#software for pathology lab
Explore tagged Tumblr posts
Text
0 notes
Text
Unleash the Power of Technology in Your Lab with Lab Software
In today’s fast-paced healthcare environment, efficiency is paramount. Laboratories, especially in pathology and hospital settings, require robust software solutions to manage their extensive data and workflows effectively. The integration of cutting-edge lab software, such as Hospital Management System HMS software , Laboratory Information Management Systems (LIMS) for pathology, and Hospital Enterprise Resource Planning (ERP) software, can significantly enhance a lab’s operational efficiency. This article delves into how these advanced software solutions can revolutionise your lab’s performance.

HMS Software: Streamlining Hospital Operations
Hospital Management System (HMS) software is designed to manage the comprehensive operations of a hospital. It integrates various functions such as patient registration, appointment scheduling, billing, and inventory management. For pathology labs, HMS software offers seamless integration with laboratory operations, ensuring that patient information flows smoothly from the hospital’s departments to the lab.
HMS software reduces administrative burdens and minimises errors by automating data entry and management. This leads to improved patient care, as healthcare providers can access accurate and up-to-date information promptly. Furthermore, HMS software enhances communication between different hospital departments, fostering a collaborative environment.
LIMS for Pathology: Enhancing Lab Workflow
Laboratory Information Management Systems LIMS for pathology are specifically designed for managing laboratory data and workflows. In pathology labs, LIMS software plays a crucial role in sample tracking, test result management, and quality control. It ensures that every sample is accurately tracked from collection to result delivery, reducing the risk of sample mix-ups and errors.
LIMS for pathology streamlines the workflow by automating routine tasks, such as data entry and report generation. This not only saves time but also improves the accuracy of lab results. With features like electronic record-keeping and automated alerts, LIMS software helps labs maintain compliance with regulatory standards, ensuring high-quality outcomes.
Hospital ERP Software: Integrating Operations
Hospital Enterprise Resource Planning (ERP) software integrates various hospital operations into a unified system. It covers everything from financial management and human resources to supply chain management and patient care. For pathology labs, integrating with hospital ERP software means better resource management and coordination.
Hospital ERP software provides real-time data analytics, helping lab managers make informed decisions about resource allocation and process improvements. This leads to enhanced productivity and cost-efficiency. By integrating lab operations with other hospital functions, ERP software ensures that the lab operates as an integral part of the hospital ecosystem, leading to better overall patient care.

The adoption of advanced lab software solutions like HMS software, LIMS for pathology, and hospital ERP software can transform the efficiency and effectiveness of pathology labs. These tools automate routine tasks, improve data accuracy, and enhance communication within the hospital. By streamlining workflows and integrating operations, they enable labs to deliver faster, more reliable results, ultimately improving patient care. Investing in cutting-edge lab software is not just a technological upgrade; it’s a strategic move towards operational excellence.
0 notes
Text
Discover Advanced Pathology Lab Software Designed for Patna - Riya Techno Software
Revolutionize diagnostics in Patna with Riya Techno Software! Get cutting-edge pathology software for seamless operations & accurate results.
0 notes
Text

Laboratory Management System In India | pathology lab software laboratory management system application can manage and track laboratory data and operations. It also offers a wide range of functionalities and features to support various laboratory processes and workflows. https://noetic-labs.com/Laboratory-Management-System.html
0 notes
Text
Pathology Software: Online Payments?
In order to ensure that labs receive payment as soon as possible, modern pathology technologies are often integrated with billing interfaces. In addition to billing integrations, laboratories usually offer patients the option of co-paying. Therefore, adding a self-payment feature to the pathology software could be advantageous for both lab service providers and patients.
It can be beneficial to give pathology software systems the ability to accept digital payments in the modern era. It is true that we can simplify the management of incoming payments for lab staff and patients by integrating digital payment options into pathology software. Furthermore, we can provide lab service providers with an intuitive dashboard to track payments and notify patients of outstanding balances.
0 notes
Note
re: breast cancer ai, is the testing that would need to be done to make sure it's an accurate result invasive or expensive or both?
It seems I jumped the gun when I reblogged that article. Despite them using a mammogram on the post's images, this AI innovation is for pathology, not radiology. I was talking about computer-aided detection for mammography, but this is a different beast entirely.
--
So some background, DCIS is known as ductal carcinoma in situ and is a pre-cancerous or a non-invasive cancerous lesion of the breast, depending on who you ask. Approximately 1/3 of people who have this develop actual breaat cancer aka it leaves the duct and start invading other things. So to make sure cancer doesn't develop, people are often recommended to excise it or even get a mastectomy - the removal of the whole breast - to treat it.
But doesn't that sound a little extreme when 67% of people may not even develop it?
I mean, look at prostate cancer, where urologists watch and wait to see if cancer will progress using labs, imaging, and occasionally biopsy. Because by the time you are diagnosed with prostate cancer, you're more likely to die from something else like a heart attack, old age, etc than from the cancer itself because it tends to grow so slowly. And getting a preemptive removal of the prostate - prostatectomy - has a lot of unwanted consequences including urinary incontinence and erectile dysfunction.
