#smart on fhir integration
Explore tagged Tumblr posts
Text

FHIR stands for Fast Healthcare Interoperability Resources. The main functionality of FHIR is to elaborate data formats, resources, and an app programming interface for the prevailing EHR. By letting us integrate the FHIR interoperability into your app, we offer some great features during the entire process. So you need not look back and rest assured of the massive growth of your healthcare business.
#smart on fhir#fhir interoperability#fhir integration#smart fhir#fhir software#smart on fhir applications#smart on fhir integration
0 notes
Text
Custom Healthcare Software – Bridging Gaps in Specialized Care
No Two Patients Are Alike – So Why Should Their Systems Be?
Healthcare is deeply personal. A treatment plan that works for one person may be completely ineffective—or even harmful—for another. The same logic applies to the systems used to deliver and manage care. Hospitals, clinics, and research institutions often operate with different workflows, specialties, patient populations, and goals. Off-the-shelf software, while useful for general tasks, often falls short in addressing these nuanced needs. That’s where custom healthcare software becomes essential.
Custom healthcare software development services empower medical institutions to build digital tools tailored to their exact requirements. Whether it’s a cancer center managing clinical trials, a rural clinic optimizing resource allocation, or a mental health platform designing a confidential user experience—custom solutions offer unmatched flexibility and precision.
More than just adding unique features, customization allows for deeper integration with legacy systems, regional compliance frameworks, and staff workflows. This leads to smoother operations, better outcomes, and ultimately, a higher standard of care. In a 2023 report by Deloitte, 74% of healthcare executives stated that customization was critical to their digital transformation success.
Custom software is not a luxury—it’s an investment in clinical excellence.
Why Customization Matters
1. Specialized Medical Needs
Oncology centers require software for managing radiation protocols and genetic data
Pediatric care needs developmentally appropriate interfaces and alerts
Psychiatric facilities prioritize secure, confidential data access
2. Workflow Optimization
Tailored dashboards for different departments (ER vs. pharmacy)
Automation of routine administrative tasks
Smart notifications based on local hospital policies
3. Regulatory Adaptability
Custom modules for GDPR, HIPAA, or national-level healthcare compliance
Built-in audit trails and consent management
Support for multiple languages and accessibility standards
Built for Integration
Unlike generic platforms, custom healthcare software is designed to:
Seamlessly plug into existing EHR or HIS systems
Connect with medical devices, wearables, or lab software
Support both cloud-based and on-premise environments
Standards like FHIR (Fast Healthcare Interoperability Resources) are used as the foundation for building APIs that allow secure, real-time data exchange between systems.
Case Study: Specialized Cancer Research Institute
A European cancer research facility partnered with developers to build a custom platform that:
Captured patient-reported side effects in real time
Integrated genomic data from third-party labs
Automatically flagged trial candidates based on health history
The result? Reduced trial onboarding time by 60% and a 22% increase in participant retention.
Conclusion: Software That Reflects Your Mission
A proper and a custom healthcare software and its' development isn't about bells and whistles—it's about alignment. When digital tools reflect the unique goals and needs of an institution, care becomes not only more efficient but more compassionate. For providers striving to go beyond average, custom development is the path to truly transformative care.
0 notes
Text
Referral Management Software Trends in 2025

In 2025, referral management software is no longer just a support tool—it's a strategic asset. As someone who has helped clinics and hospital systems implement these platforms, I’ve seen the transformation up close. The shift from outdated manual tracking to intelligent, patient-focused systems is reshaping how care is delivered.
AI-Powered Triage Is Here
Artificial intelligence now sits at the heart of smart referral routing. As reported by KLAS Research, 68% of health networks in 2024 used AI to triage urgent referrals first. This is not only about velocity—it's about accuracy and safety. AI minimizes bottlenecks by directing referrals to the right specialists as soon as possible.
Interoperability Drives Real Results
Smooth integration with CRMs and EHRs is no longer a choice. With the likes of HL7 and FHIR becoming the standard, interoperability is to be expected. "We reduced referral delays by 40% by integrating our referral platform with Epic," states Dr. Leena Patel, an Austin hospital administrator. Data sharing in real-time enables quicker decisions and improved outcomes.
Patients Expect More Transparency
Today's patients demand updates, reminders, and access. Contemporary referral technology is mobile-notificating, self-scheduling, and feedback-enabled. This transformation increases trust and decreases no-shows. No-shows still account for more than $150 billion in lost revenue each year in the U.S.—a figure smart systems are assisting to decrease.
Analytics Are Driving Smarter Decisions
Information is the new currency of healthcare. Referral analytics now inform staffing, detect gaps, and optimize operations. A hospital on the East Coast increased referral completion by 22% after taking action based on intelligence from its dashboard. It's not about the numbers—it's about giving the right care at the right time.
Security Remains Mission-Critical
With increased cyber threats, security is more critical than ever. Contemporary platforms have role-based access, audit trails, and complete encryption. HIPAA and GDPR support are built into the software. In 2025, healthcare providers are putting priority on vendors who prioritize security as a starting point, rather than an afterthought.
Customization Leads the Way
Every practice is unique. Behavioral health clinics are not like orthopedic centers. Leading referral platforms now provide modular architecture and specialty-specific templates. This is a level of flexibility that enables practices to map the software to their precise workflows, minimizing friction and enhancing efficiency.
Conclusion
By 2025, referral management software is setting the standard for how care flows through the system. With AI, patient engagement, and actionable data taking the charge, early adopters are earning a competitive advantage. Smarter referrals are not just a fad—they're the way of healthcare's future.
1 note
·
View note
Text
Choosing the Right Hospital Management Software

Selecting the best hospital management system software is a high‑stakes decision that shapes how your hospital cares for patients, controls costs, and meets compliance mandates. With hundreds of options on the market, a structured, data‑driven approach helps you avoid expensive missteps and positions your facility for long‑term success.
Define Your Hospital’s Strategic Goals
Begin with a clear vision. List the top three to five outcomes you must achieve in the next three years—such as faster discharge times, seamless telehealth, or tighter revenue‑cycle control. A 2023 HIMSS buyer’s guide recommends aligning software requirements with measurable strategic goals before viewing demos.
Assess Core Modules of a Healthcare Management System
Every healthcare management system should cover these essentials:
Patient Registration & Scheduling
Electronic Health Records (EHR) Integration
OPD/IPD Billing & Insurance
Pharmacy and Inventory Management
Laboratory & Medical Device Interfaces
Business Intelligence Dashboards
Match each module to a documented pain point so you avoid paying for features you will never use.
Evaluate Vendor Reliability and Support
Not all vendors deliver the same level of partnership. Investigate:
Clinical Domain Expertise – proven deployments in tertiary‑care hospitals
24 × 7 Support & Training – on‑site onboarding and local language help desks
Financial Stability – long‑term roadmap and R&D investment
Client References – speak with hospitals of similar size and speciality
According to the World Health Organization’s Digital Health framework, strong vendor governance is critical for sustainable digital‑health programmes.
Compare Deployment and Integration Options
Cloud vs. On‑Premise
Cloud offers lower upfront costs and rapid scaling, while on‑premise installations give you full control of data residency. The U.S. National Institute of Standards and Technology notes that either model can be secure if encryption, access controls, and continuous monitoring are enforced.
Interoperability Standards
Confirm support for HL7, FHIR, DICOM, and open APIs. Seamless exchange with labs, imaging, and national health databases prevents vendor lock‑in and future‑proofs your investment.
Calculate Total Cost of Ownership
Look beyond licence fees. Include:
Implementation & Data Migration
Hardware or Cloud Hosting
Maintenance & Version Upgrades
Training & Change‑Management Costs
Build a five‑year TCO model to see the full financial picture.
Demand Hands‑On Demonstrations and Proof of Concept
Test drive the short‑listed platforms with real workflows:
Map a typical patient journey—appointment to discharge.
Measure click counts, load times, and error rates.
Involve end‑users (nurses, pharmacists, accountants) for feedback.
A structured pilot reveals usability gaps that glossy brochures hide.
Think Long Term: Roadmap and Innovation
Ask vendors about:
AI‑Driven Decision Support – predictive triage, bed forecasting
IoMT Integration – streaming vitals from smart devices
Low‑Code Customization – drag‑and‑drop form builders for rapid tweaks
Regulatory Updates – automatic compliance patches for NABH, HIPAA, GST
Choosing a forward‑looking hospital software company like MediBest ensures your solution evolves with clinical and regulatory demands.
Why MediBest Stands Out
All‑in‑One Platform – clinical, administrative, and financial modules under one login
Scalable Architecture – supports multi‑location networks and thousands of concurrent users
Secure‑by‑Design – field‑level encryption, MFA, and 99.9 % uptime SLA
Rapid Implementation – phased rollouts with dedicated success teams
Extensive Local Support – 24 × 7 hotline and on‑site trainers across India
With MediBest, hospitals gain a robust healthcare management system software that delivers measurable ROI from day one.
Frequently Asked Questions
1. What factors should I consider when selecting hospital management system software? Prioritise alignment with strategic goals, comprehensive modules, interoperability standards, vendor reliability, and total cost of ownership. Hands‑on demos with end‑users are essential.
2. Is cloud‑based hospital management software secure? Yes—if the provider uses ISO 27001‑certified data centres, end‑to‑end encryption, and continuous monitoring. Both cloud and on‑premise models can meet HIPAA and NABH standards when configured correctly.
3. How long does it take to implement a healthcare management system? Timelines range from 4 to 12 months. A phased approach—starting with registration and billing, then adding labs, pharmacy, and advanced modules—minimises service disruption and speeds user adoption.
Ready to See MediBest in Action?
Partner with MediBest, the trusted hospital software company powering digital transformation across India.
Corporate Office 303, IT Park Center, IT Park Sinhasa Indore, Madhya Pradesh, 452013
Call Now +91 79098 11515 +91 97139 01529 +91 91713 41515
0 notes
Text
Why eClinicalWorks Software Integration is the Future of Smart Healthcare?
In today’s fast-paced healthcare environment, integrating systems is no longer a luxury—it’s a necessity. Healthcare providers using ECW EMR and ECW EHR platforms need seamless connectivity to other systems to optimize operations and improve patient care. That’s where eClinicalWorks integration steps in, offering powerful tools to unify various aspects of clinical workflows. From lab systems and medical devices to billing and patient portals, eClinicalWorks integration software makes everything work better together.

