#nonrestoration
Text
Big ass ebony slut gets fucked hard and deep
Angel Wicky Steak & Blowjob Event at SecretFriends full video
Naked teenage boy cumshot video clips gay xxx He got his wonderful
Korean Porn HOT REDHEADED Korean
Bib boob teen fucking hot
Brazilian anal sex
Naturally busty lesbian
Slippery asian cowgirl Vicki Chase
Foot JOI with self toe sucking
Thick Ass MILF Lesbian Seduction
#blockhole#agreement#pathobiologist#valu#Ludgathian#multicrystalline#green-garbed#oc#pauperizer#nonrestoration#ocht#delegate#presumed#aeronauts#sweet-singing#agas#Diadelphia#ephedrin#perfectionistic#ectozoa
0 notes
Note
Unfollowed
Unfollowed due to PUS reasons
Unfollowed and blocked
Unfollowed and shamed
Shame
Shame
Shame
(Jk id rather die then let u go, your writing is sometimes the thing that makes it worth getting up in the morning but fr why the fuck would you share that showerthough???????)
Why must i suffer alone???? (i was reading about tooth infections for my exams and i remembered a patient i did and he had a lot of pus in his tooth and i only had to extract his nonrestorable tooth, but DAMN I WAS TEMPTED TO SQUEEZE THE PUS OUT OF IT😭 which ofc then lead to this deranged thought🤢)
also, just wanna tell u guys that yes, when i did my first patient ever, i was kinda grossed out, but then it became really fun and it doesnt affect me anymore- not the blood, not the spit, and definitely not the pus. so, dont feel concious when u do go to your dentist (exceptt maybe... you know, brush your teeth/rinse out whatever u had for ur last meal. Dont like to see bits and pieces of that stuck in there)
20 notes
·
View notes
Text
Understanding Insomnia: Causes, Consequences, and Solutions

Sleep is a fundamental aspect of our lives, essential for maintaining physical,mental, and emotional health. Yet, for many, a peaceful night's rest remains elusive due to a condition known as insomnia. Insomnia affects millions of people worldwide, interfering with their ability to fall asleep or stay asleep, and often leading to a range of physical and psychological consequences. In this article, we will delve into the world of insomnia, exploring its common triggers, potential consequences, and various treatment approaches, with a particular focus on comparing Cognitive-Behavioral Therapy for Insomnia (CBT-I) and medications as treatment options.
Insomnia Unveiled
Insomnia is a sleep disorder characterized by persistent difficulties in initiating or maintaining sleep, or experiencing non-restorative sleep, despite having ample opportunity for rest. It can occur intermittently (Acute) or persist for extended periods (Chronic), taking a toll on an individual's daily life and overall well-being. It should be noted that the diagnostic criteria of insomnia is: Difficulty falling asleep, staying asleep or nonrestorative sleep despite adequate opportunity and circumstance to sleep with this impairment in sleep is associated with daytime impairment or distress, and sleep difficulty occuring at least 3 times per week for at least 1 month.
Common Triggers of Insomnia
Understanding the triggers of insomnia is crucial for identifying and addressing the root causes. Several factors can contribute to the development of this sleep disorder:
Stress and Anxiety: High levels of stress and anxiety are among the leading causes of insomnia. Racing thoughts, worries, and a heightened state of alertness can make it difficult to relax and fall asleep.
Poor Sleep Habits: Irregular sleep schedules, excessive use of electronic devices before bedtime, and a lack of a consistent sleep routine can disrupt the body's natural sleep-wake cycle.
Medical Conditions: Certain medical conditions such as chronic pain, asthma, allergies, and gastrointestinal problems can make it uncomfortable or even painful to sleep.
Medications and Substance Use: Some medications and substances, including caffeine, nicotine, and alcohol, can interfere with sleep patterns.
Psychological Disorders: Conditions like depression and bipolar disorder are often associated with insomnia, as they can lead to disturbances in sleep patterns.
Environmental Factors: Noise, light, an uncomfortable mattress, or an unsuitable room temperature can all disrupt sleep.
Types of Insomnia
Insomnia can manifest in various forms, depending on its duration and underlying causes. Understanding these types can aid in the diagnosis and treatment of the condition:
Acute Insomnia: This is a brief episode of sleeplessness that lasts for a few nights to a few weeks. It is often triggered by a specific event, such as stress, travel, or illness, and typically resolves on its own once the triggering factor is addressed.
Chronic Insomnia: Chronic insomnia occurs when an individual experiences sleep disturbances at least three nights a week for three months or longer. It is often associated with underlying medical or psychological conditions.
Onset Insomnia: Onset insomnia refers to difficulties in falling asleep at the beginning of the night. It may be related to factors such as stress, poor sleep habits, or an irregular sleep schedule.
Maintenance Insomnia: Maintenance insomnia involves waking up during the night and having trouble falling back asleep. This type of insomnia is often associated with medical conditions or anxiety.
Comorbid Insomnia: Comorbid insomnia occurs alongside other medical or psychological disorders, such as depression, anxiety, or chronic pain. Treating the underlying condition is crucial for managing comorbid insomnia.
Potential Consequences of Insomnia
The impact of insomnia extends beyond mere sleeplessness. It can have a profound effect on an individual's physical and mental health, as well as their overall quality of life:
Daytime Fatigue and Impaired Cognitive Function: Persistent fatigue, reduced concentration, and impaired memory are common daytime consequences of insomnia. This can hinder productivity and increase the risk of accidents.
Mood Disorders: Chronic insomnia is strongly linked to mood disorders, including depression and anxiety. The relationship between insomnia and these conditions is often bidirectional, with one exacerbating the other.
Physical Health Complications: Insomnia is associated with an increased risk of various health issues, such as obesity, heart disease, diabetes, and hypertension.
Reduced Quality of Life: Individuals with insomnia often report a diminished quality of life due to the constant struggle with sleeplessness and its repercussions.
Seeking Relief from Insomnia
Fortunately, there are numerous strategies and treatments available to address insomnia and its underlying causes. The choice of treatment depends on the severity and duration of the condition, as well as the individual's specific needs and preferences.
Lifestyle Changes
Sleep Hygiene: Establishing a bedtime routine and maintaining a consistent sleep schedule can help regulate the body's internal clock. Avoiding stimulants, such as caffeine and nicotine, before bedtime is also essential.
Stress Management: Techniques like meditation, deep breathing exercises, and progressive muscle relaxation can reduce stress and anxiety, making it easier to fall asleep.
Dietary Adjustments: Avoiding heavy meals close to bedtime and limiting alcohol intake can improve sleep quality.
Exercise: Regular physical activity has been shown to promote better sleep, but it's important to avoid intense workouts too close to bedtime.
Behavioral Therapies
Cognitive-Behavioral Therapy for Insomnia (CBT-I): CBT-I is a highly effective approach that addresses the cognitive and behavioral factors contributing to insomnia. It helps individuals change their thoughts and behaviors surrounding sleep, promoting healthier sleep patterns.
CBT-I involves working with a trained therapist to identify and challenge negative thought patterns about sleep, establish a consistent sleep schedule, and implement relaxation techniques. It aims to address the root causes of insomnia rather than merely masking the symptoms.
Biofeedback: This technique involves monitoring physiological parameters such as heart rate and muscle tension and using feedback to learn to control them, which can help manage insomnia.
Medications
Prescription Medications: In some cases, doctors may prescribe medications to help manage insomnia, including sedatives and sleep aids. These should be used under medical supervision due to the risk of dependence and side effects. Medications are typically considered when other treatments have proven ineffective, or when insomnia is severe and significantly impairs daily functioning.
Medications can provide short-term relief, but they do not address the underlying causes of insomnia and may come with potential side effects and the risk of dependence.
Comparing CBT-I to Medications
When considering treatment options for insomnia, it's essential to weigh the pros and cons of Cognitive-Behavioral Therapy for Insomnia (CBT-I) and medications:
CBT-I
Addresses Root Causes: CBT-I focuses on identifying and addressing the underlying causes of insomnia, making it a long-term solution that can lead to sustained improvements in sleep quality.
Minimal Side Effects: CBT-I typically has no side effects, making it a safe option for most individuals.
Reduces Dependency: Unlike medications, CBT-I does not carry the risk of dependence or withdrawal symptoms.
