#ehr integration
Explore tagged Tumblr posts
Text
A Cheat Sheet for EHR Data Conversion and Migration

Bid farewell to data headaches and embrace a seamless transition between Electronic Health Record (EHR) systems! Moving to a new Electronic Health Record (EHR) can feel like scaling Mount Data Everest, but fear not, brave healthcare hero. This cheat sheet is your trusty sherpa, guiding you through the tricky terrain of data conversion and migration.
Before You Begin
Investigate how both your current and future EHR systems handle data export and import. Is it a database dump, APIs, or file transfers? The sooner you understand, the smoother the migration.
Do not assume that all data is easily transferable. Scrutinize your data to ensure it meets the new system’s requirements, as not all elements may seamlessly make the journey.
Don’t rely on cumbersome claim transfers. Wrap up outstanding accounts receivable in your old system before making the switch.
Schedule your migration around holidays to minimize disruption and give your team (and the data!) breathing room.
Conversion Strategies
Embrace a phased approach. Move demographics, appointments, and master lists first. Clinical data can wait (gasp!). This lets your team and the new EHR prioritize and get you online ASAP.
Conduct multiple tests, running trial conversions on small patient samples (say 30 patients). You’ll unearth issues before they become mountain-sized problems.
Consider retaining temporary access to your old system for reference purposes. It’s like a safety net for those “oh, I forgot that!” moments.
Not everything needs a new home. Utilize an archival system for data you don’t need in the new EHR.
Data Essentials
Ensure a smooth migration by prioritizing the transfer of the following essential data:
Patient Information: Demographics, insurance scans, policy details, historic charges/balances.
Appointments: Both past and future appointments, meticulously organized.
Master Lists: Categorize and transfer insurance providers, referral sources, and other relevant lists.
Clinical Data: Chart PDFs, discrete text data, allergies, medications, problem lists, immunizations, and progress notes.
Procedures: Transfer detailed information such as CPT codes, modifiers, and pre-authorization codes.
CCDAs: Acquire the Summary of Care document, a valuable data repository.
Financials: Limited financial data may be transferred, but confirm the specifics with your new EHR to ensure accuracy.
Bonus Tip: Make a list of all your EHR integration points like FHIR, HL7 V2, APIs, CSV files. Don’t leave any data orphans behind!
But fear not, weary traveler! You don’t have to climb this mountain alone. We’re here to help with expert guidance, proven strategies, and a team of data Sherpas ready to tackle any conversion challenge. Contact us today for a free consultation and let’s turn your EHR migration into a smooth and stress-free journey!
Remember, with the right plan and a helping hand, even the mightiest data peak can be conquered.
You may find this article on Falkondata website by following this link: https://falkondata.com/ehr-data-conversion-cheat-sheet/
2 notes
·
View notes
Text
Why EHR Integration Game-Changer for Healthcare

In today’s fast-paced healthcare environment, Electronic Health Record (EHR) integration isn’t just a tech upgrade—it’s a transformative shift that redefines how practices deliver care, manage operations, and interact with patients. As digital healthcare continues to evolve, EHR integration is proving to be a game-changer for clinics, hospitals, and virtual care platforms alike.
Read more: Why EHR Integration is a Game-Changer for Healthcare Practices
0 notes
Text

#real-time health data tracking#EHR integration#cloud-based security#chronic disease management#hospital readmission reduction#operational efficiency#healthcare compliance#a user-friendly interface#scalability#patient engagement#healthcare innovation.
