Don't wanna be here? Send us removal request.
Text
Blender - Animation
I have used alot of tutorials to try and create the animation that I was looking for. It has been really difficult and time intensive as I don't really have any experience with animation.
Hopefully I pass.
Animated Flower in blender

Initially this was what I was going to try and construct. It took hours to try and construct each of the leaves as I had to get used to the keys in the program. I then had difficulty with the verticle add and didn't realise I would need them to create the tendrils. I progressed on and thought I would just be able to illuminate the flower. This tutorial included nodes and textures and using the clouds texture to have the leaves moving. I attempted to follow the tutorial but ended up not being able to complete as I had changed some of the constructs of the flower extruding and bevelling and changed the shape therefore wasn't able to select the outside. I did write some instruction down and tried to animate the leaves with empty to diplace the textures but I was unable to set up the keyframes or change it too linear. I gave up!
Grass
I thought it would be great to add some real looking grass to the animation. I again followed a tutorial using particles. The first tutorial I did with the grass ended up looking like someone had just painted clumpy brush strokes everywhere. Even though I had changed the seed, and how many strands the lengths of the hair. The parent child combo I don't think worked they way I had intended.
So the next time I did it I used the advanced settings and changed the hair length, number of strands, changed the brownian and left it at the. It ended up a much better image of grass than what I initially had.
I tried to animate parts but again I have found it really difficult.
Beehive and animated Bees
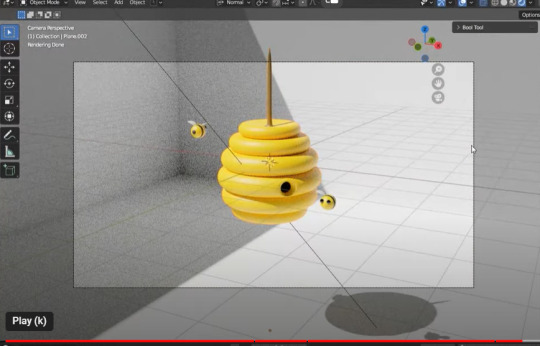
This initially has taken be about 7 hours to complete. I am much more familiar with how the commands and how they now work in blender. I have been able to create this stylised beehive however again the struggle is real to try and capture and render the animation. Even adding the keyframes to have the bees moving has been no short of difficult. Sometimes it works sometimes it doesn't. I did have a look at the nodes but it was so complex and above my understanding of blender I had to stop and just attempt to do the basics.

I am attempting to add the sun in there and another animal. But l we will see how it goes.
I was able to put in a background and add constraints.... to my little bees. in the constraints by changing the influence allows the bee to be located close to the bezier curve. The higher the influence the further away it is.
Touch Designer
One of the mistakes I think will touch designer is not really understanding what you are actually doing. I have repeated tutorials multiple times and then realised that I hadn't connected a node properly or something else would not display. Very frustrating when you actually don't understand the concept of the whole node system anyway.
Created a geometry instancing with tubes in a grid. The tubes are rotating in the grid in a sort of snake like fashion with multiple colours. Attempted to change it too a circle and the whole effect was gone. Quickly changed it back.
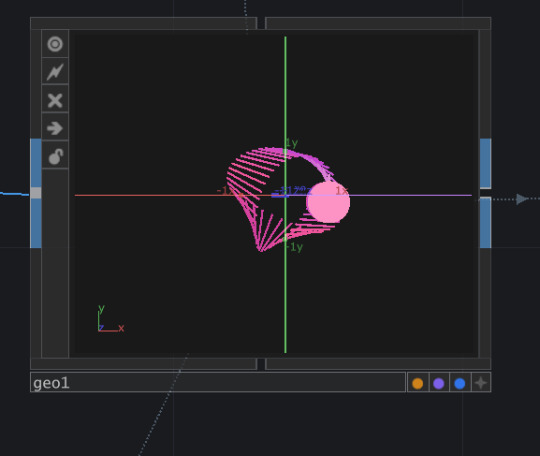
The second option if tried was using the particle system to create an amazing animation. I thought I was struggling to export the video but I eventually got it working. I did attempt to
Krita
2D animation - I watch so many 2d animation videos watching toddler TV I was really inspired by the Bluey cartoon. Quite simple but really easy to follow. I have got a little bit lost along the way whilst trying to do my animation. I have found the process really difficult .

