#Patient Flow Analysis Software
Explore tagged Tumblr posts
Text
Comprehending Medical Coding and Billing: Your Essential Guide to Healthcare Revenue Management
Understanding Medical Coding and Billing: Your Essential guide to Healthcare Revenue Management
In today’s fast-paced healthcare industry, efficient revenue cycle management is crucial for the financial health of medical practices and hospitals alike. At the core of this process are two vital components: medical coding and medical billing. Despite their importance, manny healthcare providers and patients remain unfamiliar wiht how these systems work and why they matter. This thorough guide aims to demystify medical coding and billing, highlighting their importance for healthcare revenue management, and providing practical tips to optimize their use.
What Is Medical Coding?
Medical coding involves translating healthcare diagnoses, procedures, medical services, and equipment into standardized alphanumeric codes. These codes are essential for billing purposes, insurance claims, and statistical analysis. The coding process ensures accuracy in documentation and facilitates a smooth interaction between healthcare providers, insurers, and government agencies.
Types of Medical Codes
ICD Codes (International Classification of Diseases): Used to document diagnoses and reasons for patient visits. For example, ICD-10-CM codes like E11.9 for Type 2 Diabetes Mellitus without complications.
CPT Codes (Current Procedural Terminology): Describe medical procedures and services provided by healthcare professionals. For example, 99213 for outpatient office visit of low to moderate complexity.
HCPCS Codes (Healthcare Common Procedure Coding System): Include supplies,equipment,and non-physician services not covered by CPT.As an example,ambulance services and durable medical equipment.
The Medical billing Process
Medical billing is the process of submitting and following up on claims with health insurance companies to receive payment for services rendered by healthcare providers.Its a critical component of revenue cycle management that directly impacts cash flow.
Steps in Medical Billing
Patient registration and insurance verification: Collect accurate patient details and confirm insurance coverage.
Charge capture: Record all billable services, procedures, and supplies used during a patient visit.
Coding and claim generation: Apply appropriate medical codes to charges to create a claim.
Claim submission: Send claims electronically or via paper to insurance companies or payers.
Claim adjudication: Insurance reviews the claim, approves, denies, or requests additional data.
Payment posting and follow-up: Record payments and pursue unpaid claims through appeals if necessary.
Why Accurate Medical coding and Billing Are critical
Proper coding and billing are essential for several reasons:
Maximize revenue: Accurate and complete codes ensure healthcare providers receive appropriate reimbursement.
Reduce claim denials: Precise coding minimizes the chances of claims being rejected or delayed.
Ensure compliance: Correct coding helps avoid legal issues and penalties related to coding violations or fraud.
Improve patient experience: Transparent billing and accurate insurance claims streamline the billing process and reduce patient confusion.
Benefits of Efficient Medical Coding and Billing
Benefits
Description
Increased Revenue
Optimized coding captures all billable services, boosting income.
Fewer Denials
Accurate claims reduce rejection and rework, speeding up payments.
Better compliance
Proper coding adheres to regulations,avoiding legal issues.
Enhanced Data Analytics
Reliable data supports strategic planning and performance improvement.
Practical Tips for Effective Medical Coding & Billing
Invest in Training: Regularly update your coding staff on the latest CPT, ICD, and HCPCS codes.
Use Advanced Software: Utilize reliable Electronic Health Record (EHR) and billing software with built-in coding support.
Perform Regular Audits: Periodically review coding and billing practices to identify discrepancies or errors.
Verify insurance Coverage: Confirm patient coverage details before procedures to prevent claim issues.
Stay Compliant: Keep up with payer policies,coding updates,and regulatory changes.
Case Study: Improving Revenue Through Accurate Coding
Dr. Smith’s Family Practice experienced frequent claim rejections, leading to delayed payments and revenue loss. By implementing comprehensive staff training, upgrading to an integrated billing software, and conducting monthly audits, Dr. Smith’s practice increased claim approval rates from 75% to 95%. The result was a 20% increase in monthly revenue within six months.This case underscores the importance of precise coding and vigilant billing practices for healthcare revenue enhancement.
First-Hand experience: Insights from a medical Billing Specialist
As a billing specialist, I’ve seen firsthand how meticulous coding and billing practices can transform a practice’s financial stability. Consistent updates on coding guidelines, thorough documentation, and proactive communication with payers are key. When coding is accurate, the claims process becomes smoother, payments are faster, and patient satisfaction improves. Remember, in healthcare revenue management, attention to detail makes all the difference.
Conclusion
Understanding medical coding and billing is fundamental for effective healthcare revenue management. Accurate coding guarantees proper reimbursement, reduces claim rejections, and ensures compliance. Meanwhile, streamlined billing processes enhance cash flow and improve the overall financial health of healthcare providers. Investing in education, technology, and best practices in coding and billing can considerably impact your practice’s success. Whether your a healthcare professional or a patient, grasping these concepts fosters transparency, efficiency, and confidence in the healthcare system.
Empower your practice today by mastering the essentials of medical coding and billing-your pathway to optimized revenue cycle management and better patient care!
https://medicalbillingcertificationprograms.org/comprehending-medical-coding-and-billing-your-essential-guide-to-healthcare-revenue-management/
0 notes
Text
The Ultimate Guide to Complete Medical Billing: Streamline Your Healthcare Revenue heute
The Ultimate Guide too complete Medical Billing: Streamline Your Healthcare Revenue heute
Welcome to the definitive guide on medical billing! Whether you’re a healthcare provider looking to optimize your revenue cycle or an administrator aiming to reduce billing errors, understanding the ins and outs of complete medical billing is essential. In this article, you’ll discover practical tips, benefits, and real-world case studies to help you streamline your healthcare revenue today.
Introduction to medical Billing: Why It Matters
Medical billing is a critical component of the healthcare industry. it involves translating healthcare services into standardized codes, submitting claims to insurance companies, and ensuring healthcare providers receive fair reimbursement. Proper medical billing management enhances cash flow, reduces claim denials, and ensures compliance with healthcare regulations. Mastering complete medical billing is thus vital for the sustainability and growth of any medical practice or healthcare institution.
Understanding the Components of Complete Medical Billing
Complete medical billing encompasses multiple stages, from patient registration to payment processing. Here’s a breakdown of its key components:
Patient Registration: Collecting accurate personal and insurance information
Insurance Verification: Confirming patient coverage before services are rendered
coding and Documentation: Assigning accurate ICD-10, CPT, and HCPCS codes
claim Submission: Sending electronic or paper claims to payers
Payment Posting: Recording payments and adjustments
Follow-Up & Denial Management: Resolving rejected claims and appeals
Reporting & Analysis: Monitoring financial performance and optimizing processes
Key Benefits of Efficient Medical Billing
Implementing streamlined medical billing processes offers numerous advantages:
increased revenue: Faster and accurate reimbursements
Reduced Claim Denials: Minimizing errors and appeals
Improved Cash Flow: Consistent revenue cycle management
Regulatory Compliance: staying compliant with HIPAA and other laws
Operational Efficiency: Saving time and reducing administrative burden
Practical Tips to Streamline your Medical Billing Process
1. Invest in Advanced Medical Billing Software
Using reliable billing software can automate many tasks, reduce errors, and provide real-time reporting.Look for features like integrated coding, claim scrubbing, and electronic submissions.
2. Verify Insurance Details prior to Service
Pre-authorization and verification can prevent denied claims due to missing coverage information, saving time and resources.
3.Train Your Staff Regularly
Keeping your team updated on coding guidelines, regulations, and claim submission protocols ensures accuracy and compliance.
4. Implement Denial Management Practices
Develop a system for tracking denials, analyzing patterns, and appealing rejections promptly to recover lost revenue.
5. Maintain Clear Documentation
Proper and thorough documentation of services provided supports accurate coding and reduces claim rejections.
Case study: How a Small Clinic Increased Revenue by 30%
Challenge
Solution
outcome
High claim denial rate and slow reimbursements
Implemented an advanced billing system with denial management and staff training
Revenues increased by 30% within six months, and claim denials decreased by 65%
first-Hand Experience: Tips from Industry Professionals
Many healthcare providers share that integrating automated billing solutions and focusing on continuous education of billing staff are key to success. One billing supervisor states, “Regular audits and proactive denial management are game-changers for improving cash flow.”
Conclusion: Achieve Healthcare Revenue Optimization Today
Efficient medical billing is a cornerstone of financial stability in the healthcare sector. By understanding its components, embracing technological solutions, and following practical best practices, healthcare providers can considerably enhance revenue, reduce administrative burdens, and deliver better patient care. Start implementing these strategies today to streamline your medical billing process and take control of your healthcare revenue.
Additional Resources & Next Steps
Explore reputable medical billing software options
Attend industry webinars on coding updates
Consult with billing experts for tailored solutions
© 2024 Your Healthcare Solutions. All rights reserved.
https://medicalcodingandbillingclasses.net/the-ultimate-guide-to-complete-medical-billing-streamline-your-healthcare-revenue-heute/
0 notes
Text
Improving Your Practice: Top Medical Billing Solutions in Phoenix for 2023
Streamlining Your Practice: Top Medical Billing Solutions in phoenix for 2023
In an era where efficiency and accuracy are pivotal for healthcare providers, selecting the right medical billing solution can drastically enhance your practice’s revenue cycle. As we step into 2023, Phoenix offers a variety of medical billing solutions tailored to meet the unique needs of healthcare professionals. In this article,we will explore the top options available,their benefits,and tips for implementation,ensuring your practice remains efficient and profitable.
Why Choose a Medical Billing Solution?
Medical billing plays a crucial role in the healthcare revenue cycle. An efficient medical billing solution can:
Reduce claim denials and rejections
Improve cash flow and revenue collection
Automate time-consuming processes
Enhance patient satisfaction through clear billing
Top Medical Billing Solutions in phoenix for 2023
1. MedBillingExperts
MedBillingExperts offers extensive billing services tailored to providers of all sizes. Their services include:
end-to-end billing solutions
Denial management
Custom reporting and analytics
By leveraging advanced technology, MedBillingExperts significantly reduces billing errors and improves turnaround times.
