#pathognomonic
Text
Concurso playeras mojadas
Daddy fuck me with his big uncut cock
Bdsm gay digs his fist into tight ass
Alguien de TULTEPEC o CUAUTITLAN
Asian big tits wife gangbanged infront of husband brutally
Sucking dick while her nigga outside the door
Lascivious twink Zack Randall practices self sucking in solo
BEST DEEP NAVEL VOYUER VIDEO
I will show you the secret to having the hardest orgasm JOI
Anal casero con orgasmo
#Gta#mammillaplasty#discouraged#law-breaker#McComb#nonecclesiastical#bargainee#viviparism#associator's#avertible#tomjohn#lumbo-inguinal#marquessate#firmance#pathognomonical#phylogenesis#substantiallying#nimble-wittedness#recalled#diaphyseal
0 notes
Text
Old man young hairy girl Frannkie And The Gang Tag Team A Door To
Ugly bitch sucks BBC
novinha morena dancando de calcinha
Busty Teen TS Stroking Her Cock While Showing Her Fuckable Ass
Double lesbian foot worship
Boy teen gay porn nude At this point he has stopped seeing the vid
Ma chienne en action
مره شمال هايجه اوى ببزاز ملبن مع عشيقها تمص الزبر بمزاج و تتموحن وبعدها تتناك وتكيف كسها الحيحان
EvilAngel - Kira Noir Gets Ass Plowed By Owen Grey
EVASIVE ANGLES Big Boobie Teen Babysitter with Sabrina Taylor
#associator's#avertible#tomjohn#lumbo-inguinal#marquessate#firmance#pathognomonical#phylogenesis#substantiallying#nimble-wittedness#recalled#diaphyseal#Capri#Jhansi#Tates#cooked#well-penned#Elba#yellow-labeled#Loeffler
0 notes
Text
Brincadeira amadora
Hottie Keisha Grey Straddles BF In A Camping Tent
Three Young German Girls Masturbation on Cam Together
Venezolana de increible cuerpo hace baile frente a su webcam
Real femboi amateur strips and masturbates
Mass Effect VR Peebee fuck
Amateur slavery with hot girls
asian girl pounded by black dick
Bouncing Boobs Ultimate Slut
Philippine girlfriend love anal sex
#OTR#phelonions#intermede#SABME#Gta#mammillaplasty#discouraged#law-breaker#McComb#nonecclesiastical#bargainee#viviparism#associator's#avertible#tomjohn#lumbo-inguinal#marquessate#firmance#pathognomonical#phylogenesis
1 note
·
View note
Text
Protonmail email address = pathognomonic sign hes quirked up
4 notes
·
View notes
Text
Here's a rule of thumb for infant head circumference: it should be ~35 cm at birth, ~40 cm at 3 months, ~45 cm at 9 months, ~50 cm at 3 years, and ~55 cm at 9 years.
In Rett Syndrome (RTT), most growth parameters diminish, often to below the 2nd%ile: first OFC (1 mo), next weight (6 mo), then length (17 mo). Of these, microcephaly is most pathognomonic and reflects slowed brain growth. ~1/2 have preserved body size, and mean BMI is similar to unaffected children. Yet pubertal growth spurts are rare.
Dr. Dana Cummings (Children's Hospital of Pittsburgh Neurology) and https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3468773/
2 notes
·
View notes
Text
In the general population as a whole (ie, not just those who are sleepy), the presence or absence of SOREMPs on repeated MSLTs is also quite variable, suggesting that this may not be the best feature to use in discriminating among diseases. Indeed, prominent narcolepsy researchers have concluded that the presence of 2 or more sleep-onset REM periods [eg, on the MSLT] does not appear to have any specific pathognomonic significance.
THATS WHAT IM FUCKING SAYINGGGG, THE MSLT IS A BAD TEST!!!
#tag ramble incoming#so xywav was recently approved as a treatment for idiopathic hypersomnia#and i am hoping that is a step in the direction of like#further differentiating type 1 and 2 narcolepsy#and taking ih more seriously#i don't know enough to actually theorize that t2n and ih are the same disorder but the page this quote is from (the hypersomnia foundation)#lists several areas of overlap in everything from symptoms to brain chemicals#whereas like!!! t1n and t2n have the massive difference of cataplexy vs no cataplexy#and from what i can tell hypocretin deficiency vs no hypocretin deficiency#anyway sorry what i am hoping for is that we're moving towards a point where t1n can be diagnosed#based on cataplexy and/or hypocretin levels (bc cataplexy isnt always severe enough to be observed)#and t2n and ih can be diagnosed based on other symptoms#with effective treatments available for all three diagnoses so getting the wrong one doesnt fuck you over forever#and no one has to take the goddamn mslt
16 notes
·
View notes
Text
Medical vocab of the day:
“Pathognomonic”,
From the Greek “pathos,” meaning “suffering, disease”
And the Spanish “gnomos,” meaning “gnomes”
4 notes
·
View notes
Text
Diffuse ST segment elevations = pericarditis. PR segment depression is pathognomonic
4 notes
·
View notes
Text
Lupine Publishers|To Compare the Retinal and Choroidal Thickness in Fuchs Uveitis Syndrome Patients with Healthy Controls Using Optical Coherence Tomography Seen at Tertiary Care Center
To Compare the Retinal and Choroidal Thickness in Fuchs Uveitis Syndrome Patients with Healthy Controls Using Optical Coherence Tomography Seen at Tertiary Care Center

Abstract
Purpose: To compare the retinal and choroidal thickness in Fuchs Uveitis Syndrome patients with healthy controls using optical coherence tomography seen at tertiary care center.
