#serological testing
Explore tagged Tumblr posts
Text
Serology Test Kits and CRP Turbilatex
In today’s healthcare landscape, early diagnosis and targeted treatment are crucial to improving patient outcomes. Two powerful diagnostic tools — the Serology Test Kit and the CRP Turbilatex — help clinicians make informed decisions quickly and efficiently. This blog explores how these tools work, what they detect, and why they’re so important in both routine and emergency medical settings.
What is a Serology Test Kit?
A Serology Test Kit is designed to detect antibodies or antigens in a patient’s blood. These kits are commonly used to diagnose infectious diseases, autoimmune disorders, and other conditions where the immune system plays a central role.
Common Uses:
Infectious diseases like HIV, hepatitis, syphilis, dengue, and COVID-19
Autoimmune diseases such as lupus or rheumatoid arthritis
Allergy testing and vaccine response assessment
How It Works:
Serology kits typically use ELISA (enzyme-linked immunosorbent assay), lateral flow, or chemiluminescent immunoassay technologies to detect the presence of IgM or IgG antibodies, or specific antigens.
Why It Matters:
Serological testing provides insights into a patient’s immune status and helps track the course of infection. It’s essential for outbreak control, epidemiological surveillance, and disease screening.
What is CRP Turbilatex?
CRP Turbilatex is a reagent used in turbidimetric immunoassays to measure C-reactive protein (CRP) levels in blood. CRP is an important biomarker of inflammation and is elevated in conditions such as:
Bacterial infections
Autoimmune diseases
Cardiovascular risk
Post-surgical complications
How It Works:
CRP Turbilatex uses latex particles coated with anti-CRP antibodies. When mixed with a patient’s serum, any CRP present binds to the latex particles, causing visible turbidity. This turbidity is measured by automated analyzers to determine CRP concentration.
Clinical Significance:
High CRP levels often suggest acute bacterial infection or severe inflammation
Moderate levels may indicate chronic inflammatory conditions
Normal levels can help rule out bacterial causes in differential diagnosis
Advantages:
Rapid and reliable
Automated and quantitative
Suitable for high-throughput laboratories
Combining Serology and CRP Testing for Better Diagnosis
While a Serology Test Kit helps determine exposure to specific pathogens or immune conditions, CRP Turbilatex offers insight into the severity and nature of inflammation. Used together, they provide a comprehensive picture:
In infectious disease diagnosis, serology can confirm the pathogen, and CRP helps assess the severity and guide treatment.
In autoimmune conditions, serology identifies specific autoantibodies, while CRP indicates ongoing inflammation.
For post-operative care, CRP monitoring can signal infection or complications even before clinical symptoms appear.
Final Thoughts
The combination of a Serology Test Kit and CRP Turbilatex is a powerful diagnostic strategy. These tools are widely used in hospitals, diagnostic labs, and clinics to support fast, accurate, and actionable healthcare decisions. As medical diagnostics continue to evolve, the integration of serological and inflammatory markers remains central to personalized and preventive medicine.
0 notes
Text
https://social.studentb.eu/read-blog/188255_serological-testing-market-share-overview-competitive-analysis-and-forecast-2031.html
The Serological Testing Market in 2023 is US$ 4.81 billion, and is expected to reach US$ 8.22 billion by 2031 at a CAGR of 6.90%.
0 notes
Text
Located in the heart of Thrissur, Hygea Med Laboratories is a leading Medical Laboratory in Thrissur that offers top-notch and comprehensive diagnostic services. With a team of highly skilled professionals and state-of-the-art equipment, Hygea Med Laboratories is dedicated to providing the best and quality services to the residents of Thrissur.
When it comes to healthcare, accuracy and reliability are of utmost importance. That's where Hygea Med Laboratories stands out. The laboratory is equipped with the latest technology and follows strict quality control measures to ensure accurate and precise test results every time. This not only helps in accurate diagnosis but also aids in better treatment and management of diseases.
Hygea Med Laboratories offers a wide range of diagnostic services including blood tests, urine tests, imaging services, and more. The laboratory is equipped with advanced equipment and machines, which are regularly maintained and calibrated by a team of trained technicians. This ensures that the results obtained are accurate and reliable.