2. iMarque Solutions
iMarque Solutions focuses on outsourcing billing services with a strong emphasis on account management. Their advantages include:
24/7 support and availability
Flexible pricing models
Integration with various EHR systems
Practices utilizing iMarque have experienced seamless operations and improved cash flow within weeks.
3. AdvancedMD
AdvancedMD is an all-in-one solution offering cloud-based medical billing and practice management. Key features include:
Automated billing processes
Patient scheduling and management tools
Integrated telehealth solutions
Their platform has been recognized for improving patient engagement and operational efficiency.
4. Kareo
Kareo provides a user-amiable platform designed for self-reliant practices. Notable features include:
Comprehensive billing and collections tools
Client relationship management (CRM) features
Robust reporting capabilities
Kareo’s intuitive platform simplifies the billing process, allowing providers to focus on patient care.
5. MD Tech Solutions
MD Tech Solutions specializes in providing tailored billing services specifically for small to medium-sized practices. their offerings include:
Personalized billing plans
Detailed revenue cycle analysis
Continuous support and consultation services
Clients have reported better management of accounts receivables thanks to MD Tech’s dedicated support.
Benefits of Using Medical Billing Solutions
Utilizing an effective medical billing solution can yield numerous benefits:
Increased efficiency through automation
Greater accuracy in coding and billing
Timely collections leading to improved cash flow
reduced administrative workload for staff
Practical tips for Implementing a Medical Billing Solution
When transitioning to a new medical billing system, consider these practical tips:
Assess Your needs: Determine the specific needs of your practice before selecting a solution.
Engage Your Team: Include staff in decision-making to ensure the chosen solution meets their workflow requirements.
Test the Software: Take advantage of free trials to evaluate the software’s features and compatibility with existing systems.
Training and Support: Ensure that your staff receives adequate training and that an ongoing support channel is available.
Case Studies: Success Stories from phoenix Medical Practices
Case Study 1: Family health Associates
After implementing MedBillingExperts, Family Health Associates reduced their claim denial rate by 30%. The practice attributes this success to the comprehensive training provided to their staff and the advanced analytics tools offered by the billing solution.
Case Study 2: Phoenix Orthopedics
Phoenix Orthopedics saw a 25% increase in cash flow within three months of integrating AdvancedMD.This was largely due to the software’s automation features that streamlined the billing process, allowing physicians to spend more time with patients.
First-Hand Experience: Transitioning to a new Billing Solution
As a healthcare provider in Phoenix, transitioning to a new medical billing solution can seem intimidating.However, many practices have reported positive outcomes. For instance,one local clinic shared that the seamless integration of Kareo into their existing EHR system was a game-changer. They noted improved patient satisfaction and a more balanced workload amongst their billing staff.
Conclusion
Choosing the right medical billing solution is vital for the financial health of your practice. The top medical billing services available in Phoenix for 2023 offer a blend of automation, customization, and support tailored to your unique needs. By adopting these solutions, you can streamline your operations, enhance patient experiences, and ultimately drive your practice towards greater success. Take the time to evaluate your options, utilize the tips provided, and become part of the growing number of Phoenix healthcare providers thriving in an efficient billing environment.
youtube
https://medicalbillingcodingcourses.net/improving-your-practice-top-medical-billing-solutions-in-phoenix-for-2023/
0 notes
Text
North America Sepsis Diagnostics Market Global Size, Share, Trends, Application Analysis and Growth by Forecast (2021-2028)
The North America sepsis diagnostics market is expected to grow from US$ 279.06 million in 2021 to US$ 513.33 million by 2028. It is estimated to record a CAGR of 9.1% from 2021 to 2028.
High Incidence of Sepsis due to Increasing Nosocomial Infections Drives North America Sepsis Diagnostics Market
Infection is the root cause of sepsis, and it primarily affects immunocompromised people, such as those taking chemotherapy, having a splenectomy, and suffering from AIDS and diabetes and other chronic illnesses. Among several types of infections, nosocomial infections are the primary cause of morbidity and mortality among hospitalized patients. According to the "2020 National and State Healthcare-Associated Infections Progress Report" published by the Centers for Disease Control and Prevention (CDC) in 2021, the US recorded about 24%, 35%, and 15% increase in central line-associated bloodstream infections, ventilator-associated events, and Methicillin-resistant Staphylococcus aureus (MRSA) bacteremia, respectively, between 2019 and 2020.
As per a report published by the Global Sepsis Alliance (GSA), nearly 26 million people develop sepsis every year, and approximately 8 million deaths are reported due to sepsis across the world. Thus, the rising bloodstream infections will increase the adoption of sepsis diagnostic products. Also, deaths are often a consequence of diarrheal diseases or lower respiratory infections. Most deaths can be prevented through early diagnosis and appropriate clinical management. Thus, the high incidence rate of sepsis is expected to boost the demand for sepsis diagnostic products, which would support the North America sepsis diagnostics market growth during the forecast period.
Download our Sample PDF Report
@ https://www.businessmarketinsights.com/sample/BMIRE00025664
North America Sepsis Diagnostics Strategic Insights
Strategic insights for the North America Sepsis Diagnostics provides data-driven analysis of the industry landscape, including current trends, key players, and regional nuances. These insights offer actionable recommendations, enabling readers to differentiate themselves from competitors by identifying untapped segments or developing unique value propositions. Leveraging data analytics, these insights help industry players anticipate the market shifts, whether investors, manufacturers, or other stakeholders. A future-oriented perspective is essential, helping stakeholders anticipate market shifts and position themselves for long-term success in this dynamic region. Ultimately, effective strategic insights empower readers to make informed decisions that drive profitability and achieve their business objectives within the market.
North America Sepsis Diagnostics Market Segmentation
North America Sepsis Diagnostics Market By Product
Instruments
Reagents and Assays
Blood Culture Media
Software
North America Sepsis Diagnostics Market By Technology
Molecular Diagnostics
By Flow Cytometry, Microfluidics, Immunoassay, Biomarkers, Microbiology)
North America Sepsis Diagnostics Market By Method
Automated Diagnostics and Conventional Diagnostics
North America Sepsis Diagnostics Market By Test Type
Point-of-Care Tests and Laboratory Tests
North America Sepsis Diagnostics Market Regions and Countries Covered
North America
US
Canada
Mexico
North America Sepsis Diagnostics Market leaders and key company profiles
Abbott
BD
bioMerieux SA
Danaher (Beckman Coulter)
F. HOFFMANN-LA ROCHE LTD.
Immunexpress Inc.
Luminex Corporation
T2 Biosystems, Inc.
THERMO FISHER SCIENTIFIC INC.
About Us:
Business Market Insights is a market research platform that provides subscription service for industry and company reports. Our research team has extensive professional expertise in domains such as Electronics & Semiconductor; Aerospace & Defense; Automotive & Transportation; Energy & Power; Healthcare; Manufacturing & Construction; Food & Beverages; Chemicals & Materials; and Technology, Media, & Telecommunications
0 notes
Text
Outsourcing Medical Billing with Real-Time Dashboards: Enhancing Transparency & Accountability

In a report published by Verified Market Research, the Revenue Cycle Management (RCM) software market stood at $105.18 billion in 2020 and is expected to reach a whopping $249.44 billion by 2028.
This growth is a significant change in the adoption of digital means by medical practices to enhance financial processes through outsourcing medical billing and coding services providers in India.
But it is more complicated than ever to manage the finances of a medical practice. Physicians have to balance many administrative duties with constant cash flow, effective billing, and prompt reimbursement. That is where real-time dashboards can step in to provide a streamlined, user-friendly interface that brings together vital revenue cycle performance metrics. When combined with outsourcing, dashboards deliver even more value by providing financial transparency, minimizing administrative burden, and enhancing accountability across the hospitals.
As a GPS provides real-time traffic information to reroute drivers, the dashboard also provides real-time views into claims status, revenue performance, coding errors, and more. It enables providers to identify bottlenecks, fix errors, and make data-driven decisions. This blog will discuss how real-time dashboards by outsourced medical billing and coding companies increase transparency and accountability.
How do Real-Time Dashboards improve Transparency & Accountability?
Real-time dashboards utilized by outsourcing medical billing and coding services providers in India are significant in providing increased transparency and accountability. The following are the most prominent tools incorporated into these dashboards that assist in the fulfillment of these objectives for medical practices:
1. Claim Tracking
Claim tracking is one of the most critical elements of real-time RCM dashboards. This platform allows providers to track claims from the point of submission to the payer till reimbursement or denial. Through software like AdvancedMD, medical billing and coding companies give real-time updates on claim status, including rejection, submission, adjudication, and payment. This degree of visibility equips healthcare professionals with the ability to correct as soon as delays or denials occur, thus keeping losses to a minimum while enhancing overall claim success rates.
2. Patient Billing
Patient billing software integrated into real-time dashboards makes financial interactions with patients more transparent and streamlined. With software such as Kareo, these tools enable the generation of correct invoices, monitor outstanding balances, and handle payment plans. Outsourcing offshore medical billing and coding services in India with the utilization of these tools guarantees the timely delivery of statements to patients, eliminating confusion and disputes. The tools also enhance cash flow through simple payment facilitation via online portals and automated reminders, adding accountability to patient collections.
3. Financial Reporting
Real-time dashboards include powerful financial reporting tools, like those of athenahealth, to create in-depth financial statements, performance reports, and trend analyses. Outsourcing companies use these reports to offer physicians real-time metrics for revenue, collection, aging AR, and more. These highly customizable reports enable practices to benchmark performance and detect trends, enabling rapid, well-informed decision-making. The availability of financial insights fosters complete transparency between the provider and the billing partner.