What Services Are Covered Under eClinicalWorks Integration?
eClinicalWorks integration services cover a broad range of functions to meet the growing needs of modern healthcare providers. These services empower practices to build a unified and efficient clinical environment.
1. Patient Management Integration: Connects appointment scheduling and patient demographics to ECW EHR systems for a streamlined front-desk experience.
2. Revenue Cycle Automation: Syncs ECW EMR with billing software, automating claim submissions and reducing delays in reimbursements.
3. Lab System Connectivity: Ensures lab reports are automatically delivered into patient records within eClinicalWorks software.
4. E-Prescription Integration: Links ECW to pharmacy networks, making prescription management faster and error-free.
5. Imaging System Integration: Transfers radiology images and reports directly into the patient chart in the ECW platform.
These integrations are designed not only to save time but also to reduce manual errors and data fragmentation across departments.
How Does eClinicalWorks Software Improve Healthcare Workflows?
The beauty of eClinicalWorks software lies in how it simplifies data movement while increasing visibility across teams. It supports structured decision-making by consolidating all clinical data in one place. When the right data is accessible at the right time, outcomes improve naturally. Additionally, by integrating ECW EMR with various systems, providers eliminate redundant documentation and manual entries. This reduces the administrative burden and allows clinicians to focus more on patient care.
How Do Medical Imaging Platforms Integrate With ECW EHR?
Medical imaging plays a crucial role in diagnostics. Integrating these platforms into ECW EHR can enhance clinical accuracy and reduce turnaround times.
Real-Time Access: Images and reports are available instantly inside the patient’s ECW chart.
Reduced Manual Transfers: Eliminates the need for uploading or scanning documents manually.
Streamlined Diagnostics: Radiologists and primary care providers share synchronized data, improving collaboration.
Improved Documentation: Images are tagged and stored automatically in the patient’s electronic chart.
Standardized Communication: Data is shared in standardized formats, enhancing interoperability across platforms.
These features contribute to more efficient and informed medical decisions, benefiting both providers and patients.
What Role Does Laboratory System Integration Play?
Connecting lab systems with ECW EMR software allows for faster clinical action and improved patient satisfaction. eClinicalWorks integration services ensure that lab results are imported directly into the EHR, flagged for provider review, and recorded in the patient's history—all without human intervention. This not only improves turnaround times but also significantly reduces the possibility of transcription errors.
How Do eClinicalWorks Integration Services Support Compliance and Security?
Compliance is a key concern for any healthcare provider. ECW EHR integration is developed to comply with industry standards like HL7 and FHIR. It also ensures HIPAA-compliant data sharing. Whether you're integrating eClinicalWorks software with payment platforms or lab systems, the process respects patient confidentiality and secures sensitive data.
Conclusion:
eClinicalWorks integration is redefining how practices operate, communicate, and care for patients. Whether it’s connecting eClinicalworks EMR software with lab platforms or automating your billing process, eClinicalWorks integration software delivers a reliable, scalable, and secure solution. With the right eClinicalWorks integration services, healthcare providers can streamline operations, minimize risks, and provide better, faster, and smarter patient care.
0 notes
Text
Zambia's Top Hospitals Reveal: Electronic Health Records (EHR) Implementation Leads to 35% Patients Satisfaction Boost

