Text

I put together this Inktober prompt list for the Harvey discord server! You're welcome to use it too! 🥰
There are both daily prompts and weekly themes. If you don't have time to create every day, you can just use the theme of the week!
Text:
Week 1: Seasons of the Valley
Spring Blossoms
Summer Sun
Autumn Chill
Cozy Winter
Favorite Festival
Week 2: Heart Events
First Meeting
Gift-Giving
Date Night
Rivalry
Proposal
Wedding Day
Happily Ever After
Week 3: The Wonders of Nature
Wild Animals
Mushroom/Bat Cave
Forest Spirits
Waterfalls
Mountain
Cindersap Forest
Secret Woods
Week 4: Finding Your Niche
Cheese
Gemstones
Foraging
Legendary Fish
Monsters
Adventuring
Mastery
Week 5: Stardew Legends
Ancient Fruit
Golden Chicken
Summit
Grandpa's Ghost
Farmer's Legacy
98 notes
·
View notes
Text







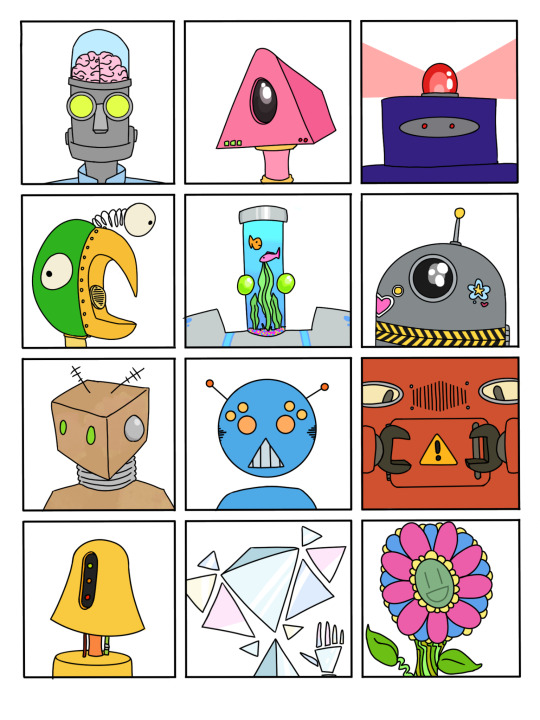

Had to do a repost with all 9 species! It's fun seeing them next to each other, noticing similarities and differences across all of them. Which one is your favorite?
Top to bottom, left to right:
Santornans, Lunestrians, Laranthians
Eshenali, Zairs, Atraxans
Sucralites, Kokoro, Humans
#robot art#other skies#aliens#HUMIES#i'm sooooooo proud of you for finishing all these#they look absolutely AMAZING!!!!!!!! 🥰 i hope you're proud to finally add em to the handbook!!!
18 notes
·
View notes
Text

Reposting this on my own art account.... I was mysteriously compelled to draw @xxacidnekoxx 's Tidbit ^^
51 notes
·
View notes
Text

My brain said "DRAW DRAGON." I couldn't fight with it. I had no idea what kind of dragon, but I'm actually pretty satisfied at the thought of a fuzzy, scaly dragon that looks like a butterfly and protects them/ is protected by them.
#this is like me + my bf combined omg#i love the concept!!! and the art is mindblowingly beautiful!!!#art#dragons
16 notes
·
View notes
Text

Wyatt enjoyers may I interest you in another rabbit her name is Elwig :) 🍫🃏
57 notes
·
View notes
Text

smaugust day 7 - “dinosaur”
I turned my favorite dinosaur, parasaurolophus, into a dragon! I love this guy, they were so fun to design! a bit complex though, so flat colors only so I could get this out on time. I didn’t have a lot of time yesterday, so I had to skip a day, but that’s all right :)
21 notes
·
View notes
Text
More AI art complaints
Ok, so now that I have been looking for decor for when I eventually move out and when I looked up dragon stuff, I keep finding AI generated stuff on Amazon. It pisses me off for multiple reasons! These AI generated dragon items are disgusting, ugly and unethical!

