#sclerosing osteitis
Text
Condensing Osteitis: Symptoms, Diagnosis and Management
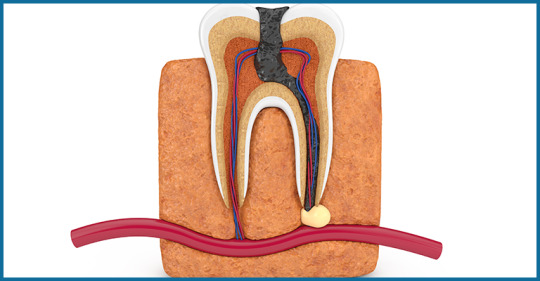
Focal sclerosing Osteomyelitis, also known as Condensing Osteitis, is an infection of the tissues around the root, or a periapical inflammatory disease. This is not a usual situation.
Here's some vital information to help you understand the fundamental features, symptoms, diagnosis, and treatment of this unusual tooth issue.

What is it?
The tooth consists of two parts: the crown and the root. The crown is the visible component of the tooth inside the mouth, whereas the root is lodged inside the jaw bone. The periapical area refers to the area surrounding the apex or root tips. Condensing osteitis is an inflammatory illness affecting the periapical area. It is typically regarded as an inflammatory trigger.
Symptoms
It is usually symptomless with only intermittent episodes of discomfort, therefore your endodontist can identify it via an x-ray.
Condensing osteitis is most common in young people, however it can also occur in other age groups.
This disorder is more common in the molar region, but it can also occur in other tooth regions.
Diagnosis and Management
When condensing osteitis is detected, the first and most important action is to consult an endodontist. The care begins with a thorough evaluation of the affected tooth.
The endodontist will examine the pulp tissue of the tooth for vitality. The pulp tissue is the tooth's internal soft tissue, which contains nerves and blood vessels and helps to keep the tooth alive by providing sustenance.
This can be accomplished using a variety of pulp vitality testing procedures. The choice of test is determined on the patient's major complaint.
If the pulp contains necrosis or dead tissue, or if the inflammation is severe, the tooth must be extracted as it cannot be saved.
Prognosis
To your surprise, if the bone produced as a result of infection is not producing symptoms or discomfort, there is no need for treatment and the tooth can be left as is.
It has been discovered that such teeth remain normal and can work normally for years without any problems.
However, remember that a periodic checkup is required so that your endodontist can check for changes using x-rays. If necessary, the treatment can be performed. When the problematic tooth is taken, the socket left behind is the area of condensing osteitis of the jaw, and it can be left that way. It is painless and referred to as osteosclerosis of the bone scar.
For more information read the full blog here : https://www.orisdentalcenter.ae/blog/condensing-osteitis-symptoms-diagnosis-and-management/
#condensing osteitis#sclerosing osteitis#garre osteomyelitis#garre's sclerosing osteomyelitis#Osteomyelitis#osteomyelitis disease#osteomyelitis symptoms#Periodontitis#tooth psin#tooth infection#dental
0 notes
Text
Les osteitis des maxillaires pdf
LES OSTEITIS DES MAXILLAIRES PDF >>Download (Descargar)
vk.cc/c7jKeU
LES OSTEITIS DES MAXILLAIRES PDF >> Leer en línea
bit.do/fSmfG
de A Encinas Bascones · 2013 · Citado por 3 — Es una forma localizada de osteítis fibrosa quística a la que se llega después de una Tumeur brune bilatérale des maxillaires. a propos d un cas. El Texto completo está disponible en PDF. Bibliografía. [1.] M.S. Shanmugham, S.F. Alhady. Hyperparathyroidism with osteitis fibrosa cystica in the maxilla. We report two complicated cases of florid cemento-osseous dysplasia, one with facial deformity and the other with chronic osteitis. Discussion. The diagnosis of motivazione del paziente, abuso di droghe, alcool e tabacco, osteiti Les implants insérés dans le maxillaire supérieur ne doivent pas perforer le. de B Ramos · 2001 · Citado por 10 — View PDF; Download Full Issue Brown tumor, or osteoclastoma, is one of the manifestations of osteitis Tumeur brune bilatérale des maxillaires. de A Uribarri Echevarría · 1997 — La enfermedad ósea de Paget (EP) u osteitis defor- frecuentes las osteitis y osteomielitis, así como las lisée au maxillaire inferieur. maxillaires et mandibules), probablement tous ceux qu' il a eusous ses yeux, sans tenir compte des différentes lo calités d' oú ils procédai-ent,.de L Benjellou · 2011 — to as sclerosing osteitis, multiple enostoses, diffuse chronic osteomyelitis, gigantiform cementoma, and antérieure du maxillaire supérieur. Rev. Mens. se manifiesta la osteítis fibrosa quística, que representa el esta- Tumeur brune bilatérale des maxillaires. A propos d'un cas.
