Text
Shoulder Surgery: Restoring Mobility and Relieving Pain
Shoulder surgery is a medical procedure that can bring relief to individuals experiencing a range of shoulder-related issues, from chronic pain to injuries and degenerative conditions. In this article, we'll explore the various aspects of shoulder surgery, its common types, and what patients can expect during the process.

Common Types of Shoulder Surgery:
Rotator Cuff Repair: Rotator cuff tears are a prevalent cause of shoulder pain. Surgery involves stitching or reattaching the torn tendons to restore function.
Labrum Repair: The labrum is a cartilage ring that stabilizes the shoulder joint. Surgery may be needed to repair labral tears, often caused by overuse or injury.
Shoulder Arthroscopy: This minimally invasive technique allows surgeons to diagnose and treat various shoulder conditions, including rotator cuff tears, impingement, and loose cartilage.
Shoulder Replacement: In cases of severe joint damage due to arthritis or injury, total or partial shoulder replacement surgery can alleviate pain and restore mobility.
Preparing for Surgery:
Consultation with an orthopedic surgeon is the first step. The surgeon will evaluate your condition, discuss surgical options, and provide pre-operative instructions.
Pre-operative preparations may include fasting before surgery, discontinuing certain medications, and arranging for post-operative care.
The Surgical Procedure:
Shoulder surgeries are typically performed under general anesthesia, ensuring you're comfortable and pain-free throughout the procedure.
Surgeons use specialized instruments to access and repair the affected area, often through small incisions, minimizing scarring.
Recovery and Rehabilitation:
Post-surgery, you'll spend time in a recovery area to monitor vital signs and manage any immediate discomfort.
Physical therapy is essential for regaining shoulder strength and range of motion. It helps prevent stiffness and ensures a quicker return to normal activities.
Recovery times vary depending on the type of surgery but generally range from a few weeks to several months.
Potential Risks and Complications:
Like any surgical procedure, shoulder surgery carries risks, including infection, bleeding, and adverse reactions to anesthesia.
Adhering to post-operative care instructions and attending follow-up appointments can help minimize these risks.
Long-Term Benefits:
Successful shoulder surgery can significantly improve your quality of life by reducing pain and restoring mobility.
Patients often regain the ability to perform daily activities, enjoy hobbies, and return to work without shoulder-related limitations.
REFERENCE:
TX Hospitals Group, Hyderabad is one of the country’s largest and fastest-growing chains of multi-super specialty hospitals.
CONTACT : 9089489089
Book an appointment now
0 notes
Text
Septoplasty: Breathing Easier and Living Better
Septoplasty is a surgical procedure designed to correct a deviated septum, the thin wall of cartilage and bone that separates the two nostrils in the nose. A deviated septum can result in various issues, including impaired breathing and chronic nasal congestion. In this article, we will explore the details of septoplasty, its benefits, the surgical process, and what patients can expect during recovery.
Understanding Septal Deviation
A deviated septum can be congenital or the result of injury. When the septum is not in the center of the nose, it can obstruct one or both nasal passages, causing breathing difficulties. Common symptoms of a deviated septum include chronic nasal congestion, snoring, difficulty breathing through one or both nostrils, and recurrent sinus infections. Septoplasty is a surgical solution aimed at alleviating these issues.
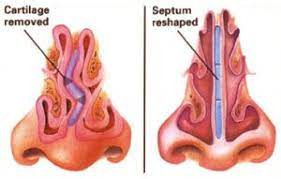
The Septoplasty Procedure
Septoplasty is typically performed as an outpatient procedure, meaning patients can go home the same day. It can be done under local or general anesthesia, depending on the patient's preference and the surgeon's recommendation. During the procedure:
An incision is made inside the nostril to access the deviated septum.
The surgeon carefully lifts the mucous membrane covering the septum.
The deviated or displaced cartilage and bone are then reshaped or removed.
The mucous membrane is repositioned over the corrected septum, and the incision is closed with absorbable sutures.
The goal of septoplasty is to straighten the septum and improve airflow through the nostrils, thus alleviating breathing difficulties.