One of the key factors that make Hygea Med Laboratories stand out from other medical laboratories in Thrissur is their team of highly skilled professionals. The laboratory has a team of experienced and qualified pathologists, technicians, and support staff who are well-trained in their respective fields. They are dedicated to providing patients with the best care and ensuring that all tests are conducted with utmost accuracy and efficiency.
At Hygea Med Laboratories, patient comfort and convenience are given top priority. The laboratory has a spacious waiting area and comfortable sample collection rooms to ensure a stress-free experience for patients. The staff is friendly and approachable, making the entire process of getting tests done hassle-free.
Apart from providing quality diagnostic services, Hygea Med Laboratories also offers home sample collection services. This is especially beneficial for elderly patients or those who are unable to visit the laboratory. The samples are collected by trained phlebotomists and are transported to the laboratory with utmost care and efficiency.
In addition to its top-notch services, Hygea Med Laboratories also maintains a strict code of ethics and confidentiality. Patient information and test results are kept confidential and are only shared with authorized individuals. This ensures that patients feel comfortable and secure while getting their tests done.
Overall, Hygea Med Laboratories is the go-to medical laboratory in Thrissur for accurate and reliable diagnostic services. The laboratory's commitment to quality, advanced technology, and skilled professionals make it the best choice for all your healthcare needs. So, the next time you need to get a test done, head to Hygea Med Laboratories for a hassle-free and superior experience.
#Hygea Med Laboratories#Thrissur#Medical Laboratory#Diagnostic Services#Healthcare Thrissur#Pathology Services#Clinical Laboratory#Medical Testing#Diagnostic Center#Thrissur Healthcare#Laboratory Services#Health Checkups#Medical Tests#Blood Tests#Urine Analysis#Biochemistry Tests#Microbiology Tests#Serology Tests#Immunology Tests#Hematology Tests
0 notes
Text
Checkout the Best Quality of Nutrient Agar (TM 341) at TM Media
If you are looking for Nutrient Agar manufactured by TM Media serve as fundamental culture substrates, supporting microorganisms, fostering the growth of fastidious species when enriched with serum or blood. They're instrumental in purity checks before biochemical or serological tests. Nutrient Agar, especially suitable for educational purposes, facilitates prolonged culture survival at room temperature without the risk of overgrowth associated with more nutrient-rich substrates. As a non-selective medium, it finds routine use in cultivating a variety of microorganisms, aiding in their enumeration. The versatility of Nutrient Agar is enhanced by supplementing it with diverse biological fluids like horse or sheep blood, serum, or egg yolk, making it apt for the cultivation of specific fastidious organisms.
Visit the Website - https://www.tmmedia.in/

0 notes
Text
Serological Testing Market
#Serological Testing Market scope#Serological Testing Market report#Serological Testing Market research
0 notes
Text
Amoebiasis
Intestinal disease (amoebiasis) is primarily caused by E. histolytica. E. dispar is generally considered non-pathogenic and the pathogenicity of E. moshkovskii is uncertain.
0 notes
Text
Overview of Serology Test | Serology Tests in Ahmedabad
Serology tests are blood tests that look for antibodies in your blood. EA Laboratories offer Immunology and Serology in India.
#laboratory testing#multispecialty testing laboratory#endocrine lab#Serology test in Ahmedabad#serology test lab
1 note
·
View note
Text
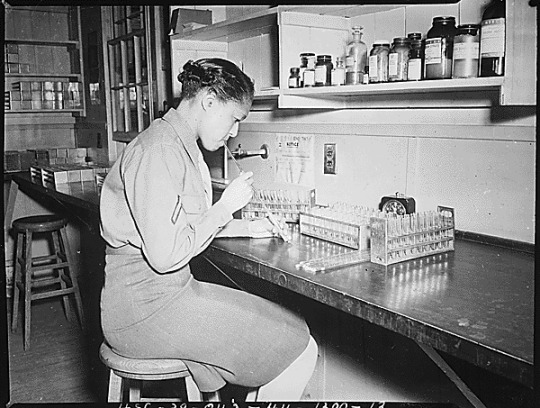
"Pfc. Johnnie Mae Welton, Negro WAC, laboratory technician trainee, conducts an experiment in the serology laboratory sf the Fort Jackson Station Hospital, Fort Jackson, SC."
