#What are the 5 stages of kidney failure?
Text
I also spend a lot of time trying to convince people to prevent problems, because prevention still works better than cures. Don't fucking smoke! I would instantly become the best doctor who ever lived if I could just convince all my patients to quit smoking. Avoid alcohol! Don't do meth! Don't do fentanyl! Things that are poisons will poison you in ways you understand, in the short term, but also ways you can't really understand until you've watched dozens of people die from it thirty years later, struggling to breathe from their COPD or weak and nauseated beyond bearing from their end-stage liver disease. I watched a man take 3 weeks in the ICU to die from what meth did to his heart. Your heart isn't meant to beat 145 times a minute for weeks on end. Your liver isn't meant to metabolize 5 shots of gin a day. You aren't going to be able to use denial and willpower to repair the damage your own habits did.
I drink a lot less now than I did before I went into medicine. Lot of different reasons, including that I'm older and more settled. But I can't look at it the same way I used to; I can't brush off as a "fun quirk" what I know is alcohol use on a level that risks withdrawal seizures if they were to suddenly stop, like some of my family members do, nervously asking me about their loved one's drinking when we're alone because beneath the jokes they know it's a problem.
If you're having more than one, maybe two drinks a day on average, over a long period of time, you are damaging your body in ways you don't understand. You're setting up a permanent heightened inflammatory state. Your heart cells don't like alcohol; Google "alcohol-induced cardiomyopathy." Your esophagus and stomach respond to incessant bathing in poison by first developing wounds and then cancer. Your liver, of course, doesn't like it. Your liver not only converts poisons to harmless substances you can excrete, it also makes your platelets, so your blood can clot. It makes albumin, a protein that's essentially for keeping water in your blood vessels and not letting it leach into your tissues. So people who are dying of liver failure are in pain and weak and tired and sad the whole fucking time! And the only solution, a liver transplant, will come with a lifetime of medication and specialist check-ups and the knowledge that if you fuck up and kill this liver, too, no one is going to be eager to give you another try.
I don't guilt-trip my alcoholic patients with liver disease. I don't guilt-trip my smokers with COPD. They chose to cope with substances for reasons, even if I disagree with their reasons, even if those reasons are opaque to me. They will suffer the natural consequences of those actions whether I guilt-trip them or not. I want them to continue to see me, I want them to be honest with me. Other people will lay enough guilt on them. And nothing I can say or do would ever compare to the physical and mental suffering that goes with those diseases.
But if you can prevent these diseases in yourself, prevent them. Quit smoking. Do it now. Your lungs are going to look better starting almost immediately, with positive changes continuing for many years. Drink less alcohol. Sure, it's fun, sure, it's a longstanding human tradition, but it is also unfortunately a straight up poison and your body knows that no matter how persuasively you argue about the obvious failure of Prohibition. You can't argue with a cell. You can't convince your kidneys that high blood pressure shouldn't damage them. They are a system; they do what they do; they existed long before prefrontal cortex existed to justify what we want to do but know to be harmful.
1K notes
·
View notes
Text
If The Lamp's theory about the DHMIS world being a sort of purgatory is true, then this is what I think life might've been like for Duck and Red Guy before joining Yellow Guy/David.
(TW: mentions of suicide)
Duck:
Was a Sergeant and an Air Pilot in the British Mililary during WW2, hence why he is so fixated on it. As shown in DHMIS 2, Jobs, and Death.

Forged medical/enlistment documents, which lead to many deaths, a fact he tried to suppress in his mind, as referenced in "Worm in Our Brain" song.
Developed PTSD after the war, filled with regret over his actions during it. Wanted to establish a "digital currency based on respect" to make up for his actions.
Had constant fighting within his biological family, though he was in denial about this, as shown in Family.

Always wanted to be a father figure, but he never had the chance, hence why insists on being "the father" in Family.
Had a fascination with space, conspiracy theories, and the rapid expansion of technology, as referenced in Jobs, DHMIS 2 and possibly Death.
He had a blackbelt in Karate, as shown in Death.
Was a fan of James Bond, as shown on his poster in his "customized area" in Transport.
Secretly performed drag at underground bars for money, as shown in Family in his infamous crossdressing scene.
Won a tournament at some point, as referenced in Death.
Had bouts of rage due to PTSD, often resorting to biting others. (Yellow Guy would compare this behaviour to a dog whenever he visited his father, hence why Duck appears as one in the flashback in Transport.)
Witnessed Yellow Guy/David's death in a nearby (retirement?) home next to Roy. (Next to another full house/orphanage? Possibly the origins of the teachers?) As shown in the flashback in Transport.
Developed diabetes at some point, and died from kidney failure (a lack of water). Both are referenced during Death and Electricity.

Red Guy:
Worked a 9 to 5 office job that he hated and felt pressured into working, as shown in DHMIS 6. Eventually he climbed up the cooperate latter, becoming the boss, but he was still miserable, as referenced in Jobs.
Lived in a small community in England in the 40's by himself. As referenced in Transport, where Red Guy subconsciously wants and tries to return to "Clayhill."


Mostly lived an uneventful life.
Enjoyed puppet shows, junveille songs, and child-like hobbies, but he was rejected for this interest. He ended up developing a sense of apathy as an attempt to fit in, as referenced in DHMIS 6.
Enjoyed cooking as a hobby, as referenced in Death.
Often attended bars, where he would try to express his creatvity through dancing and singing. Unfortunately, he was frequently booed off stage, as referenced in DHMIS 6.

Was another witness to Yellow Guy/David's death.
Died as a result of suicide because of repeated rejection by his peers/family, drowning himself in a nearby lake, as referenced in Death and Family.
On a final note, I think Lesley might've worked at the Vaccum Cleaner Shop before she died? I think it would explain her fixation on inanimate objects. The figurine even looks like her.