Now, to my fellow dragons, let me tell you how I identify AI generated dragons

Inconsistent number of wing fingers. Above is a dragon who has 6 wing fingers on one wing while they have only three on the other

2. Asymmetrical horns, this one is usually the biggest dead give away due to the head being the main focus. Usually the horns aren't even, not to bash dragons who have horn defects, but as seen above this dragon is also growing an extra horn, which might not be healthy. In addition the ear fin is completely missing on the other side of the head

3. Weird anatomy, as you can see the hind legs have weird proportions and one of the front talons has an extra talon, as well as the wings not being a consistent size. This can also include weird uneven scales
Just wanted to offer a talon out to help my fellow dragons, this makes finding dragon decor hard for us since the otherkin and therian communities also tie into art communities, and seeing our art being eaten up and spat out like this is upsetting. Support artists, only by from artists, avoid amazon for dragon paintings and screw AI
129 notes
·
View notes
Text







Another set of Sparklefur OCs, just for fun! Some of these are a bit old and I just haven't posted them. Top to bottom, left to right:
Toasty the s'mores giraffe
Juul the vape viper
Squeaky the rubber ducky
Babs the bubblegum hamster
Goober the PB&J pajama shark (PB&PJ shark)
Hakucho the ramune swan (swamune)
Wes the rootbeer float bear (root bear float)
Part 1
Part 2
18 notes
·
View notes
Text
Updated-ish art of iris my Robo cat girl

8 notes
·
View notes
Text



I was inspired by Ryōko Kui's Dungeon Meshi artwork, especially her grids of each fantasy race, and wanted to do something similar for my original species in Other Skies. I felt it would be a good challenge and would be useful to future players, since it shows a variety of folk from each species.
In order from top to bottom, this set includes Santornans, Lunestrians, and Laranthians.
I tried to include multiple ages, genders, and body types in each one. It's been quite fun so far! My plan is to post them in sets of 3 until all 9 species are represented.
#art#robot art#aliens#other skies#the Laranthians are my fav so far 🥰#i love the feral baby bussin' out and the bloody one + grey buzzcut one are 👌🏽👌🏽👌🏽🤲🏽🫶🏽#not to mention the worm worshiper and the person in the bottom right!!!!
40 notes
·
View notes
Text
List Of Alternate Universes
Alternate Universe (also known as alternate reality), is commonly abbreviated as AU and it is a descriptor used to characterize fanworks which change one or more elements of the source work’s canon. The term most often refers to fanfiction, but fanart can also depicted the characters in AUs.
Unlike regular fanfiction, which generally remains within the boundaries of the canon set out by the author, alternate universe fiction writers like to explore the possibilities of pivotal changes made to characters’ history, motivations, or environment.
Keep reading
14K notes
·
View notes
Text
Healthcare and Medical Tips for Writers - INJURIES
Ever wanted to write an injury or hospital scene but found yourself lacking the precise knowledge? Ever been hesitant to google, or found that google doesn't give you a straight answer?
Well, you've come to the right place!
Here you will find information on: Wounds and wound care (bandaging, casting, stitches, staples, etc), trauma, emergency room care, blood loss, hypothermia AND SO MUCH MORE!
Source(s): A (so far) seven year career in healthcare, in hospital/ETC, hospice/end of life, and clinic settings, as well as NCLEX and MCAT textbooks.
Let's begin! (ps. this is a LONG post!)

