, but the clinical evi- dence suggests that honey may be useful in certain circumstances. Its use should be con- sidered when more conventional therapies have failed. The usefulness in the management of Helicobacter pylori is less compelling, and in light of the other effective and safe treatments available, is probably not worth further inves- tigation.
REFERENCES
1. Moore OA, Smith LA, Campbell F, et al. Systematic review of the use of honey as a wound dressing. BMC Complement Altern Med 2001;1:2.
2. Cooper RA, Molan PC, Harding KG. Antibacterial ac- tivity of honey against strains of Staphylococcus aureus from infected wounds. J Royal Soc Med 1999; 92:283–285
3. Cooper R, Molan P. The use of honey as an antisep- tic in managing Pseudomonas infection. J Wound Care 1999;8:161–164.
4. Dunford C, Cooper R, Molan P. Using honey as a dressing for infected skin lesions. Nurs Times 2000;96 (14 Suppl):7–9.
5. Ali AT, Chowdhury HN, al Humayyd MS. Inhibitory effect of natual honey on Helicobacter pylori. Trop Gastroenterol 1991;12:139–143.
6. Al Somal N, Coley KE, Molan PC, et al. Susceptibil- ity of Helicobacter pylori to the antibacterial activity of Manuka honey. J R Soc Med 1994;87:9–12.
7. Osato MS, Reddy SG, Graham DY. Osmotic effect of honey on growth and viability of Helicobacter pylori. Dig Dis Sciences 1999;44:462–464.
8. Booth, RG. Gastric lymphoma. J R Soc Med 1994; 87:644.
9. McGovern DPB, Abbas SZ, Vivian G, et al. Manuka honey against Helicobacter pylori. J R Soc Med 1999; 92:439.
10. Drouin E. Helicobacter pylori: Novel therapies. Can J Gastroenterol 1999;13:581–583.
11. Efem SE. Clinical observations on the wound healing properties of honey. Br J Surg 1988;75:679–681.
12. Dold D, Du DH, Dziao ST. The antibacterial, heat- and light-sensitive inhibitory substance, inhibine, in nat- ural honey. Z Hyg Infektionskrankh 1937;121:333.
13. White JW, Mary JR, Suber H, et al. The identification of inhibine, the antibacterial factor in honey as hy- drogen peroxide and its origin in a honey glucose- oxidase system. Biochim Biophys Acta 1963;73:57–70.
14. Efem SE. Recent advances in the management of Fournier’s gangrene: preliminary observations. Surgery 1993;113:200–204.
15. Hejase MJ, Simonin JE, Bihrle R, et al. Genital Fournier’s gangrene: experience with 38 patients. Urology 1996; 47:734–739.
16. Armon PJ. The use of honey in the treatment of in- fected wounds. Trop Doct 1980;10:91.
17. Vardi A, Barzilay Z, Linder N, et al. Local application
of honey for treatment of neonatal postoperative wounds. Acta Paediatr 1998;87:429–432.
18. Subrahmanyam M. Topical application of honey in treatment of burns. Br J Surg 1991;78:497–498.
19. Subrahmanyam M. A prospective randomised clini- cal and histological study of superficial burnwound healing with honey and silver sulfadiazine. Burns 1998;24:157–161.
20. Subrahmanyam M. Honey dressing versus boiled potato peel in the treatment of burns: A prospective randomized study. Burns 1996;22:491–493.
21. Subrahmanyam M. Honey-impregnated gauze ver- sus amniotic membrane in the treatment of burns. Burns 1994;20:331–333.
22. Subrahmanyam M. Honey-impregnated gauze versus polyurethane film (OpSite) in the treatment of burns— a prospective randomised study. Br J Plast Surg 1993;46:322–323.
23. Subrahmanyam M. Early tangential excision and skin grafting of moderate burns is superior to honey dress- ing: A prospective randomised trial. Burns 1999;25: 729–731.
24. Obaseiki-Ebor EE, Afonya TC, Onyekweli AO. Pre- liminary report on the antimicrobial activity of honey distillate. J Pharm Pharmacol 1983;35:748–749.
25. Obaseiki-Ebor EE, Afonya TC. In-vitro evaluation of the anticandidiasis activity of honey distillate (HY-1) compared with that of some antimycotic agents. J Pharm Pharmacol 1984;36:283–284.
26. Willix DJ, Molan PC, Harfoot CG. A comparison of the sensitivity of wound-infecting species of bacteria to the antibacterial activity of Manuka honey and other honey. J Appl Bacteriol 1992;73:388–394.
27. Allen KL, Molan PC, Reid GM. A survey of the an- tibacterial activity of some New Zealand honeys. J Pharm Pharmacol 1991;43:817–822.
28. Efem SE, Udoh KT, Iwara CI. The antimicrobial spec- trum of honey and its clinical significance. Infection. 1992;20:227–229.