4. Revenue Analysis
Revenue analysis tools, such as those within eClinicalWorks, offer a deeper understanding of income sources, payer mix, procedure profitability, and reimbursement trends. Outsourced offshore medical billing and coding services in India use these tools to highlight areas where revenue is leaking or where reimbursements are suboptimal. Also, dashboards enable providers to take corrective measures, renegotiate contracts, or improve documentation practices by continuously monitoring these financial variables in real time. This will ultimately ensure financial accountability and maximize income for the healthcare practices.
5. Coding Assistance
Proper and accurate coding is the foundation of effective medical billing. Real-time dashboards with coding support tools, like DrChrono, assist coders and billers in assigning the proper codes by making intelligent recommendations, warning of mismatches, and verifying adherence to up-to-date guidelines. This tool is a dependency for outsourcing companies in order to minimize coding mistakes, which are one of the leading causes of claim denials and audits. Not only does this tool guarantee compliance, but it also builds trust by reducing the financial risks associated with incorrect coding.
6. Appointment Scheduling
Although often overlooked, appointment scheduling tools such as PracticeSuite are critical to billing productivity. Integrated into real-time dashboards, these tools coordinate provider calendars, avoid overlapping appointments, and document services and bills correctly. Moreover, outsourced billing staff use this data to cross-check visit information, check eligibility, and send claims on time. This coordination reduces billing errors and supports a seamless patient journey, reinforcing operational transparency.
Outsourcing to Info Hub Consultancy Services
With the healthcare sector increasingly becoming more data-driven and financially complicated, the demand for transparent, real-time, and effective revenue cycle management has never been higher. Real-time dashboards are the fundamental tools that deliver accurate, end-to-end financial information, maximize billing productivity, minimize regulatory risks, and aid in enhanced patient engagement. All these features, coupled with ease of integration with EHR systems, make the healthcare providers better placed to tackle the finance side of care provision.
Medical practices can gain access to the customizable dashboards by outsourcing to Info Hub Consultancy Services. Our trained medical billers and coders deliver quarterly performance reports that highlight areas for improvement and facilitate proactive decision-making. With cutting-edge analytics, our staff enables practices to thrive in value-based contracts as well as identify new sources of revenue while staying focused on patient care.
#Outsource Medical Billing#Medical Billing Company#Best Outsource Medical Billing and coding Company#Offshore Medical Billing and coding#Offshore Medical Billing Services India#Offshore Medical Billing Agency India#Offshore Medical Billing Company In India#Outsource Medical Billing Services Agency India#Offshore Medical Billing and Coding#Offshore Medical Billing and Coding Services#Offshore Medical Billing and Coding Agency#1 outsource medical billing services company india#top outsource medical billing company#cheap outsource mental health billing company
0 notes
Text
Tech Innovations Boosting DME Billing Processes

The Durable Medical Equipment (DME) billing process, traditionally marked by manual and often cumbersome steps, can significantly improve through various technological advancements. These innovations streamline workflows, reduce errors, and ensure faster and more accurate billing, ultimately benefiting both healthcare providers and patients. Here’s an in-depth look at the tech innovations revolutionizing DME billing.
Artificial Intelligence (AI)
Automated prior authorization leverages Artificial Intelligence (AI) to handle the process of benefits verification and obtaining prior authorizations. This technology interfaces with insurance systems to automatically check patient coverage details and secure the necessary approvals before services are rendered.
Impact:
Faster Patient Care: By automating the prior authorization process, patients can receive their DME more quickly. Traditional methods often involve significant wait times, delaying patient care. Automation significantly cuts down these delays.
Increased Efficiency: Reducing the need for manual paperwork and phone calls allows administrative staff to focus on more critical, value-added tasks. This not only boosts operational efficiency but also reduces administrative burdens.
Improved Accuracy: Automation reduces the likelihood of errors associated with manual data entry and communication. This ensures that authorizations are complete and accurate, preventing potential denials or delays in the DME billing process.
Electronic Health Records (EHR)
Electronic Health Records (EHR) are digital versions of patients’ paper charts. They store comprehensive patient information, including medical history, diagnoses, treatment plans, immunization dates, allergies, radiology images, and laboratory test results.
Impact:
Improved Billing Accuracy: With all necessary patient information readily available, EHR systems help reduce DME billing errors. Accurate and complete information is crucial for generating precise bills and avoiding discrepancies.
Faster Reimbursement Cycles: EHRs streamline the sharing of patient information between healthcare providers and payers. This seamless flow of information accelerates the DME billing process, leading to quicker reimbursements.
Reduced Errors: The risk of lost paperwork and incomplete information is minimized, leading to more accurate billing. This also reduces the likelihood of claims being denied or delayed due to missing or incorrect information.
Digital Technology for Financial Transactions
Digital technology assists in managing financial transactions by recording them in the correct accounts and providing accurate financial information in real-time. This includes automated systems for billing, payments, and financial reporting.
Impact:
Real-Time Financial Information: DME providers can access up-to-date financial information, enabling them to make informed financial decisions quickly. This real-time insight is vital for effective financial management.
Accuracy: Digital systems reduce errors in financial records by automating the entry and processing of financial transactions. This accuracy is critical for maintaining trust and ensuring proper financial management.
Efficiency: By streamlining financial management processes, digital technology makes them faster and more reliable. This efficiency translates into better resource allocation and improved overall financial health of the hospitals.
Software and Applications
Various software and applications assist in data collection, processing, and analysis. These tools are designed to enhance productivity and simplify complex tasks. Examples include billing software, data analytics tools, and customer relationship management (CRM) systems.
Impact:
Enhanced Data Processing: Software tools improve data collection and analysis speed and accuracy. This is essential for generating accurate bills and managing patient information effectively.
Increased Productivity: Automating routine tasks allows staff to focus on higher-priority activities, such as patient care and strategic planning. This shift boosts overall productivity and operational efficiency.
Better Decision-Making: Advanced data analytics tools provide actionable insights, enabling DME providers to make informed decisions. These insights can lead to improved patient outcomes and more efficient operations.
Computer-Assisted Coding (CAC)
Computer-assisted coding (CAC) uses computer algorithms and natural language processing (NLP) to assist medical coders in assigning the correct DME billing codes based on clinical documentation. CAC systems analyze electronic health records, transcriptions, and other medical documents to identify and suggest relevant codes based on the patient’s diagnosis and procedures performed.
Impact:
Efficiency: CAC significantly speeds up the coding process by automating the identification of relevant codes. This reduces the time spent on manual coding and allows for quicker claim submissions.
Accuracy: By reducing the likelihood of human error, CAC ensures that the correct codes are used for DME billing. This accuracy is crucial for preventing claim denials and ensuring proper reimbursement.
Consistency: CAC provides uniformity in coding practices, ensuring that all coders follow the same guidelines and standards. This consistency helps maintain the integrity of the billing process across different healthcare providers.
Blockchain Technology
Blockchain technology offers a secure and transparent way to handle billing by using a decentralized, tamper-proof digital ledger. This technology can store and manage patient records and billing information securely.
Impact:
Enhanced Security: Blockchain’s advanced encryption techniques protect sensitive patient information from unauthorized access and breaches. This level of security is essential for maintaining patient trust and complying with healthcare regulations.
Data Integrity: The immutability of blockchain ensures that all data is accurate and cannot be altered or tampered with. This integrity is critical for maintaining accurate and reliable billing records.
Transparency: Blockchain allows all parties involved in the billing process, including healthcare providers, patients, and insurers, to access the same information. This transparency reduces disputes and enhances trust among all stakeholders.
Outsourcing as Best Alternative
Despite the transformative potential of technological innovations, many Durable Medical Equipment (DME) providers may still encounter persistent challenges in their billing processes. These challenges can stem from various factors, such as the complexity of insurance claims, the need for specialized knowledge, and the initial investment required to implement and maintain advanced tech innovations in DME Billing. In all such scenarios, outsourcing DME billing to 24/7 Medical Billing services emerges as a highly effective solution. DME providers can leverage both cutting-edge technology and professional expertise by outsourcing to streamline their billing operations. So, what are you waiting for? Contact the experts right now to leverage the benefit of tech transformations.
Content Source: [https://www.247medicalbillingservices.com/blog/tech-innovations-dme-billing-processes]
For More Information:
Call us at 888-502-0537 or Sales: [email protected]
Support: [email protected]
Visit at https://www.247medicalbillingservices...
Our Office Locations:
Ohio: 28405 Osborn Road, Cleveland, OH, 44140
Texas: 2028 E Ben White Blvd, #240-1030 Austin TX, 78741
Subscribe @247medicalbillingservices
Follow us on social media channels-
Facebook: https://www.facebook.com/247MBS
Twitter: https://x.com/247MBServices
Instagram: https://www.instagram.com/247mbs/
LinkedIn: https://www.linkedin.com/company/24-7-medical-billing-services/
#DME Billing#Durable Medical Equipment (DME) Billing#DME Billing New York#DME Billing services#Durable Medical Equipment (DME) Billing Services#DME Billing services USA#Durable Medical Equipment Billing Massachusetts#top Durable Medical Equipment Billing company#Durable Medical Equipment Billing Services Rhode Island#DME Medical Services Connecticut#Durable Medical Equipment Billing Agency Delaware#DME Billing Agency Florida#Durable Medical Equipment Billing Company Georgia#DME Billing Company New Jersey#Best DME Billing Company South Carolina#Top DME Billing Company Texas#Top DME Billing Company Ohio#Professional DME Billing Company USA#Cheap DME Billing Company Virginia#Outsourcing DME Billing Ohio#Outsourcing DME Billing Services Florida#Durable Medical Equipment Billing Services Company#DME Billing Services Company Georgia#Best DME Billing Services Company#Best Durable Medical Equipment Coding Services Company#Leading DME Billing and Coding Services Company#Durable Medical Equipment Billing Company California#Top DME Billing and Coding Company Pennsylvania#Professional DME Billing Company New Hampshire#Cheap DME Billing services Oklahoma
0 notes
Text
Neurointerventional Devices Market Dynamics: Regulatory Challenges and Opportunities for Industry Players
The neurointerventional devices market is experiencing significant growth, driven by advancements in medical technology and an increasing prevalence of neurovascular diseases. However, this growth is accompanied by a complex regulatory landscape that presents both challenges and opportunities for industry players.

