#catatonia
Text
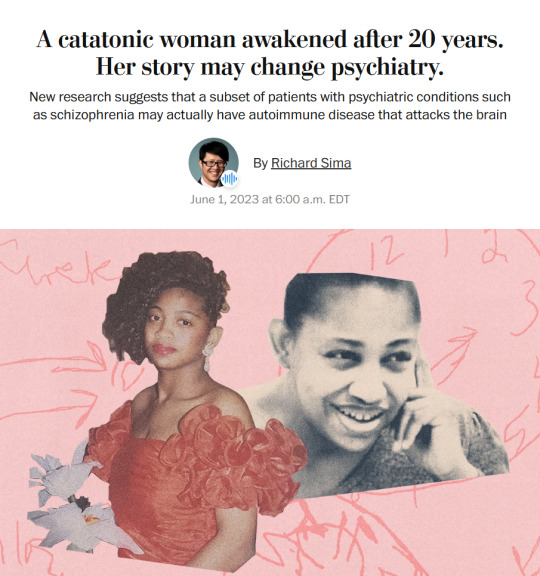
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,�� said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Text
The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.”
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries reminiscent of a scene from “Awakenings,” the famous book and movie inspired by the awakening of catatonic patients treated by the late neurologist and writer Oliver Sacks.
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other peoplewith similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients,the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.”
– A catatonic woman awakened after 20 years. Her story may change psychiatry.
#block JavaScript in site settings if article is paywalled#April burrel#disability#schizophrenia#lupus#mental illness#catatonia#chronic illness#institutionalization#psychiatry#medical science#healthcare#autoimmune disease#Washington post#knee of huss
3K notes
·
View notes
Text
I want people to understand, when I say most of my day is spent in bed, I mean that most of my day is spent in bed. That isn’t bad.
#zebrambles#autism#actually autism#actually autistic#catatonia#physically disabled#physical disability
167 notes
·
View notes
Note
could you share any more under-talked about symptoms of schizophrenia, like executive dysfunction?
I've actually been meaning to make a post like this but keep forgetting (lol that's a symptom). As a disclaimer, not everyone with schizophrenia has every one of these symptoms, and people can have a lot of these symptoms and not have schizophrenia (if they don't have the psychotic symptoms). Not all of these symptoms are seen as diagnostic criteria, some have just been observed to be very common in people with schizophrenia. (I'm excluding hallucinations and delusions because they are more well known)
• Paranoia: a pattern of behavior where a person feels distrustful and suspicious of other people and acts accordingly. This can go hand in hand with hallucinations and delusions.
• Disorganized thoughts: this can mean a lot of things. It can be not having a linear train of thought, having incoherent thoughts, thought blocking, general disorganized thoughts. (It can be hard to define because it is often hard to describe for the person experiencing it).
• Disorganized speech: this is often a result of the disorganized thoughts. This can include loose associations like rapidly shifting between topics with no connections between the topics. Perseveration, which is repeating the same things over and over again. Made up words that only have meaning to the speaker. Use of rhyming words without meaning. Word salad, which is when cognitive disorganization is severe, it can be nearly impossible to understand what the person is saying, but the person speaking doesn't know they aren't making sense.
• Trouble concentrating: lack of concentration, switching from topic to topic, not being able to focus on one thing. (This is pretty self explanatory).
• Movement disorders: catatonia can be repetitive non goal directed movements. It can also be complete or partial immobility, mutism, vacant staring, and rigidity. Although not a symptom, tardive dyskinesia can occur in schizophrenia as a result of antipsychotics medication.
• Anhedonia: a loss of pleasure in activities that the person once enjoyed. Or the inability to feel pleasure at all.
• Atypical or non-existent emotional expression: Flat or blunted affect is an inability to show emotions characterized by a lack of facial expression, a monotone voice, and no hand gestures. On the other hand people can also have inappropriate affect, where the emotional expression doesn't align with typical reactions or even the person's own feelings.
