#Brainstem Midbrain Notes
Explore tagged Tumblr posts
Text
Brainstem Midbrain Notes
#MendelsLaws#HereditaryTraits#ScienceOfInheritance#MendelianInheritance#GeneticDiscoveries#BiologyLessons#MendelsPrinciples#GeneticsEducation#HereditaryScience#Brainstem Midbrain Notes
0 notes
Text
Also preserved in our archive
By Kevin Kavanagh, MD
(Follow the link to get all the links!)
Over the last month, volumes of impactful scientific research have been published regarding long-term COVID-19. These findings clearly describe our society's precarious state and the desperate need to change course. We must start controlling our impulses to partake in desirable but risky behavior and instead prioritize controlling the spread of COVID-19.
Most concerning was a large survey by Shijie Quin and colleagues involving over 74,000 participants in China that found the incidence of long-term COVID-19 in their country to be between 10% and 30%. The researchers documented recurrent infections and found that although reinfections were associated with milder disease, they were also associated with “a higher incidence and severity of long COVID.” In addition, they reported that vaccinations reduced long-term symptoms by 30% to 70%. Dr. Ziyad Al-Aly noted that the reported symptoms in this study of brain fog and cognitive decline mirrored other studies from across the world. Long COVID is a worldwide problem that does not involve just one nation or society.
The dangers COVID-19 poses to health care workers were underscored by research from the King’s College of London that found a third of health care workers had symptoms of long COVID. And patients are also not spared. NSW Ministry of Health data reported that in Australian hospitals, thousands of patients have caught COVID-19, and hundreds have died. In the US, we are handling this situation by burying our heads in the sand. We are not counting nor reporting health care-associated COVID-19.
Many of us were hoping that children would be less affected. They would become immune early, and the disease would burn out. These hopes were dashed by a recent NIH study (RECOVER-Pediatrics cohort STUDY) covered by Medscape, which reported that “20% of kids (ages 6-11) and 14% of teens met researchers' threshold for long COVID.”
Unfortunately, there is mounting evidence regarding the role that brain injury plays in long-term COVID-19. The finding by Shijie Quin and colleagues that cognitive dysfunction is a major part of long COVID was also substantiated by Catarina Rua and colleagues in the journal Brain, who documented with imaging studies persistent damage in COVID-19 patients’ brainstems (medulla, pons, and midbrain regions) 93 to 548 days after hospital admission.
In a highly controversial challenge study performed in the United Kingdom, 18 of 34 healthy young adults (aged 18 to 30) volunteers developed COVID-19 after exposure to the virus. One had an asymptomatic infection, and the remaining (17) developed a mild one. Comparing pre-and post-test results with follow-up at 30, 90, 180, 270, and 360 days, the research documented deficiencies in memory and executive function tasks.
Executive function relates to judgment, anger control, and managing emotions and actions. There is mounting research finding that executive function is one of the primary cognitive functions degraded in long COVID. Rosalia-Dacosta-Aguayo and colleagues have reported in 53 subjects with mild to moderate long COVID, 59% had deficits in executive function. Using imaging studies, the researchers documented that the cognitive impairment was “linked” to changes in brain structure. Of the 53 participants, 43 had mild to moderate COVID-19, 9 were treated in the hospital, and none were in the ICU.
Degradation of executive function can have a plethora of societal manifestations. For example, auto insurance is the leading sector experiencing the largest inflation in the US, which rose almost 21% in the 12 months ending in February 2024. Increased claims and traffic deaths have driven this increase. I would assert that this phenomenon is a manifestation of post-COVID deficiencies in executive function, which has caused an increase in risky driving behavior. In December 2022, Infection Control Today® discussed an American Journal of Medicine article that observed a significant increase in traffic accidents in vaccine-hesitant individuals. A 2024 study by the American Automobile Association found that risk driving spiked, as did an associated increase in fatal traffic accidents. A study published this month (October 8, 2024) in Neurology reported a correlation between COVID-19 cases and traffic accidents.
It has been shown that patients who experience disturbances in smell have an increased risk of developing “behavioral, functional, and structural brain alterations.” This virus has a propensity to affect the brain, including the prefrontal cortex. One of the first researchers to describe the propensity of this virus to infect the brain was Fernanda Crunfli, PhD, and colleagues, who observed infection of astrocytes. This was a surprising finding since brain cells (astrocytes) do not have ACE2 receptors. Thus, the researchers postulated a second method of cellular entry. This postulate was confirmed by researchers from the University of Illinois and Northwestern University, who observed that while infecting the lungs, the virus can mutate, losing its furan cleavage site, which enhances its ability to infect the central nervous system.
Thus, a picture is starting to form of an insidious, dangerous pathogen that, upon infection, can change the host's behavior to manifest risky behavior, increasing the spread of the SARS-CoV-2 virus and repeating the cycle. Acquiring such an ability is an example of evolutionary pressure to enhance the virus's survival.
All the above is depressing but also largely preventable. Chinese philosopher Lao Tzu stated that if you do not change directions, you may end up where you are headed. We must prioritize vaccinations, use N95 masks, and clean indoor air to stop this virus's spread. Only then will we be headed in the correct direction.
#mask up#public health#wear a mask#pandemic#covid#wear a respirator#covid 19#still coviding#coronavirus#sars cov 2#long covid#covid is airborne#covid is not over#covid conscious
73 notes
·
View notes
Text
Gross anatomy See also: Evolution of the brain § Evolution of the human brain, and Neuroscience of sex differences The adult human brain weighs on average about 1.2–1.4 kg (2.6–3.1 lb) which is about 2% of the total body weight,[2][3] with a volume of around 1260 cm3 in men and 1130 cm3 in women.[4] There is substantial individual variation,[4] with the standard reference range for men being 1,180–1,620 g (2.60–3.57 lb)[5] and for women 1,030–1,400 g (2.27–3.09 lb).[6]
The cerebrum, consisting of the cerebral hemispheres, forms the largest part of the brain and overlies the other brain structures.[7] The outer region of the hemispheres, the cerebral cortex, is grey matter, consisting of cortical layers of neurons. Each hemisphere is divided into four main lobes – the frontal lobe, parietal lobe, temporal lobe, and occipital lobe.[8] Three other lobes are included by some sources which are a central lobe, a limbic lobe, and an insular lobe.[9] The central lobe comprises the precentral gyrus and the postcentral gyrus and is included since it forms a distinct functional role.[9][10]
The brainstem, resembling a stalk, attaches to and leaves the cerebrum at the start of the midbrain area. The brainstem includes the midbrain, the pons, and the medulla oblongata. Behind the brainstem is the cerebellum (Latin: little brain).[7]
The cerebrum, brainstem, cerebellum, and spinal cord are covered by four[11] membranes called meninges. The membranes are the tough dura mater; the middle arachnoid mater and the more delicate inner pia mater. Between the arachnoid mater and the pia mater is the subarachnoid space and subarachnoid cisterns, which contain the cerebrospinal fluid.[12] The outermost membrane of the cerebral cortex is the basement membrane of the pia mater called the glia limitans and is an important part of the blood–brain barrier.[13] The living brain is very soft, having a gel-like consistency similar to soft tofu.[14] The cortical layers of neurons constitute much of the cerebral grey matter, while the deeper subcortical regions of myelinated axons, make up the white matter.[7] The white matter of the brain makes up about half of the total brain volume.[15]
Structural and functional areas of the human brain A diagram showing various structures within the human brain Human brain bisected in the sagittal plane, showing the white matter of the corpus callosum A diagram of the functional areas of the human brain Functional areas of the human brain. Dashed areas shown are commonly left hemisphere dominant. Cerebrum Main articles: Cerebrum and Cerebral cortex
Major gyri and sulci on the lateral surface of the cortex
Lobes of the brain The cerebrum is the largest part of the brain and is divided into nearly symmetrical left and right hemispheres by a deep groove, the longitudinal fissure.[16] Asymmetry between the lobes is noted as a petalia.[17] The hemispheres are connected by five commissures that span the longitudinal fissure, the largest of these is the corpus callosum.[7] Each hemisphere is conventionally divided into four main lobes; the frontal lobe, parietal lobe, temporal lobe, and occipital lobe, named according to the skull bones that overlie them.[8] Each lobe is associated with one or two specialised functions though there is some functional overlap between them.[18] The surface of the brain is folded into ridges (gyri) and grooves (sulci), many of which are named, usually according to their position, such as the frontal gyrus of the frontal lobe or the central sulcus separating the central regions of the hemispheres. There are many small variations in the secondary and tertiary folds.[19]