Method: 16 patients with unilateral Fuchs Uveitis Syndrome (FUS) and 20 healthy control subjects were enrolled in this retrospective study. Spectral domain optical coherence tomography was used to measure the central foveal thickness (CFT), retinal nerve fiber layer (RNFL) thickness and sub foveal choroidal thickness (SFCT) of the eyes with FUS and compared with the unaffected fellow eye and healthy controls.
Results: The mean age of the patients was 35.2 ± 8 years. Seven patients (60%) were male, and nine (40%) were female. Diffuse stellate keratic precipitates (KPs) were seen in all patients. Mild anterior chamber reaction was noted 62.5%. Heterochromia was observed in 87.5% of the eyes, cataract in 43.8% of the eyes, and vitreous cells and debris in 37.5% of the eyes. The mean CFT was (249.7 ± 27.4𝜇m) in affected eyes, (251.5± 23.1 𝜇m) in unaffected eyes of FUS and (253.3 ± 29.2 𝜇m) in healthy control which were statistically insignificant on comparison (𝑝 value > 0.05). The mean SFCT was significantly thinner in eyes with FUS (272.47 ± 13.12 μm) than in the fellow eyes without FUS (316.37 ± 16.13 μm; p = 0.04). and control (320.27 ± 18.15). The average RNFL thickness was found to be (106 ± 14.2 μm) in eyes with FUS, (108 ± 16.5μm) in eyes without FUS and (112 ±13.8μm) in healthy control which were statistically not significant (p value > 0.05).
Conclusion: We conclude that affected eyes in patients with FUS tend to have thinner choroids as compared to unaffected fellow eyes which is consistent with previous studies. It might be associated with chronic inflammation induced choroidal is chaemic changes. Future studies using swept source OCT will further improve precision to get choroid findings more accurate.
Keywords:Choroid; Fuchs Uveitis Syndrome; SD-OCT; Retinal Nerve Fiber Layer
Introduction
Fuchs’ uveitis syndrome (FUS) is an intraocular inflammatory condition that involves anterior segment, lens, vitreous humor and optic disc. It accounts for 2-11% of all uveitis cases [1]. Although many genetic, immunological, vascular and sympathetic theories have been proposed, recent studies show evidence of rubella or herpes simplex virus, toxoplasma association in some cases of FUS [2]. It is a frequently unilateral and typical age at presentation is 30-40 years [3,4]. The diagnostic criteria include stellate keratic precipitates (KPs) scattered diffusely all over cornea, chronic lowgrade anterior chamber reactions, iris atrophy with or without heterochromia, absence of posterior synechiae, vitreous opacities and macular edema [5]. It affects both genders equally and the prognosis is usually good [6]. Iris atrophy and heterochromia are due to atrophy and depigmentation of all iris layers, although it is not pathognomonic. Recently, fluorescein angiography (FA) had provided better information about the posterior segment involvement in FUS [7-9]. Optical Coherent Tomography (OCT) is a routinely employed noninvasive tool in detecting most posterior pole retinal abnormalities. The Enhanced Depth Imaging (EDI) in spectral domain (SD) OCT and swept source (SS) OCT allow visualizing the choroid more accurately [10,11]. Some studies documented the changes in choroidal thickness using EDI-OCT in uveitic conditions, such as Vogt–Koyanagi–Harada (VKH) disease, Behçet disease (BD), ocular sarcoidosis providing remarkable information about disease activity [12,13]. The natural course of the disease is slow to progress, without substantial reduction of visual acuity until significant vitreous opacities or cataract develop. FUS is often misdiagnosed or diagnosed delay leading to posterior subcapsular opacity and elevated IOP mainly due to long-term corticosteroid therapy. There are very few reports in the literature comparing macular, RNFL and choroidal thickness in FUS patients. The purpose of the current study was to measure central foveal thickness (CFT), subfoveal choroidal thickness (SFCT) and retinal nerve fiber layer (RNFL) thickness, in patients with FUS and to compare these with the unaffected fellow eyes and the age, sex and refractive equivalent-matched healthy controls. To the best of our knowledge, it is the first comparative study to evaluate SFCT and other parameters in FUS using spectral domain SD-OCT on FUS from central India.
