#Axitinib 5 mg
Text
Kidney Cancer Treatment:- Jastinihb 5 Mg Capsule
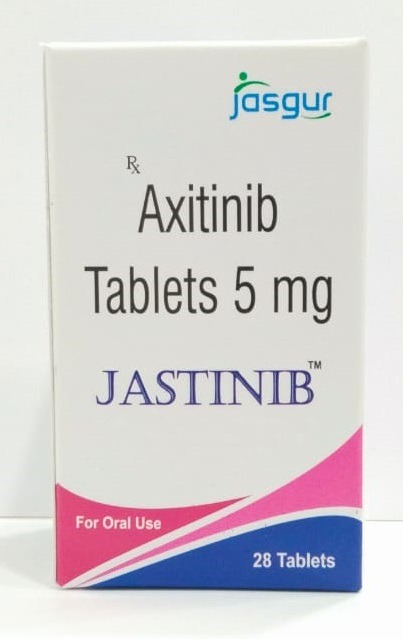
Empower your cancer journey with Jastinib 5 mg capsule from Jasgur Life Sciences. Designed to inhibit VEGF receptors, this innovative medication holds promise for patients battling advanced renal cell carcinoma. With Jastinib, embrace a brighter future and reclaim control over your health.
#cancer medicines#cancer cure#kidney cancer treatment#jasgur life sciences#Cancer drugs#Axitinib 5 mg#Jastinib 5 mg capsule#Cancer tablets#Anti kidney cancer drugs#Jastinib 5 mg#Jastinib#Axitinib 5 mg capsule
0 notes
Text
Inlyta (axitinib) is a prescription drug used to treat advanced kidney cancer in adults. The drug comes as an oral tablet that’s usually taken twice per day.
Specifically, Inlyta is prescribed:
as the first treatment for advanced renal cell carcinoma (RCC). In this instance, Inlyta is used in combination with either avelumab (Bavencio) or pembrolizumab (Keytruda).
by itself to treat advanced RCC when another type of treatment hasn’t worked
The active ingredient in Inlyta is axitinib. (An active ingredient is what makes a drug work.) Inlyta belongs to a group of drugs called kinase inhibitors.
This article describes the dosages of Inlyta, as well as its strengths and how to take it. To learn more about Inlyta, see this in-depth article.
* Advanced means that it’s spread to other areas of the body or can’t be surgically removed.
What is Inlyta’s dosage?
This section describes the usual dosages of Inlyta.
What is Inlyta’s form?
Inlyta comes as an oral tablet.
What strengths does Inlyta have?
Inlyta comes in two strengths: 1 milligram (mg) and 5 mg.
What are the usual dosages of Inlyta?
The information below describes Inlyta dosages that are commonly used or recommended. But be sure to take the dosage your doctor prescribes. They’ll determine the best dosage to fit your needs and may adjust it until they reach the right amount for you.
Dosage for RCC
The typical starting dosage of Inlyta for adults with RCC is 5 mg taken twice per day (every 12 hours). Depending on your particular situation, your doctor may prescribe Inlyta alone or in combination with either avelumab (Bavencio) or pembrolizumab (Keytruda).
If you’re taking Inlyta alone and don’t have bothersome side effects after about 2 weeks, your doctor may increase your dosage from 5 mg to 7 mg twice daily.
If you still aren’t experiencing serious side effects, they may further increase your dosage to 10 mg twice daily. If you have high blood pressure or take medication for high blood pressure, your doctor may increase your dose more slowly.
The dosage of avelumab, when used in combination with Inlyta, is 800 mg. Avelumab is given as a 60-minute intravenous (IV) infusion (an injection into a vein given over time) by a healthcare professional once every 2 weeks.
With this combination therapy, your doctor may increase your dosage of Inlyta after 2 weeks (or longer) based on your response to treatment.
The dosage of pembrolizumab when used in combination with Inlyta is 200 mg. This is given as an IV infusion over the course of 30 minutes by a healthcare professional. You’ll either receive 200 mg once every 3 weeks or 400 mg once every 6 weeks.
With this combination therapy, your doctor may increase your dosage of Inlyta after 6 weeks (or longer) based on your response to treatment.
Your doctor will monitor how you respond to treatment with Inlyta and adjust your dosage accordingly. If you experience certain side effects, they may lower your dose, pause, or stop your treatment.
For more information about your dosage of Inlyta, talk with your doctor.
Is Inlyta used long-term?
Yes, Inlyta is usually a long-term treatment. If you and your doctor determine that it’s safe and effective for your condition, you’ll likely take it long-term.
Dosage adjustments
In certain cases, you may need dosage adjustments for Inlyta.
If you have moderate liver problems, your doctor will adjust your dosage of Inlyta. With liver problems, it may take longer for the drug to leave your body. This can increase your risk of side effects. Typically, your doctor will reduce your starting dosage by half of the usual dosage for RCC. They may adjust your dosage further (up or down) based on how you respond to treatment.
