#transplantimaging
Text
Ultrasound is the first imaging modality of choice for imaging transplant kidneys, which can evaluate vasculature and for the presence of hematoma or urinoma. A nuclear renogram can also be performed to assess graft function.
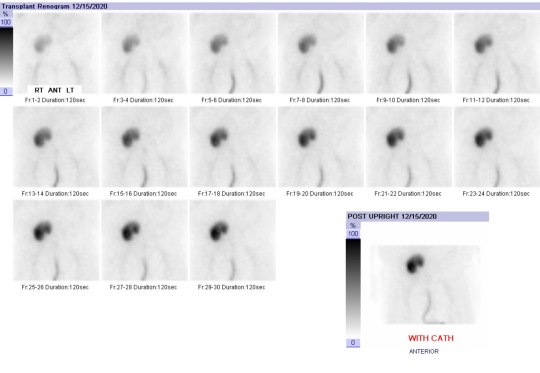
Today's case is a renogram of a patient 4 days post renal transplant with poor urine output. Ultrasound revealed elevated resistive indices. Renogram shows poor perfusion (early images with transplant similar to iliac blood pool), minimal excretion, and persistent cortical retention of tracer throughout the study. Findings may indicate severe ATN, renal artery stenosis, or transplant rejection. This case was likely severe ATN as there was no intervention and graft function recovered.
#TeachingRounds#FOAMEd#FOAMRAd#Radiology#nuclearmedicine#transplant#transplantimaging#transplantmedicine#renaltransplant#kidneytransplant#renogram
2 notes
·
View notes
Photo

Organs needed Image copyright NHS Blood and TransplantImage caption The NHS runs campaigns to encourage donors to register – but rules differ across the UK…
0 notes
Text

Stem cell transplantation (SCT) can cause a host of complications. Graft versus host disease (GVHD) is common and can be severe, affecting many organ systems. In acute GVHD, end-organ damage is the result of recipient's APCs interacting with donor T-cells, leading to donor T-cell activation with a resultant cell-mediated and inflammatory cascade. The pathophysiology of chronic GVHD is not well understood. Skin, small intestine, and liver are most commonly affected; lung involvement is less common.
Acute GVHD typically occurs within 100 days post SCT and can cause bowel wall thickening and/or dilatation, biliary abnormalities, ascites, pulmonary edema, diffuse alveolar hemorrhage, and a myriad of other findings. Chronic GVHD typically occurs within 2 years of SCT and may affect skin, mouth, GI tract, liver, lungs, muscles, joints, or genitals. Imaging is based on presenting symptoms.
Read more about the complications of SCT (including GVHD) from the American Cancer Society. https://www.cancer.org/.../transplant-side-effects.html
Today’s case is a patient 2 months post SCT who presented with shortness of breath, nausea, and vomiting. Lungs demonstrate upper lung predominant groundglass opacities and interstitial thickening, worrisome for acute GVHD. The cecum is thickened and enhancing, with pneumatosis, likely indicating typhlitis (neutropenic colitis). There is also moderate volume ascites.
Case courtesy of Hoe Han Guan, Radiopaedia.org, rID: 166522
#TeachingRounds#FOAMEd#FOAMRAd#Radiology#transplant#transplantimaging#transplantmedicine#infectiousdisease#pulmonology#gastroenterology#hematology#GVHD#stemcelltransplant
2 notes
·
View notes
Text

Complications of lung transplantation include immediate (24 hours to 1 week post-transplant), intermediate (1 week to ~4 months), and late (>4 months to years). Recall that infection can occur at any point and as such is not listed below.
Immediate complications include post-surgical complications, mechanical problems due to size mismatch, primary graft dysfunction (pulmonary edema, seen in most patients), acute rejection (common, treated with steroids with good prognosis, not an imaging diagnosis), and hyperacute rejection (causes florid pulmonary edema, extremely poor prognosis).