• Alogia: when someone speaks less, says fewer words or only speaks in response to others. This can be a result of disorganized thoughts.
• Social withdrawal: avoiding people and activities that someone once enjoyed. Not actively being present during social situations. Can progress to total isolation.
• Avolition: a severe lack of initiative to accomplish purposeful tasks. This is a big reason some people with schizophrenia can't work/go to school, can't do chores, and can't keep up with their basic hygiene. Even if the person wants to do these tasks, it may be extremely difficult or impossible for them to get themselves to start or complete the task due to the lack of motivation.
• Executive dysfunction: a behavioral symptom that disrupts a person's ability to manage their own thoughts, emotions and actions. This can include focussing too much on one thing, being easily distracted, spacing out, struggling to switch between tasks, problems with impulse control and trouble starting difficult or boring tasks. Several schizophrenia symptoms fit into the umbrella of executive dysfunction, so when researching you will either see the specific ones listed out, or just simply described as executive dysfunction.
• Alexithymia: significant challenges in recognizing, expressing, and describing one's own emotions.
• Poor memory: this can include working memory deficits like trouble planning, organizing, and carrying out daily chores such as running errands, because it requires mentally formulating a “to do” list organized by time and location. Many people with schizophrenia also report trouble with their episodic memory, which means they have trouble recollecting things in the context of their place and time. (A lot of sources say "trouble with memory" is a symptom but they don't specify).
• Trouble with decision making: people with schizophrenia have been shown to have trouble with decision making due to a decline in the understanding and reasoning aspects of it.
• Sensory processing deficits: this has been widely reported in schizophrenia, and include impairments in visual processing, auditory processing, olfactory and sensorimotor systems. This can lead to having strong positive or negative reactions to sensory information.
• Sleep troubles: though disturbed sleep isn't included in the diagnostic criteria for schizophrenia, it is still a significant problem that up to 80% of people with the condition experience. People with schizophrenia may have various sleep problems, including insomnia, excessive daytime sleepiness, and trouble with consistent sleep routines.
• Anosognosia: also called "lack of insight," is a symptom that impairs a person's ability to understand and perceive their illness. This is a big reason people with schizophrenia may refuse to get, or stay with treatment.
#answered#mental illness#nd#schizophrenia#neurodivergent#schizophrenic#psychosis#actuallyschizophrenic#mental health awareness#pseriouslypsychotic#executive dysfunction#paranoia#word salad#avolition#disorganized thoughts#catatonia#concentration issues#anhedonia#flat affect#blunted affect#inappropriate affect#alogia#social withdrawal#isolation#alexithymia#memory issues#sensory issues#insomnia#excessive daytime sleepiness#anosognosia
390 notes
·
View notes
Text
what is (chronic) autistic catatonia?
// why specify “autistic” catatonia? //
catatonia most common associate with schizophrenia, but increase realize also happen in things like bipolar & depression.
if look at some of typical catatonia diagnostic criteria in DSM 5 (but in easier words): catalepsy & waxy flexibility, grimacing (hold same stiff facial movement), mutism, echolalia, echopraxia (copy movement), exaggerated mannerisms, stereotypies/repetitive movements, etc… wait! some of these things happen in autism!!! (like 7 out of total 12 can be seen in autism)
this is why important to know how recognize catatonia in autism. because overlap.
catatonia in schizophrenia most common start fast and get worse fast. but chronic autistic catatonia typically slow onset and slow but visible deterioration. (always have exceptions though)
not know a lot about schizophrenia catatonia, so this post largely focus on autism. everything below, when say “catatonia” or “autistic catatonia,” mean chronic autistic catatonia with deterioration.
