Text
I’m having a babbbyyy
I am 23 weeks pregnant.
And in all of the circumstances going on in the world right now, all of the uncertainty we face and the constant change - this is one thing I have that I am absolutely ecstatic about.
My husband and I will have our own little offspring in around about 4 months time, our parents will gain their first grandchild and my siblings will all become Uncles and Aunts - and hard to believe for me but my Uncle will turn into a Great Uncle and my Gran will be a great grandmother (or Gran Gran). It feels so exciting, not just for me, but for a huge next step for our family.
My feelings about it have been a bit of a rollercoaster at times.
Charles and I were both over the moon when I took the test (I definitely struggled with the disbelief more than he did), we are extremely lucky because we didn’t actually have any time to worry about us struggling to concieve, because before we knew it I was pregnant.
Instantly I felt I had something I had to protect, and my stresses in life (work, home etc etc) seemed to become less important. Of course, the big things stayed important but all the little things I got my knickers in a twist about before just... bothered me less. A huge, unexpected, relief.
For a few weeks it was just our secret (we were both allowed to tell one friend to stop us spontaneously combusting), but it didn’t feel real in many ways, but since our families were told, and since our 12 week and 20 week scan it has just become more and more real.
We are over half way there, my bump is visible now. I fluctuate between unbelievable excitement, every time I feel our baby squirm, or catch my shape changing in the mirror -- and utter terror because time is going by so so quickly, and I know nothing about what it means to be a mother, not really, and I have not been around many babies (only those at work really, who I adore caring for, but are not typical ‘well’ babies, so many things are different). I have some small concept of how our lives are about to change, but I know I do not even know part of it really.
I would say I have 6 days a week of pure excitement and 1 of terror and holy-hell please can everything slow down a bit.
Of course, there are other things to consider with my health too - that I have been asked a lot about during this process, especially by people who care for me.
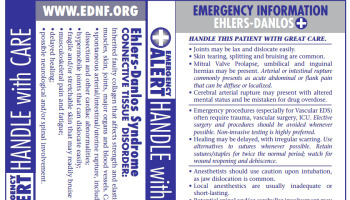
I have Hypermobile Ehlers Danlos Syndrome.
This means I am under specialist care, purely because I have an underlying condition. I am also under genetics, for the future of our baby. My birth choices are limited (but this is no issue to me, as I always would have chosen to be in the John Radcliffe). It has put me through some challenging times, especially initially, with my own body, that I hadn’t really predicted.
Firstly, for the baby: Our child has a 50% chance of having Hypermobile Ehlers Danlos Syndrome. This suprised me somewhat because I thought it was autosomal recessive, but it turns out although they have not found the specific genetics of the condition, they are confident it is autosomal dominant which gives our child a higher chance of being super-bendy and rather dislocate-y like myself. Am I worried? Not particularly. There are many much worse conditions that a child could be genetically pre-disposed to, or develop in a life time. It just means as our child grows we will have to keep a check on how flexible they are, if they have dislocations or recurrent dislocations and any other symptoms, and mostly what we can do to keep them strong (and in my head, avoid lots of contact sport but Charles would love a rugby player for a son/daughter!)
Secondly, for me: Pregnancy was a bit of a nightmare for the first 10-16 weeks, my pain escalated, my dislocations became much more frequent and also more varied, instead of just popping out my thumbs and shoulders a few times a day I was also suffering from dilocated ribs, toes, and even a collar bone that popped out (with a sickening sound) as I lifted a folder off a shelf on a night shift. I was exhausted, completely crippled by exhaustion (normal chronic fatigue + growing a human = bloody hell). I was advised not to take ibuprofen/naproxen, which is my most helpful medication post-dislocation so that was hard, thankfully at approx 12 weeks the obscetrician told me it was fine for me to continue taking ibuprofen until 24 weeks - much to the dismay of my midwives - which helped to ride it out a bit longer. I had terrible sickness and reflux, I suppose it was bound to happen when I already suffer from nausea and reflux but it did make eating a challenge, and during one week around 7 weeks I didn’t hold down food for fluid for 5 days and my GP gave me cyclizine with the advice that if it didn’t work in 24hrs I needed to be admitted for IVs. Driving to walk was always horrendous, and my sickness and nausea appeared to happen at any and all times of day. Happily, since about 16 weeks this has gone completely! Reflux is an issue, but what’s new. Also happy to report that since about 16/17 weeks my joints have only hurt and dislocated a regular amount, a pre-pregnancy amount, and I am so so grateful. I have some pelvic/hip and coccyx pain but nothing that isn’t manageable with paracetamol and hot water bottles. I’ve even been able to reduce my gabapentin dose a little in the past few weeks, which is a massive achievement! I’m only as tired as I was pre-pregnancy (naps are a must, always), and I feel really good in myself.
Other struggles: Admittedly, I have always been very body-conscious and struggled with food since I was aorund 14 years old.... so from about 10 weeks to nearly 20 weeks I really really struggled with the physical changes my body was going through. I didn’t look obviously pregnant, but I fit my trousers differently, and became very hateful of the paunch that was developing and how little control I had over any of it. I continued to look after myself, but I hated looking in a mirror or being touched. It was a real knock for my self-esteem. Thankfully, since I belly has morphed into a small but more obvious bump, and I have been able to feel Baby B squirm and thump at times, and feel how solid my stomach is - it has become much much more enjoyable! I hate not being able to wear 50% of my clothes, and will soon to be unable to fit into my Mum’s stretchy jeggings either - but I have a few maternity bits of clothing from Charles, and I don’t loathe my shape now that it is getting more and more pregnant-looking and less just like I’ve over-indulged!
I’ve battled with wondering if something awful will happen; sadly almost all of my experience with babies has been where I work at the hospice, and although not all babies have the same outcome there - it is always fraught with challenges and very emotional for new parents. This has settled a lot but I think it is the nature of working in a children’s hospice and not having had my own child yet. I’m feeling less worried, and it certainly isn’t stopping me enjoying it, I’m just all too aware of what can happen. I’m a lot less neurotic than I thought I would be, thankfully!
Mostly now, I am excited.
I enjoy feeling Baby B move around.
I look forward to finding out whether Baby B is a boy or a child when it graces us with its presence.
I’m even looking forward to learning how little I know! For the stresses, for the change to my life, for not being able to sleep for 10+ hours solid.
23 weeks, and 3 days pregnant,
We have a our first bit of baby equipment - a pram! A beautiful Silvercross Wayfairer. It arrived yesterday and makes everything even more real!
We also have our first little Baby Shoes which were a christmas present from Charles’s parents.
Only a few months to go until little Baby Butters comes along. Unbelievable excitement.
1 note
·
View note
Text
My Hypermobile Ehlers Danlos Syndrome.
May has nearly ended, making it the last day of Ehlers Danlos Syndrome Awareness month (although, let’s be honest, the only thing on anybody’s mind right now is Coronavirus!) - so here is my two cents worth, my update of how it is affecting me currently!
First to report, if I compare myself to a year ago, it is really easy to see how far I have come. Of course, my condition will always be there and affects me still, but not quite as consistently bad as it was this time last year.
This time last year I wouldn’t go anywhere without my knee and ankle supports, my hand splints, my neck wrap that heats up, to help with pain, my TENs machine, pain killers. Last summer I went on holiday with my best friend and, although I LOVED the holiday, I could barely eat due to such severe reflux and nausea, and even on nights out I was wearing various supports/splints.
Now, in 2020 - my symptoms appear to go in phases more than they did last year. Last year my symptoms were consistently present, every day I had pain, dizziness and extreme fatigue that led me to miss most afternoons, I had dislocations and subluxations most days, I had many unexplained injuries, and struggled with food most days. Thankfully this is no longer current!
Now, I have some days with little to no pain, that was unheard of last year!
Often, when I do have pain, it is manageable with ibuprofen and paracetamol most of the time (as well as my regular gabapentin and amitriptyline). Awesome!
Usually when I have pain, it is in one or two joints at a time only (the joints remain my thumbs, wrists, elbows, shoulders, neck, jaw, knees and hips) as opposed to multiple, which makes it easier to get on with the day.