1 note
·
View note
Text
Enhancing Healthcare Efficiency Through Seamless EHR Integration
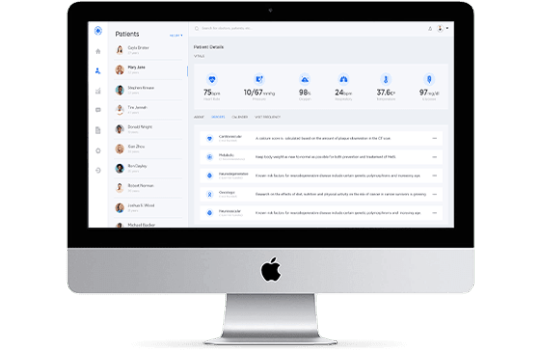
In today’s healthcare landscape, efficient and interconnected systems are essential for delivering quality patient care. Electronic Health Record (EHR) integration serves as the backbone for achieving this goal, offering a unified platform that connects disparate healthcare systems and streamlines operations. The growing reliance on EHR integration services highlights the need for robust integration solutions that improve clinical workflows, data accessibility, and overall patient outcomes.
Bridging Disparate Systems
Healthcare providers often use various software applications for managing clinical, administrative, and operational tasks. EHR integration solutions acts as a bridge between these systems, enabling seamless communication and data exchange. Whether it’s linking laboratory systems, pharmacy management platforms, or billing software, integration ensures that vital patient information is accessible in real-time, reducing delays and errors in care delivery.
Driving Interoperability
Interoperability is a key challenge in modern healthcare, as data silos can hinder collaboration between providers. A well-executed EHR integration addresses this challenge by aligning systems to a common standard. This ensures that data flows smoothly across platforms, empowering healthcare professionals with the information they need to make informed decisions.
Integration also facilitates compliance with regulatory standards, such as the HL7 and FHIR frameworks, ensuring data accuracy and secure sharing across healthcare networks.
Enhancing Patient-Centered Care
At the heart of EHR integration is the goal of improving patient care. By consolidating patient data into a single source of truth, clinicians can access comprehensive medical histories, including test results, prescriptions, and treatment plans. This holistic view not only enhances diagnosis and treatment but also reduces the likelihood of duplicate tests and medication errors.
Additionally, integrated systems allow patients to engage more actively in their healthcare journey. Features like patient portals provide individuals with easy access to their records, fostering transparency and trust between patients and providers.
Improving Operational Efficiency
For healthcare organizations, streamlined workflows translate into cost savings and better resource allocation. EHR integration eliminates redundancies and automates routine processes such as appointment scheduling, claims processing, and report generation. By reducing administrative burdens, healthcare staff can dedicate more time to patient care, ultimately improving service quality.
The Road Ahead
As healthcare continues to evolve, EHR integration remains a cornerstone for achieving a connected and efficient ecosystem. By bridging gaps between systems, enhancing data accessibility, and fostering interoperability, it lays the foundation for a future where technology empowers better health outcomes and operational excellence. Embracing these solutions is not just a technological upgrade but a step towards transforming healthcare delivery.
#ehr integration software#ehr integration services#ehr integration api#ehr integration#ehr integration solutions#EMR/EHR INTEGRATION#CUSTOM EHR INTEGRATION SOLUTIONS#ehr data integration
0 notes
Text
The healthcare industry has adopted technology widely and taken steps towards digital transformation. However, in order to make a complete digital shift, healthcare needs to streamline their data management. Although healthcare is one of the biggest sectors with huge amounts of data. It has to be secured and easily accessible. This is where two technological advancements, i.e., EMR vs EHR, play major roles.
#ehr software#emr software#emr system#emr vs ehr#ehr integration#benefits of ehr#emr integration#ehr benefits#benefits of emr#emr benefits
0 notes
Text
The Importance Of EHR Integration Services In Healthcare

In the fast-paced world of healthcare, Electronic Health Records (EHRs) have revolutionised the way patient information is stored and shared. The widespread adoption of EHRs has presented healthcare organisations with a new challenge: seamlessly integrating EHRs with other systems and applications for efficient data exchange. This is where EHR integration services come into play. In this blog post, we will delve into the significance of EHR integration services and their impact on the healthcare landscape.
Simplifying Data Exchange for Seamless Collaboration:
EHR integration services serve as the bridge that simplifies the exchange of data between various healthcare systems and applications. By implementing EHR integration, healthcare providers can effortlessly share patient data across platforms such as EHRs, laboratory systems, radiology systems, billing systems, and other crucial healthcare applications. This streamlined data exchange process not only saves time but also minimises errors associated with manual data entry.