The healthcare sector in Zambia is undergoing a digital revolution, with hospitals and clinics increasingly adopting Electronic Health Records (EHR) Management Systems to enhance efficiency, accuracy, and patient care. Research indicates that medical facilities utilizing EHR medical billing and hospital database management systems experience 25% higher patient satisfaction rates due to streamlined workflows, reduced errors, and improved data security.
This comprehensive guide explores how EHR systems in healthcare, hospital administration systems, and health record systems contribute to superior healthcare delivery while optimizing operational efficiency. We’ll also examine key features of modern EHR solutions and their impact on patient satisfaction in Zambia.
The Importance of Digital Healthcare in Zambia
As Zambia strives to enhance its healthcare infrastructure, the implementation of electronic health systems is a key driver of transformation. In urban centers and rural areas alike, hospitals are seeking reliable hospital database management systems to handle increasing patient loads, complex workflows, and growing demands for quality care.
The transition from manual record-keeping to an electronic health record management system provides a wide range of benefits. These include faster access to patient data, streamlined operations, enhanced communication among departments, and real-time tracking of patient outcomes. In fact, the data indicates that facilities using an integrated hospital electronic medical records system are better equipped to deliver timely, coordinated, and personalized care.
Digital Transformation of Medical Records and Billing Systems
1. Centralized Electronic Health Records (EHRs)
Digital storage of patient histories, diagnoses, treatments, and lab results.
Real-time access improves decision-making and reduces errors.
Eliminates paper records, enhancing efficiency and care continuity.
2. Seamless Interoperability
Secure data exchange between hospitals, clinics, and labs using HL7/FHIR standards.
Reduces duplicate tests and streamlines referrals.
Supports telemedicine, benefiting remote and underserved areas.
3. Secure Role-Based Access Control (RBAC)
Restricts data access by role (doctors, nurses, admins).
Protects patient privacy and prevents unauthorized changes.
Complies with data protection laws (e.g., HIPAA, GDPR).
4. Mobile Access for Healthcare Providers
Doctors access records on smartphones/tablets during rounds or emergencies.
Speeds up treatment with instant patient data retrieval.
Improves care in remote locations with limited infrastructure.
5. Audit Trails for Accountability
Tracks all record access and modifications.
Detailed logging of all system access and modifications
Identifies security breaches for quick resolution.
Ensures compliance with healthcare regulations.
6. Patient Portals for Self-Service
Patients view lab results, book appointments, and request refills online.
Reduces administrative workload for hospitals.
Enhances patient engagement and satisfaction.
ZRA Smart Invoice Integration
Generates tax-compliant digital invoices for healthcare services
Links directly to national revenue authority systems
Tracks and submits all medical invoices digitally
Processes VAT according to regulatory standards
Maintains compliant financial records for audits
Features of Electronic Health Records that Drive Patient Satisfaction
The features of electronic health records contribute directly to improved patient experiences. Here are a few key features that matter:
Real-time Access to Medical History: Healthcare professionals can instantly retrieve patient data, including previous treatments, lab results, prescriptions, and diagnoses.
Accurate and Efficient Medical Billing: EHR in medical billing minimizes human error, reduces claim rejections, and accelerates the reimbursement process.
Integrated Pharmacy Management System: Seamless medication tracking ensures patients receive the right prescriptions at the right time.
Advanced Patient Management Tools: These help with appointment scheduling, reminders, and follow-ups, which significantly enhance the patient journey.
Why EHR Improves Healthcare Delivery
The introduction of an EHR management system improves the workflow for both patients and medical staff. Doctors no longer need to sift through paper files or worry about illegible handwriting. Instead, everything is digitized and easily accessible through a centralized hospital administration system.
Moreover, hospital record management systems ensure that all medical documents, diagnostic reports, and administrative data are stored securely and can be retrieved effortlessly. This not only improves clinical decision-making but also boosts trust between healthcare providers and patients.
With electronic health records in healthcare, coordination across departments improves dramatically. For instance, a doctor in the emergency room can quickly review a patient’s allergies or past surgeries, helping them make accurate, informed decisions on the spot.
Multi-Hospital Networks and Scalability
Zambia is also seeing the growth of multi-hospital networks, and for these, a multi-hospital hospital management system is vital. A centralized system allows seamless communication and data sharing between different branches. Whether a patient visits a hospital in Lusaka or Ndola, their medical records remain consistent and up-to-date.
This interconnected approach leads to better continuity of care and fewer instances of misdiagnosis or treatment duplication. In turn, this consistency fosters a higher level of patient trust and satisfaction.
The Role of HMS Software in Hospital Efficiency
At the heart of this digital transformation is HMS software. This software suite typically includes modules for:
Patient registration and management
Inpatient and outpatient tracking
Laboratory and radiology integration
Billing and financial management
Inventory and pharmacy control
The right hospital management software supports all aspects of clinical and administrative workflows. It acts as a backbone for healthcare facilities aiming to improve service delivery and operational performance.
The Impact on Rural Clinics and Small Facilities
While urban hospitals in Zambia are leading the charge, rural clinics are not far behind. With the help of cloud-based solutions and mobile-compatible platforms, even small healthcare providers can implement a cost-effective health record system.
Cloud-based hospital management systems ensure data is securely stored offsite, minimizing risks associated with physical record loss or data corruption. Furthermore, healthcare workers in remote areas can use tablets or smartphones to update and access records, improving service delivery in under-resourced locations.
Conclusion: A Better Future with EHR Management Systems
The data speaks volumes—Zambian hospitals that embrace electronic health record management systems are seeing measurable improvements in patient satisfaction. As the country continues to prioritize healthcare modernization, the use of electronic health systems, EHR medical billing, and hospital administration systems will play a pivotal role.
Healthcare providers, from large urban hospitals to small rural clinics, must consider the long-term benefits of investing in a comprehensive hospital record management system. With better patient management, improved communication, and efficient operations, EHR is not just a tool—it's a game-changer.
If you're part of a healthcare institution looking to enhance care quality, reduce costs, and boost patient trust, now is the time to explore a reliable HMS software solution.
#EHRSystemsinHealthcare#ElectronicHealthSystems#EHRMedicalBilling#EHRManagementSystem#HealthRecordSystem#HospitalElectronicMedicalRecords#FeaturesofElectronicHealthRecords#ElectronicHealthRecordsinHealthcare#clinicalHealthRecords#hospitalmanagementsystem#EHRinHospitals#InteroperableElectronicHealthRecords#EHRSystem
0 notes
Text
Harnessing the Power of HL7 to Elevate Healthcare Application Development in 2024

HL7 integration in healthcare is now critical for businesses striving to enhance operations and improve patient care. By enabling seamless data exchange across various systems, HL7 integration serves as a cornerstone for data interoperability in healthcare.
Through efficient access, sharing, and use of patient information, HL7 integration supports the delivery of coordinated, high-quality care. It is vital in streamlining clinical workflows, reducing data silos, and ensuring that critical health data is always available. This, in turn, drives significant improvements in both patient outcomes and operational productivity.
With the global healthcare data integration market continuing its rapid growth, organizations are increasingly focused on adopting HL7 standards to remain competitive and elevate their service quality.

This growth highlights how important HL7 integration has become in today’s healthcare, offering greater efficiency and better patient outcomes. By adopting HL7 standards, healthcare organizations can ensure data is shared accurately, quickly, and securely, setting the stage for better patient care and smoother operations.
In this blog, we’ll look at the many benefits and real-world examples of HL7 integration. It will serve as a guide for healthcare businesses on how to use this technology to improve services and boost patient satisfaction.
Key Takeaway:
Integrating HL7 in healthcare app development, breaking down data silos by ensuring seamless communication between isolated healthcare systems, enabling efficient data exchange across various platforms.
HL7 streamlines clinical workflows by automating data transmission, reducing manual errors and administrative burdens, and allowing healthcare professionals to focus more on patient care.
HL7 integration improves operational efficiency by accelerating processes such as billing, scheduling, and claims management, reducing delays and increasing productivity.
HL7 supports telehealth and remote care by enabling telehealth platforms to seamlessly integrate with healthcare systems, improving access to care for patients in remote locations.
Why Does Your Business Need HL7 Integration in Modern Healthcare?

The healthcare industry heavily depends on various IT systems, like Electronic Health Records (EHR) and Laboratory Information Systems (LIS). However, these systems often operate in isolation, creating data silos that obstruct the seamless exchange of information. This breakdown in communication can compromise patient care, and emphasize the need for standardized protocols.
Health Level Seven (HL7) has emerged as a global standard for healthcare data exchange, ensuring system data interoperability across the board. Essentially, HL7 acts as a universal translator, bridging gaps between different healthcare IT systems. Thereby fostering a more cohesive and efficient environment.
To fully harness the power of HL7 integration, healthcare organizations typically adopt two main strategies:
Point-to-Point interface: It facilitates direct data exchanges between two systems, but this approach can be limiting and complex.
HL7 Integration Engine: This serves as sophisticated middleware, streamlining communication across multiple systems by managing data formats and message flow. This reduces the need to develop numerous individual interfaces, significantly simplifying the integration process.
Incorporating HL7 integration isn’t just about boosting data-sharing capabilities. It’s a strategic move that leads to a more unified, efficient, and patient-centered healthcare ecosystem. By adopting HL7 integration, healthcare businesses can achieve real-time information flow, better decision-making, and ultimately, improved patient outcomes.
What is SMART on FHIR?
Fast Healthcare Interoperability Resources (FHIR) provides a standardized framework for healthcare data formats and API-driven access. Its primary objective is to ensure medical data is interoperable, accessible, and shareable across providers, patients, and applications, including those used in medical IoT application development. Essentially, FHIR aims to break down data silos, facilitating seamless healthcare data exchange.
Building on FHIR, SMART on FHIR enhances these capabilities by introducing robust authorization and authentication protocols. This security framework allows healthcare professionals and patients to install or create SMART apps that connect securely to Electronic Health Record (EHR) systems. These apps enable the safe retrieval, sharing, and use of patient data, streamlining clinical workflows and enhancing patient engagement.
SMART on FHIR transforms the healthcare ecosystem by making EHR systems more dynamic and adaptable. By leveraging SMART apps, healthcare providers can implement customized solutions that meet specific clinical needs, without compromising data security. This elevates the potential for more personalized, data-driven care delivery.
Challenges of HL7 in Healthcare App Development
HL7 integration offers substantial benefits for healthcare IT systems, yet it also presents several challenges that can affect both implementation and operational effectiveness. Below is an overview of the primary challenges healthcare organizations face during HL7 integration.
Complexity and Variability of Standards
The complexity and variability of HL7 standards pose significant hurdles to integration. Different healthcare systems often interpret these standards differently, leading to inconsistencies and complications during data exchange. Aligning these varying interpretations requires extensive mapping and customization. This process can be resource-intensive, demanding substantial time and effort to ensure seamless interoperability.
With multiple versions of HL7 in use, compatibility across systems adds another layer of complexity. Successfully navigating these challenges is crucial for achieving smooth data interoperability in healthcare.
Data Privacy and Security Compliance
Protecting patient data during HL7 integration presents a major challenge, as healthcare data is highly sensitive. Compliance with regulations like HIPAA is essential to secure patient information, which must be encrypted and safely transmitted across systems. Every data exchange point introduces potential vulnerabilities for breaches.
Organizations need to invest in robust security measures, such as access controls, audit trails, and regular security assessments. Failing to meet these standards can result in penalties and a loss of trust, making stringent data privacy and security measures critical to the success of HL7 integration.
Interoperability Between Different HL7 Versions
Achieving interoperability across different versions of HL7 is another key challenge. Many healthcare systems operate on varying versions of HL7, complicating the process of data sharing.
Migrating from older versions, like HL7 v2, to newer ones, such as FHIR, often involves complex mapping and translation efforts to maintain data integrity. Differences in data structure and semantics across versions further complicate this migration. Healthcare organizations must invest in specialized interoperability solutions to bridge these gaps, ensuring efficient and accurate data exchange across diverse healthcare IT environments.
Resource and Technical Expertise
The successful implementation of HL7 integration requires specialized resources and technical expertise. The complexity of healthcare data, coupled with HL7 protocols, demands skilled professionals who are well-versed in HL7 integration tools.
Many organizations struggle to find these experts, making the integration process more challenging. Training existing staff or hiring new talent can be both time-consuming and costly.
Additionally, adapting integration tools to meet specific healthcare needs adds another layer of complexity. This underscores the importance of investing in the education and support of healthcare IT professionals to overcome the challenges of HL7 integration effectively.
By addressing these challenges, healthcare organizations can unlock the full potential of HL7 integration, driving more efficient data interoperability in healthcare and better patient outcomes.
Benefits of HL7 in Healthcare App Development

