Get trusted medical device repair services, high-quality parts, and accessories for all your healthcare equipment needs. Ensure optimal performance and reliability with our expert solutions.THE BIOMED GUYS
Don't wanna be here? Send us removal request.
Text
ECG vs Telemetry: Key Differences, Use Cases & Technician Roles
Cardiovascular diseases are one of the major causes of death throughout the world, with 17.9 million people dying annually from heart-related conditions, according to the World Health Organization. This staggering statistic underscores the critical need for effective cardiac monitoring to track heart health. In this context, ECG and telemetry play pivotal roles in diagnosing and managing heart rhythm abnormalities. An electrocardiogram (ECG) provides a snapshot of the heart's electrical activity, allowing healthcare providers to identify irregularities in a patient's heart rhythm. On the other hand, a telemetry monitor offers continuous monitoring, providing real-time data on a patient's heart activity, especially for those at high risk or under intensive care. The growing demand for advanced technologies in managing cardiovascular health is evident as the relevant market is valued at USD 28.1 billion in 2021. Understanding the key differences, use cases, and technician roles in ECG vs telemetry is essential for optimizing patient outcomes.

What Is an ECG (Electrocardiogram)?
An electrocardiogram (ECG or EKG) is a medical test that records the heart's electrical activity. It helps detect heart rhythm abnormalities, blockages, and other cardiac issues. Developed in the early 20th century, the ECG has become a fundamental tool in diagnosing heart conditions worldwide. Measuring the electrical impulses that trigger heartbeats provides valuable insights into the heart's health.

How It Works
A 12-lead ECG involves electrodes on specific body areas to capture the heart's electrical signals from different angles. The ECG leads detect and record electrical impulses traveling through the heart, allowing healthcare professionals to analyze heart rhythms, identify abnormalities, and make diagnoses. This setup provides a detailed, comprehensive view of the heart's activity.
Pros & Cons
Pros: A diagnostic ECG offers a snapshot of heart health, which is ideal for quick assessments of heart rhythm and abnormalities.
Cons: Its primary limitation is the duration of monitoring—typically only minutes—and it does not allow for mobility, as patients are generally confined to a stationary position.
What Is Telemetry Monitoring?
Telemetry monitoring is the continuous remote monitoring of a patient's heart activity, particularly in hospital settings. It allows healthcare providers to track cardiac health in real time, offering more flexibility and real-time intervention than traditional ECG testing.

How It Works
A 3–5 lead setup captures the heart's electrical signals in telemetry monitoring. The leads are connected to a wireless transmitter that sends the data to a central station for monitoring. This allows healthcare providers to continuously monitor a patient's heart activity from a distance, ensuring quick responses to abnormalities.
Pros & Cons
Pros: Cardiac telemetry offers real-time surveillance, enabling prompt intervention if any changes in heart rhythm are detected. It also allows for ambulatory range, meaning patients can move around while monitored. The built-in alarm systems ensure that any dangerous changes in heart activity are quickly noticed.
Cons: While telemetry offers continuous monitoring, it can sometimes be less detailed than a 12-lead ECG, and it depends on wireless technology, which may face connectivity issues in specific hospital environments.
Key Differences Between ECG and Telemetry
While both ECG and telemetry monitoring serve to track heart activity, they differ significantly in their applications, capabilities, and monitoring methods. Understanding these differences helps healthcare providers choose the most appropriate tool for diagnosing and managing cardiac conditions. Below, we go in-depth into the key distinctions in primary use, duration, leads, mobility, data output, and focus, clearly comparing each system's strengths and limitations.
Primary Use, Duration, Leads
ECG is primarily used for diagnostic purposes, providing a snapshot of heart activity for a short period. With a 12-lead ECG, healthcare providers can quickly assess the heart's rhythm and detect any irregularities. Typically, this test is brief, lasting only a few minutes. In contrast, telemetry monitoring is used for continuous monitoring, particularly for patients who need ongoing observation, such as those in critical care or recovery. Using a 3–5 lead setup, telemetry provides real-time data for extended periods, allowing for the detection of heart rhythm changes over time.
Mobility & Setting
ECG is often performed in a clinical setting where the patient remains stationary for the duration of the test. Mobility is limited as it requires a fixed connection to the equipment, and patients generally cannot move freely during the test. On the other hand, telemetry monitoring provides ambulatory monitoring, allowing patients to move around while their heart activity is tracked. This makes telemetry ideal for monitoring patients in hospital settings, offering flexibility without compromising safety, as the wireless system can transmit data remotely, even during mobility.
Data Output & Focus
An ECG focuses on providing detailed, high-quality information about the heart's electrical activity in real-time. The data output is often in the form of a printout or digital graph representing the heart's rhythm at the moment of testing. Its primary focus is on diagnosing specific cardiac issues during the test period. Telemetry monitoring, on the other hand, provides continuous surveillance. The data output is displayed in real-time on a central monitoring station, offering ongoing heart rhythm tracking. Telemetry focuses on long-term monitoring to detect sudden changes or abnormalities, particularly in patients at higher risk.
Clinical Use Cases & When to Use Each
ECG and telemetry monitoring are invaluable tools in cardiac care, but they serve different purposes depending on the clinical scenario. Understanding when to use each can help healthcare providers deliver the best care. In this section, we will learn about the clinical use cases for both tests and provide examples of situations where each tool is most beneficial.

ECG is most commonly used in acute diagnostic settings or as part of routine pre-operative screenings. It effectively detects heart rhythm abnormalities or myocardial infarctions (heart attacks) during a clinical visit. For instance, a patient showcasing acute chest pain may undergo an ECG to assess for signs of ischemia or arrhythmias quickly. Additionally, ECG is frequently used as a diagnostic tool before surgery to evaluate any pre-existing heart conditions that could complicate anesthesia. It is a go-to test for quick, in-the-moment assessments of heart function.
Telemetry Use Cases
Telemetry monitoring is primarily used for patients requiring continuous cardiac surveillance. After a myocardial infarction (MI), patients are often placed under telemetry monitoring to track heart rhythms and detect complications like arrhythmias or ischemia. It is also a key tool in arrhythmia surveillance, where patients with abnormal heart rhythms are monitored in real time. In step-down units, telemetry provides ongoing monitoring for stable patients who still require observation. This method is essential for detecting early warning signs that may require intervention.
