Text
A few days ago I turned 25, making this blog probably around 3 years old. I haven’t been updating much. However, my 22 year old self would have been excited about me graduating this year.
Forward to three years later, I will not be graduating this year.
I took a leave last July 10, 2017 as I suffered from a mental breakdown. At the time, my social anxiety disorder was just recently diagnosed and I was on Vortrioxetine for two weeks. And two weeks after that fateful day, I decided I’ll just take the year off and try my best to come back on the next academic year.
I can go on forever about my experience about how it’s like living with an anxiety disorder, but you’ve basically read so much about it. I am equally tired of explaining to everyone what I am going through.
But for the most part, I’m doing okay. I am actually eager about going back, to get this degree over and done (for now, at least) and finally pursue my dream -- which is to find my life somewhere other than in this place.
In the first few months of my period of depression I kept a separate tumblr blog for my depressive antics and I myself wouldn’t want to go back to any of that. It was pretty bad. Hey, I still get bad days especially when I am at my parents’. For the most part, I’m okay.
I have fallen in love once again with vintage style and fashion. I get weird looks but it makes me happy... in a weird way.
5 notes
·
View notes
Text
Give the ones you love wings to fly, roots to come back, and reasons to stay.
The Dalai Lama
3K notes
·
View notes
Quote
Just imagine becoming the way you used to be as a very young child, before you understood the meaning of any word, before opinions took over your mind. The real you is loving, joyful, and free. The real you is just like a flower, just like the wind, just like the ocean, just like the sun.
Don Miguel Ruiz (via lazyyogi)
2K notes
·
View notes
Text
Demoralisation.
We’ve talked a lot about demoralisation amongst doctors, but I think it’s not always easy to understand. Because we do love our jobs and we do want to help people. We want to love our jobs. We all started off desperately wanting to be doctors, and many of us do actually enjoy the doctoring bit. So why are we all so down? I’ll try to give you a taste. Imagine wanting to do something, to be someone so badly, that you spent your entire childhood and adolescence working singlemindedly towards it. You give it your everything, extra study, more tests, the works. Imagine being the smart kid at school, eager to work hard and impress, and being good at many things. Imagine being able to be nearly anything you could have wanted. Imagine spending the best years of your life stuck in revision whilst everyone around you was partying or dating or doing things that were fun. Imagine paying serious money for the privilege, and taking years out of your life to achieve it. Years studying. Years not working. Years of getting into debt when you could have been supporting yourself or your family. Imagine being so happy to graduate and finally be able to help people. Imagine your nervous, frenzied first attempts at being a doctor in the big bad world out there. Imagine the excitement of succeeding. Imagine missing friends’ weddings and relatives’ funerals because there was nobody else who could be there to keep your patients safe. Imagine having to make countless excuses to friends and to family and to partners. Imagine all the dates who decided “this is just too… complicated for me. Sorry.” Imagine losing touch with friends because you were always moving, always busy, and always tired. Sometimes they will understand, sometimes they won’t. Imagine all your friends working reasonable hours, earning a decent amount and having time to actually have some semblance of a life. Imagine rarely being able to see even the ones that understand and love you for who you are. Imagine starting to forget what it’s like to have a hobby or do something that isn’t work. Imagine starting to forget who you are, where your role ends and where your personhood begins. Imagine working long days and silly shifts only to come home and head straight for your books. For exams you struggle to pay yourself. Imagine being a single parent, and having to wonder whether you can afford to do this job because it’s so hard to get childcare. Imagine hearing your child say “You’re never home. I miss you” nearly every day. Imagine your partner telling you that you seem to be working more and more lately. Imagine feeling that you are neglecting your own loved ones in trying to keep everyone else’s safe. Imagine fearing that you will end up resenting the job you love, because it will have taken so much from your life. Imagine feeling forced to work another last minute shift because there was literally nobody else. Imagine gradually finding that more and more, every day was short staffed and busy. Imagine feeling that you aren’t giving your best care because you are stuggling just to get the urgent things done and keep patients safe. Imagine skipping meals and lack of sleep