Wouldn't it be nice then if we could figure out what forms of DCIS would turn into full-blown cancer and what sort would behave more like prostate cancer?
Well, we do have some tech in the works, I believe, in the form of RNA sequencing, where you look at the cancer's genetic profile to see if it will go bad quickly. But RNA sequencing is expensive, and I don't believe it's common place yet.
And that's what the MIT research comes in. They are stating they can predict the behavior of DCIS, whether it'll act good or bad, by taking tissue samples of past known DCIS (and already having documented their behavior if they turned into cancer or not and how fast they do), using a chromatin stain to create slides, and feeding them into an AI to generate a predictive model that could tell from a tissue slide how DCIS will behave based on the model.
Staining and creating slides is cheaper than doing RNA sequencing according to the article ( I do not have the numbers on hand, but it seems like it'd be right), so this is a big deal as it both is cheaper for the patient and may allow a patient to avoid unneeded surgery.
Of course, the model needs to be validated to see if it works in practice, but it sounds promising.
---
As for what I was taking about erroneously, it's called computer-aided detection, and it analyzes mammogram images.
The CAD software can detect areas that are suspicious on a mammogram and alert a radiologist to them. The problem is that it can mark areas that may seem suspicious to the computer but seems normal to the mammographer. But what does a mammographer do with that information then?
The normal workflow of mammography is that you find a suspicious lesion on screening mammogram, ask the patient to come back to take diagnostic / magnified / compression images aka the breast getting smooshed views (more cost and discomfort), and if it's still suspicious with additional views you do a biopsy (invasive).
If the CAD is wrong but you test, you have done unnecessary imaging or worse even an unnecessary biopsy.
But if you the mammographer say that the CAD is wrong when it's right, you just missed cancer and put yourself in a very tight spot if they run the CAD software on your images.
To answer your question from what I was referring to, yes, the testing to confirm all the findings that the CAD points out would add a lot of unnecessary tests and biopsies for the patient.
2 notes
·
View notes
Text
Spatial Genomics Transcriptomics Market to Surge with Single-Cell Resolution

The Global Spatial Genomics Transcriptomics Market is estimated to be valued at USD 335.8 Mn in 2025 and is expected to exhibit a CAGR of 13% over the forecast period 2025 to 2032.
Spatial genomics and transcriptomics products enable high-resolution mapping of gene expression within tissue sections, combining imaging-based sequencing with computational analytics. These platforms offer single-cell resolution and multiplexed detection of thousands of transcripts, giving researchers unprecedented insights into cellular heterogeneity and microenvironmental interactions. Advantages include precise localization of biomarkers, improved target validation in oncology and neuroscience, and accelerated drug discovery through deeper tumor-immune profiling. As demand grows for integrated multi-omics and digital pathology workflows, Spatial Genomics Transcriptomics Market Insights is an instruments and reagents—such as barcoded slides, fluorescence-based probes, and advanced bioinformatics software—are becoming essential tools in academic and commercial research labs. The need for robust spatial profiling in personalized medicine and biomarker discovery continues to drive adoption, while ongoing innovations reduce data-analysis bottlenecks.
Get more insights on,Spatial Genomics Transcriptomics Market
#CoherentMarketInsights#SpatialGenomicsTranscriptomicsMarket#SpatialGenomicsTranscriptomics#SpatialGenomicsTranscriptomicsMarketInsights#Kits&Reagents
0 notes
Text
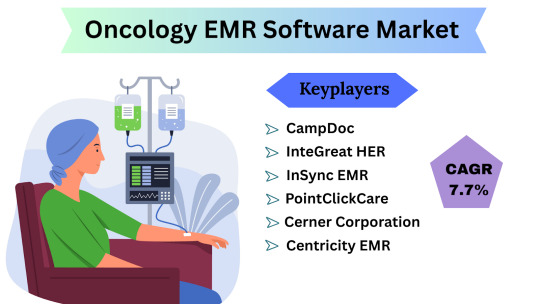
Oncology EMR Software Market Size, Share & Trends Analysis Report By Product ,By End-use, And Segment Forecasts (2024-2031)
Oncology EMR Software Market Overview and Estimation The Oncology EMR (Electronic Medical Records) Software Market Size is poised for steady expansion, driven by growing cancer incidence, the push for value-based care, and the digitization of clinical workflows in oncology centers. According to industry data, the market is expected to grow at a compound annual growth rate (CAGR) of 7.7% from 2024 through 2031, reflecting strong uptake of specialized EMR solutions that integrate treatment planning, chemotherapy ordering, and oncology-specific analytics.
Oncology EMR Software Latest News and Trends In recent months, several key trends have shaped the Oncology EMR landscape:
Artificial Intelligence & Machine Learning Integration Leading vendors are embedding AI-driven decision-support modules into their EMRs to assist oncologists with protocol selection, early adverse-event detection, and personalized treatment pathways.