#dhmis#dont hug me im scared#dhmis red guy#dhmis duck#dhmis analysis#dhmis theory#dhmis purgatory#ramblings
715 notes
·
View notes
Text
Shadow left by COVID-19 pandemic on the future - Republished Aug 1, 2024
The rapid global spread of vaccinations for coronavirus disease 2019 (COVID-19), the development of effective anti-COVID-19 drugs, and the establishment of treatment for preventing and managing severe cases have become great game changers in bringing the COVID-19 pandemic to an end, leading us into a life of coexistence with COVID-19, namely “with COVID-19 era”. Now is the time to look back and examine what happened during the COVID-19 pandemic, how healthcare, society, and culture were affected, and what problems have been left for the future.
In 2020, in the early stages of the COVID-19 pandemic, it was reported that the COVID-19 virus utilizes ACE2 as a receptor when infecting host cells [1]. Because there were earlier experimental studies in which ARBs and ACE inhibitors increased ACE2 expression in animal tissues, some researchers considered that COVID-19 infectivity may be augmented in patients with hypertension or heart failure who are taking these drugs [2]. Based on this hypothesis, concerns that ARBs and ACE inhibitors might be risk factors for COVID-19 infection and worsening spread through SNS and some mass media. In fact, during the first wave of COVID-19 infections in the Europe, not a little number of patients self-discontinued taking ARBs and ACE inhibitors. Therefore, the Japanese Society of Hypertension and Japanese Circulation Society, as well as the European Society of Cardiology, European Society of Hypertension, and American Heart Association released urgent statements as academic specialists that ARBs and ACE inhibitors prescribed under the guideline-directed medical treatment should not be discontinued [3, 4]. Thereafter, numerous observational and registry studies conducted in countries around the world, including Japan, showed that ARBs and ACE inhibitors had neutral or negative impact on infectivity or severity of COVID-19 [5, 6], confirming that these statements were correct. Kai et al. conducted a systematic review of animal studies including 88 articles and found that administration of ARBs and ACE inhibitors, as well as other antihypertensive drugs, rarely increased ACE2 expression or activity in the tissues, including the hearts, kidney, arteries, and lungs, of the intact animals and animal models of hypertension or heart, kidney, and vascular diseases [7]. In this issue of Hypertension Research, Natsume et al. reported that the number of ARB and ACE inhibitor prescriptions did not decrease, but rather increased, during the COVID-19 pandemic in Japan, based on the Japanese National Database (NDB) Open Data [8]. This finding suggests the importance of academia to take a decisive stance in pointing in the right direction based on scientific evidence and expert consensus to the public and practitioners in emergency situations such as COVID-19 pandemics, and is proof that proper medical care has been achieved in Japan during the pandemic.
Read the rest and get the references at either link!
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#still coviding#public health#wear a respirator
5 notes
·
View notes
Text
Here's something that I doubt everyone knows about the disability crisis in the United States. For a civilian to get disability payments, they have to be "totally" disabled; in other words, you have to prove you cannot get any job in any industry based on Department of Labor statistics in your state, not *just* that you have a debilitating condition. For a veteran to get disability payments, they have to prove a percentage of how disabled they are, and getting 100% disability as a veteran is no easy task wording is critical in the documentation if anyone at any point in your medical history intentionally or not downplays your disability you will get percentage points taken off how much pay you get as a disabled veteran. This is particularly difficult for people with any pride or dignity left because, in both civilian and veteran cases, you must explain just how awful it is in explicit terms and quantifiable, dehumanized ways to sate the court's interest, or you will not get "total" disability. Furthermore, until you are considered "permanently" disabled, you must repeat this process every 3-5 years. Yet, again no one anywhere can talk about you improving or you're out (for civilians), or your disability percentage amount is reduced (for veterans.) Also, if you manage to prove a "permanent" disability, you still get checked every seven years to make sure it's still "permanent." Finally, to get your student loans discharged as a civilian, you must prove your disabled status is both "total and permanent," guess what if one of those changes? Those loans come right back. Also, your loans go into forbearance if you're" totally disabled" and not considered "permanent" or "short-term" (more than 2 weeks, up to a year). Yes, that is the one that accrues interest. Not deferment. For short-term disability, you can defer, but if you're long-term, non-permanent, you forbear. Most people on long-term disability are medically permanently disabled but not in the eyes of the law because of their age, even if it is a chronic or progressive disease. This is why people die waiting for total disability, let alone permanent. My disability attorney said straight to my face 10 years ago, "You should get disability because you have a chronic disabling condition in two systems, but it's going to be a fight because you are so young." I was 28, by the way. She said if I had "just Lupus" or "just medication-resistant dysthymia and generalized anxiety," I wouldn't have stood a chance. My cousin "just" had Lupus and was in end-stage renal failure, it took her 3 years to get disability, and by then, she had a kidney transplant. She was in her 20s and on her parents' insurance. I have a friend whose veteran husband couldn't get 100% VA disability because some doctor at some VA clinic years ago had written down "mild back pain" when describing the pain he felt from degenerative disc disease and 2 herniated discs. It took years to get that one note out of his file. No matter what any other doctor said. So when I say you can't comprehend the disability crisis in the United States, I'm talking about this. Thanks for coming to my TED Talk.
18 notes
·
View notes
Text
15 questions, 15 mutuals
Thanks for the tag @apothecarose!
1. Are you named after anyone?
Not intentionally. My first name is my cousin's middle name and my middle name is my aunt's (her mom) middle name.
2. When was the last time you cried?
Like 3 hours ago because Spouse was yelling to me about my hoodie that I left somewhere randomly after they asked me to throw some towels in the wash and I just got overwhelmed. Yay depression!
3. Do you have kids?
no
4. What sports do you play/have played?
I played roller derby in Milwaukee's rec league. I want to get back into it now that I'm in Chicago (I had a problem with the Brewcity Bruisers, which is why I stopped), but I'm not sure my body will let me.
5. Do you use sarcasm?
Never, lol
6. What's the first thing you notice about people?
Maybe eye color? IDK
7. What’s your eye color?
green
8. Scary movies or happy endings?
Happy endings. I cannot stand scary movies.