Material and Methods
This retrospective study was conducted at a tertiary care center from central India. The medical records of 16 patients with FUS and 20 healthy controls between september 2018 and august 2021 were reviewed. Data including age, sex, ocular and medical history, ophthalmic examination, laboratory work-up and OCT parameters were retrieved from patient record. Aii patients had best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, Goldmann applanation tonometry and dilated fundoscopy. The inclusion criteria were diagnosed unilateral FUS based on clinical findings and fundus sufficient for its visualization on clinical examination. Bilateral FUS, history of previous ocular surgery, eyes with dense cataract or media opacity obscuring the visualization of choroid, presence of a coexisting ocular or systemic disease and use of any topical or systemic medications. were excluded from study. The control group consisted of age-, sex-, and refractive equivalent-matched healthy controls who visited ophthalmology clinic for routine examination. The laboratory investigations included complete blood counts, angiotensin converting enzyme, mantoux test and venereal disease research laboratory tests etc. To exclude other causes of anterior or intermediate uveitis. The CFT and RNFL thickness of eyes with FUS were evaluated with SD-OCT and compared with the unaffected fellow eyes and healthy controls. The EDI mode was used to evaluate SFCT. SFCT was defined as the vertical distance from the outermost hyperreflective line of the retinal pigment epithelium (RPE) to choroid-sclera junction under the center of the fovea and was measured using the calipers available within the software. The RNFL thickness (from the inner margin of the internal limiting membrane to the outer margin of the RNFL layer) was automatically segmented using software version. Average RNFL was used for analysis. Statistical analyses were performed with R version 4.0.5. Data were recorded as the mean ± standard deviation (SD). Quantitative data was analyzed using one way analysis of variance (ANOVA) test. An independent 𝑡-test and Chi-square test were used to compare variables between patients with FUS and healthy control subjects. A value of 𝑝< 0.05 was considered to be statistically significant for all analyses.
Results
16 patients with FUS (9 females and 7 males) and 20 healthy control subjects (11 females and 9 males) were included for analysis in this study. The mean age of FUS patients was 35.2±8 years, while it was 38.4± 6years for controls, which was statistically insignificant (𝑝>0.05) (Table 1). Gender differences in both groups were also statistically insignificant (𝑝>0.05). Blurred vision and floaters were the most frequent presenting symptoms {5 patients, (31.3%) and 4 patients (25%) respectively}. Other symptoms included red eye (1 patient, 6.3%), photophobia (1 patient, 6.3%). Three patients were asymptomatic (18.75%), and the diagnosed during a routine eye examination (Table 2). Iris atrophy was present in 5 patients. Heterochromia was present in 14 patients. Cataract was present in 7 patients. Stellate keratic precipitates were noted in all patients. Mild anterior chamber reactions were seen in 10 patients. Vitreous cells or debris were observed in 6 patients (Table 3). The cause of visual impairment was cataract in all cases. The central foveal thickness was 249.7±27.4𝜇m in the affected eyes, 251.5±23.1 𝜇m in the unaffected eyes of FUS patients, and 253.3±29.2 𝜇m in control subjects. There were no significant differences in central foveal thickness between the affected and unaffected eyes of FUS patients (𝑝 = 0.93) or between the affected eyes of FUS patients and the eyes of control subjects (𝑝 = 0.9). The mean SFCT was found to be 272.47 ± 13.12μm in eyes with FUS and 316.37± 16.13μm in eyes without FUS (p = 0.04) and 320.27 ± 18.15𝜇m in the eyes of healthy control subjects. There was choroidal thinning at fovea in the affected eyes of FUS patients compared with the unaffected eyes or control subjects, Average RNFL thickness was 106 ±14.2𝜇m in the affected eyes of FUS patients, 108±16.5𝜇min the unaffected eyes of FUS patients, and 112 ± 13.8𝜇m in the eyes of healthy control subjects (Table 4). No significant differences in RNFL thickness were observed between the affected and unaffected eyes of FUS patients (𝑝 = 0.92) or between the affected eyes of FUS patients and the eyes of control subjects (𝑝 = 0.76)
Table 1: Demographic analysis.
Table 2: Presenting symptoms.
Table 3: Characteristic of FUS patients.
Table 4: Thickness of fovea, sub foveal choroid, and RNFL in FUS & control.
