Text
Mastering Revenue Cycle Management: Unveiling Key Performance Indicators (KPIs) for Success

Our seasoned revenue cycle management professionals have chosen the 20 most influential KPIs for medical providers, including the RCM process from patient scheduling to payment. The KPIs are organized by billing phase and supplemented by our internal benchmarks or the relevant industry standard.
The Top 20 Healthcare RCM KPIs
The advantages of effective revenue cycle management cannot be emphasized. However, with over a hundred indicators to monitor the health of their RCM, it can be difficult. Knowing the proper KPIs – the most important to the business — can save you time and effort, allowing you to concentrate on generating business outcomes. Discover a comprehensive list of essential KPIs, from Days in Accounts Receivable (AR) to First Pass Acceptance Rate. Gain insights into each metric's role and significance in maintaining a healthy revenue cycle.
No-show or cancellation rate
The no-show or cancellation rate is when your patients cancel or don't attend appointments, typically measured monthly. The formula to calculate the no-show rate is:
No-show rate = Missed appointments / Total number of booked appointments
Exclusion Percentage
Exclusions are the patient accounts that failed the eligibility and benefits checks (that don't have active insurance coverage), were unable to get the active insurance details, had coverage terminated claims, or had incomplete demographics while verifying the status. The formula to calculate the exclusion percentage is as follows:
Exclusion percentage = Number of accounts that failed eligibility checks / Total number of accounts verified
Denials Due to Authorization Percentage
Prior authorization is critical when you have to render a service and ensure that claims are paid. The denial due to incorrect or no authorization percentage is a critical metric to ensure collections and reduce claim write-offs. The formula to calculate the denial percentage due to authorization is:
Denial due to authorization percentage = Value of claim denied for authorization issues / Total value of denials
Unbilled Claims Percentage
Unbilled claims percentage refers to claims not billed to average daily claims volume. There are many reasons for the hold claims, but they should be resolved promptly for faster payments or denied for a timely filing limit. The formula to calculate the percentage of the unbilled claim is as follows:
Unbilled claims percentage = Number of claims unbilled / Average daily claims volume
Clean Claim Ratio
The clean claim ratio is the percentage of claims the insurance payer accepts without rejection.
Clean claim ratio = Number of claims accepted by insurance without changes / Total number of claims
Initial Denial Percentage
The initial denial is the number of denials received from the overall claims submitted to the insurance, expressed as a percentage. The formula to calculate the initial denial percentage is:
Initial denial percentage = Number of denials received for the first time / Total number of claims submitted
Strategies for Improvement
Equip yourself with practical strategies for improving key metrics. Learn how to address common challenges and elevate your organization's financial health.
Conclusion:
Wrap up your journey through the intricacies of Healthcare Revenue Cycle Management armed with the knowledge to optimize performance, boost efficiency, and confidently navigate the complexities of healthcare finance. Ready to revolutionize your approach to RCM? Dive into our latest blog post for a transformative exploration of Revenue Cycle Management KPIs.
#healthcare revenue cycle management services#medical billing and coding for physicians#medical coding for physicians
0 notes
Text
Tips to Boost Practice's Revenue with Expert Physician Coding and Billing Services

Are you looking for physician billing and coding services for your practice? If you need an instant solution to your billing and collection headaches, keep reading this informational piece.
In today's fast-paced medical industry, efficient medical coding for physicians is crucial to ensure maximum revenue collection and smooth business operations. A result-focused RCM service provider is all you need to streamline your physician coding. It offers expert physician billing and coding services. These providers leverage modern technology and has a team of certified professionals to optimize the billing process and boost your practice's revenue.
Challenges of Medical Billing and Physician Coding
Medical billing and coding is a complex task. It can be error-prone and time-consuming. Even the slightest error in claim submission can lead to revenue blocks from payers. Various factors, such as improper provider credentialing, patient insurance eligibility, claim submission, and claim follow-up create hurdles in revenue performance.
