#zirconia milling machine
Text
Enhance Your Dental Practice with Dotta Dental's Advanced Zirconia Milling Machine
Introducing Dotta Dental's Advanced Zirconia Milling Machine - the perfect solution to enhance your dental practice. With cutting-edge CAD/CAM technology, this state-of-the-art machine is designed specifically for dental professionals who prioritise precision and efficiency.
Our dental zirconia milling machine is meticulously engineered to deliver exceptional results. It utilizes the latest advancements in zirconia milling technology, ensuring superior quality restorations with optimal fit, strength, and aesthetics. Whether you're crafting crowns, bridges, or implant abutments, our machine guarantees consistent and accurate results every time.
0 notes
Text
0 notes
Text
Unlocking the Perfect Smile: The Marvels of Implant Abutments
Dental implants are a popular restorative option for patients with missing teeth. An implant consists of a small titanium post that is surgically inserted into the jawbone, which serves as the root of the tooth. After the implant has been placed, an abutment is attached to it, which connects the implant to the implant crown. In this blog, we will explore what an abutment is, its role in implant dentistry, and the types of implant abutments available.
What is an Abutment in Dental Implant?
An abutment in a dental implant is a connector that attaches to the implant post and protrudes above the gum line. The implant abutment serves as a foundation for the implant crown, which is the visible part of the tooth restoration. The abutment can be made of different materials, including titanium, zirconia, or porcelain. It is usually placed after the implant post has integrated into the jawbone.
Role of Abutment in Dental Implant
The abutment in dental implant plays a crucial role in implant dentistry. It connects the implant post to the implant crown and serves as a support for the crown. The abutment is designed to fit precisely with the implant post and the implant crown to ensure stability and prevent any movement. It is also responsible for creating an aesthetic appearance that matches the surrounding natural teeth.
Types of Implant Abutments
There are different types of implant abutments available, depending on the implant system and the patient's needs. Here are some of the commonly used implant abutments:
Stock Abutments: Stock abutments are pre-manufactured abutments that come in different shapes and sizes. They are available for most implant systems and can be used in standard cases. Stock abutments are a cost-effective option, but they may not provide the best aesthetic results.
Custom Abutments: Custom abutments are made specifically for a patient's implant case. They are designed to match the contours of the implant post and the implant crown, providing better aesthetic results. Custom abutments are more expensive than stock abutments, but they offer better outcomes.
Angled Abutments: Angled abutments are used in cases where the implant post is not placed vertically. They allow for proper alignment of the implant crown and improve the aesthetic appearance of the restoration.
Implant Abutment Crown
The implant abutment crown is the visible part of the tooth restoration that attaches to the abutment. It is usually made of porcelain or ceramic material, which provides an aesthetic appearance that matches the surrounding natural teeth. The implant abutment crown is designed to fit precisely with the abutment and provide stability and support.
Conclusion
An abutment in a dental implant plays a vital role in implant dentistry. It connects the implant post to the implant crown and provides stability and support for the restoration. Choosing the right type of implant abutment depends on the implant system and the patient's needs. Monumental Dental Engineering offers a wide range of implant abutments and dental milling machines to meet the needs of dentists and dental laboratories. With the right equipment and materials, you can provide your patients with the best possible dental care.
3 notes
·
View notes
Text
Dental Laboratory Supplies That Are Transforming the Industry
The world of dental care is undergoing significant changes, thanks to new advancements in technology and an increasing demand for precision and efficiency. Dental laboratory supplies in the USA play a pivotal role in this transformation, offering innovative solutions that are reshaping how dental practices operate. As the industry evolves, the role of dental equipment suppliers and the quality of dental lab supply become crucial for delivering top-notch patient care and achieving the best results.
How Dental Laboratory Supplies Are Evolving
Recently, the dental industry has seen major advancements in laboratory technology. Dental laboratory supplies in the USA now include a range of sophisticated tools and materials that boost the accuracy and efficiency of dental procedures. From cutting-edge diagnostic equipment to high-precision manufacturing tools, these supplies are essential for modern dental laboratories.
This evolution mirrors broader trends in healthcare, emphasizing innovation and quality. Dental practices are increasingly relying on dental equipment suppliers to provide advanced tools that meet high performance standards and reliability.
Key Innovations in Dental Laboratory Supplies
Several innovations are making a big impact in the realm of dental laboratory supplies:
Advanced Imaging Systems: Modern imaging systems have transformed diagnostics and treatment planning. Digital X-rays and 3D imaging technologies offer detailed views of dental structures, leading to more accurate assessments and better treatment outcomes. These systems are a critical part of dental laboratory supplies and are being adopted more widely.
Precision Milling Machines: The introduction of precision milling machines has greatly improved the production of dental prosthetics and restorations. These machines enable the creation of custom dental crowns, bridges, and dentures with exceptional accuracy and durability. The ability to produce high-quality restorations quickly is a significant leap in dental lab supply.
Innovative Materials: Advances in materials science have led to new dental materials with enhanced aesthetics, strength, and biocompatibility. Materials like zirconia and advanced resin composites are now commonly used, offering patients durable and natural-looking results.
Digital Workflow Integration: Digital workflows are streamlining many aspects of the production process in dental laboratories. From digital impressions to computer-aided design (CAD) and computer-aided manufacturing (CAM), these technologies create a smooth transition from diagnosis to treatment, improving both efficiency and accuracy.
Why Choosing the Right Dental Equipment Suppliers Matters
Selecting the right dental equipment suppliers is essential for ensuring that dental practices have access to high-quality dental lab supply. Reputable suppliers not only provide top-of-the-line equipment but also offer essential support and training to maximize the effectiveness of their products. The relationship between dental practices and suppliers is key to maintaining quality and consistency in dental care.
When choosing dental equipment suppliers, consider their range of products, reputation, and the level of customer support they offer. Trusted suppliers should provide comprehensive solutions that meet the specific needs of dental laboratories and practices, ensuring they have the best tools available.
How Alvy Dental Stands Out
Alvy Dental is a leading provider of exceptional dental laboratory supplies and equipment. Committed to quality and innovation, Alvy Dental offers a broad range of products designed to meet the highest performance standards. From advanced imaging systems to precision milling machines and innovative materials, Alvy Dental supports dental practices with top-tier tools and solutions.
By choosing Alvy Dental, dental professionals gain access to high-quality dental lab supply and outstanding support, helping them deliver superior care to their patients. Alvy Dental is dedicated to being a trusted partner in the evolving dental technology landscape, enhancing the capabilities of dental laboratories and practices across the USA.
The role of dental laboratory supplies in the USA is crucial in advancing the field of dentistry. Innovations in equipment and materials are changing how dental laboratories function, providing tools that enhance precision, efficiency, and patient outcomes. Selecting the right dental equipment suppliers is key to accessing top-quality supplies and ensuring successful dental treatments. Alvy Dental is proud to offer leading dental lab supply, committed to supporting the dental industry with cutting-edge solutions and exceptional service.
0 notes
Text
Understanding Dental Crowns: Types, Procedures, and Comprehensive Care

Introduction:
Dental crowns are a vital component of restorative dentistry, offering both functional and aesthetic benefits. Whether you're dealing with a damaged tooth, want to enhance your smile, or need to protect a weakened tooth, dental crowns provide a reliable solution. In this detailed guide, we will explore what dental crowns are, why you might need one, the different types available, and what to expect during the procedure. We’ll also discuss the benefits, risks, and how to care for your crown to ensure it lasts for years.
What is a Dental Crown?
A dental crown is a custom-made cap that covers a damaged, decayed, or unattractive tooth. It restores the tooth’s shape, size, strength, and appearance. Crowns can be made from various materials, including porcelain, metal, or a combination of both, and are designed to blend seamlessly with your natural teeth.
When Would You Need a Dental Crown?
Dental crowns are recommended in several situations, including:
To protect a weak tooth from breaking or to hold together parts of a cracked tooth.
To restore an already broken or severely worn down tooth.
To cover and support a tooth with a large filling when there isn’t much tooth left.
To hold a dental bridge in place.
To cover misshapen or severely discolored teeth.
To cover a dental implant.
To make a cosmetic modification to improve the appearance of a smile.
There are several types of dental crowns available, each with its own advantages:
Metal crowns
Dental technicians use several metals to make dental crowns, including gold, palladium, nickel and chromium. Metal crowns rarely chip or break, last the longest in terms of wear and only require a small amount of enamel removal. They can also withstand biting and chewing forces.
The metallic color is the main drawback of this type of crown. Metal crowns are a good choice for out-of-sight molars.
Porcelain-fused-to-metal (PFM) crowns
Porcelain-fused-to-metal (PFM) crowns combine the durability of metal and the natural look of porcelain. Dentists can match these crowns to the shade of your own teeth.
Despite their strength, PFM crowns have some drawbacks. For example, the porcelain coating may chip off over time, exposing the metal underneath. In addition, PFM crowns may gradually wear down the enamel on your opposing teeth (the teeth that touch your crown when you close your mouth).
PFM crowns last almost as long as metal crowns. They can restore both front and back teeth.
Pressed ceramic crowns
A pressed ceramic crown has a hard inner core. It’s similar to a PFM, but the core is ceramic instead of metal. To make this inner core, a technician melts and presses ceramic in an oven at a very high temperature. Next, they add multiple layers of porcelain. Like all-porcelain crowns, pressed ceramic crowns mimic the translucency of natural tooth enamel.
Pressed ceramic crowns have the same drawbacks as PFM crowns. The layers of ceramic can chip away over time. Dentists use pressed ceramic crowns on front and back teeth.
All-ceramic or porcelain crowns
All-ceramic or porcelain crowns mimic the appearance of tooth enamel more than any other crown type. They’re also a good choice if you have metal allergies.
Lab technicians use many different materials to make ceramic crowns, but one of the most popular is zirconium dioxide. Zirconia crowns are extremely durable and can withstand heavier forces than other types of ceramic crowns. They’re also gentle on your opposing teeth, resulting in less enamel wear.