9. Any talents?
I can sing and I used to play violin. I'm also a pretty good email developer (one of my superiors called me a powerhouse). Hello Fresh has made me decent at cooking too.
10. Where were you born?
Kenosha, WI
11. What are your hobbies?
reading, knitting, cross stitch, designing cross stitch patterns
12. Do you have any pets?
2 dogs and a cat
Lola Lou:

She's a Pitbull/AmStaff/Boxer mix. She's 11 (her face is more gray now). She used to be my mom's dog, but I insisted on taking her after she passed away.
Mable Ann:

She's half German Shepherd, half 13 other breeds, including 2% Basset Hound, thus the short legs. She's 4.
Meeah May:

She's a Turkish Angora mix. She'll be 17 next month. She's old, crotchety and refuses to die, despite having asthma and stage 1 kidney failure.
13. How tall are you?
5'2"ish
14. Favorite subject in school?
Choir and photography
15. Dream job?
Singer or Music Director at WXRT. But honestly, I really enjoy my job because the only day I worked most of the day this week was yesterday. Monday, Tuesday and today I did a little work in the morning and had literally nothing else to do for the rest of the day. I'm also really good at it and the rest of the marketing team all really appreciates and is impressed with my work and who doesn't love hearing that?
I guess I'm supposed to tag 15 people, most of which I'm sure will have already been tagged, so here goes: @a-noble-dragon, @catandherfandoms, @flamingohistorian, @beck404, @jettestar, @mallpretzles, @ramonaflow, @grapehyasynth, @goodiecornbread, @hullomoon, @tyfinn, @jesuisici33, @madlori, @olinsghost and @jamilas-pen No pressure, obvs
7 notes
·
View notes
Text
Mornings
As I sit in the bathroom, I find my eyes have fallen on a very old steel step. It folds out into 3 steps, and has a handy seat on the top step. The seat is fake leather, and I know it over 35 years old. It was my wife's when we started living together. I see splashes of paint, and I remember each one, the color, the room, and yes even the house.
It takes me back a bitter road of love.
The first color come from our first house. I can't say it where we fell in love, because we leaped into love. We were perfect together.I learned when people say a relationship takes a lot of work, they have no idea what they are talking about. We were married 29 years, and never had one major fight. We were like 2 perfect gears together.
Another color is from our second house in Colorado. We moved there because she missed her mother. We found that even though she lived across the alley from her son, she was unable to take care of herself. She was messing up her meds and had fallen and broken her collarbone. We decided to find a house to suit both mom and us.
We found a home that we loved. It was quite a drive from where I worked, about 120 miles round trip, but it wasn't about me. We moved mom with us, and my new barn became a home for a lot of junk, and my 1968 Chevelle convertible. I didn't drive it much, because it sucked gas like a vacuum cleaner. I drove back and forth to work everyday, until she was diagnosed with cancer.
She had been feeling run down for almost a year. Finally her doctor had a bone marrow test, and a pet scan. It was non-Hodgkin's lymphoma, and it was stage 4. I turned in for retirement to take care of her. We could not make the mortgage payment, and decided to move. Mom had passed in 2013, her last years in a home for people with dementia. Enough said.
We put the home on the market. It took almost a year to sell it. I had researched other places to live. She had live in Colorado all her life except the time she lived with me in California. She told me that she wanted to move out of Colorado, because this wasn't her Colorado anymore.
We ended up selling and buying very quickly. One home that I had looked at was the one I am sitting in right now, although not in the bathroom anymore. We got moved and she found a fantastic doctor. He said she needed another round of chemo, and we had a meager Christmas that year, facing another round of sickness, loss of hair, well, you get the idea.
She went through 4 treatments. She wasn't that sick, and lost little hair. After the treatments she was declared cancer free. We celebrated, but I had reservations. I knew this type of cancer comes back from experience.
It did.
It came back 4 times. She went through chemo, having her spleen out, septic shock from an UTI, and the death of her best friend. The 4th time she had started chemo, and got infections through her PICC line, put in for the chemo.
She went into the hospital again with infections. She had done this 3 times already. I didn't know this was the last. I watch as she had ups and downs, 18 days in ICU. About 5 days before she lost the fight, she told me she was so tired of fighting. I knew in my gut I was going to lose my bride. She rallied about 3 days before the end, but I knew this happens sometimes. The doctors tried one last treatment to fight the bacterial, fungal, and yeast infections in her blood and lungs. I agreed, but the drug killed her already weak kidneys. The last 2 days I told her she could go. I prayed for her to go, as terrible as that sounds. I knew she had a fear of dialysis, and told me many times she wasn't going to live like that, having watched her first husband died from kidney failure.
Everyday I go up and sit by her bed, once she was sitting up, but had to have help even to stand. The last few days as she went in and out of reality, I'd sit and quietly sing to her. When I sang "Nights in White Satin", she'd smile, except the last 2 days, but I sang to her anyway.
I was called to the hospital because they said she was going. I cried all the way there. I sat until 3 am on 5/5/2022. I had to go home and take care of our animals. I intended to come right back, but like an idiot, I sat down. I woke at 8:30 am, and got in the truck. At 8:45, the nurse called and said she had passed at 8:40 am.
She had told me many times she didn't want me to sit and watch her die. Well Angel, I never denied you anything.
Rest in Peace my Love.
2 notes
·
View notes
Note
Hi Wayfaring! My dad found out that he has kidney disease from his autoimmune disease getting worse. We hear a lot of terms like kidney function % and protein being in his urine. Would you please do a lil rundown on kidney disease and what these things mean? Can kidney function improve and can the cells regrow or is it just that he needs to stop it getting worse because they can’t be repaired? Thank you :)
Ok, here’s some basic definitions for kidney disease:
- GFR or creatinine clearance: a number indicating how well the kidneys are filtering proteins and other wastes out of the blood. A normal GFR would be >60. When they’re talking about % of normal kidney function that’s more of a layman’s term and isn’t as specific.