Your doctor may need to reduce your Inlyta dose by half if you’re taking certain other medications called CYP3A4/5 inhibitors. This type of drug is known to interact with Inlyta and can increase its effects as well as your risk of side effects. Examples of CYP3A4/5 inhibitor drugs include certain:
antifungals, such as ketoconazole
antibiotics, such as clarithromycin
antivirals, such as atazanavir
Your doctor may adjust your dosage of Inlyta based on your response to Inlyta in combination with other drugs.
Tell your doctor if you have liver problems and about all the other medications you take. They’ll determine whether you need Inlyta dosage adjustments.
What factors can affect my dosage?
The dosage of Inlyta you’re prescribed may depend on several factors. These include:
the severity of your RCC
How do you respond to treatment with Inlyta?
other medications you take (see the “Dosage adjustments” section above)
other conditions you may have (see the “Dosage adjustments” section above)
How is Inlyta taken?
Inlyta comes as an oral tablet you take with a glass of water approximately every 12 hours. You can take it with or without food. Do not cut, crush, or chew Inlyta tablets. Swallow them whole. If you have trouble swallowing tablets, see this article for tips on how to take this form of medication.
For information on the expiration, storage, and disposal of Inlyta, talk with your doctor or pharmacist.
Accessible drug containers and labels
Some pharmacies provide medication labels that:
have large print
use braille
feature a code you can scan with a smartphone to change the text to audio
Your doctor or pharmacist may be able to recommend pharmacies that offer these accessibility features if your current pharmacy doesn’t.
Let your pharmacist know if you have trouble opening medication bottles. They may have tips to help, or they may be able to supply Inlyta in an easy-open container.
What if I miss a dose?
If you miss a dose of Inlyta or vomit after taking a dose, skip that missed dose and continue with your next scheduled dose at its regular time. Do not take two doses of Inlyta at once to make up for a missed dose. If you’re not sure whether you should take a missed dose, ask your doctor or pharmacist.
If you need help remembering to take your dose of Inlyta on time, try using a medication reminder. This can include setting an alarm or downloading a reminder app on your phone.
What should be done in case of overdose?
Do not take more Inlyta than your doctor prescribes, as this can lead to harmful effects.
Symptoms of overdose
Symptoms caused by an overdose of Inlyta can include:
high blood pressure
dizziness
seizure
bleeding, which can be very serious and even cause death in rare cases
What to do in case you take too much Inlyta
Call your doctor right away if you think you’ve taken too much Inlyta. You can also call 800-222-1222 to reach America’s Poison Centers or use its online resource. But if you have severe symptoms, immediately call 911 (or your local emergency number) or go to the nearest emergency room.
Frequently asked questions
Below are answers to some commonly asked questions about Inlyta’s dosage.
Is Inlyta’s dosage similar to that of Keytruda?
No, it’s not. While Inlyta and Keytruda (pembrolizumab) are both used to treat types of RCC, the forms and dosages of these two drugs are different.
Inlyta is used in combination with Keytruda as a first-time treatment for advanced RCC. Inlyta comes as an oral tablet. Keytruda comes as a liquid solution given as an IV infusion by a healthcare professional.
For more information about dosages and dosing schedules for these two drugs, see the “Dosage for RCC” section above. Your doctor will prescribe the drug or drug combination and dosages that are right for you. Talk with them to learn more about how these two drugs compare.
How long does it take for Inlyta to start working?
Inlyta starts to work after your first dose, but because of how it works, you likely won’t feel it working in your body. Your doctor will monitor you during treatment to make sure the drug is effectively treating your condition.
If you have other questions about what to expect from your Inlyta treatment, talk with your doctor.
What should I ask my doctor?
The sections above describe the usual dosages provided by Inlyta’s manufacturer. If your doctor recommends this drug, they’ll prescribe the dosage that’s right for you. Do not change your dosage of Inlyta without their recommendation. Only take this drug exactly as prescribed.
Talk with your doctor if you have questions or concerns about your current dosage. Examples of questions you may want to ask include:
Will a lower dosage of Inlyta still work to treat my cancer?
Do I have a higher risk of side effects with a higher dosage of Inlyta?
How does the dosage of Inlyta compare with that of Nivolumab (Opdivo)?
0 notes
Link

Presentation Axinix 5 Mg
Axinix 5 Tablet Each film coated tablet contains Axitinib INN 5 mg.
Description
Mechanism of ActionAxinix 5 Mg (Axitinib) has been shown to inhibit receptor tyrosine kinases including vascular endothelial growth factor receptors (VEGFR)-1, VEGFR-2, and VEGFR-3 at therapeutic plasma concentrations. These receptors are implicated in pathologic angiogenesis, tumor growth, and cancer progression. VEGF-mediated endothelial cell proliferation and survival were inhibited by Axitinib in vitro and in mouse models. Axinix 5 Mg (Axitinib) was shown to inhibit tumor growth and phosphorylation of VEGFR-2 in tumor xenograft mouse models.