Sustained Benefits: Many individuals who undergo CBT-I experience lasting improvements in their sleep patterns even after the therapy has concluded.
Medications
Quick Relief: Medications can provide relatively rapid relief from insomnia symptoms, making them suitable for short-term use in severe cases.
Limited Duration: Medications are typically recommended for short-term use due to the potential for dependence and side effects.
Masking Symptoms: Medications may mask the symptoms of insomnia without addressing the underlying causes, potentially leading to a return of sleep problems when the medication is discontinued.
Potential Side Effects: Depending on the medication, side effects can include dizziness, drowsiness, and impaired coordination, which may affect daytime functioning.
In conclusion, insomnia is a common sleep disorder with a range of potential causes and consequences. When seeking treatment for insomnia, it's crucial to consider the options available and their respective benefits and drawbacks. Cognitive-Behavioral Therapy for Insomnia (CBT-I) is often regarded as a first-line treatment due to its ability to address the root causes of insomnia and provide lasting relief without the potential for dependence or side effects. Medications, while effective for short-term symptom relief, should be used cautiously and under medical supervision to minimize the risk of dependency and side effects. Ultimately, the choice between CBT-I and medications should be made in consultation with a healthcare provider, taking into account individual needs and circumstances. A good night's sleep is within reach, and with the right approach, insomnia can be effectively managed, improving overall quality of life.
#insomnia management#chronic insomnia#acute insomnia#can't sleep#i just want to sleep#sleep habits#restorative sleep#better sleep#life balance#overall wellness#overall wellbeing#sleep simply well
0 notes
Text
Obstructive Sleep Apnea Treatment

Obstructive Sleep Apnea Treatment
Overview Obstructive Sleep Apnea Treatment
Obstructive sleep apnea is the most common sleep-related breathing disorder. It causes you to repeatedly stop and start breathing while you sleep.There are different types of sleep apnea, but the most common is obstructive sleep apnea. This type of apnea occurs when your throat muscles relax intermittently during sleep and block your airway. A telltale sign of obstructive sleep apnea is snoring. Treatment for obstructive sleep apnea is available. One treatment is a device that uses positive pressure to keep the airway open while you sleep. Another option is a mouthpiece that protrudes your jaw while you sleep. In some cases, surgery is also an option.


Symptoms
- Excessive daytime sleepiness
- Loud snoring
- Observed episodes of stopped breathing during sleep
- Abrupt awakenings accompanied by gasping or choking
- Awakening with a dry mouth or sore throat
- Morning headache
- Difficulty concentrating during the day
- Mood changes, such as depression or irritability
- High blood pressure
- Decreased libido
- Snoring loud enough to disturb your sleep or that of others
- Waking up gasping or choking
- Pausing in your breathing during sleep
- Having excessive daytime drowsiness, which may cause you to fall asleep while working, watching television or even driving a vehicle
Abstract
The diagnosis and treatment of obstructive sleep apnea is discussed in the context of recent diagnostic and therapeutic advances.
Introduction
Obstructive sleep apnea (OSA) is characterized by episodes of pauses or shallow breathing during sleep. These episodes are due to complete or partial collapse of the upper airway. Most often, respiratory events were associated with snoring, oxygen desaturation, and brief sleep arousals.Sleep apnea is usually worse during supine and REM (rapid eye movement) sleep. Drinking alcohol or taking sedatives can make snoring and OSA worse.
Diagnostic Criteria Obstructive Sleep Apnea Treatment
Modified from International Classification of Sleep Disorders – Third edition (ICSD-3)5 (A and B) or C satisfies the criteria:A. The presence of one or more of the following- The patient complains of sleepiness, nonrestorative sleep, fatigue, or insomnia.
- The patient wakes with breath holding, gasping, or choking.
- The bed partner or an observer reports habitual snoring or breathing interruptions in sleep.
- The patient has hypertension, a mood disorder, cognitive dysfunction, coronary artery disease, stroke, congestive heart failure, atrial fibrillation, or type 2 diabetes mellitus.B. Polysomnography (PSG) or out-of-center sleep testing (OCST) demonstratesFive or more predominantly obstructive respiratory events (obstructive apneas, hypopneas, or respiratory effort related arousals ) per hour of sleep during a PSG or per hour of monitoring (OCST).C. PSG or OCST demonstratesFifteen or more predominantly obstructive respiratory events (apneas, hypopneas, or RERAs) per hour of sleep during a PSG or per hour of monitoring (OCST).
Lifestyle and home remedies
In many cases, self-care may be the most appropriate way for you to deal with obstructive sleep apnea. Try these tips:- Lose weight. If you're overweight or obese, even a moderate loss of excess weight may help relieve constriction of your airway. Losing weight can also improve your health and quality of life and might reduce your daytime sleepiness.
- Exercise. Exercising, such as aerobic exercise and strength training, can help improve your condition. Aim to exercise about 150 minutes a week, and generally try to exercise most days of the week.
- Avoid alcohol and medications such as anti-anxiety drugs and sleeping pills. Alcohol, some anti-anxiety medications, and some sleeping pills can worsen obstructive sleep apnea and sleepiness.
- Sleep on your side or stomach rather than on your back. Sleeping on your back can cause your tongue and soft palate to rest against the back of your throat and block your airway.To prevent sleeping on your back, try sewing a tennis ball in the back of your pajama top or place pillows behind you while you sleep on your side.
- Keep your nasal passages open while you sleep. If you have congestion, use a saline nasal spray to help keep your nasal passages open. Talk to your doctor about using nasal decongestants or antihistamines, because some medications may be recommended for only short-term use.
Treatment
Lifestyle changesObstructive Sleep Apnea Treatment For milder cases of obstructive sleep apnea, your doctor might recommend lifestyle changes:- Lose weight if you're overweight.
- Exercise regularly.
- Drink alcohol moderately, if at all. Don't drink in the hours before bedtime.
- Quit smoking.
- Use a nasal decongestant or allergy medications.
- Don't sleep on your back.
- Avoid taking sedative medications such as anti-anxiety drugs or sleeping pills.If these measures do not improve your sleep, or if your apnea is moderate to severe, your doctor may recommend other treatments. Certain devices can help open blocked airways. In other cases, surgery may be required.
Conclusion
OSA is a serious disease that affects approximately 12 percent of American adults. Most patients go undiagnosed and pose a serious public health and economic burden. The STOP-BANG score serves as a reliable screening tool to identify patients who may have OSA. Appropriate treatment modalities should be instituted after early diagnosis in the laboratory using PSG or HSAT.Currently, CPAP remains the treatment of choice for moderate and severe OSA. Although not as effective as CPAP, there are acceptable alternatives for patients with mild OSA and severe OSA who cannot tolerate or adhere to CPAP. New therapies continue to emerge as the search for the most effective and best-tolerated treatments continues.
Facebook
Twitter
Youtube
Link
Frequently Asked Questions
Which type of doctor is best for sleep apnea?
#apnea #primary care #diagnose #medicine #obstructive #symptoms #care physicians #cpap An evaluation by a heart specialist, known as a cardiologist, or a doctor who specializes in the nervous system, called a neurologist, might be necessary to look for causes of central sleep apnea.Obstructive Sleep Apnea Treatment
Does ENT treat obstructive sleep apnea?
Yes, ENT (ear, nose, and throat) doctors can treat obstructive sleep apnea. Obstructive sleep apnea (OSA) is a sleep disorder that is caused by an obstruction of your airway during sleep.It is characterized by snoring, pauses in breathing, and gasping for air. ENTs are medical specialists that specialize in diagnosing and treating disorders and diseases of the ear, nose, and throat.This includes conditions that affect your breathing, such as obstructive sleep apnea. When diagnosing and treating OSA, an ENT will perform a physical examination and take a medical history.They may also order tests, such as a sleep study, to look for signs of OSA. If OSA is diagnosed, an ENT may recommend lifestyle changes, such as weight loss, avoiding alcohol and smoking, as well as sleeping on your side.
What is the most best treatment for patients with obstructive sleep apnea?
Obstructive sleep apnea (OSA) is a disorder characterized by recurrent episodes of partial or complete upper airway obstruction during sleep. It is a common sleep disorder that can have serious implications for a person’s overall health and well-being.The most effective treatment for patients with OSA is continuous positive airway pressure (CPAP) therapy. CPAP therapy is a non-invasive treatment that uses a machine to deliver a steady stream of pressurized air to keep the airway open while sleeping.The pressure is adjusted to match the individual’s needs and is typically determined by a sleep specialist. The CPAP machine is connected to a mask that fits over the nose or mouth and is worn while sleeping.