I no longer carry all my different supports and splints with me, only my thumb support! I no longer wear kinesiology tape on a regular basis, I rarely need my TENs machine or hot water bottle for pain management, and I rarely have full dislocations at the moment (although my thumb does still sublux daily).
i do still really struggle with the chronic debilitating fatigue caused by pain, although my pain tends to be lower level than previously, it is still present on the vast majority of days. I need sleep, and often, such as following meals, sleep takes me for many hours even when I have other things I need to be doing. I still suffer with dizziness, but generally there is a more predictable pattern; that week every month, and when it is hot outside. I still suffer with reflux, that is the only point that has not eased at all, and I hate it as my appetite remains minuscule and I wish I could enjoy food more without worrying about the frequent mini-vomits after.
I think in the past year I have learned a lot more about what affects my symptoms on a daily basis. Although I will always have some base level of pain, and I will always have fluctuating symptoms that make some days easy and somedays incredibly difficult, I have definitely noticed that when my anxiety is high (thanks, coronavirus) that my pain also increases, and cannot and does not reduce again until I am more stress-free and less tense. I have noticed how big of an impact my shift pattern can have on my pain and chronic fatigue, and thankfully new recommendations have come in from Occupational Health so that will help, and I have noticed how much certain actions (holding my tooth brush too tightly, writing a lot, giving blended diets via gastrostomies) causes increased subluxations and dislocations, so I can try to reduce how often I do these, or change my technique. I have noticed how much over-doing it one day has an impact the following few days - although I still need to work at not doing this, or choosing my moments more wisely.
I am learning about chronic pain to better understand my condition, and I am learning about self-compassion to help me be kinder to myself when my symptoms flare (because I can be very cruel to myself). I am doing my physiotherapy exercises more. I am resting when I need it and trying not to beat myself up about it. I am trying to better manage my emotional wellbeing, to try to avoid the inevitable escalation of symptoms when I do become anxious, stressed or have low mood.
Now my symptoms appear to fluctuate in phases more than they did last year; a few days to a week of bad symptoms and then they ease again usually, I find I am more positive about it and less fixated on pain or dislocations, because I know it will ease again. That has made a HUGE different to how I cope.
Hypermobile Ehlers Danlos Syndrome will always affect my daily life, but as opposed to last year, I know longer feel like it is consistently getting worse - in fact, I feel I understand it and have a little more control of my symptom management through my own actions and my own emotional wellbeing. This is a massive relief.
#hypermobile ehlers danlos syndrome#HEDS#EDS#ehlers danlos syndrome#EDS awareness#chronic pain#chronic fatigue
2 notes
·
View notes
Text
What do I do? Where do I work?
Figure it out.
I work at a service that everybody wishes they didnt need. The first visits often scary. The last visits often when the worst has happened.
What is the worst? The worst is when their child/sibling/grandchild/nephew or niece or friend has died.
I work at a service that this week (written a while ago): Hosted a BBC radio show, live from the play room.
A service where some guests had a jacuzzi everyday. A service with live music on some days. And a visit from a Golden Retriever on another. A service that had a boat trip recently, and a big event where people ran through coloured bubbles, and last year we had our own fireworks display!
A service full of singing, laughter, great food, baking.
A service full of support, sibling support, play teams, social work, family support, medical support, bereavement support. Then of course, outreach support and the support of the nurses and carers on the care team each day.
A team which would not function without fundraisers, who get creative, without donations from people who pay attention we would not survive as a service.
You've probably figured it out now, but just in case you haven't, here are a few things I've done in the year I've worked there:
- Supported and splashed with many children in the jacuzzi, and with families.
- Eaten many meals with families
- Given many children blended diets via their gastrostomy
- Been in a lot of fancy dress
- Given a lot of medications
- Completed a lot of care plans with families
- Supported a crying parent
- Supported a seizing child
- Done a lot of singing
- Watched a tonne of Peppa pig
- Suctioned the airways of children to help them breathe
- Cleaned a lot of bums
- Cried
- Read a lot of stories
- Liased with funeral directors and coroners
- Liased with schools
- Met Jack Whitehall when he visited
- Quickly put oxygen on a child losing colour
- Dressed as one of Santas helpers
- Seen many children after they have died.
- Dressed a few children after they have died.
- Been to the cinema with patients and staff
- Had a monkey on my shoulder at work once
- Met a penguin at work once
- Read a child the last story they ever heard
- Spent my every moment trying to make a childs last days pain free
- Lots of visits to the ice cream parlour
- Lots of painting
- Been invited to many childrens funerals
- Been chased by children with fake swords
- Been a listening ear for parents at whatever time, in person or on the phone
- learnt about many conditions and syndromes
- and diseases and cancers
- Met some incredibly resilient people (staff, patients and families)
- hugged parents just after their child has died.
- prepared aunts and uncles before they seen their loved one, after they have died.
- had many really hard discussions
- and laughed, lots.
- smiled, lots.
More about the service again?
We are a service that our families use to cope, to catch up on sleep, to step back and just be mum and dad (not also a medic, nurse, physio, carer etc), a service that allows parents to put down a few of their worries and responsibilities for a while and relax. A service that enables parents to get a break so they can keep caring for their child, with very complex health needs, when they go home. A service that allows teenagers with complex health to have a break from parents also, a little bit more independence if that's what they want, and a step away where people know their needs. Once you use our services, we are somewhere to contact when your child is sick and you need advice, a place that understands the complexities of your situation, a place here to help wherever we can.
A place to fall if your child has a terminal illness. A place where people are gathered to care for your child, and your family.
Have you guessed?
I am a nurse at a children's hospice.
Usually, people get some of what I do right, because hospice connitates death - and yes, we do have children who come to stay with us as they die, that is a huge part of what we do... but we also support many families who have children that are not actively dying, but have a condition or disease that means they are expected to die before they turn 19. A child with complex needs, a degenerative condition, a progressive illness, or high risk because of episodes such a seizures, respiratory arrest, cardiac disorders, muscular dystrophy, brain damage etc etc. We have children who have fallen victim to a brain tumour that was too aggressive to fix. Children who are dying of a number of cancers, cardiac disorders, metabolic conditions and many more I am yet to meet and care for.
We care for them. We care for their families. We try to take some weight off the shoulders of families who always have to do more, often whose whole lives are about this sick child, whose every day centres around their care needs. When a child dies, we try to support them to have it in the way they and their family would prefer. The most comforting way, whilst managing distressing symptoms the child may have.
It is both utterly joyous and heart breaking. I love working there. It's the biggest privilege in the world.
But I wish, above anything, that people understood more of what a children's hospice is about, people can understand that my job is sad, yes, but it is also so so full of love and joy and happiness. I wish people understood this, not for me, but for the families who are afraid to use us, but could hugely benefit from it. Families who are exhausted, who spend their lives wrapped in medical supplies and stress, who could really do with meeting other families in a similar position, with staff who understand and doctors on hand to always give advice and to teach parents how to cope with new symptoms. Parents who don't yet realise that we support in the home as well as in the hospice, and that continues when a child is actively dying if a family wants it to be facilitated at home.
A children's hospice, like Helen and Douglas House, does so much more than people are aware.
I love my job, its ever changing but always meaningful and I hope people can come to understand and support this vast service more.
8 notes
·
View notes
Text
Advocacy and annual health checks are vital.
Let’s begin this post with a boring but highly relevant title! This leads on to what is usually a fairly rambling post, but reaching the (title) point towards the end.
My main focus of this post is the unbelievably weird and gentle and kind man that is my baby brother.

There we are, being adorable.
Charlie is 21. He works in Asda full time and has done for a couple of years now (if he reads this, I’m sure I will be corrected to exactly how many months), he’s the tallest of the family at nearly a foot taller than me. He is obsessed with musicals, doctor who, the stock market comparisons for different food stores, blue-link wikipedia binges, and of course - experiences in retail. He also loves hugs. And dogs!
