#trends in ophthalmology open access journal
Text
Lupine Publishers|To Compare the Retinal and Choroidal Thickness in Fuchs Uveitis Syndrome Patients with Healthy Controls Using Optical Coherence Tomography Seen at Tertiary Care Center
To Compare the Retinal and Choroidal Thickness in Fuchs Uveitis Syndrome Patients with Healthy Controls Using Optical Coherence Tomography Seen at Tertiary Care Center

Abstract
Purpose: To compare the retinal and choroidal thickness in Fuchs Uveitis Syndrome patients with healthy controls using optical coherence tomography seen at tertiary care center.
Method: 16 patients with unilateral Fuchs Uveitis Syndrome (FUS) and 20 healthy control subjects were enrolled in this retrospective study. Spectral domain optical coherence tomography was used to measure the central foveal thickness (CFT), retinal nerve fiber layer (RNFL) thickness and sub foveal choroidal thickness (SFCT) of the eyes with FUS and compared with the unaffected fellow eye and healthy controls.
Results: The mean age of the patients was 35.2 ± 8 years. Seven patients (60%) were male, and nine (40%) were female. Diffuse stellate keratic precipitates (KPs) were seen in all patients. Mild anterior chamber reaction was noted 62.5%. Heterochromia was observed in 87.5% of the eyes, cataract in 43.8% of the eyes, and vitreous cells and debris in 37.5% of the eyes. The mean CFT was (249.7 ± 27.4𝜇m) in affected eyes, (251.5± 23.1 𝜇m) in unaffected eyes of FUS and (253.3 ± 29.2 𝜇m) in healthy control which were statistically insignificant on comparison (𝑝 value > 0.05). The mean SFCT was significantly thinner in eyes with FUS (272.47 ± 13.12 μm) than in the fellow eyes without FUS (316.37 ± 16.13 μm; p = 0.04). and control (320.27 ± 18.15). The average RNFL thickness was found to be (106 ± 14.2 μm) in eyes with FUS, (108 ± 16.5μm) in eyes without FUS and (112 ±13.8μm) in healthy control which were statistically not significant (p value > 0.05).
Conclusion: We conclude that affected eyes in patients with FUS tend to have thinner choroids as compared to unaffected fellow eyes which is consistent with previous studies. It might be associated with chronic inflammation induced choroidal is chaemic changes. Future studies using swept source OCT will further improve precision to get choroid findings more accurate.
Keywords:Choroid; Fuchs Uveitis Syndrome; SD-OCT; Retinal Nerve Fiber Layer
Introduction
Fuchs’ uveitis syndrome (FUS) is an intraocular inflammatory condition that involves anterior segment, lens, vitreous humor and optic disc. It accounts for 2-11% of all uveitis cases [1]. Although many genetic, immunological, vascular and sympathetic theories have been proposed, recent studies show evidence of rubella or herpes simplex virus, toxoplasma association in some cases of FUS [2]. It is a frequently unilateral and typical age at presentation is 30-40 years [3,4]. The diagnostic criteria include stellate keratic precipitates (KPs) scattered diffusely all over cornea, chronic lowgrade anterior chamber reactions, iris atrophy with or without heterochromia, absence of posterior synechiae, vitreous opacities and macular edema [5]. It affects both genders equally and the prognosis is usually good [6]. Iris atrophy and heterochromia are due to atrophy and depigmentation of all iris layers, although it is not pathognomonic. Recently, fluorescein angiography (FA) had provided better information about the posterior segment involvement in FUS [7-9]. Optical Coherent Tomography (OCT) is a routinely employed noninvasive tool in detecting most posterior pole retinal abnormalities. The Enhanced Depth Imaging (EDI) in spectral domain (SD) OCT and swept source (SS) OCT allow visualizing the choroid more accurately [10,11]. Some studies documented the changes in choroidal thickness using EDI-OCT in uveitic conditions, such as Vogt–Koyanagi–Harada (VKH) disease, Behçet disease (BD), ocular sarcoidosis providing remarkable information about disease activity [12,13]. The natural course of the disease is slow to progress, without substantial reduction of visual acuity until significant vitreous opacities or cataract develop. FUS is often misdiagnosed or diagnosed delay leading to posterior subcapsular opacity and elevated IOP mainly due to long-term corticosteroid therapy. There are very few reports in the literature comparing macular, RNFL and choroidal thickness in FUS patients. The purpose of the current study was to measure central foveal thickness (CFT), subfoveal choroidal thickness (SFCT) and retinal nerve fiber layer (RNFL) thickness, in patients with FUS and to compare these with the unaffected fellow eyes and the age, sex and refractive equivalent-matched healthy controls. To the best of our knowledge, it is the first comparative study to evaluate SFCT and other parameters in FUS using spectral domain SD-OCT on FUS from central India.
Material and Methods
This retrospective study was conducted at a tertiary care center from central India. The medical records of 16 patients with FUS and 20 healthy controls between september 2018 and august 2021 were reviewed. Data including age, sex, ocular and medical history, ophthalmic examination, laboratory work-up and OCT parameters were retrieved from patient record. Aii patients had best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, Goldmann applanation tonometry and dilated fundoscopy. The inclusion criteria were diagnosed unilateral FUS based on clinical findings and fundus sufficient for its visualization on clinical examination. Bilateral FUS, history of previous ocular surgery, eyes with dense cataract or media opacity obscuring the visualization of choroid, presence of a coexisting ocular or systemic disease and use of any topical or systemic medications. were excluded from study. The control group consisted of age-, sex-, and refractive equivalent-matched healthy controls who visited ophthalmology clinic for routine examination. The laboratory investigations included complete blood counts, angiotensin converting enzyme, mantoux test and venereal disease research laboratory tests etc. To exclude other causes of anterior or intermediate uveitis. The CFT and RNFL thickness of eyes with FUS were evaluated with SD-OCT and compared with the unaffected fellow eyes and healthy controls. The EDI mode was used to evaluate SFCT. SFCT was defined as the vertical distance from the outermost hyperreflective line of the retinal pigment epithelium (RPE) to choroid-sclera junction under the center of the fovea and was measured using the calipers available within the software. The RNFL thickness (from the inner margin of the internal limiting membrane to the outer margin of the RNFL layer) was automatically segmented using software version. Average RNFL was used for analysis. Statistical analyses were performed with R version 4.0.5. Data were recorded as the mean ± standard deviation (SD). Quantitative data was analyzed using one way analysis of variance (ANOVA) test. An independent 𝑡-test and Chi-square test were used to compare variables between patients with FUS and healthy control subjects. A value of 𝑝< 0.05 was considered to be statistically significant for all analyses.
Results
16 patients with FUS (9 females and 7 males) and 20 healthy control subjects (11 females and 9 males) were included for analysis in this study. The mean age of FUS patients was 35.2±8 years, while it was 38.4± 6years for controls, which was statistically insignificant (𝑝>0.05) (Table 1). Gender differences in both groups were also statistically insignificant (𝑝>0.05). Blurred vision and floaters were the most frequent presenting symptoms {5 patients, (31.3%) and 4 patients (25%) respectively}. Other symptoms included red eye (1 patient, 6.3%), photophobia (1 patient, 6.3%). Three patients were asymptomatic (18.75%), and the diagnosed during a routine eye examination (Table 2). Iris atrophy was present in 5 patients. Heterochromia was present in 14 patients. Cataract was present in 7 patients. Stellate keratic precipitates were noted in all patients. Mild anterior chamber reactions were seen in 10 patients. Vitreous cells or debris were observed in 6 patients (Table 3). The cause of visual impairment was cataract in all cases. The central foveal thickness was 249.7±27.4𝜇m in the affected eyes, 251.5±23.1 𝜇m in the unaffected eyes of FUS patients, and 253.3±29.2 𝜇m in control subjects. There were no significant differences in central foveal thickness between the affected and unaffected eyes of FUS patients (𝑝 = 0.93) or between the affected eyes of FUS patients and the eyes of control subjects (𝑝 = 0.9). The mean SFCT was found to be 272.47 ± 13.12μm in eyes with FUS and 316.37± 16.13μm in eyes without FUS (p = 0.04) and 320.27 ± 18.15𝜇m in the eyes of healthy control subjects. There was choroidal thinning at fovea in the affected eyes of FUS patients compared with the unaffected eyes or control subjects, Average RNFL thickness was 106 ±14.2𝜇m in the affected eyes of FUS patients, 108±16.5𝜇min the unaffected eyes of FUS patients, and 112 ± 13.8𝜇m in the eyes of healthy control subjects (Table 4). No significant differences in RNFL thickness were observed between the affected and unaffected eyes of FUS patients (𝑝 = 0.92) or between the affected eyes of FUS patients and the eyes of control subjects (𝑝 = 0.76)
Table 1: Demographic analysis.
Table 2: Presenting symptoms.
Table 3: Characteristic of FUS patients.
Table 4: Thickness of fovea, sub foveal choroid, and RNFL in FUS & control.
Discussion
To our knowledge, very few comparative studies on FUS patients have been done till yet. In the present study, we compared central foveal thickness, retinal nerve fiber layer and subfoveal choroidal thickness between the affected eyes, the unaffected eyes of FUS patients and healthy controls from central India. Although we found choroidal thinning at fovea in the affected eyes of FUS patients compared with the unaffected eyes of FUS patients or control subjects, there was no statistically significant difference in RNFL and central foveal thickness. FUS was first described in 1906, recent studies have focused on various viral agents and the etiology of FUS remains controversial. In FUS, persistence of chronic lowgrade inflammation for years leads to various degrees of atrophy of the iris and ciliary body. As the choroid being more vulnerable to the effects of the inflammatory and vascular diseases than other tissues, imaging of choroid is important for understanding the pathophysiology of various diseases. EDI mode using SD-OCT devices enables cross-sectional, high resolution better visualization of the choroid. Many studies have documented the effect of various acute and chronic ocular inflammatory conditions on choroidal abnormalities. Nakayama et al. showed that choroidal thickness as a marker for the degree of choroidal inflammation in acute Vogt- Koyanagi-Harada disease using EDI-OCT [14]. Kim et al. found an increase in subfoveal choroidal thickness in the acute phase of Behcet’s posterior uveitis [15]. Multiple studies suggest that increased blood flow and choroidal effusion is the mechanism responsible for choroidal thickening in acute inflammation [16,17]. However, Coskun et al. observed the thinning of subfoveal choroid in chronic Behcet’sassociated posterior uveitis probably due to chronic inflammation induced fibrosis [18]. Very few studies from Turkey and Italy like Balci and Ozsutsus, Kardes et al. and Carquaglia et al. showed the comparison between the affected and fellow eye in FUS patients [19-21] (Table 5). The study by Kardes et al. had findings consistent with the study of Balci and Ozsutsus. We propose that chronic anterior chamber and vitreous inflammation in eyes with FUS may affect choroidal perfusion, which may result in ischaemic changes leading to atrophy and fibrosis of the choroid tissue, thereby reducing choroidal thickness. Limitations of our study is being retrospective nature and small sample size. We have used SD OCT in this study and with advent of new imaging methods designed specifically for the choroid, SS OCT which allows examination of the choriocapillaris, and larger choroidal vessels more clearly can further improve precision to determine the inner and outer boundaries of the choroid findings in the future. To conclude, we found subfoveal thinner choroid in FUS as compared to uninvolved fellow eyes, but we could not find a statistically significant comparison of foveal and RNFL thickness in FUS versus unaffected eye. Our findings are also consistent with those of previous studies. As this is the first analysis of its kind from central India, longitudinal studies with large sample size would help in more understanding of the effect of chronic inflammation on the choroid in FUS in future.
Table 5: Comparison between different studies of mean sub foveal choroidal thickness (SFCT).
For more information about Trends in Ophthalmology Open Access Journal archive page click on below link
https://lupinepublishers.com/ophthalmology-journal/archive.php
For more information about lupine publishers page click on below link
https://lupinepublishers.com/index.php
#lupine publishers#lupine publishers group#lupine publishers LLC#trends in ophthalmology open access journal#tooaj
2 notes
·
View notes
Text
Macular Abnormality after Successful Surgery for Idiopathic Macular Hole Assessed Using Optical Coherence Tomography | Crimson Publishers
Macular Abnormality after Successful Surgery for Idiopathic Macular Hole Assessed Using Optical Coherence Tomography by Nazimul Hussain in Medical & Surgical Ophthalmology Research
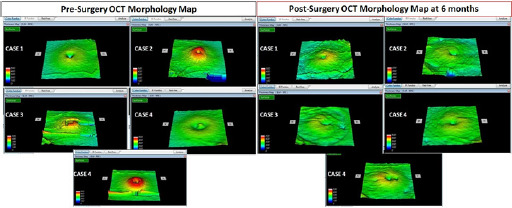
Purpose: Macular changes following Internal Limiting Membrane peeling after successful Macular hole closure using optical coherence tomography.
Methods: 5 eyes of 5 patients were included in the study. The inclusion criteria were idiopathic full thickness macular hole and completed at least 6 months follow up. All patients underwent optical coherence tomography assessment before and after surgery until 6 months. Macular thickness and morphology map was analyzed before and after surgery.
Results: There were 3 males and 2 females. The age range from 45 to 59 years. Conspicuous irregular surface of the inner retina on Optical Coherence Tomography surface topography was evident in all eyes at 6 months. This was also associated with downward slope of the temporal macula seen on surface topography. There was trend towards decrease in subfield thickness especially in the T1, S1, I1 and N1 6 months after surgery. The average decrease was -60.4 microns in T1, -20.4 microns in S1, -13.0 microns in I1 and -23.4 microns in N1.
Conclusion: In this small case series brilliant blue assisted ILM peeling after successful macular whole closure showed evidence of decrease in macular thickness in all first subfield quadrant and downward slope of the temporal macula as well as conspicuous irregularity of the inner retina.
https://crimsonpublishers.com/msor/fulltext/MSOR.000517.php
For more open access journals in Crimson Publishers please click on link: https://crimsonpublishers.com
For More Articles on Medical Research Please click on: https://crimsonpublishers.com/msor/
#Crimson Publishers#Crimson Publishers Journals#Crimson Publishers LLC#Journal of Ophthalmology and Ophthalmic Surgery#Ophthalmology open access journals
18 notes
·
View notes
Text
Lupine Publishers | Ribociclib as New Cause of Cornea Verticillata
Lupine Publishers | Trends in Ophthalmology Open Access Journal
Abstract
Our purpose is to describe the appearance of a new origin of Cornea Verticillata through a clinical case of a 67-years-old female patient with breast cancer who was being treated by Ribociclib and attended the consultation of ophthalmology by halos vision. Exploration was performed by visual acuity, slit lamp examination, fluorescein staining, retinography and corneal topography. We observed cornea verticillata in our patient, she did not need specific treatment and the findings remained stable over time.
Keywords:Cornea Verticillata; Ribociclib; Breast cancer; Adverse effect; Amiodarone
Introduction
Cornea Verticillata a is an often asymptomatic and reversible corneal alteration caused by certain diseases and drugs [1,2]. Our goal is to announce a new cause of this finding. Ribociclib is a drug used in breast cancer therapy [3]. It is important to know the adverse effects of new drugs and their ocular repercussion. Herein we present a clinical case of Cornea Verticillata as a consequence of Ribociclib therapy.