Stop Motion
Watching the stop Motion on instagram inspired me to get all creative. I initially created clay pieces and separately created a litte stop motion video of the body parts coming together. Although I was okay it probably wasn't at the level we needed. I attempted to do another animation with a rabbit and some wire armature. The model kept breaking and was just to pliable. I made another rabbit and flowers and give it another go with more wire and a thicker armarture but again it wasn't as robust as it needed to be. Although the stop motion was okay just wasn't as flowing and blending as I liked. Having the characters walk in an upright position is extremely difficult without ways to hold them up.
1 note
·
View note
Text
Process Documentation - Wearable device
Wearable: some form of custom device that can be worn on the body, that either
senses something about the body or the environmental context of the wearer, or
gathers data from the internet and translates it into some form of communication/alert/action to/on the body, or
responds in some other way to the body, or the environment, or the relationship between the two
Initial Research -
What elements contributes to agitation in an elderly person with a cognition impairment.
how can we use sensors to detect biometric information in a bid to reduce the use of chemical restraints and sedatives in an Emergency Department.
DEMENTIA
This neurocognitive decline can make it difficult for people living with dementia to process and manage environmental stimuli as they become more vulnerable to social and physical stressors (Kales et al., 2015; Smith et al., 2004)
As a result, up to 90% of people living with dementia will at some stage develop Behavioural and Psychological Symptoms of Dementia (BPSD) (Lagana et al., 2022), manifesting in various verbal and nonverbal behaviours, including apathy and depression (Tible et al., 2017). More overt forms of BPSD are referred to as ‘responsive behaviours’, understanding that they often reflect an attempt to communicate or respond to a situation or environment (Yous et al., 2019). Of these responsive behaviours, agitation and aggression are often considered the most distressing form, as they may compromise the safety of the person living with dementia and those around them (Tible et al., 2017).
Behavioural and psychological symptoms of dementia often present or are exacerbated during acute hospital admission. This is in response to common physical stressors, such as temperature, light and noise levels and social stressors, such as the inability to communicate and form therapeutic relationships (Caspar et al., 2018; Lourida et al., 2020).
DEMENTIA - Sundowning
Sundowning, also known as "sundowner's syndrome," refers to a phenomenon commonly observed in individuals with dementia, particularly during the late afternoon or evening. Here’s an overview of what it involves:
Characteristics of Sundowning
Increased Agitation: Individuals may become more restless, anxious, or agitated as the day progresses. This can manifest as irritability, confusion, or aggressive behavior.
Confusion: People may experience heightened confusion or disorientation during the evening hours, leading to difficulty recognizing familiar surroundings or people.
Mood Changes: Emotional swings can become more pronounced, with individuals exhibiting sadness, anger, or frustration.
Sleep Disturbances: Sundowning can also be associated with difficulties in falling asleep or staying asleep, contributing to overall fatigue and agitation.
Causes
While the exact cause of sundowning is not fully understood, several factors may contribute to its occurrence:
Circadian Rhythm Disruption: Changes in the body’s internal clock may lead to increased confusion during evening hours.
Fatigue: Accumulated fatigue throughout the day can contribute to heightened agitation and confusion.
Reduced Lighting: Diminished natural light in the evening can create shadows and unfamiliarity, leading to anxiety.
Overstimulation: A busy day with too much activity or noise may overwhelm the individual as the day winds down.
Management Strategies
To help manage sundowning, caregivers can consider several approaches:
Establish a Routine: Maintaining a consistent daily schedule can provide a sense of security and predictability.
Create a Calm Environment: Dim lights and reduce noise in the evening to create a calming atmosphere. Soft music or familiar scents may help.
Encourage Relaxation: Activities such as gentle stretching, reading, or listening to soothing music can promote relaxation in the evening.
Limit Stimulants: Reducing caffeine or sugar intake later in the day may help decrease agitation.
Monitor Activity Levels: Ensure that the individual is engaged throughout the day but avoid overstimulation.
Provide Reassurance: Offering comfort and reassurance during episodes of confusion can help alleviate anxiety.
PITCHED - Pain, infection, Thirst, constipation, Hunger, Environment and Drugs.
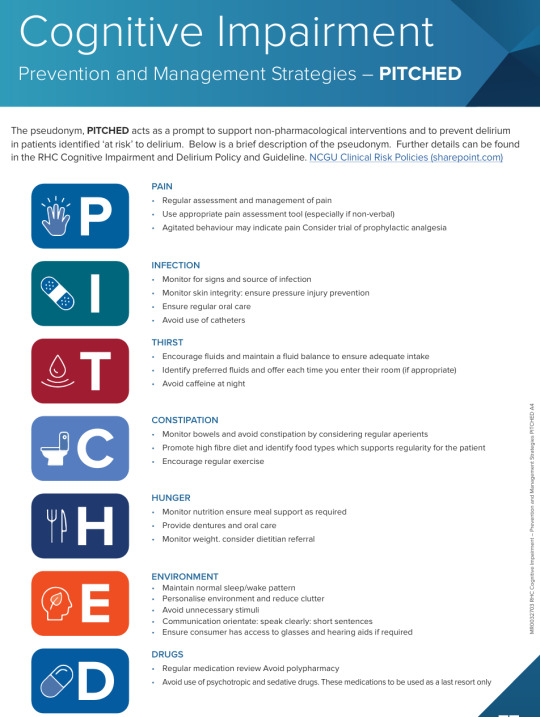
Agitation in an emergency department is common for elderly people especially with dementia and delirium.
Environment Factors
Unfamiliar Environment: The ED can be chaotic and disorienting, leading to increased anxiety and agitation.
Sensory Overload: Bright lights, loud noises, and the presence of many people can overwhelm elderly patients, causing distress.
Lack of Routine: Disruption of familiar routines can heighten feelings of insecurity and agitation.
Psychological Factors
Anxiety and Fear: Concerns about their health, treatment, or being in an unfamiliar environment can lead to heightened anxiety.
Cognitive Decline: Patients with dementia or cognitive impairment may struggle to understand their situation, leading to frustration and agitation.
Social Isolation: Feelings of loneliness or separation from caregivers or loved ones can contribute to agitation.
Social and Emotional Factors
Loss of Independence: The perception of losing control or independence can provoke agitation.
Past Trauma or Experience: Previous negative experiences in medical settings can trigger anxiety and agitation in similar situations.
Current Research
Smart Devices and Wearable Technologies to Detect and Monitor Mental Health Conditions and Stress: A Systematic Review - PMC (nih.gov)
Vital signs, neural activity (electroencephalogram ((EEG)), heart rate (electrocardiogram ((ECG)), skin temperature, and skin conductance response (electrodermal activity) can provide important information about an individual’s health status.
Devices that can sense increased agitation typically rely on various types of sensors and technology. Here are some common examples:
Wearable Devices: Smartwatches and fitness trackers often have sensors that monitor heart rate, skin temperature, and galvanic skin response, which can indicate stress or agitation.
Mobile Apps: Some apps analyze voice tone and speech patterns to detect changes in emotional states, potentially indicating agitation.
Environmental Sensors: Cameras with facial recognition software can assess changes in facial expressions that may signal agitation.
Biometric Sensors: Devices that measure physiological responses like blood pressure, heart rate variability, and respiration can indicate heightened agitation.
Smart Home Devices: Certain smart home systems can integrate multiple sensors (like cameras and environmental sensors) to monitor behavior and detect signs of agitation.
Therapeutic Robots: Some robots designed for emotional support can sense agitation through vocal and visual cues and respond accordingly.
What already currently Exists on the market
Dementia-friendly wearable devices designed to detect agitation focus on user-friendliness, comfort, and reliability. Here are some options:
Smartwatches:
Apple Watch: Features like heart rate monitoring and fall detection can help caregivers notice signs of agitation.
Fitbit: Models with heart rate and sleep tracking can alert caregivers to unusual patterns.
Fitness Trackers:
Garmin Vivosmart: This tracker monitors activity levels and can provide insights into changes in behavior or agitation through activity patterns.
Specialized Wearables:
Mindset: A device designed specifically for older adults that monitors stress levels and can alert caregivers if agitation is detected.
Seniors’ Comfort Devices: Some wearables focus on providing calming stimuli, which can help in managing agitation.
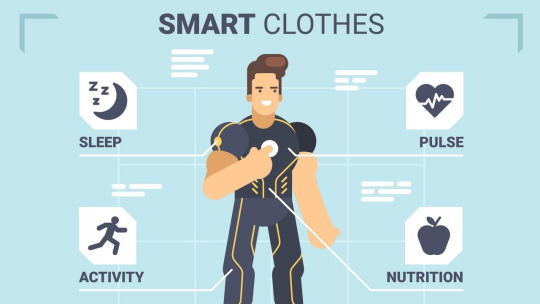
Smart Clothing:
Certain textiles integrated with sensors can monitor heart rate and stress levels, providing data to caregivers.
GPS Trackers:
While not specifically for agitation, devices like the AngelSense can help caregivers monitor location and movement patterns, which can indicate agitation or wandering.
Emotion-Sensing Wearables:
Devices like Empatica Embrace can detect physiological signs of stress and send alerts to caregivers.
When selecting a device, consider ease of use, comfort, and the specific needs of the individual with dementia to ensure it fits seamlessly
their daily life.
INTERNET OF THINGS IOT
Lots of work has been done however they are all facing the similar issues in which many of them test the prototype and get not so good feedback about the size, shape, design, and so on.
IoT-Based Wearable Devices for Patients Suffering from Alzheimer Disease - PMC (nih.gov)
Galvanic skin response (GSR) is generally considered a useful measure of physiological arousal, but its accuracy can vary based on several factors:
Sensitivity to Changes: GSR is sensitive to emotional and physiological changes, making it good for detecting arousal related to agitation, stress, or excitement.
Individual Differences: Responses can vary significantly between individuals due to factors like skin type, hydration levels, and baseline stress levels.
Context: Environmental factors, such as temperature and humidity, can influence GSR readings, affecting accuracy.
Calibration: Accurate interpretation often requires proper calibration and context-specific understanding, as GSR alone doesn’t provide insights into the specific emotions being experienced.
Supplementary Data: For improved accuracy, GSR is often used alongside other physiological measures (like heart rate or respiration) and behavioral observations.
While GSR can be a valuable tool in monitoring emotional states, it's best used as part of a broader assessment strategy rather than in isolation.
What vital sign is the biggest predictor of agitation
The heart rate is often considered the most significant predictor of agitation. Elevated heart rates can indicate increased physiological arousal, which is commonly associated with agitation, anxiety, or stress.
While other vital signs like blood pressure and respiration rate can also signal agitation, heart rate changes tend to be more immediate and responsive to emotional states. Monitoring heart rate variability can provide further insights into a person’s stress levels and overall emotional well-being.
Combining heart rate data with observations of behavior can enhance the understanding of agitation in individuals, especially in those with conditions like dementia.
heart rate data and irratic movement predictor of agitation
Heart Rate: An elevated heart rate is often a direct indicator of physiological arousal associated with stress or agitation. Sudden spikes in heart rate can signal acute agitation.
Erratic Movement: Increased physical activity, such as pacing, fidgeting, or other restless movements, often correlates with agitation. These behaviors can indicate discomfort, anxiety, or a need to escape a stressful situation.
When monitored together, these two factors can provide a clearer picture of a person's emotional state:
Correlation: A simultaneous increase in heart rate and erratic movement can reinforce the idea that the individual is experiencing significant agitation.
Timeliness: Changes in heart rate can occur quickly, allowing caregivers to respond promptly to signs of distress.
Behavioral Context: Observing erratic movements alongside heart rate data can help caregivers interpret the situation more accurately, allowing for tailored interventions.
In practice, devices that track both heart rate and movement (like smartwatches or fitness trackers) can be useful tools for monitoring agitation in real-time, especially for individuals with conditions such as dementia.
Wearable Biosensors: An Alternative and Practical Approach in Healthcare and Disease Monitoring - PMC (nih.gov)
Would using a sensory Therapy device with the monitor inside work?
Sensory therapy is a helpful way to calm and soothe without using medication. It’s an effective way to reduce anxiety, calm nerves, and provide comfort.
what are the best materials to use?? fur?
Nonpharmacological tactile activity interventions for reducing behavioural and psychological symptoms of dementia in the acute hospital setting: An integrative review - Davis - 2023 - Journal of Clinical Nursing - Wiley Online Library
Most effective - Pharmocological interventions.
There is limited evidence exploring tactile activity interventions for reducing behavioural and psychological symptoms of dementia in acute hospital settings. Individualised approaches in combination with staffing expertise appear central to implementation.
Best Textiles to use ?
5 Textile Considerations When Designing For Dementia - Materialised
The cognitive and sensory impairments people living with dementia may encounter can affect their experience of the world. This means that visual cues, surface texture and patterning are extremely important for signalling where they are, promoting independence and dignity.
One of these is clothing – finding comfortable, easy-to-wear garments that don’t exacerbate confusion or agitation can be a real pain point.
It’s important to choose soft, breathable material that won’t irritate their skin or cause discomfort.
Consideration should be given to contrast, Tactility, patterns, durability and colour.