Example Scenarios
Consider the following patient scenarios to better understand when to use ECG versus telemetry. A patient who presents to the emergency room with chest pain may first undergo an ECG to diagnose a possible heart attack or arrhythmia quickly. If the diagnosis is confirmed, the patient may be transferred to a telemetry unit for continuous monitoring to track their recovery and detect any new issues, such as arrhythmias or further ischemic events. These examples highlight how each method is used in different phases of care to ensure optimal patient management.
Technician Roles: ECG Technician vs Telemetry Technician
While both ECG and telemetry technicians play essential roles in cardiac care, their duties and responsibilities vary based on the technology they use. Understanding the distinction between the roles is crucial for ensuring efficient and accurate heart health monitoring.

ECG Tech Duties
An ECG technician is responsible for preparing patients for an ECG test. This includes patient prep, such as explaining the procedure, ensuring the patient is comfortable, and correctly positioning the electrodes. The technician then places the ECG leads on the patient's body in the correct locations to capture accurate heart signals. After the ECG operation, the technician monitors the output, ensuring the heart's electrical activity is recorded clearly. They must also be familiar with troubleshooting technical issues if the test produces unreliable results.
Telemetry Tech Duties
A telemetry technician is responsible for continuously monitoring patients' cardiac health. Their primary duty is making sure that the patient stay connected to a telemetry monitor are effectively observed for heart rhythm changes. They respond promptly to alarm systems if an abnormal rhythm is detected, alerting the healthcare team when necessary. The technician also documents the patient's heart activity, ensuring all data is accurately recorded for clinical review. Their role is vital in identifying early signs of deterioration, making timely interventions possible.
Training & Certification
ECG and telemetry technicians require specific education and training to perform their duties. ECG techs typically complete a certificate program or associate degree relevant to cardiovascular technology or any related field. They are trained in the proper placement of ECG leads and the interpretation of heart rhythms. Certification in ECG is available through organizations like the American Society of Phlebotomy Technicians (ASPT) or the Cardiovascular Credentialing International (CCI). Telemetry techs, on the other hand, often complete specialized training programs focusing on continuous cardiac monitoring and alarm response systems. While certification is not always required, some employers prefer candidates to have certification in cardiac telemetry. Both roles require ongoing education to keep up with advances in technology and standards of care.
Wrapping Up
ECG and telemetry play essential roles in cardiac care, each serving unique purposes for diagnosing and monitoring heart health. While ECG offers a detailed snapshot of heart activity for short-term diagnostics, telemetry provides continuous, real-time surveillance for patients requiring extended observation. Understanding the differences in the various technologies can help healthcare professionals choose the right tool based on patient needs. The Biomed Guys offers top-quality medical devices and cardiac monitoring solutions for those needing reliable medical equipment. Check out our products today to uplift your healthcare practice and patient care.
To know more: https://thebiomedguys.com/blog/ecg-vs-telemetry-key-differences-use-cases-technician-roles/
0 notes
Text
Telemetry vs EKG: Key Differences, Procedures, and Career Paths
As the demand for real-time cardiac diagnostics grows, understanding the distinction between telemetry and EKG becomes increasingly essential for healthcare professionals and patients. The global cardiac monitoring & rhythm management devices market, valued at USD 27.04 billion in 2023, it is likely to reach USD 40.61 billion by 2033, highlighting the surge in demand for technologies like ECG and cardiac telemetry monitoring. With cardiovascular diseases accounting for 17.9 million deaths each year globally, early detection through accurate monitoring methods is more critical than ever.
This article explains the key differences between telemetry vs EKG, the procedures involved, and the career opportunities within each field. Whether you're a medical student, a practicing clinician, or someone considering a healthcare career, understanding EKG vs. telemetry can help clarify how each tool supports patient care and long-term outcomes.
What Is an EKG?
To learn about the role of cardiac monitoring in clinical settings, it’s essential to start with the basics of an EKG. Often used in emergency and routine care, an EKG provides a snapshot of the heart’s electrical activity. Unlike telemetry, which offers continuous monitoring, an EKG is typically a one-time diagnostic test to evaluate symptoms like chest pain or irregular heartbeat. This section will cover what an EKG is, how it works, and what patients and healthcare professionals, particularly those pursuing EKG technician duties, should know about the process and its significance.

Definition and Purpose
An electrocardiogram (EKG or ECG) is a 12-lead diagnostic test that records the heart’s electrical signals over a brief period. It plays a vital role in identifying arrhythmias, myocardial infarctions (heart attacks), and structural abnormalities such as left ventricular hypertrophy. Each lead offers a unique angle of the heart’s activity, allowing clinicians to pinpoint problem areas.
The EKG test is often a first step in diagnosing cardiac concerns and guiding further treatment. EKG technician duties include preparing patients, operating the equipment, and ensuring accurate data collection. For those considering a healthcare role, obtaining an EKG certification can open doors to entry-level cardiac care positions.
Procedure and Workflow
The EKG test procedure is straightforward but must be performed with precision to ensure reliable results. The patient is asked to lie flat and remain still. According to AHA guidelines, the technician cleans specific skin areas and attaches ten electrodes—four limb and six chest electrodes. These electrodes capture electrical signals from various heart angles, producing a printed or digital tracing.
A physician then interprets the tracing to detect abnormalities. EKG technician duties include ensuring the leads are correctly placed, verifying patient identity, and troubleshooting any artifacts or irregular signals. Understanding this workflow is essential for anyone working toward EKG certification or exploring hands-on patient care roles.
Clinical Uses
An EKG is widely used in various clinical settings for acute and routine diagnostics. In emergency rooms, it helps detect life-threatening conditions like myocardial infarctions and arrhythmias within minutes. In outpatient clinics, it is frequently used for screenings and monitoring patients with known cardiac issues. EKGs are also a key component of stress testing, where heart activity is evaluated during physical exertion to uncover hidden abnormalities. These tests provide critical insights into heart function. They are often part of routine evaluations for patients with chest pain, dizziness, or palpitations, making them essential in preventive and acute care.
What Is Cardiac Telemetry?
