#GERD specialist
Text
Get effective strategies to combat Gastroesophageal Reflux Disease (GERD) with expert guidance from Dr. Vikrant Kale. Learn essential tips and treatments for managing GERD symptoms and improving your quality of life.
0 notes
Text
Kaizen Acidity Care is the one-stop solution for all types of acid reflux, Acidity, GERD treatment, and GERD Surgery in Pune. Dr. Vikrant Kale (Medical Gastroenterologist) and Dr. Samrat Jankar (Surgical Gastroenterologist) are the most expert and qualified gastroenterologists in Pune who provides the best treatment for acid reflux.
#GERD treatment#GERD specialist#GERD surgery#Acid Reflux treatment#gastroenterologist#Stomach Specialist#Laparoscopic Surgeon
0 notes
Text
I love male nurses.
I have never had a shitty male nurse.
#he looked like a thinner karrion that was going gray#and upon hearing half my problem was immediately like 'yeah might be time to get them out screw that'#and told me he got his out during his residency 10 years ago and it was awful but beat dealing with shit constantly#but then thr pa was like :))) i dont see anything:))) just up ur gerd pill again :)))) maybe itll help:)))#and gave me a referral but wants me to wait to call. urgh.#just. let me. see. the fucking. specialist. ffs#they said my tonsils were big BEFORE ANY OF THIS SHIT EVER STARTED#and ya'll like :)))))))) this is normal!!! :)))))
5 notes
·
View notes
Text
Acid Reflux Treatment Dubai | Gerd Specialist In Dubai - Dr Balaji
DESCRIPTION
If you seek Acid Reflux Treatment in Dubai, consult Dr Balaji Nagammapudur, a Gerd Specialist in Dubai. Experience expert care for effective Acid Reflux Treatment. Contact us now.
#bariatric surgeon dubai
Dr. Balaji Nagammapudur | Upper GI Surgeon in Dubai | Weight Loss Surgery Dubai | Bariatric Surgery In Dubai
+971-501015597
+44-7404056272
0 notes
Text

gastroenterology specialist:-
Gastroenterology Specialist at Apex Multispeciality Hospital delivers expert care for digestive disorders. With advanced diagnostics and personalized treatment plans, our specialists ensure comprehensive management of conditions like GERD, IBS, and more. Trust our experienced team for compassionate care and effective solutions. Visit us for top-tier gastroenterological services and reclaim your digestive health today.
#Gastroenterology Specialist at Apex Multispeciality Hospital delivers expert care for digestive disorders. With advanced diagnostics and per#our specialists ensure comprehensive management of conditions like GERD#IBS#and more. Trust our experienced team for compassionate care and effective solutions. Visit us for top-tier gastroenterological services and#Gastroenterology Specialist
0 notes
Text
औषधेविना अॅसिडिटी दूर करण्यासाठी 5 बेस्ट उपाय - डॉ सम्राट जानकर
0 notes
Text
Explore the reasons why tracking the frequency of heartburn occurrences is essential for proactive health management. Uncover insights into potential triggers, effective symptom management, and the overall improvement of digestive well-being. Take charge of your heartburn experience with informed tracking and personalized care strategies.
#heartburn insights#heartburn tracking#frequency of heartburn#managing heartburn#digestive health#heartburn symptom#gerd#gastroenterologist#gstroenterologist specialist#acid reflux#celiac disease#gastroesophageal reflux disease#colonoscopy#irritable bowel syndrome#hepatitis
0 notes
Text
youtube
What are the causes of abdominal pain and digestive disorders? A description of its treatment, Watch the full Video
#heartburn treatment in Coimbatore#best treatment for gerd in Coimbatore#gerd specialist in Coimbatore#Youtube
0 notes
Text
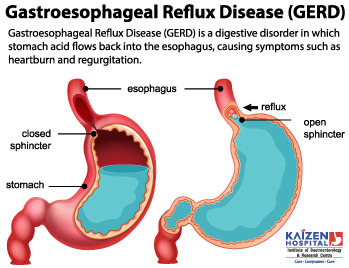
When acid reflux back from stomach to esophagus due to lax valve between esophagus and stomach and produce damage to the inner lining of esophagus called GERD (Gastro Esophageal Reflux Disease).
What are the Symptoms of GERD (Gastro Esophageal Reflux Disease)?
Heartburn: this is the most common symptom of GERD (Gastro Esophageal Reflux Disease). This is a burning feeling which rises from the upper abdomen or lower chest up towards the neck.
Pain abdomen or chest pain, dyspepsia
Some uncommon symptoms of GERD: these may occur and can make the diagnosis difficult.