0 notes
Text
Axitinib
In this article, we will discuss Axitinib (Dosage Overview). So, let’s get started.
IndicationsAxitinib is indicated for the treatment of advanced renal cell carcinoma (RCC) after failure of one prior systemic therapy.DosageRecommended DosingThe recommended starting oral dose of axitinib is 5 mg twice daily. Administer axitinib doses approximately 12 hours apart with or without food. Axitinib…
View On WordPress
0 notes
Text
Lupine Publishers | Effect of Tyrosine Kinase Inhibitors on Renal Functions

Lupine publishers | Journal of Urology & Nephrology Studies
Abstract
Background: We aim to document if any difference exists for renal functions between metastatic and non-metastatic patients.
Methods: The study population included 12 metastatic and 15 non-metastatic patients. Metastatic renal cancer patients using the TKIs were compared to non- metastatic patients.
Results:Preoperative estimated glomerular filtration rate (e-GFR) was significantly low in metastatic patients than nonmetastatic patients (p: 0.048). A trend toward increased acute kidney injury during hospital stay in the non-metastatic group was observed, but this fell just short of statistical significance (p: 0.109). Two groups did not differ significantly in terms of postoperative e-GFR (p: 0.256). No statistically significant differences were observed in actual e- GFR between two groups (p: 0.638). No statistically significant differences were found in pre-TKIs and post-TKIs e-GFR values (p: 0.735). Proteinuria was statistically more common in metastatic patients than non-metastatic patients (p<0.001). No statistically significant difference in age, sex, follow-up period, NSAIDs use, antihypertensive and ARBs/ACEIs use were documented between the two groups.
Conclusion: Increased risk for proteinuria was documented in metastatic patients with TKIs use. However, use of the TKIs had no effect on e- GFR. No statistically significant differences were observed in actual e- GFR between two groups.
keywords: Hypertension, Glomerular Filtration Rate, Proteinuria, Tyrosine- Kinase Inhibitors
Abbrevations: RCC: Renal cell carcinoma , TKIs: Tyrosine-Kinase Inhibitors, AKI: Acute Kidney Injury, NSAIDs: Non-Steroidal Anti-Inflammatory Drugs, ARBs: Angiotensin Receptor Blockers, ACEIs: Angiotensin Converting Enzyme Inhibitors, ARBs: Angiotensin Receptor Blockers, CCBs: Calcium Channel Blockers, e- GFR: Estimated Glomerular Filtration Rate
Introduction
Renal cell carcinoma (RCC) accounts for approximately 3% of adult malignancies [1]. Treatment options for the RCC include surgery, radiotherapy and immunotherapy [2]. Besides these options, molecular-targeted therapies in the form of tyrosinekinase inhibitors (TKIs) are commonly used. These agents are well tolerated compared to previously used options (interleukin 2 or interferon-α) and the use of these agents results in longer progression-free survival and increased response rates [3-5]. Despite the advances achieved with these agents, use of the TKIs results in side effects such as fatigue, nausea, diarrhea, gastrointestinal hemorrhage, dysphonia, and palmar-plantar erythrodysaesthesia [6]. Hypertension and proteinuria are also usually encountered after the start of these agents [7-9]. In this study, we compared clinical features between patients with renal cell carcinoma with and without the TKIs treatment and aim to document if any difference exists for renal functions between metastatic and non-metastatic patients during their follow up period.
Materials and Methods
The patients diagnosed with the RCC and followed up at Istanbul Health Sciences University Haydarpaşa Numune Education and Research Hospital oncology polyclinics between 2009 and 2016 were evaluated. Eligible 12 metastatic patients who received a nephrectomy and were treated with the TKIs were included in the metastatic group. Fifteen non-metastatic RCC patients who only received a nephrectomy formed the non-metastatic group. Metastatic patients who did not receive a nephrectomy, patients on dialysis, and patients with insufficient data were excluded. Patients’ demographics and laboratory data were collected from the hospital records and via telephone. The clinical, demographic, and laboratory parameters were compared between the two groups. The data collected included patient age, sex, follow-up time, nephrology follow-up, mortality, history of perioperative acute kidney injury(AKI), use of non-steroidal anti-inflammatory drugs (NSAIDs), use of antihypertensive medications including angiotensin converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs), calcium channel blockers(CCBs), and alpha and beta blockers. The data also included laboratory parameters such as estimated glomerular filtration rate (e-GFR) (calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation 2) and proteinuria (assessed using dipstick and 24-hour urine collection). Creatinine levels before the operations were used to calculate postoperative e-GFR, and postoperative creatinine levels taken just before hospital discharge were used to calculate postoperative e-GFR. Actual e-GFR was calculated using creatinine levels measured at the last hospital visit. Perioperative AKI was defined using the acute kidney injury network classification system. Increase in serum creatinine of 0.3 mg/dl or more within 48 hours or ≥ 1.5 times baseline within 7 days was used in order to define perioperative AKI. Urine volume was not used as a criterion because data for urine volume were not available.