Enhancing Care Coordination for Optimal Outcomes:
Using EHR integration helps healthcare providers work together better. They can see all the important information about a patient, like medical history and test results, in one place. This helps them make good decisions and ensures everyone involved in the patient’s care knows what’s going on. The outcome is that care is well-coordinated, leading to better results for the patient.
Boosting Efficiency for Uninterrupted Patient Care:
Integrated EHR systems help healthcare providers work more efficiently. Instead of wasting time switching between different apps to find patient information, they can quickly access all the data they need in one place. This saves time on manual tasks and lets providers concentrate on giving better care to patients.
Upholding Patient Safety with Accurate and Timely Information:
Patient safety is a top priority in healthcare, and EHR integration services play a crucial role in ensuring it. By seamlessly integrating EHRs with other systems, providers gain access to up-to-date patient information that is accurate and timely. This robust information flow allows providers to identify potential risks promptly and take appropriate action, such as updating treatment plans or sharing critical alerts with other care providers. The result is enhanced patient safety and a reduction in medical errors.
Promoting Compatibility for Seamless Data Exchange:
EHR integration services help different EHR systems talk to each other easily. This makes it simple to share patient data between different healthcare providers and organizations, making coordinated care easier. These services also make it possible for EHR systems to work with other devices like medical tools and wearables, making patient information more accessible and supporting complete patient care.
Facilitating Interoperability for Comprehensive Patient Care:
EHR integration services help different healthcare systems talk to each other easily. This means that healthcare providers can see all the information about a patient’s health in one place, no matter where they received care. By sharing information between systems, EHR integration makes sure patients get consistent care and supports a complete approach to treatment.
Empowering Data-Driven Decision Making:
By integrating EHR systems with other healthcare applications, providers gain access to a wealth of data that can be leveraged for informed decision-making. EHR integration services enable the aggregation and analysis of patient data from multiple sources, allowing healthcare professionals to identify trends, track outcomes, and personalise treatment plans based on evidence-based practices. This data-driven approach enhances clinical decision-making, leading to improved patient outcomes and quality of care.
Enabling Scalability and Future-Proofing Healthcare Systems:
Investing in EHR integration services not only addresses current data exchange challenges but also future-proofs healthcare systems for scalability and technological advancements. Integrated EHR systems can easily adapt to evolving healthcare technologies, such as AI-driven analytics, telehealth platforms, and population health management tools. This scalability ensures that healthcare organisations can efficiently incorporate new innovations and expand their services without disrupting existing workflows, ultimately enhancing operational efficiency and competitiveness in the healthcare market.
Driving Innovation and Collaboration in Healthcare Delivery:
EHR integration services serve as a catalyst for innovation and collaboration in healthcare delivery by fostering a connected ecosystem of healthcare providers, patients, and technology solutions. Integrated EHR systems enable seamless sharing of data for research, population health management, and clinical trials, driving advancements in medical knowledge and treatment outcomes. Furthermore, EHR integration promotes collaboration among interdisciplinary care teams, allowing for coordinated care delivery and improved patient engagement.
In today’s digital healthcare landscape, the significance of EHR integration services cannot be overstated. They simplify data exchange, enhance care coordination, boost workflow efficiency, improve patient safety, promote compatibility in the exchange of medical information while empowering decision-making through interoperability support regulatory compliance & security measures enabling scalability & future-proofing driving innovation & collaboration in healthcare delivery Equipped with these services; healthcare organisations can adapt to emerging trends like telemedicine & remote monitoring while ensuring highest standards of care Investing in EHR integration services is vital towards staying competitive & navigating modern healthcare effectively.
0 notes
Text
Breaking Down Barriers: The Importance of Interoperability in Healthcare
In today's digital age, the adoption of Electronic Health Record (EHR) software has transformed the way healthcare providers manage patient information and deliver care. EHR solutions streamline processes, enhance communication, and improve patient outcomes. However, one critical factor that can significantly impact the effectiveness of EHR systems is interoperability. Let's explore why interoperability matters in healthcare and how it can benefit patients, providers, and the healthcare ecosystem as a whole.

