#ABG LAB
Explore tagged Tumblr posts
Text
The Quiet Fury

Previous | Next [Series Masterlist] Pairing: Dr. Michael “Robby” Robinavitch x F!SeniorResident!Reader Summary: Your authority is tested by a cocky fourth-year med student who mistakes the ER for his personal playground.
Word Count: 1.3 K Content Warning: Medical procedures, blood, will most likely be medically inaccurate at times, unresolved tension.
By 1:14 p.m., the ER had the brittle, caffeinated energy of early afternoon. The trauma bay had been turned over twice, a stroke alert rerouted to neuro, and the stack of charts on your tablet had reached an aggressive number. Your hair was falling out of its clip. Your lunch remained unopened in the lounge fridge. And your intern was flirting with a nurse during rounds.
James Whitmore was a fourth-year med student on rotation, assigned to shadow you for the next four weeks. Technically still a student, practically a problem. He had the kind of polished smile that belonged on an alumni magazine cover and the overconfidence of someone who had never been truly scared in a code room. You could already feel it, that subtle entitlement, the lack of preparation, the empty glances when you gave instructions.
You had tried, the first two hours. Gently redirecting. Clarifying. Giving him room to prove he was more than charm and an upward trajectory. But he was more interested in chatting up the new ED nurse than examining his patient. More concerned with what you were doing later than documenting the rhythm strip you’d asked for.
“You know,” he said now, grinning like this was a meet-cute and not an ICU board, “you don’t look like someone who leads a trauma team. No offense.”
You didn’t answer. You didn’t even look up.
Instead, you clicked through labs on the tablet and murmured, “ABG’s back. Go interpret it. Present to me in five.”
He lingered. “You always this serious, Dr. Sheridan?”
You finally met his eyes.
“Only when someone’s dying,” you said coldly. “Which is usually.”
He gave a half-laugh, unsure if it was a joke. You didn’t clarify. You moved past him and toward Bed 6, where a patient was vomiting blood into a basin while her mother cried softly in the corner. Your pulse recalibrated, not with nerves, but with necessity. You could be tired later.
Whitmore followed, his stethoscope still around his neck like a fashion statement, it was getting harder for you to not roll your eyes.
Later, as you updated notes in the hub, you caught a glimpse of him across the hall, leaned too casually against the counter near two of his intern friends. You weren’t listening. Not at first. But you felt it, a shift in the room. Dana stiffening behind the desk. A nurse's eyes narrowing. The slight drop in temperature that meant someone had said something wrong.
Across the floor, by the medication station, Robby was finishing up notes on a post-code debrief when he caught Whitmore’s voice, low and smirking, drifting toward the central hub.
“…yeah, she’s cute in that mean, icy way. You know, a challenge. I give it three shifts before she cracks. Bet she’s crazy once you get her to—"
He didn’t finish. Someone coughed, startled. A tech turned sharply. Robby’s hand paused mid-scroll over his tablet.
He blinked once. Then turned.
He was forty feet away, but he could already feel it like a fissure in the tile beneath them, the cold fury in your eyes, the way you were walking toward Whitmore with the unhurried precision of someone who had not yet decided whether to destroy a person publicly or in private. Your hands were calm. Your shoulders square. You didn’t yell.
You didn’t need to.
“Mr. Whitmore,” you said, voice flat as steel. “Step into the staff lounge. Now.”
The kid hesitated.
Wrong move.
Robby watched you disappear behind the door. Watched the team shift around the hub in respectful silence. No one said a word. Even the printers seemed quieter.
You closed the door behind you.
Then, still calm, still composed, you turned to your intern.
“I don’t know what kind of rotations you’ve done before,” you began, your voice quiet but sharp as frost. “But I am not here for your amusement. I’m not here to play games with you, or compete with your insecurities, or make your ego feel bigger when you get bored during rounds.”
He opened his mouth.
You raised a hand. He stopped.
“You are in an Emergency Department. You are a guest in my house, and if you can’t show basic respect to your patients or to your senior, then you can leave now. I’ll sign the damn form. But what you will not do is treat this place, or the people in it, like a frat party you wandered into by mistake.”
His face changed then. A flush of something like embarrassment, something like shock. You didn’t care which.
“I suggest,” you continued, eyes not wavering from his, “that you get with the program. Fast.”
He swallowed. “Yes, Dr. Sheridan.”
You nodded once. “Good. You’re on labs until further notice.”
You opened the door for him to leave, only to find Robby there, leaned casually against the wall, arms crossed. His eyes flicked between you and Whitmore, unreadable.
The student mumbled something, not quite an apology, not quite coherent, and headed toward the lab station like a dog with its tail tucked.
You didn’t speak. You moved to close the door again and turn back toward the lounge room. He waited a beat, then two. Long enough to give the illusion of space. Long enough not to look like he’d been watching. Then he followed.
He knocked once on the edge of the lounge door before stepping in. You stood by the sink, filling a cup with water, back turned. Your grip on the plastic rim was too tight.
"You handled that well," he said quietly.
You didn’t turn around. “Thanks.”
A pause. You took a sip, then set the cup down, your shoulders rigid.
Robby moved to stand beside you, leaving a careful amount of space between them. The hum of the fridge filled the silence.
“He won’t do it again,” you said, eyes fixed on the sink.
“I know,” he said. “Not if he values his career.”
You gave a short, humorless exhale, not quite a laugh.
He glanced at you, then away. “You okay?”
Another pause.
Then you nodded, still not looking at him. “Yeah. Just annoyed.”
“Okay,” he said. “But if that changes…”
You looked at him for a long moment. Then offered the faintest curve of your mouth, not a smile, but something close. Gratitude maybe. Recognition.
“Thanks, Dr. Robinavitch.”
He gave her a smile in return. “Anytime, Sher.”
And with that, he stepped out, leaving the door open behind him. Just a crack.
Enough for her to breathe.
Whitmore was alone at the lab station when Robby found him. Still cocky, despite it all. The kind of cocky that didn’t learn until the lesson was painful.
Robby approached quietly.
“You got a minute, Mr. Whitmore?”
The kid turned, startled, then nodded. “Yes, Dr. Robinavitch.”
Robby didn’t raise his voice. He didn’t even look angry. That was the worst part.
He just stepped closer, lowered his voice, and said, “You ever speak about Dr. Sheridan like that again, and I will personally end your chances of matching into anything but urgent care in rural Alaska. Are we clear?”
Whitmore blanched. “Sir, I didn’t—”
“You did,” Robby said, cool and clinical. “And I suggest you use your remaining days here wisely. Listen. Learn. Show some respect. Because you’re not the smartest man in this room. And you sure as hell aren’t the toughest.”
Whitmore swallowed. “Understood.”
“Good.” Robby offered him a smile that wasn’t really a smile. “Now go run the troponins.”
Robby didn’t move for a while. Just stood there, hands in his pockets, watching the chaos of the ER reassemble itself. His gaze flicked to the patient board. To the rooms. Then, finally, back to you.
You were at the end of the hallway now, instructing a nurse, your voice steady again. Calm. Efficient. But he could see it in the way your fingers tapped against the tablet. The way your jaw stayed locked.
——————————————
Two chapters in one day!
I couldn’t help myself bahhahah I needed y’all to read this one. My toxic trait is buying the people I love presents and needing to tell them what it is or I’ll explode.
I told myself I was going to pace myself but all chapters are sitting in my queue tempting me.
#michael robinavitch#michael robinavitch x reader#the pitt#the pitt hbo#the pitt imagine#the pitt fanfiction#dr robby#dr robby x reader#dr robinavitch x reader#dr robby imagine#dr michael robinavitch#dr robinavitch#noah wyle#the pitt max#the pitt x reader#the pitt x you#michael robinavitch x you#dr. robby x you#fanfic#fanfiction
584 notes
·
View notes
Text
The Bench Across the Street
AO3
Part 1 | Previous | Part 13 | Next
Summary: What if Abby is hurting and forcing Frank to take benzos to “control” his ADHD?
What if few hours after the argument, Frank is brought to the ED on a brink of an overdose and some unexplainable injuries.
TW: Abuse, Overdose, Suicide Attempt
Tags: Dark!Abby | Frank whump | Frank-centric | Miscommunication | Abusive!Abby | abusive relationships | threats of violence | implied/reference child endangerment | is this considered AU? | spousal abuse | men can be victims of abuse too
——————————————————————————————————
Frank
“It’s Langdon’s son.”
The world tilted sideways.
I didn’t move.
Couldn’t.
It took a full second—maybe two—for the words to hit.
Langdon’s son.
Tanner.
My Tanner.
Someone called out for the trauma bay to be cleared. Nurses started moving faster, shouting for peds consults and crash cart.
The noise in the ER sharpened and blurred all at once.
I was still standing there, coffee dripping from my hand, forgotten on the floor, when Dana appeared by my side. “Frank,” she said quietly, touching my elbow. “Go.”
That broke me loose.
I ran.
~~~~~~~
The ambulance bay doors swing open with a crash.
The gurney wheeled through. Small form strapped down, oxygen mask covering most of his face, pale arms limp at his sides.
Tanner.
Tiny. Motionless.
The paramedics rattled off numbers as they pushed him into the trauma bay.
BP 72/38
HR 50s
RR 13 and shallow.
“Collapsed after snack time. Teacher reports clumsiness, weakness over the past week. Down for about 3 minutes before EMS arrival. Oxygen saturations in the low 80s. Glucose normal. No witnessed seizure activity.”
I moved without thinking—snapping gloves on, shoving past the nurse reaching out for the monitors.
I had to touch him.
I had to be sure that he was still breathing.
“Langdon!” Robby’s voice, cutting through the chaos.
I didn’t stop.
I squeezed Tanner’s tiny wrist between my fingers, felt the sluggish thud of his pulse.
“Langdon!” Robby barked again, stepping in front of me.
I tore my eyes off Tanner long enough to glare at him.
“You know you can’t,” Robby said, quieter now. “You know you have to step back.”
The rules.
The stupid, goddamn rules.
I stared at him, breathing like I’d ran a marathon.
Logic warred with instincts, hot and brutal.
I could save my son.
I could fix him.
If I just—
No.
No you can’t.
You’re not his doctor.
You're his father.
Slowly, mechanically, I peeled off the gloves. Dropping them on the floor. Stumbling backward, feeling like I’d been ripped out of my own skin.
Dr. Shah had already arrived—peds attending, PICU trained and steady as stone—took my place immediately, issuing orders, seamlessly taking over the case. “Two litters by weight, wide open please!” Shah ordered, “Start second line access. Blood draws for labs—CBC, CMP, ABG, LFTs. Someone call CT. We need to get his head checked. Can we also get radiology in here for x-ray, please? Add an ECG to the order. ”
He wasn’t shouting.
He wasn’t panicking.
The team around him moved efficiently.
Doing everything right.
Doing everything I should have been doing.
Tanner’s teacher hovered near the door, crying into her hands.
I didn’t hear a word she said.
I fumbled my phone out of my pocket.
Mia.
I had to call Mia.
It rang once.
Twice.
“Frank?” She answered, immediate and alert.
“It’s Tanner,” I rasped, voice breaking. “Collapsed. Bradycardic. Hypotensive. I—Mia, please.”