Record Group 111: Records of the Office of the Chief Signal OfficerSeries: Photographs of American Military Activities
This black and white photograph shows Pfc. Johnnie Mae Walton, an African American woman in the Women’s Army Corp, sitting at a lab table. She wears a military uniform and her hair is tied back. She appears to be blowing through a straw into a test tube. Three racks of test tubes are on the lab table before her.
229 notes
·
View notes
Text
Also preserved in our archive
(This number is likely underinflated by 1. lack of diagnosis 2. lack of education in the population about what long covid is 3. people getting long covid but powering through their symptoms and acting like nothing is wrong [a huge problem in the US even before covid])
By Jim Wappes
A study today demonstrates that last year, about 8% of US adults reported that they ever had long COVID, and those who currently had the condition or currently had activity-limiting long COVID were both under 4%, but a leading US expert on long COVID explains the limitations of such data and why estimates of the prevalence of the condition can vary so widely.
And he notes that, even when considering low estimated long-COVID rates, as in today's study, when the percentages are applied to the population as a whole, the impact is massive.
Long COVID—also known as post-COVID condition (PCC)—is generally defined as having symptoms 3 months or longer after an acute COVID-19 infection.
Only 3.6% currently had long COVID The study, published as a research letter in JAMA Network Open by scientists from the Centers for Disease Control and Prevention (CDC), involved 29,522 US adult respondents to the National Health Interview Survey, a nationally representative household survey.
For the survey, investigators randomly selected one adult from each eligible household to answer more detailed questions about their health. The response rate was 47%. The selected adults were asked whether they had ever had COVID-19, if they had symptoms lasting 3 months or more that they didn't have before COVID-19, if they had symptoms now, and whether these current symptoms limited their ability to carry out daily tasks compared with pre-COVID.
The authors didn't specify what percentage of respondents self-reported COVID-19, but CDC serology data reveal that, by the end of 2023, 87.2% of Americans had infection-induced antibodies to SARS-CoV-2, indicating a previous infection.
The study authors reported that 8.4% of the adults said they ever had long COVID, 3.6% currently had long COVID, and 2.3% currently had activity-limiting long COVID. In 2022, 6.9% said they had ever had long COVID, and 3.4% reported it at the time of the interview. The third question was new in 2023.
They researchers also noted, "Significant differences across all 3 outcomes were observed by sex, sexual orientation, age, race and Hispanic origin, family income, and urbanization." They said the prevalence of all three outcomes decreased with higher family income and was higher in rural residents.
Study limitations The study authors write, "A limitation of this work is that the data were from self-reports and were not confirmed by medical evaluation."
Ziyad Al-Aly, MD, chief of research and development at the VA St. Louis Health Care System and a preeminent expert on long COVID who was not involved in the study, said the low response rate is another limitation of the study. "It is unclear how this low response rate biases the results." He also said that self-diagnosis "may miss a lot of PCC."
"I also note lack of any information on infection," he said in an email. "Because most people abandoned testing, a lot of people get COVID without knowing it; they subsequently develop health problems (that could be PCC) and cannot attribute them to an infection and won't be able to identify them as PCC.
"We entered a phase where PCC is now intermingled with baseline disease, and consequently it has become harder to detect through these kinds of surveys."
Why do reported rates of long COVID vary so widely? The prevalence of long COVID reported in today's study is markedly lower that other recent studies. Al-Aly and colleagues, in a July study in the New England Journal of Medicine, noted a 10.4% long-COVID prevalence a full year after the original infection when solely assessing people infected with the original SARS-CoV-2 strain. Subsequent variants were tied to lower rates of PCC, but the cumulative total would be much higher than 8.4%.
Last month, Massachusetts General Hospital researchers used artificial intelligence to estimate that 23% of the population has had the condition at some point. A second July study determined that 12% of Japanese adults developed long COVID after an Omicron infection alone. An October study found that 25% of previously healthy US Marines showed signs of long COVID following even mild or asymptomatic COVID-19.
A study in September estimated that the prevalence of long COVID in people with disabilities is 41%, compared with 19% in non-disabled participants. And two studies published in August found a 34% prevalence of long COVID in women and an 84% rate 1 year after infection in Italian adults.