Recovery and Results
After septoplasty, patients can expect some discomfort, swelling, and nasal congestion for a few days to a week. It's crucial to follow post-operative instructions, which may include using saline nasal sprays, avoiding strenuous activities, and refraining from blowing the nose forcefully. Most patients can resume regular activities within a week, but complete healing may take a few weeks to several months.
The results of septoplasty can be life-changing for individuals who have struggled with nasal obstruction and breathing issues. Improved airflow can lead to better sleep quality, reduced snoring, and decreased susceptibility to sinus infections. Many patients report feeling more energetic and better able to concentrate after septoplasty.
REFERENCE:
TX Hospitals Group, Hyderabad is one of the country’s largest and fastest-growing chains of multi-super specialty hospitals.
CONTACT : 9089489089
Book an appointment now
0 notes
Text
Coronary Artery Bypass Grafting in Hyderabad
0 notes
Text
Sebaceous Cyst: Understanding, Treatment, and Prevention
A sebaceous cyst, also known as an epidermal cyst, is a common benign growth that develops beneath the skin. These cysts typically occur when a hair follicle becomes blocked, leading to the accumulation of keratin, a protein found in skin cells. Sebaceous cysts can occur anywhere on the body but are most commonly found on the face, neck, back, or chest. While usually harmless, they can become uncomfortable or unsightly, prompting individuals to seek treatment.
Characteristics of Sebaceous Cysts:
Sebaceous cysts are typically small, round, and firm to the touch.
They often appear as a raised bump or lump just beneath the skin's surface.
The cysts are usually painless unless they become infected or inflamed.
In some cases, a sebaceous cyst may drain a thick, yellowish, foul-smelling substance.
Treatment Options:
Watchful Waiting: Many sebaceous cysts do not require treatment and may resolve on their own. However, if a cyst becomes painful, infected, or cosmetically bothersome, medical attention is necessary.
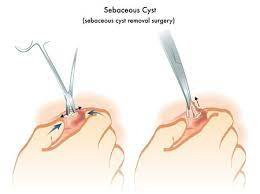
Incision and Drainage: A healthcare provider can perform a minor procedure to drain the contents of an inflamed or infected cyst. Local anesthesia is typically administered to minimize discomfort.
Excision: Surgical removal of the cyst may be recommended to prevent recurrence or address larger or more problematic cysts. This procedure is often performed under local anesthesia.
Laser Therapy: Laser treatment may be an option for some sebaceous cysts, especially if they are small and not deeply embedded in the skin.
Prevention and Home Care:
While it may not always be possible to prevent sebaceous cysts, there are steps individuals can take to minimize the risk of developing them:
Maintain good hygiene by washing the skin regularly.
Avoid squeezing or picking at any skin lesions to reduce the risk of infection.
Manage acne or other skin conditions that may contribute to cyst formation.
Protect the skin from trauma or injury that could lead to blocked hair follicles.
REFERENCE:
TX Hospitals Group, Hyderabad is one of the country’s largest and fastest-growing chains of multi-super specialty hospitals.
CONTACT : 9089489089
Book an appointment now
0 notes
Text
Rotator Cuff Surgery: Procedure, Recovery, and Expectations
Rotator cuff surgery is a medical procedure performed to repair a damaged or torn rotator cuff, a group of tendons and muscles that surround the shoulder joint. These injuries can result from overuse, trauma, or the natural aging process. When conservative treatments like physical therapy and medications fail to alleviate symptoms and restore shoulder function, surgery may be recommended. In this article, we will delve into the rotator cuff surgery procedure, the recovery process, and what patients can expect.
Procedure:
Preparation: Rotator cuff surgery is typically performed under general anesthesia, which ensures the patient is unconscious during the procedure. Occasionally, regional anesthesia or a combination of both may be used.
Access: The surgeon makes small incisions in the shoulder area to access the damaged rotator cuff.
Tendon Repair: Depending on the extent of the injury, the surgeon may reattach the torn tendon to the bone using sutures or anchors. In cases where the tendon is severely damaged and cannot be reattached, a graft may be used to reinforce the repair.