so often that it becomes normal. Imagine feeling like you can’t take sick leave because there is nobody else to kee people safe. Imagine things getting busier and busier until work is a nearly constant grind and you barely have time to think. Imagine nearly every day being a ‘major incident’. Imagine increasing pressure from all your colleagues. Imagine feeling unsupported by your seniors or your colleagues on a regular basis. Imagine being left to deal with difficult situations on your own. Imagine how hard it is to deal with grave situations, and how emotionally draining and heartbreaking it can be. Imagine patients and relatives who don’t see the pressure you are under. Imagine those who scream, yell, demand things are done right away or threaten to sue. Imagine those who are verbally abusive or violent. Imagine the ones that make all your colleagues cry, and from whom you have to hide your tears. Imagine how often your colleagues never report abuse because they don’t feel that they can. Imagine a context where failings are subjected to ‘trial by media’ and individuals are vilified, but the systemic failings which caused mistakes to happen are neither acknowledged nor addressed. Imagine a culture where doctors are under duty by the GMC to whistleblow, but given no legal protection if they do so. Imagine all your colleagues talking about considering leaving the profession. Imagine your colleagues who have already left telling you life is much better abroad or outside of medicine. Imagine nearly every speciality reporting recruitment shortages, bad morale and overwork. Imagine knowing that you are twice as likely to suffer from mental health problems or suicide. Imagine becoming more and more afraid that you will slip up due to tiredness. Imagine fearing the impact that this could have on your patients and their families, and how you might live with yourself. Imagine knowing that if you did, you would probably lose your job, but the employers and those who caused those conditions to happen would face no consequences. Imagine having to talk close friends off the ledge. Not just once, but on a regular basis. Imagine knowing that some people don’t succeed. Imagine knowing that this will only get worse if things deteriorate. Imagine your boss saying that you’re not doing enough. Imagine them saying that you all need to work more days. Imagine them saying that there just need to be more cuts. Imagine your employer having already cut so many things that everyone is always struggling. Imagine a context where services are not appropriately funded, and then individuals working within are blamed for predictable shortcomings which could have been avoided with appropriate funding and safeguards. Imagine fearing that instead of proper investment, those whose job it is to look after your healthcare system may be trying to privatise it for profit. Imagine wondering if your patients and your children will be able to afford healthcare in the future. Imagine your boss taking the safeguards away which limit how much time your employer can make you work. Imagine your boss reducing pay for the agency staff who are filling empty posts and keeping things afloat. Imagine being expected to work more hours, more weekends for less pay. Imagine the constant pressure to see more patients in less time, and being given less resources to look after them. Imagine knowing that you will probably work far longer than any rostered hours. Imagine knowing that your senior colleagues are fighting a similar battle and their conditions may be similarly affected. Imagine finding out how many of them can’t wait to retire, and remembering the days when doctors used to love working late into life. Imagine realising that you may not win this battle. Imagine your boss telling everyone they just don’t understand why you are all demoralised and telling everyone that you’re actually getting a pay rise and less hours. Imagine the public believing the lies. Imagine the media believing that everyone is demoralised because the union is telling us to be. Imagine the public telling you that you knew what you were getting into. Imagine the public telling you that you are overpaid, greedy, lazy, incompetent and ought to shut up and get back to work. Imagine the public telling you that the way your profession have chosen to voice your concerns (striking) is unacceptable, but not listening to any of the other ways your colleagues have tried to engage them. Imagine hearing over and over again that the system, which is underfunded compared to every other Western country, is ‘unsustainable’ when this is not true. Imagine just wanting to do your job and help people, but feeling bogged down in difficulties that should never be a part of your job. Imagine loving being a doctor but hating what it has become. Imagine fearing that situations may get so bad that you too may be forced to leave for your own sanity and health. This is why so many of my peers are demoralised.
1K notes
·
View notes
Text
friends, lemme share this little gem with you