Wearable Textiles may be more appropriate for dementia patients because they are less bulky.
Building a platform so a caregivers and families can have up to date information about the wellbeing of the patient.
There are some already available -
1. CareSmart
A platform that provides health tracking, medication reminders, and alerts for caregivers.
Lively
Offers wearable devices and a corresponding app that tracks health metrics and sends alerts to caregivers.
3. GrandCare
A comprehensive system that combines health monitoring, communication, and reminders for seniors and their caregivers.
4. Dementia Care App by CareConnect
Designed specifically for caregivers, it includes features for tracking daily activities, medication schedules, and mood tracking.
5. LifePod
An AI-powered voice assistant that offers reminders, alerts, and companionship while keeping caregivers informed.
6. Wellness Coach
A mobile app designed to help caregivers track and manage the health and wellbeing of dementia patients.
Can I change the application or look at modifying it?
These apps more focus on a broader range of services. Like a virtual health provider.
I am looking at a more focused interface just on a couple of modalities. Heart rate and movement.... ? noise activity?
Fully Integrated, Stretchable, Wireless Skin-Conformal Bioelectronics for Continuous Stress Monitoring in Daily Life
Current Evidence for Continuous Vital Signs Monitoring by Wearable Wireless Devices in Hospitalized Adults: Systematic Review - PMC (nih.gov)
it would be really difficult to actually play someone's favourite song as we may not know them or have any previous history. There are many similar devices out there but I want it specifically to be to the ED. The ED is noisy and the nurses are really task focused and can be very busy and chaotic. It would be better for the device to display lights on an interface or a set of lights or something.
There are alot of wearable devices but not really sure that it would work in the ED due to infection control and the idea of it being disposable or how we would manage that.
Exploring the ideas of washable materials or disposable materials
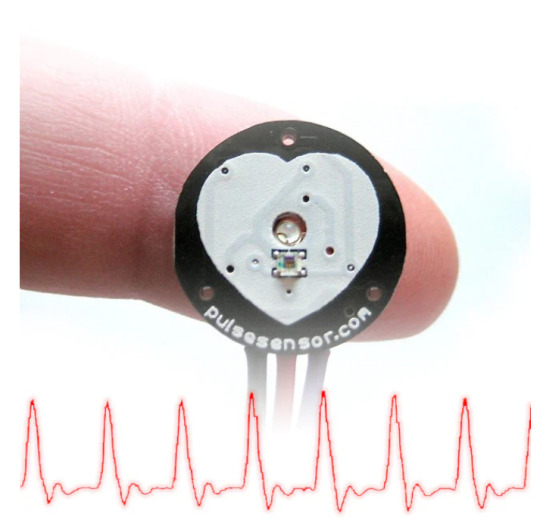
How to monitor pulse rate:
Living electrodes based on green algae in hydrogels
May in the future to be able to use seaweed gel to conduct a circuit - reading the biometric data.
Dorset: AI socks trial could help people with dementia and autism (bbc.com)
these socks are machine washable and detect temp, movement, heart rate and sweat. Then sends the data to AI to interpret and alert carers that the person is escalating.
The machine washable socks are paired with an app, installed on a smartphone.
A sensor embedded in one of the socks collects data from the foot and the ankle of the wearer which is sent to the AI, which estimates whether the person is distressed.
The care team would then be alerted through the app.
Dr Zeke Steer, Milbotix founder, was inspired to make the product after his grandmother began to show signs of early onset dementia.
He said partnering with the council meant the company could "hear the expert voices of people providing and receiving care".
"We are committed to building a product that genuinely help carers and improves wearers' overall wellbeing," he added.