https://www.tumblr.com/mimitiban/697908831038128128/arquitetura-neolitica-pdf-writer, https://www.tumblr.com/mimitiban/697909272361795584/nature-and-scope-of-business-policy-pdf, https://www.tumblr.com/mimitiban/697908831038128128/arquitetura-neolitica-pdf-writer, https://www.tumblr.com/mimitiban/697909272361795584/nature-and-scope-of-business-policy-pdf, https://www.tumblr.com/mimitiban/697908971982422016/jurnal-senyawa-hidrokarbon-pdf.
0 notes
Text
Lupine Publishers | Two Rare Cases of Monostotic Paget’s Disease of Bone in Adult Female

Lupine Publishers | Orthopedics and Sports Medicine
Abstract
Introduction: Paget’s disease of bone is a metabolic bone condition characterized by increased bone resorption by osteoclasts with simultaneous new bone formation. The result of which is bone appears expanded with both lytic and sclerotic areas. The bone eventually becomes weak and starts producing symptoms such as pain, difficulty in walking if it involves the weight bearing bones, pathological fracture and systemic symptoms related to increased bone turnover.
Case presentation: Here we are reporting two adult female cases of monostotic Paget’s disease involving tibia. A 58-year-old female and a 47 year old female who presented with complaints of pain in the leg with history of fever. Blood investigations showed elevated alkaline phosphatase with normal serum calcium and phosphorous. X ray of tibia showed lytic and sclerotic areas. MRI showed features of Paget’s disease of tibia. Biopsy of tibia confirmed the diagnosis to be monostotic Paget’s disease of tibia. They were managed conservatively with oral bisphosphonates.
Conclusion: Monostotic Paget’s disease even though is a rare disease it is encountered now and then in Indian population. It has to be differentiated from other lesions producing similar clinical picture such as secondary osteosarcoma, sclerosing osteomyelitis and metastasis. Early diagnosis and appropriate treatment will reduce pain, deformity and the need for surgical intervention with good symptomatic and radiological recovery.
Keywords: Paget’s Disease; Monostotic Type; Tibia; Rare Condition; Indian Population
Introduction
Paget’s disease of bone was first described by Sir James Paget as early as in the year 1877 [1]. This disease is also known as osteitis deformans. It can either involve a single bone (monostotic) or can involve many bones (polyostotic). This is a type of metabolic bone disease characterized by increased bone resorption and formation of new bone which is consistent with the presence of both lytic and sclerotic areas on radiology. The excessive remodelling makes the bone enlarged , weak and deformed. This disease commonly affects elderly white adults of age above 50 years. The prevalence of Paget’s disease increases with age and is slightly more common in men. Paget’s is rare under 25 years and unusual before 40 years of age [2].
Case 1
58-year-old female came with complaints of pain over the right knee for the past 2 weeks and difficulty in weight bearing over right lower limb. Pain was insidious in onset, aggravated in the night and relieved with rest and medications. No history of radiation of pain or history of pain elsewhere in the body. There was history of fever and there was no history of trauma. There was no history of loss of weight or loss of appetite. On examination there was no swelling, no scars or no sinuses, no visible pulsations or no dilated veins over right knee, there was no bowing. Warmth was present over the right proximal tibia, tenderness was present over right proximal tibia with broadening and thickening. The range of movements of knee joint was not affected and was not associated with any pain, there was no distal neurovascular deficits and distal pulses were well felt. Laboratory investigations showed normal calcium (9mg/dl) and normal phosphorus (3.7mg/dl). Serum alkaline phosphatase levels were elevated (148 IU/L). Plain x ray was done which showed sclerosis over right proximal tibia and lytic lesion over right tibial tuberosity with cortical thickening and widening (Figure 1,2).
Figure 1: X ray of right proximal tibia antero-posterior view.
Figure 2: X ray of right proximal tibia lateral view.
