#tumor biomarker
Explore tagged Tumblr posts
Text
youtube
#Nectin-4#urothelial carcinoma#metastatic cancer#platinum-based chemotherapy#bladder cancer#tumor biomarker#cancer prognosis#chemotherapy resistance#immune evasion#tumor progression#overall survival#progression-free survival#cancer treatment#oncology research#targeted therapy#personalized medicine#translational research#clinical outcomes#tumor biology#bladder cancer awareness.#Youtube
0 notes
Text
A recent review published in Cancers highlights the significant role of progranulin in cancer development. The growth factor has been found to promote tumor growth by enhancing cancer cell proliferation, migration, and resistance to chemotherapy. It also influences the tumor microenvironment and immune surveillance. Despite these findings, the molecular mechanisms behind progranulin’s oncogenic role are not yet fully understood. Researchers from the Sbarro Health Research Organization and Temple University suggest that further exploration of progranulin could lead to novel therapeutic strategies, including its potential as a diagnostic and prognostic marker for cancer.
#Progranulin#Cancer research#Tumor growth#Cancer development#Oncology#Tumor microenvironment#Chemotherapy resistance#Cancer cell proliferation#Molecular mechanisms#Cancer biomarkers#Cancer treatment#Immunotherapy#Cancer diagnostics#Prognostic markers#Cancer therapy#Sbarro Health Research Organization
1 note
·
View note
Text
Nuovo test per prevedere il rischio di cancro colorettale nei pazienti con malattie infiammatorie intestinali
Le malattie infiammatorie intestinali (IBD), tra cui la colite ulcerosa e la malattia di Crohn, sono condizioni croniche caratterizzate da un’infiammazione persistente del tratto gastrointestinale. I pazienti affetti da queste patologie presentano un rischio significativamente aumentato di sviluppare il cancro colorettale (CRC), soprattutto in presenza di infiammazione cronica di lunga durata e…
#biomarkers#epigenetica#fattore di rischio#flogosi cronica#malattia infiammatoria intestinale#oncogene#oncosoppressore#prevenzione#salute pubblica#Screening per il tumore del colon-retto#Tumore del colon-retto
0 notes
Text
Cancer Biomarkers Market is Trending by Increasing Personalized Care
Cancer biomarkers are biological molecules found in blood, tissues, or other body fluids whose presence indicates normal or abnormal processes, or conditions of concern regarding health. They are used in patient diagnosis, staging, treatment selection, monitoring of cancer progression or recurrence. Cancer biomarkers help in early cancer detection and assessing the likelihood of cancer recurrence after treatment. They play an important role in cancer risk assessment, screening, diagnosis, prognosis, and predicting treatment response for a variety of cancers. With increasing technological advancements, more personalized and targeted treatment options are emerging. This is fueling the demand for cancer biomarkers to help physicians detect cancer in early stages, determine the best treatment for each patient, monitor the effectiveness of treatment, and check for signs of recurrence.
The Global Cancer Biomarkers Market is estimated to be valued at US$ 25.60 billion in 2024 and is expected to exhibit a CAGR of 12% over the forecast period 2024 to 2031. Key Takeaways Key players operating in the Cancer Biomarkers are Schlumberger Limited, Rockwell Automation Inc., SIS-TECH Solutions LP, Emerson Electric Company, HIMA Paul Hildebrandt GmbH, Honeywell International Inc., Siemens AG, Yokogawa Electric Corporation, Schneider Electric SE, and ABB Ltd. The increasing prevalence of cancer globally has boosted the usage of cancer biomarkers. Rising demand for non-invasive diagnostic techniques along with increasing funding for cancer research are fueling the market growth. Growing awareness regarding the benefits of early detection of cancer is further driving the demand for cancer biomarkers. The growing Cancer Biomarkers Market demand for personalized medicine is also propelling the demand for cancer biomarkers. Personalized medicine focuses on classifying individuals based on their susceptibility and likely response to particular treatment. This allows clinicians to choose the most safe and effective treatment for each patient. Many companies are increasingly investing in biomarker research and development to introduce innovative cancer diagnostics and targeted therapies. The increasing global incidence of cancer has encouraged market players to expand their geographical presence. Emerging countries in Asia Pacific and Latin America offer lucrative opportunities for players due to growing healthcare investments, favorable government policies, and rising patient disposable incomes in these regions. Players are also focusing on partnerships, mergers, acquisitions, and collaborations with research institutes and biotechs to strengthen their product portfolios and geographical footprints. Market Key Trends Next-generation sequencing (NGS) has emerged as a key trend in the global cancer biomarkers market. NGS helps to discover and validate novel biomarkers by generating huge amounts of DNA sequence data from tumor and normal samples. It allows comprehensive genomic profiling of tumors to guide treatment decisions. NGS enables the analysis of multiple biomarkers simultaneously compared to traditional techniques. This allows physicians to obtain a complete molecular profile of the tumor specific to each patient for precision diagnosis and treatment selection.
