#fhir software
Explore tagged Tumblr posts
Text

FHIR stands for Fast Healthcare Interoperability Resources. The main functionality of FHIR is to elaborate data formats, resources, and an app programming interface for the prevailing EHR. By letting us integrate the FHIR interoperability into your app, we offer some great features during the entire process. So you need not look back and rest assured of the massive growth of your healthcare business.
#smart on fhir#fhir interoperability#fhir integration#smart fhir#fhir software#smart on fhir applications#smart on fhir integration
0 notes
Text
Hire Best Talent in Healthcare IT
2 notes
·
View notes
Text
HL7 Platforms Explained: The Backbone of Healthcare Communication Standards
In today's fast-changing healthcare environment, a healthcare interoperability solution is essential for seamless communication among various medical systems. Hospitals, labs, clinics, and other healthcare providers use many different software applications, devices, and data formats. Without a proper system to connect these, sharing important patient information can become slow, incomplete, or error-prone. This is where HL7 platforms come in as the foundation for making healthcare data flow smoothly and securely.
HL7 platforms are the key technology behind many healthcare interoperability solutions used worldwide. They help different healthcare systems “talk” to each other using common standards, enabling better coordination of care. In this blog, we will explain what HL7 platforms are, why they matter, and how they support modern tools like FHIR compliant interoperability software. We will also show how healthcare organizations benefit by adopting these platforms.

What is an HL7 Platform?
An HL7 platform is a software framework or tool that supports the HL7 standard for healthcare data exchange. HL7 stands for Health Level Seven, which is a set of international standards that define how health information is packaged and shared between computer systems.
These platforms act as translators and routers. They take medical data from one system, convert it into a common HL7 format, and then send it to another system that understands that format. This process allows different applications — such as electronic health records (EHRs), lab systems, and billing software — to exchange information accurately and quickly.
By using an HL7 platform, hospitals and clinics reduce the need for manual data entry, lower errors, and speed up patient care.
Why Are Healthcare Interoperability Platforms Important?
Healthcare is complex, with many stakeholders involved. Different departments and providers often use different software systems. Without a healthcare interoperability solution, these systems work in isolation, which can cause delays and miscommunication.
Healthcare interoperability platforms help solve this problem by connecting systems and enabling them to share data in real time. They improve patient safety by giving doctors access to complete medical histories, test results, and medication lists without delay. This better communication also cuts costs by avoiding duplicate tests and unnecessary procedures.
Moreover, interoperability platforms help healthcare providers meet regulatory requirements for data sharing and privacy. They build trust by ensuring patient information is exchanged securely and only with authorized parties.

How HL7 Platforms Work with FHIR Compliant Interoperability Software
In recent years, HL7 introduced a newer standard called FHIR (Fast Healthcare Interoperability Resources). FHIR simplifies healthcare data exchange by using modern web technologies such as RESTful APIs and JSON/XML formats. This makes integration faster and easier compared to older HL7 versions.
Many healthcare organizations are now adopting FHIR compliant interoperability software alongside traditional HL7 platforms. This software supports both the HL7 standards and FHIR, providing a flexible way to connect new and legacy systems.
HL7 platforms play a vital role in bridging older systems that use classic HL7 messaging with modern applications designed for FHIR. This combined approach helps healthcare providers gradually upgrade their technology without disrupting patient care.
Benefits of Using HL7 Platforms in Healthcare
Using HL7 platforms as part of a healthcare interoperability solution offers several key benefits:
1. Seamless Data Exchange
HL7 platforms ensure smooth and standardized data flow between different healthcare systems, allowing accurate and timely access to patient information.
2. Enhanced Patient Care
Better data sharing leads to improved diagnosis and treatment decisions. Clinicians have full medical histories and test results at their fingertips.
3. Cost Savings
By reducing duplicated tests and manual paperwork, HL7 platforms lower administrative costs and reduce delays in patient care.
4. Regulatory Compliance
These platforms help meet health data exchange regulations and maintain patient privacy by controlling data access and sharing.
5. Support for New Technologies
HL7 platforms work with FHIR and other modern standards, enabling healthcare providers to adopt innovative digital health tools without starting from scratch.
How Helixbeat Supports Your Healthcare Interoperability Needs
Helixbeat offers advanced healthcare interoperability platforms designed to help organizations manage and exchange health data effectively. With our expertise in FHIR compliant interoperability software, we deliver solutions that connect your existing systems and new digital tools.
Our platforms provide secure, scalable, and easy-to-use interfaces that improve collaboration across healthcare teams. Whether you are implementing HL7 messaging or transitioning to FHIR, Helixbeat’s solutions can adapt to your needs.
Contact us today to learn how Helixbeat can help your organization build a robust healthcare interoperability solution that improves patient outcomes and operational efficiency.

