#2d And 3d Mammograms
Text
Breast cancer is deadlier for Black women. A study of mammograms could help close the gap
Breast cancer is deadlier for Black women. A study of mammograms could help close the gap
https://www.statnews.com/2023/10/17/breast-cancer-3d-mammograms-study-black-women/?utm_campaign=rss
Are 3D mammograms better than standard 2D imaging for catching advanced cancers?
A clinical trial is recruiting thousands of volunteers — including a large number of Black women who face disparities in breast cancer death rates — to try to find out.
Read the rest…
via STAT Health - Science, medicine and healthcare news https://www.statnews.com/category/health/
October 17, 2023 at 11:53AM
2 notes
·
View notes
Text
Breast Imaging Market Insights: Technological Breakthroughs Boosting Global Adoption

The Breast Imaging Market is expected to grow significantly from USD 4.2 billion in 2023 to USD 7.1 billion by 2030, reflecting a compound annual growth rate (CAGR) of 8.0%. This expansion is driven by a combination of rising breast cancer cases, technological advancements, and growing awareness about early detection. In this article, we will dive deep into the factors influencing the breast imaging market, the types of imaging technologies available, and the market’s regional analysis.
Global Market Overview
The breast imaging market has seen impressive growth over recent years, with an estimated value of USD 4.2 billion in 2023. By 2030, this market is projected to reach USD 7.1 billion, driven primarily by innovations in imaging technology and the rising global prevalence of breast cancer. The expected CAGR of 8.0% showcases the increasing importance of breast imaging in healthcare.
Factors Driving the Growth of the Breast Imaging Market
Rising Breast Cancer Prevalence: One of the most significant drivers of the breast imaging market is the alarming increase in breast cancer cases worldwide. According to the World Health Organization (WHO), breast cancer is the most commonly diagnosed cancer among women. Early detection through imaging has proven to improve survival rates, making it a cornerstone in cancer management.
Technological Advancements: The continuous advancement in imaging technologies, such as the transition from traditional 2D mammography to 3D digital mammography, has fueled market growth. These innovations provide clearer images, improving diagnostic accuracy and reducing false positives and negatives.
Awareness and Early Detection Programs: Governments and health organizations are investing heavily in breast cancer awareness campaigns, pushing for regular screenings, especially for women over the age of 40. This has led to an increased demand for imaging services, thereby contributing to market growth.
Download Sample Report @ https://intentmarketresearch.com/latest-reports/breast-imaging-market-3590.html
Challenges in the Breast Imaging Market
High Costs of Imaging Technology: While the demand for breast imaging is rising, the high costs of advanced imaging technologies remain a barrier, particularly in low-income regions. The need for affordable imaging solutions is a significant challenge for both manufacturers and healthcare providers.
Limited Access in Developing Regions: In many developing countries, access to high-quality breast imaging remains limited due to inadequate healthcare infrastructure and the unavailability of trained professionals. This disparity hinders market growth in these regions.
Key Types of Breast Imaging Technologies
Mammography: Mammography is the most widely used breast imaging technology, and it has evolved significantly over the years. The shift from 2D to 3D mammography has led to more accurate detection of small tumors, which may not be visible on traditional mammograms.
Ultrasound Imaging: Ultrasound is often used as a supplementary imaging tool, especially for women with dense breast tissue. It provides real-time images, helping doctors detect abnormalities that may not be visible on mammograms.
Magnetic Resonance Imaging (MRI): MRI is known for its high sensitivity in detecting breast abnormalities. It is particularly useful for high-risk patients and those with dense breast tissue. However, the high cost of MRI remains a limitation for widespread use.
Nuclear Imaging: Technologies like PET (Positron Emission Tomography) and Molecular Breast Imaging (MBI) are gaining traction in the market. These imaging modalities offer precise molecular-level details, which can be critical for detecting early-stage cancer.
Optical Imaging: Still in its nascent stage, optical imaging is being explored for its potential to offer non-invasive and radiation-free imaging. This could represent the future of breast imaging technology.
Regional Analysis of the Breast Imaging Market
North America: North America holds the largest share in the global breast imaging market, driven by the high prevalence of breast cancer, advanced healthcare infrastructure, and the availability of leading imaging technologies.
Europe: Europe is also a significant player in the breast imaging market, with increasing investments in healthcare technologies and rising adoption of advanced breast imaging solutions.
Asia-Pacific: The Asia-Pacific region is the fastest-growing market for breast imaging. This growth is fueled by increasing healthcare spending, rising awareness of breast cancer, and improvements in healthcare infrastructure, especially in countries like China and India.
Latin America and Middle East & Africa: While these regions represent smaller portions of the global market, they offer significant growth potential. Improving healthcare infrastructure and increasing awareness campaigns are expected to boost demand for breast imaging services in the coming years.
Impact of COVID-19 on the Breast Imaging Market
The COVID-19 pandemic had a profound impact on the breast imaging market, with many elective procedures and screenings delayed or canceled. However, as the world moves towards post-pandemic recovery, there is a resurgence in demand for breast imaging services, particularly as delayed diagnoses are being addressed.
These companies are at the forefront of developing innovative breast imaging technologies to meet the growing demand.
Access Full Report @ https://intentmarketresearch.com/latest-reports/breast-imaging-market-3590.html
Emerging Trends in Breast Imaging
AI and Machine Learning in Imaging: Artificial intelligence (AI) and machine learning are revolutionizing breast imaging by improving diagnostic accuracy and efficiency. AI-powered tools are being integrated into imaging systems to help radiologists interpret images more quickly and accurately.
Personalized Breast Imaging: The future of breast imaging may also involve more personalized approaches, where imaging modalities are tailored to individual risk factors, such as genetics and breast density.
Future Outlook for the Breast Imaging Market
With a projected market value of USD 7.1 billion by 2030, the breast imaging market is poised for significant growth. Advancements in technology, combined with rising awareness and government initiatives, will continue to drive the market forward.
Conclusion
The breast imaging market is on a path of rapid expansion, driven by the increasing prevalence of breast cancer and technological innovations. As awareness grows and access to imaging improves, the demand for effective breast imaging solutions will continue to rise. The future looks promising, with AI, personalized imaging, and new technologies on the horizon.
FAQs
What are the key factors driving the breast imaging market growth?
The growth is driven by rising breast cancer cases, technological advancements in imaging, and increased awareness of early detection.
Which imaging technology is most commonly used?
Mammography, particularly 3D mammography, is the most widely used breast imaging technology.
How has COVID-19 affected breast imaging services?
The pandemic caused delays in screenings, but demand is recovering as healthcare services normalize.
What are the challenges in the breast imaging market?
High costs and limited access to advanced technologies in developing regions are major challenges.