// before move on— //
sometimes professionals do connect autistic shutdown with/as catatonia or catatonia episode or catatonia-like episode to draw connection. this not talk about that. this about chronic ones with deterioration. personally for community identity purpose i don’t enjoy (already have term for shutdown). but personal opinion aside, again this about the temporary vs long term all the time. if experience temporary shutdown, remember to leave space for and not same as those of us deal with chronic autistic catatonia.
important to distinguish from autism because autism and catatonia share many symptoms. (for example, physical stimming or “stereotypies” is autism diagnostic criteria AND catatonia criteria). autistic catatonia should only be suspected IF have new symptoms OR change in type & pattern of old symptoms. cannot. stress. this. enough. again. it not about IF you have these symptoms it’s about WHEN and HOW and CHANGE. it's about NEW.
and. please do not diagnose self based on one tumblr post. yes even if i do extensive research and cite sources and have lived experience. many many many disorders look similar. am all here for educated self diagnosis because medical system inequitable BUT am also sick of every time write this a bunch people comment “oh never heard this this is so me.” one tumblr post not educated self dx. it not a cool new thing to add to carrd to hoard as much medical label as can, it miserable it makes my life hell it not a joke it not cool. not every autistic have chronic catatonia, not every shutdown means chronic catatonia, even if you autistic and see these signs, may be separate unrelated disorder altogether, like Infectious, metabolic, endocrinological, neurological, autoimmune diseases, all can see catatonia (Dhossche et al, 2006). some of you all will read this and truly think this is answer been looking for so long—great! still, please do more research.
// chronic autistic catatonia with deterioration and breakdown //
the key defining symptoms of chronic autistic catatonia is gradual lose functioning and difficulty with voluntary movements (shah, 2019, p21). “gradual lose functioning” will come with regression in independence & ADLs & quality of life. it usually gradual, chronic, and complex. but can vary in severity. some need prompts on some day & some situations, while others need prompt and even physical assistance for almost everything.
how common? have seen statistic estimate from 10% - 20% of autistic people adolescents & above experience chronic autistic catatonia.
typical onset for autistic catatonia is adolescence. some study samples is 15-19, some as early as 13. some professionals think this autistic catatonia may be a reason for many autism late regression (Ghaziuddin, 2021).
can happen regardless of gender, IQ (yes shitty), “autism severity/functioning labels” (is what most studies use, so i keep, but yes have issues, probably also mean happens regardless of autism level 1/2/3 and support needs before catatonia, but need more research to confirm since these thing don’t equal eachother).
// primary symptoms //
from book "Catatonia, Shutdown and Breakdown in Autism: A Psycho-Ecological Approach" by dr amitta shah, recommend read at least first two chapter and appendix.
1. Increased slowness
often first sign but not always
periods of inactivity or immobility between actions which appears as slowness, e.g walking, responses (verbal & body), self care, mealtime, etc
2. Movement difficulties (freezing and getting stuck)
difficult initiate/start movement
freeze or become "stuck" in middle of activity for few seconds to minutes
hesitate & "to and fro" movements
difficulty cross threshold/transitions like door way
difficulty stop action/movement once started
affect speech content, fluency, & volume
eat & drink difficult (like movement for fork & knife, chewing and swallowing, etc)
spend long time in one place
(new) ritualistic behaviors
3. Movement abnormalities
repetitive movements like in tourette's & parkinsons
e.g. sudden jerky movement, tremors, involuntary movements, blinking, grimacing, unusual & uncomfortable postures, locked in postures, increase in repetitive movements, etc.
4. Prompt dependence
may not be able to do some or any movement/activity, unable to move from one place to another, unable to change posture, etc without external/outside prompt
5. Passivity and apparent lack of motivation
look unmotivated & unwilling to do stuff, include activities used to like, probably because can't do voluntary action or have trouble with request and make decison.
6. Posturing
classic catatonia symptom of being stuck in one posture, sometimes for hours
7. Periods of shutdown
8. Catatonic excitement
episodic & short lasting
e.g. uncontrollable & frenzied movement and vocalizations, sensory/perceptual distortions, aggressive & destructive outbursts that not like self
9. Fluctuations of difficulty
e.g. some days better can do more need less prompt! other days worse. sometimes emergency can act as almost like a prompt! but fluctuate doesn't mean difficulty voluntary
// secondary difficulties //
Social withdrawal and communication problems
Decline in self-help skills
Incontinence
‘Challenging’ behavior
Mobility and muscle wastage
Physical problems
Breakdown
// autism breakdown //
can be in addition to autistic catatonia. can look like autism is getting worse, even though autism by itself not progressive disorder!
i also call this autism late regression. separate between autistic catatonia & this not very clear, not enough research.