Regulatory Challenges
Stringent Approval Processes: Regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have rigorous approval processes for neurointerventional devices. In the United States, devices must undergo either the 510(k) premarket notification or the more stringent premarket approval (PMA) process. The 510(k) pathway allows devices that are substantially equivalent to existing approved devices to gain faster market access. For instance, the recent approval of the Penumbra Jet 7, used for thrombectomy procedures in acute ischemic stroke, exemplifies how the FDA’s expedited processes can facilitate innovation while maintaining safety standards. Conversely, the PMA pathway requires extensive clinical trials and comprehensive data analysis, as seen with Medtronic’s flow diversion systems, ensuring high safety and efficacy standards before reaching healthcare providers .
Post-Market Surveillance: Both the FDA and EMA mandate post-market surveillance to monitor the performance of neurointerventional devices after approval. This involves collecting real-world data and reporting adverse events, which can lead to further investigations and potential device recalls if safety concerns arise. For example, certain embolization coils faced scrutiny due to reports of device failures in clinical settings, prompting manufacturers to enhance quality control measures and update labeling to inform users of potential risks .
International Regulatory Variations: Regulatory requirements vary significantly across regions. In Europe, the Medical Device Regulation (MDR) has introduced stricter guidelines for the approval and post-market surveillance of devices. Manufacturers must now demonstrate not only the safety and efficacy of their products but also ensure a robust quality management system. This regulatory shift aims to protect patients and improve the overall quality of medical devices available in the market .
Opportunities for Industry Players
Technological Advancements: Emerging technologies such as artificial intelligence (AI) and robotics are influencing the regulatory landscape. The integration of AI in neurointerventional devices is prompting regulatory bodies to establish new guidelines that address the unique challenges of software-driven technologies. The FDA has begun to develop frameworks for the regulation of AI-based devices, emphasizing the importance of continuous learning and adaptability in these technologies .
International Harmonization: Organizations like the International Organization for Standardization (ISO) and the International Electrotechnical Commission (IEC) are working to create unified guidelines that can simplify the approval process across different regions. This harmonization can facilitate faster market entry for innovative devices while maintaining high safety standards .
Emerging Markets: As healthcare infrastructure improves in regions like Asia-Pacific and Latin America, there is a growing demand for advanced neurointerventional solutions. Companies can capitalize on this trend by developing tailored products that cater to the specific needs of these markets. Additionally, ongoing research and development initiatives focusing on innovative technologies present significant opportunities for market players to differentiate themselves and capture a larger market share .
Conclusion
The neurointerventional devices market presents a dynamic landscape characterized by stringent regulatory requirements and emerging opportunities. Industry players must navigate these challenges and leverage technological advancements and international harmonization efforts to drive growth and innovation. By staying informed and adaptable, companies can successfully navigate the regulatory landscape and capitalize on the opportunities within this expanding market.
0 notes
Text
Learning Home Medical Billing: Essential Tips for Streamlined Processes and Increased Revenue
Mastering Home Medical Billing: Essential Tips for streamlined Processes and Increased Revenue
in today’s healthcare environment, effective medical billing practices are pivotal for home Medical Equipment (HME) businesses and healthcare providers alike. Mastering home medical billing not only facilitates a streamlined process but also leads to increased revenue. This comprehensive guide covers essential tips,practical insights,and hands-on experiences to help you optimize your billing processes.
Understanding Home Medical Billing
Home medical billing involves the preparation and submission of claims for payment by insurance providers or patients for medical services, supplies, and equipment delivered in the home setting. Efficient billing practices ensure that healthcare providers are reimbursed quickly and accurately, optimizing financial stability for the organization.
The Importance of Streamlined Processes
Streamlined processes in medical billing are vital for several reasons:
Increased Revenue: Efficient billing processes reduce the time it takes to receive payments.
Reduced Errors: Streamlined workflows minimize the chances of mistakes in claims submission.
Organizational Efficiency: A well-structured billing process enhances productivity and employee morale.
Essential tips for Streamlined Home Medical Billing
1. Invest in Quality Medical Billing Software
Choosing the right medical billing software is critical for streamlining your billing processes. A quality software solution should:
Automate claim submissions
Provide real-time tracking
Integrate with electronic health record (EHR) systems
Offer comprehensive reporting capabilities
2. Understand Insurance Policies
Different insurance companies have different policies. Understanding these regulations helps ensure compliance and improves reimbursement rates. Make sure to:
stay updated with changes in insurance policies
Communicate with insurance representatives when unclear
Educate patients about their coverage options
3. Implement a Robust Verification Process
Before providing services,verify patients’ insurance eligibility and benefits. A thorough verification process can considerably reduce claims denials. Consider the following:
Confirm coverage details at the time of service
Document all communications for future reference
regularly update your eligibility verification process based on insurance changes
4. Focus on Accurate Coding
Successful billing relies heavily on the accuracy of medical coding.Incorrect codes can lead to denials and delays.Key strategies include:
Stay updated with the latest coding guidelines (ICD-10, CPT)
Use software that assists with coding recommendations
Employ certified professional coders to ensure accuracy
5. develop a Follow-Up System
Follow-ups on claims and patient payments are essential for maintaining cash flow. Create a systematic approach by:
Setting up reminders for pending claims
Developing a script for follow-up calls
Regularly training your team on effective interaction with payers and patients
6. Regularly Analyse Your Billing Performance
Periodic performance analysis helps you identify areas for advancement.Use metrics like denial rates, days in accounts receivable, and collection rates to evaluate your processes:
Metric
Description
Ideal Rate
Denial Rate
Percentage of claims denied by payers
Less than 5%
Days in A/R
Average days taken to collect payment
30 days or less
Collection Rate
Percentage of billed services collected
95% or higher
Benefits of Efficient Home Medical billing
Mastering home medical billing provides numerous benefits, including:
Improved Cash Flow: Faster payments lead to better cash management.
Stronger patient Relationships: Transparency and communication regarding billing enhance patient trust.
Regulatory Compliance: staying informed about regulations mitigates legal risks.
Case Studies: Real World Applications
Case Study 1: Streamlining Processes for a Small HME Provider
A small home medical equipment provider implemented updated billing software and invested in training staff on coding accuracy. As a result:
Claim denials decreased by 40% within six months.
Days in accounts receivable improved from 60 to 30 days.
Case Study 2: Enhancing Patient Engagement in Billing
A larger healthcare provider revamped its communication strategy, incorporating patient education through workshops.This led to:
A 20% increase in timely payments.
Higher patient satisfaction scores related to billing concerns.
First-Hand Experience: A Billing Specialist’s Perspective
As a billing specialist with over five years of experience, I’ve witnessed firsthand how critical attention to detail and robust processes can transform a healthcare provider’s financial health. Institutions that prioritize efficient billing not only thrive financially but also establish long-lasting patient relationships built on trust and transparency.
Conclusion
Mastering home medical billing is essential for any healthcare provider committed to streamlining processes and increasing revenue. By investing in quality software, understanding insurance policies, focusing on accurate coding, and regularly analyzing billing performance, providers can create a sustainable billing process that fosters resilience. Follow these essential tips, and your organization will be well on its way to mastering the art of home medical billing.
youtube
https://medicalbillingcertificationprograms.org/learning-home-medical-billing-essential-tips-for-streamlined-processes-and-increased-revenue/
0 notes
Text
Optimizing Revenue: Essential Tips for Streamlining Your Medical Billing Process with ABC Medical Billing
Maximizing Revenue: Essential Tips for Streamlining Your medical Billing process with ABC Medical Billing
In the fast-paced world of healthcare, maximizing revenue is pivotal for your practice’s financial health. An optimized medical billing process is crucial in achieving this goal. Working with ABC Medical Billing can help you streamline your billing practices, reduce claim denials, and strengthen your overall revenue cycle. In this article,we’ll explore essential tips for enhancing your medical billing process,ensuring you’re not leaving any money on the table.
Understanding the Importance of Streamlined Medical Billing
The medical billing process is a vital aspect of the healthcare industry, influencing cash flow and operational efficiency. A streamlined process can lead too:
Reduced claim denials
Faster payment cycles
Improved patient satisfaction
Enhanced practice reputation
Benefits of Partnering with ABC Medical Billing
ABC Medical Billing specializes in simplifying your billing processes, allowing healthcare providers to focus on patient care. Here are some benefits of partnering with ABC:
Expertise: Access a team of billing professionals who understand the complexities of insurance claims.
Technology: Utilize cutting-edge billing software that boasts automation and accuracy.
Compliance: Stay compliant with the latest healthcare regulations and standards.
Analytics: Get detailed reports to help you understand your financial health.
Essential Tips for Streamlining your Medical Billing Process
1. Invest in a Robust Billing software
Utilizing advanced billing software tailored for medical practices can significantly simplify your billing tasks. ABC Medical Billing offers integrated solutions that automate many aspects of billing, reducing errors and freeing up staff time.
2. Maintain Accurate Patient Facts
One of the leading causes of claim denials is inaccurate patient information. Ensure that your staff is trained to gather complete and correct data during patient registration. This includes:
Full names
Insurance details
Date of birth
Contact information
3. Regular Training for Your Billing Team
Having a learned billing team is essential. Regular training sessions on coding updates, compliance changes, and software tools can help improve billing accuracy and efficiency.
4. Implement a Pre-Authorization Process
Before services are rendered, ensure that you obtain pre-authorization for procedures that require it. This process helps to minimize claim denials and delays in payments.