While an EKG offers a snapshot of heart activity at a single point, cardiac telemetry allows for real-time monitoring over extended periods. Telemetry systems are used primarily in hospitals and specialized care settings, which are vital in continuously tracking a patient’s cardiac rhythm without restricting mobility.
These systems are beneficial for patients at risk of sudden cardiac events, those recovering from surgery, or individuals with fluctuating heart conditions. This section goes in-depth about how cardiac telemetry works, the equipment involved, and its many clinical applications, highlighting the importance of cardiac monitoring devices in both inpatient and ambulatory monitoring scenarios.

Definition and Purpose
Cardiac telemetry is a form of real-time monitoring that continuously tracks the heart’s electrical activity using 3- to 5-lead systems. Unlike the 12-lead EKG, telemetry provides an ongoing data stream transmitted wirelessly to a central station. This allows healthcare professionals to observe changes in cardiac rhythm as they occur, making it crucial for early detection of arrhythmias, ischemic events, or cardiac instability.
Telemetry is most commonly used in hospitals, but its role expands into ambulatory monitoring for patients requiring extended observation outside of inpatient care. It bridges the gap between momentary diagnostics and long-term heart health surveillance.
Equipment and Leads
Cardiac telemetry systems have a few essential components: a portable transmitter, electrode leads, and a central monitoring station. The transmitter, worn by the patient, collects ECG signals via 3–5 electrodes strategically placed on the chest. These signals are wirelessly sent to a central station where trained staff monitor patients’ heart rhythms around the clock.
Cardiac monitoring devices may also include alarm systems that trigger alerts in case of dangerous heart rate changes or signal disruptions. This setup ensures that healthcare teams can respond swiftly to any abnormalities in cardiac rhythm, improving outcomes in critical and progressive care environments.
Clinical Uses
Cardiac telemetry plays a vital role in various clinical settings. It is widely used for inpatient surveillance, especially in telemetry and intensive care, where constant heart monitoring is essential. Post-operative patients recovering from cardiac or major surgeries are frequently monitored through telemetry to detect complications early.
In ambulatory monitoring, portable telemetry devices allow patients to perform daily activities while their cardiac rhythm is monitored remotely. These systems are also used in step-down units for patients transitioning from the ICU to general care. Across all applications, telemetry supports proactive care by enabling fast response to cardiac irregularities as they happen.
Telemetry vs EKG: Key Differences
Understanding the distinctions between telemetry and EKG is essential for healthcare providers, patients, and those pursuing cardiac diagnostics careers. While both tools serve to monitor heart activity, they differ significantly in purpose, duration, setup, and output. This telemetry vs ECG comparison is critical in tailoring the right diagnostic or monitoring strategy based on patient needs. With 3–6 million Americans estimated to have atrial fibrillation, and the EKG test procedure or telemetry often being the first step in detection, knowing their differences aids in clinical decision-making. The employment of cardiovascular technologists is also projected to grow by 4% by 2032, making this knowledge valuable for career-minded individuals in patient monitoring.

Purpose & Duration
The core difference between telemetry and EKG lies in their purpose and how long they are used. An EKG, specifically a 12-lead ECG, captures a momentary snapshot of heart activity, ideal for diagnosing arrhythmias, myocardial infarctions, or structural abnormalities during a scheduled test or emergency visit. In contrast, 3-lead telemetry or 5-lead systems are used for continuous surveillance, often spanning hours to days. Telemetry is crucial in monitoring hospitalized patients for evolving or intermittent cardiac issues. However, studies suggest that prolonged telemetry in low-risk cases may not improve outcomes and can lead to alarm fatigue, highlighting the need for proper utilization based on clinical necessity.
Lead Configuration & Mobility
The difference in lead configuration is striking when comparing a 12-lead ECG and 3-lead telemetry. The EKG uses 10 electrodes to generate 12 different views of the heart, offering detailed diagnostics from a fixed, static position. It’s generally performed while the patient is lying down and still. Conversely, telemetry uses fewer leads—typically 3 to 5—allowing for more flexible and mobile patient monitoring. Patients can move around within the hospital while still being continuously observed. This mobility makes telemetry ideal for longer-term care settings but limits its diagnostic depth compared to a standard EKG setup.
Data Output & Interpretation
Another point in the telemetry vs ECG comparison is how data is recorded and interpreted. An EKG provides a static tracing that a clinician manually reviews for abnormalities. This makes it highly effective for acute diagnostics and official medical records. In contrast, telemetry systems offer real-time alerts and continuous streams of heart rhythm data monitored by nursing staff or telemetry technicians. While this ongoing data is essential for catching sudden cardiac events, it also requires careful triaging to avoid false alarms. Both systems play complementary roles, with EKGs used for definitive diagnosis and telemetry for ongoing cardiac rhythm surveillance.
Roles and Responsibilities
EKG and telemetry technicians play essential roles in cardiac care, but their day-to-day responsibilities vary depending on the setting and the equipment used. Whether capturing a single diagnostic tracing or monitoring heart rhythms around the clock, these professionals are the first line of observation in identifying potentially life-threatening cardiac events. Understanding the duties specific to each role helps clarify career expectations and necessary skills.
EKG Technician Duties
EKG technicians are responsible for conducting electrocardiogram tests under physician supervision. Their duties include preparing patients, applying electrodes, performing the EKG test procedure, and ensuring high-quality tracings free from artifact or interference. They must know basic heart anatomy and be able to identify common abnormalities for preliminary review, though formal interpretation is left to physicians. Additional tasks may include stress testing, Holter monitor setup, and maintaining equipment. EKG technicians often work in outpatient clinics, hospitals, or diagnostic labs, supporting timely cardiac diagnostics across various care settings.
Telemetry Technician Duties
Telemetry technicians are primarily responsible for continuous cardiac rhythm monitoring, often from a centralized hospital unit. They monitor multiple patients’ heart rhythms in real time, review rhythm strips, and identify irregularities such as arrhythmias, bradycardia, or asystole. Upon detecting abnormalities, they must quickly alert the medical team to ensure timely intervention. This role demands strong attention to detail, recognizing emergent conditions, and practical communication skills. Telemetry technicians often collaborate with nurses and physicians to ensure proper patient monitoring, especially in telemetry units, ICUs, and post-op recovery areas.