How will AI impact the future of breast imaging?
AI will enhance diagnostic accuracy and efficiency, helping radiologists detect cancer earlier and more accurately.
Contact Us
US: +1 463-583-2713
0 notes
Text
Exploring the Range of Medical Imaging Services: What You Need to Know
Medical imaging is a key part of diagnosing and checking various health problems. Thanks to advances in technology, there are now several different imaging techniques, each with its own benefits. Knowing about these different imaging services can help you make better choices about your health care. Here’s a simple look at some common imaging services.
Understanding CT Scans
A CT scan Computerized Tomography is a commonly used imaging technique. It uses X-rays to take detailed pictures of the inside of your body, showing more than regular X-rays can. CT scans are useful for looking at the brain, chest, abdomen, and pelvis. They help doctors see your internal organs, bones, tissues, and blood vessels clearly. If you have a serious injury, infection, or suspected cancer, a CT scan can provide important information to help guide your treatment.
PET-CT Scans for Cancer
For people with cancer, imaging is important for both diagnosis and treatment. A PET CT scan for cancer combines two powerful tools: Positron Emission Tomography (PET) and Computerized Tomography (CT). This combination gives doctors detailed images of how your tissues and organs are working. It helps them find the exact location of cancer cells, see how well treatment is working, and check for any return of cancer. PET-CT scans are very accurate and are often the preferred method for doctors treating cancer.
Fast Breast MRI: Quick and Detailed Breast Imaging
Breast imaging has improved with the fast breast MRI. Unlike mammograms, which use low-dose X-rays, an MRI uses magnetic fields and radio waves to take detailed pictures of the breast. A fast breast MRI is especially helpful for women with dense breast tissue, where mammograms might not catch everything. The “fast” part means the scan is quicker without losing image quality. This method is often used for high-risk patients or those needing very detailed imaging.
3D Ultrasound: Better Prenatal Care
Parents can benefit from advanced technology like 3D ultrasound. Unlike the regular 2D ultrasound, which shows flat images, 3D ultrasound creates three-dimensional pictures, giving a clearer view of the baby. This is very helpful in prenatal care, as it helps detect any problems early on. Many parents also choose 3D ultrasound for a more realistic image of their baby, which can be a special part of the pregnancy experience.
Conclusion
Knowing about the different types of medical imaging services helps you make better health decisions. Whether it’s a CT scan for detailed images of the inside of your body, a PET-CT scan for precise cancer detection, a fast breast MRI for quick breast imaging, or a better parental service, 3D ultrasound in Ventura has its own strengths. At Palms Imaging, experts provide the best services with the latest technologies. As technology advances, they know these imaging services will continue to play a crucial role in diagnosing and treating health conditions, ensuring patients receive the best possible care. For more details, visit the website.
0 notes
Text
Breast Imaging: Exploring the Technologies Improving Early Detection

Breast radiation image photography utilizes various technologies to examine breast tissue for abnormalities that could indicate breast cancer or other issues. Understanding the different modalities used can help in choosing the right exam.
Mammography
Mammography is considered the gold standard breast cancer screening tool. A low-dose x-ray of the breast is used to detect subtle changes in breast tissue up to two years before a physical exam. Digital mammograms can find 30-40% more invasive Breast Imaging than film mammograms and are now the standard of care in the U.S. Mammograms are best at finding microcalcifications and masses but have limitations in detecting tumors in women under 50 with dense breast tissue.
Breast Ultrasound
An ultrasound uses high-frequency sound waves to create images of breast tissue. It is helpful in differentiating between solid masses and fluid-filled cysts. Ultrasound is often used along with mammograms for women with dense breast tissue, a personal history of breast cancer, or suspicious areas found during a physical exam or mammogram. It provides additional information on the shape, outline, and internal look of abnormalities.
Breast MRI
A breast MRI uses a strong magnetic field and radio waves to produce detailed images of breast tissue. Considered the most sensitive exam, MRI has an advantage over mammograms and ultrasounds in women at high risk for breast cancer due to genetic mutations or a family history. It can detect cancers too small for other methods and monitor treatment response in patients already diagnosed. However, MRIs also have more false positives requiring follow up exams.
Molecular Breast Imaging
Molecular breast radiation image photography (MBI) uses specialized cameras and radiotracers injected into the body to image the molecular activity in breast tissue. It is more sensitive than mammography or ultrasound in women with dense breasts but not as common as other modalities. MBI does expose patients to ionizing radiation though less than a mammogram. Research continues to define its role as a supplemental screening tool.
Advances in 3D Mammography - Tomosynthesis
3D mammography, also known as breast tomosynthesis, is an advance over 2D digital mammography. It takes multiple low-dose x-ray images of the breast from different angles and uses computer algorithms to construct 3D views. This reduces tissue overlap, allowing radiologists to better detect small invasive cancers and differentiate suspicious abnormalities from overlying tissues. Studies show a substantial improvement in accuracy over 2D mammograms alone, especially for women with dense breasts. Tomosynthesis is becoming a standard component of digital screening mammograms.
The Role of Breast Biopsies
When an abnormality is spotted on a mammogram, ultrasound, or MRI, a breast biopsy may be recommended. Several methods can be used depending on the type and location of the abnormality. A core needle biopsy uses a long hollow needle to extract a sample of breast tissue for analysis under a microscope. A vacuum-assisted biopsy also removes multiple samples. Stereotactic or image-guided biopsy utilizes mammogram images to pinpoint the exact location for sampling. Surgical biopsies may follow if previous methods are unsuccessful in obtaining an adequate tissue sample. The goal is to definitively diagnose any suspicious breast changes as cancerous or noncancerous.
Emerging Technologies on the Horizon
Research continues to explore new technologies and applications that may improve breast cancer screening and diagnosis. Among these are diffuse optical tomography which measures light absorption in breast tissue as a possible low-cost supplement to mammography. Breast-specific gamma imaging traces radiotracers to provide 3D images highlighting areas of molecular changes within the breast. AI and machine learning are showing potential to aid radiologists in analyzing breast images, especially in women with dense breasts. Whole breast ultrasound, contrast-enhanced spectral mammography, and molecular breast tissue markers are also areas attracting research interest. Advances aim to achieve earlier cancer detection when treatments are most effective.
How Imaging Modalities are Used Together
The various breast radiation image photography exams all play important but different roles and work best when used as complementary tools. Mammography remains the primary screening method, supplemented by ultrasound or MRI as needed based on density, risk factors, or suspicious findings. Newer 3D mammography provides a significant upgrade over previous 2D imaging. Biopsies remain essential to diagnose suspicious areas.
NO single exam examines all breast tissue or captures every potential abnormality. By combining modalities strategically, radiologists gain a more complete picture for accurate evaluation and monitoring of women's breast health over time. Continuous technological advancements hold promise to further enhance early detection capabilities.