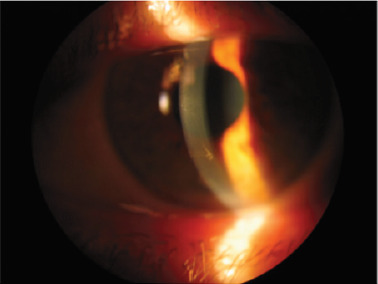
Clinical Case
A 67-year-old woman with a history of breast cancer comes to our office for feeling halos and blurred vision. The patient was diagnosed with metastatic breast cancer for 2 years, treated by tumerectomy and oral Ribociclib (500 mg daily). She had no known ocular history or allergies. The visual acuity with its optical correction was 0.8 (decimal scale) for both eyes. In the anterior pole biomicroscopy, a transparent cornea with pigmented verticillata keratopathy was seen (Figure 1). An incipient nuclear cataract could also be observed. The rest of the parameters corresponded to normality. The intraocular pressure was 15 mmHG in both eyes and the fundoscopy showed no significant findings. A Schirmer type I test was performed, which was 20 mm in the right eye and 15 mm in the left eye. Fluorescein staining showed no epithelial damage (Figure 2). The corneal tomography (Pentacam, Okulus Optikgerate GmbH, Wetzlar, Germany) revealed a regular astigmatism with the rule, with central pachymetry of 540 microns in the right eye and 530 microns in the left eye. There were no corneal thinning points or irregularities in either eye (Figure 3). Retinography and autofluorescence, as well as optical coherence tomography, did not show significant findings. Given the good visual acuity of the patient and the benign finding of verticillata cornea secondary to Ribociclib, observation and monitoring of the lesion was decided. The patient was evaluated at 3 and 6 months after the consultation, resulting in a similar exploration to the previous ones. She is currently in treatment with Ribociclib and topical lubricants on demand.
Discussion
The Verticillata cornea is a keratopathy, often unnoticed, that occurs in the corneal apex after the use of certain drugs or in the context of a systemic disease [4]. Its characteristic shape allows diagnosis through biomicroscopic exploration. It is usually a benign and not very symptomatic disorder that disappears if it is secondary to a triggering factor. Among the diseases most related to this picture are Fabry disease or Cystinosis [5]. The drugs that most often cause cornea Verticillata are amiodarone, chloroquines, tamoxifen and indomethacin, among many others. Ribociclib is an antineoplastic drug that inhibits cyclins and is administered orally as a treatment for metastatic breast cancer [6]. Its indication is approved for breast neoplasms with positive Hormone Receptors and negative Epidermoid Growth Receptor [7]. Since the introduction of the drug, the resistance to previous therapies in this type of tumors has been reduced by 20%. Among the most frequent side effects are neutropenia, alteration of liver enzymes and digestive symptoms such as nausea, diarrhea or vomiting. At present, the use of this drug has not been linked to the appearance of Verticillate cornea. It is always important to perform a detailed ocular exploration of the cornea verticillate secondary to drugs, since we can also find associated retinal toxicity. The retinography and the autofluorescence image can help us in the screening. The withdrawal of the drug is usually not necessary due to its benignity, although close monitoring of the lesions is recommended.
Conclusion
The multidisciplinary work between oncologists and ophthalmologists is necessary for the management of these patients. Ribociclib could result a new cause of Cornea Verticillate.
https://lupinepublishers.com/ophthalmology-journal/fulltext/ribociclib-as-new-cause-of-cornea-verticillata.ID.000138.php
For more Lupine Publishers Open Access Journals Please visit our website: https://twitter.com/lupine_online
For more Trends in Ophthalmology Please Click
Here: https://lupinepublishers.com/ophthalmology-journal/
To Know more Open Access Publishers Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
0 notes
Text
Iris Publishers- Open Access journals of Ophthalmology & Vision Research
Demographics and Pattern of Referral of Participants at a One-Week Long Free Glaucoma Screening Event
Authored by Elizabeth A Awoyesuku*
Abstract
Aim: The aim was to elucidate the demographic characteristics of the participants who presented at a week-long free eye screening programme to mark the World Glaucoma Week 2019 at the Ophthalmology department, University of Port Harcourt Teaching Hospital and their sources of referral.
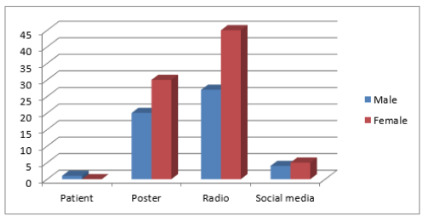
Methodology: Members of the public were invited for free eye screening at the department of Ophthalmology, University of Port Harcourt Teaching Hospital using several channels of information dissemination including electronic media (Radio), Posters /Banners and Social media. Each had a comprehensive ocular examination done. Those identified with glaucoma were referred for follow-up in the glaucoma clinic. Data obtained was analyzed using SPSS version 21. The age groups gender, other demographic distribution of the subjects amongst other were presented using frequency tables and charts.
Results: A total of 133 participants (266 eyes) responded to the invitation for free eye screening. 39.1% were male and 60.9% female with a mean age of 42.26 years ±14.58. 48.2% were in the age group of 31-50years. 45.9% of the participants were civil servants with 63.9% of them having a tertiary form of education. 54.5% of participants presented for the screening after listening to radio announcement. The Prevalence of glaucoma in this study was 4.13%.
Conclusion: Women accessed free eye screening more than men in our study and the mass media (Radio announcement) resulted in the most means of referral. The prevalence of glaucoma from our study was 4.13%.
Keywords: Demographics; Glaucoma screening; Pattern of referral
Introduction
Primary Open Angle Glaucoma (POAG) is a chronic condition characterized by loss of retinal ganglion cells. Increased intraocular pressure, positive family history, older age and African descent place an individual at an increased risk for glaucoma [1].
The prevalence of POAG ranges from 1.1% to 3.0% in Western populations, and from 4.2% to 8.8% in populations of African descent [2]. Subgroups of population at risk for developing glaucoma have insufficient knowledge and need to be identified and targeted [3]. In developing countries detecting glaucoma access to care is further limited by poor access to health facilities [4].
In an effort to reverse the trend the World Glaucoma Association and World Glaucoma Patient Association through a joint initiative put together the ‘World Glaucoma Week’ which encourages annual week-long intensive advocacy and mass enlightenment programs to increase awareness of the disease as well as screening to improve case finding [5].
This annual event has been celebrated yearly by the department of Ophthalmology, University of Port Harcourt and this year 2019 a study was undertaken to elucidate the demographics of the population as well as the best means of information dissemination which resulted in access of care with the aim of planning future glaucoma screening activities and improving case finding.
Materials and Methods
Members of the public were invited for free eye screening at the department of Ophthalmology, University of Port Harcourt Teaching Hospital using several channels of information dissemination. A total of 133 persons participated and each had a comprehensive ocular examination done including a visual acuity examination (unaided, Pinhole), Slit lamp examination of anterior segment, Dilated Slit lamp biomicroscopy with +78D lens, Non-contact tonometry, Pachymetry and perimetry. Those identified with glaucoma were referred for follow-up in the glaucoma clinic. Data obtained was analyzed using SPSS version 21. Mean and standard deviations were determined for age. The age groups gender, other demographic distribution of the subjects amongst other were presented using frequency tables and charts Statistical significance was put at p ≤ 0.05. A diagnosis of glaucoma was made following dilated slit lamp biomicroscope with VCDR >0.7, demonstrable perimetric changes and elevated intraocular pressures above 21mmHg
Results and Discussion
As the population increases in developing countries so also will the number of persons with glaucoma increase leading to worsening socioeconomic burden of the disease [6]. In Nigeria, the National Blindness and Visual Impairment Survey had a prevalence of glaucoma related blindness in above 40years was 5.02-6.9% [7]. The World Glaucoma Week is a joint initiative between the World Glaucoma Association and the World Glaucoma Patient Association. It has been celebrated over 9 years all over the world including Nigeria with a total of 626 events were recorded during the week March 10th-16th 2019 [5]. Most of the events are geared towards improving public awareness of the disease. The World Glaucoma week has also been used to gather data on causes of visual impairment as was seen in the World Glaucoma screening in 2016, 449 persons were screened during the week [8].
The World Glaucoma Week was celebrated in our department by having free glaucoma screening. Using many channels of information dissemination members of the public were invited for a week-long free glaucoma screening. The demographic characteristics of the population are found in the table below (Table 1&2) (Figure 1).
Gender
In a report by Janicijevic K, et al. [9] a review of 10 years of annual glaucoma screening activities showed a preponderance of females accessing the free screening which corroborates our study findings where women were more in number. A study in the South East of Nigeria by Kizor Akairaiwe [10] however found more men availing themselves for screening than women. There is gender inequality in accessing healthcare as most women do not have the finances required to do this, it’s no wonder they may resort to free eye care activities such as outreaches.
Age
(Table 3) Several studies show most of the participants of free eye care programmers tend to be in the 5th to 6th decade of life [10-13]. Glaucoma typically is asymptomatic until late stages and is more likely to affect those of black race with positive family history and advancing age [14]. this was emphasized during various forms of information dissemination and is therefore not surprising that our study had a lot of people in the 5th and 6th decades of life presenting. This may also be postulated to be same in other studies aside from the fact that visual disorders increase with increasing age and therefore the elderly are more likely to access care since they would be symptomatic. Age group 21-30years had a significant use of print media (Figure 2).
Majority of the Figure 3participants in our study were civil servants. This maybe because Port Harcourt (South-South Nigeria) being an oil producing community has a lot of office workers. This is unlike that in Enugu [10] (South- East Nigeria) where majority were businessmen or Odukpani, Cross Rivers State and Ethiopia where farmers topped the number Majority of the population assessed screening because of radio announcement followed closely by information on posters [15,16] (Figure 3) (Table 4).
Sources of referral /means of information dissemination
Electronic Media (Radio) was the highest means of information dissemination in our study Most of the referrals were by electronic media, Posters (print media) featured in age group 21-30years while social media (Digital media) didn’t play a significant role across all age groups. This was same as that of Akaraiwe, et al. [10]. In the study by Adekoya, et al. [12] most patients were self-referred. Electronic media did not however feature significantly in the study at Ethiopia by Tenkir, et al. [15]. This can be explained by the fact that most rural areas in Nigeria have access to the radio unlike in Ethiopia where radio services were sparse at the time of the study.
Educational level
Most of the participants in our study had tertiary level of education same as the study in the South East Nigeria [10] while in Ethiopia [15] mainly secondary school educational graduates accessed the outreach. This is in sharp contrast to Amoomo A [17]. in Namibia where 64.8% of the respondents were unemployed and 44.5% had not completed primary school education.
Prevalence of glaucoma
(Figure 4) The population-based survey of the prevalence and types of glaucoma in Nigeria: results from the Nigerian National Blindness and Visual impairment survey have put the overall prevalence of Glaucoma in above 40years at 5.02%. Risk factors for increased prevalence were illiteracy, increasing age, males and Igbo ethnic group [18]. The prevalence of glaucoma of glaucoma in our study (South-South Nigeria) was 4.13%, 14.5% in the South-East Nigeria [10], and 7.3% in South-Western Nigeria [19].
Case finding for glaucoma is a continuous process though it may not be economically viable, in spite of this; screening is a great challenge in low economies such as Nigeria. [20] The World Glaucoma Week is a good opportunity to improve public awareness of Glaucoma as well as improve case finding in Nigeria.
Conclusion
Women accessed free eye screening more than men in our study and the mass media (Radio announcement) resulted in the most means of referral. The prevalence of glaucoma from our study was 4.13%.
To read more about this article: https://irispublishers.com/wjovr/fulltext/demographics-and-pattern-of-referral-of-participants-at-a-one-week-long-free-glaucoma-screening-event.ID.000549.php
Indexing List of Iris Publishers: https://medium.com/@irispublishers/what-is-the-indexing-list-of-iris-publishers-4ace353e4eee
Iris publishers google scholar citations:
https://scholar.google.co.in/scholar?hl=en&as_sdt=0%2C5&q=irispublishers&btnG=
0 notes
Text
Macular Abnormality after Successful Surgery for Idiopathic Macular Hole Assessed Using Optical Coherence Tomography in Crimson Publishers: Medical Research
Macular Abnormality after Successful Surgery for Idiopathic Macular Hole Assessed Using Optical Coherence Tomography by Nazimul Hussain in Medical & Surgical Ophthalmology Research
Purpose: Macular changes following Internal Limiting Membrane peeling after successful Macular hole closure using optical coherence tomography.
Methods: 5 eyes of 5 patients were included in the study. The inclusion criteria were idiopathic full thickness macular hole and completed at least 6 months follow up. All patients underwent optical coherence tomography assessment before and after surgery until 6 months. Macular thickness and morphology map was analyzed before and after surgery.
Results: There were 3 males and 2 females. The age range from 45 to 59 years. Conspicuous irregular surface of the inner retina on Optical Coherence Tomography surface topography was evident in all eyes at 6 months. This was also associated with downward slope of the temporal macula seen on surface topography. There was trend towards decrease in subfield thickness especially in the T1, S1, I1 and N1 6 months after surgery. The average decrease was -60.4 microns in T1, -20.4 microns in S1, -13.0 microns in I1 and -23.4 microns in N1.
Conclusion: In this small case series brilliant blue assisted ILM peeling after successful macular whole closure showed evidence of decrease in macular thickness in all first subfield quadrant and downward slope of the temporal macula as well as conspicuous irregularity of the inner retina.
https://crimsonpublishers.com/msor/fulltext/MSOR.000517.php
For more open access journals in crimson publishers please click on link: https://crimsonpublishers.com
For More Articles on Medical Research Please click on: https://crimsonpublishers.com/msor/
0 notes
Text
Retinal Blood Vessels Extraction: Introduction and Future Trends- Juniper Publishers
Juniper Publishers- JOJ Ophthalmology
Abstract
Retinal vascular structure is an imperative marker of numerous retinal and systemic maladies, which has persuaded the origination of different image segmentation strategies for the veins. The core target of this article is to distinctively introduce the open research issues in the retinal blood vessels segmentation and to discuss the similarities and dissimilarities between different approaches utilized to isolate blood vessels in retina images. The contemporary implications, the future strategies, and the open complications in automatic retinal vessels detection are also encapsulated.
Keywords: Review; Retina images; Blood vessels; Segmentation; Vasculature; Drive; Stare
Go to
Introduction
Segmentation play a key part in therapeutic imaging. Segmentation is utilized as a part of a many application, for example, investigation of physical structure, medical screening during evaluation of tortuosity, stenosis and angiogenesis [1]. In clinical analysis, segmentation assists the patients' to detect the level of the severity of the ailments. But, the aforesaid applications demand an adequate segmentation procedures that can isolate diverse sizes of the vessels as well as recognize irregularities in the vessels for better assessment. A portion of the accessible procedures are manual based. Manual isolation of vessel and non-vessel pixels is irksome, complex and time consuming, particularly during the investigation of enormous and composite databases when contrasted with computerized/ automatic segmentation [2]. In spite of the fact that the computerized procedures are deliberated to be precise and quick, despite everything they confront difficulties, for example, trouble in recognizing vessels from the non-vessels because of impediment created by blockage tissues, trouble in segmenting diverse widths of vessels particularly unhealthy vessels because of existence of artifacts in medical images, which leads to misclassification.
The vascular network of retina photograph contain the significant details which are utilized for the identification and exploration of different retinal disorders, for example, hypertension [3], glaucoma [4], and diabetes [5]. The eye's expert utilized fundus camera for capturing retinal photograph of the patients. These retinal photographs are used by the ophthalmologist for inspections, screening and analysis of various retinal disorders. The segmentation of blood vessels in retina images display significant vascular variations which are used for recognition and diagnoses of various ophthalmic abnormalities. The structure of vessel and non-vessel pixels is very homogenous in retinal images, which make vessels hard to isolate from the background pixels. Consequently, it is compulsory to utilize an appropriate image segmentation framework for precise extraction of retinal vasculature. These procedures depend on the image structures, for example, the cross-sectional profiles, identical intensity sections and boundaries [6].