Acromioplasty: Sometimes, the surgeon may perform an acromioplasty, a procedure to remove a small part of the acromion (a bone at the top of the shoulder blade). This can help create more space for the rotator cuff tendons.
Closure: The incisions are closed with sutures or staples, and a sterile dressing is applied.
Recovery:
Recovery from rotator cuff surgery is a gradual process that may vary depending on the extent of the repair and the patient's overall health. Here are some general aspects of the recovery process:
Pain Management: Pain and discomfort are common after surgery and are managed with prescribed pain medications.
Immobilization: Patients often need to wear a sling to immobilize the shoulder and protect the repair for a period specified by the surgeon.
Physical Therapy: Physical therapy is a crucial component of recovery. It helps restore shoulder strength and range of motion. Therapy usually begins a few weeks after surgery.
Activity Restrictions: Patients are advised to avoid activities that could stress the shoulder, such as lifting heavy objects or reaching overhead, during the initial phase of recovery.
Follow-Up Appointments: Regular follow-up appointments with the surgeon are essential to monitor healing and assess progress.
Return to Normal Activities: The timeline for returning to normal activities varies but may take several months. Patients should follow their surgeon's guidance on when it's safe to resume specific activities.
Expectations:
While rotator cuff surgery can significantly improve shoulder function and reduce pain, it's essential to have realistic expectations. Factors like the extent of the injury, age, overall health, and adherence to rehabilitation exercises can influence the outcome. Many patients experience substantial pain relief and functional improvement, but it may take time to regain full strength and range of motion.
REFERENCE:
TX Hospitals Group, Hyderabad is one of the country’s largest and fastest-growing chains of multi-super specialty hospitals.
CONTACT : 9089489089
Book an appointment now
0 notes
Text
Circumcision is a surgical procedure that involves the removal of the foreskin, a fold of skin covering the head of the penis. It is commonly performed for cultural, religious, or medical reasons. The surgery is typically done on newborns or infants, but it can also be performed on older individuals. It is a relatively simple and quick procedure, often done under local anesthesia for older patients or without anesthesia for infants. After the procedure, proper wound care and hygiene are essential during the healing process.
0 notes
Text
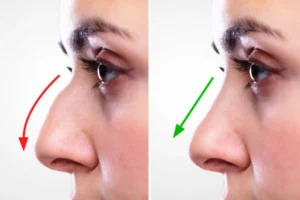
Rhinoplasty (Nose Job): Enhancing Aesthetics and Functionality
Rhinoplasty, commonly referred to as a "nose job," is a surgical procedure that focuses on reshaping and enhancing the appearance and functionality of the nose. It is one of the most popular cosmetic surgeries worldwide, sought after by individuals who want to improve their nasal aesthetics or correct breathing problems. In this article, we will explore what rhinoplasty entails, its primary goals, surgical techniques, and the recovery process.
Goals of Rhinoplasty:
Rhinoplasty can achieve several aesthetic and functional goals, including:
Improved Nasal Symmetry: Correcting asymmetry in the nose, such as uneven nostrils or a crooked bridge.
Nasal Size Reduction or Augmentation: Altering the size and proportion of the nose to create a more balanced facial appearance.
Nasal Tip Refinement: Reshaping the nasal tip to achieve a more refined or defined appearance.
Bridge Straightening: Correcting a dorsal hump or bump on the bridge of the nose.
Enhanced Breathing: Addressing structural issues within the nose to improve airflow and alleviate breathing difficulties.
Types of Rhinoplasty Procedures:
Rhinoplasty procedures can be categorized into two primary types:
Open Rhinoplasty: In this approach, an incision is made across the columella (the strip of skin between the nostrils) to provide a clear view of the nasal structures. Open rhinoplasty is often chosen for more extensive or complex nose reshaping.
Closed Rhinoplasty: This technique involves incisions made entirely inside the nostrils, providing less visibility but resulting in no external scarring. Closed rhinoplasty is typically chosen for less complex procedures or when minimal changes are required.
