#workplace Lung function testing
Explore tagged Tumblr posts
Text
Why Mandatory Drug and Alcohol Testing at Workplaces is a Must for Health and Safety
In today’s fast-paced industries, ensuring the safety, health, and productivity of workers is more critical than ever. Among the many workplace health practices, drug and alcohol testing stands out as a powerful tool to prevent accidents, maintain workplace integrity, and uphold a culture of responsibility. At Audiomet, we believe mandatory drug and alcohol testing isn’t just a policy—it's a proactive step towards creating safer work environments.
But what makes this testing truly essential? Let’s dive in.
Safety First: Reducing Risks and Hazards
A worker under the influence of drugs or alcohol is significantly more likely to cause or be involved in an accident. Whether operating heavy machinery, working at heights, or managing hazardous substances, impaired judgment can have catastrophic consequences—not just for the individual but for their entire team.
Industries where hazardous substances management, chemical management, and dangerous goods management are part of daily operations especially benefit from routine drug and alcohol testing. Ensuring a sober workforce is a key element in reducing workplace incidents and near-misses.
Health Check Foundations: Building a Safer Environment
Mandatory testing programs don’t operate in isolation—they are often part of a broader occupational health and safety strategy. Integrating drug and alcohol testing with routine medical checks, health checks, and occupational hygiene assessments ensures a comprehensive view of a worker's well-being.
Health professionals often recommend combining drug and alcohol screening with other essential evaluations such as:
Spirometry (to assess lung function),
Flu vaccinations and other vaccination services to reduce illness,
Skin checks to identify occupational dermatological conditions,
Audiometric testing and hearing testing to detect early signs of hearing loss.
These services, often delivered on-site, create a complete health profile and help maintain a fit and reliable workforce.
Improving Workplace Culture and Morale
When workers know their safety and health are a priority, it fosters a culture of trust, responsibility, and mutual respect. Mandatory drug and alcohol policies serve as a deterrent for substance misuse and show that the company values its people and their well-being.
This proactive stance aligns perfectly with initiatives such as health and safety management programs, fit testing, and occupational hygiene strategies. It promotes accountability at every level—whether a worker is handling welding fumes, exposed to silica and dust, or working in environments with volatile organic compounds (VOCs).
Legal and Regulatory Compliance
In many industries, including construction, mining, transport, and manufacturing, drug and alcohol testing is not just recommended—it’s required. Companies that fail to implement these programs risk non-compliance with occupational health and safety laws, which can result in severe penalties, loss of reputation, and legal liability.
Implementing robust testing is often complemented by regular noise assessments, dust monitoring, VOC monitoring, and vapor and fumes assessments. These environmental checks not only support regulatory compliance but also help in assessing the full spectrum of workplace exposures.
Preventing Long-Term Health Issues
Substance use can exacerbate the risks associated with other workplace hazards. For instance, a worker exposed to chemical vapors while under the influence may suffer more severe health effects. Combining mandatory testing with regular environmental noise assessments and hazardous substances assessments provides a multilayered approach to risk prevention.
This holistic approach is especially important in industries where exposure to welding fumes, silica dust, and hazardous chemicals is common. A strong testing policy ensures that compromised individuals are identified early and can be supported before long-term damage occurs.
Data-Driven Safety: Continuous Improvement
Modern workplace health is about data and trends. Regular occupational hygiene assessments—combined with health metrics from drug and alcohol testing—allow organisations to identify patterns, intervene early, and design better safety protocols. It’s not just about checking boxes; it’s about ongoing improvement.
This strategy is further enhanced by monitoring tools like:
Dust and noise monitoring to assess air and sound quality,
VOC and vapor monitoring for chemical exposure,
Silica and dust assessments to mitigate respiratory risks.
These services, delivered by Audiomet’s team of experienced professionals, contribute to a smarter, safer, and more sustainable workplace.
Final Thoughts: Responsibility Beyond Compliance
Making drug and alcohol testing mandatory sends a clear message: the safety of every worker matters. It’s a commitment to a workplace that values alertness, fitness for duty, and health above all. When integrated with comprehensive health services like audiometric testing, spirometry, flu vaccinations, and occupational hygiene assessments, it creates a strong safety net for all employees.
At Audiomet, we understand that workplace health isn't a one-size-fits-all solution. Our tailored services, ranging from fit testing and noise assessments to chemical and vapor monitoring, are designed to support your safety culture at every level.
Let’s create a safer future—one worker, one policy, one test at a time.
#hearing testing#occupational hygiene assessment#workplace lung function testing#aesthetic#alternative#Workplace Hearing Tests#Spirometry#Drug And Alcohol Test#Vaccination#Health Checks#Workplace Noise Assessment#Skin Check#Environmental Noise Assessment
0 notes
Text
The Growing Need for Mobile Medical Services in Alberton, South Africa
In recent years, the demand for mobile medical services has surged globally, and Alberton, South Africa, is no exception. As the healthcare landscape evolves, mobile medical solutions are becoming increasingly vital in providing accessible, efficient, and timely care. This article explores why mobile medical services are gaining prominence in Alberton and how 101 Mobile Medical Solutions is at the forefront of this transformation.
1. The Rise of Mobile Medical Services
Mobile medical services refer to healthcare that is delivered through mobile units, such as vans or buses equipped with medical facilities and personnel. These services have gained traction due to their ability to bring healthcare directly to individuals in need, eliminating barriers such as transportation and accessibility.
2. Meeting the Needs of Alberton’s Diverse Population
Alberton is a dynamic community with diverse needs. The area's growing population, combined with the increasing prevalence of chronic conditions, has highlighted the necessity for accessible medical care. Mobile medical services address these needs by offering:
Convenience: Mobile units can reach patients who might otherwise have difficulty accessing traditional healthcare facilities. This is especially important for those living in remote or deprived areas.
Efficiency: Mobile medical services can quickly respond to public health emergencies and provide on-site care, reducing wait times and improving health outcomes.
Comprehensive Care: From routine check-ups to specialized screenings, mobile medical units offer a range of services that cater to various health needs.
3. Benefits for Local Businesses and Industries
Alberton's industrial and business sectors benefit significantly from mobile medical services. For instance:
Employee Health Management: Mobile medical services can conduct on-site health screenings, occupational health assessments, and wellness programs, ensuring that employees receive timely care without leaving their workplace.
Compliance: Industries with stringent health and safety regulations can rely on mobile medical units to meet compliance requirements, such as drug testing, hearing tests, and physical examinations.
4. Enhancing Emergency Response
Mobile medical services play a crucial role in emergency response situations. Their ability to deploy quickly to disaster sites or accident scenes ensures that critical care is delivered promptly, potentially saving lives and improving recovery rates.

5. The Role of 101 Mobile Medical Solutions
At 101 Mobile Medical Solutions, we are committed to addressing the growing healthcare needs of Alberton. Our state-of-the-art mobile units are capable of providing the following facilities:
Mobile Occupational Health Services: Ensuring that local businesses comply with health and safety regulations.
Mobile X-ray Services: Offering diagnostic imaging services on-site.
Employee Medical Screening: Conducting comprehensive health checks for businesses.
Drug & Urine Testing Services: Providing essential testing for workplace safety and compliance.
Lung Function Testing and Vision Screening Services: Assessing and monitoring employees' health.
Audiometric Hearing Testing and Physical Examination Services: Ensuring overall employee well-being.
On-Site Clinic Management: Managing temporary clinics for large events or emergencies.
Employee Wellness Programs: Promoting health and wellness among staff.
6. Future Trends and Innovations
The future of mobile medical services in Alberton looks promising. Advances in telemedicine, portable diagnostic tools, and data management systems are set to enhance the capabilities of mobile units. These innovations will further improve the efficiency, accuracy, and reach of mobile medical services.
Conclusion
The growing need for mobile medical services in Alberton underscores the importance of adaptable, accessible healthcare solutions. With 101 Mobile Medical Solutions leading the charge, residents and businesses can benefit from comprehensive, on-site care that meets the evolving demands of the community. As mobile medical services continue to evolve, Alberton will remain at the forefront of this essential healthcare revolution.
FAQs
Q1: What types of services does 101 Mobile Medical Solutions offer?
A1: We offer a range of services, including mobile occupational health assessments, mobile X-ray services, employee medical screening, drug and urine testing, lung function testing, vision screening, audiometric hearing testing, and on-site clinic management.
Q2: How can businesses in Alberton benefit from mobile medical services?
A2: Businesses can benefit by ensuring compliance with health regulations, providing convenient access to health services for employees, and implementing wellness programs that enhance overall employee health and productivity.
Q3: Are mobile medical services available for emergency situations?
A3: Yes, mobile medical services are equipped to handle emergency situations, providing prompt care and support during crises, accidents, or public health emergencies.
Q4: How can I schedule a mobile medical service for my business or event?
A4: You can contact us directly through our website or phone to discuss your needs and schedule a service. Our team will work with you to ensure that we meet your specific requirements.
#Mobile Medical Services#Mobile Occupational Health Services#Mobile X-Ray Services#Employee Medical Screening#Drug & Urine Testing Service#Lung Function Testing#Vision Screening Services#Audiometric Hearing Testing#Physical Examination Service#On-Site Clinic Management#Employee Wellness Programs#Mining Health and Safety Solutions#On-Site Medical Testing#Employee Medical Examinations#Occupational Health Services#Workplace Health Programs#Medical Surveillance Programs#Audiometric Testing Services#Drug and Alcohol Testing Services#Workplace Safety Compliance#Employee Health Assessments#Mobile Healthcare Solutions#Mobile Clinic Services#Mobile Health Clinic#Health Surveillance Process#Medical Screening Programmes#Medical Monitoring Program#On-Site & Travel Clinic#Occupational Health Safety#Occupational Health and Safety Service Providers
0 notes
Text
What Is COPD?

Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition that makes breathing difficult. It primarily includes two main conditions: chronic bronchitis and emphysema. COPD is a leading cause of morbidity and mortality worldwide, often caused by long-term exposure to harmful irritants like cigarette smoke, air pollution, and occupational dust.
Causes of COPD
COPD develops due to long-term exposure to lung irritants. The most common causes include:
Smoking – The leading cause of COPD, responsible for nearly 90% of cases.
Air Pollution – Long-term exposure to pollutants in the environment or workplace.
Genetic Factors – A rare genetic disorder called Alpha-1 Antitrypsin Deficiency can cause COPD.
Respiratory Infections – Frequent lung infections during childhood can contribute to COPD development.
Passive Smoking – Being around smokers for extended periods can also contribute.
Exposure to Chemicals and Dust – People working in industries such as mining, farming, or construction are at higher risk.
Aging – The risk of COPD increases with age as lung function naturally declines.
Symptoms of COPD
The symptoms of COPD develop gradually and worsen over time. Common signs include:
Persistent cough with mucus
Shortness of breath, especially during physical activity
Wheezing and chest tightness
Frequent respiratory infections
Fatigue and unintended weight loss
Swelling in ankles, feet, or legs in severe cases
Cyanosis – A bluish tint to lips or fingernails due to low oxygen levels
Stages of COPD
COPD is classified into four stages based on the severity:
Mild (Stage 1) – Occasional cough with mucus, minimal impact on daily activities.
Moderate (Stage 2) – Increased breathlessness, especially during exertion.
Severe (Stage 3) – Frequent flare-ups, significant limitation in physical activities.
Very Severe (Stage 4) – Extreme shortness of breath, high risk of complications, and need for oxygen therapy.
How Is COPD Diagnosed?
COPD is diagnosed through the following tests:
Spirometry (Lung Function Test) – Measures lung capacity and airflow obstruction.
Chest X-ray or CT Scan – Helps detect lung damage.
Blood Tests – Checks oxygen and carbon dioxide levels.
Arterial Blood Gas Analysis – Determines how well your lungs exchange gases.
Six-minute Walk Test – Evaluates exercise tolerance and oxygen levels.
Treatment Options for COPD
While COPD has no cure, treatment can help manage symptoms and improve quality of life. Common treatment methods include:
Medications:
Bronchodilators – Help relax airway muscles.
Corticosteroids – Reduce inflammation in the lungs.
Antibiotics – Used during infections to prevent exacerbations.
Oxygen Therapy:
Helps patients with low blood oxygen levels.
Portable oxygen concentrators provide mobility and independence.
Pulmonary Rehabilitation:
Involves exercise training, nutrition advice, and breathing techniques.
Surgical Treatments:
Lung Volume Reduction Surgery (LVRS) – Removes damaged lung tissue to improve breathing.
Lung Transplant – For end-stage COPD patients.
Lifestyle Modifications:
Quitting smoking.
Avoiding exposure to pollutants.
Maintaining a balanced diet.
Regular physical activity.
Medical Equipment That Helps COPD Patients
Several medical devices help improve breathing and overall health for COPD patients:
Oxygen Concentrators: Provide a continuous supply of oxygen to patients with low blood oxygen levels.
BiPAP Machines – Used for non-invasive ventilation to assist with breathing during sleep.
Nebulizers – Deliver medication directly to the lungs for quick relief.
Pulse Oximeters – Help monitor oxygen levels in the blood at home.
Portable Oxygen Cylinders – Allow mobility for COPD patients who need supplemental oxygen.
Hospital Beds – Adjustable beds that help in comfortable positioning and better breathing.
Chest Physiotherapy Devices – Assist in clearing mucus from the lungs.
How Healthy Jeena Sikho Helps You

If you or a loved one is dealing with COPD, Healthy Jeena Sikho provides high-quality medical equipment to support respiratory health. We offer oxygen concentrators, BiPAP machines, nebulizers, hospital beds, and pulse oximeters for rent and sale. Our services are available across North India, ensuring access to essential medical care at an affordable cost. Visit www.healthyjeenasikho.com for more details.
Frequently Asked Questions (FAQs)
1. Can COPD be cured?
No, COPD is a chronic condition, but treatments can help manage symptoms and improve quality of life.
2. Is COPD only caused by smoking?
No, while smoking is the leading cause, air pollution, genetic factors, and occupational exposure also contribute.
3. How can I prevent COPD?
Avoid smoking, limit exposure to pollutants, maintain good respiratory hygiene, and follow a healthy lifestyle.
4. Can COPD patients exercise?
Yes, light to moderate exercises like walking and breathing exercises can help strengthen the lungs.
5. When should a COPD patient use oxygen therapy?
Oxygen therapy is recommended when blood oxygen levels drop significantly. A doctor can assess if it’s needed.
6. What foods should COPD patients eat?
COPD patients should eat protein-rich foods, fruits, vegetables, and avoid processed foods high in sodium.
7. How does a BiPAP machine help with COPD?
A BiPAP machine assists in breathing by providing positive air pressure, reducing shortness of breath.
8. Can COPD be reversed if diagnosed early?
No, but early intervention can slow progression and improve quality of life.
9. Does COPD affect sleep?
Yes, COPD can cause sleep disturbances due to breathing difficulties. Using a BiPAP or oxygen therapy can help.
10. Where can I rent or buy medical equipment for COPD in North India?
You can rent or buy oxygen concentrators, BiPAP machines, nebulizers, and more from Healthy Jeena Sikho. Visit www.healthyjeenasikho.com for details.
2 notes
·
View notes
Text
Breathe Easy With Spirometry Testing at Kearns Medical Centre
Wherever the workplace involves construction, chemicals, or dust, the implications for respiratory health differ with risk factors present. At Kearns Medical Centre we have the ability to complete spirometry testing to help assess lung function and pick up any respiratory issues sooner, before they develop into serious health problems.
Spirometry is a fast, easy, reliable, and non-invasive lung function assessment that measures how quickly and how much air an individual can breathe into and out of the lungs. Furthermore, it is critical to diagnosing similar conditions like asthma, COPD, and work related lung diseases.
Whether you are the employer responsible for the health of your employees, or the individual in a high-risk industry, regularly assessing each individual's lung function using spirometry should form the basis of maintaining long term respiratory health.
Protect your workers.
Compliable legaly.
Breathe Easy.
Book your appointment at Kearns Medical Centre, Unit 6, 70 Kearns Avenue, NSW.
📞 Call: 02 46046071
📩 Email: [email protected]

#Spirometry#WorkplaceHealth#LungFunctionTest#KearnsMedicalCentre#BreatheEasy#OccupationalHealth#LungHealth#NSWHealthcare
0 notes
Text
TB Awareness: Early Signs You Shouldn’t Ignore

Tuberculosis (TB) continues to be one of the most pressing health concerns in India. It affects millions every year—yet, many people ignore the early symptoms until the disease becomes severe and harder to treat.
As an experienced TB doctor in Varanasi, I often see patients who could have recovered faster and more easily if they had recognized the early warning signs of TB and sought medical attention in time.
In this blog, we’ll explore what TB is, its early symptoms, how it spreads, and why timely intervention from a qualified chest specialist is crucial.
What is Tuberculosis?

Tuberculosis is an infectious disease caused by the bacteria Mycobacterium tuberculosis. It typically affects the lungs but can also impact other parts of the body like the spine, brain, and kidneys. TB spreads through the air when an infected person coughs or sneezes, making it highly contagious, especially in crowded environments.
There are two main types of TB:
Latent TB: The bacteria remain inactive and cause no symptoms. However, it can become active in the future.
Active TB: The person shows symptoms and can transmit the disease to others.
Early Warning Signs of TB You Shouldn’t Ignore
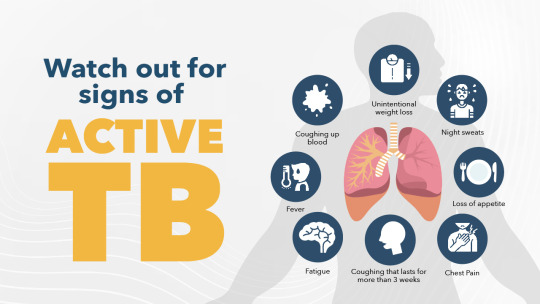
Being aware of the early signs of TB can make all the difference. If you experience any of the following symptoms, it's important to consult a TB doctor in Varanasi as soon as possible:
1. Persistent Cough
If you've had a cough that lasts more than two weeks, especially one that worsens or produces blood-tinged sputum, it may be a sign of pulmonary TB.
2. Unexplained Weight Loss
Losing weight without trying can be a sign of many diseases—including TB. It usually happens due to loss of appetite and the body’s response to the infection.
3. Fever and Night Sweats
Low-grade fevers that occur in the evenings, along with excessive night sweats, are classic signs of TB.
4. Chest Pain
Pain while breathing or coughing may indicate TB infection in the lungs. It can feel like tightness or pressure in the chest.
5. Fatigue
Prolonged tiredness and weakness are common in TB patients due to the body’s ongoing fight against the infection.
6. Shortness of Breath
In more advanced cases, TB can cause difficulty in breathing and reduced lung function.
Why You Should See a TB Doctor in Varanasi

In Varanasi, air quality, crowded living conditions, and delayed diagnosis contribute to rising TB cases. Seeking care from a chest specialist or TB doctor in Varanasi can lead to early detection, prompt treatment, and full recovery.
Dr. Vikas Jaiswal, at Lung + Plus Clinic, specializes in diagnosing and treating TB with advanced tools and patient-centric care. Early diagnosis is key to avoiding complications and preventing the spread of TB to others.
How is TB Diagnosed?
A TB doctor typically uses a combination of the following diagnostic tools:
Chest X-rays
Sputum test (to detect TB bacteria)
Tuberculin skin test (Mantoux test)
Blood tests (e.g., IGRA)
CT Scan, if required
Treatment and Care
TB treatment usually involves a 6-month course of antibiotics. Stopping treatment early or missing doses can lead to drug-resistant TB, which is much harder to treat.
At Lung + Plus Clinic, Dr. Vikas Jaiswal ensures complete monitoring and personalized treatment plans to manage both drug-sensitive and drug-resistant TB effectively.
Who Is at Risk?
People with weakened immune systems (like those with diabetes, HIV)
Elderly individuals
Smokers
Malnourished or underweight individuals
People living in close quarters (slums, hostels, jails)
Prevention Tips from a TB Doctor in Varanasi