Same-day dental crowns
Many dentists use CAD/CAM (computer-aided design and manufacturing) technology to create crowns in their office while you wait. This software allows your dentist to take digital dental impressions of your teeth, and then use those impressions to design a custom crown. Once your dentist designs your crown, they’ll send the image files to an on-site milling machine. The machine will craft your new crown from a solid block of ceramic.
The main advantage of CAD/CAM technology is that you can get a dental crown in just one office visit. However, same-day crowns aren’t for everyone. Ask your dentist if you’re a candidate.
All-resin crowns
Dental crowns made out of resin are generally less expensive than other types of crowns. But they’re fragile and more likely to break compared to porcelain-fused-to-metal (PFM) crowns.
Dentists often use resin to make temporary crowns. They last three to five years on average.
First Visit: Preparation:
Temporary Crown Removal: The temporary crown is removed, and the custom-made crown is placed on the tooth.
Cementing: The dentist checks the fit and color of the crown. If everything looks good, the crown is permanently cemented into place.
What are the Benefits of Dental Crowns?
Restoration of Function: Crowns restore the ability to bite and chew normally.
Protection: They protect weak teeth from further damage or decay.
Aesthetic Improvement: Crowns can significantly enhance the appearance of damaged or discolored teeth.
Durability: With proper care, crowns can last many years, providing long-term benefits.
What are the Risks of Dental Crowns?
Sensitivity: Some patients may experience sensitivity to hot or cold temperatures after getting a crown.
Chipping or Breaking: Although rare, crowns made of porcelain can chip or break under excessive force.
Loose Crown: Over time, the cement that holds the crown in place may wear out, causing the crown to become loose.
Allergic Reactions: Although uncommon, some patients may have allergic reactions to the materials used in the crown.
How Long Does It Take to Feel Better After a Dental Crown Procedure?
Most patients feel better within a few days after the procedure. It’s normal to experience some sensitivity or discomfort initially, but this usually subsides quickly.
Foods to Avoid with a Crown To prolong the life of your crown, it’s advisable to avoid:
Hard foods like nuts and ice that could crack the crown.
Sticky foods like caramel and chewing gum that could pull the crown off.
Sugary foods that can lead to decay around the crown.
Are Dental Crowns Permanent? Dental crowns are not permanent, but they are long-lasting. With proper care, a crown can last anywhere from 10 to 30 years. The longevity depends on the material used, the location of the crown, and your oral hygiene practices.
Additional Details
Veneers vs. Crowns: Which Option is Right for Me? Veneers are a thinner, more conservative option that only covers the front surface of the tooth, making them ideal for cosmetic changes. Crowns, on the other hand, encase the entire tooth and are better for teeth that need strengthening or have significant damage.
What’s the Most Common Alternative to a Crown? A common alternative to a crown is a dental veneer or an inlay/onlay. These options are less invasive but may not provide the same level of protection as a crown, particularly for teeth that are heavily damaged.
Dental Cap vs. Crown: Is There a Difference? The terms "dental cap" and "crown" are often used interchangeably. Both refer to the same dental restoration used to cover and protect a damaged tooth.
Conclusion:
Dental crowns are a versatile and effective solution for restoring damaged teeth, enhancing aesthetics, and providing long-term protection. Whether you're dealing with a cracked tooth, severe decay, or simply want to improve your smile, a dental crown can be the right choice. At My Scottsdale Dentist, we offer a range of crown options tailored to your specific needs. To learn more or schedule an appointment, contact us today and take the first step toward a healthier, more beautiful smile.
#all-on-4 implants treatment#scottsdale#all-on-4 implants#dental treatment#dental implants#dentistry#my scottsdale dentist#scottsdale dental care#dental bridge scottsdale#dental services#Crowns dental care#Dental Crowns Scottsdale#crowns Scottsdale#dental care#dental health#dentist
0 notes
Text
Wondering What's Next in Cosmetic Dentistry Innovations?

The world of cosmetic dentistry is constantly evolving, offering exciting new possibilities for achieving a dazzling smile. From minimally invasive procedures to digital technology advancements, the future promises remarkable transformations for those seeking a smile makeover. Let's explore some of the most promising innovations on the horizon that can soon be available at a cosmetic dentist in Palm Springs.
Minimally Invasive Techniques: Achieving Big Results with Smaller Steps
The trend towards minimally invasive procedures continues to gain momentum. Here's how cosmetic dentistry is embracing this approach:
Advanced Veneers: Veneers are thin shells of porcelain or composite resin bonded to the front surface of teeth to improve their appearance. Traditionally, some tooth enamel needed removal for veneer placement. Now, advancements in materials and techniques allow for ultra-thin veneers that require minimal to no enamel reduction, preserving more of the natural tooth structure.
Laser Gum Reshaping: Uneven gumlines can detract from a smile's aesthetics. Laser gum reshaping offers a precise and controlled method to reshape the gum tissue for a more balanced and symmetrical appearance. This minimally invasive procedure minimizes bleeding and discomfort compared to traditional methods.
Digital Dentistry: Revolutionizing Smile Design
Digital technology is transforming the way cosmetic dentists in Palm Springs plan and execute smile transformations:
Digital Smile Design (DSD): DSD utilizes digital imaging and software to create a virtual mockup of your ideal smile. This allows you to visualize the desired outcome before any procedures begin and collaborate with your dentist to achieve the perfect results.
Computer-Aided Design/Computer-Aided Manufacturing (CAD/CAM): CAD/CAM technology streamlines the creation of custom dental restorations like crowns and veneers. Digital impressions are taken of your teeth, and then a computer designs the restoration precisely. This design is then sent to a milling machine that crafts the restoration with exceptional accuracy and efficiency.
Biocompatible Materials: Enhancing Aesthetics with Natural-Looking Results
The development of new biocompatible materials is pushing the boundaries of what's possible in cosmetic dentistry:
Metal-Free Restorations: Traditional dental crowns often contain metal, which can sometimes show a dark line at the gum margin. New advancements in materials like zirconia allow for restorations that are incredibly strong, durable, and mimic the natural translucency of teeth, offering a more natural-looking aesthetic.
Biomimetic Dentistry: This emerging field focuses on using materials that mimic the natural structure and function of teeth. These materials can potentially promote regeneration of tooth tissue and offer more long-lasting solutions for certain cosmetic concerns.
The Future of Cosmetic Dentistry: A Brighter, Healthier Smile Awaits
These are just a few examples of the exciting advancements shaping the future of cosmetic dentistry. As technology continues to evolve, we can expect even more innovative and personalized approaches to achieving a healthy, beautiful smile. If you're considering a smile makeover, consulting with a qualified cosmetic dentist in Palm Springs is the first step. They can discuss your goals, assess your oral health, and recommend the most suitable treatment options based on the latest advancements and your unique needs. With the power of these emerging innovations, achieving a smile you love can be a reality.
0 notes
Text
The Evolution of Dental Implant Technology: What's New in the Field?

Are you considering dental implant technology to restore your smile? If so, you're in luck, as this field has seen incredible advancements in recent years. From improved materials to more efficient procedures, the evolution of dental implant technology has transformed the way we approach tooth replacement.
In this article, we will explore the latest innovations in the field of dental implant technology and how they are revolutionizing the industry. Whether you are a patient seeking information on the newest options available or a dental professional looking to stay up-to-date with the latest advancements, this article will provide you with valuable insights.
Traditional dental implant techniques
Dental implants have been used for decades to replace missing teeth. Traditional implant techniques involve the insertion of a titanium post into the jawbone, which acts as an artificial tooth root. Over time, the jawbone fuses with the implant, providing a solid foundation for a crown or denture.
However, traditional dental implant procedures often required multiple appointments and a lengthy healing period. Patients had to wait for the implant to integrate with the jawbone before receiving their final restoration, which could take several months.
The evolution of dental implant technology
In recent years, dental implant technology has undergone significant advancements, making the entire process faster, more efficient, and less invasive. These innovations have not only improved patient experience but also increased the success rate of dental implant procedures.
One of the most notable advancements is the development of new materials for dental implants. Traditional implants are made from titanium, which has excellent biocompatibility and durability. However, newer materials, such as zirconia and titanium alloys, offer enhanced biocompatibility and longevity, making them ideal for dental implant applications.
Another area of evolution is implant design. Modern implants feature innovative designs that improve stability and reduce healing time. For example, some implants have a tapered shape that allows for better integration with the jawbone, while others have a roughened surface that promotes osseointegration.
Advancements in dental implant materials
The choice of materials for dental implants plays a crucial role in the success of the procedure. In recent years, researchers have focused on developing materials that offer improved biocompatibility, durability, and aesthetics.
Zirconia implants have gained popularity due to their excellent biocompatibility and natural appearance. These implants are made from a ceramic material that closely resembles natural teeth, making them an ideal choice for patients looking for a more aesthetic solution.
Titanium alloys, on the other hand, offer exceptional strength and durability. These implants are often used in cases where high load-bearing capacity is required, such as in the posterior region of the mouth.
Computer-aided design and manufacturing (CAD/CAM) in dental implantology
Computer-aided design and manufacturing (CAD/CAM) technology has revolutionized the field of dental implantology. This technology allows for the precise planning and fabrication of dental restorations, resulting in better aesthetic outcomes and improved patient satisfaction.
With CAD/CAM technology, dental professionals can create a virtual model of the patient's mouth and design custom-made restorations that perfectly fit their unique anatomy. These restorations can then be milled from a block of material, such as zirconia or titanium, using a computer-controlled milling machine.
CAD/CAM technology not only improves the accuracy and fit of dental restorations but also reduces the turnaround time, allowing patients to receive their final restorations in a shorter period.