Interoperability Accelerators The 21st Century Cures Act in the U.S. and similar initiatives in Europe and Asia have intensified focus on seamless data exchange. Oncology EMRs are increasingly adopting FHIR-based APIs to share patient summaries, radiation therapy plans, and pathology results across hospitals, labs, and registries.
Cloud-Native Deployments A shift from on-premises implementations toward cloud-hosted, subscription-based models is underway—driven by lower upfront costs, faster upgrades, and enhanced remote-access capabilities for multi-site cancer centers.
Tele-oncology Modules COVID-era telehealth uptake has extended to specialty care: vendors now bundle video-consultation, e-consent, and remote symptom-reporting features directly within oncology EMRs, reducing the friction of managing virtual visits.
Real-World Evidence (RWE) Collection Payers and life-science firms are collaborating to use de-identified EMR data for RWE studies. Oncology EMRs are being enhanced to capture structured patient-reported outcomes and longitudinal safety data to support post-market surveillance and value dossiers.
Get Free Sample Pdf : https://www.datamintelligence.com/download-sample/oncology-emr-software-market
Oncology EMR Software Market Segmentation
The Oncology EMR market can be described across multiple dimensions, each demonstrating unique adoption dynamics:
By Component: Solutions (software licenses and perpetual-license packages) constitute the bulk of spending, as oncology centers prefer comprehensive suites that encompass treatment ordering, protocol management, and outcome tracking. Services—primarily customization, integration, and training—account for a significant share of revenue, especially among large academic cancer institutes requiring complex interfacing with laboratory, radiology, and pharmacy systems.
By Deployment Type: Historically, on-premises deployments led the market; however, recent migration trends show cloud-based oncology EMRs capturing nearly two-fifths of new deals by revenue share. Smaller hospitals and outpatient clinics favor cloud subscriptions for lower capital expenditure and predictable operating costs, while top-tier cancer centers continue to invest in on-prem deployments for tighter control over data sovereignty and advanced customization.
By End User: Comprehensive Cancer Centers represent the largest end-user segment, given their high patient volumes and the need for integrated care pathways. Hospitals with designated oncology wings follow closely, leveraging EMRs to coordinate multidisciplinary tumor-board discussions. Specialty outpatient clinics and physician practices collectively make up the remaining slice, adopting lightweight, focused solutions for chemotherapy ordering and patient scheduling.
By Functionality: Core modules—patient demographics, clinical documentation, and order entry—comprise the foundational spend. Advanced functionalities such as chemotherapy regimen libraries, radiation therapy interfacing, and billing-code mapping are driving incremental growth, together representing more than half of total annual license revenues.
Oncology EMR Software Regional Analysis: USA & Japan
United States: The U.S. commands the largest slice—approximately 40% of global Oncology EMR revenues—propelled by a mature healthcare IT infrastructure and robust reimbursement frameworks. The 21st Century Cures Act’s information-blocking rules have incentivized providers to adopt interoperable, certified EMR systems, while Medicare’s Oncology Care Model encourages tight integration between EMR data and value-based payment programs. The U.S. market is projected to grow at a CAGR slightly above the global average, fueled by consolidation among health systems and expansion of outpatient oncology networks.
Japan: Japan represents roughly 12–15% of global Oncology EMR spend, with steady annual growth. Government initiatives such as the “Society 5.0” healthcare vision and the Ministry of Health, Labour and Welfare’s push for digital hospital adoption have accelerated EMR deployments. However, slower legacy-system turnover and stringent data-localization policies temper cloud-migration rates. Local players often partner with global vendors to align with Japan’s unique clinical workflows and language requirements.
Key Highlights from Recent Reports
Oncology EMR solutions with integrated clinical-trial matching capabilities are seeing over 20% higher adoption rates at academic cancer centers.
Cloud-hosted oncology EMRs are reducing total cost of ownership by up to 25%, largely through automated updates and shared-service support models.
Interoperability accelerators such as SMART on FHIR apps are projected to triple in number by 2026, enabling rapid third-party innovation within oncology workflows.
Oncology EMR Software Key Players & Competitive Landscape:
The market is moderately consolidated, with the top five vendors holding a combined share of over 60%. Recent M&A and research highlights include:
Epic Systems – Dominant in large health systems; piloting AI-driven regimen optimization tools.
Oracle Cerner – Following the Cerner acquisition, expanding cloud-native oncology modules.
Allscripts – Partnering with life-sciences firms to integrate RWE-capture features.
GE Healthcare – Leveraging its imaging-informatics heritage to offer unified EMR-PACS-RT workflows.
athenahealth – Gaining traction among specialty clinics with its flexible, subscription-based oncology package.
Additionally, smaller niche vendors such as Aria (Oncology Information System by Varian) and Elekta iO EMR continue to innovate around radiation-oncology integrations and research-data export.