Al-Aly explains: "Variation in incidence and prevalence estimates generally stems from variation in study designs (eg, surveys of self-reported Long Covid vs cohort studies, etc), definition of Long Covid (eg, narrow vs broad definition), population being studied, predominant variant, vaccination rates, etc."
He added, "When reviewing the totality of evidence, all the estimates suggest that [long COVID] is a serious problem affecting a sizable number of [the] US population. This is a problem that demands attention—we cannot ignore it."
He also noted that, even when considering the lower percentages in today's study, when you extrapolate them to the entire US population, the numbers are substantial. "Although it may appear to be a small percentage, 2.3% of people 'currently had activity-limiting PCC' is huge when translated into absolute numbers."
Study link: jamanetwork.com/journals/jamanetworkopen/fullarticle/2828033
#mask up#public health#wear a mask#wear a respirator#pandemic#covid#still coviding#covid 19#coronavirus#sars cov 2#long covid
53 notes
·
View notes
Text
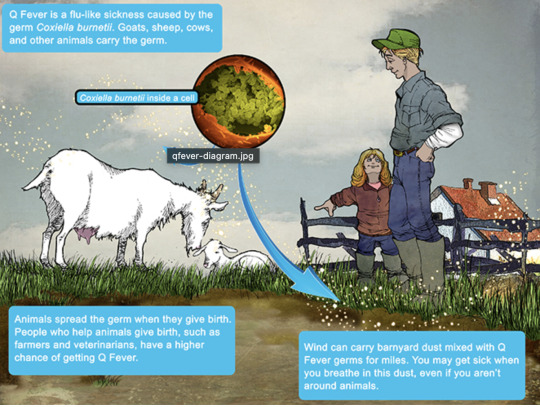
Q Fever
Aka, Query fever. What a weird name for a disease. Imagine telling people that's what you got.

in the 30s-40s, an Australian pathologist in QLD/Brisbane, came across an outbreak of the same or similar illness among abbatoir or slaughterhouse workers.
At the time, he called the disease "Q" fever or query as a temporary name until the pathogen could be identified. Unfortunately it stuck.
decades later, now nobel prize winner and virologist, MacFarlane Burnett isolated and identified the microbe responsible. I think this discovery contributed to his prize. i forget already.
Microbe responsible: Coxiella burnetti. Named for Burnett and HR Cox, the American bacteriologist who found the genus Coxiella where C burnetti falls under.
Initially they felt it was related to Rickettsia, responsible for Rocky Mountain Spotted Fever, but as science progressed, this was disproven.
Now for a Case Report
A 55 yo Italian man with a history of aortic valve replacement was diagnosed with pyrexia of unknown origin twice. Further signs included myalgias/splenomegaly/night sweats. The 2nd time he was admitted for PUO he deteriorated rather dramatically and was put on meropenem and teicoplanin.
A host of organisms was tested for on serological testing based on the man's travel and epidemiological history, all negative. Even a rheumatological panel was done, also less revealing. He also had a history of MGUS (a haem disoder), which is kind of a red herring here.
Cultures were negative, no vegetations were seen on a TTE - so they did consider IE. Which is an important differential for PUO.
Eventually a PET-CT was done (often favoured when investigations do not yield much for a sick patient with fevers), finally revealing a focus of infectious on his ascending aorta, where he'd also had previous surgery done. And in a round about way, they also further identified Coxiella Burnetti. He was treated doxycycline and hydroxychloroquine. As it's so rare in Italy, it wasn't really considered even though he mentioned rural travel.
Bottomline: Q Fever is an important consideration in the work up for culture negative IE. Further to this, always consider IE in the differentials for PUO particularly if they're at increased risk for IE (prosthetic valves, damaged valves, select congenital heart issues, previous IE). IE can present with night sweats, fevers, weight loss and splenomegaly. It can be insidious and chronic in nature. other risk factors can be more suggestive as we'll get into below.
Causative organism
Coxiella burnetti, it's a zoonoses - i.e. transmissible from animals. Special powers: very tough/hardy, can survive extreme environments (high temps and UV light etc.) over prolonged periods and is resistant to many common disinfectants/surface cleaners.