The outer part of the cerebrum is the cerebral cortex, made up of grey matter arranged in layers. It is 2 to 4 millimetres (0.079 to 0.157 in) thick, and deeply folded to give a convoluted appearance.[20] Beneath the cortex is the cerebral white matter. The largest part of the cerebral cortex is the neocortex, which has six neuronal layers. The rest of the cortex is of allocortex, which has three or four layers.[7]
The cortex is mapped by divisions into about fifty different functional areas known as Brodmann's areas. These areas are distinctly different when seen under a microscope.[21] The cortex is divided into two main functional areas – a motor cortex and a sensory cortex.[22] The primary motor cortex, which sends axons down to motor neurons in the brainstem and spinal cord, occupies the rear portion of the frontal lobe, directly in front of the somatosensory area. The primary sensory areas receive signals from the sensory nerves and tracts by way of relay nuclei in the thalamus. Primary sensory areas include the visual cortex of the occipital lobe, the auditory cortex in parts of the temporal lobe and insular cortex, and the somatosensory cortex in the parietal lobe. The remaining parts of the cortex are called the association areas. These areas receive input from the sensory areas and lower parts of the brain and are involved in the complex cognitive processes of perception, thought, and decision-making.[23] The main functions of the frontal lobe are to control attention, abstract thinking, behaviour, problem-solving tasks, and physical reactions and personality.[24][25] The occipital lobe is the smallest lobe; its main functions are visual reception, visual-spatial processing, movement, and colour recognition.[24][25] There is a smaller occipital lobule in the lobe known as the cuneus. The temporal lobe controls auditory and visual memories, language, and some hearing and speech.[24]
Cortical folds and white matter in horizontal bisection of head The cerebrum contains the ventricles where the cerebrospinal fluid is produced and circulated. Below the corpus callosum is the septum pellucidum, a membrane that separates the lateral ventricles. Beneath the lateral ventricles is the thalamus and to the front and below is the hypothalamus. The hypothalamus leads on to the pituitary gland. At the back of the thalamus is the brainstem.[26]
The basal ganglia, also called basal nuclei, are a set of structures deep within the hemispheres involved in behaviour and movement regulation.[27] The largest component is the striatum, others are the globus pallidus, the substantia nigra and the subthalamic nucleus.[27] The striatum is divided into a ventral striatum, and dorsal striatum, subdivisions that are based upon function and connections. The ventral striatum consists of the nucleus accumbens and the olfactory tubercle whereas the dorsal striatum consists of the caudate nucleus and the putamen. The putamen and the globus pallidus lie separated from the lateral ventricles and thalamus by the internal capsule, whereas the caudate nucleus stretches around and abuts the lateral ventricles on their outer sides.[28] At the deepest part of the lateral sulcus between the insular cortex and the striatum is a thin neuronal sheet called the claustrum.[29]
Below and in front of the striatum are a number of basal forebrain structures. These include the nucleus basalis, diagonal band of Broca, substantia innominata, and the medial septal nucleus. These structures are important in producing the neurotransmitter, acetylcholine, which is then distributed widely throughout the brain. The basal forebrain, in particular the nucleus basalis, is considered to be the major cholinergic output of the central nervous system to the striatum and neocortex.[30]
Cerebellum
Human brain viewed from below, showing cerebellum and brainstem Main article: Cerebellum The cerebellum is divided into an anterior lobe, a posterior lobe, and the flocculonodular lobe.[31] The anterior and posterior lobes are connected in the middle by the vermis.[32] Compared to the cerebral cortex, the cerebellum has a much thinner outer cortex that is narrowly furrowed into numerous curved transverse fissures.[32] Viewed from underneath between the two lobes is the third lobe the flocculonodular lobe.[33] The cerebellum rests at the back of the cranial cavity, lying beneath the occipital lobes, and is separated from these by the cerebellar tentorium, a sheet of fibre.[34]
It is connected to the brainstem by three pairs of nerve tracts called cerebellar peduncles. The superior pair connects to the midbrain; the middle pair connects to the medulla, and the inferior pair connects to the pons.[32] The cerebellum consists of an inner medulla of white matter and an outer cortex of richly folded grey matter.[34] The cerebellum's anterior and posterior lobes appear to play a role in the coordination and smoothing of complex motor movements, and the flocculonodular lobe in the maintenance of balance[35] although debate exists as to its cognitive, behavioural and motor functions.[36]
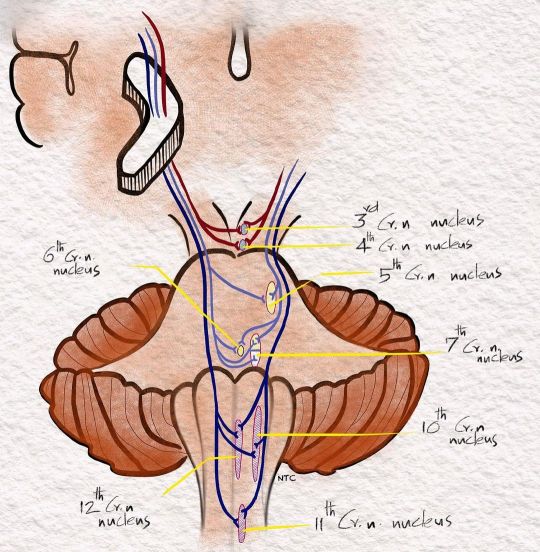
Brainstem Main article: Brainstem The brainstem lies beneath the cerebrum and consists of the midbrain, pons and medulla. It lies in the back part of the skull, resting on the part of the base known as the clivus, and ends at the foramen magnum, a large opening in the occipital bone. The brainstem continues below this as the spinal cord,[37] protected by the vertebral column.
Ten of the twelve pairs of cranial nerves[a] emerge directly from the brainstem.[37] The brainstem also contains many cranial nerve nuclei and nuclei of peripheral nerves, as well as nuclei involved in the regulation of many essential processes including breathing, control of eye movements and balance.[38][37] The reticular formation, a network of nuclei of ill-defined formation, is present within and along the length of the brainstem.[37] Many nerve tracts, which transmit information to and from the cerebral cortex to the rest of the body, pass through the brainstem.[37]
Microanatomy The human brain is primarily composed of neurons, glial cells, neural stem cells, and blood vessels. Types of neuron include interneurons, pyramidal cells including Betz cells, motor neurons (upper and lower motor neurons), and cerebellar Purkinje cells. Betz cells are the largest cells (by size of cell body) in the nervous system.[39] The adult human brain is estimated to contain 86±8 billion neurons, with a roughly equal number (85±10 billion) of non-neuronal cells.[40] Out of these neurons, 16 billion (19%) are located in the cerebral cortex, and 69 billion (80%) are in the cerebellum.[3][40]
Types of glial cell are astrocytes (including Bergmann glia), oligodendrocytes, ependymal cells (including tanycytes), radial glial cells, microglia, and a subtype of oligodendrocyte progenitor cells. Astrocytes are the largest of the glial cells. They are stellate cells with many processes radiating from their cell bodies. Some of these processes end as perivascular end-feet on capillary walls.[41] The glia limitans of the cortex is made up of astrocyte foot processes that serve in part to contain the cells of the brain.[13]
Mast cells are white blood cells that interact in the neuroimmune system in the brain.[42] Mast cells in the central nervous system are present in a number of structures including the meninges;[42] they mediate neuroimmune responses in inflammatory conditions and help to maintain the blood–brain barrier, particularly in brain regions where the barrier is absent.[42][43] Mast cells serve the same general functions in the body and central nervous system, such as effecting or regulating allergic responses, innate and adaptive immunity, autoimmunity, and inflammation.[42] Mast cells serve as the main effector cell through which pathogens can affect the biochemical signaling that takes place between the gastrointestinal tract and the central nervous system.[44][45]
Some 400 genes are shown to be brain-specific. In all neurons, ELAVL3 is expressed, and in pyramidal neurons, NRGN and REEP2 are also expressed. GAD1 – essential for the biosynthesis of the neurotransmitter GABA – is expressed in interneurons. Proteins expressed in glial cells include astrocyte markers GFAP and S100B whereas myelin basic protein and the transcription factor OLIG2 are expressed in oligodendrocytes.[46]
Cerebrospinal fluid
Cerebrospinal fluid circulates in spaces around and within the brain Main article: Cerebrospinal fluid Cerebrospinal fluid is a clear, colourless transcellular fluid that circulates around the brain in the subarachnoid space, in the ventricular system, and in the central canal of the spinal cord. It also fills some gaps in the subarachnoid space, known as subarachnoid cisterns.[47] The four ventricles, two lateral, a third, and a fourth ventricle, all contain a choroid plexus that produces cerebrospinal fluid.[48] The third ventricle lies in the midline and is connected to the lateral ventricles.[47] A single duct, the cerebral aqueduct between the pons and the cerebellum, connects the third ventricle to the fourth ventricle.[49] Three separate openings, the middle and two lateral apertures, drain the cerebrospinal fluid from the fourth ventricle to the cisterna magna, one of the major cisterns. From here, cerebrospinal fluid circulates around the brain and spinal cord in the subarachnoid space, between the arachnoid mater and pia mater.[47] At any one time, there is about 150mL of cerebrospinal fluid – most within the subarachnoid space. It is constantly being regenerated and absorbed, and is replaced about once every 5–6 hours.[47]
A glymphatic system has been described[50][51][52] as the lymphatic drainage system of the brain. The brain-wide glymphatic pathway includes drainage routes from the cerebrospinal fluid, and from the meningeal lymphatic vessels that are associated with the dural sinuses, and run alongside the cerebral blood vessels.[53][54] The pathway drains interstitial fluid from the tissue of the brain.[54]