FIRST! The inner flap:



oh dear indeed…



some people crayons are jerks.




:’(


:D

:D :D :D :D :D :D :D :’’’’) :’’’’’’’’)))))))))))



i just have a lot of feelings about this book and think everyone should own it
450K notes
·
View notes
Photo







Meme na Mindanaw (A lullabye for peace in Mindanao) by Albert Alejo
“Meme na, O Mindanaw Iduyan-duyan ko ikaw. Sa gubot di maminaw Aron dili ka mapukaw. Damguhon mo ang kalinaw Sa umaabot nga adlaw Ugma ipohon makalakaw Ngadto sa wala na’y mingaw. Ssshhh! Ayaw mo pagsaba Mapukaw ang bata! Ssshhh! Ayaw na mo pag-away Ang bata madamay! Damguhon mo ang kalinaw Sa umaabot nga adlaw Ugma pohon makalakaw Ngadto sa wala na’y mingaw Pasagdi ang bata intawon Magdamgo nga malinawon. Magmata na, O Mindanaw Ania na ang kalinaw.”
English:
Sleep now, my dear Mindanaw, I will cradle you to sleep, Don’t allow the fighting outside Awaken you from slumber. Dream, dream of peace In the coming days Tomorrow, who knows, you can walk To where there are no more tears. Husssh! Don’t be noisy You might disturb the child asleep Hussh! Stop all this fighting You might also hit the child! Dream, dream of peace In the coming days Tomorrow, who knows, you can walk To where there are no more tears. Please let the child sleep And let him dream in peace Wake up, my dear Mindanaw Peace is coming to us now
Photo Source: [x]
458 notes
·
View notes
Photo



In a feministic two-for-one, we all get to celebrate International Women’s Day today and Women’s History Month all month.
There are an incredible number of Tumblrs out there channeling their pride, frustration, and solidarity into art. Art to be reblogged and shared and appreciated. So let us point you to our International Women’s Day tag. It’s a beautiful thing to behold.
Animated portrait by @rozkazaz, watercolor by @cbc, Rosie illustration by @knifesonart, women from everywhere by @sarafratini, raised fist by @jessicamaccormackrmack, Ruth Bader Ginsburg by @ciaraoneillart.
23K notes
·
View notes
Text
Signs seen in Aortic regurgitation mnemonic
Hello! In this post, I talk about the signs seen in Aortic regurgitation and share a few mnemonics with you. I also inserted some gifs to make it fun.
I recommend using mnemonics for the signs you can’t remember after learning them thoroughly than trying to memorize the mnemonics first :)
Let’s get started :D
de Musset’s sign: Rhythmic nodding or bobbing of the head in synchrony with the beating of the heart.
Mnemonic: Imagine a musketeer, raising his hat and then bowing his head stylishly.

Muller sign: Systolic pulsations of uvula. Mnemonic: M for Muller, M for mouth. Muller’s sign is seen in the mouth. You could also think of MU in MUller - Muller, Uvula.

Quincke’s sign: Regurgitant blood flow into a dilated left ventricle during diastole leads to a decrease in diastolic pressure and a consequent increase in stroke volume, resulting in blanching and flushing, respectively, of the nail bed.
PS: They are pulsations which are SEEN, they are NOT FELT.
Quincke’s pulse is the capillary pulsations and any thing that demonstrates these pulsations may be known as Quincke’s sign. (I don’t know for sure though.)
Other ways to see Quincke’s pulse:
- While drawing the thumb nail sharply across the forehead, one can cause a red mark, which can be seen paling and flushing with each beat of the heart.
- When pressing a glass slide on the inner part of the lower lip, the same capillary pulsation will be seen.
So these two can also be called Quincke’s signs! :)
Mnemonic: I honestly don’t have a mnemonic for this one. Uhh.. How about.. “Quickly keep Quiet with Quincke’s finger on your lips?” The Q’s to remind you of Quincke. Finger for nail bed. Lips for the glass slide thingy.