A.
Allergic Reactions: See also, Anaphylaxis. Allergic reactions can be caused by a number of environmental, food, drug, and animal irritants. Reactions vary in severity from mild itching, sneezing, cough, etc to severe with what is called anaphylaxis, which is covered further down.
Mild reactions (hives, itching, sneezing, coughing, watery eyes, hay fever etc.) can typically be treated with over the counter antihistamines (benadryl, allegra), decongestants, anti-itch creams, or eye drops.
Severe reactions (difficulty breathing, throat or tongue swelling, racing heart, etc) require medical attention. Reactions can start out mild and very quickly become severe. The earliest symptoms are typically a cough with tightness in the chest, swelling (tongue, lips) and weak, thready pulse.
--
Accidental Amputation: This occurs when a piece of the body is severed, either totally or partially during the course of an injury or accident. Most often affected: fingers, toes, ears.
What to do: STOP THE BLEEDING (see Blood Loss)! This is priority one. Elevate the injured area if possible. If their neck, back, or head is also injured, do not move them. Apply steady and direct pressure to the wound with cloth, bandages, whatever is available. If there is an object in the wound (i.e. something punctured through it), DO NOT REMOVE IT! Apply pressure around it. If blood soaks through the first cloth, do not remove it, apply more on top of it. Tourniquets, while often seen in movies, are typically not practical unless the injury is severe (major body part- leg, arm.) Watch the person for signs of SHOCK (see section below). In some cases, the amputated part can be reattached, so be sure to retrieve it and keep it cold, if possible.
Why can't I use a tourniquet? Preventing arterial blood flow to a limb will cause ischemia, and continuous application for longer than 2 hours can cause permanent nerve, vascular, or muscular injury and even skin necrosis. Incorrectly placed tourniquets can actually increase blood flow from soft distal tissue injury! Typically, simply applying pressure is the best and most indicated technique for saving someone's life.
When can I use a tourniquet? Extreme hemorrhages where the bleeding cannot be stopped via applied pressure may call for tourniquet use. EXAMPLE: Leg amputated above the knee where femoral artery bleeding is present. REMEMBER! Keep it applied for two hours or less. If you are dealing with multiple injured persons, a tourniquet may be your best bet for keeping all of those people alive.
--
Anaphylaxis: (See also, Allergic Reaction) Anaphylaxis typically begins within 30 minutes of exposure to an allergen. The affected person may experience:
-coughing, wheezing, chest pain
-fainting, dizziness
-hives, swollen tongue or lips
-vomiting, diarrhea, cramps
-weak, thready pulse and pale skin
-many people report a sense of "impending doom" right before anaphylaxis.
Anaphylaxis moves VERY quickly, and can lead to SHOCK and LOSS OF CONSCIOUSNESS within minutes. Epinephrine is the most effective treatment for anaphylaxis, and it should be administered via shot in the thigh as soon as possible.
Contrary to popular belief, a person's life is not necessarily saved when epi is administered in the field. They still need medical help! Some people require INTUBATION, either en route in the ambulance or at the hospital to assist with breathing. Doctors may also administer intravenous antihistamines and steroids.
1 in 5 people also experience a second anaphylactic reaction within 12 hours of the first. This is known as biphasic anaphylaxis.
--
Asthma Attacks: Asthma attacks are a sudden onset of worsening asthma symptoms brought on by the tightening of muscles around your airways known as a "bronchospasm". Someone suffering from an asthma attack will experience:
-Severe wheezing both with inhalation and exhalation
-Coughing
-Rapid breathing
-Chest tightness
-Tight neck and chest muscles (retractions)
-Panic
-Difficulty speaking
-Paleness, sweating
-Blue lips and nail beds (cyanosis)
Use of a rescue inhaler is vital, but is sometimes not enough. Keep the person calm, have them breathe out fully, then take a deep puff of the inhaler and hold for ten seconds. Repeat this process four times, waiting a minute between each puff.
If symptoms do not improve, they need immediate medical attention! Gradually, the lungs will tighten to the point that there is so little air movement that the person is no longer wheezing. This is called "silent chest" and is a very dangerous sign. They may begin to develop a dusky blue hue to their lips due to lack of oxygen.
B.
Blood Loss: The human body contains about five liters of blood. When you begin to lose blood, either from external or internal injury, it is put into four classes or stages.
Class I: Up to 750 mL or 15% volume lost.
Class II: 750 - 1000mL or 15-30% lost.
Class III: 1500 - 2000mL or 30-40% lost.
Class IV: Greater than 2000mL or 40% lost.
VISUAL GUIDE TO BLOOD LOSS HERE
Blood pressure and heart rate remain close to normal up to about 30% blood loss. Once this point is reached, the following symptoms begin:
- Rapid heart rate (120+ bpm)
- Low blood pressure
- Rapid breathing
At 40% or 2000mL of blood loss, you will die. This is roughly 0.53 gallons in the average adult.
When you lose a lot of blood or fluids from your body rapidly, you experience what is known as Hypovolemic Shock. It occurs when the heart is unable to pump enough blood to the body.
Also see: SHOCK below.
--
Broken Bones: Fractures of bones in the body are typically classified in two or three MAJOR categories in the trauma/field setting (and several other subcategories):
Stable: The broken ends of the bone line up and are barely out of place
Compound: The skin may be pierced by the bone or by a blow that breaks the skin at the time of the fracture. The bone may or may not be visible.