Also, for those who don’t know him (skip if you do), he has autism and learning disabilities. He’s also had hypotonia (low muscle tone) since he was a baby, so his posture continues to be poor and he wears splints on his legs and super-cool (and MASSIVE) pedro boots to support his weak muscles. He has (very well managed, currently) issues with obsessive compulsive disorder and anxiety and (the main focus of this post), he was recently diagnosed with ulcerative colitis.
So, let’s talk about this last point because it leads onto THE point.
Ulcerative colitis is one of the inflammatory bowel diseases where your body has a reaction to normal bacteria, and believes it is foreign and starts fighting it, an autoimmune condition, causes inflammation and ulcers along the rectum/colon and upwards. It is life-long, and can go through long periods of not affecting daily life until a big flare up will (unless you’re Charlie), put people with UC in agony, spending most of their days on the toilet, often anaemic due to bleeding inside the colon, and sometimes results in hospital admissions for anaemia and dehydration - but for people diagnosed with UC results in a huge increase of medications during a flare up to get on top of it, limited social life or work during that period until there is a handle on it again.
Now, for Charlie’s and your sake I won’t go into the details of his bowels - but I will tell you that symptoms for this had began probably as far back as last May. Charlie had been excreting blood ever since, and spent a good portion of his day in the toilet. To begin with, it wasn’t that awful or that obvious - and we, his family, did not know. Fast forward to December 2018, and we are all sufficiently concerned about it. Mum had taken him to the GP, only to be fobbed off that it was another issue of constipation and ‘probably’ haemorrhoids (obviously, they did not check), just take extra laxatives. Charlie was spending a huge amount of his work time in the toilet by this stage, and his employers are amazing with him but it’s not ideal, he has also had embarrassing episodes occasionally, and we - his family - were all too aware of the blood that continued leaving him due to the patterns around the toilet (TMI?). So, when my sister came home after christmas we started a bowel chart for him - and the truth was outed, many times he was visiting the toilet, it was just blood and nothing else. We also got a true picture of how many times a day. Then, I took him back to the GP, a summary of the bowel charts in hand and decided on not leaving until further testing had been ordered. It was, and then a couple of weeks later I attended the colonoscopy with him where - yes, it was confirmed, that our poor boy has ulcers extensively, and that was the cause of the bleeding (another concern was obviously the C-bomb), treatment was to be commenced immediately. Now Charlie will be on life-long medication and management, but a lot of that will be done by us his family. He can take the tablets, sure, but he will not notice or be particularly bothered for another flare up so we have to keep on top of that and manage any other complications. Mum has taken him to follow up appointments at the IBD clinic, and thankfully the GP are now taking it seriously.
But this leads me onto my point.
Adults with learning disabilities qualify for annual health checks, and they are SO SO important. But the how and when and who with is important too. Charlie is a very able man, he’s really intelligent and he works - but without us (his family) being advocates for him, we still would not be at this stage. People with learning disabilities need their GPs to advocate for them, but this requires an understanding of the processing abilities of that individual and - we all know - GPs do not have time. Charlie comes across so able, so when healthcare professionals ask him questions about his bowels or other health aspects, he will answer the question - but that doesn’t mean he’s understanding and often the point is missed. Abby (my sister), when discussing the issues with him broke it down into words and phrases charlie understood, so we could get a proper picture of what was happening, and when I took Charlie to the doctors and for his colonoscopy I spent the time interpreting to Charlie what the doctors meant, and vice versa, and re-wording questions to Charlie so he could give the true answer. Sometimes that is all being an advocate involves. Without my mum, my sister and I doing this, we still probably wouldn’t have gotten any further. Charlie does not feel pain, part of his autism (and no, all people with autism are not the same and some feel pain acutely), but that meant he wasn’t giving standard answers or putting the urgency on that most people with this condition would - he was just getting on with daily life.
This is a problem, not just for Charlie, but for people with a huge range of disabilities and learning disabilities - and it’s vital those who know them become advocates. An annual health check is great, but without an advocate for those who need it, huge things can still get missed - and a reminder that people with learning disabilities have a life-expectancy 20 years shorter than those without - and a big part of this comes down to their health needs not being met. If you are a carer, a family member, a friend, a nurse, a doctor, an OT, etc etc - any person close to those with learning disabilities, with a professional responsibility and without, just check that they have a good advocate, and talk to them and their advocate about concerns so that they are properly treated, promptly - and if they don’t have an advocate, it is our shared responsibility to ensure somebody steps up to the plate!
Thanks for coming on this ramble with me, it’d probably be more concise... but I must get ready for work.
1 note
·
View note
Photo



A reminder to myself and others: It’s important to let yourself rest when you need it 💙
54K notes
·
View notes
Text
My dysfunctional family (but not in the way you think)
I’ve been a qualified nurse now for three and a half years, and had three years of training prior to that. A lot of learning has been done in that time, and my current job provides me with the opportunity to constantly be learning new things. However, all of this training and this nursing does not equate all of the medical knowledge I have gained over the years.
What has? My dysfunctional family.
As a phrase usually used to describe families with difficult circumstances, and difficult relationships with one another, but I am using it very literally, as each of us within the family have ‘functions’ that are failing us, and I mean medical ones (psychological and physical, both long-term and temporary).
Let’s list some shall we?
* Autism
* Attention deficit hyperactive disorder (ADHD)
* Ehlers Danlos Syndrome (EDS hypermobile and classical)
* Hypotonia
* Benine tremor
* Irritable bowel syndrome (IBS)
* Postural orthostatic tachycardia (POTs)
* Ulcerative colitis
* Idiopathic thrombocytopenia
* Raynauds
* Anorexia
* Obsessive compulsive disorder (OCD)
* Ataxia
* Migraines
* Anaemia
* Chronic constipation
* Gastroparesis
* Anxiety
* Depression
* Relapsing remitting multiple sclerosis (MS)
* Ankylosing spondylitis
* Atrial tachycardia
* Transient Ischemic Attack (TIA)
* Glandular Fever
* Hernias
* Prolapses
* Dislocations
* Blood poisoning
* Appendicitis
* Diverticulitis
* Gastroesophageal Reflux Disease (GERD)
* Mast Cell Activation syndrome (MCAs)
Then we have some additions from our partners that I’ve learned lots more about:
* Type 1 diabetes
* Crohns disease
I consider, as a family, us to be a reasonably healthy bunch - we look healthy, we look after ourselves, but yet we have always been plagued by different illnesses that need managing, some of which will always need managing, and that’s unfortunate.
If we take a positive from this: I have learned a HUGE amount of medical knowledge, of different conditions and of the functions of the anatomy, that I simply would not have learned if it wasn’t through our family and our bodies functioning poorly. This knowledge I can use in my everyday working life, and build on, and because it’s relevant to my family - i’ll remember it better!
If I could click my fingers and make many of these issues go away, I would, but as I can’t, I may as well use this knowledge to my advantage!
Thank you, to my dysfunctional family!
0 notes
Text
She keeps losing her pen.
She keeps losing her pen.
Does she know her glasses are there, on her head?
Can she function without a list?
Oh, there she goes again
She forgot something, or misplaced it.
Again.
It seems other people are in charge,
they keep track of her
What does she keep track of?
Well...
She remembers every child, every patient,
Not just their names, and faces and diagnoses.
Inside that brain of hers,
which cannot keep track of her specs, pen or badge,
she has an encyclopedia of everything
everything that matters.
Your child.
Name and face is only the beginning,
Diagnoses, allergies, medications, emergency plans, care plans, feed routines - a huge amount of information.
Safely stored in between the ears,
alongside the information of 100 of more other patients.
But it’s not just that, she also remembers;
Your child’s favourite foods, stories, music, hobbies, habits, how to soothe them, how to make them laugh, how to ease their pain, how to wind down, how to distract, how to gain trust. Pets, siblings - and, of course, you!
As a care team we don’t get time to read the whole history before you arrive (care plans - yes we do!), so when we ask about your holiday, pets, work, school, and other family members - it’s because we remember, not because we read it!
She, who never has a pen,
also has a plan in that brain of hers for any eventuality the
ring-ring-ring
of that phone could bring.
