#pancreatic cancer bilirubin levels
Text
Understanding Jaundice: Causes, Symptoms, Diagnosis, and Treatment

What is Jaundice?
Jaundice is a medical condition characterized by the yellowing of the skin and the whites of the eyes. This yellow color is due to an excess of bilirubin, a yellow-orange bile pigment, in the blood. Bilirubin is produced during the normal breakdown of red blood cells and is usually processed by the liver. When there is a disruption in this process, jaundice can occur.
Causes of Jaundice
Jaundice can be caused by various underlying conditions, which are broadly categorized into pre-hepatic (before bile is made in the liver), hepatic (issues within the liver), and post-hepatic (after bile is made).
Pre-Hepatic Causes:
Hemolytic anemia: Accelerated breakdown of red blood cells increases bilirubin production.
Sickle cell anemia: Abnormal red blood cells break down more rapidly.
Malaria: Infection causes red blood cell destruction.
Hepatic Causes:
Hepatitis: Inflammation of the liver reduces its ability to process bilirubin.
Cirrhosis: Chronic liver damage from various causes leads to scarring and liver dysfunction.
Liver cancer: Malignant cells impair liver function.
Genetic disorders: Conditions like Gilbert's syndrome affect bilirubin metabolism.
Post-Hepatic Causes:
Gallstones: Block the bile ducts, preventing bilirubin excretion.
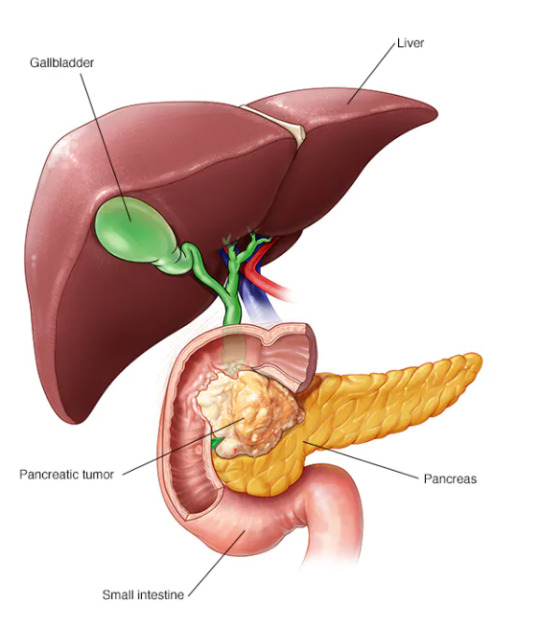
Pancreatic cancer: Tumors can compress the bile ducts.
Biliary atresia: Congenital condition where bile ducts are absent or blocked.
Symptoms of Jaundice
Yellowing of the skin and eyes
Dark urine
Pale stools
Itchy skin
Fatigue
Abdominal pain
Weight loss
Vomiting
Diagnosis of Jaundice
Diagnosing jaundice involves a combination of clinical evaluation and laboratory tests:
Physical Examination: A doctor will look for signs of jaundice and other related symptoms.
Laboratory Tests:
Bilirubin Levels: Blood tests to measure total and direct (conjugated) bilirubin.
Complete Blood Count (CBC): To check for hemolytic anemia.
Liver Function Tests (LFTs): To assess the liver's health and functioning.
Viral Hepatitis Panel: To detect hepatitis viruses.
Imaging Studies:
Ultrasound: To visualize the liver, gallbladder, and bile ducts.
CT Scan/MRI: For more detailed imaging.
Liver Biopsy: In some cases, a small tissue sample from the liver may be examined to determine the cause of liver dysfunction.
Treatment of Jaundice
The treatment of jaundice focuses on addressing the underlying cause:
Pre-Hepatic Jaundice:
Treating the underlying hemolytic disorders or infections.
Hepatic Jaundice:
Hepatitis: Antiviral or immunosuppressive drugs.
Cirrhosis: Lifestyle changes, medications, or possibly a liver transplant.
Liver Cancer: Surgery, chemotherapy, or radiation therapy.
Post-Hepatic Jaundice:
Gallstones: Medications to dissolve stones or surgery to remove them.
Tumors: Surgical removal, chemotherapy, or radiotherapy.
Biliary Atresia: Surgery to reconstruct bile ducts or liver transplant.

Managing Jaundice
Dietary Changes: Eating a balanced diet rich in fruits, vegetables, and lean protein can support liver health.
Hydration: Drinking plenty of fluids helps maintain kidney function and aids in the excretion of bilirubin.
Avoid Alcohol: Alcohol can exacerbate liver damage.
Medication Management: Some medications can cause liver damage; consult a doctor before taking new medications.
When to See a Doctor
Seek medical attention if you notice symptoms of jaundice, especially if accompanied by severe abdominal pain, confusion, or blood in vomit or stool, as these could indicate a serious underlying condition.
Understanding jaundice and its underlying causes, symptoms, diagnosis, and treatment is crucial for effective management and recovery. If you suspect jaundice, it's important to seek medical attention promptly.
Important Information:
Conference Name: 14th World Gastroenterology, IBD & Hepatology Conference
Short Name: 14GHUCG2024
Dates: December 17-19, 2024
Venue: Dubai, UAE
Email: [email protected]
Visit: https://gastroenterology.universeconferences.com/
Call for Papers: https://gastroenterology.universeconferences.com/submit-abstract/
Register here: https://gastroenterology.universeconferences.com/registration/
Exhibitor/Sponsor: https://gastroenterology.universeconferences.com/exhibit-sponsor-opportunities/
Call Us: +12073070027
WhatsApp Us: +442033222718
0 notes
Text
Decoding the Whispering Assassin: Unveiling Pancreatic Cancer Symptoms

Pancreatic cancer is often referred to as the "whispering assassin" because it tends to hide in the shadows, silently advancing before manifesting noticeable symptoms. Understanding the subtleties of these symptoms is crucial for early detection, as pancreatic cancer is notorious for its late-stage diagnosis and high mortality rate. In this article, we will delve deep into the enigmatic world of pancreatic cancer symptoms, shedding light on its covert nature and the importance of recognizing these signs. Let's embark on this journey to decipher the whispers of pancreatic cancer and raise awareness about the critical need for vigilance.
1. The Unseen Intruder: Pancreatic Cancer Unveiled
Pancreatic cancer, a malignant disease that affects the pancreas, can be insidious in its onset. The pancreas, a vital organ located behind the stomach, plays a crucial role in digestion and hormone regulation. However, when cancer invades this organ, it can disrupt its normal functions and lead to a cascade of symptoms.
2. The Silent Onset: Early Pancreatic Cancer Symptoms
Early-stage pancreatic cancer often proceeds without any conspicuous symptoms, making it challenging to detect. Nevertheless, some subtle signs may give an inkling that something is amiss within the pancreas.
2.1. Unexplained Weight Loss
Sudden, unexplained weight loss is a common early indicator of pancreatic cancer. When cancer disrupts the pancreas's ability to produce digestive enzymes, the body struggles to absorb nutrients, leading to unintended weight loss.
2.2. Abdominal Pain
Pancreatic cancer can cause discomfort or pain in the upper abdomen or back. This pain may be dull and persistent, worsening after meals or when lying down. It is often mistaken for other less severe conditions.
2.3. Jaundice
Jaundice, characterized by yellowing of the skin and the whites of the eyes, can occur when pancreatic cancer obstructs the bile duct. This obstruction leads to a buildup of bilirubin in the bloodstream, resulting in the classic yellow hue associated with jaundice.
3. The Hidden Culprit: Advanced Pancreatic Cancer Symptoms
As pancreatic cancer advances, the symptoms become more pronounced and alarming, demanding immediate attention.
3.1. Dark Urine and Pale Stools
The blockage of the bile duct due to pancreatic cancer can also cause changes in urine and stool color. Dark urine and pale stools may signal an issue with the pancreas or bile duct, which should be investigated promptly.
3.2. Loss of Appetite and Nausea
Advanced pancreatic cancer can further disrupt the digestive process, leading to a loss of appetite and persistent nausea. This can make it difficult for individuals to maintain their normal eating habits.
3.3. Blood Clots
Pancreatic cancer can increase the risk of blood clots, leading to conditions such as deep vein thrombosis (DVT) or pulmonary embolism (PE). If you experience sudden pain, swelling, or redness in your limbs, seek medical attention immediately.
3.4. Diabetes Onset or Worsening
In some cases, pancreatic cancer can affect the production of insulin, resulting in the development of diabetes or the worsening of pre-existing diabetes. This sudden change in blood sugar levels should be investigated by a healthcare professional.
4. The Elusive Diagnosis: Pancreatic Cancer and its Mimickers
One of the challenges in diagnosing pancreatic cancer is its ability to mimic other, less severe conditions. This can lead to delayed diagnosis and treatment. Let's explore some conditions that may be mistaken for pancreatic cancer.
4.1. Pancreatitis
Pancreatitis, an inflammation of the pancreas, shares symptoms such as abdominal pain and nausea with pancreatic cancer. A careful evaluation by a healthcare provider is necessary to differentiate between the two.
4.2. Gallstones
Gallstones can also cause abdominal pain and jaundice, making it easy to confuse their symptoms with those of pancreatic cancer. Imaging studies can help determine the underlying cause.
4.3. Gastrointestinal Disorders
Conditions like irritable bowel syndrome (IBS) or gastritis can lead to weight loss and digestive discomfort, similar to early pancreatic cancer symptoms. A thorough examination is essential to rule out cancer.
5. The Importance of Early Detection: Pancreatic Cancer Screening
Given the elusive nature of pancreatic cancer symptoms, early detection becomes paramount for improving survival rates. While there is no routine screening test for pancreatic cancer, certain individuals with risk factors should consider regular check-ups and discussions with their healthcare providers.
5.1. Family History
Individuals with a family history of pancreatic cancer are at an increased risk. Close relatives, such as parents, siblings, or children, who have had pancreatic cancer may indicate a hereditary predisposition. Genetic counseling and screening may be recommended in such cases.
5.2. Inherited Genetic Syndromes
Certain genetic syndromes, such as Lynch syndrome and familial atypical multiple mole melanoma (FAMMM) syndrome, are associated with an elevated risk of pancreatic cancer. Those with a family history of these syndromes should undergo regular screenings.
5.3. Chronic Pancreatitis
Chronic pancreatitis, especially if it develops at a young age, can increase the risk of developing pancreatic cancer. Patients with chronic pancreatitis should be closely monitored.
5.4. Smoking and Obesity
Smoking and obesity have been linked to an increased risk of pancreatic cancer. Lifestyle modifications, such as quitting smoking and maintaining a healthy weight, can help reduce this risk.
6. The Detective Work: Diagnosis and Treatment
When pancreatic cancer is suspected, a series of diagnostic tests are conducted to confirm the presence of the disease and determine its stage. These tests may include:
6.1. Imaging Scans
CT scans, MRI scans, and endoscopic ultrasound (EUS) can provide detailed images of the pancreas, helping doctors assess the tumor's size, location, and spread.
6.2. Biopsy
A biopsy involves the removal of a small tissue sample from the pancreas for examination under a microscope. It is the definitive way to confirm the presence of cancer.
6.3. Blood Tests
Blood tests may reveal elevated levels of specific tumor markers, such as CA 19-9, which can indicate the presence of pancreatic cancer.
7. The Battle Plan: Pancreatic Cancer Treatment
The treatment approach for pancreatic cancer depends on its stage, location, and the patient's overall health. Common treatment options include:
7.1. Surgery
Surgery aims to remove the tumor and, in some cases, a portion of the pancreas. Surgical options may include a Whipple procedure, distal pancreatectomy, or total pancreatectomy.
7.2. Radiation Therapy
Radiation therapy uses high-energy X-rays or other particles to target and destroy cancer cells. It may be used before or after surgery or in combination with chemotherapy.