5. Optimize Claim Submission Processes
Create a systematic approach for submitting claims to insurance providers. Aim for clean claim submissions with all required documentation.ABC Medical Billing can assist in monitoring claim statuses to ensure timely payments.
Case Studies: Success with ABC Medical Billing
case Study 1: Family Health Clinic
The Family Health Clinic experienced a 30% increase in revenue within six months of partnering with ABC Medical billing. By adopting a new billing system and streamlining processes, they reduced claim denials significantly.
Case Study 2: A Town General Practice
A Town General Practice switched to ABC Medical Billing and reduced their payment cycle from 45 days to just 30 days.They credited this turnaround to improved charge capture and efficient claims processing.
First-Hand Experience: Why Choose ABC Medical Billing
As a practice manager, I witnessed a remarkable conversion after partnering with ABC Medical Billing. The ease of dialog, detailed analytics provided, and the team’s knowledge in navigating insurance complexities have all contributed to an improved financial landscape in our practice.
Cost Analysis Table
Billing Method
Cost
Time to Payment
Claim Denial Rate
in-House Billing
$2,500/month
45 days
10%
ABC Medical Billing
$2,000/month
30 days
5%
Conclusion
Streamlining your medical billing process is essential for maximizing revenue and ensuring a smooth revenue cycle. Partnering with ABC Medical Billing offers innovative solutions and expertise that can help your practice thrive. Focus on delivering exceptional patient care while ABC handles the complexities of billing. By employing the tips outlined in this article, you can significantly enhance your billing operations and achieve financial success.
youtube
https://medicalcodingandbillingclasses.net/optimizing-revenue-essential-tips-for-streamlining-your-medical-billing-process-with-abc-medical-billing/
0 notes
Text
Leading 10 Medical Billing Companies in NY: Streamline Your Practice's Revenue Today!
Top 10 Medical Billing Companies in NY: Streamline Your Practise’s Revenue Today!
Top 10 Medical Billing Companies in NY: Streamline Your Practice’s Revenue Today!
In the ever-evolving landscape of healthcare, effective revenue management is crucial for the success of medical practices. A dedicated medical billing company can help streamline your practice’s revenue cycle management, reduce claim denials, and improve cash flow. If you’re in New York and looking for reliable medical billing services, you’re in the right place. This article highlights the top 10 medical billing companies in NY that can boost your practice’s financial performance.
Why Choose a Medical Billing Company?
Outsourcing your medical billing provides numerous benefits, including:
Increased Efficiency: Focus on patient care while billing experts handle claims and payments.
Reduced Errors: Professional billing companies reduce claim denials and rejections.
Stay updated: These companies keep abreast of the latest coding and billing regulations, ensuring compliance.
Cost Saving: Lower operational costs by avoiding in-house billing staff and expenses.
Top 10 Medical Billing Companies in NY
1. AdvancedMD
Headquarters: New York City, NY
Overview: AdvancedMD offers extensive revenue cycle management services tailored to practices of all sizes. Their cloud-based platform enhances billing efficiency and ensures real-time tracking.
2. eCatalyst Healthcare Solutions
Headquarters: Albany, NY
Overview: Specializing in billing for physicians and healthcare facilities, eCatalyst focuses on optimizing revenue cycle processes and reducing claim rejections.
3. Medical Billing Experts
Headquarters: Buffalo, NY
Overview: As a leading provider, Medical Billing Experts offer personalized billing services with a focus on increasing collections and reducing administrative burdens.
4. Billing Advantage
Headquarters: Rochester, NY
Overview: This company is known for its comprehensive analysis of billing processes and improvement strategies that help maximize revenue flow for practices.
5. MedBillingExperts
Headquarters: White Plains,NY
Overview: MedBillingExperts provides end-to-end billing solutions with a focus on transparency,client training,and seamless integration with existing software.
6. iMarque Solutions
Headquarters: New York, NY
Overview: iMarque specializes in a range of billing services, including revenue cycle analytics that help uncover areas for financial improvement.
7. Access Healthcare
Headquarters: Syracuse, NY
Overview: With a robust suite of technology-driven solutions, Access Healthcare is adept at catering to diverse healthcare settings, enhancing financial outcomes through effective billing practices.
8. Cogneesol
Headquarters: Long Island, NY
Overview: Cogneesol offers tailored medical billing services that emphasize ethical billing practices and maximizing reimbursements for healthcare providers.
9. eClaim Solutions
Headquarters: New York,NY
Overview: eClaim specializes in electronic claims processing with tools to streamline billing tasks and enhance cash flow significantly.
10. ClaimCare
Headquarters: Manhattan, NY
Overview: ClaimCare provides adaptive billing solutions designed to suit your practice’s needs, resulting in a higher rate of successful claims and faster payments.
benefits of Using Medical Billing Services
Using a medical billing company can yield numerous benefits for healthcare providers:
Improved cash flow and reimbursement rates.
Fewer billing errors leading to reduced claims denials.
Access to professional expertise in coding and billing regulations.
more time for healthcare providers to focus on patient care.
Practical tips for Choosing the Right Medical Billing Company
When selecting a medical billing service, consider the following tips:
Assess Experience: Look for a company with a solid track record in your specialty.
Check Credentials: Ensure they are certified and comply with healthcare regulations.
Read Reviews: Customer testimonials will give insights into their service quality.
Evaluate Software: Assess whether their technology integrates well with your existing practice management systems.
Case Study: How Medical Billing Experts Boosted collections
A mid-sized clinic in New York faced challenges with delayed payments and high claim denials. After hiring Medical Billing Experts, they experienced a 30% increase in collections within six months. By implementing streamlined processes and providing dedicated coding teams, medical Billing Experts significantly improved the clinic’s revenue flow.
Conclusion
Outsourcing your medical billing can lead to important improvements in your practice’s financial health. The top 10 medical billing companies in NY mentioned above offer a range of services designed to cater to different healthcare settings. by choosing the right partner, you can streamline your revenue cycle, reduce administrative burdens, and focus on what matters most—providing excellent patient care.
Consider your practice’s unique needs, check for the company’s experience and track record, and take the first step toward better financial management today!
youtube
https://medicalbillingcodingcourses.net/leading-10-medical-billing-companies-in-ny-streamline-your-practices-revenue-today/
0 notes
Text
North America Sepsis Diagnostics Market Size, Competitors Strategy, Regional Analysis and Industry Growth by Forecast (2021-2028)
The North America sepsis diagnostics market is expected to grow from US$ 279.06 million in 2021 to US$ 513.33 million by 2028. It is estimated to record a CAGR of 9.1% from 2021 to 2028.
High Incidence of Sepsis due to Increasing Nosocomial Infections Drives North America Sepsis Diagnostics Market
The underlying cause of sepsis is infection, with a heightened risk among immunocompromised individuals, such as those receiving chemotherapy, individuals who have undergone splenectomy, and those with AIDS, diabetes, and other chronic conditions. Among various types of infections, nosocomial infections are a leading cause of illness and mortality in hospitalized patients. The Centers for Disease Control and Prevention's (CDC) "2020 National and State Healthcare-Associated Infections Progress Report" (published in 2021) indicated that the US experienced increases of about 24% in central line-associated bloodstream infections, 35% in ventilator-associated events, and 15% in Methicillin-resistant Staphylococcus aureus (MRSA) bacteremia between 2019 and 2020. As per a report by the Global Sepsis Alliance (GSA), approximately 26 million people worldwide develop sepsis annually, leading to roughly 8 million deaths. Consequently, the increasing incidence of bloodstream infections is anticipated to fuel greater adoption of sepsis diagnostic products. Furthermore, mortality frequently arises from diarrheal diseases or lower respiratory infections, many of which are preventable through early diagnosis and appropriate clinical management. Thus, the high incidence rate of sepsis is expected to boost the demand for sepsis diagnostic products, which would support the expansion of the North America sepsis diagnostics industry during the forecast period.
Download our Sample PDF Report
@ https://www.businessmarketinsights.com/sample/BMIRE00025664
North America Sepsis Diagnostics Strategic Insights
Strategic insights for the North America Sepsis Diagnostics sector provide data-informed analysis of the industry's environment, encompassing current trends, major players, and regional specificities. These insights offer actionable recommendations, allowing readers to distinguish themselves from competitors by identifying unexploited segments or developing unique value propositions. By utilizing data analytics, these insights help industry participants—whether investors, manufacturers, or other stakeholders—to anticipate market evolutions. A forward-looking approach is crucial, enabling stakeholders to predict market shifts and strategically position themselves for sustained success within this dynamic region. Ultimately, effective strategic insights empower readers to make well-informed decisions that drive profitability and achieve their business objectives within the market.
North America Sepsis Diagnostics Market Segmentation
North America Sepsis Diagnostics Market: By Product
Instruments
Reagents and Assays
Blood Culture Media
Software
North America Sepsis Diagnostics Market: By Technology
Molecular Diagnostics
North America Sepsis Diagnostics Market: By Flow
(Cytometry, Microfluidics, Immunoassay, Biomarkers, Microbiology)
North America Sepsis Diagnostics Market: By Method
Automated Diagnostics and Conventional Diagnostics
North America Sepsis Diagnostics Market: By Test Type
Point-of-Care Tests and Laboratory Tests
North America Sepsis Diagnostics Market: Regions and Countries Covered
North America
US
Canada
Mexico
North America Sepsis Diagnostics Market: Market leaders and key company profiles
Abbott
BD
bioMerieux SA
Danaher (Beckman Coulter)
F. HOFFMANN-LA ROCHE LTD.
Immunexpress Inc.
Luminex Corporation
T2 Biosystems, Inc.
THERMO FISHER SCIENTIFIC INC.