It's an intracellular pathogen and gram negative coccobacilli (PINK!)
name coccobaccili reminds me of cocopuffs.
it's mainly associated with farm animals, which the CDC so wholesomely displays on its website on Q fever (wtf).

goats, sheep, cattle typically (but many other animals, even birds, dogs and horses can be reservoirs)
in particular bodily fluids - amniotic fluid, placenta, faeces/urine, milk etc.
you can get it through unpasteurized milk and through inhaling it if it lands on dust in the area
ever visit a farm or petting zoo lately? OMG WASH YOU HANDS.

That said, it's typically inhaled in inorganic dust. You inhale it, it goes to the lungs, and then the bloodstream.
Increased risk for Coxiella burnetti (What to take on history of exposures and when to strongly consider it)
live on a farm or near one
exposure to a farm
work as a vet on a farm
farm worker, dairy workers, researchers on these animals/facilities
slaughterhouse/abbatoir
Also from CDC:
Clinical presentation
Most won't get sick after exposure and remain asymptomatic, a very small minority does. even though it is highly infectious.
incubation time is 2-3 weeks (consider this time in your history of exposure, did they work on the farm 2-3 weeks ago as opposed to yesterday).
Nonspecific acute infectious symptoms:
nonspecific systemic fevers/malaise/arthralgias/myalgias--> key is high fevers though and can be associated with headache and photophobia.
non specific GI - N/V/diarrhoea
respiratory ones - SOB or cough, consider it as atypical cause of community acquired pneumonia.
rare: hepatitis and jaundice (granulomatous) or encephalitis with neurological complications such as demyelinating disease or CN palsies, also haemolytic anaemia and HLH (yikes)

really it's the history of exposure that will lead you down the garden path to Q fever.
Chronic Q fever is perhaps worse, and can present as culture negative IE/PUO. Months/years later, as B symptoms as above above + LOW/LOA, night sweats. More likely to occur if you are predisposed for IE as above, have a weakened immune system for any reason, including pregnancy.
Chronic Q fever has a mortality of 10% if left untreated. About <5% of those with acute Q fever develop this if left untreated. Speculation is that it's more of an autoimmune process or abnormal immunological response to the bacteria.
To be honest, most who walk in the door with community acquired pneumonia get treated empirically for atypicals anyway, (standard course of doxycycline), so we hardly really ponder the question of Q fever in every patient. But if they present chronically and did not have atypical cover at the onset of acute symptoms, then it's something important to consider.
Other important conditions - can cause complications in pregnant women and 20% will get post Q fever syndrome. like chronic fatigue.
investigations
Serology! nice and easy. Look for IgG antibodies in the chronic presentation. Or PCR. Down side to serology - can take 2-3 days for the body to make said antibodies to the bacteria for detection. PCR can be done on any fluids/tissue sent.
Cultures useless, hence it fall under the umbrella of culture negative (hard to grow outside a host cell, it is an obligate intracellular pathogen).
Other hints on bloods (as serology/PCR takes time to return) - elevated or low platelet's, transaminitis with normal bili, opacities in CXR with hilar lymphadenopathy, CSF will show raised protein levels if done when encephalitis is suspected.
imaging can also support the diagnosis.. as illustrated by the case report.
Treatment
Acute disease - as standard for atypical bugs, doxycycline 100 mg BD for 14 days. Alternatives - TMP SMX or Clarithromycin.
Chronic Q fever or IE:
native valves: doxycycline and hydroxychloroquine (200 TDS) for 18 months
prosthetic: same but 24 months
why hydroxy: enhances the action of doxycycline (increases the pH of the phagolysosome)
Follow-up: look for 4 fold decrease in IGG
Sources:
CDC
Stat Pearls
Wiki as linked above
#australian history#medblr#medblrs#infectious disease#infectious diseases#q fever#coxiella#coxiella burnetti
76 notes
·
View notes
Text
Serology, Blood Grouping, and Urine Strip Test Kits
In the world of healthcare, accurate and timely diagnostics are crucial for effective treatment and disease prevention. Oscar Bio offers a range of innovative test kits designed to meet diverse diagnostic needs. From serology testing to blood grouping and urine analysis, these kits provide reliable, user-friendly, and cost-effective solutions. In this blog, we’ll explore Oscar Bio’s Serology Test Kit, Blood Grouping Kit, and Urine Strip Test Kit, their applications, and why they are trusted by healthcare professionals and individuals alike.