7.3. Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells or inhibit their growth. It can be administered before or after surgery or as a standalone treatment for advanced cases.
7.4. Targeted Therapy
Targeted therapy drugs are designed to target specific molecules involved in cancer growth. They may be used in conjunction with chemotherapy.
8. The Outlook: Living with Pancreatic Cancer
A diagnosis of pancreatic cancer can be daunting, but it's essential to remember that advances in medical research and treatment options continue to improve the outlook for patients. Support from healthcare professionals, friends, and family is invaluable during this journey.
8.1. Clinical Trials
Participating in clinical trials can provide access to cutting-edge treatments and therapies that may offer hope for improved outcomes.
8.2. Palliative Care
Palliative care focuses on providing relief from the symptoms and side effects of cancer treatment. It can enhance the quality of life for individuals living with advanced pancreatic cancer.
9. The Final Word: Awareness Saves Lives
In the realm of pancreatic cancer, awareness is the key to early detection and improved survival rates. Understanding the subtle signs and risk factors associated with this disease empowers individuals to take action and seek timely medical attention.
Conclusion
Pancreatic cancer may be a silent intruder, but with knowledge and vigilance, its whispers can be heard. Recognizing the subtle symptoms and risk factors associated with this disease is the first step towards early detection and effective treatment. By shedding light on the enigmatic world of pancreatic cancer symptoms, we hope to inspire awareness, encourage early diagnosis, and ultimately save lives. In the battle against the "whispering assassin," knowledge is our most potent weapon.
Read the full article
0 notes
Text
Unraveling the Signs of Liver Metastasis Symptoms
Liver metastasis refers to the spread of cancerous cells from another part of the body to the liver. It is a common occurrence in advanced stages of various types of cancers, including colorectal, breast, lung, and pancreatic cancers. Recognizing the symptoms of liver metastasis is crucial for early detection and effective treatment. In this article, we will explore the common signs and symptoms associated with liver metastasis.
Abdominal Discomfort and Pain:
One of the primary symptoms of liver metastasis is abdominal discomfort or pain. The pain may vary in intensity and can be felt as a dull ache, tenderness, or sharp twinges. The discomfort may be localized to the upper right side of the abdomen, where the liver is situated, or it may radiate to the back or right shoulder.
Jaundice:
Jaundice is a condition characterized by yellowing of the skin and eyes. Liver metastasis can obstruct the bile ducts, leading to a buildup of bilirubin in the body. This excess bilirubin can result in jaundice. Symptoms of jaundice include yellow skin and eyes, dark urine, pale stools, and itching.
Fatigue and Weakness:
Liver metastasis can cause fatigue and weakness due to the compromised liver function. The liver plays a vital role in metabolizing nutrients and removing toxins from the body. When cancer cells invade the liver, it hampers its ability to perform these functions efficiently, leading to fatigue, weakness, and a general decline in energy levels.
Unexplained Weight Loss:
Unintentional weight loss is a common symptom associated with advanced stages of cancer, including liver metastasis. Cancer cells can alter metabolism, leading to a loss of appetite and difficulty in maintaining a healthy weight. If you experience significant weight loss without a clear explanation, it is advisable to consult a healthcare professional for further evaluation.
Enlarged Liver:
As cancer spreads to the liver, it can cause hepatomegaly, or an enlarged liver. An enlarged liver may be palpable during a physical examination or observed through medical imaging tests. It can contribute to abdominal swelling or a feeling of fullness.
Nausea, Vomiting, and Digestive Issues:
Liver metastasis can disrupt normal digestion, leading to symptoms such as nausea, vomiting, and indigestion. The liver produces bile, which aids in the digestion and absorption of fats. When the liver is affected by metastatic cancer, bile production may be impaired, resulting in gastrointestinal disturbances.
Fluid Buildup:
Liver metastasis can disrupt the liver's ability to maintain fluid balance in the body. As a result, fluid may accumulate in the abdomen, causing a condition called ascites. Symptoms of ascites include abdominal bloating, discomfort, and a visibly distended abdomen.
Liver metastasis can present with a range of symptoms, which can vary depending on the extent of the cancer spread and the underlying primary cancer. Early detection and prompt medical intervention are crucial for better treatment outcomes. If you experience any persistent or concerning symptoms associated with liver metastasis, it is essential to consult a healthcare professional for a comprehensive evaluation and appropriate management.
0 notes
Text
When does Pancreatic Cancer show its early warning signs?
The development of malignant cells in the tissues of the pancreas, an organ in the abdomen that is essential for digestion and blood sugar management, results in pancreatic cancer. With only a 10% five-year survival rate, it is a very dangerous kind of cancer. Unfortunately, because pancreatic cancer sometimes doesn't show symptoms until it has progressed to other body areas, it is frequently difficult to diagnose early.
However, being aware of the early indicators of pancreatic cancer can assist raise the likelihood of early discovery, providing greater options for treatment and better results. The finest country in the world for treating pancreatic cancer is India. Understanding pancreatic cancer's early warning symptoms and its consequences in India are crucial.
Pancreatic Cancer: An Overview
Your pancreas is around 6 inches or 15 centimetres long and resembles a pear flipped on its side. Your body produces (secretes) chemicals like insulin to help it metabolise the sugar in the meals you eat. It also produces digestive juices to help in the digestion of meals and nutrient absorption.
The Functions of the Pancreas
The pancreas generates enzymes that aid in the digestion of food and hormones such as insulin that regulate blood sugar levels. It is deep within the abdomen, behind the stomach.
Different Kinds Pancreatic Cancer
There are two forms of pancreatic cancer:
Exocrine tumors
Endocrine tumors
Out of which Exocrine tumours, account for around 95% of cases, grow in cells that manufacture digestive enzymes. Endocrine tumours, also known as pancreatic neuroendocrine tumours (PNETs), arise from cells that create hormones.
The Cause of Pancreatic Cancer
Pancreatic cancer is the outcome of DNA alterations (mutations) in pancreatic cells. A cell's DNA contains the instructions that tell it what to do. These mutations give the cells the instructions to proliferate out of control and continue to exist after normal cells would die. As they accumulate, these cells may become a tumour.
The pancreas, a vital organ in the belly, is affected by pancreatic cancer, a dangerous and sometimes fatal condition. The likelihood of effective therapy increases with earlier pancreatic cancer detection. The importance of early detection and the early warning signals of pancreatic cancer will be covered in this blog.
Progression of Pancreatic Cancer
Although the primary aetiology of pancreatic cancer is unclear, various risk factors have been discovered. Age, family history, smoking and tobacco use, obesity and poor nutrition, chronic pancreatitis, and diabetes are all risk factors.
The Advantages of Early Detection
Early identification of pancreatic cancer can considerably improve treatment outcomes. When pancreatic cancer is detected early, it is more likely to be localised and treatable. Patients with early-stage pancreatic cancer have a substantially better chance of surviving than those with advanced illness.
Pancreatic Cancer Early Detection Challenges
One of the difficulties in detecting pancreatic cancer early is that the disease's early stages frequently do not present any symptoms. When symptoms occur, cancer may have already migrated to other regions of the body, making treatment more difficult.
Screening's Role in Early Detection
Screening techniques, such as imaging scans and blood testing, can aid in the early detection of pancreatic cancer. However, there is no standard pancreatic cancer screening test, and screening is often only suggested for patients who are at high risk for the illness.
Typical Early Warning Signs
Jaundice
It is a disorder in which the skin and eyes become yellow owing to bilirubin accumulation in the body. If the tumour is positioned in the head of the pancreas, where it might block the bile duct, this can be a symptom of pancreatic cancer.
Pain in the abdomen
One of the most prevalent signs of pancreatic cancer is abdominal discomfort. The discomfort is felt in the upper abdomen and might be severe or continual.
Unusual Weight Loss
Even if the person is eating appropriately, unexplained weight loss might occur. It's also a prevalent side effect of pancreatic cancer.
Appetite Suppression
Another symptom of pancreatic cancer is loss of appetite, which can be caused by a combination of causes such as pain and nausea.
Digestive Problems
Nausea, vomiting, diarrhoea, and constipation are all symptoms of pancreatic cancer.
Back Ache
If the tumour is in the body or the pancreas tail, back discomfort is a common symptom.
Pancreatic Cancer comes with multiple Risk Factors
Age: Pancreatic cancer risk increases with age, with most instances occurring in those over 60.
History of the Family: Those with a family history of pancreatic cancer are more likely to get the illness.
Tobacco Use and Smoking: Tobacco use and smoking are key risk factors for pancreatic cancer, with smokers being two to three times more likely than nonsmokers to get the illness.
Obesity and poor dietary habits: Obesity and a high-fat, processed-food diet have been related to an increased risk of pancreatic cancer.
Chronic pancreatitis: Prolonged pancreas inflammation increases the chance of developing pancreatic cancer.
Diabetes: Diabetics are at a slightly increased risk of acquiring pancreatic cancer.
Why is India the best place to seek treatment for pancreatic cancer?
India is well-known for having one of the greatest healthcare systems in the world. Indian Hospitals are outfitted with cutting-edge facilities and medical equipment, making them a popular destination for people seeking superior medical care. This is especially true for patients with pancreatic cancer, since India is home to some of the world's top pancreatic cancer treatment centres and specialists.
India is also recognised for valuing interdisciplinary treatment. This implies that patients are treated by a multidisciplinary team of professionals, including medical and surgical oncologists, radiologists, pathologists, and dietitians. This interdisciplinary approach guarantees that patients receive complete, individualised treatment that is customised to their specific need.
Furthermore, India is at the forefront of pancreatic cancer research, with many of its healthcare facilities conducting clinical trials and studies to create new and creative therapies. In India, patients have access to cutting-edge therapies like immunotherapy and targeted therapy.
Conclusion
India is one of the greatest places for pancreatic cancer treatment, with world-class hospitals, top doctors, and cutting-edge technology. Patients receive thorough and individualised therapy as a result of the emphasis on interdisciplinary care, while continuing research and clinical trials enable access to cutting-edge therapies. While the cost of therapy may be greater in India than in other countries, the quality of care and likelihood of success make it a top choice for patients seeking advanced pancreatic cancer treatment.
0 notes
Text
What is pancreatic cancer? What are the symptoms and treatment methods? 2023
New Post has been published on https://bankakredin.com/what-is-pancreatic-cancer-what-are-the-symptoms-and-treatment-methods-2023/
What is pancreatic cancer? What are the symptoms and treatment methods? 2023
The pancreas is an organ that has very important functions in the body, located at the back of the abdomen and adjacent to the stomach, duodenum and large intestine, which is about 15 cm long. The pancreas ensures the digestion of the consumed foods and keeping the glucose obtained from these foods at the required levels in the blood. Apart from this, the smallest damage to the pancreas, which has many vital functions, can lead to consequences that affect the whole body.
What is pancreatic cancer?
Malignant masses that tend to proliferate in any part of the pancreas are called pancreatic cancer. Although cancers formed in this organ can develop in all parts of the organ, they most commonly spread in the head region. The most common type of pancreatic cancer is adenocarcinoma. Since adenocarcinoma originates from aggressive cells, it can progress rapidly and metastasize to surrounding tissues.
What are the symptoms of pancreatic cancer?
Pancreatic cancer can progress insidiously without any symptoms in its initial stages. However, the most common pancreatic cancer symptoms that started to appear in the later stages are; symptoms such as weight loss, abdominal pain, jaundice, loss of appetite, nausea-vomiting, weakness, fatigue, diarrhea, indigestion, back pain, glass paste-colored stools, pallor, sudden onset diabetes and depression without a family history. Rapid weight loss is seen in patients as a result of malnutrition along with bloating, indigestion and loss of appetite. One of the earliest and most common symptoms is jaundice. Initially, jaundice appears in the eyes, then yellowing of the skin, darkening of the urine color and turning into ‘tea-colored urine’, and finally results in an abnormal lightening of the stool color, defined as ‘glass paste’. The cause of jaundice is the inhibition of the excretion of bilirubin produced by the liver to the duodenum as a result of obstruction of the biliary tract by pancreatic cancer. While the pain is a mild discomfort, which is defined as vague abdominal pain, it takes the form of abdominal pain in the back in the future. It is blunt in nature. It is often associated with symptoms of bloating and indigestion. in the future, it takes the form of abdominal pain that hits the back. It is blunt in nature. It is often associated with symptoms of bloating and indigestion. in the future, it takes the form of abdominal pain that hits the back. It is blunt in nature. It is often associated with symptoms of bloating and indigestion.