- chronic kidney disease: broken down into stages defined by GFR or creatinine clearance. Stages 1 and 2 are essentially normal kidney function. Stage 3 (3a is a GFR of 45-59. 3b is GFR of 30-44) is where we start having to adjust dosages on certain drugs because the kidneys don’t clear them as quickly as normal. Stage 5 (GFR of <15) is end stage renal failure, where a person would be on dialysis and/or a transplant list.
- protein being in the urine is basically from leaky filters. There are lots of things that can cause protein in the urine.
Kidney function can improve depending on what is damaging it. In the case of an autoimmune disease, it typically clogs up the filtration system with antibodies, so as the antibodies decrease, the filtration improves. The problem comes when things get so clogged up that the tissue can’t get adequate oxygen and dies. That would not be reversible and the kidney does not regenerate like the liver does. Knowing whether the damage was permanent or not would really require a kidney biopsy. Ultimately with kidney disease you try to slow down progression of disease as much as possible to prevent having to move to dialysis or transplant.
15 notes
·
View notes
Note
hi I wish you the best ❤️ this sounds like a really stressful situation and I hope you can get what you need
thank you so much! im really happy and overwhelmed (positive) by all the kind words and support I’ve received and were nearing 1,500 usd in donations already. im holding on and just trying to ignore bad feelings and cope with jokes :) also however grim, just thinking about things i wanna catch up on so im looking forward to watch, read and see things i always put off. i have a year before stage 5/total kidney failure so i wanna make it a good one :)
5 notes
·
View notes
Text
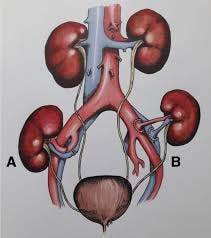
Best Hospital in Lucknow for Urology & Kidney Transplant- Wellsun Super specialty Hospital
Urology is a medical specialty that focuses on the diagnosis and treatment of conditions related to the urinary tract system in both males and females. This includes the kidneys, bladder, ureters, and urethra. Urologists are trained to manage various urological conditions such as urinary tract infections, kidney stones, prostate problems, and urinary incontinence.

Kidney transplant, on the other hand, is a surgical procedure in which a healthy kidney from a donor is transplanted into a person with end-stage kidney disease. This procedure is typically performed when other treatments, such as dialysis, are no longer effective in managing kidney failure. Kidney transplant offers the potential for improved quality of life and long-term survival for individuals with kidney failure.
It's important to consult with a qualified urologist or transplant surgeon for personalized advice and treatment options related to urology and kidney transplant.
What our expert say’s
Urology is a medical specialty that deals with the diagnosis and treatment of conditions related to the urinary tract system in both males and females. This includes the kidneys, bladder, urethras, and urethra. Urologists are trained to manage various urological conditions, including but not limited to:
1. Urinary tract infections (UTIs): Symptoms may include frequent urination, pain or burning during urination, cloudy or bloody urine, and a strong urge to urinate.
2. Kidney stones: Symptoms can include severe pain in the back or side, blood in the urine, frequent urination, and pain during urination.
3. Prostate problems: Common conditions include benign prostatic hyperplasia (BPH) and prostate cancer. Symptoms may include difficulty urinating, weak urine flow, frequent urination (especially at night), and blood in the urine.
4. Urinary incontinence: This refers to the involuntary loss of urine. Symptoms can vary depending on the type of incontinence but may include leakage during physical activity, coughing, or sneezing, frequent urination, and a sudden strong urge to urinate.
5. Erectile dysfunction: This is the inability to achieve or maintain an erection sufficient for sexual intercourse. It can be a symptom of various underlying conditions, including vascular disease, diabetes, or psychological factors.
It's important to note that these are just a few examples, and there are many other urological conditions with their own specific symptoms. If you are experiencing any urological symptoms or concerns, it is recommended to consult with a urologist for proper evaluation and diagnosis.
Feel Free to Call Our 24*7 Consultant ,
email id- [email protected]
Mobile no : 18008991200,+91-6389010203
#hospital#medicine#multispecialityclinic#wellsun#healthcare#health tips#medical care#health and wellness#doctors#city
2 notes
·
View notes
Text
tell me why I had to learn through a TIKTOK that ppl with sickle cell trait (the thing I have) shouldn't stay in high altitude areas for long bc it makes the blood cells sickled and without treatment this can lead to KIDNEY FAILURE. this girl stayed in the Guatemalan mountains and then came back to America and was consistently sick for 5 years before a black woman doctor discovered that the sickle cell had damaged her kidneys and she was in early stages of kidney failure
and keep in mind the only thing I have ever been told abt SCT is that I need to do genetic testing w a partner so our kid doesn't have SCD. I have been told that there are no other symptoms when there are actually plenty apparently. black athletes sometimes just drop dead on the track from this bc of the exertion. it's a good thing I'm lazy as fuck bc apparently youre supposed to pace yourself and not do too vigorous exercising bc there's also a 50% increased risk of muscle breakdown. what the fuck. why have I had to learn abt this thru Google and tiktok. what the fuck
4 notes
·
View notes
Text
Kidney Failure Treatment Without Dialysis: Alternative Medication To Treat Kidney Failure

Chronic Kidney Disease (CKD) and Its Complications
Chronic kidney disease (CKD) refers to the gradual loss of kidney function over time. The kidneys play a crucial role in filtering waste and excess fluids from the blood, which are then excreted in urine. When renal function diminishes, harmful levels of waste accumulate, leading to various health complications. Early diagnosis and chronic kidney disease treatment are important to slow the progression of the disease.
CKD is classified into five stages based on the estimated glomerular filtration rate (eGFR), which measures how well your kidneys are working. Stage 1 indicates mild kidney damage, while stage 5 indicates kidney failure, where there is a need for Treatment for kidney failure. Many factors can lead to CKD, including diabetes, high blood pressure, and genetic conditions. As CKD progresses, it can cause serious health problems, such as high creatinine levels, high blood pressure, anaemia, bone disease, and heart disease.
Complications of Chronic Kidney Disease
Anaemia: Healthy kidneys produce a hormone called erythropoietin, which helps in red blood cell production. When kidney function declines, anaemia can result, causing fatigue, weakness, and shortness of breath.