Porter’s Analysis Threat of new entrants: High capital requirements and strong intellectual property rights protections limit new entrants in this competitive market.
Bargaining power of buyers: Large pharmaceutical companies have significant bargaining power over biotech companies developing novel biomarkers, putting pricing pressure.
Bargaining power of suppliers: Suppliers of analytical instruments and clinical testing kits have some bargaining power as they provide core tools and technologies needed by most companies in this space.
Threat of new substitutes: Biomarkers able to better diagnose, monitor, or predict therapeutic responses could emerge as substitutes over time.
Competitive rivalry: Intense competition exists among large pharmaceutical companies and smaller biotech firms to develop and commercialize novel cancer biomarker diagnostic tests and services. Geographical Regions North America currently accounts for the largest share of the global cancer biomarkers market, in terms of value, owing to the high adoption of advanced cancer diagnostic techniques and presence of leading biomarker testing companies in the region. The Asia Pacific market is expected to grow at the fastest rate during the forecast period, due to growing awareness regarding early cancer detection, increasing healthcare expenditure, and expanding base of pharma & biotech companies in China, India, and other Asia Pacific countries.
Get more insights on Cancer Biomarkers Market
For Deeper Insights, Find the Report in the Language that You want
French
German
Italian
Russian
Japanese
Chinese
Korean
Portuguese
Vaagisha brings over three years of expertise as a content editor in the market research domain. Originally a creative writer, she discovered her passion for editing, combining her flair for writing with a meticulous eye for detail. Her ability to craft and refine compelling content makes her an invaluable asset in delivering polished and engaging write-ups.
(LinkedIn: https://www.linkedin.com/in/vaagisha-singh-8080b91)

#Coherent Market Insights#Cancer Biomarkers Market#Cancer Biomarkers#Oncology Biomarkers#Tumor Markers#Cancer Diagnosis#Biomarker Discovery#Cancer Detection#Prognostic Biomarkers#Predictive Biomarkers
0 notes
Text
Personalized Approaches to Cutaneous Squamous Cell Carcinoma Treatment: Targeting Tumor Diversity
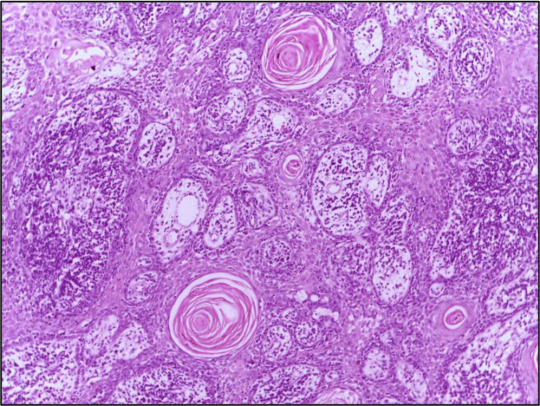
Cutaneous Squamous Cell Carcinoma (cSCC) is a heterogeneous disease characterized by diverse clinical and molecular features. Personalized treatment approaches that take into account the unique characteristics of individual tumors have emerged as a promising strategy to improve treatment outcomes and patient survival.
Understanding Cutaneous Squamous Cell Carcinoma: Cutaneous Squamous Cell Carcinoma (cSCC) is a type of skin cancer that arises from the malignant transformation of squamous cells in the epidermis or its appendages. It encompasses a spectrum of disease presentations, ranging from localized lesions to metastatic tumors with varying clinical behaviors.
Tumor Heterogeneity and Molecular Subtypes: Cutaneous Squamous Cell Carcinoma (cSCC) exhibits considerable heterogeneity at the molecular level, with distinct genetic alterations and signaling pathways driving tumor progression and metastasis. Molecular subtyping studies have identified different subgroups of cSCC tumors based on their genomic profiles, providing insights into tumor diversity and potential therapeutic targets.
Precision Medicine in cSCC Treatment: Precision medicine approaches aim to tailor treatment strategies to the specific molecular characteristics of individual tumors, allowing for more targeted and effective therapies. By identifying actionable mutations or biomarkers, clinicians can select therapies that are most likely to benefit patients while minimizing the risk of treatment-related toxicities.
Genomic Profiling and Biomarker Identification: Advances in genomic sequencing technologies have enabled comprehensive profiling of cSCC tumors, revealing recurrent mutations in genes involved in cell cycle regulation, DNA repair, and immune evasion. Biomarker identification efforts seek to identify predictive markers of treatment response and prognosis, guiding treatment decisions in personalized medicine.
Get More Insights On This Topic: Cutaneous Squamous Cell Carcinoma
#Cutaneous Squamous Cell Carcinoma#Skin Cancer#Tumor Heterogeneity#Precision Medicine#Molecular Subtypes#Targeted Therapy#Immunotherapy#Biomarker Identification#Personalized Treatment
0 notes
Text
"A medical technology company in Australia is aiming for a world-first: it wants to launch a blood test for endometriosis (sometimes called 'endo' for short) within the first half of this year [2025].