Billing and coding service providers should understand physicians' challenges in managing their revenue cycle. Their RCM services should be designed to address these challenges and optimize revenue flow for your practice. Here's what you can expect from a physician billing and coding service provider:
Certified medical coders
A team of certified coders with years of experience employs advanced technologies like ML, AI, and RPA to eliminate errors in your billing process.
Revenue-focused services
Maximizing revenue collection from payers is a primary goal. They offer end-to-end RCM services to increase your cash flow efficiently.
Streamlined claim submission
Highly experienced professionals manage your claim submission process, ensuring maximum service reimbursement.
Regular audits and thorough analytics
Stay informed about your practice's financial performance through regular audits and comprehensive reports.
Customized RCM solutions
Tailored RCM solutions that align with your needs and business goals.
Medical billing and coding for physician service providers prioritize client satisfaction and ensure that all their solutions comply with HIPPA protocols. Their physician billing system processes all claims through a secured communication network, safeguarding sensitive patient information.
You must also look for comprehensive practice management solutions that integrate seamlessly with your existing Electronic Health Records (EHR) system, eliminating additional IT infrastructure.
Select a partner that has delivered results in the past. Look for impressive results, including a significant reduction in turnaround time, higher clean claim percentages, improved patient collections, and enhanced reimbursement rates. Integrate with a reimbursement model, built on years of knowledge and experience, consistently delivers expected results.
With Plutus Health's expert physician coding and billing services, you can optimize your practice's revenue flow, streamline billing processes, and stay ahead of your competitors in the healthcare industry. Experience the difference in your practice's growth and revenue by partnering with Plutus Health today. Take the first step towards maximizing your revenue and practice growth - Schedule an expert call or consult with our team of professionals now.
#physician billing and coding#physician coding#medical billing and coding for physicians#medical coding for physicians
0 notes
Text
Mastering Prior Authorization in Healthcare: An Overview and Step-by-Step Process
Prior authorization is the most important process in healthcare RCM. Due to errors in prior authorization, claims over $21 million were denied, while that of $291k was written off. It is important to get prior permission from payers to collect payment for the services offered as a healthcare treatment to the patients. Insurance payers might not approve some tests or treatments; practices must wait until they get permission or inform the patients about the costs.
Prior authorization (PA) is a long process that requires the collaboration and involvement of patients, payers, and healthcare providers. This blog will help you understand the prior authorization process and the steps involved in it.
Explain prior authorization
It is a process followed by insurance providers to check if the suggested medical procedures, tests, or treatments are necessary for that medical condition. Insurance payers reject reimbursements if a healthcare provider fails to take prior authorization.
Insurance payers suggest healthcare providers offer less expensive treatments to patients wherever possible. Practices should consider less expensive drugs before going with an expensive one. It completely depends on the insurance company to accept or reject a particular process.
What does a prior authorization check?
Drug or service is necessary.
Are the same services suggested more than once?
Are the services beneficial to patients?
Do the services make sense based on the cost?
Ways to do prior authorization
Healthcare providers should be in-network with the payer to get authorization. Practices should thoroughly verify patient documents and take authorization before starting treatment. Healthcare providers' staff should connect with payers and give all the patient details before admitting them.
Prior authorization steps
Determine if the treatment or service requires prior authorization.
Identify the responsible party for locating patient plan data and managing benefits.
Understand the process of submitting patient data, as each payer has different rules.
Ensure proper transmission of service and patient data.
Await the payer's response and provide follow-up data if necessary.
Communicate pre-authorization results to the team and patients.
Take necessary steps to reattempt denied authorizations
Ways to handle prior authorization denials
Medical billers and coders strive to provide the best services and submit clean claims, but insurance companies keep changing their authorization rules resulting in denials.