Blood supply Main article: Cerebral circulation
Two circulations joining at the circle of Willis (inferior view)
Diagram showing features of cerebral outer membranes and supply of blood vessels The internal carotid arteries supply oxygenated blood to the front of the brain and the vertebral arteries supply blood to the back of the brain.[55] These two circulations join in the circle of Willis, a ring of connected arteries that lies in the interpeduncular cistern between the midbrain and pons.[56]
The internal carotid arteries are branches of the common carotid arteries. They enter the cranium through the carotid canal, travel through the cavernous sinus and enter the subarachnoid space.[57] They then enter the circle of Willis, with two branches, the anterior cerebral arteries emerging. These branches travel forward and then upward along the longitudinal fissure, and supply the front and midline parts of the brain.[58] One or more small anterior communicating arteries join the two anterior cerebral arteries shortly after they emerge as branches.[58] The internal carotid arteries continue forward as the middle cerebral arteries. They travel sideways along the sphenoid bone of the eye socket, then upwards through the insula cortex, where final branches arise. The middle cerebral arteries send branches along their length.[57]
The vertebral arteries emerge as branches of the left and right subclavian arteries. They travel upward through transverse foramina which are spaces in the cervical vertebrae. Each side enters the cranial cavity through the foramen magnum along the corresponding side of the medulla.[57] They give off one of the three cerebellar branches. The vertebral arteries join in front of the middle part of the medulla to form the larger basilar artery, which sends multiple branches to supply the medulla and pons, and the two other anterior and superior cerebellar branches.[59] Finally, the basilar artery divides into two posterior cerebral arteries. These travel outwards, around the superior cerebellar peduncles, and along the top of the cerebellar tentorium, where it sends branches to supply the temporal and occipital lobes.[59] Each posterior cerebral artery sends a small posterior communicating artery to join with the internal carotid arteries.
Blood drainage Cerebral veins drain deoxygenated blood from the brain. The brain has two main networks of veins: an exterior or superficial network, on the surface of the cerebrum that has three branches, and an interior network. These two networks communicate via anastomosing (joining) veins.[60] The veins of the brain drain into larger cavities of the dural venous sinuses usually situated between the dura mater and the covering of the skull.[61] Blood from the cerebellum and midbrain drains into the great cerebral vein. Blood from the medulla and pons of the brainstem have a variable pattern of drainage, either into the spinal veins or into adjacent cerebral veins.[60]
The blood in the deep part of the brain drains, through a venous plexus into the cavernous sinus at the front, and the superior and inferior petrosal sinuses at the sides, and the inferior sagittal sinus at the back.[61] Blood drains from the outer brain into the large superior sagittal sinus, which rests in the midline on top of the brain. Blood from here joins with blood from the straight sinus at the confluence of sinuses.[61]
Blood from here drains into the left and right transverse sinuses.[61] These then drain into the sigmoid sinuses, which receive blood from the cavernous sinus and superior and inferior petrosal sinuses. The sigmoid drains into the large internal jugular veins.[61][60]
The blood–brain barrier The larger arteries throughout the brain supply blood to smaller capillaries. These smallest of blood vessels in the brain, are lined with cells joined by tight junctions and so fluids do not seep in or leak out to the same degree as they do in other capillaries; this creates the blood–brain barrier.[43] Pericytes play a major role in the formation of the tight junctions.[62] The barrier is less permeable to larger molecules, but is still permeable to water, carbon dioxide, oxygen, and most fat-soluble substances (including anaesthetics and alcohol).[43] The blood-brain barrier is not present in the circumventricular organs—which are structures in the brain that may need to respond to changes in body fluids—such as the pineal gland, area postrema, and some areas of the hypothalamus.[43] There is a similar blood–cerebrospinal fluid barrier, which serves the same purpose as the blood–brain barrier, but facilitates the transport of different substances into the brain due to the distinct structural characteristics between the two barrier systems.[43][63]
Development Main article: Development of the nervous system in humans Further information: Development of the human brain
Neurulation and neural crest cells Simple drawing of the lateral view of the three primary vesicle stage of the three to four week old embryo shown in different colors, and the five secondary vesicle stage of the five week old embryo shown in different colors and a lateral view of this Primary and secondary vesicle stages of development in the early embryo to the fifth week Very simple drawing of the front end of a human embryo, showing each vesicle of the developing brain in a different color. Brain of a human embryo in the sixth week of development At the beginning of the third week of development, the embryonic ectoderm forms a thickened strip called the neural plate.[64] By the fourth week of development the neural plate has widened to give a broad cephalic end, a less broad middle part and a narrow caudal end. These swellings are known as the primary brain vesicles and represent the beginnings of the forebrain (prosencephalon), midbrain (mesencephalon), and hindbrain (rhombencephalon).[65]
Neural crest cells (derived from the ectoderm) populate the lateral edges of the plate at the neural folds. In the fourth week—during the neurulation stage—the neural folds close to form the neural tube, bringing together the neural crest cells at the neural crest.[66] The neural crest runs the length of the tube with cranial neural crest cells at the cephalic end and caudal neural crest cells at the tail. Cells detach from the crest and migrate in a craniocaudal (head to tail) wave inside the tube.[66] Cells at the cephalic end give rise to the brain, and cells at the caudal end give rise to the spinal cord.[67]
The tube flexes as it grows, forming the crescent-shaped cerebral hemispheres at the head. The cerebral hemispheres first appear on day 32.[68] Early in the fourth week, the cephalic part bends sharply forward in a cephalic flexure.[66] This flexed part becomes the forebrain (prosencephalon); the adjoining curving part becomes the midbrain (mesencephalon) and the part caudal to the flexure becomes the hindbrain (rhombencephalon). These areas are formed as swellings known as the three primary brain vesicles. In the fifth week of development five secondary brain vesicles have formed.[69] The forebrain separates into two vesicles – an anterior telencephalon and a posterior diencephalon. The telencephalon gives rise to the cerebral cortex, basal ganglia, and related structures. The diencephalon gives rise to the thalamus and hypothalamus. The hindbrain also splits into two areas – the metencephalon and the myelencephalon. The metencephalon gives rise to the cerebellum and pons. The myelencephalon gives rise to the medulla oblongata.[70] Also during the fifth week, the brain divides into repeating segments called neuromeres.[65][71] In the hindbrain these are known as rhombomeres.[72]
A characteristic of the brain is the cortical folding known as gyrification. For just over five months of prenatal development the cortex is smooth. By the gestational age of 24 weeks, the wrinkled morphology showing the fissures that begin to mark out the lobes of the brain is evident.[73] Why the cortex wrinkles and folds is not well-understood, but gyrification has been linked to intelligence and neurological disorders, and a number of gyrification theories have been proposed.[73] These theories include those based on mechanical buckling,[74][18] axonal tension,[75] and differential tangential expansion.[74] What is clear is that gyrification is not a random process, but rather a complex developmentally predetermined process which generates patterns of folds that are consistent between individuals and most species.[74][76]
The first groove to appear in the fourth month is the lateral cerebral fossa.[68] The expanding caudal end of the hemisphere has to curve over in a forward direction to fit into the restricted space. This covers the fossa and turns it into a much deeper ridge known as the lateral sulcus and this marks out the temporal lobe.[68] By the sixth month other sulci have formed that demarcate the frontal, parietal, and occipital lobes.[68] A gene present in the human genome (ARHGAP11B) may play a major role in gyrification and encephalisation.[77]
0 notes
Text
Brainstem
-- connects the brain to the spinal cord
-- controls most necessary basic activities
-- has three major parts
Parts of the Brainstem -- midbrain = controls some reflexes -- pons = regulates breathing -- medulla oblongata = connects the brain to the spinal cord; controls most other necessary functions like heart function and swallowing
Patreon | Ko-fi
#studyblr#notes#medblr#medical notes#med notes#anatomy and physiology#neurology#biology#neurology notes#biology notes#bio#bio notes#anatomy and physiology notes#anatomy#physiology#anatomy notes#physiology notes#brainstem#pons#midbrain#medulla oblongata
2 notes
·
View notes
Text
READINGS - Handbook of Art Therapy / Chapter 2
Malchiodi, Cathy A. “Art Therapy and the Brain.” Handbook of Art Therapy, edited by Cathy A Malchiodi, Guilford Press, 2012, pp. 17-26.