In a recent peer-reviewed trial, its novel test proved 99.7 percent accurate at distinguishing severe cases of endometriosis from patients without the disease but with similar symptoms.
Even in the early stages of the disease, when blood markers may be harder to pick out, the test's accuracy remained over 85 percent.
The company behind the patent, Proteomics International, says it is currently adapting the method "for use in a clinical environment," with a target launch date in Australia for the second quarter of this year [2025].
The test is called PromarkerEndo.
"This advancement marks a significant step toward non-invasive, personalized care for a condition that has long been underserved by current medical approaches," managing director of Proteomics International Richard Lipscombe said in a press release from December 30.
Endometriosis is a common inflammatory disease that occurs when tissue similar to the lining of the uterus grows in other parts of the body, forming lesions. The disease can be very painful, and yet the average patient often suffers debilitating symptoms for up to seven years before they are properly diagnosed.
While there are numerous reasons for such a long delay, symptoms of endometriosis are often highly variable, unpredictable, difficult to measure or describe, and dismissed or overlooked by doctors.
Today, the only definitive way to diagnose endometriosis is via keyhole surgery called a laparoscopy, which is expensive, invasive, and carries risks.
Proteomics International is hoping to change that.
In collaboration with researchers at the University of Melbourne and the Royal Women's Hospital, the company compared the bloodwork data from 749 participants of mostly European descent.
Some had endometriosis and others had symptoms that were similar to endo but without the lesions. All participants had a laparoscopy to confirm the presence or absence of the disease.
Sifting through the bloodwork, researchers ran several different algorithms to figure out which proteins in the blood were best at predicting endometriosis of varying stages.
Building on previous research, a panel of 10 proteins showed a "clear association" with endometriosis.
For years now, scientists have investigated possible blood biomarkers of endometriosis to see if they could differentiate between those who have endo and those who do not. Similar to cancerous tumors, endo lesions can establish their own blood supply, and if cervical cancer can be diagnosed via a blood test, it seemed possible that endometriosis could be, too...
Proteomics International claims patents for PromarkerEndo are "pending in all major jurisdictions," starting first in Australia.
It remains to be seen if the company's blood test lives up to the hype and is approved by the Australian Therapeutic Goods Administration (TGA). But that's not outside the realm of possibility.
In November of 2023, some researchers predicted that a "reliable non-invasive biomarker for endometriosis is highly likely in the coming years."
Perhaps this is the year."
-via ScienceAlert, January 9, 2025
--
Note: As someone with endometriosis, let me say that this is a HUGE deal. The condition is incredibly common, incredibly understudied, and incredibly often dismissed. Massive sexism at work here.
I got very lucky and got diagnosed after about 6 months of chronic pain (and extra extra lucky, because my pain went away with medication). But as the article says, the average time to diagnosis is seven years.
Being able to confirm endometriosis diagnoses/rates without invasive surgery will also lead to huge progress in studying/creating treatments for endo.
And fyi: If you have a period that is so painful that you can't stand up, or have to go home from school/work, or vomit, or anything else debilitating (or if any of those things apply if you forget to take pain meds), that is NOT NORMAL, and you should talk to a competent gynecologist asap.
#endometriosis#periods#menstrual cycle#menstruation#chronic pain#period pain#period problems#period cramps#medical news#medical sexism#australia#good news#hope
4K notes
·
View notes
Text
We aim to Prevent You From Falling Sick At An Early Stage | FMD
When an astrologer predicts future events for you, the sense of excitement and amazement is undeniable, isn't it? It's an experience that captivates and intrigues, offering a glimpse into the possibilities that lie ahead. When both positive and negative factors that could impact your life are known beforehand, you are better equipped to make informed decisions.
But what can happen when you know the future of your health? Knowing the future of your health empowers you to proactively make the right decision that positively influences your overall well-being. It allows you to adopt preventive measures, make lifestyle adjustments, and prioritize self-care, ultimately steering you toward a healthier and more fulfilling life. By gaining insights into potential health outcomes, you make rational decisions and actively take part in shaping a future where your well-being is your priority.

How First Medical Diagnostics Empowers Early Detection
At First Medical Diagnostics, we're more than just a healthcare provider; we're your partners in well-being. We understand that staying healthy isn't just about reacting to illness – it's about being proactive, taking charge, and living your best life. Our mission is deeply rooted in this philosophy. We're not only here to diagnose diseases and symptoms but to be your true companion in prevention.
Imagine a healthcare experience where we work together to identify potential health issues in their earliest stages. It's like having a personalized early warning system for your well-being. By catching concerns before they have a chance to disrupt your life, we empower you to stay in control and live each day to the fullest.
Why Early Detection Matters?
Early detection is a game-changer in healthcare. It can significantly improve patient outcomes and increase the chances of successful treatment. By identifying diseases or conditions at a primary stage, healthcare professionals can intervene sooner and implement preventive measures. It can also lead to cost savings, as treating a disease in its early stages is often less expensive than treating it in its advanced stages.