What is Interoperability in Healthcare?
Interoperability refers to the ability of different healthcare systems, software, and devices to securely exchange and use patient information seamlessly. In other words, interoperability enables EHR solutions from different vendors to communicate with each other and share data efficiently, regardless of the platform or technology used.
Why Does Interoperability Matter?
Enhanced Care Coordination: Interoperability enables healthcare providers to access comprehensive patient information from various sources in real-time, facilitating seamless care coordination across different specialties, settings, and organizations. This ensures that providers have a complete picture of a patient's medical history, medications, allergies, and treatment plans, leading to more informed decision-making and better outcomes.
Improved Patient Safety: By promoting the exchange of accurate and up-to-date patient information, interoperability helps reduce the risk of errors, duplicate tests, and adverse drug events. This enhances patient safety and reduces the likelihood of medical errors that can result from incomplete or fragmented health records.
Efficient Workflow: Interoperable EHR software solutions streamline workflows by eliminating the need for manual data entry, faxing, and paper-based processes. This saves time, reduces administrative burden, and allows healthcare providers to focus more on patient care, ultimately improving efficiency and productivity.
Empowered Patients: Interoperability gives patients greater control over their health information, allowing them to access and share their medical records securely with other healthcare providers as needed. This promotes patient engagement, empowers individuals to take an active role in their healthcare decisions, and fosters collaboration between patients and providers.
Interoperability Standards: To achieve seamless data exchange, interoperability standards such as HL7 (Health Level Seven) and FHIR (Fast Healthcare Interoperability Resources) play a crucial role. These standards establish common formats, protocols, and vocabularies for exchanging health information, ensuring compatibility and consistency across different systems.
Interoperability and Population Health Management: Interoperable EHR solutions facilitate population health management initiatives by aggregating and analyzing data from diverse sources. This enables healthcare organizations to identify trends, track outcomes, and implement targeted interventions to improve the health of entire patient populations.
Conclusion
In an increasingly interconnected healthcare landscape, interoperability is essential for optimizing patient care, improving clinical outcomes, and driving innovation. By breaking down data silos and enabling seamless information exchange, interoperable EHR software solutions empower healthcare providers to deliver more coordinated, efficient, and patient-centered care.
At Meditab, we recognize the critical role that interoperability plays in advancing healthcare delivery. Our comprehensive EHR solution is designed to promote interoperability, enabling seamless data exchange and collaboration across the healthcare continuum. To learn more about our interoperable EHR software solution and how it can benefit your practice, visit our website here or contact us today.
Together, let's embrace interoperability and harness the power of connected health to transform the future of healthcare delivery.
#ehr software#ehr solutions#ehr software companies#ehr integration#interoperability#interoperability healthcare
0 notes
Text
2024: The Dawn of Interconnected Healthcare

Envision a world where medical records seamlessly traverse between hospitals, medical practices, and pharmacies, guiding care decisions. Healthcare's future shines bright in 2024, illuminated by three major trends poised to revolutionize how we experience and deliver health: interoperability, revenue cycle management (RCM) optimization, and empowered patient engagement.
Interoperability
The longstanding aspiration of unlocking healthcare data is finally becoming a reality. After years of anticipation, 2023 witnessed the momentous launch of the nationwide data exchange powered by TEFCA (Trusted Exchange Framework and Common Agreement). This landmark framework acts as a key, unlocking data silos and allowing medical records to flow freely across different healthcare systems nationwide. This unprecedented data liberation promises to harmonize care coordination, drastically reducing medical errors and eliminating redundant tests. The future of healthcare looks brighter than ever, with patients empowered to actively participate in their own journey by easily accessing their complete medical picture across disparate providers.