NOTES + QUOTES:
“Art therapy has historically resisted an association with science and has favoured a more art-based stance in its philosophy and practice” (Malchiodi 17).
“As science learns more about the connection between emotions and health, stress and disease, and the brain and the immune systems, art therapy is discovering new frontiers for the use of imagery and art expression in treatment” (Malchiodi 17).
“Damasio (1994), Sapolsky (2004), and Ramachandran (1999, 2005), among others, have described the neurological and physiological phenomena related to memory, how images are conceptualized, and how they affect the brain and body” (Malchiodi 17).
“… have broadened our understanding of how the brain, human physiology, and emotions are intricately intertwined; the importance of early attachment on neurological functions throughout life; and the impact of trauma on memory” (Malchiodi 17).
“Images and image formation, whether mental images or those drawn on paper, are important in all art therapy practice because through art making clients are invited to reframe how they feel, respond to an event or experience, and work on emotional and behavioural change” (Malchiodi 18).
“Finally, art making is an experience that can simultaneously engage many parts of the brain including the cortical (symbolizing, decision making, and planning), the limbic (affect and emotion), and the midbrain/brainstem (sensory and kinaesthetic systems)” (Malchiodi 20).
“Additionally, depending on the course of art therapy, individuals may be also asked to talk about their art, tapping the left hemisphere’s language centers, connecting words to experiences that may be nonverbal (right hemisphere) (Malchiodi, 2008)” (Malchiodi 20).
“In other words, according to Damasio (2000), our bodies respond to mental images as if they are reality. He also notes that images are not just visual and include all sensory modalities: auditory, olfactory, gustatory, and somatosensory (touch, muscular, temperature, paint, visceral, and vestibular senses)” (Malchiodi 20).
“Because the core of traumatic experiences is physiological, the expression and processing of sensory memories of the traumatic even are essential to successful intervention and resolution (Schore, 2003). Art is a natural sensory mode of expression because it involves touch, smell and other senses within the experience” (Malchiodi 21).
“Art expression may help to bridge the implicit (sensory) and explicit (declarative) memories of a stressful event by facilitating the creation of a narrative through which the person can explore certain memories and why they are so upsetting” (Malchiodi 21).
“In art therapy, relational aspects include the presence of art media; anticipation of art making; learning what paint, clay or other materials can do; and receiving materials and assistance from the therapist. These are experiences that emphasize interaction through experiential, tactile, and visual exchanges, not just verbal communication, between the client and the therapist” (Malchiodi 22).
“In brief, the positive enjoyment found in drawing, painting, making a ceramic pot, woodworking, knitting, and other creative activities, if experienced on a regular basis, can improve mood in a fashion similar to the chemical changes produced by an effective antidepressant” (Malchiodi 24).
0 notes
Text
READINGS - Handbook of Art Therapy / Chapter 2
Malchiodi, Cathy A. "Art Therapy and the Brain." Handbook of Art Therapy, edited by Cathy A Malchiodi, Guilford Press, 2012, pp. 17-26.
NOTES + QUOTES:
"Art therapy has historically resisted an association with science and has favoured a more art-based stance in its philosophy and practice" (Malchiodi 17).
"As science learns more about the connection between emotions and health, stress and disease, and the brain and the immune systems, art therapy is discovering new frontiers for the use of imagery and art expression in treatment" (Malchiodi 17).
"Damasio (1994), Sapolsky (2004), and Ramachandran (1999, 2005), among others, have described the neurological and physiological phenomena related to memory, how images are conceptualized, and how they affect the brain and body" (Malchiodi 17).
"... have broadened our understanding of how the brain, human physiology, and emotions are intricately intertwined; the importance of early attachment on neurological functions throughout life; and the impact of trauma on memory" (Malchiodi 17).
"Images and image formation, whether mental images or those drawn on paper, are important in all art therapy practice because through art making clients are invited to reframe how they feel, respond to an event or experience, and work on emotional and behavioural change" (Malchiodi 18).
"Finally, art making is an experience that can simultaneously engage many parts of the brain including the cortical (symbolizing, decision making, and planning), the limbic (affect and emotion), and the midbrain/brainstem (sensory and kinaesthetic systems)" (Malchiodi 20).
"Additionally, depending on the course of art therapy, individuals may be also asked to talk about their art, tapping the left hemisphere's language centers, connecting words to experiences that may be nonverbal (right hemisphere) (Malchiodi, 2008)" (Malchiodi 20).
"In other words, according to Damasio (2000), our bodies respond to mental images as if they are reality. He also notes that images are not just visual and include all sensory modalities: auditory, olfactory, gustatory, and somatosensory (touch, muscular, temperature, paint, visceral, and vestibular senses)" (Malchiodi 20).
"Because the core of traumatic experiences is physiological, the expression and processing of sensory memories of the traumatic even are essential to successful intervention and resolution (Schore, 2003). Art is a natural sensory mode of expression because it involves touch, smell and other senses within the experience" (Malchiodi 21).
"Art expression may help to bridge the implicit (sensory) and explicit (declarative) memories of a stressful event by facilitating the creation of a narrative through which the person can explore certain memories and why they are so upsetting" (Malchiodi 21).
"In art therapy, relational aspects include the presence of art media; anticipation of art making; learning what paint, clay or other materials can do; and receiving materials and assistance from the therapist. These are experiences that emphasize interaction through experiential, tactile, and visual exchanges, not just verbal communication, between the client and the therapist" (Malchiodi 22).
"In brief, the positive enjoyment found in drawing, painting, making a ceramic pot, woodworking, knitting, and other creative activities, if experienced on a regular basis, can improve mood in a fashion similar to the chemical changes produced by an effective antidepressant" (Malchiodi 24).
0 notes
Photo
Corticobulbar fibres- The lower part of the face receives UMN fibres from the opposite side alone while the upper part of the face and all other motor cranial nerves get bilateral innervation For discussion of this image follow ‘Clinical neurology with KD’ podcast episode one -Approach to weakness, in Apple podcast, Spotify or Google podcast. Full notes are available on the neurologyteachingclub.com website The corticobulbar fibres arise from the lower third of the motor homunculus. They descend in corona radiata and genu of the internal capsule to reach the brainstem. In the midbrain, it is in the medial part of the cerebral peduncle. In the basis pontis, the corticobulbar fibres are intermixed with the corticospinal tract. All motor cranial nerves receive corticobulbar fibres from the bilateral motor cortex except the lower part of the face. The lower part of the face gets corticobulbar fibres only from the contralateral motor cortex. That is why the lower part of the opposite face alone is affected in lesions involving the motor cortex, corona radiata or internal capsule. The other cranial nerves are spared as they get 50% of their fibres from the unaffected side. So a patient with a right internal capsule lesion will have left hemiplegia with left upper motor neuron facial palsy as the lower face gets its upper motor neuron only from the opposite side. The left lower part of the face alone is affected, and the facial palsy is on the same side of hemiplegia. The facial deviation is to the opposite side of hemiplegia. The eye closure will be normal as the upper part has bilateral representation. All other motor cranial nerves lose 50% of their upper motor innervation, but they will be asymptomatic as the rest 50% takes up the function. #clinicalneurologywithkd #neurologyteachingclub #NTC #neurology #neurosciences #neuro #clinicalneurology #medicine #clinicalmedicine #kdpodcast #mbbs #medicos #doctors #neuroanatomy #casediscussion #medicinecase #casepresentation #medicineresidents #residency #neuroimages #NEET #finalmbbs #approachtohemiplegiapodcast #mcq #neetpg #uppermotorneuron #corticospinaltract #pyramidaltract #corticobulbartract #umnfacial https://www.instagram.com/p/CWPUQ87vtVK/?utm_medium=tumblr
#clinicalneurologywithkd#neurologyteachingclub#ntc#neurology#neurosciences#neuro#clinicalneurology#medicine#clinicalmedicine#kdpodcast#mbbs#medicos#doctors#neuroanatomy#casediscussion#medicinecase#casepresentation#medicineresidents#residency#neuroimages#neet#finalmbbs#approachtohemiplegiapodcast#mcq#neetpg#uppermotorneuron#corticospinaltract#pyramidaltract#corticobulbartract#umnfacial
0 notes
Text
Sequitura’s Psychology Notes bc study hours
===PART 1: Early Psychology===
Nativism vs. empiricism - nature vs. nurture, basically. One theory was mainly promoted by philosophers - that people are hardcoded with certain traits from birth that cannot be developed or changed. The other end of the spectrum is empiricism, the theory that the mind starts as a blank slate affected by experiences over time.(edited)
Introspection vs. experiments - different methods early psychologists used to find out about the mind. Introspection was when subjects described their experiences out loud to scientists and was championed by Freud. It was discovered that no one’s description of their own mental experiences match 100% of the time, but this method did turn into early psychotherapy. Experiments are more objective ways to discover how the mind works via behavior. Skinner was one of the earliest experimentalists (and a decrier of psychoanalysis as scientific evidence.)