29. Wahdan HA. Causes of the antimicrobial activity of honey. Infection. 1998;26:26–31.
Address reprint requests to: Nicholas Namias, M.D., F.A.C.S. P.O. Box 016960 (D-40)
Miami, FL 33101 E-mail: [email protected]
This article has been cited by:
1. Joy Bardy, Nicholas J Slevin, Kathleen L Mais, Alexander Molassiotis. 2008. A systematic review of honey uses and its potential value within oncology care. Journal of Clinical Nursing 17:19, 2604-2623. [CrossRef]
2. Ali Ayyıldız, K. Turgay Akgül, Özden Cebeci, Barış Nuhoğlu, Muzaffer Çaydere, Hüseyin Üstün, Cankon Germiyanoğlu. 2007. Intraurethral honey application for urethral injury: an experimental study. International Urology and Nephrology 39:3, 815. [CrossRef]
3. Arne Simon, Kai Sofka, Gertrud Wiszniewsky, Gisela Blaser, Udo Bode, Gudrun Fleischhack. 2006. Wound care with antibacterial honey (Medihoney) in pediatric hematology–oncology. Supportive Care in Cancer 14:1,
91. [CrossRef]
https://cloverhoney.web.id/
https://cloverhoney.web.id/clover-honey-madu-hdi/
https://cloverhoney.web.id/propoelix/
https://cloverhoney.web.id/royal-jelly-hdi/
https://cloverhoney.web.id/clover-honey-harga/
https://cloverhoney.web.id/propoelix-harga/
https://cloverhoney.web.id/hdi-propoelix-adalah/
https://cloverhoney.web.id/manfaat-propoelix/
https://cloverhoney.web.id/madu-hdi-harga/
https://cloverhoney.web.id/propoelix-plus/
https://cloverhoney.web.id/madu-hdi-manfaatnya/
https://cloverhoney.web.id/clover-honey-manfaatnya/
0 notes
Note
WIP Guess: friends, home, laparotomy
Somehow none of my WIPs have the word laparotomy! Although only one is actually set in the hospital haha. Here are the others though!She presumes some are friends of Elinor’s, maybe some are Edward’s family and wonders if they know her, or at least of her. “It’s from my first pack of cards, I was given them by one of the staff at the children’s home."[Send me a word and I will post a sentence from a WIP]
1 note
·
View note
Text
Injury Profiles: Evisceration
Hey everyone! Welcome to a new series I’m calling Mangled Mondays.
The point of Mangled Mondays will be to give an injury profile every Monday. Not only is the alliteration fun, I know that I personally wish that I could personify Monday so that I could mangle it and then go back to bed.
(And yes, I know we’re starting this on a Friday, but that’s happening because… reasons.)
So without further ado I give you Mangled Mondays: Evisceration…

Lethality Index
4
What Is It?
Evisceration, also known as disembowelment, is any form of injury that ends with your character’s insides on the outside, with their guts hanging out. Their bowels are literally in their lap.
The abdomen is essentially a madhouse of overpacking. The intestine, or small bowel, is approximately 25 feet of tightly bunched material that is held in place by a thick membrane called the peritoneum, which lines the abdominal cavity and is folded over those densely packed organs. When the peritoneum is ruptured, the guts come out.
The interesting thing about this injury is that the intestines themselves don’t even need to rupture for this to be an absolutely devastating and likely-to-be-deadly injury. Even if the bowels are miraculously intact, the odds of getting an infection are extremely high, and your character’s life is on the line.
Meanwhile, they have a problem: they have guts in their hands and they can’t get them back in!
If this injury is the result of some kind of fight, the character will be left vulnerable to additional injury, though an attack that leaves its victim extruding sausage into the open is likely to make the attacker think the job has been done. Either way, this character is instantly out of the fight, even if they retain strength; the horror of the injury is enough to disable them as a fighter.
In reality, in the majority of cases in which any part of the abdominal contents is welcomed to the outside world, what comes out is not actually an organ, but the omentum, a great protective apron of tough, fibrous tissue and fat that protects the underlying organs. However, characters with these injuries are still in deep trouble: 8 in 10 wounds with an evisceration will include another internal injury that requires surgical repair.
Lethality
While some forms of evisceration are inherently lethal, including those with massive hemorrhage or where the entire abdominal contents are extruded and mangled or destroyed, it’s far more common for the protrusions through the abdominal wall to be fairly small, no more than a few inches.
In the former case, exsanguination (heavy blood loss) is the primary concern. In the latter, the real worry is infection.
Abdominal trauma in general is extremely prone to infection, because the gut is colonized with billions of bacteria. These are usually either neutral or beneficial to the body when they stay where they belong, but when they cross into the bloodstream, these bacteria can cause sepsis and death within days.
Clinical Signs:
Elvis has left the building.
Erm, the bowels have left the abdomen. Or at least, something has left the abdomen; most often it’s the omentum.
Protruding tissue may look gray or may be obvious loops of bowel; these look like raw sausage without the fennel.
Symptoms:
Pain
How Does It Happen?
In order for matter to exit the abdominal cavity, it needs…
…a clear exit pathway. This typically involves a slashing injury to the abdominal wall, though it’s of course possible for the injury to come from a stab wound. Exit wounds from gunshots are also known to cause eviscerations.
Immediate Treatment
Characters who aim to support a character with an evisceration have their work cut out for them.
First, they must get over their own emotions at the sight of their comrade with their “guts hanging out.” They may, in fact, need to be gutsy in how they handle the situation.
(I’m here Tuesdays and Thursdays, try the veal… or the sausage. Refunds can be requested from any reputable retailer.)
Next, bleeding must be managed as best it can be.
Characters with medical training will know that the exposed bowel must be kept wet, and so will use whatever’s handy as a wet dressing, soaking it with water (sterile for preference, distilled second, tap as a last resort) and applying it to the exposed tissue.
Afterwards, characters might use a piece of plastic, such as a plastic bag cut into a square and taped down on all sides, to protect the wound from contamination. (Given that we’re discussing a wound with the potential for perforated bowels, it may already be contaminated.)
Getting this character to a trauma surgeon is of the utmost importance, because characters simply don’t know what’s going on inside.
Definitive Treatment
Surgery / Hospitalization
Trauma teams are going to be very concerned about patients with eviscerations, and the larger and more out-spilly the wound, the more concerned they will be.
The character will be given an overall trauma evaluation in the emergency department, where they will get IVs, blood products if they need them, and the first round of antibiotics. Then it’s a short, rapid trip to the operating room.
As a side note, in the US, stab wounds must be reported to local law enforcement. Relevant clothing will be preserved as evidence, and security will likely be close by until the police arrive.
In the operating room, the character will be anesthetized, and the abdomen will be opened to explore the wound. This is known as an exploratory laparotomy. An(other) incision will be made into the abdominal wall, which will likely run 4–6 inches in length, and surgeons will then examine the underlying tissue. Things that need stitches will be stitched.
If there is potential for the large or small bowel to be nicked, the character will undergo peritoneal lavage, meaning that sterile saline will be poured into the abdomen and then drained with suction and examined. Lavage is designed not only to flush out any free feces but also to examine whether (and how much) blood and fecal matter are in the abdomen.
After the repairs are made, the abdomen will be closed, first with a layer of sutures to close the peritoneum. Then the skin will be closed with a separate layer of sutures or staples.