FAQs About HL7 Platforms and Healthcare Interoperability
1. What is the main purpose of an HL7 platform?
An HL7 platform standardizes and manages the exchange of healthcare information between different software systems to improve communication and patient care.
2. How does FHIR relate to HL7?
FHIR is a modern standard developed by HL7 that uses web technologies for faster and easier healthcare data exchange compared to older HL7 versions.
3. Why is healthcare interoperability important?
Interoperability allows different healthcare systems to share patient data efficiently, improving care quality, reducing errors, and cutting costs.
4. Can HL7 platforms work with existing hospital software?
Yes, HL7 platforms are designed to integrate with many legacy systems as well as new healthcare applications, enabling smooth data exchange.
5. How does Helixbeat support healthcare interoperability?
Helixbeat provides scalable and secure interoperability platforms, including FHIR compliant software, that connect diverse healthcare systems seamlessly.
#electronic health record systems#electronic medical records software#FHIR compliant interoperability software#healthcare interoperability platforms#hl7 platform
0 notes
Text
Explore how Xyram's implementation of SMART on FHIR applications streamlines administrative workflows with standardized prior authorization and interoperable data exchange protocols, now live with end-customers.
#it services#software development#digital transformation#enterprise application development#FHIR applications
0 notes
Text

Best Outcomes as a Secure ePRO and Patient Intake Platform:
Reduced Reliance on Centralized Data: By using Best Outcomes for ePROs and patient intake, Ascension hospitals and other healthcare providers can move some patient data to a secure, separate platform. This reduces the attack surface of their core systems.
Enhanced Patient Privacy: Best Outcomes emphasizes patient data privacy. Its focus on security can be a selling point to healthcare providers concerned about data breaches.
Improved Patient Experience: Best Outcomes' streamlined digital patient intake (DPI) can minimize disruptions caused by the cyberattack. Faster registration and reduced waiting times would be a welcome improvement for patients during this challenging time.
Actionable Data and Insights: Even with limited access to central systems, doctors can leverage Best Outcomes' data and insights to continue making informed care decisions.
#Bestoutcomes ePROS tool#PROs tool#Best ePROs tool#ehr software#patientcare#MIPS measures#EMR tool#FHIR tool
1 note
·
View note
Text
HL7 Interface Integration: How is HL7 implemented in Healthcare
In the healthcare landscape, where the seamless and secure exchange of information is paramount, HL7 stands as the linchpin connecting disparate systems and fostering interoperability.
HL7, stands for Health Level Seven, is a set of international standards for the exchange, integration, sharing, and retrieval of electronic health information. It is the most widely used messaging standard in healthcare, facilitating the communication and interoperability between different healthcare systems, devices, and applications.
As per the latest data, approximately 95% of hospitals in the United States utilize HL7 standards to facilitate interoperability and information exchange among healthcare systems and applications. HL7 is the universal language that enables diverse healthcare applications and systems to exchange crucial data.
In the future, as the healthcare industry continues its digital transformation, the significance of HL7 integration cannot be overstated. It not only streamlines communication between different entities within the healthcare ecosystem but also plays a pivotal role in enhancing patient care, improving operational efficiency, and ensuring compliance with evolving standards.
Our guide explores the intricate world of HL7 integration, its standards, benefits, and its transformative influence on healthcare organizations. It introduces you to a trusted partner, Rockit, that leverages the full potential of HL7.
A Closer Look at HL7 And The Primary Data Standards
Delving into the intricate world of HL7 standards, let’s unravel the checklist that defines its essence:
Communication Backbone: HL7 stands as the orchestrator of healthcare platforms, seamlessly weaving a tapestry of communication among diverse systems.
Essential Standards: At the heart of HL7 are pivotal standards—HL7 V2, HL7 CDA, HL7 EHR, and HL7 FHIR—each playing a crucial role in shaping the landscape of healthcare data exchange.
Interoperability Marvel: By ensuring interoperability, diverse healthcare systems can collaborate effortlessly and share vital information.
Revolutionizing Exchange: Overcoming challenges, HL7 spearheads a revolution in data exchange by providing standardized approaches that transcend the complexities of disparate systems.
Core Components: The foundation of HL7 rests on two pillars—the [RIM (Reference Information Model)] and messaging standards, forming a robust structure for the organization and representation of healthcare information.
Blueprint with RIM: The RIM serves as a blueprint, ensuring standardized data organization for consistency across different healthcare entities.
Flexible Messaging: HL7 messaging standards are not rigid; they are customizable to meet the specific needs of different healthcare scenarios.
Continuous Evolution: HL7 is not static; it evolves continuously, adapting to technological advancements and proactively addressing emerging challenges in the dynamic healthcare landscape.
Crucial Role: HL7 is not just an element; it is indispensable, playing a crucial role in enabling the seamless exchange of information and, consequently, elevating the standards of patient care.
What is the Role of HL7 in Healthcare?