“I’m coming.”
I didn’t have anything left to say. I just stood there, watching the team work over my son.
~~~~~~~
They were clearing him out of the trauma bay when I saw her.
Mia.
She was wearing hoodie and sweats, hair pulled back in rough twists, moving fast but sharp, eyes sweeping around the ER.
She caught sight of me, frozen just outside the peds room they’d just wheeled Tanner in.
Her steps barely slowed. She didn’t call my name. Didn’t ask questions. Just brushed her knuckles against my sleeve, steady and sure.
“Come here,” said said quietly, steering me towards the peds room. The walls were painted in bright cartoon forest scenes. Foxes curled under the tree. Bears smiling from behind the bushes. Deer with wide, glassy eyes.
It should have been comforting.
It made my stomach twist.
The nurse was adjusting the fluids.
The portable monitor beeping sluggishly.
The tech was setting up the mobile x-ray as we stood just inside the door.
Dr. Shah scanned through the early blood work orders, typing quick notes.
“Vitals still unstable but improving slightly with fluids. Oxygen holding at 90%. Well start with basic pannels and imaging before considering expanded tests.”
I clung onto the doorframe, watching every twitch of Tanner’s body under the blanket.
Mia stayed by my side, arms crossed, calm as stone. Holding me in place when the world wanted to tear itself open.
Mia guided me to a chair shoved by the foot of the bed.
Not speaking.
Just pressing me down with one hand on my shoulder until I sat, knees wide, elbows on thighs, hands dangling uselessly between them.
I stared at the floor.
At the pattern of cheap tiles, scuffed and dirty.
At the rubber wheels of the IV pole.
anywhere but Tanner.
Because looking at Tanner would break whatever scraps were holding me together.
The clock on the wall ticked loud and slow.
Every second scratched too long.
Every breath scraped raw against my ribs.
Mia sat next to me, close enough to feel the heat of her body, solid and still.
She didn’t speak.
She didn’t move.
She just stayed.
An anchor in a storm too big to survive.
~~~~~~~
A nurse came and went, checking the monitors.
Another tech drifted in with the portable ECG, electrodes sticking to Tanner’s tiny chest like spider legs.
The beep of his heart echoed through the room.
Too slow.
Too fragile.
~~~~~~~
I didn’t know how long we sat like that.
Thirty minutes?
Ten minutes?
Time lost meaning when every second weight a thousand pounds.
I didn’t speak.
Mia didn’t push.
The only thing moving in the room was the slow, sluggish drip of fluids into my son’s veins.
~~~~~~~
The door creaked open.
I didn’t look up.
I couldn’t.
But I heard Robby’s footsteps crossing the tiles.
He cleared his throat once—awkward and brittle. “Mia,” he said first, like he wasn’t sure who he was speaking to, “Frank.”
Mia tilted her head acknowledging him.
I stayed silent.
Robby shifted his weight
“The hospital contacted Abby,” he started quietly. “Standard procedure. The school also called her too, before we even got the ambulance report.”
The words hit like a punch to the gut.
Of course they had.
Of course.
I stared at the tile a little harder, willing it to crack open and swallow me.
Robby lingered like he might say more. Then he gave up and left, pulling the door shut behind him with a soft click.
~~~~~~~
Mia stayed with me.
Waited.
She didn’t offer comfort.
She knew better than that.
She knew there was no comfort left.
Only the waiting.
Only the dread.
~~~~~~~
The bloodwork came back next.
Dana came into the room, holding the tablet containing Tanner’s chart.
I stood up, barely stopping myself from snatching the tablet from her hands.
CBC – normal.
CMP – normal except slight hyponatremia.
LFTs – mild transaminitis.
ABG – mild metabolic acidosis.
ECG – normal sinus rhythm, slow but stable.
No answers.
Nothing that explained why my son was lying unconscious in a bed under painted trees.
I gave the tablet back.
My legs gave out a second later.
I dropped back into the chair.
Mia moved closer—but not touching—but close enough that I could feel her breathing alongside mine.
The door stayed closed.
The machine kept beeping.
The walls pressed closer.
Every cartoon fox. Every smiling bear.
Watching.
Waiting.
The air felt too thick to breathe.
I pressed the heels of my hands into my eyes, trying to stop the burning.
Trying to stop the scream building low in my throat.
Trying to survive the next second.
And the next.
And the next.
Because if I stopped even once.
I knew I’d never start again.
~~~~~~~
I didn’t want to leave the room.
Every cell in my body told me to stay planted next to Tanner’s bed, to watch the slow rise and fall of his chest, to measure the gap between each monitor beep like I could predict what would happen next.
But I still had my job to do. I’m still part of the ER team until 16:00.
And even if I wasn’t cleared to treat my son. I still had to do my shift handoff.
So I stood in the hallway outside the peds room, barely upright, going through the motions while Samira reviewed the final updates on the triage board.
I nodded at the appropriate times.
Maybe.
I think.
I honestly couldn’t hear half of what she said.
My eyes kept darting back towards the peds room behind her.
Every breath felt like a countdown.
Samira was kind about it—gentle even—but I could see the discomfort in her eyes.
She knew.
Everyone knew.
That my son was on the other side of that glass door.
She reached the end of the board and paused, tapping softly on the tablet. “That’s everything,” She said softly, “I’ve got everything from here.”
I nodded, swallowing down whatever the hell was caught in my throat.
“Thanks.”
She didn’t say anything else.
Just gave me a careful look and turned down the hall.
I barely had the time to breathe before I heard the echo of fast steps coming up the hallway.
I turned already knowing.
Already feeling it in my gut.
And there she was.
Abby.
Coat flung open, shoes loud against the tiles, purse bouncing at her hip.
I didn’t breathe.
Didn’t blink.
Just stared at the glass door of the peds room, where Tanner lay still under too many wires.
And waited for her to reach me.
She spotted me the moment she turned the corner.
Her face tightened immediately. Not grief. Not worry.
Something colder. Sharper.
“What the hell happened?” She snapped as soon as she was close enough.
I stepped forward, blocking the door out of instinct—a move so small, so quick, I barely knew I was doing it until we were shoulder to shoulder.
She stopped abruptly, eyes narrowing.
“I should’ve been called the moment it happened,” she hissed “Why didn’t you call me?”
My hand was on the door handle.
Not turning it.
Not letting it go.
She reached for it, but I didn’t move.
“Abby.” I said, voice too thin.
She paused.
A flicker of suspicion passed through her face.
And in that single beat, I realized just how badly I didn’t want to be alone in that room with her. How much of me still didn’t know what she is capable of. And just how terrifying that is to truly admit.
“Frank,” she started slowly, “move.”
“He’s barely stable,” I managed. “They’re running tests. They’re—he’s okay for now.”
She stared at me like I was speaking a different language.
“He’s my son,” she snapped. “Let me in.”
“I’m not stopping you.” My hands tightened around the handle, contradicting the words. “I just–need you to be calm, Abby. Don’t make this about us. Just be his mom.”
There was a moment
A breath of silence between us, just long enough for the air to thicken.
Then she nodded once, too sharp to feel genuine.
“I’m always his mom.”
I stepped back.
Let the door open slowly.
Abby entered the room without another word and went straight to Tanner’s bedside.
I didn’t follow her in.
I couldn’t.
I hovered near the threshold, caught between panic and disbelief, every inch of my body poised to intervene if she so much as shifted the wrong way.
Abby leaned down over Tanner’s bed, brushed his hair from his forehead and whispered something I couldn’t hear.
She didn’t scream.
Didn’t lash out.
Not yet.
But I watched her with the kind of attention I usually reserved for unstable trauma patients.
Waiting for a sign of escalation.
Waiting for something to crack.
Mia’s voice came softly behind me, “I need to step out. Make some calls.”
I turned toward her, barely able to nod.
She lingered for a beat longer than necessary. Eyes sweeping Abby. Then me.
Then she left, the door hissing quietly shut behind her.
And I was alone.
With Abby.
With the pressure in my chest mounting like a collapsed lung.
It wasn’t long after Mia had left that I felt the air shifted.
I could still hear her steps echoing down the hallway, then nothing. Just the quiet buzz of machines, the beep of the monitor, the near silent his of Tanner’s oxygen.
And Abby, sitting perfectly still beside him, like she’d never moved from that spot.
She adjusted his blanket softly.
Methodically.
Like it was something she had done a hundred of times— like there were eyes watching and she needed to be seen doing the right thing.
She didn’t look at me when she spoke.
“You must’ve been so scared.”
I blinked.
Wasn’t sure if it was a question or a trap.
I gave her nothing.
She turned just slightly, enough to just glance over her shoulder.
“I know I was.” She added. “When the school called. My heart just dropped. I was already halfway out the door before they even finished the sentence.”
Still watching me.
Waiting for something.
“Did he seem off to you this week? Before this?” She asked, voice light.
I swallowed.
Hard.
“I didn’t really–he was with you.”
Her smile was small.
Too small.
“Right,” she said, nodding slowly, “of course.”
She turned back to Tanner.
Brushed his hair from his forehead with the back of his hand again.
“I guess he didn’t mention anything to you. About not feeling well. Or being dizzy. Or tired.”
I couldn’t tell if she was asking or accusing.
My throat was dry.
“No,” I said. “He didn’t say anything to me.”
“Strange,” she murmured. “He usually tells you everything, doesn’t he?”
My stomach twisted.
She kept her eyes on Tanner, her voice soft and syrupy.
“They said he collapsed after snack time. That he’d been acting clumsy, weak, off. All week.”
Her fingers played with the cuff of his hospital gown.
“I guessed you missed it.”
I flinched.
Just barely.
But she saw it.
Of course she did.
Her smile returned—barely a curve of her mouth.
“I mean, I don’t blame you,” she said. “You’ve been under a lot of stress. You were even—what was it? Admitted for seventy-two hours?”
I felt heat crawl up my neck.
My heart pounded too fast.
She stood up slowly, like she was rising from something sacred.
“I only bring it up because maybe…you’re not seeing things clearly. That happens sometimes. After something like that.”
She moved towards me.
Not quickly.
Not threatening.
Just enough to close the space.
She lowered her voice, pitched it like a secret between old friends.
“And I know how much you love him. I do. So if you're worried—if you think something happened—you should tell someone. You should be honest.”
I opened my mouth, but the words died there.
She reached out.
Touched my arm, gentle as wind.
“And if it was something at school,” she added, “or even something he got into at our place—no one would blame you.”
That was it.
That was the knife.
Wrapped in silked.
Pressed just deep enough to make me bleed.
I stepped back.
Barely breathed.
“I didn’t—“ my voice cracked, “I would never—“
She nodded, serene.
“I know,” she said, “but you’ve been…struggling. We both know that.”
She turned back toward the bed.
Sat down again.
Took Tanner’s hand like it belonged to her.
And smiled like she hadn’t dismantled me with a dozen perfectly measured words.
The room was still vibrating with what she said.
The sound of her voice clung to the corners like smoke.
I stood frozen by the sink, one hand gripping the counter so tightly my knuckles burned. Tanner’s monitor beeped on—slow and steady—but my own pulse was too fast.
She didn’t say I did it.