Prior authorization denials can be expensive, and healthcare providers should handle them as a priority. Insurance companies ask for prior authorization before healthcare providers start giving services to patients. Here are the top ways to handle prior authorization denials:
Know the right time to appeal
Stay prepared for denials
Check for all medical codes
Strictly follow all the payer guidelines
Common prior authorization hurdles
Prior authorization is a complex process. Healthcare providers need to follow all the processes to streamline the complete process. To streamline the process, you should first know the prior authorization hurdles:
Management of cost
The necessity of the treatment
Administrative mistakes
Unfilled details
Procedural errors
Proper steps not followed
How to minimize prior authorization delays
Prior authorization is a lengthy and time-consuming process. Due to limited time and resources, healthcare providers delay prior authorization resulting in lost revenue. Prior authorization delay also hampers patient care. Here are the most effective ways to minimize prior authorization delays.
Search for effective low-priced drugs
Prescribe drugs that do not need authorization
List down the treatments that do not require authorization
Follow guidelines
Educate staff
Have a prior authorization team
Use cutting-edge technologies
Have a robust denial management system
Do you have sufficient time and staff to take prior authorization for each patient? If not, connect with Plutus Health. With 15+ years of experience in providing end-to-end RCM services, Plutus Health has seamlessly helped all its clients to achieve their desired results. Our prior authorization team ensures all the documents are collected on time and takes authorization before you give services to the patients.
Do you want to know more about Plutus Health's prior authorization process, explore this blog: https://www.plutushealthinc.com/post/prior-authorization-in-healthcare-overview-purpose-process
#rcm services#revenue cycle process in healthcare#prior authorization#prior authorization in healthcare
0 notes
Text
AR management tips and tricks by professionals that no one tells you
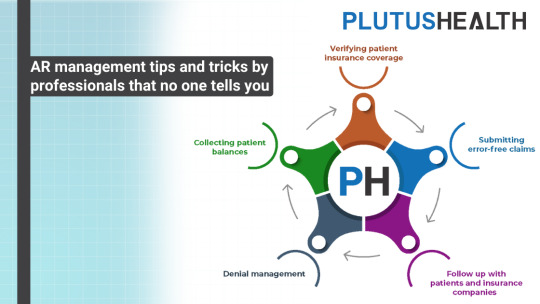
Healthcare providers lose 5-15% of annual revenue because of improper AR (accounts receivable) management. A report published by the Medical Group Management Association (MGMA) found that the average AR days for over 13% of healthcare providers is 120 days.
Most healthcare providers need help managing their AR and collecting their payments on time. In this article, our experts with 15+ years of experience have explained tips, tricks, and the importance of AR management.
Blog index:
Definition of AR management in healthcare RCM
Importance of AR management
Stages of AR management
Efficient AR management tips
Definition of AR management in healthcare RCM
Tracking and collecting payments from patients and payers for the healthcare services offered is called AR management. It is advised that the average AR for a healthcare organization should be <25 days.
Here are the steps involved in AR management:
The first and most important step in accounts receivable management is verifying patient insurance coverage. Verification helps to understand the current insurance status of the patient.
Healthcare providers need to submit error-free claims the first time. Claim scrubbing and submitting error-free claims is the next step that plays a vital role in AR management.
Following up with payers and patients is crucial as cash flow directly depends on how well you get engaged with your patients and payers.
Denials can hamper the revenue of the healthcare provider. Managing your denials is vital to manage your account receivable.
Analyzing the reports and payments is important for healthcare providers as it will give a clear idea of what payments need to be collected.
Importance of AR management
The financial health of the healthcare provider depends on how well they manage the AR. From the patient's call for an appointment until the final payment is received, AR management is important to streamline the cash flow. Here are a few other reasons why AR management is important:
Smooth cash flow
Revenue optimization
High patient satisfaction
Compliance
Stages of AR management
AR management can happen primarily in 3 stages. Each stage needs to be followed properly to get the desired results.