Watson’s water hammer pulse: A pulse that is bounding and forceful, rapidly increasing and subsequently collapsing, it resembles the strike of waterhammer, a Victorian toy.
Mnemonic: This image. Look at the bounding of poor Donald’s head :P

Traube’s sign: A ‘pistol shot’ systolic sound heard over the femoral artery.
Mnemonic: You keep pistol (gun) in your trousers in the belt (which is near the femoral area). So pistol shot is traubes (trousers) sign which is the sound over the femoral vein.

Light house sign: Alternate flushing and blanching of forehead. Mnemonic: Imagine a light house flashing lights on and off. Your forehead becomes a light house, going pale and flushed, as if lights are going on and off in your head.
Gerhardt’s sign: Also known as “Sailer’s sign”, in severe aortic valve regurgitation, Gerhardt’s sign is present when pulsations of the spleen are detected in the presence of splenomegaly. This is from the large forward stroke volume that is present in this state.
Mnemonic: GPS - Gerhardt Pulsatile Spleen (Sailer too)
Here’s a sailor navigating with no GPS :P

Landolfi’s sign: It is alternating dilation and constriction of the pupils in time with the patient’s heartbeat. The sign is a result of the increase in pulse pressure that occurs with aortic insufficiency.
Mnemonic: You dream of the lands you wish to visit with your wide eyes :P

Becker’s sign: Presence of visible (through an opthalmoscope) pulsation of retinal arteries.
Mnemonic: BeckeR. Becker sign - Retinal artery pulsations.
Duroziez’s sign: Audible diastolic murmur which can be heard over the femoral artery when it is compressed with the bell of a stethoscope.
Mnemonic: D for Diastolic murmur, D for Duroziez, D for Deaf (It’s audible xD).

Got no mnemonic for these but posting them for the sake of completion :)
Mayne’s sign: Drop of at least 15 mmHg in the diastolic blood pressure on raising the arm.

Okay.. Enough of stupid images :P
Rosenbach sign: The pulsation of the liver during systole caused by the high stroke volume.
Hill’s sign: Popliteal cuff systolic pressure exceeding brachial cuff systolic pressure by more than 10 - 20 mm Hg.
Lincoln sign: Pulsatile popliteal.
Sherman sign: Dorsalis pedis pulse is quickly located and unexpectedly prominent in age >75 yr.
Ashrafian sign: Pulsatile pseudo-proptosis.
Corrigan’s pulse: A jerky carotid pulse characterized by full expansion followed by quick collapse. Also known as Dancing carotid. *tempted to put a dancing gif*
Pulsus biferiens: Click here.
Locomotor brachii: Prominent pulsation of brachial artery seen in aortic regurgitation.
Did you know? Dilatation of the heart with hypertrophy is called “ox-heart” in AR.
That’s all! I’m in America, having a wonderful time with other international medical students. Things aren’t going quite as expected so far but I am learning a lot. I need you guys to pray for me :)I hope I get a strong letter of recommendation from my professors and get acquainted with people who will make getting Internal Medicine residency in a University Hospital easier for me. Pray for me, guys. -IkaN
243 notes
·
View notes
Photo
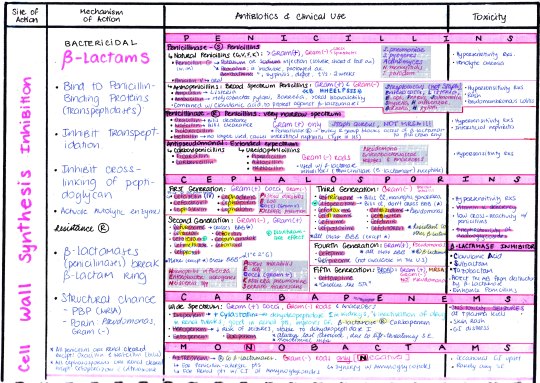
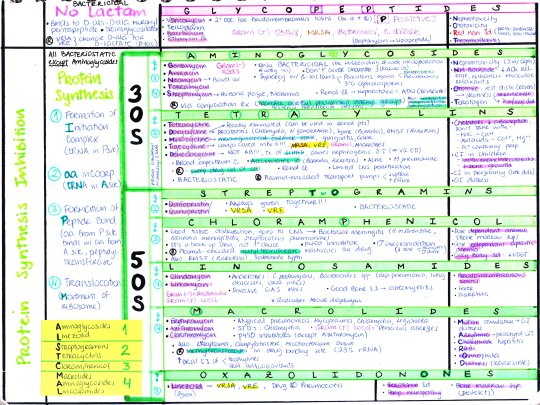
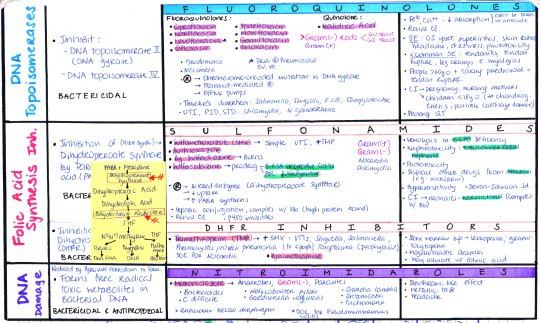
ANTIBIOTICS: COMPLETE CHART
[Download: AB1, AB2, AB3]
[Antibiotic Cheat Sheet]
2K notes
·
View notes
Photo