The TKIs used as targeted therapy for our patients were sunitinib, pazopanib, and axitinib. Available creatinine measurements before and after the TKIs treatment were used to present the effect of the TKIs on renal function. Statistical analyses were performed using the MedCalc Statistical Software version 12.7.7 (MedCalc Software bvba, Ostend, Belgium; http://www. medcalc.org; 2013). The normality of continuous variables was investigated using the Shapiro-Wilk test. Descriptive statistics are presented using the mean and standard deviation for normally distributed variables and median (and minimum–maximum) for the non-normally distributed variables. Student’s t-test was used to compare two normally distributed groups. Non-parametric statistical methods were used for values with skewed distributions. The Mann-Whitney U test was used to compare two non-normally distributed groups. The χ² test was used for categorical variables and expressed as observation counts (and percentages). Statistical significance was accepted when the two-sided p value was lower than 0.05.
Results
The study population consisted of 22 males and 5 female patients. The mean age of study population was 59.2±11.3 years. Clinical and laboratory parameters of metastatic and nonmetastatic patients are listed in Table 1. Preoperative e-GFR was significantly lower in metastatic patients when compared to nonmetastatic patients (p: 0.048). When two groups were compared, a trend toward the increased AKI during hospital stay in the nonmetastatic group was observed, but this fell just short of statistical significance (p: 0.109). There was no statistically significant result between two groups when two groups were compared for postoperative e-GFR (p: 0.256). The statistically nonsignificant result for postoperative e-GFR between two groups was also observed for actual e-GFR (p: 0.638) and no statistically significant differences were found between pre-TKI and post-TKI e-GFR values (p: 0.735). Proteinuria was more common in metastatic patients than non-metastatic patients (p<0.001). In metastatic group 8 patients had proteinuria. Four patients out of these 8 patients had 24-hour proteinuria measurements. One patient had nephrotic range proteinuria and the other three patients had non-nephrotic range proteinuria. No biopsies were performed on these patients with proteinuria. Two metastatic patients had negative results for proteinuria. Data for dipstick proteinuria were unavailable for the other two patients. Only one patient in the non-metastatic group had proteinuria and it was at a level of less than 1 gr/day. There was no statistically significant differences in age, sex, follow-up period, NSAIDs use, antihypertensive and ARBs/ACEIs use, and follow-up time between metastatic and non- metastatic patients. Follow-up times for metastatic and non-metastatic patients were 29.9±19.6 and 25.2±9.4 months; respectively. Three patients died during the follow-up period and all were in the metastatic group.
Table 1: Clinical and laboratory parameters.
e-GFR: Estimated glomerular filtration rate; NSAİDs: Non-steroidal anti-inflammatory drugs; ARBs/ACEIs: angiotension receptor blockers/ angiotension converting enzyme inhibitors; * antihypertensive use rather than ARBs/ACEIs
Discussion
Nearly all patients taking the TKIs experience a rise in blood pressure. Systemic vasoconstriction and volume overload are parts of the mechanisms responsible for systemic hypertension caused by TKIs [7]. Despite the risk of hypertension occurrence, the development of hypertension is mostly a good prognostic sign because it is associated with longer progression free and overall survival and can be used as a biomarker for tumor responsiveness [10]. Regarding our study, there was no statistically significant results between groups for ACEIs/ARBs and other antihypertensive use. Proteinuria is another important side effect that can be encountered after the start of targeted agents. In the kidney, the vascular endothelial growth factor pathway is known to be responsible for proteinuria after the start of TKIs [11]. In the study of Baek et al. [12] initiation of sunitinib therapy was related to proteinuria and aggravation of preexisting proteinuria in 17.6% and 23.1% of patients; respectively [12]. Again in the COMPARZ study, discontinuation of treatment because of proteinuria was observed in 3% and 1% the of patients treated with pazopanib and sunitinib; respectively [13]. In our study, most of the patients treated with the TKIs had proteinuria. However, only one patient had nephroticrange proteinuria. We did not perform a renal biopsy on this patient but important data can be obtained through this procedure. Biopsyproven acute interstitial nephritis, thrombotic microangiopathy and acute tubular necrosis have also been encountered after the TKIs use [14-16]. In our study, there was no statistically significant difference between pre-TKIs and pre-TKIs e-GFR values. However, patients can develop renal insufficiency during treatment with targeted agents. A study by Zhu et al. [17] showed the development of renal insufficiency in the RCC patients receiving sunitinib [17]. In our study, despite the statistically significant result for preoperative e- GFR in favor of non- metastatic patients, there was no statistically significant results for postoperative e-GFR between two groups which may be due to the high percentage of patients with AKI in the non-metastatic group. Despite the tumor burden and use of the TKIs in metastatic patients, the non-significant result for postoperative e-GFR between two groups did not change at last hospital visit. The small sample size and retrospective nature of the study are important limitations that should be considered. However, renal side effects encountered after use of the TKIs were emphasized in this study with comparing metastatic and non-metastatic RCC patients. In conclusion, increased risk for proteinuria was documented in metastatic patients with TKIs use. However, use of the TKIs had no effect on e- GFR. There was also no statistically significant difference for the actual e-GFR between the two groups despite the higher preoperative e-GFR observed for non- metastatic patients.