Why Diagnostic Testing Matters?
Diagnostic tests are essential for:
Identifying diseases and infections early.
Monitoring chronic conditions.
Ensuring safe blood transfusions and organ transplants.
Providing insights into overall health through routine check-ups.
Oscar Bio’s diagnostic kits are designed to deliver accurate results quickly, making them indispensable tools for healthcare providers and individuals.
Serology Test Kit: Detecting Antibodies with Precision
What is Serology Testing?
Serology testing involves detecting antibodies or antigens in blood serum to diagnose infections, immune responses, or past exposure to pathogens. It’s widely used for infectious disease screening and immunity assessment.
Oscar Bio’s Serology Test Kit
This kit is designed to detect specific antibodies or antigens in blood samples, providing accurate results for conditions like HIV, HCV, and syphilis. It’s ideal for clinical settings, research, and public health initiatives.
Applications of Serology Test Kits:
Screening for infectious diseases (e.g., HIV, hepatitis, syphilis).
Assessing immunity to vaccines or past infections.
Monitoring autoimmune diseases.
Conducting epidemiological studies.
Blood Grouping Kit: Ensuring Safe Transfusions
What is Blood Grouping?
Blood grouping determines an individual’s blood type based on the presence of specific antigens on red blood cells. It’s critical for safe blood transfusions, organ transplants, and prenatal care.
Oscar Bio’s Blood Grouping Kit
This kit provides a quick and accurate way to determine blood types (A, B, AB, O) and Rh factors (positive or negative). It’s widely used in hospitals, blood banks, and emergency settings.
Applications of Blood Grouping Kits
Ensuring compatibility for blood transfusions.
Identifying blood types for organ transplants.
Prenatal testing to prevent Rh incompatibility.
Emergency medical situations requiring immediate blood typing.
Urine Strip Test Kit: Comprehensive Urine Analysis
What is Urine Analysis?
Urine analysis involves testing urine for various parameters, such as glucose, protein, pH, and infection markers. It’s a non-invasive way to assess kidney function, detect infections, and monitor chronic conditions.
Oscar Bio’s Urine Strip Test Kit
This kit uses reagent strips to analyze multiple urine parameters simultaneously. It’s a quick, convenient, and cost-effective tool for routine health check-ups and diagnostic purposes.
Applications of Urine Strip Test Kits
Detecting urinary tract infections (UTIs).
Monitoring kidney function and diabetes.
Screening for metabolic disorders.
Routine health check-ups.
Why Choose Oscar Bio’s Diagnostic Kits?
1.Accuracy and Reliability: Oscar Bio’s kits are designed to deliver precise results, ensuring confidence in your diagnosis.
2. Ease of Use: Clear instructions and user-friendly designs make these kits accessible to both professionals and individuals.
3. Quick Results: Rapid testing capabilities save time and enable timely decision-making.
4. Affordability: High-quality diagnostics at competitive prices make Oscar Bio’s kits accessible to all.
5. Versatility: From serology to urine analysis, Oscar Bio offers a wide range of tests to meet diverse needs.
When to Use These Test Kits
Serology Test Kit : — For infectious disease screening. — To assess immunity or past infections. — In research or public health initiatives.
Blood Grouping Kit : — Before blood transfusions or organ transplants. — During prenatal care. — In emergency medical situations.
Urine Strip Test Kit : — For routine health check-ups. — To detect UTIs or kidney issues. — To monitor chronic conditions like diabetes.
Final Thoughts
Oscar Bio’s Serology Test Kit, Blood Grouping Kit, and Urine Strip Test Kit are essential tools for accurate and timely diagnostics. Whether you’re a healthcare professional, researcher, or individual looking to take control of your health, these kits provide reliable solutions for a wide range of diagnostic needs.
Take the first step toward better health today. With Oscar Bio’s innovative and trusted diagnostic solutions, you can stay informed, take action, and prioritize your health with confidence. Accurate diagnostics are the foundation of a healthier future!