Discussion
To our knowledge, very few comparative studies on FUS patients have been done till yet. In the present study, we compared central foveal thickness, retinal nerve fiber layer and subfoveal choroidal thickness between the affected eyes, the unaffected eyes of FUS patients and healthy controls from central India. Although we found choroidal thinning at fovea in the affected eyes of FUS patients compared with the unaffected eyes of FUS patients or control subjects, there was no statistically significant difference in RNFL and central foveal thickness. FUS was first described in 1906, recent studies have focused on various viral agents and the etiology of FUS remains controversial. In FUS, persistence of chronic lowgrade inflammation for years leads to various degrees of atrophy of the iris and ciliary body. As the choroid being more vulnerable to the effects of the inflammatory and vascular diseases than other tissues, imaging of choroid is important for understanding the pathophysiology of various diseases. EDI mode using SD-OCT devices enables cross-sectional, high resolution better visualization of the choroid. Many studies have documented the effect of various acute and chronic ocular inflammatory conditions on choroidal abnormalities. Nakayama et al. showed that choroidal thickness as a marker for the degree of choroidal inflammation in acute Vogt- Koyanagi-Harada disease using EDI-OCT [14]. Kim et al. found an increase in subfoveal choroidal thickness in the acute phase of Behcet’s posterior uveitis [15]. Multiple studies suggest that increased blood flow and choroidal effusion is the mechanism responsible for choroidal thickening in acute inflammation [16,17]. However, Coskun et al. observed the thinning of subfoveal choroid in chronic Behcet’sassociated posterior uveitis probably due to chronic inflammation induced fibrosis [18]. Very few studies from Turkey and Italy like Balci and Ozsutsus, Kardes et al. and Carquaglia et al. showed the comparison between the affected and fellow eye in FUS patients [19-21] (Table 5). The study by Kardes et al. had findings consistent with the study of Balci and Ozsutsus. We propose that chronic anterior chamber and vitreous inflammation in eyes with FUS may affect choroidal perfusion, which may result in ischaemic changes leading to atrophy and fibrosis of the choroid tissue, thereby reducing choroidal thickness. Limitations of our study is being retrospective nature and small sample size. We have used SD OCT in this study and with advent of new imaging methods designed specifically for the choroid, SS OCT which allows examination of the choriocapillaris, and larger choroidal vessels more clearly can further improve precision to determine the inner and outer boundaries of the choroid findings in the future. To conclude, we found subfoveal thinner choroid in FUS as compared to uninvolved fellow eyes, but we could not find a statistically significant comparison of foveal and RNFL thickness in FUS versus unaffected eye. Our findings are also consistent with those of previous studies. As this is the first analysis of its kind from central India, longitudinal studies with large sample size would help in more understanding of the effect of chronic inflammation on the choroid in FUS in future.
Table 5: Comparison between different studies of mean sub foveal choroidal thickness (SFCT).
For more information about Trends in Ophthalmology Open Access Journal archive page click on below link
https://lupinepublishers.com/ophthalmology-journal/archive.php
For more information about lupine publishers page click on below link
https://lupinepublishers.com/index.php
#lupine publishers#lupine publishers group#lupine publishers LLC#trends in ophthalmology open access journal#tooaj
2 notes
·
View notes
Text
Malakoplakie of the ovary: Case report and litterature review
Introduction
Malakoplakie, also known as malakoplasia [1], is an inflammatory granulomatous disease induced by defective phagocytic macrophagic activity. It usually affects the whole body, but the genitourinary tract in about 75% of reported cases. Other organs such as the gastrointestinal tract, thyroid, pancreas, liver, brain, lymph nodes, adrenals, skin, bones, backpertis and ovary are less common. It represents a deficit in the macrophagic digestion of bacteria, but its precise pathogenesis is not yet clear [1]. Its treatment is essentially based on antibiotic therapy [2]. We report a malakoplakie observation in order to expose the difficulties associated with its management in a resource-limited environment.
Clinical case
This was a 41-year-old patient who had been admitted to the emergency room for pelvic pain for a month and was operating in a febrile setting. The accompanying signs were digestive type made of diarrhea and vomiting. No urinary symptoms were found. Clinical examination showed a patient with an alteration of the general condition, a hyperthermia at 39 degrees, a painful swelling of the left iliac pit with abdominal defense located in left iliac pit. Biology had shown hyper leucocytosis at 15,000/mm3 predominantly polynuclear neutrophils associated with anemia at 5g/dL. The abdominal ultrasound had been objectified: a localized abscess in the pelvis with bilateral pyelolo-calicial dilation without visible barrier, right and left inguinal adenopathies without obvious compression, and medium-abundance ascite. The surgical indication retained; the patient benefited from an exploratory laparotomy that found a voluminous peritoneal abscess at the expense of the left ovary. A wash of the peritoneal cavity associated with a left oophorectomy was performed. Cytobacteriological examination of abscess fluid had isolated gram-negative bacillus such as Escherichia coli. Cytobacteriological examination of the urine was sterile. The surgical suites were simple with apyrexia and an amendment of abdominal pain under double probabilistic antibiotic therapy. The patient was discharged on the 6th day post-operative.