Conclusion
The Oncology EMR Software Market is on a solid growth trajectory, underpinned by a projected 7.7% CAGR through 2031. As precision oncology, real-world evidence demands, and regulatory imperatives converge, providers will increasingly seek comprehensive, interoperable EMR platforms tailored to the complexities of cancer care. The transition toward cloud-native deployments and AI-enabled decision support will accelerate operational efficiencies, while regional dynamics—particularly in the U.S. and Japan—will shape adoption paths. Overall, the market is set to mature from a basic digital-record offering into a sophisticated, intelligence-driven platform central to the future of oncology treatment delivery.
0 notes
Text
How Hospital Management Software Drives Operational Excellence in Modern Healthcare
The demands on modern hospitals have never been greater. From rising patient volumes to the complexity of compliance, hospitals today require a digital solution that enhances accuracy, agility, and efficiency. That’s where Hospital Management Software like Grapes IDMR becomes not just helpful but essential.
Designed for professionals in healthcare administration and technical operations, Grapes IDMR offers a robust, end-to-end platform that empowers hospitals to optimize their services and processes. In this article, we’ll explore how this software supports operational excellence across departments, and why it’s becoming the gold standard for medical institutions across India and beyond.
Unified Systems for Consistent and Efficient Hospital Operations
In traditional hospital setups, departments often work in silos nursing, pharmacy, pathology, billing, radiology, etc., each operating with its own systems or paperwork. This lack of integration leads to communication gaps, redundant work, and delayed patient care.
Grapes IDMR solves this by integrating all critical hospital functions within a single ecosystem. Each module from OPD/IPD management to discharge and billing is connected to a central database, ensuring data is always synchronized and available in real-time. Administrators no longer need to switch between tools or chase departments for updates. Instead, Grapes IDMR enables consistent workflows and automated notifications, ensuring that everyone from doctors to back-office teams is on the same page.
Improving Efficiency and Reducing Turnaround Time
Hospital efficiency depends on how fast and accurately staff can manage appointments, patient records, lab results, diagnostics, and prescriptions. Grapes IDMR automates these steps, dramatically reducing the time required for each.
For instance, a diagnostic report from the pathology lab is instantly available to the consulting doctor, who can immediately adjust the treatment plan without any paper handling or delays. Nurses can track medication administration schedules directly from the system, minimizing errors and improving compliance. Moreover, the appointment management system within Grapes IDMR uses intelligent scheduling algorithms to reduce patient wait times and improve resource utilization. The result is faster service delivery, better patient throughput, and higher satisfaction.
Financial Transparency and Smarter Revenue Management
Financial management is critical to a hospital’s sustainability. Grapes IDMR simplifies this by offering integrated billing, accounting, and insurance claim processing under one umbrella. Every service rendered whether it’s a test, consultation, or procedure is automatically recorded and billed.
The billing engine supports complex configurations like multi-department charges, consumables, service packages, and doctor-wise revenue distribution. For insurance-covered patients, the software handles real-time eligibility checks, e-claim submissions, and tracking reducing denials and improving collection cycles. Hospitals benefit from transparent, auditable financial data, while administrators gain insights into profit centers, pending receivables, and daily revenue summaries with a single click.
Role-Based Access and Workflow Control
In a healthcare setup, not every user should have access to all data. Grapes IDMR offers role-based access control, ensuring that information is shared strictly on a need-to-know basis. Doctors, nurses, lab staff, pharmacists, and administrators each get tailored dashboards and permissions according to their roles.
This layered control not only secures sensitive data but also prevents workflow interruptions. Staff can complete their responsibilities faster because the system is optimized for their specific tasks, reducing friction and training time. Additionally, audit trails maintain a record of every user action—supporting accountability, transparency, and compliance with health regulations like HIPAA, NABH, and GDPR.
Custom Reporting and Decision-Making Tools
Hospitals need data to make informed decisions about performance, resource planning, clinical outcomes, and finances. Grapes IDMR offers over 200 pre-configured reports, along with a powerful custom report builder.
You can track metrics such as:
Bed occupancy rate
Doctor efficiency
Laboratory turnaround time
Pharmacy stock movements
Patient satisfaction trends
With visual dashboards and exportable reports, administrators and department heads can identify bottlenecks, implement corrective actions, and drive continuous improvement—all in real-time.
Flexible and Scalable to Any Hospital Size
Not all hospitals are the same. A general hospital, a specialty center, and a rural clinic have very different operational needs. That’s why Grapes IDMR is modular and scalable. Whether you need a basic OPD and billing setup or a full suite covering HR, payroll, diagnostics, and asset management, the software can be deployed according to your priorities.
Moreover, for multi-location hospitals or healthcare chains, Grapes IDMR enables centralized control with branch-wise reporting. Each facility remains autonomous in daily operations, while head office teams can oversee performance, compliance, and growth strategies from a single interface.