She didn’t have to.
She said enough to plant the seed, coat it in sympathy, and leave me to drown in the silence that grew from it.
Then-
A knock.
Soft.
The door creaked open.
“Hey,” Dana said, stepping in with her usual calm, like a storm could never touch her. “I’ve got to grab the second round of labs. CT’s holding. Result’s not back yet.”
Her voice was casual.
But her eyes-
Her eyes moved like scalpels.
She looked at Tanner first, then me.
Paused for just a second longer than usual.
Then shifted her gaze to Abby—sitting upright, a little too composed, like she knew how to sit in grief but not feel it.
Dana’s mouth pressed into a neutral line.
“Frank,” she said gently, “Mind giving me a hand real quick?”
I blinked.
She wasn’t asking for help.
She was giving me an out.
Abby straightened.
“Oh- do you need him?” She asked quickly. “I’d…I’d rather not be alone right now. Frank’s his father. And I’m scared. I haven’t even gotten to speak to the doctor treating our son yet.”
Her voice just trembled—just enough.
Not too much.
Practiced.
Polished.
Dana raised an eyebrow.
Didn’t speak for a second.
Then turned to me.
“You can stay,” she said. “Up to you. Just thought I’d check.”
The offer sat there.
Thick in the air.
I looked at Abby—sitting like a glass doll perfectly arranged.
And at Dana—waiting, quiet, knowing.
My voice barely worked.
“I’ll stay,” I answered because I didn’t know what would happen if I left.
Dana nodded.
But she didn’t drop it.
Her eyes locked on mine for a moment longer.
Not pushing.
Just steady.
Seeing.
Then she turned back to the bed, snapping gloves on as she prepped the vials.
Abby leaned in and brushed her thumb over Tanner’s hand again, like she was painting the image of a mother.
But Dana didn’t look at her again.
She only looked at me.
And I knew—
She’d seen it.
All of it.
#dr frank langdon#frank langdon#dr frank langdon x reader#frank langdon x reader#the pitt#the pitt hbo#the pitt fanfiction#hbo max#the pitt fandom#fanfic writing#fanfictions#fanfics#fanfiction#fanfic#fandom#ao3 writer#ao3feed#archive of our own#ao3 link#ao3#ao3 fanfic
29 notes
·
View notes
Text
Through the Haze: Part 4
The trauma bay buzzed with clinical urgency.l
Connor stood at the head of the bed, intently observing Emily’s monitor. The ventilator hissed rhythmically beside her. Nurses darted in and out with labs and IV bags, while Will rapidly input orders into the EHR terminal nearby.
Jay and Matt stood silently at the far end of the trauma bay, out of the way but completely locked in, watching helplessly as their sister and girlfriend was worked up like a trauma patient. Jay’s fists were clenched tight behind his back, Matt’s jaw tight, eyes unreadable but glassy.
“CT’s uploading now,” Connor said to Will, nodding to the monitor. “Let's pull the EVD kit just in case. I want to be ready if we’re looking at cerebral edema.”
Will moved to the bedside, checking Emily’s IV sites. “Sodium’s low—131. That could’ve lowered her seizure threshold. Keppra level came back subtherapeutic, only 8 mcg/mL. She’s probably been missing doses.”
Matt exhaled sharply at that, rubbing a hand over his face.
A nurse slid the stat CT results up on the monitor. Connor scanned the images in silence for a beat before speaking.
“No evidence of intracranial hemorrhage or mass. No midline shift. Some mild diffuse cerebral edema, likely postictal. No hydrocephalus. We’re okay for now.”
Will added, “Her lactate’s elevated—3.9 mmol/L. That’s postictal lactic acidosis from the sustained seizure activity. Her ABG shows mild respiratory acidosis, but ventilation’s compensating. pH 7.29, PaCO₂’s sitting at 48, PaO₂ at 88 on 60% FiO₂.”
Connor nodded. “Keep her sedated on propofol, 10 mcg/kg/min, titrate to BIS around 60. EEG is en route: we need to rule out non-convulsive status. We’ll hold off on mannitol or hypertonic saline unless her ICP trends up.”
As another nurse adjusted the lines, Connor glanced up and finally addressed the silent tension in the room.
“Guys,” he said, gently but firmly to Jay and Matt. “You’ve been here every second, I get it….. but we need the space to work.”
Jay started to protest, but Matt placed a hand on his shoulder. “We’ll wait outside,” he said, voice hoarse.
Both men hesitated for one last look at her.
Emily’s body was still now, chest rising and falling in time with the ventilator, face peaceful but pale, the endotracheal tube taped to her mouth. Around her, it looked more like a warzone than a hospital: lines, meds, wires, machines. She looked small beneath it all.
Matt leaned against the wall, head down, arms crossed. Jay stood nearby, pacing slowly, eyes still locked on the trauma room doors like he could burn through them.
“She’s been having seizures and didn’t tell anyone,” Matt finally said. “We would’ve gotten her help. Monitored her meds.”
Jay ran a hand through his hair. “She thought she was protecting us. She didn’t want to be a burden. She probably downplayed every symptom.”
Matt shook his head. “She could’ve died.”
Jay’s voice was tight. “She still could.”
A silence passed between them. Heavy. Shared. Grieving.
Connor stepped out twenty minutes later, pulling off his gloves and scrubbing a hand through his hair. Will followed.
“She’s stable,” Connor began. “No evidence of acute intracranial pathology. Postictal cerebral edema is resolving with sedation. Her Keppra levels were subtherapeutic—she’s been missing doses.”
“We’ve placed a central line and started continuous EEG monitoring. No seizure activity now. We’ll keep her sedated for a few hours, maybe overnight, to allow her brain to rest.”
Jay straightened. “What happens when she wakes up?”
Will replied, “We’ll extubate if her ABGs normalize and she’s breathing spontaneously. But she’s going to be disoriented. Scared. And probably ashamed she didn’t tell you.”
Matt’s voice was quiet. “She doesn’t get to be ashamed. She gets to be alive.”
Connor gave a faint nod. “You can sit with her once she’s up in the ICU. She’ll need you both.”
Jay exhaled, shoulders sagging. “We’ll be there. Every damn second.”
The soft rhythmic beeping of the cardiac monitor filled the quiet ICU room. The sedation had been tapered over the last two hours, and Emily’s EEG was now quiet—no epileptiform activity noted. Her vitals were borderline but stable: HR 98, BP 112/68, SpO₂ holding at 95% on a low-pressure ventilator setting. The propofol was running low-dose to ease the transition back to consciousness.
Jay sat at the bedside, one hand curled gently around Emily’s, the other resting on the blanket over her knee. Matt sat on the opposite side, slumped in a chair, eyes bloodshot but locked on his sister.
The ventilator sighed softly with each breath, keeping her oxygenated while the rest of her system caught up. Her forehead was lightly coated in sweat, her brows twitching—little signs she was nearing consciousness.
“Em,” Jay whispered softly. “You’re okay. You’re in the ICU. You’re safe.”
Her eyelashes fluttered.
Then. her fingers twitched.
And suddenly—wide, panicked eyes opened, pupils dilated and darting, chest rising fast against the vent tubing.
Emily began to thrash slightly, her brain screaming breathe even as the tube in her throat kept her from doing it on her own.
“Emily….hey……hey….stop, you're intubated,” Jay said quickly, standing, hand moving to her shoulder. “You’re okay. You’re okay.”
Her HR spiked on the monitor—113. 127. 142
“She’s trying to fight the vent,” Matt said, rising fast. “She’s going to self-extubate—Jay—”
The monitor let out a sharp alarm—high heart rate, O₂ sat dipping.
Jay hit the call button hard, “We need help in here now!”
Will burst through the door not thirty seconds later, Connor on his heels.
“She’s post-sedation agitated,” Will assessed immediately, moving to her head. “Pulling against the tube—RR’s up to 32. HR 148. She’s panicking.”a as
Will gently held her face. “Emily, it’s Will. I need you to stay still. You’ve got a breathing tube in right now, and we’ll take it out as soon as it’s safe, okay? Just blink if you can hear me.”
Emily blinked once. Her eyes were full of tears, terror radiating from them.
Jay stepped in close, taking her hand again. “You’re okay, baby. You had seizures, but you’re stable now. You’re safe.”
Connor checked the monitor again. “She’s trying to overbreathe the vent. Let’s sedate lightly—low dose fentanyl, 25 mcg. That’ll calm her respiratory drive without knocking her out again.”
The nurse pushed the medication. Within a minute, Emily’s HR slowed to 110, and her grip on Jay’s hand relaxed slightly.
Then…..a sudden stiffening.
Will froze. “Hang on—”
The EEG alarmed.
Connor’s voice was immediate: “Focal onset—right hemisphere spike wave—secondary generalization.”
Emily’s body began to seize again—her arms jerking slightly, then stiffening as her legs tensed and back arched on the bed.
“Status recurrence. Push Ativan—2 mg IV,” Will ordered. “Hold the sedation otherwise.”
Jay backed away just enough to give them space, eyes wide, breath shaky. “Jesus…”
Matt stood by the window, both hands covering his mouth.
Will kept a hand on her chest, monitoring the rigidity. “Okay, she’s cycling. Short duration. Lasted about 45 seconds. EEG’s calming. Vitals stabilizing.”
Connor checked her pupils again. “No postictal coma. She’s staying borderline conscious, just altered.”
Will exhaled slowly. “She needs an updated neuro consult. We’ll increase her maintenance AED dose to 1.5 grams Keppra daily and start a loading dose of Vimpat tonight. We’ll get a 24-hour EEG to monitor any subclinical activity.”
He turned to Jay and Matt. “She’s fighting…. hard. And she’s scared. When she’s awake enough to come off the vent, she’s going to need you both right there.”
Emily blinked awake again to soft light and Jay’s voice.
“No tube now,” he whispered, sitting close, brushing damp hair from her temple. “You’re breathing on your own, Em.”
She let out a small, raspy cough.
Matt leaned over her opposite shoulder. “Hey, hey, don’t talk yet. Just nod, okay?”
Her eyes were already filling with tears.
“Where…?” she rasped.
“You’re at Med,” Jay said gently. “You had a series of seizures—one in the gym and one just a little while ago here. You’re stable now.”
Emily’s chest hitched, panic starting to climb again.
“I couldn’t… move… I couldn’t breathe—” she gasped, tears spilling down her cheeks. Her voice was shaky, slurred but full of fear. “I thought… I thought I died.”
Jay cupped her face. “You didn’t. You held on. You’re okay. We’ve got you.”
But her breathing quickened—20. 24. 32.
Will re-entered just as the pulse ox dropped from 96 to 91.
“She’s hyperventilating—panic attack,” he said quickly, moving to her side.
“Emily,” he said firmly, but kindly. “You’re safe. You’re not seizing. You’re just scared. Breathe with me. In for four, hold for two, out for four.”
Jay leaned close, matching the rhythm. “With me, Em. In… hold… out…”
Tears streamed down her face, her whole body trembling. But her breathing started to fall into sync.
Connor monitored the EEG from the screen. “No seizure activity. This is pure anxiety response.”
Matt finally moved close enough to press a kiss to the top of her head. “You scared the hell out of us, Em. But you’re gonna be okay.”