Compliance with Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Institutional approval has been obtained.
For more Lupine Publishers Open Access Journals Please visit our website:
http://www.lupinepublishers.us/
For more Urology Journal articles Please Click Here:
https://lupinepublishers.com/urology-nephrology-journal/
To Know More About Open Access Publishers Please Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
#Lupinepublishers#Lupine publishers#Lupine publishing group#Journal of Nephrology#Journal of Urology
0 notes
Text
AMM européenne pour Bavencio* + Inlyta* dans le cancer du rein
Pfizer et Merck KGaA ont annoncé mardi dans un communiqué que leur immunothérapie Bavencio* (avélumab) avait obtenu une extension d'autorisation de mise sur le marché (AMM) européenne en association avec l'inhibiteur de tyrosine kinase axitinib (Inlyta*, Pfizer) dans le cancer du rein.
L'extension homologuée par la Commission européenne porte sur le traitement en première ligne du carcinome rénal avancé chez les patients adultes.
L'anti-PDL1 Bavencio* est indiqué sur le marché européen depuis septembre 2017 en monothérapie dans le traitement du carcinome à cellules de Merkel (CCM) métastatique. Inlyta* est quant à lui homologué depuis 2012 dans le cancer du rein avancé après échec d’un traitement antérieur par sunitinib ou cytokine.
Aux Etats-Unis, l'association est homologuée dans le carcinome rénal avancé depuis la mi-mai (cf dépêche du 15/05/2019 à 17:51).
Bavencio* + Inlyta* viennent ainsi concurrencer les associations Keytruda* (pembrolizumab, Merck & Co) + Inlyta* et Opdivo* (nivolumab, Bristol-Myers Squibb -BMS) + Yervoy* (ipilimumab, idem), autorisées en Europe depuis respectivement janvier et septembre.
La nouvelle homologation se base sur les données de la phase III JAVELIN Renal 101 qui ont montré une amélioration de la survie sans progression avec l'association par rapport au sunitinib. Les résultats ont été présentés en octobre 2018 (cf dépêche du 22/10/2018 à 09:39).
En 2018, 136.500 nouveaux cas de cancer du rein ont été diagnostiqués en Europe et environ 54.700 personnes en sont mortes, indiquent les deux laboratoires dans leur communiqué. Le carcinome rénal avancé représente environ 90% des diagnostics, ajoutent-ils.
Avec cette extension d'indication, la section posologie du résumé des caractéristiques du produit (RCP) a été mise à jour: dans le carcinome rénal avancé, Bavencio* s'administre par dose de 800 mg en intraveineuse pendant 60 minutes toutes les deux semaines, en parallèle d'une prise orale d'axitinib 5 mg deux fois par jour.
0 notes
Text
An Open Label Phase Ib Dose Escalation Study of TRC105 (Anti‐Endoglin Antibody) with Axitinib in Patients with Metastatic Renal Cell Carcinoma
AbstractBackground.TRC105 is an IgG1 endoglin monoclonal antibody that potentiates VEGF inhibitors in preclinical models. We assessed safety, pharmacokinetics, and antitumor activity of TRC105 in combination with axitinib in patients with metastatic renal cell carcinoma (mRCC).Subjects, Materials, and Methods.Heavily pretreated mRCC patients were treated with TRC105 weekly (8 mg/kg and then 10 mg/kg) in combination with axitinib (initially at 5 mg b.i.d. and then escalated per patient tolerance to a maximum of 10 mg b.i.d.) until disease progression or unacceptable toxicity using a standard 3 + 3 phase I design.Results.Eighteen patients (median number of prior therapies = 3) were treated. TRC105 dose escalation proceeded to 10 mg/kg weekly without dose‐limiting toxicity. Adverse event characteristics of each drug were not increased in frequency or severity when the two drugs were administered concurrently. TRC105 and axitinib demonstrated preliminary evidence of activity, including partial responses (PR) by RECIST in 29% of patients, and median progression‐free survival (11.3 months). None of the patients with PR had PR to prior first‐line treatment. Lower baseline levels of osteopontin and higher baseline levels of TGF‐β receptor 3 correlated with overall response rate.Conclusion.TRC105 at 8 and 10 mg/kg weekly was well tolerated in combination with axitinib, with encouraging evidence of activity in patients with mRCC. A multicenter, randomized phase II trial of TRC105 and axitinib has recently completed enrollment (NCT01806064).Implications for Practice.TRC105 is a monoclonal antibody to endoglin (CD105), a receptor densely expressed on proliferating endothelial cells and also on renal cancer stem cells that is implicated as a mediator of resistance to inhibitors of the VEGF pathway. In this Phase I trial, TRC105 combined safely with axitinib at the recommended single agent doses of each drug in patients with renal cell carcinoma. The combination demonstrated durable activity in a VEGF inhibitor‐refractory population and modulated several angiogenic biomarkers. A randomized Phase II trial testing TRC105 in combination with axitinib in clear cell renal cell carcinoma has completed accrual.