Conclusion: Excellence Starts with Digital Precision
In today’s healthcare economy, excellence depends on how fast, accurately, and transparently a hospital can operate. Grapes IDMR, a leading hospital management software, empowers institutions to meet this challenge with confidence. It replaces paperwork and disconnected systems with intelligent automation, real-time coordination, and reliable analytics. For hospital professionals, it means fewer manual processes, lower costs, and higher performance across the board.
Get the system that moves with your hospital’s mission.
Contact Grapes Innovative Solutions Today:
Phone: +91 7510330000
Email: [email protected]
Website: Grapes Innovative Solution
Take control of your operations. Let Grapes IDMR power your next phase of growth.
1. How does Grapes IDMR improve day-to-day hospital operations?Grapes IDMR integrates all departments like OPD, IPD, billing, diagnostics, pharmacy, and admin into one system, automating routine tasks and enabling real-time data sharing to reduce delays and improve efficiency.
2. Is Grapes IDMR secure and compliant with healthcare regulations?Yes, Grapes IDMR is built with 256-bit encryption, audit trails, role-based access, and compliance with global standards like HIPAA, NABH, and GDPR to ensure complete data security and legal adherence.
3. Can Grapes IDMR be customized for different sizes and types of hospitals?Absolutely. Grapes IDMR is modular and scalable, allowing hospitals to implement only the features they need whether they’re a small clinic, specialty center, or a multi-location hospital network.
#HospitalManagementSoftware #GrapesIDMR #HealthcareIT #HealthTechIndia #DigitalHospitals #MedicalSoftware #SmartHealthcare #HospitalAutomation #OperationalExcellence #HealthcareSolutions #CloudHMS #IntegratedHospitalSystem #HospitalEfficiency #HospitalBilling #DigitalTransformationHealthcare #PaperlessHealthcare #HospitalWorkflow #MedicalAdminTools #EHRSystem #HealthcareCompliance #GDPRCompliance #HIPAAReady #HospitalRevenueManagement #ModularHMS #HealthcareInnovation #RealTimeDataHealthcare #AdminEfficiency #DoctorDashboard #PatientExperienceTech #GrapesHMS
0 notes
Text
Unleash Efficiency: Riya Techno's Pathology Lab Software Tops in Patna
Boost your lab's productivity with Riya Techno's top Pathology Lab Software in Patna. Streamline processes & unleash efficiency in diagnostics!
0 notes
Text

laboratory management system application can manage and track laboratory data and operations. It also offers a wide range of functionalities and features to support various laboratory processes and workflows.
0 notes
Text
B.Sc. Medical Lab Technology: Course Details, Scope & Careers
Behind every accurate diagnosis and effective treatment lies a skilled professional working in the background — a Medical Laboratory Technologist. If you're someone who finds purpose in science and precision, then pursuing a B.Sc. in Medical Lab Technology (MLT) can be your gateway into the healthcare sector.
In this blog, we’ll cover what the course entails, the skills you'll gain, and the diverse career paths waiting for you after graduation.
What is B.Sc. in Medical Lab Technology?
B.Sc. Medical Lab Technology is a 3-year undergraduate degree that prepares students to perform diagnostic tests, handle laboratory equipment, and assist doctors in detecting diseases. It’s a vital part of the healthcare system, ensuring that patients receive accurate and timely diagnosis.
📘 Learn more about the course from Apeejay Stya University, a reputed institution offering a well-rounded B.Sc. MLT program with modern lab infrastructure.
Course Details
Duration: 3 years (6 semesters)
Eligibility: 10+2 in Science (Physics, Chemistry, Biology/Math)
Admission Process: Merit-based or via entrance exams (depending on the institution)
Mode: Full-time
Core Subjects You’ll Study:
Human Anatomy & Physiology
Biochemistry
Microbiology
Clinical Pathology
Hematology
Immunology
Blood Banking
Medical Ethics & Patient Safety
Instrumentation & Quality Control
Practical training and internships are often an integral part of the curriculum, offering real-world experience in hospital labs and diagnostic centers.
Skills You’ll Gain
By the end of the program, graduates develop:
Proficiency in diagnostic testing and lab procedures
Attention to detail and data analysis
Operation of lab instruments and software
Knowledge of safety protocols and quality standards
Communication and teamwork in clinical environments
Career Scope After B.Sc. MLT
With the rapid growth of diagnostic labs and healthcare facilities, skilled lab technologists are in high demand. Here are some popular job roles:
Medical Laboratory Technologist
Pathology Lab Technician
Blood Bank Technician
Microbiologist (Lab Assistant)
Research Assistant in Healthcare
Quality Control Analyst in Pharma
Technical Officer in Diagnostic Labs
Healthcare Data Analyst (with additional certifications)
Graduates can also opt for higher studies such as M.Sc. MLT, Master’s in Public Health, or specialized diplomas in Clinical Biochemistry, Cytogenetics, or Molecular Biology.
Why Choose B.Sc. MLT?