1. exacerbation of autism
1a. increased social withdrawl, isolation, avoidance of social situations
1b. increased communication difficulties
1c. increased repetitive and ritualistic behavior
2. decrease in tolerance & resilience
easily disturbed, irratable, angry
3. increase in "challenging" behaviors
e.g. self injurious behaviors
4. decrease in concentration & focus
5. decrease in engagement & enjoyment
// treatment //
for catatonia (autistic or not), typical treatment is lorazepam and/or ECT.
specific to catatonia in autism, Dhossche et al. (2006) separate it to mild/moderate/severe and give recommend treatment according to that (do not come here and argue about severity labels, because fuck! mild depression and severe depression of course have different suggested treatments and severity important to know. Remember we talk about autistic catatonia).
note: this is one paper! not the only way! yes have problems like most psych/autism papers, just here to give example (of range of symptoms and treatment route!). NOT MEDICAL ADVICE. (not even endorsement)
mild: slight impairment in social & job things without limit efficiency as a whole (essentially still able to function for most part but difficult).
moderate: more obvious struggles in all areas, but ambulatory and don't need acute medical services for feeding or vitals
severe: typically medical emergency, acute stupor, immobility for most of day, bedridden, need other people help feed. also malignant catatonia which can be life-threatening (fever, altered consciousness, stupor, and autonomic instability as evidenced by lability of blood pressure, tachycardia, vasoconstriction, and diaphoresis, whatever any of that means)
the "shaw-wing approach": very brief summary, keep person active and do thing they enjoy, use verbal & gentle physical prompts, have structure & routine.
lorazopem challenge: take 2-4 mg of lorazopem to see changes in next 2-5 minutes. if no change, another 1 mg and reassess
lorazopem trial up to 24 mg. (note difference between challenge & trial)
bilateral ECT, last resort.
mild: "shaw-wing approach" -> 2 week lorazopem trial if no imporvement in 1 month -> if effective, do both, if not, just shaw-wing approach
moderate: depends on prefernece, either shaw-wing alone or shaw-wing and 2 week lorazopem trial -> if not effective, do 2 week lorazopem trial if havent already -> if not, bilateral ECT
severe: lorazepam challenge test -> if not effective, bilateral ECT; -> if lorazopem challange positive, 1 week lorazopem trial -> continue if successful, bilateral ECT if not.
can sound extreme, but rememeber for many severe catatonia (autistic or not), it is medical emergency. can be life-threatening. there's no/not a lot of time.
it possible to make partial recovery, as in get better but not to before catatonia. but overall, many permanently lose previous level of functioning.
references
Dhossche, D. M., Shah, A., & Wing, L. (2006). Blueprints for the assessment, treatment, and future study of Catatonia in autism spectrum disorders. International Review of Neurobiology, 267–284. https://doi.org/10.1016/s0074-7742(05)72016-x
Ghaziuddin, M. (2021). Catatonia: A common cause of late regression in autism. Frontiers in Psychiatry, 12. https://doi.org/10.3389/fpsyt.2021.674009
Ghaziuddin, M., Quinlan, P., & Ghaziuddin, N. (2005). Catatonia in autism: A distinct subtype? Journal of Intellectual Disability Research, 49(1), 102–105. https://doi.org/10.1111/j.1365-2788.2005.00666.x
Shah, A. (2019). Catatonia, shutdown and breakdown in autism: A psycho-ecological approach. Jessica Kingsley Publishers.