For any time a buzzer goes off.
A constant awareness of all other staff at hand, and her own little track of their special skills, relationships and wellbeing.
She, who always loses (”misplaces”) her glasses,
she contains all of that, and is also always looking ahead,
planning,
for how to best support your child and family, and her team,
both for that admission and future ongoing support.
For fun activities, but also with grief, continuing care challenges, meetings, reviews, service access.
It’s all on her agenda, and it won’t be missed.
So, when she’s “misplaced” her glasses,
and lost another pen
Just hand her another pen, gently point out the glasses on her head.
Her brain contains all of the necessary information, and she does her job so brilliantly - is it any surprise those things don’t stick?
0 notes
Text
Pacing: Me, myself, and my EDS.
I usually use this blog to talk about specifically nursing topics, but today I’m talking about myself, and in a way, what I need to do to keep doing what I love, and that is something I am not very good at: Pacing.
I have Ehlers Danlos Syndrome.
(But no, I do not yet know what type as I am awaiting full diagnostic screening.)
My lovely sister has Ehlers Danlos Syndrome, classic type, and has been diagnosed for some time now. She’s suffered no end with her dislocations, her dizziness, her reflux and funky heart rate and poor healing etc etc etc, but up until around a year ago I suffered very little pain (obviously, seeing her in pain will always suck, but I always considered myself the luckier one). When I did, I rested and managed. I’ve had physiotherapy for various parts of me over the years but it’s always been a short term treatment, I tried to maintain strength for a long time, I’ve always sat in funky positions and been hypermobile without pain associated and I had only dislocated my shoulders (and from last year, my knuckles)..... until this past year.
This past year has been a huge learning curve for me, and I have some learning points now, but I must admit I haven’t quite put them into action.
So, a few things I struggle with now that I previously managed:
- Hip subluxations (mostly my left side, although my right side does it too, and so frequently I could not count how many times a day).
- Dislocation of my fingers and thumbs, at random
- Dislocating/subluxing my shoulders, in my sleep.
- Pain and weakness at the base of my neck, onto my spine. (Suspected cranio-cervical instability, by me, discussed with Doc, but totally unconfirmed)
- Dizziness associated with the neck pain (HUGE problem if driving for prolonged periods or sat doing training/looking at powerpoints/cinema)
- Dizziness upon standing up (*sung in my family as ‘hello, darkness, my old friend’ because it’s very common to us) - often causing me to then lower myself back to the ground/chair until I can see enough to try again
- Constant headaches
- Visual difficulty, difficult to explain but like an out of focus camera, massively worse when my pain is high that day or I’m extremely tired
- Reflux (very regular, swallowing down mini-vomits has become a new normal for me)
- Very poor healing of cuts etc
- Oh the bruises, constant unexplainable bruising
- NO POO aka constipation, and let’s be honest - nobody likes to be full of shit.
- Difficulties digesting, feeling totally overwhelmingly full at sometimes small bits of food (then bring on the regurgitation).
- Ankles and knees rolling inwards, and bending outwards in totally unnatural ways, and it hurts.
- EVERYTHING clunks and has to click back into a comfortable place on a position change.
- I sleep a lot, but I never feel rested.
However my main overall points:
- I hurt. I really hurt. I rarely have a day or a few hours without pain, if I do I usually want to make the most of it - which then undoubtably leaves me in pain. For people who don’t have constant chronic pain, it’s difficult to explain but it is utterly, totally exhausting. Under everything, all day, I’m fighting pain, and balancing it with what I need to do, and also fighting to avoid subluxations and dizziness and my balance issues. And with how pain killers will or won’t enable me to continue with my day.
- I am EXHAUSTED. All the time. I need 10 hours of sleep a night just to keep going, and I rarely manage more than 6. I work shifts etc but I really don’t think that’s what causes it, it’s all the time fighting unstable joints and continuing on top of pain - those whirring away underneath, fighting my body, it’s exhausting. And I really struggle to stay conscious. When I work 07:30-15:00, I NEED a 2+ hour nap or more when I get home just to have the energy to eat a meal.
Management at the moment:
- Omeprazole
- Codeine
- Naproxen (or ibruprofen if it’s not too bad)
- Paracetamol
- Peptobismal// Rennie’s
- Lots of fluids and salt in my diet to increase my blood pressure and try to reduce dizziness (not working)
- SLEEP
- Meals planned in, larger ones when I’m with people I’m comfortable to vomit around// not at work.
- Osteopathy
- Physiotherapy (I’m in waiting actually, not yet started)
- CBT privately
- Knee supports
- Ankle supports
and my favourite
- Hot water bottles
- Heat bags (my favourite is a Sloth called Rufus)
- Hot baths
(Not a cure but really does help).
And thankfully I have a hugely supportive family and boyfriend and friends, who accept my need for rest, who understand my pain as much as they can (sadly, Abby and Rosie have it too, so get it way more than I wish they understood), and who help a lot.
However, I need to do something to help myself: I need to pace myself, and specifically, I’m talking about at work.
I work in a children’s hospice, and I LOVE my job. Truly, I do. I love putting everything I have into a shift, and I find myself doing it all the time. I’m energetic, I’m a team player and I am constantly learning (all of which uses my energy). I often get given the very energetic mobile children to look after, because I can enjoy it and because I usually keep up (even though the after effects are bad). I work nights, and different day shifts. I work full time. Sometimes it isn’t physically hard (better days for me), but it is always mentally exhausting and emotionally taxing at times.
My problem is, I’m putting ALL of my energies into work - and I have none left for me, for my family, for my boyfriend, for my friends -- and it isn’t healthy.
Then, I feel guilty for not having energy left over for these other parts of my life. I travel to my boyfriend (and him to me) a lot, to my Uni friends sometimes, to Scotland and here and there. Often living out of a bag, because I feel guilty if I don’t manage to do these things.
I have this terrible fear of missing out, and of letting people down. The two as a combination are terribly destructive to pacing myself: In my head, if I pace myself and don’t do the absolute maximum for everyone around me, I’m letting them down, if I do pace myself I might be missing out on experiences, and might be causing other people to miss out too - and if I don’t pace myself, my pain and fatigue will ensure I miss out anyway.
All round, it’s shit.
And I am very good at asking for help when it comes to learning at work, if I don’t know something, if I’m unsure I will always ask - but if it’s due to my body being incapable, or too exhausted to do something, I won’t. It goes on the back burner. I’ll cope, i’ll say, I’ll be fine.
I work with incredibly compassionate people, understanding people, and it is no fault of theirs that I push myself too far. I have talked to some about my EDS, and have received nothing but kindness.
But I do not get kindness from myself.
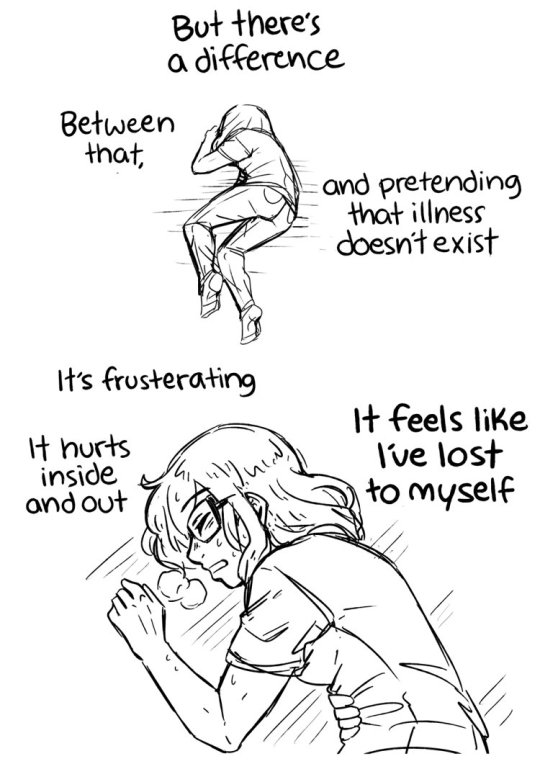
And when something is an ‘invisible illness’ it’s very easy to convince yourself it’s in your head, and I constantly rebuke myself for being lazy, bone idle, a slob - and have to be told by others that I am not those things, but I have a chronic condition and pain and exhaustion feed each other if the aren’t managed. It’s a constant battle between feeling guilty, and like a fraud and between being so overcome by pain and exhaustion I can’t even feel.