With data flowing from diverse systems in healthcare, HL7 emerges as the key to unraveling complexities. The healthcare landscape, with its myriad systems, applications, and devices, demands a unified language for efficient communication. HL7 integration steps into this arena, revolutionizing the exchange of patient information, test results, and medication orders.
By addressing the intricacies of clinical workflows, messaging standards, real-time precision, batch processing, and fortified security protocols, HL7 emerges as the sentient in achieving a cohesive and interconnected healthcare ecosystem.
Enhanced Clinical Workflows
HL7 stands as the guardian of accurate and secure data exchange, ensuring consistency in the flow of information across systems and applications. Employing a sophisticated message-based approach, healthcare systems communicate through HL7 messages, each following a meticulously defined message profile. This profile outlines the format, content, and significance of every data element within the message.
The Symphony of HL7 Messaging Standards
HL7’s versatile messaging standards, known as HL7 v2.x messages, serve diverse purposes, from patient admission to laboratory orders and results reporting. These messages traverse the healthcare network using established transport protocols like TCP/IP or web services, ensuring robust and reliable data exchange.
Real-Time Precision and Batch Brilliance
HL7 messages adapt to the urgency and volume of data, offering real-time precision for critical information like emergency department admissions or laboratory alerts. Simultaneously, the batch mode efficiently handles non-urgent data, such as daily patient summaries or billing information.
Fortified Security Protocols
HL7’s commitment extends to security, with support for multiple communication protocols—TCP/IP, HTTP, and HTTPS. This fortification ensures that healthcare systems exchange data securely over networks. Additionally, HL7 messages can be encrypted and digitally signed, guaranteeing data integrity and confidentiality.
Benefits of HL7 Integration for Healthcare Providers
HL7 integration emerges as a game-changer for healthcare, offering a spectrum of benefits:
Enhanced Interoperability: HL7 breaks down data silos, fostering seamless communication between disparate healthcare systems and improving collaboration.
Elevated Patient Care: Facilitating the exchange of timely and accurate information, HL7 integration provides a comprehensive view of a patient’s medical history, enabling well-informed clinical decisions and ultimately enhancing patient care outcomes.
Revolutionized Workflows: Automation through HL7 integration reduces manual data entry and administrative burdens, allowing healthcare professionals to redirect their focus to direct patient care, thereby improving efficiency and productivity.
Optimized Resource Allocation: Integrating systems and applications enables healthcare organizations to optimize the allocation of resources, leading to cost savings and improved operational efficiency. For instance, HL7 integration facilitates real-time updates on bed capacity, allowing hospitals to make informed decisions about patient admissions and transfers.
The impact of HL7 integration extends beyond breaking down barriers—it transforms the healthcare landscape by promoting collaboration, improving patient care, streamlining workflows, and optimizing resource utilization. The power of HL7 lies in its ability to not only connect systems but to revolutionize how healthcare is delivered and managed.
Use Cases And Challenges of HL7 Integration
Use Cases
HL7 integration finds application in various healthcare settings:
Electronic Health Record (EHR) integration: HL7 facilitates the exchange of patient data between EHR systems, ensuring healthcare providers have access to complete and accurate patient information.
Laboratory information system integration: HL7 allows for seamless communication between laboratory systems and EHRs, enabling timely reporting of lab results and enhancing diagnostic workflows.
Clinical decision support integration: HL7 integration enables the integration of clinical decision support systems with EHRs, providing healthcare providers with real-time alerts, reminders, and evidence-based guidelines for improved decision-making.
Challenges
While HL7 integration offers significant benefits, it is not without its challenges. Some common challenges include:
Data standardization: Ensuring data consistency and standardization across different systems can be complex, requiring mapping and transformation of data elements to match the target system’s requirements.
System complexity: Integrating multiple systems with different technologies and protocols requires careful planning, configuration, and monitoring to ensure smooth data exchange.
Security and privacy concerns: As healthcare data is highly sensitive, maintaining privacy and security during data exchange is crucial. HL7 integration solutions must adhere to stringent data protection regulations, such as HIPAA.
How Can Rockit Help with HL7 and Interoperability?
From app development to expert talent sourcing, Rockit provides robust and scalable end-to-end software solutions that allow healthcare organizations to achieve seamless data exchange and interoperability. Our expertise in HL7 ensures that the solutions we deliver align with industry standards, facilitating effective communication across diverse healthcare systems. By leveraging HL7’s messaging standards, real-time precision, and security protocols, our team ensures that the software solutions we develop contribute to the vision of seamless healthcare, promoting efficient sharing of patient information.
Additionally, Rockit Healthcare solutions prioritize security and compliance, ensuring that patient data is protected throughout the integration process.
By partnering with Rockit, healthcare businesses can unlock the full potential of HL7 integration, streamline their operations, and improve patient care.
