#Sanders markx
Text
Sanders markx

#Sanders markx how to
Steve on Migrants are welcome on the island of Martha’s Vineyard….philg on Migrants are welcome on the island of Martha’s Vineyard….Ricky on The Jews of Martha’s Vineyard stand with immigrants and refugees.Wouldn’t that be evidence that Marx was right? Once a country is rich enough, the working class citizens will demand socialism and many of the elites will go along with this. Suppose that Bernie wins the primary elections and then at least wins the popular vote in November. He studies the genetics of psychiatric disorders such as. Americans on welfare today have a far higher material standard of living than did middle class Americans in Marx’s time. Sander Markx is a psychiatrist at Columbia University/Precision Psychiatry which researches more modern treatments of psychiatry. right now is in an unprecedented position of material prosperity. forarallel lamination sled, just tape the sandpaper right onto the mdf board. To make the sleds,ut strips of 150 grit sand paper and taped them down to the top of the mdf board with twosided carpet tape.lso puthin stop block at the end of the sled to help keep the sander from shooting the lamination out the end.
#Sanders markx how to
What if the socialist governments that returned to a market system, e.g., in Russia and China, were not evidence that Marx was wrong, but only that the particular countries that had adopted socialism weren’t rich enough? How To Make A Simple Thickness Sander Build Your. ( the Bolsheviks got a big boost from Germany, though, which may have distorted the natural course of history) It was supposed to be a rich industrialized country that turned socialist and, ultimately, communist, not a relatively poor and just-beginning-to-industrialize country such as Russia. The best that one has been able to say about him was that he was a great historian and sociologist, but a failure as a prophet. Karl Marx remains one of the most referenced and taught authors in Academia today. Author links open overlay panelLiam J.DrewGregg W.CrabtreeSanderMarkxKimberly L.StarkFlorenceChaverneffBinXuJunMukaiKarineFenelonPei-KenHsuJoseph A.Gogos.

0 notes
Text
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
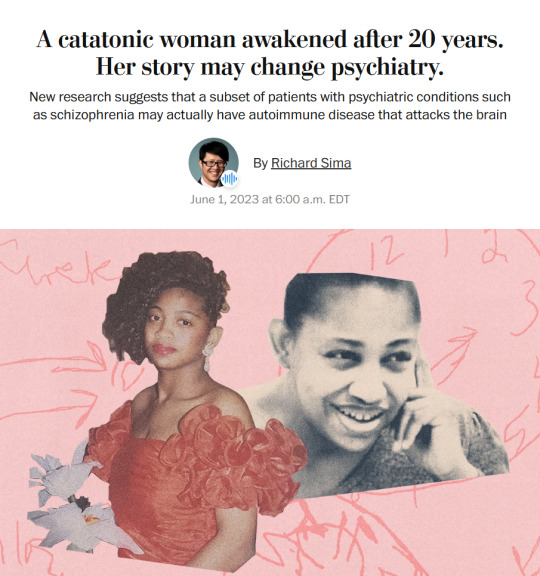
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Text
The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.”
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries reminiscent of a scene from “Awakenings,” the famous book and movie inspired by the awakening of catatonic patients treated by the late neurologist and writer Oliver Sacks.
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other peoplewith similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients,the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.”
– A catatonic woman awakened after 20 years. Her story may change psychiatry.
#block JavaScript in site settings if article is paywalled#April burrel#disability#schizophrenia#lupus#mental illness#catatonia#chronic illness#institutionalization#psychiatry#medical science#healthcare#autoimmune disease#Washington post#knee of huss
3K notes
·
View notes
Text
https://wapo.st/3WLBZPb
A catatonic woman awakened after 20 years. Her story may change psychiatry.
New research suggests that a subset of patients with psychiatric conditions like schizophrenia may actually have autoimmune disease that attacks the brain.
https://www.washingtonpost.com/wp-apps/imrs.php?src=https://s3.amazonaws.com/arc-authors/washpost/c42cbd70-f957-4f16-b5f1-3843b944f86d.png&w=196&h=196
By Richard Sima
June 1, 2023
New research findings suggest that some patients’ psychiatric conditions may be caused or aggravated by underlying autoimmune diseases. It’s hoped that a better understanding of the links between immunological issues and psychiatric conditions like schizophrenia and depression could open new paths to treatments for such patients. Sander Markx, director of precision psychiatry at Columbia University, spoke to The Washington Post about successfully treating patients with schizophrenia and schizoaffective disorder by treating their underlying cases of lupus. One patient was even able to leave a psychiatric hospital where she’d lived for nearly two decades after being catatonic for almost 20 years. The SNF Center for Precision Psychiatry and Mental Health at Columbia is now working on autoimmunity screenings on patients at long-term facilities in New York. Thomas Smith, chief medical officer for the New York State Office of Mental Health, said such analyses could help “save someone’s life, get them out of the hospital, have them live in the community, go home.”
#psychology#psychiatry#illness#healing#schizophrenia#autoimmune disease#Richard Sima#WAPO#body Alive
115 notes
·
View notes
Text
Woman awakens after 20 years in catatonic state. The reason may change psychiatry forever.
Woman awakens after 20 years in catatonic state. The reason may change psychiatry forever.
https://theheartysoul.com/catatonic-woman-awakened-after-20-years/
It was in the year 2000 when medical student Sanders Markx first met April Burrell. At that point, April had already been living in a psychiatric institution for nearly six years. Diagnosed with a severe form of schizophrenia at age 21, she was in what the medical world calls a catatonic state. Twenty years later, […]
The post Woman awakens after 20 years in catatonic state. The reason may change psychiatry forever. appeared first on The Hearty Soul.
via The Hearty Soul https://theheartysoul.com/
May 28, 2024 at 10:16AM
0 notes
Text
Hospitalisée 20ans pour schizophrénie, elle avait en réalité un lupus
0 notes