Bone and Mineral Disorders: CKD can disrupt the balance of calcium and phosphorus in the blood, leading to bone weakness and fractures.
Addressing these complications requires a comprehensive chronic kidney disease treatment plan that may include medication and lifestyle changes.
What Is High Creatinine in Kidney Disease?
Creatinine is a waste product produced by muscle metabolism, and healthy kidneys filter it from the blood. When kidneys are damaged or functioning poorly, creatinine levels in the blood rise. High creatinine levels are often an indicator of impaired kidney function or chronic kidney disease.
For kidney disease patients, managing high creatinine levels is critical as it reflects how well the kidneys are filtering wastes. Measuring creatinine levels is a common way to assess the stage of CKD and monitor disease progression. Also, you have to take homeopathy high creatinine treatment.
Home Remedies to Control High Creatinine Levels
In the absence of kidney failure, there are several home remedies to control and reduce high creatinine levels that can be used to improve kidney function and reduce pressure on the kidneys.
Reduce Protein Intake: High-protein diets can increase creatinine production. By reducing the consumption of red meat and other high-protein foods, kidney patients can reduce the load on their kidneys. However, always consult with a healthcare provider before starting any herbal high creatinine treatment.
Eat a Low-Sodium Diet: Salt can increase blood pressure and cause fluid retention, both of which can exacerbate kidney damage. Eating a low-sodium diet can help manage blood pressure and reduce the workload on the kidneys.
Avoid Strenuous Exercise: Over-exercising can lead to elevated creatinine levels as muscles break down and produce more creatinine. Moderating physical activity can help control creatinine production.
These home remedies are most effective when combined with a prescribed homeopathy kidney problem medication regimen. Lifestyle changes and dietary adjustments are essential parts of any chronic kidney disease treatment plan.
How Is High Creatinine Harmful for Kidney Patients?
High creatinine levels in kidney patients are indicative of decreased kidney function, but they also contribute to various health risks. Elevated creatinine can lead to the following problems:
Worsening Kidney Function: When creatinine levels remain high, it signifies that the kidneys are struggling to perform their job, potentially speeding up the progression toward kidney failure.
Increased Risk of Cardiovascular Disease: High creatinine is associated with an increased risk of heart problems in CKD patients. The buildup of waste products in the bloodstream can lead to inflammation and damage to blood vessels, increasing the likelihood of heart disease and strokes. This way, You have to suggest adopting kidney failure treatment without dialysis.
Toxin Buildup: With higher creatinine levels, other toxins also accumulate in the body, leading to nausea, fatigue, loss of appetite, and confusion. This can reduce the quality of life for kidney patients and increase the likelihood of hospitalization.
Fluid Imbalance: High creatinine levels may indicate impaired kidney function, leading to the retention of fluids. This can cause swelling in the legs, hands, and face and also increase the risk of high blood pressure and heart failure.
In severe cases, if high creatinine levels are not managed, patients may progress to end-stage renal disease (ESRD), where the kidneys are no longer able to filter waste. At this stage, Treatment for kidney diseases typically involves either kidney failure treatment without dialysis.
Treatment for Kidney Failure Without Dialysis
One of the most common concerns for patients with advanced CKD is whether there is a cure for chronic kidney disease or a way to manage kidney failure without dialysis. Some patients seek alternatives due to the restrictions and lifestyle changes dialysis imposes. homeopathic Treatment for kidney failure and lifestyle modifications may help delay or even avoid the need for dialysis:
Dietary Changes: A renal diet that restricts protein, sodium, and phosphorus can help reduce the strain on kidneys and slow the progression of CKD. This type of diet, combined with appropriate homeopathic kidney problem medication, is often a key part of cure for chronic kidney disease.
Lifestyle Changes: Regular exercise, quitting smoking, and managing stress are critical factors in maintaining kidney health.
Unfortunately, there are many cures for chronic kidney disease. However, with early intervention and the right chronic kidney disease treatment, patients can significantly slow the progression of CKD and maintain their quality of life for longer periods without needing dialysis.In conclusion, managing kidney disease and high creatinine levels requires a homeopathic holistic approach that includes medical intervention, dietary changes, and lifestyle modifications. Effective treatment for kidney failure is possible in the early stages, offering hope for patients looking to maintain their kidney function and health.
0 notes
Text
Understanding High Blood Pressure Symptoms and What They Mean for Your Health
High blood pressure, also known as hypertension, is a common yet serious condition that affects millions of people worldwide. Often called the "silent killer" because it can go unnoticed for years, hypertension can lead to severe complications like heart disease, stroke, and kidney damage if left untreated. Understanding the symptoms and early warning signs of high blood pressure is essential for managing this condition effectively.
In this blog post, we'll explore the key symptoms of high blood pressure, how they manifest, and what you can do to monitor and manage this condition for better long-term health.
What is High Blood Pressure?
Before diving into the symptoms, it's important to understand what high blood pressure is. Blood pressure refers to the force exerted by circulating blood on the walls of your arteries. When this force is consistently too high, it strains your heart and blood vessels, increasing the risk of serious health issues.
Blood pressure is measured using two numbers:
Systolic Pressure: The pressure in your arteries when your heart beats.
Diastolic Pressure: The pressure in your arteries when your heart rests between beats.
A normal blood pressure reading is typically around 120/80 mm Hg. Hypertension is diagnosed when readings consistently exceed 130/80 mm Hg.
Common Symptoms of High Blood Pressure
One of the reasons high blood pressure is dangerous is that it often has no clear symptoms in its early stages. Many people don't realize they have hypertension until they experience a serious health event like a heart attack or stroke. However, there are some high blood pressure symptoms. Here are some of the most common ones:
1. Headaches
While headaches are common and can occur for various reasons, persistent or severe headaches can be a sign of high blood pressure. If you're experiencing frequent headaches, particularly in the morning, it might be worth checking your blood pressure.