Reviews and studies on the methodologies for extraction of vascular tree in medicinal images are present in the literature. Fraz et al. [7] categorize the retinal vessels extraction methods into seven groups based on the image processing techniques, namely, pattern recognition methods, mathematical morphology approaches, vessel tracking schemes, model based methods, parallel hardware based systems, multi-scale based procedures and matched filter based methodologies. Supervised and unsupervised approaches are in the sub-group of pattern recognition methods. Supervised schemes utilized already learned and trained data to choose whether a pixel belongs to a vessel or not, while unsupervised procedures achieve the vessel extraction with no earlier marked information. The word mathematical morphology is utilized as a tool for extracting image segments that are valuable in the demonstration and explanation of region shapes such as features, edges, skeletons and curved structures. Vessel tracking systems fragment a vessel between two points utilizing neighbourhood data and work at the level of a solitary vessel rather than the whole vascular network. The concept behind multi-scale frameworks for vasculature detection is to isolate facts associated with the blood vessel having variable size at multi scales. The computation time complexity of retinal vessel detection frameworks and requirements for real-time execution is resolved by parallel hardware based implementation of procedures. The matched filter based methodologies analyze the dissimilarities of the intensity level of the cross-section profile of the retinal image with the pre-set template or kernel.
Go to
Discussion and Future Trends
The target of this article is to discuss the open issues related to retinal blood vessels segmentation and to guide the scholars towards the interesting research directions. The recent vasculature segmentation methodologies still face trouble in isolating vessels due to image artifacts (such as intensity variations, noise, motion artifacts). A little number of available approaches are competent to detect vessels in medical images of different modalities. Researchers can further investigate to reduce the computation time, especially in supervised methods. A robust technique is required to segment blood vessels in healthy, unhealthy (disease infected) and noisy retinal images, to handle a large datasets containing images of different resolutions, to detect vessels of different widths, to locate vessels at their correct positions and to accurately compute vessels width. Another open area is to compute arteriolar-to-venular ratio (AVR) to isolate artery and veins. Complex preprocessing and postprocessing issue need to be addressed to decrease the computation time. Adaptive capabilities is required to control over-segmentation and under-segmentation under varying image conditions. The human intervention need to be eliminated for selection of region of interest, threshold selection and initial seed point selection.
Go to
Conclusion
The extraction of the retinal blood vessels has been a vigorously investigated zone in present age. The perfect localization of the retinal vasculature develops the foundation of numerous automated computer aided systems for analysis and detection of cardiovascular and ophthalmologic disorders. Even though many promising methods and strategies have been developed, there is still opportunity to get better in blood vessel extraction approaches.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com
For more articles in JOJ Ophthalmology (JOJO) please click on: https://juniperpublishers.com/jojo/index.php
For more Open Access Journals please click on: https://juniperpublishers.com
0 notes
Text
Iris Publishers_Publisher | Iris Publishers - Scilit
Iris Publishers
View All Journals
Publisher information Total number of journals: 13 (13 active journals in 2018) Total number of papers: 359
Number of journals
Number of articles
Filter: Yearly Monthly Journals Open access journals From: To: Refine Search Journals Books Proceedings Top 10 journals Archives in Neurology & Neuroscience Current publisher:
Iris Publishers (10.33552)
EISSN : 26411911 Total articles: 58
View Journal information
Current Trends in Civil & Structural Engineering Current publisher:
Iris Publishers (10.33552)
EISSN : 26436876 Total articles: 43
View Journal information
Journal of Textile Science & Fashion Technology Current publisher:
Iris Publishers (10.33552)
EISSN : 2641192X Total articles: 42
View Journal information
World Journal of Gynecology & Womens Health Current publisher:
Iris Publishers (10.33552)
EISSN : 26416247 Total articles: 35
View Journal information
World Journal of Agriculture and Soil Science Current publisher:
Iris Publishers (10.33552)
EISSN : 26416379 Total articles: 34
View Journal information
Global Journal of Engineering Sciences Current publisher:
Iris Publishers (10.33552)
EISSN : 26412039 Total articles: 28
View Journal information
Annals of Biostatistics & Biometric Applications Current publisher:
Iris Publishers (10.33552)
EISSN : 26416336 Total articles: 26
View Journal information
Open Access Journal of Addiction and Psychology Current publisher:
Iris Publishers (10.33552)
EISSN : 26416271 Total articles: 23
View Journal information
Online Journal of Dentistry & Oral Health Current publisher:
Iris Publishers (10.33552)
EISSN : 26411962 Total articles: 20
View Journal information
World Journal of Ophthalmology & Vision Research Current publisher:
Iris Publishers (10.33552)
EISSN : 26416360 Total articles: 18
View Journal information
View All Journals
https://www.scilit.net/publisher/11297
0 notes
Text
Publisher | Iris Publishers - Scilit
Iris Publishers
View All Journals
Publisher informationTotal number of journals: 13 (13 active journals in 2018)Total number of papers: 359
Number of journals
Number of articles
Filter:YearlyMonthlyJournalsOpen access journalsFrom: 2018 2017 2016 2015 2014 2013 2012 2011 2010 2009 2008 2007 2006 2005 2004 2003 2002 2001 2000 1999 1998 1997 1996 1995 1994 To: 2018 2017 2016 2015 2014 2013 2012 2011 2010 2009 2008 2007 2006 2005 2004 2003 2002 2001 2000 1999 1998 1997 1996 1995 1994 Refine SearchJournalsBooksProceedingsTop 10 journalsArchives in Neurology & NeuroscienceCurrent publisher:
Iris Publishers (10.33552)
EISSN : 26411911Total articles: 58
View Journal information
Current Trends in Civil & Structural EngineeringCurrent publisher:
Iris Publishers (10.33552)
EISSN : 26436876Total articles: 43
View Journal information
Journal of Textile Science & Fashion TechnologyCurrent publisher:
Iris Publishers (10.33552)
EISSN : 2641192XTotal articles: 42
View Journal information
World Journal of Gynecology & Womens HealthCurrent publisher:
Iris Publishers (10.33552)
EISSN : 26416247Total articles: 35
View Journal information
World Journal of Agriculture and Soil ScienceCurrent publisher:
Iris Publishers (10.33552)
EISSN : 26416379Total articles: 34
View Journal information
Global Journal of Engineering SciencesCurrent publisher:
Iris Publishers (10.33552)
EISSN : 26412039Total articles: 28
View Journal information
Annals of Biostatistics & Biometric ApplicationsCurrent publisher:
Iris Publishers (10.33552)
EISSN : 26416336Total articles: 26
View Journal information
Open Access Journal of Addiction and PsychologyCurrent publisher:
Iris Publishers (10.33552)
EISSN : 26416271Total articles: 23
View Journal information
Online Journal of Dentistry & Oral HealthCurrent publisher:
Iris Publishers (10.33552)
EISSN : 26411962Total articles: 20
View Journal information
World Journal of Ophthalmology & Vision ResearchCurrent publisher:
Iris Publishers (10.33552)
EISSN : 26416360Total articles: 18
View Journal information
View All Journals
https://www.scilit.net/publisher/11297
0 notes
Text
Ophthalmic Surgical Devices and Therapeutics (Eye Care) Market is Expected to Demonstrate a CAGR of 5.8% From 2018 to 2026
Transparency Market Research (TMR) has published a new report titled, “Ophthalmic Surgical Devices and Therapeutics Market – Global Industry Analysis, Size, Share, Growth, Trends, and Forecast, 2018–2026”. According to the report, the ophthalmic surgical devices and therapeutics market is expected to reach at US$ 43,794.4 Mn by the end of 2018. The market is anticipated to reach US$ 68,898.4 Mn by 2026 and expand at a CAGR of 5.8% from 2018 to 2026. Rise in number of geriatric patients, increase in awareness regarding eye disorders, and high unmet medical needs are expected to augment the global market from 2018 to 2026. The ophthalmic surgical devices and therapeutics market is projected to expand owing to an increase in the prevalence of eye-related disorders among the population, demand for better treatments, and developing healthcare infrastructure in various countries across the globe.
Increasing geriatric population and rising awareness regarding eye diseases
According to data published by the United Nations Department of Economics and Social Affairs, the geriatric population is expected to double by the end of 2050 and is projected to reach nearly 2.1 billion. This increasing geriatric population is prone to significant risk of eye-related disorders, including blindness. Public awareness regarding common eye conditions is increasing in developing countries, leading to early diagnosis and treatment of eye diseases. Furthermore, there are a large number of organizations dedicated to fight blindness, restore vision, and create awareness regarding eye health. National Eye Institute, National Association for Visually Handicapped, National Federation of the Blind, and Prevent Blindness are some eye health organizations concerned with prevention of eye diseases.
Request a PDF Sample: https://www.transparencymarketresearch.com/sample/sample.php?flag=S&rep_id=60669
Increase in incidence rates of eye related disorders
According to the World Health Organization (WHO), there are 285 million visually impaired people globally, approximately 90% of them reside in low to middle income countries. Furthermore, approximately 95 million people suffer from cataract, and 20 million suffer from various eye conditions, including glaucoma, muscular degeneration, infections, and childhood-related conditions. Significant rise in incidence of eye-related diseases, especially in developed countries, is anticipated to drive the ophthalmic surgical devices and therapeutics market between 2018 and 2026. Patients undergoing open angle glaucoma and age related macular degeneration (AMD) in the U.S., were 2.7 million and 2.1 million, respectively. This number is projected to increase to 3.3 million and 2.5 million, respectively, by 2020. Increasing patient pool in developing countries as well as developed countries is estimated to propel healthcare spending for eye treatments in these countries and drive the ophthalmic surgical devices and therapeutics market.
High unmet needs for refractive corrections
According to an article published by the British Journal of Visual Impairment, refractive errors are the leading cause of visual impairment and at the same time, most treatable cause of visual impairment in children. Furthermore, according to this article, more than 90% of people with refractive errors reside in low-income and poor countries and cost is a major obstacle to accessing glasses and meeting the need for correction. Studies indicate that rates of willingness to pay for glasses are low, and cost and affordability is a primary reason for not using glasses in China, India, countries in Africa, and several developing countries across the globe.
Request Brochure of Report: https://www.transparencymarketresearch.com/sample/sample.php?flag=B&rep_id=60669
Therapeutics segment dominates the global market due to its choice as first line of treatment for ocular diseases
In terms of product type, therapeutics is a highly attractive segment of the global ophthalmic surgical devices and therapeutics market, followed by surgical devices and vision care segments. This is attributable to the preference for drugs as the first line of treatment for any eye-related diseases. Expansion of the segment is primarily attributed to the increased prevalence of glaucoma and ocular infections among the population. According an article published by the American Academy of Ophthalmology, the global prevalence of glaucoma for population aged 40 to 80 years is 3.54%. The prevalence of primary open-angle glaucoma is considerably high in Africa, i.e., 4.2%, and the prevalence of primary angle-closure glaucoma (PACG) is significantly high in Asia, i.e., 1.09%.
North America dominates the global market owing to significant technological advancements in the region
North America dominates the global ophthalmic surgical devices and therapeutics market due to a large patient pool, high cost of specialty branded drugs, high cost of ocular surgeries, and increase in the geriatric population in the region. The region is estimated to maintain its dominance during the forecast period. According a U.S eye disease statistics, published by the American Academy of Ophthalmology, cataract, age-related macular degeneration, glaucoma, and diabetic retinopathy are the most common causes of visual impairment among the population in the U.S. Additionally, approximately 7.32 million people in the U.S. are expected to suffer from primary open-angle glaucoma by 2050. Moreover, rising healthcare expenditure and increasing investments are key factors that are anticipated to boost the ophthalmic surgical devices and therapeutics market in the next few years. The ophthalmic surgical devices and therapeutics market in Asia Pacific is projected to expand at a notable CAGR due to increasing awareness regarding eye diseases in developing countries and government initiatives introduced in the region.
Investments by key players is driving the global ophthalmic surgical devices and therapeutics market.
Key players dominating the ophthalmic surgical devices and therapeutics market include Allergan Plc., Johnson & Johnson Services, Inc., F. Hoffmann-La Roche Ltd., Novartis AG, Bausch Health Companies Inc., Regeneron Pharmaceuticals, Inc., Santen Pharmaceutical Co., Ltd., Carl Zeiss Meditec AG, HOYA Corporation, and Bayer AG.
About us:
Transparency Market Research (TMR) is a U.S.-based provider of syndicated research, customized research, and consulting services. TMR’s global and regional market intelligence coverage includes industries such as pharmaceutical, chemicals and materials, technology and media, food and beverages, and consumer goods, among others. Each TMR research report provides clients with a 360-degree view of the market with statistical forecasts, competitive landscape, detailed segmentation, key trends, and strategic recommendations.
Contact us:
Transparency Market Research
90 State Street,
Suite 700,
Albany
NY – 12207
United States
Tel: +1-518-618-1030
USA – Canada Toll Free 866-552-3453
Email: [email protected]
Website: http://www.transparencymarketresearch.com/
0 notes
Text
lupine publishers|Ophthalmic Manifestations of COVID-19 and its Association with Heparan Sulfate Receptors
Ophthalmic Manifestations of COVID-19 and its Association with Heparan Sulfate Receptors
Abstract
Coronavirus disease-2019 (COVID-19) caused by a novel enveloped, positive sense, single stranded RNA virus called Severe
Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) started originally in Wuhan, China. By March 2020, the disease was
declared a global pandemic as the virus spread to all major countries in the world. Initially, it was believed that the virus was
transmitted through inhalation of respiratory droplets from an infected person. But given the exponential increase in the number
of infected people, more modes of transmission were explored. While all possible routes of transmission of this virus are still
undetermined many studies implicate the eyes as the initial site of infection and conjunctivitis as an early symptom of COVID-19.
In this review, we summarize various studies that suggest SARS-CoV-2’s presence on ocular surfaces and that the eyes can be a
gateway for transfer of SARS-CoV-2 to the extraocular sites including the lungs. We also explore the role of heparan sulfate, a newly
discovered co-receptor for the virus in ocular manifestations.
Keywords: SARS-CoV-2; COVID-19; Ocular; Heparan Sulfate; ACE 2; Conjunctivitis
Introduction
Coronaviruses (CoV) are a large family of enveloped RNA
viruses. Structurally, a typical virion consists of envelope proteins
and spike proteins protruding from its envelope surrounding the
nucleocapsid. The spike proteins play an important role in binding
to host cells. These viruses cause severe respiratory and enteric
infections in humans as well as animals. A newly discovered strain,
severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is
responsible for the ongoing global outbreak of coronavirus disease
2019 (COVID-19) [1]. Initially pneumonia, cough and respiratory
problems were the only reported symptoms for COVID-19 [2]. But
there have been many reports of inflammation and irritation of
eye in COVID-19 patients. While conjunctivitis or pink eye has not
been established as an official symptom for COVID-19, few studies
indicate it as an ocular manifestation of SARS-CoV-2 infection [3, 4].