Comminuted: The bone shatters into three or more pieces.
What to do: Immobilize the affected area immediately to prevent further injury or displacement of bone. Apply pressure if there is external blood loss. Monitor for signs of internal blood loss (see BLOOD LOSS above)
Most fractures are treated with further immobilization (casting, bracing, screws/bars/pins) and re-setting (traction) of the bones as needed.
The downtime for fractures varies from several weeks to several months. Pain typically subsides LONG before the fracture is healed enough for the stress of normal activities.
During recovery, the affected person can expect to lose muscle strength and range of motion.
--
Burns: Burns are classified into Six (though typically condensed to four) stages or "degrees":
-First Degree (superficial): These burns only affect the outer layer of the skin (epidermis). The affected area is red, painful and dry. Think of a mild sunburn. Long-term or lingering tissue damage is extremely rare and usually includes a simple change in skin color.
These can be treated at home or in the field, as the body is still able to regulate temperature or protect the body from infection.
-Second Degree (partial thickness): These burns involve the epidermis and the lower layer of skin (dermis). The site is red, blistered, and swollen/painful.
Second degree burns are often the most painful because the nerve cells of the dermis are exposed, and are characterized by the blisters they cause. The skin loses its ability to block infection and regulate temperature at this degree.
-Third Degree (full thickness): These burns destroy the dermis and epidermis and often penetrates the innermost layer of the skin (subcutaneous tissue). The site may look white or blackened and charred.
Third degree burns cause additional loss of fluid and heat, plus an increased risk of infection. They also cause nerve death, so the area may have no feeling.
-Fourth, Fifth, and Sixth Degree: These burns destroy the first three layers of the skin. Some classifications differentiate that fourth degree includes fat, fifth muscle, and sixth bone. Others simply lump them all into fourth degree.
There is no feeling in the area due to the destruction of nerve endings. The body is extremely vulnerable to infection.
Severe burns (third and up) cause an explosive inflammatory response in the body.
From NIMH: A normal inflammatory response protects the body from invaders, such as bacteria, viruses, fungi, cancerous cells, toxins, and foreign materials. It activates in response to infection, injury, or other threat. It is designed to destroy the cause of the problem, contain the damage, and clean up the mess left by dead cells and other debris.
But, when faced with large or deep burns, it can overreact, often making the injury more severe and harming the heart, lungs, blood vessels, kidneys, and other organ systems.
During this inflammatory response, fluid is lost rapidly and may lead to SHOCK (see below).
Infection is also a MAJOR concern with severe burns. Burns damage the skin’s protective barrier, meaning foreign invaders like bacteria can sneak past. Burns also severely weaken the immune system, so the body is less able to fight. Infections can occur not only in the affected skin area, but also in organs such as the lungs or bloodstream.
C.
Concussion: Concussions are a type of head injury that occurs during trauma to the brain. Sudden, direct blows to the head that make your brain move often cause concussions. They are the least severe type of Traumatic Brain Injury (TBI).
Depending on their severity, concussions can cause a myriad of symptoms as they impair brain function:
-Confusion
-Clumsiness
-Slurred speech
-Vomiting, nausea
-Headache
-Dizziness or vertigo
-Visual disturbances (blurriness, light sensitivity)
-Ringing in ears
-Behavior or personality changes
-Memory loss
-Fatigue
Grade 1 and 2 concussions are typically treated with rest and downtime until symptoms subside. You do NOT have to keep a person with a concussion awake! That is a persistent myth.
Grade 3 concussions occur when loss of consciousness is experienced. Evaluation by a trained medical professional is vital to assess cognitive function and possible internal injuries/bleeding. Doctors/paramedics may ask questions such as:
-"Where do you live?" "Who is the president?" or "What is your name?" to gauge your cognition.
After any head injury, the first line of testing is CT or MRI scans of the brain to rule out bleeding or swelling.
In some cases, concussion symptoms may persist for months in what is known as Post-Concussion Syndrome.
--
Cardiopulmonary Resuscitation (CPR): CPR is given during cardiac and breathing emergencies. If a person is unconscious/unresponsive and/or is not breathing, CPR may be performed.
To perform CPR:
- Place the person flat on their back on a firm surface.
- Give 30 chest compressions:
Body position: Shoulders directly over hands; elbows locked
Hand position: Two hands centered on the chest
Depth: At least 2 inches
Rate: 100 to 120 per minute
Allow chest to return to normal position after each compression
Giving rescue breaths is often a matter of preference. If there is a risk of personal harm to the person giving CPR due to blood-borne or saliva-borne pathogens, DO NOT GIVE BREATHS.
-Give 2 Rescue Breaths:
Open the airway to a past-neutral position using the head-tilt/chin-lift technique
Ensure each breath lasts about 1 second and makes the chest rise; allow air to exit before giving the next breath
Continue giving CPR in sets of 30 compressions and 2 breaths until help arrives or the person is resuscitated. Use an Automated External Defibrillator (AED) as soon as possible.
D.
Dehydration: Dehydration occurs when your body does not have enough fluid and electrolytes to function properly. Early symptoms of mild to moderate dehydration may include:
- Thirst
- Dry mouth
- Headache
- Dark urine
- Dizziness, lightheadedness
Mild dehydration can be treated with increased water or oral re-hydration solution intake. You can make your own oral rehydration solution: 6 teaspoons of sugar with half a teaspoon of salt in one liter of boiled water.
Severe dehydration may cause:
- Extreme thirst
- Very dry mouth
- Rapid breathing
- Increased heart rate and low blood pressure
- Fever
- Little to no urine output
- Irritability, drowsiness, or confusion
Severe dehydration requires replenishment of fluids and electrolytes via intravenous treatment.
The average person in good physical condition can survive without water for THREE DAYS, though at that point, bodily function is severely impaired.
--
Drowning: Drowning occurs when water enters the lungs, thereby preventing breathing and oxygen transfer.
Drowning can occur in as little as 20-40 seconds. In some cases, as little as 118mL or .5 cups of water entering the lungs can cause death.
If a person is found unconscious/not breathing/without a pulse in the water, the following course of action should be taken:
- Remove them from the water
- Perform CPR (see above)
E.
Electric Shock: Electric shock occurs when someone is exposed to an electric energy source, which flows through a portion of the body.
Muscles are stimulated by electricity. When a current 10mA or above travels through our body's flexor muscles, a person may experience a sustained contraction. Example: the muscles in the forearms that close the fingers. The person may be unable to release the source or electric shock, thereby increasing the severity.
When a current of 10mA or above travels through extensor muscles, the opposite happens and the body violently lengthens the limbs away from the body. Though it seems like a movie trope, a victim can be propelled several meters away from the source if their hip muscles are affected.
Muscles, ligaments and tendons may tear as a result of the sudden contraction caused by an electric shock. Tissue can also be burned if the shock is lasting or the current is high.
Shocks of 50mA or above that pass through the heart can cause cardiac arrest (see HEART ATTACK below). An outside current passing through the heart can disrupt the rhythm and cause ventricular fibrillation, which causes the heart to stop pumping. Victims rapidly lose consciousness and can die within minutes.
This disruption of the heart's rhythm can even occur hours following the shock.
F.
Frostbite: Frostbite occurs when the skin and underlying tissues freeze. It is typically classified into three stages:
Frostnip: Cold exposure leads to numbness in the affected area. As the skin warms, a person may feel pain and tingling. Frostnip does not cause lasting damage.
Superficial Frostbite: This stage causes slight changes in the color of the skin. The skin itself may begin to feel warm. If you treat with re-warming at this stage, the skin may look mottled. Fluid blisters may appear within 12-36 hours.
Deep or Severe Frostbite: At this stage, all layers of skin and underlying tissue begin to be affected. Skin may turn white or blue-gray and all sensation of cold and pain are lost. Joints and muscles stop working and large blisters form 24-48 hours after re-warming. The tissue then turns hard and black as it dies.
Severe cases of frostbite may cause blood clots, which can lead to thrombosis and death. The full extent of the damage may take weeks to develop.
In all cases, the area must be re-warmed. In more severe cases, surgical removal of the affected area may be required, up to and including amputation of limbs.
G.
Gangrene: Gangrene is the death of body tissue that occurs due to lack of blood flow or severe bacterial infections. Most commonly, the fingers and toes are affected, but it can also occur internally.
Symptoms of gangrene include:
- Skin discoloration: pale, blue, purple, black, or red depending on the infection type.
- Swelling
- Blisters
- Sudden pain followed swiftly by lack of feeling
- Foul-smelling discharge from the wound
If the gangrene extends to tissue beneath the surface, the person may also experience fever and a feeling of general unwellness.
If the germs spread into your bloodstream, sepsis and septic shock can occur.
Gangrene that progresses to tissue death may require surgical debridement or even amputation of the affected limb.
H.
Heart Attack: Cardiac arrest occurs when the blood no longer flows to a section of the heart and it can no longer get oxygen. If the flow isn't restored promptly, the section may begin to die.
Symptoms of cardiac arrest differ wildly from person to person depending on gender, general health, and age, but usually include:
- Chest pain, which is generally center or left sided. It may feel like pressure, squeezing, or fullness.
- Upper body discomfort, usually in the arm, neck, jaw, or upper stomach.
- Shortness of breath.
Also commonly reported: cold sweat, unusual tiredness, nausea, dizziness, a feeling of impending doom.
Contrary to television depictions, heart attacks are not always instantaneous chest pain and declination of function. Sometimes, the process may take days.
Healthcare professionals may start the following before even definitively knowing the person is having a heart attack:
- Aspirin to prevent clotting
- Nitroglycerin to improve blood flow
- Oxygen therapy
- Pain medication
Once cardiac arrest is the confirmed diagnosis, intravenous clot-dissolving medications (tissue plasminogen activator (tPA), alteplase, reteplase, etc) and coronary angioplasty are given to open blocked arteries.
--
Hypothermia: Hypothermia occurs when the body has an abnormally low temperature (below 95°F (35°C)).
Body temperature is regulated by the hypothalamus in the brain. When exposed to cold, the hypothalamus begins to raise the body temperature through shivering and increased muscle tone.