Design Concept 1 Agitation wrist band/arm strap that played music to calm the patient.
Agitation is a common problem in the Emergency Department with high stimulus for a dementia patient. The idea was to identify agitation early and use music therapy to assist with reduction in stressors.
Pros - reduction in stress and agitation. Calmer patient. Reduction in the risks of developing delirium, reduced hospital time and reduction in Medication managment.
Cons - Unaware of patients favourite songs. Would need to consider hearing impairment and disruption to other patients. Need device or sound system linked in to facilitate.
Design Concept 2
Wearable clothing that detected agitation early but was attached to an interface that could alert Nurses in the ED that the patient was getting agitated. Similar to cardiac monitoring.
Pro- Displays on stationary computer continuous monitoring interface so that the nurse could see whilst monitoring cardiac output.
Cons - The clothing may be removed. The nurse isn't always monitoring the stationary computer. So potentially elevations would be missed. Not all patients are accepting of clothing or items unless they are familiar in advanced dementia/alzheimers.
Design Concept 3
Wearable clothing that detected agitation early but was attached to a light or alert system that could alert Nurses in the ED that the patient was getting agitated. through a bright visual cue outside the patients room
Pro - easy visual cue for the nurses to establish who was escalating and provide some intervention.
Con - the wearable clothing may still be an issue....
Maybe a biopatch could be attached to the patient on their back instead so as to not agitate or aggravate them as it may not be felt. ??
In the future seaweed gel could be used as a conductor to create electronic components in wearable design instead of metal.

Process
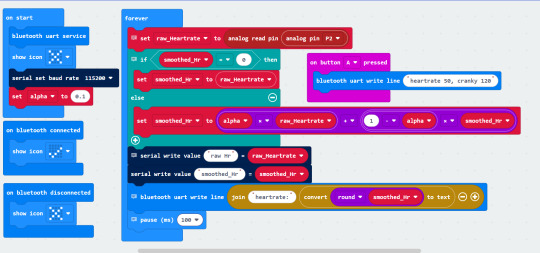
Code to play music if the motion and heart rate exceed the threshold

couldn't get the sats prob pulse monitor to work but did have the microbit. Just keeps playing music because the heart rate monitor is not attached.
now going to change it so it lights up instead...
but there are already socks on the market that can be reappropriated - will try and recreate those and then attach it to the interface.