Adopting a standardized framework like HL7 is more than just creating a streamlined data transmission route. It brings multiple advantages that enhance the entire healthcare documentation process. Let’s explore the key benefits of HL7 integration within healthcare systems.
Enhanced Interoperability and Data Exchange
Healthcare operates with a vast array of document management systems. Ensuring their seamless interoperability is crucial for efficient operations. HL7 integration enables smooth data exchange through standardized triggers and message types. For example, events like patient registration, discharge, or order cancellations are transformed into structured messages. These are recognized by the HL7 framework, regardless of the system in use. HL7’s universal code recognition facilitates encrypted and uninterrupted data flow across systems, making information exchange frictionless.
Improved Patient Care Coordination and Outcomes
In healthcare, timely access to accurate information is paramount. HL7 integration accelerates the retrieval of clinical data from various institutions, minimizing the risk of errors due to system incompatibilities. By reducing the time required to gather patient data, HL7 ensures more effective and coordinated patient care. This real-time data access optimizes clinical decision-making and, consequently, improves patient outcomes. In essence, HL7 creates an integrated data ecosystem that enhances the overall quality of care.
Streamlined Workflows and Boosted Efficiency
By automating data management, HL7 integration reduces the manual workload for healthcare providers, allowing them to focus more on patient care rather than wrestling with fragmented systems.
Automation with HL7 also minimizes errors from manual data entry, significantly improving workflow efficiency. Fewer manual tasks translate to quicker documentation processes and a more efficient healthcare environment.
Superior Data Accuracy and Accessibility
Different documentation systems often lead to inconsistent data formats, increasing the risk of transmission errors. HL7 mitigates this by messaging systems to ensure that data remains accurate and intact throughout the transmission process. HL7’s reliability in data integrity reduces errors and safeguards the accessibility of precise information across healthcare app development.
Increased Operational Efficiency
Integrating HL7 streamlines healthcare workflows by reducing manual data entry errors and administrative burdens. Automated data exchanges replace time-consuming manual tasks, which improves productivity and accelerates healthcare operations. This results in faster, more efficient service delivery, optimizing resource utilization across the healthcare system.
Improved Regulatory Compliance
Adhering to healthcare regulations becomes more manageable with accurate data handling. HL7 integration ensures that healthcare organizations comply with privacy laws by automating compliance reporting and reducing manual errors. This not only minimizes the risk of non-compliance penalties but also strengthens trust among patients and regulators by safeguarding sensitive information.
Effective Data Analysis
By unifying data from various sources, HL7 integration makes healthcare data more accessible and interpretable. This supports advanced analytics, enabling healthcare providers to derive deeper insights for improved patient care strategies. Predictive models become more precise, helping identify trends and make informed decisions that enhance treatment plans and preventive care.
HL7 integration empowers healthcare organizations with greater efficiency, compliance, and improved patient outcomes. It lays the foundation for advanced healthcare interoperability, driving innovation and transforming the future of patient care.
Use Cases of Integration of HL7 in Healthcare App Development

Now, the benefits of HL7 integration in healthcare are evident. Let’s dive deeper into practical use cases that demonstrate how it powers modern healthcare app development.
Integration of Electronic Health Records (EHRs)
HL7’s data interoperability is vital for connecting disparate EHR systems across healthcare facilities. By integrating Health Level Seven into EHRs, healthcare professionals can achieve secure, rapid, and seamless patient data exchange. This capability enhances patient care and significantly reduces the time needed to gather essential medical records.
Here’s how the HL7 process works:
A doctor initiates a patient data request from Facility A to Facility B. The HL7 framework converts the request into a specific message format compatible with the receiving EHR system. Upon receiving the request, the second EHR, after granting access, retrieves the data, encrypts it using HL7 protocols, and security sends it back. The original EHR decrypts the data, stores it, and makes it accessible to the healthcare provider.

This streamlined process allows doctors to effortlessly access laboratory results, diagnoses, and prescriptions from various facilities. For patients, this means they no longer need to worry about managing or recalling all their paperwork from multiple institutions. Since HL7 encrypts data during transmission, patients can be assured that their information remains secure.
Automated Laboratory Information Systems (LIS) Connectivity
By automating the transmission of lab results to EHRs, integration HL7 in healthcare app development eliminates manual data entry errors, significantly speeding up the diagnostic process. This integration guarantees rapid delivery of laboratory findings to healthcare providers, enabling faster diagnosis and treatment decisions. Automated la-to-EHR communication boosts clinical efficiency and accuracy, facilitating swift patient care responses.
Enhanced Integration of Radiology Information Systems (RIS) and PACS
The integration of RIS and PACS systems, facilitated by HL7, streamlines the entire diagnostic imaging process. Radiologists can quickly access, share, and interpret medical images, reducing patient wait time for critical diagnoses. This enhanced flow of imagining data across platforms ensures faster analysis and treatment, improving the quality of care for patients undergoing diagnostic tests.
Streamlined Pharmaceutical Systems Integration

HL7 integration empowers pharmacies by connecting them directly with EHR systems, ensuring accurate and timely medication management. It facilitates seamless communication between healthcare providers and pharmacists, reducing prescription errors and simplifying the medication refill process. This real-time connectivity enhances patient safety, optimizes treatment plans, and ensures that prescriptions are handled efficiently.
Real-Time Public Health Reporting
HL7-FHIR integration enables the rapid reporting of diseases to public health authorities, providing real-time data for monitoring health trends. This immediate exchange of information supports faster responses to public health emergencies, such as outbreaks or pandemics. The integration strengthens public health surveillance, ensuring that healthcare systems are equipped to handle health crises efficiently.
Intelligent Clinical Decision Support System (CDSS)
HL7 integration fuels CDSS platforms by providing access to real-time patient data from multiple sources. This allows CDSS to deliver evidence-based, personalized recommendations to healthcare providers, improving decision-making. The system empowers clinicians with actionable insights, ultimately enhancing patient safety, optimizing care pathways, and improving clinical outcomes.
Unified Patient Scheduling Systems