Education and Certification Paths
While both roles provide entry points into cardiac care, the training and certification requirements for EKG and telemetry technicians differ slightly. Whether seeking formal education or learning on the job, understanding the available credentials can help you advance in the field.

EKG Tech Training
To become an EKG technician, candidates typically complete a short certificate program—often three to six months—through a vocational school, community college, or allied health training center. These programs combine classroom instruction and hands-on practice with EKG equipment. Prerequisites may consist of a high school diploma or GED. One of the most recognized credentials is the Certified EKG Technician (CET) certification, offered by the National Healthcareer Association (NHA), which validates knowledge in lead placement, patient preparation, and basic cardiac interpretation. CET certification can improve job prospects and is often required by employers.
Telemetry Tech Training
Training for telemetry technicians may start with fundamental courses in cardiac anatomy, medical terminology, and basic ECG interpretation. However, many employers also provide on-the-job training, especially for entry-level candidates with healthcare experience. Some positions may require previous work as a nursing assistant or EKG technician. A well-regarded credential in this field is the Certified Rhythm Analysis Technician (CRAT), offered by Cardiovascular Credentialing International (CCI). This certification demonstrates proficiency in reading and analyzing heart rhythms, critical for effective patient monitoring in acute and subacute care settings.
Career Outlook and Salary
If you're considering a career in cardiac diagnostics, knowing each role's earning potential and job stability is essential. Let’s compare the salary trends and employment projections for EKG and telemetry technicians.
Salary Comparison
EKG and telemetry technicians contribute significantly to cardiac care, yet their compensation varies based on region, experience, and workplace setting.
EKG Technicians: The average hourly wage for EKG technicians in the United States is approximately $23.91, from $11.54 to $41.11 per hour. Annual salaries can vary by state- for instance, Massachusetts reports an average of $103,570, while California offers around $89,780
Telemetry Technicians: Telemetry technicians earn an average hourly wage of $24.46, with reported salaries ranging between $15.58 and $38.41. Annual earnings also differ by location—for example, California's average is approximately $53,566, whereas Oklahoma reports around $60,580.
Job Growth Projections
Employment opportunities for cardiovascular technologists and technicians, encompassing both EKG and telemetry roles, are projected to grow by 4% from 2022 to 2032, which aligns with the average growth of all other occupations. This growth is led by an aging population and the increasing prevalence of heart-related conditions, underscoring the sustained demand for skilled professionals in cardiac monitoring.
Benefits and Limitations
Each monitoring method—EKG and telemetry—has strengths and trade-offs. Understanding these can help guide appropriate clinical use and inform career decisions.

Advantages of EKG Testing
EKG testing offers a detailed snapshot of the heart's electrical activity, making it invaluable for diagnosing arrhythmias, myocardial infarctions, and structural abnormalities. The 12-lead ECG provides comprehensive views from multiple angles, facilitating accurate assessments. Its non-invasive nature and quick execution make it a staple in emergency and routine cardiac evaluations.
Advantages of Telemetry Monitoring
Telemetry monitoring enables continuous, real-time observation of a patient's cardiac rhythm, which is crucial in intensive care units and post-operative recovery settings. Utilizing 3–5 lead systems, telemetry allows patients to move while ensuring their heart activity is consistently monitored. This ongoing surveillance helps with early detection of transient arrhythmias and other cardiac events that might not be captured during a standard EKG.
Challenges
While telemetry provides continuous monitoring, its overuse, especially in low-risk patients, can lead to alarm fatigue among healthcare staff, potentially desensitizing them to critical alerts. Additionally, unnecessary telemetry can strain resources and may not always contribute to improved patient outcomes. Applying telemetry judiciously and adhering to established guidelines are essential to maximize patient care and resource utilization.
Wrapping up
Understanding the difference between telemetry and EKG is essential for selecting the right cardiac monitoring approach in various clinical scenarios. While the 12-lead EKG offers detailed diagnostics in a static setting, telemetry enables real-time, continuous observation for dynamic patient care. Both play complementary roles in the early detection, diagnosis, and monitoring heart conditions. Cardiovascular diseases continue to among one of the leading health concerns, so skilled technicians and reliable cardiac monitoring devices are more important than ever. Whether you’re a healthcare provider or aspiring technician, staying informed about these tools is vital to delivering effective patient care.
Get high-quality telemetry and EKG equipment and essential parts at The Biomed Guys—trusted solutions for modern cardiac care.
To know more: https://thebiomedguys.com/blog/telemetry-vs-ekg-key-differences-procedures-and-career-paths/
Website: https://thebiomedguys.com/
0 notes
Text
Medical Supply Rental: A Complete Guide to Renting Medical Equipment
Introduction
Medical supply rental is a service that provides healthcare facilities, patients, and caregivers with short-term access to medical equipment without the long-term commitment and financial burden of purchasing it outright. Whether for home use, a temporary need, or during recovery after surgery, medical supply rental services ensure that individuals and healthcare providers have access to essential equipment when it’s most needed.
In this comprehensive guide, we will explore everything you need to know about medical supply rentals—how they work, the types of equipment available, the benefits of renting, how to choose the right supplier, and tips for managing rented medical supplies. Whether you’re a patient in need of temporary medical equipment or a healthcare professional managing patient care, this guide provides valuable insights to help you make informed decisions.
What is Medical Supply Rental?
Medical supply rental refers to the practice of leasing medical equipment for short-term use rather than purchasing it. Rental services offer everything from home care equipment to specialized devices used in hospitals or long-term care facilities. These services are ideal for individuals recovering from surgery or chronic conditions, healthcare providers needing additional equipment, or those in need of temporary medical care.
Common Types of Medical Equipment Available for Rent
Mobility Equipment: Wheelchairs, walkers, rollators, crutches, and scooters for patients with limited mobility.
Respiratory Equipment: Oxygen concentrators, CPAP machines, nebulizers, and ventilators.
Hospital Beds: Adjustable beds for patients with limited mobility or those recovering at home.
Patient Monitoring Devices: Blood pressure monitors, pulse oximeters, thermometers, and ECG machines.
Home Care Supplies: Bedside commodes, shower chairs, and lifts for improved comfort and safety at home.
Surgical Equipment: Tools and instruments used during medical procedures or in post-operative care.