Intermediate complications include acute rejection, airway dehiscence, airway stenosis, and pulmonary artery stenosis. Late complications include PTLD and chronic lung allograft dysfunction (which can present with either restrictive or obstructive pattern of PFTs).
For further reading, here is a book chapter giving an overview of this topic. www.ncbi.nlm.nih.gov/pmc/articles/PMC7122723/pdf/978-3-319-94914-7_Chapter_26.pdf
Today’s case is an expiratory image from HRCT of a patient with bronchiolitis obliterans syndrome, the obstructive type of chronic lung allograft dysfunction. Note the right lung groundglass opacities with air trapping (black areas) and left lung bronchiectasis.
Case courtesy of Bruno Di Muzio, Radiopaedia.org, rID: 65183
#TeachingRounds#FOAMEd#FOAMRAd#Radiology#transplant#transplantimaging#transplantmedicine#lungtransplant#pulmonology
2 notes
·
View notes
Text
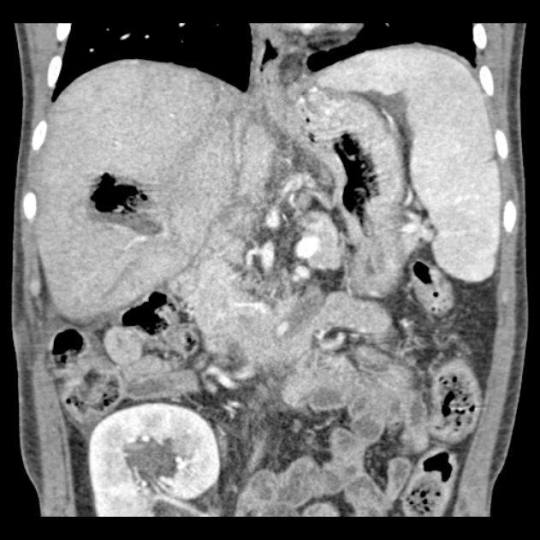
A potential complication of any transplant (including stem cell transplantation) is post-transplant lymphoproliferative disorder (PTLD). As the name suggests this is a lymphatic proliferation that can involve any lymphatic tissue in the body. Common sites of involvement are mesentery, small bowel, lung, and lymph nodes.
PTLD is a spectrum from lymphoid hyperplasia to malignancy. Patients typically present with PTLD 1 month to 7 years after transplant. Patients who present later tend to have more aggressive tumor and poorer prognosis. Read more at link below.
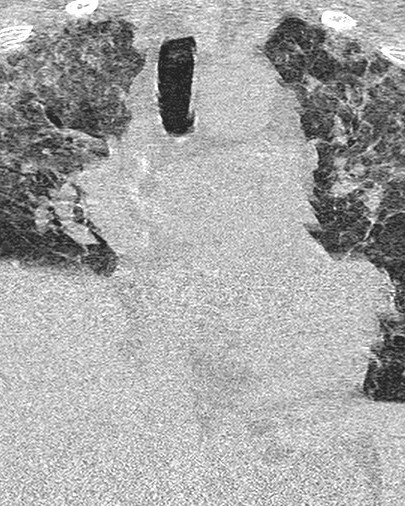
Today's case is a patient with a history of kidney transplant who presented with abdominal pain. CT revealed small bowel thickening and peritoneal nodularity. Biopsy confirmed PTLD.
2 notes
·
View notes
Text
After liver transplantation, ultrasound is the modality of choice for initial evaluation of suspected complications, and follow-up CT or MRI may be warranted depending on findings. (note that transplant rejection is typically diagnosed by biopsy rather than imaging). At ultrasound, the single most important consideration is to evaluate flow in the hepatic arteries, which provide sole blood supply to the bile ducts.
Immediately following transplantation, perihepatic hematoma, right pleural effusion, minimal ascites, and periportal edema are expected imaging findings.
