Don't wanna be here? Send us removal request.
Text
Macro #3
Advocate for political, social or economic policies and programs that will improve health in diverse populations – Centers of political power are almost always located in urban areas, which is part of the reason why rural areas and populations can be overlooked by policy and legislation. This trend will continue unless people organize and groups make the needs of rural populations known. My group and I worked to combat this lack of awareness for rural issues, specifically for the rural population of those with intellectual and developmental disabilities. The I/DD population can be greatly benefited by the transformation and expansion of Medicaid. Most people with I/DD rely on Medicaid for their healthcare, but in North Carolina your options and available services are considerably restricted because of the low reimbursement. Individuals with I/DD are impacted to a greater extent because their conditions are often complex and require multiple providers and services from a variety of specialties, but are limited to who they can see for care due to Medicaid. This barrier is worsened when you consider aging with I/DD. The I/DD population lives longer and life spans grow as time goes on, which poses a problem for this population because it means that they can age out of Medicaid coverage. Medicaid transformation addresses a few of these issues, which is why we created a social media campaign to spread awareness of what the transformation can do for this population so that they can better inform their policy makers about how it can benefit or harm them. Medicaid transformation in North Carolina means that the method of reimbursement for Medicaid would move from a fee for service model to a managed care model, with provisions and tailored plans that would extend into adulthood for people with I/DD. This benefits and breaks down multiple barriers for this rural population. Moving to Managed care for Medicaid recipients means that providers would be compensated for the number of patients that they are serving instead of for each individual service that they provide. This model would, in theory, incentivize clinicians to take on Medicaid patients because they would still be able to make money and would not lose money for providing their services. Managed care is also beneficial because it covers disciplines that were considered separate, as one, to promote a more holistic approach to health care. Managed care integrates physical health with mental health. This integration is extremely important for those with I/DD because there is often a mental health disorder found to be comorbid with I/DD. Due to these benefits, my team conducted a social media campaign to show what Medicaid transformation is, the effects it will have on the I/DD population and how members of this population feel about the changes that are coming. The reach of our campaign was not as wide as we would have liked, because this issue of Medicaid is very politicized. We were originally going to use the platforms of Campbell University and Special Olympics NC’s Instagram pages to put out our information, however, due to the politics of the issue, both institutions had to remain neutral on the topic. Nevertheless, we created a “fake” Instagram to put up our advocacy campaign to see what it could’ve become even with the small reach that we had. Through researching this issue I realized that there were many nuanced aspects to this issue and system of reimbursement. While Medicaid transformation does present possible benefits to patients, it presents a wicked problem that can only be dealt with once transformation comes to fruition. A potential harm with a policy shift in this way would be a reduction in quality of care. If provider’s are only getting paid based on the number of patients they see, then potentially there could be problems with provider’s not performing adequate assessments and tests, so that they can simply get the next patient through the doors. A policy like this must be accompanied with mandates for a certain level of quality of care to prevent a decline in patient care outcomes. Other concerns are also that the reimbursement will still be too low, but at this point for NC it is merely speculation until changes are implemented. This illustrates the wickedness with any policy before it is fully made and implemented, there is a very real issue of access to healthcare for the rural I/DD population, but will addressing that issue in this way actually result in a better outcome? We won’t know the answer until it happens. However, this is why our advocacy campaign was so important. There needs to be change for those with I/DD and the people that these policies affect the most have to be educated on what is happening so that they can lead the charge to make sure the right changes are made. Even if Medicaid transformation is not the end-all be-all, it is a step in the right direction and with an educated populace it can get to where it needs to be.
0 notes
Text
Macro #2