What are the causes of pancreatic cancer?
Although the cause of the disease is unknown, it is more common in smokers and obese individuals. In almost 30% of patients, the cause of pancreatic cancer is smoking. Pancreatic cancer associated with adult diabetes is controversial. Having a family history of cancer is also among the causes of pancreatic cancer. The disease is more common in men than women, and the risk of developing this disease increases with age. The average age at catching pancreatic cancer worldwide is 63 for men and 67 for women.
How is pancreatic cancer diagnosed?
Diagnosis can be difficult, especially in the early stages, as the disease presents with insidious symptoms. In patients who apply to the health institution in the early period, it is of great importance that the patient is well examined by the physician and that the necessary diagnostic tests are applied in order to diagnose the disease.
Ultrasonography: Ultrasonography is the first examination method to be applied in the suspicion of pancreatic cancer. The presence of a hard or cystic mass in the pancreas gives information about the size of the mass, its relationship with other surrounding structures, and its proximity to vascular structures.
Laboratory tests: Serum bilirubin, alkaline phosphatase, liver transaminases and values such as CEA, CA19-9 and CA-125 were increased. Bilirubin in the urine is positive.
Computed tomography (CT) and magnetic resonance imaging (MR): CT gives very important information about pancreatic tumors when taken orally and intravenously with contrast medication. It has a diagnostic feature of approximately 95% or more. MR imaging is also important in the differential diagnosis of the tumor. These two examinations can be used together when necessary, ensuring the correct results for the surgery decision to be given to the patient and the correct staging of the tumor.
Individuals diagnosed with the disease as a result of the tests should be evaluated in detail in terms of pancreatic cancer stages, and the treatment process should be started immediately after the stage of the disease is determined.
How is pancreatic cancer treated?
At the beginning of the process for pancreatic cancer treatment, at the end of physical examination, laboratory and radiological examinations, the stage of the pancreatic tumor, its relationship with neighboring organs, especially whether it has spread to adjacent vessels and/or distant organs, and the chance of surgical removal are evaluated. Surgery cannot be performed in advanced stage tumors. Along with the chemotherapy to be applied to these patients, some interventions can be applied to improve the comfort of life by correcting the existing jaundice, providing nutritional support and reducing pain. For this purpose, placing a tube (stent) that provides passage to the bile duct with endoscopy from the mouth through the stomach, draining the bile out with the help of a needle placed from the abdominal skin to the intrahepatic biliary tract with the help of a needle, advanced pain relief techniques,
Surgical Treatment: If the tumor is suitable for surgical removal, ‘Whipple surgery’ is performed. In addition, if the tumor is located in the body and tail of the pancreas, relatively easier resection methods can be applied. Surgical removal of the tumor is the only cure for these patients. In pancreatic head tumors, surgery is more complicated since it is not possible to surgically remove only the head of the pancreas. In Whipple surgery; Together with the head of the pancreas, the gallbladder, part of the main bile duct, duodenum, part of the stomach and surrounding lymph nodes are removed as a block.
Radiation Therapy: Radiation therapy, also called radiotherapy, involves using high-energy rays to kill cancer cells. Radiation therapy only affects cells in the area being treated. Radiotherapy is applied alone or in combination with chemotherapy, especially if the location and size of the tumor complicates the surgery or in cases where surgery cannot be performed. Radiotherapy can be combined with chemotherapy to shrink the tumor before surgery. In some cases, radiotherapy may be given to prevent recurrences after surgery.
Chemotherapy: It is the use of anticancer drugs to kill cancer cells. In pancreatic cancers, drug treatment called chemotherapy can be applied, taking into account the general conditions of the patients before or after surgery. Chemotherapy may be used in conjunction with radiotherapy to shrink the tumor prior to surgery or as a primary treatment in place of surgery. Surgery and radiotherapy have no place in extensive advanced disease. By administering chemotherapy to this group of patients, their quality of life can be significantly improved.
after treatment
Survival: The chance of full recovery after surgery with early diagnosis is less than 50%. Anticancer drugs and radiation therapy increase the rate of recovery. However, survival rates are not good after surgeries that leave cancer cells behind or in cases where there is spread to neighboring organs.
Prevention: In order to prevent pancreatic cancer, it is necessary to stay away from tobacco, eat a balanced diet, do regular exercise and get rid of excess weight.
NOTE: The text here is a general information and may vary depending on the patient and the condition of the disease, so consult with a Medical Oncology specialist for personal evaluation.
what is pancreatic cancer,what are the signs that pancreatic cancer is getting worse,who is pancreatic cancer most common in,does pancreatic cancer,is pancreatic rest cancer,can you have pancreatic cancer without a tumor,can you have pancreatic cancer without symptoms,can you have pancreatic cancer for years without knowing,can you have pancreatic cancer and not know it,can you have pancreatic cancer without pancreatitis,how did i get pancreatic cancer,what type of pancreatic cancer is the worst,what is the end of pancreatic cancer like,what type of pancreatic cancer is curable,what is pancreatic cancer and how do you get it,how do i know what stage my pancreatic cancer is,how do you know what stage pancreatic cancer is,what happens when diagnosed with pancreatic cancer,has anyone cured pancreatic cancer,what do you die of with pancreatic cancer,
#can you have pancreatic cancer and not know it#can you have pancreatic cancer for years without knowing#can you have pancreatic cancer without a tumor#can you have pancreatic cancer without pancreatitis#can you have pancreatic cancer without symptoms#does pancreatic cancer#has anyone cured pancreatic cancer#how did i get pancreatic cancer#how do i know what stage my pancreatic cancer is#how do you know what stage pancreatic cancer is#is pancreatic rest cancer#what are the signs that pancreatic cancer is getting worse#what do you die of with pancreatic cancer#what happens when diagnosed with pancreatic cancer#what is pancreatic cancer#what is pancreatic cancer and how do you get it#what is the end of pancreatic cancer like#what type of pancreatic cancer is curable#what type of pancreatic cancer is the worst#who is pancreatic cancer most common in
0 notes
Text
post ain't long it's wrong, can't study till dawn? yawn
100 days of productivity
day 44 + 45
CVS/RS
rheumatoid pleural effusions closely mimic complicated parapneumonic effusion on analysis, w/ ph <7.2, marked ↑LDH and notably glucose <30 (in fact glucose >30 almost rules out rheumatoid effusion)
in afib, digoxin will slow ventricular rate but is unlikely to cardiovert the rhythm
itraconazole in ABPA causes a 50% reduction in steroid dose and 25% reduction in anti-aspergillus IgE, and either partial or complete resolution of CXR infiltrates or improvement in PFTs/exercise tolerance
TRALI can happen as early as 15 minutes into the transfusion apparently?????
mesothelioma is an abject death sentence. The most you can do for patients beyond stage 1 is chemotherapy (limited survival benefit with platinics), radiotherapy to biopsy/thoracoscopy tracts only and surgery (lung-sparing debulking ± pleurodesis for recurrent effusions; radical surgery has shown no survival benefit)
mild tachy + broad qRs in haemodynamically stable pt s/p PCI for MI → likely to be LBBB developing; watch and wait
CNS/Ophthal/Psych
PSP looks similar to parkinson's bc it affects the opposite pathway as parkinsons (striatonigral vs nigrostriatal)
the best response you can get from deep brain stimulation for parkinsons = the best response you got from medication; DBS will NOT add a greater response compared to maximum medical therapy
without any other information, parkinson's ssx w/ dementia WITHIN 1 year of onset, it's Lewy body dementia; if it's more than 1 year, it's parkinson's w/ 2° dementia
choroidal neovascularisation with NO OTHER fundal signs: wet mac degen > diabetic retinopathy
focal dystonias are better treated with botox than with medication
SAH is unlikely to cause cranial nerve palsies other than III and maybe VI; pituitary apoplexy presents similarly with very severe headache/projectile vomiting/AMS, while affecting nerves III, IV, V-1 and VI
MS relapse: 500 mg PO or 1 g IV methylpred x5 days
there is no difference in risk of progression to Korsakoff when Wernicke is treated w/ glucose first vs w/ thiamine first
Endocrine/Repro
hyperaldosteronism: hyperplasia > adenoma
acute alcohol consumption can trigger hypoglycaemic events as the liver uses up NAD+ for each step of the alcohol detox pathway, where NAD+ is an important cofactor for the malate-oxalate shuttle used in gluconeogenesis
cinacalcet's major indication is hyperparathyroidism taht can't be corrected w/ surgery (eg, unfit pts)
Rheum/Derm/Immuno
topical steroid potency: hydrocortisone < clobetasol butyrate, betamethasone valerate low-dose < betamethasone valerate high-dose, fluticasone propionate < clobetasol propionate
onycholysis: trauma, tinea (infections), thyrotoxicosis, tetracyclines
pseudoxanthoma elasticum is assoc w/ mitral prolapse, renovascular htn, PVD, CAD, GIT bleeds and retinal vessel abnormalities
IgE values are normally distributed, so about 2.5% of the pop has raised IgE and 2.5% has reduced
s/p parathyroidectomy → acute drop in PTH → bones that are used to high levels of PTH experience a relative hypoPTHism → ↑blastic ↓clastic activity → acute bony uptake of calcium, PO4 and importantly magnesium = hungry bone syndrome (replace calcium and magnesium!)
carpal tunnel pain can radiate retrogradely to the forearm and sometimes even the arm
periarticular osteoporosis → RA
punched out erosions in juxtaarticular bone → gout
GIT
Peutz-Jeghers: small bowel hamartomas → intussusception, colorectal cancer, pigmented lesions (classically perioral/mucosal, but also palms/soles)
pernicious anaemia: parietal cell Abs (common) > intrinsic factor Abs (specific)
haemochromatosis: venesection → keep ferritin <50 and transferrin sat <50%
passing stools frequently, elevated inflammatory markers, ↑faecal calprotectin, PPI but not in demographic for IBD → take a colonoscopy and biopsy, this is probably microscopic colitis (and PPIs can trigger at any age)
liver biopsy is not indicated for Gilbert's—it is sufficient to do routine CBCs/LFTs w/ bilirubin analysis
pancreolauryl (fluorescein dilaurate) is quite nonspecific and will not pinpoint the exact pancreatic disease
hep A can be precided by short diarrhoeal illness`
in an IBD (esp UC) pt who comes >10 yrs after initial symptoms with recent change in bowel habits, offer urgent colonoscopy to r/o ca colon BEFORE starting on treatment
Onc/Haem
MTX + antifolate antibiotics: makes sense not to give them together—they can cause fulminant marrow failure
leukaemia can very rarely lead to acute painful scrotal swelling
5q- syndrome = myelodysplasia, but with thrombocytosis; diff from essential thrombocythaemia by anaemia with normal reticulocyte count and leukopaenia in the former
radiotherapy is a primary modality of tx in retinal, CNS, skin, oesophageal, cervical, vaginal and prostatic tumours; it is adjuvant in all other tumours
the commonest presentations of CMV s/p txp are pneumonia or pulmonary infiltrates
Renal/Biochem
SIADH causing drugs - SIADH Causes Poor Voiding: Sedatives (barbiturates), Indomethacin (NSAIDs), Antidepressants (TCAs/SSRIs), thiazide Diuretics, 1st gen antiHistamines, Cyclophosphamide/antiConvulsants, 1st gen antiPsychotics, Vinca alkaloids
malaria: irreversible nephrosis (esp memb or FSGS) > nephritis
2° syphilis: reversible nephritis > nephrosis
even if the patient doesn't qualify for ACEis/ARBs for HTN, give them first-line anyway if concomitant renal disease
kidney size difference >1 cm is significant
for drugs that will be dialysed out on dialysis days, dose them immediately after dialysis on those days
only urge incontinence is not primarily managed with pelvic floor exercises
Pharm/Toxo
valproate ADRs - VALPROATE: Vomiting, Alopecia/Anorexia, Liver tox, Pancreatitis/PCOS, Redistributed fat (weight gain/lipodystrophy), Oedema, hyperAmmonaemia/Ataxia, Tremor/Thrombocytopaenia, Enzyme inhibitor
opioid withdrawal: methadone is the best single tx and avoids needing to give multiple drugs to cover ssx (eg, clonidine + dextromethorphan + loperamide)
aminoglycosides preferentially affect proximal tubular cells
the classic pattern of symptoms in both cotton workers and workers at factories that process nitrates is that of 'Monday disease'
toxicities for which measuring the blood levels is indicated - SLIME TiPP: Salicylates, Lithium, Iron, Methanol, Ethylene glycol, Theophylline, Paraquat, Paracetamol
amphetamine tox → hyponatraemia due to water retention, worsened by the excessive thirst; hyperkalaemia → rhabdo; hypokalaemia not seen because amphetamines tho sympathetomimetic do not have affinity for the β2 receptor like cocaine does
#100 days of productivity#studyblr#studying#med school#medblr#mine#long post#very long post#don't be mad that i f-#i love that vine so much tbh
18 notes
·
View notes
Text
Kidney function tests
Creatinine
Creatinine is a waste product produced in muscles from the breakdown of a creatine.