What is obstructive sleep apnea in ENT?
Obstructive sleep apnea (OSA) is a disorder in which breathing is periodically stopped or reduced while you’re asleep because the muscles in your neck and tongue aren’t able to maintain the airway open despite your efforts to breathe, depriving your body of oxygen.
What is the best treatment for obstructive sleep apnea?
Continuous positive airway pressure (CPAP)Because it can reduce the symptoms of OSA7 and enhance quality of life, CPAP is regarded as the gold standard treatment for the condition. Via the use of a mask interface, CPAP functions as a pneumatic splint that maintains consistent positive pressure in the upper airway.
Can obstructive sleep apnea be cured?
While there is no cure for sleep apnea, studies show that certain lifestyle factors can reverse or make your sleep apnea less intense. Other treatment or surgical options can also reverse the condition. Sleep apnea happens when your upper airway muscles relax while you sleep. This causes you to not get enough air
What is the newest treatment for sleep apnea?
Inspire is an alternative to CPAP that works inside your body while you sleep. It’s a small device placed during a same-day, outpatient procedure. When you’re ready for bed, simply click the remote to turn Inspire on. While you sleep, Inspire opens your airway, allowing you to breathe normally and sleep peacefully.
Can sleep apnea be cured naturally?
“The only way to ‘cure’ sleep apnea naturally is with significant lifestyle changes,” notes Dr. May. Generally, sleep apnea symptoms like daytime sleepiness and comorbidities like heart disease and excess weight can be treated thus. For example, daytime sleepiness can be curbed with a cup of coffee.
What is the first line treatment for sleep apnea?
Positive airway pressure (PAP) is first-line therapy for all patients with moderate to severe OSA, those with mild OSA syndrome, and any patients with significant comorbidities (e.g. depression, diabetes, hypertension). 8 PAP works as a pneumatic splint, relieving upper airway obstruction during sleep.
Is obstructive sleep apnea serious?
Obstructive sleep apnea is considered a serious medical condition. Complications can include: Daytime fatigue and sleepiness. Because of a lack of restorative sleep at night, people with obstructive sleep apnea often have severe daytime drowsiness, fatigue and irritability.
Can you live a long life with sleep apnea?
If left untreated, obstructive sleep apnea can shorten your life from anywhere between 12-15 years. While there is no permanent cure for obstructive sleep apnea, diagnosis and treatment will alleviate its effects. Proper treatment can ensure that your OSA won’t shorten your life.
Can sleep apnea be cured by homeopathy?
Lachesis is considered as the best homeopathic medicine for curing sleep apnea. Lachesis cures the sleeping problem caused due to the frequent relaxation of the throat muscles. If you’re suffering from sleep apnea, you can take the medicine Lachesis.
What is the main cause of sleep apnea?
Obesity, large tonsils, or changes in hormone levels can all restrict the airway and raise the chance of developing obstructive sleep apnea. When your brain fails to send the impulses required to breathe, central sleep apnea results.
What age range is obstructive sleep apnea?
Anyone at any age can have obstructive sleep apnea, but it’s most common in middle-aged and older adults. Only about 2% of children have obstructive sleep apnea. It’s also more common in men than in women.
What is the most successful sleep apnea surgery?
Maxillomandibular advancement (MMA) is one of the procedures with the best success rates for treating sleep apnea, with a rate of roughly 87%. According to other studies, it ranges between 75% and 100%. However, due of the jaw displacement, specialists warn that it creates drastic alterations in physical appearance.
Can Ayurveda cure sleep apnea?
Yes. Ayurveda offers effective treatment for Sleep apnea through various internal medicines, treatment procedures and body purification therapies.
What is the most serious sleep apnea?
Obstructive sleep apnea is classified by severity: Severe obstructive sleep apnea means that your AHI is greater than 30 (more than 30 episodes per hour) Moderate obstructive sleep apnea means that your AHI is between 15 and 30. Mild obstructive sleep apnea means that your AHI is between 5 and 15.
What is the best sleep position for sleep apnea?
Sleep apnea and snoring: Obstructive sleep apnea causes the airways to close off when a person is asleep, resulting in breathing pauses. It frequently occurs along with snoring. You can lessen snoring and mild apnea by lying on your side or stomach to keep the airways open. Salas cites
What vitamins help sleep apnea?
Vitamins C, D, E, B6 and B12 all play a significant role in health and each of these has been shown to be very effective in combating sleep apnea and helping ensure good health
Who suffers from sleep apnea?
Males are two to three times as likely than women to develop sleep apnea. But, women who are overweight or have undergone menopause are at higher risk. being more senior. Older persons are considerably more likely to have sleep apnea.
What age does obstructive sleep apnea start?
When a child stops breathing while they are asleep, it is called obstructive sleep apnea (OSA). The airway is usually blocked (obstructed), which results in the stoppage of breathing. Children of all ages can develop obstructive sleep apnea, but those with it tend to be between the ages of two and six.
What foods cause sleep apnea?
5 Foods That Can Make Sleep Apnea Worse- Bananas. Bananas are full of healthful nutrients, and they are delicious. …
- Refined Carbohydrates. Whole grain foods are great for your health because they contain lots of nutrients and contribute to satiety. …
- Dairy. …
- Alcohol. …
- Fatty Meats.
Who is at risk for obstructive sleep apnea?
The major risk factors for obstructive sleep apnea are obesity, a family history of snoring or apnea, and being male



Obstructive Sleep Apnea Treatment
Sleep apnea doctor in kolkata
Are you looking for a sleep apnea doctor in Kolkata? If so, you’ve come to the right place. Sleep apnea is a sleep disorder that can have serious and long-term effects on your health and wellbeing. It is important to find an experienced and knowledgeable doctor who can provide the best care for your condition.Dr. Hironmoy Sil
35 Years Experience
Address:60 d/1A doctor S.C.banerjee Road , kolkata-700010
Contact: +91-09830022224
Timing: MON-SAT (
Read the full article
0 notes
Text
Impacted wisdom teeth
Impacted wisdom teeth is a condition where the third molars (wisdom teeth) are prevented from erupting into the mouth. This can be caused by a physical barrier, such as other teeth, or when the tooth is angled away from a vertical position. Completely unerupted wisdom teeth usually result in no symptoms, although they can sometimes develop cysts or neoplasms. Partially erupted wisdom teeth can develop cavities or pericoronitis. Removal of impacted wisdom teeth is advised in the case of certain pathologies, such as nonrestorable caries or cysts.
Wisdom teeth likely become impacted because of the jaw being too small for the teeth to erupt well, probably caused by not chewing enough crunchy and hard foods such as fruits and vegetables in the years of physical growth. Impacted wisdom teeth are classified by their direction of impaction, their depth compared to the biting surface of adjacent teeth and the amount of the tooth’s crown that extends through gum tissue or bone. Impacted wisdom teeth can also be classified by the presence or absence of symptoms and disease.
Screening for the presence of wisdom teeth often begins in late adolescence when a partially developed tooth may become impacted. Screening commonly includes a clinical examination as well as x-rays such as panoramic radiographs. Infection resulting from impacted wisdom teeth can be initially treated with antibiotics, local debridement or surgical removal of the gum overlying the tooth. Over time, most of these treatments tend to fail and patients develop recurrent symptoms. The most common treatment for recurrent pericoronitis is wisdom tooth removal.
The risks of wisdom tooth removal are roughly proportional to the difficulty of the extraction. Sometimes, when there is a high risk to the inferior alveolar nerve, only the crown of the tooth will be removed (intentionally leaving the roots) in a procedure called a coronectomy. The long-term risk of coronectomy is that chronic infection can persist from the tooth remnants. The prognosis for the second molar is good following the wisdom teeth removal with the likelihood of bone loss after surgery increased when the extractions are completed in people who are 25 years of age or older. A treatment controversy exists about the need for and timing of the removal of disease-free impacted wisdom teeth.