Parting Thoughts
As technology advances and healthcare systems become more interconnected, HL7 is poised to play a central role in shaping the data exchange landscape. The ongoing development and adoption of HL7 standards are expected to streamline communication, foster innovation further, and ultimately contribute to a more unified and efficient healthcare ecosystem.
By understanding the importance, benefits, use cases, and challenges of HL7 integration, businesses can make informed decisions and leverage the expertise of companies like Rockit to unlock the full potential of this transformative technology.
Article source: https://rockitteam.com/blogs/hl7-interface-integration-how-is-hl7-implemented-in-healthcare/
0 notes
Text
TYPES OF APIS: A COMPREHENSIVE OVERVIEW
Simple Object Access Protocol (SOAP) APIs are a protocol for exchanging structured information for implementing web services. SOAP APIs use XML for message formatting and are known for their robustness and security features.
0 notes
Text
Why MediBest Leads in Hospital System Software
Hospitals face tighter margins, rising patient expectations, and stricter data-privacy rules. A powerful, future-ready hospital management system software is now the backbone of safe, efficient care. MediBest—India’s most comprehensive hospital software company—unites every clinical, administrative, and financial workflow on one secure platform, giving hospitals an edge today and tomorrow.

What Makes MediBest the Benchmark in Healthcare Management Systems
MediBest was built for real-world hospital pressures: high footfall, complex specialties, and multi-location growth.
Core Modules of MediBest Healthcare Management System Software
MediBest’s healthcare management system software ships with every module hospitals need—no bolt-ons:
Electronic Health Records & CPOE for real-time, error-free documentation.
AI-driven scheduling that balances beds, staff, and theatres.
Integrated billing & claims with payer rules to cut denials.
Pharmacy, inventory & biomedical tracking to curb leakage.
Analytics dashboards comparing live KPIs against national benchmarks.
MediBest encrypts every transaction end-to-end, logs all access, and supports role-based permissions. Quarterly updates keep your hospital aligned with NABH, HIPAA, and upcoming EU AI rules. Bi-directional HL7/FHIR interfaces healthcare management system software near me ensure seamless data flow to labs, imaging, national registries, and public-health portals.
Rapid Implementation Roadmap
Define success metrics—LOS, claim cycle, infection rate.
Phase migration—start with EHR; add billing and inventory next.
Parallel runs to validate data accuracy.
Role-specific training for faster adoption.
Post-go-live audits every 30 days to refine workflows.
MediBest’s specialists handle mapping, testing, and onsite coaching, so IT teams stay focused on care delivery. Click here :
Frequently Asked Questions
1. Why is hospital management system software critical today? It digitizes every workflow—appointments, orders, billing—cutting delays and errors, while giving leaders real-time data to make better decisions.
2. How does MediBest differ from other hospital software companies? MediBest offers a single-platform solution with native PACS, mobile apps, and machine integrations, backed by local 24 × 7 support and modular pricing.
3. Can small hospitals afford MediBest healthcare management system software? Yes. Subscription tiers and lightweight cloud deployment let community hospitals start small and expand features as they grow.
CONTACT :-
MADHYA BHARAT CERAMICS :-
Chandapura Road, Pashupatinath Mandir road, Mandsaur M.P. 458001 India
Email us : [email protected] [email protected] us on : +91-8827697111 (Siddharth Jain) +91-9425105256 (Sushil Jain)
Call us on : +91-8827697111 (Siddharth Jain) +91-9425105256 (Sushil Jain)
0 notes
Text

SMART on FHIR is an extension of FHIR in that it creates a structure for applications that can articulate with a range of healthcare systems. SMART aims to innovate healthcare applications that will enable interoperability and usability. Also, the SMART framework consists of guidelines and tools for developing interchangeable and modular applications that work in various contexts of the healthcare domain. This way, applications developed with the help of SMART on FHIR can function in different contexts without significant adjustments.
0 notes
Text
FHIR Server Fusion: Advanced Healthcare Interoperability Solution for Seamless Data Exchange
Helixbeat’s FHIR Server Fusion enables secure, standardized healthcare data exchange across systems. Enhance interoperability, improve patient care, and streamline clinical workflows with this scalable and efficient healthcare interoperability solution built on FHIR standards.
#healthcare interoperability solution#FHIR compliant interoperability software#healthcare interoperability platforms#hl7 platform
0 notes
Text
How to Choose the Best Healthcare App Development Company
The global healthcare industry is undergoing a digital transformation, and mobile apps are at the forefront of this revolution. From telemedicine and patient engagement to medical records and remote monitoring, healthcare apps have become indispensable for both providers and patients.
But building a secure, compliant, and user-friendly healthcare app is not a simple task. It requires deep domain knowledge, technical expertise, and a clear understanding of healthcare regulations like HIPAA, HL7, and GDPR. That’s why choosing the right healthcare app development company is critical to your project's success.