Beta-Lactams
Beta-lactams are a wide range of antibiotics, the first of which to be discovered was penicillin, which Alexander Fleming identified in 1928. All beta-lactam antibiotics contain a beta-lactam ring; they include penicillins, such as amoxicillin, and cephalosporins. They work by interfering with the synthesis of peptidoglycan, an important component of the bacterial cell wall, and are mostly used against gram-positive bacteria. Bacteria can, however, develop resistance to beta-lactams via several routes, including the production of enzymes that break down the beta-lactam ring. In the NHS, penicillins are the most commonly prescribed antibiotics, with amoxicillin being the most common in the class.
Sulfonamides
Prontosil, a sulfonamide, was the first commercially available antibiotic, developed in 1932. A significant number of sulfonamide antibiotics were subsequently developed, defined as broad-spectrum antibiotics capable of acting on both Gram-positive and Gram-negative bacteria. Unlike the beta-lactams, they do not act by directly killing the bacteria, but by inhibiting bacterial synthesis of the B vitamin folate, thus preventing growth and reproduction of the bacteria. In the present day, sulfonamides are rarely used, partially due to the development of bacterial resistance, but also due to concern about unwanted effects such as hepatotoxicity.
Aminoglycosides
Aminoglycosides inhibit the synthesis of proteins in bacteria, eventually leading to cell death. They are only effective against certain Gram-negative bacteria, as well as some Gram-positive bacteria, but are not absorbed during digestion, so must be injected. In the treatment of tuberculosis, streptomycin was the first drug found to be effective; however, due to issues with toxicity of aminoglycosides, their present day use is limited.
Tetracyclines
Tetracyclines are broad-spectrum antibiotics, active against both Gram-positive and Gram-negative bacteria. Like the sulfonamides, they inhibit protein synthesis, inhibiting growth and reproduction of bacteria. Their use is decreasing to increasing instances of bacterial resistance; however, they still find use in treatment of acne, urinary tract, and respiratory tract infections, as well as chlamydia infections. They must be taken in isolation, often two hours before or after eating, as they can easily bind with food, reducing their absorption.
Chloramphenicol
Another broad-spectrum antibiotic, chloramphenicol also acts by inhibiting protein synthesis, and thus growth and reproduction of bacteria. However, it is also bactericidal against a limited number of bacteria. Due to the possibility of serious toxic effects, in developed countries it is generally only used in cases where infections are deemed to be life-threatening, although it is also occasionally used in the treatment of eye infections. Despite this, it is a much more common antibiotic in developing countries due to its low cost and availability, and is recommended by the World Health Organisation as an effective first line treatment for meningitis in those countries with a low income.
Macrolides
Much like the beta-lactams, the macrolides are mainly effective against Gram-positive bacteria; however, they act in a bacteriostatic manner, preventing growth and reproduction by inhibiting protein synthesis. Their effectiveness is marginally broader than that of penicillins, and they have been shown to be effective against several species of bacteria that penicillins are not. Whilst some bacterial species have developed resistance to macrolides, they are still the second most commonly prescribed antibiotics in the NHS, with erythromycin being the most commonly prescribed in the class.
Glycopeptides