With HL7 integration, healthcare facilities can synchronize appointment schedules across multiple services, eliminating double bookings and reducing patient wait times. This interoperability ensures a smooth, coordinated patient experience, improving satisfaction and operational efficiency. Streamlined scheduling allows healthcare teams to manage resources effectively while ensuring timely care for patients.
Expanding Telehealth Services
HL7 integration revolutionizes telehealth by connecting remote consultation platforms with EHRs, enabling virtual care to be just as efficient as in-person visits. Patients can access healthcare from any location, and providers can easily review medical histories and prescribe treatments digitally. This seamless digital bridge increases healthcare accessibility and reduces the need for physical visits, digitally transforming how care is delivered.
Secure Health Data Interchange (HDI)
HL7 integration ensures the safe and efficient exchange of health data across healthcare institutions, enabling comprehensive, up-to-date patient information at every touchpoint. This secure data sharing supports better-informed treatment decisions and improves the continuity of care, enhancing patient outcomes. HDI networks powered by HL7 create a cohesive healthcare ecosystem where data is shared responsibly.
Efficient Financial and Client Management
HL7 integration automates the process of medical claims submission, processing, and tracking, drastically reducing errors and delays. Healthcare organizations benefit from faster reimbursement cycles, improved cash flow, and more accurate billing. By simplifying claims management, HL7 ensures financial processes are as streamlined as clinical workflows, supporting the financial health of medical institutions.
Conclusion
In today’s fast-evolving healthcare landscape, staying ahead of the curve is essential. The rapid adoption of telemedicine and increasing patient demands for better access and control underscore the need for innovation. HL7 standards have become the backbone of healthcare data integration. For healthcare providers and medtech startups, embracing this opportunity is crucial to building stronger, more efficient data ecosystems. Ultimately, it benefits both businesses and their clients.
At TechAhead, we bring extensive Tech integration expertise to the table. We are committed to ensuring your transition to HL7 is seamless and efficient. Our expert engineers excel in developing and testing reliable software, all within a budget that works for you.
Source URL: https://www.techaheadcorp.com/blog/harnessing-hl7-power-healthcare-apps/
0 notes
Text
The Evolution of IoT in Healthcare Market: From Concept to Reality
The evolution of the Internet of Things (IoT) in the healthcare market has transformed the industry, moving from conceptual ideas to tangible applications that are reshaping patient care, medical research, and healthcare delivery.

Buy the Full Report for IoT in the Healthcare Industry Analysis, Download a Free Sample Report
Here's an overview of the journey from concept to reality:
Conceptualization Phase:
The concept of IoT in healthcare emerged from the recognition of the potential of interconnected devices and sensors to revolutionize medical monitoring, diagnosis, and treatment. Early discussions focused on leveraging IoT technologies to improve patient outcomes, enhance efficiency, and reduce healthcare costs.
Technological Advancements:
Rapid advancements in sensor technology, wireless connectivity, cloud computing, and data analytics laid the foundation for IoT solutions in healthcare. Miniaturization of sensors, improvements in battery life, and the development of low-power communication protocols enabled the deployment of IoT devices in various medical settings.
Pilot Projects and Proof of Concepts:
Healthcare providers, medical device manufacturers, and technology companies began conducting pilot projects and proof of concepts to test the feasibility and efficacy of IoT solutions in real-world healthcare settings. These initiatives focused on areas such as remote patient monitoring, chronic disease management, medication adherence, and preventive care.
Integration with Electronic Health Records (EHRs):
Integration of IoT devices with electronic health records (EHRs) and health information systems became a priority to enable seamless data sharing, interoperability, and accessibility of patient data. IoT-enabled medical devices began to communicate directly with EHR platforms, allowing healthcare providers to access real-time patient information and make data-driven decisions.
Expansion of Use Cases:
The scope of IoT applications in healthcare expanded to encompass a wide range of use cases, including telemedicine, wearable health trackers, smart hospital infrastructure, ambient assisted living, and personalized medicine. IoT-enabled devices and platforms empowered patients to actively participate in their healthcare management and enabled healthcare providers to deliver more personalized and proactive care.
Data Security and Privacy Concerns:
The proliferation of IoT devices in healthcare raised concerns about data security, patient privacy, and regulatory compliance. Healthcare organizations implemented robust cybersecurity measures, encryption protocols, and data privacy frameworks to protect sensitive health information and ensure compliance with regulations such as the Health Insurance Portability and Accountability Act (HIPAA).
Regulatory Frameworks and Standards:
Regulatory agencies and standards organizations developed frameworks and guidelines specific to IoT in healthcare to address safety, efficacy, interoperability, and data security requirements. Standards such as Continua Health Alliance, ISO/IEEE 11073, and Fast Healthcare Interoperability Resources (FHIR) emerged to facilitate the adoption and integration of IoT technologies in healthcare.
Market Growth and Commercialization:
The IoT healthcare market witnessed significant growth as demand for connected medical devices, remote monitoring solutions, and digital health platforms surged. Technology companies, startups, and established healthcare providers capitalized on market opportunities, investing in research, development, and commercialization of IoT-enabled products and services.
Future Outlook:
The evolution of IoT in healthcare continues, with ongoing innovation in areas such as artificial intelligence (AI), machine learning, edge computing, and 5G connectivity. These advancements are expected to further enhance the capabilities of IoT solutions, enabling more precise diagnostics, personalized treatments, and predictive analytics to improve patient outcomes and healthcare delivery.
Overall, the journey of IoT in healthcare from concept to reality has been marked by technological innovation, regulatory scrutiny, and market adoption, with the potential to revolutionize the way healthcare is delivered and experienced in the future.
0 notes
Text
A smart, handy, colposcope for clinics - Gyneye
Women who undergo cervical examinations often report anxiety and heightened stress; they often report negative exam experiences due to concerns about the outcome and the invasive nature of the examination. Therefore, there is a demand for a tool that facilitates a more trauma-informed cervical exam.
The field of cervical examination has taken a big leap with the introduction of portable, handheld, non-contact, digital colposcopes. The method provides clearer and more reliable imaging. Digital colposcopes are designed to provide better magnification and illumination during examination of the cervix, while also being smaller, lighter, and more cost-effective. This allows medical professionals to easily and accurately diagnose and treat cervical diseases.
Precision is the key
Cervical examination relies on accuracy. Sharper imaging allows precise diagnoses, and therefore a precise follow-up care. Gyneye uses medical-grade, high-definition cameras that offer clear imagery, even at high optical zooms, while reducing glare. For instance, with increased magnification, Gyneye's cameras can detect differences in tissue texture, structure and color. These differences would otherwise be missed with a standard stationary colposcope.
A portability approach - for clinics/private practices
Different clinical settings require different approaches. While some facilities are spacious, with plenty of room for equipment, others are small, with limited space. As compared to stationary colposcopes, a handheld digital colposcope like Gyneye is much more compact and portable, and can be handled easily. By doing so, you can free up room space for other medical purposes.
Workflow management & telemedicine
It is possible to seamlessly integrate patients' electronic medical records (EMRs) with Gyneye smart colposcope. By directly uploading images to patient files, the data is immediately available for future reference. Furthermore, by integrating Telemedicine, both Gynecologists and Oncologists can consult together and review images at the same time. This results in better and faster outcomes for patients, particularly in remote settings/community cervical screenings.
Quick exam turnaround times
There is no doubt that digital colposcopes can save an extraordinary amount of time compared to the existing technology. Since every step from the cervical exam to the uploading of images is done digitally, the system can save around 50% of the time. As a result, clinicians and patients can spend less time in vulnerable positions seeking cervical diagnoses. This is a welcome development for both parties. Gyneye's digital colposcopes have revolutionized a once-lengthy process and made it possible to complete it in just a few minutes.
Gyneye Digital Colposcope - What it has to offer
Gyneye digital colposcopes feature ergonomic features and are easy to use and learn. As a result, health practitioners will benefit from enhanced image quality, an improved examination process, a simplified workflow and a shorter examination time. This will equally contribute to a trauma-informed experience for patients.
Gyneye features:
· High-resolution cameras with precise auto-focusing and crystal-clear imagery.
· A second LED light source to capture the true color of tissue to provide an accurate diagnosis.
· The autofocus feature allows for quick examinations without the need to focus and refocus the colposcope and move it around to obtain accurate images.
Engineered to work with low resource settings and advanced medical setup.
HL7 compliant and FHIR-enabled and can interface easily with other hospitals.
Gyneye ensures your clinic, practice, or hospital uses the most advanced colposcopy devices. Please contact us to schedule a free demo and consultation or to learn more about our services. We offer competitive prices and provide ongoing customer service and technical support. Our experienced team is always available to answer any questions you may have. We look forward to hearing from you.
#cervixinwomen#cervicalcancerscreening#cervicalcancer#cervicalcancerscreeningdevice#hpvinwomen#cervix
0 notes
Text
Everything You Need to Know About HL7 FHIR