Her voice cracked as she whispered, “I’m sorry…”
Jay took her hand and squeezed. “Don’t be. Just promise you won’t fight this alone anymore.”
Will nodded, stepping back as her numbers finally stabilized. “She’s through the worst of it.”
And surrounded by love—she finally believed it.
#one chicago imagine#jay halstead x you#jay halstead x reader#matt casey x sister reader#matt casey x reader#conor rhodes x reader#will halstead x reader
10 notes
·
View notes
Text
ABG Interpretation Notes, Mnemonics, and Workbook by Nurse Sarah
ABG Interpretation Notes, Mnemonics, and Workbook by Nurse Sarah! If you are studying arterial blood gas interpretation, you may feel a little overwhelmed about all the material you must know in order to interpret the lab values. For example, you may be completely confused on acid-base imbalances (respiratory acidosis vs, respiratory alkalosis or metabolic acidosis vs, metabolic alkalosis), if…

View On WordPress
4 notes
·
View notes
Text
Phlebotomist Technician Salary: How Much Do They Earn in 2024?
Phlebotomist Technician Salary: How much do They Earn in 2024?
Are you considering a career as a phlebotomist technician or simply curious about the earning potential in 2024? Phlebotomists play a crucial role in healthcare by drawing blood for testing, transfusions, research, and donations. This vital profession offers a blend of healthcare service,steady employment,and room for career growth. In this comprehensive guide, we’ll explore the latest salary trends, factors affecting earnings, benefits, practical tips, and real-world insights for phlebotomist technicians in 2024.
What Does a Phlebotomist Technician Do?
Before diving into salary details, it’s essential to understand what being a phlebotomist technician involves. These professionals are trained to safely and efficiently draw blood samples from patients or donors. Responsibilities include:
Preparing patients for blood draws
collecting blood samples using various techniques
labeling and handling specimens carefully
Maintaining sterile environments and safety protocols
Ensuring proper storage and transportation of samples
Documenting patient details and procedures accurately
Phlebotomist Technician Salary Overview in 2024
The earning potential of phlebotomist technicians varies based on multiple factors such as geographic location, work setting, experience, and certifications. As of 2024, the average annual salary for a phlebotomist technician in the United States is approximately $36,000 to $42,000. Though, this range can fluctuate substantially depending on several variables.
Regional Salary Variations
Region
Average salary (Annual)
Top Earning Potential
Southern States
$34,000
$45,000 (Florida, Texas)
Northern States
$38,000
$48,000 (New York, Illinois)
Western States
$40,000
$50,000 (California, Nevada)
Factors That Influence a Phlebotomist Technician’s Salary
Experience & certification: Certified phlebotomists tend to earn more than entry-level technicians.
work Setting: Hospitals and specialty clinics frequently enough offer higher salaries than standalone laboratories.
Geographic Location: Urban centers and high-cost states typically pay more.
Demand & industry Growth: Increased demand for healthcare professionals impacts salaries positively.
In-Demand Skills That Boost Salary
Strong patient dialogue & care skills
Knowledge of advanced blood collection techniques
Proficiency with laboratory information systems (LIS)
Second language fluency (e.g., Spanish)
Additional certifications (e.g., Phlebotomy Technician Certification)
Career Growth and Salary Progression
Many phlebotomists use this role as a stepping stone toward more advanced medical careers, such as ultrasound technicians, medical assistants, or lab technologists.as you gain experience and certifications, your earning potential increases:
Entry-level Phlebotomist: $30,000 – $35,000/year
Experienced/certified Technician: $45,000 – $55,000/year
Supervisor or Lead Phlebotomist: $55,000+ annually
Benefits of a Career as a Phlebotomist Technician
Steady employment with high demand for healthcare professionals
Flexible work environments and hours
Opportunities for certification and specialization
Contributing to vital healthcare services
Less physically demanding compared to some medical roles
Practical Tips to Maximize Your Salary in 2024
Obtain Certification: Certifications such as NHA Certified Phlebotomy Technician can open doors to higher pay.
Gain Experience: Work in diverse healthcare settings to diversify skills and boost income.
Specialize: Consider additional certifications in areas like arterial blood gases (ABG) or pediatric phlebotomy.
relocate: Moving to regions with higher demand and pay can significantly increase earnings.
Stay Informed: Keep up with industry trends and licensing requirements to remain competitive.
Case Study: A Day in the Life of a Successful Phlebotomist in 2024
Meet Lisa, a Certified Phlebotomist in Chicago
Lisa started her career as a basic phlebotomist earning around $32,000 annually. over three years, she earned certifications in pediatric blood draws and arterial blood gases, which allowed her to elevate her role. Today, Lisa earns approximately $50,000 per year working in a top-tier hospital. Her proactive approach to professional development has been key to her increased earning potential and job satisfaction.
First-Hand Tips from Phlebotomists in 2024
“Networking within healthcare facilities opened up additional part-time opportunities for me.” – Mark, Certified Phlebotomist
“Always focus on patient comfort and safety-it makes you stand out.” – Jane, Laboratory Technician
“Invest in certifications related to specialized blood collection techniques.” – Carlos, Healthcare Professional
Conclusion
Becoming a phlebotomist technician in 2024 offers a rewarding career path with competitive salary prospects, especially for those certified and experienced. With the healthcare industry continuously growing, demand for skilled phlebotomists remains high. By understanding regional variations, acquiring relevant certifications, and gaining practical experience, you can significantly enhance your earning potential. Whether you’re just starting or seeking to advance your career, the opportunities in the phlebotomy field are promising. Take proactive steps today to maximize your salary and enjoy a fulfilling healthcare career in 2024!
https://phlebotomytechnicianschools.org/phlebotomist-technician-salary-how-much-do-they-earn-in-2024/
0 notes
Text
Opening Phlebotomy: Essential Medical Terminology Every Technician Should Know
Unlocking phlebotomy: Essential Medical Terminology Every Technician Should Know
Phlebotomy is a vital component of the healthcare system, serving as the bridge between patients and diagnostic laboratory testing. As healthcare continues to evolve, so dose the language used within it. Understanding essential medical terminology is crucial for phlebotomy technicians who want to excel in their careers. In this article, we’ll explore key terms related to phlebotomy, benefits of mastering this terminology, practical tips, and much more!
Why Medical Terminology Matters in Phlebotomy
Medical terminology is the foundation of dialog within the healthcare field. For phlebotomy technicians, a strong grasp of this language not only enhances interactions with patients and colleagues but also ensures accuracy in procedures and documentation. here are some reasons why it matters:
Improved Communication: Clear communication with nurses, doctors, and laboratory staff is crucial for effective patient care.
Enhanced Patient Experience: Understanding terms allows technicians to explain procedures and alleviate patient anxiety.
Accuracy in Documentation: Proper terminology helps in maintaining precise medical records.
Essential Medical Terminology for Phlebotomy Technicians
Below is a curated list of essential terms every phlebotomy technician should become familiar with:
Term
Definition
Phlebotomy
The practice of drawing blood for medical testing or donation.
Venipuncture
Insertion of a needle into a vein to collect blood.
Arterial Blood Gas (ABG)
A test measuring the acidity (pH) and levels of oxygen and carbon dioxide in the blood.
Anticoagulants
Medications that prevent blood clotting, often contained in blood collection tubes.
Hemolysis
The destruction of red blood cells, which can affect test results.
Lab Order
A request issued by a physician specifying tests to be performed on a sample.
Capillary Blood Collection
A method of obtaining blood via a small prick in the skin,commonly used in children.
Benefits of Mastering Medical Terminology
Being well-versed in medical terminology provides numerous benefits:
Increased Job marketability: Employers value candidates who can communicate effectively and understand medical jargon.
Enhanced Understanding of Procedures: Knowledge of terms can improve your comprehension of procedures and their implications.
Professional Development: mastery of terminology can lead to further educational opportunities and certifications.
Practical Tips for Learning Medical Terminology
Learning medical terminology can be overwhelming, but here are some practical tips to facilitate the process:
Create Flashcards: Write down a term on one side and its definition on the other for quick review.
Utilize Apps and Online Resources: There are many educational platforms that offer interactive quizzes and lessons.
Engage in Group Study: Collaborating with fellow students or colleagues can reinforce learning.
Practice Precise Usage: Use the terminology in your everyday conversations to build confidence.
Attend Workshops: Look for local or online workshops focusing on medical terminology.
Case studies: Real-Life Applications
To understand the importance of medical terminology in phlebotomy, consider the following case studies:
Case Study 1: Patient Interaction
A phlebotomy technician encountered a nervous patient unsure about the venipuncture procedure. By explaining the process using simple, clear medical terms, the technician was able to ease the patient’s anxiety and facilitate a triumphant blood draw.
Case Study 2: Collaboration with Healthcare Professionals
A technician who understood lab orders and anticoagulant types prevented a critical mishap by ensuring that the correct blood collection tubes were used for coagulation tests. This knowledge not only improved patient safety but also enhanced teamwork with lab staff.
First-Hand Experiences: Insights from Phlebotomy Technicians
Hearing from those in the field can provide invaluable insights. Here are a few experiences shared by seasoned phlebotomy technicians:
Jane D.: “Understanding medical terminology has enabled me to communicate effectively with nurses and doctors.It’s impressive how much smoother our processes have become.”
Mark R.: “When I started, I struggled with the terminology. Now, I feel confident explaining procedures to patients, which has really improved their experience.”
Conclusion: The Key to Success in Phlebotomy
Mastering essential medical terminology is an critically important investment for phlebotomy technicians. By understanding and using the language of medicine, technicians can enhance communication, improve patient care, and boost their professional development. Continuous learning and submission of these terms will not only benefit your career but also contribute to a more efficient healthcare environment. Embrace the journey of unlocking phlebotomy through the power of language!