Get More Insights On, Breast Imaging
About Author:
Money Singh is a seasoned content writer with over four years of experience in the market research sector. Her expertise spans various industries, including food and beverages, biotechnology, chemical and materials, defense and aerospace, consumer goods, etc. (https://www.linkedin.com/in/money-singh-590844163
#Mammography#Digital Mammography#Breast Cancer Screening#Diagnostic Imaging#Breast Health#Breast Density
0 notes
Text
A mammogram is an essential and painless procedure that is crucial for maintaining your breast health!
"The pain associated with mammography is a significant impediment to women's participation in breast screening."
Breast cancer becoming a serious concern and significantly influences global health burden, with high rates of incidence and mortality among women. Screening mammography drives positive changes among breast cancer victims by early detection and improved survival rates.
However, the pain associated with 3D mammography has been recognised as a substantial barrier preventing women from participating in breast screening programs. This research article aims to explore the impact of breast screening procedures from mammography giving comfort on women's willingness to undergo breast screening and suggests potential strategies to address breast health issues.
The Significance of Mammography Diagnostic Instruments Screening:
3D Mammography Diagnostic Instruments is a screening method primarily used to detect breast cancer in its early stages, often before symptoms manifest.
Detecting a medical condition at an early stage can significantly increase the chances of successful treatment and improve the survival rates of the patient. Considering the high prevalence of breast cancer, it is essential to encourage month-interval mammography screening participation among women to enhance early detection and reduce mortality rates.

The Pain Barrier From Traditional 2D Mammography:
The discomfort experienced during a traditional 2D mammogram, including compression and breast positioning, is a common concern among women. The physical pain associated with the procedure can range from mild discomfort to intense levels that deter women from participating in regular screenings.
Fear of potential pain and anxiety related to the procedure have been consistently identified as recurring themes influencing screening avoidance, particularly among women who have never undergone traditional 2D mammography.
Psychological Factors:
In addition to physical discomfort, psychological factors contribute to the pain barrier in 2D mammography. Anxiety, embarrassment, and fear of the unknown can intensify the perception of pain. Negative experiences shared by peers or through media sources might amplify these fears.
Addressing these psychological factors is crucial to mitigating the pain barrier and encouraging women to prioritise their breast health through month-interval screenings.
Few Statistics That Drew Importance of Mammography Diagnostic Instruments Breast Health Screening!
The age-standardized breast cancer incidence rate is a useful parameter for comparing breast cancer rates in populations with different age groups. It is calculated by taking a weighted average of age-specific rates based on a standard age distribution. This allows for fair comparisons between different groups or countries.
The global death toll from breast cancer in 2020 was recorded at 684,996, representing 6.9% of all cancer-related deaths.
It is estimated that in 2022, a person has a 1 in 105 (or 0.95%) risk of dying from breast cancer by the age of 85. The risk for males is 1 in 4,732 (0.02%), while for females, it is 1 in 53 (1.9%).
The survival rate for localised or Stage 1 breast cancer in the United States is 99% within 5 years, according to the American Cancer Society.
In 2020, there were an estimated 2.3 million new cases of breast cancer worldwide, accounting for 11.7% of all new cancer cases.
Out of these new cases, 20,640 are expected to be breast cancer diagnosed in 2022, with 212 cases occurring in males and 20,428 cases in females.
In 2022, it is estimated that there will be 3,214 deaths from breast cancer globally, with 36 deaths occurring in males and 3,178 deaths in females.
In Australia, there were 3,144 deaths attributed to breast cancer in 2020, with 34 deaths occurring in males and 3,110 deaths in females.
Early 3D mammogram screening accurate detection of breast cancer with comfort!
Have you been hesitant to undergo a 3D mammogram screening because of the pain associated with the procedure? Many women share this concern, but it is important to understand the benefits of month-interval 3D mammogram screening in detecting breast cancer early and improving survival rates.
Mammography uses X-rays to detect early breast cancers but to get an accurate reading, the mammography diagnostic instruments do not need to compress the breasts. This zero compression can cause comfort or no pain, leading some women to opt out of regular screenings. Approximately, 35% of women report pain with the procedure.
That's why a recent review was conducted by Dawn Miller, Vicki Livingstone, and G Peter Herbison, (Cochrane Breast Cancer Group) in their systematic review, (University of Otago) Women's and Children's Health, Dunedin School of Medicine has identified and evaluated different interventions designed to reduce the pain and discomfort that women experience during mammography screening procedures. The review only included well-designed and relevant studies, with a total of seven studies meeting the criteria.
The studies included a variety of interventions, such as providing women with verbal or written information before the procedure, using pain relief medication before the examination, using a breast cushion to pad the mammography equipment, patient-controlled compression of the breast, and reducing compression force by the technician.
The results showed that giving women experience of the procedure before the mammogram can reduce pain and discomfort during the mammography test.
Additionally, when women had more control over breast compression, it could also reduce the pain they experience. However, there was no significant change in pain when a technician reduced the compression force.
So, Instudy, breast cushions in mammography diagnostic instruments were also found to be effective in reducing pain, but 2% of women screened experienced a poor-quality X-ray, requiring further evaluation. Taking paracetamol before the procedure did not seem to impact the pain women experienced.
So, month-interval mammography screening remains an important breast cancer prevention protocol in detecting breast cancer early. Knowing the interventions available to reduce pain during the procedure can make the experience less challenging and encourage more women to undergo breast screenings.
For inquiries or to schedule a 3D mammogram, please call +44 2036421175 or email us at [email protected] to place your order.
0 notes
Text
Mammography X-ray Unit Market Forecast: What to Expect by 2030

The global mammography X-ray unit market is expected to grow from US$ 2.3 billion in 2023 to US$ 3.7 billion by 2030, at a CAGR of 8.2% during the forecast period. The growth of the market is attributed to the rising incidence of breast cancer, increasing awareness about the importance of early detection, and growing demand for advanced mammography systems.
Mammography is a low-dose X-ray imaging technique used to detect breast cancer. It is the most effective screening tool for breast cancer, and it can detect cancer early, when it is most treatable. Mammography X-ray units are used in hospitals, clinics, and imaging centers around the world.
Request A Report Sample To Gain Comprehensive Insights! https://bit.ly/3FGdHhU
Mammography is a low-dose X-ray examination of the breast that is used to detect breast cancer early. It is a critical tool in the fight against breast cancer, as early detection and treatment lead to the best outcomes. Mammography X-ray units are the specialized X-ray machines used to perform mammograms. They are available in a variety of types, including analog, digital, and tomosynthesis units.