1 note
·
View note
Text
https://twikkers.nl/blogs/262948/Serological-Testing-Market-Share-Overview-Competitive-Analysis-and-Forecast-2031
The Serological Testing Market in 2023 is US$ 4.81 billion, and is expected to reach US$ 8.22 billion by 2031 at a CAGR of 6.90%.
0 notes
Text
Table summarizing common forensic serology tests, their purpose, and the sample type analyzed
#forensic#forensics#forensic science#criminology#criminalistic#evidence#crime#forensic field#crime scene investigation#forensic science notes
11 notes
·
View notes
Text
Tempat Jual Tabung Plain dari Prima Medikatama DI TANGERANG
Dalam dunia medis, peralatan yang digunakan harus memenuhi standar ketat untuk memastikan hasil yang akurat dalam setiap pengujian.
Salah satu perangkat penting dalam dunia medis adalah tabung plain.
Artikel ini akan membahas tabung plain dari Prima Medikatama, sebuah perusahaan terkemuka di TANGERANG yang menyediakan produk berkualitas tinggi untuk kebutuhan medis.
Tabung Plain: Spesifikasi dan Kegunaan
Tabung plain Prima Medikatama memiliki spesifikasi yang sangat penting untuk memastikan pengujian berjalan dengan baik.
Tabung ini memiliki ukuran 3ml/3cc dan terbuat dari bahan plastik berkualitas tinggi.
Setiap kotak berisi 100 tabung, dengan berat total setelah dipacking sekitar 800 gram.
Dimensi packingnya adalah P: 20cm, L: 18cm, T: 15cm. Harga yang ditawarkan sangat kompetitif, yaitu 120.000 rupiah per box.
Tabung plain ini dirancang untuk digunakan dalam berbagai prosedur medis, terutama dalam pemeriksaan kimia darah, imunologi, serologi, dan crossmatching test pada bank darah.
Keunggulan utama dari tabung plain ini adalah bahwa mereka tidak mengandung zat aditif apa pun.
Hal ini sangat penting, karena zat aditif dalam tabung pengumpul darah dapat memengaruhi hasil pengujian, terutama dalam pemeriksaan kimia darah.
Dengan tabung plain Prima Medikatama, darah akan tetap segar dan tidak akan menggumpal sebelum diuji.
Keunggulan Tabung Plain Prima Medikatama
Kualitas Tinggi: Prima Medikatama dikenal sebagai produsen yang mengutamakan kualitas. Tabung plain mereka terbuat dari bahan plastik yang kuat dan tahan lama.
Spesifikasi yang Akurat: Dengan ukuran 3ml/3cc, tabung ini memungkinkan pengukuran yang sangat tepat. Hasil pengujian akan menjadi acuan yang baik bagi tenaga medis.
Kuantitas yang Memadai: Setiap kotak berisi 100 tabung, sehingga Anda tidak perlu khawatir kehabisan persediaan saat Anda membutuhkannya.
Harga Terjangkau: Harga 120.000 rupiah per box adalah penawaran yang sangat menguntungkan. Prima Medikatama berusaha memberikan nilai terbaik kepada pelanggannya.
Pemakaian Tabung Plain
Tabung plain Prima Medikatama digunakan dalam berbagai prosedur medis, termasuk:
Pemeriksaan Kimia Darah: Tabung ini memungkinkan pengambilan dan penyimpanan darah tanpa pengaruh dari zat aditif. Ini sangat penting dalam pengujian kimia darah yang memerlukan sampel yang murni.
Pemeriksaan Imunologi: Dalam pengujian imunologi, tabung plain memastikan bahwa sampel darah tidak terkontaminasi oleh bahan tambahan.
Pemeriksaan Serologi: Dalam pemeriksaan serologi, hasil yang akurat adalah segalanya. Tabung plain Prima Medikatama memastikan hasil yang andal.
Crossmatching Test di Bank Darah: Tabung ini sangat penting dalam pengujian kompatibilitas darah sebelum transfusi. Ketepatan hasil adalah kunci dalam prosedur ini.
FAQ (Pertanyaan yang Sering Diajukan)
Apa yang membedakan tabung plain Prima Medikatama dari produk sejenis? Tabung plain Prima Medikatama unggul karena mereka tidak mengandung zat aditif apa pun. Hal ini membuat hasil pengujian menjadi lebih akurat, terutama dalam pemeriksaan kimia darah.