Supporters of early removal cite the increasing risks for extraction over time and the costs of monitoring the wisdom teeth. Supporters for retaining wisdom teeth cite the risk and cost of unnecessary surgery. The condition affects up to 72% of the Swedish population. Wisdom teeth have been described in the ancient texts of Plato and Hippocrates, the works of Darwin and in the earliest manuals of operative dentistry. It was the meeting of sterile technique, radiology, and anesthesia in the late 19th and early 20th centuries that allowed the more routine management of impacted wisdom teeth
Originally published here: https://forestray.dentist/kb/impacted-wisdom-teeth/
0 notes
Text
Lupine Publishers | Apnea, Hypopnea and Their Individual Effects on Daytime Sleepiness and Sleep Quality

Lupine Publishers | Journal of Otolaryngology
Abstract
Background: Obstructive sleep apnea and hypopnea syndrome (OSA) is defined as a reduction or cessation of the airflow in the human airway. It effects nearly 18 million Americans and weight gain is the main predisposing factor. In this study, we aimed to investigate the effects of apnea and hypopnea individually.
Material and Methods: 83 participants were included in the study and they are divided into two groups as apnea predominant or hypopnea predominant. Pittsburg quality of sleep index (PQSI) and Epworth sleepiness scale (ESS) are completed for all subjects and full-night attended polysomnographic evaluations are done.
Results: ANOVA test was used to compare the inter-group variances. Between the two study groups, no statistical significance was reported between the PSQI or ESS scores.
Conclusion: The effects of apnea and hypopnea are similar on sleep quality or day-time sleepiness, however further studies also investigating the duration of the events as well are needed.
Abbreviations: OSA: Obstructive Sleep Apnea/Hypopnea Syndrome; PSG: Polysomnography; PSQI: Pittsburgh Sleep Quality Index; ESS: Epworth Sleepiness Scale.
Introduction
Obstructive sleep apnea and hypopnea syndrome (OSA) is reviewed under the sleep related breathing disorders. The diagnostic criteria must satisfy daytime sleepiness, fatigue or nonrestorative sleep, waking up with breath holding, gasping or choking, witnessed apnea periods and comorbidities such as hypertension, mood disorder, cognitive dysfunction, coronary artery disease or type 2 diabetes mellitus may accompany the disease. The full-night polisomnography (PSG) must demonstrate at least five obstructive respiratory events (apnea, hypopnea, respiratory effort related arousals) per hour of sleep (apnea/hypopnea index, AHI), but AHI below 15 needs the abovementioned signs for a complete diagnosis [1]. OSA may be seen in any age group, nevertheless published data from several countries indicate that OSA associated with daytime sleepiness occurs in 3% to 7% of adult men and 2% to 5% of adult women. However, because many individuals with OSA do not endorse daytime sleepiness, the prevalence of the disease is likely much higher [2]. The major predisposing factor for OSA is excess body weight. It has been estimated that nearly 60% of moderate to severe OSA is attributable to obesity. The risk of OSA increases as the degree of additional weight increases, with an extremely high prevalence of OSA in people with morbid obesity [3]. Several factors are implicated in the development of OSA [4].
The main cause addresses the reduction of the expansion forces of the dilator muscles of the upper airways. The capacity of the muscles decreases more during the REM sleep. Additional factors are excessive or elongated tissues of the soft palate, macroglossia, tonsillar hypertrophy, and a redundant pharyngeal mucosa [5]. OSA and comorbidities such as stroke, hypertension, metabolic syndrome, cardiovascular diseases or endocrinologic disorders are well taught in years, however the individual effects of apnea or hypopnea alone are never considered. To best of our knowledge, the published data does not mention which entity alone is more harmful to systemic functions or at least sleep, apnea or hypopnea? The Pittsburgh Sleep Quality Index (PSQI) is an effective instrument used to measure the quality of sleep in the adult. It differentiates “poor” from “good” sleep by measuring seven domains: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction over the last month. A global sum of “5” or greater indicates a “poor” sleeper [6]. The Epworth Sleepiness Scale (ESS) is a self-administered questionnaire with 8 questions. Respondents are asked to rate, on a 4-point scale, their usual chances of dozing off or falling asleep while engaged in eight different activities. The higher the ESS score, the higher that person’s daytime sleepiness and scores higher than 10 are significant. In this study, we compared apnea versus hypopnea due to the sleep quality and daytime sleepiness individually.
Materials and Methods
Between July 2017 and January 2019, 327 cases complaining of snoring, daytime sleepiness and witnessed sleep apnea periods were referred to full-night polisomnography. 150 cases were diagnosed as OSA were enrolled in the study. After the final assessment, a total number of 83 participants were chosen. The ethical committee approval was taken from Okmeydani Training and Research Hospital (48670771-514.10) and informed consent are taken from all participants.
PSG
3 Channel EEG (F4-M1, C4-M1, O2-M1), 2 channel EOG, chin, right and left tibialis anterior EMG, body position sensor, oro-nasal thermal sensor, nasal pressure sensor, thoracic and abdominal sensors, ECG, pulse-oximetry and synchronous video recordings and breath sound recordings were the parameters recorded through the night. The examination, sleep and wake periods and sleep related disorders were scored according to the criteria of the American Academy of Sleep Medicine [7].
Clinical Examination and Laboratory Tests
All participants underwent a detailed otolaryngologic examination including the fiberoptic naso-pharyngolaryngoscopy. Mueller maneuver was made to detect the pharyngeal collapse, vallecula epiglottica was visualized to assess the bulkiness, Friedmann Tongue Positions and Tonsil Gradings are made to determine the glossopharyngeal patency. Complete blood count and routine biochemical blood tests including the thyroid function tests were studied. PSQI and ESS were completed for each participant.
Study Design
In order to emphasize the individual effects of apnea or hypopnea, each PSG were examined and if apnea was higher than hypopnea by 50% or vice versa, that participant was included in the study. The study group, therefore, was divided into two as apnea predominant (AP) and hypopnea predominant (HP). Comorbid pulmonary or neurologic disorders, sleep disorders other that OSA (Central sleep apnea, Hypersomnolence, Parasomnias, Circadian rhythm disorders, etc.) were excluded. Also, pediatric population were not included in the study.
Statistical Analysis
A statistical analysis was performed using IBM SPSS Statistics 22 (IBM SPSS, Turkey). Continuous data was displayed as the mean ± standard deviation. Statistical significance was a p-value of greater than 0.05. A Shapiro–Wilk test showed the normal distribution of the parameters. ANOVA test was used to compare the normally distributed inter-group comparisons of the descriptive statistical methods (mean, standard deviation, and frequency) and the quantitative data.
Results
A total number of 83 participants aged between 24-64 years (mean 46±10 years) were studied. 61 were male (73.49%) and 22 were female (26.51%). The inter-group characteristics are shown in Table 1. The PSQI between AP and HP groups were not statistically significant (p=0.205). Similarly, ESS between AP and HP groups were also not statistically significant (p=0.240) (Figure 1).
Figure 1: AP versus HP by means of PSQI and ESS.
Table 1: Subject characteristics and statistical comparisons.
ANOVA test showed no statistical significance among variances.