Recovery After Rhinoplasty:
Recovery following rhinoplasty varies from person to person and depends on the extent of the procedure. However, there are some common aspects of recovery:
Postoperative Swelling and Bruising: Swelling and bruising around the nose and eyes are common and typically peak within the first 48 hours. Cold compresses and head elevation can help reduce these symptoms.
Pain Management: Pain and discomfort are usually mild and can be managed with prescribed medications.
Nasal Packing and Splints: Patients may have nasal packing and splints in place immediately after surgery to support the newly shaped nose. These are typically removed within a week.
Return to Normal Activities: Most patients can return to work or school within a week or two, but strenuous activities should be avoided for a few weeks.
Follow-Up Appointments: Regular follow-up visits with the surgeon are essential to monitor healing, remove sutures or splints, and address any concerns.
Rhinoplasty can enhance facial harmony and self-confidence by reshaping the nose to meet the patient's aesthetic goals. It can also alleviate breathing difficulties associated with structural nasal issues. However, it's crucial to have realistic expectations and consult with a board-certified plastic surgeon or otolaryngologist who specializes in rhinoplasty to discuss your specific concerns and desired outcomes before undergoing the procedure.
REFERENCE:
TX Hospitals Group, Hyderabad is one of the country’s largest and fastest-growing chains of multi-super specialty hospitals.
CONTACT : 9089489089
Book an appointment now
0 notes
Text
Prostate Surgery: Understanding the Procedure, Risks, and Recovery
Prostate surgery is a medical procedure performed to address various prostate-related conditions, most commonly prostate cancer and benign prostatic hyperplasia (BPH). This surgery can significantly improve a patient's quality of life, but it's essential to understand the procedure, risks, and recovery process.
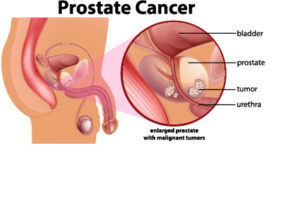
Prostate Surgery Procedures: There are several types of prostate surgery, each tailored to the specific condition and patient's needs. The most common procedures include:
Radical Prostatectomy: This surgery is primarily used to treat prostate cancer. It involves the removal of the entire prostate gland. Depending on the patient's condition, the surgeon may use traditional open surgery, laparoscopic techniques, or robot-assisted surgery.
Transurethral Resection of the Prostate (TURP): TURP is a minimally invasive procedure for BPH. A thin tube with a camera and cutting tool is inserted through the urethra to remove excess prostate tissue.
Transurethral Incision of the Prostate (TUIP): Similar to TURP, TUIP is used for BPH. However, instead of removing tissue, small incisions are made in the prostate to relieve pressure on the urethra.
Risks and Complications: Prostate surgery, like any surgical procedure, carries certain risks and potential complications. These may include:
Infection: There is a risk of infection at the surgical site or in the urinary tract.
Bleeding: Post-surgery bleeding can occur, requiring medical attention.
Urinary Incontinence: Temporary or permanent loss of bladder control can occur, especially after radical prostatectomy.
Erectile Dysfunction: This is a potential side effect of prostate surgery, particularly with radical prostatectomy, although techniques have improved to preserve nerve function.
Stricture: Narrowing of the urethra can lead to difficulty urinating.
Blood Clots: Clots can form in the legs or lungs, though this is relatively rare.
Recovery Process: Recovery after prostate surgery varies depending on the type of procedure performed. However, some general guidelines apply:
Hospital Stay: Patients may spend a few days in the hospital after radical prostatectomy, while minimally invasive procedures may allow for a shorter stay or even same-day discharge.
Pain Management: Pain and discomfort are common post-surgery. Medications are prescribed to manage pain.
Catheter Use: Patients often require a catheter to help with urination for a period after surgery.
Physical Activity: Gradual resumption of normal activities is encouraged, but heavy lifting and strenuous exercise should be avoided initially.
Follow-up Care: Regular follow-up appointments with the urologist are essential to monitor recovery and address any concerns.
REFERENCE:
TX Hospitals Group, Hyderabad is one of the country’s largest and fastest-growing chains of multi-super specialty hospitals.