We had differential diagnosis as Garre’s sclerosing osteomyelitis of right proximal tibia, metastasis of right proximal tibia and secondary osteosarcoma. MRI of the right proximal tibia was done which showed diffuse cortical thickening of the involved tibia, heterogenous signal with normal fatty marrow, an intracortical cystic lesion measuring 4.2 x 1.5 x 2.3 cm noted just below the tibial tuberosity without any pathological fracture which was consistent with Paget’s disease (Figure 3). CT guided biopsy was done from the lesion to confirm the diagnosis and the specimen was sent for histopathological study which came as monostotic Paget’s disease of right tibia (Figure 4, 5). She was treated with analgesics for pain and was started on oral bisphosphonates T. Alendronate 70mg weekly along with calcium supplementation. On follow up patient was symptomatically better and is mobilising well.
Figure 3: MRI right knee.
Figure 4: CT of right tibia.
Figure 5: Needle insertion under CT guidance.
Case 2
47-year-old female came with complaints of pain in the right leg and deformity of the right leg for one month. Pain is insidious in onset , aggravated on weight bearing , relieved on rest and medication. There was no radiation in pain, increased in night. Pain was associated with deformity and the deformity aggravated on weight bearing. There was no history of fever, no history of loss of weight or loss of appetite, no history of any other limb involvement and no history of trauma.On examination there was a Varus deformity of 10 degrees, there was no visible swelling , no dilated veins or no scars or no sinuses or any visible pulsations. There was warmth and tenderness diffusely over the right leg. Varus of the right leg of 10 degrees. Range of movements of knee and ankle were not affected and was not associate with any pain. There was no distal neurovascular deficits and distal pulses were well felt (Figure 6,7). Laboratory findings were calcium was normal (9.3mg/dl) and phosphorous was normal (4.4mg/dl). Serum Alkaline phosphatase was elevated (173 IU/L ). ESR and CRP were normal. Plain x ray was done which showed lysis and sclerosis of entire right tibia with widening and thickening of cortex (Figure 8). We had differential diagnosis as Garre’s sclerosing osteomyelitis of tibia, metastasis and secondary osteosarcoma of tibia. MRI right leg was done which showed involvement of entire tibia predominantly the proximal aspect including the articular cartilage with cystic areas, subcutaneous edema and thickened cortex with features of mixed phases of Paget’s disease (Figure 9,10). Core needle biopsy of the right proximal tibia was done to confirm the diagnosis and the specimen was sent for histopathological study. The diagnosis was confirmed to be monostotic Paget’s disease of right tibia. She was started on oral Alendronate 70mg once a day weekly along with calcium supplementation and analgesia for pain. Deformity correction was planned on a later date but the patient was symptomatically better and was mobilised so did not come.
Figure 6: Clinical picture.
Figure 7: Clinical picture.
Figure 8: X ray of right leg antero-posterior and lateral view showing cortical widening with lysis and sclerosis predominantly involving proximal tibia and articular cartilage with Varus deformity.
Figure 9: MRI of right knee showing cystic areas and edema inside the marrow and subcutaneous space.
Figure 10: MRI of right knee.
Discussion
Paget’s disease of bone also known as osteitis deformans is a skeletal disease seen in elderly above 50 years of age characterized by increased bone resorption and increased bone turnover. It has a familial tendency of transmission common in first degree relatives of affected patients but it can also be caused by certain viral infections such as paramyxovirus or measles virus Paget’s disease is most common in the United Kingdom and Western Europe but is also common in British immigrants to Australia, New Zealand, South Africa, and South America. The disease is uncommon in African blacks, Scandinavia, China, Japan, Southeast Asia, and the Indian subcontinent [3]. First-degree relatives of patients with Paget’s disease have an increased risk particularly if the patient has an early age of diagnosis and the disease is extensive [4]. This suggests that there is familial trend and genetic factor plays an important role in Paget’s disease. Rural life and animal contacts are associated with a greater risk of Paget’s disease in [5,6], this suggests that animals may carry infectious agents causing the disease. The nuclear inclusion bodies in osteoclasts in Paget’s disease resemble that of viruses [7]. but if viruses play a role as a causative agent for the disease remains unclear. Classical PDB is caused due to mutations in SQSTM1 that encodes for a protein known as p62 that plays an important role in osteoclast regulation. These mutations are only in 5-10% of sporadic cases and in 40-50% of familial cases [8]. Paget’s disease is a chronic disease involving the skeletal system primarily. It is characterized by increased bone resorption by osteoclast followed by increased bone formation by osteoblasts. The osteoclasts are increased in number and size and may contain more than one nuclei. The nuclei may contain inclusion bodies that resemble viral particles [9].The initial pathology is because of increased resorption of bone by osteoclast due to abnormal activation of RANKL and increased expression of interleukin-6 ( IL-6) , the osteoblasts are also increased in number but they are morphologically normal suggesting that the main pathology is due to osteoclastic resorption of bone.