Another code tried where both the movement and the heartrate were visible. The movement needs to be adjusted to mimic normal body movements and then what would be outside that.
Microbit Blue tooth - Agitation Detector.
Where to place the device
Hands - pull them off or pick at them, Arms - same issues. So placing the microbit in a pair of socks would have been a great iteration and in the future may work however through the process have found that there are too many contributing factors that would actually hinder the data.
Including peripheral vascular diseases therefore limiting blood flow to the peripheral areas.
Another issue I found was the use of medication to control blood pressure and heart rate could also impede the signals putting into a pair of Socks.
In the future a wearable patch would be ideal but for the moment still a work in progress.
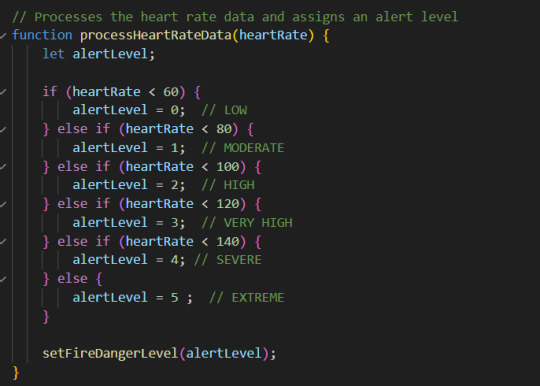
Initially I was looking at the best method for detecting agitation is movement and heart rate. However detecting irregular or irractic moving in a mobile patient would be extremely difficult and could be only applied to a select cohort of patients particularly those who are non ambulatory. This being the case for the purpose of task 3 I have pivoted slightly and am just going to use heart rate to indicate the changes in agigation. An acceleromotor also is not that affective unless it is used in conjunction with another piece of biometric data. Heart rate is the most responsive and will give a good indicator of agitation.
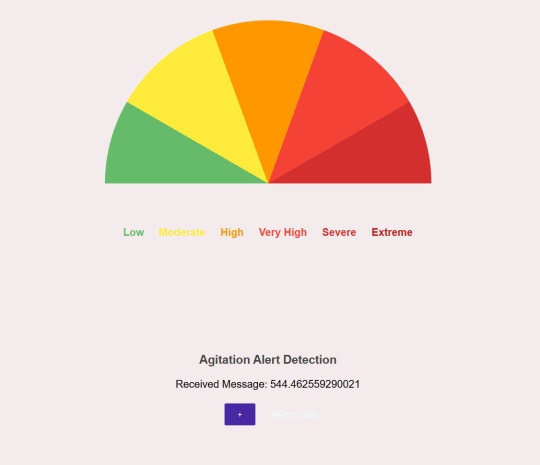
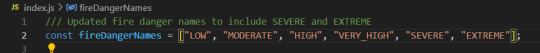
Connecting the microbit and have the styling responsive to the mobile phone/computer interface.
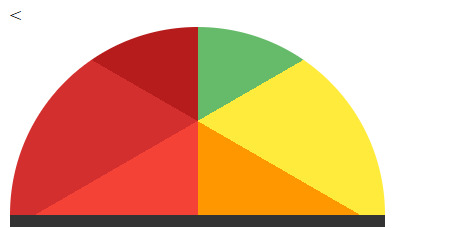
Every time I tried to create the semi circle and changed the background conic gradient in the CSS Styling I woul put the starting point of the wedges in the middle of the semicircle or it would turn it upside down.
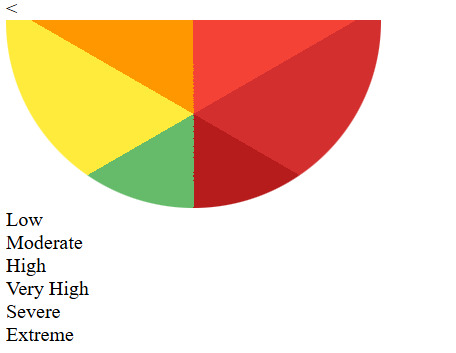
I had to change it multiple times to try and figure out how to get the gradient responding or looking the way I wanted them to look. I was definately trial and error. Eventually I was able to use the code below to visually represent the alert levels. I was many hours of trial and error to establish the right code. It was really difficult to achieve as the way I wanted it set up the coding wasn't the way you would normally do it so made it so complicated to actually achieve the results.

However I am still having difficulty converting the raw data even though I have added the parse int......
it just doesn't want to work.... But on the plus l have been able to blue tooth to my computer making it much easier to work with the interface. '
Have been using a similar code but would not work on the interface as it won't change the data or parse it properly to activate the agitation levels.

I am going to try this one and see if I am able to get it to work based on the raw and smoothed pulse rate data.
Unfortunately I lost both access to the computer and the raw data was still not being read correctly and with this code I lost the simulator as nil serial write code commands were in there. I recompleted the code.
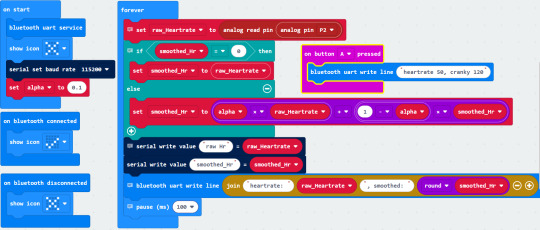
I was able to see the heart rate via the pulse monitor. But wasn't able to convert the heart rate to respond to the interface correctly. It wouldn't work and certainly wouldn't respond to the interface how I wanted it too.
So I just used simulated data to start with so I could get the corresponding styling to work appropriately on the interface.
Concept :
I wanted the heart rate to be visually represented on the interface by highlighting the wedge of the corresponding colour.
Really difficult to achieve to begin with. So I started with just having the different levels and the heading illuminate proving much harder than intended as I was trying to place the headings on the curve of the semicircle.
The names eneded up skewed and in all different positions. So I settled for placing the corresponding name under the different colours. I was able to get these to highlight easily enough and respond to the heart rate.
I added the flashing alert so as nursing staff could identify if the heart rate was at extreme and each of the levels now are visual corresponding the the heart rate.

As documented you can see that the heart rate is moderate . I may have to change the names as it is supposed to be an agitation detector....... This seems a little catastrophic when it is supposed to be referring to an agitation level.

Flashing - for severe agitation.
I was able to get the styling working based on the simulated heart rate.
However it meant that the wearable device would effectively not have worked.
After some debugging it was found that the incoming message from the microbit was too long and therefore crashing out the system.
Changing the microbit code allowed the smoothed heartrate only to come through and there was also an issues with the javascript that has also been fixed.
The new code for the microbit.
The heartrate is now displaying and am able to connect to the bluetooth on the computer.
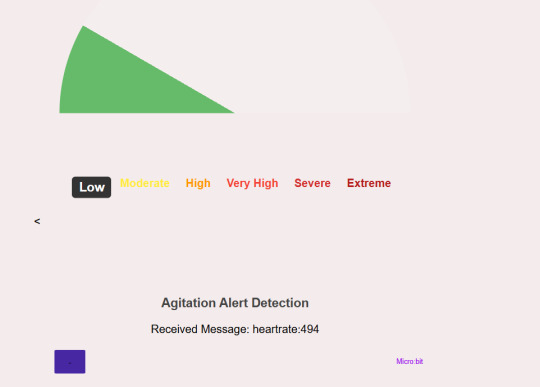
I have just realised the the very high visual doesn't actually high light the word very high?
Not sure what is happening there.
checked the CSS -