Renting these supplies helps reduce upfront costs for individuals and healthcare organizations while ensuring that patients have the equipment they need during their recovery or treatment.
Benefits of Medical Supply Rental
1. Cost-Effective Solution
One of the primary reasons individuals and healthcare facilities opt for medical supply rentals is cost savings. Medical equipment can be expensive, especially specialized devices like ventilators or CPAP machines. Renting instead of purchasing allows patients to access the necessary equipment without bearing the high costs of full ownership. This is particularly useful for patients who only need equipment for a limited time.
2. No Long-Term Commitment
Renting medical equipment offers flexibility, allowing patients and healthcare providers to return equipment once it’s no longer needed. For example, a patient recovering from surgery may only need a hospital bed or mobility aids for a few weeks or months. Rental agreements allow for the return of equipment after the period of use, reducing the burden of long-term ownership.
3. Access to High-Quality Equipment
Rental services often provide access to high-quality, well-maintained equipment. Many individuals and healthcare facilities may not have the resources to purchase state-of-the-art equipment, but by renting, they can access the best tools and machines for their specific needs without the significant financial investment.
4. Maintenance and Repairs Included
Most medical supply rental companies include maintenance and repair services as part of the rental agreement. This ensures that the equipment remains in good working condition throughout its rental period, and any issues are addressed promptly, preventing disruption in care. This can be a huge relief for patients and caregivers who may not have the technical knowledge to repair or maintain complex equipment.
5. Convenience and Flexibility
With medical supply rental, individuals and healthcare facilities don’t have to worry about storage or transportation issues once the equipment is no longer needed. Rental companies typically offer delivery and pickup services, which makes the process incredibly convenient. Furthermore, many rental agreements allow extensions if the need for the equipment continues longer than expected.
Choosing the Right Medical Supply Rental Service
When selecting a medical supply rental company, it’s important to choose one that meets your specific needs. Here are key factors to consider when making your decision:
1. Quality and Range of Equipment
The rental company should offer a wide range of high-quality, well-maintained equipment. Ensure that the equipment provided is FDA-approved and meets industry safety standards. Look for a provider that offers both general and specialized equipment, depending on your needs.
2. Customer Service and Support
Responsive customer service is vital when renting medical supplies. You should be able to contact the provider easily for any questions or concerns. The company should also offer support during the rental period, such as assistance with setup, operation, or maintenance of the equipment.
3. Delivery and Pickup Services
Choose a company that offers convenient delivery and pickup services, especially if you don’t have the means to transport large medical equipment. Timely delivery is also critical for ensuring that you have the necessary equipment available when you need it most.
4. Insurance Coverage and Payment Options
In some cases, medical insurance may cover the cost of renting equipment. It’s important to check whether the rental company accepts insurance or provides financing options if necessary. Be sure to inquire about the payment terms, including whether there are any hidden fees for delivery, maintenance, or late returns.
5. Reputation and Reviews
Do some research on the rental company’s reputation. Look for online reviews and testimonials from previous customers to ensure that they offer quality equipment and reliable service. A company with a long track record of satisfied customers is more likely to meet your expectations.
Types of Medical Equipment Available for Rent
Medical supply rental companies offer a wide range of products. Below are some of the most commonly rented medical equipment:
1. Mobility Aids
Wheelchairs: Available in manual and electric versions.
Walkers: Suitable for individuals with limited mobility.
Scooters: Electric mobility scooters for individuals with more severe mobility issues.
2. Respiratory Equipment
Oxygen Concentrators: For patients who need additional oxygen support.
CPAP and BiPAP Machines: Used for individuals with sleep apnea or respiratory issues.
Nebulizers: For patients with chronic respiratory conditions like asthma.
3. Hospital Beds and Accessories
Adjustable Hospital Beds: Customizable beds with features such as adjustable headrests and footrests.
Mattresses and Bed Rails: Often rented along with hospital beds for patient comfort and safety.
4. Patient Monitoring Equipment
Blood Pressure Monitors: For regularly tracking blood pressure.
Thermometers: Digital or infrared thermometers to monitor body temperature.
Pulse Oximeters: To measure oxygen saturation levels in the blood.
5. Home Care Equipment
Bedside Commodes: For individuals with limited mobility.
Shower Chairs: For safe bathing.
Patient Lifts: To assist caregivers in moving patients safely.
Maintenance and Care of Rented Medical Equipment
While renting medical supplies, it’s important to take care of the equipment to ensure it functions correctly and remains hygienic. Here are some tips for maintaining rented medical equipment:
1. Clean and Sanitize Regularly
Depending on the type of equipment, regular cleaning and sanitization may be required. Follow the manufacturer’s instructions on how to clean and disinfect the equipment to ensure its safety and longevity.
2. Inspect for Damage
Before using the equipment, always inspect it for any visible damage. Report any issues to the rental company immediately, so they can repair or replace the item.
3. Follow Usage Instructions
Ensure you follow the provided instructions carefully when using medical equipment. Misuse can not only cause harm but can also void the rental agreement or cause additional charges.
4. Return on Time
Be mindful of the rental period and ensure that the equipment is returned on time to avoid late fees or charges for additional usage.
Conclusion
Medical supply rental is an excellent solution for individuals and healthcare providers who need temporary access to essential medical equipment. With its cost-effective, flexible nature, renting medical equipment ensures that patients receive the care they need without the financial burden of purchasing expensive devices. Whether you need mobility aids, respiratory devices, or patient monitoring tools, medical supply rental services offer an efficient and convenient way to manage medical needs.
By choosing the right supplier and taking proper care of the rented equipment, you can ensure a smooth and effective experience with rented medical supplies.
Website: https://thebiomedguys.com/
0 notes
Text
ECG Lead Positioning: Complete Guide to 3-, 5- and 12-Lead Electrode Placement

ECG lead positioning is a crucial aspect of accurate heart monitoring, essential for diagnosing various cardiac conditions. Proper ECG electrode placement ensures that the heart's electrical activity is captured accurately, helping healthcare providers interpret the results effectively. As many as 50% of ICU ECGs have misplacements in V1/V2, highlighting the significant error rate in chest lead placement and the importance of accurately counting intercostal spaces. Whether you're using a 3-lead, 5-lead, or 12-lead configuration, understanding the correct placement of each electrode is vital for reliable data.