Complications of transplantation include complications of vascular anastomosis (hepatic artery thrombosis/stenosis, pseudoaneurysm, hepatic or portal vein thrombosis), complications of biliary anastomosis (bile leak, biliary obstruction). Other complications include biliary necrosis, abscess, and PTLD (to be discussed later this week).
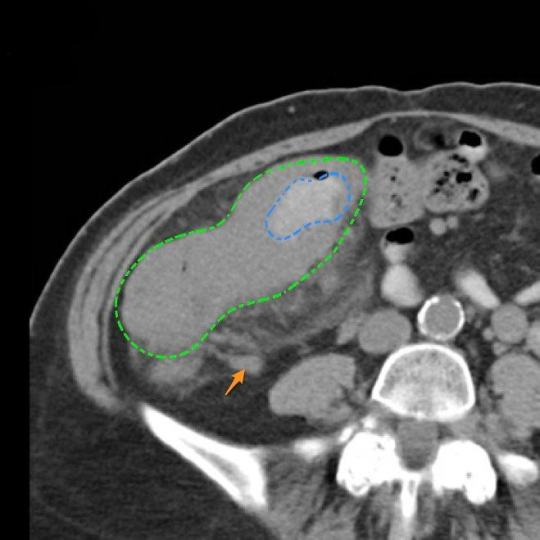
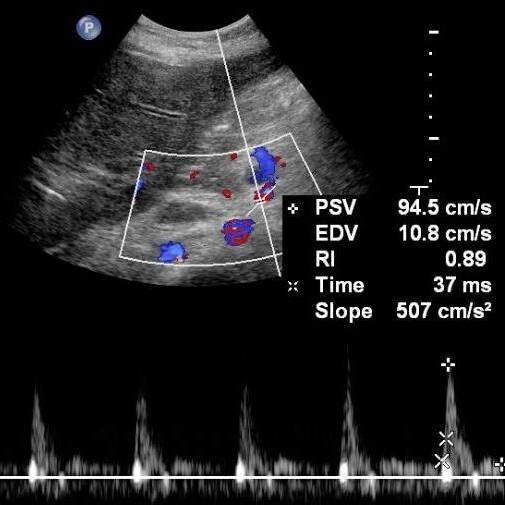
Today’s case is an ultrasound of a transplanted liver showing normal systolic velocity but elevated resistive index in the hepatic artery (0.89, normal 0.5-0.7) which indicates impaired diastolic flow. At follow-up CT, findings were consistent with biliary necrosis, with abscess (2nd image). Case courtesy of Jan Frank Gerstenmaier, Radiopaedia.org, rID: 21876
#TeachingRounds#FOAMEd#FOAMRAd#Radiology#transplant#transplantimaging#transplantmedicine#hepatology#gastroenteroloy#liver#livertransplant
2 notes
·
View notes
Text

As a follow-up to last week's discussion of organ donation, this week we will discuss post-transplant imaging. This is a broad topic covering many organ systems but we hope the pearls we present will expand your knowledge and benefit your practice.
Patients who have undergone any transplant are at elevated risk for infection due to immunosuppression. In addition to pathogens that may affect healthy patients, immunosuppressed patients are at risk for opportunistic infections (infections that would not typically occur in an immunocompetent patient) such as aspergillosis, pseudomonas, CMV, and a host of others. Providers caring for post-transplant patients should have a low threshold to culture or image patients with early signs of infection.
Today's case depicts a bone marrow transplant patient who developed angioinvasive pulmonary aspergillosis. The classic finding is solid nodules with a groundglass halo (indicating angioinvasion), but imaging findings in early pulmonary aspergillosis may be nonspecific (scattered solid nodules and/or groundglass opacities). Early detection and pharmacologic intervention are key.
Case courtesy of Frank Gaillard, Radiopaedia.org, rID: 8538
#TeachingRounds#FOAMEd#FOAMRAd#Radiology#transplant#transplantimaging#transplantmedicine#infectiousdisease#pulmonology
1 note
·
View note