Stage 1: Pre invoice
Credit check conduction
Payment term establishment
Setting up a patient account
Stage 2: Invoicing
Accurate invoice generation
Prompt invoice delivery
Unpaid claim follow-up
Stage 3: Payment & collections
Collect payments
Resolve denials
Reconciliation
Efficient AR management tips
Efficient AR management ensures timely payment and minimizes write-offs. Here are a few tips to efficiently manage AR.
Patient insurance eligibility verification
Precise coding
Claim scrubbing and submission
Following up on outstanding payments
Check denials and appeal status
Create payment plans
Appropriate staff training
AR management can be done in-house or outsourced to providers like Plutus Health, with years of experience serving the healthcare industry. Outsourcing helps to take off the burden from the internal staff and helps to collect payment on time.
1 note
·
View note
Text
Best-in-class Cardiology Billing Services to Increase Your Profits

Are you fed up with battling your cardiology billing and coding costs? Do you wish to increase the revenue of your cardiology practice? Plutus Health has got you covered with its cardiology revenue cycle management (RCM) services that help you boost your income, eliminate denials, errors, and A/R days, and streamline your billing and coding process.
Plutus Health - A Trusted Cardiology Billing Company
Plutus Health is a cardiology billing company that provides AAPC-certified coders, denial and accounts receivable management, and one-click assistance 24/7. With the best cardiology medical billing services from Plutus Health, you can stop compromising on your revenue performance and stand out from your competitors.
Stop Compromising on Your Revenue Performance
Cardiology billing can be challenging since individuals with heart disease have high financial needs and significant out-of-pocket expenses. Only a fixed fee is paid by payers depending on patient policies, and even the smallest mistakes in claim submission result in payment delays or denials. Even patients will not fulfill their financial obligations because they are preparing for such a high price. This causes practices to lose a lot of money.
To capture all procedures and diagnoses and guarantee a clean claim rate better than 95%, Plutus Health educates its clients on proper coding principles and clinical documentation enhancement initiatives. To decrease cardiac claim denials, we also adhere to all LCD rules.
Cost-effective RCM Solutions
Our professional and cost-effective cardiology EHR billing services maximize reimbursement, result in a quicker cash flow, and increase reimbursements for your company. We process all denials within 72 hours and bill out all charges in 48 hours. Payments are also posted within 48 hours after receiving ERA/EOBs. Additionally, we keep abreast of new LCDs, coding standards, clinical circumstances, and technological advancements to support medical need and record ICDs in a comprehensive manner to match clinical scenarios.
Specialized Cardiology Coding and Billing
For all sub-specialties of cardiology, including invasive, general non-invasive, cardiovascular, cardiothoracic, and interventional cardiology, we offer specific coding and billing services. Cardiology medical billing, coding, and collections, including AR and Denials Management, can be efficiently handled by our team of experts with more than 15 years of combined experience.
Optimize Your Cardiology Coding and Billing
A team of experts at Plutus Health with more than 15 years of combined experience in the field of cardiology RCM can easily handle cardiac and cardiothoracic surgery medical billing, coding, and collections, including managing AR and denials. Our specialists conduct in-depth pre-billing audits to decrease cardiac insurance denials, continuously check our payments against agreed-upon sums to ensure that there are no under-payments, and prioritize handling the AR if no information is available by the payer's payment cycle.
Streamline Your Cardiology Revenue Cycle Management Services with Plutus Health
For more than 15 years, Plutus Health has offered cardiology billing and coding. We take particular care while preparing cardiology claims, and our thorough pre-verification paperwork makes sure that we stop our cardiology clients from losing money. We submit accurate claims and receive very nearly 100% of the costs incurred by cardiology offices.
Our cardiology RCM services go beyond simple coding and billing for practices. To receive 100% reimbursement, it takes a lot of work, so we offer a comprehensive method to optimize.