http://bit.ly/2Dw4FTY
0 notes
Text
Patients with metastatic renal cell carcinoma who benefit from axitinib dose titration: analysis from a randomised, double-blind phase II study
Abstract
Background
A prospective, randomised phase II study demonstrated clinical benefit of axitinib dose titration in a subset of treatment-naïve patients treated with axitinib for metastatic renal cell carcinoma. This analysis evaluated patient baseline characteristics that may impact overall survival (OS) with axitinib dose titration.
Methods
Following a 4-week lead-in period during which all patients received axitinib 5 mg twice-daily (bid); patients meeting the predefined randomisation criteria were randomly assigned to receive axitinib 5 mg bid plus either axitinib or placebo titration. In exploratory analyses, patients were grouped into those who achieved OS ≥24 versus < 24 months, and compared their baseline characteristics with Fisher’s exact test or Cochran-Armitage trend exact test, with a 5% significance level. Potential predictive baseline characteristics associated with effect of axitinib dose titration on OS were investigated using a Cox proportional hazard model.
Results
Overall, 112 patients were randomised. Three of 56 patients receiving axitinib titration were censored; of the remaining 53, 33 (62%) achieved OS ≥24 months versus 20 (38%) with OS < 24 months. Patients with OS ≥24 vs. < 24 months, respectively, had significantly fewer metastatic sites (≤2 metastases: 52% vs. 10%; ≥3 metastases: 48% vs. 90%), fewer lymph node (45% vs. 75%) or liver (15% vs. 45%) metastases, higher haemoglobin level (i.e., ≥ lower limit of normal: 67% vs. 25%) at baseline, lower neutrophil (≤ upper limit of normal, 97% vs. 75%) and platelet (≤ upper limit of normal, 82% vs. 50%) levels at baseline and ≥ 1 year between histopathological diagnosis and treatment (64% vs. 15%). The primary reason for treatment discontinuation in both OS groups was disease progression. The frequency of toxicity-related discontinuation was comparable between the 2 groups, indicating that it was not a factor for a shorter OS. The multivariate analysis showed that ≥1 year from histopathological diagnosis to treatment and baseline haemoglobin level equal or greater than lower limit of normal were significant covariates associated with favourable OS in patients receiving axitinib titration.
Conclusions
The current analyses identified potentially predictive factors that could help selecting patients who may benefit from axitinib dose titration.
Trial registration
ClinicalTrials.gov identifier, NCT00835978. Registered prospectively, February 4, 2009.
http://bit.ly/2CTATcR
0 notes
Text
Baisses de prix à venir pour les anticancéreux de Pfizer Xalkori* et Inlyta*
Le Journal officiel de mardi a publié un arrêté prévoyant des baisses de prix en 2019 pour deux anticancéreux de Pfizer, Inlyta* (axitinib) et Xalkori* (crizotinib).
La baisse de prix d'Inlyta* prendra effet le 1er janvier 2019 et sera de 3%. Ses prix publics TTC (hors honoraires de dispensation) s'étaleront de 355,29 euros pour 28 comprimés à 1 mg à 4.462,24 euros pour 56 comprimés à 7 mg.
Le 2 janvier 2019, le prix de Xalkori* sera de 15% à 4.407,76 euros pour ses deux dosages à 200 mg et 250 mg.
Le produit de contraste Sonovue* (hexafluorure de soufre, Bracco Imaging) va connaître une double baisse, d'abord au 2 janvier 2019, puis au 2 janvier 2020. Elle sera au total de 22% et portera son prix à 69,83 euros.
Au 1er janvier 2019, l'analogue de la GnRH Synarel* (nafaréline, Pfizer) coûtera 114,94 euros, soit une baisse de 5%.
Le prix de plusieurs autres spécialités baissera au 2 janvier 2019. Il s'agit de:
l'antiviral Tamiflu* (oseltamivir, Roche), avec une baisse de 20% à 8,93 euros pour 30 mg, 13,51 euros pour 45 mg et 19,09 euros pour 75 mg
l'anti-diurétique Minirin*/Minirinmelt* (desmopressine en comprimés/en lyophilisats oraux), avec une baisse de 8% pour des prix allant de 19,94 euros (30 comprimés à 0,1 mg) à 123,71 euros (100 comprimés à 120 µg)
l'anti-asthmatique Atimos* et son similiaire Formoair* (formotérol en solution pour inhalation, 100 doses de 12 µg en flacon pressurisé, Chiesi), avec une baisse de 15% à 36,06 euros
le médicament à usage diagnostique Hexvix* (hexylaminolévulinate, Ipsen), avec une baisse de 9% à 420,79 euros
le traitement de la thrombocytémie essentielle Xagrid* (anagrélide, Shire), avec une baisse de 20% à 332,87 euros
la vitamine D3 en solution buvable en gouttes Adrigyl* 10.000 UI/mL (Crinex), avec une baisse de 4% à 1,65 euro.