Early detection of a health problem leads to prompt intervention, often with less invasive and more effective options. This can result in better health outcomes and a higher chance of successful treatment. For example, if a person notices early symptoms of cancer and seeks medical attention, they may be able to receive targeted therapy or surgery, which can be less invasive than later-stage treatments like chemotherapy. For this, we offer a PanTum Test that helps in the early detection of cancer cells and prevents you from suffering in the future.
Better treatment results: There is a substantial increase in the chance of a full recovery and a successful course of treatment with early intervention. Early intervention allows for the identification and management of health conditions at their early stages, when they are most treatable. By detecting and addressing problems early on, medical professionals can prevent the progression of diseases and minimize potential complications.
Reduced burden on healthcare systems: By preventing serious illnesses, we alleviate the strain on hospitals and resources, benefiting everyone. This reduction in burden allows healthcare systems to allocate their resources more efficiently, ensuring that those who truly need medical attention receive it promptly. It also helps in decreasing waiting times for treatments and surgeries, improving overall patient care.
Specialized Tests, Powered by German Expertise:
Our specialized tests bring you the latest in German expertise, ensuring accuracy and reliability. We don't stop at just offering test results instead our group of medical specialists will assist you at every turn, providing:
Professional interpretation of your test results: We'll discuss the significance of your test results and how they may affect your health.
Personalized consultations: After talking about your lifestyle and risk factors, we'll create a strategy specifically for controlling your health and lowering your chance of getting sick in the future.
After the initial consultation, we're here to help with ongoing support and monitoring. We'll make any necessary changes to your plan and still provide ongoing monitoring.
Investing in Your Future Well-Being
Investing in early detection is a future-oriented investment. It's about assuming responsibility for your health and giving yourself the tools you need to live a longer, better life. First Medical Diagnostics is dedicated to giving you the resources required to do this.
We believe that everyone should have access to state-of-the-art medical treatment and individualized diagnostics. For this reason, we provide customizable testing plans and alternatives to fit your requirements and price range.
For more information,
Call us at +91 8800929600
Visit us at www.fmdindia.in
#pantum#fmd#fmdindia#cancer#cancerdetection#earlydetectioncancertest#cancertest#cancerprevention#TKTL1#immunecells#macrophages#Apo10#multitumor#enzymes#biomarkers#monocites#EDIM#tumor#health#prevention#curedisease#curable#cure#food
1 note
·
View note
Text
Liquid Biopsy: Evolving Trends in Breast Cancer
The global breast cancer liquid biopsy market size is expected to reach USD 1.7 billion by 2030, expandingat a CAGR of 22.7% from 2022 to 2030, according to a new report by Grand View Research, Inc. The growth is attributed to the rising preference for non-invasive methods, rising awareness of early diagnosis and treatment, and rising prevalence of breast cancer. For instance, according to WHO, in 2020, globally, 685,000 women lost their lives to breast cancer, and 2.3 million women were affected by it. Liquid biopsies have been suggested as a revolutionary technique for the early identification of breast cancer, which boosts its adoption and spurs growth. With the increasing prevalence of breast cancer, there is a high demand to provide proper diagnostics tools for detecting cancer at an early stage and early treatment.
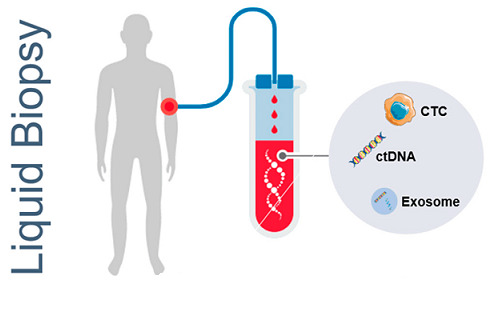
Breast Cancer Liquid Biopsy Market Report Highlights
In 2021, the circulating tumor cells segment held a dominant revenue share owing to the effectiveness and precision offered by CTCs in the detection of cancer
The early detection segment is projected to grow at the fastest CAGR over the forecast period, owing to the increasing adoption of liquid biopsy in early diagnosis of cancer and the rising need to provide effective treatment
Treatment selection was the highest revenue-generating segment in 2021 owing to the availability of a high number of products that aid treatment selection
Asia Pacific is expected to witness the fastest growth during the forecast period owing to increasing prevalence, improving healthcare infrastructure, and growing population
Gain deeper insights on the market and receive your free copy with TOC now @: Breast Cancer Liquid Biopsy Market Report
There has been increasing R&D in the field of diagnostics to cater to the rising demand. For instance, in June 2022, according to study findings from BioFluidica, patients with HER2-positive breast cancer had success rates while receiving tailored HER2-directed therapy.The clinical significance of liquid biopsy is becoming more well-known as a result of ongoing developments in related fields. Additional interventional clinical trials and the creation of an algorithm to properly combine circulating biomarkers are required to make these technologies widely accessible.