OSA is defined as the reduction or cessation of airflow for at least ten seconds. The entity is almost every time in association with snoring, and between the snores, airflow may stop completely (apnea) or reduction in the airflow (hypopnea) may happen. If there is a body effort to breathe, the disease is termed obstructive, otherwise it is central. In the presence of a collapsible airway, sleepinduced loss of tonic input to the upper airway dilator muscle motor neurons allows the pharyngeal airway to collapse [8]. The general reaction to this airway obstruction is arousal; sleep then resumes, leading to repeated cycling of sleep, intermittent hypoxia, and arousal throughout the night. Neurocognitive effects of OSA include daytime sleepiness and impaired memory and concentration; cognitive impairment and neural injury may develop in association with sleep apnea [9,10]. Sleep-disordered breathing and OSA are not reported frequently in animals but a natural animal model
Discussion
OSA is defined as the reduction or cessation of airflow for at least ten seconds. The entity is almost every time in association with snoring, and between the snores, airflow may stop completely (apnea) or reduction in the airflow (hypopnea) may happen. If there is a body effort to breathe, the disease is termed obstructive, otherwise it is central. In the presence of a collapsible airway, sleepinduced loss of tonic input to the upper airway dilator muscle motor neurons allows the pharyngeal airway to collapse [8]. The general reaction to this airway obstruction is arousal; sleep then resumes, leading to repeated cycling of sleep, intermittent hypoxia, and arousal throughout the night. Neurocognitive effects of OSA include daytime sleepiness and impaired memory and concentration; cognitive impairment and neural injury may develop in association with sleep apnea [9,10]. Sleep-disordered breathing and OSA are not reported frequently in animals but a natural animal model of OSA is English bulldogs, which have been used to study upper airway anatomy and physiology and the pharmacologic treatment of OSA. English bulldogs have an enlarged soft palate and narrow oropharynx and display many of the clinical features of OSA, including snoring, sleep-disordered breathing, oxyhemoglobin desaturation during sleep, frequent arousal from sleep, and hypersomnolence with shortened sleep latencies [11]. OSA in English bulldogs is not related to obesity, as it often is in humans. OSA has been modeled in a variety of species by using surgical tracheostomy and subsequent intermittent occlusion of the endotracheal tube [12]. Schoorlemmer et al. [13] produced obstructive apnea in conscious rats by using an inflatable balloon implanted in the trachea and apneic episodes of as long as 16 s in duration could be created during sleep. However, animal models of intermittent hypoxemia have several drawbacks. In many cases, the models mimic severe human OSA and may be less applicable to most clinical OSA. In addition, animals exposed to intermittent hypoxemia develop hypocapnia, whereas human OSA is characterized by hypercapnia. Furthermore, human OSA typically is associated with obesity, which is not always considered in animal studies. In addition, OSA causes sleep fragmentation, which may have independent effects on metabolism. Thus, exposure of animals to intermittent hypoxemia produces repeated arousals and changes in sleep architecture that are comparable to those in clinical OSA, yet the effects may not be persistent, limiting their use for studying long-term metabolic consequences of OSA [14].
Animal models are troublesome to study the long-term effects of sleep fragmentation. The sleep quality is a bio-psycho-social parameter that may never be evaluated in animal models; for example, as we refer to excessive daytime sleepiness, the subject is asked whether the sleepiness occurs in the passive state such as resting periods or during the active periods such as work-time or social interactions. Moreover, the sleep architecture, ultradian rhythm or sleep quality may not be assessed in animal models. In our study, the effects of apnea or hypopnea on sleep quality or daytime sleepiness did not differ. This might have several reasons; first of all, all PSG were done elsewhere, our otolaryngology clinic is not capable to perform full-night attended PSG. This situation has some major drawbacks; it is impossible to mark each breath disorders epoch by epoch on the screen of the test computer, but we rather have a brief report of the night. This makes it impossible to calculate the duration of the respiratory events. Therefore, we only could compare the nature of the events by their scores or numbers (Table 1). Secondly, there are some other factors that may interfere with the sleep architecture such as drops in the oxygen levels; not every subject has the same decreasement in their oxyhemoglobine when they have the same level and duration of airway collapse. Thirdly, limb movements also disrupt the sleep quality and impede normal daytime cognitive functions. Finally, arousals are another issue to study; if OSA is recently developed in the subject, the peripheric chemoreceptors detecting the airflow cessation are more sensitive and arousal happens imminently, if the disease is longer the receptors may become insensitive that happens in sleep continuity despite the airflow cessation. Nonetheless, to best of our knowledge, there is no other study that tried to investigate the effects of apnea of hypopnea individually on sleep quality or daytime sleepiness.
Conclusion
The effects of apnea and hypopnea are similar on sleep quality or daytime sleepiness, however further studies also investigating the duration of the events as well are needed.
For more Lupine Publishers Open Access Journals Please visit our website: h
http://lupinepublishers.us/
For more Journal of Otolaryngology-ENT Research articles Please Click Here:
https://lupinepublishers.com/otolaryngology-journal/
To Know More About Open Access Publishers Please Click on Lupine Publishers
#Lupine Publishers#Lupine Publishers Group#Open Access Publishers#Otolaryngology Journal#Rhinology Journal
47 notes
·
View notes
Text
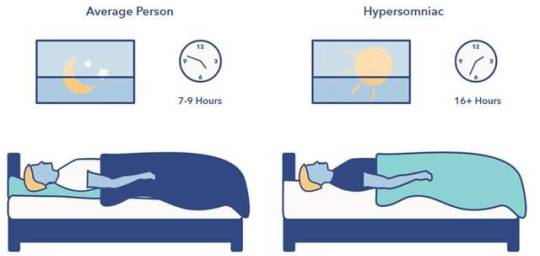
Hypersomnolence Disorder
Hypersomnolence is a condition where a person experiences significant episodes of sleepiness, even after having 7 hours or more of quality sleep. Other terms used to describe hypersomnolence include excessive daytime sleepiness, excessive daytime somnolence, and hypersomnia.
Hypersomnolence has three categories: acute, subacute, and persistent.
• acute hypersomnolence, lasting 1 month or less
• subacute hypersomnolence, lasting 1 to 3 months
• persistent hypersomnolence, lasting more than 3 months
Recurrent periods of an irrepressible need to sleep, lapsing into sleep, or napping occurring within the same day is a necessary feature of Narcolepsy. These must have been occurring at least three times per week over the past 3 months
Features and Symptoms
1. Hypersomnolence is a broad diagnostic term and includes symptoms of excessive quantity of sleep, deteriorated quality of wakefulness, and sleep inertia (i.e., a period of impaired performance and reduced vigilance following awakening from the regular sleep episode or from a nap)
2. The persistent need for sleep can lead to automatic behavior (usually of a very routine, low-complexity type) that the individual carries out with little or no subsequent recall
3. the sleep is often nonrestorative and is followed by difficulty awakening in the morning
Diagnosis
1. Self-reported excessive sleepiness (hypersomnolence) despite a main sleep period lasting at least 7 hours
2. The hypersomnolence occurs at least three times per week, for at least 3 months
3. The hypersomnolence is accompanied by significant distress or impairment in cognitive, social, occupational, or other important areas of functioning
4. The hypersomnolence is not better explained by and does not occur exclusively during the course of another sleep disorder
5. The hypersomnolence is not attributable to the physiological effects of a substance
6. Coexisting mental and medical disorders do not adequately explain the predominant complaint of hypersomnolence
Treatment
Stimulants are most commonly prescribed to treat hypersomnolence. In addition to medications, a doctor may recommend making changes to a person's "sleep hygiene" to help them get a good night's sleep.
1 note
·
View note
Photo

Intentional replantation has been defined as the deliberate extraction of a tooth and after evaluation of root surfaces, endodontic manipulation, and repair, placement of the tooth back in into its original socket. The procedure now involves multiple surgical steps that must be executed with precision for the best outcome. First, the selected tooth is carefully extracted so as not to induce fracture, thereby rendering the tooth nonrestorable, and also to minimize damage to the periodontal ligament (PDL). Survival of PDL cells has been noted to be a critical factor influencing successful healing. After extraction of the tooth, the roots are examined for fractures, additional canals or portals of exit, isthmi, and any additional anatomic features requiring attention. Root inspection is best accomplished with the aid of a dental operating microscope. Following root inspection, root resections are made using a high-speed handpiece, ideally of at least 3 mm, which has been shown to eliminate 98% of apical ramifications and 93% of lateral canals. In the event that granulomatous tissue remains attached to the root ends on extraction, it is carefully curetted or is removed when the root is resected. The root canals are then prepared to receive a root-end filling using either a high-speed handpiece or ultrasonic instrumentation. The ideal root-end preparation has been described as a class I cavity, at least 3 mm in depth, with parallel walls and consistent with the natural anatomic outline of the root canal space. Mineral trioxide aggregate (MTA), and calcium silicate cements, have shown superior ability to seal the root canal system and demonstrate greater biocompatibility. Once root-end fillings have been completed, the tooth is ready for reimplantation into its original socket. A recent systematic review of the literature by Torabinejad et al found an overall 88% survival rate for intentionally replanted teeth, with more contemporary studies demonstrating success rates as high as 95%. Because of recently reported high survival rates, intentional replantation might now be considered among more commonly accepted treatment options. #Dentist #dentistry (at Kuwait City) https://www.instagram.com/p/CZK8GzeMG-7/?utm_medium=tumblr
0 notes
Text
7 Suspicion checks you might be experiencing or getting into depression
New Post has been published on https://newscheckz.com/7-suspicion-checks-you-might-be-experiencing-or-getting-into-depression/
7 Suspicion checks you might be experiencing or getting into depression
People with depression often experience additional symptoms like sadness, feelings of irritability, and decreased energy.