Creatine is part of the cycle that produces energy needed to contract muscles.
Both creatine and creatinine are produced at a relatively constant rate.
Almost all creatinine is excreted by the kidneys, so blood levels are a good measure of how well your kidneys are working.
If low:
Low levels are not common and are not usually a cause for concern.
As creatinine levels are related to the amount of muscle the person has, low levels may be a consequence of decreased muscle mass (such as in the elderly) but may also be occasionally found in advanced liver disease.
If high:
Kidneys break down creatinine - if levels are high, they’re not working properly -->
Damage to or swelling of blood vessels in the kidneys (glomerulonephritis) caused by, eg, infection or autoimmune diseases bacterial infection of the kidneys (pyelonephritis)
Death of cells in the kidneys’ small tubes (acute tubular necrosis) caused, for example, by drugs or toxins
Prostate disease, kidney stone, or other causes of urinary tract obstruction.
Reduced blood flow to the kidney due to shock, dehydration, congestive heart failure, atherosclerosis, or complications of diabetes
Creatinine blood levels can also increase temporarily as a result of muscle injury and are generally slightly lower during pregnancy.
Urea
Urea is the final breakdown product of the amino acids found in proteins. Nitrogen in the form of ammonia is produced in the liver when protein is broken down. The nitrogen combines with other chemicals in the liver to form the waste product urea. Healthy kidneys remove more than 90% of the urea the body produces.
If Low:
Low urea levels are not common and are not usually a cause for concern. They can be seen in severe liver disease or malnutrition but are not used to diagnose or monitor these conditions. Low urea levels are also seen in normal pregnancy.
· If high:
High urea levels suggest poor kidney function.
Acute or chronic kidney disease.
However, there are many things besides kidney disease that can affect urea levels such as decreased blood flow to the kidneys as in congestive heart failure, shock, stress, recent heart attack or severe burns; bleeding from the gastrointestinal tract; conditions that cause obstruction of urine flow; or dehydration.
Albumin
Albumin is the most abundant protein in the blood. It keeps fluid from leaking out of blood vessels; nourishes tissues; and transports hormones, vitamins, drugs, enzymes, and ions like calcium throughout the body. Albumin is made in the liver and is extremely sensitive to liver damage.
If low:
Low albumin concentrations in the blood can suggest liver disease. Liver enzyme tests are requested to help determine which type of liver disease.
Diseases in which the kidneys cannot prevent albumin from leaking from the blood into the urine and being lost.
Also seen in severe inflammation or shock.
Conditions in which the body does not properly absorb and digest protein such as Crohn’s disease.
If high:
High albumin concentrations in the blood usually reflect dehydration.
This is a very long list so click keep reading to read the rest!
Phosphate
In the body, phosphorus is combined with oxygen to form a variety of phosphates (PO4). Phosphates are vital for energy production, muscle and nerve function, and bone growth. They also play an important role as a buffer, helping to maintain the body’s acid-base balance.
If low: (hypophosphataemia)
Hypercalcaemia (high levels of calcium), especially when due to high levels of parathyroid hormone (PTH)
Overuse of diuretics (drugs that encourage urination)
Severe burns
Diabetic ketoacidosis after treatment
Hypothyroidism
Hypokalaemia (low levels of potassium)
Chronic antacid use
Rickets and osteomalacia (due to Vitamin D deficiencies)
Increased production of insulin
If high: (hyperphosphataemia)
Kidney failure
Hypoparathyroidism (underactive parathyroid gland)
Hypocalcaemia (abnormally low levels of calcium)
Diabetic ketoacidosis when first seen
Phosphate supplementation
Alkaline phosphatase
Alkaline phosphatase is an enzyme found in high levels in bone and liver. Smaller amounts of ALP are found in the placenta and in the intestines. Each of these makes different forms of ALP (isoenzymes).
If low
Zinc deficiency. Magnesium deficiency. Anaemia. Poor nutrition.
Hypophosphatasia (Metabolism disorder, in born). Hypothyroidism. Wilsons disease.
If High:
Raised levels of ALP are usually due to a disorder of either the bone or liver.
If other liver function tests are also raised, this usually indicates that the ALP is coming from the liver.
However, if calcium and phosphate measurements are abnormal, this suggests that the ALP might be coming from bone.
In some forms of liver disease, such as hepatitis, ALP is usually much less elevated than AST or ALT.
However, when the bile ducts are blocked (for example by gallstones, scars from previous gallstones or surgery, or by a tumour), ALP and bilirubin may be increased much more than either AST or ALT.
ALP can also be raised in bone diseases such as Paget’s disease (where bones become enlarged and deformed), in certain cancers that spread to bone or in vitamin D deficiency.
Calcium
99% of calcium is found in the bones, and most of the rest circulates in the blood. Roughly half of calcium is referred to as 'free' (or 'ionized') and is active within the body; the remaining half, referred to as 'bound' calcium, is attached to protein and other compounds and is inactive.
If low: (hypocalcaemia)
The most common cause of low total calcium is low protein levels, especially low albumin. When low protein is the problem, the 'free' calcium level remains normal.
Underactive parathyroid gland (hypoparathyroidism)
Decreased dietary intake of calcium
Decreased levels of vitamin D
magnesium deficiency
too much phosphate
acute inflammation of the pancreas
chronic kidney disease
calcium ions becoming bound to protein (alkalosis)
bone disease
malnutrition, and alcoholism.
If high: (hypercalcaemia)
Hyperparathyroidism (increase in parathyroid gland function) usually caused by a benign tumour on the parathyroid gland.
Cancer when spread to the bones, which releases calcium into the blood, or when it causes a hormone similar to PTH to increase calcium levels.
Hyperthyroidism, Sarcoidosis, Tuberculosis, Too much Vit D, Drugs that increase diuretics.
Potassium:
Abnormal concentration can alter the function of the nerves and muscles.
If low: (hypokalaemia)
vomiting,
diarrhoea, and insufficient potassium intake (rare).
In diabetes, potassium concentration may fall after insulin injection.
If high:
(hyperkalaemia)
kidney disease
Addison's disease
tissue injury
infection
diabetes
excessive intravenous potassium intake (in patients on a drip)
Glucose:
If low: (hypoglycaemia)
Adrenal disease (Addison's disease)
Alcohol/ drugs, such as: paracetamol and anabolic steroids
Extensive liver disease
Hypopituitarism
Hypothyroidism
Insulin overdose
Insulinomas (insulin-producing pancreatic tumours)
If high:
High levels of glucose most frequently indicate diabetes, in fasting blood glucose test: <7mmol/L is indicative and in oral glucose test ites <11 mmol/L .
Acromegaly
Acute stress (response to trauma, heart attack, and stroke for instance)
Long-term kidney disease
Cushing's syndrome
Drugs, including: corticosteroids, tricyclic antidepressants, oestrogens (birth control pills and hormone replacement therapy [HRT]), lithium..
Hyperthyroidism
Pancreatic cancer. Pancreatitis
Triglyceride:
Most triglycerides are found in fat (adipose) tissue, but some circulate in the blood to provide fuel for muscles to work.
If low:
Hyperthyroidism. Malnutrition. Certain medications and drugs can deplete fat, leading to low triglycerides.
If high: (e.g. at least 10-15 mmol/L) --> pancreatitis.
Parathyroid hormone:
Part of a ‘feedback loop’ that includes calcium, PTH, vitamin D, and to some extent phosphate and magnesium. PTH is secreted into the bloodstream in response to low blood calcium concentration.
If both PTH and calcium results are normal, and appropriate relative to each other, then it is likely that the body’s calcium regulation system is functioning properly.
Low --> conditions causing hypercalcaemia, or to an abnormality in PTH production causing hypoparathyroidism.
High --> hyperparathyroidism, which is most frequently caused by a benign parathyroid tumour.
Calcium - PTH Relationship
Calcium low and PTH high, then PTH working. Low calcium may be investigated.
Calcium low and PTH normal or low --> hypoparathyroidism.
Calcium high and PTH --> hyperparathyroidism.
Calcium normal and PTH high --> vitamin D deficiency or chronic kidney disease.
Amylase
Released from the pancreas into the digestive tract to help digest starch. It is usually present in the blood in small quantities. When cells in the pancreas are injured or if the pancreatic duct is blocked (by a gallstone or rarely by a tumour) increased amounts of amylase find their way into the bloodstream.
If high:
Pancreatitis which is a severe inflammation (often 5-10 times normal)
Cancer of the pancreas, gallbladder disease, a perforated ulcer, obstruction of the intestinal tract, mumps or ectopic pregnancy.
Increased blood amylase with normal or low urine amylase may indicate decreased kidney function or the presence of macroamylase.
#medicine#biomed#biomedicine#notes#medblr#studyblr#sciblr#premed#nursing#biology#human biology#med#biomedical science#science#renal#renal system#kidneys#kidney#kfts#kft#kidney function tests#clinical#chemistry#biochemistry#2#3#tests
472 notes
·
View notes
Text
Anion gap, alk/acidosis, lipase, A1C, UUN, labs, specialized labs, clinical presentation, BUN, Creatinine
Anion gap (will cover this in more depth with diabetes) is calculated from sodium level – (chloride + bicarbonate). You could do (sodium + potassium) – (chloride + bicarbonate). Potassium contributes so little that it’s often omitted, however. Anion gap means something else is contributing to the acid-base balance, not just the exchange of chloride for bicarbonate, for example.