To provide some history, a study conducted during the 2003 Severe
Acute Respiratory Syndrome (SARS) outbreak detected SARS-CoV
in tear samples of SARS patients in Singapore [5]. Insufficient eye
protective equipment was considered to be one of the reasons
for SARS-CoV transmission, indicating a concern that respiratory
illness could be transmitted through ocular secretions [6,7]. Similar
alarming situations have been raised with SARS-CoV-2 especially
amongst the healthcare professionals involved with eye care and
the healthcare workers present in the triage area and involved
with checking symptoms of the patients and sample collection
[8]. This also puts ophthalmologists and other healthcare workers
at risk who are examining the COVID-19 patients manifesting
conjunctivitis. An Ophthalmologist, Li Wenliang, MD died because
of COVID-19. The source of transmission of the virus was later
found out to be an asymptomatic glaucoma patient who visited
his clinic [8]. COVID-19 is normally believed to be transmitted by
respiratory droplets [9]. However, some growing body of evidence
links conjunctivitis to the early stages of COVID-19 infection [4].
The ocular surface might also act as a point of entry and facilitate
coronavirus transmission. Thus, to combat a global threat like
COVID-19 with many asymptomatic patients, it is imperative to
understand these other unexplored pathways for infection and the
underlying mechanisms.
SARS CoV-2 Host Cell Entry
SARS-CoV-2 entry into the host cell is mediated via its spike
glycoprotein S. The spike uses angiotensin-converting enzyme 2
(ACE2) as its receptor on host cells to facilitate the infection as a
primary receptor [10]. SARS-CoV-2 spike protein binds with both
cell surface heparan sulfate receptor and angiotensin-converting
enzyme 2 (ACE2) by binding with its receptor-binding domain
(RBD). Docking studies suggest a heparin/heparan sulfate-binding
site adjacent to the ACE2-binding site. Both ACE2 and heparin can
bind independently to spike protein in vitro, and a ternary complex
can be generated using heparin as a scaffold. Electron micrographs
of spike protein suggest that heparin enhances the open
conformation of the RBD that binds ACE2. On cells, spike protein
binding depends on both heparan sulfate and ACE2 [11]. In a study
conducted by Wan and co-workers, it has been shown that the S
glycoprotein of SARS-CoV-2 has a receptor binding domain (RBD)
and the residue 394 (Glutamine) is responsible for binding with
ACE2 receptors [12]. The S glycoprotein is activated by proteolytic
cleavage by transmembrane serine protease (TMPRSS2) or the
protease Furin (also known as Paired Basic Amino Acid Cleaving
Enzyme) for interaction with ACE2 [13]. In TMPRSS2-negative
cells, the cysteine proteases cathepsin B/L can facilitate S protein
cleavage [14]. Furin acts by cleaving S1 subunit of spike protein
which leads to conformational changes in S2 subunit of the spike
protein. These changes expose the membrane proteins needed for
virus to fuse with membrane to enter the cell as represented in
Figure 1[13]. Certain human coronaviruses like HCoV-NL63 need
co-receptor such as heparan sulphate (HS) in addition to ACE on
host cell membrane for the virus to bind and facilitate its entry into
the host cell. HS has also been indicated to play an important role in
SARS-CoV’s ability to infect [15]. Studies show reduction in heparin
or heparinase leads to decrease in SARS-CoV entry in cells [16].
SARS-CoV-2 displays conformational changes during binding of the
virus RBD and the host cell heparan sulphate [17].
Ocular Viral Transmission
Globally, governments are trying to impose different
preventative measures to contain COVID-19. All nations are
employing nationwide lockdowns, but epidemiologic data indicate
differences in disease incidence. Some countries have been
successful in flattening the curve whereas even after stay at home
orders, the cases are exponentially rising in some other countries.
This points towards an incomplete understanding of the modes of
transmission. Several studies suggest transmission modes through
aerosols and fomites especially given the high transmissibility
rate and some molecular characteristics of the virus [18]. Thus,
to reduce disease transmission, it is necessary to research into all
possible ways of disease transmission.
Previous studies have demonstrated that the mucosa of the
ocular surface and respiratory tract express identical receptors
for certain respiratory viruses [19-22]. On the basis of the
epidemiological information from earlier Coronavirus infections,
various theories have been anticipated such as:
a) The conjunctiva can act as a site of direct inoculation by
droplets containing virus particles.
b) The nasolacrimal duct acts as a route of virus infection to the
upper respiratory tract.
c) Haematogenic (from blood) infection of the lacrimal glands
[23].
In case of SARS-CoV-2, also a respiratory virus, interaction of its
spike protein with host ACE2 is responsible for viral entry as well
as human-to-human transmission [9,10]. Thus, the expression of
receptor ACE2 on the surface of corneal epithelium and conjunctival
epithelial tissues indicates a plausible role of eye in COVID-19
transmission. But the level of ACE2 expression observed in the
ocular tissues was found to be much lower than the respiratory
and kidney tissues [17]. Also, the binding ability of SARS-CoV spike
protein to the ACE2 expressed on the ocular surfaces was observed
to be weaker than the binding ability with the ACE2 receptors on
the surface of Vero E6 cells in-vitro and the lung tissues in-vivo [20].
In this review, we suggest ocular transmission in addition to
transmission by respiratory droplets, fomites and aerosols as a
mode of SARS-CoV-2 transmission. Respiratory viral infections
leading to development of ocular symptoms have been previously
documented [4]. Scientists have hypothesized a model for eye as a
gateway to transmission of virus to the respiratory tract. According
to the anatomy, the mucosa of the conjunctiva and corneal
epithelium and the upper respiratory tract are connected by the
nasolacrimal duct [19]. When a drop of liquid is inserted into the
eye the liquid is partially absorbed by the cornea and conjunctiva
but mostly is passed into the nasal cavity through nasolacrimal
duct and then transported to the upper respiratory tract including
pharynx and trachea or else it can be taken to the gastrointestinal
tract as shown in Figure 2 [24]. This ocular surface to systemic
transmission hypothesis originally proposed by Belser has been
further corroborated by viral inoculations of adenoviruses and
influenza viruses in the cornea of animal models including mice,
rats and rabbits. And presence of viral loads in tear samples from
these animals have been detected [19]. CoVs can result in a wide
spectrum of ocular infections in animals. The conjunctival swabs
of 90% cats infected with feline CoV (FCoV) had the FCoV antigen.
This indicates the probability of ocular manifestations of SARS-
CoV-2 in patients similar to the CoVs of animals [25]. The potential
of infection through ocular secretions is currently unknown, and it
remains unclear how SARS-CoV-2 accumulates in ocular secretions.
Possible theories include direct inoculation of the ocular tissues
from respiratory droplets or aerosolized viral particles, migration
from the nasopharynx via the nasolacrimal duct, or even
hematogenous spread through the lacrimal gland [26].
For more information about Trends in Ophthalmology Open Access Journal archive page click on below link
https://lupinepublishers.com/ophthalmology-journal/archive.php
For more information about lupine publishers page click on below link
https://lupinepublishers.com/index.php
0 notes
Text
Lupine Publishers | What I have learnt from “Starlight Test”
Trends in Ophthalmology Open Access Journal (TOOAJ)
Editorial
Now I am 76 years old and retired from work years ago and at present I am forgetting not only English but also Japanese, therefore, I am very much curious and unbelievable why nowadays I receive letters of invitation for writing papers. To those invitations from journals, I have declined the offers because of lack of my ability. However, I have moved the letter from Ms. Patricia David just beginning “start each day with grateful heart”. I am aged therefore; each day is very precious, and I am very much thankful for that I was happened to be born not ant nor cockroach but one of the human beings in this beautiful earth.
My Childhood and Youth
When I was a child I enjoyed watching a group of ants working busily to send food to their small house which was just a hole in my garden. At that time, I thought that I was watching them closely however, they could not recognize me as a whole being. I realized functions of eyes are different among creatures. I heard dogs do not have colour vision. When I graduated from university (it is shameful to tell; I graduated from English Literature Department) in 1966, I found the job offer for orthoptists on the bulletin of my university. At that time, there was no occupation named as “orthoptist” in Japan and in 1972, I got a national licence as a certified orthoptist.
Working Days in Nagoya University
I worked as an orthoptist mainly at the Department Ophthalmology Nagoya University School of Medicine for 25 years. I worked under the late Professor Hiroshi Ichikawa (specialty: colour vision) Professor Shinobu Awaya (speciality: strabismus and amblyopia) Professor Yozo Miyake, at present the Director of Aichi Medical University, (specialty: retinal diseases and electro retinogram) The all professors were not only splendid scholars but also very impartial and liberal to the all staffs. I worked under Professor Miyake for the longest. He encouraged us to write papers in English and to apply them to western journals.
Measuring Binocular Visual Field of Patients by Handmade Perimeter Named “Starlight Test”
After busy outpatients’ clinic which usually postponed to around 2 o’clock or later, I used to examine visual acuity and visual field of in patients of the Department of Brain Surgery. Measuring their visual field with Goldman or Humphrey perimeter, I was really surprised that patients of complete hemianopia were not conscious of their visual field loss. I have examined plenty of visual fields of patients; not only intracranial diseases but also glaucoma, retinitis pigmentosa, functional visual field loss of children and I have come to have strong wish to know how they were seeing their surroundings [1-6]. This curiosity induced me to make “starlight test (Figure 1). We also examined strabismus patients whose amblyopia and strabismus had been treated yet still have some residual deviation [2]. The visual field of Figure 2 showed discrepancy in among instruments but the result of starlight test which showed the complete bitemporal hemianopia which was coincided with the result of 10-2 of Humphrey [4]. The reason why they show bitemporal hemianopia at fixation point is in binocular condition, patients with lesions of the optic chiasm is caused by the compression of the decussating optic nerve fibers resulting in the loss of overlapping visual field at fixation point.
Working as a Teacher
After retirement from Nagoya University at age of 60, I was offered from Department of Orthoptics and Vision Science, Aichi Shukutoku University in Nagoya city as a teacher and worked there until 70. As I got research expenditure from the University, I acquired the copyright for “30 cm Visual Filed Card ”which was supplement of the book entitled “Neurological Ophthalmology for clinical use (309 pages) written by Fujino Tei published by Igaku shoin Tokyo, 2001 and distributed all students and let them examine their visual fields by themselves, I made not only white cards, but also, red, green, yellow, blue cards too (Figure 3).
My Message to Readers
VISION 2020 is the worldwide campaign of the WHO started in 1999. The aim of campaign is to eliminate the main causes of all preventable and treatable blindness by the year 2020. For this purpose, I would like to suggest using stereo tests for screening. Stereo tests are easy, cost effective tests which able to examine from 3 years old to the aged. Among the stereo tests I recommend the Lang stereo test I, or II which need not to use glasses and less of false positive (Figure 4). The tests define the examinees have normal binocular vision or not. In my study [3], in patients from optic chiasmal lesions, before surgery, 3 out of 13 patients (23.0 %) passed the Lang and after surgery, 9 out of 13 (69.2%) patients passed the Lang. I believe simple Lang tests are able to save people not only from blindness but also their lives.
For more information about Trends in Ophthalmology Open Access Journal (TOOAJ)
Please Click Here: https://lupinepublishers.com/ophthalmology-journal/archive.php
4 notes
·
View notes
Text
Lupine Publishers | Intravitreal Injection of Ranibizumab in Macular Edema Secondary to Retinal Vein Occlusion
Trends in Ophthalmology Open Access Journal (TOOAJ)
Abstract
Aim: This study aimed to evaluate the safety and efficacy of intravitreal Ranibizumab 0.5mg in the treatment of macular edema secondary to retinal vein occlusion.
Patients & Methods: This was a prospective interventional analytical study included 39 eyes of 39 patients with retinal vein occlusion. Ophthalmic examination included assessment of visual acuity, measurement of intraocular pressure, and fundus examination. All patients were scanned using Swept source optical coherence tomography (3D DRI OCT Triton [plus], Topcon Corporation, Tokyo, Japan) to assess central macular thickness. The changes of visual acuity, IOP, and central macular thickness were assessed. Data were analyzed via Kolmogorov-Smirnov test and Wilcoxon signed rank.
Results: The mean age was 56.56 ± 9.6, 48.7% were male and 51.3% were females. Hypertension was detected in 69.2%, and hyperlipidemia in 2.6%. The mean best corrected visual acuity was 1.5 logMAR, 1.00 logMAR,1.00 logMAR, preoperative, fourth month, six months postoperative, respectively, (p<0.001). The mean central macular thickness was 675 μ, 306 u, 264 u, preoperative, fourth month, six months postoperative, respectively, (p< 0.001). The OP was 16.5 mmHg, 16.9 mmHg, 17.1 mmHg, preoperative, fourth month, six months postoperative, respectively, (p=0.423). There were no observed significant ocular adverse events such as ocular inflammation, sterile and infectious endophthalmitis, or sustained increase in intraocular pressure with the use of intravitreal ranizumab injections.
Conclusion: Intravitreal Ranibizumab injections as monotherapy have shown promising results with BCVA improvement and a decrease of central macular thickness in patients with macular edema secondary to retinal vein occlusion.
Keywords: Ranibizumab; Macular Thickness; OCT; Visual Acuity
Introduction
Retinal vein occlusion (RVO) is the most common retinal vascular disease after diabetic retinopathy [1]. Depending on the area of retinal venous drainage effectively occluded it is broadly classified as either central retinal vein occlusion (CRVO), hemispheric retinal vein occlusion , or branch retinal vein occlusion (BRVO) [2]. Although the exact etiology of RVO remains elusive, it is likely to follow a thrombotic event. In CRVO this may occur in the central retinal vein (CRV) at the lamina cribrosa or at a variable distance in its journey within the optic nerve posterior to the lamina cribrosa [2]. Hypoxia-induced expression of vascular endothelial growth factor (VEGF) is thought to be a trigger for macular edema. High intravitreal levels of VEGF have been found in patients with retinal vein occlusion [3]. Upregulation of VEGF is associated with breakdown of the blood-retina barrier with increased vascular permeability resulting in retinal edema, stimulation of endothelial cell growth, and neovascularization [4,5]. Macular edema leads to vision loss in many patients with either central or branch retinal vein occlusions (CRVO or BRVO). BRVO is the more common of the two presentations, accounting for approximately 80% of RVO [6].
Recently, there has been interest in the use of vascular endothelial growth factor (VEGF) inhibition in the treatment of RVO because of the observation of increased VEGF in the vitreous and aqueous of patients with these conditions [7].
Patients and Methods
Study Population
This was a prospective interventional analytical study conducted at Mansoura ophthalmic center, Mansoura university. The study protocol approved by medical research ethics committee, faculty of medicine, Mansoura University (code number: MS/16.02.108). Informed consent was obtained from each participant in the study after assuring confidentiality.
Inclusion criteria
Included patients older than 18, both gender, patients with clinically significant macular edema secondary to retinal vein occlusion and central macular thickness (CMT) was > 250 um by optical coherence tomography.
Exclusion Criteria
Included patients with macular scar, macular hole, uveitis, neovascular glaucoma, age related macular degeneration, diabetic macular edema, patients had undergone treatment for macular edema secondary to retinal vein occlusion triamcinolone and vitrectomy. Also, patient has relevant malignant systemic disease, and media opacity that does not permit optical coherence tomography acquisition with good signal strength were excluded.
Ocular Examination
All subjects underwent an ophthalmic examination including assessment of visual acuity using Snellen chart at 6 meter distance and converted to log MAR, anterior segment evaluation using slit lamp biomicroscope (Haag Streit BP 900) (Haag-Streit, Koeniz, Switzerland), refraction using auto-refractometer (Topcon , KR- 800), intraocular pressure (IOP) measurement using Goldman applanation tonometry, Fundus examination using slit lamp bio microscopy using non-contact Volk lens +78 D or +90 D, Ocular coherence tomography imaging for CMT (central macular thickness).