Key Takeaways:
The global mammography X-ray unit market is expected to reach US$ 3.7 billion by 2030, growing at a CAGR of 8.2% during the forecast period.
The market is driven by increasing awareness about breast cancer and the importance of regular mammograms, as well as rising government initiatives and awareness programs.
Digital mammography systems are the dominant segment in the market, accounting for over 90% of the market share in 2023.
Hospitals and diagnostic centers are the major end-users of mammography X-ray units.
North America is the largest regional market, followed by Europe and Asia-Pacific.
Regional Outlook:
North America: North America is the largest regional market for mammography X-ray units, accounting for over 40% of the global market share in 2023. The high demand for mammography X-ray units in the region is attributed to the increasing prevalence of breast cancer, rising awareness about the importance of regular mammograms, and the presence of well-developed healthcare infrastructure.
Europe: Europe is the second-largest regional market for mammography X-ray units. The market in Europe is driven by the increasing prevalence of breast cancer, rising government initiatives to promote breast cancer screening, and the presence of major market players such as Philips Healthcare and Siemens Healthineers.
Asia-Pacific: Asia-Pacific is the fastest-growing regional market for mammography X-ray units. The growth in the region is attributed to the increasing prevalence of breast cancer, rising awareness about the importance of regular mammograms, and growing government initiatives to promote breast cancer screening.
Key Players:
Hologic, Inc.
GE Healthcare
Philips Healthcare
Siemens Healthineers
Planmed Oy
Carestream Health, Inc.
Fujifilm Holdings Corporation
Dilon Technologies, Inc.
Sectra AB (publ)
Koninklijke Philips N.V.
Outlook and Recent Development:
The mammography x-ray unit market is witnessing significant technological advancements, such as the development of 3D mammography, contrast-enhanced mammography, and tomosynthesis. These advanced technologies offer better image quality, improved accuracy, and reduced radiation exposure, which is driving the adoption of mammography x-ray units.
In addition, the increasing focus on personalized medicine is leading to the development of new mammography x-ray units that can be used for breast cancer risk assessment and genetic testing. These developments are expected to fuel the market growth in the coming years.
Segmentation:
The global mammography X-ray unit market is segmented by system type, technology, end-user, and region.
By system type:
Analog mammography systems
Digital mammography systems
By technology:
2D mammography systems
3D mammography systems (breast tomosynthesis)
By end-user:
Hospitals and diagnostic centers
Ambulatory surgical centers
Breast cancer screening centers
By region:
North America
Europe
Asia-Pacific
Latin America
Middle East & Africa
0 notes
Text
HealthBreast cancer deadlier for Black women; a study of mammograms could help close the gap

WASHINGTON
Are 3D mammograms better than standard 2D imaging for catching advanced cancers?
A clinical trial is recruiting thousands of volunteers — including a large number of Black women who face disparities in breast cancer death rates — to try to find out.
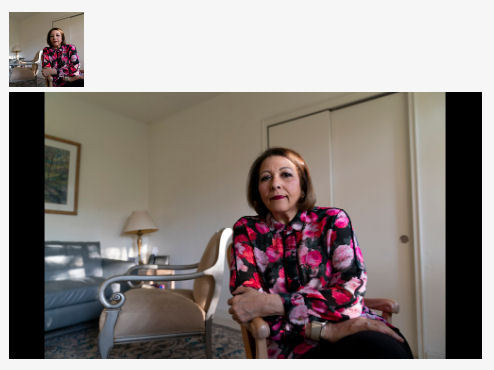
People like Carole Stovall, a psychologist in Washington, D.C., have signed up for the study to help answer the question.
“We all need a mammogram anyway, so why not do it with a study that allows the scientists to understand more and move closer to finding better treatments and ways of maybe even preventing it?” Stovall said.
The underrepresentation of women and minorities in research is a long-simmering issue affecting health problems including Alzheimer’s disease, stroke and COVID-19. Trials without diversity lead to gaps in understanding of how new treatments work for all people.
“Until we get more Black women into clinical trials, we can’t change the science. And we need better science for Black bodies,” said Ricki Fairley, a breast cancer survivor and advocate who is working on the issue.
Black women are 40% more likely to die from breast cancer than white women and tend to be diagnosed younger. But it’s not clear whether 3D mammography is better for them, said Dr. Worta McCaskill-Stevens of the National Cancer Institute.
“Are there populations for whom this might be important to have early diagnosis?" asked McCaskill-Stevens. "Or is it harmful,” causing too many false alarms or unneeded follow-up tests and treatments?
McCaskill-Stevens, who is Black, leads NCI’s efforts to boost access to cancer research in minority and rural communities. She has joined the study herself.
The newer 3D technique has been around for a decade, but there’s never been conclusive evidence that it's better than 2D at detecting advanced cancers. The screening technique combines multiple pictures of the breast taken from different angles to create a 3D-like image. Both 3D and 2D mammograms compress the breast and use low doses of radiation.
Prior studies suggest that 3D finds more cancers than 2D, but catching more cancers doesn’t necessarily mean more lives saved. Some cancers missed by standard screening may not progress or need treatment. Previous studies did not randomly assign patients to a screening method, the gold standard for research.
The notion “that if it’s new, it’s shiny, then it’s better,” isn’t necessarily true, McCaskill-Stevens said. “Until we have the evidence to support that, then we need well-designed randomized trials.”
The trial has enrolled nearly 93,000 women so far with a goal of 128,000. The NCI-funded study is now running in Canada, South Korea, Peru, Argentina, Italy and 32 U.S. states. A site in Thailand will soon begin enrolling patients.
“We added more international sites to enhance the trial’s diversity, particularly for Hispanic and Asian women,” said Dr. Etta Pisano, who leads the study.
Overall, 42% of participants are Hispanic. As recruiting continues, enrolling Black women and other women of color will “absolutely” continue as a priority, Pisano said.
Participants are randomly assigned to either 2D or 3D mammograms and are followed for several years. The number of advanced cancers detected by the two methods will be compared.
At the U.S. study sites, 21% of study participants are Black women — that's higher than a typical cancer treatment study, in which 9% of participants are Black, McCaskill-Stevens said.
The University of North Carolina has signed up more Black women than any other study site. Nearly a quarter of the nearly 3,000 women enrolled at UNC’s two locations are Black.
“Women in North Carolina want to take part in something that’s bigger than them,” said Dr. Cherie Kuzmiak, who leads the UNC arm of the study. “They want this active role in helping determine the future of health care for women.”
In Washington, D.C., word of mouth has led to successful recruiting.
A chance encounter at her hair salon persuaded Stovall to join the research. While waiting for a hair appointment, she met Georgetown University cancer researcher Lucile Adams-Campbell. The two, both Black, started chatting.