Complete your vaccination – especially the BCG vaccine.
Avoid close contact with TB patients during their active phase.
Cover your mouth and nose when coughing or sneezing.
Ensure proper ventilation in your home or workplace.
Follow full course of treatment if diagnosed.
Visit the Best TB Doctor in Varanasi Today
If you’re experiencing any of the symptoms mentioned above, don’t delay. TB is curable—but only with timely diagnosis and proper treatment. As a trusted TB doctor in Varanasi, Dr. Vikas Jaiswal offers advanced care, accurate diagnosis, and full support throughout your treatment journey.
🏥 Book Your Consultation at Lung + Plus Clinic
📍 Lung + Plus Clinic – Varanasi 👨⚕️ Dr. Vikas Jaiswal, Chest Specialist, TB & Asthma Doctor
#TB doctor#TB doctor in varanasi#TB specialist in varanasi#pulmonologist in varanasi#TB Doctor near me
0 notes
Text
NP HEALTH PROBLEM Common Health Problem in Primary Care Nurse Practitioner Practice and Recommendations for Its Medical Management Nurses are the initial point of contact for the patients in many medical settings, and the nurse practitioners (NP) are the primary source for providing basic medical care such as physical examinations, diagnostic tests, providing counseling, and writing prescriptions. A large growth is being witnessed in nurse practitioners around the world due to the arising pandemics; however, they have been of great help in usual health cases since they function in institutes like clinics, hospitals, schools, and workplaces. As they are the first initial source of medical care for the patients, they are the first-hand problem solvers since they have to guide them according to their medical requirements. This paper analyzes a common health problem faced by NPs and would recommend medical management for it. In further sections, the problem would be deeply analyzed for evaluation and providing suggestions. Healthcare Problem Identified Asthma inhalers are a source of relief for asthma patients since they are breathed directly into the lungs for the prevention of symptoms of this disease. The correct usage of inhalers is crucial for controlling the disease, and various studies have shown that patients were unable to use the asthma device incorrectly, causing uncontrolled asthma. Repeated education is needed; this should include physical demonstrations of the inhalers, checking if the patient's technique is workable, correcting the technique, and rechecking for its effectivity. It was also observed that trained staff id required for better instructing of the patients, and for this purpose, nurse practitioners play an important part. Additionally, the choice of the inhaler should depend on the cost-effectiveness, whether the patient can afford it or not so that he should be able to use it correctly and enhance its compliance. A study indicated that metered-dose inhaler (MDI) had the most frequent number of errors; in terms of coordination, 45 percent, speed, and depth of inspiration 44 percent, no breath-hold after inhalation 46 percent (Sanchis, Gich & Pedersen, 2016). Even dry powder inhalers (DPI) were checked for errors too, which revealed that incorrect preparations accounted for 29 percent error, no full expiration before inhalation was 46 percent, and no holding of breath after inhalation was 37 percent. The general prevalence of the correct technique was 31 percent. These problems occurred soon after metered-dose inhalers were launched. However, efforts were made to educate the patients about their usage. Nonetheless, there were still some patients who could not understand the particular method. The instruction methods included regular training programs, printed materials, videos, and software. Nurse practitioners also helped in the first-hand instructions to make it easier for them, including both children and adults. Chronic obstructive pulmonary disease (COPD) together with asthma are the two of the highly ranked diseases in the world that are leading causes of deaths of around 339 million people globally (Bhushan et al., 2018). It accounts for up to 1000 people dying each day, including both children and adults. COPD is the fourth leading cause of death and can go up in the rank in third place by the year 2020. Various studies have indicated that improper use of inhalers has led to an increase in asthma and COPD. Therefore hospital visits have surged as well. As it was noted that poor inhalation technique was the main reason for increased clinical visits, this was also because patients missed at least one serious step of the technique and had low literacy levels. The poor technique has been linked to factors like age, sex, educational levels, and emotive problems (Milanese et al., 2019). Younger asthmatic patients have reported more mishandling of the device, which resulted in poor disease control. In older patients, COPD is more common but requires prescribed medication, including inhalers. High rates of poor device handling were also reported among these patients, inducing severe exacerbations. In epidemiological terms, children have been more prone to this disease as compared to adults. Still, it would be difficult to reside upon these results since there have been different definitions of age for asthma status around the world (Dharmage, Perret & Custovic, 2019). For older people, the co-morbidity rates are hard to define since asthma symptoms could be related to breathlessness or COPD, inciting to heart failure. Environmental exposure at an early age, such as those among children, is the primary cause of early asthma. In utero parental smoking can provoke asthma in young children; studies have revealed that female smokers are more likely to have asthma as compared to non-smokers, but this data might not apply to men. Outdoor air pollutants are globally manipulating the quality of air inhaled by children and adults; thus, impacting heavily on asthmatic patients. Indoor allergens also should not be ignored since they have intense effects on asthmatic subjects. Occupational exposures are greatly affecting asthma patients since there are now two categories: work aggravated asthma (WEA) and occupational asthma (OA). Lifestyle factors, such as westernization and eating habits, have a command over asthma severity as well. In pathophysiological terms, the rise in asthmatic cases is due to extra clean air conditions, especially in western culture, since it would expose them less to the environment and increase the infections. When they interact with the outdoor air, the chances of getting air pollutants into the lungs and upsetting the immune systems rise. Bronchiolar inflammation is bound to happen to produce less resistance against asthma. The inflammation hurts trachea and bronchi, accelerating an increase in mucus production and a decrease in mucus clearance. Practice Guideline The clinical practice guideline addresses the identified health problem, which is poor inhaler education among asthma patients. The guidelines focus on the pivotal diagnosis stage and the asthma management for devising bronchodilator therapies and keeping track of periodic measurements of lung functioning before and after the therapy (Amerigroup Real Solutions, 2016). This practice guideline is based on current evidence that is available within the last five years. It was published in the year 2016 in line with US data. The strength of this evidence is the detailed information provided about the aesthetic patients and precautions for them. Also, there are follow up plans once the asthma action design has been put to effect. The practice guideline adequately directs the health care provider in the management of asthmatic interventions. There is a thorough description of the contributing factors for this disease, what triggers the patients and what methods should be used to avoid them, assessment and monitoring techniques are guided, pharmacotherapy is mentioned for better identification of individual's needs, and patient education plan, which is the basis of the problem identified in this paper. The clinical guidelines clearly state management procedures for the health care provider that includes reducing impairment and maintain normal lung function. This is guided by maintaining normal activity levels, and this is only possible when risks are reduced. The associated risks could be diminished by avoiding exacerbations, lessening the requirement of emergency or in-patient care, stopping failure of lung function, for children preventing shrinkage of lung growth, and lowering negative outcomes of the therapy. The performance of the clinical guidelines in the management of athematic patients is evident since combination and assessment of clinical therapies under the guidelines have improved the accuracy of asthma severity assessment (Dima, De Bruin & Ganse, 2016). The link between the provision of medical care services and the recipients is critical. Since this link is provided by the nurse practitioners who are the initial contacts for the patients, they play a vital part in assessing asthma severity. Practice guidelines provide a meaningful direction to the practitioners for reviewing asthma severity and provide appropriate pieces of advice for better therapies, including inhaler use. The health care services can impact asthma controlling in two parts: stirring asthma management process directly through medical care and altering caregiver and patient behaviors through behavioral care. It is well known that the performance of these two parts, medical and behavioral care, can be influenced by the clinical guidelines so that health care professionals, such as nurse practitioners, directly mold the patients' control in the disease. The control can be brought if clinical guidelines shape the modifiable factors of health care providers, such as medical knowledge, communication skills, training methods, and treatment techniques. All the recommendations of these related sections are presented in the practice guidelines which nurse practitioners can make use of for better patient education for asthma control. However, there are non-modifiable factors, too, like the experience of the nurse practitioner, his gender, and age. Educational interventions have been reported mitigating the outcomes of asthma in children and adult patients with an average follow up time of five months (Press et al., 2020). In the short term, the disease was controlled due to better educational techniques, either through physical demonstrations or sometimes virtual (V-TTG: virtual teach to goal) as well. Long term follow-ups were mainly held for those who consistently showed manhandling and poor disease control even after instructions being given. A guideline-recommended inhaler education was provided to the subjects through cost-effective virtual training. Inhaler techniques were examined using a 12-step checklist that was also in practice in the previous intervention studies. The effectuality of patient management can be checked by numerous designs, including health technology assessment, which would help in examining what technology and thereupatic methods are best in delivering positive results for asthma patients. Randomized methods can be useful as well, which include random allocation of probers for assessing the efficacy of installed methods in the clinical setting based on the clinical guidelines. Virtual monitoring that includes video monitoring through surveillance cameras within the clinical premises would help know whether patient management is done productively. For the past ten years, mobile phone technology has been very valuable. In the future, it can create wonders for asthma patients in impactful management and monitoring of adherence to inhaler methods (Morton et al., 2020). Nurse practitioners can assess through mobile monitored video apps whether the patients are adhering to underlying steps of inhaler use and what step they are missing, which is responsible for uncontrolled asthma. Web-based programs or e-health can help assess the patients and their adherence to self-management policies. It provides a flexible forum for patients to come forward and discuss their issues, and this can be achieved via education, empowerment, and active participation of both the nurse practitioners and the patients. Analysis Taking into consideration the future health care needs of patients with poor inhaler education, the pivotal role of nurse practitioners could not be ignored. Training should be given to the nurses for correct techniques, which later should be transferred to the patients for overcoming symptoms of asthma. It is not wrong to assert that successful nurse education would reap fruitful results in disabling consequences for asthma patients. Training can be provided hospital-wide through one-on-one education methods, classes through the web, or unit-based education (Scullion, 2018). Placebo devices could be used for giving demonstrations to the nurse practitioners so that they get aware of the using techniques. Afterward, they could transfer this knowledge accurately to the patients. These devices would not be useful for nurse practitioners only but also for the patients so that they get familiar with their use beforehand. Nurse education should also include getting aware of all the new medications in the market and what medicines are obsolete so that when an asthma patient comes in for urgent help, he could be prescribed with up-to-date medications. In the future, there is a demand to