Guided implant surgery: A game-changer in dental implant procedures
Guided implant surgery is a revolutionary technique that combines computer-guided planning with minimally invasive surgery. This technique allows for the precise placement of dental implants, reducing the risk of complications and improving the overall success rate of the procedure.
With guided implant surgery, a three-dimensional virtual model of the patient's mouth is created using specialized software. The implant position, size, and angulation are planned in advance, taking into account the patient's unique anatomy and esthetic requirements.
During the surgery, a surgical guide, which acts as a template, is used to guide the placement of the implants. This ensures accurate positioning and minimizes the risk of damage to surrounding structures.
Guided implant surgery offers numerous benefits, including reduced surgical time, less post-operative discomfort, and improved esthetic outcomes. It is especially beneficial in complex cases where precise implant placement is critical.
Immediate load dental implants: The future of tooth replacement
Immediate load dental implants, also known as same-day implants or teeth-in-a-day, have revolutionized the field of tooth replacement. With this technique, patients can receive a fully functional set of teeth on the same day as their implant surgery, eliminating the need for a lengthy healing period.
Immediate load implants are designed to provide immediate stability and support for a temporary restoration. These temporary restorations are fabricated in advance and can be attached to the implants immediately after surgery.
The ability to restore function and esthetics immediately after implant placement has significant advantages for patients. They can resume eating, speaking, and smiling with confidence right away, without having to wait for the traditional healing period.
However, not all patients are suitable candidates for immediate load implants. Factors such as bone quality, implant stability, and the patient's oral health need to be carefully evaluated before determining if this technique is appropriate.
3D printing in dental implantology
3D printing, also known as additive manufacturing, has revolutionized various industries, including dentistry. This technology allows for the fabrication of custom-made dental implants, surgical guides, and dental restorations with unparalleled precision and efficiency.
With 3D printing, dental professionals can create highly accurate models of the patient's mouth, which serve as a basis for treatment planning and implant fabrication. These models can be used to create surgical guides, which ensure precise implant placement during surgery.
In addition to surgical guides, 3D printing can be used to fabricate custom-made dental restorations, such as crowns, bridges, and dentures. This technology allows for the creation of highly aesthetic and functional restorations that perfectly fit the patient's unique anatomy.
The role of 3D printing in dental implantology is continuously evolving, with ongoing research focusing on developing new materials and techniques to further improve patient outcomes.
The role of digital dentistry in dental implant technology
Digital dentistry has significantly contributed to the evolution of dental implant technology. This field encompasses various technologies, including digital imaging, computer-aided design and manufacturing, and computer-guided surgery.
Digital imaging, such as cone beam computed tomography (CBCT), allows for precise three-dimensional imaging of the patient's oral structures. This information is invaluable for treatment planning, implant placement, and the fabrication of surgical guides.
Computer-aided design and manufacturing (CAD/CAM) technology, as mentioned earlier, enables the precise fabrication of dental restorations and surgical guides. It streamlines the entire treatment process, from planning to final restoration delivery.
Computer-guided surgery, as discussed in the previous section, ensures accurate implant placement and minimizes the risk of complications. This technology has revolutionized the field of implantology, making the procedure more predictable and efficient.
Digital dentistry has not only improved the accuracy and efficiency of dental implant procedures but has also enhanced patient communication and involvement in the treatment process. Patients can visualize the proposed treatment outcome and actively participate in decision-making.
The evolution of dental implant technology has transformed the field of dentistry, offering patients more efficient, comfortable, and aesthetically pleasing tooth replacement options. From advancements in materials to innovative techniques, dental professionals can now provide tailored solutions that meet the unique needs of each patient.
As technology continues to advance, we can expect further breakthroughs in dental implant technology, further improving patient outcomes and satisfaction. Whether you are a patient or a dental professional, staying informed about the latest advancements in the field is crucial for making informed decisions and providing the best possible care.

Finding the right dental clinic is crucial for maintaining your oral health and ensuring that you receive the best possible care. Your teeth and gums play a vital role in your overall well-being, so it's essential to prioritize your dental care. Here at Arvada Dental Center & Implants, we understand the importance of choosing the right dental clinic, and we are committed to providing exceptional care to our patients in Arvada, CO.
Factors to Consider When Choosing a Dental Clinic
When selecting a dental clinic, there are several factors to consider to ensure that you make an informed decision. These factors include the location and convenience of the clinic, the reputation and credentials of the dentists, the range of services offered, the technology and equipment available, the reviews and testimonials from previous patients, the insurance and payment options accepted, and the accessibility of emergency services. Let's explore each of these factors in more detail.
Location and Convenience
The location of the dental clinic is an important consideration, as you want a clinic that is easily accessible and convenient for your needs. Ideally, choose a clinic that is close to your home or workplace, as this will make it easier for you to schedule regular check-ups and appointments. At Arvada Dental Center & Implants, we are conveniently located in Arvada, CO, making it convenient for residents in the area to access our services.
Reputation and Credentials
When choosing a dental clinic, it's important to research the reputation and credentials of the dentists. Look for dentists who are highly qualified and experienced, as this will give you confidence in their ability to provide top-notch care. Check if the dentists are members of professional organizations and if they have received any awards or recognition for their work. At Arvada Dental Center & Implants, our team of dentists is highly trained and experienced, and we take pride in delivering exceptional care to our patients.
Range of Services Offered
Consider the range of services offered by the dental clinic to ensure that they can meet all your dental needs. Look for a clinic that provides a comprehensive range of general and specialized dental services, including routine check-ups, cleanings, fillings, orthodontics, cosmetic dentistry, and dental implants. At Arvada Dental Center & Implants, we offer a wide range of services to cater to the diverse needs of our patients, ensuring that they receive the highest quality care under one roof.
Technology and Equipment
Advancements in dental technology have revolutionized the field of dentistry, allowing for more precise diagnoses and effective treatments. When choosing a dental clinic, inquire about the technology and equipment they have available. Look for clinics that invest in state-of-the-art technology, such as digital X-rays, intraoral cameras, and laser dentistry. At Arvada Dental Center & Implants, we stay up to date with the latest advancements in dental technology, ensuring that our patients receive the most advanced and effective treatments.
Reviews and Testimonials
Reading reviews and testimonials from previous patients can provide valuable insights into the quality of care provided by a dental clinic. Look for clinics that have positive reviews and testimonials, as this indicates a high level of patient satisfaction. You can also ask for recommendations from friends, family, or colleagues who have had positive experiences with a particular dental clinic. At Arvada Dental Center & Implants, we are proud of the positive reviews and testimonials we have received from our satisfied patients, reflecting our commitment to delivering exceptional care.
Insurance and Payment Options
Before choosing a dental clinic, consider the insurance and payment options they accept. Dental treatments can be costly, so it's important to find a clinic that accepts your insurance plan or offers flexible payment options, such as payment plans or financing options. At Arvada Dental Center & Implants, we work with a variety of insurance providers and offer convenient payment options to help make dental care more affordable and accessible for our patients.
Accessibility and Emergency Services
In case of dental emergencies, it's crucial to choose a dental clinic that offers accessibility and emergency services. Look for clinics that have extended hours, weekend availability, or emergency on-call services. This ensures that you can receive prompt care in case of unexpected dental issues. At Arvada Dental Center & Implants, we understand that dental emergencies can happen at any time, which is why we offer extended hours and emergency services to address our patients' urgent dental needs.
Top Dentists in Arvada, CO
Arvada, CO is home to many highly skilled and reputable dentists who are dedicated to providing exceptional care. When searching for a top dentist in Arvada, consider the factors mentioned above and explore the qualifications, experience, and expertise of the dentists. At Arvada Dental Center & Implants, we are proud to have a team of top dentists who are committed to delivering personalized care and achieving optimal oral health for our patients.
In conclusion, choosing the right dental clinic and top dentist in Arvada, CO is essential for maintaining your oral health and receiving exceptional care. Consider factors such as location and convenience, reputation and credentials, range of services offered, technology and equipment, reviews and testimonials, insurance and payment options, and accessibility and emergency services. At Arvada Dental Center & Implants, we meet all these criteria and more, ensuring that our patients receive the highest quality dental care in a warm and welcoming environment. Book your appointment with us today and experience the difference in quality care and exceptional results.
Arvada Dental Center & Implants
6695 Wadsworth Blvd, Arvada, CO 80003
303–421–7611
https://arvadadentalcenter.com/
0 notes
Text
Advancing Dental Technology: Insights into the Germany Dental CAD-CAM Market
In the realm of dentistry, technological advancements have transformed the landscape, offering more precise, efficient, and patient-friendly solutions than ever before. Among these innovations, Computer-Aided Design and Computer-Aided Manufacturing (CAD-CAM) technology has emerged as a game-changer, revolutionizing the way dental restorations are designed and fabricated. In this article, we delve into the Germany Dental CAD-CAM market, exploring its significance, trends, and impact on dental practices across the country.
Dental CAD-CAM technology integrates computer software and hardware to design and manufacture dental restorations, including crowns, bridges, veneers, and dental implants, with unparalleled precision and accuracy. By digitizing the traditional dental laboratory workflow, CAD-CAM systems enable dentists and dental technicians to create customized restorations that fit seamlessly within a patient's oral anatomy, ensuring optimal aesthetics, comfort, and functionality.
One of the key advantages of Dental CAD-CAM technology is its ability to streamline the dental restoration process, reducing turnaround times and eliminating the need for multiple appointments. With CAD-CAM systems, dental professionals can capture digital impressions of a patient's teeth using intraoral scanners, design virtual restorations on a computer screen, and fabricate final restorations chairside or in a dental laboratory using computer-controlled milling machines or 3D printers.