The character will be in surgical ICU for a few days, and there’s a distinct possibility that they’ll need to return to the OR for further surgery if the abdomen continues to bleed or infection becomes apparent.
Colostomy & Ileostomy
In some cases, especially where the small intestine or colon has been significantly damaged, the character will be given a surgical hole through which to poop (defecate). If this is in the colon it’s a colostomy, an ileostomy if it’s in the small bowel. Fecal matter will thus drain into a bag rather than be excreted through the rectum and anus.
This is especially common if the colon itself has been injured by the evisceration.
Post-Operative Care
The character will be given ice chips on the first day and likely clear fluids by the second or third day. They will also likely have a tube running from the nose to the stomach for the first two days after surgery, which is hooked up to suction; this is to drain the stomach of bodily fluids.
Characters may be eating solid food as soon as three days after the surgery.
The wound will likely have a small tube in place which will provide suction on the wound to help drain any fluid that accumulates as part of the healing process; this fluid is called serosanguinous fluid and is an orangey yellow. The drain will likely be removed after 2 days.
The dressings will be changed every four to 48 hours, especially if they soak through; earlier on, dressing changes will be more frequent.
Characters with a colostomy will be taught how to clean the stoma (opening) with warm water, and will be instructed on how feces collects into the bag.
In the Austere Environment
Outside of a hospital environment, the best that can be done is to gently push the relevant pieces of abdominal contents back into the wound, stitch the wound closed, wait, and hope. Antibiotics, if available, should be used.
This will only be realistically survivable if the character comes to Death’s door, knocks, and waits patiently while Death herself deliberates; that is, the character will almost invariably become septic, or incredibly sick with infection.
For more on this, see Part 5: Miscellaneous Trauma, entry on Sepsis.
The Rocky Road to Recovery
Capabilities Retained
Characters will be able to use all four limbs, and walking is possible beginning a few hours after surgery.
Disabilities: Temporary
As anyone who has strained a muscle doing sit-ups or yoga can tell you, a surprising number of actions involve the core muscles of the abdomen. It will take a few weeks for the abdominal muscles to heal, much less the skin, and everything from leaning over to making a bowel movement and coughing can cause pain and discomfort; ability to run, move heavy weights, etc., will take some weeks to return.
Disabilities: Permanent
Amazingly enough, intestines are quick-healing, and the muscle damage is reparable. Characters who don’t need permanent colostomies will have avoided having any significant long-term consequences, other than a wicked scar.
Features of Recovery: Hospital Stay
Discussed above.
Features of Recovery: PT/OT
There are two main focuses of physical therapy after laparotomy: walking, and core strength. The first is accomplished with assistance: first, if needed, a walker, then an assistant or a steady pole, until finally the character will simply walk as they did before, if more slowly.
Core strength is compromised by the injury to the abdominal muscles, from both the wound and the surgery, and will take some time to return. However, once the wound is no longer at risk of ripping open, strength will be rebuilt with exercises like crunches, planks, side planks, and something called a Superman, where the character lies prone (on their belly) with their arms and legs extended and raises one arm-and-opposite-leg pair at a time.
The New Normal
Other than a permanent scar on the abdomen, characters may not have any significant changes to their lifestyle after their surgical wounds heal.
Future Risks
Characters who suffer any kind of insult to the intestines are at risk of a complication known as adhesions, which are essentially large pockets of scar tissue, which typically develop years after the injury itself. Adhesions are mostly benign, but they can cause frequent constipation or even bowel obstruction as they pinch off an area of small or large intestine, and are the most common cause of such symptoms in developed nations.
In severe cases, adhesions can strangle the bowel. On the vascular side, this strangulation causes obstruction of blood flow to the bowel and can cause death of the tissue. But it can also cause the bowel to swell with feces and rupture, which can cause lethal bleeding. If the character doesn’t bleed to death, they may succumb to infection.
If these adhesions become problematic, they may need to be surgically removed – a process that can cause additional adhesions down the line.
Total Recovery Time (Typical)
Suture and wound healing: 6 weeks
Full strength: 12 weeks
Sensory
Sights
The abdomen is lined with four layers of protection for the underlying organs. The skin is what we all know it to be. The fat is a yellow layer whose thickness varies based on body type, but which may have substantial thickness and weight in heavier characters. The muscles are bright pink and will bleed, and the peritoneum is thick, white, and fibrous. (If the evisceration is small, it’s the omentum, the outer layer of the peritoneum, that will come out.)
If the bowel or intestine is pierced, the viewer will be able to see brown material ooze from the nicked sections.
Smells
In addition to the coppery stench of blood, this character will smell strongly of feces if the colon or small bowel is pierced.
Sounds
Imagine the sound of wet meat hitting concrete. That’s about what a disembowelment will sound like.
Sensations
In addition to the pain, characters who are being disemboweled may feel a sliding or falling feeling as their bowels come out.
If the bowels are stuffed back in, they’ll feel a significant amount of pressure and pain during the push.
Medslang
A laparotomy is known between colleagues as a “lappy,” with the specific procedure – exploratory laparotomy – being known as an “ex lap.”
Exploring the small or large intestine for damage and necrosis (tissue death) is known as “running the bowel.”
When attempting to put them back into place, surgeons might be said to be “playing Hide the Sausage” with the intestines. Note that this will not be said in front of the patient unless they’re under anesthesia, as it’s somewhat less than polite.
Key Points
Eviscerations are rapidly lethal when large portions of bowel are removed or damaged, as bleeding can be significant.
On the smaller end of the scale, it’s possible that only the omentum, the flap that covers and protects the intestines, protrudes through the skin.
The risk of infection is great if the wound is not properly managed. (See the entry on Sepsis.)
Eviscerated bowel must be kept moist to prevent additional damage.
xoxo, Aunt Scripty
[disclaimer]
This post is an excerpt from Blood on the Page Volume One: A Writer’s Compendium of Injuries. The book details thirty-one injuries with which to maim, mangle, and maul your characters, as well as nine indispensable articles of Wound Wisdom covering everything from burn stages to suture selection.