check whether the inhalator's use and their methods are properly utilized by the asthma patients to control the disease. For this purpose, there are many tools to aid patients in precise inhaler handling. In-check DIAL allows the health care specialists to train patients about the inhalers as it assesses the peak inspiratory flow. There is another device called Trainhaler used for training patients on the same grounds; though, it has an additional feature that its mouth-piece, called Flo-Tone, can be changed for each individual as it is convenient for multi-patient usage. The future health care needs of asthma patients also require the nurse practitioners to be aware of the religious or cultural concerns while using an inhaler. This means some populations might not be able to use inhalers due to some extent of alcohol mixed with the medication. Moreover, some cultural beliefs hinder them from using inhalers as they take it as impolite or a type of oral drug. Some studies have shown that mothers of asthmatic children have been apprehensive of the use of drugs or inhalers for their children since either they were not completely comfortable with the medical system or they were unsure of the chemical formulation of the inhalers. With the emergence and increased need for e-health, asthma control requires smart inhalers, which would allow the patients to connect with the help of Bluetooth connectivity and collect data by a health app or website. This could be accessed later by the patient (self-management), his nurse practitioner, or specific asthma doctor to whom he regularly visits. Furthermore, these inhalers allow the patient to set reminders for taking medications, and enablement of efficiency can be monitored as well. Technology should be considered seriously regarding asthma control since it helps in making healthcare more tailored, reachable, and acceptable to patients. Changes in global demographics are bringing changes to the US as well that would directly affect the clinical practice guidelines and healthcare within the country. For instance, Millennials (people with ages 23 to 28) would increase in number as compared to Baby Boomers (ages 55 to 73). Still, there is a greater population, Generation Z, maturing to adulthood (Cilluffo & Cohn, 2019). Millennials are more educated, leading to the fact that high literacy would bring high education about inhaler use and fewer mistakes, resulting in lower asthma cases. Generation Z is arguably the most ethnically diverse and most educated generation by far, hence, assuming to be more informative about inhaler use. Forty-eight percent of Generation Z people are racial or ethnic minorities and are expected to be the largest US racial group casting votes. This huge category of voters would help in framing the healthcare system of the country, directly influencing the clinical guidelines. Changes in family patterns are highly evident; the unmarried parents living with a child has increased from 7 percent to 25 percent. US children living with unmarried parents are now 32 percent, which was 13 percent back in 1968. Stay-at-home parents represent 18 percent of the US population. These facts show that children who would be cared for and monitored by their parents regarding asthma control would be fashioned accordingly. The clinical guidelines have to be designed accordingly so that guidelines include the role of parents in controlling asthma in young ones. The immigrants in the US have been increasing rapidly but remain low as compared to other countries. This means that the inclusion of people from a variety of cultures and religious beliefs would be entering the US, thus forcing the country to revise its clinical guidelines. Household income is highest in recent years in the US, and this is more apparent in some racial groups. This could pattern the use of inhalers since rich people would be more likely to opt for more advanced and expensive medications for asthma control, thus aiming at lower disease prevalence. Clinical practitioners can guide these people regarding the most suitable medications that they can afford and adhere to. Changes in healthcare policies also greatly imply how asthma patients take medications and what health care insurance plans they have to utilize. For case in point, with the new Affordable Care Act (ACA), the protection for asthma people still exists, but they have to look for medicines that are listed on that plan; only those supplements would be free of cost. This means if one medication suits them but is not listed in free coverage, then asthma patients would have to buy it from the appointed shop. If clinical guidelines were to be revised, the changes could be based on the above-mentioned shifting world demographics, which would consequently influence the US health care trends. These could be used as evidence for revising the practice guidelines. Three basic changing drifts- an aging population, increased ethnicity, and urbanization- would outline the way nurse practitioners would have to intervene for better provision of support to asthma patients for inhaler education. If practice guidelines were to be changed based on the aging population, then it should be kept in mind that prolonged ages would lead to asthma care over several years. Besides integrating traditional practice guidelines about inhaler education, the use of smart apps would be beneficial. The clinical guidelines should include education about such apps, for all age groups encompassing Baby Boomers, Millennials, and Generation Z. Clinical guidelines should be revised for increased ethnicity since immigrants have largely grown in numbers within the US, and people from different cultures are entering the states. Practice guidelines should cater to the religious and cultural aspects of ethnic asthmatic patients so that inhaler use should take into consideration whether or not it contains alcohol or is deemed inappropriate for oral use. Additionally, if Hispanic people are coming into a region, they might feel comfortable talking to a Hispanic doctor. So, hiring of culturally competent practitioners should be considered for inhaler education of asthmatic patients; their recruitment in the healthcare workforce and training is a grave need of current times. Clinical guidelines should be revised for rising urbanization since people's lifestyles and eating habits would be changed. Highly educated individuals would be increasingly aware of inhaler use; hence, asthma could be controlled. Nevertheless, if they are living in urban areas, there is more likeliness that the areas would have more vehicles and more air pollution; therefore, triggering of asthma is inevitable. For such patients, clinical guidelines should include self-management techniques such as knowing one's trigger points, knowing the medications and dosage, being familiar with the inhaler device, and steps involved in inhaler use. Individuals living in urban regions would be more alert to the technological methods for checking their asthma symptoms and should be in constant contact with their nurse practitioner with the monitoring apps. Read the full article
0 notes
Text
What Are Pulmonary Function Tests?
Pulmonary Function Tests (PFTs) check how well your lungs work. These tests help find and monitor lung problems like asthma and COPD.
What Are Pulmonary Function Tests?
PFTs are simple, non-invasive tests that measure lung capacity, airflow, and how well oxygen moves into your blood. They help doctors diagnose breathing issues.
Types of Pulmonary Function Tests
Spirometry – Checks how much air you can breathe in and out.
Lung Volume Test – Measures the total amount of air your lungs can hold.
Diffusion Capacity Test – Tests how well your lungs pass oxygen to your blood.
Who Needs a PFT?
People with a long-lasting cough, shortness of breath, or wheezing.
Those with lung conditions like asthma or COPD.
Patients needing lung checks before surgery or workplace screenings.
How to Prepare for a PFT?
Do not smoke or eat a heavy meal before the test.
Wear loose, comfortable clothes.
Follow any instructions from your doctor.
Why Are These Tests Important?
Accurate Diagnosis – Helps find lung problems early.
Better Treatment Plans – Helps doctors track and manage conditions.
Improved Health Monitoring – Useful for people with long-term lung diseases.
Pulmonary Function Tests are important for checking lung health and making sure you get the right treatment when needed.
0 notes
Text
Childhood to Adult Asthma Care: Holistic Treatment at MagnAid Hospitals
Asthma is a chronic respiratory condition that affects millions of people worldwide. It impacts the airways, causing inflammation and narrowing, making it difficult to breathe. At MagnAid Hospitals, we understand how disruptive asthma can be to everyday life, and our specialized pulmonology team is committed to offering comprehensive care for asthma patients of all ages.
What is Asthma? Asthma is characterized by recurrent episodes of wheezing, coughing, chest tightness, and shortness of breath. These symptoms can vary in severity and frequency. Triggers for asthma attacks include allergens (such as pollen, dust mites, and pet dander), pollution, cold air, respiratory infections, physical activity, and even emotional stress. Understanding what causes your asthma symptoms is key to effective management.
Types of Asthma:
Allergic Asthma: Triggered by allergens like pollen, dust, and mold.
Non-Allergic Asthma: Triggered by environmental factors such as smoke, pollution, and cold air.
Exercise-Induced Bronchoconstriction (EIB): Symptoms occur during or after exercise.
Occupational Asthma: Caused by workplace irritants like chemicals or dust.
Childhood Asthma: A common chronic condition in children that requires careful management.
Why Choose MagnAid for Asthma Care?
Accurate Diagnosis: We utilize advanced diagnostic techniques such as spirometry, peak flow measurements, allergy testing, and imaging studies to ensure an accurate and thorough assessment.
Customized Treatment Plans: Every asthma patient is unique. We create individualized plans combining medications, inhaler techniques, lifestyle changes, and avoidance of triggers.
Multidisciplinary Approach: Our pulmonologists collaborate with allergy specialists, dietitians, and respiratory therapists to offer holistic care.
Asthma Education & Counseling: We prioritize educating patients and families on asthma action plans, emergency measures, and long-term disease control.
24/7 Emergency Response: Our hospital is equipped to handle severe asthma attacks with quick and effective emergency care.
Treatment Options Available at MagnAid Hospitals:
Inhaled corticosteroids
Long-acting beta agonists (LABA)
Leukotriene modifiers
Combination inhalers
Biologic therapies for severe asthma
Allergy immunotherapy (in selected cases)
Pulmonary rehabilitation programs
Asthma in Children and Special Care: Children require extra attention and monitoring. At MagnAid Hospitals, we offer pediatric asthma clinics where children receive age-appropriate education and treatments to help them live active and fulfilling lives.
Living with Asthma: Managing asthma is not just about medications. It’s also about adopting healthy lifestyle habits, identifying and avoiding triggers, maintaining good indoor air quality, exercising with caution, and regularly monitoring lung function.
Signs That You Should See a Pulmonologist Immediately:
Frequent coughing, especially at night or early morning
Shortness of breath during mild activity or while resting
Chest tightness or discomfort
Increased use of quick-relief inhalers
Difficulty speaking during an attack
Symptoms that interfere with daily life or sleep
Pulmonary Rehabilitation Programs at MagnAid: For patients with moderate to severe asthma, we offer pulmonary rehabilitation programs designed to enhance lung function, build stamina, and improve quality of life. These programs include breathing exercises, physical training, nutritional counseling, and psychological support.
Our Commitment: At MagnAid Hospitals, we believe that with the right support and medical care, asthma can be effectively controlled. Our goal is to empower patients with the tools and knowledge needed to take charge of their respiratory health.
Book Your Appointment Today Take control of your breathing and experience a better quality of life. Let the specialists at MagnAid Hospitals help you manage your asthma with care and expertise.
MagnAid Hospitals - Every Breath Matters. Every Life Matters.
1 note
·
View note
Text
Building a Healthier Workforce: The Real Impact of Prioritizing Workplace Health and Safety
In the modern workplace, the concept of workplace health and safety has evolved far beyond compliance checklists and first aid kits. Today, it’s about fostering environments where employees feel protected, valued, and empowered to do their best work—because a healthy team is the foundation of any successful business.
At Audiomet, we understand the unique challenges Australian employers face in managing health risks, staying compliant with regulations, and supporting their workforce’s overall wellbeing. As a national workplace health provider, we offer a comprehensive range of solutions designed to simplify and strengthen your health and safety efforts—from onsite workplace screening to mobile health services and occupational hygiene assessments.
Let’s explore why taking health and safety seriously pays off—and how Audiomet can help.