Request the sample copy of report @ https://www.globalinsightservices.com/request-sample/GIS24743
Moreover, Dental CAD-CAM technology offers significant benefits in terms of restoration accuracy and longevity. By eliminating the human error associated with traditional manual fabrication techniques, CAD-CAM systems produce restorations with precise marginal fit, occlusal alignment, and contouring, resulting in superior clinical outcomes and patient satisfaction. Additionally, CAD-CAM materials such as zirconia, lithium disilicate, and resin-based composites offer excellent strength, durability, and biocompatibility, ensuring long-lasting restorations that withstand the rigors of daily oral function.
In recent years, there has been a growing demand for Digital Dentistry solutions, including CAD-CAM technology, driven by advancements in digital imaging, materials science, and software algorithms. Dental practices across Germany are increasingly adopting CAD-CAM systems to enhance their clinical workflows, improve treatment outcomes, and differentiate themselves in a competitive market. Moreover, the COVID-19 pandemic has accelerated the adoption of Digital Dentistry solutions, as dental professionals seek to minimize patient contact and enhance infection control protocols while maintaining high-quality care.
Furthermore, the Germany Dental CAD-CAM market is characterized by ongoing innovation and collaboration between dental equipment manufacturers, software developers, and dental professionals. Manufacturers are investing in research and development to improve system capabilities, enhance user experience, and expand the range of materials compatible with CAD-CAM workflows. Additionally, software developers are integrating artificial intelligence (AI) and machine learning algorithms into CAD-CAM software to automate design processes, optimize material selection, and improve restoration quality and consistency.
In conclusion, Dental CAD-CAM technology represents a transformative force in modern dentistry, offering precision, efficiency, and customization that were previously unimaginable. In Germany, CAD-CAM systems have become indispensable tools for dental practices seeking to deliver high-quality restorative care while maximizing patient comfort and satisfaction. By embracing innovation, collaboration, and digital transformation, the Germany Dental CAD-CAM market is poised for continued growth and advancement, shaping the future of dental technology and patient care.
0 notes
Text
Dental Laboratories Market: A Comprehensive Analysis of Growth Trends
Introduction
The global healthcare industry is witnessing unprecedented transformation, fueled by technological innovations, shifting demographics, and evolving consumer preferences. Within this dynamic landscape, the dental industry stands out as a sector experiencing significant growth and change. Dental laboratories, which play a crucial role in the fabrication of dental prosthetics and restorations, are at the forefront of this evolution.
Request for a sample, here: https://www.nextmsc.com/dental-laboratories-market/request-sample
According to a study by Next Move Strategy Consulting, the global Dental Laboratories Market size is predicted to reach USD 45.84 billion with a Compound Annual Growth Rate (CAGR) of 5.9% by 2030. This forecast underscores the remarkable growth trajectory expected within the dental industry, highlighting the increasing demand for dental laboratory services worldwide.

In this comprehensive analysis, we will delve deeper into the growth trends shaping the dental laboratories market, exploring key drivers, challenges, and opportunities. From technological advancements to demographic shifts and changing consumer preferences, we will examine the factors driving growth and transformation within the dental laboratory industry.
Technological Advancements Fueling Innovation
Technological innovation has emerged as a primary catalyst driving growth in the dental laboratories market. In recent years, the advent of digital dentistry has revolutionized the way dental prosthetics are designed, manufactured, and delivered. Computer-Aided Design/Computer-Aided Manufacturing (CAD/CAM) technology, 3D printing, and intraoral scanning systems have transformed traditional workflows, enabling precision customization, faster turnaround times, and enhanced patient outcomes.
CAD/CAM technology allows dental technicians to digitally design prosthetic restorations with unparalleled precision and accuracy. These digital designs are then translated into physical restorations using computer-controlled milling machines or 3D printers. This digitization of the manufacturing process not only improves the quality and consistency of dental prosthetics but also reduces production time and costs.
Similarly, intraoral scanning systems have replaced traditional impression techniques, allowing dentists to capture highly accurate digital impressions of patients' teeth and oral tissues. These digital impressions can be seamlessly integrated into CAD/CAM workflows, facilitating the fabrication of precise, custom-fitted restorations with minimal patient discomfort.
Furthermore, advancements in materials science have expanded the range of available materials for dental prosthetics, offering improved aesthetics, durability, and biocompatibility. From zirconia and lithium disilicate ceramics to high-performance polymers and composite resins, dental laboratories now have access to a diverse array of materials to meet the diverse needs and preferences of patients.
Rising Demand for Aesthetic Dentistry
In addition to technological advancements, there has been a significant increase in demand for aesthetic dentistry procedures worldwide. In today's image-conscious society, patients are increasingly seeking dental restorations that not only restore function but also enhance the appearance of their smiles. This trend has led to a surge in orders for veneers, crowns, bridges, and other cosmetic dental solutions, driving revenue growth for dental laboratories specializing in aesthetic dentistry.
Advancements in materials and technology have played a crucial role in meeting the growing demand for aesthetic dental restorations. Tooth-colored ceramic materials, such as lithium disilicate and zirconia, offer superior aesthetics and translucency, closely mimicking the natural appearance of teeth. CAD/CAM technology allows for precise customization and shade matching, ensuring seamless integration with patients' existing dentition.
Moreover, the rise of social media and celebrity culture has heightened awareness of dental aesthetics, prompting more individuals to seek cosmetic dental treatments to achieve the perfect smile. From Hollywood celebrities to social media influencers, the desire for a radiant, flawless smile has become increasingly prevalent, driving demand for cosmetic dental procedures and, consequently, dental laboratory services.
Aging Population Driving Restorative Dentistry
The global demographic shift towards an aging population has significant implications for the dental laboratories market. As individuals age, they are more susceptible to dental conditions such as tooth decay, gum disease, and tooth loss, necessitating restorative dental treatments. Consequently, there is a growing need for dental prosthetics, implants, and dentures, driving demand for laboratory-fabricated restorations.
The aging population is particularly pronounced in developed economies, where advancements in healthcare and lifestyle factors have contributed to increased life expectancy. In the United States, for example, the baby boomer generation—those born between 1946 and 1964—is entering retirement age in large numbers, leading to a surge in demand for dental services, including restorative dentistry.
Furthermore, the prevalence of chronic conditions such as diabetes and cardiovascular disease, which are known risk factors for oral health problems, further underscores the importance of restorative dental care among older adults. Dental laboratories play a critical role in providing customized, durable prosthetic solutions to restore oral function and improve quality of life for aging individuals.
Shift Towards Outsourcing Dental Laboratory Services
In recent years, there has been a noticeable trend among dental practitioners towards outsourcing laboratory services rather than investing in in-house facilities. Outsourcing offers several advantages, including cost savings, access to specialized expertise, and streamlined workflow management. Dental laboratories have capitalized on this trend by offering a wide range of outsourcing solutions tailored to the needs of dental practices, thereby expanding their market reach and revenue potential.
Inquire before buying, here: https://www.nextmsc.com/dental-laboratories-market/inquire-before-buying
Outsourcing dental laboratory services allows dentists to focus on patient care and clinical activities without the burden of managing laboratory operations. By partnering with reputable dental laboratories, dentists can ensure high-quality, consistent results for their patients while optimizing practice efficiency and profitability. Moreover, outsourcing enables dental practices to access a broader range of services and expertise than would be feasible to maintain in-house.
For dental laboratories, outsourcing represents a significant growth opportunity, allowing them to leverage economies of scale, invest in advanced technologies, and expand their service offerings. By establishing collaborative partnerships with dental practices, laboratories can foster long-term relationships based on trust, reliability, and mutual success. This shift towards outsourcing is expected to drive further consolidation within the dental laboratories market as larger players seek to capitalize on economies of scale and geographic expansion.
Challenges and Opportunities
Despite the promising growth prospects, the dental laboratories market faces certain challenges that warrant attention. Regulatory compliance, for example, remains a key concern, particularly in light of increasing scrutiny and oversight from regulatory authorities. Dental laboratories must ensure compliance with stringent quality standards, infection control protocols, and privacy regulations to safeguard patient health and confidentiality.
Furthermore, reimbursement issues pose a significant challenge for dental laboratories, particularly in markets with complex and fragmented healthcare systems. Reimbursement rates for dental prosthetics and laboratory services vary widely depending on factors such as insurance coverage, payer policies, and regional differences in pricing. Navigating this reimbursement landscape requires careful negotiation, documentation, and coding practices to ensure fair compensation for services rendered.
Moreover, dental laboratories face stiff competition from overseas manufacturers and outsourcing providers, particularly in regions with lower labor costs and less stringent regulatory requirements. To remain competitive, dental laboratories must differentiate themselves through superior quality, innovation, and customer-centric services. Embracing digital technologies, investing in staff training, and adopting lean manufacturing practices can help laboratories enhance efficiency, reduce costs, and deliver value-added services to customers.
Despite these challenges, the dental laboratories market presents numerous opportunities for growth and expansion. The increasing prevalence of dental disorders and oral health issues, coupled with rising consumer awareness and disposable income, is driving demand for dental laboratory services worldwide. By capitalizing on emerging trends such as digital dentistry, aesthetic dentistry, and outsourcing, dental laboratories can position themselves for long-term success and sustainability.
Conclusion
In conclusion, the dental laboratories market is poised for significant growth in the coming years, driven by technological advancements, changing consumer preferences, and demographic trends. Market players who can adapt to these evolving dynamics and capitalize on emerging opportunities will be well-positioned to thrive in this dynamic industry landscape. As the demand for dental laboratory services continues to rise, innovation and strategic partnerships will be key drivers of success in the pursuit of sustainable growth.
From CAD/CAM technology to aesthetic dentistry and outsourcing solutions, dental laboratories have a wealth of opportunities to explore and leverage in the quest to meet the evolving needs of dental practitioners and patients alike. By embracing innovation, fostering collaboration, and delivering value-added services, dental laboratories can play a pivotal role in advancing oral healthcare and improving patient outcomes worldwide.