Signed print and digital editions of the book are available for preorder [on IndieGoGo] through 10/15. Unsigned digital editions are available on [Amazon] and [everywhere else].
The book will be out 10/23, just in time for NaNoWriMo!
Injury Profiles: Evisceration was originally published on ScriptMedicBlog.com
#abdominal trauma#Blood on the Page#evisceration#homicide#injury profiles#mangled mondays#penetrating trauma#masterposts#crossposts
350 notes
·
View notes
Text
Juniper Publishers| Surgical Repair of Inguinal Direct Hernia without Cremaster Resection
Journal of Surgery
-
JuniperPublishers
Abstract
Preservation of the cremaster muscle during the surgical repair of the direct inguinal hernia. keeping the funtion of the cremaster.
Cremaster muscle:The cremaster muscle is all around of the inguinal cord, the main funtion is elevation of the testis also is protecting the elements of the inguinal cord.
Concept:The direct inguinal hernia is locate at the triangule of Hesselbach of the inguinal region,this triangule components are the inguinal ligament of Poupart. The epigastric blood vessels pack close to the deep inguinal ring and the external border of the rectal muscle.That is the Hesselbach triangule and the main component of the wall in this triangule is the transversalis fascia. For that reason is the most weak point of the abdominal wall. History-Inguinal hernia repair has made enormous progress throughout the ages. Surgical techniques have rapidly evolved since Eduardo Bassini proposed his first procedure. When analyzing original articles since the sixteenth century, it becomes apparent that all surgical techniques for repair of the inguinal hernial orifice can be traced back to two simple repair principles. The first is reinforcement of the anterior wall of the inguinal canal and tightening of the external inguinal ring (Stromayr 1559, Purmann 1694, Czerny 1877) and the second is reinforcement of the posterior wall of the inguinal canal and the tightening of the internal inguinal ring, either externally (Lucas-Championnière 1881, Bassini 1889, Lotheissen 1898, McVay 1942, Shouldice 1945, Lichtenstein 1987, Stoppa 1989) or via an intraabdominal approach by laparotomy (Tait 1891) or laparoscopically (Ger 1990, Velez and Klein 1990). We have tried to provide a systematic order to the diverse procedures of surgery of inguinal hernias according to their repair principles. We also point out their historical development.
Indications: Any palpable mass,painful,that increase with any physical effort or Valsalva maniouver mean that the patient has an inguinal hernia,can be direct when is coming from the Hesselbach triangule or indirect whem arise into the inguinal canal,both need to have a surgical procedure to repair the defect.
Procedure: The most common procedures to repair the direct hernia are the Zimmerman and Mc Vay, but most of the surgeons actually prefer just to close the posterior wall (fascia transversalis) repairing the Hesselbach triangule.can be manually using non absorbible suture open surgery with a small incision or laparoscopic procedure, how the laparoscopic procedure dont perform disection of the cremaster muscle, we start to perform the open procedure the same way,and this approach was who show,that doing this kind of closing of the posterior wall we can preserve the funtion of the cremaster muscle. Ralph Ger described the first potential laparoscopic inguinal hernia repair in 1982. He describes a metallic clip applying device to close the hernia sac during laparotomy for other operations.
Go to
Introduction
He eventually describes one case of laparoscopic inguinal henria repair in a similar fashion with metallic lips only [1-5]. His approach was applicabe to hernia sacs with defects less than 1.25 cm. He did not describe reconstructing the inguinal floor and his approach was not applicable for direct inguinal hernias. The first total extraperitoneal approach (TEP) to inguinal hernia repair was first described by McKernon and Laws in 1993. As with the transabdominal approach (TAPP), the principles touted by Rives and Stoppa for open preperitoneal repair of a large mesh providing coverage over all defects, distributing intra-abdominal pressure over the large mesh area, and requiring minimal fixation, were primary principles of the laparoscopic approach to inguinal hernia repair. The indications for laparoscopic inguinal hernia repair, TAPP or TEP, are the same for open inguinal hernia repair. They may be ideal for bilateral inguinal hernias and recurrences from anterior approaches, but is also appropriate with unilateral primary hernias when the surgeon is comfortable with the technique. For young, active males with primary hernias, it may ofter decreased pain and an earlier return to activity. Prior lower abdominal surgery or pelvic radiation are strong relative contraindications, as these may make access to the preperitoneal space difficult.
Go to
Conclusion
We would like to mention that the open procedure with preservation of cremaster muscle had been the same results that the laparoscopic procedure, also in good hands is very fast procedure and less expensive ,because the surgeon dont need any special tools like the laparoscopic approach. The recovery time was the same,and the patient can go home the same day, also can be perform just with sedation and local anesthesic.
To read more articles in
Journal of Surgery
Please Click on:
https://juniperpublishers.com/oajs/index.php
For More
Open Access Journals
in
Juniper Publishers
Click on:
https://juniperpublishers.com/journals.php
juniper publishers Linkedin
0 notes
Text
The Rest of Our Lives
Hello everyone! I found the inspiration for this prompt while searching around Tumblr this morning. The prompt includes the following statement: “I want to love you the rest of my life. Why won’t you let me.” I thought that this perfectly describes Omelia’s situation right now. I really believe that they are still in love with each other, but one of them is hesitant to say it. This prompt includes moments from 14x07 and then becomes an AU of sort. I hope you all enjoy it :)
It’s been over two weeks since we exchanged our rings back but I can’t help feeling that it was a mistake. Sure our situation is complicated, but I’m sure that we can fix it. It’s not about how to fix it, it’s more of a should we fix it situation.
Work becomes a little more complicated as we don’t know how to act around each other. It wasn’t nearly this awkward before our separation. Consults and surgery are two different things. Consults become more tense and awkward than ever before. Especially the one afternoon there was a mass casualty at a local fair. Amelia and I ended up working on the same case, which included a middle aged man with both abdominal and head injuries. Interestingly enough we have been working on more cases together ever since we decided to separate. I have a gut feeling that this case will be different however.