Bagaimana cara memesan tabung plain dari Prima Medikatama? Anda dapat menghubungi Prima Medikatama langsung untuk memesan tabung plain mereka. Mereka akan dengan senang hati membantu Anda.
Apakah tabung plain ini cocok untuk penggunaan satu kali atau bisa digunakan lagi? Tabung plain ini dirancang untuk penggunaan satu kali. Penggunaan ulang dapat mengakibatkan kontaminasi dan hasil yang tidak akurat.
Berapa lama waktu pengiriman setelah memesan tabung plain dari Prima Medikatama? Waktu pengiriman dapat bervariasi tergantung pada lokasi Anda. Prima Medikatama akan memberikan perkiraan waktu pengiriman saat Anda memesan.
Apakah Prima Medikatama juga menyediakan produk lain selain tabung plain? Ya, Prima Medikatama memiliki berbagai produk medis lainnya. Anda dapat mengunjungi situs web mereka atau menghubungi mereka untuk informasi lebih lanjut.
Kesimpulan
Tabung plain dari Prima Medikatama adalah solusi yang sangat baik untuk berbagai kebutuhan medis, terutama dalam pengujian kimia darah, imunologi, serologi, dan crossmatching test di bank darah.
Dengan spesifikasi yang akurat, kualitas tinggi, dan harga terjangkau, produk ini dapat diandalkan untuk memberikan hasil yang akurat dan andal.
Jika Anda mencari tabung plain berkualitas, Prima Medikatama di TANGERANG adalah tempat yang tepat untuk mencarinya.
Dapatkan produk berkualitas dan hasil pengujian yang andal dengan tabung plain Prima Medikatama.
Untuk informasi lebih lanjut atau untuk memesan Tabung Plain, jangan ragu untuk menghubungi kami melalui https://wa.me/6282311150090 atau dengan mengklik tombol “Tabung Plain ” Untuk Pemesanan.
#Probe Cleanser Mindray#Reagen Kimia Darah CHOLESTEROL MR#Diluent Mindray 20L#Reagen Widal Test#Alat Kesehatan Habis Pakai#Reagen Kimia Darah AST/GOT EVOGEN#Tabung EDTA 3 ML#Reagen Pemeriksaan Golongan Darah
87 notes
·
View notes
Text
Serological Testing Market
#Serological Testing Market scope#Serological Testing Market report#Serological Testing Market research
0 notes
Text

Dr. William Augustus Hinton (December 15, 1883- August 8, 1959) was a bacteriologist and the first Black Professor at Harvard University. He was born in Chicago to former enslaved Maria Clark and Augustus Hinton. He attended the University of Kansas before transferring to Harvard, where he earned a BS.
He taught at Walden University and the Agricultural and Mechanical College. He attended summer courses at the University of Chicago to further his studies in Physiology and Bacteriology. He earned his MD from Harvard Medical School with honors in three years.
He was not allowed to pursue a career in surgery due to racial discrimination. He taught antibody diagnostic methods known as serological techniques at Harvard’s Wassermann Laboratory. He was a volunteer assistant at the Department of Pathology at Massachusetts General Hospital, where he performed autopsies on those who died of syphilis.
He would go on to change the course of medical history with his findings. He used serology to develop a new method of diagnosing syphilis and, as a result, became an expert on the disease. He was named Director of the Laboratory Department at Boston Dispensary. He returned to Harvard, where he taught preventive medicine, immunology, and bacteriology.
He became the first Black scientist to become a member of the American Society for Microbiology. He created a flocculation test for syphilis. He developed another syphilis test with a colleague known as the Davies-Hinton test which was considered a medical breakthrough. He became the first African American to publish a medical textbook titled Syphilis and Its Treatment.
He was an assistant teacher and a lecturer. He was promoted to Professor toward the end of his career, he was named Clinical Professor of Bacteriology and Immunology, making him the first Black full Professor at the institution.
After retiring from Harvard, he worked as a physician at the Mass Hospital School for Crippled Children and served as a special consultant to the US Public Health Service. #africanhistory365 #africanexcellence
5 notes
·
View notes