0 notes
Text
Axitinib Versus Placebo as an Adjuvant Treatment for Renal Cell Carcinoma: Results From the Phase III, Randomized ATLAS Trial
Abstract
Background
The ATLAS trial compared axitinib versus placebo in patients with locoregional renal cell carcinoma (RCC) at risk of recurrence after nephrectomy.
Patients and Methods
In a phase III, randomized, double-blind trial, patients had >50% clear-cell RCC, had undergone nephrectomy, and had no evidence of macroscopic residual or metastatic disease (independent review committee [IRC] confirmed). The intent-to-treat population included all randomized patients (≥pT2 and/or N+, any Fuhrman grade [FG], Eastern Cooperative Oncology Group status 0/1). Patients (stratified by risk group/country) received (1:1) oral twice-daily axitinib 5 mg or placebo for ≤3 years, with a 1-year minimum unless recurrence, occurrence of second primary malignancy, significant toxicity, or consent withdrawal. The primary end point was disease-free survival (DFS) per IRC. A prespecified DFS analysis in the highest-risk subpopulation (pT3, FG ≥ 3 or pT4 and/or N+, any T, any FG) was conducted.
Results
A total of 724 patients (363 versus 361, axitinib versus placebo) were randomized from May 8, 2012, to July 1, 2016. The trial was stopped due to futility at a preplanned interim analysis at 203 DFS events. There was no significant difference in DFS per IRC (hazard ratio [HR] = 0.870; 95% confidence interval [CI]: 0.660–1.147; P=0.3211). In the highest-risk subpopulation, a 36% and 27% reduction in risk of a DFS event (HR; 95% CI) was observed per investigator (0.641; 0.468–0.879; P=0.0051), and by IRC (0.735; 0.525–1.028; P=0.0704), respectively. Overall survival data were not mature. Similar adverse events (AEs; 99% versus 92%) and serious AEs (19% versus 14%), but more grade 3/4 AEs (61% versus 30%) were reported for axitinib versus placebo.
Conclusions
ATLAS did not meet its primary end point; however, improvement in DFS per investigator was seen in the highest-risk subpopulation. No new safety signals were reported.
Trial registration number
NCT01599754
https://ift.tt/2PfYVpk
0 notes
Text
Carcinome rénal avancé ou métastatique: l'association pembrolizumab + axitinib prolonge la survie
L'association de pembrolizumab (Keytruda*, Merck & Co) et d'axitinib (Inlyta*, Pfizer) a permis de prolonger à la fois la survie globale et la survie sans progression, en traitement de première ligne, dans un essai clinique de phase III, a annoncé Merck, jeudi dans un communiqué.
Dans cette étude KEYNOTE-426, l'association de l'anti-PD-1 pembrolizumab et de l'inhibiteur de tyrosine kinase axitinib, en première ligne, a atteint les deux critères principaux d'évaluation, avec un allongement statistiquement significatif et cliniquement important de la survie globale et de la survie sans progression, par rapport au sunitinib seul, indique le groupe américain sans préciser les chiffres.
Le critère secondaire clé du taux de réponse objective a également été atteint.
Le profil de sécurité du pembrolizumab et de l'axitinib observé dans cet essai correspondait à ce qui a déjà été rapporté dans de précédentes études.
Les résultats seront présentés à un prochain congrès médical et soumis aux autorités réglementaires à travers le monde, ajoute Merck.
Dans KEYNOTE-426, 862 patients avec un carcinome rénal avancé ou métastatique ont été randomisés en ouvert entre l'association de pembrolizumab à 200 mg IV toutes les trois semaines + axitinib per os à 5 mg deux fois par jour jusqu'à 24 mois et le sunitinib per os à 50 mg en prise unique quotidienne pendant 4 semaines, suivi d'un arrêt de traitement de 2 semaines.