Swept Source OCT Imaging
Three dimensional deep range imaging OCT Triton Plus (3D DRI OCT TRITON [plus],Topcon Corporation, Tokyo, Japan) with a high speed of 100,000 axial scans/s and center wavelength of 1,050 nm (version 10.07),digital and optical axial resolution of 2.6 μm and 8 μm in tissue , respectively and transverse resolution of 20 μm. The steps of scanning were done as follows, Mydriatic ( tropicamide 1%) eye drop used to achieve a pupil dilatation to assure maximal OCT signal and analysis in patients prior to OCT examination. The patient’s chin was positioned in the chin rest. The patient was asked to fixate on a target point inside the instrument the phase is completed by a camera, located inside the instrument that displays the fundus and scan beam. After the patient scanning was finished, analysis protocol was used to obtain circular maps on the macula.
The steps of OCT imaging were done as follows:
• Mydriatic eye drops Swixolate (Cyclopentolate Hydrochloride 10mg/ml CHEMIPHARM) eye drops three times within 30 minutes were used to achieve as much pupil dilatation as we can to assure maximal OCT signal and analysis in patient’s eyes prior to OCT examination.
• The patient’s chin was positioned in the chin rest.
• The patient was asked to fixate on a target point inside the instrument the phase is completed by a camera, located inside the instrument that displays the fundus and scan beam.
• After the patient scanning was finished, analysis protocol was used to obtain circular maps on the fovea (Figure 1).
Interpretation
Macular thickness was reported according to Early Treatment of Diabetic Retinopathy Study. Early Treatment Diabetic Retinopathy Study ring is a 6μm macular thickness map centered on the foveola that divided the macula into nine regions. It was divided into three rings, with the central ring corresponding to the fovea (1 μm diameter), the middle ring corresponding to the parafovea (2μm diameter), and the outer ring corresponding to the perifovea (3μm diameter) and then divided into four quadrants, namely superior, nasal, inferior and temporal except for the central circle (Figure 2). Central macular thickness (CMT; foveal thickness) was defined as the average macular thickness in the central 1 μm, average macular thickness was defined as the mean of thicknesses in nine regions, and macular volume was defined as the sum of volumes in all nine regions. The macular retinal map divides the region into a central area with a radius of 500 microns, and two concentric rings inner parafoveal ring and outer perifoveal ring which were divided into four quadrants. The analysis program reports the corresponding mean thickness in each of the areas using assigned colors to indicate retinal thickness in the region under analysis. The analysis program reports the corresponding mean thickness in each of the areas using assigned colors to indicate retinal thickness in the region under analysis.
Intravitreal Injection of Ranibizumab
Treatment protocol
Ranibizumab (0.5mg, 0.05mL) was injected intravitreally under complete sterile conditions via the pars plana once monthly for 3 months.
Treatment procedure
Intravitreal injections were carried out, under aseptic conditions at mansoura ophthalmic center operating theater.
Preoperative preparation
Prophylactic topical antibiotic (Vigamox ED Q.I.D) on the day before the operative day. Pupil dilatation: One hour before surgery the pupil was dilated with cyclopentolate Hcl 1% every 10 minutes for half an hour preoperatively.
Preparation and Administration
Ranibizumab (Lucentis) (Genentech/Roche, USA) is supplied as a preservative-free, colorless to pale yellow, sterile solution placed in a single-use glass vial. The dose is 0.5mg dose vial (delivers 0.05mL of 10mg/mL Ranibizumab). Lucentis should be inspected visually for particulate matter and discoloration prior to administration. The contents of a vial of ranibizumab should be drawn using a 19-gauge filter needle. A sterile small gauge x ½ inch-needle should replace the filter needle for the injection.
Follow Up
Follow-up was one day and one week after injection and then every month for six months.
Outcomes
Outcomes included BCVA (functional response) and central foveal thickness (anatomical response),IOP and complications. Patient response were classified according to change in BCVA into good response in patients gaining more than 2lines on Snellen chart, moderate response in patients gaining less than 2lines and poor response in patients showing stable vision on chart with improvement of vision .
Statistical analysis
Data were analyzed with Statistical Package for the Social Sciences (SPSS) software package version 24.0 (Armonk, NY.IBM Cor).The normality of data was first tested with one-sample Kolmogorov-Smirnov test. Qualitative data were described using number and percent. Parametric data (normally distributed data) were described as mean (SD), non-parametric (non-normally distributed data) were described as median. Wilcoxon signed rank (for non-parametric data) was used to compare change within the same group pre and postoperative injection. P Level is considered statistically significant <0.05.
Result
Thirty-nine (19 CRVO and 20 BRVO) eyes of 39 patients were enrolled in the study with mean age of 56.56 ± 9.6 (range 24–69). 48.7% were male and 51.3% were females. Hypertension was detected in 69.2%, Hyperlipidemia in 2.6%. The mean best corrected visual acuity was 1.5 log MAR, 1.00 log MAR,1.00 log MAR, preoperative, fourth month, six months postoperative, respectively, (p< 0.001) (Table 1) ( Figure 3). The mean central macular thickness was 675μ, 306 u, 264 u, preoperative, fourth month, six months postoperative, respectively, (p< 0.001) ( Table 2) ( Figure 4). The OP was 16.5 mmHg, 16.8 mmHg, 16.5 mmHg , preoperative, fourth month, six months postoperative, respectively, (p=0.423). The mean BCVA in branch retinal vein occlusion is nearly the same in central retinal vein occlusion pre and postoperative while preoperative CMT is significantly higher in central retinal vein occlusion than branch retinal vein occlusion while postoperative there was significant improvement in CMT in both central and branch retinal vein occlusion but no statistically significant difference between both. The mean IOP in branch retinal vein occlusion is nearly the same in central retinal vein occlusion pre and postoperative with no statistically significant difference (Table 3).
Declarations
Ethics approval and consent to participate; This interventional study was approved by the ethics committee of Faculty of medicine, Mansoura university (Registration Number: MS/16.02.108), Date:) and adhered to the tents of Declaration of Helsinki. All subjects provided written informed consent prior to study participation.
For more information about Trends in Ophthalmology Open Access Journal (TOOAJ)
Please Click Here: https://lupinepublishers.com/ophthalmology-journal/archive.php
4 notes
·
View notes
Text
Lupine Publishers | A Review of Metabolic Sensors in Glaucoma
Trends in Ophthalmology Open Access Journal (TOOAJ)
Abstract
Glaucoma is the second leading cause of irreversible blindness worldwide. It is a multifactorial, progressive, chronic optic neuropathy that is characterized by loss of retinal ganglion cells (RGC) and optic nerve head (ONH) cupping including extra cellular matrix (ECM) remodelling and fibrosis at the lamina cribrosa (LC). Clinically this results in chronic, progressive peripheral visual field loss. The pathogenesis of glaucoma is not yet fully understood. Therefore, there is an urgent need to identify and target the underlying mechanisms governing ECM remodelling of the LC, in order to stop the progressive, chronic damage to the LC/ONH and irreversible visual field loss. This review identifies and examines some of the key metabolic processes and cellular sensors involved in the pathogenesis of ECM fibrosis in general but herein specifically in glaucoma, including mitochondrial dysfunction and adenosine monophosphate activated protein kinase (AMPK) upregulation. Furthermore, the development of novel therapeutics such as nicotinamide (NAM) and metformin are discussed as promising potential future therapeutic options for glaucoma.
Keywords: Glaucoma; Fibrosis; Extracellular Matrix (Ecm) Mitochondrial Dysfunction; Adenosine Monophosphate Activated Protein Kinase (Ampk); Nicotinamide (Nam); Metformin
Introduction
Glaucoma is the second leading cause of irreversible blindness worldwide. More than 67 million people are affected by glaucoma, which has a global prevalence of 3.5% in persons over the age of forty years [1]. Glaucoma is heterogenous group of progressive optic neuropathy disorders resulting in loss of peripheral field vision. The primary risk factor associated with the development of glaucoma is elevated intraocular pressure (IOP). Currently, lowering IOP is the only pharmacological treatment available for managing glaucoma [2]. However, there is a subset of glaucoma patients with normal IOP. Studies have shown that normal tension glaucoma (NTG) accounts for approximately 30% of all patients diagnosed with glaucoma [1]. This poses a significant treatment obstacle, as the efficacy of IOP lowering drops is highly variable among this cohort of NTG patients [3]. The major clinical presentations of glaucoma include cupping and pallor of the ONH. Glaucoma is characterized by loss of retinal ganglion cells (RGC) and optic nerve head (ONH) cupping [3]. This dysfunction occurs in the cells of the lamina cribrosa (LC) region, which is a three-dimensional (3D), fenestrated, mesh like structure located in the ONH. Under normal circumstances, the LC functions as a structural support to unmyelinated RGC axons as they pass through posteriorly, before exiting the eye to the brain, becoming the optic nerve [4,5]. The LC is a biomechanically weaker structure when compared to the rest of the sclera and is thereby the putative site of RGC damage in glaucoma. Laminar cupping is connective tissue-based, with the LC progressively moving posteriorly and excavating beneath the anterior sclera canal leading to remodelling of extracellular matrix (ECM), stiffness and consequently fibrosis of the LC connective tissue in the ONH [3], which is driven by profibrotic growth factors such as transforming growth factor- beta (TGFβ) [6] and backward bowing. This results in optic nerve axon compression, axonal loss and, ultimately, chronic, progressive peripheral visual field defects [7].
The cellular mechanisms involved in glaucoma are not fully understood. Understanding these processes will lead to new methods of preventing chronic glaucomatous vision loss when conventional IOP-lowering treatments either fail to prevent progression (up to 20% of glaucoma patients continue to progress to blindness) [5], or adequate target pressures cannot be achieved due to ineffectiveness of or poor tolerance to medication. Thus, there is an urgent need to identify and target the underlying mechanisms of metabolism governing remodelling of the LC, in order to stop the progressive, chronic damage to the LC/ONH and irreversible visual field loss. This review aims to identify and examine some of the key metabolic processes and cellular sensors involved in the pathogenesis of fibrosis in glaucoma and investigate potential therapeutic options.
Fibrosis
Whilst the pathogenesis of glaucoma has yet to be fully elucidated, it is known that connective tissue fibrosis is one of the major pathological drivers of the disease. The term fibrosis is defined as the process of unchecked wound healing [8]. Fibrosis is involved in the pathogenesis of many systemic diseases involving multiple tissue and organ systems such as the heart, liver, lungs and kidneys. Fibrosis results in chronic, progressive, pathological destruction of tissue and organ function [9,10]. The normal wound healing response of tissues to damage is a highly complex process, involving activation of the coagulation cascade, inflammation, angiogenesis, cellular proliferation and tissue remodelling [10]. Activated fibroblasts, known as collagen producing myofibroblasts that are highly contractile, drive the wound healing response to an acute injury by remodelling extracellular matrix (ECM) resulting in the restoration of tissue integrity and previously damaged parenchymal cells [11-12]. This normal wound healing process becomes dysregulated and uncontrolled in states of chronic inflammation, recurrent or repetitive injury or chronic hypoxia, resulting in tissue fibrosis. The ECM is composed primarily of fibrous proteins (primarily collagens, glycoproteins such as fibronectins and vitronectins, and laminins) and proteoglycans [11]. ECM provides structural and biochemical support to cells and tissues in multicellular organisms, in addition to functioning biochemically as a substrate for cell adhesion, growth and differentiation. Thus, ECM is essential for normal connective tissue structure, architecture, differentiation, and homeostasis [14].
Fibrosis in Glaucoma
Fibrosis is characterized by a pathological deposition and accumulation of ECM by myofibroblasts. It is already known that there is an excessive accumulation of ECM in glaucomatous LC tissue, trabecular meshwork (TM) cells and Schlemm’s Canal [11], which results in ONH remodelling and damage. In response to elevated IOP, the ECM genes of glaucomatous LC cells become structurally stiffer and less compliant than normal LC cells, thereby acting as a pro-fibrotic driver of disease [12-15]. ECM stiffness is also a hallmark of tissue ageing. It is known that aged tissues display decreased levels of proteins cadherin and catenin, thin basement membranes and apoptotic resistant, senescent fibroblasts which release fibronectin, matrix metalloproteinases (MMPs) and pro-fibrotic cytokines [13]. Furthermore, aged tissues display a defective upregulation of cross-linked collagen fibres which drives tissue stiffness and rigidity [12], and older age is a significant risk factor for glaucoma. Several other pro-fibrotic mediators are overexpressed in glaucoma, including cytokine transforming growth factor ß (TGFß) and thrombospondin-1 (TSP-1) [3]. TGFß, which is present in the aqueous humour, is a pro-fibrotic cytokine that induces the differentiation of fibroblasts to their collagen secreting form, myofibroblasts. TGFß controls ECM synthesis and activates ECM through the signal transducer family Smad proteins [16,17]. When activated, Smad proteins translocate to the nucleus where they function to regulate gene transcription [13,15]. Our group has shown that LC cells from glaucoma donors [9] have many characteristics of myofibroblasts including the expression of α-SMA, and a marked expression of pro-fibrotic ECM genes and proteins (e.g. collagen 1A1, periostin, fibronectin) upon stimulation with TGFβ [10], cyclic stretch11, and oxidative stress [12]. In another study, we found an increase of F-actin stress fibres (indicating enhanced cellular reorganisation) and increased substrate stiffness elicits a myofibroblastic phenotype in human LC cells [13,14].
Mitochondrial Dysfunction in Glaucoma
Mitochondria, commonly known as the ‘powerhouse’ of the eukaryotic cell, are cellular organelles responsible for the energy production of the cell, and the regulation of cellular metabolism [18]. Mitochondria produce adenosine triphosphate (ATP) primarily through oxidative phosphorylation (OXPHOS), in addition to glycolysis and the Krebs cycle (citric acid cycle). Energy disruption, particularly mitochondrial dysfunction, which results in the toxic accumulation of reactive oxygen species (ROS) within cells has been studied in several disease models over the past decade including cancer, diabetes, and neurodegenerative diseases including Alzheimer’s Disease, muscular dystrophy [19]. A number of studies have examined the role of mitochondrial dysfunction in both human and animal models of glaucoma.
Mitochondrial Dysfunction Studied in Glaucomatous TM Cells
TM cells in glaucomatous human POAG patient eyes were shown to have dysfunctional and defective mitochondria, which resulted in uncontrolled, elevated IOP. These TM cells were more also more vulnerable to Ca2+stress when compared to healthy aged, matched controls, and authors postulated that this vulnerability contributes to sustained, chronic rise in IOP [20]. A recent study of a cohort of ocular hypertensive patients with a longstanding history of raised IOP (‘susceptible’), but whom had never developed glaucoma was performed. Lascaratos etl al found that the ‘susceptible’ patient cohort with ocular hypertension demonstrated both higher levels of mitochondria and ADP phosphorylation, and were better able to withstand and manage cellular stresses such as oxidative stress and excess calcium, versus patients with glaucoma and aged matched controls [21]. They concluded that enhanced mitochondrial activity in a systemic capacity confers protection to the development of RGC damage, ON damage and ultimately the development of glaucoma in addition to identifying mitochondria as a disease biomarker [21]. It has been shown via electron microscope analysis that mitochondria found in the ON in glaucomatous eyes are notably smaller and fewer when compared to normal age matched eyes [22,23] Furthermore, studies have demonstrated a reduced number of cristae within mitochondria, which means cells contain less tools to perform effective OXPHOS. Consequently, cells possess lower and deficient energy capacity [19,23]. This has a direct downstream effect on axonal survival in circumstances such as glucose depletion. Axons require functional mitochondria in order to survive on lactate, which normally bypasses the process of glycolysis on conversion to pyruvate. However, it has been demonstrated in glaucomatous optic nerves that mitochondria are not capable of effective regeneration, thereby leading to downstream axonal death [22].