The accelerated resorption and turnover of bone causes the bone to be expanded and laying down of immature collagen fibres makes the bone structurally weak and the bone deforms In India Paget’s disease is rare [10,11].Many times the disease is diagnosed incidentally on routine blood or radiological investigations. In the musculoskeletal system the disease is characterised by pain over the involved bone , there is warmth due to increased vascularity, Deformity of the bone is present especially in weight bearing bones example bowing of femur or tibia, pathological fractures, osteoarthritis of joints adjacent to the involved bone. If the skull is involved there will be frontal bossing. If the spine is involved there will be back pain, radiating pain if there is canal stenosis or cord compression, in severe cases there can be paraplegia. The most commonly involved bones are spine, skull, pelvis, femur and tibia. Here one patient had pain, the other patient had pain and deformity with involvement of tibia in both the cases. Serum calcium, Serum phosphorous levels, Parathyroid hormone levels and Vit D levels [12] are usually normal unless the disease is extensive involving many areas. Bone specific alkaline phosphatase (BAP) seems to have the best diagnostic accuracy as a measure of bone formation, with a sensitivity of 84% and a specificity of 100% [13]. Both the patients who presented to us had normal serum phosphorous, normal serum calcium levels, normal parathyroid hormone and elevated alkaline phosphatase levels. Plain X ray of the involved site will show mixed areas of lytic and sclerotic lesions, bony enlargement, cortical thickening, increased trabeculae and bowing if weight bearing bones are involved. In the above cases we saw all findings in x rays.
Isotope bone scan shows increased uptake in affected areas. Here we did not do isotope bone scan instead we did MRI of the involved leg which showed features of Paget disease.
To confirm the diagnosis we did biopsy, computed tomography guided biopsy of tibia using trephine needle for one patient and core needle biopsy of tibia for the other patient and the specimen was sent for histopathological study. In both the cases it was reported as monostotic Paget disease consistent with our MRI findings.Our cases are unique in the sense both the patients were young female one in early 50’s and the other in late 40’s and both of them had primary involvement of only tibia without any other bone involvement such as pelvis, femur which are most common sites. Asymptomatic lesions do not need any treatment but regular follow up is necessary. In lesions producing symptoms or causing bowing of large weight bearing bones need treatment. The main goal of treatment is to prevent osteoclastic resorption of bone. Bisphosphonates or calcitonin can be used while bisphosphonates being gold standard of treatment for medical management of Paget’s disease. Bisphosphonates such as etidronate, pamidronate, alendronate, risedronate and zoledronic acid [13]. While alendronate and risedronate are given orally whereas pamidronate and zoledronic acid are given intravenously. The potency of bisphosphonates in inhibiting osteoclastic bone resorption may be related to their ability to inhibit farnesyl diphosphate synthase [14]. Common side effects with oral bisphosphonates are gastrointestinal and oesophageal disturbances which is why it advised to take the drugs early in the morning. In those with gastrointestinal problems intravenous infusion of bisphosphonates can be given but there can be side effects such as transient bone pain, headache , myalgia and nausea. Response to treatment is observed by reduction in the level of serum alkaline phosphatase, improvement in bone pain and radiological improvement of the involved bone. Here once the diagnosis was confirmed by biopsy we started both the patients on oral alendronate 70mg weekly. Both the patients had symptomatic relief of bone pain and were mobilising well two months following the initiation of treatment.In a small number of patients surgery might be indicated if there is pathological fracture for fracture stabilisation , deformity of long bones which causes difficulty in walking or if the patient feels is cosmetically unacceptable in the form of corrective osteotomy , Paget’s disease is known to cause secondary osteoarthritis hence in selected cases total joint arthroplasty maybe necessary [15]. Paget’s disease is a highly vascular condition hence surgery should be done after adequate treatment of the disease to reduce blood loss.