Anatomopathological examination one month after the operation of the exeresis was found: ovarian tissue with large outbreaks of inflammation, in which histiocytes predated and lymphocytes were found in smaller quantities. In the cytoplasms of macrophages, there were bodies of Michaelis-Gutmann, pathognomonic of malakoplakie (Figures 1,2).
0 notes
Link
The classical symptoms of PD are characterized by progressive motor dysfunction, including rest tremor, bradykinesia, rigidity, and postural instability, which is noticeable when there is already 60% dopaminergic neuronal loss in the substantia nigra.
In addition to motor symptoms, non-motor manifestations such as rapid eye movement sleep behavior disorder (RBD), gastrointestinal dysfunction, olfactory disruption, neuropsychiatric symptoms, and sensory dysfunction also exist in patients with PD and compromise their quality of life.5 Of note, these non-motor PD symptoms can occur years before the onset of classical motor symptoms.6 Thus, they are therefore now considered prodromal clinical markers before the onset of the classical motor manifestations, according to the International Movement Disorders Society.7 Among these prodromal symptoms, constipation is the most prevalent and earliest pre-motor feature and can precede motor symptoms by decades.
The pathological hallmark of PD is progressive dopaminergic neuronal degeneration and intraneuronal accumulations of misfolded α-synuclein (Lewy bodies) in the substantia nigra.3 The pathological α-synuclein can transmit from cell to cell in a prion-like fashion to promote the neurodegenerative process of this disease.9,10 Recent postmortem evidence indicates that Lewy body pathology is first detectable outside the brain, starting from neurons in the gut enteric nervous system (ENS) and olfactory bulbs.11 These neuropathology observations are consistent with the findings that non-motor symptoms of PD, especially constipation, can precede the onset of motor symptoms.8 Further in vivo PD animal model studies demonstrated that pathological forms of α-synuclein, after injection into the intestinal wall, can be transported from the gut to the brain via the vagus nerve, reaching the dorsal motor nucleus of the vagus nerve in the brainstem.12, 13, 14 However, although this pathology finding has given rise to the idea that PD pathology originates in the peripheral ENS and then invades the brain via retrograde axonal transport through the vagus nerve, a small fraction of patients do not show pathology in the ENS. In about one-third of patients, the PD neuropathology begins in the brain itself and then travels downward.15 Hence, it is hypothesized that PD can be divided into a gut-first (body first) and a brain-first subtype.15 The former is tightly associated with chronic constipation and RBD during the prodromal phase and the latter is most often sparing of gastrointestinal symptoms and is RBD-negative during the prodromal phase. These findings reinforce the concept that PD is a heterogeneous disorder with diverse initial triggers and propagation trajectories of α-synuclein, suggesting that tailored disease-modifying therapy is needed for patients with different subtypes.
The various recently observed gut microenvironmental changes in the early stages of the disease may play a vital role in PD, especially those with the body-first subtype of the disease. Patients whose disease begins in the gut may benefit most from interventions that target the gut. In this review, we summarize recent evidence for altered gut microenvironments contributing to PD through the gut–brain axis. Furthermore, there is a plethora of evidence, including our previous study, for altered gut microbiota in patients with PD compared with unaffected controls.
There is much evidence that the vagus nerve transports α-synuclein from the gut to the brain.12 Pathological α-synuclein fibrils injected into the duodenum can move from the muscular layer of the duodenum to the brain and then from neuron to neuron across the synapses through the vagus nerve in a PD animal model.12 Furthermore, recent evidence indicates that protein nucleation and aggregation may be influenced by E. coli's secretion of curli, which induces neuronal deposition of α-synuclein in the ENS.29,31 The abundance of E. coli at the colonic mucosa correlates with enteric α-synuclein deposition in PD patients.