I begin an abdominal ultrasound while Amelia is performing a routine neurological exam. After a moment, she informs me that he has all function and movement. “Okay, let’s get him up to the OR then,” I announce to the interns around me. “Wait! I want a head CT,” Amelia interjects suddenly. “Amelia, there is no indication that he needs one, and you cleared him. Why do you think he needs one?” I question. “I have a feeling that there is something wrong.” Amelia responds to Owen’s question. “We don’t have time to run a head CT Amelia, he needs to go to surgery now.” Owen responds with slight annoyance. “Fine, have it your way Owen. Don’t page me when he suddenly starts to code.” Amelia replies while meeting Owen’s eyes with a deadly glare.
Going against Amelia’s pleas, Owen rushed their patient for an emergency laparotomy foregoing her request for a head CT.
“Dr. Shepherd?” An intern questioned while making her way over to the nurses station where Amelia was standing. “Yes? How’s our guy?” Amelia replied while looking at the intern. “Um, his wife is here with their kids and I-I don’t know what to tell them.” The intern stated nervously. “Uh, well, was the head CT clear?” Amelia replied. “Uh, um,” The intern quickly replied back. “Um what?” Amelia questioned confusedly.
Moments later, the door to OR 3 burst open to reveal an angry Amelia with an intern closely following behind. “You skipped his CT?” Amelia questioned Owen with growing anger. “He was bleeding out,” Owen replied without looking up from his patient currently on the operating table. “If you were going to skip a CT, you should have paged me.” Amelia said while countering Owen’s reply. “I made a call, Amelia, and it was the right call. His liver was actively bleeding. I threw his spleen into the trash and he’s still--” Owen began to reply to Amelia’s statement when he was interrupted by the intern across the table from, “Dr. Hunt,” The intern interjected sheepishly. “What?” Owen replied quickly. “She’s gone,” The intern said while focusing back to the task at hand.
About 15 minutes later Amelia appeared yet again into OR 3, this time with a different mission. “Dr. Hunt,” Amelia said while entering the operating room. “Yes Nurse Linda?” Owen replied to Amelia not knowing that she was the one that called his name. “Amelia? What the hell?” Owen said as Amelia approaches him with a protective vest in her hands. “Put this on. You’ll need it to protect you from the radiation,” Amelia replied to a confused Owen. “What radiation?” Owen questioned Amelia still confused about the present situation unfolding. “Skipping a head CT is not your call. It is mine. So you’ve left me no choice but to bring the CT in here,” Amelia replied while putting the protective vest around Owen’s upper body, her hands momentarily lingering behind his back when the vest got stuck. “Is this about this morning?” Owen asks still confused at the whole situation at hand. “What?” Amelia replies while continuing to help Owen into the vest. “You seemed fine. You ate the french toast,” Owen replied while looking Amelia in the eyes this time. “Stop talking!” Amelia retorted making her way over to the CT machine. “Amelia, there is no indication that there’s a head injury. Zero,” Owen replied while trying to maintain eye contact with Amelia. “I heard she had a brain tumor. You think they didn’t get it all?” The intern across from Owen interjected. “I heard that,” Amelia said while looking at the CT machine.
“Almost done. You see how easy that is?” Amelia says as the CT machine continues to whir. “He would have bled out if we had waited for the CT. And you’re reading too much into this man because--” Owen starts to reply before Amelia interjects, “It’s okay. You can say it. Dr. Hunt thinks my decision-making is clouded because my brother died under similar circumstances. But he’s wrong.” Amelia replies while concentrating once more on the CT machine. “Am I?” Owen questions while looking up at Amelia. ‘You are. He has an expanding epidural hematoma,” Amelia replies while making eye contact with Owen. “Wait. What? Wow,” Owen responds while looking at the scan on the CT machine. “Okay, let’s get this thing out of here! Prep for a craniotomy,” Amelia announces while making her way into the scrub room.
“See there? It’s a simple procedure, but not doing it would’ve killed him. All this fuss for something as little as one, two, three,” Amelia says while looking at Owen. Chuckling Owen replies: “Okay. ‘I told you so is a little unbecoming on you.’ Also, he’d be dead if I’d done it your way,” Owen replies while meeting Amelia’s gaze. “Fair enough. He’s alive. That’s what matters,” Amelia says looking over at one of the interns. Suddenly Ben Warren appeared in OR 2. “Shepherd, you’re needed in OR 3.” Ben says while looking at Amelia. “Amelia, I’m sorry if I implied that--” Owen started saying before Amelia interrupted him. “No. It's okay. You were right. I mean, not about this morning. French toast was excellent this morning. But about Derek. He was in my head. He saved this guy. He was that good.” Amelia replied while looking at Owen and continued making her way out of the current OR to the next one. Right after Amelia made her way out of the OR, Owen retorted her previous statement by adding: “You know, one could argue I'm kind of saving him, too, but I'm gonna let it go. Yeah. I'm letting it go.”
Shortly after their surgery Amelia and Owen made their way to the gallery in OR 1. They made their way there together after Maggie insisted that they join her for a surprise. They reluctantly followed her to the gallery as they had planned to talk. Upon arriving to the gallery, all three of the surgeons were pleasantly surprised at the amount of people that had shown up. Moments later they all peered over at the small tv screen that was in the corner of the gallery to see Catherine Avery and Jackson appear on the screen. After a short pause Catherine begins speaking: “Good evening, ladies and gentlemen. It is my distinct privilege and honor to award this year's Harper Avery for Surgical Innovation. This award is named for my dear friend, who we lost this year which makes this award ever more meaningful. Harper Avery was a very complicated man. But his love for medical innovation was pure, and that describes this year's winner. So, without further ado, the Harper Avery for Surgical Innovation goes to Dr. Meredith Grey!”