As we look towards the future, it is clear that the dental laboratories market will remain a dynamic and competitive environment, characterized by continuous innovation, evolution, and growth. By staying abreast of industry trends, anticipating market demands, and embracing change, dental laboratories can navigate the complexities of the healthcare landscape and emerge as leaders in the delivery of high-quality, patient-centered dental prosthetics and restorations.
#dentallaboratories#dentalcare#healthcare#biotechnology#diagnostics#market research#markettrends#business insights
0 notes
Text
Zygomatic Implants: A Revolutionary Solution for Dental Restoration
Outline:
Introduction to Zygomatic Implants
Definition and purpose
Brief history
Advantages over traditional implants
Understanding Zygomatic Implants
Anatomy of the zygomatic bone
How zygomatic implants work
Candidates for zygomatic implants
Procedure for Zygomatic Implants
Pre-operative assessments
Surgical techniques
Post-operative care
Benefits of Zygomatic Implants
Immediate results
Reduced need for bone grafting
Improved stability and durability
Risks and Complications
Potential complications
How to minimize risks
Comparing Zygomatic Implants with Traditional Implants
Differences in procedure
Long-term outcomes
Cost of Zygomatic Implants
Factors affecting cost
Insurance coverage
Choosing the Right Provider
Qualifications and experience
Patient reviews and testimonials
Frequently Asked Questions (FAQs)
How long do zygomatic implants last?
Are zygomatic implants suitable for everyone?
Is the procedure painful?
Can zygomatic implants be used for full mouth restoration?
How much downtime is expected after the surgery?
Zygomatic Implants: A Revolutionary Solution for Dental Restoration
Dental implants have transformed the field of dentistry, providing patients with a reliable and durable solution for tooth replacement. However, traditional implants may not be suitable for everyone, especially those with severe bone loss in the upper jaw. In such cases, zygomatic implants offer a revolutionary alternative, providing stability and support even in the absence of adequate bone structure.
Understanding Zygomatic Implants
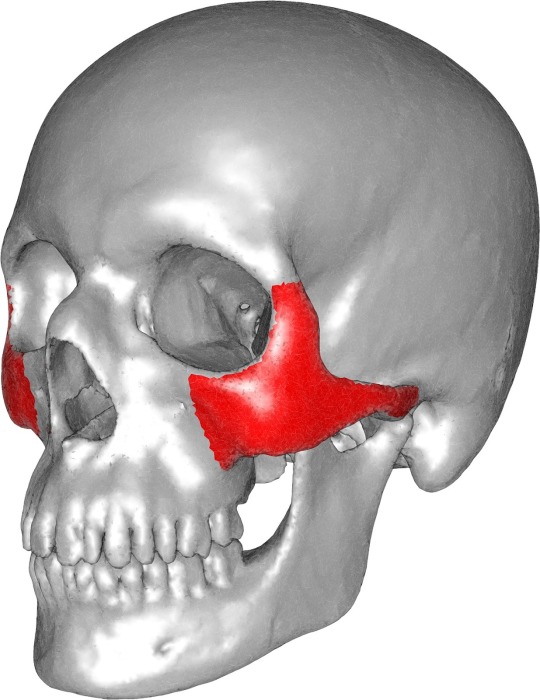
Zygomatic implants, also known as zygoma implants or zygomaticomaxillary implants, are a type of dental implant designed to anchor to the zygomatic bone, or cheekbone. Unlike traditional implants that are anchored into the jawbone, zygomatic implants utilize the dense bone structure of the cheekbone for support.
The zygomatic bone extends from the cheek to the area near the orbit of the eye, providing a strong foundation for dental implants. This makes zygomatic implants an ideal solution for patients who have experienced significant bone loss in the upper jaw due to conditions such as periodontal disease or trauma.
Procedure for Zygomatic Implants
The procedure for placing zygomatic implants typically involves a comprehensive assessment of the patient's oral health and bone structure. Advanced imaging techniques such as CT scans may be used to evaluate the condition of the jawbone and identify the optimal placement of the implants.
Surgical placement of zygomatic implants is performed under local or general anesthesia, depending on the patient's preference and the complexity of the procedure. The implants are strategically placed into the zygomatic bone through small incisions made in the gum tissue. In some cases, additional procedures such as bone grafting may be performed to enhance the stability of the implants.
After the implants are securely in place, temporary prosthetic teeth may be attached to provide immediate functionality and aesthetics. Once the implants have fully integrated with the surrounding bone, permanent prosthetic teeth are fabricated and attached to the implants, restoring the patient's ability to chew, speak, and smile with confidence.
Benefits of Zygomatic Implants
Zygomatic implants offer several advantages over traditional implants, making them an attractive option for patients with complex dental needs:
Immediate Results:
Unlike traditional implants that require months of healing before prosthetic teeth can be attached, zygomatic implants allow for immediate loading, meaning that temporary teeth can be attached on the same day as the surgery.
Reduced Need for Bone Grafting:
Because zygomatic implants utilize the dense bone of the cheekbone for support, there is often no need for bone grafting procedures, reducing overall treatment time and complexity.
Improved Stability and Durability:
The anchorage provided by the zygomatic bone results in superior stability and durability compared to traditional implants, minimizing the risk of implant failure and ensuring long-term success.
Risks and Complications
While zygomatic implants are generally safe and effective, like any surgical procedure, there are potential risks and complications that patients should be aware of. These may include infection, nerve damage, sinus issues, and implant failure. However, these risks can be minimized by choosing a qualified and experienced dental provider and following post-operative care instructions diligently.
Comparing Zygomatic Implants with Traditional Implants
While both zygomatic implants and traditional implants offer effective solutions for tooth replacement, there are some key differences between the two procedures. Traditional implants require a sufficient amount of healthy jawbone for successful placement, whereas zygomatic implants can be used even in cases of severe bone loss. Additionally, zygomatic implants often provide faster results and require fewer surgical procedures compared to traditional implants.
Cost of Zygomatic Implants
The cost of zygomatic implants varies depending on several factors, including the number of implants required, the complexity of the procedure, the geographic location of the dental provider, and whether additional procedures such as bone grafting are necessary. While zygomatic implants may initially seem more expensive than traditional implants, they offer significant long-term benefits and can ultimately be a cost-effective solution for patients with complex dental needs. Some dental insurance plans may cover a portion of the cost of zygomatic implants, so it's important to check with your provider to understand your coverage options.
Choosing the Right Provider
When considering zygomatic implants, it's essential to choose a qualified and experienced dental provider who specializes in implant dentistry. Look for a provider who has undergone extensive training in the placement of zygomatic implants and who has a track record of successful outcomes. Reading patient reviews and testimonials can also help you evaluate the quality of care provided by a dental practice and ensure that you are making an informed decision about your dental health.
Conclusion
Zygomatic implants offer a revolutionary solution for patients with complex dental needs, providing stability, functionality, and aesthetics even in cases of severe bone loss in the upper jaw. By understanding the benefits, risks, and considerations associated with zygomatic implants, patients can make informed decisions about their dental health and regain confidence in their smiles.
Frequently Asked Questions (FAQs)
How long do zygomatic implants last?
Zygomatic implants are designed to be a permanent solution for tooth replacement and can last a lifetime with proper care and maintenance.
Are zygomatic implants suitable for everyone?
While zygomatic implants offer significant benefits for patients with severe bone loss in the upper jaw, they may not be suitable for everyone. It's essential to undergo a thorough evaluation with a qualified dental provider to determine if you are a candidate for zygomatic implants.
Is the procedure painful?
The procedure for placing zygomatic implants is performed under anesthesia, so patients typically do not experience pain during the surgery. Some discomfort and swelling may occur during the recovery period, but this can be managed with pain medication prescribed by your dental provider.
Can zygomatic implants be used for full mouth restoration?
Yes, zygomatic implants can be used to replace multiple missing teeth and provide support for full mouth restoration procedures.
How much downtime is expected after the surgery?
While recovery times can vary depending on the individual patient and the complexity of the procedure, most patients can expect to resume normal activities within a few days to a week after surgery.
0 notes
Text
Dotta Dental - Leading Supplier of Zirconia Milling Machine | CAD CAM System Supplier

Explore Dotta Dental, the professional CAD CAM system supplier offering top-quality zirconia milling machines. Enhance your dental practice with our one-stop shopping experience for dental milling machines, 3D scanners, 3D printers, and furnaces. Elevate your dental CAD CAM system with Dotta Dental today.
0 notes
Text
Revolutionizing Dentistry: Innovative Technology and Materials in Modern Partial
Introduction
In recent years, the field of dentistry has witnessed remarkable advancements in technology and materials, particularly in the realm of partial dentures. These advancements have revolutionized the way dental professionals approach tooth replacement, offering patients improved aesthetics, comfort, and functionality. From digital scanning and design to the development of cutting-edge materials, this article explores the innovative technologies and materials driving the evolution of modern Partial Dentures Timonium.
Digital Dentistry: Precision and Efficiency
One of the most significant advancements in modern dentistry is the integration of digital technologies throughout the treatment process. Digital scanning systems, such as intraoral scanners, have replaced traditional impressions, offering numerous benefits including increased accuracy, improved patient comfort, and streamlined workflow for dental professionals. With the ability to capture highly detailed 3D images of the oral cavity, digital scanning facilitates the precise design and fabrication of partial dentures.
Computer-Aided Design (CAD) and Computer-Aided Manufacturing (CAM) technologies have further enhanced the precision and efficiency of partial denture fabrication. CAD software enables dental technicians to digitally design custom prostheses that meet the unique anatomical and functional requirements of each patient. CAM systems, including 3D printers and milling machines, then translate these digital designs into physical restorations with unparalleled accuracy and consistency. This integration of digital technologies has revolutionized the production of partial dentures, offering patients superior fit and aesthetics compared to traditional methods.
Advanced Materials: Strength, Durability, and Aesthetics
In addition to technological advancements, the development of innovative materials has played a pivotal role in enhancing the performance and aesthetics of modern partial dentures. Traditional materials such as acrylic resin and metal alloys have been surpassed by newer options that offer superior strength, durability, and biocompatibility.