About Us:
Business Market Insights is a market research platform that provides subscription service for industry and company reports. Our research team has extensive professional expertise in domains such as Electronics & Semiconductor; Aerospace & Defense; Automotive & Transportation; Energy & Power; Healthcare; Manufacturing & Construction; Food & Beverages; Chemicals & Materials; and Technology, Media, & Telecommunications
#North America Sepsis Diagnostics Market#North America Sepsis Diagnostics Market Size#North America Sepsis Diagnostics Market Strategy
0 notes
Text
Top Workflow Solutions That Are Transforming Business Efficiency in 2025
Workflow solutions are digital platforms or systems designed to automate, manage, and optimize business processes. These tools replace manual, repetitive tasks with streamlined, rule-based automation—allowing teams to focus on high-value work.
From task tracking to cross-departmental collaboration, workflow solutions help reduce bottlenecks, enforce accountability, and increase visibility into operations.

1. Low-Code Workflow Platforms
Low-code platforms like Cflow, Monday.com, are leading the charge in 2025. These tools empower non-technical users to design and deploy custom workflows without writing complex code. Companies can automate HR onboarding, IT service requests, procurement approvals, and more—all within days.
Why it matters: Speed to implementation and ease of use mean businesses can adapt workflows in real-time, keeping up with fast-changing demands.
2. AI-Powered Workflow Automation
Artificial intelligence is no longer futuristic—it's fully embedded in today’s workflow solutions. Tools like UiPath and Zapier AI are automating decision-making, routing, and even predictive scheduling.
For example, AI can now analyze incoming support tickets and automatically assign them to the right team member based on workload, past performance, and sentiment analysis.
Why it matters: AI eliminates human error, speeds up response times, and enables proactive business decisions based on real-time data.
3. Integrated Workflow Ecosystems
In 2025, siloed software is out. Businesses are adopting workflow ecosystems that connect seamlessly with their existing tools—CRM, ERP, HRMS, and cloud storage.
Solutions like Make (formerly Integromat) and Microsoft Power Automate excel in connecting platforms. They unify tools like Slack, Salesforce, Google Workspace, and SAP into one coherent system.
Why it matters: Unified systems eliminate data silos, reduce duplicate work, and ensure a smooth flow of information across departments.
4. Mobile-First Workflow Applications
With hybrid and remote work here to stay, mobile-first workflow apps are dominating the landscape. Solutions like Asana, ClickUp, and Trello now offer robust mobile experiences that let teams collaborate, assign tasks, and approve processes from anywhere.
Why it matters: Accessibility boosts engagement and ensures productivity, even when employees are not at their desks.
5. Industry-Specific Workflow Solutions
Custom-fit workflow software is growing rapidly in sectors like healthcare, construction, legal, and logistics. For instance, tools tailored for healthcare automate patient onboarding and medical records, while construction-specific platforms handle site inspections and project approvals.
Why it matters: Industry-specific workflows reduce compliance risks and improve operational precision.
Key Benefits of Modern Workflow Solutions
Time savings: Automating routine tasks can reduce process time by up to 70%.
Consistency: Workflow rules ensure tasks are done the same way every time.
Transparency: Real-time dashboards allow managers to track progress and performance.
Scalability: Digital workflows grow with your organization—no need to reinvent the wheel.
youtube
Final Thoughts
In 2025, top-performing businesses are not just using workflow solutions—they are building entire digital ecosystems around them. Whether you're automating internal processes or enhancing customer experiences, choosing the right workflow solution is key to staying ahead.
The tools mentioned above represent the forefront of operational efficiency and digital agility. As industries continue to evolve, investing in scalable, intelligent workflow systems is no longer a luxury—it's a necessity.
SITES WE SUPPORT
AI Job Hire Flow - Weebly
SOCIAL LINKS Facebook Twitter LinkedIn
0 notes
Text
U.S. Revenue Cycle Management Market: The Impact of Value-Based Care on Revenue Strategies
U.S. Revenue Cycle Management Industry Overview
The U.S. Revenue Cycle Management Market, valued at approximately $172.24 billion in 2024, is projected to grow at a CAGR of 10.1% from 2025 to 2030. The swiftly evolving healthcare landscape, marked by increasing digitalization, has created opportunities for the adoption of healthcare IT services, including revenue cycle management (RCM) systems. These systems aim to organize and streamline healthcare organization workflows through synchronized management software solutions. RCM solutions integrate payment models, reimbursement guidelines, codes, and interactions with third-party payers. The complexities inherent in billing and ensuring accurate payment for medical services are anticipated to drive the demand for innovative RCM solutions.
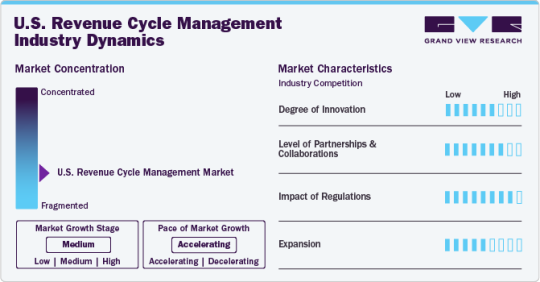
The practice of U.S. healthcare entities outsourcing RCM is gaining momentum due to its increasing advantages. The market is expected to experience substantial growth as a result of the intricate and labor-intensive nature of RCM processes, a shortage of qualified healthcare professionals, the necessity for cost-effective solutions, and the challenges presented by strict regulations, financial constraints, and staff shortages within the healthcare sector. Consequently, healthcare providers are increasingly choosing to outsource RCM tasks to specialized companies to optimize processes, decrease expenses, enhance accuracy, and prioritize patient care over administrative duties. This trend is likely to persist as providers seek efficient cash flow, cost reductions, and improved value-based care delivery.
Detailed Segmentation:
Component Insights
The software segment is anticipated to grow significantly during the forecast period, owing to a growing demand for digitalization and streamlining of operational workflows to improve patient care. The growing amount of unorganized data generated from multiple healthcare functionalities requires centralization and consolidation, which is anticipated to drive the software segment over the forecast period.
Product Insights
The integrated segment dominated the market in 2024 with a market share of over 71.84% and is anticipated to grow at the fastest rate during the forecast period. This is attributed to the constant technological advancements and rapid adoption of integrated RCM solutions by healthcare organizations. Furthermore, integrated solutions provide a synchronized and streamlined platform for financial activities with a standardized data collection and analysis process, which is expected to drive the market over the forecast period.
Delivery Mode Insights
The web-based segment dominated the market in 2024 with a market share of over 56.76%. Web-based solutions are being increasingly implemented since these solutions are to be installed off-site and do not require additional hardware or storage. Affordability and rapid deployment are some of the benefits offered by web-based solutions. athernaOne, e-Hospital Systems, Simplex HIMES, and Advanced HIMS are examples of web-based practice management solutions. The cloud-based segment is anticipated to grow at the fastest rate during the forecast period.
Specialty Insights
The cardiology segment held a significant share of 7.15% in 2024 and is expected to grow at the fastest rate during the forecast period. Cardiology treatments are expensive procedures requiring RCM services; these services help enhance the procedure's effectiveness & patient care and seamlessly manage medical billing. According to an Elsevier, Inc. paper in September 2023, approximately 6.7 million U.S. adults aged 20 years and above had heart failure, and the prevalence is projected to reach 8.5 million by 2030. The rising prevalence of cardiovascular diseases directly increases the workload burden on healthcare providers and healthcare payers, which is expected to drive the segment.
Sourcing Insights
The in-house segment dominated the market in 2024 and accounted for a revenue share of over 70.82%. The segment growth is attributed to associated benefits, such as complete control of coding operations, patient information confidentiality, and accessibility of in-house medical billers. One of the major challenges in-house RCM services face is the requirement of a large medical staff to handle the patient’s medical data. Healthcare providers need to employ trained billers and coders, which can result in backlogs if one of them is ineffective, jeopardizing the entire revenue cycle.
End-use Insights
The hospitals segment is expected to grow at the fastest rate during the forecast period. This is attributed to the growing presence of renowned and well-established hospitals in the U.S. and the rising number of patient care regulatory reforms & guidelines introduced by regulatory agencies. Hospitals are focusing on implementing innovative RCM solutions by collaborating with vendors to transform the reimbursement scenario, which is anticipated to boost segment growth. Moreover, the growing demand to optimize hospitals’ workflow to improve efficiency and productivity is expected to boost the adoption of integrated RCM systems in hospitals.
Function Insights
The claims management segment dominated the market in 2024 with a market share of over 52.78%. This is attributed to the swiftly expanding patient pool, the rising geriatric population, and the introduction of advantageous government programs related to medical insurance coverage. In addition, the adoption of risk- or value-based reimbursement models is boosting the implementation of enhanced supervision and revenue cycle prediction, particularly for high-risk & vulnerable patient groups.
Gather more insights about the market drivers, restraints, and growth of the U.S. Revenue Cycle Management Market
Key Companies & Market Share Insights
Some emerging companies in the market are Aidéo Technologies, Access Healthcare, TELCOR, CorroHealth, and others. Key players' strategies to strengthen their market presence include new product launches, partnerships & collaborations, mergers & acquisitions, and geographical expansion.
Key U.S. Revenue Cycle Management Companies:
athenahealth, Inc.
Cerner Corporation
eClinicalWorks
Epic Systems Corporation
McKesson Corporation
NXGN Management, LLC
Oncospark, Inc.
R1 RCM, Inc.
The SSI Group, Inc.
Veradigm LLC (Allscripts Healthcare LLC)
Order a free sample PDF of the Market Intelligence Study, published by Grand View Research.
Recent Developments
In January 2025, Access Healthcare received a strategic investment from New Mountain Capital, LLC. This investment is noteworthy because it originates from a reputable, growth-focused firm that manages around USD 55 billion in assets. The partnership intends to enhance Access Healthcare's capabilities and support its expansion into new markets.