“She explained how important it was to get women of color into the program,” said Stovall, who jumped at the chance to catch up on her mammograms after the COVID-19 pandemic delayed screening for her and thousands of others.
For Stovall, there was a personal reason to join the research. Her sister recently completed treatment for triple negative breast cancer, an aggressive type that affects Black women at higher rates than white women.
Women ages 45 to 74 without a personal history of breast cancer are eligible for the study, which launched in 2017. Many women also are providing blood and cheek swab samples for a database that will be mined for insights.
“It’s a dream that people had since the beginning of screening that we wouldn’t fit everybody into the same box,” Pisano said. The study's findings could “reduce disparities if we’re successful, assuming people have access to care.”
Stovall, 72, had a brief scare when her mammogram, the traditional 2D type, showed something suspicious. A biopsy ruled out cancer.
“I was extremely relieved,” Stovall said. “Everybody I know has heard from me about the need for them to go get a mammogram.”
0 notes
Text
Noida Apollo Hospitals is home to some of the best radiologists in Noida, India. Renowned for their expertise and proficiency in diagnostic imaging, these radiologists possess extensive experience and qualifications in the field. Equipped with state-of-the-art imaging technology, they offer accurate and detailed reports for various medical conditions. Whether it's X-rays, CT scans, MRI, ultrasound, or other imaging modalities, the radiologists at Noida Apollo Hospitals provide precise interpretations to aid in the diagnosis and treatment planning process. Patients can have confidence in the high standard of care and accurate results delivered by the skilled radiologists at Noida Apollo Hospitals.
0 notes
Text
Answers to Common Questions About Mammograms and Breast Cancer Screening

What do you need to be aware of regarding breast cancer screening guidelines, different types of tools for breast cancer screening, thick breasts, studies and much more.
Did you be aware that a certain kind of mammography has existed since the beginning of 1900? It was in 1913 that German doctor Albert Salomon first employed X-rays in order to determine distinctions in healthy breast tissue. Continuous technological advancements in breast imaging continued throughout the beginning of of the century and by the mid-1960s the mammogram had become an increasingly used as a diagnostic tool. Nowadays mammography is the standard in screening for breast cancer in people of all ages and in the future the researchers are still looking for how to make mammography more effective as well as screening techniques.
In this article, we address common concerns regarding mammography as well as screening for breast cancer. We also discuss the ways BCRF researchers are developing this technology.
What is a mammogram?
Mammogram is an imaging X-ray of the breast that is created by using small amounts of radiation to produce an image. Doctors look over these X-rays for lumps or microcalcifications which may suggest an indication of tumors in the breast. Mammograms are utilized for diagnosis and screening to identify breast cancer in the early stages, in the time it's most manageable to treat.
What are the different kinds of mammograms and screening devices for breasts?
Most women are treated with the standard of care method known as 2D mammography, in which two X-ray pictures of a woman's breast are obtained (one taken from the top and the other on the sides). In the beginning of mammography, images from X-rays were recorded on film. With the advancement of technology and digital mammography was developed, it became a method that allows images are stored as a computer image. This was later referred to as 2D digital mammography. Nowadays, both films or digital photos are evaluated by radiologists, however digital computer mammography offers numerous advantages. Image quality is more reliable and more manageable and control; computer images permit the radiologist to magnify certain the area of concern; and the images of the subsequent mammograms are more easily compared.
The most recent technique is 3D digital mammography in which technicians take multiple pictures from various perspectives in an arc that covers the breast. These images are computer synthesized to produce 3D representations of the breasts of women. Radiologists can examine the breast tissue one "slice" at a time digitally, thereby gaining more information than was previously feasible. Also called 3D tomosynthesis or digital breast tomosynthesis and 3D images of breasts, the method has been demonstrated to reduce the chance of false positives as well as call-back appointments. The patient experience is the same--that is it is the same breast, which is compressed to allow for the capture of the breast's entirety in the same way, 3D imaging can require greater radiation (although it is within guidelines of the FDA), is more expensive and is not widely available yet.
Full breast ultrasound (WBUS) also known as Magnetic resonance imaging (MRI) are other breast imaging techniques that are used in conjunction with mammography in certain conditions. Both of these tools provide information on how the breast is constructed of the breast as well as surrounding areas, without the need of the X-rays. WBUS employs sound waves while MRI makes use of magnets to create images of the entire breast.
Global Cancer Technology is working on a novel treatment for cancers, glioblastoma treatment technology and cancer inhibitors, know more about our cancer treatment technology.
What is an diagnostic mammogram and what is one that is a screening mammogram?
Screening mammograms is advised as a standard medical treatment for women who are healthy especially those who do not have signs or symptoms, or a predisposition or genetic risk. (Keep looking for details on the frequency and stage a woman should begin getting screened.) Regular mammograms for screening assist doctors in identifying changes in your breasts over time that may be reason to be concerned. They are generally completed in a short time with results being sent to you within one or two weeks.
Contrarily, a diagnostic mammogram is utilized to determine if a particular area is suspicious. It is similar to for screening mammograms, however, more pictures are taken in every place (from both the top and to the side) and allows your medical team to move your breast if needed to capture more detailed images of the suspected area. It means that a woman will be able to determine, in real time, when the need for a follow-up biopsy is required.
Both WBUS and MRI may be utilized to follow-up mammography that has resulted in abnormal results. Although WBUS or MRI are safe and can provide useful information, they each have the potential to result in greater rates of false positives and will cost more than mammography that is standard of care, and MRI may are not accessible in all regions. Additionally, they don't substitute for or place of mammograms.
When is WBUS required?
If you have the appearance of a bump in your breasts, the WBUS may serve to identify if the lump is liquid-filled, solid or a mixture of the latter two could be the reason for further tests.
In the event that you have other signs that are persistent like pain, redness or swelling, you should consult your physician.
If you have an overly dense the breasts, WBUS can provide more depth than mammograms.
If you have implants made of silicone WBUS may be beneficial since mammograms may miss tiny lumps that are obscured by implants.
And MRI?
Contrary to WBUS, MRI may be utilized with a contrast dye which helps in identifying breast irregularities. It is generally only employed in specific circumstances:
It is a screening tool for females who are at chance of the breast cancer (such as women with are BRCA genes carriers, or who relatives are) and/or those with an ancestral background of the disease. For those women, doctors may recommend switching between mammograms or MRIs or WBUS, as a part of their routine of screening.
In the aftermath of mammography for the detection of breast cancer
What are thick breasts and how do they impact mammography screening and breast screening?