#autistic catatonia#actuallyautistic#actually autistic#autism#autistic#long post#catatonia#loaf screm
690 notes
·
View notes
Text
Common experiences that mimic psychosis:
1. Hypnagogic and hypnopompic hallucinations
Hypnagogic and hypnopompic hallucinations are hallucinations that occur upon falling asleep and waking up. They are typically audio or visual. They're fairly common and can happen regularly, occasionally, or only once. Though people with psychosis can have these experiences too, they're not indicative of developing schizophrenia or any psychotic disorder. But they're a good way to empathize with those who do have these disorders and experience hallucinations.
2. Sleep paralysis
Sleep paralysis is a temporary inability to move or speak and commonly includes hallucinations. This experience can be scary, both my nature of being paralyzed and because the hallucinations are often threatening. This is also not indicative of schizophrenia or any psychotic disorder, but it's also a good way to empathize. People with schizophrenia can have catatonia (when a person stops moving) and of course, again, there's the hallucinations.
#schizospec#psychosis#schizophrenia#schizoaffective#mental illness#schizophrenia awareness#hallucinations#delusions#catatonia#sleep paralysis
87 notes
·
View notes
Text
The dissociation is hitting again and it really sucks, I wonder if any other systems have very catatonic switches.
When we are really dissociated we can't move at all and we can't interact with the outside world really.
We're just kind of stuck in our head until it passes which can be a while it really sucks
-Evan (the host)
#did system#did alter#did community#dissociative identity disorder#osddid#dissociation#dissociative amnesia#dissociative identities#traumagenic system#catatonia#mental health
77 notes
·
View notes
Text
Blinded windows
Mere steps behind, beyond barred, blinded
windows, a world inhales, ingests, and
suitably regurgitates those benevolent rays
—
sent forth from their lonely-yet-loving star
as exponentially warming breaths — more
gold lustre means further smiles, themselves
—
then followed by countless beams, until all living
things are ablaze with joy — that is, excepting
he: imprisoned; held perpetual victim to air made
—
fetid through indecision’s grim preservative
influence; four unmarked walls his fixed-
term mausoleum; no burial dirge but pulse-
—
beats barely whispered; blank stare revealing
how completely resignation has quite entirely
taken fully paralysing possession over any
—
cell or thought bearing
strength left for effecting
my escaping this body’s
—
agonisingly
frigid, isolated
persistence
@nosebleedclub February Prompts 29. blank stare
#nosebleedclub#blank stare#poetry#writing#spilled ink#poetsontumblr#my poetry#prompt#depression#catatonia
35 notes
·
View notes
Text
cw, breif mention of self injuries stimming
if your a cr*pple punk whos wants to keep mentally disabled people out your spaces i want you to know that mental disabilities affect people physically too.
i want you to look me in the eyes while im catatonic and cant move anything but my eyes, while i cry over how much my had hurts from writing, while my head feels like its being split open or while im screaming and banging my head into a concrete wall because everything hurts so much and tell me im not disabled enough to talk about my physical symptoms.
i get that you want your own space to talk about your physical disabilities but why can't a mentally disabled person whose physical symptoms stop them from living their life also be a part of that?
#just because its coused by a mental illnesses or nuerodevelopmental disorder dosent mean thr physical symptoms just dont exist#fun fact not evey mentally disabled person is just a little anxious some of us cant leave our houses or even our beds#disability#MERDs#autism#sensory processing disorder#mental health#mental disabilities#physical disabilities#cripple punk#cpunk#cripple posting#catatonia
134 notes
·
View notes
Text
"catatonia"
image: a grey shape of a cat's head, with a red square-ish shape on each side stopping it from moving.
#disability#catatonia#autism#actually autistic#communication symbol#communication image#aac symbol#aac image#aac emoji#custom emoji
20 notes
·
View notes
Text
Autistic Thing of the day:
Autistic Catatonia 😵
I made a TikTok on this too with the same info (link here!)
I wanted to talk about autistic catatonia, which isn’t something I’d heard about until I researched it on my own. When I brought it up to my doctor, she said it made perfect sense.
Autistic catatonia affects, at minimum, about ten percent of autistic people. And the best way I can describe it is “getting stuck.”