Conclusion
Monostotic Paget’s disease even though is a rare disease it is encountered now and then in Indian population. It has to be differentiated from other lesions producing similar clinical picture such as secondary osteosarcoma, sclerosing osteomyelitis and metastasis. Early diagnosis and appropriate treatment will reduce pain, deformity and the need for surgical intervention with good symptomatic and radiological recovery.
For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
Please click here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/archive.php
8 notes
·
View notes
Text
Bear with me here I'm a Tumblr noob
The most difficult part of beginning this is trying to remember where it began, because chronic pain has been deeply ingrained in my life since I can remember. Another thing I hesitate over is the eye rolls it might already have received – when you’ve lived your life not always in the best health emotionally and physically, you become hyper aware (and anxious) of peoples impressions of you. I have tried to carefully manage these impressions all my life. But I am tired.
This is in no way intended to be a sob story. I am a hugely privileged and happy person with a life full of wonderful supportive people who astound me with their patience and love every day. What this is, is brutal honesty on a subject I have never felt able to be truly honest about. And that is living with constant pain from conditions that cannot be cured. It is a specific set of problems with no real answers and as far as I can see, something that is not addressed in the truthful way that it should be.
It makes sense to me to start now, today, as I’m sitting here feeling some sort of manic no-fucks-left-to-give urge to put it all out there. I have always told myself I should write about it because reading about other people’s experiences has always given me new strength and insight made me feel less isolated. Physically, I feel the usual: aching in my back, legs, shoulder, fatigue and slight nausea but today is a good day. I have just returned from the doctor after at least an hour of reviewing medication, discussing the next invasive investigations (that have become so routine) as well as blood tests.
This is because of a sudden a new symptom: a rash that looks like bleeding under the skin coupled with intense itching and dermatographism (he suggests I write my name on my skin to ‘impress my friends’ and of course I immediately try it out – I appreciate a doctor with a sense of humour). He suggests weakened capillaries, possible problems with liver function and stresses the importance of no more anti-inflammatory tablets and no more alcohol if I want to limit the already sky high risk of bleeding in my gut. In front of him are my medical history and list of medications and he almost laughs as he tells me that it has got to a very complicated point. Several of them interact, one that keeps my moods up and another that keeps my pain down (as much as it is ever down) and then there’s the fact that this new rashy itching ridiculousness could actually be a side effect of the SSRI’s and be worsened by the anti inflammatories that I have been taking for 18 years without so much as a days break. More medication leads to more complication, everything has a side effect and going cold turkey means days in bed wondering what the point is of ever getting out of it.
At this point in the post, I’m already apprehensive of sounding overly dramatic as well as feeling guilty because I know that people suffer much worse than I do. But over the years I’ve become expert at dismissing my own pain as well as not giving myself any credit for coping with it, and that has revealed to be a very unhealthy and damaging attitude for me. Anyone with chronic pain will understand the intensity of the situation and how it becomes a part of you whether you resist it or not. Anyone who hasn’t experienced it can try their best to understand or dismiss it as an exaggeration, which is their prerogative.
I grew up in a typically British culture of ‘get on with it’, ‘don’t be a malingerer’ and ‘get it sorted’. These are all very helpful attitudes until you reach a point where emotionally and physically there is no getting it sorted. When the three main problems (endometriosis, sclerosing osteitis and anxiety/depression) are incurable, you have to adopt a significantly different approach. On a daily basis, I look fine, so I am expected to act fine and as soon as that mask starts to slip I see the people around me getting frustrated. I know they do. I can sense the irritation when I call in sick to work, again, and bail on a night out and wince in pain as soon as I get out of bed and attempt to explain to the person I’ve just been on a date with that it’s more complicated than us having a stress free, casual situationship, whether I want to or not. These feelings are not exclusive to me or my conditions, they are something that people with all kinds of mental and physical difficulties will feel but that people generally don’t want to talk about or even listen to.
The feeling that your body and mind is inherently broken means you run the risk of being involved with the wrong people, in my experience. At my lowest point I searched for some kind of sustainable romantic connection (that I often don’t feel capable of having) in all the wrong places and at the expense of my own wellbeing. It’s all fun and #romance until the point at which I seem to shut down because I don’t feel comfortable with the burden that I am on a partner.