We don’t often pair depression with physical pain but research shows this mental illness can really hurt.
Depression hurts. And while we often pair this mental illness with emotional pain like sadness, crying, and feelings of hopelessness, researchTrusted Source shows that depression can manifest as physical pain, too.
While we don’t often think of depression as physical pain, some cultures do; especially those where it’s “taboo” to openly talk about mental health.
For example, in Chinese and Korean cultures, depression is considered a myth. So patients, unaware that physical pain may be a sign of psychological distress, go to doctors to treat their physical symptoms instead of describing depression.
But keeping these physical symptoms top of mind is just as important as the emotional effects.
For one, it’s a great way to keep in check with your body and mind. Physical symptoms can signal when a depressive period is about to begin or clue you in to whether or not you may be experiencing depression.
On the other hand, physical symptoms demonstrate that depression is, in fact, very real and can be detrimental to our overall well-being.
Here are seven of the most common physical symptoms of depression:
Digestive problems or irregular bowel schedules
Digestive problems, like constipation and diarrhea can be embarrassing and uncomfortable.
Often caused by food poisoning or gastrointestinal viruses, it’s easy to assume that gut discomfort stems from a physical illness.
But emotions like sadness, anxiety, and overwhelm can disrupt our digestive tracks. One 2011 studyTrusted Source suggests a link between anxiety, depression, and gastrointestinal pain.
Fatigue or consistent lower energy levels
Fatigue is a common symptom of depression. Occasionally we all experience lower energy levels and can feel sluggish in the morning, hoping to stay in bed and watch TV instead of going to work.
While we often believe exhaustion stems from stress, depression can also cause fatigue.
However, unlike everyday fatigue, depression-related fatigue can also cause concentration problems, feelings of irritability, and apathy.
Dr. Maurizio FavaTrusted Source, Director of the Clinical Research Program at Boston’s Massachusetts General Hospital, points out that depressed individuals often experience nonrestorative sleep, meaning that they feel sluggish even after getting a full night of rest.
However, because many physical illnesses, like infections and viruses, can also cause fatigue, it can be challenging to discern whether or not the exhaustion is related to depression.
One way to tell: While everyday fatigue is a sign of this mental illness, other symptoms like sadness, feeling hopeless, and anhedonia (lack of pleasure in day-to-day activities) may also be present when you are depressed.
Back pain or aching muscles all over
Shot of a young businessman suffering from backache while working at his desk during a late night at work
You might feel okay in the morning, but once you’re at work or sitting at a school desk, your back starts to hurt.
It could be stress, or it could be depression. Although they’re often associated with bad posture or injuries, backaches can also be a symptom of psychological distress.
A 2017 research studyTrusted Source of 1,013 Canadian university students found a direct association between depression and backaches.
Psychologists and psychiatrists have long believed emotional issues can cause chronic aches and pains, but the specifics are still being researched, such as the connection between depression and the body’s inflammatory response.
Newer studies suggestTrusted Source that inflammation in the body may have something to do with the neurocircuits in our brain.
It’s thought that inflammation may interrupt brain signalsTrusted Source, and therefore may have a role in depression and how we treat it.
Headaches
Almost everyone experiences occasional headaches. They’re so common that we often write them off as nothing serious.
Stressful work situations, like conflict with a co-worker, can even trigger these headaches.
However, your headache might not always be induced by stress, especially if you’ve tolerated your co-worker in the past. If you notice a switch to daily headaches, it could be a sign of depression.
Unlike excruciating migraine headaches, depression-related headaches don’t necessarily impair one’s functioning.
Described by the National Headache Foundation as “tension headaches,” this type of head pain may feel like a mild throbbing sensation, especially around the eyebrows.
While these headaches are helped by over-the-counter pain medication, they typically re-occur regularly. Sometimes chronic tension headaches can be a symptom of major depressive disorder.
However, headaches aren’t the only indication that your pain may be psychological. People with depression often experience additional symptoms like sadness, feelings of irritability, and decreased energy.
Decreased pain tolerance
This means, everything hurts more. Does it ever feel like your nerves are on fire and yet you can’t find any physical reason for your pain? As it turns out, depression and pain often co-exist.
One 2015 study showed a correlation between people who are depressed and decreased pain tolerance, while another study in 2010 showed that pain has a greater impact on people who are depressed.
These two symptoms don’t have clear cause-and-effect relationship, but it’s important to evaluate them together, especially if your doctor recommends medication.
Some research suggestsTrusted Source that using anti-depressants may not only help relieve depression, but can also act as an analgesic, combatting pain.
Eye problems or decreasing vision
Do you find that the world looks blurry? While depression may cause the world to look grey and bleak, one 2010 research study in Germany suggests that this mental health concern may actually affect one’s eyesight.
In that study of 80 people, depressed individuals had difficulty seeing differences in black and white. Known by researchers as “contrast perception,” this might explain why depression can make the world look hazy.
Stomach pain or uneasiness in the abdomen
That sinking feeling in your stomach is one of the most recognizable signs of depression.
However, when your abdomen starts to cramp, it’s easy to write it off as gas or menstrual pain.
Pain that worsens, especially when stress arises, may be a sign of depression. In fact, Harvard Medical School researchers suggest that stomach discomfort like cramps, bloating, and nausea may be a sign of poor mental health.
What’s the link? According to those Harvard researchers, depression can cause (or be a result of) an inflamed digestive system, with pain that’s easily mistaken for illnesses like inflammatory bowel disease or irritable bowel syndrome.
Doctors and scientists sometimes refer to the gut as the “second brain,” because they have found a connection between gut health and mental well-being.
Our stomachs are full of good bacteria and if there’s an imbalance of good bacteria, symptoms of anxiety and depression may arise.
Eating a balanced diet and taking probiotics can improve one’s gut health, which may enhance mood, too, but further research is needed.
Pain is another way your brain communicates
If you feel discomfort identifying and talking about distressing emotions, like sadness, anger, and shame, this could cause feelings to manifest differently in the body.
If you’re experiencing any of these physical symptoms for a prolonged period of time, make an appointment with your primary care doctor or nurse practitioner.
According to the American Psychological Association, depression is one of the most common mental illnesses, affecting 14.8 million American adults each year.
Depression can be caused by a variety of factors, such as genetics, exposure to childhood stress or trauma, and brain chemistry.
People with depression often need professional help, like psychotherapy and medication, to fully recover.
So at your appointment, if you suspect these physical symptoms might be more than surface level, request to be screened for depression and anxiety. This way your healthcare provider can connect you with the help you need.
0 notes
Text
Fibromyalgia- Causes, Symptoms, Treatment
Fibromyalgia is a chronic condition which leads to pain in the muscle and bones, causes general fatigue, areas of tenderness and sleep disturbances. Fibromyalgia is difficult to diagnose as its symptoms are similar to that of other diseases. However, at the time of diagnosis, the focus is made on the musculoskeletal pain and severity of the pain.

Additional symptoms that help to diagnose the disease are nonrestorative sleep, headaches, depression, anxiety, trouble in focusing on one activity, pain in the lower belly, dry eyes and bladder problems. In case of fibromyalgia patients, it so happens that the brain and nerves tend to overreact to normal signals of pain. It happens due to chemical imbalance in the brain or due to ill functioning of the dorsal root ganglion which further affects the central pain sensitization. It also affects the emotions and energy level of the patient.
Earlier people were diagnosed with fibromyalgia by the pressing the areas of trigger points which causes extreme pain. Some of the common trigger points are back of the head, tops of the shoulders, upper chest, hips, knees and outer elbows. It was this pain which marked the start of this disease. In case of chest pain, the pain is similar to that of a heart attack. The pain centers in the cartilage that connects the ribs to the breastbone. The pain shall also extend upto shoulders and arms at times. It may even be difficult to catch your breath with such severe pain. In case of leg pain or back pain, a feeling of numbness or creepy crawling sensation is felt. The limbs of the leg shall be so heavy that it feels as if it held down by weights.