The gallery and OR full of people erupted into cheers and applause upon hearing the news. Moments later they all focused their attention back onto the tv screen as Catherine appeared at the podium. “Here to accept on her behalf, Dr. Jackson Avery.” She says while stepping away from the podium to allow Jackson to speak. “Thank you. Incredible. Knowing very well that she might win tonight, Dr. Grey opted to stay in Seattle. A trauma came in, and she knew that she was the right doctor for the job. That's one of the many reasons that I'm so very, very proud to call her my colleague and my friend. Now, Dr. Grey has experienced more loss in her life than I think most of us would deem fair. She lost her little sister, Lexie Grey, who I know would love to be here tonight with us. She lost her husband, Dr. Derek Shepherd, who knew with total certainty that this night would happen. And she also lost her mother, Dr. Ellis Grey, who won this award twice, once as a resident and probably would have won a few more if she hadn't been taken from all of us so young. The most amazing thing about Meredith, though, is that she takes all that pain, all that loss, and she turns it into drive drive to save lives, to make things better, and despite all that she's lost, she continued to find joy in her work as a surgeon, as a teacher, as a mother. And she managed to share that joy through her spirit of discovery and of possibility and of hope right in the face of darkness. I am profoundly grateful for the lessons that I have learned from Meredith Grey, and it is my distinct honor to accept this award on her behalf. Congrats, Meredith!”
After everyone shuffled their way out of the packed gallery I made a point to talk to catch up to Amelia. I had to lightly jog to catch up to her but when I did, I laced my hand with hers and brought us into an empty on-call room. “Owen? What is going on?” Amelia asks while I turn around and lock the door. “You said that you wanted to talk, so I brought us here to do just that,” Owen replied while still holding her hands. “Okay, so what do you want to talk about Owen?” Amelia questions me as we sit on one of the beds in the room. After a break in silence I begin by saying: “Amelia, I know that we are separated. But the way that you were second guessing me and the way you barged into the OR, I feel like you are regretting our decision after all,” Owen replies while looking Amelia in the eyes.
“I had the feeling that we made the wrong decision as soon as we took off our rings. But I was afraid that you didn’t love me anymore. And when I walked in on you and Carina this morning in our kitchen, I really thought the chance of us getting back together was over” Amelia says while looking away from Owen.
“You really thought that I didn’t love you anymore?” Owen asks sincerely while looking at Amelia.
“Well that’s what it seemed like when I walked in the house this morning. You were so caught up with Carina that you didn’t even notice that I came in,” Amelia responds while keeping her gaze away from Owen’s.
“Amelia. Just because we are separated doesn’t mean that I don’t still love you,” Owen says while regaining eye contact with Amelia.
“Well I wasn’t sure by the way that you disregarded me this morning at home and at work today,” Amelia replies.
“I’m sorry if I made you feel uncomfortable at home and at work today. Believe me I was very uncomfortable at home this morning,” Owen says while he begins to blush.
“You were uncomfortable this morning? I couldn’t tell at all by the way that you were looking at Carina and her delicious french toast,” Amelia replies with a hint of a laugh.
“Yes I was. I’m surprised you didn’t notice,” Owen says while continuing to look at Amelia.
“I wasn’t able to focus on much with the smell of that french toast and you standing there naked,” Amelia replied mischievously while rubbing her hands up his arms.
“Amelia Shepherd!” Owen countered back unable to stop himself from laughing.
“Well can you blame me?” Amelia replies while moving her hands up around Owen’s neck.
“Now that you mention it, I can’t really blame you,” Owen says as he pulls Amelia as close as their bodies will allow into a passionate kiss.
Hours later after several rounds of lovemaking in the on-call room, Owen gently shook Amelia awake as he got off the bed. It took Amelia a second to realize what he was doing. And when she did she simply said: “Owen Hunt, what do you think you are doing?”
“Amelia,” Owen starts to say down on one knee, “Will you marry me, again?”
I stare down at him stunned by his action. “Owen, are you serious?”
“As serious as I will ever be. Marry me again, Amelia. I want to love you for the rest of my life. Why won’t you let me?” Owen responds with increasing anxiety as Amelia has yet to say a word.
“Owen, you realize that we aren’t actually divorced, and that we are still technically married, right?” Amelia replied with a small grin on her face.
Owen notices her grin and smiles back at her. “I know, but I want us to start over. With everything that we have gone through in these past few months, I truly believe that we deserve a fresh start.” Owen adds
“I want to love you for the rest of my life. Why won’t you let me Amelia,” Owen questions her while taking her hands in his.
“It’s not that I won’t let you, it’s if I should let you love me. After all that has happened, you know that I still love you, right?” Amelia replies while maintaining deep eye contact with Owen.
“Well I’d hope so after the way you acted this morning with Carina, and in the OR, not to mention what we just did for hours in this very room” Owen added while laughing and winking at her. “It’s not funny! I’m just trying to decide what is best for us at this point,” Amelia says while laughing and looking down at him.
“I think what I’m trying to say is that we should start over,” Owen replies while looking up at her.
“Well I wouldn’t be opposed to that idea,” Amelia says with a hint of sarcasm.
“Oh really? Hmmm, well then what should we do now?” Owen replies while looking at Amelia.
“I have a great idea, would you like to hear it?” Amelia asks Owen while pulling him up to sit next to her on the bed.
“I am very interested in hearing your idea, Dr. Shepherd,” Owen replied while grabbing her hand.
“Okay well,” Amelia starts to say as she pulls Owen in for a passionate kiss.
“I’m really liking this idea so far. But you didn’t answer my question, Amelia. Will you marry me and spend the rest of your life with me?” Owen asks while still trying to catch his breath.
“Yes Owen. A million times yes. Will you just shut up and kiss me again already?” Amelia says impatiently.
“Absolutely, wife” Owen replies while smiling and once again kissing Amelia.
I hope you all like it. Sorry I haven’t been posting many fics lately. College has been keeping me very busy.
50 notes
·
View notes
Text
Near Fatal Carbon Dioxide Embolism during Laparoscopy and its Successful Aspiration Using Ultrasound Guided Catheter-Juniper Publishers

Abstract
Significant carbon dioxide embolism is an extremely rare but potentially fatal complication during laparoscopic surgeries. Until now, carbon-Di-oxide (CO2) is the agent of choice to create the pneumoperitoneum; consequently, there is inherit risk of CO2 embolism. Clinical symptoms of this embolism may be asymptomatic to cardiovascular collapse to neurological injury depending on the amount and rate of carbon dioxide absorption into body. Here we describe a case of near fetal gas (CO2) embolism in a morbidly obese patient undergoing laparoscopic cholecystectomy.