Identify and distinguish the access to care barriers and the health care utilization challenges that affect the health of rural communities. The population with intellectual and developmental disabilities face many challenges and barriers, particularly if they live in a rural area. The barriers that my team and I focused on for our project were those barriers felt in healthcare. We researched and evaluated what might prevent those in the I/DD population in Harnett county from receiving the healthcare that they need. The following barriers were shown to have an impact on the Harnett county, I/DD population. Lack of specialists – while Harnett county is positioned close to the urban Wake county, there is still a significant distance that must be traveled for parents and patients who may need services because Harnett county and has few, if any, specialists that many with I/DD need. Provider experience – many primary care providers have little to no experience with patients who have I/DD. So finding one that will be open to providing care and do so in a quality way can be difficult, and this difficulty is compounded in a place like Harnett county where the overall number of providers is already less than in a place like Wake county. Medicaid problems – most people with I/DD do not have traditional insurance and rely on Medicaid to pay for their healthcare. Due to the low reimbursement rate, many providers will not take on patients who have Medicaid, or require them to pay out of their own pockets which most cannot do, which in turn reduces access to available providers even further.
As a team, our goal was to address some of these issues with MedFest and influence factors that could change the outlook of access and the barriers this populations faces in the future. MedFest addresses the issue of distance and willing providers by bringing them to the I/DD population. Our MedFest event and the two upcoming MedFests, in particular, bring clinical providers to local schools to provide care for this population where they are at. This alleviates the burden on parents to take the time and resources, which they may not have, to take their child to get a physical. While this does not give a permanent solution to the issue of access, it gives a momentary reprieve for the burden of healthcare on this population. This examination also lets students and parents know if there is a possible need to see a specialist, even though our MedFest event could not give direct access to specialists, we could supply the students with information and that is often half the battle. MedFest also has long term effects on the outlook of access for the I/DD population. MedFest brings together clinicians and future clinicians to experience providing care for patients with I/DD. This helps to eliminate the stigma and unwillingness of clinicians to provide care in the traditional setting for those with I/DD. As more clinicians are exposed to this population and are able to learn about the barriers that they face, they can take the matter into their own hands and be the change that this population needs. By providing this avenue for clinicians to gain personal experience with I/DD, MedFest is increasing the number of clinicians who can treat this population now and, by including clinical students, in the future as well.
The final barrier, Medicaid, is one that our MedFest event could not address directly, which is why our advocacy campaign is aimed towards educating the public on this topic. The I/DD population’s reliance on Medicaid and the low reimbursement of Medicaid causes a wicked problem for both sides. On the one hand, clinicians cannot maintain their practice if the majority of their patients have insurance that will pay less than the costs of the services. On the other hand, if providers don’t accept Medicaid, and it’s the only method of payment for this population, then they either have to go without care or bear the full weight of the health care costs. There has to be a fundamental change with how the reimbursement is structured and implemented so that people with I/DD are not put at a disadvantage, but also so that clinicians are compensated for the services that they provide. The issue is complex and multi-layered, the hope is that the coming transformation will help to ease this barrier to access, but only time can tell for sure. In the meantime, events and organizations like MedFest who can provide this care for no cost to the participants are extremely important as they help to provide care in the now and work towards a future of better and more plentiful care for this population in the future.
0 notes
Text
Macro #1
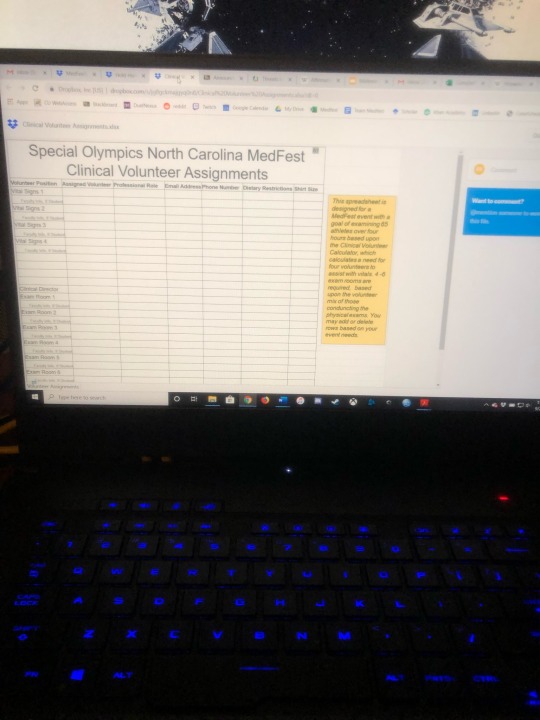