All the levels are identified there.
Will check the java :
Seems to be nominated there too!!
Will now check the html :
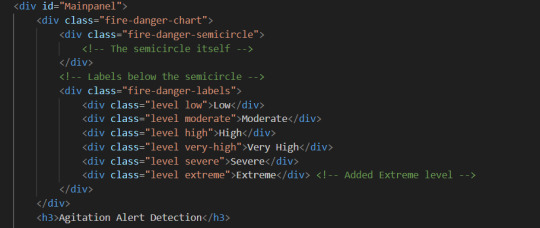
In each section it appears to be mentioned so I am not sure why that level is not being highlighted.
After a little bit of research I changed a few things -
HTML -
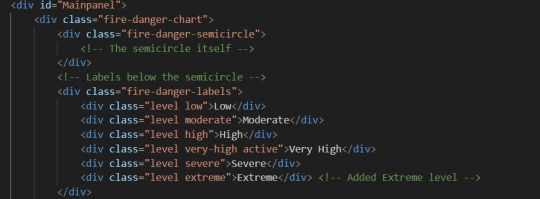
just made the level - very-high active
CSS -
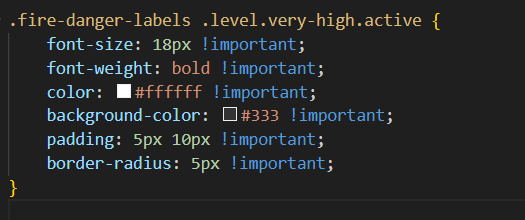
I initially tried out this to see if I could get it too work. Still not happening - Then checked the developer tools and it says :
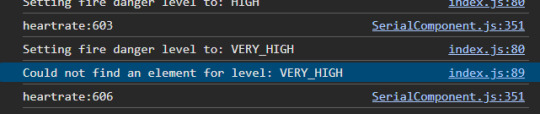
just went through all the code and found :
That in this part of the code it doesn't match to the rest of the description of very high due to the underscore between the words as all the other descriptions are very-high.
I went ahead and changed the code.

The problem is fixed. It is all now working as initially intended in the concept.
But I think it would be better to change the names of the levels - to be more indicative of escalating behaviour rather than catastrophise it all and be a cause of concern to patients, nurses and doctors in the department.
Updated the code...... the names look better.
Wearable Device
With changing from the socks I had to come up with another idea the would both be able to house the microbit, battery pack and pulse sensor. Research suggest that tactile/sensory items can have a positive effect on a patient with dementia. So I have decided to house the microbit in a material called tubi - grip common to ED in like a wrist guard fashion and add some sensory elements so the patients can fiddle with those instead.
0 notes
Text
RESEARCH - Intentional Lifestyling
Intentional life styling Australians are styling their lives rapidly after reflective periods during lockdowns and isolation by bringing ahead major life decisions like moving homes, changing locations, jobs, hobbies and social commitments. It’s the trend of designing lifestyles with intentionality and clarity.
Using this mind set I have come up with the idea to use AI with the intention to design ones own health team. With moving homes changing location and social commitments we can attempt to create our own health team of allied health, GP, natural therapists, surgeons if necessary and have all the health data stored on our medicare cards via QR so as to obtain the best health care providers based on our needs, personal preferences, personalities, financial situations and localities.
Our Health System
Medicare – the foundation of our health system
Medicare has been Australia’s universal health care scheme since 1984. Its 3 major parts are:
medical services
public hospitals
medicines
Medicare is available to Australian and New Zealand citizens, permanent residents in Australia, and people from countries with reciprocal agreements.
Medicare covers all of the cost of public hospital services. It also covers some or all of the costs of other health services. These can include services provided by GPs and medical specialists. They can also include physiotherapy, community nurses and basic dental services for children.
The other important part of Medicare is the Pharmaceutical Benefits Scheme (PBS). The PBS makes some prescription medicines cheaper.
Health system challenges
Australian health system challenges include:
an ageing population and increasing demand on health services
increasing rates of chronic disease
costs of medical research and innovations
making the best use of emerging health technologies
making better use of health data
These challenges look set to continue in coming decades.
Cost of health care in Australia
Australia’s health system is complex — and so are its funding arrangements. It is funded by:
all levels of government
non-government organisations
private health insurers
individuals when they pay out-of-pocket costs for products and services that aren’t fully subsidised or reimbursed
In 2016–17, Australia spent nearly $181 billion on health:
41% by the Australian Government
27% by state and territory governments
17% by individuals (for products and services that aren’t fully subsidised or reimbursed)
9% by private health insurers
6% by non-government organisations
Health spending was about 10% of gross domestic product. This means $1 in every $10 spent in Australia went to health.
The Australian Government usually funds most of the spending for medical services and subsidised medicines. It also funds most of the $5.5 billion spent on health research in Australia in 2016–17.
State and territory governments fund most of the spending for community health services.
The Australian Government and state and territory governments share funding of public hospital services.
https://www.health.gov.au/about-us/the-australian-health-system
0 notes
Text
You are to create a persuasive pitch for your own innovative, new product concept that addresses a gap that you have identified in the market.
Health Harmony ???
Matching specialists to patients is an important aspect of healthcare. According to a blog post by Philips Global, there is a concept of a healthcare system that can match each patient with their perfect GP, specialist, or even hospital based on acuity, capability, availability, location and even personality type.
Communication is the key to health literacy. If we have health providers we trust then we are more likely to understand and comprehend.
NPHS Summary (health.gov.au)
Statistics have found that Gen Y and Gen Z are more likely to quit a job if the employers ethics and values are not in line with their own. Looking at health prevention if the GP, Specialists and Allied health providers were matched with the person then potentially would improve health literacy and preventative health care being undertaken.
What if we could match every patient to their ideal doctor? - Blog | Philips
Study on specialist outpatient matching appointment and the balance matching model | SpringerLink
Patient / procedure matching protocols | Australian Commission on Safety and Quality in Health Care
Australian Attitudes
I understand that “she’ll be right” is a phrase used by Australians to emphasize a laidback attitude to life. However, this attitude doesn’t always work when it comes to health. According to the Australian Physiotherapy Association (APA), tradies are being urged to ditch the old-school ‘she’ll be right’ attitude to their health so they can continue to support Australia’s economic recovery. The APA wants tradies to take care of their health and not delay seeking help for medical problems. The region’s Men’s Health Coordinator is also encouraging men not to delay seeking help for medical problems, as part of Men’s Health Week.
Using AI to construct algorithms and information based on present forms conduct searches and matches... similar to e-harmony but with integrated health care - ecosystem.
Gen Y, or Millennials, were born between 1981 and 1994/6, and are currently between 25 and 40 years old. They were raised by Baby Boomers and tend to value collaboration, feedback, and recognition. Gen Z is the newest generation, born between 1997 and 2012, and are currently between 9 and 24 years old. They were raised by Generation X and tend to value independence, privacy, and security1
Although we have an elderly population many of those are not longer contributing to the funding of the health system. How can we ensure younger people are more health literate going forward and we can prevent chronic conditions.
Broadening the definition of HL, the World Health Organization explains that it “means more than being able to read pamphlets and successfully make appointments. By improving people's access to health information and their capacity to use it effectively, health literacy is critical to empowerment.16”
The Evolution of Health Literacy and Communication: Introducing Health Harmonics (sciencedirectassets.com)
Patients’ healthcare, education, engagement, and empowerment rights’ framework: Patients’, caretakers’ and health care workers’ perspectives from Oromia, Ethiopia - ProQuest
The study identified three major categories of healthcare rights (clinical, socio-cultural, and organizational), incorporating supporting elements of education, engagement, and empowerment.
Study participants reported detailed rights the patients would have during hospital visits which included the right to timely access to care and treatment, adequate medications) with full respect, dignity, and without any discrimination. Patients widely perceived that they had the right to tell their illness history and know their illness in the language they can understand. It was also widely agreed that patients have the right to be educated and guided to make informed choices of services, procedures, and medications.
Additionally, patients reported that they had the right to be accompanied by caretakers together with the right to use facilities and resources and get instructions on how to utilize these resources, the right to be protected from exposure to infections and unsafe conditions in hospitals, right to get a diet of their preference, and right to referral for further care. Nevertheless, there was a common concern among patients and caretakers that these rights were mostly non-existent in practice which were due to barriers related to patients (fear of consequence; a sense of dependency, feeling of powerlessness, perceptions of low medical literacy), health workers (negligence, lack of awareness and recognition of patient rights, undermining patients), and facilities’ readiness and support, including lack of guiding framework.
RESEARCH
Intentional life styling, where Australians are styling their lives rapidly after reflective periods during lockdowns and isolation by bringing ahead major life decisions like moving homes, changing locations, jobs, hobbies and social commitments.
With this in mind being able to choose your own health team to improved health literacy and reduce the burden to the health system.
Evidence supports the close relationship between people’s health and the living and working conditions which form their social environment (Baum 2018; Wilkinson and Marmot 2003). Factors such as socioeconomic position, conditions of employment, the distribution of wealth, empowerment and social support – known collectively as the social determinants of health – act together to strengthen or undermine the health of individuals and communities.
https://www.aihw.gov.au/reports/australias-health/social-determinants-of-health
The World Health Organization (WHO) describes social determinants as ‘the non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies and political systems’ (Senate Standing Committees on Community Affairs 2013; WHO 2022).
Social determinants form part of the wider determinants of health which also include the environmental, structural, economic, cultural, biomedical, commercial and digital factors in our lives (Department of Health 2021).
The National Preventive Health Strategy presents a powerful opportunity for Australia to build a sustainable prevention system for the future – building on previous success and momentum, addressing the increasing burden of disease, reducing health inequity and increasing preparedness for emerging health threats.
https://www.health.gov.au/sites/default/files/documents/2021/12/national-preventive-health-strategy-2021-2030_1.pdf
More holistically, health is a state of physical, mental and social wellbeing, and for Aboriginal and Torres Strait Islander people and other communities, this also includes cultural wellbeing.
Australian Health Care System.
Australia’s long-term health reforms
All Australian governments have agreed to progress long-term system-wide health reforms under the NHRA.
The long-term reforms will examine how well the different components of the health system interact. Governments will work with the health sector to better understand and remove systemic barriers to improving health care.
The reforms will give local health services the flexibility to try new solutions to address these barriers and improve service delivery. This will ensure health services best suit the needs of their local community.
The 6 reforms outlined in Schedule C of the NHRA are:
empowering people through health literacy – person-centred health information and support will empower people to manage their own health well and engage effectively with health services
prevention and wellbeing – to reduce the burden of long-term chronic conditions and improve people’s quality of life
paying for value and outcomes – enabling new and flexible ways for governments to pay for health services
joint planning and funding at a local level – improving the way health services are planned and delivered at the local level
enhanced health data – integrating data to support better health outcomes and save lives
nationally cohesive health technology assessment – improving health technology decisions will deliver safe, effective and affordable care.
The National Health Reform Agreement Long Term Reforms Roadmap was endorsed by all Australian Health Ministers at the Health Ministers’ Meeting on 17 September 2021.
More holistically, health is a state of physical, mental and social wellbeing, and for Aboriginal and Torres Strait Islander people and other communities, this also includes cultural wellbeing1, Australians in good health are better able to lead fulfilling and productive lives, participating fully in their community, in their education and/or in their employment. The benefits of this are experienced system-wide with decreased disease burden leading to a reduction in the pressures on our health and aged care systems, and economic benefits demonstrated by an increase in Australia’s gross domestic product (GDP).
https://www.health.gov.au/sites/default/files/documents/2021/12/national-preventive-health-strategy-2021-2030_1.pdf
0 notes
Text
Worm Farming or Vermiculture.....