More Than a Duty: The Value of Occupational Health
Workplace health isn’t just about avoiding fines or insurance claims. It’s about creating a thriving work culture.
With the rise in remote work, hybrid models, and high-demand industries, occupational health has become more essential than ever. By addressing factors like fatigue, stress, exposure to hazards, and chronic illnesses early, businesses can prevent disruptions, reduce absenteeism, and retain top talent.
At Audiomet, our services support a full spectrum of needs, including:
Occupational hygiene and occupational hygiene assessment
Workplace health screening and employee health checks
Environmental consulting for safe and sustainable workspaces
Healthcare consulting for strategic health planning
Whether you’re running a manufacturing plant or managing a corporate office, we help tailor solutions that meet your workforce's specific risks and needs.
Mobile Health Screening: Workplace Wellness That Comes to You
We know how hard it can be to coordinate health services across large teams and multiple locations. That’s why Audiomet offers mobile health screening services—fully equipped units that travel to your worksite, minimizing disruption while maximizing coverage.
Our mobile health screening unit is ideal for delivering:
Hearing testing, including workplace audiometric testing and OHS audiometric testing
Workplace spirometry and lung function testing
Employee drug and alcohol testing
Workplace skin checks and flu vaccinations
Mobile services make it easier for employees to participate in preventative health screening, boosting both compliance and engagement. When health checks are convenient and accessible, participation skyrockets—and so does your team’s trust in your commitment to their wellbeing.
Sound Matters: Hearing Protection and Prevention
Noise-induced hearing loss prevention is one of the most overlooked aspects of workplace safety—yet it can have a profound impact on quality of life and productivity.
Our team specializes in workplace hearing tests and employees audiometric testing, helping identify early signs of hearing damage. Regular assessments allow you to intervene before hearing loss becomes permanent, and demonstrate your compliance with workplace safety regulations.
We also provide occupational noise assessments, industrial noise assessments, and workplace noise management solutions to keep your environment within safe decibel ranges. Whether you're in heavy industry, manufacturing, or logistics, we’ll help you build a noise strategy that’s proactive and protective.
Workplace Spirometry & Lung Function Testing: Breathing Easy on the Job
For employees exposed to dust, fumes, or other airborne irritants, lung health monitoring is essential. That’s why we offer complete workplace spirometry testing, including:
Occupational health spirometry testing
Workplace lung function testing
Support for occupational lung disease prevention
Regular testing ensures early detection of respiratory conditions and helps track the effectiveness of workplace controls like ventilation and PPE. Our services are available both onsite and through our mobile health screening company, making it easier than ever to safeguard your team's respiratory health.