Mitochondrial Dysfunction Studied in Glaucomatous Retinae
In glaucoma, defective mitochondrial function is associated with both disease susceptibility and disease resistance [19]. In fact, in vivo studies of mice have demonstrated mitochondrial dysfunction to be one of the primary detectable features of stressed RGC’s in response to elevated IOP [24]. Inman et al. demonstrated that defective mitochondrial DNA and metabolic dysregulation occur prior to evidence of neurodegeneration [19]. It is established that RGC’s require a large quantity of ATP due to the dense axonal volume of mitochondria surrounding the OHN. Mitochondrial dysfunction in RGCs, which results in defective cellular repair process thereby enhances their susceptibility to apoptosis and subsequent glaucomatous pathogenesis [25]. Harun et al. studied DBA/2J mice models and showed that monocarboylate transporters (MCT), which function as lactate and ketone transportation molecules, are under expressed in glaucomatous retinae, and result in decreased ATP production [26] Mice received an injection of MCT2 (AAV2:MCT2) in order to restore MCT2 to normal cellular levels, and it was shown that RGCs were preserved in this group of mice. Importantly, following the induction of MCT2 overexpression in DBA/2 J retinae via AAV2:MCT2 injection, mitochondrial function in the retinae of these mice improved. Additionally, an increase in RGC density and an enhancement of energy homeostasis were also noted in DBA/2J mice versus the untreated cohort. This study demonstrates both the neuroprotective effect of MCT2 on glaucomatous RGCs, in addition to highlighting the potential therapeutic benefit enhanced cellular energy input may have in glaucoma treatment in the future [26].
Mitochondrial Dysfunction in Blood Analyses of Glaucoma Patients
Mitochondrial dysfunction in lymphocytes of a cohort of primary open angle glaucoma (POAG) patients has been examined [27]. Lee et al. analysed ATP production and cellular respiration in POAG patients and found that POAG lymphoblasts displayed decreased levels of complex 1-driven ATP synthesis and complex-1 driven maximal respiration when compared to controls. Complex 1 (NADH: ubiquinone oxidoreductase), whose role is electron transport, is the biggest enzymatic complex of the mitochondrial respiratory chain [28]. There was no difference in complex-2 linked respiration between the two groups, nor was there any difference in ATP production when cells were grown on galactose media (thereby reliant on mitochondria OXPHOS [27]). Similarly, another recent study conducted a comparative analysis of mitochondrial OXPHOS complex-1 dysfunction in patients with Leber Hereditary Optic Neuropathy (LHON) when compared to POAG patients. LHON is a mitochondrially inherited disorder involving complex-1 mutations, and is characterized by the quick, aggressive and irreversible loss of RGCs [29]. POAG, LHON and normal lymphoblasts were cultured on galactose media, and the growth rates of the groups were examined. POAG lymphoblasts and LHON lymphoblasts grew 1.47 and 2.35 times slower than control lymphoblasts. Furthermore, when compared to controls, POAG lymphoblasts demonstrated an 18% reduction in complex-1 activity, versus a 29% decreased in LHON lymphoblasts. Finally, when complex-1 ATP synthesis between the groups was compared to control samples, a 19% reduction was noted among the POAG group whereas a 17% decrease was observed in LHON patients [29]. This study demonstrates OXPHOS impairment in both POAG and LHON patients and proposes that the milder dysfunction of the POAG group versus LHON patients might reflect a less aggressive nature and progression of glaucoma. Finally, this study highlights the potential role of restoring mitochondrial function as a promising therapeutic target for diseases characterized by mitochondrial dysfunction, including glaucoma. A study using Gene-Set Analyses was conducted on a cohort of POAG and NTG patients to assess mitochondrial gene associations [30]. Khawaja et al. identified a strong association between POAG and lipid metabolism pathways (P<0.002) and butanoate metabolism, which is a carbohydrate metabolism pathway (P<0.004). This study demonstrates an important role of lipid and carbohydrate metabolism in the disease pathogenesis of POAG.
Mitochondrial Dysfunction in Glaucomatous LC Cells
Our group has demonstrated that glaucoma LC cells proliferate at a higher rate than normal LC cells [15] and show mitochondrial dysfunction [16]. Kamel et al. conducted a detailed mitochondrial bioenergetic assessment on normal and glaucoma human LC cells [31] which revealed significantly abnormal mitochondrial respiratory bioenergetic function in human glaucoma LC cells when compared to controls. Decreased ATP production at basal levels, reduced OXPHOS and increased glycolysis were observed. Furthermore, MCT1 (OXPHOS marker), MCT4 (glycolysis marker), MTHFD2 (folate-mediated one-carbon metabolism marker), and GLS2 (glutaminolysis marker) were overexpressed in the glaucoma patient cohort. Thus, the findings of this study indicate that glaucoma cells undergo a process of ‘metabolic reprogramming’, and essentially switch from OXPHOS to aerobic glycolysis. This phenomenon is known as ‘the Warburg effect’, and it is a well-known, longstanding feature of neoplastic cells and cancer associated fibroblasts (CAF) [32,33].
The Role of Nicotinamide (NAM) in Glaucoma
NAD+ is activated by caloric restriction, fasting, exercise and AMPK. NAD+ is metabolised to nicotinamide (NAM) by NAD+ consuming enzymes such as CD38, Sirtuins and poly adenosine diphosphate ribose polymerase (PARPs). NAM is a water-soluble form of niacin (Vitamin B3). NAM can be converted to nicotinamide mononucleotide (NMN) by nicotinamide phosphoribosyl transferase (NAMPT) and then to NAD+ by nicotinamide mononucleotide adeneylytransferase 1 and 3 (NMNAT 1-3), via the salvage and pathway. Nicotinamide N-Methyl Transferase (NNMT) catalyses the methylation of NAM to N-methyl-nicotinamide (metNAM), which is subsequently metabolised further to N1-methyl-2-pyridine-5-carboxamide (2py) or N1-methyl-4-ppyridone-3-carboxamide (4py) utilizing the methyl donor S-adenosyl methionine (SAM) from the methionine cycle. 2py and 4py are the primary metabolites of NAM. NAM in reversing or halting disease pathogenesis. For example, NAM supplementation studied in obesity models in mice resulted in reduced oxidative stress and inflammation as well as repleted glycogen storage capacity [34]. NAM supplementation however, had no direct effect on lifespan, rather it enhanced healthspan [34].
The potential role of bioavailable NAM as a drug therapeutic target has been studies in animal models of glaucoma [24]. Williams, et al. studied DBA/2J mice models and showed that nicotinamide has a neuroprotective role in glaucoma. In glaucoma, reduced levels of NAD+, mitochondrial damage and glutathione depletion result in fragile, vulnerable RGCs. A single molecule of low dose NAM (NAMLo), high dose NAM (NAMHi) and finally NMNAT gene therapy was administered [24]. NAMLo mice demonstrated neuronal protection against glaucoma development, with no mitchondrial dysfunction, and decreased levels of DNA damage observed. NAMLo had no impact on IOP levels. 93% of NAMHi mice displayed no cellular signs optic nerve damage. Furthermore, NAMHi had a protective effect on IOP levels. This study implies that NAMHi confers not only a protective effect against glaucoma development but a protective effect on cellular types other than RGCs [24]. Another recent study led by Hiu, et al. demonstrated an improvement of inner retinal function in glaucoma patients following the administration of NAM supplementation [35]. They conducted a randomised control trial of fifty-seven patients with known, well controlled glaucoma. Patients were commenced on a regimen of NAM over three months. (1.5g/day for 6/52 followed by 3.0g/day for 6/52). Photopic negative response (PhNR) which is an electroretinogram (ERG) parameter was used as the measurement of inner retinal function (Saturated PhNR amplitude = Vmax). The study found that Vmax improved by 14.8%(p=0.02) in patients receiving NAM versus 5.2% (p=0.27) in the placebo group. When comparing visual field (VF) mean deviation (MD) 27% of patients on NAM improved by ≥1dB, and additionally fewer patients on NAM demonstrated any worsening of VF (4%), versus the control group (p=0.02). This study further highlights a promising potential for NAM supplementation in the treatment of glaucoma, although it is clear that further studies must be performed on a larger scale in order to fully elucidate the effectiveness and determine the long term safety of NAM in glaucoma therapy.
Nicotinamide adenine dinucleotide (NAD+) is found in the cytoplasm, mitochondria and nuclei of eukaryotic cells [36]. NAD+ plays a central role in the regulation of several biological processes including metabolism, cell signalling, DNA repair and cellular longevity [37]. Reduction in NAD+ levels have been associated with several age-related diseases, including carcinoma, cardiovascular disease (CAD), neurodegenerative and metabolic disorders [38]. NMNAT2, an enzyme producing NAD is essential for RGCs, healthy axons and in the prevention of axonal degeneration [39]. NMNAT2 is a survival factor necessary for axon survival. NMNAT2 null mice demonstrate truncated RGC axons and have no optic tract. Furthermore, siRNA knockdown of NMNAT2 results in the degeneration of neurons despite the absence of injury [39]. Mice were injected with AAV2.2 which contained the Nmnat1 gene. >70% of mice treated with this vector were found to have no clinical or pathological signs of optic nerve damage. Finally, mice were treated with both Nmat1 gene in addition to NAMLo. 84% of mice receiving this combination therapy were free of any glaucomatous damage, therefore it is postulated that a combination therapy confers additional protection and reduces vulnerability of the RGC cells of the LC to glaucomatous changes [24]. A number of studies have examined the potential therapeutic role of NAM in Parkinsons Disease (PD) patients. One mouse model study conducted by Harrison et al. showed that NAM administration improved locomotor responses and lessened dopamine depletion, thereby demonstrating a neuroprotective role for NAM [40]. Conversely, however, other studies have shown that NAM is associated with PD and exacerbates neurodegeneration [41]. Interestingly, levels of NNMT and metNAM were found to be raised in PD brains [42]. These conflicting reports warrant further analyses and studies in order to accurately elucidate the role of NAM in PD and neurodegenerative diseases.
Nicotinamide N-Methyl Transferase (NNMT)
Nicotinamide N-Methyl Transferase (NNMT) is a cytosolic enzyme that is expressed at the highest level in the liver [40]. NNMT catalyses the methylation of NAM to N-methyl-nicotinamide (metNAM), which is subsequently metabolised further to N1-methyl-2-pyridine-5-carboxamide (2py) or N1-methyl-4-ppyridone-3-carboxamide (4py) utilizing the methyl donor S-adenosyl methionine (SAM) [37,40] [Figure 1]. NNMT eliminates NAM from the NAD+ synthesis pathway, resulting in depleted levels of NAD+. NNMT is expressed in several tissues such as the heart, brain, kidney and muscle, and its upregulation and overexpression has been linked with various disease pathogenesis such as cancer, metabolic, neurodegenerative and inflammatory disorders [37,43]. Furthermore, there have been several associations between high levels of SAM, which is a homocysteine precursor, and insulin resistance and cardiovascular disease (CAD) [44,45]. Importantly, high levels of serum NNMT and NAM are associated with increased severity of CAD [46]. In mice models, techniques such as genetic knockdown and drug inhibition of NNMT was found to be protective against obesity and type two diabetes [47]. Authors treated mice with a molecular analogue of NAD (JBSNF000088), which inhibited NNMT activity. Mice treated with the analogue displayed lowered body weight, an improvement to normal glucose tolerance and an improvement in insulin sensitivity [47].
Future Directions and Conclusion
The cellular mechanisms involved in glaucoma are yet to be fully elucidated. Understanding these processes will lead to new methods of preventing chronic glaucomatous vision loss when conventional IOP-lowering treatments either fail to prevent progression (up to 20% of glaucoma patients continue to progress to blindness) or adequate target pressures cannot be achieved due to ineffectiveness or poor tolerance to medication. Thus, there is a clear unmet need to target the underlying mechanisms governing the progressive fibrotic remodelling of the LC, to halt the progressive and ongoing fibrotic damage to the LC/ONH and visual field loss. It is clear that there are multiple systemic cellular processes at play simultaneously, and when combined, result in the development of glaucoma. Glaucoma may be described as a multifactorial disease entity, and it is likely that in the future, there will be no ‘one size fits all’ therapeutic option. It is evident, however, that mitochondrial dysfunction plays an integral role in the aetiology of glaucoma, and that the dysregulation of this organelle directly results in RGC susceptibility and vulnerability. Several studies have highlighted promising therapeutic targets in halting or even reversing this progression, including nicotinamide, insulin and metformin. AMPK is a highly conserved master regulator of metabolism, both at the cellular and organismal levels, whose function is extremely relevant not only for normal physiology, but also for the understanding of many metabolic diseases [54]. The examination of novel mechanisms of AMPK as the key metabolic sensor in LC cells in glaucoma will be vital to understand the driving force underlying fibrotic changes occurring in the LC. These activated LC myofibroblasts drive the fibrotic processes occurring in the LC. The glaucoma LC cells adapt to their pro-fibrotic role by increasing their proliferation, reducing apoptosis, and augmenting their metabolism. These activated LC myofibroblasts essentially undergo ‘metabolic reprogramming’ to utilise alternative high-energy sources to enhance cellular growth and development. Halting the pro-fibrotic activity and metabolism of glaucoma LC cells by restoring AMPK expression and activity to normal levels, could lead to a new therapeutic approach to reduce fibrosis in glaucoma. In conclusion, glaucoma is a multifactorial, progressive, chronic optic neuropathy. The second leading cause of irreversible blindness worldwide, the development of novel therapeutics to combat this disease is of paramount importance. This review has identified several key metabolic sensors whose dysregulation and dysfunction directly drive and promote disease development and progression. Whilst there have been several potential treatment options investigated for this disease in the last decade, it is clear that further research and clinical trials to fully determine the suitability and effectiveness of therapeutic targets are necessary.
For more information about Trends in Ophthalmology Open Access Journal (TOOAJ)
Please Click Here: https://lupinepublishers.com/ophthalmology-journal/archive.php
4 notes
·
View notes
Text
Lupine Publishers | Functional and Morphological Changes in Diabetic Macular Oedema: Baseline Correlations, and Changes with Pharmacological Treatments
Trends in Ophthalmology Open Access Journal (TOOAJ)
Introduction
Several pharmacologic agents are now available for the treatment of DMO including anti-VEGF agents [1-6] and corticosteroids [1-11]. The introduction and frequency of these treatments has coincided with the introduction of less invasive investigating and monitoring systems including OCT [12-17] and fundus related perimetry, also known as microperimetry (MP) [18, 23]. OCT is now well established in the evaluation of DMO, especially with the recent advances with spectral domain models [1-27]. It has contributed significantly to our understanding of the anatomical changes of DMO and the intra-retinal damage and provides a valuable tool for the follow-up of macular oedema [14]. Carpineto, et al. [22] studied the role of MP in evaluating fixation patterns and retinal sensitivity in patients who had clinically significant macular oedema with a diffuse pattern and type 2 diabetes mellitus. Furthermore, Okada, et al. [21] demonstrated a significant correlation between retinal sensitivity as measured by MP, visual acuity and foveal thickness as measured by OCT in eyes with DMO. Previous studies have also investigated the role of MP and fundus autofluorescence (FAF) in evaluating outcomes in DMO treated with laser photocoagulation and micro pulse laser photocoagulation [18]. More recently, Comyn, et al. [28] reported functional and morphologic changes in eyes treated with ranibizumab or laser photocoagulation in the LUCIDATE Study. Similarly, Reznicek, et al. [29] and Kim, et al. [30] have reported functional outcomes of DMO eyes treated with anti-VEGF therapies. These available MP studies on DMO, however, used the first generation of MP technology (MP-1, Nidek Co; Japan) [18,22] where the analysis of fixation stability was not studied as a main outcome of visual function affected by DMO. A more recent study by Kim, et al. [30] used the spectral OCT/SLO system (Optos OCT SLO, Optos, Scotland).