Localization of function (phrenology) - it is an old idea that different parts of the brain have different functions. Previously, it was believed that phrenology (analyzing the shape of the skull) could determine what strengths and weaknesses a person had, but these days, more scientific methods are used (such as brainscans and case studies of patients with brain damage.)
Other fields of psychology - 1. Evolution. There are some skills every species has right at birth, meaning that some skills were developed by a species' ancestors and aren't learned. 2. Comparative. Comparing how different species have similar psychological traits. For example, if a chimpanzee watches a human swinging from something, the parts of the chimp's brain that control motor control will show more activity. 3. Computational. Treating the brain as a computational organ. Treats it as having certain rules that it follows consistently. Sometimes theorizes how far a machine can get before it's considered living.
===PART 2: Neuroscience===
I already talked about neurons with James, so I'm not going to go into them.
How action potential works -
1 The cell starts polarized at around -70mV. There is more Na+ inside the cell and more K+ outside the cell.
2 A stimulous Na+ channels open, causing Na+ to flow out of the cell and depolarize it (around +40mV)
3 K+ channels open, causing K+ to rush in (and Na+ channels to close), repolarizing the cell. The cell becomes hyperpolarized at around -90mV.
4 Protein pumps open, using ATP to force Na+ back in the cell and K+ back out. The cell returns to its resting state of around -70mV.
Frontal lobe - thinking, motor control, speech (toward the front)
Parietal lobe - touch, orientation of body parts in reference to each other (on top)
Occipital lobe - sight, visual interpretation (on back)
Temporal lobe - audio processing, language comprehension, memory (toward the bottom)
Brainstem - involuntary functions such as bladder control, breathing, heart rate, blood pressure, digestion, and balance
Midbrain - controls movement, sleep, alertness and temperature limbic system (deal with emotions and memory) hippocampus - learning/memory amygdala - emotions
===Part 3: Sensation + Perception===
uhh I don't really feel like going over this. Already did and think I remember everything. Lateral inhibition is the ability for an excited neuron to cause neighboring neurons to become less excited, though. Enhances edges.
===Part 4: Learning===
Habituation - you get used to something the more it happens.
Sensitization - you get more sensitive to something the more it happens.
CS, UCS, CR, UCR - stands for four different variables in classical conditioning: conditioned stimulus, unconditioned stimulus, conditioned response, unconditioned response. An example is getting a dog to salivate at the sound of a bell. 1. UCS - food UCR - salivation 2. CS - bell no response 3. CS + UCS - bell + food UCR - salivation 4. CS - bell CR - salivation
Reinforcement - a stimulus meant to incentivize a reason to do/not do something Punishment - a stimulus meant to make doing/not doing something less appealing
classical conditioning - getting a response to something that would normally have no response dishabituation - getting a response to return more quickly than it would if you were being introduced to it for the first time
rewards and punishments are more effective if they occur every time the behavior occurs, rather than once every couple of times (schedule of reward/punishment)
0 notes
Text
Brainstem Midbrain Notes
#MendelsLaws#HereditaryTraits#ScienceOfInheritance#MendelianInheritance#GeneticDiscoveries#BiologyLessons#MendelsPrinciples#GeneticsEducation#HereditaryScience#Brainstem Midbrain Notes
0 notes
Text
Cerebellum (Ataxia)
1. Speech.
2. Point-to-Point Reaching, Rapid Alternating Movements.
3. Gait.
Note:
Unidrectional Nystagmus suggests peripheral cause (Vestibular).
Multidirectional or Up / Down Nystagmus suggests central cause (Midbrain, Cerebellum).
Problems with the Cranial Nerves (Double Vision, Facial Movements, Swallowing) suggest that there is a problem in the Brainstem, outside the cerebellum.
- III and IV (Midbrain).
- VI and VII (Pons).
- XI and X (Medulla).
If there is no Cranial Nerve involvement then it is unlikely that the Brainstem is involved, but there cerebellum can still be involved.
Weakness suggest that the cause of the Ataxia is outside the cerebellum in the Corticospinal Tract that has cerebellar pathways.
https://medskl.com/module/index/ataxia-gait
0 notes
Text
Gradblr Challenge, Day 11 (Right?)
3.16.17–1:15am Hey all, I actually managed to do a lot of studying for my Mammalian Neurobiology exam! My process is to make mininotes–typed notes that contain a page’s worth of info, plus any pertinent pictures. For an anatomy class, that’s usually a lot, and there’s usually a lot of terminology to go with it, so for each unit (or region) I generally have to make two or three pages. These always include sample questions, areas to review, and terms that should be familiar, which are all kindly supplied by the professor. So I’ve made mininotes for the forebrain areas (5 pages 😥), midbrain (1 page), pons (1 page), medulla and brainstem (2 pages) and an overview of CNS divisions (2 pages). Tomorrow I hope to do the cranial nerves, which will likely be a LOT of pages, and the cerebellum. No picture today, but since I’ll be doing electrophysiology tomorrow I can post lots of science-y pictures then! Glad to be productive today. @gradblrchallenge
4 notes
·
View notes
Text

Patreon | Ko-fi
#studyblr#notes#medblr#medical notes#med notes#divisions of the brain#neurology#brain#brain notes#brain divisions#brain divisions notes#brain division notes#cerebellum#corpus callosum#pons#midbrain#medulla#medulla oblongata#brainstem
3 notes
·
View notes
Photo

New Post has been published on http://centersforrehabservices.com/opiate-addiction-treatment/
OPIATE ADDICTION TREATMENT
WHAT ARE OPIATES?
The origin of opium and its use can be traced back to as far as 3400 BC in Mesopotamia; the region now called Iran and Iraq. It was a very profiting trade commodity at the period. From there it spread to Egypt and Asia. There is a wide range of drugs described as opiates. They were described as valiums but now as a term for abused drugs. They are naturally occurring drugs containing nitrogen compounds which are physiologically classified as poisonous’ Codeine and morphine are quick examples of opiate drugs. These are drugs used for the treatment of unmanageable pain. An opioid is a term or word used for drugs that are opioid receptors. Note, narcotic is derived from the Greek word for stupor. It was a term for the description of the medications for sleep impairment. Recently, it is used as a legal term to describe drugs that are abused.
HOW OPIOIDS ACT
In simple terms, opioids activate opioid receptors which are transported through the central nervous system (CNS) in the nuclei of the tractus solitaries, thalamus, substantiagelatinosa (PG), a periaqueductal gray area (PAG) and the cerebral cortex of the spinal cord. They are stimulated by endogenous peptides (endorphins, dynorphins, and enkephalins) whichare produced in response to noxious stimulation
These receptors are identified as:
Note, they are named based on their prototype agonists using Greek letters.
MOP (mu (µ) opioid peptide receptor). It’s an agonist receptor found primarily in the brain stem and media thalamus. They are known to be responsible for supraspinal analgesia, sedation, euphoria, decreased gastrointestinal motility, physical dependence, and respiratory depression.
KOP (kappa (k) opioid peptide receptor). It’s an agonist ketocyclazocine. They are found primarily in the limbic and other diencephalic areas, brainstem and spinal cord. They are identified to be responsible for spinal analgesia, dyspnea dependence, sedation, dysphoria and respiratory depression.
DOP (delta (ò) opioid peptide receptor). It’s an agonist delta-alanine-leucine-enkephaline. They are found more in the brain. Scientists are still studying their effects. They are assumed to be responsible for psychomimetic and dysphoric effects.