Metabolic acidosis: Low pH, a low HCO3- concentration. Compensatory hyperventilation that contributes to a decreased pCO2. Most common causes: Inability of kidneys to excrete dietary hydrogen ion load, increase in hydrogen ion generation due to an addition of hydrogen ions or a loss of bicarbonate
Metabolic alkalosis: High pH, a high bicarbonate- concentration, and compensatory hypoventilation that contributes to an increased pCO2. Most common causes: loss of gastric acid from vomiting or nasogastric suction, loss of intravascular volume and chloride from diuretic use. Overtreatment of metabolic acidosis with bicarbonate. Excess of acetate in PN (parenteral nutrition), which becomes metabolized to bicarbonate
A1C distinguishes between diabetes and hyperglycemia associated with metabolic stress
Protein: Again:
First start by converting the protein intake of the patient (94g in this example) to grams of nitrogen. Second, calculate their nitrogen balance. We find that the patient is in negative nitrogen balance. Nitrogen balance should be the same amount of nitrogen coming into the body as is coming out in the urine. Third: Correct the deficit to get into nitrogen balance. Take that -2g of deficit that they are at (take the minus sign away), and multiply that by 6.25g of protein (1g of nitrogen = 6.25g of protein). Correcting the deficit of nitrogen finds that the patient will require 12.5 more grams of protein just to get into nitrogen balance. Fourth, we still need the patient to be in positive nitrogen balance, so, we increase protein and shoot for 2g more protein to promote anabolism (goal for anabolism is +2-4g of nitrogen a day more). So, that low end we are aiming for is 2g of nitrogen: 2N (6.25g of protein/1g of nitrogen) = 12.5g of protein needed to put the patient in positive nitrogen balance. Fifth, we want to try to promote anabolism, so we have to add the amount of protein that puts the patient at nitrogen balance to the amount of protein that puts the patient in positive nitrogen balance, and add the sum of those two to the amount of protein the patient is taking in (the 94g). Hence the new protein goal is 94g + 12.5g + 12.5g = 119g of protein/day or approximately 120g of protein per day.
Remember: even though you prescribed 100g of protein a day, the patient only actually got 94g. So, that’s why you use 94g in these calculations.
A valid 24-hour urine collection can be difficult to collect
Conversion factor of UUN to total nitrogen excretion may not be accurate in certain conditions: burns, major wounds, diarrhea, vomiting
Factor of 0.85 converts UUN to TUN
Assumes that 85% of urinary nitrogen is from urea
Other nitrogen sources in urine= ammonia, proteins
Conditions that alter or increase ammonia excretion will lead to underestimation
Ex if Adam had liver disease and ammonia excretion was higher/ UUN only 75%
◦ UUN = 13 (13/0.75) = 17 (vs 15)
Diminished renal function alters results
For the most part you are addressing whether the patient is renal insufficient or dehydrated. BUN:Cre ratio, if high BUN and Cre is normal, then it's usually dehydration. If the BUN and Cre are high, it's often renal failure.
LABS:
K+, Cr, and Phosphate are often looked at when assessing kidney function. K+, Mg2+, phosphate are often looked at together as well
Refeeding syndrome (hemodilution, hemodynamics) is indicated by labs. Lab error (e.g. blood that has been sitting out too long, things degrade), stress impacts labs, components of the blood (e.g. serum iron) need to be looked at with other portions of bloodwork. Disease states affect labs. High blood glucose can begin to displace sodium, causing sodium to appear low (false low result), like in diabetic ketoacidosis.
• Think about which labs are affected by which organ system
• Lungs: chloride, acetate
• Kidneys: BUN, creatinine, potassium, phosphorus, albumin, calcium
• Heart: Sodium, BUN (volume status)
• Pancreas: Blood glucose, serum lipase
• Liver: Liver function tests
• Liver disease: colloidal pressure AKA oncotic pressure. With liver disease, you’re not going to make as much visceral proteins (like albumin), which hang onto the water portion of the blood. If albumin is not hanging on, it will start to seep out and accumulate in different places (third spacing).
• Pleural effusions are seen commonly in malignancy. Ascites from cancer, for example. Just because patient doesn't have liver disease doesn't mean they won't have issues with fluid. Extra fluid creates a dilution efffect (causing sodium and albumin, calcium, etc. appear low. If you take those labs at face value, you can be thrown off.
Liver disease: colloidal pressure AKA oncotic pressure. With liver disease, you’re not going to make as much visceral proteins (like albumin), which hang onto the water portion of the blood. If albumin is not hanging on, it will start to seep out and accumulate in different places (third spacing).
Pleural effusions are seen commonly in malignancy. Ascites from cancer, for example. Just because patient doesn't have liver disease doesn't mean they won't have issues with fluid. Extra fluid creates a dilution effect (causing sodium and albumin, calcium, etc. appear low. If you take those labs at face value, you can be thrown off.
Serum sodium doesn't really relate to dietary sodium. Serum sodium is a marker of fluid status, because salt is like a sponge and pulls in a lot of fluid. So, if sodium is really low, often times there’s a fluid issue going on. High sodium indicates a fluid deficit.
• Potassium: 3.4– 5.1 mmol/L
• Magnesium: 1.7 – 2.6 mg/dL
• Low magnesium can make it difficult to successfully replete potassium and phosphorus (SO YOU WANT TO MAKE SURE MAGNESIUM IS NORMAL)
• Phosphorus: 2.4 – 4.3 mg/dL
Story: Patient with a phosphorus of 7 starting nutrition at a slow rate, but then his team gave him a bunch of dextrose-containing fluids to correct a sodium issue, and his phosphorus then dipped to a 2! This results from massive refeeding. The trends in your potassium, magnesium, phosphorus are important. What essentially happened was that the glucose (dextrose) activated insulin, and insulin activation caused a massive shift intracellularly of phosphorus, leading to lower levels of phosphorus in the blood. When not eating much, your cells aren’t taking in magnesium and phosphorus, etc. So, again, sugar stimulates intracellular shift because insulin will activate when sugar is reintroduced, leading to even lower blood levels of minerals. Your heart won’t have enough potassium to beat properly, your lungs won’t have enough phosphorus to breathe well. Certain diuretics can lead to potassium deficiency, E.g. thiamin follows potassium (Wernicke's Encephalopathy), certain diuretics that are potassium wasting come with a risk of thiamin deficiency. Can fix this by prophylactically give thiamin in anticipation of potassium drop.
CONSEQUENCES OF REPLETING TOO QUICKLY
• Low potassium: cardiac arrhythmia, cardiac arrest
• Low magnesium: seizure, coma
• Low phosphorus: respiratory distress, difficulty breathing/getting off mechanical ventilation
Patients who are at risk for refeeding syndrome can have a number of different conditions to begin with:
• Anorexia nervosa
• Chronic alcoholism
• Cancer
• Post-surgery (NPO for many days pre- and post-op)
• Elderly (poor dentition, reduced thirst/taste sensation)
• Uncontrolled diabetes mellitus (electrolyte abnormalities, polyuria)
• Critically ill and unfed for >7 days
• Inflammatory bowel disease, chronic pancreatitis, short bowel syndrome
• Cystic fibrosis
• Long-term antacid use (phosphorus levels are often low 2/2 magnesium and aluminum salts in the medications)
• Long term diuretic use (potassium-wasting) such as with CHF
• Patients who are vomiting frequently
Patients with poor blood levels at baseline (K/Mg/P) will be at risk of intracellular shifts and thus lower blood lab values. Patients with SBD have reduced absorptive capacity, for example, and are at risk for refeeding syndrome.
• When a patient is experiencing hyperkalemia (K+ > 5.1 mmol/L), there are a number of treatments a Team may utilize
• 50% Dextrose ampule + Insulin
• Calcium Gluconate
• Kayexalate or Lokelma
• Why would we use these medications? (insulin will stimulate intracellular K+ shift, Lokelma and Kayexalate bind potassium)
Giving dextrose and insulin mimics refeeding. So, you are pulling potassium out of the blood and giving it to the cells.
Giving dextrose and insulin mimics refeeding. So, you are pulling potassium out of the blood and giving it to the cells. With renal patients who are often in a hyperkalemic state, kayexalate and lokelma will stop potassium absorption in GI tract. When someone’s potassium hits the ceiling, arrhythmia can occur. Calcium is given to offset that. If a pt is hyperkalemic and EKG changes are seen, patient is given 2g of calcium. Calcium gluconate is the preferred IV administration for hypocalcemia (Severe symptomatic hypocalcemia should be corrected promptly with IV administration of calcium gluconate over 10 minutes to control symptoms. Calcium gluconate is the preferred salt for peripheral venous administration to avoid extravasation—leakage of liquid into surrounding tissue.)
Specialized labs: Liver function tests give you enzymes (alanine aminotransferase and aspartate aminotransferase, ALT and AST) and you are also given bilirubin as s measure of liver function, as bilirubin is a waste product of heme metabolism. When liver is not functioning well, bilirubin won't be cleared well. At that point, liver is also not good at clearing minerals such as copper and manganese.
Liver function tests give you enzymes (alanine aminotransferase and aspartate aminotransferase, ALT and AST) and you are also given bilirubin as s measure of liver function, as bilirubin is a waste product of heme metabolism. When liver is not functioning well, bilirubin won't be cleared well. At that point, liver is also not good at clearing minerals such as copper and manganese.
When T. bili is >5 mg/dL, give PO multivitamin without minerals, or remove copper and manganese from your TPN (total parenteral nutrition) solution
If patient is eating, give them a multivitamin without minerals. If patient is on TPN, remove copper and manganese, as toxicity of these can risk brain damage.
Blood and iron studies: Hemoglobin is the last thing to change. Look at ferritin as an earlier sign. Hematocrit can respond to anemia, but also to an overflow of other blood cells. Professor Trussler works with blood in the heme oncology setting. White blood cells in certain type of malignancies (e.g. leukemia) are elevated. Blood smear can count white blood cells and immature white blood cells (blasts). High blasts signals that something is wrong in bone marrow and they’re pumping a lot of immature white blood cells out. Also, immature blasts are a measure of whether someone’s chemotherapy has been effective. Treatment decisions can be made on this.
Absolute number of neutrophils can be used to determine treatment decisions. Low neutrophil count can be used as a guideline for a neutropenic (low bacteria) diet.
A1C: 3-month average blood glucose. When someone is acutely ill, you can see high glucose in the blood, but this is not diabetes, it’s “stress hyperglycemia” (due to injury). But if this is prolonged, an A1C can help you see if they have undiagnosed prediabetes. A1C is useful for newly diagnosed diabetic patients.
Lipase: You shouldn't be seeing a lot of lipase in the bloodstream, as this indicates pancreatic damage (e.g. pancreatitis)
Vitamin and mineral labs get expensive, so you don't want to be checking EVERYTHING for every situation. There are some vitamins and minerals where a serum lab isn't going to be helpful. E.g. pyridoxine (B6), Per the American Society of Parenteral and Enteral Nutrition (A.S.P.E.N.), you need serum B6, 24-urinary B6, erythrocyte AST, and erythrocyte ALT to assess sufficiency of B6.
Common vitamin labs:
· Someone who is having trouble absorbing fat will be at risk for vitamin A deficiency. Vitamin A is key to skin integrity and building (a pressure injury/injuries not healing well may indicate vitamin A deficiency), with substance use disorder deficiency comes up because you’re generating a lot of free radical damage from substance use disorders and the vitamin A is getting used up for that. Vitamin A is protein bound (RBP), so you can look at C-reactive protein in combination with this, because vitamin A may look low when it's not (falsely low result).
· B12 is worth looking at, esp. for vegans, vegetarians, elderly, heavy alcohol or substance users, and patients with IBD.
· Vitamin C builds collagen matrix for skin, thus wounds could cause a vitamin C deficiency in wound patients. Dialysis causes water loss, so you can lose vitamin C. COVID-19 may cause a vitamin C deficiency (the antioxidant vitamin is getting used up).
· Check vitamin D, after it's activated by the kidneys a second time, that active form doesn't last very long, so it may not give you a good result. Vitamin D labs are good to check for elderly patients who don’t synthesize enough vitamin D, and for kidney injury patients because their kidneys aren’t activating as much vitamin D. Checking vitamin D for oncology patients is also great, because they may have some complications in certain cancer treatments. COVID-19 appears to be affecting vitamin D levels.
· Vitamin E is good to check in a patient who is malabsorbing fat. If you think someone is malabsorbing, the team can do more work up.