Along with office-based E/M visits, our billing and coding for cardiology also includes complex cardiology billing codes and rules, office notes, SOAP, and operative notes, payer-specific policy and payer guidelines, pre-billing audits (which include CPT and DX validation, eligibility, and patient yearly deductible), cardiology insurance denial management, and cardiology-related terminology.
You can streamline your cardiology revenue cycle management services with Plutus Health and get outcomes you can count on. The average turnaround time for our cardiology clinics has decreased to 48 hours, the clean claim percentage has increased dramatically to 95%, the automated payment collections have increased to 35%, and the average (NCPR) collections have reached a staggering reimbursement of 98%. Also, we have lowered A/R days to 25 days and decreased denial rates for cardiology offices to an average of 5%.
To learn how to get the highest possible compensation for your claims, speak to our cardiology billing specialists right away.
#cardiology coding#RCM Cardiology#Cardiology Medical billing services#Cardiology Insurance Denials#cardiology coding services#Cardiology Billing Company#Cardiology Claim Denials#cardiology ehr billing services#cardiology revenue cycle management#Billing companies for cardiology#Cardiology Medical Billing and Coding
0 notes
Text
Streamlining Your Revenue Cycle: How Medical Billing Companies Can Help

Medical billing services are essential for healthcare providers to receive timely and accurate reimbursement. Medical RCM is a complex process that involves coding and submitting clean claims, following up on denied claims, posting payments, and handling patient billing and collections. It requires specialized knowledge and expertise that many healthcare providers still need.
Outsourcing medical billing services to professionals can help practices streamline their healthcare revenue cycle management and improve their financial performance. This article will explain the benefits of partnering with a medical billing company, how to choose the right provider, and the services offered by top companies.
Benefits of partnering with a medical billing company
Improved revenue cycle management
Effective revenue cycle management is critical for healthcare providers to ensure timely and accurate service reimbursement. Medical billing companies like Plutus Health can help healthcare providers optimize their revenue cycle management by identifying inefficiencies in their billing processes, monitoring claims submissions and denials, and implementing best practices for revenue cycle management.
Medical billing companies have access to advanced technology and software that can automate many billing processes, reducing the risk of errors and delays. They also have a team of expert billers and coders who stay up-to-date with the latest billing regulations and requirements, ensuring that claims are submitted correctly and promptly.
Reduced administrative burden
Medical billing is a time-consuming and labor-intensive process that requires significant administrative resources. Outsourcing medical billing services to professional healthcare revenue cycle management providers can help practices reduce their administrative burden, allowing them to focus on patient care and other core activities.
Professionals can handle all aspects of the billing process, from claims submissions and denial management to patient billing and collections. It can free up healthcare providers' time and resources, enabling them to devote more attention to patient care and other critical activities.
Access to expert billing knowledge and technology
Medical billing is a complex and ever-changing field that requires specialized knowledge and expertise. Medical billing companies have a team of expert billers and coders who have in-depth knowledge of the healthcare industry, medical billing regulations, and insurance requirements.
Medical billing companies also have access to advanced technology and software that can automate many billing processes, reducing the risk of errors and delays. It help healthcare providers save time and resources while ensuring timely and accurate reimbursement.
How to choose the right medical billing company?
Choosing the right medical billing company is critical for healthcare providers to optimize their revenue cycle management and maximize their financial performance. When selecting a provider, practices should consider many factors, including:
Experience and expertise
Reputation and track record
Service offerings and capabilities
Technology platforms and integrations
Pricing models and fee structures
Customer service and support
Healthcare providers should also ask questions during the evaluation process, such as:
How long have you been in business?
What types of healthcare providers do you serve?
What is your process for handling denied claims?
What technology platforms do you use?
What is your pricing model?
How do you handle customer service and support?