Whether you’re a hospital, a medical startup, a clinic, or a health tech entrepreneur, this guide will help you make an informed decision when selecting a development partner.
1. Understand Your Project Scope and Goals
Before you start your search, clearly define the goals of your app. Are you building a fitness tracker, a mental health platform, a teleconsultation service, or a full-fledged EHR system?
Knowing your app’s purpose will help you filter out companies that specialize in your required solution. A healthcare software development company with experience in similar projects will understand the user flows, compliance requirements, and performance expectations your app must meet.
2. Look for Industry-Specific Experience
Healthcare is a highly regulated and sensitive domain. Your development partner should not only understand mobile and web technologies but also have industry-specific experience in healthtech.
Check if the healthcare app development company has built apps that involve:
Electronic Health Records (EHR)
Remote Patient Monitoring (RPM)
Telemedicine platforms
Health and wellness tracking
Lab report and diagnostic data integration
AI-based health risk assessments
Such experience proves the company is equipped to handle healthcare-specific challenges like patient privacy, interoperability, and clinical data security.
3. Verify Regulatory Compliance Expertise
One of the most critical aspects of healthcare app development is regulatory compliance. A misstep can lead to legal issues, financial penalties, and a loss of user trust.
Ensure the healthcare software development company has a track record of building apps compliant with relevant healthcare standards, such as:
HIPAA (Health Insurance Portability and Accountability Act) – for U.S.-based apps
GDPR – for handling data of European Union citizens
HL7/FHIR – for interoperability between healthcare systems
FDA regulations – for medical device and diagnostic apps
Ask the company how they handle data encryption, secure login, user authentication, and access control.
4. Evaluate Technical Proficiency and Stack
Your healthcare app will need a solid technology stack that ensures performance, scalability, and data security. A trustworthy healthcare app development company will be proficient in the following:
Frontend: React Native, Flutter, Swift, Kotlin for cross-platform and native development
Backend: Node.js, Python, .NET for server-side logic and API integrations
Databases: PostgreSQL, MongoDB, and healthcare-compliant data storage solutions
Cloud & DevOps: AWS, Azure, or Google Cloud with CI/CD pipelines and scalable architecture
Security: SSL/TLS encryption, biometric authentication, multi-factor authentication (MFA)
Ask to see case studies or code samples to assess their engineering standards.

5. Check Their Portfolio and Case Studies
Reviewing the portfolio of a healthcare app development company is a must. This will help you understand the types of solutions they've built, the industries they've served, and the challenges they've solved.
Ask for client testimonials, live demos, or app store links. Pay close attention to:
Design aesthetics and user interface quality
App speed and responsiveness
Security features and data protection methods
Integration with third-party APIs (e.g., pharmacy APIs, diagnostic labs, payment gateways)
This due diligence gives you confidence in their ability to deliver a healthcare-grade product.
6. Ensure UI/UX Expertise in Healthcare Design
A great app isn’t just functional—it must be easy to use for patients, doctors, and admins alike. Healthcare users range from tech-savvy Gen Z to elderly patients, so the interface needs to be intuitive, accessible, and inclusive.
Choose a healthcare software development company with skilled UI/UX designers who understand healthcare workflows, patient-centric design, and WCAG accessibility guidelines. Features like larger buttons, simplified navigation, and voice commands can improve engagement significantly.
7. Post-Launch Support and Maintenance
Healthcare apps require ongoing support to fix bugs, release updates, comply with new laws, and add features. Ask the company:
Do they offer post-launch support?
How do they handle emergency updates?
What are their SLAs for response and resolution?
A dependable healthcare app development company should be your long-term partner, not just a one-time vendor.
8. Check Pricing and Engagement Models
Pricing should be transparent and flexible. Many companies offer multiple engagement models such as:
Fixed-price (for well-defined projects)
Time and material (for agile, evolving projects)
Dedicated teams (for long-term partnerships)
Make sure the pricing aligns with your budget and allows scalability as your app grows. Also, ask about hidden costs related to hosting, licensing, or third-party APIs.
Final Thoughts
Choosing the best healthcare app development company is a strategic decision that can make or break your healthtech venture. From regulatory compliance and technical expertise to UX design and post-launch support, every aspect must be evaluated carefully.
A reliable healthcare software development company will not only help you build a compliant and scalable app but also empower your business with digital tools that improve patient care, operational efficiency, and health outcomes.
Take your time, ask the right questions, and choose a development partner that truly understands the complexity and responsibility of working in the healthcare space.
For more information, visit us: -
Software Application Development for Logistics
Best Fintech App Developers
App to Buy Groceries
0 notes
Text
Custom Healthcare Software – Bridging Gaps in Specialized Care
No Two Patients Are Alike – So Why Should Their Systems Be?