Sigma (Sigma (ó) agonist N-ally Inno metazocine). They are responsible or psychomimetic effects, dysphoria, and stress-induced depression. Sigma has not been considered as an opioid receptor anymore. It is still the target site for phencyclidine (PCP) and its analogs.
NOP (nociceptinorphanin FQ peptide receptor). They were identified in 1985 to have stronghyperalgesic effects. They have little semblance to the MU receptors. They are antagonists. They are likely to be antidepressants and analgesics.
CLASSES
There are four chemical classes of opioids:
Phenanthrenes are the prototypical opioids. The presenceof a 6-hydroxyl may be associated with ahigher incidence of nausea and hallucinations.For example, morphine and codeine (both with6-hydroxyl groups) are associated with more nauseathan hydromorphone and oxycodone (whichdo not have 6-hydroxyl groups). Opioids in thiscluster include morphine, codeine, hydromorphone, levorphanol, oxycodone, hydrocodone, oxymorphone, buprenorphine, nalbuphine, andbutorphanol.
Benzomorphans have only pentazocine as a member of this class. It is an agonist/antagonist with a high incidence of dysphoria.
Phenylpiperidines include fentanyl, alfentanil, sufentanil, and meperidine. Fentanyl has the highest affinity for the mu receptor.
Diphenylmethanesinclude propoxyphene and methadone.
Call Us Now!We're Here To Help 24/7 866-945-3402
EFFECTS OF OPIATES
Note, opiates ( drugs) occur as agonists, partial agonists, and antagonist. However, the most of the commonly acquired opioids are agonists. Agonist act by stimulating the opioid receptors: The Central Nervous System (CNS), Cardiovascular System, The Respiratory System, Gastrointestinal System, Endocrine System
They act as sedatives, resulting indrowsiness and loss of concentration.
As analgesic, effective in the relief of pain
It causes restlessness and a sense of ecstasy
It can cause hallucinations
Profuse sweating
Restlessness
Joint pains
Nausea and vomiting
Increase level of salivating
Arthritis
Irritability
Vomiting and diarrhea
Chest pain and excessive heart beat or racing.
Call Us Now!We're Here To Help 24/7 866-945-3402
METHOD OF INTAKE
There so many drugs classified as opiate drugs with the broader name of opium. Codeine, morphine are opioids, heroin is another derivative of the family. Opiates can either be taking by smoking, snorted, by injection, and it can also be inhaled (chasing). It all depends on the user’s convenient method; they all produce the same effect. However, the injection has the fastest effect.
HOW DOES ADDICTION START?
Numerous factors, both individual and the immediate environment, influence whether a particular person who experiments with opioid drugs will continue taking them long enough to become dependent or addicted. For some individuals, the capability to provide intense feelings of pleasure is a critical reason for staying on the drug. When heroin, oxycodone, or any other opiate travels through the bloodstream to the brain, the chemicals attach to specialized proteins, called mu-opioid receptors, on the surfaces of opiate-sensitive neurons(brain cells). The linkage of these chemicals with the receptors triggers the same biochemical brain processes that reward people with feelings of pleasure when they engage in activities that promote basic life functions, such as eating and sex. This process is how addiction starts, and this is also the challenge when treating patients or drug addicts to isolate the natural occurring feeling from the drug induced feeling.Opioids are prescribed therapeutically to relieve pain, but when opioids activate these reward processes in the absence of significant pain, they can motivate repeated use of the drug simply for pleasure. Note, this is when an addict induces the feeling by the utilization of these drugs.
One of the brain circuits that are activated by opioids is the mesolimbic (midbrain) reward system. This system generates signals in a part of the brain called the ventral tegmental area (VTA) that result in the release of the chemical dopamine (DA) in another part of the brain, the nucleus accumbens (NAc). This release of DA into the NAc causes feelings of pleasure. Other areas of the brain create a lasting record or memory that associates these euphoric feelings with the circumstances and theenvironment in which they occur. The craving for more of the drugs is excited by these longing.
Note, in the early stages of abuse, the opioid’s stimulation of the brain’s reward system is a primary reason that some people take drugs repeatedly. However, the compulsion to use opioids builds over time to extend beyond a mere drive for pleasure. This increased urge is related to tolerance and dependence.
ADVERSE EFFECTS OF ADDICTION
Addiction to opioids has substantialadverseconsequences like every other narcotic, not just on the individual but at the family level, social and the general public. Drug addiction mostly is associated with the continuous and uncontrollable use of drugsto the point of fatality. There is a wide range of drugs that fall under the opioids classification. These drugs occur naturally and are synthetic or semi-synthetic. Some of which are morphine and codeine. These drugs could be obtained clinically and used under medical supervision for the cure and management of different levels of unmanageable pain. Opioids mimic the natural opioid substances produced by the brain thus making the abuser glued and dependent on the introduced substance. The brain embraces theseintroducedelements not recognizing them as artificial agents. The after effect is what the addict suffers: physical and emotional changes and imbalance, mental and psychological malfunction.
FAMILY
Neglect of family and responsibilities
Battering and abuse of wife and children
Divorce
Neglect of domestic responsibilities
Aggression
Tiresome care for addicted family members
Financial losses
Stigma
Untimely death
SOCIAL
A rise in the number of HIV and Hepatitis cases as a result of theuse of infected syringes by adrug addict, especially when they take it in a group or share the fix.
A rise in the rate of crime linked to citizens that are influenced by drugs. Also stealing to raise money for the next fix.
A rise in the rate of mental cases and premature death
A toll on budgetary allocation for treatment and rehabilitation.
TREATMENT
Statistics show that the abuse of opiate drugs is on the rise daily. This daily rise has given concern to stakeholders in the society, especially in the health sector. Treatment for opiate addiction is costly and energy sapping, on this note, medical caregivers have advocated that the treatment should not be given free of charge. Against this development, the American Society of Interventional Pain Physicians (ASIPP) and the American Psychiatric Association (APA) in a communiqué have given guidelines for the treatment of addicts.
One of the methods for the treatment of opiates is the Methadone Maintenance Treatment developed in the 1930s by a German scientist for the treatment of addicts under rehabilitation. It ‘s hard to treatdrug addicts without them still craving for it, a dose of the MMT satisfies the patient and also serves more as a curative therapy. The treatment can span up to fifteen years, but the beauty of it is that it does not have identifiednegative effect on the patient.
Treatment with methadone requires a daily dosage of the drug; this implies that the patient visits the center daily to be administered with the daily intake. There are cases of stable and compliant patients being trusted to take home some doses, thus reducing the stress of daily visits to the center
AFTER TREATMENT EFFECTS
Feelings of being stigmatized
Turning to a recluse
Finding it difficult to reintegrate into the society
Becoming a responsibility and burden to the family and the community at large
Call Us Now!We're Here To Help 24/7 866-945-3402
#heroin treatment#inpatient drug rehab#opiate addiction#Inpatient Drug Rehab#Substance Abuse Assessment
0 notes
Text
Biopsy-Proven Brain Metastases from Prostate Adenocarcinoma on 68Ga PSMA PET/CT: Case Series and Review of the Literature-Juniper publishers

Abstract
Prostate cancer brain metastases are extremely rare and typically occur at a late stage in the course of the disease with poor prognosis. However, the incidence is rising as novel antiandrogens and radionuclide therapy prolong survival and change the natural course of the disease. Surveillance imaging of the brain is not the current standard of care. We present two cases of patients who had brain metastases from prostate adenocarcinoma initially detected on prostate specific membrane antigen (PSMA) positron emission tomography/computed tomography (PET/CT) and also provide a review of the epidemiology, pathogenesis, imaging features, pathogenesis and current treatment modalities of prostate cancer brain metastases. Our patient with multiple brain metastases is still alive three and a half years post initial diagnosis after being successfully treated with surgery, androgen deprivation therapy and radiosurgery. This is the longest survival time of any patient with multiple brain metastases and systemic disease. We postulate that overall survival will increase with earlier detection and treatment of brain metastases from a prostate cancer primary and that scanning vertex to mid-thigh should be standard practice with PSMA PET imaging.
Keywords: Brain metastasis; Prostate cancer; Neuroradiology; Ga68PSMA PET/CT
Abbrevations: PCa: Prostate Cancer; Ga: Gallium; PSMA: Prostate Specific Membrane Antigen; PET/CT: Positron Emission Tomography/Computed Tomography; MRI: Magnetic Resonance Imaging; SRS: Stereotactic Radiosurgery; Gy: Gray; PSA: Prostate Specific Antigen; PAP: Prostatic Acid Phosphatase; ADT: Androgen Deprivation Therapy
Case 1
A neurologically intact 66-year-old man presented for a Ga68 prostate specific membrane antigen (PSMA) positron emission tomography (PET) scan due to a rising prostate specific antigen (PSA) level of 7.4ng/ml thirteen years after a successful radical prostatectomy for a Gleason 7 prostate cancer (PCa).