Medical billing services offered by top companies
Medical billing companies like Plutus Health offer many services to help healthcare providers optimize their revenue cycle management and maximize their financial performance. Some of the key services offered by top companies include:
Claims submission and tracking: Medical billing companies can handle all aspects of claims submissions, from coding and billing to submission and tracking. They can also monitor claims for errors and omissions, ensuring they are submitted correctly and on time.
Payment posting and reconciliation: Medical billing companies can post payments and reconcile accounts, ensuring that healthcare providers receive timely and accurate reimbursement for their services.
Denial management and appeals: Medical billing companies can seamlessly handle denials and appeals, identifying the root cause and appealing denied claims on behalf of healthcare providers.
Patient billing and collections: Medical billing companies can handle patient billing and collections, ensuring that patients are billed appropriately and promptly and that collections are handled professionally and efficiently.
How medical billing companies differ from one another
Not all medical billing companies are created equal. There are many factors that differentiate medical billing companies from one another, including:
Pricing models and fee structures: Medical billing companies may charge a percentage of collections, a flat fee per claim, or a hybrid model. Healthcare providers need to understand the pricing model and fee structure of each medical billing company they consider, as this can significantly impact their financial performance.
Technology platforms and integrations: Medical billing companies may use different technology platforms and integrations to automate their billing processes and improve efficiency. Healthcare providers must understand the technology platforms and integrations used by each medical billing company they consider, as this can impact the quality and accuracy of their billing services.
Customer service and support: Medical billing companies may offer different levels of customer service and support, including dedicated account managers, 24/7 support, and online portals for tracking claims and payments. Healthcare providers must understand the customer service and support offered by each medical billing company they consider, as this can impact their satisfaction and overall experience.
Conclusion Outsourcing medical billing services to a professional medical billing company can help healthcare providers optimize their revenue cycle management and financial performance. You can consult Plutus Health for your end-to-end medical RCM services. They have been in the healthcare RCM industry for 15+ years and have shown exceptional results for their clients. Click here to contact Plutus Health’s medical billing and coding experts.
#medical billing company#medical billing services#plutushealthinc#best medical billing companies#medical billing and coding services#medical coding services companies
0 notes
Text
Maximizing Your Practice's Growth with Accurate Mental Health Billing Services

Are you sick of investigating unpaid and rejected claims? Are you trying to find a mental health billing company that can adhere to payer and regional regulations? Go no further than Plutus Health, a reliable partner to handle your revenue cycle management (RCM) services for mental health.
With one-click help available 24/7* 365 days a year, Plutus Health is a group of AAPC-trained and certified mental health coders who offer end-to-end mental health billing solutions. As your go-to billing and coding experts for mental health, we promise to streamline your billing procedures, improve your coding and billing system, and carry out thorough pre-billing audits to decrease denials.
Because of the many types of treatments provided to patients, as well as the insurance plans, deductibles, and other differences by state, payer, and plan, mental health billing can get complicated. With decades of experience in the field of mental health coding and billing, Plutus Health promises to make your coding and billing experience more successful and less stressful.
Our group of certified coders works on your claims and consistently delivers the outcomes your practice needs. We submit accurate claims with the utmost care in order to increase your practice's first-pass ratio. Our mental health billing professionals are experienced in creating and putting into practice successful procedures that will increase our clients' financial viability. You can count on a hands-on approach and a dedication to producing top-notch results.
The top mental health billing insurance denials, such as incorrect CPT codes, provider not enrolled, missing/invalid information, excluded or non-covered charges, billing to the wrong payer, duplicate billing, overlapping claims, and contractual obligation, are handled by Plutus Health with guaranteed results.
The average turnaround time for claims at mental health practices has decreased to 48 hours, and their share of clean claims has increased to 95%. The average (NCPR) collections have achieved a staggering reimbursement of 98%, while automated patient payment collections have increased to 35%. lowered the average amount of denials for mental health practices to 5%, and the average amount of time it takes for mental health practices working with Plutus Health to receive payment is now 25 days.