Less common vitamin labs:
If the vitamin is water soluble, there’s less risk of toxicity, so you can give it prophylactically. For example, folate costs about $1, so it can be given for 3 days prophylactically.
B1 (thiamin) is given prophylactically if you think the patient is deficient. At Brigham and Women’s, if you anticipate that someone might refeed, you give them thiamin for the first few days that they’re getting nutrition support to anticipate that shift with potassium.
Professor T doesn’t usually check vitamin K often, because gut microbiota make vitamin K. Prothrombin (PT-INR, a marker of blood clotting) is a better indicator of vitamin K sufficiency because the clotting factors in your blood need vitamin K to work. If you were truly functionally deficient, you would have trouble clotting.
Common mineral labs
Both copper and ceruloplasmin must be low in order to diagnose a true copper deficiency. Bariatric patients tend to be low, esp. in Roux-en-Y gastric bypass patients, as the surgery is bypassing some of the areas where copper is absorbed. Wouldn't normally suspect a copper deficiency unless there's some sort of malabsorptive process occurring.
Zinc deficiency is caused by (and can also cause) diarrhea. If you have someone with diarrhea that isn’t resolving, it could be due to zinc deficiency, and also zinc could be causing the diarrhea. Zinc is lower in stressed state. If a patient is borderline deficient and their CRP is very high, you may want to hold off on repleting zinc, and then check zinc levels again.
Selenium, like zinc, decreases when someone has diarrhea, but can also cause diarrhea as a side effect of deficiency. Selenium will be low in substance use disorder patients, as it participates in antioxidant functioning (where antioxidants get used up).
Less common mineral labs:
Manganese: No good lab test to measure for this. If worried patient is getting too much, try to just remove it. E.g. taking manganese out of total parenteral nutrition, or giving a supplement that doesn’t have manganese. Manganese toxicity can cause brain damage
Chromium: No real lab measure for chromium, either, but people on long term TPN might develop this deficiency. Sometimes chromium is given prophylactically. People who are diabetic can be low in chromium, but it is difficult to figure out because you can’t check this mineral.
Specialty Lab
• Fecal Calprotectin
• Marker of inflammatory bowel disease
• Protein released by immune cells (neutrophils) at sites of inflammation in the GI tract, which is then excreted in the stool
• Low level (10-50 mcg/mg): likely IBS or viral infection
• Moderate level (>50 mcg/mg): potential IBD flare or worsening inflammatory condition such as parasitic infection
#anion gap#alkalosis#acidosis#lipase#A1C#UUN#labs#specialized labs#clinical#BUN#creatinine#dietetics#Medical Nutrition Therapy
2 notes
·
View notes
Text
gastrointestinal system studies
case study – 43 yo female, dyspepsia and fatigue
» physical examination
abdominal pain
pale skin, looks ill
» laboratory testing and assays
macrocytic anemia (large red blood cells, few in number) | possibly arrest in early stages of differentiation in bone marrow
(microcytic anemia is a small RBC size, having to do with iron deficiency)
low Vitamin B12 levels | B12 is important for RBC differentiation and development
elevated serum gastrin levels (marker of abnormal GI activity)
» endoscopy / colonoscopy
run a probe with attached light down esophagus (can also grab biopsy samples) | colonoscopy is from rectum
healthy stomach has folds with glands in it
patient’s stomach has atrophic folds - it’s smooth, regressed folds
presence of cyst / tumor / polyp
pH = 6, low gastric acid aka hypochlorhydria
» biopsy procedure
cardia → body → antrum of stomach, which all have different linings
general: stomach lumen → lumen lining cells → (area-specific linings)
(body = pink and mitochondria-heavy, mutinous and oxyntic glands with gastric acid secretions, as well as ECL) specifically pink, mitochondria, and presence of oxyntic glands in histology
(antrum = mutinous glands and G-neuroendocrine hormonal cells, secreting gastrin)
G-cell gastrin from antrum binds ECL → ECL secretes histamine → histamine stimulates acid from oxyntic glands
patient biopsy from antrum has glands spaced far apart, and spatial extension causes stomach folds to pull out and become smooth
patient biopsy from antrum has lymphocytes (increased purple nucleus stains) – chronic gastritis | acute is neutrophils
patient’s body has “antralized” → metaplasia, or a change in tissue to look like another organ’s tissue after injury and bodily adaptations
verdict from biopsy: atrophic metaplasia chronic lymphatic gastritis
» assessing the cyst / tumor mass
carcinoid - neuroendocrine cells form malignant tumor
cancer cells have bypassed stroma
» summary
pale skin = anemic = bleeding or low RBC count
fold atrophy = chronic inflammation stretches lamina of stomach = high pH because glands ≠ making acid
biopsy = metaplastic, atrophic, lymphocyte proliferations, tumor mass
» AMAG diagnosis: autoimmune metaplastic atrophic gastritis
auto-antibodies are made against oxyntic gland’s parietal cells
antibodies recruit lymphocytes, which begin destroying oxyntic glands
body becomes “antralized” because pink oxyntic glands are destroyed
stomach grows back cells, but they are mucin-secreting cells and pH stays low because gastrin ≠ responded to
gastrin over-secretion to compensate → gastrin becomes a growth factor and NE cells in antrum begin to proliferate
NE cells acquire some cancerous mutation → and the tumor forms
case study – 40 yo female, episodic abdominal pain, jaundice, fever
» physical examination
colicky upper right quadrant – pain occurs intermittently
especially after a meal or when contact is made to area
painful jaundice
» laboratory assays
WBC, bilirubin, amylase and lipase build-up | possible pancreatic injury
alkaline phosphatase – made by cells in bile ducts
» imaging – abdominal ultrasound and ERCP
ultrasound: gallbladder is enlarged, contains gallstones
ERCP: analyze tiny bile and pancreatic ducts, as well as gallbladder, via injection of dye through esophageal line to duodenum
imaging of dye from bile, cystic, and pancreatic ducts and can see all three organs
filling defect - dye cannot get to pancreatic duct or gallbladder
slow transit - dye takes a long time to get to liver from bile ducts
bile duct injury, pancreatic injury, gallbladder blockage
bile stops moving and grows infected → fever and inflammation, WBC up
» verdict from the ERCP: gallstone pancreatitis
gallbladder stones exit the gallbladder alongside bile after a fatty meal, and stone blocks pancreatic duct
another stone blocks the cystic duct and causes pain
stones - commonly cholesterol, or other types and compositions
digestive enzymes spill out into pancreas and auto-digest it causing more pain
can inject stone-dissolving substances, or elective cholecystectomy (gallbladder removal, voluntary) if needed
any GI surgical procedure → adhesin tissue builds up and pins parts of bowel, blocks it → need to re-operate when things build up and infection occurs
case study – 45 yo male, rectal bleeding
» physical examination:
medical history: HIV+
otherwise normal
» laboratory testing and assays
undetectable HIV viral load (i.e., taking anti-retroviral medications well)
normal T-cell counts (visit is not due to HIV flare-up)
RPR+ (IgG) against syphilis | IgM is recent infection, IgG is long-time infection, high sensitivity
rectal bleeding could be due to gonorrhea, HPV
» colonoscopy findings
flat, barely raised polyp on right, sessile → removed for biopsy
glands of the area are crowded, overgrown and hypertrophic
lumens are irregular, branched and serrated instead of round in healthy patients
diagnosis: sessile serrated adenoma, pre-cancerous so removed
large, raised polyp on left, pedunculated → removed
overgrown, hypertrophic lining - cancerous epithelial cells
pre-cancerous polyp, mushroom-like → has not yet invaded stroma
diagnosis: tubular adenoma, where the growth looks like a tube
upper colon is spotted with white plaques (ulcers - fibrin and inflammatory cells), and inflamed, eroded → biopsy
» rectal biopsy to find source of bleeding
abundance of inflammatory cells, lamina expanded as a result of overcrowding
neutrophils from acute inflammation; plasma cells from chronic inflammation
acute inflammation turned chronic, essentially → silver staining reveals syphilis organisms in rectum
» verdict: syphilis in rectum causing rectal bleeding
4 notes
·
View notes
Text
Intussusception is the most common cause of intestinal obstruction in children between 3 months and 6 years of age.
Symptoms of amebic dysentery (or colitis) to some extent may mimic symptoms of ulcerative colitis or Crohn's disease. Usually, the illness lasts about 2 weeks, but it can recur without treatment. The general symptoms include abdominal cramps, diarrhea, passage of 3 to 8 semi-formed stools per day, passage of soft stools with mucus and occasional blood, fatigue, excessive flatulence, rectal pain during bowel movement (tenesmus), and unintentional weight loss. Severe symptoms include abdominal tenderness, bloody stools, and passage of liquid stools with streaks of blood, passage of 10 to 20 stools per day, fever, and vomiting. Amebic colitis is the result of invasive infection of the colonic mucosa by Entamoeba histolytica (E. histolytica).
Zollinger-Ellison Syndrome (ZES) presents with marked gastric acid secretion, ulcer disease of the upper GI tract including the stomach and duodenum, and non-beta islet cell tumors of the pancreas, but it does not normally affect the Islets of Langerhans. Zollinger-Ellison is commonly associated with tumors of delta cells of the pancreas. However, the tumors are also commonly located in other areas such as the duodenum and abdominal lymph nodes. Note that hyper-acidity in the duodenum inactivates pancreatic enzymes and results in diarrhea. Differential diagnosis of ZES includes gastroesophageal reflux disease, MEN1 (Wermer syndrome), peptic ulcer disease, helicobacter pylori infection, gastric outlet obstruction, pernicious anemia, achlorhydria, and pancreatic cancer. Note that hyalinization of the Islets of Langerhans is associated with Diabetes mellitus.
I didn't know that MEN1 is also called "Wermer syndrome." Now I know.
Hepatoblastoma is the most common malignant primary liver tumor in children. I only got that right because I remember Dr. Plummer saying that blast tumors are associated with kids.
Most esophageal varices are located in the lower third of the esophagus.
Apparently, phytate exerts the most profound inhibitory effects on the absorption of zinc (Zn) from the lumen of the small intestine. Never heard of phytate. When I googled it, this is what came up:
Phytate, or phytic acid, is a naturally occurring compound found in all plant foods like beans, grains, nuts, and seeds. In the past, there were concerns that foods high in phytates might reduce the absorption of minerals.
Zinc deficiency has been found in some populations that consume large quantities of unrefined foods. The phytate in these foods may decrease zinc absorption. Note that picolinic acid is the body's prime natural chelator. It is the most efficient chelator for minerals such as chromium, zinc, manganese, copper, iron, and perhaps molybdenum. Zinc picolinate is actually readily absorbable.
Never heard of picolinic acid either.
The most common bacteria linked to ascending cholangitis are gram-negative enteric bacteria, in particular Escherichia coli, followed by Klebsiella and Enterobacter. Treatment consists of antibacterial therapy and removal of gallstones. Note that the presence of antibodies against hepatitis B surface antigen will rule out a hepatitis B infection, and interferon-alfa or ribavirin administration is mostly indicated for hepatitis C treatment.
Unresolved PUD can cause perforations. Perforated ulcers are the most commonly encountered dreaded consequence. Note that common symptoms of perforation include: (1) sudden development of sharp abdominal pain; (2) rigidity and tenderness of the abdomen; (3) symptoms of shock (fainting, hypotension, excessive sweating, and confusion); and (4) bloody vomitus or tarry stool. Also note that demonstration of “free air” on radiological examination is highly indicative of a perforated viscus organ. An erect chest x-ray or an upright abdominal x-ray is by far the best initial diagnostic screening test.
GERD and Barrett’s esophagus are related to inappropriate relaxation of the lower esophageal sphincter.
Hiatal hernia predisposes to GERD and may causes herniation of the stomach into the thoracic cavity.
Crigler-Najjar Syndrome patients are unable to conjugate bilirubin. Unconjugated hyperbilirubinemia quite often causes death due to kernicterus.