CONTACT : 9089489089
Book an appointment now
0 notes
Text
Expert Cerebral Aneurysm Surgery in Hyderabad - Skilled surgeons providing advanced treatments for cerebral aneurysms. Book an appointment now.
0 notes
Text
Experience relief from hand pain with expert Carpal Tunnel Syndrome Surgery in Hyderabad. Book your consultation now!
0 notes
Text
Percutaneous Nephrolithotomy Surgery: A Minimally Invasive Approach to Kidney Stone Removal
Percutaneous nephrolithotomy (PCNL) is a surgical procedure designed to remove kidney stones that are large, complex, or located in challenging areas of the kidney. Kidney stones, also known as renal calculi, can cause severe pain and lead to complications if left untreated. PCNL offers an effective and minimally invasive solution for patients with such stones. In this article, we will explore what PCNL is, its indications, and what patients can expect from the procedure.
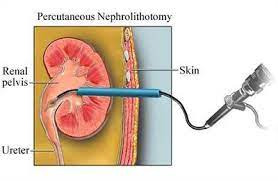
What is Percutaneous Nephrolithotomy (PCNL)?
PCNL is a minimally invasive surgical technique used to remove kidney stones through a small incision made in the patient's back. It is particularly suitable for larger stones that cannot be effectively treated with non-invasive methods like shock wave lithotripsy or ureteroscopy.
Indications for PCNL:
Large Kidney Stones: PCNL is most commonly used to treat large stones that are too big to pass on their own or are causing significant pain and obstruction.
Complex Stones: Stones that are irregularly shaped or located in challenging areas of the kidney may require PCNL for effective removal.
Stones Resistant to Other Treatments: If other treatments like lithotripsy or ureteroscopy have failed to break down or remove the stones, PCNL may be recommended.
The PCNL Procedure:
PCNL is typically performed under general anesthesia. During the procedure, the surgeon makes a small incision in the patient's back, just below the ribcage, to access the kidney. Using fluoroscopy or ultrasound guidance, a nephroscope is inserted through the incision and into the kidney. The surgeon then uses specialized instruments to break up and remove the kidney stones.
Once the stones are removed, a temporary drainage tube, known as a nephrostomy tube, is often placed to help drain urine and residual stone fragments. This tube is usually removed a day or two after the surgery. The incision is closed with stitches or adhesive strips.
Recovery and Results:
Recovery from PCNL can vary depending on the size and complexity of the stones and the patient's overall health. Most patients can expect to spend a day or two in the hospital after the procedure. Pain and discomfort are common during the initial recovery period and can be managed with medication.
The success rate of PCNL in completely removing kidney stones is high, and many patients experience significant relief from pain and improved kidney function following the procedure. However, like any surgical procedure, there are potential risks and complications, including bleeding, infection, and injury to surrounding organs.
REFERENCE:
TX Hospitals Group, Hyderabad is one of the country’s largest and fastest-growing chains of multi-super specialty hospitals.
CONTACT : 9089489089
Book an appointment now
0 notes
Text
Discover the cost of breast augmentation Surgery in Hyderabad and find experienced surgeons. Book a consultation now!
0 notes
Text
Percutaneous Nephrolithotomy Surgery: A Minimally Invasive Approach to Kidney Stone Removal
Percutaneous Nephrolithotomy (PCNL) is a surgical procedure used to remove large or complex kidney stones that cannot be treated effectively with non-invasive methods such as shock wave lithotripsy or ureteroscopy. PCNL involves accessing the kidney through a small incision in the back and is considered a highly effective and minimally invasive approach for kidney stone removal. In this article, we will explore PCNL, its indications, surgical process, recovery, and potential benefits.
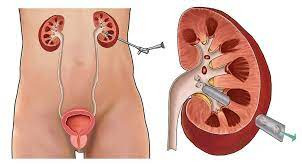
Understanding Kidney Stones: Kidney stones are hard mineral deposits that can form in the kidneys. These stones can vary in size and composition and can cause significant pain, urinary tract infections, and even kidney damage when left untreated. While smaller stones often pass naturally, larger or complex stones may require surgical intervention.