Contribute meaningfully to patient care and diagnostics
High demand in hospitals, private labs, research centers, and pharmaceutical firms
Offers a stable career with opportunities for specialization
Ideal for science enthusiasts looking for a hands-on healthcare role
Shorter course duration compared to medical degrees, yet with impactful outcomes
Conclusion
B.Sc. Medical Lab Technology is more than just a course — it's a profession that ensures accurate diagnosis and supports life-saving treatment. With healthcare systems expanding and becoming more tech-driven, MLT professionals are not just behind the scenes anymore — they are frontline contributors to better health outcomes.
🔬 Interested in joining this exciting field? Explore the program in detail at Apeejay Stya University and start your journey towards a rewarding healthcare career.
0 notes
Text
What Are the Benefits of Using AI in Healthcare and Hospitals?

In the middle of a busy hospital, doctors are managing overflowing patient loads, nurses are stretched thin, and administrators are juggling data across outdated systems. It’s a scene that plays out daily in healthcare facilities around the world.
Artificial Intelligence in Healthcare is emerging as a powerful solution to these everyday challenges, offering smarter ways to manage care, streamline operations, and support medical staff in real-time.
But what if many of those manual tasks could be handled automatically?
What if decision-making became faster, more accurate, and personalized, not someday but today?
That’s exactly what artificial intelligence (AI) in healthcare is making possible.
From improving diagnostic accuracy to reducing administrative overhead, AI in healthcare and hospitals is proving to be more than just a trend. It’s a real solution to real problems.
This detailed blog is your practical guide to understanding the clear, measurable benefits AI is bringing to the healthcare industry.
What Is Artificial Intelligence in Healthcare Industry?
Artificial Intelligence (AI) in healthcare industry refers to the application of advanced algorithms, machine learning models, and data-driven technologies that mimic human reasoning and decision-making to improve healthcare delivery. These AI-powered systems are designed to analyze massive volumes of structured and unstructured data, from medical records and different types of lab results to imaging scans and real-time patient monitoring, and extract meaningful insights in seconds.
Unlike traditional software that follows static rules, AI-based systems continuously learn and evolve from every new single data input it gets, and this allows them to not only identify patterns and trends but also predict outcomes, suggest treatments, and smartly automate tasks that previously required manual effort or specialist intervention.
Common AI applications in healthcare include:
Detecting anomalies in radiology and pathology scans
Forecasting patient deterioration or hospital readmission risks
Assisting with drug discovery and clinical trial matching
Streamlining administrative tasks like billing, coding, and scheduling
Personalizing care through AI-driven patient recommendations
By reducing the cognitive load on clinicians and enhancing decision-making with real-time insights, Artificial Intelligence in healthcare helps drive better outcomes, faster interventions, and more efficient operations. This ultimately benefits both patients and providers.
Why Is AI Important for Modern Hospitals and Healthcare Providers?
Hospitals today are under pressure to deliver faster care, improve patient experiences, and reduce costs overall, all at the same time. AI meets these demands head-on.
Here’s how:
Faster decision-making: AI can analyze patient data instantly and offer decision support in real-time.
Reduced manual workload: Automating repetitive tasks saves time for doctors, nurses, and administrative staff.
Data-driven insights: AI uncovers trends and patterns that help identify risks earlier and tailor treatments more precisely.
The result? Better care delivery and smoother hospital operations without burning out your team.
How Does AI Improve Diagnostics and Patient Outcomes?
Accurate diagnosis is critical. However, humans are limited by time and cognitive capacity. AI tools help bridge the gap by scanning through complex medical data faster and often with higher accuracy.
Real examples:
Radiology: AI models detect early signs of tumors or fractures in X-rays, MRIs, or CT scans that even skilled radiologists may miss.
Pathology: Algorithms identify anomalies in tissue samples or lab reports with high accuracy.
Predictive analysis: AI evaluates a patient’s vitals and historical data to predict conditions like heart failure or sepsis before symptoms escalate.
By supporting clinical decisions, AI helps reduce diagnostic errors and leads to faster, more targeted treatments.
In What Ways Does AI Support Doctors and Medical Staff?
AI doesn’t replace clinicians. It supports them.
Here’s how:
Voice-to-text transcription reduces paperwork and frees up doctors to spend more time with patients.
Clinical decision support systems (CDSS) recommend personalized treatment options based on patient history and medical literature.
AI-powered workflow tools automate scheduling, billing, and reporting, easing administrative burden.
When AI handles the backend complexity, caregivers get to focus more on what matters most: the patient.
Can AI Help Reduce Operational Costs in Hospitals?
Yes, significantly.
Managing hospital resources is costly, from staffing and scheduling to equipment usage. AI helps optimize these operations by:
Forecasting patient admission rates to better allocate staff.
Minimizing unnecessary lab tests through intelligent recommendations.
Automating inventory management for pharmaceuticals and supplies.
Reducing claim denials and billing errors with AI-powered revenue cycle management.
The result is leaner operations, improved financial health, and better use of staff time.