2. Dizziness or Lightheadedness
Feeling dizzy or lightheaded can occur when blood pressure is either too high or too low. If you're experiencing frequent dizziness, it's important to get your blood pressure checked to rule out hypertension or other cardiovascular issues.
3. Blurred or Double Vision
High blood pressure can damage blood vessels in the eyes, leading to blurred or double vision. This symptom should never be ignored, as it could indicate a hypertensive crisis (a dangerously high blood pressure that requires immediate medical attention).
4. Chest Pain
Chest pain, also known as angina, can result from high blood pressure straining the heart. If you're experiencing chest pain, especially if it's accompanied by shortness of breath, nausea, or sweating, seek medical help immediately. Chest pain could be a sign of a heart attack or other serious condition.
5. Shortness of Breath
High blood pressure can lead to heart failure or other cardiovascular complications, making it harder for your heart to pump blood effectively. As a result, you may feel short of breath, especially during physical activity. This symptom should not be ignored and warrants a medical evaluation.
6. Nosebleeds
Although nosebleeds aren't common in everyone with high blood pressure, they can occur during hypertensive crises. If you're experiencing frequent or unexplained nosebleeds, it may be linked to hypertension, and it's advisable to seek medical advice.
7. Fatigue
Feeling unusually tired or fatigued could be a symptom of high blood pressure, especially if it occurs without a clear cause. Hypertension puts extra strain on your heart and body, which can result in physical exhaustion.
0 notes
Text
Understanding Chronic Kidney Disease
Chronic kidney disease (CKD) is a serious condition that affects the kidneys’ ability to filter waste and excess fluids from the body. In India, around 17% of the adult population suffers from CKD. As the disease advances, it can lead to kidney failure, requiring dialysis or a kidney transplant to sustain life.

What is Chronic Kidney Disease (CKD)?
Chronic Kidney Disease is a slow and ongoing decline of renal function for not less than three months. 8% to 16% of the entire global population suffer from diabetes and hypertension.
In its initial form, no sign would indicate the presence of disease. As it develops, the person would be easily diagnosed with fatigue, swelling and other issues such as cardiovascular diseases.
Chronic Kidney Disease Stages
Nephrologists divide the disease into five stages based on the glomerular filtration rate (GFR), which measures how much blood the kidneys can filter per minute.
Stage 1: Normal or High GFR (≥90 mL/min)
The kidneys still function at a normal or high level, with a GFR of 90 mL/min or higher. However, there may be signs of kidney damage, such as protein in the urine. At this stage, symptoms are usually mild or absent.
Stage 2: Mild Reduction in GFR (60–89 mL/min)
Kidney function shows a mild reduction, with a GFR between 60 and 89 mL/min. Symptoms may include frequent urinary tract infections, high blood pressure, and swelling in the hands and feet.
Stage 3: Moderate Reduction in GFR (30–59 mL/min)
This stage is divided into two subgroups: stage 3a (GFR 45–59 mL/min) and stage 3b (GFR 30–44 mL/min). Here, kidney function shows a moderate reduction, and symptoms may include changes in urination, swelling in the hands and feet, weakness, fatigue, dry and itchy skin, back pain, and muscle cramping.
Stage 4: Severe Reduction in GFR (15–29 mL/min)
Kidney function reduces, with a GFR between 15 and 29 mL/min. Symptoms may include anaemia, decreased appetite, bone disease, and abnormal levels of phosphorus, calcium, and vitamin D.
Stage 5: Kidney Failure (GFR <15 mL/min or on dialysis)
Also known as end-stage renal disease (ESRD), this is the most severe stage of CKD. Here, the kidneys fail, with a GFR of less than 15 mL/min, or the patient requires dialysis. Symptoms may include all those mentioned in the previous stages, as well as nausea, vomiting, and confusion.
Causes of Chronic Kidney Disease
Chronic kidney disease symptoms result from many health issues. Understanding the main causes, risk factors, and preventive measures can help mitigate the impact of this disease.
Main Causes of CKD
Diabetes: This leading chronic kidney disease causes results when high blood sugar levels damage the kidneys’ filtering units over time, leading to diabetic kidney disease. Early signs often include protein in the urine, indicating damage to the kidney’s filters.
Hypertension: High BP damages the blood vessels in the kidneys, impairing their ability to filter waste. This creates a harsh cycle, as kidney damage can further increase blood pressure.
Glomerulonephritis: This refers to inflammation of the kidney’s filtering units (glomeruli). Conditions such as IgA nephropathy and lupus nephritis fall under this category and can lead to kidney damage.
Polycystic Kidney Disease (PKD): A genetic disorder characterised by the growth of a large number of cysts in the kidneys, PKD can badly affect kidney function over time.
Recurrent Kidney Infections: Chronic infections can lead to scarring and damage to the kidneys, contributing to CKD.
Obstructive Uropathy: Conditions like kidney stones or an enlarged prostate can obstruct urine flow, causing kidney damage.
Toxic Substances: Long-term exposure to certain medications (like NSAIDs) and heavy metals (like lead) can harm the kidneys.
Risk Factors Associated with CKD
Many factors can increase the likelihood of developing the disease:
Family History: A genetic predisposition to kidney disease can increase risk.
Age: The risk of chronic kidney disease increases with age, particularly in individuals over 60.
Ethnicity: Certain ethnic groups, including South Asians and African Americans, face a higher risk for CKD.
Conclusion
Chronic kidney disease remains a public health concern, especially in India, where a large portion of the adult population is affected. The progressive nature of CKD highlights the urgent need for early detection and management to prevent its escalation into end-stage renal disease, which requires intensive treatments like dialysis or kidney transplantation.
Regular check-ups with nephrologists at the best hospital In Haryana, such as SS Kidney Hospital, are important for those at risk or diagnosed with CKD to monitor kidney function and manage symptoms.