Recurrent cough
Asthma
Wheeze
Sore throat
Hoarseness of voice
Tooth and gum problem
Severe chest pain
Investigations Required are GERD (Gastro Esophageal Reflux Disease)?
Tests are not usually necessary if you have typical symptoms. You need to have upper GI endoscopy to confirm and establish the extent of damage. There are GERD where endoscopy may be negative. There are other investigations; like 24 hour pH analysis which is highly sensitive test to confirm GERD. Other tests like manometry, chest x ray, ECG might be needed.
What can we do to reduce the GERD (Gastro Esophageal Reflux Disease) symptoms?
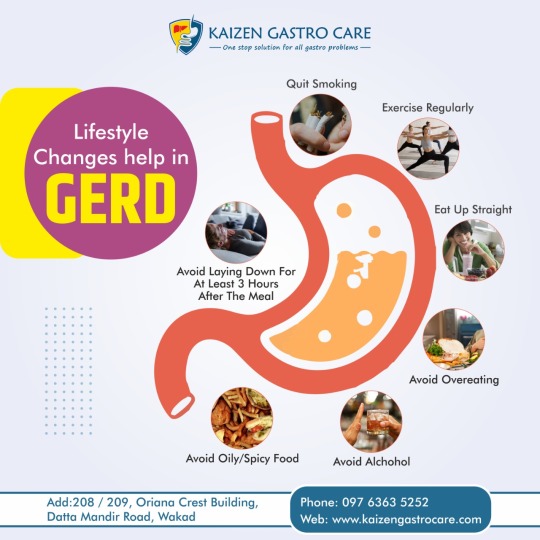
The following lifestyle changes may help to reduce the reflux:
Stop smoking
Some foods and drinks – Foods and drinks those might be responsible for reflux are peppermints, chocolate, spicy foods, hot drinks, coffee, and alcoholic drinks. Also, avoiding large-volume meals may help. Certain medications like pain killers may worsen the symptoms
Weight loss – If you are overweight, losing some weight may help to improve the symptoms.
Posture – Lying down or bending forward may increase reflux. Wearing tight belts may increase intraabdominal pressure and increases the reflux.
Bedtime
Avoid sleeping within 2 – 3 hours of meal.
Raise head end of the bed by 1- 20 cm.
What are the treatment options for GERD (Gastro Esophageal Reflux Disease)?
Medications – antacids, H2 blockers, proton pump inhibitors, prokinetic agents
Surgical treatment – laparoscopic fundoplication
Choice of treatment depends on severity and duration of symptoms, presence or absence of complications.
Are there any complications from GERD (Gastro Esophageal Reflux Disease)?
Scarring and stricture of esophagus, lung, gum and tooth problem, Barrett\’s esophagus and sometimes cancer of the esophagus.
#best gastroenterology hospital india#best doctor gastroenterologist in ahmedabad#best gastro doctor in india#best gastro specialist in ahmedabad#best gastro doctor in ahmedabad#ahmedabad gastrology doctor#best doctor gastrology in india#best gastro liver hospital in india#best gastro hospital in india#ahmedabad gastro hospital#gerd#GERD (Gastro Esophageal Reflux Disease) symptoms#GERD (Gastro Esophageal Reflux Disease) Causes#GERD (Gastro Esophageal Reflux Disease)
0 notes
Text
- ED trigger warning -
Being skinny ruined my life. If you’re thin and think to yourself, “why don’t fat people just lose weight?” Please read this
I was the “ideal fat” in the sense that I did everything skinny people wanted me to do. I tried every diet in the book. I exercised regularly. I worked with doctors and dietitians to figure out the best way to lose weight. But nothing worked. I did everything “right” to lose weight, and my weight stayed the same
But the thin people in my life kept telling me that I wouldn’t be happy, attractive, healthy, etc. until I lost weight. So, heartbroken, I came to the conclusion that anorexia was the only option left. It felt safer than bariatric surgery, and was obviously much more affordable
I became the perfect anorexic. 700 cal a day or less, except once a week I allowed myself 1400 cal. For reference, my body required at least 2800 to maintain weight, and at least 1800 to keep my organs and stuff fully functioning. Still, 700 a day, I persisted because everyone in my life told me weight loss was all that mattered. If dieting didn’t work, anorexia had to
And it did. My weight dropped all the way down to 110 pounds. I was skinny - underweight, even - in all sense of the word. The people in my life saw it as a miracle. The ultimate success story. My mother, my “friends,” my doctors, they all congratulated me on my accomplishment
When I confessed my eating disorder to my doctor, he told me, “that’s not the best way to go about it, but I’m glad you lost the weight.” My mother took pictures of me and sent them to relatives to brag
Okay, great. I was skinny. I did what I set out to do. But there were severe consequences
The most obvious was my joint pain doubled, maybe even tripled, to the point that I couldn’t leave the house without a wheelchair
I also developed several health complications, including fatty liver disease and extremely painful GERD. I had to see a handful of specialists and get an endoscopy because of severe stomach pain
My partner, who was the only person who saw my weight loss for what it was (a horrible thing that only happened because of an eating disorder), convinced me to enter a recovery program
For nearly a year, I relearned how to feed myself. I ate everything I was told to eat, nothing more and nothing less. My diet was 100% in the hands of somebody else