PSMA demonstrated an unusual distribution of disease with intensely PSMA avid foci in an enlarged mediastinal lymph node, within small lung nodules and in two PSMA avid brain foci within the right temporal and left occipital lobes. Brain MRI revealed a large 6.5cm complex enhancing lesion in the right temporal lobe compressing the temporal horn and the body of the right lateral ventricle. The cystic component of the mass showed no restricted diffusion. A second 1.1cm lesion was noted in the left occipital lobe superior to the ventricular trigone with peripherally restricted diffusion and increased diffusibility centrally (Figure 1).
The patient underwent a right temporal craniotomy and excision with gross total resection achieved (Figure 2). Histology confirmed metastatic prostatic adenocarcinoma with positive immunohistochemistry for PAP and PSA. The patient received adjuvant stereotactic radiosurgery (SRS) to the right temporal lobe cavity, left parietal lobe mass and hormonal manipulation with androgen deprivation therapy (ADT).
Nine months postoperatively, the patient remained clinically well with no neurological symptomology and undetectable PSA with ongoing ADT. MRI brain confirmed no recurrence in the right temporal lobe cavity but an increase in the size of the left occipital lobe lesion. PSMA PET/CT demonstrated mild persistent increased PSMA avidity in a solitary focus in the left occipital lobe. Complete metabolic response at all other metastatic sites with no new disease found. The patient was treated with further SRS (14Gy in a single fraction) to the region of PSMA avidity in the left occipital lobe. Three and a half years post operatively, he remains well with good disease control.
Case 2
A 71-year-old man with metastatic castration resistant prostate cancer previously treated with external beam radiotherapy, ADT, radium 223 therapy and docetaxel presented with a three-week history of increasing confusion and ataxia.
MRI brain revealed a well circumscribed 2.4 x 2.0cm cystic, enhancing mass in the left para-median thalamus and midbrain compressing the cerebral aqueduct and five other lesions throughout the bilateral cerebellar hemispheres. The thalamic cyst was biopsied and aspirated, but his symptoms persisted. Histologic examination confirmed metastatic prostatic adenocarcinoma. He was treated with whole-brain radiotherapy but passed away two months following radiation treatment.
Introduction
Intraparenchymal metastases from a prostate adenocarcinoma primary is rare and only occur in an estimated 0.6-1.9% of patients [1-3]. However, the incidence is increasing as novel antiandrogens and radionuclide therapy prolong survival and change the natural course of the disease.
On the 1st of May 2018, a comprehensive literature search examining peer-reviewed, English language articles from 1982 to 2018 was performed on multiple databases, yielding 1286 articles. These articles were reviewed and selected for studies that met the following inclusion criteria;
a) Patients with intraparenchymal metastases from prostate adenocarcinoma proven either on antemortem resection or stereotactic biopsy and
b) Metastases confirmed on CT or MR brain imaging.
Additional relevant studies were also searched manually in the reference lists of identified studies and by using the “related articles” tool in PubMed. Patients with dural or skull-based tumours extending into the brain were excluded from the review. We found 1286 articles and considered 29 articles eligible. A total of 47 men with brain metastases from prostate adenocarcinoma origin confirmed on radiological imaging and antemortem biopsy was thus identified in the literature (including our 2 cases reported here).
Discussion
Epidemiology
For patients with brain parenchymal metastases from prostate adenocarcinoma of any subtype, the mean at diagnosis of brain metastasis was 66.3 years (range, 48-88 years) and the median age was 66 years.
35 of the 47 men had known prostate adenocarcinoma at the time of their cerebral metastasis diagnosis whilst for 12 men this was the initial presentation of their primary prostate tumour. The mean age at diagnosis of brain metastasis for men with known prostate cancer (PCa) was 65.5 years (range, 48- 88 years). In patients with cerebral metastases as the initial presentation of their primary tumour, the mean age of brain metastasis diagnosis was 66.4 years (range, 56-75 years).
Hatzoglou et al. [4] study of 7 patients with biopsy proven brain metastasis from prostate adenocarcinoma was not included as we were unable to differentiate the patients’ mean age at diagnosis of brain metastasis from other patients in their cohort who had biopsy from other sites of distant disease confirming metastatic PCa.
Timing and symptoms
Patients with metastatic disease to the brain developed disease an average of 4.4 years (range, 3 days to 13 years) after the initial diagnosis of their PCa. New therapies increasing overall survival time gives the tumour enough time to develop brain metastases, that is usually a late event of the disease [5,6].
Neurological manifestations on presentation varied according to the anatomical site with most metastases situated in arterial border zones and the junction between the cortex and subcortical white matter. The majority of patients (95.7%) presented with overlapping neurological signs and symptoms. 22 patients presented with headache, the most common presenting complaint at diagnosis followed by motor weakness (n=16), ataxia (n=13), confusion (n=10), seizures (n=8), speech impairment (n=7) and visual field disturbances(n=4). In the two neurologically asymptomatic patients, the brain metastases were diagnosed on surveillance imaging after a rise in PSA.
In 11 patients, the brain was the sole site of distant metastasis [7-16]. In patients with metastatic disease, the most common extra prostatic sites were bone (61.7%), lungs (26.4%), liver (16.1%) and lymph nodes (13%).
Lesion characteristics
A total of 73 metastases was seen in the 47 patients. 39 patients (83%) had a solitary brain metastasis whereas the other 8 patients (17%) had multiple metastases. Four patients (8.5%) had two metastases and 4 patients (8.5%) had 6 or more brain metastases.
The frontal lobe (n=15) and the cerebellum (n=15) were the most prevalent sites of metastases followed by the parietal (n=14), temporal (n=12) and occipital (n=6) lobes. One patient had a solitary metastasis in the temporo-parietal lobe and one case involved the parieto-occipital lobe. Five patients had 6 metastases in the brainstem. Two cases involved the cavernous sinus and one patient (our case) had a metastasis in the thalamus. 49 patients (67.1%) had parenchymal metastases located in the cerebral hemispheres which corresponds to what is known about the distribution of parenchymal metastases from other primary cancers.
15 patients (20.5%) with brain metastases from PCa origin were found in the cerebellum and only 8.2% of metastases were found in the brainstem. This distribution of intracranial metastases is similar to metastases from breast, lung and melanoma where approximately 15% of metastases are found in the cerebellum. Brainstem are uncommon sites especially for solitary lesions and account for <1% of all brain metastases. Interestingly 3 patients (4.1%) in our review of all the literature to date had solitary metastases in the brainstem [8-9,17].
31 patients (68.9%) had one or more metastatic brain lesions in the supratentorial compartment [7,9-13,16,18-25], 11 patients (24.4%) in the infratentorial compartment [8- 10,13-14,17,23,26] and 3 patients (6.7%) in both compartments [27-29]. Two patients with lesions in the cavernous sinus were excluded.
Intraparenchymal cerebral metastases from prostate adenocarcinoma are rare and multiple metastases without systemic disease is exceedingly uncommon. In the largest case series to date of 16280 patients with brain metastases from prostate cancer by Tremont-Lukats et al. [1] only 103 patients (0.6%) had parenchymal brain metastases. In most cases the metastases were singular (86%) and supratentorial (76%). Only 3 patients (2.9%) of the cohort had both infratentorial and supratentorial metastases.
A more recent case series by Hatzoglou et al. [4] found 10 patients (47.6%) of their cohort had both supratentorial and infratentorial metastases. This is significantly higher than other case series to date and is likely due to MRI images from Hatzoglou’s case series being reviewed by a neuroradiologist versus some cases in our review being limited to only single slice images of patients’ CT or MRI which limits our ability to ascertain the distribution of lesions outside of our two cases.
Gross pathology
Parenchymal metastases are generally round, discrete lesions. The metastases in our review had variable peritumoural oedema, necrosis and mass. Non-uniformity in the spatial distribution of the parenchymal metastases suggests that vulnerability to metastases differ according to its anatomical location. Our review found parenchymal metastases from PCa had a predilection for the frontal lobe and cerebellum (n=15, 20.5%) which is consistent with other large case series which found 17-25% of metastases from PCa were found in the cerebellum [1,4]. Unlike melanoma, renal cell carcinoma and choriocarcinoma which are particularly prone to developing intratumoural haemorrhages, brain metastases from PCa was not found to have intratumoural haemorrhage on imaging or histopathology. All of the patients included in our review had biopsy confirmed adenocarcinoma with positive immunohistochemical staining for PSA and PAP.