A plethora of studies have investigated changes in the gut microbiota in patients with PD compared with healthy controls using either 16 S rRNA gene amplicon surveys or shotgun metagenomic sequencing analysis.35, 36, 37, 38, 39, 40, 41, 42 Meta-analyses have shown that the relative abundance of various phyla of anti-inflammatory and short-chain fatty acid (SCFA)-producing bacteria, including Blautia, Coprococcus, Roseburia, Lachnospira, Fusicatenibacter, and Faecalibacterium, are reduced in PD patients compared with controls. In contrast, the amounts of Lactobacillus, Bifidobacterium, and Akkermansia are higher in PD patients than in unaffected participants from different ethnicities.38, 39, 40, 41 Notably, opportunistic pathogens and pro-inflammatory bacteria at the phylum level, including Corynebacterium, Porphyromonas, Alistipes, Bacteroides, Escherichia, and Megasphaera, are also enriched in PD.40,43 In metagenomic research, gene markers from the gut microbiome were found to accurately discriminate PD patients from healthy controls, with most of the identified markers belonging to Bacteroides and Escherichia species.44 Although PD medications affect the structure of the gut microbiota, these changes are detectable in drug-naïve early-stage PD patients.36,43,45
Changes in the gut microbiota also correlate with disease progression in PD. A decrease in the SCFA-producing microbiota and increase in pro-inflammatory bacteria correlate with motor and cognitive severity in patients with PD.38,40,46 Compared with transplantation of fecal gut microbiota from healthy donors, such transplantation from PD patients leads to worsened motor symptoms in a transgenic rodent model of PD.47 A 3-year longitudinal follow-up study of PD patients revealed that a reduced amount of Roseburia species predicted faster progression of both motor and non-motor symptoms of PD.48 A lower abundance of SCFA-producing bacteria, including Fusicatenibacter and Faecalibacterium, correlates with elevated fecal inflammatory calprotectin levels in PD patients.49 Furthermore, enrichment in Bacteroides and Bifidobacterium has been linked to elevated expression of systemic and fecal inflammatory markers IFN-γ, TNF-α, and neutrophil gelatinase-associated lipocalin in patients with PD.42,50 The increased levels of Lactobacillaceae and Bifidobacteriaceae in PD patients require further investigation, as they are usually recognized as probiotics for improving constipation.51 Therefore, distinct gut microbiota species promote enteric α-synuclein aggregation or gut inflammation to facilitate the occurrence and progression of PD.
The composition of gut microbiota also influences the pharmaceutical treatment responses in PD patients. The growing literature has shown the role of the gut microbiome in the pharmacokinetics of prescription drugs and the effects that the drugs can have in turn on the composition of the gut microbiome,52,53 indicating a potential interaction between PD medications and the microbiome. Prior studies have shown that anti-PD medications, including catechol-O-methyl transferase (COMT) inhibitors and anticholinergics, have gastrointestinal side effects, which may be related to the changes of the gut microbiome.54,55 Furthermore, bacterial tyrosine decarboxylase, which can convert levodopa to dopamine, could limit its bioavailability and may contribute to the interindividual responses to levodopa treatment among patients with PD.56,57 Enterococcus faecalis was found to be the dominant microorganism responsible for levodopa decarboxylation and restrict levels of levodopa in the treatment of PD.57 Dopamine produced by gut bacterial metabolism of levodopa decarboxylation can also impair intestinal motility, which could provide an explanation for bacterial overgrowth in the small intestine associated with motor fluctuation in PD.58 These observations lend support to the notion that the composition of the gut microbiome may affect the treatment efficacy and potential side effects of levodopa treatment in patients with PD.
Srivastav et al. treated animals with an oral probiotic mixture containing Lactobacillus rhamnosus GG, Bifidobacterium animalis lactis, and Lactobacillus acidophilus for 30 days, after which the mice were given MPTP injections.62 The results showed that mice receiving this probiotic mixture reduced dopaminergic neurodegeneration by upregulating neurotrophic factors and increasing striatal neuronal responses to dopamine.62 Using the same toxin-induced PD model, Liao et al. fed mice with Lacobacillus plantarum PS128 for 28 days, then gave them MPTP injections for 4 days. The results showed that feeding with Lacobacillus plantarum PS128 mitigated neuronal degeneration, attenuated oxidative stress and neuroinflammation, and rescued the locomotor defects of MPTP-injected PD mice.63 Sun et al. treated MPTP-injected mice with the probiotic Clostridium butyricum for 4 weeks and demonstrated improved motor deficits, attenuated dopaminergic neuron loss, improved synaptic dysfunction, and reduced microglia activation in the treated mice.64 This beneficial effect was associated with increased colonic levels of glucagon-like peptide-1 (GLP-1), colonic G protein–coupled receptors GPR41/43, and other components of the cerebral GLP-1 receptor pathway.57 Of note, the incretin hormone GLP-1 was recently found to regulate neurogenesis and synaptic plasticity,65 and GLP-1 agonists may be neuroprotective in PD pathogenesis.66 Similarly, a 3-week treatment with Lactobacillus fermentum U-21 reduced nigra dopaminergic cell loss in a paraquat-toxin model of PD.67