A less intrusive technique for identifying non-hematological malignancies has been developed as a result of technological breakthroughs in continuing research on circulating biomarkers. Compared to traditional tumor biopsy, liquid biopsy is thought to be a promising option for patient monitoring in real time. For instance, in April 2022, Epic Sciences, Inc., launched DefineMBC, a blood test based on liquid biopsy technology for the diagnosis of metastatic breast cancer to its CLIA laboratory portfolio.
#Breast Cancer#Liquid Biopsy#Cancer Detection#Biomarkers#Medical Diagnosis#Precision Medicine#Cancer Screening#Tumor Markers#Molecular Diagnostics#Healthcare Technology#Cancer Research#Liquid Biopsy Market#Oncology#Personalized Medicine#Biotechnology
0 notes
Text
How AI is Being Used to Predict Diseases from Genomic Data

Introduction
Ever wonder if science fiction got one thing right about the future of healthcare? Turns out, it might be the idea that computers will one day predict diseases before they strike. Thanks to Artificial Intelligence (AI) and genomics, we’re well on our way to making that a reality. From decoding the human genome at lightning speeds to spotting hidden disease patterns that even experts can’t see, AI-powered genomics is revolutionizing preventative care.
This article explores how AI is applied to genomic data, why it matters for the future of medicine, and what breakthroughs are on the horizon. Whether you’re a tech enthusiast, a healthcare professional, or simply curious about the potential of your own DNA, keep reading to find out how AI is rewriting the rules for disease prediction.
1. The Genomic Data Boom
In 2003, scientists completed the Human Genome Project, mapping out 3.2 billion base pairs in our DNA. Since then, genomic sequencing has become faster and more affordable, creating a flood of genetic data. However, sifting through that data by hand to predict diseases is nearly impossible. Enter machine learning—a key subset of AI that excels at identifying patterns in massive, complex datasets.
Why It Matters:
Reduced analysis time: Machine learning algorithms can sort through billions of base pairs in a fraction of the time it would take humans.
Actionable insights: Pinpointing which genes are associated with certain illnesses can lead to early diagnoses and personalized treatments.
2. AI’s Role in Early Disease Detection
Cancer: Imagine detecting cancerous changes in cells before a single tumor forms. By analyzing subtle genomic variants, AI can flag the earliest indicators of diseases such as breast, lung, or prostate cancer. Neurodegenerative Disorders: Alzheimer’s and Parkinson’s often remain undiagnosed until noticeable symptoms appear. AI tools scour genetic data to highlight risk factors and potentially allow for interventions years before traditional symptom-based diagnoses. Rare Diseases: Genetic disorders like Cystic Fibrosis or Huntington’s disease can be complex to diagnose. AI helps identify critical gene mutations, speeding up the path to diagnosis and paving the way for more targeted treatments.
Real-World Impact:
A patient’s entire genomic sequence is analyzed alongside millions of others, spotting tiny “red flags” for diseases.
Doctors can then focus on prevention: lifestyle changes, close monitoring, or early intervention.
3. The Magic of Machine Learning in Genomics
Supervised Learning: Models are fed labeled data—genomic profiles of patients who have certain diseases and those who do not. The AI learns patterns in the DNA that correlate with the disease.
Unsupervised Learning: This is where AI digs into unlabeled data, discovering hidden clusters and relationships. This can reveal brand-new biomarkers or gene mutations nobody suspected were relevant.
Deep Learning: Think of this as AI with “layers”—neural networks that continuously refine their understanding of gene sequences. They’re especially good at pinpointing complex, non-obvious patterns.
4. Personalized Medicine: The Future is Now
We often talk about “one-size-fits-all” medicine, but that approach ignores unique differences in our genes. Precision Medicine flips that on its head by tailoring treatments to your genetic profile, making therapies more effective and reducing side effects. By identifying which treatments you’re likely to respond to, AI can save time, money, and—most importantly—lives.
Pharmacogenomics (the study of how genes affect a person’s response to drugs) is one area booming with potential. Predictive AI models can identify drug-gene interactions, guiding doctors to prescribe the right medication at the right dose the first time.
5. Breaking Down Barriers and Ethical Considerations
1. Data Privacy
Genomic data is incredibly personal. AI companies and healthcare providers must ensure compliance with regulations like HIPAA and GDPR to keep that data safe.
2. Algorithmic Bias
AI is only as good as the data it trains on. Lack of diversity in genomic datasets can lead to inaccuracies or inequalities in healthcare outcomes.
3. Cost and Accessibility
While the price of DNA sequencing has dropped significantly, integrating AI-driven genomic testing into mainstream healthcare systems still faces cost and infrastructure challenges.
6. What’s Next?
Realtime Genomic Tracking: We can imagine a future where your genome is part of your regular health check-up—analyzed continuously by AI to catch new mutations as they develop.
Wider Disease Scope: AI’s role will likely expand beyond predicting just one or two types of conditions. Cardiovascular diseases, autoimmune disorders, and metabolic syndromes are all on the list of potential AI breakthroughs.