Indications for PCNL: PCNL is typically recommended when kidney stones meet one or more of the following criteria:
Size: Stones that are larger than 2 cm in diameter are difficult to pass naturally and are more effectively treated with PCNL.
Complexity: Stones that are irregularly shaped, located in a calyx deep within the kidney, or associated with anatomical abnormalities.
Failure of Other Treatments: Stones that have not responded to other treatments such as shock wave lithotripsy or ureteroscopy.
The PCNL Procedure: Percutaneous Nephrolithotomy involves the following key steps:
Anesthesia: The patient is placed under general or regional anesthesia to ensure comfort during the procedure.
Incision: A small incision (usually less than 1 cm) is made in the patient's back, typically in the area overlying the kidney where the stone is located.
Guidewire Insertion: A thin, flexible guidewire is inserted through the incision and directed into the kidney.
Dilation: A series of dilators are used to gently enlarge the access tract, creating a pathway to the stone.
Stone Removal: A nephroscope (a thin, tube-like instrument with a camera) is inserted through the access tract to visualize and remove the kidney stone using various tools, such as lasers, graspers, or ultrasonic devices.
Closure: Once the stone is completely removed, the access tract is often closed with a suture or adhesive.
Recovery and Benefits: Recovery from PCNL can vary based on factors like the size and complexity of the stone, but here are some general aspects of recovery:
Post-Op Care: After the procedure, patients typically stay in the hospital for a short period for observation. Pain and discomfort are managed with medications.
Return to Normal Activities: Most patients can return to normal activities within a few weeks, depending on the extent of the surgery.
Benefits: PCNL is highly effective in removing large or complex kidney stones, reducing pain, and preventing recurrent urinary tract infections. It can also help preserve kidney function.
Potential Risks: While PCNL is generally a safe procedure, there are some potential risks and complications, including bleeding, infection, injury to surrounding structures, and post-operative pain.
REFERENCE:
TX Hospitals Group, Hyderabad is one of the country’s largest and fastest-growing chains of multi-super specialty hospitals.
CONTACT : 9089489089
Book an appointment now
0 notes
Text
Looking for trusted bariatric surgery in Hyderabad? Discover top-notch bariatric surgeons and effective weight loss solutions. Contact us today for a consultation.
0 notes
Text
Myomectomy: Surgical Treatment for Uterine Fibroids
A myomectomy is a surgical procedure performed to remove uterine fibroids, which are noncancerous growths that develop in the wall of the uterus. This surgical option is chosen by many women who wish to preserve their fertility or avoid a hysterectomy, which involves the removal of the entire uterus. In this article, we will explore what a myomectomy entails, its purposes, the different techniques used, and what to expect during recovery.
Understanding Myomectomy:
A myomectomy is a surgical procedure designed to remove fibroids while leaving the uterus intact. Uterine fibroids, also known as leiomyomas or myomas, can vary in size and number and may cause symptoms such as heavy menstrual bleeding, pelvic pain, and pressure on nearby organs. Myomectomy is an excellent option for women who want to retain their reproductive capabilities or keep their uterus for personal reasons.
Purposes of Myomectomy:
Myomectomy is primarily performed for the following reasons:
Fertility Preservation: For women who wish to conceive and have uterine fibroids, myomectomy can remove the fibroids that may interfere with fertility.
Symptom Relief: Myomectomy can alleviate symptoms associated with fibroids, such as heavy menstrual bleeding, pelvic pain, and pressure on the bladder or rectum.
Different Myomectomy Techniques:
There are several techniques for performing myomectomy, and the choice of method depends on factors such as the size, number, and location of the fibroids, as well as the patient's overall health. The main approaches include:
Abdominal Myomectomy: This involves making an incision in the abdominal wall (usually a horizontal "bikini" incision) to access and remove the fibroids. It is commonly used for larger fibroids or when multiple fibroids are present.
Laparoscopic or Minimally Invasive Myomectomy: In this approach, small incisions are made in the abdomen, and a laparoscope (a thin, lighted tube with a camera) and specialized surgical instruments are used to remove the fibroids. This technique typically results in shorter recovery times and less scarring.