Healthcare is deeply personal. A treatment plan that works for one person may be completely ineffective—or even harmful—for another. The same logic applies to the systems used to deliver and manage care. Hospitals, clinics, and research institutions often operate with different workflows, specialties, patient populations, and goals. Off-the-shelf software, while useful for general tasks, often falls short in addressing these nuanced needs. That’s where custom healthcare software becomes essential.
Custom healthcare software development services empower medical institutions to build digital tools tailored to their exact requirements. Whether it’s a cancer center managing clinical trials, a rural clinic optimizing resource allocation, or a mental health platform designing a confidential user experience—custom solutions offer unmatched flexibility and precision.
More than just adding unique features, customization allows for deeper integration with legacy systems, regional compliance frameworks, and staff workflows. This leads to smoother operations, better outcomes, and ultimately, a higher standard of care. In a 2023 report by Deloitte, 74% of healthcare executives stated that customization was critical to their digital transformation success.
Custom software is not a luxury—it’s an investment in clinical excellence.
Why Customization Matters
1. Specialized Medical Needs
Oncology centers require software for managing radiation protocols and genetic data
Pediatric care needs developmentally appropriate interfaces and alerts
Psychiatric facilities prioritize secure, confidential data access
2. Workflow Optimization
Tailored dashboards for different departments (ER vs. pharmacy)
Automation of routine administrative tasks
Smart notifications based on local hospital policies
3. Regulatory Adaptability
Custom modules for GDPR, HIPAA, or national-level healthcare compliance
Built-in audit trails and consent management
Support for multiple languages and accessibility standards
Built for Integration
Unlike generic platforms, custom healthcare software is designed to:
Seamlessly plug into existing EHR or HIS systems
Connect with medical devices, wearables, or lab software
Support both cloud-based and on-premise environments
Standards like FHIR (Fast Healthcare Interoperability Resources) are used as the foundation for building APIs that allow secure, real-time data exchange between systems.
Case Study: Specialized Cancer Research Institute
A European cancer research facility partnered with developers to build a custom platform that:
Captured patient-reported side effects in real time
Integrated genomic data from third-party labs
Automatically flagged trial candidates based on health history
The result? Reduced trial onboarding time by 60% and a 22% increase in participant retention.
Conclusion: Software That Reflects Your Mission
A proper and a custom healthcare software and its' development isn't about bells and whistles—it's about alignment. When digital tools reflect the unique goals and needs of an institution, care becomes not only more efficient but more compassionate. For providers striving to go beyond average, custom development is the path to truly transformative care.
0 notes
Text
Epic Integration: A Strategic Investment for Healthcare Efficiency
As healthcare systems evolve, the demand for reliable Epic integration services is growing rapidly. NHS trusts and private providers alike require seamless connectivity between electronic systems to improve patient care, streamline workflows, and ensure compliance. Whether you're implementing Epic for the first time or enhancing existing infrastructure, robust Epic integration solutions are essential.
What is Epic Integration?
Epic integration refers to the process of connecting the Epic Electronic Health Record (EHR) system with other healthcare applications and platforms. This ensures that data flows smoothly across systems, helping healthcare professionals access the right information at the right time. From diagnostics and imaging to billing and scheduling, integration eliminates data silos and enhances operational efficiency.
Benefits of Epic Systems Integration
Epic systems integration delivers tangible benefits for healthcare providers. These include:
Improved clinical workflows: Automatic data sharing reduces manual input, cutting errors and saving time.
Enhanced patient care: Real-time access to comprehensive patient records helps clinicians make better-informed decisions.
Regulatory compliance: Integrated systems simplify audit trails and support data governance.
Cost-efficiency: Integration reduces duplicate testing and administrative overheads.
Whether connecting with third-party software or internal systems, integration is vital for healthcare IT strategy.
Leveraging Epic API Integration
One of the key methods for connecting external applications to Epic is through Epic API integration. Epic provides a range of secure, standards-based APIs such as HL7, FHIR, and proprietary web services. These allow developers to build custom workflows and link apps that support clinicians, patients, and administrators.
From mobile apps that track patient recovery to analytics platforms that enhance population health management, API-driven integrations provide flexibility and innovation.
Epic EHR Integration: A Core Healthcare Priority
Epic EHR integration ensures that all health-related data is centralised and accessible. This is critical for multidisciplinary teams working across various departments. When done right, it enables faster diagnosis, improved treatment planning, and more personalised care.
It also supports nationwide health data initiatives by ensuring interoperability with NHS Digital systems and other healthcare providers.
Understanding Epic EMR Integration
The terms Epic EMR integration and EHR are often used interchangeably. However, EMR typically refers to a patient’s digital medical records within a single organisation. Integration at this level helps clinicians within the same hospital or trust share and update records without delay, leading to more efficient care delivery.