Hypothermia occurs in stages with clear symptoms:
Mild (Body temperature of 90–95°F (32–35°C)): Garbled or unclear speech, pale and dry skin, loss of motor function, tiredness, memory loss, lack of judgement, hunger, increased heart rate, shivering.
Moderate (Body temperature of 82–90°F (28–32°C)): Lethargy, enlarged and unresponsive pupils, low blood pressure, slow heart rate, paradoxical undressing due to feeling warm, continued decline in cognition. Shivering stops between 86–90°F (30–32°C).
Severe (Body temperature of less than 82°F (28°C)): Unresponsiveness, decline in heart rate and blood pressure, lung congestion, loss of reflexes, eventually failure of heart and lung function.
Immediate treatment includes moving the person to a warm, dry place or sheltering them from the elements. Removing wet clothing. Covering the person with a blanket or dry clothing/garments. Making skin-to-skin contact. If able, making them drink a warm beverage.
Avoid jostling or abruptly moving the person, as this can trigger a fatal heart arrhythmia.
If the person becomes unconscious and has no pulse or breath sounds, administer CPR (see above). A person who has hypothermia can appear dead and still be resuscitated.
Clinical treatment in a healthcare setting may involve: Core warming with warm intravenous fluids and even hemodialysis (filtering of blood with a machine).
L.
Loss of Consciousness: Unconsciousness can occur for a number of reasons including: head trauma, drug and alcohol use, lac of oxygen, and panic.
Severity of brain injuries that are accompanied by LoC are defined in four stages:
Mild: Unconscious for <15 minutes
Moderate: Unconscious for 15 minutes to six hours.
Severe: Unconscious for 6 - 48 hours.
Very Severe: Unconscious for > 48 hours.
R.
Rabies: Rabies is a zoonotic disease caused by an infection with the Lyssavirus genus. It is transmitted by the saliva of infected animals. Dog bites account for about 99% of human rabies cases.
If not immediately treated, rabies almost always fatal to the host. Unfortunately, rabies also has a highly varied incubation period (days, weeks, or months). This period varies based on:
- Location of the exposure site (proximity to the brain)
- Type of rabies virus
- Existing immunity
Early symptoms of rabies are flu-like, including: weakness, discomfort, fever, or headache. Bite site discomfort is also common (prickling, itching). This may last for days.
Symptoms then move to cerebral dysfunction, including: anxiety, confusion, and agitation. This then progresses to delirium, hallucinations, hydrophobia (fear or aversion to water) and insomnia.
Once clinical signs of rabies appear, the disease is almost always fatal. Treatment is merely aimed at supporting the person and lessening symptoms.
Less than 20 cases of human survival from clinical rabies have been documented on record.
The only true way to treat rabies is with pre or post-exposure prophylaxis (PEP) with rabies immune globulin before clinical signs appear.
S.
Shock: Shock is a critical body condition brought on by sudden drop in blood flow within the body. It can results from trauma, blood loss, burns, poisoning, and even allergic reactions.
If left untreated, it can lead to organ damage and death.
Signs of shock may include:
- Cool, clammy skin
- Pale or ashen tone
- Cyanosis (blue tinge to lips and nail beds. NOTE: May appear gray in darker skin tones!)
- Rapid pulse (tachycardia)
- Fast breathing (tachypnea)
- Nausea and vomiting
- Enlarged, unresponsive pupils
- Weakness
- Fatigue
- Change in mental status (agitation, anger, anxiety)
- Loss of consciousness
Treatment depends on the cause and the severity, but may include: intravenous fluids, CPR if breathing stops, epinephrine if the person is experiencing an allergic reaction.
--
Smoke Inhalation: Smoke inhalation is the leading cause of death during fires. The mechanism of action is complex and includes thermal injuries, chemical injury, and asphyxiation and toxicity.
There are three different types/causes of smoke inhalation injury:
Simple Asphyxiants:
- Combustion can use up oxygen near a fire and deprive the victim of oxygen.
- Smoke itself can contain byproducts that do not directly harm the victim, but that take up needed space that oxygen would occupy. Carbon dioxide, for example.
Irritant Compounds: Combustion that occurs during a fire can create chemicals that damage the skin and mucous membranes. This causes disruption in the function of the respiratory tract, which causes swelling, airway collapse, and respiratory failure. Examples include: sulfur dioxide, ammonia, and chlorine.
Chemical Asphyxiants: Some fires can produce compounds that cause disruption at the cellular level, interfering with the body's ability to exchange oxygen correctly and lead to cell death. Examples include: carbon monoxide, hydrogen sulfide, and hydrogen cyanide.
Symptoms of smoke inhalation may include:
-Cough
-Shortness of breath
-Noisy or hoarse breathing
-Bloodshot eyes
-Changes in skin color
-Blackening of the nostrils and throat caused by soot
-Headache
-Changes in cognition
Medical intervention and testing may include:
-Chest x-ray
-Pulse oximetry (checking your blood oxygen levels)
-Blood tests: CBC, CMP, arterial blood gasses, and carboxyhemoglobin and methoglobin levels.
Treatment varies by severity, but may include:
-Bed rest
-Oxygen
-Hyperbaric oxygenation (in the case of carbon monoxide poisioning)
--
Stitches: Stitches are a type of wound closure that assists in healing the skin and underlying tissue when bandages or adhesive are insufficient.
A good rule of thumb is 5-6 stitches per inch of wound.
Each stitch is an individual piece of filament knotted off, rather than a continued thread like you would see in fabric.
423 notes
·
View notes
Text