Several studies have demonstrated the potential benefits of probiotic supplementation in patients with PD. A total of seven clinical trials were identified, which were all randomized clinical trials68, 69, 70, 71, 72, 73, 74 (Table 1). Consumption of fermented milk containing multiple probiotic strains can improve constipation in patients with PD.62 Similar beneficial effects in improving bowel movements were also noted in PD patients in most of the probiotic clinical trials.51,73 Evidence seems to demonstrate that probiotic intake can improve bowel movement and reduce gastrointestinal symptoms. There are two studies measuring non-gastrointestinal symptoms of PD as one of the primary outcomes of probiotic clinical trials.71,74 Probiotic supplementation containing Bifidobacterium bifidum, L. acidophilus, L. fermentum and Lactobacillus reuteri for a period of 12 weeks has been observed to improve some symptoms in PD patients as measured by total MDS-UPDRS scores.71
One recent open-label clinical trial with 87 participants showed improvement of non-motor symptom scores, reduced fecal inflammatory marker of calprotectin and increased fecal butyrate in patients with PD who received prebiotic supplement with resistant starch compared to those without prebiotic intervention.78 Several in vivo studies have shown that lower abundance of SCFAs butyrate-producing bacteria could be corrected by the administration of prebiotic fibers, which in turn reduce the gut inflammatory processes, improve gut barrier function, and peristalsis.79,80 SCFAs have a key role in modulating the cross-talks in the gut–brain axis through modulating the gut barrier and blood–brain barrier integrity, inflammatory processes, inhibition of histone deacetylase to promote neuronal survival.81 Of note, an in vivo study using a transgenic a-synuclein–expressing mouse model demonstrated that a germ-free environment eliminates PD phenotypes but that oral feeding with SCFAs remerged the disease-related neuropathology by microglial activation.82 As the effects of SCFAs may depend on the concentration and the different subtypes, the effect of SCFAs in the PD process requires more studies.
0 notes
Text
Review strengthens evidence that repetitive head impacts can cause CTE
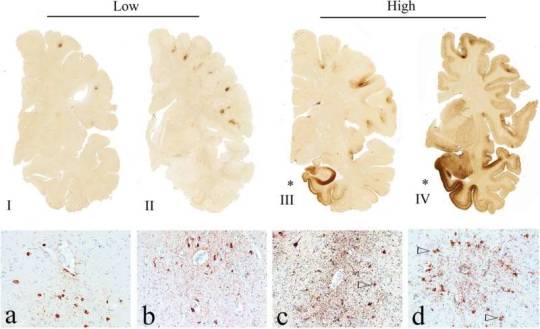
The pathognomonic lesion of CTE and the staging schemes of pathological severity (adapted with permission from [83]). Representative images of p-tau pathology at Low and High chronic traumatic encephalopathy (CTE) pathological stage using the abbreviated staging scheme recommended by the second NINDS/NIBIB consensus panel (low–high) [11] and the McKee staging scheme (I–IV) [4, 79]. Low CTE is…
View On WordPress
0 notes
Text
Why Do Women Visit a Gynecologist?
What usually brings a woman to the gynecologist or to her doctor is because she probably has symptoms, or she has concerns. I should say more often concerns than symptoms. There are various symptoms of ovarian cysts, and I'm going to bunch these symptoms - I'm going to just list them, and then talk about why they are not necessarily pathognomonic, basically why they don't indicate that there's really, truly a problem. Because they're vague symptoms.
Number one obviously is pain or pressure in the abdomen, sometimes an intermittent ache in the lower back or thighs. That's a common complaint. And of course these pain and pressure and intermittent aches can be from a lot of things. But obviously pelvic pain is something that can be associated with a cystic mass, and I'm going to use that term, since we don't know what kind of ovarian cyst it is. Best Gynecologist in Jaipur
It can be very bad. So on one slight it can be slight, and the other side it can be very, very painful, which also leads into another one, is painful intercourse, and in this case, because there's a mass occupying lesion. This can be one of the - one of the main symptoms as well, so another form of the pain. There can be - actually as far as pain, there can be very painful menstruation. Their periods can be rather painful. Typically, these type of period pains are associated with the endometriomas, because, again, the endometrioma, the chocolate cyst is also growing every month just like the lining of the uterus. And depending where the endometrioma cyst is, can also cause problems with pain and painful intercourse.
There can be - any time you have intra-abdominal pressure or pain you can get nausea, you can get vomiting. But there are a small percentage of people that have this during each period anyway. So just because we have an episode of nausea or vomiting doesn't mean that you have an ovarian cyst by any means. And that's why this list of symptoms which New York OB/GYN Christopher Freville is giving is sort of non-specific, but it certainly is - can be present. You also can have constipation, a bladder-emptying problem.