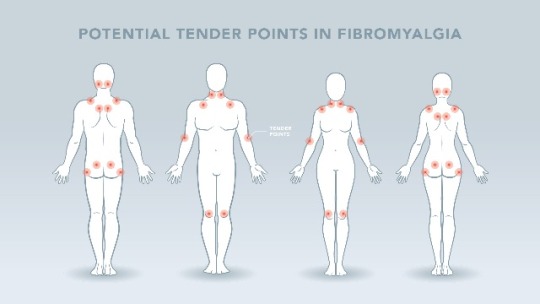
But it is difficult to diagnose what leads to such pain. It is believed that Fibromyalgia is felt due to genetic disposition, along with a set of triggers like infection, trauma and stress. Even a past illness can trigger fibromyalgia. It may also be a result of the genetic mutations that runs in a family. People who have the habit of taking excess stress or trauma can also leave a long lasting effect on the body.
Fibromyalgia diagnosis is done post 3 months after one has had pin on both sides of the body along with above and below the waist. Unfortunately, no lab test and X ray can detect this disease.
The current scenario is such that there are no specific medications for this disease. Thus, medications like
· Tramadol (Ultram)
Ibuprofen (Advil)
· Acetaminophen (Tylenol)
· Duloxetine(Cymbalta)
· Milnacipran HCL(Savella)
· Antiseizure drugs like Gabapentin(Neurontin)
· Pregabalin(Lyrica) are some of the FDA approved medicines that treat Fibromyalgia.
The medicines should be taken under the guidance of the doctors, which can then be bought from the nearest medical store or ordered from the best online medical app in India.
Natural remedies like physical therapy, acupuncture, 5-HTP, meditation, yoga, tai chi, exercise, massage therapy along with a balanced healthy diet are also recommended by the doctors for speedy recoveries. The doctor also suggests eating fruits and vegetables, whole grains, low fat dairy, lean protein, have plenty of water, reduce sugar intake and maintain a healthy weight.
Fibromyalgia is usually experienced in middle age. Thus, it is of utmost importance to take a continuous medication for proper cure and a healthy lifestyle. It is a chronic disease which requires a healthcare provider, therapist for the best outcomes. A healthy diet with regular exercise is what is required in order to avoid such complex diseases to be a part of our lives.
0 notes
Text
How Dangerous Is Sleep Deprivation?
Researchers aren't exactly sure how long people can do without rest. Lab researches discover rats die within 11-32 days of consistent wakefulness, even without a noticeable physiological cause.
Other research discovers relentless low-quality sleep is related to mortality. Some insomnia signs, especially difficulty initiating nonrestorative and asleep rest, are associated with a decently greater danger of death. One more research discovers older grownups that take control of 30 minutes to go to sleep have double the death risk of non-insomniac equivalents.
If sleep deprivation itself isn't creating death, is there a correlation? Yes.
Sleep apnea is a common condition that causes sleep starvation. If you're awakening in the evening gasping for air, or you feel frequently tired, you could be suffering from sleep apnea. Make sure to visit sleep centers in Tennessee for diagnosis.
0 notes
Text
Mechanical behavior of endocrowns fabricated with different CAD-CAM ceramic systems
The Journal of Prosthetic Dentistry
Available online 10 February 2020

Abstract
Statement of problem
The mechanical behavior of ceramic endocrowns is unclear.
Purpose
The purpose of this in vitro and 3-dimensional finite element analysis (3D-FEA) study was to evaluate the mechanical behavior of endodontically treated teeth restored with ceramic endocrowns made by using different computer-aided design and computer-aided manufacturing (CAD-CAM) systems.
Material and methods
Sixty mandibular human molars were endodontically treated, prepared for endocrowns, and divided into 4 groups (n=15) according to the following various ceramic systems: leucite-based glass ceramic (LC group), lithium disilicate-based glass ceramic (LD group), glass ceramic based on zirconia-reinforced lithium silicate (LSZ group), and monolithic zirconia (ZR group). After adhesive bonding, the specimens were subjected to thermomechanical loading and then to fracture resistance testing in a universal testing machine. The failure mode of the specimens was qualitatively evaluated. Three-dimensional FEA was performed to evaluate the stress distribution in each group. Data were analyzed by using a 1-way ANOVA and the Tukey HSD test (α=.05).
Results
Statistically significant differences among the groups were observed (P<.05). The outcomes of the LC, LD, and LSZ groups were similar (1178 N, 1935 N, and 1859 N) but different from those of the ZR group (6333 N). The LC and LD groups had a higher ratio of restorable failures, while LSZ and ZR had more nonrestorable failures. Fractographic analysis indicated a regular failure pattern in the ZR group and irregular failure patterns in the other groups. Three-dimensional FEA revealed similar values and stress pattern distributions among the groups.
Conclusions
The mechanical performance of monolithic zirconia was better than that of the other ceramic endocrowns considered in this research; however, monolithic zirconia presented a higher rate of catastrophic tooth structure failure.
0 notes
Text
Lupine Publishers | Apnea, Hypopnea and Their Individual Effects on Daytime Sleepiness and Sleep Quality

Lupine Publishers | Journal of Otolaryngology
Abstract
Background: Obstructive sleep apnea and hypopnea syndrome (OSA) is defined as a reduction or cessation of the airflow in the human airway. It effects nearly 18 million Americans and weight gain is the main predisposing factor. In this study, we aimed to investigate the effects of apnea and hypopnea individually.
Material and Methods: 83 participants were included in the study and they are divided into two groups as apnea predominant or hypopnea predominant. Pittsburg quality of sleep index (PQSI) and Epworth sleepiness scale (ESS) are completed for all subjects and full-night attended polysomnographic evaluations are done.
Results: ANOVA test was used to compare the inter-group variances. Between the two study groups, no statistical significance was reported between the PSQI or ESS scores.
Conclusion: The effects of apnea and hypopnea are similar on sleep quality or day-time sleepiness, however further studies also investigating the duration of the events as well are needed.
Abbreviations: OSA: Obstructive Sleep Apnea/Hypopnea Syndrome; PSG: Polysomnography; PSQI: Pittsburgh Sleep Quality Index; ESS: Epworth Sleepiness Scale.
Introduction
Obstructive sleep apnea and hypopnea syndrome (OSA) is reviewed under the sleep related breathing disorders. The diagnostic criteria must satisfy daytime sleepiness, fatigue or nonrestorative sleep, waking up with breath holding, gasping or choking, witnessed apnea periods and comorbidities such as hypertension, mood disorder, cognitive dysfunction, coronary artery disease or type 2 diabetes mellitus may accompany the disease. The full-night polisomnography (PSG) must demonstrate at least five obstructive respiratory events (apnea, hypopnea, respiratory effort related arousals) per hour of sleep (apnea/hypopnea index, AHI), but AHI below 15 needs the abovementioned signs for a complete diagnosis [1]. OSA may be seen in any age group, nevertheless published data from several countries indicate that OSA associated with daytime sleepiness occurs in 3% to 7% of adult men and 2% to 5% of adult women. However, because many individuals with OSA do not endorse daytime sleepiness, the prevalence of the disease is likely much higher [2]. The major predisposing factor for OSA is excess body weight. It has been estimated that nearly 60% of moderate to severe OSA is attributable to obesity. The risk of OSA increases as the degree of additional weight increases, with an extremely high prevalence of OSA in people with morbid obesity [3]. Several factors are implicated in the development of OSA [4].
The main cause addresses the reduction of the expansion forces of the dilator muscles of the upper airways. The capacity of the muscles decreases more during the REM sleep. Additional factors are excessive or elongated tissues of the soft palate, macroglossia, tonsillar hypertrophy, and a redundant pharyngeal mucosa [5]. OSA and comorbidities such as stroke, hypertension, metabolic syndrome, cardiovascular diseases or endocrinologic disorders are well taught in years, however the individual effects of apnea or hypopnea alone are never considered. To best of our knowledge, the published data does not mention which entity alone is more harmful to systemic functions or at least sleep, apnea or hypopnea? The Pittsburgh Sleep Quality Index (PSQI) is an effective instrument used to measure the quality of sleep in the adult. It differentiates “poor” from “good” sleep by measuring seven domains: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction over the last month. A global sum of “5” or greater indicates a “poor” sleeper [6]. The Epworth Sleepiness Scale (ESS) is a self-administered questionnaire with 8 questions. Respondents are asked to rate, on a 4-point scale, their usual chances of dozing off or falling asleep while engaged in eight different activities. The higher the ESS score, the higher that person’s daytime sleepiness and scores higher than 10 are significant. In this study, we compared apnea versus hypopnea due to the sleep quality and daytime sleepiness individually.