How Does AI Enhance Patient Engagement and Personalization?
Modern patients expect fast, personalized, and on-demand care. AI helps providers deliver it.
AI chatbots assist patients with appointment booking, pre-checkup queries, and medication reminders.
Recommendation engines suggest wellness tips, therapies, or content based on patient behavior.
Patient portals powered by AI enable tailored follow-ups and ongoing health monitoring.
This not only improves satisfaction but also boosts adherence to treatment, a win for both the provider and the patient.
What Role Does AI Play in Predictive Healthcare and Prevention?
Prevention is better than cure, said by the Dutch humanist Desiderius Erasmus, and AI excels at prevention.
Using large datasets, AI can predict disease outbreaks, hospital readmission risks, or which patients are at risk of developing chronic illnesses. By intervening earlier, healthcare providers can save lives and cut down on emergency treatments.
Some AI tools use wearable device data (like heart rate or sleep cycles) to identify changes in patient health and alert care teams before an issue becomes critical.
Is AI Improving Access to Healthcare in Rural or Underserved Areas?
Absolutely, AI is bridging the healthcare gap by making expert-level care more accessible, even where there are few specialists available.
Telemedicine platforms use AI to triage patients remotely and prioritize those needing urgent care.
Mobile diagnostic tools powered by AI help screen for eye disease, skin conditions, and more without needing a local specialist.
Language processing tools break down communication barriers between patients and providers across regions.
By reducing the need for in-person visits and empowering local clinics, AI is helping bring quality care to underserved populations.
What Are the Benefits of AI-Powered Chatbots in Healthcare?
AI chatbots are one of the most practical and cost-effective tools hospitals can deploy today.
They assist with:
Answering common patient questions 24/7.
Providing initial symptom assessments.
Booking or modifying appointments.
Sharing post-treatment care instructions.
Collecting feedback after discharge.
These bots not only reduce strain on front-desk staff but also make patients feel supported at every step of their journey.
How Secure and Ethical Is AI in Medical Environments?
Security and ethics are serious concerns, and rightfully so. Healthcare AI-powered systems must comply with regulations like HIPAA and GDPR to ensure data privacy.
Leading providers implement:
Data encryption and secure cloud infrastructure.
Access controls to ensure only the right, authorized personnel can view patient data.
Bias audits to ensure AI does not reinforce discrimination in diagnosis or treatment.
Trust is central to healthcare. That’s why any AI solution must be transparent, explainable, and constantly monitored.
What Are the Long-Term Benefits of Artificial Intelligence in Healthcare?
While many healthcare providers are already seeing the short-term benefits of Artificial Intelligence, such as faster diagnoses and streamlined workflows, its true potential lies in the long-term transformation of the entire healthcare ecosystem.
AI is not just a smart tool for efficiency. It’s a foundational technology that is shaping how healthcare systems will operate, grow, and deliver care in the years to come.
Let’s explore the key areas where Artificial Intelligence in healthcare is creating sustainable, long-term improvements for both care providers and patients.
Reduces Clinician Burnout at the Scale
By automating repetitive, administrative, and time-intensive tasks like charting, billing, data entry, and even appointment scheduling, AI, with the help of different AI Algorithms, frees up clinicians to focus more on direct patient care. This reduces stress and improves job satisfaction over the long term.
Improves Accuracy & Personalization of Treatments with AI-powered Algorithms
AI Algorithms continuously learn from new patient data, medical literature, and real-world outcomes. Over time, this enables more precise diagnoses, tailored treatment plans, and adaptive care paths that evolve based on the patient’s response.
Reduces Readmission and Improves Long-Term Health Outcomes
Predictive models powered by AI can flag patients who are likely to be readmitted or develop complications. With earlier interventions and better follow-ups, hospitals can proactively reduce emergency visits and improve recovery trajectories.
Provides Deep Insights from Population-Level Data
AI helps public health systems monitor, track, and respond to population health trends. It identifies hotspots for disease outbreaks, analyzes social determinants of health, and informs better policymaking through large-scale pattern recognition.
Supports Scalable, Future-Ready Infrastructure
As healthcare data grows exponentially, AI-powered systems are designed to scale alongside it. With each patient interaction, the system becomes smarter, helping healthcare providers build robust, intelligent infrastructures that evolve with new technology, data sources, and care models.
Artificial Intelligence in healthcare is more than a temporary upgrade. It is an investment in agility, resilience, and smarter decision-making that ensures healthcare systems are not just equipped for today’s demands but ready for tomorrow’s possibilities.
Should Healthcare Startups and Clinics Invest in AI Right Now?
If you're building or scaling a healthcare business in 2025, now is the right time to explore AI integration.
You don’t need massive budgets or deep tech teams to get started. Many AI solutions are cloud-based, API-driven, and scalable for small and mid-sized providers.
Whether it's automating front-office tasks, enhancing diagnostics, or offering better patient support, Artificial Intelligence in healthcare is no longer a luxury. It's a competitive advantage.