And I gained back every pound I has lost. All of the work to become thin went right out the window. It was proven to me that thinness and health were incompatible with my body. If I wanted to be thin, I had to forgo my physical and mental well-being. And vise-versa
Prior to the anorexia, I never once struggled with binge eating. I was naturally an intuitive eater, and I did a good job of having a well rounded diet. After the anorexia, after recovery, I developed a binge eating disorder. I had spent so long starving myself, that my brain and body got stuck in survival mode, desperate to consume any and all calories out of fear that I might starve again. To this day I struggle with binge eating
I did everything thin people wanted of me. I dieted. I exercised. And when all else failed, I starved myself. Now I have liver disease, stomach issues, and BED. Not to mention the loads of mental issues that accumulated as a result of my weight loss journey. During the throes of my anorexia, I had to be hospitalized for suicidal ideation
When you tell fat people to “just lose weight” you are suggesting they give themselves illnesses for which treatments are not always effective. You are asking fat people to destroy their stomachs and livers. When a fat person loses so much weight that they become skinny, they are likely giving up so much of their health in efforts to be treated like a human being
If you’re thin, do your part. Treat fat people like people before we tear our bodies apart
5K notes
·
View notes
Text
Explore the Difference between GERD and heartburn with Dr. Vikrant Kale. Gain insights into the distinctions, symptoms, and effective management strategies for a healthier, heartburn-free life. Trust Dr. Kale's expertise to navigate the intricacies of gastrointestinal health.
0 notes
Text
Gastroesophageal reflux disease occurs when stomach acid repeatedly flows back into the tube connecting your mouth and stomach.
Kaizen Gastro Care specialist Dr. Vikrant Kale explores the symptoms and causes & of lifestyle changes to help with GERD. If you notice any symptoms of GERD, then book an appointment today with our best GERD specialist in Pune. Get the Right Treatment For GERD!!! Visit: https://www.kaizengastrocare.com/gerd-surgery-in-pune/
#GERD treatment#GERD surgery#GERD specialist#gastroenterologist#Laparoscopic Surgeon#acidity treatment#stomach specialist
0 notes
Text
#best hernia surgeon in jabalpur#hernia specialist in jabalpur#laparoscopic hernia specialist in jabalpur#gallbladder surgeon in jabalpur#GERD surgery in Jabalpur#hernia surgery#gallbladder surgery in jabalpur#laparoscopic surgery#laparoscopic surgeon in jabalpur
0 notes
Note
oh wow I am so sorry to hear about your daughter having EOE - that sounds really rough. How do you navigate that?
At this point, with a lot of flailing.
It took 3.5 years to even get her properly diagnosed, not through lack of trying-- it's just a hard thing to differentiate, and the specialists that can actually do the test are dealing with a huge number of patients so they're always backed up. We're lucky: we live only an hour from the state children's hospital where they can do the diagnostic procedures, and it has a dedicated EOE specialty clinic that's one of the best in the country. It still takes 2 months to get an appointment as an established patient, and it took even longer to get her in on the initial referral. We're also lucky that she was able to explain to us what she was experiencing in a way that a doctor could take seriously and act on, and we're lucky that her primary care doctor did so.
But generally speaking, things suck spectacularly for pediatric EOE and GERD patients right now, at least in the US. The best medicine for treating it is omeprazole (prilosec), and there was exactly one manufacturer that made it in a suspension that small children could take. Well, that manufacturer decided it wasn't profitable enough, so they quit making it altogether. So now the next best, lansoprazole (prevacid), is on national back order for months because every child that was on the other one is now needing to switch.
So my daughter is currently on the next next best thing, because it was that or nothing, and it's just not working great for her. It keeps her from the worst of the pain, but she's back to not wanting to eat anything but bagels, one specific brand of cereal, and string cheese.
Back when she was officially diagnosed, her doctor gave us the option of going on a super dose of PPI meds, jumping straight to the steroids, or doing a full elimination diet with a nutritionist. For a kid, none of those options are great.