#hospital in haryana#hospital in rewari#kidney hospital in haryana#urologist near me#kidney stone removal
0 notes
Text
Understanding Chronic Kidney Disease: Symptoms, Causes, and Treatments

Being one of the best kidney specialists in Surat, our experts say that the Chronic Kidney Disease (CKD) is a condition that affects millions of people worldwide, yet many are unaware of their condition until the disease has progressed significantly. This silent threat to health can have serious consequences if left unchecked, but with early detection and proper management, many people with CKD can lead full, active lives. In this blog post, we’ll explore what CKD is, its symptoms, causes, and available treatments to help you better understand this common but often overlooked condition.
What is Chronic Kidney Disease?
Your kidneys are remarkable organs that filter waste and excess fluids from your blood, regulate blood pressure, produce hormones, and help maintain bone strength. Chronic Kidney Disease occurs when these bean-shaped organs are damaged and can’t perform their vital functions effectively.
CKD is typically a progressive condition, meaning it worsens over time. Renal specialists from SIDS Hospital, well-known as one of the best hospitals in Surat, say that it’s divided into five stages based on how well the kidneys are working, with stage 1 being the mildest and stage 5 (also known as end-stage renal disease or kidney failure) being the most severe.
Recognizing the Symptoms
One of the reasons CKD is often called a “silent disease” is that symptoms may not appear until the condition has advanced significantly. However, some people may experience:
1. Fatigue and weakness
2. Difficulty concentrating
3. Decreased appetite
4. Trouble sleeping
5. Muscle cramping, especially at night
6. Swollen feet and ankles
7. Puffiness around the eyes, especially in the morning
8. Dry, itchy skin
9. Need to urinate more often, especially at night
As the disease progresses, additional symptoms may include:
10. Nausea and vomiting
11. Shortness of breath
12. Chest pain
13. Persistent itching
14. High blood pressure that’s difficult to control
It’s important to note that these symptoms can be caused by other conditions as well. If you’re experiencing any of these persistently, it’s crucial to consult with the best kidneys stone specialist in Surat for proper evaluation.
Understanding the Causes
Chronic Kidney Disease can result from various factors, but the two leading causes are diabetes and high blood pressure. These conditions can damage the blood vessels in your kidneys over time, impairing their ability to filter waste effectively.
Other potential causes of CKD include:
1. Glomerulonephritis — inflammation of the kidney’s filtering units
2. Polycystic kidney disease — an inherited disorder causing cysts to grow in the kidneys
3. Prolonged obstruction of the urinary tract
4. Recurrent kidney infections
5. Certain autoimmune disorders like lupus
6. Overuse of certain medications, particularly non-steroidal anti-inflammatory drugs (NSAIDs)
According to the best kidney stone specialists in Surat, some people are at higher risk of developing CKD such as:
- Being over 60 years old
- Having a family history of kidney disease
- Being of African American, Native American, or Asian descent
Having a history of cardiovascular disease
Treatment Options
While there’s no cure for Chronic Kidney Disease, various treatments can slow its progression and manage symptoms. The treatment plan will depend on the underlying cause and the stage of the disease.
1. Lifestyle Changes: Often, the first line of defence against CKD progression involves lifestyle modifications. These may include:
- Following a kidney-friendly diet low in sodium, phosphorus, and protein
- Maintaining a healthy weight
- Quitting smoking
- Limiting alcohol intake
- Regular exercise as approved by your doctor
2. Medications: Various medications may be prescribed to manage symptoms and complications of CKD, such as:
- Blood pressure medications
- Medications to lower cholesterol levels
- Drugs to treat anaemia
- Medications to relieve swelling
- Vitamin D and calcium supplements to protect bones
3. Treating Underlying Conditions: If diabetes or high blood pressure is causing your CKD, managing these conditions effectively is crucial to slowing kidney damage.
4. Dialysis: In advanced stages of CKD, when the kidneys can no longer filter waste effectively, dialysis may be necessary. This treatment uses a machine to filter waste from your blood.
5. Kidney Transplant: For some patients with end-stage kidney disease, a kidney transplant may be an option. This involves surgically placing a healthy kidney from a donor into your body.
Prevention and Early Detection
The best way to deal with Chronic Kidney Disease is to prevent it from developing in the first place. Regular check-ups with the best kidney specialists in Surat, especially if you have risk factors for CKD, can help catch the disease early. Simple blood and urine tests can detect CKD before symptoms appear.
Conclusion
If you’re diagnosed with CKD, remember that knowledge is power. Understanding your condition, following your treatment plan, and maintaining open communication with your healthcare team from the best hospital in Surat can significantly impact your quality of life and slow the progression of the disease. Many people with CKD lead full, active lives.
If you have concerns about your kidney health, don’t hesitate to speak with our renal experts at SIDS Hospital. Early detection and treatment can make a world of difference in managing Chronic Kidney Disease and maintaining your overall health and well-being.
0 notes
Text
What is a kidney transplant, and who is a candidate for this procedure?
A kidney transplant is a surgical procedure that involves placing a healthy kidney from a donor into the body of a person with kidney failure. This procedure is typically recommended for individuals whose kidneys have ceased to function adequately, necessitating an alternative to dialysis for managing kidney function and overall health.
Who is a Candidate for a Kidney Transplant?
Eligibility for a kidney transplant depends on several factors, including the patient’s overall health, kidney function, and the presence of other medical conditions. The following criteria help determine if someone is a suitable candidate:
End-Stage Renal Disease (ESRD) or Kidney Failure:
Candidates typically have ESRD, where kidneys have lost about 85–90% of their function. This condition often requires dialysis, a treatment that performs the kidneys’ functions artificially.
2. Good General Health:
Patients need to be in good overall health to handle the stress of surgery and the long-term use of immunosuppressive medications. Chronic conditions like diabetes, heart disease, or severe infections might affect eligibility.
3. Adherence to Treatment:
Candidates must be able to adhere to a strict regimen of medications and follow-up care. Successful transplantation requires lifelong use of immunosuppressants to prevent rejection of the new kidney.
4. Absence of Active Cancer or Severe Infections:
Active cancer or severe infections can complicate surgery and the healing process, making these conditions a contraindication for transplantation until they are adequately treated or resolved.