Drug & Alcohol Testing: Promoting a Safe and Sober Workplace
Substance misuse can put entire teams at risk—especially in high-responsibility roles. Our discreet and professional drug and alcohol screening services support safer workplaces with:
Employee drug and alcohol testing
Workplace drug and alcohol test programs
Full workplace drug and alcohol test Melbourne coverage
We help businesses create clear, compassionate policies and conduct regular screenings to promote accountability, safety, and support for employees who may be struggling.
Vaccination & Flu Clinics: Boosting Immunity, Reducing Downtime
Keeping your team protected from seasonal illnesses is an easy, cost-effective way to reduce sick leave and maintain productivity. Audiomet offers:
Employee vaccinations and workplace vaccinations
Onsite flu vaccination clinics
Coverage for employee vaccinations Melbourne-wide
Vaccination programs are a simple but powerful investment in your workforce’s wellbeing. They show you care—and they make it easier for employees to stay healthy during critical times of the year.
Skin Checks & Early Detection
Skin cancer is a leading concern in Australia. Our workplace skin checks, including onsite skin checks and employee skin checks Melbourne, can help catch suspicious lesions early. It’s just another way we help your business protect what matters most: your people.
Partner with Audiomet: Melbourne’s Leading OHS Provider
At Audiomet, we’ve spent years helping businesses across Australia—from small local teams to large industrial operations—stay compliant, healthy, and future-ready. As a trusted occupational health & safety provider, we offer holistic, human-centered solutions that support both compliance and culture.
So whether you need an OHS consultant in Melbourne, a corporate health check, or help with environmental noise assessments, we’ve got you covered.
Let’s Build a Healthier Future Together
Workplace health and safety isn’t just about rules—it’s about people. When you invest in their wellbeing, the benefits ripple through your whole organization: better morale, fewer absences, higher retention, and a stronger brand.
🔗 Visit audiomet.com.au to explore our services, or contact us to create a custom plan that meets your team’s needs.
#Workplace health and safety#occupational health#occupational hygiene#Environmental Consulting#Healthcare Consulting#ohs occupational health and safety#Workplace health screening#occupational hygiene assessment#workplace health and safety Melbourne#OHS Consultants Melbourne#Preventative Health Screening#Onsite workplace screening#National workplace health provider#Workplace safety regulations compliance#mobile health screening Services#mobile health screening unit#mobile health screening company#occupational hygiene service provider#occupational Health & Safety provider#hearing testing#Noise-induced hearing loss prevention#Workplace Audiometric Testing#Workplace hearing tests#Employees Audiometric Testing#OHS Audiometric Testing#Workplace hearing tests Melbourne#Workplace Spirometry#workplace Lung function testing#Occupational lung disease prevention#workplace spirometry testing
0 notes
Text
The Ultimate Guide to Understanding Mobile Medical Services
In today's fast-paced world, convenience and accessibility are paramount, especially when it comes to healthcare. Mobile medical services are revolutionizing the way we approach healthcare delivery by bringing essential medical services directly to individuals, whether at home, in the workplace, or remote areas. This comprehensive guide will delve into what mobile medical services entail, their benefits, and how 101 Mobile Medical Solutions can enhance your healthcare experience.
What Are Mobile Medical Services?
Mobile medical services refer to healthcare services that are provided in a mobile setting, such as a van, truck, or portable unit. These services can include a range of medical treatments, diagnostics, and preventive care, all delivered outside of a traditional hospital or clinic environment.
Types of Mobile Medical Services
1. Mobile Occupational Health Services
Mobile occupational health services are designed to cater to the healthcare needs of employees in various industries. These services often include health screenings, vaccinations, and drug testing, all administered on-site at the workplace.
2. Mobile X-Ray Services
Mobile X-ray services bring radiographic imaging directly to patients. This service is especially useful for individuals who have difficulty traveling to a clinic or hospital for imaging studies.
3. Mobile Clinics
Mobile clinics are equipped with medical professionals and a range of medical equipment to offer primary care, urgent care, and preventive services in a mobile setting. These clinics are often used in underserved or rural areas where access to healthcare is limited.
4. Employee Wellness Programs
Mobile medical services often include wellness programs designed to promote health and prevent illness among employees. These programs can feature health assessments, fitness coaching, and nutritional advice.
Benefits of Mobile Medical Services
1. Convenience
One of the most significant advantages of mobile medical services is the convenience they offer. Patients can receive care without having to travel to a medical facility, which is particularly beneficial for those with mobility issues or busy schedules.
2. Accessibility
Mobile medical services improve healthcare accessibility, especially in remote or undeserved areas. By bringing medical services to these locations, healthcare providers can ensure that more people receive the care they need.
3. Cost-Effectiveness
In many cases, mobile medical services can be more cost-effective than traditional healthcare settings. By reducing the need for physical space and overhead costs associated with stationary clinics, mobile services can offer lower prices for patients.
4. Timely Care
Mobile medical services can provide timely care in emergencies or urgent situations. The ability to deliver medical services on-site can help prevent delays and reduce the risk of complications.

How 101 Mobile Medical Solutions Can Help
Comprehensive Mobile Medical Services
101 Mobile Medical Solutions offers a range of mobile medical services designed to meet diverse healthcare needs. Our services include:
Mobile X-ray and Diagnostic Imaging: State-of-the-art imaging equipment for accurate diagnostics delivered directly to your location.
On-Site Occupational Health Services: Health screenings, vaccinations, and drug testing tailored to the needs of your workforce.
Employee Wellness Programs: Comprehensive programs aimed at enhancing the overall health and well-being of employees.
Mobile Clinics: Fully equipped mobile units providing primary and urgent care in various locations.
Why Choose 101 Mobile Medical Solutions?
1. Experienced Professionals
Our team comprises highly skilled medical professionals with extensive experience in mobile healthcare. We ensure that all services are provided with the highest standards of care.
2. State-of-the-Art Equipment
We use advanced medical equipment and technology to deliver accurate and effective healthcare services. Our mobile units are equipped with the latest tools to ensure quality care.
3. Flexible Scheduling
We understand the importance of flexibility in healthcare. Our services are designed to fit your schedule, whether you need routine check-ups or urgent care.
4. Comprehensive Care
101 Mobile Medical Solutions offers a full spectrum of mobile medical services to address various healthcare needs, from preventive services to urgent medical care.
FAQs
Q: What types of mobile medical services are available?
A: Mobile medical services can include occupational health screenings, X-ray and diagnostic imaging, primary and urgent care through mobile clinics, and employee wellness programs.
Q: How do mobile medical services benefit businesses?
A: Mobile medical services benefit businesses by providing on-site healthcare, reducing employee downtime, and ensuring a healthier workforce. Services like health screenings and vaccinations can be delivered directly at the workplace.
Q: Does insurance cover mobile medical services?
A: Coverage for mobile medical services can vary depending on the insurance provider and plan. It's advisable to check with your insurance provider to understand what services are covered.
Q: How do I schedule a mobile medical service?
A: To schedule a mobile medical service with 101 Mobile Medical Solutions, contact us through our website or call our customer service team. We will assist you in setting up an appointment that fits your needs.
Q: Can mobile medical services be used in emergencies?
A: Yes, mobile medical services can be used in emergencies. Our mobile units are equipped to handle urgent medical situations and provide timely care.
Conclusion
Mobile medical services are transforming healthcare delivery by providing convenient, accessible, and cost-effective care. With 101 Mobile Medical Solutions, you can experience the benefits of high-quality mobile medical services tailored to meet your specific needs. Whether you're a business seeking on-site health solutions or an individual needing accessible care, our services are designed to enhance your healthcare experience. Contact us today to learn more about how we can help you stay healthy.
#Mobile Medical Services#Mobile Occupational Health Services#Mobile X-Ray Services#Employee Medical Screening#Drug & Urine Testing Service#Lung Function Testing#Vision Screening Services#Audiometric Hearing Testing#Physical Examination Service#On-Site Clinic Management#Employee Wellness Programs#Mining Health and Safety Solutions#On-Site Medical Testing#Employee Medical Examinations#Occupational Health Services#Workplace Health Programs#Medical Surveillance Programs#Audiometric Testing Services#Drug and Alcohol Testing Services#Workplace Safety Compliance#Employee Health Assessments#Mobile Healthcare Solutions#Mobile Clinic Services#Mobile Health Clinic#Health Surveillance Process#Medical Screening Programmes#Medical Monitoring Program#On-Site & Travel Clinic#Occupational Health Safety#Occupational Health and Safety Service Providers
0 notes
Text
Book a Comprehensive Lung & Respiratory Checkup Online in Chennai Today
Lung health is crucial for overall well-being, yet many people overlook regular checkups until serious symptoms arise. With rising air pollution, smoking habits, and respiratory infections, early detection of lung diseases is more important than ever. Booking a lung & respiratory checkup online in Chennai with Asto Labs provides a convenient and effective way to monitor your respiratory health without the hassle of hospital visits.