In this guide, we will learn about the essential steps involved in ECG electrode placement, with a special focus on precordial lead placement and its importance in diagnosing issues like MI mimics and other abnormalities. Additionally, we’ll go in-depth into the ECG troubleshooting tips to resolve common challenges during electrode application. Accurate lead positioning can be the difference between a precise diagnosis and a misleading result, so it is essential to get it right every time.
What Is an ECG and Why Proper Lead Placement Matters
An ECG records the heart's electrical activity. It is a vital tool for diagnosing arrhythmias, heart attacks, and other cardiovascular issues. Proper lead placement is crucial for accurate results, as misplacement can lead to incorrect interpretations, ultimately affecting diagnosis. For example, improper positioning of the limb leads or precordial electrodes can distort the heart's electrical signals.
Following AHA ECG guidelines is essential to ensure precision in placement, such as using intercostal space landmarks and understanding Lewis lead placement or the Fontaine lead technique for optimal readings. Statistics show that 0.4%–4% of ECGs experience limb lead reversals, which can significantly impact diagnostic accuracy (Peberdy MA, Ornato JP, Acad Emerg Med 1994). This emphasizes double-checking limb electrode placement to avoid diagnostic errors and improve patient outcomes.

Types of ECG Configurations
Understanding the different ECG configurations and their clinical applications is crucial for obtaining accurate diagnostic results. The 3-lead, 5-lead, and 12-lead systems each serve specific roles in cardiac monitoring, and the appropriate lead placement can provide critical insights into heart function. Let’s learn about the different systems, focusing on their unique placement requirements and the clinical situations where they are most effective.
3-Electrode System
The 3-lead ECG placement is one of the most basic systems, typically used for continuous cardiac monitoring, such as in ambulatory patients or during transport. In this configuration, the electrodes are placed on the right arm, the left arm, and the left leg (RA, LA, LL). The three leads derived from these electrodes—Lead I, II, and III—are bipolar, capturing the heart's electrical activity from three angles. This system is particularly useful in emergency settings and is often found in telemetry units.
5-Electrode (Telemetry) System
In the 5-lead ECG system, the placement of five ECG electrodes is improved with additional electrodes for more comprehensive monitoring, especially in telemetry and critical care settings. The standard color coding used by the AHA helps prevent errors in placement. The electrodes are placed on the right arm, the left arm, left leg, and right leg (RA, LA, LL, and RL) for limb leads, while the additional (V) chest lead options provide more detailed data on the heart's electrical signals. This system offers better heart rhythm detection and is commonly used for real-time monitoring of patients in hospitals or emergency departments.
12-Lead ECG Basics
The placement of 12-lead ECG is the most comprehensive and widely used system, providing detailed information about the heart's electrical activity. In this configuration, there are 10 electrodes: 4 limb electrodes (RA, LA, LL, RL) and six precordial electrodes (V1-V6) placed on the chest. The 12 leads derived from these electrodes offer an in-depth look at the heart from various angles, helping to identify conditions like myocardial infarctions (MI), arrhythmias, and other cardiac abnormalities. This system is the standard for diagnosing multiple cardiac conditions and is commonly used in hospitals and clinical settings.
Standard 12-Lead Electrode Placement
Proper electrode placement is crucial for accurate and consistent readings. This standardized procedure ensures the measurement of electrical activity from multiple angles, offering valuable insights into heart health. The following guidelines outline the appropriate positioning of limb electrodes and precordial leads to ensure accurate 12-lead ECG placement.
Limb Electrodes (RA, LA, RL, LL)
The limb electrodes are essential for establishing the reference points necessary for interpreting the heart's electrical activity.
These electrodes are typically placed on the arms and legs, with the Right Arm (RA), Left Arm (LA), Right Leg (RL), and Left Leg (LL) positioned in specific anatomical locations.
The ground lead, usually, Right Leg (RL), stabilizes the ECG signal by reducing interference.
It is essential to avoid limb lead reversal, as improper placement can misinterpret the heart's electrical activity.
Additionally, torso placed electrodes versus distal placement helps ensure accurate readings from the body's extremities to the heart's core.
Precordial Leads V1-V6
The precordial leads get placed on the chest, providing a clear view of the heart's electrical activity in the horizontal plane.
Each lead (V1 through V6) is positioned on the chest at precise locations, including intercostal spaces, the sternal borders, and mid-clavicular and mid-axillary lines.
V1 is positioned at the fourth intercostal space, right of the sternum, while V6 is placed at the fifth intercostal space, along the mid-axillary line.
Proper placement of 12-lead ECG electrodes across these anatomical landmarks ensures a comprehensive view of the heart’s function.
Additionally, accurate 12-lead ECG placement is crucial for detecting abnormal patterns or conditions that may not be visible in standard two- or three-lead ECGs.
Common Placement Errors and How to Avoid Them
Accurate electrode placement is essential for a reliable ECG reading. Misplacement can distort the results, leading to misdiagnosis or incorrect interpretation. The following are common placement errors and tips on how to avoid them.
Limb Lead Reversals
One of the most frequent placement errors is limb lead reversal. This happens when the right arm (RA) and left arm (LA) or right leg (RL) and left leg (LL) are swapped. Such reversals can lead to incorrect limb leads and affect the overall ECG waveform, causing inaccurate representations of the heart's electrical activity. To avoid limb lead reversal, always double-check the positioning of the electrodes on the patient's limbs.
V1/V2 Electrodes Placed Too High
Another standard error occurs when the V1 and V2 electrodes are placed too high on the chest. These leads should be placed in the fourth intercostal space, at the right and left sternal borders, respectively. When positioned too high, they fail to capture the correct electrical signals from the heart's ventricles, leading to an inaccurate representation of the anterior heart wall. To avoid this, always ensure that V1 and V2 are placed at the correct anatomical landmarks.
V4-V6 Misleveling
Misleveling of leads V4 through V6 is another issue affecting ECG morphology. V4 should be placed at the fifth intercostal space along the midclavicular line, while V5 and V6 are placed along the anterior axillary and mid-axillary lines. If these leads are misaligned, it can distort the interpretation of the heart's electrical activity, especially in the lateral chest leads. Proper anatomical placement and alignment are key to avoiding this mistake.