Glycopeptides include the drug vancomycin – commonly used as a ‘drug of last resort’, when other antibiotics have failed. Whilst this used to be the last line of defence against infections, particularly MRSA, the more recent development of newer antibiotics in other classes has provided other options. Nonetheless, there remain strict guidelines on the circumstances in which vancomycin can be used to treat infections, in order to delay the development of resistance. The bacteria against which glycopeptides are active are otherwise somewhat limited, and in most they inhibit growth and reproduction rather than killing bacteria directly.
Oxazolidinones
Oxazolidinones are active against Gram-positive bacteria, and act by inhibiting protein synthesis, and hence growth and reproduction. Linezolid, approved for use in 2000, was the first marketed antibiotic in the class, although the compound cycloserine has been used as a second line tuberculosis treatment since 1956. Whilst linezolid is expensive, resistance seems to be developing relatively slowly since its introduction.
Ansamycins
This class of antibiotics are effective against Gram-positive bacteria, as well as some Gram-negative bacteria. They inhibit the production of RNA, which has important biological roles inside the cells of the bacteria, and as such leads to the death of the bacterial cells. A subclass of antibiotics, rifamycins, are used to treat tuberculosis and leprosy. Uncommonly, ansamycins can also demonstrate anti-viral activity.
Quinolones
Quinolones are bactericidal compounds that interfere with the replication and transcription of DNA in bacteria cells. They are broad-spectrum antibiotics, and are widely used for urinary tract infections, as well as other hospital-acquired infections where resistance to older classes of antibiotics is suspected. Additionally, their use for veterinary purposes is widespread; a use that has been criticised in some quarters for hastening the development of resistance. Resistance to quinolones can be particularly rapid in its development; in the US, they were the most commonly prescribed antibiotics in 2002, and their prescription for unrecommended conditions or viral infections is also thought to be a significant contributor to the development of resistance.
Streptogramins
Streptogramins are unusual in that they are usually administered as a combination of two antibiotic drugs from the different groups within the class: streptogramin A and streptogramin B. On their own, these compounds only show growth-inhibiting activity, but combined they have a synergistic effect and are capable of directly killing bacteria cells, by inhibiting the synthesis of proteins. They are often used to treat resistant infections, although resistance to the streptogramins themselves has also developed.
Lipopeptides
Discovered in 1987, lipopeptides are the most recent class of antibiotics, and are bactericidal against Gram-positive bacteria. Daptomycin is the most commonly used member of the class; it has a unique mechanism of action, disrupting several aspects of cell membrane function in bacteria. This unique mechanism of action also seems to be advantageous in that, currently, incidences of resistance to the drug seem to be rare – though they have been reported. It is given via injection, and commonly used to treat infections in the skin and tissue.
Antibiotic Resistance
Bacterial resistance to antibiotics is on the rise, to the extent that it has been made the focus of this year’s Longitude Prize. The prize is offering a £10 million prize fund for the development of a cheap and easy to use bacterial infection test kit, in the hope that this will allow doctors to prescribe the correct antibiotics at the correct time for patients, and also prevent the prescribing of antibiotics in the cases of viral infections. It’s hoped both of these measures will help slow the development of antibiotic resistance in bacteria.
SOURCE : CompoundChem
1K notes
·
View notes
Photo