Collaborative Ecosystems: Tech giants, pharmaceutical companies, and healthcare providers are increasingly partnering to pool resources and data, accelerating the path to life-changing genomic discoveries.
7. Why You Should Care
This isn’t just about futuristic research; it’s a glimpse of tomorrow’s medicine. The more we rely on AI for genomic analysis, the more proactive we can be about our health. From drastically reducing the time to diagnose rare diseases to providing tailor-made treatments for common ones, AI is reshaping how we prevent and treat illnesses on a global scale.
Final Thoughts: Shaping the Future of Genomic Healthcare
AI’s impact on disease prediction through genomic data isn’t just a high-tech novelty—it’s a turning point in how we approach healthcare. Early detection, faster diagnosis, personalized treatment—these are no longer mere dreams but tangible realities thanks to the synergy of big data and cutting-edge machine learning.
As we address challenges like data privacy and algorithmic bias, one thing’s certain: the future of healthcare will be defined by how well we harness the power of our own genetic codes. If you’re as excited as we are about this transformative journey, share this post, spark discussions, and help spread the word about the life-changing possibilities of AI-driven genomics.
#genomics#bioinformatics#biotechcareers#datascience#biopractify#aiinbiotech#biotechnology#bioinformaticstools#biotech#machinelearning
4 notes
·
View notes
Text
youtube
#Tumor biology#cancer progression#tumor microenvironment#metastasis#oncogenes#tumor suppressor genes#angiogenesis#apoptosis#cell proliferation#cancer biomarkers#tumor heterogeneity#cancer stem cells#immuno-oncology#molecular oncology#cancer metabolism#genomic instability#drug resistance#tumor invasion#epigenetic alterations#cancer immunotherapy.#Youtube
2 notes
·
View notes
Text
Mark your calendar for these health tech conferences in 2024-2025

- By InnoNurse Staff -
Interested in health technology-related events for fall 2024 and 2025? Fierce Healthcare has compiled a list of key conferences, both virtual and in-person, scheduled for the upcoming seasons.
Read more at Fierce Healthcare
///
Other recent news and insights
Lapsi transforms the stethoscope into a health tracking data platform (TechCrunch)
UK: The Department of Health and Social Care set to review clinical risk standards for digital health technologies (Digital Health)
AI-based cancer test determines if chemotherapy is needed (The Financial Express)
New tool enhances microscopic imaging by eliminating motion artifacts (UC Berkeley/Tech Xplore)
Researchers integrate a fast optical coherence tomography system into neurosurgical microscopes (Optica)
AI model achieves clinical-expert-level accuracy in complex medical scans (UCLA/Medical Xpress)
Bioinformatics reveals the hidden prevalence of repeat expansion disorders (Queen Mary University of London/Medical Xpress)
Ultrasound detects 96% of ovarian cancers in postmenopausal women (University of Birmingham)
AI ‘liquid biopsies’ using cell-free DNA and protein biomarkers could improve early ovarian cancer detection (Johns Hopkins Technology Ventures)
Mammograms show potential for detecting heart disease (UC San Diego/Medical Xpress)
IMRT and proton therapy provide similar quality of life and tumor control for prostate cancer patients (American Society for Radiation Oncology/Medical Xpress)
Machine learning enhances MRI video quality (Graz University of Technology/Medical Xpress)
Robotic surgery for colorectal cancer reduces pain and accelerates recovery (Beth Israel Deaconess Medical Center)
Global human brain mapping project releases its first data set (Allen Institute)
AI could speed up PCR tests, aiding faster DNA diagnostics and forensics (Flinders University/Medical Xpress)
AI-powered apps may detect depression through eye snapshots (Stevens Institute of Technology/Medical Xpress)
#events#health tech#digital health#medtech#biotech#health informatics#data science#neuroscience#imaging#radiology#diagnostics#ai#robotics#cancer#lapsi#government#uk
2 notes
·
View notes
Text
Le caratteristiche dell'alfa-fetoproteina nella diagnostica medica: dai meccanismi cellulari al ruolo di biomarker
Alfa-fetoproteina: nozioni generali L’alfa-fetoproteina (AFP) è una glicoproteina che gioca un ruolo fondamentale nella biologia umana, specialmente durante lo sviluppo embrionale e fetale. È considerata un importante marker clinico sia per condizioni fisiologiche normali che patologiche, come nel caso di specifiche malattie epatiche e neoplasie. L’AFP è una proteina di circa 590 aminoacidi, con…
#alfa-fetoproteina#apoptosi#autoimmunità#biomarker#carcinoma epatico#cellule tumorali#cirrosi epatica#espressione genica#fattore di rischio#immunosoppressione#proliferazione cellulare#prostaglandina E2#signaling pathway#sistema immunitario#tumore testicolare
0 notes
Text
Cancer Biomarkers Market Poised to Exhibit a CAGR of 7.3% by 2031

Cancer biomarkers are substances whose presence is indicative of some biological condition, processes, or pathology. They can be used for cancer diagnosis or checking effectiveness of treatment. Being non-invasive procedures, demand for cancer biomarkers is growing rapidly. They aid in early detection of cancer during screening programs and reduce cost of cancer treatment. Global cancer biomarkers market is estimated to be valued at USD 25.60 Bn in 2024 and is expected to reach USD 59.01 Bn by 2031, exhibiting a compound annual growth rate (CAGR) of 12.7% from 2024 to 2031.