Keywords: Carbondioxide embolism; Laparoscopy; Cholecystectomy; Carboperitoneum
Abbreviations: ASA: American Society of Anaesthesiology; BMI: Body Mass Index; INR: International Normalisation Ratio; IPPV: Intermittent Positive Pressure Ventilation; TOF: Train Of Four; CPR: Cardiopulmonary Resuscitation; ROSC: Return of Spontaneous Circulation; TEE: Transesophageal Echocardiography
Introduction
Laparoscopy has become a standard of care for most intra-abdominal diagnostic and therapeutic procedures as it has many advantages such as more rapid return to daily activities, less post-operative pain, shorter hospital stay, and significant cost savings. Until now, carbon-Di-oxide (CO2) is the agent of choice to create the pneumoperitoneum; consequently, there is inherit risk of CO2 embolism. Significant carbon dioxide embolism is an extremely rare but potentially fatal complication during laparoscopic surgeries [1-3]. The magnitude or severity of symptoms depend on the rapidity and volume of gas (CO2) entry into the venous circulation. Large rapid entry of CO2 can leads to predictable chain of pathophysiological events which may continue to cardiovascular collapse and death. Depending on the amount and rapidity of CO2 absorption, symptoms very from hypercapnia, hypoxemia, decreased in end tidal CO2, arrhythmias, myocardial ischemia, cardiac arrest. Most cases of CO2 embolism occurs due to its inadvertent injection of CO2 directly into a vessel (large vein, artery) or very vascular solid organs during the initial insufflation phase of creating pneumoperitoneum. We encountered a case of unanticipated massive gas embolism (CO2) without many of the usual clinical features during the dissection phase in laparoscopic cholecystectomy.
Case Report
A 25 year super morbidly obese female weighting 110 kg, height of 158 cm (body mass index [BMI] of 44 kg/m2) and American Society of Anaesthesiology (ASA) physical status of 3 was posted for laparoscopic cholecystectomy. There was no other obesity associated medical problems except for occasional snoring but no other suggestive history of Obstructive Sleep Apnea. General and physical examination including airway assessment was unremarkable except for super morbid obesity. Routine preoperative laboratory investigation (complete blood count, serum creatinine, blood glucose) were within normal range. There were mild elevation of hepatic enzymes but prothrombine time and international normalisation ratio (INR) were within normal range.
General Anaesthesia (GA) with endotracheal intubation was planned. She was premedicated with ranitidine 50 mg along with 10 mg of metoclopramide intravenously (IV), 45 minutes prior to induction of GA. On arrival to preoperative holding area, 2 mg of intravenous midazolam was administered.
All gadget and equipment to manage super morbid obese were kept ready including difficult airway cart. Patient was induced on the operating table in ramped position. After applying the standard monitors (pulse oxymetry, non-invasive blood pressure, electrocardiogram [ECG]) and preoxygenation with 1OO % O2 for 3 minutes; GA was induced with fentanyl 150 microgram, followed by propofol 200mg; after confirming the ability to ventilate with bag-mask, 40mg of atracurium was administered to facilitate endotracheal intubation. The patient was intubated using portex cuffed 7.5mm orotracheal tube and confirmed with waveform capnography and presence of bilateral breath sound on auscultation. Maintenance of anesthesia was dne by 60% oxygen in air with sevoflurane (end tidal 2%), and remifentanyl infusion @100-400 microgram/hour. Intermittent positive pressure ventilation (IPPV) done with tidal volume of 400 ml, respiratory rate of 18/minute and PEEP of 6cm water. Apart from capnography, temperature and neuromuscular in the form of Train of Four (TOF) monitoring was initiated soon after endotracheal intubation.
Surgery started with creation of pneumoperitoneum by CO2 insufflation through varess needles targeting intraabdominal pressure of 15cm water; trocars were passed through the standard port under direct intraperitoneal vision. Patient remained stable during the gas insufflation and introduction of trocars; gall bladder was identified, operating table adjusted for proper surgical access. After clipping the cystic duct and artery; during the dissection of gall bladder from the liver bed, surgeon noticed profused oozing from the gall bladder bed; within a minute there was sudden drop in end tidal carbon dioxide from 37 to 7mmHg, the patient became cyanosed with saturation (Sp02) below 50%, and heart rate dropped from 96/minute to 40/minute with very faint brachial pulse on palpation. Blood pressure recheck revealed a mere systolic reading of 60mmHg without recordable diastolic. Immediately called for extra help, inspired oxygen concentration increased to 100% and ventilator switch to manual mode; Surgeons were immediately notified and asked to hold the surgery and to release the carboperitoneum. A quick check for airway and circuit connection did not revealed any malfunction; a provision diagnosis of Carbon di-oxide embolism was made; rapid boluses of iv fluid flushed, decided to put the patient in left lateral position to prevent CO2 lodging in the pulmonary artery. While attempting to give left lateral (Durant position), patient went into cardiac arrest (asystole in the ECG trace, with no palpable pulse). Immediately patient was repositioned supine, chest compressions started and asked for iv epinephrine 1mg. While Cardiopulmonary resuscitation (CPR) was ongoing, right internal jugular vein was canulated quickly using ultrasound guidance and a triple lumen central venous catheter inserted up to 20cm; immediately, all the three ports of central line were aspirated for gas. Approximately, a total of 25ml of gas was aspirated. Following aspiration of gas, CPR continued for another two cycles before getting the return of spontaneous circulation (ROSC). CPR lasted about 13min with four dosage of epinephrine (1mg each). Finally CPR terminated with ROSC with a heart rate of 130/minute, blood pressure of 139/86 mmHg and Sp02 was 92%. Oxygen saturation slowly improved to 98% over 15min after increasing the PEEP to 10 cm of water. Arterial blood gas immediately after ROSC revealed mild respiratory acidosis with pH7.21, PaCo2 53 mmHg, PaO2 78 mmHg, HCo3- 20 mmol/l. Blood glucose, electrolytes were all within normal limits.