Perform effectively on an interprofessional team. This competency is clearly seen through what myself and my team did during and before this event. For the event to take place at all, we had to coordinate with a long list of people from different professions: teachers, principals, doctors, dentists, Campbell health science faculty from varying disciplines, and clinical students themselves. The team worked with the principle to arrange a place for the event to be held. We worked with the teachers to distribute the required athlete packets to the students and to arrange travel for them to the MedFest event. I specifically worked with all the clinical coordinators and volunteers to make sure we had enough medical staff to meet the needs of the athletes for the event. I met multiple times with PA, DO, and PT faculty to go over plans and ensure that any and all needs that they recognized would be taken care of. Dr. Mann and Ramona Albrecht took the initiative to help expand the pool of volunteers even further by inviting community clinicians and students from the school of nursing to join our numbers. I was able to connect with these individuals and integrate them into our plan. I also worked with local health offices to ensure that if athletes needed follow-up evaluations and did not have a primary physician or dentist, that they would have a place to go. The day of the event was a huge success and this was largely due to the excellent performance of my team and all of our collaborators. I helped give all of the clinical volunteers a run down of how an event like MedFest works and educated them on how to best work together during this process. We were able to more than double the number of athletes seen at the previous year’s MedFest and it is largely due to the awesome team work that our volunteers and my team showed throughout the day. Whether they were teachers bringing in students, nurses taking vitals or PA students conducting exams, we all worked together effortlessly and accomplished an amazing task at MedFest.
Interprofessional teamwork and continuity of care can be especially difficult in the grander scheme of healthcare in the rural setting, particularly for the population with intellectual and developmental disabilities. The I/DD population already has difficulty getting access to healthcare for various reasons, whether it be clinician unwillingness, inexperience, or simply not accepting Medicaid. Rurality exacerbates these barriers by adding extra distance between providers, and rural places naturally have fewer providers in general. Therefore, it is a huge challenge to the rural I/DD population to not only receive the specialized care that they need, but then to also have that care integrated with adequate communication between professions. Special Olympics North Carolina uses MedFest to help this symptom, but it is a short-term, stop-gap solution. The true task of breaking down barriers and increasing access to care for this rural population is dynamic and requires movement across the spectrum of professions. Privacy concerns have often been a barrier that has made it difficult for people to receive continuous care across professions, particularly for those who need services from behavioral/mental health and social services, like many of the I/DD population does. Many areas and healthcare systems are trying to move toward a more integrated system of healthcare, where professionals from across these fields can interact and manage care more cohesively, but there are even more areas, particularly rural, where this is not being heavily considered. Interprofessional communication and continuity can be an issue for anyone, but when so few specialists have little to no experience with the I/DD population, it makes the issue even worse. If more providers are exposed and are trained to the I/DD population, then their communication about plans of care may be able to be increased significantly and allow for a more seamless transition for the I/DD patient from clinician to clinician. The barriers that come with a rural setting are still there, but if care can become more integrated and providers can be better trained to care for this population, then we can hope to see major improvements in their health outcomes in the future.
MedFest can help to act as a catalyst for the interprofessional conversation of the I/DD population. It allows for real clinicians and students to have real experiences with this population. That experience will translate to greater access for this population in the future. While systematic an innovative solutions are necessary to create a more integrated system of healthcare, particularly for rural populations, the work that MedFest and Special Olympics NC are doing are a great asset for the education of professionals and the destigmatization and care of the I/DD population.
0 notes
Photo



MedFest was a huge success this week! Thank you to all the volunteers and this amazing team who made this awesome event possible!
0 notes
Text
First batch of supplies for MedFest this week! It’s almost here!
0 notes
Text
Another busy week of emails and meetings to get everything together for MedFest on 10/23! Can’t wait for this event!
0 notes
Text
Working on supplies and recruitment this week for Team Medfest!
0 notes
Text


Last week was full of meetings for the clinical part of Team Medfest! Thanks to Team Oral Health for working with us! I’m excited for this event!
1 note
·
View note
Text

Had an awesome meeting this week with our coordinator Holly for Team Medfest!
1 note
·
View note
Text

Working hard for Team Medfest after a teleconference with our preceptor!
1 note
·
View note
Text

First meeting with our preceptor this week! Excited to get this project underway!
1 note
·
View note