Imaging features
The cerebral metastases had highly variable imaging appearance and was difficult to differentiate from metastases originating from other primary tumour sites. Eight patients in our review only had CT imaging of their cerebral metastases [7,9,18-21,26]. On non-contrast CT imaging, most metastases were isodense to slightly hypodense relative to grey matter. The majority of parenchymal metastases enhanced strongly following contrast administration.
On axial T1-weighted MRI, most of the parenchymal lesions were mildly hypointense. On post gadolinium imaging, nearly all of the non-haemorrhagic metastases showed enhancement with patterns of disease varying from solid uniform enhancement to nodular or ring like lesions. FLAIR imaging also demonstrated significant variability in lesion cellularity, presence of haemorrhage and amount of peritumoural oedema. On diffusion weighted imaging (DWI), well differentiated adenocarcinoma metastases generally showed no diffusion restriction compared to highly cellular metastases which demonstrated diffusion restriction.
Cystic intraparenchymal metastases from PCa are rare with only eight cases documented in literature to date, including our two patients [11,19,22-23,27,30]. Five patients had solitary cystic lesions and three patients had multiple cystic lesions. Intralesional restricted diffusion was present in both our patients.
Unlike true intraparenchymal cerebral metastases of prostate adenocarcinoma origin, prostate cancer is the second most common primary after breast cancer to metastasize to the dura [5] and poses a radiological diagnostic challenge especially when it presents as a solitary lesion which can be mistaken for a meningioma as up to 44% of prostate metastases have a dural tail [6,31,32]. Distinguishing between the two lesions is important due to the poor prognosis of intracranial metastatic PCa and the potential for conservative management versus active treatment if a radiological diagnosis is made. The incidence of brain metastases in the most recent series of 16,280 prostate cancer patients is reported to be around 0.63% [1] which is less than the 1-2.4% incidence reported in autoptic series [3,33-34] with the incidence of brain metastases being detected in the pre-MRI era the same as in the post MRI era [1]. We postulate that advances in MR imaging such as triple dose gadolinium and or 3.0Tesla (T) MRIs have led to earlier detection of metastases in PCa patients which allow earlier treatment and thus decrease the potential for further extraprostatic spread.
Ga68 PSMA PET/CT imaging appears to have superseded F18 FDG PET/CT, CT and MR imaging not only in the staging of PCa but also in the detection of PSMA-avid disease and is increasingly being used for restaging recurrent PCa. Our case demonstrates the importance of scanning from vertex to mid-thigh as albeit rare, PCa can metastasize to the brain and earlier detection and treatment correlates directly with improved survival time and quality of life.
Treatment
All of the patients included in our review underwent either surgical resection (n=37) or stereotactic biopsy (n=9) of their intracranial lesion which confirmed their diagnosis on histopathology. 31 patients (66%) underwent whole-brain irradiation; 22 patients had adjuvant whole-brain radiotherapy post-surgical resection of their lesion and 9 patients had whole-brain radiotherapy as their primary treatment. Three patients had stereotactic radiosurgery (SRS) to their lesion; 1 in conjunction with whole-brain radiotherapy post-surgical resection and 2 patients had SRS post-surgical resection of the main symptomatic lesion. 6 patients had trimodality treatment with surgical resection, whole-brain radiotherapy and ADT [10,13,18-19,24-26]. One patient had surgical resection of the dominant metastasis, SRS to another metastasis and also received concurrent androgen deprivation therapy (our case).
Surgical resection with adjuvant whole-brain radiotherapy has been the Gold standard for treating solitary metastasis in the brain. This combined strategy has been evaluated in randomised controlled trials to significantly prolong survival, alleviate neurological symptoms and reduce the risk of recurrence when compared with surgical resection or whole-brain radiotherapy alone [35].
ADT have also been found to bring both symptomatic and radiological improvement [36-37] leading not only to an increase in the overall survival time but also an improved quality of life and is thus used in both the curative and palliative settings in patients with prostate adenocarcinoma.
Prognosis
For the 41 patients who had documented survival times from the initial detection of their brain metastases, the mean survival time was 13.7 months (range, 3 days to 7 years). The patient who had the longest survival time of 7 years in our series had a solitary metastasis in the cerebellum that was resected en bloc and also underwent a bilateral orchiectomy. Previous case series have reported a median duration from diagnosis to death of between 3.5 to 31 months [1,38-39]. Patients without systemic disease were less likely to have brain lesions [4]. Patients with brain metastasis as the sole site of extra-prostatic disease had a mean overall survival time of 24.6 months (range, 1month to 7 years) compared to 13.4 months (range, 3 days to 5 years) in patients with systemic disease.
We postulate that advances in imaging such as Ga68 PSMA PET/CT, triple dose gadolinium and 3.0 Tesla (T) MRIs have led to earlier detection of metastases in PCa patients which allow the patient to be treated earlier thus decreasing the potential for further extraprostatic spread and the increased incidence of patients presenting with brain metastases as the sole site of disease from their primary PCa.
Solitary brain metastasis has better prognosis than patients with multiple brain metastases. The overall survival time for patients with a solitary brain metastasis was 14.3 compared to 7.2 months (range, 3 days to 29 months) for patients with multiple metastases. Our patient had the longest survival time for a patient with multiple brain metastases of three years likely due to low volume disease in the brain post-surgical resection and exceptional response to ADT at the extracranial metastatic sites.
The mean overall survival time for patients who had surgical resection was 20.3months (range, 3 weeks to 7 years). The mean overall survival time for patients who had stereotactic biopsies was considerably shorter at 6.25 months (range, 1month to 2years). This latter cohort of patients either had disease in the brainstem that was unresectable [8,17,21] or had multiple cerebral metastases [13,16,28].
Prior to the introduction of docetaxel in 2002, the incidence of prostatic brain metastasis from 1994 to 2002 was 0.8%. In the post-docetaxel era (2002-2011), this incidence had increased to 2.8%. This represents a 239% increase in the frequency of brain metastases from PCa between the two observation periods [40]. As the appearance of parenchymal metastases usually occurs in the late phase of the disease process it appears that the increase in frequency may actually reflect a gain in overall survival. In general patients are living longer with brain metastases in the context of PCa due to advances in imaging ability, systemic treatment and increased surveillance.
Pathogenesis
PCa rarely metastasizes to the brain with the incidence in large case series ranging from 0.63 to 1.1% [2,41] which suggests that the brain parenchyma is resistant to the establishment of metastatic foci by prostate carcinoma cells.
Currently the pathogenesis of cerebral metastases from PCa is unknown however in summary there are two main mechanisms postulated;
a) Single step spread via Batson’s paravertebral venous plexus draining the prostate. Low pressure in the large venous plexus allowing Valsalva maneuver to generate enough pressure to reverse blood flow from the IVC to the venous plexus, avoiding the lung and reaching the CNS. This mechanism however does not explain the absence of vertebral metastases and
b) Multi step haematogenous spread where secondary seeding of tumour cells to the brain occur from a primary metastatic focus involving the lungs or bones with brain metastasis usually a late event in the course of prostate cancer.
Haematogenous metastases have a special predilection for arterial border zones and the junction between the cortex and subcortical white matter. PSA is a sensitive indicator of the presence of disease however serum levels of PSA did not correlate to the development of brain metastases in our cases which is consistent with what is found in other case series [11,22].
Conclusion
Intraparenchymal spread of prostate cancer should be considered in men over the age of 60 years as a treatable cause of gradual neurological deterioration especially if a cranial malignancy or hyperostosis is found. The incidence of intraparenchymal brain metastasis is only expected to increase due to the longer life expectancy of patients with prostate adenocarcinoma with novel therapies. Patients undergoing Ga68-PSMA PET/CT for staging of PCa or when there is a PSA rise should be scanned from vertex to mid-thigh as albeit rare, prostate cancer brain metastases is a not to be missed differential in this particular group of patients.
Consent
The patients provided informed consent to the publication of their data, de-identified PET and MRI scans. No ethics approval through an institutional committee on human research was required.
To know more about Open Access Journal of Head Neck & Spine Surgery please click on:
https://juniperpublishers.com/jhnss/index.php
To know more about Open access Journals Publishers please click on : Juniper Publishers
To know more about juniper publishers: https://juniperpublishers.business.site/
#Head and Neck Surgery Journal#Journal of Head Neck & Spine Surgery#Journal of Spine Surgery#Juniper Publishers#Open Access Journals
0 notes