0 notes
Text
Phase I study of axitinib and everolimus in metastatic solid tumours and extension to metastatic renal cell carcinoma: Results of EVAX study
Publication date: November 2017
Source:European Journal of Cancer, Volume 85
Author(s): Alain Ravaud, Carlos Gomez-Roca, Marie-Quitterie Picat, Laurence Digue, Christine Chevreau, Anne Gimbert, Emmanuelle Chauzit, Rémi Sitta, François Cornelis, Julien Asselineau, Richard Aziza, Amaury Daste, Cathy Quemener, Jessica Baud, Andréas Bikfalvi, Delphine Pedenon–Périchout, Adelaïde Doussau, Mathieu Molimard, Jean-Pierre Delord
PurposeAnti-angiogenic and mammalian target of rapamycin inhibitors have shown efficacy in solid tumours. Reported combination of both drugs was deemed to be too toxic. Due to a potential favourable safety profile of axitinib (AX), a phase I study combining everolimus (EV) and AX for solid tumours was explored.Experimental designPatients (pts) with advanced cancers were enrolled in an escalation phase I study to investigate the safety of the combination. Pharmacokinetic profile and functional vascular imaging were performed. An extension to pts with naive metastatic renal cell carcinoma (MRCC) was explored.Results15 pts were included over three different dose levels (DLs); DL 0: AX 3 mg BID (twice daily)/EV 5 mg OD (once daily); DL 1: AX 5 mg BID/EV 5 mg OD and DL 2: AX 5 mg BID/EV 10 mg OD for 28 d. One dose-limiting toxicity (DLT) was reported at DL 0: grade (Gr) III diarrhoea and one DLT at DL 2: Gr III asthenia. Three severe adverse events (AEs) in two pts were unexpected: jaw osteonecrosis, recurrent renal failure and cardiomyopathy. Maximum tolerated dose (MTD) was level 2. After 1st cycle, Gr III or Gr II AEs of interest were mainly asthenia, diarrhoea and anorexia. All pts but one showed tumour shrinkage. Partial responses (PRs) were seen in one pt with bladder carcinoma and in one pt in 1st line MRCC in the escalating phase. In the extension phase in naive MRCC treated at MTD, five pts had a PR and one pt had a prolonged stable disease.ConclusionThe recommended dose for phase II is AX 5 mg BID/EV 10 mg OD.
http://ift.tt/2j25c9j
0 notes
Text
Axitinib for Gemcitabine-refractory Advanced Biliary Tract Cancer: Report of 5 Cases
Background/Aim: Vascular endothelial growth factor receptor (VEGFR) has been identified as a treatment target for biliary tract cancer (BTC) and axitinib is a selective inhibitor of vascular endothelial growth factor receptor (VEGFR)-1/2/3. This study was conducted as a preliminary evaluation of the safety and efficacy of axitinib for patients with advanced BTC. Patients and Methods: Patients refractory to gemcitabine-based regimens were administered axitinib at the dose of 5 mg twice daily. Results: Five patients (3 male and 2 female) with a median age of 68 years were enrolled. Although 3 patients developed treatment-related grade 3/4 adverse events (AEs), none of these patients required discontinuation of the protocol treatment due to the AEs. Partial response (PR) was achieved in 1 patient, with a 67% reduction. The response was classified as stable disease (SD) in 3 patients and as progressive disease (PD) in 1 patient. Overall survival (OS) and progression-free survival (PFS) ranged from 2.0 to 19.9 months and 1.5 to 7.4 months, respectively. Conclusion: This preliminary study suggested that axitinib is well-tolerated and might exert promising activity in patients with BTC.
http://ift.tt/2tdRtgZ
0 notes
Text
A phase 2 study of the efficacy and biomarker on the combination of transarterial chemoembolization and axitinib in the treatment of inoperable hepatocellular carcinoma
BACKGROUND
A surge of vascular endothelial growth factor (VEGF) after transarterial chemoembolization (TACE) may contribute to tumor progression. Axitinib is a potent antiangiogenic agent with main activity against VEGF receptors 1 to 3. To the authors' knowledge, its role in combination with TACE for the treatment of patients with inoperable hepatocellular carcinoma (HCC) is unclear.
METHODS
A phase 2 clinical trial (ClinicalTrials.gov identifier NCT01352728) was conducted to evaluate the combination treatment. Patients with inoperable HCC who were potential candidates for TACE initiated treatment with axitinib at a dose of 5 mg twice daily and were evaluated for the need for TACE every 8 weeks. Axitinib was withheld 24 hours before TACE, and resumed 24 hours afterward when fulfilling predefined criteria. Radiologic assessment was conducted every 8 weeks. The primary endpoint was the 2-year overall survival (OS) rate.
RESULTS
A total of 50 patients were recruited from March 2011 to April 2014. The mean age of the patients was 61.8 years, and 46 patients (92%) had hepatitis B infection. The Barcelona Clinic Liver Cancer stage B/C percentage was 76% (38 cases)/24% (12 cases). The 2-year OS rate was 43.7%, and the median OS was 18.8 months in the intention-to-treat population. Among the evaluable population (44 patients), 40.9% (18 patients) and 27.3% (12 patients) achieved complete and partial responses, respectively. Common grade 3 or above axitinib-related complications included hand-foot skin reaction (14%) and hypertension (24%). The presence of hypertension during treatment was found to be an independent prognosticator (hazard ratio, 0.563; P = .0073) suggestive of a contributory role of axitinib to efficacy.
CONCLUSIONS
The combination of axitinib and TACE was potentially efficacious for patients with inoperable HCC with a high radiologic response rate. Cancer 2017. © 2017 American Cancer Society.
http://ift.tt/2rG4sH2
0 notes