MP allows for the exact topographic correlation between fundus abnormalities and corresponding functional alterations by integration, with different methods, of differential light threshold (more commonly known as retinal sensitivity) and fundus imaging. The Nidek MP-1 is a mesopic test that requires pupil dilation or a 5–10 min dark light adaptation before starting the examination. The Optos system relied on pupil dilatation and 15-minute dark adaptation used a fixation target in the shape of a cross of 1° size and the MP was performed with Goldmann III size dot stimuli utilising 13 stimulus points and a four to two staircase strategy [31]. More recently, Centervue (Padova, Italy) developed a 3rd generation of MP systems, the Macular Integrity Assessment (MAIA). The greatest advantage of the MAIA is the ease of the operation since it does not require mydriasis; the much lower cost compared to other instruments is an added advantage. It utilizes the Scanning Laser Ophthalmoscope (SLO) technology to image the retina with higher resolution (of 1024 x 1024 pixels) and a more effective eye tracker to monitor the eye movement at 25 times per second improving reliability and usability for operators and patients [18-31]. In addition, the MAIA is the only instrument that offers automatic estimates on PRL characteristics during early and late fixation [31]. This study aims to evaluate the ability of MAIA MP in detecting early changes in retinal function not only with the analysis of retinal sensitivity, but also with the analysis of fixation behaviour in eyes with DMO and investigate their correlation with central macular thickness measured with OCT and visual acuity (LogMAR) at baseline and in 3 months from commencing treatment intravitreal anti-VEGF therapies.
Methods
In a prospective, observational case series study, 23 consecutive patients with clinically significant DMO (Table 1A, 1B) presenting to the practice of WMA in the University Hospital, Queen’s Medical Centre, Nottingham, were recruited into this study from August 2013 to July 2014. This study was approved by the institutional review body (National Research Ethics Service Committee ref: 12/EM/0116; R&D ref 12OY004). Full ophthalmological assessment was done. Informed consent was obtained from all the participants. Subjects received intravitreal injections of ranibizumab (Novartis UK, Frimley Park) 0.5mg in 0.5ml at 4 weekly intervals times 3, and then pro re nata as per NICE TA 237. By implication, all eyes had DMO with foveal thickness of 400 microns or more. Logarithm of the minimum angle of resolution (LogMAR) best-corrected visual acuity (BCVA) was evaluated by means of an Early Treatment of Diabetic Retinopathy Study chart (ETDRS). Foveal thickness was measured with the Topcon 2000 OCT (Topcon, Tokyo, Japan). Age, duration of diabetes, haemoglobin A1c (HbA1c) levels, duration of symptoms, history of previous laser photocoagulation, or vitrectomy were recorded. OCT examinations were analysed for vitreomacular adhesion/traction, and cystoid macular changes were quantified. All the participants were assessed for visual function with the Macular Integrity Assessment MP (MAIA MP) instrument (CentreVue, Padua, Italy). Retina sensitivity (RS) and Fixation stability were assessed with MAIA MP over the central retina (10 degrees) projecting 37 light stimuli points with a, “4-2” projection strategy. The examinations were performed at baseline and months 3 after treatment. Main outcome measures were fixation characteristics and mean retinal sensitivities. The MAIA MP images were exported into the Topcon OCT system through the Topcon import-reference-image software for the manual morphological-functional correlation analysis. As the selected MP grid map measures light sensitivity in the central 3mm of the retina, only the standard internal retinal subfields (central, inner superior, inner nasal, inner inferior, inner temporal) as defined in the Age-Related Eye Disease Study (AREDS) [31] were investigated. The outer OCT subfields were ignored in the current analysis. The statistical analysis was performed with linear regression, Pearson’s product-moment correlation coefficient and two-tailed paired t test, without correcting for multiple comparisons, using GraphPad Prism 6. A p value less than 0.05 was considered statistically significant.
Results
Forty-two (42) eyes of 23 patients with mean age of 65 yearsold (min = 25, max = 91) were recruited into this study. Patient characteristics including age, type and duration of diabetes, haemoglobin A1c (HbA1c) levels, duration of DMO symptoms, and history of previous laser photocoagulation, or vitrectomy are summarised in Table 3 and Table 4. The duration of DMO symptoms/ presence varied from 14 to 60 (average of 30.09 months). LogMAR VAs and OCTs were performed at similar visits. At baseline, MP parameters of mean retinal threshold sensitivity (TS) (Figure 7.1) and fixation stability (FS) (Figure 7.2) demonstrated a wide range of values (TS: mean = 19.27dB, min = 0dB, max = 29.4dB) (FS: mean = 72.4%, min = 11%, max = 100%) at baseline. At baseline, the LogMAR VAs ranged from 0.0 to 0.98. The central macular thickness measured with OCT (central subfield) ranged from 244 to 841 microns at baseline. VA measurements showed higher correlation with functional MP values of TS (r = 0.617) and FS (r = 0.725), than those found with central macular thickness measured with OCT (r = 0.221). These correlations between VA and the MP parameters are presented in Figure 7.3, Figure 7.4, Figure 7.5. The correlation between TS and FS was moderate (r = 0.442), whilst correlation with DMO duration was low as shown in Table 5.
The morphological changes of macular thickness, intraretinal cysts or subretinal fluid (SRF) on OCT decreased in all internal subfields at 3 months with treatment compared to baseline values. In particular the central subfield showed a statistically significant thickness reduction from 445.3 ± 129.9 μ at baseline to 337.4 ± 107.4 μ (p = 0.01). The other OCT internal subfields changes represented in Figure 7.6, also showed statistically significant reductions in thickness (p < 0.05). Changes in intraretinal cysts and SRF also showed significant reduction at 3 months compared to baseline (p<0.05). The LogMAR VA measurements demonstrated an overall improvement over the time (Figure 7.7); however, the changes were not statistically significant (p = 0.12). The TS and FS demonstrated only slight improvements in the minimum and maximum limits as shown in Figure 7.8 and Figure 7.9 respectively the with time, which were not statistically significant (p values of 0.71 and 0.82 respectively). Table summarized the morphological and functional changes 3 months after treatment initiation. The Pearson’s product-moment correlation coefficient at 3 months after treatment commencement showed a higher, although moderate correlation between logMAR VA with both parametric parameters of TS (r = 0.42) and FS (r = 0.58), than the correlation shown with OCT values (r < 0.25), as demonstrated in Table 6.
Discussion
The morphological changes and VA data in our cohort confirm the clinical efficacy of treatments of DMO with intravitreal injections of ranibizumab. Okada, et al (2006) reported that eyes with DMO had reduced sensitivity as measured with the Nidek MP1 compared to eyes with normal macula. Vujosevic, [19] showed a correlation between VA and MP sensitivity in eyes with DMO. [32] reported significant correlations between CRT; the functional parameters of BCVA (in letters) and MP, at baseline and after 3 injections of ranibizumab. In the study by [30], there was no correlation between the retinal sensitivity measurements (MP and contrast sensitivity) with macular thickness measurements on OCT in eyes with DMO, although the equipment and examination strategies used were different. The integrity of the IS/OS junction (ellipsoid zone), and the outer retinal appearance on the OCT may provide adequate information. This may allow us to distinguish between thin macula, which is scarred, and which is due to resolution of oedema.
Retinal sensitivity on the Nidek MP1 improved at 12 weeks in eyes with DMO treated with ranibizumab or laser, and the improvement continued till week 48. No correlations with OCT measurements were, however, reported in that study. Our analysis at baseline demonstrates that LogMAR VA may be more correlated to functional macular parameters of threshold sensitivity and fixation stability as measured with MP than morphological changes measured with OCT. Similarly, there was better correlation between VA and macular sensitivity (TS and FS) at 3 months after treatment commencement. Macular oedema associated with retinal vascular conditions may affect central vision such that significant reduction leads to the development of eccentric fixation. Generally, ophthalmologic examinations including OCT and MP are based on patient’s ability to observe a fixation target, and adequately maintain that fixation during the examination process. If foveal function is affected, such examinations may not be accurate as fixation may not be optimally located over the foveal area, and therefore the central values reported by OCT, may represent eccentric values. The absence of significant change in functional measures of VA, and TS and FS at 3 months compared to baseline may imply that the functional loss in DMO especially of long duration may not be reversible in the short-term, as the neural disorganisation may not be reversible. This suggestion supports that of Vujosevic, et al. [19], that MP may be useful in predicting functional outcomes in eyes DMO. The DMO in our patients had been present for long duration and will support the suggested neural disruption. A larger cohort with recent onset of DMO would demonstrate better restoration of retinal sensitivity with treatment. Although the present analysis suggests a stronger correlation between the MP functional parameters with LogMAR VA, a longer follow-up with a larger sample test is needed to confirm these findings. The findings from this study demonstrate that patients with good visual acuity show highly stable fixation (P1 > 90%) due to the intact integrity of cone photoreceptors which describes good foveal vision. Okada [21] have postulated that mean retinal sensitivities measured with MP are significantly correlated to visual acuity and foveal thickness. However, the results from this analysis suggest that fixation stability may be a new important parameter to describe functional macular function. The lack of strong correlation between all the measured values, however, indicates that measurement of visual function with MP may be considered as an important tool to better diagnose retinal pathologies as part of multimodality imaging, responding to the need to combine morpho-functional information, and combining different images from different measurement technologies. Further studies are, however, needed to better understand the relationship between macular morphology and the different parameters of macular function. The main limitations of this study are the small number of patients, chronicity of DMO, and short follow-up. A larger number of patients with recent onset of DMO, followed up for a longer period will provide further valuable information on the role of MP in evaluating outcomes in the treatment of diabetic macular oedema.
For more Information Trends in Ophthalmology
https://lupinepublishers.com/ophthalmology-journal/index.php
please click here: https://lupinepublishers.com/ophthalmology-journal/archive.php
7 notes
·
View notes
Text
Lupine Publishers | A Review of Achromatopsia
Trends in Ophthalmology Open Access Journal (TOOAJ)
Abstract
Congenital achromatopsia is a hereditary form of day blindness caused by cone photoreceptor dysfunction, with an incidence of approximately 1 in 30,000. This inherited disorder is characterized by a lack of color discrimination, nystagmus, photophobia, and low visual acuity (< 0.2). The most typical genetic mutations are autosomal recessive changes in CNGA3, CNGB3, GNAT2, PDE6H, PDE6C, or ATF6. It should not be confused with cerebral achromatopsia, which is an acquired form of total color blindness that can result from illness, trauma, or some other cause. Color plays an essential role in our lives. It can change actions, influence thinking, and cause reactions. As a powerful type of communication, color is irreplaceable. Green means “go” and red means “stop”. Traffic lights send this global meaning. Color vision deficiency, creates challenges in the daily lives of those who have an insufficient visual sense.Purpose: The aim of this review is to examine the literature published on achromatopsia and summarize the diagnosis, management, genetic characteristics, and the recent advances in gene therapy.Conclusions: Congenital achromatopsia is a complex inherited disease. Management of achromatopsia is multifaceted. There is currently no cure for achromatopsia, although gene therapy is a therapeutic option already being studied in clinical trials. The most recent study in human adults can be classified as safe and positive in terms of efficacy.Keywords: Achromatopsia (ACHM); Gene therapyIntroductionGo toAchromatopsia is a condition characterized by a partial or total absence of color vision [1]. People with complete achromatopsia cannot perceive any colors; they only see white, black, and shades of gray. Incomplete achromatopsia is a milder form of the disease that allows some color discrimination [1]. Oliver Sacks, in The Case of Color-blind Painter [2], transcribe the disturbing story of one of his cerebral achromatopsia patients after a car accident in the following way: Mr. I. could hardly tolerate the changed aspects of people (“like animated grey statues”) any more than he could tolerate his own appearance in the mirror: he shunned social intercourse and found sexual intercourse impossible. He saw people’s fesh, his wife’s fesh, his own fesh, as an abhorrent grey; “fesh-colored” now appeared “rat-colored” to him. Congenital achromatopsia also involves other problems with vision, including an increased sensitivity to light and glare (photophobia), involuntary back-and-forth eye movements (nystagmus), significantly reduced sharpness of vision (low visual acuity) [1], usually lower than 20/200 because of central vision loss, and reduced conemediated electroretinographic (ERG) amplitudes [3]. Affected individuals can also have vision problems in the first few months of life, such as hyperopia (farsightedness) or, less commonly, myopia (nearsightedness).
Achromatopsia is different from the more typical forms of color vision deficiency (also called color blindness), in which people can perceive color but have difficulty distinguishing between specific colors, such as red and green [1]. In this disease, cone photoreceptors, the retinal sensory neurons mediating color vision, seem viable but fail to generate an electrical response to light [4,5]. All individuals with achromatopsia (achromats) have impaired color discrimination along all three axes of color vision corresponding to the three cone classes [6]. Cerebral achromatopsia is an acquired disorder caused by injury to the cerebral cortex of the brain, instead of defectiveness in the cells of the eye’s retina. This condition is often mistaken for congenital achromatopsia but physiological deficits of both disorders are completely different. It is a consequence of cortical damage that arises through ischemia or infarction of a specific area in the ventral occipitotemporal cortex of humans [7]. This damage is almost always the result of injury or illness [8]. Medical history and age at presentation will help to differentiate this condition from congenital achromatopsia. Additionally, these patients nearly always have additional neurologic symptoms beyond the loss of color vision [8].EpidemiologyAchromatopsia is a relatively uncommon disorder that affects an estimated 1 in 30,000 people worldwide [9]. Complete achromatopsia is more common than incomplete achromatopsia. Its incidence varies in different parts of the world. Because there is a genetic link, it is more common in regions where there is a high rate of consanguineous marriages (marriages between relatives) and in the eastern Pacific islands of Pingelap [10], approximately five percent of the atoll’s 3,000 inhabitants are afflicted [11,12]. The people of this region have termed achromatopsia “maskun”, which literally means “not see” in Pingelapese [13]. The condition can be traced back to 1775, when Typhoon Lengkieki decimated the population in the island, leaving only a handful of survivors to repopulate the islands. One of the few survivors was a carrier of the rare genetic mutation and passing it on to his descendants, he became the genetic founder for the vision disorder four generations later [14]. Oliver Sacks wrote his book, The Island of the Colorblind (1997), which story chronicles Oliver Sack’s 1994 quest with Knut Nordby and Bob Wasserman to the isolated atoll of Pingelap in Micronesia.Photoreceptors: rods and conesFigure 1: Schematic diagram of vertebrate rod and cone photoreceptors. Retrieved from Photoreceptor Phosphodiesterase (PDE6): A G- Protein-Activated PDE Regulating Visual Excitation in Rod and Cone Photoreceptor, Cells Rick H Cote 2006.