0 notes
Text
Behaviour Change
Where does it start?
Children are the most prominent advocates for change !!
Worm farming to reduce household waste
Worm Juice to fertilise gardens & new crops
Worm compost to regenerate soil
Households are the biggest contributors to food waste.
how to build an easy and cheap worm Farm
0 notes
Text
Who do you want to develop for???
Developing worm farms for kids..... or Gardening enthusiast, environmental enthusiast
How to set up your own worm farm?? how do you develop compost.....
If people knew about the waste would they want to change it?
Would they want to make a difference?
What could be the incentive
0 notes
Text
Zine - Vis Communication & Culture
Ideation - Food Waste.
Why we need to reduce food waste
Food waste, whether it be food that never leaves the farm, food that is lost during transport, or food that is wasted from the hospitality sector and households, has significant economic and environmental impacts:
One third of the world's food is wasted.
25% of water used in agriculture is used to grow food that is ultimately wasted – throwing away one burger wastes the same amount of water as a 90 minute shower.
Food waste produces eight per cent of global greenhouse gas emissions. If food waste was a country it would be the third largest greenhouse gas emitter, behind the USA and China.
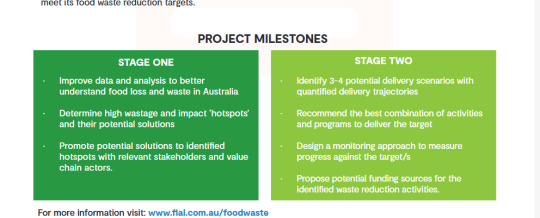
Food waste is also a major problem in Australia. The National Food Waste Strategy Feasibility Study produced by Food Innovation Australia Limited reported that:
Food waste costs the economy around $36.6 billion each year.
Each year we waste around 7.6 million tonnes of food across the supply and consumption chain – this wastage equals about 312kg per person, equivalent to around one in five bags of groceries or $2,000 to $2,500 per household per year.
Food waste accounts for approximately 3% of Australia’s annual greenhouse gas emissions.
Australia uses around 2600 gigalitres of water to grow food that is wasted – this equates to the volume of water in five Sydney Harbours.
The amount of land used to grow wasted food covers in excess of 25 million hectares, a landmass larger than the state of Victoria.