One of the most notable advancements in partial denture materials is the widespread adoption of high-performance polymers, such as thermoplastic resins. These materials combine the strength and durability of traditional acrylics with enhanced flexibility and fracture resistance, making them ideal for use in removable partial dentures. Thermoplastic resins also offer excellent aesthetics, as they can be color-matched to natural teeth for seamless integration with the patient's smile.
Another innovative material revolutionizing partial dentures is zirconia. Zirconia is a biocompatible ceramic material known for its exceptional strength and durability, making it an ideal choice for fabricating partial denture frameworks. Unlike traditional metal frameworks, zirconia restorations are lightweight, hypoallergenic, and highly resistant to corrosion and plaque accumulation. Additionally, zirconia can be milled with precision using CAD/CAM technology, ensuring optimal fit and comfort for the patient.
Furthermore, the emergence of nanotechnology has opened up new possibilities in dental materials science. Nanocomposites, which consist of nano-sized particles dispersed within a polymer matrix, offer improved mechanical properties and enhanced aesthetics compared to conventional materials. These advanced composites can be used to fabricate partial denture bases and teeth with superior strength, wear resistance, and lifelike appearance.
Patient-Centered Design: Comfort and Aesthetics
Beyond technological and material advancements, modern partial dentures are designed with a focus on patient-centered care, prioritizing comfort, functionality, and aesthetics. Digital design software allows dental professionals to customize the shape, size, and contour of partial dentures to ensure optimal fit and comfort for each patient. Additionally, advancements in 3D printing technology enable the fabrication of partial dentures with thin, lightweight structures that minimize bulkiness and improve patient comfort.
Aesthetics are also a key consideration in the design of modern partial dentures. With the ability to digitally simulate the final restoration, dental technicians can work closely with patients to achieve their desired aesthetic outcome, including natural-looking tooth shapes, colors, and translucency. Advanced materials such as zirconia and nanocomposites further enhance the aesthetic appeal of partial dentures, providing patients with restorations that closely resemble natural teeth.
Conclusion
Innovative technology and materials have revolutionized the field of Partial Dentures Timonium., offering patients and dental professionals unprecedented levels of precision, durability, and aesthetics. Digital scanning and design technologies have improved the accuracy and efficiency of partial denture fabrication, while advanced materials such as thermoplastic resins, zirconia, and nanocomposites have enhanced the strength, durability, and aesthetics of these prostheses. By embracing these advancements, dental professionals can provide patients with partial dentures that not only restore function but also enhance their quality of life and confidence in their smiles.
0 notes
Text
Achieve Precision and Efficiency with a Dental Crown Milling Machine
In the field of dentistry, technology continues to revolutionize dental procedures, providing accurate and efficient solutions for both dentists and patients. One such technological advancement is the Dental Crown Milling Machine. This cutting-edge equipment enables dental professionals to fabricate dental crowns with unmatched precision, convenience, and speed. In this blog post, we will explore the features and benefits of a Dental Crown Milling Machine, along with its price range, to highlight how it has transformed the dental industry.
What is a Dental Crown Milling Machine?
A Dental Crown Milling Machine, also known as a CAD/CAM milling machine, is a state-of-the-art equipment used in dental laboratories and clinics to fabricate dental crowns with exceptional accuracy and efficiency. It utilizes computer-aided design (CAD) and computer-aided manufacturing (CAM) technology to create precise dental restorations, including crowns, inlays, and onlays, from a variety of materials such as zirconia, lithium disilicate, and metal alloys.
Benefits of a Dental Crown Milling Machine
Enhanced Precision: Dental Crown Milling Machines offer unparalleled precision, ensuring that dental restorations fit seamlessly in patients' mouths. The CAD/CAM software allows for detailed customization, resulting in accurate and aesthetic dental crowns that blend seamlessly with the patient's natural teeth.
Time Efficiency: With a Dental Crown Milling Machine, the traditional process of manually fabricating dental crowns is streamlined. The machine automates many labor-intensive tasks, reducing the time required to create high-quality restorations. This enables dentists to provide faster treatment to patients, enhancing their overall experience.
Cost-Effectiveness: Although Dental Crown Milling Machines require an initial investment, they offer long-term cost savings. By eliminating the need for outsourcing crown fabrication to external dental laboratories, dentists can significantly reduce costs associated with laboratory fees and shipping expenses. Additionally, in-house production allows for better control over the quality of the final product.
Versatility: Dental Crown Milling Machines are compatible with a wide range of dental materials, including ceramics, composites, and metals. This versatility empowers dental professionals to select the most suitable material for each patient's unique needs, ensuring long-lasting and aesthetically pleasing dental restorations.
Dental Crown Milling Machine Price Range
The Dental Crown Milling Machine Price varies depending on factors such as brand, features, and specifications. Entry-level machines designed for smaller dental practices typically range from $15,000 to $30,000. These machines offer basic functionalities and are suitable for low to moderate case volumes.
Mid-range Dental Crown Milling Machines, which cater to medium-sized dental labs or busy practices, are priced between $30,000 and $60,000. These machines offer advanced features such as multiple axis milling, high-speed machining, and improved software capabilities.
High-end Dental Crown Milling Machines, designed for large dental laboratories and high-volume practices, can range from $60,000 to $100,000 or more. These machines provide cutting-edge technology, exceptional milling precision, and advanced automation features.
It is essential to consider factors such as reliability, support, warranty, and training when investing in a Dental Crown Milling Machine. Researching different brands and consulting with industry experts can help dentists make an informed decision based on their specific requirements and budget.
Conclusion
If you are the one looking for Dental Crown Milling Machine , look no further than Monumental Dental Engineering. The Dental Crown Milling Machine has revolutionized the field of dentistry by offering accurate, efficient, and cost-effective solutions for fabricating dental crowns. With its precision, time-saving capabilities, and compatibility with various materials, this advanced equipment has become an invaluable asset for dental professionals. While the price range may vary depending on the machine's features and specifications, the long-term benefits and increased patient satisfaction make it a worthwhile investment. By incorporating a Dental Crown Milling Machine into their practice, dentists can provide superior dental restorations and enhance the overall quality of care they deliver.
#dental machines#dental milling machines#cad-cam dental abutments#implant abutments#business#dental milling machine for sale#dental#marketing
1 note
·
View note
Text
What Is The Outstanding Characteristics for ZTA?
ZTA (Zirconia Toughened Alumina) is a composite material made from alumina and zirconia. It combines the outstanding characteristics of both materials.
Compared to conventional alumina, ZTA possesses superior hardness, higher flexural strength, and similar density. Compared to conventional zirconia, it possesses a lower coefficient of linear thermal expansion and higher thermal conductivity.
By leveraging these features, ZTA has been widely adopted in milling parts and wear-resistant parts that require cooling.

ZTA (Zirconia Toughened Alumina)
Features:
- High Stiffness and Outstanding Wear Resistance
- Stiffer than alumina with outstanding wear resistance equivalent to zirconia.
- High Thermal Conductivity and Low Thermal Expansion
- Suppresses thermal deformation through thermal conductivity and low thermal expansion equivalent to alumina. Suitable for components requiring a cooling Mechanism.
- High Strength and Specific Rigidity
- Approximately twice as strong as alumina and contributes to low-weight design through high specific rigidity.
Below is the material properties for ZTA:
Properties
Unit
ZTA ceramic
Zirconia Content
%
20%
Color
white
Volume density
g /cm3
4.1
Water Absorption
%
0
Crystal Size(Grain Size)
μm
5-6
Vickers Hardness, HV1.0
Gpa
≥15
Flexural Strength
Mpa
≥500
Coefficient of linear expansion
20-500℃
1x10-6mm/℃
6.5~7.5
20-800℃
6.5~8.0
Thermal conductivity
W/m·K( 20℃)
≥20.9
Specific Heat Capacity
KJ/(kg*K)
≥0.8
Dielectric Strength
KV/mm
≥9
Volume resistivity
Ω·cm 20℃
≥1014
Ω·cm 300℃
≥1011
Ω·cm 500℃
≥109
Dielectric Constant
1MHz
9-10
Tangent Of Dielectric Loss
1MHz
≤5x10-4
Surface Roughness
μm
0.1-0.4 after the machine
Read the full article
0 notes
Text


#grinding #zirconia #ball #beads #ceramic
Application: Ball Stirred mill, Stirred mill, Stripping machine, Polishing machine, Sand mill etc.
Company Website: www.wear-ceramic.com
Email:[email protected]
2 notes
·
View notes
Text
In vitro Comparison of Marginal Fit of Cad-Cam Zirconia, SMLS Co-Cr, Pressable Lithium Disilicate, and Cast Ni-Cr Copings - Juniper Publishers
In vitro Comparison of Marginal Fit of Cad-Cam Zirconia, SMLS Co-Cr, Pressable Lithium Disilicate, and Cast Ni-Cr Copings
Authored by Jitendra J Mete
Abstract
Context:Clinically acceptable marginal fit of crowns has been the focus of various investigations. There is limited literature comparing marginal accuracy CAD-CAM zirconia, SMLS Co-Cr, Pressable Lithium Disilicate, and cast Ni-Cr copings.
Aim:Evaluate and compare marginal accuracy of CAD-CAM zirconia, SMLS Co-Cr, Pressable lithium Disilicate, and cast Ni-Cr copings.
Methods and Material: Forty copings were fabricated (Ten each in Group I - CAD- CAM zirconia, Group II - SMLS Co-Cr, Group III - lithium disilicate, and Group IV- cast Ni-Cr copings) on a standardized stainless steel model with long chamfer finish line. Four areas around the tooth surface namely mesial (M), distal (D), buccal (B) and lingual (L) surfaces were digitally analyzed for marginal fit under the stereomicroscope.