Special ECG Configurations and Advanced Leads
Standard 12-lead ECG configurations may not provide enough detail in specific clinical situations, especially for detecting conditions like right ventricular or posterior myocardial infarction (MI). Special ECG configurations and advanced lead placements offer upgraded views of the heart's electrical activity, allowing for more accurate diagnoses in challenging cases. These advanced configurations, including right-sided ECG, posterior leads, and specialized leads like the Lewis and Fontaine leads, are crucial tools for clinicians.
Right-Sided ECG (V3R-V6R)
A right-sided ECG is beneficial in diagnosing right ventricular infarction (RV infarction). In this configuration, additional precordial leads, V3R through V6R, are placed on the right side of the chest to provide a view of the right heart's electrical activity. These leads mirror the standard precordial leads but are placed over the right chest, allowing for better assessment of the right ventricle. The right-sided configuration can help detect RV infarctions that may not be apparent in the standard 12-lead ECG. Proper placement of these leads ensures accurate detection of correct heart abnormalities, essential for timely intervention and treatment.
Posterior Leads (V7-V9)
Posterior leads (V7-V9) are placed along the left axillary, scapular, and paraspinal lines to provide a clear view of the posterior wall of the heart. This configuration is critical for diagnosing posterior myocardial infarction (MI), a condition often missed with standard ECG placements. By positioning these leads in the posterior chest, clinicians can better observe electrical activity from the back of the heart. Early detection of posterior MI using these leads can significantly improve patient outcomes. Correct placement of the posterior leads is essential for obtaining accurate readings that will guide treatment decisions.
Lewis Lead
The Lewis lead configuration amplifies atrial activity, making it particularly useful in cases of atrial flutter or wide-complex tachycardia. This lead system places electrodes on the chest to improve the visibility of atrial electrical signals that might otherwise be masked by more prominent ventricular activity. The Lewis lead configuration helps clinicians distinguish between atrial and ventricular arrhythmias by focusing on the atrial waveforms. The proper Lewis lead placement can aid in diagnosing and managing arrhythmias more effectively, allowing for better patient care.
Fontaine Leads
Fontaine leads are a specialized configuration of bipolar precordial leads used primarily to identify epsilon waves and atrial potentials. These leads are placed in specific locations across the chest to provide a clearer view of the electrical signals originating in the atria and the heart's epicardial surface. Fontaine lead placement is particularly useful in diagnosing arrhythmias and conditions like arrhythmogenic right ventricular cardiomyopathy (ARVC), where abnormal electrical activity in the heart muscle can be identified. This advanced lead system provides valuable insights into the heart's electrical activity, enabling more precise diagnoses and effective treatment for patients with various cardiac conditions.
Patient Variations and Practical Tips
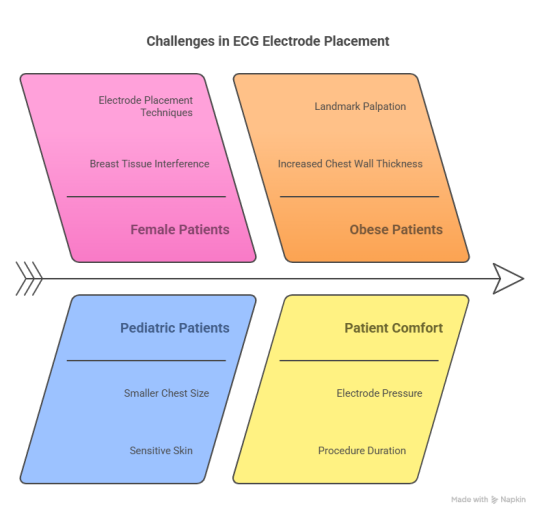
When performing an ECG, it’s essential to consider the patient's unique characteristics and anatomical variations. Proper electrode placement can be more challenging in specific populations, such as females, pediatric patients, and obese patients. Adjusting the approach to these variations ensures accurate ECG readings, which is critical for effective diagnosis and treatment. It's also important to ensure patient comfort during the procedure, as this can affect the reading quality and the patient's experience.
Female Patients
In female patients, breast tissue can interfere with the correct placement of precordial leads, particularly V3-V6. One common technique to address this is breast displacement, where the breast is gently moved aside to allow for the proper placement of the electrodes.
If displacement is not possible or uncomfortable, under-breast placement of leads (just below the breast) can provide accurate readings without causing discomfort. Ensuring the electrodes are securely placed while avoiding pressure on the breast is essential to maintaining both comfort and the integrity of the ECG recording.
Pediatric Patients
Pediatric patients, especially infants and young children, present unique challenges due to their smaller chest size. When placing electrodes on children, it is essential to adjust intercostal landmarks to account for their shorter torsos. For instance, the fourth intercostal space may need to be lower or higher than usual, as per the child’s age and size.
The placement of limb leads might require modifications to ensure the electrodes make proper contact with the skin, as pediatric skin can be more sensitive. Taking extra care to position the leads accurately in a smaller chest ensures the ECG captures precise electrical activity for accurate diagnosis.
Obese Patients
Obese patients may present challenges locating the standard anatomical landmarks due to increased chest wall thickness and body fat. In such cases, palpating landmarks carefully is crucial to ensure accurate electrode placement.
Additional stabilization methods, such as securing the electrodes with tape or adhesive pads, can help prevent the leads from shifting during the procedure. In some cases, slight modifications in electrode placement may be necessary to achieve the best signal quality, such as placing the leads slightly higher or lower than typical locations. Ensuring secure electrode attachment helps in obtaining a precise and reliable ECG reading.
Best Practices and Artifact Reduction
To ensure accurate and reliable ECG readings, following best practices for electrode placement, skin preparation, and cable management is crucial. Proper attention to these factors can significantly reduce common artifacts and improve the overall quality of the ECG recording.
Skin Preparation
Skin preparation is essential for reducing impedance and improving electrode contact. To achieve this, gently clean the skin using alcohol wipes or a skin-prep solution to remove oils, dirt, or other residues that could hinder electrical conductivity. In patients with excessive body hair, shaving the area where electrodes will be placed may be necessary to make a clean and secure connection. Proper skin prep ensures that the electrodes maintain good contact, which helps to obtain clearer ECG signals without distortion.