I’ve dealt with this my entire life, I plan to do something, or respond to someone, and my mind goes blank and I just can’t move. If I fight it, my anxiety goes through the roof. I can’t talk or respond, only maybe stim a little or communicate using eye contact or eye gaze. For me, it can last anywhere from a few seconds to several hours.
Unfortunately, my bodily functions still continue when I’m stuck, so I have to be guided to the bathroom, need help in the shower, and kept out of harm’s way. My partner and I both have ADHD and have a similar thing happen but can still kind of move even if it's difficult, but that’s more executive dysfunction.
This is also a little different than derealization and depersonalization in that most people still feel entirely like themselves when these episodes happen, your inside mentality is the same. I can carry on commentary in my head during these episodes and I feel like I'm myself, just stuck.
Being catatonic is almost like every cell in my body is frozen in time. I know what’s going on around me, but my brain just can’t make that connection and that spark of purposeful movement doesn’t make it outside of my own mind. I wish there was a better way to explain it.
A lot of autistic people experience this differently. Some people have this and believe it's a shutdown (which is a little different because in shutdowns usually you can communicate.)
People with mild catatonia may feel like they've "gone nonverbal" and also feel physically stuck, although others can assist you to move if needed.
A lot of people have this experience when they're frightened of experiencing high levels of overstimulation. I've always said it's like my brain pressed pause on my life, because I wouldn't.
If you know someone who goes through something like this, make sure they stay safe, hydrated, and make sure to check in on them even if they don't respond. I like when my partner acts like nothing’s up, he will just hang out with me there. Some people like touch when they get stuck while others don’t. This can happen no matter what your support need level is in general. This actually happens often enough where it increases my support need level, I need to be supervised anyway. 😅
Once I realized this was a feature of my autism, I was able to come up with a plan with my loved ones because it happens about 2-3 times a week. Ever since I started taking ADHD meds it happens less, and research has found that benzo medications can actually prevent this from happening and help the episodes. Research needs to catch up to the rest of us on this one!
But if you experience this or periods of hyperactivity where you also feel like you can't interact with others on your own command, it may be autistic catatonia.
Hopefully this helps someone! 🤟🏻
#actually autistic#autism#autistic catatonia#catatonia#neurodivergent#adhd#audhd#ptsd#autistic thing of the day#dan.posts#autistic#autism things#autistic adult#high support needs#actually disabled
312 notes
·
View notes
Text

'Catatonia'. Filipe Pagliuso.
26 notes
·
View notes
Text
Other dissociative symptoms include uncontrollable daydreaming or frequently getting lost in your thoughts, spacing out, feelings of being unreal or that your surroundings are unreal, feeling disconnected from aspects of yourself such as your emotions or physical sensations, regularly experiencing brain fog, recurrent gaps in your memory.
These symptoms are significant enough that occur on a regular basis and get in the way functioning, so much so that you have to accommodate for them. They cannot be explained by physical causes, such as drugs or head trauma. They can be the result of any mental disorder, such as BPD, DID, autism, ADHD, and more! Dissociation is debated a lot in the psychology community, but for now, we'll treat it as a phenomenon that everyone experiences at least once but can become pathological.
Please reblog for a larger sample size! ᐠ( ᐛ )ᐟ
(This poll may not be the best. I didn't want to include another option, but you can still write your answer in the tags if you'd like.)
#polls#post#actuallydid#dissociative identity disorder#dissociation#actually dissociative#depersonalization#derealization#catatonia
20 notes
·
View notes
Text
People will be truly supportive of my autism until I mention that my autism is personally regressive and getting “worse” then they suddenly aren’t ally’s because autism definitely can’t get worse and stays the same with everyone. Like what?
#zebrambles#catatonia#autism regression#autism catatonia#autism#autistic#actually autistic#actually autism#medium support needs
139 notes
·
View notes
Text
That Mrs. Robinson skit is doing the rounds again and rightly so, but may I humbly present msheen doing the Joker dance to International Velvet.