I'm playing on a multiplayer farm with @cryptidelf and @lildrownedrat where each of us is playing a Creature of some kind. Here they are dressed up in their best clothes for the Egg Festival! Left to right:
Crunchy the Faun (he/they/it) - @cryptidelf
Ryu the Dragon (he/him/The Dragon) - mine!
Strawberry the Alien (he/they) - @lildrownedrat
They collectively own a black cat named Locust!
21 notes
·
View notes
Text

Does it count as furry if there's no fur?
70 notes
·
View notes
Text



I don’t know if people still follow me here, but I’m opening 🌱 COMMISSIONS 🌱
- email [email protected]
- full arts available in portrait or landscape
- NSFW OK but extra charges
- full res file handover for printing
- will love you forever
🖌️ PORTFOLIO 🎨
#this is incredible work and i desperately need more nsfw artists to commission from 😭#keeping this in the front of my mind#commissions#art
38 notes
·
View notes
Text
some people think writers are so eloquent and good with words, but the reality is that we can sit there with our fingers on the keyboard going, “what’s the word for non-sunlight lighting? Like, fake lighting?” and for ten minutes, all our brain will supply is “unofficial”, and we know that’s not the right word, but it’s the only word we can come up with…until finally it’s like our face got smashed into a brick wall and we remember the word we want is “artificial”.
223K notes
·
View notes
Text
I want to write a book called “your character dies in the woods” that details all the pitfalls and dangers of being out on the road & in the wild for people without outdoors/wilderness experience bc I cannot keep reading narratives brush over life threatening conditions like nothing is happening.
I just read a book by one of my favorite authors whose plots are essentially airtight, but the MC was walking on a country road on a cold winter night and she was knocked down and fell into a drainage ditch covered in ice, broke through and got covered in icy mud and water.
Then she had a “miserable” 3 more miles to walk to the inn.
Babes she would not MAKE it to that inn.
105K notes
·
View notes