#Artificial Intelligence in Healthcare#AI in Healthcare#AI in Healthcare Benefits#Artificial Intelligence for Healthcare#Healthcare Business in 2025
0 notes
Text
Mastering Hospital Operations with Intelligent HMS Software
The complexity of running a healthcare facility demands more than just manpower it calls for digital intelligence. That’s where HMS software becomes indispensable. With the ability to oversee every aspect of a hospital’s ecosystem, it serves as a centralized platform for clinical, administrative, and operational excellence.
One such solution making waves in healthcare technology is Grapes IDMR, a product developed by Grapes Innovative Solutions. It delivers a complete digital framework that hospital leaders can depend on for accuracy, efficiency, and real-time visibility.
Understanding the Core Need for HMS Software
Running a hospital isn’t limited to doctors and nurses. There are appointments to book, pharmacy inventories to manage, labs to coordinate, bills to generate, and staff to supervise. These tasks, when disconnected, result in slower service, human errors, and a frustrating experience for both patients and healthcare providers. HMS software bridges this gap by connecting all hospital departments under one interface. With digital workflows, tasks are streamlined, redundancies are reduced, and hospitals function as well-oiled machines.
Grapes IDMR: The Complete Digital Control Center
Grapes IDMR stands out for its intuitive interface and modular build. Designed for both small clinics and large multispecialty hospitals, it empowers healthcare teams to digitize their processes without overwhelming them with technical complexity.
The software encompasses a full suite of modules:
Patient Registration & EMR
Outpatient & Inpatient Flow
Pharmacy & Inventory
Pathology & Imaging
Billing, Insurance & Packages
Nursing, Ward, and ICU Management
Doctor Roster, Leaves & Appointments
Procurement, HR, and Admin Panels
Each module can work independently or as part of a bigger connected workflow.
The Ecosystem Inside Grapes IDMR
Clinical Management:
Doctors, nurses, and clinical staff can quickly access patient histories, allergies, diagnoses, medications, and lab reports in a single view. It enables:
Quick consultation decisions
Better coordination between departments
Seamless communication with nursing staff
Patient-Centered Tracking:
From initial registration to discharge, patients are continuously monitored across modules. With the HMS software, their every encounter, transaction, and update is traceable, reducing errors and confusion.
Admin and Finance Tools:
Administrators get a complete picture of operations. From daily patient flow reports to real-time revenue snapshots and pending dues, Grapes IDMR enables data-driven decision-making.
What Makes Grapes Innovative Solutions a Trusted Partner?
Grapes Innovative Solutions is more than a software developer it’s a healthcare technology enabler. With years of experience in the healthcare sector, their approach focuses on usability, affordability, and impact.
Highlights include:
Personalized onboarding
Branch-wise deployment
Continuous updates and tech support
Integration with mobile apps
Compatibility with Tally, accounting software, and biometric systems
The company takes pride in its close collaboration with hospitals, listening to their feedback and evolving the product with real-world insights.
conclusion
Efficient hospitals don’t happen by accident. They are built on systems that allow their people to do what they do best care for patients. With HMS software like Grapes IDMR, healthcare institutions gain a dependable ally in managing clinical, financial, and administrative workflows. When backed by a tech partner like Grapes Innovative Solutions, hospitals can take the digital leap confidently knowing they’re supported by experience, innovation, and an unwavering commitment to better healthcare.
Reach out via Gmail: [email protected] the official website: Best hms software in india
Call us : 7510330000
Frequently Asked Questions
Can Grapes IDMR be accessed remotely?Yes, the software supports remote access through secure login, ideal for multi-location management and offsite consultations.
Is staff training included?Yes, Grapes Innovative Solutions provides complete training for all user levels during and after implementation.
How soon can it be deployed in a hospital? Depending on hospital size and module selection, basic deployment can begin within a week, followed by full-scale rollout.
#HMSsoftware#HealthcareDigitization#HospitalDataManagement#SmartHospitalSystem#DigitalHealthIndia#GrapesIDMR#GrapesInnovativeSolutions#PharmacyTracking#LabDataManagement#HospitalBillingSoftware#ElectronicMedicalRecords#SecurePatientData#AdminControlPanel#IPManagement#OPDWorkflowTool#HospitalDashboard#ProcurementAutomation#HospitalInventory#NursingStationSoftware#DoctorConsultationApp#HospitalFinanceModule#MedicalHistoryDigital#MobileHMSAccess#MultibranchHealthcareSoftware#HospitalITSuite
0 notes
Text
Smarter Lab Operations Start with NZCares Lab Management Software
Streamline your diagnostics with NZCares Laboratory Information Management System. From home collections to instant report generation, our platform automates lab workflows and reduces reporting errors.
Equipped with live sample tracking and AI-powered accuracy checks, it’s ideal for modern pathology labs and diagnostic centers.
🔗 https://www.nzcares.com/laboratory-information-management-system

0 notes