Importance of Lung & Respiratory Checkups
Lung diseases such as asthma, chronic obstructive pulmonary disease (COPD), lung infections, and even lung cancer can develop silently. A routine Lung Health Checkup in Chennai can help detect potential issues early, allowing for timely intervention and treatment. Some of the key benefits include:
Better Treatment Outcomes – Early diagnosis leads to effective management.
Monitoring Existing Conditions – Helps track asthma, COPD, or other lung diseases.
Improved Lung Function – Ensures optimal oxygen supply to the body.
What Does a Lung & Respiratory Checkup Include?
A lung & respiratory checkup in Chennai typically involves a set of diagnostic tests designed to assess lung function and detect abnormalities. At Asto Labs, we offer a comprehensive screening package that includes:
Chest X-Ray – Detects infections, lung damage, or fluid buildup.
Spirometry Test – Checks for breathing disorders like asthma and COPD.
Blood Tests – Analyzes oxygen levels and detects infections.
CT Scan (if needed) – Provides detailed images of the lungs for deeper analysis.
With lungs check up at home in Chennai, you can get tested without stepping out of your house. Asto Labs ensures a hassle-free experience by providing expert sample collection services at your doorstep.
Why Choose an Online Lung & Respiratory Checkup in Chennai?
Booking a lungs check up online in Chennai with Asto Labs offers several advantages, including:
Convenience – No need to visit a hospital; book tests from home.
Home Sample Collection – Our experts collect samples from your doorstep.
Faster Results – Receive reports digitally for quick diagnosis.
Expert Consultation – Online doctor consultations for further guidance.
At Asto Labs, we provide reliable and accurate lung & respiratory checkups in Chennai with advanced diagnostic technology and expert medical support. Whether you need a lung health checkup in Chennai or a lungs check up at home in Chennai, we ensure precision and care in every test.
Who Should Get a Lung & Respiratory Checkup?
A lung checkup in Chennai is recommended for individuals with:
Persistent cough, shortness of breath, or wheezing
Smoking history (current or past)
Exposure to air pollution or workplace toxins
Family history of lung disease
Pre-existing respiratory conditions like asthma or COPD
Conclusion:
Taking care of your lung health has never been easier. With Asto Labs, you can book a lung & respiratory checkup online in Chennai in just a few clicks. Our expert team ensures accurate diagnosis and timely reports to help you stay on top of your health.
Whether you prefer a Lungs Check Up Online in Chennai or a lungs check up at home in Chennai, we provide flexible options to suit your needs. Book your lung health checkup in Chennai today and breathe easy with early detection!
0 notes
Text
The Importance of Pre-Employment Health Checkups: Ensuring a Healthy Workforce
Introduction
A company’s success depends not only on skills and experience but also on the health and well-being of its employees. A Pre Employment Health Checkup is a crucial step in the hiring process, ensuring that potential employees are medically fit for the job. Many organizations now prioritize health screenings to minimize workplace health risks, enhance productivity, and reduce absenteeism. Preethi Hospitals, Madurai, offers comprehensive pre-employment health checkup packages tailored to various industries, ensuring a healthier workforce.
What Is a Pre-Employment Health Checkup?
A Pre-Employment Health Checkup is a medical screening process conducted before hiring a candidate. It assesses overall health conditions, detects underlying medical issues, and determines whether the individual is fit for the job role. Different industries may require specific tests based on the nature of work, exposure to hazards, or physical demands.
Why Is a Pre-Employment Health Checkup Necessary?
Employers and employees benefit significantly from pre-employment health assessments. Here’s why it is essential:
Ensures Workplace Safety – Certain jobs, especially in industries like construction, manufacturing, and healthcare, demand high physical and mental fitness. Health screenings help prevent workplace accidents by ensuring employees are fit for their roles.
Reduces Healthcare Costs – Identifying medical conditions early can help manage them effectively, reducing long-term medical expenses for both employees and employers.
Enhances Productivity – Healthy employees perform better, leading to increased efficiency and a positive work environment.
Prevents Spread of Infectious Diseases – Regular health screenings help detect contagious diseases, ensuring a safer workplace.
Compliance with Industry Regulations – Some industries have mandatory health checkup requirements that organizations must adhere to for legal compliance.
Key Components of a Pre-Employment Health Checkup
A standard pre-employment health checkup includes multiple tests based on job requirements. Some of the most common tests include:
General Physical Examination – Assessing vital signs, BMI, and overall health.
Blood Tests – Checking for diabetes, cholesterol levels, and liver/kidney function.
Vision and Hearing Tests – Ensuring candidates meet necessary visual and auditory standards.
Chest X-Ray – Detecting any lung infections or respiratory issues.
ECG (Electrocardiogram) – Evaluating heart health, especially for roles involving physical exertion.
Urine Analysis – Screening for infections and metabolic disorders.
Drug and Alcohol Testing – Required in industries where safety is a priority, such as transportation and construction.
Industries That Require Pre-Employment Health Checkups
Certain industries mandate pre-employment medical screenings due to the nature of work. These include:
Healthcare – Ensuring doctors, nurses, and medical staff are free from infectious diseases.
Manufacturing & Construction – Verifying physical endurance and safety compliance.
IT & Corporate Sector – Identifying lifestyle-related health risks like obesity, diabetes, or stress disorders.
Aviation & Transportation – Ensuring pilots, drivers, and crew members are fit to operate machinery safely.
Hospitality Industry – Preventing the spread of infections in hotels and restaurants.
How Preethi Hospitals, Madurai, Ensures a Reliable Health Screening Process
Preethi Hospitals, Madurai, provides a comprehensive Pre-Employment Health Checkup package designed to meet industry-specific requirements. With state-of-the-art diagnostic facilities, experienced healthcare professionals, and a streamlined process, Preethi Hospitals ensures accurate and timely medical assessments.
Steps in a Pre-Employment Health Checkup at Preethi Hospitals, Madurai
Appointment Scheduling – Candidates can book an appointment online or visit the hospital directly.
Medical History Assessment – A detailed discussion about past medical conditions and lifestyle factors.
Physical Examination & Diagnostic Tests – Conducting the required medical tests based on job specifications.
Doctor’s Evaluation & Report Generation – Comprehensive analysis of the test results with recommendations.
Report Submission to Employer – A detailed report is shared with both the candidate and employer.
Benefits for Employers and Employees
For Employers: Reduces employee turnover, ensures compliance, and fosters a healthier work environment.
For Employees: Provides early health insights, promotes wellness, and boosts confidence in job readiness.
Conclusion
A Pre-Employment Health Checkup is not just a formal requirement but an essential practice to ensure workplace safety and well-being. Companies that invest in employee health benefit from enhanced productivity, reduced absenteeism, and a healthier work environment. Preethi Hospitals, Madurai, offers customized health screening solutions, ensuring that both employers and employees are well-prepared for a successful and healthy professional journey.

0 notes
Text
The Importance of Spirometry Testing - Particularly in 'High Risk' Work Environments
If your business operates in construction or handling of chemicals, or you work in dusty or high-risk environments, your employees' lung health may be at risk without anyone being the wiser. Spirometry testing within the Greenfield Medical Centre is an important part of keeping lungs healthy.
Spirometry is a simple, non-invasive breathing test used to assess the health of the lungs. Spirometry is an excellent early detection method for conditions such as Asthma, COPD, and other illnesses that affect the respiratory tract, before it compromises work or quality of life.
At Greenfield Medical Centre, our experienced occupational medical team can deliver professional assessments of lung function to support your business's ability to maintain workplace health and safety. Regular Spirometry testing can ensure that your workforce remains healthy, productive, and compliant with occupational health practice.
✅ Quick and reliable testing
✅ Useful for WHS requirements
✅ Important for high-risk industries
📍 Visit us at the Greenfield Park Shopping Centre or contact us at 📞 02 9002 1300 | ✉️ [email protected]

#SpirometryTesting#WorkplaceHealth#GreenfieldMedical#OccupationalHealth#ConstructionSafety#LungHealth#WHSCompliance
0 notes
Text
Understanding Lung Cancer: Insights, Real-Life Stories, and Expert Care
Lung cancer remains one of the most challenging health concerns globally, affecting millions every year. In India, particularly in metro cities like Delhi and Gurgaon, the number of cases is on the rise due to increasing pollution, smoking, and other environmental factors. Early diagnosis and expert medical intervention are crucial for combating this life-threatening disease. If you or your loved one is facing a similar challenge, finding the Best Pulmonologist in Delhi / Gurgaon can make a significant difference in your journey to recovery.
Dr. Prashant Saxena is Senior Director & Head Pulmonology, Critical Care and Sleep Medicine Fortis Hospital, Vasant Kunj, Delhi and Fortis Hospital, Gurugram. He underwent Fellowship training in Westmead & Liverpool Hospitals, Sydney, Australia. He is an expert in the field of Interventional Pulmonology & Critical Care.