In September 2024, CorroHealth, completed the acquisition of the Xtend healthcare revenue cycle management business from Navient. This strategic move is significant for several reasons, which will be explored in detail below. As part of this transaction, over 925 employees from Xtend have joined CorroHealth’s workforce. This addition not only expands CorroHealth’s team but also brings in valuable expertise that can enhance their operational capabilities.
0 notes
Text
Why Patient Experience Matters: Using Software to Improve Satisfaction
Introduction
The healthcare environment has had some radical changes, putting a fresh emphasis on patient experience as one of the core markers of success. The time when medical care was only about diagnosis and treatment is well and truly gone. Patients expect much more today—personalized care, uninterrupted communication, less waiting time, and digital engagement.
Therefore, CMS and PES software have become indispensable for modern-day healthcare providers. Modern Clinic Management Software and Patient Experience Software streamline operations, increase engagement, elevate patient satisfaction, and lead to improved healthcare outcomes.
But, in what way does software make a contribution to improving patient experience? Let us discuss the role of technology in modern-day healthcare and how in-filling some advanced software solutions would soon prove to be a game changer for patient satisfaction.
The Importance of Patient Experience in Modern Healthcare
Why is Patient Experience Important?
Patient experience is not optional; it impacts retention and loyalty, health outcomes, and their very lives. Evidence shows patients who experience good patient care experiences follow treatment plans, place trust in providers, and return for the care they need. On the contrary, unfriendly experiences lead to noncompliance, adverse publicity, and lawsuits.
Elements that Determine Patient Experience
A few things affect patient satisfaction:
Scheduling-the long waits and the convoluted process to book appointments irritate the patient.
Communication-Poor communication between doctor and patient leads them to leave dissatisfied.
Facility efficiency-An ill-organized work flow elevates the stress levels of both patients and staff.
Billing & Payments-Making them frustrated due to a confusing billing process.
Follow-up care-Apathy toward post-treatment care erodes patient confidence in providers.
Hence methods Clinic Management System improves patient experience
It is a Clinic Management System (CMS) for patients and healthcare providers, since it is an all-in-one platform tailored to entertain clinic processes in a way that automates and strengthens the operations pertaining to clinic multifunctional values.
Main Advantage of a Clinic Management System
Simple Appointment Scheduling
Patients can book, reschedule, or cancel appointments online without having to call.
Automated reminders eliminate no-shows and thus increase productivity for clinics.
The Effectiveness of Efficient Patient Check-ins
Digital check-in equals no more long queues or waiting times.
Patients can update personal and medical details before arriving.
Enhanced Communicational Feature
ensuring patients timely notifications of appointments, test results, and follow-ups.
Chatbots & Virtual Assistants are manufactured for answering common questions.
Data Security/Compliance
Patient data is organized and secured with Electronic Health Records (EHRs).
They comply with HIPAA, GDPR, and other regulatory standards.
Billings and Payments
On-line payments will make transactions quicker and hassle-free.
Open Billing would help eliminate confusion and disputes.
Real Life Effect of Clinic Management System
Research indicates that clinics that make use of the CMS software have reported a 30 percent increase in patient satisfaction scores since they are able to provide their services faster and increase patient engagement.
Reducing the administrative burden allows the provider to focus on what matters the most—patient care.
Improving Patient Satisfaction Using Patient Experience Software
Patient Experience Software (PES) is built specifically for measuring as well as improving patient satisfaction via digital tools and other feedback mechanisms.
How Patient Experience Software Works:
Collects Feedback from Patients Automated survey after appointments.
Real time sentiment analysis of patients improves interaction.
It Enhances Communication
Two-way messaging for appointment reminders and follow-ups.
Telehealth services for remote consultations.
It Gives Personalized Care
AI-Driven Analytics to predict patient's needs ad recommend care plans.
Helps the providers to address issues proactively.
Measurable satisfaction in real-time
Wait times, appointment efficiency, and any interactions with the patient are evaluated.
The actionable insights are regarding service improvements.
Reasons Why Clinics Need Patient Experience Software
72 % of patients expect real-time communication with their healthcare provider.
Clinics implementing PES report improved patient retention up to 40%.
It is using Patient Experience Software for bridging the gap between the expectations of patients and what is actually delivered by the healthcare providers in terms of service quality.
The Significance of Technology in Overhauling Healthcare
Artificial Intelligence (AI) in Patient Experience
AI chatbots are available for patients round-the-clock.
AI helps analyze patient comments for improving deficient areas.
Telehealth and Virtual Care
Offers remote consultations to decrease on-site clinic visits.
Provides easier access to patients living in remote areas.
Mobile Apps for Patient Engagement
Enable patients to keep track of health records while receiving reminders and communicating with doctors.
Push notifications enhance adherence to medications.
Cloud-based Healthcare Solutions
SAFE storage of EHR records keeps the data accessible.
Helps facilitate easy cooperation between several health providers.
Conclusion
Patient experience is becoming more critical in a competitive healthcare environment. Clinics that are harnessing technology, such as Clinic Management Systems and Patient Experience Software, are thereby efficiently delivering care that is faster, smoother, and personalized.
Introducing the right software solution will help clinics operate more efficiently, bolster patient satisfaction, and improve health outcomes.
If you want to enhance the patient experience and clinic productivity, Clinthora should be your next stop. It is a complete Clinic Management System designed for modern healthcare facilities.
FAQs
How does Clinic Management Systems improve efficiency?
CMS automates scheduling, billing, and patient records, effectively cutting down on administrative work as well as waiting times.
What features should I look for in Patient Experience Software?
Core features would include collection of feedback, AI powered analytics for real-time patient engagement, and telehealth.
Does technology help in curbing patient no-shows?
Definitely! Automated reminders complement the online booking system and aid in reducing last-minute cancellations and no-shows.
Is telehealth a feature of Patient Experience Software?
Most Patient Experience Software providers offer telehealth functionality to enable remote consultations or follow-up appointments.
What should be the compliance requirements for Clinic Management Software?
CMS shall confirm HIPAA, GDPR, and any other data security regulations to protect the identity of patients.
How does AI improve patient experience?
AI analyzes patient feedback, anticipates needs, and automates interaction – an integration that enhances satisfaction levels.
0 notes
Text
¶ … Oral Candidosis in Patients With Advanced Cancer and Nursing Intervention Andrew N. Davies, et al. (2008) in the work entitled: "Oral Candidosis in Community-Based Patients with Advanced Cancer" reports that oral candidosis is a "significant cause of morbidity in patients with advanced cancer." Oral candidosis is described as "an opportunistic infection...relatively common in patients with early cancer, particularly in those with hematological malignancies, those receiving systemic chemotherapy and those receiving head and neck radiotherapy." (Davies, et al., 2008, p. 509) Davies et al. (2008) states that oral candidosis is not "...a single clinical entity, but a spectrum of very different clinical entities." (p.509) Davies et al. (2008) reports a study that included individuals with a diagnosis of advanced cancer and who were over the age of 18 years. The study reported is a "prospective, observational study" which is a study of a qualitative nature. The study contained a clinical component which involved completion of a study questionnaire and assessment of the Eastern Cooperative Oncology Group (ECOG) "performance status, clinical examination of the oral cavity, measurement of the unstimulated whole salivary flow rate, and performance of an oral rinse." (Davies, et al., 2008, p.509) Additionally it is reported that oral swabs were taken from subjects "with appearances indicative of oral candidosis on clinical examination of the oral cavity." (Davies, et al., 2008, p.509) The laboratory component of the protocol is stated to have involved "standard procedures to isolate enumerate, and identify yeasts from the clinical specimens. Yeasts were isolated using CHROMagar Candida and indentified using the API 20 C. Aux yeast identification system, and if necessary DNA sequencing." (Davies, et al., 2008, p.509) Data analysis in the quantitative portion of the study was conducted using the software package Statistical Package for the Social Sciences version 13.0 which calculated the descriptive statistics and this is stated to have included both percentages and frequencies for various clinical and microbiological parameters." (Davies, et al., 2008, p. 509) There were a total of 396 participants in the study reported by Davies, et al. (2008). Findings in the study include that the "prevalence of oral candidosis has been reported to vary between 8% and 94% in patients with advanced cancer." (Davies, et al., 2008, p. 512) A poor ECOG performance status is reported to be "an important risk factor for oral candidosis." (Davies, et al., 2008, p. 512) Findings additionally states that candidosis is "extremely high in patients admitted to hospice." (Davies, et al., 2008, p.512) There are also indications by the study results that there is "an association between systemic corticosteroids and oral candidosis." (Davies, et al., 2008, p.512) There is a "strong association between oral candidosis and the use of topical (inhaled) corticosteroids" however the study did not find an association between "systemic antibiotics and oral candidosis." (Davies, et al., 2008, p.512) The study found that screening for oral candidosis in early cancer is important to begin early treatment before patients develop local symptoms which include those of oral discomfort, taste disturbance and prior to their developing distant complications which includes esophageal candidosis, or systemic candidosis. The work of Chang, Molassiotis, Chan and Lee (2007) entitled: "Nursing Management of Oral Mucositis in Cancer Patients" reports that reduction of oral mucositis development through promotion of patient compliance with oral care regimens "can be achieved by teaching patients meticulous oral care during chemotherapy, reinforcement of these instructions as well as regular nursing assessment of the oral cavity." (p.20) The study reported in the work of Chang, Molassiotis, Chan and Lee (2007) had the aim of determining the "current nursing oral care practice and mucositis-related outcomes for patients undergoing chemotherapy." (p.20) The study was comprised by two phases with the second phase focusing on the provision to nurses of education on oral care and prevention of