Key Takeaways Key players operating in the Cancer Biomarkers market are Schlumberger Limited, Rockwell Automation Inc., SIS-TECH Solutions LP, Emerson Electric Company, HIMA Paul Hildebrandt GmbH, Honeywell International Inc., Siemens AG, Yokogawa Electric Corporation, Schneider Electric SE, and ABB Ltd. They are investing heavily in biomarker detection methods and panels targeting unmet clinical needs. Rising incidence of cancer across the world is driving for Cancer Biomarkers Market Demand. Biomarkers help in cancer screening and detecting disease at early stages. This improves treatment outcomes and survival rates significantly. Initiatives by governments and cancer councils to spread cancer awareness are also boosting the market. Global expansion strategies adopted by leading players are expected to support market growth during the forecast period. They are expanding their footprint in emerging markets of Asia Pacific, Latin America, and Middle East & Africa to tap the high growth opportunities. This will increase access to advanced cancer diagnostic solutions. Market Key Trends The use of artificial intelligence and machine learning algorithms to discover novel biomarkers from large datasets is a key trend in the market. It helps accelerate the process of biomarker identification. Genomic and proteomic biomarkers are also gaining traction for their role in cancer detection as well as tracking cancer progression and drug response. Development of personalized diagnostics based on multi-omics approaches and liquid biopsy tests are some other trends expected to shape the market.
Porter’s Analysis Threat of new entrants: The cancer biomarkers market requires huge capital investments in R&D for developing novel biomarkers and testing kits which makes the entry difficult for new players. Bargaining power of buyers: Buyers have moderate bargaining power in this market as there are many players offering similar cancer biomarker testing services. Bargaining power of suppliers: Suppliers have low bargaining power due to availability of alternative raw material suppliers in the market. Threat of new substitutes: Substitutes have low threat as there are limited substitutes available for cancer biomarker tests. Competitive rivalry: The market is highly competitive due to presence of many global as well as regional players. Geographical Regions North America region accounts for the largest share of the cancer biomarkers market in terms of value due to presence of major players, rising healthcare expenditure and increasing prevalence of cancer in the region. Asia Pacific is expected to grow at the fastest CAGR during the forecast period owing to increasing awareness regarding cancer, improving healthcare infrastructure and rising access to diagnostic services in emerging economies of China and India in this region.
Get more insights on Cancer Biomarkers Market
About Author:
Money Singh is a seasoned content writer with over four years of experience in the market research sector. Her expertise spans various industries, including food and beverages, biotechnology, chemical and materials, defense and aerospace, consumer goods, etc. (https://www.linkedin.com/in/money-singh-590844163)
#Coherent Market Insights#Cancer Biomarkers Market#Cancer Biomarkers#Oncology#Cancer Diagnostics#Molecular Markers#Tumor Markers#Biomarker Discovery#Predictive Biomarkers
0 notes
Text

Targeted Therapy:
Precision or targeted therapies encompass medications engineered to disrupt specific molecules implicated in the progression of cancer. In contrast to conventional chemotherapy's broad impact on fast-dividing cells, precision therapies selectively target cancer cells while preserving healthy tissue integrity. These drugs aim at various molecular pathways involved in cancer development, including signaling cascades, angiogenesis, and DNA repair mechanisms.
An illustrative example of precision therapy is the application of tyrosine kinase inhibitors (TKIs) in treating specific cancer types like non-small cell lung cancer (NSCLC) and chronic myeloid leukemia (CML). TKIs hinder the activity of particular tyrosine kinases, crucial enzymes in cancer-promoting cell signaling pathways. By obstructing these kinases, TKIs effectively inhibit tumor growth and extend patient survival.
Likewise, monoclonal antibodies represent another form of precision therapy, binding to specific proteins on cancer cell surfaces, initiating immune-mediated tumor destruction. These antibodies can also be combined with cytotoxic agents or radioactive isotopes to heighten their anti-cancer properties.
Personalized Chemotherapy:
While precision therapies are central to personalized medicine, tailored chemotherapy remains vital in cancer treatment. Tailored chemotherapy involves customizing traditional cytotoxic drugs to suit the unique characteristics of each patient's tumor. This may involve adjusting drug doses, combining different agents, or selecting chemotherapy regimens based on tumor biology and patient-specific factors.