RCM Evolution
Picture cloud-based RCM platforms powered by AI automation, where bills are personalized, claims processed seamlessly, and denials tackled proactively. We are well on the path to realizing this vision. According to a recent survey conducted by Change Healthcare, 98% of healthcare leaders across the US plan to leverage AI across their revenue cycle within the next three years. This aligns with several other studies from organizations like HFMA and NBER, all highlighting the rising adoption of AI for tasks like automated claims processing, personalized billing, and proactive denial management. This growing focus on AI-powered RCM is fueled by its potential to support value-based care models, where providers are rewarded for improved patient outcomes rather than just the number of procedures performed.
Patient Engagement, Redefined
With virtual care models taking center stage, AI advances like Google’s PaLM2 and others are fueling a patient-centric healthcare revolution. Robust language models tailor interventions, while intelligent assistants handle appointments and provide real-time support. The healthcare landscape is transitioning from hospital to the comfort of our homes, empowered by convenient virtual consultations and remote monitoring.
Beyond the Horizon
This glimpse into the healthcare landscape of 2024 is just the first act. Picture wearable sensors feeding real-time health data into AI-powered models that predict and prevent illnesses. The possibilities are limitless, driven by ongoing technological advancements and an unwavering commitment to patient-centered care.
So, buckle up. We stand on the precipice of a transformative era where data intertwines with innovation, finances align with outcomes, and patients rightfully take center stage in their well-being. The future of healthcare is not merely interconnected – it's genuinely human-centric, and 2024 is only the beginning.
Ready to make this journey easier? Reach out to Falkondata and discover how we can streamline your process and achieve your goals.
#ehr#future of healthcare#health and wellness#AdvancedMD#Falkondata#interoperability#EHR Integration#FHIR#health tech#patient care#medical billing services#healthcare industry#hl7
0 notes
Text
Best Practices for Successful EHR Data Integration
Introduction
In the dynamic landscape of modern healthcare, the adoption of Electronic Health Record (EHR) systems has revolutionized patient care and management. These digital repositories of patient information offer unparalleled benefits in terms of accessibility, accuracy, and efficiency. However, the full potential of EHRs can only be harnessed when their data is seamlessly integrated across various healthcare systems. EHR data integration stands as a cornerstone of modern healthcare technology, enabling medical professionals to access comprehensive patient records, make informed decisions, and provide holistic care.
With the ever-expanding use of EHR systems, the need for effective data integration has become increasingly evident. The successful integration of EHR data across disparate systems has the potential to break down silos of information, promote interoperability, and enhance the continuum of care. Achieving this level of integration, however, demands careful planning, adherence to best practices, and a clear understanding of the challenges and opportunities associated with the process.
Comprehensive Planning and Strategy
The road to successful EHR data integration begins with comprehensive planning and a well-defined strategy. Clearly articulating integration goals and objectives is essential. Whether the aim is to streamline patient data access, improve care coordination, or enhance data analytics, having a clear roadmap guides the integration process.
Mapping out the integration process and workflow helps identify potential bottlenecks and streamline the movement of data. Each step, from data extraction and transformation to loading and validation, should be carefully considered. Moreover, anticipating challenges such as data inconsistencies, system compatibility issues, and potential disruptions to ongoing operations allows for effective mitigation strategies to be put in place.
EHR integration touches upon various aspects of healthcare operations, it's imperative to involve all relevant stakeholders in the planning phase. This could include healthcare providers, IT teams, administrators, and even patients. Their insights contribute to a holistic strategy that aligns with the broader goals of the organization and ensures that the integrated solution caters to the needs of all parties involved.
Data Quality and Standardization
Effective EHR data integration hinges on the quality and standardization of the data being integrated. Ensuring data accuracy and consistency across various systems is paramount. This involves rigorous data cleansing and validation procedures to identify and rectify any discrepancies or errors. Adhering to industry-standard data formats, such as Health Level 7 (HL7) or Fast Healthcare Interoperability Resources (FHIR), ensures that data is universally understood and can be seamlessly exchanged between different healthcare systems. By prioritizing data quality and standardization, healthcare organizations can trust the integrity of the information flowing through integrated systems.