Conclusion:
Investing in expert Epic integration services is no longer optional—it's a strategic move for any healthcare organisation aiming for excellence. From Epic systems integration to Epic API integration, choosing the right partner ensures success in an increasingly connected digital health landscape.
0 notes
Text

The API marketplace software has become an ingenious way for businesses to keep their data structured and easy to coordinate. Whether you go for the HL7 FHIR API or something else,
0 notes
Text
Referral Management Software Trends in 2025

In 2025, referral management software is no longer just a support tool—it's a strategic asset. As someone who has helped clinics and hospital systems implement these platforms, I’ve seen the transformation up close. The shift from outdated manual tracking to intelligent, patient-focused systems is reshaping how care is delivered.
AI-Powered Triage Is Here
Artificial intelligence now sits at the heart of smart referral routing. As reported by KLAS Research, 68% of health networks in 2024 used AI to triage urgent referrals first. This is not only about velocity—it's about accuracy and safety. AI minimizes bottlenecks by directing referrals to the right specialists as soon as possible.
Interoperability Drives Real Results
Smooth integration with CRMs and EHRs is no longer a choice. With the likes of HL7 and FHIR becoming the standard, interoperability is to be expected. "We reduced referral delays by 40% by integrating our referral platform with Epic," states Dr. Leena Patel, an Austin hospital administrator. Data sharing in real-time enables quicker decisions and improved outcomes.
Patients Expect More Transparency
Today's patients demand updates, reminders, and access. Contemporary referral technology is mobile-notificating, self-scheduling, and feedback-enabled. This transformation increases trust and decreases no-shows. No-shows still account for more than $150 billion in lost revenue each year in the U.S.—a figure smart systems are assisting to decrease.
Analytics Are Driving Smarter Decisions
Information is the new currency of healthcare. Referral analytics now inform staffing, detect gaps, and optimize operations. A hospital on the East Coast increased referral completion by 22% after taking action based on intelligence from its dashboard. It's not about the numbers—it's about giving the right care at the right time.
Security Remains Mission-Critical
With increased cyber threats, security is more critical than ever. Contemporary platforms have role-based access, audit trails, and complete encryption. HIPAA and GDPR support are built into the software. In 2025, healthcare providers are putting priority on vendors who prioritize security as a starting point, rather than an afterthought.
Customization Leads the Way
Every practice is unique. Behavioral health clinics are not like orthopedic centers. Leading referral platforms now provide modular architecture and specialty-specific templates. This is a level of flexibility that enables practices to map the software to their precise workflows, minimizing friction and enhancing efficiency.
Conclusion
By 2025, referral management software is setting the standard for how care flows through the system. With AI, patient engagement, and actionable data taking the charge, early adopters are earning a competitive advantage. Smarter referrals are not just a fad—they're the way of healthcare's future.
1 note
·
View note
Text
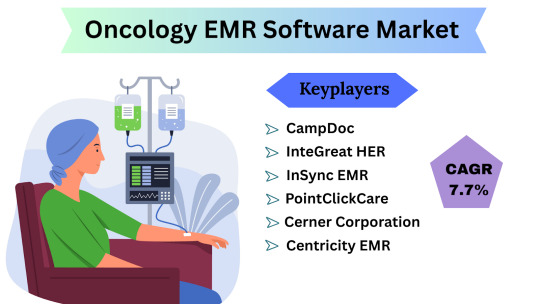
Oncology EMR Software Market Size, Share & Trends Analysis Report By Product ,By End-use, And Segment Forecasts (2024-2031)
Oncology EMR Software Market Overview and Estimation The Oncology EMR (Electronic Medical Records) Software Market Size is poised for steady expansion, driven by growing cancer incidence, the push for value-based care, and the digitization of clinical workflows in oncology centers. According to industry data, the market is expected to grow at a compound annual growth rate (CAGR) of 7.7% from 2024 through 2031, reflecting strong uptake of specialized EMR solutions that integrate treatment planning, chemotherapy ordering, and oncology-specific analytics.
Oncology EMR Software Latest News and Trends In recent months, several key trends have shaped the Oncology EMR landscape:
Artificial Intelligence & Machine Learning Integration Leading vendors are embedding AI-driven decision-support modules into their EMRs to assist oncologists with protocol selection, early adverse-event detection, and personalized treatment pathways.
Interoperability Accelerators The 21st Century Cures Act in the U.S. and similar initiatives in Europe and Asia have intensified focus on seamless data exchange. Oncology EMRs are increasingly adopting FHIR-based APIs to share patient summaries, radiation therapy plans, and pathology results across hospitals, labs, and registries.
Cloud-Native Deployments A shift from on-premises implementations toward cloud-hosted, subscription-based models is underway—driven by lower upfront costs, faster upgrades, and enhanced remote-access capabilities for multi-site cancer centers.