mucositis and comparison of patient outcomes for those patients who received chemotherapy. Emphasized in the oral care protocol were: (1) regular oral assessment; and (2) frequent mouth rinsing using normal saline or water. (Chang, Molassiotis, Chan and Lee, 2007, p.20) The study is reported to have been conducted beginning May 2002 and ending October 2004. Study results state that there was a higher incidence of mucositis in Phase I participants as well as higher level of baseline symptoms and longer duration of cancer when compared to patients in Phase II of this study. There was stated to be low adherence of nurses to oral care principles for those patients who were undergoing chemotherapy in Phase I of the study. However, the adherence of nurses to oral care principles in Phase II of the study was "significantly higher than that in Phase I and for the experimental group it was significantly higher than that for controls." (Chang, Molassiotis, Chan and Lee, 2007, p.22) It is reported by Chang, Molassiotis, Chan and Lee (2007) that the "prevalence of mucositis at day 8 in the phase II study was greater for the experimental group receiving the oral care protocol" however it is reported additionally that there was no statistical significance "adjusted for 5FU chemotherapy, as more of the corresponding patients received such treatment. " The same is stated to be true as of day 16. Stated to be an additional factor that influencing this study's findings was "...the overall low level of mucositis. Moreover, as the assessment of mucositis occurred at fixed days post commencement of chemotherapy, there was no assessment of the pre-treatment levels of mucositis." (Chang, Molassiotis, Chan and Lee, 2007, p.23.) Also reported in the findings of Chang, Molassiotis, Chan and Lee (2007) is: "The Oral Nursing Care Monitor developed for this study indicated an improvement in the level of oral care from phase I to phase II and a significantly higher level of oral care provided by the experimental group nurses in phase II. However as the maximum possible score was 24, the mean of 15.2 shows the need for further improvement in oral care as well as the education and follow-up of nurses in the implementation of oral care for patients receiving chemotherapy." (p.23) The work of Alred, et al. (1991) entitled: "Oral Health in the Terminally Ill: A Cross-Sectional Pilot Survey" reports that patients who are terminally ill "have a number of signs and symptoms related to the mouth. These include mucosal soreness and ulceration, candidosis, glossitis and Xerostomia." (Alred, et al., 1991, p.59) Alred et al. (1991) report a study that included 20 patients/participants who were all suffering from malignant disease that was advanced and formed. Not included were patients with AIDS and cardiac disease. The group was chosen through random sampling and involved measurement of salivary flow rates. Mouth dryness was stated to have been "only ascribed to the extreme situations, in that there was almost total lack of saliva at any sites in the mouth." (Alred, et al., 1991, p. 59) Details were secured concerning the participants "edentulous/teeth present / partial denture; presence of dental care is (decayed teeth); oral hygiene using the criteria of the Debris Index, recorded form the buccal surfaces of all teeth present, gingivitis based on gingival inflammation: graded as no or minimal inflammation, mild gingivitis, moderate gingivitis, or severe gingivitis; xerostomia, mucosal abnormalities; and denture type and quality of fit (good moderate or poor)." (Alred, et al., 1991, p. 60) The study reported by Alred, et al. (1991) states that 75% of the patients "complained of at least one oral symptom, indicating a high prevalence of oral signs and symptoms among patients with terminal illness." (Alred, et al., 1991, p. 61) Alred, et al. (1991) state that 60% of denture wearers "wore their prostheses continuously...despite professional recognition of the importance of leaving dentures out at night..." (p. 63) This emphasized the importance of clearly explaining to patients "the values of leaving dentures in a denture cleaner overnight...particularly in view of their high rate of candidal carriage and candidiasis." (Alred, et al., 1991, p.63) Conclusions in the study of Alred, et al. (1991) state a prevalence of "...oral coliform carriage in a group of healthy adults (median age 62 years) has been reported as 12%" compared with 47% of the terminally ill patients." (p.63) In addition it is reported that "An increased prevalence of coliforms has also been reported in the oral flora of patients on cytotoxic therapy for malignant disease," in patients who have received radiotherapy for oral and laryngeal cancer, and in patients with acute leukemia, where their importance as a potential source of systemic infection has been implied." (Alred, et al., 1991, p. 63) The work of Davies, Brailsford and Beighton (2005) entitled: "Oral Candidosis in Patients with Advanced Cancer" reports a study with the objective of determining "the epidemiology, aetiology, clinical features and microbiological aspects of oral candidosis in a cohort of cancer patients receiving specialist palliative care." (p.698) The study reported is stated to be a collaborative study involving the Department of Palliative Medicine at the Royal Marsden Hospital and the Dental Institute at Kings College London. The inclusion criteria for the study were: (1) diagnosis of advanced cancer, i.e. incurable cancer; (2) referral to the Department of Palliative Medicine. The exclusion criteria for the study were: (1) estimated prognosis of less than 1 week; (2) significant cognitive impairment, i.e. unable to provide consent; (3) significant physical impairment, i.e. unable to complete protocol; (4) clinical evidence of dehydration; (5) current/recent (less than 2 weeks) use of antifungal medication. (Davies, Brailsford and Beighton, 2005) Davies, Brailsford and Beighton (2005) report that the clinical component of the study involved "...completion of a study questionnaire (demographic data and clinical data), completion of the Memorial Symptom Assessment Scale, clinical examination of the oral cavity, measurement of the unstimulated whole salivary flow rate (UWSFR), measurement of the stimulated whole salivary flow rate (SWSFR), and performance of an oral rinse." ( p.698) The study results states that all patients/participants "...had either locally advanced, or metastatic cancer. The prevalence of different cancer diagnoses were: carcinoma breast -- 40%; carcinoma bronchus -- 16.5%; carcinoma of prostate -- 15%; carcinoma colon/rectum -- 6%; others Read the full article
0 notes
Text
Simplify Your Practice: Top 5 Medical Billing Solutions to Maximize Revenue
streamline Your Practise: top 5 Medical Billing Solutions to Maximize Revenue
Streamline Your Practice: Top 5 Medical Billing Solutions to Maximize Revenue
In the rapidly evolving healthcare landscape, efficient medical billing is crucial for maximizing revenue and ensuring the success of your practice. As healthcare providers seek to streamline operations and minimize administrative burdens, implementing the right medical billing solution has become a necessity. in this article, we’ll explore the top five medical billing solutions designed to enhance practice management, reduce claim denials, and ultimately, boost your revenue.
Understanding the Importance of Medical billing
Medical billing involves translating healthcare services into a bill that can be paid by the patient or insurance company. Proper medical billing ensures that healthcare providers get reimbursed for the services rendered, making it essential for the financial health of any practice. Here are some key reasons why optimizing your medical billing process is so important:
Improved cash Flow: Faster payments lead to better cash flow management.
reduced Errors: Automated systems minimize human error that can lead to claim denials.
Time Efficiency: Streamlined processes save time for your administrative staff.
Enhanced Patient Experience: Simplified billing can improve patient satisfaction.
Top 5 Medical Billing Solutions
1. AdvancedMD
AdvancedMD offers a complete medical billing and practice management solution, especially suitable for medium to large practices. Its cloud-based platform enables easy access to data and features.
Key features:
Automated billing and collections
Real-time claim tracking
Customizable reporting tools
Benefits: Simplifies billing processes and supports a range of specialties.
2. Kareo
Kareo is a user-friendly medical billing solution designed for small practices, offering a clear pathway to streamline billing processes.
Key Features:
Integrated billing and electronic health record (EHR) system
Claim scrubbing to reduce rejections
Patient billing portal for easy access
Benefits: simplifies the billing process and increases operational efficiency.
3. DrChrono
DrChrono is another specialized medical billing software that integrates EHR with billing, making it an efficient choice for practices of all sizes.
Key Features:
Customizable templates for various specialties
Mobile app for on-the-go billing
Patient check-in system for improved workflow
Benefits: Offers total practice management as well as billing.
4. SimplePractice
Perfect for behavioral health and therapy practices, SimplePractice provides streamlined billing solutions that cater specifically to these fields.
Key Features:
Insurance claim management
Client portal for easy communication
Superbills for swift reimbursements
Benefits: user-friendly interface that enhances the practice management experience.
5. Optum360
Optum360 offers a robust suite of billing solutions for various providers, including hospitals and large healthcare systems, focusing on revenue cycle management.
Key Features:
Advanced analytics for financial insights
Robust claim processing
Compliance support and training
benefits: Tailored solutions to meet the needs of larger organizations.
Comparative Analysis of Medical Billing Solutions
Feature
AdvancedMD
Kareo
DrChrono
SimplePractice
Optum360
Cloud-Based
Yes
Yes
Yes
Yes
No
EHR Integration
Yes
Yes
Yes
No
Yes
Specialty Specific
Yes
Yes
yes
Yes
No
Claim Scrubbing
yes
Yes
Yes
No
Yes
Benefits of Implementing Medical Billing Solutions
Adopting automated medical billing solutions can offer numerous benefits including:
Efficiency: Automating regular billing tasks saves notable time.
Accuracy: Reduces the likelihood of errors that may lead to claim rejections.
Financial Insights: provides insights into your billing practices for improved decision-making.
Client Engagement: Purple ties between patients and financial obligations improve overall service delivery.
Practical Tips for Choosing the Right Medical Billing Solution
When selecting a medical billing solution, consider the following:
Understand Your Needs: Evaluate your practice size and specialty.
Check Integration: Ensure it integrates well with existing systems like EHR.
Assess Client Support: Look for vendors offering reliable support and training.
Review Pricing Structures: Compare pricing models to find the moast cost-effective solution that fits your budget.
Conclusion
Choosing the right medical billing solution is an essential step in streamlining your practice and maximizing revenue.With technology evolving at a rapid pace,implementing the right medical billing solution can significantly enhance your practice’s efficiency,reduce errors,and improve financial performance. Evaluate your options carefully, and remember that a well-implemented billing solution can lead to increased patient satisfaction and a healthier bottom line.
By investing in the right tools, you’re not just optimizing processes; you’re investing in the future of your practice.
youtube
https://medicalcodingandbillingclasses.net/simplify-your-practice-top-5-medical-billing-solutions-to-maximize-revenue/
0 notes