Following successful resuscitation, it was decided for laparotomy and proceed with open cholecystectomy, surgery completed with surgicel (absorbable haemostat) pack in gall bladder bed and a surgical drain. After completion of surgery, patient was transfer to intensive care unit (ICU) for further management. Patient remained haemodynamically stable in ICU with normalization of ABG with adequate urine output. After 2 hours of ICU transfer, once patient started breathing on her own and followed commands, she was successfully extubated on facemask and was kept overnight for ICU monitoring. Further hospital course was unremarkable, the patient was discharged home after 6 days without any sequel.
Discussion
Incidence of clinically significant fatal Carbon dioxide embolism is a rare complication of laparoscopic surgeries (0.0014-0.6%) but with a high mortality of 28% [3]. There have been reports of carbon dioxide embolism occurring in various laparoscopic procedures [4-10].
Although, CO2 embolism can occur at any time of surgery but majority of fatal embolism occur during initial insufflation of peritoneum due to inadvertent injection of CO2 directly into a vessel (large vein, artery) or very vascular solid organs [1-3,9,11]. In our case, it was during the resection phase, there was a surgical raw area at the base of gall bladder and gas was entrained from there. Rapid entrapment of CO2 in our case might be favored by high intraperitoneal insufflation (flow rate 6 l/min) to achieve a higher intra-abdominal pressure (15cm water).
Clinical manifestation of CO2 embolism depends on the amount rapidity of gas entering into the venous system. Slow entrainment of gas results in small emboli of CO2 and the clinical effects depends on the balance between the volume of gas entering and remove from the venous system. CO2 entrapment exceeding 1ml/kg/min may be fatal in majority of cases, which may occlude pulmonary circulation, whereas rapid embolization of a large volume of gas (Gas lock) causes right ventricular outflow tract obstruction and leads to cardiovascular collapse [11,12]. Clinically, CO2embolism can present as haemodynamic changes in the form of bradycardia, tachycardia, hypotension, arrhythmias and respiratory changes that include hypoxemia (desaturation) with increase or decrease in end tidal CO2 tension. A “mill-wheel” murmur can also be auscultated [2,3]. High intra-abdominal pressure and patient position further exaggerate the haemodynamic alteration due to massive CO2 embolism. Peritoneal insufflation below 12cm water may decrease the incidence of significant CO2 embolism [13].
Sub-clinical and minor gas embolism during laparoscopy can be detected early by using invasive monitors like Transesophageal echocardiography (TEE), esophageal doppler, esophageal and precordial stethoscope which are more sensitive and allow for early detection of even minor embolism [2,14-17]. However, routine use of such invasive monitoring in laparoscopic procedures are not indicated as the incidence of significant CO2 embolism is very rare.
Capnography provides or a valuable tool for early diagnosis of gas embolism [14]. End tidal CO2 (ETCO2) monitoring has been suggested as a sensitive and non-invasive means of detecting gas embolism [14,15]. CO2 embolism can cause either increase or decrease of ETCO2 depending on amount and rapidity of gas embolism [3]. Small transient rise in ETCO2 may be seen due to increase in the dissolved CO2 in blood. Significant CO2 embolism is detected by sudden decrease in ETCO2along with haemodynamic changes and desaturation [2,3] although, other mechanical causes like endotracheal tube kinking, malposition, pneumothoraxar should also be ruled out as we did in our case.
The prognosis of these fatal complication depends on early detection and immediate intervention in order to prevent further gas entry, reduction in the volume of gas entrained and haemodynamic support. Series of interventions are very crucial for successful resuscitation. First of all, immediate cessation of insufflation with decompress carboperitoneum should be done. Patient should be ventilated with 100% oxygen to improve hypoxemia and wash out of CO2. Aggressive IV fluid boluses to increase central venous pressure to prevent further embolism of gas [18]. The patient may be placed in steep head down left lateral position (Durant manuever) and this position relieved right ventricular outflow obstruction by emboli and also resumption of pulmonary blood flow [15]. Multi-orifice central venous or pulmonary artery catheter may be inserted for confirming diagnosis and may allow aspiration of gas from the right heart, thereby relieving the gas lock status [15,19,20]. Data from experimental laborotary has shown that during venous air embolism, air remained more on the right ventricule for a long period (average 12 min) [21]. We inserted the central line fully (up to 20 cm mark) and was able to aspirate gas from all the three port. Direct aspiration of gas from both right atrium and ventricule may be best treatment for immediate improvement in the haemodynamic parameters and this can be done rapidly using ultrasound guided placement of multilumen catheter through right internal jugular vein. This intervention was the most critical in our case and without this we might had lost the patient.
Ultrasound guidance (USG) during central line insertion is a real help as it reduces the procedural time, number of attempt, decrease the failure rate and complications [22-25]. Use of USG in emergency central venous access has been included as the core or primary emergency ultrasound application by American College of Emergency Physician (ACEP) [26]. Although, there is no current guideline or recommendation for emergent central venous catheter placement for aspiration of gas during an acute setting of gas embolism with haemodynamic instability, it may be very useful treatment when clinical condition deteriorate rapidly despite other resuscitative measures.
In our case, prompt clinical diagnosis based on rapid cardiovascular collapse, with decrease in end tidal carbon dioxide (ETCO2) with desaturation and timely interventions using ultrasound guided emergency placement of central line and aspiration of CO2 helped in successful resuscitation.
Conclusion
Carbon dioxide embolism is an inherent risk of laparoscopic surgeries, it can happen at any point of time during the laparoscopic procedures. Continuous vigilance and prompt interventions is the key to successful resuscitation. Ultrasound may be a great tool in immediate placement of central venous catheter and direct aspiration of gas from the heart in massive embolism may be the most effective intervention in haemodynamically compromised patient.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com
For more articles in Journal of Anesthesia & Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
For more Open Access Journals please click on: https://juniperpublishers.com
0 notes