One approach to tailored chemotherapy utilizes predictive biomarkers to identify patients likely to respond positively to specific chemotherapy drugs. For example, certain mutations in the BRCA genes are associated with increased sensitivity to platinum-based chemotherapy in breast and ovarian cancers. By identifying these biomarkers, oncologists can identify patients who will benefit most from a particular chemotherapy regimen while minimizing potential toxicity for others.
Furthermore, progress in pharmacogenomics, which explores how genetic variations affect drug response, has provided insights into individual differences in drug metabolism and toxicity. By analyzing patients' genetic profiles, oncologists can predict their likelihood of experiencing adverse effects or poor response to chemotherapy drugs, enabling personalized dose adjustments and treatment optimization.
Early cancer detection and management is important for an improved success rate in cancer treatment. You can undergo regular health checkups to get diagnosed for cancer at an early-stage. There are many good hospitals in Mumbai that offer health checkup packages for cancer screening, such as a full body health checkup at Saifee Hospital Mumbai, which is one of the best hospitals in the country.
#chemotherapy#personalized chemotherapy#targeted therapy#full body health checkup#regular health checkups#cancer screening#cancer detection
4 notes
·
View notes
Text
Blood Tests for Cancer Screening: How Reliable Are They?
Early detection is a vital aspect of modern healthcare, particularly in the fight against cancer. Among the many tools available, the cancer screening test has gained widespread attention, especially with the emergence of blood-based screening methods. These tests promise a non-invasive and convenient way to detect cancer in its early stages, sometimes even before symptoms appear. But how reliable are they?
What Is a Cancer Screening Test?
A cancer screening test is a medical test performed on individuals without symptoms, aimed at identifying potential cancer or pre-cancerous changes. Traditional screening methods include mammography for breast cancer, colonoscopy for colorectal cancer, and Pap smears for cervical cancer. However, blood-based cancer screening tests are gaining traction for their ability to detect multiple cancer types through a single sample.
The Rise of Blood-Based Screening
Blood tests for cancer screening, sometimes referred to as “liquid biopsies,” work by identifying specific biomarkers such as circulating tumor DNA (ctDNA), proteins, or other molecular signatures associated with cancer. These tests have been developed to detect early signs of cancer with minimal discomfort, making the cancer screening test more accessible and less invasive.
This innovation has particularly raised hopes for screening cancers that are difficult to detect early, such as pancreatic, ovarian, or liver cancer. In some studies, blood-based cancer screening tests have shown promising sensitivity and specificity, especially when combined with other diagnostic methods.
Reliability: Key Metrics
The reliability of any cancer screening test depends on three main factors: sensitivity, specificity, and predictive value.
Sensitivity is the ability of the test to correctly identify those who have cancer. A highly sensitive test reduces the chance of false negatives.
Specificity measures the ability to correctly identify those who do not have cancer, minimizing false positives.
Positive Predictive Value (PPV) and Negative Predictive Value (NPV) help estimate how likely a positive or negative result truly reflects the presence or absence of disease.
Blood-based cancer screening tests vary widely in these metrics, depending on the type of cancer being screened and the technology used. For example, some tests may detect over 50 types of cancers with a reasonable degree of accuracy, while others may only be effective for one or two specific types.
Limitations of Blood Tests for Cancer
While the potential is significant, blood-based cancer screening tests still have several limitations:
False Positives: In some cases, a test may indicate cancer when none is present. This can lead to anxiety, unnecessary procedures, and increased healthcare costs.
False Negatives: A test may fail to detect cancer, providing a false sense of security and delaying necessary treatment.
Lack of Standardization: Different laboratories may use different methods and criteria, which can affect the consistency and reliability of the test results.
Limited FDA Approval: Many blood-based cancer screening tests are still in the research or experimental stages and have not yet received full regulatory approval for general use.
When Are Blood-Based Tests Most Useful?
Blood-based cancer screening tests may be most useful in combination with other screening tools or in individuals at high risk due to genetic or lifestyle factors. They can serve as an early alert system, prompting more thorough investigation through imaging or biopsy.
In high-risk populations—such as those with a family history of cancer or previous exposure to carcinogens—blood-based cancer screening tests can be a valuable part of a larger prevention strategy.
The Future of Cancer Screening
The future of cancer screening tests lies in integration. Combining blood tests with AI algorithms, genetic profiling, and traditional screening methods can offer a more holistic approach to early detection. As research advances, blood-based cancer screening tests may evolve into routine health checkups, much like blood sugar or cholesterol screenings.
Cost, accessibility, and public awareness will also play major roles in determining how widely these tests are adopted. As accuracy improves and prices come down, the cancer screening test via blood may become a cornerstone of preventive medicine.
Conclusion
Blood tests are a promising frontier in the world of cancer screening tests, offering a non-invasive, convenient way to potentially detect cancer early. However, current technology still has limitations in terms of accuracy and consistency. While they shouldn’t replace traditional screening methods just yet, they can serve as a powerful complementary tool—especially for high-risk individuals. For now, the key is to stay informed, discuss options with a healthcare provider, and use a cancer screening test as part of a comprehensive health monitoring strategy.
0 notes