Rod and cone photoreceptors are specialized neurons that function in the initial step of vision [15]. These light-sensitive cells lie at the back of the retina adjacent to the retinal pigment epithelium (RPE), a cell layer that is vital for the survival of photoreceptors [15]. Cones are mostly in the center of the retina. When retinitis pigmentosa affects them, there is a slowly loss of central vision and of the ability to see colors [15]. Rods work at very low levels of light. Only a few bits of light (photons) can activate a rod, that’s why we use these for night vision. Rods don’t help with color vision, which is why at night, we see everything in a gray scale [16]. Rods are more numerous, about 120 million, and more sensitive than cones. However, they are not sensitive to color. Rods are much more concentrated in the macula (central yellow spot) and they provide the eye’s color sensitivity. In the center of the macula is the “fovea centralis”, a 0.3 mm diameter rod-free area with densely packed and very thin cones. Rod and cone photoreceptors have similar structures (Figure 1). Photoreceptors have diameters ranging from 1 to 4 μm, being smaller at the fovea, enhancing visual acuity there. The inner segment contains the nucleus and has an axon-like process connected to a synaptic terminal. The outer segment in the cone cell has its plasma membrane invaginated into numerous closely packed parallel folds [17], forming discs. In rod cells the discs are pinched off the plasma membrane to become completely intracellular [17]. The disc membrane is densely packed with visual pigment. In rod cells, this is rhodopsin. Each type of cone cells has its characteristic cone opsin. The outer segment is continually regenerated from the base, whilst its apical tip is phagocytosed by pigment epithelial cells at the rate of 3-4 discs per hour. Photoreceptors are incapable of mitotic division [17].
In 1965 came experimental confirmation of a long-expected result - there are three types of color-sensitive cones in the retina of the human eye, red or L cones (long wavelength-64%), green or M cones (medium wavelength-32%), and blue or S cones (short wavelength-2%). They are each sensitive to different portions of the spectrum of light. Visible colors correspond to light wavelengths ranging from 400 to 700 nm [16]. Even though each cone is most sensitive to a specific color of light (where the line peaks), they also can detect other colors (Figure 2) [16].
The “blue” cones are sensitive to the peak of the light response curve at about 445nm. They are found outside the fovea centralis where the green and red cones are concentrated and they constitute only about 2% of the total number of cones. Their disadvantage in number is clear but, on the contrary, they are much more light sensitive than green and red cones [18]. However, the blue sensitivity of the final visual perception is equivalent to that of red and green, proposing that there is a somewhat selective “blue amplifier” somewhere in the visual processing in the brain [18]. Morphological studies have allowed us to differentiate the short wavelength specific (blue) cone from the medium and long wavelength specific cones in the human retina even without special antibody staining techniques [19]. S-cones have longer inner segments that project further into subretinal space than longer wavelength cones (Figure 3).
The S-cones also have smaller and morphologically different pedicles than the other two wavelength cones. Throughout the retina, the S-cones have a different distribution and do not fit into the regular hexagonal mosaic of cones typical of the other two types [20].
Conclusion
Achromatopsia is a complex inherited disease. There is currently no approved treatment for ACHM. Management of achromatopsia is multifaceted, including making the appropriate diagnosis, reducing photophobia, correcting refractive error, and utilizing low vision devices, such as high-powered magnifying glasses. To reduce photophobia and potentially improving visual acuity can be helpful the use of dark or special filter glasses or red-tinted contact lenses. However, even with the best aid techniques, daily tasks such as going to school and driving present significant obstacles. New diagnostic and therapeutic tools are being studied. Fundus autofluorescence and OCT are important imaging techniques that supply significant information about the progression of the disease. Gene therapy is an ongoing therapeutic option already being studied in clinical trials. The new gene therapy being trialed centers on correcting a defect in the CNGA3 gene. The results of a first human trial testing for achromatopsia suggest that the experimental gene therapy is safe, and potentially efficacious, opening the door to larger human trials in the future. The evidence to date suggests that gene therapy will need to be applied early in childhood in order to achieve the best possible effect. The remarkable advances in genetics have opened an exciting world to ophthalmologists to offer patients new treatments for achromatopsia. In the future, gene therapy will be a routine treatment offered to patients.
For more information about Trends in Ophthalmology Open Access Journal (TOOAJ)
Please Click Here: https://lupinepublishers.com/ophthalmology-journal/archive.php
9 notes
·
View notes
Text
Lupine Publishers| Contact Lens Materials and Modalities
Lupine Publishers| Ophthalmology Open Access Journal
Abstract
Introduction: Past two decades have seen a steep rise in the usage of contact lenses and that brought a major revolution in the materials research, design and manufacturing technologies. This also impacted the optometrists thus influencing the patient usage, modalities and duration. The current article briefs the changes in the field of contact lenses and the changing trends.
Methods: Contact lens materials and its manufacturing, wearing modalities and changing trends in prescribing them were identified, reviewed and summarized as per the topic requirements from scientific papers, authentic articles, books and websites to cover the challenges our ancestors have faced and the solutions that were provided in the past were summarized for the reader in an easy accessible way.
Conclusion: Newer generation of contact lens materials made an average contact lens wearer comfortable by wearing lenses for longer hours without discomfort and with minimal complications. Due to the advent of newer lens materials, practitioners have been given more options for choosing a best suited lens based on specific wearer requirements and needs. In this way, newly available materials and designs make the lens wear safer and less prone to complications by shifting the patient from conventional to planned replacement lenses (PRL) and from PRL to daily disposables to ensure a healthy and safer vision.
Keywords: PMMA; Rigid Gas Permeable Lenses; HEMA; Silicone Hydrogels; Extended Wear; Flexible Wear; Daily Disposables; Multifocal Contact Lenses; Aspheric; Toric
Abbreviation: CAB: Cellulose Acetate Butyrate; RGP: Rigid Gas Permeable Lens; P-HEMA: Poly Hydroxy Ethyl Methacrylate; PVP: Poly Vinyl Pyrolidone
Introduction
Contact lenses are medical devices commonly used to correct the vision without the need of spectacles. Even though the concept was very old, till 1887, a structure similar to our today's contact lens was not made. A first contact lens like structure was made in 1887 by F. A Muller by blowing glass to make a prosthetic eye. In 1930's a first contact lens made up of glass was used which covers whole the cornea and a small part of sclera was used for vision correction making glass the first contact lens material [1]. In 1937, a material named Poly methyl methacrylate (PMMA) was introduced as a contact lens material which mimics todays' scleral lens of a larger diameter. In 1948, Kevin Tuohy made a contact lens called "Microlens" which covers only cornea with 10 to 12 mm diameter [1,2]. After using PMMA as a contact lens material for some time, hypoxic complications arise due to it’s very poor oxygen permeable nature after use, making.com to explore for newer lens materials. Currently, due to its zero-oxygen permeability, it is used to make diagnostic trial contact lenses instead of actual contact lenses due to its ability to retain the parameters, ease of care and maintenance [3].
Rigid Gas Permeable Lenses (RGP)
Noting the importance of Oxygen permeability, few developments were made to the material to be permeable to oxygen. In the year 1972, Cellulose acetate butyrate (CAB) was proposed as a material to use by Irving Fatt, later in 1978 CAB as a contact lens material got FDA approved. A term (RGP) Rigid gas permeable lens was coined and the lens made with this (CAB) material was manufactured in 1978 in United States [2,4]. In the advent of silicone usage in the medical industry, Siloxane methacrylate material was developed in 1970 by using silicone molecules bonded to methyl methacrylate structures making a contact lens more oxygen permeable [2]. Siloxane acrylates material was patented in 1974 under the name Polycon and was introduced commercially in 1979 which lead the wearing time longer than CAB due to its high oxygen permeability without showing any hypoxic changes in the cornea. However, it was observed that the siloxane acrylate lenses tend to attract more of lipid and less of protein deposits on the lens surface, making the care and regime of newer RGP lens materials different than the previous lens. These deposits lead to lesser lens life than the previous lenses [2].
"Boston" a contact lens material manufacturing company started to develop working towards parameters like oxygen permeability, strength and deposit resistance for improved lens on eye performance since 1972. Elements Fluorine and Carbon were used in specific proportions to synthesize Fluoro-siloxane acrylates and Fluorocarbon acrylates were found effective in controlling the lipid deposits to occur on the lens surface with increased oxygen permeability. These materials still stand good in terms of availability, deposit resistance with good oxygen permeability [5]. Addition of Silicone, Fluorine and Carbon with appropriate amounts made it possible to achieve highest levels of oxygen permeability ever, leading to continuous wear, flexible wear and extended wear modalities possible. During this period in 1987, Fluoro-silicone acrylate material was made available [6]. Due to changing trends in the contact lens market and due to innovations in soft contact lens materials, there is a constant and a sharp decline in the RGP wearers that was observed in the past two decades due to the comfort achieved by soft contact lenses [7].
Silicone Elastomer
In 1956, Silicone elastomer material was developed by Walter Becker which has a highest ever oxygen permeability which is more flexible than RGP lenses, making the contact lens industry to explore newer ways of improvising the lens material in terms of flexibility But, for a product to manufacture out of silicone elastomer was not possible at that time due to its flexible nature, poor wettability and the material adheres to the cornea(suction). Later in 1981 a lens made up of silicone elastomer material was commercialized for correcting children to use as an overnight wear lens due to its exceedingly high oxygen permeability. This material got approved for 30 day continuous wear for non-aphakic prescriptions in 1983 making it the first extended wear lens to be produced [6,8]. Till now these elastomer lenses are available as a mode of correction for aphakia (congenital and acquired) cases mostly in children [9]. The only drawback with these lenses is the brittleness of the material and affinity to attract lipid deposits, making its usage declined in this decade [6,8].
Soft Contact Lens (Hydrogels)
Progress in contact lens materials was extremely rapid and the market equations of using RGP lenses were quickly changed after the development of Poly hydroxy ethyl methacrylate (P-HEMA) as a lens material in 1963 by Otto Wichterle. This material coined a new term called "soft contact lens" due to its soft and flexible nature. The lens made with HEMA was available in 1971 as a commercial product [2,6]. The usage of HEMA as a lens material in the current contact lens market still holds good. After the invention of HEMA as a hydrogel material, the comfort obtained by a wearer lead the path for a term called intermittent contact lens wear, which is not possible with RGP due to the discomfort it caused to an average wearer. However, the water content which is the only source of oxygen transmission through the hydrogel lens was too less when compared to RGP lenses due to their movement and tear exchange. There is a need for a diverse care and regime to be followed to soft contact lens wearers for which different contact lens solutions were devised to clean, rinse, disinfect, and hydrate and to store these lenses.
Due to limitation of water content and oxygen permeability in hydrogel lenses, there were diverse complications that were seen in the soft contact lens users and the users due to the comfort of the lenses, tend to sleep with the lenses on the cornea making the condition more worsen [10]. Observing these diverse ocular changes, few of the traditional RGP practitioners were reluctant to shift their practice and keep on dispensing RGP lenses only [11]. As there is a limitation in increasing the water content that we achieve with hydrogel lenses, scientists started to explore new ways to increase the oxygen passing through the lens which can enable the wearer to achieve better comfort lens with lesser complications [12]. Concept of Disposable soft contact lenses came into the field in 1985-1986 as the increasing complications can be counteracted by discarding the lenses before the deposits on the lens surface become sufficient enough to create problems like discomfort, bulbar conjunctival redness, allergic reactions in the upper tarsal conjunctiva and lack of oxygen supply due to deposits [13]. Gradually, frequent replacement lenses were so frequently replaced due to increasing in water content of the lenses that there is a need for a modality termed Daily disposable lenses in 1994-1995 to ensure maximum comfort and good ocular health with no requirement of care and maintenance which is a boon for existing, new contact lens wear. As the production need to meet the consumer needs a new manufacturing method called cast moulding turned the disposable modality a practically possible reality [2,14].
Even now, majority of the contact lens market share in developing countries is still contributing to Hydrogel lenses where as in developed countries, majority of the population is using silicone hydrogels and daily disposable hydrogel lenses for their visual needs [15-17]. In this stage, Silicone elastomers were more easily available and used in the market as a commercial product leading the materials science experts to turn their vision towards it. This change made them to think and combine the silicone with hydrogel lenses which set a stage for the generation of silicone hydrogels. The first silicone hydrogel lens was marketed in 2002 [2,9].
Silicone Hydrogels
In soft contact lenses the silicone material is incorporated based on the skeletal structures of classical hydrogel materials like HEMA and thereby making it a better lens material by incorporating:
a) OH groups for increasing the bound water content of the lens materials [18]
b) Materials like polyvinyl pyrolidone (PVP) for improving the wettability of the lenses [18]
Due to the innovation of Silicone hydrogel contact lenses, high oxygen transmissibility is made possible, hence by minimizing corneal hypoxia changes that include corneal oedema, Descemet’s membrane folds, microcysts, limbal hyperaemia and neovascularisation [19]. There are a few patient related .difficulties with these new lenses due to increased stiffness than existing hydrogels, hydrophobic nature and more attraction of lipid deposits. So, there is a need for a better and improved materials and designs making them readily acceptable by the patient [9]. In 2010, Custom made silicone hydrogel lenses are made available in the market [20]. In case of Silicone hydrogel lenses, these inventions can be technically classified into three phases in which the lens materials are synthesized by not only decreasing the stiffness of the lens material, but also by increasing the wettability and water content to a desired level for enhancing the comfort level of silicone hydrogel wearer equal to that achieved by a hydrogel contact lens wearer [18,19,21,22].
Developments in Silicone Hydrogel Materials
Table 1: First generation lenses.
1. Good Dk
2. Slightly stiffer
3. Deposit prone surface
4. Decreased Wettability
Table 2: Second generation lenses
b) Properties (Table 2)
2. Flexible lens material
1. Improved wettability
c) Properties (Table 3)
Table 3: Third generation lenses.
1. Better Water content
2. Decrease stiffness
3. It is a Breakthrough technology, which redefines the soft contact lens relationship between Dk and water content by having a higher Dk than water content predicts!
Contact lens advancements in the Future
a) Myopia control contact lenses are very soon going to be available in Asian countries where Myopia is more prevalent.
b) Aberrometers values combined with prescription can help customize the correction to a personalized contact lens manufacturing is possible soon [23].
c) A Multifocal design of contact lens which can have an autofocus capability near the pupillary centres of the eyes using fluid dynamics can be manufactured and fitted which can help.com gain complete visual satisfaction to the wearer [23].
d) Health monitoring systems embedded in the form of a computer chip in contact lenses will help.com plan our diet and treatment plan based on the parameters like blood sugar level, intraocular pressure [24].
e) The use of LCD crystals in the bulk of a silicone hydrogel lens can help.com to use virtual projection; digital screens in the near future will aim for [23].
f) In Contact lens materials, even though the penetration of silicone hydrogels in the current market is low, majority of the market share will shift using this material due to its break thought the invention of improved oxygen permeability, it can retain their share well in the markets in the future [17,23].
g) Improvements like anti bacterial coating on contact lenses are giving promising results which can help use them for extended wear without any worry of infections. Possibilities for making a Photo chromatic contact lenses are explored and will be achieved soon [25-29].
Modality
Silicone hydrogels will take the majority of the market and will exist even in future. Mostly the contact lenses have a freedom to wear and remove easily whenever we want and where ever you want [30-34].
Conclusion
Contact lenses have an exponential growth in material development, design and production in the last two decades.Newer technologies in the coming years can help.com make a more productive, versatile, comfortable and safer wearing lenses for the coming generations ahead [35-39].
For more Lupine Publishers Open Access Journals Please visit our website:https://lupinepublishers.us/
For more Ophthalmology Open Access Journal Please Click Here:
https://lupinepublishers.com/ophthalmology-journal/
To Know more Open Access Publishers Click on Lupine Publishers
#Lupine Publishers#Lupine Publishers group#Lupinepublishers#open access publishers#Ophthalmology Open Access Journal
64 notes
·
View notes