Because again if you have a mass, especially as we talked about on the backside of the uterus that blocks the colon. This can cause constipation, because the colon can't empty as well, and you absorb more fluids from the feces, and you get more constipated. And then again you have some things like missed periods, irregular bleeding. These are often - again, they could be a combination of either an endometrioma or the polycystic ovaries. Because the polycystic ovaries have, as you recall, one of the symptoms are irregular periods and missed periods. Gynecologist in Jaipur
So these are the symptoms, and I think that probably every woman listening to this will say well, you know, I've had three of these symptoms, I wonder if I had a cyst. Again, these are very, very vague, but you have to combine it with the symptoms, as well as some of the things that we talked about earlier regarding perhaps there's irregular periods. Do you have - has there been an increase in weight? Is there an increase in hirsutism, the hair distribution pattern? So the symptoms are - combined with the physical exam or independent of the physical exam - might dictate that the doctor then decides well I'd better do some tests.
And the first test - probably the most easiest, least painful, is an ultrasound. And ultrasound, I'm sure there's not anyone here that doesn't understand ultrasound. But briefly, it's using sound waves to image solid and cystic objects it shows on a screen. And anyone who's had a baby or anyone who knows someone who's pregnant, I'm sure has had a picture of the ultrasound of the baby being passed around the office.
0 notes
Text
Diagnosis regarding Subclinical Heart Skin lesions by Framingham Danger Score, Peripheral Artery Atheromatosis as well as Coronary Artery Calcium mineral Score: An airplane pilot Study within Asymptomatic Men and women Experiencing HIV.
Eosinophilic oesophagitis (EoE) was basically described noisy . The nineteen nineties. Even though to begin with reportedly a rare entity, EoE has rapidly be a on a regular basis recognized ailment which has a frequency of approximately One inch A couple of,1000 men and women in the USA along with European countries. The illness will be characterized by a combination of oesophageal malfunction and major eosinophilic infiltration of the oesophageal muscle. From prognosis, additional diseases which can be associated with oesophageal eosinophilic infiltration has to be eliminated. Kids with EoE typical to a multitude of signs or symptoms, whilst older people mostly usual to dysphagia with regard to strong food and chest pain. Histologic options that come with EoE look like that relating to T-helper variety Only two swelling. Endoscopy needs to be performed to create the identification, but endoscopic issues are not pathognomonic regarding EoE and the examination may not display histologic problem. Treatment method methods regarding EoE contain medicines (corticosteroids, PPIs, antiallergic as well as biologics brokers), hypo-allergenic diet plans along with oesophageal dilatation pertaining to strictures which might be unresponsive to be able to medical therapy. Wavering eosinophilic inflammation contributes to the development involving oesophageal strictures, which possibly raise the chance of food bolus impactions. To date, long-term techniques for your restorative treating this kind of persistent inflamation related ailment continue being poorly identified. Straumann, A new. & Schoepfer, The. Mirielle. Nat. Rev. Gastroenterol. Hepatol. 9, 697-704 (This year); printed on the internet 25 June The coming year; doi:12.1038/nrgastro.This year.182Aesthetic documenting associated with human being subject matter is usually utilized in biomedical martial arts styles pertaining to clinical, investigation, legitimate, educational as well as individual functions. Recommendations about training specifications regarding biomedical saving have already been issued by particular wellness authorities, associations and journals, but none with the literature talks about this through a great find more Islamic viewpoint. This article commences with attorney at law around the standard principles associated with aesthetic taking inside Islam, followed by modesty issues within biomedical saving and problems with advised consent along with privacy. In order to be deemed honest from your Islamic standpoint, each of the above mentioned requirements must conform to, or otherwise oppose, Islamic instructing.The goal of the project is to read the effect regarding nucleation, progress and also breakage for the particle size submitting (PSD) of gypsum uric acid made by the particular moist flue gasoline desulfurization (FGD) procedure. The particular constant state PSD, acquired within a falling video damp FGD initial place through desulfurization of a 1000 parts per million(V) Thus(Only two) gasoline steady stream, displayed a powerful nonlinear behaviour (in the ln(in(d)) versus. My spouse and i piece) in the budget with the particle dimensions range, compared to the well-known straight line mixed insides put together product treatment model. Any short-term population stability the break point style, suited to new information, could model an increase in the particular small fraction involving tiny allergens, but not for the level noticed experimentally. The three-parameter, size-dependent development model, used pertaining to sodium sulphate decahydrate and potash alum, surely could identify the particular trial and error info, implying sometimes size-dependent incorporation kinetics or even rate of growth dispersal.
0 notes
Text

An easily missed fracture in the acute setting is a triquetral fracture. The AP and oblique views will be normal, but careful inspection of the lateral view reveals a small bone fragment in the dorsal wrist, which is pathognomonic for triquetral fracture.
Case courtesy of Dr Derek Smith, Radiopaedia.org, rID: 47445
2 notes
·
View notes