My last long term relationship was with someone truly kind and understanding and patient and even though it broke down for a number of reasons, the pain was a big factor. Unless you experience it, which I would never wish on anyone, it is the most difficult thing to get your head around. Long term pain, fatigue and depression affects every single aspect of life: work, leisure, socialising, friendships, relationships, sex, your personality, the way you feel about your body, your finances (people generally don’t want to employ someone who can’t get out of bed for a week every month).
There’s also the fact that long term physical problems often come with mental health problems. The two are intrinsically linked and, without fail, ignored by every medical professional I have ever seen. Endometriosis in particular is everything to do with your hormones – how to manage them, control them, stop them, start them - and so you pump your body full of medications, contraceptives, coils, herbal remedies, even alcohol just to forget it’s there for a while until that just causes more discomfort than it’s worth.
I don’t have a particular point to make here other than needing understanding, and more than anything the support to tell the truth and be listened to. Chronic pain might give you the reputation of being lazy, a whinger, a hypochondriac, a party pooper and quite frankly it is boring as fuck to defend yourself against that but I am truly done.
This time last year I applied for universities but felt pessimistic about what the future would be like living like this. Today I am studying a subject that gives me purpose in a city that I love. The list of things that I appreciate about my life and where I’m at is endless, and thankfully I’ve reached a point where I can truly appreciate how lucky I am. But every day is difficult, a balancing act that I often feel I’m losing. If it’s not my body it’s my mind, or both, or people around me not understanding, or explaining for the thousandth time what endometriosis and chronic pain sufferers have to deal with.
Through here I will continue to write openly and honestly about handling a difficult set of circumstances. It is for anyone who might take any amount of comfort in it or just wants to be able to have a rant without judgement. I will not be telling you that cutting out wheat, dairy, caffeine, sugar and alcohol is the only option or that you should do yoga a thousand times a week or take sole responsibility for your health and wellbeing because for so long trying to perfect my lifestyle drove me insane. It is hard, an uphill battle where all you need is good people, empathy and a never ending supply of shitty tv and chocolate on those bed bound days and the knowledge that there will be better days even when it doesn’t feel like it.
2 notes
·
View notes
Text
condensing osteitis : Symptoms and Treatments

What is Condensing Osteitis?
Focal Sclerosing Osteomyelitis, also known as Condensing Osteitis, represents a rare yet intriguing condition affecting the periapical region of teeth. While encountering this ailment is uncommon, it can manifest even in individuals adhering to diligent oral hygiene practices. Understanding its fundamental aspects, symptoms, diagnosis, and management is pivotal for dental practitioners and patients alike.
At its core, Condensing Osteitis perturbs the periapical area surrounding a tooth's root. Unlike typical inflammatory responses leading to bone degradation, this condition prompts bone deposition, rendering the affected area radiopaque on X-rays, contrasting with the usual radiolucency associated with bone destruction.
Symptoms of Condensing Osteitis are typically subtle, often presenting as sporadic episodes of discomfort rather than persistent pain. Although prevalent among young adults, it can manifest across different age groups, with a notable predilection for the molar region, albeit occurrences in other dental regions are not unheard of.
When suspecting Condensing Osteitis, prompt referral to an endodontist is imperative. Diagnosis commences with a comprehensive examination of the afflicted tooth. Pulp vitality testing, tailored to the patient's symptoms, aids in assessing the condition of the tooth's innermost tissues. In cases of severe inflammation or necrosis, extraction may be the only viable recourse to prevent further complications.
Remarkably, if the bone deposition remains asymptomatic, intervention may not be necessary, and the affected tooth can be left untreated. Long-term prognosis suggests that such teeth can maintain normal function for extended periods, although regular monitoring through X-rays is advisable to detect any changes necessitating intervention.
In instances where extraction is deemed necessary, the resultant socket represents an area of jaw osteosclerosis, devoid of pain and commonly known as a bone scar. Monitoring these sites for any developments is prudent, although intervention may not be warranted if they remain asymptomatic.
Final Thoughts
While condensing Osteitis may be rare, its impact on dental health merits attention. Understanding its nuances empowers dental professionals to provide timely and effective management, ensuring optimal outcomes for patients. Vigilance through regular check-ups enables early detection of any changes, facilitating appropriate interventions when needed.
FOR MORE INFO VISIT OUR BLOG ON CONDENSING OSTEITIS
0 notes