But I HATE it, and I feel it’s all still fairly new to me. A year ago these symptoms became worse, but even 6 months back they had nothing on the pain I experience now. And I am not ready. I don’t want it, and I don’t know how to stop it.
When I’m at work, I don’t pace myself, because I’m too busy being totally in denial.
When I’m at home, I’m so wracked with guilt over not doing nice things with everyone or feeling lazy because I’m exhausted, that I don’t actually give myself a break.
So, after a long winded post about all of this, my message to myself is:
LEARN TO PACE YOURSELF
Give yourself a break
Talk to the kind people around you so you can do the best job possible at work without totally exhausting yourself and causing more pain
Allow yourself to rest
Look after your body as much as possible
There’s no shame in having a chronic illness, so stop beating yourself up.
For those who are only just learning about my issues with this, I leave you a few pictures explaining EDS a little:

#EDS#Ehlers danlos syndrome#spoonie#zebra#zebra warrior#hypermobility#pain#chronic pain#chronic fatigue
4 notes
·
View notes
Text
Douglas Days
Somehow June has arrived and the very real closure of Douglas House is fast approaching. Two months left, two months of caring, of amazing relationships, of laughter - but also, this time two months of goodbyes, apologies and tears - all of which are shared amongst the care team and the families and young adults who benefit from this service.
Back in January when we were told the news that Douglas House would be shutting its doors, and the care team and others of 60 strong would be made redundant, it was devastating, but there was also a faint glimmer of hope that something could be done to prevent this tragedy - but now, that has faded. Families who have another option (which I must say, are not the majority), have been signposted elsewhere, to begin the long referral process once more and have to build those trusting relationships up from scratch, and those that do not meet the catchment area of a similar service (there are only a few in the country) are left with nothing. No respite care, no hospice care, none of these staff who have known them so well over the past decade and could continue to deliver care exactly as that person would want it even as they deteriorate. Staff have all had their final dates, known their redundancy packages and some have got jobs elsewhere (a few still within Helen and Douglas House), some are still looking - and nobody wants any of it to be happening.
I guess I’m writing this because I feel the need to say what a privilege it has been the past 7 months to be part of this team, and to work with these young adults. I have never met such a compassionate, caring and experienced care team and I think it’ll take the rest of my career to find another. But also, the young adults who use this service, who have made me laugh and cry and whom in such a short time I’ve managed to form great relationships with (mention that most of our care team have been at Douglas house since the beginning or around 10 years, and have built the strongest relationships in that time with our patients). This job has taught me so so much, especially about the small things that matter in day to day life of somebody who is affected by a progressive debilitating condition. It has bought to my attention so many things to consider every single time I work with a patient, that if it hadn’t been for these experienced carers and our incredible parents and patients, I would never have even thought about.
It takes an extremely special kind of person to have worked at a Young Adults hospice for as long as most of our care team have. Although on a day to day basis things are usually pleasant, fun and uplifting, there is always that underlying knowledge that next time you see that individual they may not be capable of doing the things they can now, the knowledge that a few years ago that person could walk and now they can’t move their arms never mind their legs, or now they are ventilated full time. It’s the knowledge that every day really does count, that an infection could have devastating effects on each and every one of our patients, that this time they may seem ok, but it could also be the last time. Our care team have lost so many people over the time Douglas House has been open, and they have given the most dignified deaths, but each person gets etched into a memory, and they don’t fade. That’s why I think my care team are utterly incredible, it maybe a fun job on a day to day basis but it has a huge emotional toll, and now the constant goodbyes are even harder to take, and our carers are to used to putting others first that I think many of them are actually doing so now, despite it being detrimental to themselves.
Douglas House is a lifeline for our young adults who just need a break from the routine of having to do everything at certain times because that’s when their home carers work, or that is when fits in with their families lives, to not being able to go out and do normal things for their age - at Douglas House they can, they can stay in bed late if they want, stay up late if they want, go shopping and to the pub or cinema or on trips when they want, and not have to fit their meals/ toilet times/ activities into the convenience of their carers etc. They get to meet people with similar (and vastly different equally permanent) conditions, and just feel normal. It’s a holiday where most of them can’t go anywhere else for a break because of all the medical equipment they need.
Douglas House is a lifeline for the families of our guests, who don’t often get a break at home, often they are the 2nd carer needed for all turns/changing/hoisting or any manual handling (because there isn’t enough money for decent care packages anymore), they spend all of their days arranging appointments, ordering medications and feeds and arranging service checks for equipment, and always having that undercurrent of worry. They are often people who expected their child/sibling to die a long time ago, adjusted their life expectations to that and dedicated every moment to their child - but due to the medical miracles that many of our guests are - are still doing that now, when their child is now an adult. They’ve experienced the emotions of near-death over and over, been through surgeries, diagnosis, the progression of diseases and their child/sibling losing functions they previously had, and adjusting, constantly adjusting. When their family member is with us at Douglas House, they get a break. Time to just be themselves, to see friends, to go abroad- but often, time to finally get some rest that they really truly need.
However, Douglas House isn’t just the spectacular service provided, it’s also the memories held within that building. For our young adults, it’s not just the trips they have been out on, and the activities and games nights and parties and quizzes - often it’s memories of serious conversations they have had to have, of friendships they have made - or more potently, of friends they have lost. Douglas house is often they last place they have seen these friends, whom they have formed such an immense bond with, before they have passed away. Our young adults don’t just experience the hardship of what they are going through, but also great loss of spectacular friends, and this environment housed so many of those happy memories.
It is the same for families, memories of their child or sibling being happy, being cared for by people who adored them and met their needs, getting to be an adult and seeing them bloom into the person their condition often stops them being. Memories of them actually getting some rest, of being catered for, of being able to have a meal at the dining table with their child or young person whilst somebody else feeds them - so for once they can actually eat at the same time. Douglas house has given young adults their last big wishes - a wedding was even hosted there once for a couple in their last few days together! Many families also have memories of their child in our Starfish room after they have passed away, seeing them without all of their equipment, at peace, but also knowing their journey has come to an end. The last memories, the last breaths of their children taken inside that building.
It’s not just a service that’s so special, it’s everything that has happened within those walls since 2004 when Douglas House opened as the world’s first young adults hospice.
There is so much more I can say, but this post seems to have gone on forever as it is so I’ll leave it there.
Douglas House is irreplaceable, it is a damn shame, but it’s also the hugest privilege to have had the chance to work here with these incredible people for the past 7 months and the next 2 months. I will always be grateful.
(Excuse any typos, not had time to re-read yet)
#hospice#helen and douglas house#douglas house#young adults hospice#duchennes muscular dystrophy#respite care
0 notes
Text
The end of a place and service so truly special.
Just under two months ago I started my new job at Douglas House, part of the more known Helen and Douglas House.
For those who don’t know, Helen House provides specialist palliative care for children ages 0-18, for children with terminal conditions and life-limiting disabilities. It offers hospice care and respite care for those who have those needs. It also has specialists therapists working within it to provide bereavement support to families, sibling support to those brothers and sisters who also have to face a lot, along with play therapists and music therapists and an outreach team and lots of other bits and bobs. A beautiful building purpose built for catering to children with these complex needs.