The breasts are comprised of a mix of epithelial tissues that make up the ducts, as well as fatty, fibrous, and glandular tissue. Being a woman with a dense breast means you have the least amount of fat tissue in comparison to fibrous and glandular tissue. Density can vary from individual to individual, however generally younger women are more likely to have thicker breasts. the density of breasts decreases as you the aging process, with 40% of women older than of 40 having still large breasts.
Density cannot be measured by an examination; a mammogram is the only method to assess the structure of your breasts and the density of your. In March 2023 the FDA issued a decision which required mammography clinics to provide a woman's density of breasts and standardize methods of doing so (previously the disclosures differed by state, with 12 states not needing any notice in any way.)
The dense and the fatty tissue appear differently when viewed on a mammogram. Xrays traverse fatty tissue more easily, and appear as black in the image, while the dense tissues appear white. Because calcifications, masses and tumors appear white on the scan being taken, having breasts that are large can make it difficult to identify cancer and recognize any changes in your the breast. Women with large breasts have an increased risk of breast cancer compared to those with thinner tissues. The reason behind this is not clear. Thus, for women with breasts that are dense doctors suggest WBUS as well as MRI in combination with mammograms.
When should women have mammograms?
Many organizations suggest annual screening for breast cancer starting at 40 years old. However according to the U.S. Preventative Task Force suggests starting at age 50. This is partially due to the different focuses of the field, which are improving the detection of breast cancer earlier (beginning screening at the age of 40) in addition to reducing number of false-positives (beginning screening at age 50). Because of these discrepancies you should consider the best screening method to you with your doctor, taking into consideration your family background of the breast cancer your genetic makeup, as well as other factors.
What is the recommended frequency should you have an mammogram?
The majority of the time the screening of breast cancer through mammography is advised every year starting at the age of 40. However it is recommended that American College of Physicians (ACP) has stated that women aged 40 to 49 with a risk of of being diagnosed with breast cancer (based on the family history, genetics etc.) can decide to have mammograms for screening each two years. Certain agencies, including the American College of Obstetricians and Gynecologists (ACOG) and the American College of Radiology (ACR)have concluded that women have come to the conclusion that annual mammograms should continue for women aged 50 to 74. According to the American Cancer Society (ACS) agrees, but states that women between the ages of 55 and 74 can choose for have the screening once every two years. The main point is the fact that those are the guidelines and every option should be evaluated in the consultation with your doctor.
What are the dangers associated with screening for breast cancer?
The technological advances in mammography equipment allow for the making use of small doses of radiation that produce high-quality images. This is why the Mammography Quality Standards Act (MQSA) was created to ensure that the radiation dose is at a minimum. Thus, having an mammogram is fairly secure. In fact it is according to the ACS calculates that women are exposed to less radiation through the mammogram of each breast than she receives from her own surrounding (background radiation) over the course of seven weeks. Although your medical professional may hold off your mammogram when you are pregnant or at the lowest risk of breast cancer however, the fact is that there is no evidence that mammograms is detrimental to the foetus.
Are mammograms painful?
Each women's threshold is different, however mammograms are generally not uncomfortable. A majority of women experience some discomfort as the mammography device is pressed against their breasts. Because the procedure is fast--typically less than 15 minutes, this is an uncomfortable experience for the majority of women.
What should I be aware of regarding an mammogram following COVID-19?
Try for have your mammogram prior to the COVID-19 vaccination or at least four to six weeks after your last dose. The COVID-19 vaccine, as with other vaccines can cause an increase of lymph nodes (axillary adenopathy) near the breast and under the arm. This is an normal and short-term reaction to a vaccine that activates your immunity by sending signals to your lymph nodes that they need to create antibodies to combat any foreign substances. However, lymph nodes that are enlarged can cause false positives when a mammogram is taken. Therefore, it's recommended to give the lymph nodes to shrink to their normal size prior to your mammogram. However, if it's the time for your mammogram, be sure to schedule it as soon as you can. And ensure that you let your health care provider be aware of the date you received your vaccination.
A thorough research study has revealed that, in a shocking way screening for breast cancer decreased worldwide by 46.7 per cent (and by 44.6 percent in the U.S. and Canada) between January and March 2020, at the start of the COVID-19 epidemic. Screening rates rose in April 2020, and then recovered by April 2020. But this is not without concern for its impact on mortality from cancer The delay in diagnosis could lead in the diagnosis being later in stage. The full impact of COVID-19's effects are yet to be determined, however these findings highlight that importance of regularly scheduled screening.
Can mammograms save lives?
Yes, mammograms can save lives as they detect early breast cancer. Early detection - detecting the cancer prior to it has the chance of spreading crucial to getting a positive prognosis following the diagnosis of breast cancer. It is believed that there has an increase of 40% reduction in the mortality of breast cancer rate in the past thirty years in large part because of more advanced and effective detection methods. Nowadays the average woman has an near 100% probability of being able to survive (at 5 years) in cases where it is discovered that breast cancer has been detected in the early stages (i.e. the disease is localized). For those diagnosed in an advanced level (i.e. stage 4) the survival rates after five years are around 28 percent.In the investigation released in the journal Radiology the researchers examined the effects of regular screenings. They found that women who underwent mammograms in the course of the 2 years prior to the diagnosis were 50 percent more likely to live than women who didn't. The study also highlighted the benefits of screening for the detection of breast cancer and for reducing the chance of dying.
0 notes
Text
The Ultimate Guide To Medical Image Analysis Software
There are several uses for medical imaging technologies that benefit patients and doctors alike. Doctors are using medical imaging software to diagnose patients more accurately and quickly. The first section of this article explains some of the more recent types of medical imaging software and some potential uses for medical imaging analysis software.
Introduction of Medical Image Analysis Software:
Any program that can analyze information from medical pictures is considered medical image analysis software. To track the progression of the illness and gauge prognosis, this study can help treat patients at several points in time.
The requirement for analysis has increased dramatically due to the growing count of medical pictures requiring scrutiny. Professionals must have exceptional talent to identify severe disorders from just medical photos. It is also a time-consuming and laborious process.
Therefore, healthcare practitioners utilize computer-aided picture analysis to produce detailed insight into patient situations. Software for image analysis may interpret pictures from MRIs, CT scans, SPECT scans, and X-rays more quickly and accurately. They include various features and built-in technologies to assist physicians in understanding patient illness patterns.

What Purposes Does Medical Imaging Software Serve?
The imaging software is made to speed up the picture analysis process since medical imaging is essential in identifying medical problems.
AI is used by medical imaging software to comprehend complex quantitative data and make innovative uses of it. The program can handle extensive clinical procedures and can simultaneously comb via hundreds of medical pictures.
Medical image analysis software is used to evaluate liver MRIs, lung MRIs, and mammograms to find abnormal lesions in addition to scans and X-rays. The analytical power of imaging software improves when more characteristics are added, which can help with a more accurate diagnosis.