Common painkillers.
No, this isn’t the Judas Priest song (furthermore I like it). This is a guide to drugs used to stop pain, maybe the most used drugs with cardiovascular drugs and antidepressant. Painkillers, or analgesics, come in a number of forms, but fall broadly into two main classes: non-steroid anti-inflammatory drugs (NSAIDs) and opioids. This graphic takes a look at a selection of common painkillers, their common brand names, and how they work.
Non-steroid anti-inflammatory drugs include analgesics such as aspirin and ibuprofen, shown in the graphic, as well as naproxen. These drugs all work by inhibiting the synthesis of a class of chemical compounds called prostaglandins. Prostaglandins are produced by the body during inflammation, and they contribute significantly towards pain. NSAIDs work by inhibiting the activity of two enzymes, cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2). These enzymes catalyse prostaglandin synthesis, so when their activity is inhibited, so is the body’s manufacture of prostaglandins. The net result is a reduction in inflammation, and subsequently a reduction in pain. Painkillers have no innate method of reaching only the site of pain, but rather are distributed evenly through-out the body when you take them. They’re also non-discriminative in terms of their action, and will inhibit prostaglandin synthesis all over your body, not just at the site of pain. Prostaglandins don’t just have a role in pain in our bodies – they’re also found in the gut, where their role includes protection of the gut lining. As such, use of NSAIDs increases the risk of stomach ulcers and gastrointestinal irritation. For this reason, during sustained course of NSAIDs (for example, after surgery), drugs to help protect the gut lining may also be prescribed.
Opioids are the second major class of painkillers. These are a class of drugs related to morphine, the compound found in significant concentrations in the opium poppy. The opium poppy itself has been used for its natural painkilling properties for centuries, as the opium which can be extracted from it contains around 12% morphine. The synthetic drug heroin is also obtained from a simple chemical modification of morphines structure; many of the painkilling opioids have similarly minor differences in chemical structure. The opioids work in a different way to the NSAIDs; rather than combatting the pain at its source, they instead prevent the sensation of pain by binding to and blocking the receptors in the brain and spinal cord that are responsible for the transmission of the sensation of pain. This group of receptors are known as opioid receptors, and there are four different subtypes; the exact manner in which many of the opioids inhibit pain by binding to these receptors isn’t fully understood. Opioids may be potent painkillers, but their overuse comes with the spectre of opioid addiction. Excessive use leads to over-stimulation of the brain’s ‘reward’ pathways; the brain also tries to compensate by reducing the number of opioid receptors, meaning progressively more of the opioid is required to achieve the same highs. No single treatment is effective for all opioid dependent patients, and oddly enough, some of the opioids drugs are used in some treatments. Methadone and buprenorphine are both commonly prescribed, as they are longer acting than, for example, heroin, and so allow for less frequent dosing. Tolerance is also slow to develop, and as such their use has been associated with a reduction in the use of other opioids in opioid dependent individuals. Although fentanyl is the most potent opioid shown on the chart, more powerful opioids do exist. The most potent used in humans is sufentanil, considered to be approximately 500-1000 times stronger than morphine. Carfentanil, with a potency considered to be around 10,000 times that of morphine, is used as a general anaesthetic in large animals.
Paracetamol is something of an oddity among the painkillers, in that it’s categorized separately, rather than in one of the two main groups. Part of the reason behind this is that we still don’t have a very good idea of how paracetamol exerts its painkilling effects. It’s thought that, like the NSAIDs, it works by inhibiting cyclooxygenase enzymes, but there are also suggestions that it works on the endocannabinoid system in the body, which plays a part in pain. In short, we still don’t really know how it functions. Paracetamol also has a detraction, in that its toxic dose is relatively close to the effective dose. Excessive use or overdose can lead to damage to cells in the liver, which can in turn lead to liver failure and death.
(Source: Compound Interest).
1K notes
·
View notes
Photo

How different drug classes affect the body. Via sketchymedicine.com
2K notes
·
View notes