Interoperability and System Compatibility
One of the primary goals of EHR data integration is to achieve interoperability, enabling different healthcare systems to exchange data seamlessly. Ensuring system compatibility is crucial in this regard. The implementation of HL7 and FHIR standards facilitates the uniform sharing of data across diverse systems, regardless of the vendor or technology used. By embracing these standards, healthcare organizations can overcome the challenges of proprietary data formats and achieve true interoperability, allowing patient information to flow fluidly between EHRs, laboratories, pharmacies, and other healthcare entities.
Security and Privacy Measures
As EHR data integration involves the sharing of sensitive patient information, robust security and privacy measures are non-negotiable. Implementing strong data encryption, access controls, and authentication mechanisms safeguards patient data from unauthorized access or breaches. Compliance with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) is essential to maintain patient confidentiality. Regular security audits and vulnerability assessments help identify and address potential weaknesses, ensuring that integrated systems remain resilient against evolving cybersecurity threats.
Stakeholder Engagement and Communication
EHR data integration is success heavily depends on effective stakeholder engagement and communication. Involving all relevant parties, from medical professionals to IT personnel, fosters a collaborative approach. Clear lines of communication are established to ensure that everyone is on the same page regarding integration objectives, timelines, and potential impacts. Addressing concerns and obtaining buy-in from healthcare professionals is crucial, as they play a key role in using the integrated data to deliver quality patient care.
Testing and Validation
Before full deployment, thorough testing and validation of integrated systems are imperative. Rigorous testing ensures that data is accurately transferred and retained across systems. End-to-end testing simulates real-world scenarios to verify the seamless flow of patient information. Any identified issues or inconsistencies are addressed before the integrated system goes live, minimizing disruptions and preventing potential errors in patient care.
Training and User Adoption
Even the most technically sound integration can falter if healthcare staff are not adequately trained to use the integrated system. Comprehensive training ensures that medical professionals and support staff can effectively navigate and utilize the integrated data. Offering user-friendly interfaces and intuitive workflows encourages user adoption and minimizes resistance to change. Monitoring user feedback and addressing usability challenges contribute to the successful adoption of the integrated system.
Continuous Monitoring and Maintenance
EHR data integration is an ongoing process that requires continuous monitoring and maintenance. Regularly assessing the performance of integrated systems ensures that data is flowing smoothly and accurately. System updates and optimizations should be implemented to address any issues, accommodate changes in data requirements, and ensure the sustainability of the integrated solution over time.
Data Backup and Disaster Recovery
The critical nature of patient data necessitates robust data backup and disaster recovery strategies. Establishing regular data backups safeguards against data loss due to system failures, natural disasters, or cyberattacks. Developing contingency plans and conducting regular drills for disaster recovery ensures that patient data remains accessible and secure even in challenging situations.
Return on Investment (ROI) Assessment
EHR data integration is an investment, and evaluating its impact is essential. Assessing the ROI involves measuring both financial and operational benefits. Quantifying improvements in patient care, efficiency, reduced manual work, and enhanced data-driven decision-making contribute to understanding the value the integration brings. This assessment guides further optimization efforts and provides insights into areas that may require additional attention.
Conclusion
The journey to successful EHR data integration requires a strategic approach informed by best practices. By following comprehensive planning, ensuring data quality, fostering interoperability, prioritizing security, and engaging stakeholders effectively, healthcare organizations can create a seamlessly integrated ecosystem that empowers medical professionals to deliver high-quality patient care. Continuous monitoring, user training, disaster recovery planning, and ROI assessment contribute to the sustainability and efficacy of the integrated solution. Ultimately, adhering to these best practices sets the stage for a healthcare landscape where data flows seamlessly, insights are readily available, and patient outcomes are optimized.
0 notes
Text
Medical Practices Need to Embrace Two-Way Texting and AI

Let's face it, calling your doctor's office can be an exercise in frustration. Long hold times, automated menus, and the dreaded elevator music...it's enough to make anyone lose their cool. But what if there was a better way?