Douglas house is the same, but it is built with young adults in mind and provides a vital service for young adults aged 16-35 who have terminal illnesses and life limiting conditions/disabilities, and likewise offers well-needed respite care and hospice care for adults who often have nowhere else to turn to for these services. For hospice care, most young adults have very few options and usually dying in a hospital or in a hospice full of elderly people are the only other options, and (I am absolutely not saying the care there is not great, because I’m sure it is), that simply does not offer these young adults the best space for them to have their care needs met and still manage to enjoy themselves in the final days/weeks/months of their lives. As for people with life limiting disabilities, it offers a space to just be themselves for a while, whether they are cared for by carers or their family members, at Douglas house they can just be themselves and we will take care of the rest. Many treat it as a holiday break, and they get to do things they want during that week - whether it is simply play on the xbox and meet people with similar needs, or go to the cinema or a pub or just the ease of being able to stay in a building purpose built for them. The simple pleasures of actually being able to have a bath! Because the bath is made for people who may need hoisting into it, and has the space to do so. It’s astounding how many of our young adults can’t even have a bath at home. Our young adults get to relax, talk to others, use the sensory room or art room or computers or organise trips out - whilst knowing all their needs are taken care of, a weight off their shoulders. And for those young adults who have profound learning disabiltiies, this service is often more respite for family members who on a normal day have to deliver all of this care themselves, and often have a lot going on in their own lives - they get a well-needed break whilst knowing their child/sibling is safely in our care whilst they can meet friends, go on holiday or (most often), just get some sleep whilst not worrying. Douglas house is a lovely environment where young adults with such complex needs get to relax, often make friends with others who share similar experiences, build great relationships with staff and other young adults who understand their struggles and make all choices about their care and what they want to do. Douglas house provides the freedom and support to do that - and it supports these young adults through times of great change for their bodies as their conditions progress, and all the way through until the end of their lives, and then continues to support families with their bereavement and hold rememberance services for those that have passed away.
Sorry, I didn’t mean to get carried away, but it really is essential that people actually know what a vital and treasured service Douglas house is. Our guests know, many have been coming for many many years (some even a decade), many travel hours and hours to get to us. Families of guests who come certainly know, and the service helps them a lot. And our staff, they know. I’ve never seen a more caring team. Every ounce of love is put into this place, and many staff members (loads of them!) have been here nearly a decade or over, and that speaks volumes about any work envionrment.
Now to get onto the difficult bit: Douglas House is being shut down, and it has (potentially, if not sooner) until the end of July to continue to provide this incredible service. It’s a true tragedy. Apparently, this decision had to be made because funds are too short to continue running both, and if drastic changes were not made Helen house would cease to exist in a few years too. Reasons do not make it any less devastating for our guests and families.
60 people are going to be made redundant, although we don’t know who these people are yet - as Douglas house is closing - we can be sure at least a majority of the 40 care team members we have will be included in that.
Obviously, after starting this job less than two months ago and absolutely loving it, it is disappointing to find out I won’t have it any more in a few short months, or sooner. And as I said, many of our staff have worked here for a decade and will also be losing their jobs.
But that’s not the true tragedy, and when we found out at the beginning of the week, there was an outcry of tears and a lot of anger - but it wasn’t for us, it was for our guests and families. There are very very few services for young adults with this level of need, and they are few and far between - proven by the fact we have people travelling two hours or more just to get to us. Many of them will have nowhere to go, no more respite for them or their families (and often these short breaks really do keep a family surviving and coping), no more of this specialist and specific support for young adults as they approach the end of their lives - and with teams of carers and nurses and doctors who have built strong, trusting relationships with them over the years, who know them so well that even as their needs and abilities change (such as ability to communicate), their personality can still shine through the care given. This is an area of healthcare that has been missing for a long time, and Douglas house provided this, and will be gone. What about our guests?
If, when I had started, I had been told it was just for 6 months - I still would have chosen to work here, and I can say that with confidence. I have learnt a lot, and also met the most incredible people (in the care team, volunteers, guests and families).
However, my biggest message here it to ask for support - Helen and Douglas house needs donations, it may be too late for Douglas house (although I cannot dim that glimmer of hope), but it’s not for Helen house yet - and Helen House will need a lot of support if it is going to continue on for a long time providing that specialist palliative care. People only die once, and Helen and Douglas house both enable people to do it in a way that suits them, that gives them choices and dignity and a supportive environment for them and their families. It’s importance cannot be underestimated.
Donate at www.helenanddouglas.org.uk/support-us/donate/
#disabilities#charity#nursing#hospice#helen and douglas#douglas house#young adults#respite#duchennes muscular dystrophy
3 notes
·
View notes
Text
You don’t have to earn your right to exist.
So, to begin this post I’m going to write out my current situation.
For the past 4 months I have been unemployed, although for the past month I have had guarantee of a job I will be starting soon - just waiting for all the checks and references to clear. I have been travelling around the United States and Canada for two months with my Mum, and later returned to New York with my younger brother. I’ve also moved from my flat on my own and back into my family home. I’ve been camping with Special Kids in the UK and I’ve been to visit friends. However, for the majority of the last month (aside from the 4 days I was in New York), I have been largely doing a whole heap of nothing, and boy have I made myself feel bad about it.
I’m pointless. I’m useless. I’m a waste of space. I’m worthless. I’m stupid. I’m lazy. There’s just a few of the thoughts that go round my head constantly each day as I sit about (crocheting, knitting, reading), waiting for my job to start.
One other thing I failed to mention, I’m also broke. Completely broke. Obviously, this is to be expected after four months off work including two months abroad flying from state to state and trying to do as many things as possible, but I feel awful about that too - and Christmas approaching and my entire family being born in January does not ease the situation I have found myself in.
I’m boring. I’m isolated. I’m penniless. I’m a drain. I’m a burden. I’m a disappointment. A few more words for how I’m thinking about myself as I sit about each day.
So, there’s going to be no surprise that I’ve been pretty down on myself. Needless to go into my mental health in a public space, but let’s just say I’m not making it any better for myself.
But then I was made to think about it a different way.
I was asked “if this was one of your patients, sat around all day, would you think they were pointless?” Of course I wouldn’t. “And why not?” Because they’re a person, they’re important no matter what.
I was asked “if your brother or boyfriend or friend had no money, would you think they were a boring person because they couldn’t afford to do much?” No. “Why not?” Because money doesn’t change your personality.
“And why is it you feel you have to be exciting, all-singing all-dancing, all the time? That you have to be doing things, caring for others, just to be a worthwhile person?” I mean, I have no answer for that, but I was told that it is only I that put these expectations on myself and that other people really don’t expect me to be that way.
What I was reminded is that worth is innate. What I doing right now, whether I am sat on my bum or whether I am actually working - does not change my worth. I was told “you don’t have you earn the right to exist”, and I had never thought about it that way before. I get to exist, I get to take up space and breathe air and eat food and spend time with people, even when I feel I’m not doing anything of value. People don’t like me for the things I do, but the person I am - and although I find that really hard to believe 90% of the time, I’m going to work on that.
I should start work in the next fortnight, but for now I’m going to try really hard to not beat myself up constantly for being out of work or being broke, and instead just focus on things I can do to make my days feel meaningful. Days without structure are so hard, but not working shouldn’t define how I feel about myself because it’s not the only thing I can do.
I’m not pointless or worthless, and I don’t have to earn the right to exist - my worth is innate.
1 note
·
View note
Text
What am I going to talk about when I’m not nursing?
He used to always tell me “you’re not just a nurse to me, you’re Lucy” but then simultaneously I have everyone else saying “what are you going to talk about when you’re not working?” because at least half of my conversations must be about work.
Today I found out my last shift is the 20th July, 11 shifts, 3 weeks away... and it’s shaken me slightly.
When you become a nurse, for better or worse, everything else ends up revolving around it, it becomes part of your identity in a way many jobs don’t. Your patients and jobs and learning new things and all of your memories and experiences consume so much of you, and I haven’t minded (except when I was off work with stress and still couldn’t stop thinking about it). I love my job. I experience so so many things, I’m welcomed into so many people’s lives and I see the best and worst of them. I laugh a lot at work, I become completely over run with emotions: fear, sadness, grief, anger, happiness, pride, elation, heart-break. We laugh and cry and do everything in between.
Some days I leave work so grateful for it all, happy, (still exhausted) but glad to be a part of it all.
And some days I leave wishing to never return.
But to others, I talk about both.
So, in three weeks I will no longer be actively nursing for at least a few months. I’m excited for traveling, and I’m excited to have some time off... but I’m also scared.