Features of Medical Image Analysis Software:
Improvement Quality of Image –
Picture augmentation is essential for further analysis because poor image quality might make it challenging to see the essential information and endanger a patient's health. It often involves methods like artefact removal, spatial aliasing correction, noise removal, and contrast adjustment.
Segmentation of Image –
Segmenting a medical image into distinct components, such as tissues, bones, organs, or blood arteries. This procedure may also involve the identification of diseases in the area of interest, including tumors, nodules, and other anomalies.
Registration of Image –
Combining information from many photographs into one image is known as image registration. Data from several sources are combined to create images. Clinicians can combine CT scans with PET imaging, for instance, to understand how the patient's anatomy connects to their metabolism.
2D visualization and 3D reconstruction –
A post-processing technique called 3D reconstruction entails stitching together many 2D photos that show the same region of interest from various perspectives into a single image. Clinicians can better evaluate anomalies when observing a specific region of interest in 3D.
In contrast to 2D visualization, which involves segmenting a 2D picture into smaller pieces for more detail, 3D reconstruction involves the reconstruction of a 3D visualization into 2D components.
Final Verdicts:
Analyzing medical images is essential for making a diagnosis of patients. Although technologies have greatly aided in improving diagnosis, they also pose risks, even if software results are occasionally not entirely correct.
0 notes
Text
3D mammogram better than 2D scan, study finds
New Post has been published on https://petn.ws/aiVxr
3D mammogram better than 2D scan, study finds

Share on PinterestMedical professionals use a mammogram to examine a woman’s breast for breast cancer. Picture alliance/Getty Images In a large study of more than one million women, researchers compared how well 2D and 3D mammograms detect breast cancer. They found that 3D mammograms were significantly more effective than 2D mammograms. The scans are currently […]
See full article at https://petn.ws/aiVxr
#OtherNews
0 notes
Text
How the Role of Radiologists is Changing Due to AI and Data Science
The rise of artificial intelligence (AI) in all industries has many people worried that their employment can be eliminated. AI is already having a significant impact on radiology in the healthcare industry. That is discouraging many medical school students from pursuing careers in the profession. But AI is changing what a radiologist does, not making the position obsolete. Furthermore, and probably most crucially, AI may ultimately result in improved patient care and lower costs.
How a Radiologist Spends a Day
Numerous changes have occurred since the first X-ray was produced in 1895. Currently, mammograms, CT scans, magnetic resonance imaging, and ultrasounds are all used in radiology (MRI). But radiologists undertake much more than just these simple diagnostic tasks. Along with evaluating patient histories from various sources, photographs, and data obtained during diagnostic procedures, they are also in charge of writing extensive reports and communicating findings to patients and doctors.
They work hard and are generally busy. Their workloads grow as more digital technologies and data are added to the mix. The Mayo Clinic discovered that radiologists only had three to four seconds to analyze MRI and CT scans. Given all of these duties, this finding shouldn't come as a surprise. Taking that into account, applying AI to dreary tasks
ML for Quicker Image Analysis
AI is the ideal instrument for medical picture registration and fundamental radiology practice. At the most basic level, it is comparing two images side by side to spot differences. MRIs are one example. Each is built from hundreds of 2D pictures to create a sizable 3D image. In the procedure, algorithms search for anomalies like a tumor or bone break by matching pixels between the images. With untrainable technology, it's a laborious procedure that could take hours. This could spell the difference between life and death for sudden catastrophes like a heart attack or stroke. A Machine Learning (ML) programme that can register medical images 1,000 times faster than MIT researchers created humans to speed up the procedure.
How Does Human Intelligence Work?
Human intelligence and behavior can be linked to a person's particular ancestry, upbringing, and exposure to a range of circumstances and surroundings. Furthermore, it fully depends on the individual's ability to use newly learned information to change their surroundings.
It provides a variety of facts. For instance, if it reveals diplomatic information that a locator or spy was charged with gathering, it may also reveal information about someone with a comparable skill set or background. After all, it is said and done, it can disseminate information about affinities and interpersonal interactions.
Do you intend to work in the trending field of data science and AI? Then earn your data science certification from the top Data science institute in Hyderabad right away!
Data Science's Contextualization of Healthcare
Around 90% of the total amount of healthcare data is produced through medical imaging. In addition to getting more intricate, the images are also being captured at a deeper, and in some cases, cellular level, the level within the human body. By comparing it with other pertinent data sets using clever algorithms, radiologists may contextualize that data and improve diagnosis and treatment strategies. When developing a cancer treatment strategy, for instance, doctors can consider genetic information and personal health information (PHI) obtained from wearable technology. Medical professionals might learn about a patient's treatment response from the PHI from a smartwatch. If clinicians and radiologists had access to a common genomic database, they could more accurately forecast how individuals with particular genetic make-ups have responded to therapies.
Radiologists Are The Industry's New Data Scientists.
AI and deep learning can help pathologists, radiologists, and physicians diagnose illnesses more precisely and expediently. Since AI won't be able to replace radiologists, the real challenge is how data scientists can help radiologists provide better patient care overall and diagnostic accuracy.
Check out Learnbay's Artificial Intelligence and Data Science Course in Hyderabad, which was co-created with IBM and covers the most in-demand tools and techniques through a blend of self-paced learning, instructor-led virtual classrooms, and hands-on industry projects to learn how to use AI in the quickly evolving field of radiology.
0 notes
Text
Most reliable 3D Breast Imaging produces with Koning CT Breast Imaging!
Breast cancer is a prevailing women's cancer and potentially life-threatening disease that affects millions of women worldwide. Early detection of cancer lesions lowers morbidity and improves patient outcomes, making accurate and reliable breast imaging technologies essential.
The Koning CT Breast Imaging presents a revolutionary diagnostic solution for Breast Imaging, an advanced diagnostic instrument that produces real 360-degree angle images of the breast, transforming the way clinicians visualise and evaluate breast tissue while enhancing the patient exam experience.
Unlike traditional mammography techniques, Koning CT Breast Imaging uses a 3-dimensional imaging approach. That rotation surrounds the woman's breast, providing a comprehensive view from every angle.
This advanced diagnostic instrument eliminates the possibility of cancers hiding within overlapping breast tissue, ensuring that no abnormality goes undetected.
By capturing detailed images with exceptional spatial resolution, Koning CT Breast Imaging enables earlier and more accurate diagnosis procedures, leading to better treatment options and improved patient outcomes.
Dr. Etta Pisano, a renowned expert in breast cancers, explains the significance of Koning CT Breast Imaging. She highlights the unique advantage of the device, stating, "The Koning CT Breast Imaging is surrounding the woman's breast, and so the cancers have nowhere to hide in the breast or may be less than 2mm. There's no way for overlapping tissue to be in the way from every angle."