Stastical Analysis: Comparison between groups was done by using one-way ANOVA test followed by a Post Hoc Tukey-Kramer multiple comparisons test.
Results: The mean marginal gap (in μm) for Group I on lingual, buccal, mesial and distal surface was 37.05, 38.54, 37.61 and 36.09 respectively. The mean marginal gap (in μm) of Group II on lingual, buccal, mesial and distal surface was 48.48, 50.88, 50.12, and 49.5 respectively. The mean marginal gap (in μm) of Group III on lingual, buccal, mesial and distal surface was 63.04, 64.07, 64.97 and 65.81 respectively. The mean marginal gap (in μm) of Group IV on lingual, buccal, mesial and distal surface was 75.68, 74.75, 73.86, and 72.78 respectively.
Conclusion: The marginal fit of CAD-CAM zirconia copings is more accurate as compared to SMLS Co-Cr, pressable lithium disilicate and cast Ni-Cr alloy copings on a standardized metal model.
Keywords: Marginal Gap; Stereomicroscope; CAD – CAM; Metal Laser Sintering; Pressable Ceramic
Abbreviations: SMLS: Selective Metal Laser Sintering; Co-Cr: Cobalt-Chromium Alloy; CAD: Computer Aided Designing; CAM: Computer Aided Manufacturing; CNC: Computer Numerically Controlled (CNC); HIP: Hot Isostatic Pressing.
Introduction
The success of a dental restoration is determined by 3 main factors: esthetic value, resistance to fracture, and marginal adaptation [1-5]. Inadequate marginal fit leads to cement dissolution, plaque accumulation, which increases the risk of carious lesions & periodontal diseases [6-11].
Traditionally metal copings have been fabricated by the lost wax technique and casting method. Inaccurate marginal fit of copings fabricated by this technique may result from contraction of impression material, distortion of wax patterns, or irregularities in the cast metal. Newly developed selective metal laser sintering (SMLS) technique uses a high power laser to fuse the small particles of metal into a mass that has a desired 3-dimensional shape. The laser selectively fuses powdered material by scanning cross-sections generated from the 3-dimensional digital description of the part (for example, from a CAD file or scan data) on the surface of the powder bed. SMLS is a CAD/CAM based technique in which frameworks and metal copings can be designed and fabricated using cobalt-chromium alloy (Co-Cr). Co-Cr powdered alloy used in this technique has slight variations in composition. The molybdenum content in the alloy powder used in SMLS is comparatively less than the alloy which is used for conventional casting. After each cross section is scanned, the powder bed is lowered by one-layer thickness and a new layer of material is applied on top. The process is repeated until the part is completed. Advantage of SMLS system include easy fabrication of complicated shapes and short working time due to elimination of the procedures of fabricating a wax pattern, investing, burning and casting works [12].
Development in ceramic materials such as lithium disilicate, and zirconium oxide cores, uses of hot press and CAD-CAM equipment have opened up new path for all ceramic restorations [13]. CAD-CAM not only provides reproducible results fulfilling certain standards but also reduces the errors arising from the technicians. However, it is associated with higher cost. When measuring the marginal gap after cementation, the same number of teeth or steel dies as that of restoration sample is needed to control the variables. On the other hand, only one tooth or steel die is needed if the measurement is done without a luting agent. Investigators have found a significant increase in the marginal discrepancy after cementation [14,15]. These results, however, varied according to the luting agent. The marginal fit was, therefore, measured without cementation for variable control in this study.
There is limited literature which compares marginal accuracy of CAD-CAM zirconia, SMLS Co-Cr, Pressable lithium disilicate, and cast Ni-Cr copings. So the present in vitro study was conducted to evaluate and compare the marginal accuracy of CAD-CAM zirconia, SMLS Co-Cr, Pressable lithium disilicate, and cast Ni-Cr copings.
Methods and Material
Fabrication of stainless steel master model
For fabricating a standardized master model, a typhodont mandibular first molar tooth was first scanned using threedimensional (3-D) computer-aided designing (CAD) software. After scanning of the mandibular first molar tooth, a uniform chamfer finish line of 1.2 mm in width, 6-degrees occlusal convergence, 1.5 mm reduction on functional cusps with functional cusp bevel and 1 mm reduction on non-functional cusps simulating a prepared mandibular first molar was carried out on the CAD software. A rectangular platform measuring 4 cm in length, 3 cm in breadth and base of thickness 2 cm made of stainless steel material was chosen for the purpose of milling. To fabricate a standardized master model consisting of a metal die exactly in the centre of the rectangular platform, computer-aided manufacturing (CAM) was carried out using the data obtained from the CAD software which was then transferred to the computer numerically controlled (CNC) milling machine (LAVA CNC 500) and engraving was done. After engraving, finishing and polishing of the master model was carried out. The stainless steel metal master model was used to fabricate all the copings and also to serve as an abutment for the measurement of marginal discrepancy.
Fabrication of CAD-CAM zirconia copings
A dental CAD/CAM system, 3M LAVA CAD/CAM system (3M ESPE Dental Products St. Paul, MN U.S.A) was used to fabricate the 10 zirconia copings used in this study. Metal model of the abutment was scanned using 3M Scanner. Scanned data were then converted into CAD data. Copings for all-ceramic crowns were designed using the dental wings supported by 3M software. No cement space was included for the margin, and 45 μm was used for the axial and occlusal surfaces of the abutment. Thickness of the copings were designed to be 0.5 mm. Design data were converted into processing data and sent to the processing machine (CNC 500 LAVA 3M).The zirconia blocks were cut and milled, and then the milled blocks were finally sintered to make zirconia copings. The internal surfaces & margins of the copings after placing on die were examined using a binocular loupe (HEINE HR-C 2.5x, HEINE, Herrsching, Germany) to check the complete seating.
Fabrication of Pressable lithium disilicate copings
Ten copings were fabricated from lithium disilicate glass ceramics (IPS e.max Press, Ivoclar Vivadent AG) using a combination of the lost-wax and heat-press techniques. Die lubricant (Isocera, Bego, Germany) was applied to the metal die. Wax patterns were fabricated on the dies using dip wax technique to form wax copings. The patterns were contoured parallel to the emergence profile and margins were manually sealed under 1.5×magnification.The thickness of the copings was confirmed with a thickness gauge (POCO 2N; Kroeplin, Schluchtern, Germany) to be 0.5mm. Finally, to re-adapt the margin, the pattern was reflowed completely through the wax over a band approximately 1mm wide with a well heated instrument, PKT No.1. Wax was then added to fill the depression, and when the pattern had cooled, the marginal excess was carved and the margin was burnished. Patterns were invested in phosphate bonded investment (IPS Press VEST Speed, Ivoclar Vivadent AG). After wax elimination glass ceramic ingots (HO 2, Ivoclar Vivadent AG) were plasticized at 9300C and vacuum pressed (EP 500 press furnace, Ivoclar Vivadent AG) into an investment mold. After a holding time of 25 min the pressed crowns were divested, separated and cleaned by applying 1% hydrofluoric acid (IPS e.max Press Invex Liquid, Ivoclar Vivadent AG) for 10 min. Internal surfaces were sandblasted with 100 μm aluminum oxide at 2 bar pressure. The internal surfaces of the copings were examined using a binocular loupe (HEINE HR-C 2.5x, HEINE, Herrsching, Germany) and any visible metal nodules were removed with water cooled diamond bur. To detect the invisible nodules or irregularities, the internal surfaces of the copings was checked on the master dies using vinyl poly-siloxane disclosing paste (Fit checker; GC Corporation). After removing the copings from the die, the contact spot, marked bythe indicator on the inside of the copings was examined visually using a binocular loupe (HEINE HR-C 2.5x, HEINE, Herrsching, Germany), these marked spots were removed until no internal binding was occurred and a uniform thickness of disclosing paste achieved. Finally, the copings were fitted to metal die. All copings were manufactured under supervision by the same dental technician.
Fabrication of cast Ni-Cr alloy copings
For making nickel-chromium (Ni-Cr) alloy copings, wax patterns were fabricated in similar way as for Pressable lithium disilicate copings. The wax patterns were invested with a phosphate-bonded investment (Bellabond Plus, Bego, Germany) and cast with Ni-Cr (Bellasun, Bego, Germany) alloy using an induction casting machine (LC Cast – 60, Confident equipments). After casting, the ring was bench cooled to room temperature and divested. The copings were sandblasted with 50-μm Al2O3 at 0.2- MPa air pressure to remove the investment. The internal surfaces of the copings were examined using a binocular loupe (HEINE HR-C 2.5x, HEINE, Herrsching, Germany) and any visible metal nodules were removed with a tungsten carbide bur (No. H71EF; Brasseler GmbH and Go KG). To detect the invisible nodules or irregularities, the internal surfaces of the copings was checked on the master dies using vinyl poly-siloxane disclosing paste (Fit checker; GC Corporation). After removing the crown from the die, the contact spot, marked by the indicator on the inside of the copings was examined visually using a binocular loupe (HEINE HR-C 2.5x, HEINE, Herrsching, Germany), these marked spots were removed until no internal binding was occurred and a uniform thickness of disclosing paste achieved. Finally, the restorations were fitted to metal die. All copings were manufactured under supervision by the same dental technician.
Every finished coping was placed on the prepared metal die and checked for complete seating after which it is evaluated for the marginal fit accuracy using a stereomicroscope (Wuzhou New Found Instrument Co. Ltd., China, Model Xtl 3400 E). During stereomicroscope evaluation copings were secured to master die model using vice holder. Stereomicroscopic images were analyzed using image analysis system (Chroma Systems Pvt. Ltd. India) and measurements for marginal gap were taken on deepest portion of copings on lingual, buccal, mesial and distal. Total 160 measurements were recorded of 40 copings, 10 of each four study groups. The mean and standard deviation of marginal gap of four Groups on lingual, buccal, mesial and distal surface was calculated. Tukey-Kramer multiple comparison test was applied for comparative evaluation of marginal fit in different groups.