The body and tail of the pancreas are situated posterior to the stomach. The quadrate lobe of the liver and gall bladder are both anterior to the stomach. The right kidney is situated posterior to the duodenum and small intestine. The right crus of the diaphragm is posterior to the liver.
An anal fissure is a small split or tear in the mucosa lining the anus. Anal fissures are extremely common in young infants, but they may occur at any age. Studies suggest that 80% of infants will have had an anal fissure by the end of their first year. The rate of anal fissures decreases rapidly with age, and fissures are much less common among school-aged children. I didn't know that they were common in infants.
Cryptosporidium = acid-fast protozoan that produces voluminous watery diarrhea without blood or mucus. It is very common in AIDS patients. Entamoeba histolytica (causes amoebic colitis), shigella, enteroinvasive E. coli, campylobacter, and cryptosporidium cause bloody diarrhea.
This question was about a woman who clearly had H. pylori infection and they asked what kind of cancer she had. I chose lymphoma but then switched to adenocarcinoma, finally changing back to lymphoma and got it wrong. I thought H. pylori causes MALToma, which is a type of lymphoma. Yes, the gastric cells are secretory cells, so if they became cancerous, it would be cancer of glandular cells (the "adeno" in "adenoma" = glandular cells), but H. pylori causes MALToma. So I don't think lymphoma is necessarily the wrong answer. I was stuck between lymphoma (my initial answer because the pt clearly has a history of H. pylori infection) and adenocarcinoma. The explanation:
Helicobacter pylori infection is associated with adenocarcinoma (accounts for almost 90% of stomach cancers). Note that adenoacanthoma is an adenocarcinoma in which some of the cells exhibit squamous differentiation.
The vagus nerve passes inferiorly from a plexus associated with the hilum of the lung. Injury to the vagus nerve--> decreased gastric motility. In the mediastinum, the vagus nerves pass immediately posterior to the roots of the lungs, while the phrenic nerves pass immediately anterior to them.
Dietary long chain fatty acids (more than 12C) are transported from the intestine to the adipose tissue in the form of chylomicron triglycerides. I remembered that from learning about cholesterol. Pretty sure they get transported across the intestines. I really have to review cholesterol. Ugh.
In a question, the pt had polyuria, pruritic skin rashes that appeared in one place and then disappear and showed up elsewhere, erythematous plaques and vesicles on her thigh, anemia, hyperglycemia, and increased ACTH. I wasn't sure what it was.
The patient most likely has necrolytic migratory erythema (NME) due to glucagonoma.
Glucagonoma is a rare pancreatic alpha-cell neoplasm that is mostly seen in pre-and post-menopausal woman. Patients present with marked increase in serum glucagon level, hyperglycemia, polydipsia, and polyuria. During the early stages, the condition may mimic symptoms of mild diabetes mellitus. A characteristic skin finding in these patients is necrolytic migratory erythema (NME). The majority of these tumors are malignant, and metastasis to the liver is not uncommon. Note that glucagonoma is often associated with MEN I, and serology of the patients often show increased plasma ACTH, MSH, serotonin, and epinephrine. Treatment includes insulin administration and surgical removal of the tumors.
The mechanism of NME is not well-known but it is postulated to be due to (1) direct damage of glucagon to skin that causes necrosis; (2) serious metabolic deficiencies that cause deficiency of epidermal proteins; and (3) autoimmune conditions that damage the skin. Glucagonoma is by far the most common cause of NME. Deficiency of zinc, fatty acid, and amino acids, liver diseases, hypoalbuminemia, inflammatory bowel disease, celiac sprue, and malnutrition conditions may also be associated with NME. Given that pancreatic alpha-cell neoplasm is by far the most common cause of NME, the non-pancreatic causes of NME (e.g. liver disease or zinc deficiency) are collectively known as pseudoglucagonoma.
#Intussusception#amebic colitis#wermer#wermer syndrome#hepatoblastoma#esophageal varices#zinc#phytate#picolinic acid#zinc deficiency#ascending cholangitis#PUD#Crigler Najjar Syndrome#cryptosporidium#diarrhea#adenocanthoma#adenoacanthoma#anatomy#NME#glucagonoma
2 notes
·
View notes
Text
Best gastroenterologist in south delhi
Best gastroenterologist in south delhi
https://g.page/r/CdEGy7wshojYEAE
A gastroenterologist is a specialized doctor who deals in diagnosing and treating GI diseases in both men and women. He/she also performs endoscopic procedures by using instruments that facilitate better viewing of the GI Tract and make an accurate diagnosis.
Best gastroenterologist in south delhi
However, the surgeries are performed by those who are known as surgical gastroenterologists. The gastrointestinal system is responsible for movement and digestion of food within the gut, assimilation of nutrients and removal of waste products.
Best gastroenterologist in south delhi
The gastrointestinal tract comprises of the following organs:
Best gastroenterologist in south delhi
Mouth (salivary glands, tongue)
Pharynx
Best gastroenterologist in south delhi
Esophagus
Stomach
Small intestine
Large intestine
Liver
Gallbladder
Pancreas
Rectum
Anus
Best gastroenterologist in south delhi
However, any illness related to the mouth is treated by a dentist or oral surgeon, while any illness related to the rectum or anus is treated by a proctologist.
Best gastroenterologist in south delhi
What conditions do gastroenterologists treat?
Best gastroenterologist in south delhi
Some of the most common disorders treated by a gastroenterologist are listed below:
Best gastroenterologist in south delhi
Acid reflux - This is the most common condition which is manifested as a burning sensation in the upper part of the stomach. The burning sensation is also known as heartburn. This occurs due to regurgitation of stomach acid into the food pipe. It can be treated by making changes in food.
Best gastroenterologist in south delhi
GERD or Gastroesophageal reflux disease - This happens when the acid reflux becomes more frequent and the symptoms get worse. This affects the lower esophageal sphincter, a ring which is present between the esophagus and stomach.
Best gastroenterologist in south delhi
Hepatitis C - This is a liver disease caused by Hepatitis C virus. This virus can cause both acute and chronic hepatitis. The symptoms may vary from mild to severe and may last for a few weeks to a lifelong illness.
Best gastroenterologist in south delhi
Jaundice - It is a yellow discoloration of the skin, mucous membranes, white of the eyes due to increased levels of bilirubin in the blood. Jaundice is a symptom of some underlying chronic disorder. Bilirubin is a by-product of the natural breakdown and destruction of the red blood cells within the body.
Best gastroenterologist in south delhi
Hemorrhoids - Commonly known as piles, these refer to the swollen veins in the anus and lower rectum, similar to varicose veins. These hemorrhoids can develop inside the rectum or under the skin around the anus. Those occurring inside the rectum are called internal hemorrhoids and those under the skin are called external hemorrhoids.
Best gastroenterologist in south delhi
Pancreatitis - This is a disease in which the pancreas is inflamed. This occurs when the digestive enzymes get activated before being released into the small intestine and attack the pancreas. Pancreatitis may be acute or chronic. The acute pancreatitis is sudden inflammation taking place for a short time while chronic pancreatitis occurs a long-lasting inflammation of the pancreas.
Best gastroenterologist in south delhi
Best gastroenterologist in south delhi
Colonoscopy - a procedure done to detect colon polyps or colon cancer
Best gastroenterologist in south delhi
Endoscopic ultrasound - a procedure used to examine the upper and lower GI tract as well as other internal organs.
Best gastroenterologist in south delhi
Liver biopsy - this is done to access inflammation and fibrosis
Sigmoidoscopy - to evaluate blood loss or pain during a bowel movement.
Best gastroenterologist in south delhi
Capsule endoscopy - to examine the small intestine
Endoscopic retrograde cholangiopancreatography - to look for the gallstones tumors or any scar in the bile duct.
Best gastroenterologist in south delhi
Double balloon enteroscopy - this is also done to examine the small intestine.
Best gastroenterologist in south delhi
https://g.page/r/CdEGy7wshojYEAE
0 notes
Text
Recognizing the Symptoms and Signs of Pancreatic Cancer
Introduction:
Pancreatic cancer is a serious and often aggressive form of cancer that affects the pancreas, an organ responsible for producing enzymes that aid in digestion and regulating blood sugar levels. This type of cancer is known for its elusive nature, as it often remains undetected until it reaches an advanced stage. Recognizing the symptoms and signs of pancreatic cancer is crucial for early diagnosis and improving treatment outcomes. In this article, we will explore the common symptoms associated with pancreatic cancer to increase awareness and promote early detection.
Abdominal Pain:
Persistent and unexplained abdominal pain, often radiating to the back, is one of the most common symptoms of pancreatic cancer. The pain may worsen after eating or lying down, and individuals may experience a dull ache or sharp discomfort.
Jaundice:
Pancreatic cancer can obstruct the bile duct, leading to a buildup of bilirubin in the body. This can cause jaundice, characterized by yellowing of the skin and eyes, dark urine, pale stools, and itching. Jaundice typically occurs when the cancer affects the head of the pancreas.
Unintentional Weight Loss:
Sudden and unexplained weight loss is frequently observed in individuals with pancreatic cancer. This weight loss can occur even if the person maintains their regular diet. It is often accompanied by loss of appetite, weakness, and fatigue.
Digestive Problems:
Pancreatic cancer can interfere with the normal functioning of the digestive system. Individuals may experience changes in bowel movements, such as diarrhea or pale, oily, and foul-smelling stools. This occurs due to the impaired production of pancreatic enzymes responsible for breaking down fats.
New-Onset Diabetes:
In some cases, pancreatic cancer can cause new-onset diabetes, especially when it affects the body or tail of the pancreas. The development of diabetes without an obvious cause, especially in older adults, may be a warning sign of pancreatic cancer.
Nausea and Vomiting:
As pancreatic cancer progresses, it can lead to gastrointestinal disturbances such as nausea and vomiting. These symptoms are often experienced in conjunction with other signs like abdominal pain and weight loss.
Fatigue and Weakness:
Unexplained fatigue, weakness, and a general feeling of malaise are common in individuals with pancreatic cancer. Cancer-related fatigue can significantly impact a person’s quality of life and may not improve with rest or sleep.
Changes in Urination:
Pancreatic cancer can affect the kidneys and cause changes in urination patterns. This can manifest as frequent urination, dark-colored urine, or blood in the urine. Such symptoms should be promptly investigated by a healthcare professional.
Conclusion:
Early detection plays a vital role in the successful treatment of pancreatic cancer. While these symptoms and signs can be associated with various other conditions, it is important not to ignore their persistence or worsening. If you or someone you know experiences any of these symptoms, especially in combination, it is advisable to consult a healthcare professional for a thorough evaluation. Timely diagnosis and intervention can potentially improve treatment options and increase the chances of successful outcomes for individuals with pancreatic cancer.
0 notes
Text
Timely Vs. Delayed Laparoscopic Cholecystectomy: Know The Benefits
Gallstones are solid particles that form in the gallbladder as a result of the liver's overproduction of cholesterol and bilirubin. Previously, gallstones were treated with open surgical procedures, which required patients to stay in the hospital longer and recuperate more slowly. Laparoscopic Cholecystectomy, on the other hand, is a minimally invasive option for the treatment of gallstones. Single or more gallstones can now be removed in a few of hours with only a few tiny incisions.
Gallstones Symptoms
Gallstones do not have any active symptoms, and an individual may initially experience little or no discomfort. However, if left untreated for an extended length of time, gallstones can cause cholecystitis (gallbladder inflammation), jaundice, strong periodic pain in the belly, and other consequences. Acute abdominal pain, high fever, and skin and eye yellowing are early indicators of gallstones and should not be disregarded.