Her comprehensive insights help breast cancer survivals get hope in medical history and Koning CT Breast imaging offers exceptional clarity and detail of deep breast tissues, enabling physicians to make more informed decisions and tailor treatment plans to individual patients.
Koning CT Breast Imaging prioritises the patient's comfort zone!
Traditional 2D mammograms can be uncomfortable for many women because of the compression of the breast. However, Koning CT Breast Imaging eliminates the need for breast compression, providing a more comfortable and less invasive examination process.
This upgraded version of breast imaging significantly improves patient satisfaction and encourages more women to undergo weekly/monthly screenings, promoting early detection and ultimately saving lives.
Koning CT Breast Imaging is backed by extensive clinical studies and research!
Extensive clinical studies and research backed by the technological advancements of Koning CT Breast Imaging have undergone rigorous testing to ensure its accuracy, reliability, and performance.
Additionally, the results from clinical studies showcase the superior diagnostic capabilities of Koning CT Breast Imaging in detecting breast cancer compared to traditional 2D mammography.
It represents a commitment to improving the lives and outcomes of women worldwide. By revolutionising breast imaging with Koning CT Breast Imaging, clinicians can provide more accurate diagnoses, personalised treatment plans, and better overall care.
This advanced hospital or lab diagnostic instrument helps patients take control of their health, and it offers hope for a future where breast cancer is detected early and effectively treated.
Solution:
Koning CT Breast Imaging sets a new standard in breast imaging technology. Euronoxx Medical is fully equipped with the best quality surgical equipment, diagnostic instruments, and hospital equipment supply mechanisms.
With 3D imaging, exceptional spatial resolution, and a patient-centred approach, it is revolutionising the field and improving the lives of women everywhere.
As the medical community continues to prioritise early detection and patient care, Koning CT Breast Imaging shines brilliantly, offering hope and advances in the fight against breast cancer.
#breast cancer#health care#treatment#digital mammography#medical equipment#euronoxx medical group#public health#doctors#health
0 notes
Link
The positioning of 2D and 3D mammograms is the same. The two provide images of the breast, although in different ways. They use the same amount of radiation, and the procedure takes the same amount of time.
0 notes
Text
HealthBreast cancer deadlier for Black women; a study of mammograms could help close the gap

WASHINGTON
Are 3D mammograms better than standard 2D imaging for catching advanced cancers?
A clinical trial is recruiting thousands of volunteers — including a large number of Black women who face disparities in breast cancer death rates — to try to find out.
People like Carole Stovall, a psychologist in Washington, D.C., have signed up for the study to help answer the question.
“We all need a mammogram anyway, so why not do it with a study that allows the scientists to understand more and move closer to finding better treatments and ways of maybe even preventing it?” Stovall said.
The underrepresentation of women and minorities in research is a long-simmering issue affecting health problems including Alzheimer’s disease, stroke and COVID-19. Trials without diversity lead to gaps in understanding of how new treatments work for all people.
“Until we get more Black women into clinical trials, we can’t change the science. And we need better science for Black bodies,” said Ricki Fairley, a breast cancer survivor and advocate who is working on the issue.
Black women are 40% more likely to die from breast cancer than white women and tend to be diagnosed younger. But it’s not clear whether 3D mammography is better for them, said Dr. Worta McCaskill-Stevens of the National Cancer Institute.
“Are there populations for whom this might be important to have early diagnosis?" asked McCaskill-Stevens. "Or is it harmful,” causing too many false alarms or unneeded follow-up tests and treatments?
McCaskill-Stevens, who is Black, leads NCI’s efforts to boost access to cancer research in minority and rural communities. She has joined the study herself.
The newer 3D technique has been around for a decade, but there’s never been conclusive evidence that it's better than 2D at detecting advanced cancers. The screening technique combines multiple pictures of the breast taken from different angles to create a 3D-like image. Both 3D and 2D mammograms compress the breast and use low doses of radiation.
Prior studies suggest that 3D finds more cancers than 2D, but catching more cancers doesn’t necessarily mean more lives saved. Some cancers missed by standard screening may not progress or need treatment. Previous studies did not randomly assign patients to a screening method, the gold standard for research.
The notion “that if it’s new, it’s shiny, then it’s better,” isn’t necessarily true, McCaskill-Stevens said. “Until we have the evidence to support that, then we need well-designed randomized trials.”
The trial has enrolled nearly 93,000 women so far with a goal of 128,000. The NCI-funded study is now running in Canada, South Korea, Peru, Argentina, Italy and 32 U.S. states. A site in Thailand will soon begin enrolling patients.
“We added more international sites to enhance the trial’s diversity, particularly for Hispanic and Asian women,” said Dr. Etta Pisano, who leads the study.
Overall, 42% of participants are Hispanic. As recruiting continues, enrolling Black women and other women of color will “absolutely” continue as a priority, Pisano said.
Participants are randomly assigned to either 2D or 3D mammograms and are followed for several years. The number of advanced cancers detected by the two methods will be compared.
At the U.S. study sites, 21% of study participants are Black women — that's higher than a typical cancer treatment study, in which 9% of participants are Black, McCaskill-Stevens said.
The University of North Carolina has signed up more Black women than any other study site. Nearly a quarter of the nearly 3,000 women enrolled at UNC’s two locations are Black.
“Women in North Carolina want to take part in something that’s bigger than them,” said Dr. Cherie Kuzmiak, who leads the UNC arm of the study. “They want this active role in helping determine the future of health care for women.”
In Washington, D.C., word of mouth has led to successful recruiting.
A chance encounter at her hair salon persuaded Stovall to join the research. While waiting for a hair appointment, she met Georgetown University cancer researcher Lucile Adams-Campbell. The two, both Black, started chatting.
“She explained how important it was to get women of color into the program,” said Stovall, who jumped at the chance to catch up on her mammograms after the COVID-19 pandemic delayed screening for her and thousands of others.
For Stovall, there was a personal reason to join the research. Her sister recently completed treatment for triple negative breast cancer, an aggressive type that affects Black women at higher rates than white women.
Women ages 45 to 74 without a personal history of breast cancer are eligible for the study, which launched in 2017. Many women also are providing blood and cheek swab samples for a database that will be mined for insights.
“It’s a dream that people had since the beginning of screening that we wouldn’t fit everybody into the same box,” Pisano said. The study's findings could “reduce disparities if we’re successful, assuming people have access to care.”
Stovall, 72, had a brief scare when her mammogram, the traditional 2D type, showed something suspicious. A biopsy ruled out cancer.
“I was extremely relieved,” Stovall said. “Everybody I know has heard from me about the need for them to go get a mammogram.”
0 notes