Here's the truth: traditional voice-only medical practices are outdated. Patients shouldn't have to waste precious time on hold for simple tasks like scheduling appointments, refilling prescriptions, or paying bills. This outdated system creates a frustrating experience for everyone involved. Patients are left feeling unheard and unimportant, while overwhelmed front desk staff struggle to keep up with the constant ringing.
There's a better way. Medical practices can leverage technology to offer a more convenient and efficient experience for patients. Here's how:
Embrace two-way texting: Texting is the dominant communication method today. Studies show a 95% open rate for text messages, meaning patients are far more likely to see and respond to a text than answer a call. Two-way texting allows for real-time conversations, streamlining communication for both patients and staff. Practices can leverage this technology to:
Schedule appointments
Refill prescriptions
Send directions to the office location
Answer basic questions
Send appointment reminders and confirmations
Collect patient feedback
The good news? You don't have to ditch your existing phone number! Text-enabling technology allows you to seamlessly integrate texting with your current office phone line. This means patients can still reach you at the familiar number they know, but with the added convenience of texting.
Smarter texting with AI: Instead of a clunky AI chatbot, a smarter texting solution powered by AI can assist both staff and patients. This AI assistant can:
Understand natural language: No more robotic responses! The AI can understand the intent behind a patient's text message, allowing for a more natural and efficient conversation.
Provide automated responses: The AI can handle frequently asked questions and basic tasks like appointment confirmations, prescription refill reminders, and insurance updates.
Route complexities to staff: For more complex inquiries, the AI can seamlessly route the conversation to a staff member, ensuring all patient needs are met.
But it doesn't stop there. Here's what a winning texting solution should offer:
EHR integration: A seamless integration with your Electronic Health Record (EHR) ensures all patient information is readily available for a smooth texting experience.
Worklist management: An easy-to-use interface allows front office staff to manage their workload efficiently, prioritize messages, and collaborate with the AI assistant for faster responses.
By implementing these technologies, medical practices can:
Reduce hold times: No more waiting on hold! Patients can handle routine tasks quickly and efficiently.
Improve patient satisfaction: A more convenient experience leads to happier patients.
Increase staff efficiency: Freeing up staff from constant phone calls allows them to focus on more complex tasks and patient care.
The time for change is now. Let's ditch the outdated phone-only system and embrace a more patient-centric approach. Two-way texting with the help of an AI assistant offers a future where medical care is convenient, efficient, and puts the patient first.
Ready to transform your patients' experience? Contact us for more information.
0 notes
Text
Why EHR Integration is a Game-Changer for Healthcare Practices

In today’s fast-paced healthcare environment, Electronic Health Record (EHR) integration isn’t just a tech upgrade—it’s a transformative shift that redefines how practices deliver care, manage operations, and interact with patients. As digital healthcare continues to evolve, EHR integration is proving to be a game-changer for clinics, hospitals, and virtual care platforms alike.
Read More: Why EHR Integration Game-Changer for Healthcare
0 notes
Text
Seamless Healthcare: The Importance of EHR Integration
In today’s healthcare environment, the seamless exchange of information is crucial for improving patient care and operational efficiency. Electronic Health Records (EHR) have transformed how patient data is stored and accessed, but the effectiveness of these systems hinges on their integration with other healthcare applications. EHR integration facilitates better communication among healthcare providers, enhances data accuracy, and ultimately leads to improved patient outcomes.
Understanding EHR Integration
EHR integration refers to the process of connecting EHR integration software with other healthcare software and platforms, such as billing systems, laboratory information systems, and telemedicine applications. This connectivity allows for the sharing of patient data across different healthcare settings, ensuring that providers have access to comprehensive and up-to-date information.
Key Benefits of EHR Integration
Improved Patient Care: When healthcare providers can access a patient’s complete medical history, they are better equipped to make informed decisions. EHR integration allows for real-time data sharing, which means that clinicians can quickly retrieve vital information, such as lab results, medication history, and previous diagnoses. This holistic view of a patient’s health enables more accurate diagnoses and personalized treatment plans.