Hysteroscopic Myomectomy: This minimally invasive procedure is suitable for fibroids located inside the uterine cavity. A hysteroscope is inserted through the cervix into the uterus, and the fibroids are removed or shaved away.
Recovery and Postoperative Care:
Recovery from myomectomy varies depending on the type of procedure and individual factors. Here are some general guidelines for postoperative care:
Pain Management: Pain and discomfort are common after surgery, and pain medication may be prescribed.
Activity: Patients are typically advised to avoid strenuous activities and heavy lifting for a few weeks. The duration of recovery varies based on the surgical approach.
Fertility and Pregnancy: After myomectomy, women may need to wait for a certain period before attempting to conceive, depending on the type and extent of the procedure. It's essential to discuss fertility and pregnancy plans with a healthcare provider.
Follow-up: Regular follow-up appointments with the surgeon are crucial to monitor the healing process and discuss any concerns.
REFERENCE:
TX Hospitals Group, Hyderabad is one of the country’s largest and fastest-growing chains of multi-super specialty hospitals.
CONTACT : 9089489089
Book an appointment now
1 note
·
View note
Text
Looking for trusted bariatric surgery in Hyderabad? Discover top-notch bariatric surgeons and effective weight loss solutions. Contact us today for a consultation.
0 notes
Text
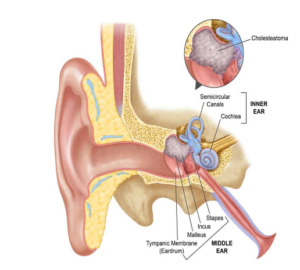
Mastoidectomy: Surgical Treatment for Mastoid Bone and Ear Infections
A mastoidectomy is a surgical procedure performed to remove infected or damaged tissue within the mastoid bone, located behind the ear. This procedure is commonly used to treat chronic ear infections that have spread to the mastoid air cells. Mastoidectomy can alleviate pain, prevent complications, and improve hearing for individuals with severe ear conditions.
Why Mastoidectomy is Needed
Mastoidectomy is typically recommended when other treatments, such as antibiotics or ear drops, fail to effectively treat chronic ear infections or when complications arise. Common indications for mastoidectomy include:
Chronic Otitis Media: Prolonged inflammation and infection of the middle ear can spread to the mastoid bone, leading to a condition known as mastoiditis.
Cholesteatoma: A cholesteatoma is an abnormal skin growth in the middle ear that can erode the mastoid bone, potentially causing hearing loss and other complications.
Abscess Formation: Infected pus can accumulate within the mastoid air cells, forming an abscess that requires surgical drainage.
The Mastoidectomy Procedure
During a mastoidectomy:
Anesthesia: The patient is placed under general anesthesia to ensure they are comfortable and pain-free during the procedure.
Incision: The surgeon makes an incision behind the ear to access the mastoid bone.
Bone Removal: The infected or damaged mastoid bone is carefully removed, creating a cavity.
Drainage and Cleaning: Any infected material, pus, or cholesteatoma is removed from the ear and mastoid area.
Closure: The incision is closed with sutures or staples.
Recovery and Rehabilitation
Recovery from mastoidectomy can vary depending on the extent of the procedure and the individual patient. Patients may experience some pain or discomfort after surgery, which can typically be managed with pain medications. It is essential to keep the surgical site clean and dry during the initial healing period. Patients are advised to follow their surgeon's instructions regarding ear care and follow-up appointments.
Benefits of Mastoidectomy
Mastoidectomy offers several benefits:
Infection Resolution: The procedure effectively removes the source of infection, preventing its spread and reducing the risk of complications.
Preservation of Hearing: In some cases, mastoidectomy can help preserve or improve hearing, especially when cholesteatoma or chronic infection has affected the structures of the ear.
Pain Relief: Patients often experience relief from the pain and discomfort associated with chronic ear infections.
REFERENCE:
TX Hospitals Group, Hyderabad is one of the country’s largest and fastest-growing chains of multi-super specialty hospitals.
CONTACT : 9089489089
Book an appointment now
0 notes