What is Lung Cancer?
Lung cancer occurs when abnormal cells in the lungs grow uncontrollably, forming tumors that interfere with normal lung functions. It is broadly categorized into:
Non-Small Cell Lung Cancer (NSCLC): The most common type, accounting for about 85% of cases.
Small Cell Lung Cancer (SCLC): A more aggressive form, often linked to smoking.
The disease progresses in stages, starting with localized tumors and, in advanced stages, spreading to other parts of the body.
Symptoms to Watch Out For
Lung cancer symptoms often go unnoticed in the early stages, making timely diagnosis challenging. However, as the disease progresses, the following symptoms might appear:
Persistent coughing, sometimes with blood
Shortness of breath
Unexplained weight loss
Chest pain
Fatigue
Recurrent infections such as pneumonia
If you notice these symptoms, consulting a Best Pulmonologist in Delhi / Gurgaon can help ensure timely intervention and treatment.
Common Causes and Risk Factors
Several factors contribute to the development of lung cancer:
Smoking: The leading cause, responsible for over 80% of cases.
Air Pollution: High levels of pollution in cities like Delhi can also increase the risk.
Genetics: A family history of lung cancer might predispose you to the disease.
Occupational Hazards: Long-term exposure to asbestos, radon, or other carcinogens in workplaces.
A Journey Through Diagnosis and Treatment
Diagnosing lung cancer typically involves imaging tests like X-rays, CT scans, and biopsies. Once diagnosed, treatment options depend on the stage and type of lung cancer.
Surgery: Effective for early-stage cancer by removing the tumor.
Chemotherapy and Radiation Therapy: Common for advanced stages to shrink or destroy cancer cells.
Targeted Therapy: Focuses on specific abnormalities in cancer cells.
Immunotherapy: Boosts the immune system to fight cancer.
Real-Life Testimonial: A Story of Hope
A 52-year-old non-smoker and fitness enthusiast from Gurgaon experienced a persistent cough and chest discomfort for months. Initially dismissing the symptoms as seasonal, she consulted her physician only when the problem worsened.
The diagnosis of stage II lung cancer came as a shock. However, under the care of the Best Pulmonologist in Delhi / Gurgaon, she underwent a successful surgery followed by targeted therapy. Today, she leads a healthy life and advocates for regular health check-ups and early diagnosis.
Another story involves a 62-year-old gentleman with a history of smoking who battled advanced lung cancer. Despite the initial grim prognosis, a combination of chemotherapy and immunotherapy extended his life significantly, allowing him to witness the marriage of his daughter and the birth of his grandson.
Why Timely Intervention Matters
Lung cancer is often labeled a silent killer due to its late diagnosis in many cases. However, regular screenings, especially for high-risk individuals, can help detect abnormalities early. Advanced diagnostic tools, along with the expertise of the Best Pulmonologist in Delhi / Gurgaon, ensure that patients receive personalized care tailored to their needs.
Preventive Measures for Lung Health
Prevention is always better than cure. Protect your lungs with these practical steps:
Quit smoking and avoid secondhand smoke.
Wear protective gear in high-risk workplaces.
Invest in air purifiers to combat indoor pollution.
Stay physically active and eat a balanced diet to boost immunity.
Seeking the Right Help
If you or someone close to you is dealing with lung health concerns, finding a qualified and experienced specialist is critical. The Best Pulmonologist in Delhi / Gurgaon will not only provide accurate diagnoses but also guide you through every step of your treatment journey with compassion and expertise.
Lung cancer is a formidable challenge, but with proper care, early detection, and the right medical support, many patients lead fulfilling lives even after a diagnosis. Remember, hope and healing begin with taking the first step toward expert consultation. Protect your lungs and cherish every breath!
0 notes
Text
NP HEALTH PROBLEM Common Health Problem in Primary Care Nurse Practitioner Practice and Recommendations for Its Medical Management Nurses are the initial point of contact for the patients in many medical settings, and the nurse practitioners (NP) are the primary source for providing basic medical care such as physical examinations, diagnostic tests, providing counseling, and writing prescriptions. A large growth is being witnessed in nurse practitioners around the world due to the arising pandemics; however, they have been of great help in usual health cases since they function in institutes like clinics, hospitals, schools, and workplaces. As they are the first initial source of medical care for the patients, they are the first-hand problem solvers since they have to guide them according to their medical requirements. This paper analyzes a common health problem faced by NPs and would recommend medical management for it. In further sections, the problem would be deeply analyzed for evaluation and providing suggestions. Healthcare Problem Identified Asthma inhalers are a source of relief for asthma patients since they are breathed directly into the lungs for the prevention of symptoms of this disease. The correct usage of inhalers is crucial for controlling the disease, and various studies have shown that patients were unable to use the asthma device incorrectly, causing uncontrolled asthma. Repeated education is needed; this should include physical demonstrations of the inhalers, checking if the patient's technique is workable, correcting the technique, and rechecking for its effectivity. It was also observed that trained staff id required for better instructing of the patients, and for this purpose, nurse practitioners play an important part. Additionally, the choice of the inhaler should depend on the cost-effectiveness, whether the patient can afford it or not so that he should be able to use it correctly and enhance its compliance. A study indicated that metered-dose inhaler (MDI) had the most frequent number of errors; in terms of coordination, 45 percent, speed, and depth of inspiration 44 percent, no breath-hold after inhalation 46 percent (Sanchis, Gich & Pedersen, 2016). Even dry powder inhalers (DPI) were checked for errors too, which revealed that incorrect preparations accounted for 29 percent error, no full expiration before inhalation was 46 percent, and no holding of breath after inhalation was 37 percent. The general prevalence of the correct technique was 31 percent. These problems occurred soon after metered-dose inhalers were launched. However, efforts were made to educate the patients about their usage. Nonetheless, there were still some patients who could not understand the particular method. The instruction methods included regular training programs, printed materials, videos, and software. Nurse practitioners also helped in the first-hand instructions to make it easier for them, including both children and adults. Chronic obstructive pulmonary disease (COPD) together with asthma are the two of the highly ranked diseases in the world that are leading causes of deaths of around 339 million people globally (Bhushan et al., 2018). It accounts for up to 1000 people dying each day, including both children and adults. COPD is the fourth leading cause of death and can go up in the rank in third place by the year 2020. Various studies have indicated that improper use of inhalers has led to an increase in asthma and COPD. Therefore hospital visits have surged as well. As it was noted that poor inhalation technique was the main reason for increased clinical visits, this was also because patients missed at least one serious step of the technique and had low literacy levels. The poor technique has been linked to factors like age, sex, educational levels, and emotive problems (Milanese et al., 2019). Younger asthmatic patients have reported more mishandling of the device, which resulted in poor disease control. In older patients, COPD is more common but requires prescribed medication, including inhalers. High rates of poor device handling were also reported among these patients, inducing severe exacerbations. In epidemiological terms, children have been more prone to this disease as compared to adults. Still, it would be difficult to reside upon these results since there have been different definitions of age for asthma status around the world (Dharmage, Perret & Custovic, 2019). For older people, the co-morbidity rates are hard to define since asthma symptoms could be related to breathlessness or COPD, inciting to heart failure. Environmental exposure at an early age, such as those among children, is the primary cause of early asthma. In utero parental smoking can provoke asthma in young children; studies have revealed that female smokers are more likely to have asthma as compared to non-smokers, but this data might not apply to men. Outdoor air pollutants are globally manipulating the quality of air inhaled by children and adults; thus, impacting heavily on asthmatic patients. Indoor allergens also should not be ignored since they have intense effects on asthmatic subjects. Occupational exposures are greatly affecting asthma patients since there are now two categories: work aggravated asthma (WEA) and occupational asthma (OA). Lifestyle factors, such as westernization and eating habits, have a command over asthma severity as well. In pathophysiological terms, the rise in asthmatic cases is due to extra clean air conditions, especially in western culture, since it would expose them less to the environment and increase the infections. When they interact with the outdoor air, the chances of getting air pollutants into the lungs and upsetting the immune systems rise. Bronchiolar inflammation is bound to happen to produce less resistance against asthma. The inflammation hurts trachea and bronchi, accelerating an increase in mucus production and a decrease in mucus clearance. Practice Guideline The clinical practice guideline addresses the identified health problem, which is poor inhaler education among asthma patients. The guidelines focus on the pivotal diagnosis stage and the asthma management for devising bronchodilator therapies and keeping track of periodic measurements of lung functioning before and after the therapy (Amerigroup Real Solutions, 2016). This practice guideline is based on current evidence that is available within the last five years. It was published in the year 2016 in line with US data. The strength of this evidence is the detailed information provided about the aesthetic patients and precautions for them. Also, there are follow up plans once the asthma action design has been put to effect. The practice guideline adequately directs the health care provider in the management of asthmatic interventions. There is a thorough description of the contributing factors for this disease, what triggers the patients and what methods should be used to avoid them, assessment and monitoring techniques are guided, pharmacotherapy is mentioned for better identification of individual's needs, and patient education plan, which is the basis of the problem identified in this paper. The clinical guidelines clearly state management procedures for the health care provider that includes reducing impairment and maintain normal lung function. This is guided by maintaining normal activity levels, and this is only possible when risks are reduced. The associated risks could be diminished by avoiding exacerbations, lessening the requirement of emergency or in-patient care, stopping failure of lung function, for children preventing shrinkage of lung growth, and lowering negative outcomes of the therapy. The performance of the clinical guidelines in the management of athematic patients is evident since combination and assessment of clinical therapies under the guidelines have improved the accuracy of asthma severity assessment (Dima, De Bruin & Ganse, 2016). The link between the provision of medical care services and the recipients is critical. Since this link is provided by the nurse practitioners who are the initial contacts for the patients, they play a vital part in assessing asthma severity. Practice guidelines provide a meaningful direction to the practitioners for reviewing asthma severity and provide appropriate pieces of advice for better therapies, including inhaler use. The health care services can impact asthma controlling in two parts: stirring asthma management process directly through medical care and altering caregiver and patient behaviors through behavioral care. It is well known that the performance of these two parts, medical and behavioral care, can be influenced by the clinical guidelines so that health care professionals, such as nurse practitioners, directly mold the patients' control in the disease. The control can be brought if clinical guidelines shape the modifiable factors of health care providers, such as medical knowledge, communication skills, training methods, and treatment techniques. All the recommendations of these related sections are presented in the practice guidelines which nurse practitioners can make use of for better patient education for asthma control. However, there are non-modifiable factors, too, like the experience of the nurse practitioner, his gender, and age. Educational interventions have been reported mitigating the outcomes of asthma in children and adult patients with an average follow up time of five months (Press et al., 2020). In the short term, the disease was controlled due to better educational techniques, either through physical demonstrations or sometimes virtual (V-TTG: virtual teach to goal) as well. Long term follow-ups were mainly held for those who consistently showed manhandling and poor disease control even after instructions being given. A guideline-recommended inhaler education was provided to the subjects through cost-effective virtual training. Inhaler techniques were examined using a 12-step checklist that was also in practice in the previous intervention studies. The effectuality of patient management can be checked by numerous designs, including health technology assessment, which would help in examining what technology and thereupatic methods are best in delivering positive results for asthma patients. Randomized methods can be useful as well, which include random allocation of probers for assessing the efficacy of installed methods in the clinical setting based on the clinical guidelines. Virtual monitoring that includes video monitoring through surveillance cameras within the clinical premises would help know whether patient management is done productively. For the past ten years, mobile phone technology has been very valuable. In the future, it can create wonders for asthma patients in impactful management and monitoring of adherence to inhaler methods (Morton et al., 2020). Nurse practitioners can assess through mobile monitored video apps whether the patients are adhering to underlying steps of inhaler use and what step they are missing, which is responsible for uncontrolled asthma. Web-based programs or e-health can help assess the patients and their adherence to self-management policies. It provides a flexible forum for patients to come forward and discuss their issues, and this can be achieved via education, empowerment, and active participation of both the nurse practitioners and the patients. Analysis Taking into consideration the future health care needs of patients with poor inhaler education, the pivotal role of nurse practitioners could not be ignored. Training should be given to the nurses for correct techniques, which later should be transferred to the patients for overcoming symptoms of asthma. It is not wrong to assert that successful nurse education would reap fruitful results in disabling consequences for asthma patients. Training can be provided hospital-wide through one-on-one education methods, classes through the web, or unit-based education (Scullion, 2018). Placebo devices could be used for giving demonstrations to the nurse practitioners so that they get aware of the using techniques. Afterward, they could transfer this knowledge accurately to the patients. These devices would not be useful for nurse practitioners only but also for the patients so that they get familiar with their use beforehand. Nurse education should also include getting aware of all the new medications in the market and what medicines are obsolete so that when an asthma patient comes in for urgent help, he could be prescribed with up-to-date medications. In the future, there is a demand to check whether the inhalator's use and their methods are properly utilized by the asthma patients to control the disease. For this purpose, there are many tools to aid patients in precise inhaler handling. In-check DIAL allows the health care specialists to train patients about the inhalers as it assesses the peak inspiratory flow. There is another device called Trainhaler used for training patients on the same grounds; though, it has an additional feature that its mouth-piece, called Flo-Tone, can be changed for each individual as it is convenient for multi-patient usage. The future health care needs of asthma patients also require the nurse practitioners to be aware of the religious or cultural concerns while using an inhaler. This means some populations might not be able to use inhalers due to some extent of alcohol mixed with the medication. Moreover, some cultural beliefs hinder them from using inhalers as they take it as impolite or a type of oral drug. Some studies have shown that mothers of asthmatic children have been apprehensive of the use of drugs or inhalers for their children since either they were not completely comfortable with the medical system or they were unsure of the chemical formulation of the inhalers. With the emergence and increased need for e-health, asthma control requires smart inhalers, which would allow the patients to connect with the help of Bluetooth connectivity and collect data by a health app or website. This could be accessed later by the patient (self-management), his nurse practitioner, or specific asthma doctor to whom he regularly visits. Furthermore, these inhalers allow the patient to set reminders for taking medications, and enablement of efficiency can be monitored as well. Technology should be considered seriously regarding asthma control since it helps in making healthcare more tailored, reachable, and acceptable to patients. Changes in global demographics are bringing changes to the US as well that would directly affect the clinical practice guidelines and healthcare within the country. For instance, Millennials (people with ages 23 to 28) would increase in number as compared to Baby Boomers (ages 55 to 73). Still, there is a greater population, Generation Z, maturing to adulthood (Cilluffo & Cohn, 2019). Millennials are more educated, leading to the fact that high literacy would bring high education about inhaler use and fewer mistakes, resulting in lower asthma cases. Generation Z is arguably the most ethnically diverse and most educated generation by far, hence, assuming to be more informative about inhaler use. Forty-eight percent of Generation Z people are racial or ethnic minorities and are expected to be the largest US racial group casting votes. This huge category of voters would help in framing the healthcare system of the country, directly influencing the clinical guidelines. Changes in family patterns are highly evident; the unmarried parents living with a child has increased from 7 percent to 25 percent. US children living with unmarried parents are now 32 percent, which was 13 percent back in 1968. Stay-at-home parents represent 18 percent of the US population. These facts show that children who would be cared for and monitored by their parents regarding asthma control would be fashioned accordingly. The clinical guidelines have to be designed accordingly so that guidelines include the role of parents in controlling asthma in young ones. The immigrants in the US have been increasing rapidly but remain low as compared to other countries. This means that the inclusion of people from a variety of cultures and religious beliefs would be entering the US, thus forcing the country to revise its clinical guidelines. Household income is highest in recent years in the US, and this is more apparent in some racial groups. This could pattern the use of inhalers since rich people would be more likely to opt for more advanced and expensive medications for asthma control, thus aiming at lower disease prevalence. Clinical practitioners can guide these people regarding the most suitable medications that they can afford and adhere to. Changes in healthcare policies also greatly imply how asthma patients take medications and what health care insurance plans they have to utilize. For case in point, with the new Affordable Care Act (ACA), the protection for asthma people still exists, but they have to look for medicines that are listed on that plan; only those supplements would be free of cost. This means if one medication suits them but is not listed in free coverage, then asthma patients would have to buy it from the appointed shop. If clinical guidelines were to be revised, the changes could be based on the above-mentioned shifting world demographics, which would consequently influence the US health care trends. These could be used as evidence for revising the practice guidelines. Three basic changing drifts- an aging population, increased ethnicity, and urbanization- would outline the way nurse practitioners would have to intervene for better provision of support to asthma patients for inhaler education. If practice guidelines were to be changed based on the aging population, then it should be kept in mind that prolonged ages would lead to asthma care over several years. Besides integrating traditional practice guidelines about inhaler education, the use of smart apps would be beneficial. The clinical guidelines should include education about such apps, for all age groups encompassing Baby Boomers, Millennials, and Generation Z. Clinical guidelines should be revised for increased ethnicity since immigrants have largely grown in numbers within the US, and people from different cultures are entering the states. Practice guidelines should cater to the religious and cultural aspects of ethnic asthmatic patients so that inhaler use should take into consideration whether or not it contains alcohol or is deemed inappropriate for oral use. Additionally, if Hispanic people are coming into a region, they might feel comfortable talking to a Hispanic doctor. So, hiring of culturally competent practitioners should be considered for inhaler education of asthmatic patients; their recruitment in the healthcare workforce and training is a grave need of current times. Clinical guidelines should be revised for rising urbanization since people's lifestyles and eating habits would be changed. Highly educated individuals would be increasingly aware of inhaler use; hence, asthma could be controlled. Nevertheless, if they are living in urban areas, there is more likeliness that the areas would have more vehicles and more air pollution; therefore, triggering of asthma is inevitable. For such patients, clinical guidelines should include self-management techniques such as knowing one's trigger points, knowing the medications and dosage, being familiar with the inhaler device, and steps involved in inhaler use. Individuals living in urban regions would be more alert to the technological methods for checking their asthma symptoms and should be in constant contact with their nurse practitioner with the monitoring apps. Read the full article
0 notes
Text
Lung Cancer: Understanding the Condition
Lung cancer is one of the most common and deadliest forms of cancer worldwide. It occurs when abnormal cells in the lungs begin to grow uncontrollably, forming tumors that can interfere with lung function.
Types of Lung Cancer:
Non-Small Cell Lung Cancer (NSCLC): This is the most common type, accounting for about 85% of all lung cancer cases. It includes subtypes like adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Small Cell Lung Cancer (SCLC): Less common but more aggressive, this type of lung cancer tends to spread more quickly.
Causes and Risk Factors:
Smoking: The leading cause of lung cancer, responsible for approximately 85% of cases. The harmful chemicals in tobacco smoke damage lung tissue.
Exposure to Radon Gas: A natural radioactive gas found in soil and rocks that can accumulate in homes.
Asbestos Exposure: Long-term exposure to asbestos increases the risk of lung cancer.
Environmental Pollutants: Prolonged exposure to air pollution and chemicals in the workplace can contribute to the development of lung cancer.
Genetic Factors: A family history of lung cancer can increase the risk.
Symptoms of Lung Cancer:
Persistent Cough: A cough that doesn't go away or worsens over time.
Coughing Up Blood: Even small amounts of blood may indicate lung cancer.
Shortness of Breath: Difficulty breathing or wheezing.
Chest Pain: Pain or discomfort in the chest, which may worsen with coughing or deep breathing.
Unexplained Weight Loss: Significant and unexplained weight loss may occur in advanced stages.
Fatigue: Feeling constantly tired or weak.
Diagnosis and Treatment:
Imaging Tests: Chest X-rays, CT scans, and PET scans can detect lung cancer and determine its spread.
Biopsy: A sample of lung tissue is examined under a microscope to confirm the diagnosis.
Surgical Treatment: Surgery to remove part or all of the lung may be an option if the cancer is localized.
Chemotherapy and Radiation Therapy: Used to kill cancer cells or shrink tumors, often combined with surgery.
Targeted Therapy and Immunotherapy: Newer treatments that focus on specific genetic mutations or boost the immune system to fight cancer.
Prevention:
Quit Smoking: The best way to reduce the risk of lung cancer is to stop smoking and avoid secondhand smoke.
Avoid Environmental Toxins: Limit exposure to pollutants like asbestos and radon.
Healthy Diet and Exercise: A healthy lifestyle can help reduce the risk of many types of cancer.
For more information on lung cancer, refer to the article Lung Cancer from Rama Mahidol University.
0 notes