This article provides a extensive overview of essential medical terminology for phlebotomy technicians, including its significance, terminology, benefits, and practical tips for mastering the vocabulary necessary for success in the field.
youtube
https://phlebotomytechnicianschools.net/opening-phlebotomy-essential-medical-terminology-every-technician-should-know/
0 notes
Text
Clinical Cardiac Nursing Concepts: Families in Crisis-Complex Health Problems I (Florida State College ICU – Plan of care Patient 1: newly admitted to ICU for pneumonia, hx: heart failure, COPD, renal disease, diabetes type 2 Strip indicates: Normal sinus rhythm, 80 bpm Assessment: pulses, shortness of breath, sugar Questions: medications? Oxygen at home? Recent hospitalization? Exertion on activity? Allergies? Onset of symptoms? Stage of COPD/ Heart failure? Where do you sleep (pillows?) Nursing interventions: 2L of oxygen, semi/high fowlers position, monitor LOC Expect vital signs to be: O2: 88-92. HR: 80. BP: elevated RR: increased Assessment findings expected: Lung auscultation (crackles), peripheral & respiratory edema, consolidation of chest x-ray Labs: CBC, BMP, Cardiac enzymes, BNP, possible ABG, urinalysis Diagnostics: Sputum culture, Chest Xray, Echocardiogram, Renal US Procedures: Medications: Mucomyst, Antibiotic, Diuretic (Furosemide), Pepcid, Beta blocker, ACE or ARB, Cardiac glycoside (Digoxin) Anticipated provider orders: Incentive spirometry, monitor intake and output, renal & cardiac diet (low fat, low sodium, DASH, Possible Venturi mask if O2 falling Consult: Cardiologist Patient 2: 55 years old, admitted 2 days ago for MI, stent placed, monitor for pseudo hematoma and infection-possible discharge home today. Strip: Symptomatic Bradycardia (40 bpm) Assess: verbal/ physical response, feel for diaphoresis, auscultate heart/ lungs, Vitals: HR: 40 BP: low Medications: beta blocker (when was last given), start Atropine 0.5 one time, IV fluids 500ml bolus Questions: Nursing interventions: stimulate, Educate: slow position changes Anticipated orders: Fluids, pacemaker Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Patient 3: SOB, extreme chest pressure, Vitals: hypertensive, tachycardiac, RR: 28, O2: 94 (Nasal cannula 3L) Monitor: STEMI Interventions: 12 lead EKG, MONA (morphine, oxygen, nitro, aspirin), LOC Assessment: chest pressure (men), epigastric, back pain & increasing fatigue (women), Labs: BMP, CBC, Cardiac enzymes, Coagulation, ABG’s, UA (drug toxicity) Procedures: Cardiac catheter (get consent), Patient 4: Palpitations, heart racing out of chest, pulse fast as fuck Monitor: SVT (Changes to Afib) Interventions: oxygen, IV access, try vagal maneuver, After vagal maneuver, went into AFIB (if AFIB and rapid, call is AFIB with RVR) Monitor: LOC (risk for stroke), Pulses (potential clot, MI), Medications: Anticoags (Warfarin, Eliquis), Diltiazem, FLECAINIDE, Possible heparin infusion (draw coags first) Diagnostics: TEE, Echocardiogram Labs: ABG, Cardiac enzymes, Coags Patient 5: Chest pain, SOB, dizziness, started a few minutes ago Monitor: Normal Sinus Rhythm Interventions: Oxygen, 12 lead EKG, Obtain IV, Blood Labs: Coags, CBC, BMP, Cardiac enzymes Possible causes: Anxiety, Heartburn, Esophageal spasm Patient 6: previous sinus rhythm, V-fib, now V-Tach V-tach with pulse: Cardioversion Patient 7: Asystole Assess patient, Check carotid pulse, non-shockable Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Call code: Epi 1 mg (2 mins CPR) Amiodarone 300mg (2 mins CPR) Epi 1 mg (2 mins CPR) Amiodarone 150mg (2 mins CPR) Epi 1m (2 mins CPR) Lidocaine 1mg/kg Assess H’s and T’s of ACLS Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Read the full article
0 notes
Text
Why is Amritam Heart Care Rajasthan's Best Choice for Heart Surgery?

Among all the heart hospitals in Jaipur, the recognized name belongs to Amritam Heart Care. Selecting a heart hospital in Jaipur requires consideration of both trustworthiness and technological capabilities for emergency care and complex surgeries, which Amritam Heart Care provides effectively.
Young professionals searching for the best heart hospital in Jaipur for heart surgery and long-term cardiac care will discover that Amritam Heart Care delivers the best services.
A Recognized Name Among the Best Heart Hospitals in Jaipur
Where Skill Meets Dedication
The top position of Amritam Heart Care as the best heart hospital in Jaipur results from premium patient treatment and state-of-the-art equipment with doctor expertise. Dr. Pankaj Goyal, a gold-medalist interventional cardiologist, leads the heart hospital in Jaipur. He provides elaborate medical attention to basic and intricate heart disease cases.
The Heart Hospital is guided by Dr. Pankaj Goyal, who holds the position of a renowned cardiologist.
Experience That Speaks for Itself
Dr. Pankaj Goyal has utilized his 15-year medical experience to transform Amritam Heart Care into the best heart hospital in Jaipur based on its dependable cardiac surgical services for patients. His expertise includes:
· Angiography & Angioplasty
· Pacemaker implantation
· Valve replacement
· Device closures like ASD/PDA/VSD
· Peripheral vascular surgery
Patients seeking the most dependable heart hospital in Jaipur trust Dr. Goyal because he maintains an unbroken record of excellence combined with his caring nature.
Amritam Heart Care Facilities
Amritam Heart Care Facilities functions as the top heart hospital in Jaipur.
The best heart hospital in Jaipur receives its name from its advanced facilities and modern diagnostic systems. The heart hospital in Jaipur provides these modern clinical facilities.
· Advance Cath Lab
· Ventilators & ABG machines
· 2D Echo and TMT
· Angiography & Angioplasty
· Pacemaker services
· IVUS/FFR/ROTABLATION
· Day Care Unit
· ABG Testing
Our tests can detect heart issues with Troponin I alongside NT-proBNP and PCT and the D-Dimer marker.
· Renal & Peripheral Angioplasty
· Heart failure programs
· CRTD/ICD device implantation
· Device closures (ASD/PDA/VSD)
· 24×7 Emergency Cardiac Response
· Ambulance and Pharmacy
· ICU, CCU, General Ward, and Luxury Rooms
The combination of these facilities positions Amritam as the top heart hospital in Jaipur to handle emergency cases and choose elective procedures.
Available 24/7 – Emergency Cardiac Services
This facility acts as a life-saving operation throughout each passing day.
The best heart hospital in Jaipur operates beyond emergency waiting periods to benefit its patients. Amritam maintains a continuous emergency service that provides quick medical care for patients experiencing heart attacks and strokes and urgent cardiac emergencies.
The hospital's prompt responsiveness positions Amritam as the most trustworthy heart hospital in Jaipur during critical situations.
Recover fast with Minimally Invasive Surgery
Modern Treatment, Minimal Pain
Advanced minimally invasive procedures represent one of the primary features of the best heart hospital in Jaipur at Amritam. These procedures result in:
· Smaller incisions
· Reduced pain
· Shorter hospital stays
· Quicker recovery
Patients select Amritam as their preferred heart hospital in Jaipur due to its reputation for safe and efficient heart surgery.
Personalized Cardiac Care
Every Heart Gets Unique Attention
Personalized medical treatment stands as the unique feature setting Amritam apart from all other heart hospitals in Jaipur. The medical institution develops unique care plans for each patient, starting at the disease recognition stage up until recovery after heart surgery.
The best heart hospital in Jaipur upholds this standard of personalized care.
Preventive Diagnostics and Regular Monitoring
The hospital maintains a continuous lead in heart problem prevention
People should consider the best heart hospital in Jaipur for both their healing needs and their ongoing preventive care requirements. Amritam offers diagnostics like:
· ECG
· Holter monitoring
· CT Coronary Angiography
· 2D Echo
· Stress tests
The heart hospital in Jaipur earns the trust of patients who want early detection because its diagnostic reports and analysis by experts are precise.
Expert Team for Critical and Surgical Cardiology
Top Specialists Under One Roof
The best heart hospital in Jaipur functions because of its team of medical specialists, including cardiologists, cardiac surgeons, anesthetists, critical care experts, and rehab professionals. And through their collective action, Amritam is recognized as the most dependable heart hospital in Jaipur for enduring medical care.
The hospital maintains a successful history of satisfied medical patients.
Patients Tell Success Stories That Make the Most Powerful Statements About Recovery
The families of hundreds of patients consider Amritam, the best heart hospital in Jaipur because they see its actual achievements rather than believing advertisements. Patients appreciate:
· Transparent billing
· Clear communication
· Clean, comfortable environment
· Successful recovery outcomes
Numerous surveys and hospital reviews show this heart hospital in Jaipur occupies the number 1 position.
Affordable Care, Transparent Costs
Quality That Doesn’t Break the Bank
At the best heart hospital in Jaipur, patients find high-quality care that doesn't lead to high costs. Amritam ensures:
· Affordable treatment options
· Transparent pricing
· Insurance support
· No hidden charges
The hospital's combination of affordable service rates and high-quality care has established it as a leading heart hospital center in Jaipur, preferred by patients from both middle-class and budget-sensitive backgrounds.
Strategically Located for Maximum Convenience
Central Location, Maximum Accessibility
The heart hospital in Jaipur, Amritam, operates at B-39 Prabhu Marg adjacent to A.C. Market in Tilak Nagar, where patients can reach easily through both public transportation and private modes. The hospital's reputation as the best heart hospital in Jaipur grows stronger because patients from various districts find easy access to its services.
Final Words: Choose the Best heart hospital in Jaipur.
Amritam Cares from the Heart
The selection of an appropriate healthcare facility for heart treatment becomes essential for the diverse geography of Rajasthan. The best heart hospital in Jaipur is Amritam Heart Care because it uses advanced technology to serve patients with a dedicated team and its mission is centered on patient care.
A consultation or emergency treatment requires you to search for Amritam, the recognized heart hospital in Jaipur.
Don't think too much and Take the First Step
Visit: B-39, Prabhu Marg, Tilak Nagar, Jaipur
Call: +91 8934076703
Email: [email protected]
The best heart hospital in Jaipur offers heart consultations through established appointments because your heart deserves quality care.
#heart hospital in jaipur#best heart hospital in jaipur#heart hospital in rajasthan#best heart hospital in rajasthan#heart surgery in jaipur#heart surgery in rajasthan#cardiac surgery hospital in jaipur#best cardiac surgery hospital in jaipur#heart hospital#jaipur heart hospital
0 notes
Text
Clinfinite Solutions Improves Blood Collection Procedures for Medical Reliability

1. Introduction
Blood collection is the cornerstone of modern medicine. From diagnosing diseases to monitoring treatment progress, this procedure plays a pivotal role in patient care. The accuracy and reliability of laboratory results heavily depend on proper blood collection techniques, making it an essential skill for healthcare professionals.
2. Preparing for Blood Collection
Proper preparation before blood collection ensures the safety and accuracy of the procedure.
Patient Identification and Consent
It is vital to verify the patient’s identity and obtain their informed consent before proceeding. Misidentification can lead to errors in diagnosis or treatment, making this step non-negotiable.
Gathering Necessary Equipment
The required materials include gloves, alcohol swabs, sterile needles, blood collection tubes, tourniquets, and labeling supplies. Ensuring that all equipment is sterile and readily available minimizes the risk of contamination and procedural delays.
Creating a Clean Environment
The area where blood is collected must be clean and sterile to prevent infection. Healthcare professionals should adhere to hygiene protocols, including handwashing and the use of personal protective equipment.
Special Precautions for Vulnerable Populations
Extra care is necessary for children, the elderly, or patients with specific conditions such as anxiety, needle phobia, or coagulation disorders. Using smaller needles or providing emotional reassurance can make the process smoother for these individuals.
3. Types of Blood Collection Methods
Different methods of blood collection are used depending on the purpose and clinical requirement.
Capillary Blood Collection
This method involves obtaining a small amount of blood through a finger prick or heel stick (for infants). It is commonly used for point-of-care testing, glucose monitoring, and neonatal screening.
Venipuncture
Venipuncture is the most common method of blood collection, where blood is drawn from a vein, typically in the arm. It is suitable for most laboratory tests, including complete blood counts (CBC) and biochemical analysis.