The PPIs reduce absorption of nutrients, which are already few and far between for a growing person with only a few tolerated foods. The steroids may have effects on a growing liver and kidneys, and also make you more prone to fungal infections and upper respiratory illnesses. Both have to be routinely dose-adjusted because the child is growing constantly, but you have to get an official weight/height check at the specialist to do so, which is always backed up. Then the elimination diet is...well, it's hard, to put it mildly, and it takes a really long time because of how delayed the reactions can be. Plus when you already don't like eating and only have a few 'safe foods', it's hard to cut back. Most people with EOE also have more than one trigger, so you have to eliminate a ton of things and hope you get them all, and you can't be on any medication while you're doing it because you have to be able to identify the point at which symptoms get better and then return.
In short, all the options suck.
We eventually decided on trying to get it under control enough with the meds to hopefully expand the foods she was willing to eat, in preparation for doing the elimination diet. It was working. Then the forced medication switch blew that all up. So we're just gonna grit our teeth and go with the elimination diet unless her specialist has another option for us.
But aside from that, it's been a lot of phone tag and appointment waiting, and a lot of readjusting the way we look at food and eating.
For her, whatever she will eat is a win. We've taken pressure off her to try new things. We still offer it, but we don't press if she's not feeling up to it. Reducing stress around the concept of trying new foods is super important, because she's already up against the stress of wondering whether it'll 'get stuck' or feel yucky or make 'the fires' worse.
We've also had to make sure we don't fall into the trap of trying to dictate how much she eats and when. Unless a meal is coming within the half hour, we let her have a snack when she's hungry-- wait too long, and she's in pain. Plus we want her to kind of train herself to respond to those hunger cues because her appetite can get so drastically reduced at times, every instance of her listening to an 'I'm hungry' is a win.
We also had to abandon the idea of the 'perfectly' balanced diet. Proteins are a struggle for her. Leafy greens are a struggle. So are other calcium containing foods like dairy and dairy alternatives. She really only likes carbs, mostly bread and fruit. But it's not like she can help it. Nobody purposefully restricts their diet just to be difficult-- a "picky eater" is someone who is struggling and needs accommodation, not judgement.
So we let her eat what she will eat, and work to find options that can get her the stuff she needs. Protein bars are a big hit with her right now, for example. A better texture than meat, they come in 'treat' flavors, and there are options that don't have all the added sugar that's gonna trigger the acid flareup. We make sure we get enriched flour and bread products so she gets at least some iron. We pick varieties that have added protein and calcium. We get juice with added vitamins and minerals. We stock the pantry with things that cater to her capabilities and needs wherever the two overlap. The goal is nutrition, whatever form that takes and whatever it looks like right now. Getting it "right" will come later. For now, we just need her to be comfortable with food and to learn how to work with her body.
This has also meant teaching her about nutrition, so we can help her take charge of her body's needs and help us think of ways to meet them. That's hard for a 3 year old, but there's a show called Storybots on Netflix, and they have a great episode on nutrition called "Why can't I eat dessert all the time?" Super accessible for kids, and has a catchy song describing macronutrient categories and why we need lots of different kinds of food, not just one kind. It was a perfect starting point, and we just kept at the explanations. Like when we would eat an apple with breakfast, we'd talk about how it has Vitamin C to help her cells be strong, fiber to help her tummy and intestines work well, and carbohydrates to help her have energy. Every time we try a new food, we talk about what's in it to help her body. That includes things like chips and cake--we're big on the concept of "all food has value, it's just some has more than others, so we eat the most of those."
So now, when she's had a "just bread" day we remind her that her body needs more than just carbs, and we can't get all our protein, fats, vitamins, and minerals from bread, so we should probably have something else too. 9 times out of 10, she'll add something to her request, like some blueberries or carrots. She might not eat a ton of it, but she tries, and that's what counts.
I know this is a mile long and probably way more than you were asking, but it's just one of those things that I have a lot to say about. I could talk all day about accessible eating and nutrition, as well as Going Off on our current medical system in the US, so if anyone has further questions, feel free to reach out.
35 notes
·
View notes
Text
Managing GERD involves making lifestyle and dietary changes to reduce the occurrence of symptoms. One of the most important aspects of managing GERD is identifying and avoiding trigger foods and beverages that can exacerbate the condition. In this blog, we'll explore some common triggers for GERD and provide tips on which foods and beverages to avoid.
#acid reflux treatment in Coimbatore#heartburn treatment in Coimbatore#best treatment for gerd in Coimbatore#best treatment for acid reflux in Coimbatore#gerd specialist in Coimbatore
0 notes