Explore the comprehensive guide on HL7 FHIR, the healthcare standard driving enhanced interoperability and innovation. Learn about its workings, benefits, implementation steps, and the challenges it addresses in the healthcare industry.
0 notes
Text
New Objectives for EHR Integration & EHR Data Sharing
Long gone are the days when patient access is the all-in-one key to staying ahead in healthtech. What are the interoperability objectives for EHR systems in healthcare today?
Several things motivate and guide hospitals, systems, technology companies, and other care providers regarding EHR interoperability including the need to:
Comply with government and agency laws and rules
Meet customer wants and demands
Prepare for waves of new data from wearables and the Internet of Medical Things (IoMT)
Establish productive partnerships that expand market opportunities
Achieve the highest defined levels of integration success
Sometimes, to make healthcare better and more accessible
Electronic Medical Record Laws and Rules
We’ve seen a long evolution from early EHR development to recognizing the need for interoperability to seeing laws with enough teeth to make it happen. Over time government mandates have also become more technology-specific, leading to the final rules of the Cares Act specifically mandating that payers and other organizations adopt specific FHIR-based interfaces to talk to each other and share data directly with patients.
Consumer and Provider Demands
People today shop for healthcare like they shop for cars or shoes. What’s the best treatment? Which doctors and providers have a strong reputation? How much will it cost?
This new world of empowered consumerism in healthcare demands more patient access to their health records and control over their health journey. They expect providers to let them easily schedule their appointments online, get updated test results and care information, and manage accurate claims and payments.
Without interoperability among all clinical, administrative, and financial systems, this vision fails. If the patient’s front door is locked, hard to open, or only lets you squeeze through a narrow opening, consumers will find a better option.
Healthcare software vendors face similarly elevated expectations. If you’re delivering software hospitals and doctors depend on to deliver care and operate effectively, you must provide the connections to share data with their other systems, partners, and patients.
Wearables and IoMT
An important extension of consumerism: Wearable and other connected healthcare devices. Medical wearable devices have become much more sophisticated, affordable, and accessible, connecting people to healthier lives in ways we only dreamed of even five years ago.
Your watch, armband, or home monitor can collect accurate data for blood pressure, heart rate, glucose levels, EKGs, health activities, and more—and share that data with your doctor. Doctors and patients can collaborate to anticipate health events and adjust treatment courses based on live data.
But this huge new influx of valuable medical data also must integrate with EHRs and other healthcare systems. This will continue in healthcare, as we find more new ways to capture patient data that create additional needs for interoperability. AI and machine learning, as well as FHIR and SMART on FHIR, will help make meaning of and successfully integrate this data.
Building Population Health Partnerships and Networks
Providers increasingly collaborate with ACOs and extended healthcare networks to ensure that people get value-based care and the best experience at every stage of the patient journey. Population health goals also link the healthcare provider communities closer than ever. Some EHR vendors have taken note. Cerner, for example, offers FHIR-based, RESTful APIs to connect with its HealthIntent population health platform.
Meeting Industry Benchmarks
Whenever a new technology option emerges, organizations step in to define the best practices and measures for how to do it as well as it can be done.
The Healthcare Information and Management System Society (HIMSS) has set this bar for data exchange, outlining the four levels of interoperability:
Level 1 – Foundational: Foundational interoperability connects HIT systems for secure data exchange.
Level 2 – Structural: Structural interoperability defines the format, structure, and syntax of data exchange. This allows health information to move between systems without losing its clinical or operational meaning.
Level 3 – Semantic: Semantic interoperability combines standardized data structures, value sets, and vocabulary to interpret data more easily. This improves healthcare quality, safety, and efficiency.
Level 4 – Organizational: Organizational interoperability facilitates secure and timely data sharing through governance, policy, and organizational regulations.
Technology advances the first three levels, while process and governance define the organizational level of interoperability. Healthcare technology companies and providers seek to advance to the highest levels the industry has defined.
Improving Healthcare, Patient Care, & Patient Engagement
It’s easy to forget just why healthcare began this complex, winding, continuing, decades-long journey to interoperability: Better care outcomes for patients. Yet we still see current articles like these telling us about the promise for interoperability to improve healthcare in the future.
Health Level 7 International (HL7) emerged in 1987 as a guiding light and influence for advancing healthcare interoperability with the mission to improve healthcare delivery and patient outcomes. Many providers and technology companies remain passionate about this promise of connecting accurate, updated patient and health data for every stakeholder in the patient journey.
But differing incentives and motivations among EHR vendors continue to complicate and sometimes slow the journey.
Technical Doctor's insight:
Contact Details : [email protected] or 877-910-0004 www.technicaldr.com
0 notes
Text
Dermatology EMR Software Market Trends Forecast Opportunity Analysis-2027

Dermatology EMR Software Market: Regional Analysis
On the basis of region, the global Dermatology EMR Software Market is segmented into North America, Latin America, Europe, Asia Pacific, Middle East, and Africa.
North America is expected to account for largest market share in the dermatology EMR software market, owing to adoption of EMR software with advanced features in the region. For instance, in July 2018, Modernizing Medicine, Inc., a U.S.-based company, at the American Academy of Dermatology (AAD) 2018 Summer Meeting, declared introduction of EMR software with new features such as, Electronic Medical Assistant, (EMA); a mobile EHR system with touch-and-swipe technology and also features the dermatology electronic health record (EHR) system, including electronic prior authorization (ePA), Real-time Prescription Benefit, and Inventory Management.
Furthermore, in March 2018, Spectralink Corporation, a U.S.-based company, released a new line of smart phones designed specifically for use in healthcare. The Spectralink Versity phones are resistant to water and chemicals. The devices run on the latest Oreo Android operating system and has built-in software to seamlessly integrate them with in-hospital EMRs.
Electronic medical records (EMRs) is a part of Electronic Health Records (EHR). Dermatology outpatients include large number of patients with chronic diseases since they need long follow-up durations for cure. Therefore, EMRs in dermatology will be useful in recording dermatological data. EMRs in dermatology also allows streamlined, one-click retrieval of old records, previous investigation reports, medical bills, X-rays, and graphics of affected area on body on which the dermatologist can analyze skin lesions along with rashes, and ulcers.
* The sample copy includes: Report Summary, Table of Contents, Segmentation, Competitive Landscape, Report Structure, Methodology.
Request a sample copy of this report: https://www.coherentmarketinsights.com/insight/request-sample/2240
Dermatology EMR Software Market: Drivers
Increasing awareness for use of EMRs in healthcare sector is expected to propel growth of the dermatology EMR software market. For instance, in November 2017, the Dubai Health Authority (DHA) completed the third and final phase of the unified electronic medical record (EMR) system Salama, in Latifa Hospital, Hatta Hospital, Thalassemia Centre, Dubai Gynecology and Fertility Centre, and all DHA Medical Fitness Centers across the United Arab Emirates (UAE). Salama stores vital patient information such as the medical history of the patient, past surgery details, lab test results, and X-ray reports, which can be easily accessed by any DHA doctor from all DHA facilities across the UAE region.
Moreover, in September 2018, MedX Health Corp., a Canadian company, launched DermSecure, its telemedicine platform, in six Ontario clinics. DermSecure telemedicine platform offers benefits to patients and primary care physicians by working with dermatologists for enhancing their skills in terms of disease diagnosis and treatment.
Furthermore, Apple Inc., in April 2018, launched Apple Health Records feature that combines data of patients’ current heath and data from their past EHR in the health app by using HL7’s Fast Healthcare Interoperability Resource (FHIR) specification. This allow users to know about their drug allergies, medications, and precautions during treatment. It also allow patients to check an EHR patient portal for information such as their laboratory test results. The users need to enter a password to view the information, as the data is encrypted.
Furthermore, advancements in the EMR software is expected to boost growth of the dermatology EMR software market. For instance, in July 2018, Yale School of Medicine in the U.S. developed voice recognition software for EMR, which will reduce time of physicians during patient consulting. Physicians can login once at the start of their shift, which will save physicians time by eliminating 20 to 140 logins per physician per day. This has improved the user experience with EMRs.
Browse Research Report: https://www.coherentmarketinsights.com/ongoing-insight/dermatology-emr-software-market-2240
Dermatology EMR Software Market: Restraint
Increasing cost of EHR services offered by key players is expected to hamper growth of the dermatology EMR software market. For instance, in February 2018, Practice Fusion, Inc., a company in North America, abandoned its business model that contributed to its popularity, as it was offering free EHR software to physicians when it was acquired by Allscripts in 2018. The company later started charging monthly subscription fee of US$ 100 per physician per month for EMR software. Therefore, maintaining the customer base could be a challenge for the company, as it was earlier offering the same service for free.
Moreover, mergers and acquisitions in the U.S. is also expected to drive growth of the market. For instance, in June 2017, athenahealth, a cloud-based EHR company, acquired Praxify Technologies in a US$ 63 million deal. Praxify Technologies originates with a number of applications, including a personal assistant program integrated with EHRs and artificial intelligence aimed at patient engagement. This acquisition is expected to improve athenahealth’s performance in providing their services.
Dermatology EMR Software Market: Competitive Analysis
Strategies adopted by key players such as acquisitions in Asia Pacific region is expected to boost growth of the dermatology EMR software market in this region. For instance, in August 2018, Persistent Systems, an India-based company, acquired Herald Health. Herald Health is a software platform that allows various hospital stakeholders to be automatically notified when data in the EHR and other data systems changes.
Key players operating in the dermatology EMR software market include Encite, Inc., MetaOptima Australia Pty Ltd, CureMD Healthcare, CloudPital, CollaborateMD Inc., eClinicalWorks, CompuGroup Medical, mdconnection, and Practice Fusion, Inc.
Buy-Now this research report: https://www.coherentmarketinsights.com/insight/buy-now/2240
About Coherent Market Insights:
Coherent Market Insights is a prominent market research and consulting firm offering action-ready syndicated research reports, custom market analysis, consulting services, and competitive analysis through various recommendations related to emerging market trends, technologies, and potential absolute dollar opportunity.
Contact Us:
mailto:[email protected]
U.S. Office:
Name: Mr. Shah
Coherent Market Insights 1001 4th Ave,
# 3200 Seattle, WA 98154, U.S.
US : +1-206-701-6702
UK : +44-020-8133-4027
JAPAN : +050-5539-1737
0 notes
Photo