Arterial Blood Collection
Arterial blood is collected from an artery, usually for arterial blood gas (ABG) analysis. This method is less common and requires specialized training due to the higher risk involved.
Each method has its unique applications, and the choice depends on the specific diagnostic needs and patient factors.
4. Key Principles for Ensuring Accuracy and Safety
Adherence to specific principles ensures that blood collection is both accurate and safe:
Aseptic Technique: Maintaining sterility throughout the procedure prevents infection.
Proper Labeling: Accurately labeling samples with patient details avoids mix-ups in the lab.
Minimizing Hemolysis: Gentle handling of the sample ensures that red blood cells remain intact, preserving the integrity of the results.
Handling Patient Anxiety: Providing reassurance and clear explanations reduces stress and improves cooperation.
5. Challenges and Common Errors in Blood Collection
Despite its routine nature, blood collection can present challenges:
Difficult Vein Access: This can occur in dehydrated or obese patients, requiring advanced skills.
Hemolysis: Improper technique or excessive force can lead to sample contamination.
Improper Tube Handling: Using the wrong tube or failing to mix anticoagulant tubes properly can compromise test results.
Addressing these challenges requires ongoing training and adherence to best practices.
6. Conclusion
Blood collection is more than simply a standard medical practice; it is an essential component in the process of correct diagnosis and treatment. Healthcare workers may ensure that this process is safe, efficient, and trustworthy for all patients if they understand and follow the concepts stated above.
Accurate blood collection requires not only expertise, but also care, empathy, and precision. When executed appropriately, it leads to better patient outcomes and a more robust healthcare system.
1 note
·
View note
Text
vitals and what FiO2, chief complaint
labs WBC CBC
reason for admission and history
ABG?
ED plan
medication
discharge
0 notes
Text
Косметолог может изменить вашу жизнь: как найти проверенных мастеров в Киеве

Как острее почувствовать весну и радость пробуждения природы? Сделать новую прическу, купить новый наряд, улыбнуться своему похорошевшему отражению в зеркале после посещения косметолога. Бьюти-практики сегодня стали обычными и для ухоженных и успешных женщин, и для многих прогрессивных мужчин.
Учитывая скорость с которой увеличивается количество людей регулярно посещающих косметолога, можно сделать вывод, что у них есть на это важная причина. Что, помимо красоты, дают людям бьюти-практики, в пресс-центре Информатор рассказала психолог Алина Дейнека.
РАЗВИТИЕ И ЛЮБОВЬ
Люди хотят развиваться. Уход за своим телом – одно из подтверждений того, что в вашей жизни есть развитие. «При помощи косметологических процедур люди меняются: становятся красивее, ухоженнее. Бьюти-процедуры в хорошем косметическом кабинете, с использованием высококачественных препаратов дают ощущение, что ты заботишься о себе и подтверждение того, что ты сам для себя ценен», — говорит Алина Дейнека.
youtube
Когда мы любим – мы что-то хорошее делаем для объекта своей любви. Это работает как в отношениях с другими людьми, так и в отношениях с самим собой. «Как можно проявить любовь к себе? Ходить в спортзал, кормить себя вкусной и полезной едой, ухаживать за своей кожей и волосами. Все это акты любви к себе. Факты, подтверждающие, что ты сконцентрирован на своем мироощущении собственной ценности», — уверена психолог.
ОБЩЕСТВЕННЫЙ СТАТУС
Как гласит народная мудрость, встречают по одежке. Но в 21 веке ситуация поменялась. Сейчас встречают не только по одежке, но и по общей ухоженности, а также уровню уверенности в себе. «После процедур повышается настроение, что сопровождается выработкой организмом определенных гормонов. Человек ощущает себя красивее, чем раньше и получает комплименты от других людей, что важно для нас всех. Ведь даже если мы очень уверены в себе и очень себя любим, нам важно, что нашу внешность кто-то хвалит, что нам говорят комплименты. Это особенно приятно, когда вы знаете, что вы что-то сделали для достижения такого результата. Так шаг за шагом жизнь меняется к лучшему потому что взращивается любовь к себе», — говорит Алина Дейнека.
КОНКУРЕНТНОЕ ПРЕИМУЩЕСТВО
Мы еще помним времена, когда мужчины считали, что для того чтобы выполнить весь спектр ухода за собой, им достаточно принять душ и побриться. Сегодня мир изменился и следить за собой не стыдно никому, независимо от пола. «Бьюти-практики несут свои бонусы не только женщинам, но и мужчинам. Современный мир благодаря соцсетям стал очень визуален. Нам нравится, когда человек хорошо выглядит. И мужчины поняли, что ухоженный вид – это дополнительный плюс в глазах женщин, деловых партнеров, любых людей, чье мнение важно для вас. Бьюти-практики стали конкурентным преимуществом, ведь пока еще не все мужчины тщательно за собой ухаживают», — говорит Алина Дейнека.
КРИТИЧЕСКОЕ МЫШЛЕНИЕ
Оно необходимо, чтобы выбрать хорошего косметолога. В идеале такой специалист должен иметь высшее медицинское образование, – уверена руководитель обучающего центра для косметологов EMET Medicine Татьяна Епифанцева. «В обучающем центре для косметологов EMET Medicine мы постоянно об этом повторяем на курсах для специалистов как с высшим, так и со средним медицинским образованием», – говорит эксперт.
По словам Татьяны Епифанцевой, в EMET Medicine обязательно запрашивают у слушателей диплом о высшем медицинском образовании или другие необходимые документы для возможности посещения тех или иных обучений. Также по телефону компании можно проверить, действительно ли такой специалист проходил в это время обучение по определенной программе.
ДОСТИЖЕНИЯ НАУКИ
Сегодня в мире существует огромное количество косметологических препаратов. Некоторые из них привозят в Украину подпольно, без соблюдения норм транспортировки. Поэтому важно убедиться, что препараты, которые собирается использовать косметолог, сертифицированы и ввезены легально. «Вы можете попросить предоставить вам и сертификат качества, и договор с официальным дистрибьютором. Лучше озаботиться этим до процедуры, чтобы потом не сталкиваться с проблемами из-за использования некачественных или испорченных неправильным хранением и транспортировкой препаратов. Если продукция была куплена у компании «Эмет», официального представителя ряда ведущих мировых производителей косметических препаратов, их подлинность вы можете проверить на сайте компании», – говорит Татьяна Епифанцева.
Официальный импортер тщательно соблюдает условия хранения и транспортировки, а государство контролирует качество легально ввезённых препаратов. Компания «Эмет» продаёт препараты косметологам только после прохождения ими соответствующего обучения и наличия необходимых дипломов, если использование препарата того требует. Мало иметь качественный сертифицированный препарат, надо знать как им пользоваться», – уверена Татьяна Епифанцева.
ПАРТНЕРЫ “ЭМЕТ” В КИЕВЕ
Клиника Литус & Эстетик Ателье ул. Льва Толстого, 25/2 (095) 362-72-37
Справка: Эмет™ — эксклюзивный представитель в Украине и странах СНГ компаний ABG LAB (USA), Medytox (линейка дермальных филлеров Neuramis), профессиональной космецевтической линии Esse на основании живых пробиотиков и microbiome friendly пилинг систем Perfect Image
Эмет™ основал обучающий центр для косметологов EMET MEDICINE и ADASSA MEDICAL CLINIC.
Эмет™ выступает премиум партнером для специалистов эстетической медицины Украины и СНГ. Создает возможности профессионального развития, предлагая полный спектр инновационных эффективных косметологических препаратов. Создаёт уникальные программы личностного роста.
#косметолог#косметология#красота#красота и здоровье#клиника литус#Эмет#ABG LAB#ADASSA MEDICAL CLINIC#филлер#Esse
0 notes
Text
ok. alright ok
i am. not fit for working in a hospital setting
#turns out the cases were both patients who were in dire condition#ofc im sad that we have patients in such condition in the first place#but im also glad it wasnt any of our stable patients taking a turn for the worse#literally i havent slept well since i started this job#i keep thinking of our patients and what i can do to help every night#or what i ought to do the next day what i need to check etc#i cant wait to be working in a more stable unit tbh#internal medicine as a whole is severely understaffed and overworked#both doctors and nursing staff#we currently do SO much-we take blood we take ABGs and analyze them we sometimes even do the couriers job and take blood down to the lab#this past week our unit was FULL and new cases kept on coming and we had no where to acommodate them#its been the most hectic week of my life#im just glad my night shift was relatively calm when it comes to new cases#pls give some love to ur local doctors my dudes#these are hard times and i promise u theyre all trying their damnest to help#burrito talks medicine#delete later
5 notes
·
View notes
Text
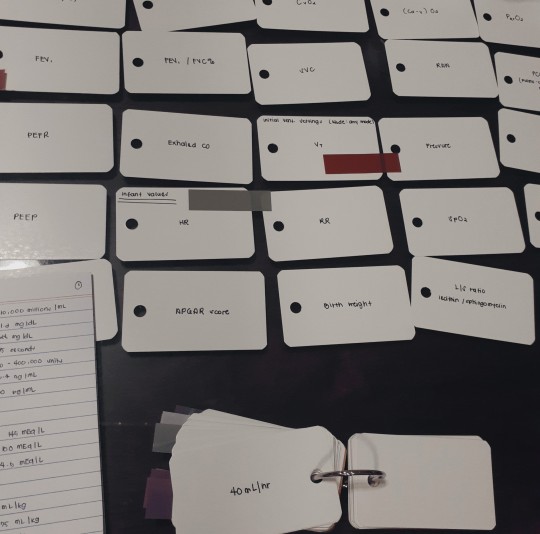


05.10.22
made flashcards for pt assessment, ABG, mech vent, normal lab values + infant lab values during the times I wasn't up to do any of the academic work I should be doing. really glad i'm done with my EKG notes, currently working on FRT II notes on perioperation and once i get done, i'll be moving on to my extra readings :)
and i should remember to also make flashcards on the lab values and indications on the decrease, increase and etc from FRT II for easy access and studying + i can put in my pocket/bag whenever
me this week: wants to splurge my non-existent money on stationary, stock up on the blank flashcards i've been using +++
#r ene#r-ene#respiratory therapy major#respiratory therapy student#respiratory student#respiratory therapy#studyblr#study#studies#student#uniblr#uni#college student#collegeblr#college studyblr#student life#studentlife#students#study aesthetic#study blog#study community#study life#study notes#study spot#study tumblr#studyblr community#studystudystudy#uni studyblr#uni student#university student
22 notes
·
View notes
Text
Family Fault Lines

Summary: Being 34 weeks pregnant isn’t easy. Being 34 weeks pregnant and an ER doctor really isn’t easy. But when a patient comes in, you need to make sure your husband is ok. Part six of The Fellow And The Intern. (Remember when this was a smut series?? Now there’s FEELINGS)
Words: 2.7k
Warnings: pregnancy, canon typical medical stuff, heart attacks, mentions of cheating, mentions of Connor Rhodes’ awful dad, traumatic childbirth, NICU time.