Results
The mean ± SD marginal gap of Group I on lingual, buccal, mesial and distal surface was 37.05 ± 4.19, 38.54 ± 3.68, 37.61 ± 4.05 and 36.09 ± 4.18 respectively. The mean ± SD marginal gap of Group II on lingual, buccal, mesial and distal surface was 48.48 ± 5.99, 50.88 ± 6.0, 50.12 ± 5.91 and 49.5 ± 5.67 respectively. The mean ± SD marginal gap of Group III on lingual, buccal, mesial and distal surface was 63.04 ± 4.21, 64.07 ± 4.26, 64.97 ± 4.41 and 65.81 ± 4.49 respectively. The mean ± SD marginal gap of Group IV on lingual, buccal, mesial and distal surface was 75.68 ± 10.38, 74.75 ± 10.68, 73.86 ± 10.71 and 72.78 ± 10.61 respectively.
Tukey-Kramer multiple comparison tests was applied for comparative evaluation of marginal fit in different groups. The marginal fit of Group I on lingual, buccal, mesial, and distal surfaces as compared to Group II, Group III and Group IV was found to be statistically significant (p<0.001) (Table 1) & (Figures 1-3). The marginal fit of Group II on lingual, buccal, mesial, and distal surfaces as compared to Group III and Group IV was found to be statistically significant (p<0.001).The marginal fit of Group III on lingual, buccal, and mesial surfaces as compared to Group IV was found to be statistically significant (p<0.001).The marginal fit of Group III on distal surface as compared to Group IV was found to be statistically not significant (p>0.05).
Discussion
The ultimate goal of successful fixed partial denture (FPD) prosthesis can be achieved only when an accurate and precise marginal fit is produced. Microleakage and marginal openings are important causes of fixed restoration failures. One of the reasons for high microleakage is the amount of marginal gap, the increase of which causes greater microleakage, because the amount of cement exposed to oral fluids depend on the extent of the marginal gap [16].
Marginal discrepancies in the range of 40-120 μm have been reported to be clinically acceptable with regard to longevity of a restoration [17]. All the copings tested in this study are in the range of 35-80 μm, which is within acceptable limits. The different materials and applied techniques in the manufacturing of crown systems have significant effects on the strength of the final restoration as well as the marginal fit. Imperfect restoration margins offer recesses for adherence of oral bacteria, which may cause secondary caries and traumatic gingival irritation [18]. This in vitro study examined the marginal adaptation of four types of copings, consisting of frameworks fabricated using CAD/CAM zirconia, selective metal laser sintering (SMLS), pressable lithium disilicate and cast nickel-chromium (Ni-Cr) alloy. The marginal discrepancies of group CAD/CAM zirconia were significantly smaller compared to those of the other three study groups.
A stainless steel die was used for making copings and served as the abutment for the measurement of marginal discrepancy for all the copings made in this study. The advantages of the stainless steel die are standardized preparation and avoidance of wear of the die during the coping fabrication and measurements. The deep chamfer finish line preparation was selected because it meets the requirements for all the four study groups used in this study [19]. The majority of marginal discrepancy is known to develop during the oxidation cycle for metal copings [20]. This is often attributed to the release of residual stresses incurred during casting, grinding or polishing phases of the procedure. As the prostheses cools from the firing temperature, the difference in thermal contraction between the metal coping and the porcelain may result in additional marginal discrepancy [21].
The mean marginal gap widths of the CAD/CAM zirconia fabricated superstructures were significantly smaller than those of the selective metal laser sintered frameworks. This finding can be attributed to advancements in scanning technology, restorationdesigning software with improved margin detection and precision milling technologies. The vertical marginal gap values obtained were within the range of clinical acceptance i.e. 40 μm to 120 μm. The CAD/CAM zirconia system mills the framework with the final dimensions out of a densely sintered Y-TZP (Yittria stabilized Tetragonal Zirconia Polycrystals) blank which is fabricated with the ‘Hot Isostatic Pressing (HIP)’ technology. This technology involves sintering partially sintered zirconia material at a high temperature in a high density, homogenous zirconia material with improved mechanical properties [22]. For CAD/CAM ceramic crowns, marginal gaps of 17 μm to 118 μm have been reported by various authors [23]. Similar results were obtained in the present study.
However, a higher accuracy was achieved with the soft, partially sintered Y-TZP ceramics compared with the hot isostatic pressed (HIP) Y-TZP blocks. This finding can be attributed to the ease of machining and the precisely controlled sintering cycle in a specially designed sintering oven which aided in achieving a consistently accurate fit. The lesser accuracy of hard HIP-YTZP ceramics can be attributed to their extreme hardness and higher flexural strength (> 1,200 MPa), which can cause greater wear of the milling burs and a reduction in the efficiency of the milling unit consequently leading to lesser accuracy of fit. The Post Hoc comparison of both hard and soft types of ceramics showed no statistical significance, indicating that either form of Y-TZP ceramic produces clinically acceptable restorations. The comparable mechanical properties and the relative ease and speed of soft Y-TZP blank milling may explain why more operators choose this method to fabricate zirconia restorations, whereas only a small number prefer the hard Y-TZP blanks [24].
The results of the present study suggest that the new zirconia ceramic systems fabricated with CAD/CAM technology presents better marginal fit as compared to selective metal laser sintered copings. These results were in accordance with a study conducted by Ece Tamac et al. [25]. The results of this study shows that selective metal laser sintered copings shows better marginal fit than pressable lithium disilicate and cast Ni-Cr alloy copings. This finding can be attributed to the fact that additive manufacturing is used during selective metal laser sintered copings fabrication and this technique uses a high power laser to fuse small particles of metal into a mass that has a desired 3-dimensional shape. The laser selectively fuses powdered material by scanning crosssections generated from a 3-dimensional digital description of the part (for example from a CAD file or scan data) on the surface of a powder bed. After each cross-section is scanned, the powder bed is lowered by one-layer thickness, a new layer of material is applied on top and the process is repeated until the part is completed. These results are in accordance with Montero J. et al who concluded that selective metal laser sintering may be an alternative to vacuum-casting of base metals to obtain passivefitting implant-supported crown copings [26].
Glass-ceramics have superior stability, biocompatibility, esthetics, and chemical inertness, making them a viable alternative restorative material. Leucite-reinforced glass-ceramics were originally designed for CAD/CAM restorations because of their high durability and ability to be milled accurately. These ceramics are reinforced by the incorporation of leucite crystals into their structure, giving them improved toughness and strength [27]. In the present study, the leucite-reinforced glass-ceramic superstructures showed higher accuracy of marginal fit compared with the cast Ni-Cr superstructures.
IPS Empress Copings show less marginal gap than the conventionally casted Ni-Cr alloy copings. IPS Empress 2 (Ivoclar Vivadent, Schaan, Liechtenstein) is a lithium-disilicate glass ceramic (SiO2-Li2O) that is fabricated through a combination of the lost-wax and heat-pressed techniques. A glass-ceramic ingot of the desired shade is plasticized at 920°C and pressed into an investment mold under vacuum and pressure. Its predecessor, IPS Empress (Ivoclar Vivadent) is a leucite-reinforced glass ceramic (SiO2-Al2O3-K2O) which, due to its strength is limited in use to single unit complete-coverage restorations in the anterior segment. IPS Empress 2 has improved flexural strength by a factor of 3 over IPS Empress, can be used for 3-unit fixed partial dentures in the anterior area and can extend to the second premolar. The framework is veneered with fluoroapatite-based veneering porcelain (IPS Eris; Ivoclar Vivadent), resulting in a semi translucent restoration with enhanced light transmission. IPS e.max press (Ivoclar Vivadent) was introduced in 2005 as an improved press-ceramic material compared to IPS Empress 2. It also consists of a lithium-disilicate pressed glass ceramic, but its physical properties and translucency are improved through a different firing process [28]. Yeo IS et al. [29] concluded that the IPS Empress 2 systems showed the smallest and most homogeneous gap dimension, whereas the conventional In-Ceram system presented the largest and more variable gap dimensions compared with the metal ceramic restorations.
The conventionally casted Ni-Cr superstructures show more marginal gap when compared with the CAD/CAM superstructures. This finding can be attributed to the expansion and contraction associated with the impression materials, gypsum, wax pattern distortion during removal and the spruing process are other factors that may affect the accuracy of superstructures fabricated using the lost-wax process [30]. These results are in accordance with a study conducted by Tamer E. Shokry et al. [31] who concluded that titanium copings fabricated by CAD/CAM demonstrated the least marginal discrepancy among all groups, while the base metal (Ni-Cr) groups exhibited the most discrepancy of all groups tested.
It is difficult to interpret the statistical results of the previous studies because of variations in sample size, the measurement per specimen and the measurement methods used. There is no standardized method to measure the marginal fit. The most common methods are ‘direct viewing, sectioning, probing and explorative and visual examinations’ [32]. In the current study, the direct viewing of the crown on a die is used to measure the marginal fit of all the copings. Direct viewing has the advantage of being nondestructive and therefore applicable to clinical practice. The vertical cervical marginal gap measurement was selected as the most frequently used to quantify the accuracy of fit of a restoration [33].
Conclusion
Within the limitations of the present study, following conclusions can be drawn:
The marginal fit of CAD/CAM zirconia copings is more accurate as compared to selective metal laser sintered (SMLS), pressable lithium disilicate and cast Ni-Cr alloy copings on a standardized metal master model.
Base metal alloy (Ni-Cr) exhibited a discrepancy that was significantly higher than the rest of the groups.
The marginal discrepancies of all the copings were within the clinically acceptable range of 80-120 μm.
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com
For more articles in Open Access Journal of Dentistry & Oral Health please click on: https://juniperpublishers.com/adoh/classification.php
To know more about Peer Review Journal of Dentistry & Oral Health
1 note
·
View note