He is the most unhinged when he is on this show and it is glorious.
#michael sheen#joker#there's something about movies#i love him your honour#catatonia#International velvet
46 notes
·
View notes
Note
I am wondering what catatonia feels like for you, if you don't mind answering. Hope you are doing well and once again wanted to tell you how important your voice is on this site.
heheh thank you, nice to see u again
gonna talk about general info about autistic catatonia and personal experiences. all the non-personal experience info are from book catatonia, shutdown, and breakdown in autism by dr amitta shah, i very much not far in book but will summarize what i read so far.
so. experience autistic catatonia. which can look different from classic acute & severe catatonia in disorders like schizophrenia (preface/p. 17). so can't speak about that kind of catatonia. but personally also have apraxia and dissociation/dissociate from body, so have hard time separate catatonia experiences from apraxia from dissociation sometimes.
types of catatonia in autism outlined by dr shah (p19-25)
1. chronic catatonia & catatonia-type deterioration and breakdown
change & deteriorate in ability to make voluntary movements & activities, to point where affect daily functioning, independence, behavior, quality of life, etc.
also occur w regression of skill & independence
may not show classic signs of acute catatonia
2. acute catatonia (general)
aka the classic signs of catatonia
3. catatonia as shutdown
temporary shutdown of social interaction & communication during acute stress & get back to normal after stress pass
4. episodic/lifelong catatonia-type difficulties
not deterioration/breakdown but have chronic or episodic difficulty start movement & activities
5. catatonia features
not necessarily diagnostic of autistic catatonia especially if don't have deterioration or affect independence
so personally. when i say autistic catatonia, mean #1, chronic catatonia. have trouble voluntarily control own movements and also deteriorate so much.
don't really mean #3. although also experience it sometimes. autistic community call it "autistic shutdown" more and like that more because distinguish from chronic autistic catatonia.
primary difficulties & manifestations of autistic catatonia (p29)
increased slowness (in walking, response, self-care, etc)
movement difficulties (diffcult initiate, freezing & getting stuck, hesitations, difficulty crossing thresholds, difficulty stopping movement, may affect speech & eating)
movement abnormalities
prompt dependence
passivity & apparent lack of motivation
posturing
periods of shutdown
catatonic excitement
fluctuation of difficulty
personally pretty much experience all of them, except for maybe #6 posturing and #8 catatonic excitement? (also don't have a lot of trouble cross threshold like go through door and such), or at least only very mild forms of 6 & 8.
personally. get stuck a lot. have trouble start thing, from get out bed to brush teeth to do homework etc, all the big and small things. sometimes want to say thing and can't get body to say thing. may freeze mid action, like typing this post, do it very slowly because freeze in between every few words. sometimes mid doing things, just start staring and freeze in the position i hold.
biggest way to describe is just. get stuck all the time. stuck in head. freeze. body inclined to stay still, have really hard time control. so many times stay in head and stim inside head when can't stim with body because can't control body.
literally like newton's first law!!!!! objects at rest will stay at rest, object in motion will stay in motion (unless acted upon by an external force aka in this situation prompts).
need a lot of prompts. verbal or even physical prompts from other people. habit charts and behavior charts and phone reminders and even alarms don't work. need someone prompt.
autistic catatonia + communication difficulties mixed together means that rarely initiate conversation (either no interest or catatonia can't), need specific concrete questions, can't answer general vague big questions. literal stuck when asked big vague questions. sometimes stop talking/freeze when finish answering the explicit part of the question bare minimum and physically cannot continue elaborate unless someone ask another follow up question for prompt (other times don't recognize need to say more but that's more autism communication differences).
somedays good days and body more unlocked. many many many days body stuck.
not really fun.
#autistic catatonia#actually autistic#actuallyautistic#level3 autism#high support needs#level 2 autism#medium support needs#moderate autism#catatonia#nd#asd#autism#autistic#actually neurodivergent#loaf screm#answered
448 notes
·
View notes