Significance of Mobile Health Apps Testing Today and Tomorrow
From retail to banking to e-commerce industries, there are applications that cover a wide range of services we use daily. The healthcare sector has also started to launch mobile app platforms across the health care delivery cycle, forming a voluminous medical app market.
Mobile health apps and devices are truly making a strong impact in the healthcare sector, as they can easily diagnose disease and prevent the likelihood of developing death-defying medical conditions like diabetes or heart disease.
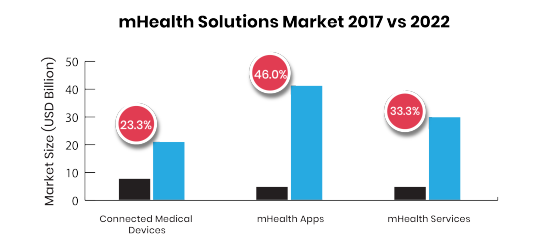
The market of mHealth (mobile health) app has been growing with the adoption of new workflows, technologies, and new business models that are transforming healthcare. With the growing adoption of mobile in this sector, the business opportunity for mHealth apps is also growing exponentially.
Market Scenario and Statistics
The global mHealth app market is estimated at US$28.320 bn in 2018 and is expected to reach up to US$102.35 bn by 2023. (source-Research and Market)
Over 318,000 health apps exist on the top app stores, nearly double the number of apps available in the year 2015 with approx. 200 or more apps being added every day (IQVIA).
These statistics speak that progressively more healthcare providers offer mobile applications to their patients, which ultimately makes the interaction between provider and patient much simpler. An increase in the coverage of mobile cellular networks and the growing accessibility of patient education technology in emerging economies have churned out better prospects for the mobile health market.
Types of mHealth applications
Healthcare Professional Finders
Symptom Checkers
Condition Education and Management
Self-Monitoring
Managing Clinical and Financial Records
Rehabilitation Programs
Remote Patient Monitoring
Prescription Filling and Compliance (Adherence)
Challenges, challenges everywhere
With the exponential growth of mHealth applications, delivering a secure and high-quality working app has become a necessity for user retention. Healthcare is sensitive to changes and innovations as lives are literally at stake. This extra cautiousness creates roadblocks, which may cause difficulties in creating a new healthcare application.
Challenges in the mHealth apps that cause a focus on Quality Assurance:
Meeting Usability Expectations
It does not matter whether your enterprise’s goal is as determined as creating a mobile version of health records or as humble as a recommendation with healthcare professional finders, the app should be convenient to use. Each mobile health app can influence several stakeholders, including caregivers, care team members, insurers, patients, admin staff, and more. The application should support their workflows easily, so QA specialists need to get a clear picture of basic user requirements.
Security and Privacy of the Devices, Data, and Apps
The need to safeguard software from breaches, malicious attacks, and nasty viruses, could disturb the whole development team. In healthcare, there is an answer to cope with such incidents: compliance with HIPAA (Health Insurance Portability and Accountability Act). If the mobile health app is compliant with this legislative regulation, then it is secured.
HIPAA act focuses on the security and privacy of health data and requires added knowledge of the vertical. In particular, QA specialists should thoroughly study the Act to assure that the test is consistent with each section of the regulation applicable to the specific product.
The Demand for Interoperable Systems and Apps
As healthcare software and app is steady goes into the cloud, even legacy systems follow the trend. Undoubtedly, smaller apps are the first to make the move. The resource acclaimed the necessity for interoperability in such applications, as new health IT technologies, priorities, and procedures, will influence changes in accepted standards for data transfer–Health Level Seven (HL7), Digital Imaging And Communications In Medicine (DICOM) and Fast Healthcare Interoperability Resources (FHIR).
QA specialists have to ensure continuous dialogue between their applications and all other systems that could connect to it, counting huge clinical systems (CRM, ERP, EHR), and an extensive choice of smart medical devices and wearable.
If the testing period won’t be consistent with all industry standards and demands, it will cause high operating costs.
Solutions- How ImpactQA Can Help You?
It is essential that mHealth providers should integrate software testing as a vital component of their digital health strategy.
Our experts completely understand the nuisances of Mobile Health applications involving legacy systems, multiple subsystems, voluminous test data, diverse data sources, and complex authentication systems.
Our QA specialists also offer Healthcare software testing solutions for diverse healthcare players such as hospitals, diagnostic centers, pharma companies, clinical labs, third-party administrators (TPA), medical equipment makers, etc.
We offer the following testing services in the healthcare domain:
Usability Testing
Mobile Apps Testing
Functional Testing
Performance Testing
Security Testing
Interoperability Testing
Systems Integration and Interface Testing
Our committed healthcare application test team has the expertise to cater to the requirements for comprehensive healthcare application tests manually and using test automation tools like Selenium, Appium, Robotium, and QTP. Our proficiency lies in building agile and robust test solutions for health institutions that help them address their need for flexible and cost-effective solutions.
LinkedIn: https://www.linkedin.com/company/impactqa-it-services-pvt-ltd/
Twitter: https://twitter.com/Impact_QA
Facebook: https://www.facebook.com/ImpactQA/
Instagram: https://www.instagram.com/impactqa/
P.S. We are always happy to read your comments and thoughts ;)
#ImpactQA#mhealth#mobile health applications#qa#qa testing services#qa testing company#healthcare#mobile health#Software Testing Services#Software Testing Company#software testing tools
0 notes
Text
Breakthrough Of Healthcare Software Development
Over the past few years, the healthcare software development industry has seen dramatic growth because of the increasing concern among hospitals and clinics to manage and monitor patients’ data. The market value of healthcare software is projected to reach around $29.9 billion by 2023. According to a survey, 55% of the American healthcare market uses software in the healthcare industry.
In this article, we will talk about various types of healthcare software available in the market to improve the performance of hospitals and clinics.
FAMILY OF MEDICAL SOFTWARE
There is a variety of software in the healthcare industry available in the market to meet the specific needs of the healthcare organization. Some of the most popular software is discussed below:
Electronic Medical Records (EMR):

EMR stands for Electronic Medical Records, which is patient-centric software. It is the most popular type of hospital management system software used around the globe. It gathers, monitor, and managers patient’s medical record which can only be viewed within one office. It gives access to patient’s information such as lab reports and diagnosis. It helps in the improvement of patient care, service and safety.
Read Also: The Complete Guide Of Telemedicine
Telemedicine:

The field of telemedicine has faced drastically improvements overtimes. About fifty years ago few hospitals started experimenting with it in order to reach patients in remote areas, but nowadays it is also used for convenient medical care. This expectation of more convenient care led to the rise of telehealth/telemedicine software and companies.
It can be real-time telemedicine, remote patient monitoring, and store-and-forward practice. More than half of the U.S. Hospitals currently have telemedicine software. The health IT market reveals that the telemedicine market is valued at nearly $19 billion in 2018.
Billing System:

There is a payment practice within the US healthcare system where the patient receives the medical care and the payment is made by the patient’s health insurance companies. ICD (International Classification of Diseases) codes are assigned to diseases; the hospital submits the claim with the insurance company through a clearinghouse in order to receive payment of services rendered. All these practices are managed by one large software i.e., billing system software.
It should be noted that there can be more than one clearinghouse and insurance companies and this is the reason why billing system software plays a great role here.
Read Also: What Is FHIR? Know About Smart On FHIR
Electronic Health Record (EHR):

Electronic Health Record is larger healthcare software which includes EMR, Telemedicine and billing system. It performs the function of appointment booking and scheduling, and also acts as a clearinghouse. The billing system is the essence of EHR. It contains contact information, appointment information, records of hospitalization and many more services it provides.
This software is becoming increasingly useful as more and more patients are going digital and want to have mobile access to their health records. According to a survey, nearly 86% of physicians have adopted EHR and it is estimated that the market of EHR will grow around $40 billion by 2024.
Hospital Information System (HIS):

Hospital Information System is a large hospital management system software which helps in carrying out management functions like administrative, financial, legal and medical in order to improve the efficiency of healthcare providers. HIS software fulfils the demand of every department. It helps in inventory management, supports the billing system and keeps a track of patient’s data and medication.
Read Also: How Home Health Care Software Became A Big Picture?
HIS offers various advantages like it boost information integrity, reduces duplication of efforts, cut down documentary cost and upgrades report retraction time.
Clinical Information System (CIS):

Clinical Information System is a computer-based platform that allows healthcare providers to store manage and retrieve patients and clinical data. It is large software which takes into account EMR, Clinical Decision Support, and a platform to train doctors.
Adoption of CIS in healthcare can help in drug inventory management and service management and helps to restrain unethical practices. CIS reduces paperwork and improves patient safety by reducing medical error, plus it also grants complete backup of data. CIS receives a massive amount of positive feedback from healthcare administrators.
Home Healthcare:
Well, it falls under the broad category of health care information technology that deals with the storage, retrieval, sharing and use of health care information and data. This is specifically designed for companies employing home health facilities. According to customer surveys by Carecenta, 77% of the businesses using home care management software have minimized their error by 95% than those who are not using.
Home care solutions are versatile depending on the requirements of various agencies. They can be made for the residential care system, permanent care system, and temporary care systems.
last words…
Dreamsoft4u is a custom healthcare software development company, which provides all kinds of healthcare software and deals with clients from all around the globe. We grow up solutions such as Telehealth/Telemedicine, EMR, HER, Practice Management System, Medical Coding and Claim Processing System, RCM, Hospital Information System, Clinic Information System, Homecare, Pharmacy, HL7, HIPPA, Health AI, Web Portals, ERP.
Want to invest in these solutions than contact us.
0 notes
Text
Dermatology EMR Software Market In-deep Analysis and Experts Review Report 2018-2026

Electronic medical records (EMRs) is a part of Electronic Health Records (EHR). Dermatology outpatients include large number of patients with chronic diseases since they need long follow-up durations for cure. Therefore, EMRs in dermatology will be useful in recording dermatological data. EMRs in dermatology also allows streamlined, one-click retrieval of old records, previous investigation reports, medical bills, X-rays, and graphics of affected area on body on which the dermatologist can analyze skin lesions along with rashes, and ulcers.
Dermatology EMR Software Market: Drivers
Increasing awareness for use of EMRs in healthcare sector is expected to propel growth of the dermatology EMR software market. For instance, in November 2017, the Dubai Health Authority (DHA) completed the third and final phase of the unified electronic medical record (EMR) system Salama, in Latifa Hospital, Hatta Hospital, Thalassemia Centre, Dubai Gynecology and Fertility Centre, and all DHA Medical Fitness Centers across the United Arab Emirates (UAE). Salama stores vital patient information such as the medical history of the patient, past surgery details, lab test results, and X-ray reports, which can be easily accessed by any DHA doctor from all DHA facilities across the UAE region.
Moreover, in September 2018, MedX Health Corp., a Canadian company, launched DermSecure, its telemedicine platform, in six Ontario clinics. DermSecure telemedicine platform offers benefits to patients and primary care physicians by working with dermatologists for enhancing their skills in terms of disease diagnosis and treatment.
Furthermore, Apple Inc., in April 2018, launched Apple Health Records feature that combines data of patients’ current heath and data from their past EHR in the health app by using HL7’s Fast Healthcare Interoperability Resource (FHIR) specification. This allow users to know about their drug allergies, medications, and precautions during treatment. It also allow patients to check an EHR patient portal for information such as their laboratory test results. The users need to enter a password to view the information, as the data is encrypted.
Furthermore, advancements in the EMR software is expected to boost growth of the dermatology EMR software market. For instance, in July 2018, Yale School of Medicine in the U.S. developed voice recognition software for EMR, which will reduce time of physicians during patient consulting. Physicians can login once at the start of their shift, which will save physicians time by eliminating 20 to 140 logins per physician per day. This has improved the user experience with EMRs.
Inquire Here Before Purchase of Research Report @ https://www.coherentmarketinsights.com/insight/talk-to-analyst/2240
Dermatology EMR Software Market: Restraint
Increasing cost of EHR services offered by key players is expected to hamper growth of the dermatology EMR software market. For instance, in February 2018, Practice Fusion, Inc., a company in North America, abandoned its business model that contributed to its popularity, as it was offering free EHR software to physicians when it was acquired by Allscripts in 2018. The company later started charging monthly subscription fee of US$ 100 per physician per month for EMR software. Therefore, maintaining the customer base could be a challenge for the company, as it was earlier offering the same service for free.
Dermatology EMR Software Market: Regional Analysis
On the basis of region, the global dermatology EMR software market is segmented into North America, Latin America, Europe, Asia Pacific, Middle East, and Africa.
North America is expected to account for largest market share in the dermatology EMR software market, owing to adoption of EMR software with advanced features in the region. For instance, in July 2018, Modernizing Medicine, Inc., a U.S.-based company, at the American Academy of Dermatology (AAD) 2018 Summer Meeting, declared introduction of EMR software with new features such as, Electronic Medical Assistant, (EMA); a mobile EHR system with touch-and-swipe technology and also features the dermatology electronic health record (EHR) system, including electronic prior authorization (ePA), Real-time Prescription Benefit, and Inventory Management.
Furthermore, in March 2018, Spectralink Corporation, a U.S.-based company, released a new line of smart phones designed specifically for use in healthcare. The Spectralink Versity phones are resistant to water and chemicals. The devices run on the latest Oreo Android operating system and has built-in software to seamlessly integrate them with in-hospital EMRs.
Moreover, mergers and acquisitions in the U.S. is also expected to drive growth of the market. For instance, in June 2017, athenahealth, a cloud-based EHR company, acquired Praxify Technologies in a US$ 63 million deal. Praxify Technologies originates with a number of applications, including a personal assistant program integrated with EHRs and artificial intelligence aimed at patient engagement. This acquisition is expected to improve athenahealth’s performance in providing their services.
Dermatology EMR Software Market: Competitive Analysis
Strategies adopted by key players such as acquisitions in Asia Pacific region is expected to boost growth of the dermatology EMR software market in this region. For instance, in August 2018, Persistent Systems, an India-based company, acquired Herald Health. Herald Health is a software platform that allows various hospital stakeholders to be automatically notified when data in the EHR and other data systems changes.
Key players operating in the dermatology EMR software market include Encite, Inc., MetaOptima Australia Pty Ltd, CureMD Healthcare, CloudPital, CollaborateMD Inc., eClinicalWorks, CompuGroup Medical, mdconnection, and Practice Fusion, Inc.
Dermatology EMR Software Market – Taxonomy
By Deployment
Cloud-based
On-premise
By End Users
Hospitals
Specialty Dermatology Clinics
Cosmetic and Plastic Surgery Centers
Others
By Region
North America
Europe
Asia Pacific
Latin America
Middle East
Africa
About Coherent Market Insights
Coherent Market Insights is a prominent market research and consulting firm offering action-ready syndicated research reports, custom market analysis, consulting services, and competitive analysis through various recommendations related to emerging market trends, technologies, and potential absolute dollar opportunity.
Contact Us
Mr. Shah
Coherent Market Insights
1001 4th Ave, #3200
Seattle, WA 98154
Tel: +1-206-701-6702
Email: [email protected]
0 notes