Tele-oncology Modules COVID-era telehealth uptake has extended to specialty care: vendors now bundle video-consultation, e-consent, and remote symptom-reporting features directly within oncology EMRs, reducing the friction of managing virtual visits.
Real-World Evidence (RWE) Collection Payers and life-science firms are collaborating to use de-identified EMR data for RWE studies. Oncology EMRs are being enhanced to capture structured patient-reported outcomes and longitudinal safety data to support post-market surveillance and value dossiers.
Get Free Sample Pdf : https://www.datamintelligence.com/download-sample/oncology-emr-software-market
Oncology EMR Software Market Segmentation
The Oncology EMR market can be described across multiple dimensions, each demonstrating unique adoption dynamics:
By Component: Solutions (software licenses and perpetual-license packages) constitute the bulk of spending, as oncology centers prefer comprehensive suites that encompass treatment ordering, protocol management, and outcome tracking. Services—primarily customization, integration, and training—account for a significant share of revenue, especially among large academic cancer institutes requiring complex interfacing with laboratory, radiology, and pharmacy systems.
By Deployment Type: Historically, on-premises deployments led the market; however, recent migration trends show cloud-based oncology EMRs capturing nearly two-fifths of new deals by revenue share. Smaller hospitals and outpatient clinics favor cloud subscriptions for lower capital expenditure and predictable operating costs, while top-tier cancer centers continue to invest in on-prem deployments for tighter control over data sovereignty and advanced customization.
By End User: Comprehensive Cancer Centers represent the largest end-user segment, given their high patient volumes and the need for integrated care pathways. Hospitals with designated oncology wings follow closely, leveraging EMRs to coordinate multidisciplinary tumor-board discussions. Specialty outpatient clinics and physician practices collectively make up the remaining slice, adopting lightweight, focused solutions for chemotherapy ordering and patient scheduling.
By Functionality: Core modules—patient demographics, clinical documentation, and order entry—comprise the foundational spend. Advanced functionalities such as chemotherapy regimen libraries, radiation therapy interfacing, and billing-code mapping are driving incremental growth, together representing more than half of total annual license revenues.
Oncology EMR Software Regional Analysis: USA & Japan
United States: The U.S. commands the largest slice—approximately 40% of global Oncology EMR revenues—propelled by a mature healthcare IT infrastructure and robust reimbursement frameworks. The 21st Century Cures Act’s information-blocking rules have incentivized providers to adopt interoperable, certified EMR systems, while Medicare’s Oncology Care Model encourages tight integration between EMR data and value-based payment programs. The U.S. market is projected to grow at a CAGR slightly above the global average, fueled by consolidation among health systems and expansion of outpatient oncology networks.
Japan: Japan represents roughly 12–15% of global Oncology EMR spend, with steady annual growth. Government initiatives such as the “Society 5.0” healthcare vision and the Ministry of Health, Labour and Welfare’s push for digital hospital adoption have accelerated EMR deployments. However, slower legacy-system turnover and stringent data-localization policies temper cloud-migration rates. Local players often partner with global vendors to align with Japan’s unique clinical workflows and language requirements.
Key Highlights from Recent Reports
Oncology EMR solutions with integrated clinical-trial matching capabilities are seeing over 20% higher adoption rates at academic cancer centers.
Cloud-hosted oncology EMRs are reducing total cost of ownership by up to 25%, largely through automated updates and shared-service support models.
Interoperability accelerators such as SMART on FHIR apps are projected to triple in number by 2026, enabling rapid third-party innovation within oncology workflows.
Oncology EMR Software Key Players & Competitive Landscape:
The market is moderately consolidated, with the top five vendors holding a combined share of over 60%. Recent M&A and research highlights include:
Epic Systems – Dominant in large health systems; piloting AI-driven regimen optimization tools.
Oracle Cerner – Following the Cerner acquisition, expanding cloud-native oncology modules.
Allscripts – Partnering with life-sciences firms to integrate RWE-capture features.
GE Healthcare – Leveraging its imaging-informatics heritage to offer unified EMR-PACS-RT workflows.
athenahealth – Gaining traction among specialty clinics with its flexible, subscription-based oncology package.
Additionally, smaller niche vendors such as Aria (Oncology Information System by Varian) and Elekta iO EMR continue to innovate around radiation-oncology integrations and research-data export.
Conclusion
The Oncology EMR Software Market is on a solid growth trajectory, underpinned by a projected 7.7% CAGR through 2031. As precision oncology, real-world evidence demands, and regulatory imperatives converge, providers will increasingly seek comprehensive, interoperable EMR platforms tailored to the complexities of cancer care. The transition toward cloud-native deployments and AI-enabled decision support will accelerate operational efficiencies, while regional dynamics—particularly in the U.S. and Japan—will shape adoption paths. Overall, the market is set to mature from a basic digital-record offering into a sophisticated, intelligence-driven platform central to the future of oncology treatment delivery.
0 notes