Materials and Methods
Between July 2017 and January 2019, 327 cases complaining of snoring, daytime sleepiness and witnessed sleep apnea periods were referred to full-night polisomnography. 150 cases were diagnosed as OSA were enrolled in the study. After the final assessment, a total number of 83 participants were chosen. The ethical committee approval was taken from Okmeydani Training and Research Hospital (48670771-514.10) and informed consent are taken from all participants.
PSG
3 Channel EEG (F4-M1, C4-M1, O2-M1), 2 channel EOG, chin, right and left tibialis anterior EMG, body position sensor, oro-nasal thermal sensor, nasal pressure sensor, thoracic and abdominal sensors, ECG, pulse-oximetry and synchronous video recordings and breath sound recordings were the parameters recorded through the night. The examination, sleep and wake periods and sleep related disorders were scored according to the criteria of the American Academy of Sleep Medicine [7].
Clinical Examination and Laboratory Tests
All participants underwent a detailed otolaryngologic examination including the fiberoptic naso-pharyngolaryngoscopy. Mueller maneuver was made to detect the pharyngeal collapse, vallecula epiglottica was visualized to assess the bulkiness, Friedmann Tongue Positions and Tonsil Gradings are made to determine the glossopharyngeal patency. Complete blood count and routine biochemical blood tests including the thyroid function tests were studied. PSQI and ESS were completed for each participant.
Study Design
In order to emphasize the individual effects of apnea or hypopnea, each PSG were examined and if apnea was higher than hypopnea by 50% or vice versa, that participant was included in the study. The study group, therefore, was divided into two as apnea predominant (AP) and hypopnea predominant (HP). Comorbid pulmonary or neurologic disorders, sleep disorders other that OSA (Central sleep apnea, Hypersomnolence, Parasomnias, Circadian rhythm disorders, etc.) were excluded. Also, pediatric population were not included in the study.
Statistical Analysis
A statistical analysis was performed using IBM SPSS Statistics 22 (IBM SPSS, Turkey). Continuous data was displayed as the mean ± standard deviation. Statistical significance was a p-value of greater than 0.05. A Shapiro–Wilk test showed the normal distribution of the parameters. ANOVA test was used to compare the normally distributed inter-group comparisons of the descriptive statistical methods (mean, standard deviation, and frequency) and the quantitative data.
Results
A total number of 83 participants aged between 24-64 years (mean 46±10 years) were studied. 61 were male (73.49%) and 22 were female (26.51%). The inter-group characteristics are shown in Table 1. The PSQI between AP and HP groups were not statistically significant (p=0.205). Similarly, ESS between AP and HP groups were also not statistically significant (p=0.240) (Figure 1).
Figure 1: AP versus HP by means of PSQI and ESS.
Table 1: Subject characteristics and statistical comparisons.
ANOVA test showed no statistical significance among variances.
OSA is defined as the reduction or cessation of airflow for at least ten seconds. The entity is almost every time in association with snoring, and between the snores, airflow may stop completely (apnea) or reduction in the airflow (hypopnea) may happen. If there is a body effort to breathe, the disease is termed obstructive, otherwise it is central. In the presence of a collapsible airway, sleepinduced loss of tonic input to the upper airway dilator muscle motor neurons allows the pharyngeal airway to collapse [8]. The general reaction to this airway obstruction is arousal; sleep then resumes, leading to repeated cycling of sleep, intermittent hypoxia, and arousal throughout the night. Neurocognitive effects of OSA include daytime sleepiness and impaired memory and concentration; cognitive impairment and neural injury may develop in association with sleep apnea [9,10]. Sleep-disordered breathing and OSA are not reported frequently in animals but a natural animal model
Discussion
OSA is defined as the reduction or cessation of airflow for at least ten seconds. The entity is almost every time in association with snoring, and between the snores, airflow may stop completely (apnea) or reduction in the airflow (hypopnea) may happen. If there is a body effort to breathe, the disease is termed obstructive, otherwise it is central. In the presence of a collapsible airway, sleepinduced loss of tonic input to the upper airway dilator muscle motor neurons allows the pharyngeal airway to collapse [8]. The general reaction to this airway obstruction is arousal; sleep then resumes, leading to repeated cycling of sleep, intermittent hypoxia, and arousal throughout the night. Neurocognitive effects of OSA include daytime sleepiness and impaired memory and concentration; cognitive impairment and neural injury may develop in association with sleep apnea [9,10]. Sleep-disordered breathing and OSA are not reported frequently in animals but a natural animal model of OSA is English bulldogs, which have been used to study upper airway anatomy and physiology and the pharmacologic treatment of OSA. English bulldogs have an enlarged soft palate and narrow oropharynx and display many of the clinical features of OSA, including snoring, sleep-disordered breathing, oxyhemoglobin desaturation during sleep, frequent arousal from sleep, and hypersomnolence with shortened sleep latencies [11]. OSA in English bulldogs is not related to obesity, as it often is in humans. OSA has been modeled in a variety of species by using surgical tracheostomy and subsequent intermittent occlusion of the endotracheal tube [12]. Schoorlemmer et al. [13] produced obstructive apnea in conscious rats by using an inflatable balloon implanted in the trachea and apneic episodes of as long as 16 s in duration could be created during sleep. However, animal models of intermittent hypoxemia have several drawbacks. In many cases, the models mimic severe human OSA and may be less applicable to most clinical OSA. In addition, animals exposed to intermittent hypoxemia develop hypocapnia, whereas human OSA is characterized by hypercapnia. Furthermore, human OSA typically is associated with obesity, which is not always considered in animal studies. In addition, OSA causes sleep fragmentation, which may have independent effects on metabolism. Thus, exposure of animals to intermittent hypoxemia produces repeated arousals and changes in sleep architecture that are comparable to those in clinical OSA, yet the effects may not be persistent, limiting their use for studying long-term metabolic consequences of OSA [14].
Animal models are troublesome to study the long-term effects of sleep fragmentation. The sleep quality is a bio-psycho-social parameter that may never be evaluated in animal models; for example, as we refer to excessive daytime sleepiness, the subject is asked whether the sleepiness occurs in the passive state such as resting periods or during the active periods such as work-time or social interactions. Moreover, the sleep architecture, ultradian rhythm or sleep quality may not be assessed in animal models. In our study, the effects of apnea or hypopnea on sleep quality or daytime sleepiness did not differ. This might have several reasons; first of all, all PSG were done elsewhere, our otolaryngology clinic is not capable to perform full-night attended PSG. This situation has some major drawbacks; it is impossible to mark each breath disorders epoch by epoch on the screen of the test computer, but we rather have a brief report of the night. This makes it impossible to calculate the duration of the respiratory events. Therefore, we only could compare the nature of the events by their scores or numbers (Table 1). Secondly, there are some other factors that may interfere with the sleep architecture such as drops in the oxygen levels; not every subject has the same decreasement in their oxyhemoglobine when they have the same level and duration of airway collapse. Thirdly, limb movements also disrupt the sleep quality and impede normal daytime cognitive functions. Finally, arousals are another issue to study; if OSA is recently developed in the subject, the peripheric chemoreceptors detecting the airflow cessation are more sensitive and arousal happens imminently, if the disease is longer the receptors may become insensitive that happens in sleep continuity despite the airflow cessation. Nonetheless, to best of our knowledge, there is no other study that tried to investigate the effects of apnea of hypopnea individually on sleep quality or daytime sleepiness.
Conclusion
The effects of apnea and hypopnea are similar on sleep quality or daytime sleepiness, however further studies also investigating the duration of the events as well are needed.
For more Lupine Publishers Open Access Journals Please visit our website: h
https://lupinepublishersgroup.com/
For more Journal of Otolaryngology-ENT Research articles Please Click Here:
https://lupinepublishers.com/otolaryngology-journal/
To Know More About Open Access Publishers Please Click on Lupine Publishers
#Lupine Publishers#Lupine Publishers Group#Lupine Publishers Indexing Sites#Journal of Otolaryngology#ENT Research Journal
0 notes
Text
November 2019
The AASM Case Study of the Month for November 2019 involves a a patient with jaw pain, headaches, snoring and nonrestorative sleep.
from Google Alert - sleep apnea https://ift.tt/2XjiGOn
0 notes