5. Support System:
A strong support system of family or friends can be crucial for managing post-surgical care, medication adherence, and follow-up appointments.
6. No Significant Psychosocial Issues:
Candidates should be free of significant psychosocial issues that could affect their ability to adhere to treatment or manage post-transplant care.
Special Considerations:
Living vs. Deceased Donor:
A kidney can come from a living donor (a person who is still alive and has agreed to donate one of their kidneys) or a deceased donor. Both sources are viable, though living donor transplants often have better outcomes due to the organ’s preserved condition.
Blood Type and Tissue Matching:
Successful transplantation requires matching blood types and, ideally, tissue antigens to minimize the risk of organ rejection. Compatibility is determined through a series of tests before the transplant.
Age and Other Health Conditions:
While age alone is not a disqualifying factor, older patients or those with multiple health conditions may need thorough evaluation to ensure they can safely undergo the procedure and benefit from it.
Conclusion
A kidney transplant can offer a life-saving alternative to dialysis for individuals with severe kidney disease. The suitability of a patient for this procedure is determined through a comprehensive evaluation process that considers medical, psychological, and social factors. If you or someone you know is experiencing kidney failure, discussing the option of a kidney transplant with a nephrologist or transplant specialist can provide valuable insights into potential treatment paths and improve overall outcomes.
#Kidney Stone Treatment Specialist in Jaipur#Best Kidney Stone Treatment in Jaipur#Best Kidney Treatment in Jaipur
0 notes
Text
How to Access Medicare-Covered Mental Health Therapy
Mental health is essential for overall well-being, particularly for seniors facing unique emotional and psychological challenges. Understanding how to access therapy covered by Medicare can significantly improve the quality of life for older adults. This step-by-step guide will help you navigate Medicare mental health coverage, ensuring you get the support you need.
Understanding Medicare Mental Health Coverage
Medicare offers various options for mental health coverage, including outpatient therapy, inpatient care, and prescription medications. Here’s a breakdown of what each part of Medicare covers:
Medicare Part A (Hospital Insurance): Covers inpatient mental health care in a hospital. This includes room, meals, nursing, and other related services and supplies.
Medicare Part B (Medical Insurance): Covers outpatient mental health services. These include visits to psychiatrists, other doctors, clinical psychologists, social workers, and counselors.
Medicare Part D (Prescription Drug Coverage): Covers medications prescribed for mental health conditions.
Medicare Advantage Plans (Part C): These plans are offered by private insurance companies that have been approved by Medicare. They often include additional benefits beyond Original Medicare (Parts A and B), which may include enhanced mental health services.
Step-by-Step Guide to Accessing Therapy Covered By Medicare
Step 1: Determine Your Eligibility
To be eligible for Medicare mental health coverage, you must be enrolled in Medicare Part A and/or Part B. Generally, individuals 65 years and older, certain younger people with disabilities, and people with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant) are eligible for Medicare.
Step 2: Identify Your Mental Health Needs
Assess your mental health needs by consulting with your primary care physician or a mental health professional. They can help determine the type of therapy that would be most beneficial. This could be individual therapy, group therapy, or another form of treatment.
Step 3: Choose the Right Medicare Plan
Review your current Medicare plan to understand what mental health services are covered. You can switch to a Medicare Advantage Plan (Part C) that offers additional mental health benefits.
Step 4: Find a Medicare-Approved Provider
Ensure that the mental health professional you choose accepts Medicare. You can find Medicare-approved providers by visiting the Medicare website or contacting Medicare directly. Verify the provider participates in Medicare to avoid unexpected out-of-pocket costs.
Step 5: Schedule an Appointment
Once you have selected a provider, schedule an appointment. Be prepared to discuss your mental health history, symptoms, and any previous treatments you’ve received. This will help the therapist develop an effective treatment plan tailored to your needs.
Step 6: Understand Your Costs
Medicare Part B typically covers 80% of the cost of outpatient mental health services after you meet the annual Part B deductible. You will be responsible for the remaining 20% coinsurance. If you have a Medicare Supplement (Medigap) plan, it may help cover these out-of-pocket costs.
For inpatient mental health services covered under Part A, you will have to pay a deductible for each benefit period. There may also be coinsurance amounts if your stay extends beyond a certain number of days.
Step 7: Attend Your Therapy Sessions
Consistently attending therapy sessions is crucial for improving your mental health. Follow your therapist’s recommendations and be open to discussing any changes or challenges you experience during your treatment.
Step 8: Monitor Your Progress
Regularly evaluate your progress with your Medicare-approved therapist. Adjustments to your treatment plan may be necessary to ensure you receive the most effective care. Don’t hesitate to communicate any concerns or issues with your therapist.
Step 9: Explore Additional Resources
Medicare provides several resources to support your mental health. These include wellness visits, screenings for depression, and other preventive services. Take advantage of these resources to maintain your mental well-being.
Step 10: Stay Informed
Medicare policies and coverage options can change. Stay informed about any updates to continue to receive the best possible care. Visit the Medicare website or speak with a Medicare representative for the latest information.
Benefits of Senior Therapy and Medicare
Senior therapy offers numerous benefits, including:
Improved Mental Health: Regular therapy can help manage symptoms of depression, anxiety, and other mental health conditions.
Enhanced Quality of Life: Therapy can improve emotional well-being and better overall quality of life.
Support for Chronic Conditions: Mental health therapy support for managing chronic conditions common in seniors.
Social Engagement: Group therapy and support groups offer opportunities for social interaction, reducing feelings of isolation.
Increased Coping Skills: Therapy can teach coping mechanisms to handle stress, grief, and other challenges.
Conclusion
Accessing therapy covered by Medicare involves understanding your coverage options, finding the right provider, and staying committed to your treatment plan. By following this step-by-step guide, seniors can take proactive steps to improve their mental health and overall quality of life.
If you or a loved one is struggling with mental health issues, don’t hesitate to seek help. Medicare mental health coverage is designed to support you in receiving the care you need. Stay informed, stay proactive, and take advantage of the resources available to ensure a healthier, happier future.
1 note
·
View note