Cable Management
Proper cable management is critical in minimizing interference and reducing motion artifacts during an ECG. Cables should be neatly arranged and secured to prevent tangling or pulling, which can cause movement-related disruptions in the signal. Using cable clips or adhesive pads to keep cables in place can reduce the risk of unwanted artifacts. Careful cable management helps maintain a consistent ECG signal throughout the recording, especially during lengthy procedures or when the patient moves.
Motion Artifact Minimization
Motion artifacts are common when patients are not still during the ECG procedure. Instruct patients to remain as still as possible to minimize motion interference and avoid talking or moving. If the patient is restless or anxious, consider using calming techniques to promote relaxation. In some cases, securing the patient’s position with comfortable restraints or padding can help reduce involuntary movement, ensuring more accurate results. Additionally, using high-quality electrodes susceptible to motion can help minimize these artifacts.
Wrapping up
Accurate ECG placement and artifact reduction are crucial to get reliable results and make informed decisions in patient care. By adhering to best practices such as proper skin preparation, cable management, and minimizing motion artifacts, healthcare professionals can ensure optimal ECG readings.
For top-quality medical products and reliable diagnostic tools, trust The Biomed Guys. We offer a wide range of high-performance ECG electrodes, cables, and other essential equipment tailored to meet the needs of healthcare providers. Check out The Biomed Guys today to learn about our products and improve the accuracy and efficiency of your diagnostics.
FAQ
1. Where should ECG leads be placed?
The limb electrodes are placed on the patient’s limbs:
RA (Right Arm): Located on the right shoulder or wrist.
LA (Left Arm): Positioned on the left shoulder or wrist.
RL (Right Leg): Placed on the right lower leg or ankle (ground electrode).
LL (Left Leg): Positioned on the left lower leg or ankle.
The precordial leads (V1-V6) are placed on the chest:
V1: 4th Intercostal Space (ICS), Right Sternal Border (RSB).
V2: 4th ICS, Left Sternal Border.
V3: Between V2 and V4.
V4: 5th ICS, Mid-Clavicular Line.
V5: 5th ICS, Anterior Axillary Line.
V6: 5th ICS, Mid-Axillary Line.
2. What is the anatomical position of the ECG lead?
The intercostal spaces (ICS) are the spaces between the ribs, where the precordial leads are placed. The sternal borders refer to the left and right sides of the sternum, where leads V1 and V2 are positioned. The mid-clavicular line is an imaginary vertical line passing through the middle of the clavicle, where V4 is placed. The anterior/mid-axillary lines run vertically down the side of the chest, and V5 and V6 are placed along these lines. Limb electrodes are placed on the arms and legs.
3. What are the 5-lead ECG placement names?
The 5-lead ECG system uses the following electrode colors according to AHA color coding:
RA (white): Right Arm
LA (black): Left Arm
RL (green): Right Leg (ground)
LL (red): Left Leg
V (brown): Precordial Lead (typically V1 or V5 for monitoring)
4. How to memorize 12-lead ECG placement?
To memorize the 12-lead ECG placement, use the anatomical sequence and mnemonic techniques. For the precordial leads, remember the sequence: 4th ICS → 5th ICS. Utilize mnemonic devices like “V1 to V6 from sternum to axilla” for lead placement. Consistent, repeated practice reinforces muscle memory, ensuring correct placement.
5. Where do you place leads 1 and 2 on an ECG?
Lead I is placed between the LA (Left Arm) and RA (Right Arm) electrodes and represents a bipolar view of the heart's electrical activity from the left to the right.
Lead II is placed between the LL (Left Leg) and RA (Right Arm) electrodes, providing a bipolar view of the heart's activity from the bottom left to the top right. The ground electrode is positioned at the RL (Right Leg).
Original Resource: https://thebiomedguys.com/blog/ecg-lead-positioning-complete-guide-to-3-5-and-12lead-electrode-placement/
Visit us here: https://thebiomedguys.com/
0 notes
Text
We’re Not Just Biomedical Technicians — We’re Just Like You
Why THE BIOMED GUYS Was Created
At THE BIOMED GUYS, we’re more than a repair shop or parts supplier. We’re real people—fathers, husbands, veterans—who have worked long hours, taken late-night emergency calls, and done whatever it takes to keep medical equipment working.
We’ve been in your shoes. That’s exactly why we started this company—to support technicians like us.
We Understand Your Struggles
Working in biomedical services isn’t easy. One minute everything is fine, and the next you're called to fix a vital machine before a patient arrives. The pressure is high, the hours are long, and the work never stops.
We know how it feels to be overwhelmed with repairs, to search endlessly for a part, or to have equipment waiting on your bench with no time to spare.
That’s why we built THE BIOMED GUYS—to take some of that weight off your shoulders.
What We Do
We offer more than just repairs. We provide:
✅ Expert repair services for patient care equipment
🔩 Hard-to-find parts and daily essentials
🛠 Useful accessories that make your job easier
🤝 Friendly support from people who get it
If you’re stuck with a machine that won’t work or need a part fast, we’re here to help.
You Fix Lives — We’ll Help Fix the Machines
Your work keeps patients safe. Our job is to help you do yours more easily. Whether you work at a hospital, a clinic, or on the go, we’ll make sure you get what you need—without stress or delays.
If you need a specific part and don’t see it on our website, just ask. We’ll help you track it down.
Our Promise to You
We stand by everything we sell and repair. If something doesn’t meet your expectations, we’ll fix it or replace it—no questions asked. We want you to feel confident when you work with us.
Our goal is simple: To earn your trust and become your go-to partner for all your repair needs.
Let’s Make Your Job Easier
We know you already do enough. So let us help make your day a little smoother. Whether it’s a replacement part, a quick repair, or just advice on what to do next, we’re always here.
Visit us at 👉 thebiomedguys.com Want to know more about who we are? Read our story 👉 About Us
FAQs
Do you work with small clinics or only big hospitals? We work with everyone—big hospitals, small clinics, and mobile providers. If you use medical equipment, we can help.
Can I get help finding a part that’s not on your site? Yes! We love a challenge. Just reach out and we’ll help you find what you’re looking for. Do your parts come with a guarantee? Yes, everything we sell or fix comes with a 100% satisfaction promise. If it’s not right, we’ll make it right.
1 note
·
View note