Enhanced Operational Efficiency: Integrating EHR systems with other healthcare applications can streamline workflows and reduce administrative burdens. By automating data entry and minimizing manual processes, healthcare organizations can save time and reduce the likelihood of errors. This increased efficiency allows staff to focus more on patient care rather than paperwork.
Better Coordination of Care: EHR integration services promotes collaboration among different healthcare providers, ensuring that everyone involved in a patient’s care is on the same page. This is particularly important for patients with chronic conditions who often see multiple specialists. Integrated systems enable seamless communication, making it easier to coordinate treatment plans and share relevant information across care teams.
Data Accuracy and Consistency: Manual data entry is prone to errors, which can have serious consequences in healthcare. EHR integration reduces the need for duplicate entries by ensuring that data is entered once and accessed by all relevant parties. This not only enhances the accuracy of patient records but also ensures that healthcare providers are working with consistent information.
Regulatory Compliance: The healthcare industry is subject to strict regulations concerning patient data security and privacy. EHR integration can facilitate compliance with these regulations by ensuring that data is securely shared and accessed only by authorized personnel. Integrated systems can also help streamline reporting requirements and improve overall data governance.
Challenges of EHR Integration
While the benefits of EHR integration are significant, the process can be complex and may present several challenges. Different EHR systems often use varying data formats, which can complicate the integration process. Additionally, ensuring data security during transmission is paramount, as any breaches can lead to severe consequences for both providers and patients.
Conclusion
EHR integration is a critical component of modern healthcare that enhances patient care, operational efficiency, and data accuracy. By connecting EHR systems with other healthcare applications, providers can create a more cohesive and collaborative healthcare environment. Despite the challenges associated with integration, the benefits far outweigh the obstacles. As healthcare continues to evolve, the push for seamless EHR integration will be essential for improving outcomes and delivering high-quality patient care. Embracing this technology will not only enhance the patient experience but also streamline operations and foster better collaboration among healthcare providers.
#ehr integration software#ehr integration services#ehr integration api#ehr integration#ehr integration solutions#EMR/EHR INTEGRATION#CUSTOM EHR INTEGRATION SOLUTIONS#ehr data integration
0 notes
Text

Hospitals require Electronic Health Record (EHR) Systems that meet physicians, staff, and patients’ needs. We know doctors and staffs already have enough to worry about; an EHR doesn’t have to fit in one of them. So just to educate you, we’ve put together a very simple, common list of challenges during the EHR implementation.
#benefits of ehr#ehr platforms#ehr development#ehr implementation#ehr integration#ehr system#ehr software
0 notes
Text
Unlocking the Value of EHR Integration Services in UK Healthcare Software Development and Revenue Cycle Management
Amid rising demand and financial pressures, UK healthcare providers are increasingly turning to digital solutions to improve care delivery and manage costs. Among the most impactful strategies are professional EHR integration services—an essential element in advancing both healthcare software development and revenue cycle management (RCM).
What Are EHR Integration Services?
EHR integration services connect clinical and non-clinical systems, such as scheduling, patient portals, and billing, into a cohesive digital ecosystem. These services eliminate data silos, reduce the risk of manual errors, and free up staff to focus on patient care rather than administrative burden.
Beyond Technology: The Strategic Case for Integration
When delivered professionally, integration services are tailored to ensure long-term operability, data security, and compliance with UK standards like HL7 and FHIR. They facilitate interoperability across NHS systems and support regulatory reporting. Financial transparency is also enhanced, improving billing processes and ensuring faster, more accurate reimbursements.
Integration’s Impact on Revenue Cycle Management
Without integration, RCM processes become fragmented, leading to inefficiencies, missed charges, and payment delays. Embedding integration into software development creates a more agile, scalable infrastructure—one that better supports real-time financial tracking, coding accuracy, and a higher standard of patient experience.
Conclusion
For NHS Trusts and independent providers alike, EHR integration services represent a foundational investment in both digital transformation and financial resilience. By streamlining revenue cycles and improving data cohesion, integration enables healthcare organisations to navigate the challenges of modern care delivery more effectively.
0 notes