What will I talk about? Who will I be when I’m no longer putting nursing first? When I’m nursing I am my best self, I’m more compassionate and patient than I have ever been in my personal life. Will that transfer to the people in my everyday life (I hope so?) or will I just lose it? Will I become silent? Will people stop finding me interesting? Will my brain be empty? Will I stop appreciating all the little tiny things?
It’s sort of horrible to think I’ve only been a qualified nurse for just under two years and it already means so much to me (this is why people never leave nursing!), but I also had the three years before that as a student where it took up of my life.
I am excited to put this weight of responsibility down for a few months, truly. But I am going to miss the guys (my patients), and my team immensely. I’m used to spending very long days with them all all the time and even when I go on holiday I miss them - but I have no plans of returning to this ward.... and that is terrifying. My team I can always keep in contact with (you can’t get rid of me that easily!) but my patients... it’s hard enough when they leave and I wonder how they are getting on, never mind me making this choice!
So, how does your job/profession become so so ingrained in your personality? I know it shouldn’t... but nursing isn’t “just a job”, if it was, I’d be no good at it.
So, they’re some thoughts on leaving my ward, my team and my nursing career (briefly)...
Realistically though, I’ll probably still talk about it all the time, I’ve got enough memories to get me through a few months. You can’t shut me up that easily.
3 notes
·
View notes
Text
An old favourite.
My Charlie has now been working at Asda for a full year, he’s beating all expectations and is kicking some serious ass. He’s still the same sweet man, he still needs a lot of assistance in new experiences but, hell, I’m so so proud of him and everything he’s become. He’s the best of our family, for sure, and none of us would deny that. He’s pure gold and kindness, wrapped up in a lovely, smiley shell.
A learning disability and a learned response.
My brother is autistic with learning disabilities, I tell people that when I talk about him, but I do not know what this is going to mean to them. Are they picturing a flappy child who doesn’t talk and has violent tendencies? Or are they picturing a perfectly able but slightly odd child who talks at you, or is distanced from everyone? Are they picturing a child who needs 24 hour care? Or are they picturing a person who is as capable at self-care as you or I, but simply struggles socially? Or do they understand that the autistic spectrum covers those and everything in between.
“He’s not very autistic”, “he’s not that disabled” I’ve heard from friends after they meet my brother. And, as ashamed as I am to say it, sometimes I have agreed simply because it is easier to do so than to explain how it really is with my younger brother.
My little brother is chatty, friendly, clean and interacts with people without seeming to struggle too much. He laughs and smiles, mostly at the appropriate time. He can make himself drinks and sandwiches without supervision. He can brush his own teeth and get himself dressed. This is what people see.
What people don’t see, is how much of what he does is a learned response.
I’m going to give you an example, or two:
- Two weeks ago, the temperature soared in England. It was 28 degrees, my brother was getting ready for school. He came downstairs with a jumper and a coat on, and it was my Mum who told him to go back upstairs and take them off because it is too hot for them. Why did he do it? Because he does that every day, that is what he has learned, and he does not have the ability to acknowledge changes and act accordingly.
- When I am home, and nobody else is but Charlie and myself I have to go in and tell Charlie to get himself a drink, or lunch. If somebody did not tell him to, or get it for him, he would not eat or drink a thing all day. He is not capable of understanding what his body needs, and why, without constant prompts.
Sometimes disabilities that are not visible are just as hard as those that are.
People expect Charlie to understand, to be able to do certain things and respond appropriately and take care of himself, when he cannot.
My Charlie is as lovely as they come, as kind, as honest. He cannot tell lies, even if it will keep him or others out of trouble (before christmas we always know what he has bought us because he cannot keep a secret). He cannot hurt you… but he also cannot hold a proper two sided conversation, but of course if you aren’t paying attention to him you won’t notice that he does not know how to respond when you ask him questions, or that he is perfectly content with you replying “yes” or “ok” every now and then and does not really know how to converse, merely talk at you. He cannot make decisions regarding his health or self-care, everything he does has been carefully introduced into his daily routine so that he has the basic skills to take care of himself. He does not recognise pain, and needs help to receive the health care he needs. He does not understand why these things are needed, he simply knows they are done. He does not understand why reactions are appropriate for certain situations, he has a very flat range of emotion, he has simply learned what reaction is appropriate and when (although his range of emotions is getting larger as he gets older). He smiles when a camera is pointed at him, but if you look at his smile it is not normal, it is forced, a combination of copying many people. He may not understand what you have asked of him, but he has learned the appropriate answer.
Don’t get me wrong, Charlie is incredibly intelligent. He can do the 176 times tables without hesitation between each multiple, without even a milli-second before the next number. He has a memory like no other. He will remember what you said to him when he was 3, or 6, or 16. He will remember every detail of what you said to him, whether you were talking for 10 hours or 2 seconds. Every detail of every conversation you had in his presence. He will memorise everything he reads on Wikipedia and repeat it word for word at you (but he is unable to tell you what these words mean, or use them in another context). He has begun to recognise sarcasm. He is very clever in his own, specific, ways.
But my little brother has learning disabilities, and autism.
He needs your help, he needs your support and he needs people to help him to understand.
Charlie is not how he first seems, and he needs you to understand that a lot of his behaviour and conversation has been learned - I am very grateful that he has learned these skills through observation and routine because it makes him much more independent that he would otherwise be, but it also presents a challenge because of what others expect of him. He needs you to pay close attention to him so you can observe how much he actually understands and how much of what he does and says is just learned.
I believe this is a struggle for a lot of people with learning disabilities, people dismiss their need for support because they do not appear to need it.
Without the support Charlie needs he will never be the independent grown up he can be.
Everything we do is learned, through observation, trial and error, life experience - and we understand why we do the things we do. Charlie does not. That is the primary difference. If you do not have the knowledge and understanding of why you act the way you do, it makes it awfully difficult to act accordingly when a situation changes, or to make decisions yourself.
My brother is autistic. Not “mildly” autistic, not “just a bit autistic” or “barely disabled”. He is autistic, and he also has learning disabilities.
People need to stop categorising people into degrees of how disabled they are - disabilities affect every person differently, and unless you really know that person you do not know the impact it has on their life.
My brother’s autism and learning disability can be deceptive because his learned responses make him appear much more able than he is - just think, how many other people are not receiving the support they need because of this?
Don’t judge, or make assumptions on people’s abilities, observe them, understand them, support them, enable them.
19 notes
·
View notes
Text
The moments that make it all worthwhile.
We all have bad days at work, and as much as I hate to admit it, recently the days keep coming one after the other for some of us with very few nice days or respite in between.
However, there are always always moments to make it all worthwhile in between.
When I leave work, I always try to think of the moment, for me, that made that day great. Sometimes these moments are just a split second, sometimes they last hours.
Take our ward for example, my moments include:
1. Sitting down for dinner with a patient and discussing the food, our favourite foods, and enjoying a meal together.
2.A patient who rarely talks, or only says the odd few words that rarely make sense, laughing at my joke, or at my singing, or even just at me being an idiot. A true smile, spreading across their face, I don’t always know the reason, but if I was there to either cause it or share it, it’s worthwhile.
3. Helping ease a person’s emotional pain in whichever way I can, sitting with them, talking about family and reminding them they are great, a hug or a comforting word that, for whatever reason, helps.
4. Enabling a patient to enjoy a bath, relax, and make it their favourite moment of the day (like it is my own), with music or chatter, or silence if that’s what they need. That moment is theirs, they do not share it with other patients because they finally get to be alone, and you can’t hear the clatter of other people where the bathroom is. They can be normal there, and at peace.
5. A patient making a joke at my expense. I will never mind that. “Ginger bollocks” was my favourite nickname from a patient, being mocked because I’m short or a terrible singer or keep forgetting what I’m doing, being called called “cuckoo” or “a wee baby” by another patient. It doesn’t matter, it if pleases them, it pleases me.
6. Recently, sitting out on our balcony in the sunshine with a few patients, them drinking a non-alcoholic beer and sitting, enjoying themselves. Even 10 minutes of this can turn my day around.