—
You were in the lounge, stretching your back out. Being pregnant was great, and by all accounts you’d had an easy pregnancy. But being an ER attending at 34 weeks pregnant was not easy. Natalie had shared her stories about how she dealt with the final trimester of her pregnancy with Owen, and it helped a little bit. Not a lot, but a bit. You wrapped the bump support around you, sighing as it helped redistribute the weight to make things a little easier. Once you stared at yourself in the mirror, and glanced at the rose gold silicone ring you wore in work, you left the room to go back to treating patients.
“Doctor Rhodes!” You turned to see Sylvie and Violet bringing in a patient. “Cornelius Rhodes, 72. Complaints of chest pain, previous history of cardiac episodes. Pulse 97, BP 130 over 90, resps 27. Gave nitro in the field, no response. Conscious and alert.” You grabbed the gurney, bringing your father in law into a trauma room, directing the team to move him over to the bed there.
“I want an ABG, lights, full cardiac enzymes, a full blood work up and get an EKG in here. Page cardiology, and put the cath lab on standby.” Your orders were obeyed, and you turned to your patient. “I’m Doctor Rhodes, an ER attending here. I’m going to look after you. When did this come on?”
His face was ashen as he struggled to breathe. “Forty...minutes. Connor?”
“I’ll see if he’s out of surgery. April, get me twenty migs of lasix, and two aspirin. I need cardiology here stat.” You checked the EKG, your worry increasing. He’d definitely had a heart attack. “I’ll be back in a minute, Mr. Rhodes. Nurse Sexton is fantastic.”
You went out to the nurses station, picking up the phone and calling Connor’s cell. If he wasn’t in surgery he always picked up.
“Rhodes.”
“Connor...” you trailed off, how could you tell him?
“Baby, are you ok? Is the baby ok?” He was frantic and you took a breath.
“We’re fine. Your dad is down here right now, I’m treating him for a heart attack. We’ve called down a cardiology consult, and the cath lab is ready for him. Sweetheart, he asked for you. I know how you feel, and you don’t have to, but I wanted to let you know.”
Your husband took a deep breath, and you could nearly feel his brain contemplating everything.
“I don’t know. Ugh. Can I have a hug when I come down?”
“You never need to ask for that. I love you, and I’ll see you in a few minutes.” You hung up, turning around and going back into the trauma room.
Cornelius was responding to the medication, his eyes closed as you checked him over. His heart rate was back to nearly normal, and you watched as the monitor beeped. Latham arrived in, and you turned to greet him.
“Is that your—“
“Yes, it’s Doctor Rhodes from trauma’s father. Looks like an MI, we’re waiting for the cardiac enzymes to confirm.” You watched as his eyes widened, and you shook your head subtly. He did an exam and you escorted him out of the trauma room to talk.
“Doctor, that’s your father in law. Should you be treating him?” You whirled around to Latham, feeling your baby kick your stomach in annoyance at moving quickly.
“I’ve never met him, Isidore. Connor doesn’t speak to his family, and I’m the attending on call right now. A big patient coming in when I’m on? I have to deal with him. And as far as I’m concerned, he’s no relation of mine or this baby.” You watched as his face softened.
“I’m sorry. Does Connor know he’s here?”
“Yes. He’s coming down once you bring him up. Are you doing a stent?”
“Probably. We’ll get in there and see what’s happening. Let him know I’ll deal with him directly.”
The two of you walked back in where Cornelius was awake again. “Mr. Rhodes, this is Doctor Latham, our head of cardio thoracic surgery. He’s going to take you upstairs to the cath lab so we can work out the best course of treatment. You’re in good hands with him.” You signed the chart to indicate you’d handed over control, before leaving the room and going back to the doctors lounge.
Connor was already in there, and you gave him the biggest hug you could with your belly in the way. You hadn’t realised how stressed you felt about treating his father until you held him and felt the stress melt away. Your baby always loved when Connor held you, kicking against your belly into Connor.
“The Squash is active today. You doing ok?” He wrapped his arm around you, settling you on the couch.
“I will be. It was weird, I know so much about this man and he’s never met me. Are you ok? It has to be a shock.”
Connor shrugged, his face slack. “Honestly? I don’t feel anything. The last time I saw him I punched him, so the fact I haven’t done that is a good thing. My then girlfriend slept with him.” You clutched your husbands hand, making sure he could feel you beside him.
“I’m just saying, we promised monogamy when we got together. I’ve no plans to ever change that.” Connor let out a low chuckle, relaxing into you.
“I love you so much. You know that, right? You and me and the Squash. None of the rest of it means anything. You two are the most important people in my life.” He leaned in to kiss you, one hand possessively on your bump while the other was wrapped around your ribs, fingers tapping gently on your tattoo.
“I love you too. I said better or worse, sickness and health, as long as we live. And we’ll get through this. And the next time someone from one of our families tries to do something ridiculous. How we ended up as the most sane ones I don’t know, but we did. And Squash is going to grow up knowing their parents are superheroes, and we love them so much.”
He kissed your temple, before helping you stand up to face the world again. You went back to treating patients, waiting to hear news about what had happened to Cornelius. As you were checking patient charts from your intern a woman walked over to you. As soon as you saw her face you knew it was Connor’s sister, and you steeled yourself.
“I’m looking for Doctor Rhodes who treated my father?” She asked, and you stood, introducing yourself.
“Your dad had a heart attack. He’s upstairs now with our cardiology team who are checking what needs to be done from here. I can bring you up to the cardiology waiting room if you’d like?” She nodded, accepting your offer. As you walked her through the ED you saw Connors eyes widen, but you shook your head slightly to stop him from coming over.
The two of you were standing in the elevator when Claire broke the silence. “When are you due?”
“Six more weeks. My husband and I are thrilled, he’s excited to be a dad.” And you were carrying her nibling in your stomach, no big deal.
“That’s fantastic. Is he in medicine?” Suddenly you realised her eyes were firmly on your ring, and you had a sneaking suspicion that she knew exactly who your husband was.
“He is.” The elevator doors opened, and you directed Claire to the waiting room, saying goodbye. All you wanted was to get back to your ER, where you ruled the roost and could work. As you stood there waiting for the elevator, you felt a wetness between your legs. No.
You made your way back downstairs, going to the doctors lounge. You’d thought your back pain was just normal end of pregnancy pain, but this was too early. You had six weeks left. You couldn’t give birth yet. A contraction hit your middle and you stopped, bending over in pain. It was happening and the baby was coming and you couldn’t do this yet. You had to keep them safe. The pain winded you, and the last thing you remembered was grabbing a chair as you collapsed.
Connor was the next one in the lounge, and his scream of your name and begging for help would be remembered by everyone in the ER that day. You were on your side, hand cradling your bump, and he immediately could see you were bleeding. He was made stand back as your friends - his friends, the people who’d watched you get married and had celebrated your pregnancy - crowded around you. He watched Natalie become a woman on a mission, whisking you up to the OR, taking charge and calling OB and trauma, anyone who could perform a c-section and get in there quickly to get in. He wanted to be in the OR, you’d planned for him to cut the cord and be there for the whole delivery, but instead he was left in the gallery watching as Natalie helped pull his baby from you and cut the cord.
There was no cry when you delivered. He watched the floppy pink body of your child be put into an incubator, so, so small. He’d only felt the baby kicking earlier that day, how had this happened? He held his breath, watching them perform CPR on the tiny infant until he heard a cry, tears shedding at the news. Once the baby was stable enough Nat wrapped them up, bringing them to the glass.
“You have a son, Connor,” she said through the microphone, watching the wonder fill his eyes. “We’re taking him to the NICU, you can see him when they finish here. It’s looking hopeful.” He tore his eyes away from the door his son disappeared through to stare at you, wishing he was in there. He was a surgeon. What was the good of being a surgeon if he couldn’t fix his wife? If he couldn’t help her when she needed it?
His tears stopped as he watched them finish stitching you up, your stomach still distended from the son who’d been in there less than an hour ago. He waited for Crockett to come over, holding his breath again for news.
“It was a placental abruption. She’s lucky she was on shift. We stopped the bleeding, and we avoided a hysterectomy. I’ll get her in recovery, you can see her in ten, ok? I just want to take out the ET tube and check sedation first.” Connor nodded, his eyes filled with thanks for the man who had been his rival but had since become a close friend.
He decided to go see their son first, before going to check on you when he was allowed. Connors one mistake was forgetting that Cardiology and OB were on the same floor. He stood outside the NICU, his eyes staring at the incubator with the carefully named “Baby Boy Rhodes”, watching Nat check him over. He didn’t notice people going past, but realised when someone stopped beside him. He turned around to see his sister standing there.
“That ER doc, she’s your wife, isn’t she?” Claire was never one for subtlety.
“Yeah. We got married eighteen months ago. That’s...that’s our son. She’s in ICU.” He saw Claire’s face fall, and she put her hand on her brothers shoulder.
“She’ll be fine. Does he have a name?”
“Not yet. I was convinced he’d be a girl. She told me I was wrong and I had to be a boy dad.” Connor let out a hoarse laugh, the last hour sinking in. He’d nearly lost you both.
“I’ll stay here to keep watch, if you want? Dad’s in recovery, it’s going to be a few hours. Go be with your wife.” Connor hugged his sister for the first time in years, before going the two floors down to the OR recovery room.
Crockett was still standing at your bed, watching your vitals cautiously. If he couldn’t do the surgery himself, Connor was glad Crockett did it. It made things a little bit easier.
“How is she?” His voice was low as he appeared, watching the blood slowly transfuse into your veins.
“She’s doing well. This is the last transfusion, after this it’ll just be fluids. We’ve got her on heavy pain meds, but fully removed sedation. She should wake up in the next while.” Crockett handed over the iPad, letting Connor see everything. It wasn’t pretty reading, seeing how low your blood pressure and pulse had fallen. But you were here and you were alive and Connor had his wife and son and even if it wasn’t the best circumstances the three of you would be ok.
You woke shortly after, going almost immediately from blissful unconsciousness to terror, realising that your stomach wasn’t moving and your organs didn’t feel squashed.
“The baby?” You asked, throat dry. Connor was beside you and his smile soothed you.
“He’s ok. Nat brought him to the NICU because he’s so small, but he’s ok. We have a son, Baby.” You grinned at his words, relaxing back into the bed. You had a son. Your baby was here and he’d be ok.
Connor gave you the details of what happened, of Nat and Crockett taking control and getting the two of you through, of his sister standing watch over your baby.
“We need a name,” you rasped, taking sips of cool water from the cup your husband held.
“I didn’t want to do it without you. We never talked about boys names.” You were unsure, and then it hit you.
“David Marcel Rhodes. We didn’t want a C name, David after Downey, and Marcel because I love Crockett but I’m not giving that name to our boy as a middle name. He saved my life, we should honour that.” You lay back and Connor pressed a kiss to your forehead.
“David Marcel Rhodes. A perfect name for a perfect boy.”
It took until the next morning before you were allowed be wheeled down to meet your son. Connor had spent the night with you, Nat and Will promising to keep an eye on David for you. Your friends were all waiting to meet your son and hear his name, and you grinned as Connor wheeled you in.
David was so small, but he was healthy. There was a minuscule nasal cannula helping him breathe, and apart from that he just had a heart monitor on. One of the nurses picked him up and laid him on your chest, and it finally felt real to you. You and Connor had made him in love and he was here at last.