Timely Vs. Delayed Laparoscopic Cholecystectomy
The most common treatment for symptomatic gallstones is laparoscopic cholecystectomy. It is affordable, safe, and promises a better life for patients after treatment. A surgeon will only recommend ELC (early laparoscopic cholecystectomy) if the inflammation does not obstruct the surgeon's view during operation. Laparoscopic cholecystectomy is usually performed during the first few days of a gallstone's diagnosis. The time points for treating acute cholecystitis, however, vary depending on the level of inflammation. Even after a diagnosis, therapy may be postponed to allow the inflammation or cholecystitis to resolve. However, this delay might result in a number of issues involving the liver and gallbladder. Let's have a look at some of the primary benefits of early LC over delayed LC.
1. Minimum Complications:
Early LC ensures that gallstones do not create other serious liver problems. In the worst-case scenario, gallstones cause gallbladder cancer in patients. Early LC has greatly reduced the death rate from acute cholecystitis or acute pancreatitis.
2. No GallBladder Attack:
With early LC, patients no longer need to suffer from prolonged excruciating abdominal pain. If LC is delayed, patients will have to bear with periodic intense pain, eventually leading to fever. A gallbladder attack can last for a few hours and can come anytime, anywhere.
3. Cost-Effective:
Early LC is also cost-effective.Gallstones can be removed in a matter of hours, and patients can be discharged from the hospital the same day. In comparison, a delayed LC requires more visits, routine diagnosis, a longer hospital stay, and more recovery time. Early LC, on the other hand, takes very little time and is incredibly cost-effective.
When To See A Doctor?
Gallstone attacks can linger for several hours, and the initial incidence of unwelcome and acute stomach/abdominal discomfort should be treated by a doctor. Because of the numerous health risks linked with gallstones, any pain in the right shoulder, upper, or central belly should not be overlooked. The doctor will conduct some regular tests, such as a CT scan and blood tests, to confirm the presence of gallstones.
Furthermore, pregnant women, people who are obese, those who take cholesterol-lowering drugs, and persons over the age of 60 are at a higher risk of developing gallstones. These people should be on the lookout for symptoms such as rapid fever, elevated heart rate, nausea, exhaustion, or confusion, and should see a doctor for a gallstone diagnosis.
The abdominal region is one of the most important in our bodies. It houses some of the most critical organs that impact our overall health. We provide the most advanced Laparoscopic surgery for gallbladders, appendices, and colons at Piyush Hospital. Dr. Rohan Patil is the most skilled laparoscopic surgeon in Jalgaon. Hundreds of people throughout town have benefited from his knowledge.
Dr. Rohan Patil is a reputed Advanced Laparoscopy, Cancer & General Surgeon in Jalgaon. He is the Founder of Piyush Hospital which is a renowned Surgical Super Speciality Hospital in Jalgaon. It provides the most comprehensive and integrated Surgical Treatment under one roof. He has a special interest in Gastrointestinal Surgery, Gastrointestinal Endoscopy, Laparoscopy, Laser Proctology & General Surgery. He has gain wide experience during his training at the prestigious Seth G.S. Medical College & K.E.M. Hospital, Mumbai. He has presented his research work at many National & International Conferences in India & Abroad. Many publications are there to his credit.
0 notes
Text
Tumour Markers
Chemical biomarkers that can be elevated by the presence of one or more types of cancer, produced directly by the tumour or by non-tumour cells as a response to the presence of a tumour. Really great tests as can use just blood/urine, but aren’t the most specific and false positives do occur.

Alpha-fetoprotein (AFP)
Glycoprotein synthesised in yolk sac, the foetal liver, and gut - will be high in a foetus and during pregnancy.
<10 ng/mL is normal for adults
>500 ng/mL could indicate liver tumour
Normally:
Produced primarily by the liver in a developing foetus
Thought to be a foetal form of albumin
suppress lymphocyte activation and antibody production in adults (immune suppressant)
Binds bilirubin, fatty acids, hormones and metals
In cancer:
Detects hepatocarcinoma (liver cancer)
Risk factors: haemochromotosis, hep B, alcoholism - cell repair and growth from this damage leads to cancers
Present in non-pathogenic liver proliferation, including the growth and repair response to the above. This makes it hard to differentiate - AFP levels can be raised in patients with liver cancer risk factors due to the factors themselves, not a cancer. Not very diagnostic!! Used in combination with other tests/factors. Sensitivity and specificity ~75%
Other hepatocellular carcinoma markers:
γGT (γ-glutamyltransferase) - biliary damage
AFP mRNA (not always together with AFP! Might not be activated)
γGT mRNA elevated
Raised cytokines (IL-8, VEGF, TGF-B1)
ALT and AST elevated - liver disease
Carcinoembryonic antigen (CEA)
a set of highly related glycoproteins involved in cell adhesion. Potentially associated with innate immune system.
Normally:
produced in gastrointestinal tissue during foetal development
production stops before birth
present only at very low levels in the blood of healthy adults.
Cancer:
Elevated in almost all patients with colorectal cancer
Can monitor recurrence of cancer (when compared to previous test results for that patient) with a sensitivity of 80% and specificity of 70%
levels may also be raised in gastric, pancreatic, lung, breast and medullary thyroid carcinomas
also some non-neoplastic (not cancer) conditions like ulcerative colitis, liver disease, pancreatitis, COPD, Crohn's disease, hypothyroidism - again, high risk groups for colorectal cancer - not a diagnostic test
Levels elevated in smokers.
Carbohydrate antigens (CA)
Including:
CA 19-9 - Pancreas
CA 15-3 Breast
CA 50 - Colorectal
CA 125 - ovarian
Levels rise only in disease states and particularly cancer, but will not rise in all patients.
Part 2 coming soon!
#medicine#biomed#medblr#studyblr#notes#biomedicine#biomedical science#med#science#biology#human biology#medical biology#2#3#oncology#biochemistry#tumours#tumor markers#tumour markers#med school#Physiology
271 notes
·
View notes
Text
Takayasu's arteritis has a strong association with ulcerative colitis. I didn’t know that.
Perforated colon carcinoma mimics the symptoms of diverticulitis on a CT scan. After treatment of diverticulitis, a follow-up endoscopy (i.e. colonoscopy) or barium enema are both commonly-utilized procedures for ruling out the presence of colon cancer.
Note that the test item uses the word “endoscopy” in a broad and generic sense. “Endoscopy” literally means “to look inside the body”. Upper GI endoscopy and colonoscopy are two specific and descriptive usages of the term “endoscopy”. A few other descriptive endoscopic procedures include, otoscopy, enteroscopy (small intestine), sigmoidoscopy, and bronchoscopy.
Omphalocele is believed to be due to an underlying genetic disorder and it is more common in babies with chromosomal aberrations such as Edward's syndrome (Trisomy 18) or Patau Syndrome (Trisomy 13). The sac is formed from an out-pouching of the peritoneum that protrudes in the midline, through the umbilicus (navel). The viscera are wrapped up internally by the peritoneum and externally by the amnion. Herniated structures within the omphalocele are the intestines and/or liver. The omphalocele can be mild, with only a small loop of intestines present outside the abdomen, or severe, containing most of the abdominal organs. Differential diagnosis of omphalocele includes gastroschisis, which is always located to the right of the umbilical cord and is often smaller in size (less than 4 cm). In contrast to omphalocele, gastroschisis does not have an overlying sac (only the small bowel is exposed). Note that omphalocele does not have an umbilical ring, whereas gastroschisis has an umbilical ring.
Oral rehydration therapy (ORT) is a simple treatment for dehydration associated with diarrhea, particularly gastroenteritis such as that caused by cholera or rotavirus. ORT consists of oral solutions of salts and sugars. Fluid from the body is normally pumped into the intestinal lumen during digestion. Since this fluid is typically isosmotic with blood, it contains a high concentration of sodium. A healthy individual will secrete 20-30 grams of sodium per day via intestinal secretions. Nearly all of this is reabsorbed by the intestine, helping to maintain constant sodium levels in the body. Because there is so much sodium secreted by the intestine, without intervention, heavy continuous diarrhea can be a very dangerous and potentially life-threatening condition within hours. This is because liquid secreted into the intestinal lumen during diarrhea passes through the gut so quickly that very little sodium is reabsorbed, leading to very low sodium levels in the body (severe hyponatremia). Sodium absorption via the intestine occurs in two stages. The first is at the outermost cells (intestinal epithelial cells) at the surface of the intestinal lumen. Sodium passes into these outermost cells by co-transport facilitated diffusion (symport diffusion). From there, sodium is pumped out of the cells (basal side) and into the extracellular space by active transport via the sodium-potassium pump. The co-transport of sodium into the epithelial cells requires glucose or galactose.
Presence of surface antigen (HbsAg) and IgM antibodies to core antigen (Anti-HbcAg) together with the symptoms of hepatitis (right upper quadrant pain) and hyperbilirubinemia are indicative of acute hepatitis B infection.
Presence of Anti-HAV (IgG) is indicative of old exposure to hepatitis A antigen or old infection. The serology of most people all over the world shows positive anti-HAV (IgG) levels. [I always recall that IgG is the antibody that means it’s gone; you’re immune because you already went through the infection.]
Note that Councilman, also known as Councilman hyaline bodies or apoptotic bodies, are acidophilic (eosinophilic) globules of cells that represent dying hepatocytes, and they are often surrounded by normal parenchyma. Liver biopsy of acute viral hepatitis typically shows panlobular lymphocytic infiltrates with ballooning hepatocytes (indicative of hepatocyte necrosis and hepatocyte apoptosis).
The mechanism of apoptotic hepatocytes is postulated to be due to the presence of HBcAg and HBeAg that induce both B and T cell responses. More specifically, damage to the hepatocyte can result from antibody-dependent, natural killer (NK) and cytotoxic T lymphocytic effects on the infected hepatocytes.
Note that only conjugated bilirubin appears in the urine and causes darkening of the urine. In early phases of acute hepatitis, the liver still retains its ability to conjugate the bile. However, an early event in acute hepatitis is widespread constriction of the biliary canaliculi. This causes the back-up of already-conjugated bile into the bloodstream, and their appearance in the urine. With chronicity of hepatitis, the liver can no longer conjugate bile, and as a result patients present with indirect hyperbilirubinemia and light-colored urine, because insoluble unconjugated bilirubin is carried by albumin and cannot be filtered.
So in acute Hep B infection, hepatocytes are destroyed by cytotoxic T cells.
A Meckel's diverticulum is an out-pouching (sack) that protrudes from the small intestine near the junction of the small intestine and the colon. It is present from birth and occurs in approximately 2% of the population. Some Meckel's diverticula can secrete acid, like the stomach, and the acid can cause ulcerations in the inner lining of the diverticulum or the tissues of the small intestine adjacent to the diverticulum. These ulcers can bleed, and the bleeding from a Meckel's diverticulum is the most common cause of gastrointestinal bleeding in children and young adults. Bleeding from a Meckel's diverticulum is painless but can be brisk and can cause bright red, dark-red, or maroon stools. A technetium-99m (99mTc) pertechnetate scan is the investigation of choice to diagnose Meckel's diverticula, and detects gastric mucosa. Since approximately 50% of symptomatic Meckel's diverticula have ectopic gastric or pancreatic cells contained within them, this is displayed as a spot on the scan distant from the stomach itself. Patients with these misplaced gastric cells may experience peptic ulcers as a consequence. Other tests, such as colonoscopy and screenings for bleeding disorders, should be performed, and angiography can assist in determining the location and severity of bleeding. Meckel's occurs more often in males than females.
Perforated duodenal ulcers can -> pneumoperitoneum. Pneumoperitoneum or intra-peritoneal free air quite commonly follows gastrointestinal tract perforation. It can be detected with plain abdominal films or ultrasonography.
The gallbladder stores bile that is not immediately needed for digestion and concentrates it by absorbing some of its water and ions.
#UC#takayasus arteritis#omphalocele#edwards syndrome#gastroschisis#cholera#ORT#hep B#meckels diverticulum#pneumoperitoneum#bile
1 note
·
View note