7. When a patient sings with me. It makes every part of me smile.
8. When I get the time to just sit, and give 20 minutes to one patient without interruption, to talk, to let them be heard. It can be idle chatter about the weather, music, the news, their past, them teaching me how to poach an egg, me giving them hope about the future. Anything. 20 minutes time with one patient, and I feel they have at least had that 1:1 time from me, that they are reminded they aren’t alone.
9. Being outside with a patient, going for a walk, in the fresh hair, noticing the birds. Most of our patients are very different outside to stuck in the ward, they come alive in a different way, and it’s a blessing to share.
We all have tough days, sometimes weeks, sometimes months. It’s never our patients’ fault, even if they are central to it at times, it can’t be helped, they are in our care for a reason.
But if you say you got through 12.5 hours and did not have a magic worthwhile moment, I’d say you either weren’t looking for it, or you didn’t try hard enough.
They’re always there. Those moments that make you say “yes, this is why I work in healthcare”.
0 notes
Text
The cracks chipped into their minds
A crevice caused and torn open by memory
Stolen parts of life.
I fill the gaps where reality and past
No longer serve to rebuild
Or develop, that man.
I turn my smiles, kindness, and laughter
Faith in them, and compassion
Into clay to fill the cracks.
Memory, this I cannot cure
I cannot build a future or past that makes sense
I cannot mend the sense of a life lost.
But my place in this world;
Is to build that feeling of safety and security
Out of my smiles.
Of belonging and worth
Out of my words
Of value and identity
Through listening
My place is to protect, to cherish
Those who are no longer able to do so,
for themselves.
- By me
2 notes
·
View notes
Text
This is now many years old, but I loved writing this post and I love re-reading it.
I have a problem with the phrase "quality of life".
I live in a flat with 4 other student nurses and a student midwife, and when we aren’t talking about food, sex, boys, shopping or drinking it often turns to more intellectual, philosophical conversations along the lines of pregnancy, abortion, and disability with the “what would you do?” question hanging over all subjects. Myself and another of the girls are studying Learning Disability Nursing so I feel like sometimes the others aren’t completely honest with us when talking about disability, but they try to be.
The midwifery student learns incredible things and we love to hear her talk when she gets back from placement, because what she does is truly amazing, but often I hear her talk about ‘quality of life’. It is a commonly used phrase, and she uses it when discussing babies who are starved of oxygen at birth and have possible brain damage, and babies who are extremely premature and will suffer serious disabilities for the rest of their lives, and how she has to talk to parents who are making the decision of whether to fight for that child’s right to live with technology, or let them die because their “quality of life” will be so poor it would only be cruel to keep them alive. She is honest on her stance, and says that she would not want to have a child who was severely disabled because she would not be able to handle it, and she would have all the tests on the fetus so she would know in advance, and could act accordingly. That is completely fair, and I do not judge her in any way shape or form. It is honest. If you will not be able to take care of a child who is severely disabled, if you will not love and want them as much as a 'normal’ child then it is best that you do not do so. I wholeheartedly believe in that…. but what I don’t believe in, is the assumption of how a child’s “quality of life” is going to be from the first days of life, because machinery and measurements and doctors can be, and often are, wrong.
Today is the 8th birthday of a little girl I know through Special Kids in the UK. She was born at 24 weeks, weighing little over 800 grams. She is severely disabled and fights for her right to live every single moment of her life. She is in a wheelchair, with limited movement and twisted arms that face backwards (I don’t really know how to describe them), she has cerebral palsy and lung conditions that require constant attention. Her speech is difficult to understand, but if you listen closely and pay attention you will get it. Her life is far from 'normal’ and she relies heavily on the miracles of technology to keep her alive and mobile. Her visits to the hospital could probably become a world record. I doubt Doctors at her birth thought very much on her survival, it did not seem positive…. but she is the happiest girl I know. She is clever, funny, and loved by every single person who meets her. I cannot describe enough just how wonderful this little girl is, and not because of her disabilities making her amazing, but simply because she, as a person, is a spark of life that makes everybody smile. She is so full of character; she strops like everyone else, she laughs more than anyone else, she smiles and can be bossy and likes to get her way, and she wants to be with her brothers and sisters, or have the attention of my older brother who loves her to bits. Her personality shines more than her disability.
She is amongst many of the people who have had me doubt the ability to assume quality of life from birth, one of many people I know who have defied all odds set against them, and become the most amazing, able, and loved people. People who have their potential so limited by their disabilities but push hard against the walls of that potential to stretch it wherever they want it to go. People who will prove every person who has ever labelled them incapable of doing things, wrong. A little boy I know has spina bifida, and rides a bike. That should be impossible, he should have total paralysis of his lower limbs, he cannot feel his legs at all, but somehow, miraculously he uses them anyway. He crawls around with the best of us, going to the park (albeit, making me carry him), joining in, never being left behind.
I believe when discussing the “quality of life” of people it is forgotten that they are a person. They are not just their shell, their body, their abilities, they are their personality, they are the people who love them, they will become their experiences and memories and every smile they share. They are not their medical condition, or their intelligence, or whether they will go to university or join the Brownies, they are a character in their own right, they are their desires and their accomplishments, they are their determination and their confidence.
I have a problem with the phrase “quality of life”, and determining it from birth because people are wrong, people are always being proven wrong and that individual who will seemingly have diminished “quality of life” could grow to do things that will change the world (I’m talking about you, Stephen Hawking).
I understand I may be bias because of my life experiences, and the people I have met, but I urge you to see the impossible as possible, to see a personality and a face, and a smile, before you see a disability, and to think of love ahead of “quality of life”. Their quality of life will be high if they are loved, do not give up on them.
Thanks for reading!
19 notes
·
View notes
Text
My home from home.
We all start the day at work with the end in sight, we know when we arrive, that at the end of the day we get to leave. We clock in, we clock out. We say good morning, and we say goodnight to each other and to our patients.
But this clock-watching habit we all do, it has to go.
Our patients, they don’t get to go home.
For 12.5 hours we may answer the same question 100 times or more, we hear the shouting and we clean up the mess, we have the same conversations over and over again, we go through the routine of the day, we fill out the same documentation and do medication and help with personal care and meals and try to get people out for walks and activities... but imagine being our patients left on the ward, left still asking those questions, to whoever is there, whether they remember it or not, still hear shouting and singing in the night, still hear doors banging and staff talking, still surrounded by the same patients (whether they have anything in common or not), and hearing other patients repeat themselves all through the night.
Our patients do not get to leave at the end of the day.
Yes, 12.5 hours can be a struggle, and on a long week that is 62.5 hours on the ward, its a long time, but it isn’t all the time.
In between that what do we do? We can sit in silence, put the TV on, read, talk to family and friends, we can go out, we can choose what we want for dinner, or to have a drink if we want, we can go to another city or country even, we can experience our version of real life.
This is their real life, they don’t get to go home.
I spend enough time at work to consider it my ‘home from home’, but is it comfortable? Is it relaxing? No, and realistically it never will be.
But our job is to make it that for our patients, some of whom never talk to family for whatever reason, some are happy and some are distressed by their dementia, some have some independence and some have none, some make little choices (but imagine the only choice in your day being what you have for dinner and what is on the TV), but none of them are free.
I believe every time we clock watch, we remind some of them that we get to leave. Every time we rush out at the end of the shift without saying goodbye to those it matters to, we remind them this is our job and that’s all we’re here for.
Our patients are people, important people, equal to us in every single way, who need caring for and need attention and companionship in a place that can get ever so lonely even when surrounded by noise and people. Our patients experience everything we do, and they’ve done what we’re doing, they’ve worked, they’re lived - they’ve just got a bit jumbled and bits have fallen out.
When we’re at work with them, we all need to be present at every moment. I, too, am guilty of clock watching, especially at the end of the shift (often in a panic to get everything done), but I wish I didn’t.
We all get to leave, we don’t need to watch the clock, because that time will come about.
Every second looking at the clock should be spent devoted to our patients, smiling, talking, watching, helping them or just sitting in silence nearby ensuring they do not feel alone.
0 notes