0 notes
Text
Culture - What is it??
It is not just how it is represented but how culture is interpreted.
Maybe a DIY culture......
0 notes
Text
Zine Creation - DES 212
IDEATION .
Ideas - Social, Political, Cultural Theme....
homelessness, poverty, breastfeeding, one use plastic, recycling, healthcare, yes vote, war in ukraine, cost of living, housing crisis, youth crime, Arts policy
National cultural policy, Addiction issues, post natal depression, Domestic violence,
gardening - creating community gardens - with bush tucker and paths elevated to be inclusive to all..
community cooking to reduce junk food consumption.
Arts in the community to make a more cohesive.
Social media and the impact on children.....!!
0 notes
Text
First iteration.......
After brain storming and bundling the ideas the first part of my artefact needed to be about education and getting the information into the community about "what a health directive was and what needed to be considered to make one"
The information was drawn from Form 4 Advanced health directive....
Currently awaiting feedback for the first iteration......
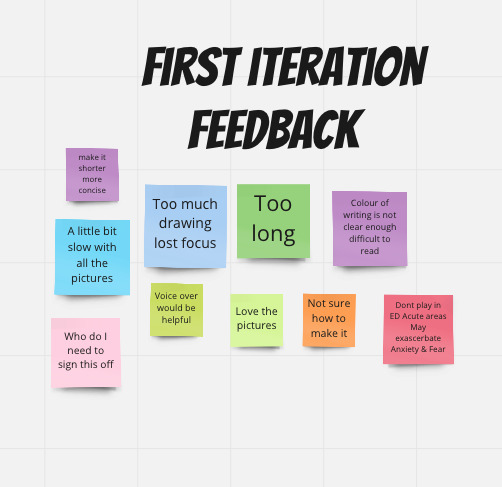
From the feedback - It was really informative but some information was missing in relation to how it actually gets made and where that happens.....
It was a tad too long with all the drawings - need to change how the presentation actually works.....
I will need to add in more information about the document and how it can be accessed by health providers in the future.....
0 notes
Text
Rapid Prototyping Ideas - IDEO pg 119.


Rapid prototyping - Health Kiosk, Phone app, Interactive video or Pop up booklet.
Health kiosk - answer questions with real time health outcomes and print out is given with patients choices to be taken to GP for further discussion,
Phone app - with similar info to kiosk - email results to client/health provider
Interactive type video - to be played in waiting rooms including real time potential outcomes
Booklet provided in pensioner pack to start the conversation about future care plan.
1 note
·
View note
Text
Assessment 3 - Health Sustainability - Research
Starting the conversation about advance care planning is an important first step in ensuring a person's preferences for future care are known and respected.
If a person's preferences are not known, doctors may use aggressive treatments that the person might not have wanted - and families may feel burdened by the worry that they will make a wrong choice.
Thinking about and planning for the future is a normal part of life so you shouldn't be afraid to raise the subject.
For family, friends and carers
Serious illness or injury can mean that a person cannot make their own decisions about health care and treatment. Starting planning early helps give the person, their family and their carer peace of mind.
Advance care planning is a normal part of life and is voluntary. Talking about values, beliefs and health and care preferences is an important part of family relationships and friendships. Most people are not used to talking about a time when they can’t make their own decisions, so they may need some time to think before they talk about their choices.
Encourage the person to speak with their family, friends, carer and doctor if they haven’t already.
Advance care planning is an ongoing conversation - it should not happen only one time. Everyone’s values and goals change, what they consider acceptable outcomes might change, so they might want to update their plan.
For health and care workers
Advance care planning conversations should be seen as a normal part of life and of a person’s ongoing healthcare plan. These conversations are voluntary. Encourage people to think about their beliefs, values and preferences regarding their current and future health care. Discuss their attitudes, life goals, and acceptable outcomes regarding healthcare treatment options.
Ideally, advance care conversations should begin when a person is medically stable, comfortable and accompanied by their substitute decision-maker(s), family, friends and/or carer.
Beginning points for advance care planning conversations can include:
when a person or family member asks about current or future treatment options and goals
at an age- or condition-related health assessment
when an older person receives their annual flu vaccination
when there is a diagnosis of a metastatic malignancy or end organ failure, indicating a poor prognosis
when there is a diagnosis of early dementia or a disease which could result in loss of capacity
if you would not be surprised if the person died within twelve months
if there are changes in care arrangements (for instance, admission to a residential aged care facility)
Care worker conversations
Care workers play an important role in supporting the person with daily activities and listening to their concerns. During your time together you can have conversations about their values and preferences. Also, encourage the person to speak with their family, friends and doctor.
For general practitioners
Consider advance care planning conversations if the patient:
has an advanced chronic illness (e.g. COPD, heart failure)
has a life limiting illness (e.g. dementia or advanced cancer)
is aged 75 years or older, or 55 years or older if they are an Aboriginal and/or Torres Strait Islander person
is a resident of, or is about to enter, an aged care facility
is at risk of losing competence (e.g. has early dementia)
has a new significant diagnosis (e.g. metastatic disease, transient ischemic attack)
is at a key point in their illness trajectory (e.g. recent or repeated hospitalisation, commenced on home oxygen)
does not have anyone (e.g. family, caregiver, friend) who could act as substitute decision-maker
may anticipate decision-making conflict about their future health care
has a carer
may likely pass away in the next 12 months
_________________________________________________

Method :IDEO Conversation Starters - using this method to find the themes surrounding advanced care planning.
1 note
·
View note
Text
Survey - Advanced Care Planning
I developed the survey to try and understand some of the complexities surrounding Advanced Care planning. Trying to establish what was the main issue as to why people haven't completed any planning.
The survey revealed that education, understanding and time really influenced decisions.
A few people knew what they were for but not everyone had them.
Need to do some interviews to find out why people had not completed them even though they knew what they were for!
1 note
·
View note