“Hi David,” you whispered as you held back tears. “You gave me a scare, you know that? But we’re here and we’re ok, and I love you so much. Are you ready to meet your family?”
Connor waved in the awaiting ED staff, who looked at you with love and affection. You stayed in your chair as Connor cleared his throat.
“Meet our son, David Marcel Rhodes. Nat, Will, we were hoping you two would do us the honour of being his godparents?” They immediately agreed, hugging Connor and putting a hand on your shoulder before they had to go back to work. Crockett stood there, looking at the small child.
“You sure? It’s an honour.”
“He’s named after Connors mentor, and the man who made sure we both got to meet him. I can’t think of a better name for him. Thank you, Crockett,” you said, holding out the arm you weren’t cradling your son with for an awkward hug.
It took a week for you, and three more days for David, but finally the two of you left Gaffney as patients to your friends celebrating. Connors dad was still on the cardiac ward, but you ignored it. The past was the last, and David was your future.
#connor rhodes imagine#connor rhodes x you#connor rhodes x reader#Connor Rhodes fanfiction#Cíara writes#blame Liv
197 notes
·
View notes
Text
Opening the Essentials: A Comprehensive Guide to Phlebotomy for Beginners
Unlocking the Essentials: A Extensive Guide to Phlebotomy for Beginners
Phlebotomy is a vital skill in the medical field, crucial for the collection of blood samples necessary for diagnostic tests. If you’re considering a career in this sector, understanding the fundamentals of phlebotomy is essential. In this guide,we will cover everything a beginner needs to know about phlebotomy,including techniques,tools,requirements,and valuable tips to set you on your path to becoming a skilled phlebotomist.
What is Phlebotomy?
Phlebotomy involves the practice of drawing blood for various medical purposes, such as laboratory testing, transfusions, or research. Trained professionals, known as phlebotomists, play an essential role in the healthcare system, ensuring safe and efficient blood collection.
Why is Phlebotomy Critically important?
Diagnostic Purposes: Blood tests help diagnose diseases, monitor health conditions, and guide treatment decisions.
transfusions: Blood collection is crucial for patients requiring transfusions, surgeries, or organ transplants.
Research: Blood samples are often used in research to advance medical science and develop new treatments.
Benefits of Pursuing a Phlebotomy Career
Choosing a career in phlebotomy comes with numerous benefits, including:
High demand for skilled phlebotomists in healthcare.
Short training duration, often just a few months.
Opportunity for career advancement in the medical field.
Ability to work in diverse settings, such as hospitals, clinics, or labs.
Essential skills and Qualities of a Phlebotomist
To be a successful phlebotomist, certain skills and qualities are necessary:
Attention to Detail: Precision is key in following protocols and avoiding errors.
Dialog Skills: Ability to explain procedures to patients and reassure them.
Manual Dexterity: Skill in using needles and other tools effectively.
Empathy and Patience: Understanding patients’ concerns and providing a calming presence.
Phlebotomy Training and Certification Requirements
Becoming a phlebotomist typically involves several steps, including:
completion of High school Diploma: This is usually the minimum educational requirement.
Phlebotomy Training Program: Enroll in an accredited training program that covers both theory and practice.
certification: Obtain certification from a recognized organization, such as the American Society for Clinical pathology (ASCP).
State Licensure: Some states require additional licensure for phlebotomists.
Tools and Equipment Used in Phlebotomy
Tool
Description
Needles
Used for drawing blood from veins; available in multiple sizes.
Blood Collection Tubes
Special tubes that contain additives for preserving blood samples.
Lancets
Small devices used for fingerstick blood samples.
Tourniquets
Used to constrict blood flow and make veins more visible.
Syringes
Used for blood draws and sometiems for injections.
Common Phlebotomy Techniques
There are several techniques used in phlebotomy, with the following being the most common:
Venipuncture: Drawing blood from a vein, typically in the arm.
Capillary Collection: Obtaining small blood samples through fingersticks or heel sticks.
ABG Sampling: Arterial blood gas sampling for assessing lung function.
Practical Tips for Beginners in Phlebotomy
Here are some practical tips to keep in mind as you begin your phlebotomy journey:
Practice Makes Perfect: Gain as much hands-on practice as possible during your training.
Establish Rapport: Build trust with patients to reduce anxiety during blood draws.
Stay Organized: Keep your workspace tidy and familiar with all tools and procedures.
Adhere to Safety Protocols: Always follow universal precautions to ensure safety for you and the patients.
First-Hand Experience: A PhlebotomistS Story
Jane,a certified phlebotomist with three years of experience,shares her insights:
“When I first started in phlebotomy,I was nervous about drawing blood. However, after my training and practicing different techniques, I developed confidence.Today, I enjoy building connections with my patients and feel proud to play a role in their healthcare. Tips that helped me were remaining calm and patient, as well as always being prepared with the right tools.”
Conclusion
Phlebotomy is an essential part of healthcare, requiring specialized skills and knowledge.With the right training and a compassionate approach towards patients,you can become a skilled phlebotomist. Whether you are drawn to practical applications of medical science or the opportunity to contribute to patient care, pursuing a career in phlebotomy can be rewarding. Remember,successful phlebotomists not only draw blood but also build trust with patients,making their experience smoother and less intimidating.
youtube
https://phlebotomytechnicianschools.net/opening-the-essentials-a-comprehensive-guide-to-phlebotomy-for-beginners/
0 notes
Text
Oncology case study Nursing Research (California State University, Long Beach) Scan to open on Studocu Studocu is not sponsored or endorsed by any college or university Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Case Study Assignment 1 Case Study, Chapter 15, Oncology: Nursing Management in Cancer Care 1. Emanuel Jones, 60 years of age, is male patient diagnosed with small cell carcinoma. He underwent surgery in the past to remove the left lower lobe of his lung. He is receiving chemotherapy. Two weeks before a round of chemotherapy, a complete blood count with differential, and a renal and metabolic profile are obtained for the patient. The patient presents to the oncology clinic for chemotherapy with a temperature of 101°F. Further assessment reveals decreased breath sounds in the right base of the right lung, and a productive cough expectorating green colored mucus. The patient is short of breath and has a pulse oximetry reading that is SaO2 of 85% on room air. The patient has a history of benign prostate hypertrophy (BPH) and has complaints of urinary frequency and burning upon urination. The patient is admitted to the oncology unit in the hospital. The oncologist orders the following: blood, sputum, and urine cultures; and a chest x-ray. An x-ray of the kidneys, ureters, bladder (KUB) is ordered. An arterial blood gas (ABG) on room air, CBC with differential, and renal and metabolic profile are ordered. Oxygen is ordered to begin with nasal cannula at 2 L/min and titrate to keep SaO2 greater than 90%. A broad-spectrum antibiotic, levofloxacin 500 mg in 100 mL of NS is ordered to be administered IV over 60 minutes once daily. (Learning Objective 8) After examining the physician orders, in what sequence should the nurse provide the care to the patient admitted to the hospital? Give the rationale for the sequence chosen. First I would obtain, per the oncologist order, the ABGs on room air and it is done before providing oxygenation to ensure accurate reading. I would then ensure that the blood and CBC with differential, as well the renal and metabolic profiles are done. These are done before the medications to ensure that the blood results are accurate and not compromised by the antibiotics. Next I would begin oxygenation at 2 L/ min to make the patient comfortable and maintain the SaO2 at 90% . This will also make him more comfortable to breath and making it easier for the patient to provide sputum without running out of breath I would then do the sputum and urine cultures after the blood tests are drawn because these specimen will not be compromised with the other test done before hand Lastly I would give the patient his antibiotics administered through an IV because all labs have been done and the medication would not compromise anymore tests. Once all that is done, I would ensure that his chest and KUB x-rays are done all at once so that the patient is comfortable and ready to rest after the the x-rays. Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 On what areas should the nurse focus the assessment to detect potential complications for Mr. Jones? I would assess the color of the urine to monitor for any blood. I would also assess his chest expansion as well as his lung sounds. I would monitor his SaO2 constantly to make sure that it is above 90% along with the oxygenation. I would also make sure to monitor his fever temper and take necessary interventions to ensure it does not increase, and if it does notify the doctor. What patient education does Mr. Jones need from the nurse to help prevent the reoccurrence of an infection and to get treatment for an infection promptly? The nurse should teach the patient about hand washing with soap and water often, especially if he is sneezing or coughing in his hands/arms. If he is to touch surface areas, to make sure that he does not touch his face, eyes, nose or other potential portals of entries. The nurse should remind him to stay away from friends or family members that may be sick, and if he has to be around them to wear a mask. He should also be instruct to finish his antibiotics if he is to be discharged with a prescription to ensure the infection is completely gone. The patient should be taught the signs and symptoms of an infection so that if they are to occur he can seek help immediately. The nurse should also try and educate the family members so that they can know what to look for and to take precautions to avoid infecting the patient. Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Case Study, Chapter 16, End-of-Life Care 1. Joe Clark, 79 years of age, is a male patient who is receiving hospice care for his terminal illnesses that include lung cancer and chronic obstructive pulmonary disease (COPD). He developed bilateral pleural effusion (fluid that accumulates in the pleural space of each lung), which has compromised his lung expansion. He states that he is short of breath and feels anxious that the next breath will be his last. The patient is admitted to the hospital for a thoracentesis (an invasive procedure used to drain the fluid from the pleural space so the lung can expand). The thoracentesis is being used as a palliative measure to relieve the discomfort he is experiencing. Low dose morphine is ordered to provide relief from dyspnea or discomfort. The patient is prescribed Proventil (albuterol) inhaler 2 puffs per day, as needed, and Flovent (fluticasone propionate) inhaler 2 puffs twice a day. The patient has 2 L/min of oxygen ordered per nasal cannula as needed for comfort. (Learning Objective 9) What nursing measures should the nurse use to manage the patient’s dyspnea? The nurse should raise the HOB to make it easier for the patient to breath as well as constantly assessing his breathing to make sure he is provided with the oxygenation when needed. The nurse should also try and ease his anxiety which can make him feel that his dyspnea is worsening. The nurse can implement complementary and alternative therapies. Administer the patient’s medication, which would be his Flovent or his Proventil which is a bronchodilator. Keep everything within reach so patient can conserve energy. The patient complains that he has no appetite and struggles to eat and breathe. What nursing measures should the nurse implement to manage this physiologic response to the terminal illnesses? The nurse should first provide oral care which will hopefully make him find foods more appealing. Helping the patient ease his anxiety may also make it easier for him to eat. The nurse can ease his anxiety by using complementary and alternative therapies, such as guided imagery or playing music for the patient. Offering cold foods as sometimes they are more often tolerated than warm foods The nurse should also maintained his room clean without foul orders in the environment as it may make him nauseous and without appetite Offering the patients his meds before a meal, if possible, to alleviate respiratory issues and making it easier for him to eat. Suggesting smaller and more frequent meals Scheduling meals around family member schedule The patient may be offered fluids such as broths, jello, or puddings, or would ask him what he feels like eating or drinking and it can be anything he finds appetizing. Downloaded by James Mcknight ([email protected]) lOMoARcPSD|28323056 Read the full article
0 notes