At Plutus Health, we recognize that billing for mental health services presents significant difficulties that could jeopardize your practice's ability to make a profit. We can assist you in streamlining patient collections and offering patient statement services that involve patients and provide them a better experience to receive faster payment for their obligations. Before to the start of services, we also examine the patients' benefits and eligibility, and patient collectibles like co-pays and deductibles are collected during the patient visit before the claim is submitted and the payer is paid.
Our mental health billing solutions are tailored to the needs of your practice and provide you with a range of services that are intended to improve your revenue cycle management. Our team of experts can efficiently handle mental health medical billing, coding, and collections for mental health service providers because to their 15+ years of experience in the RCM industry. Plutus Health wants to be your revenue cycle management partner by streamlining and improving the coding and billing process for mental health services. Speak to our mental health billing and coding specialists today to set up an expert conversation, and don't compromise on your income success.
#mental and behavioral health billing service#mental health coding and billing provider#mental health billing partner#mental health billing solutions#outsource mental health billing and coding
0 notes
Text
6 Ways to Combat Healthcare RCM Talent Shortage

Hospitals encountered billions of dollars in loss due to the healthcare skill shortage in 2022, and this upset would grow in the forthcoming years. RCM (Revenue cycle management) is primarily pendant on the workforce. The efficiency and productivity of a provider's income rely on how well the staff can address their medical billing and coding. RCM requires timely follow-ups, processing documentation, and handling denials. The ineptitude to perform the above processes leads to cash flow insufficiencies, expanded contradictions, mistakes, and reduced productivity.
The healthcare enterprise will be transient by over 122,000 by 2032, foresaw AAMC (Associates of Medical College). Skill shortage would affect caregivers, the supporting RCM professionals, and administrative staff. The labor expense would grow by $86 billion in the forthcoming year, while the other costs would increase by $49 billion.
Are you ready to fight the impending talent deficiency in the healthcare industry? Are you also encountering a revenue cycle skill shortage? After profoundly researching why there is a resource crunch in healthcare revenue cycle management, professionals specially hand out the article. We have also discussed the steps to overcome the healthcare revenue cycle skill shortage.
Ways to overpower Healthcare RCM Talent Shortage
Healthcare providers reduced patient retention in 2022 due to recurring resignations and earlier retirement. Here are the top methods to overcome the healthcare RCM talent deficiency.
Utilize cloud
Employee automation
Adequate operational framework
Enhance strategies
Make endurable transformation
Believe in outsourcing
Why is the healthcare sector encountering an RCM resource crunch?
After the Covid-19 pandemic smashed the globe, the healthcare sector is working better than its ability to provide care to consumers. Many caregivers chose to retire early or change to a distinct organization. Even the supportive and back-office staff left the association. Here are additional reasons for the resource crunch:
Earlier retirement
Workload
Low income
Higher growth option
Employees changing, retiring, or leaving their jobs leads to a resource crunch, a tremendous loss for the healthcare provider. Below are the methods to overwhelm the healthcare RCM talent shortage and expand your practice.
Utilize cloud
Cloud-based RCM software aids healthcare providers in performing tricky tasks remotely without needing more resources. Cloud-based EMR software forms a virtual infrastructure that lets healthcare providers access documents anytime, anywhere, without compromising safety.
Employee automation
Technologies like AI (artificial intelligence), RPA (robotic process automation), and ML (machine learning) aid healthcare providers in dealing with RCM staff need efficiently. You can accomplish all the process deadlines without hindering the process quality. Automation eradicates all redundant tasks decreasing the need for FTEs.
Healthcare providers can also facilitate numerous labor-intensive RCM tasks with the optimum utilization of technology. The intro of patient portals allows practices to keep patient finances with a simple click, undervaluing the cost of patient registration, sending patient statements, taking patient follow-up, and collecting payments.
Adequate operational framework
It is tough to keep and control the operating framework in the healthcare RCM due to the increased volume of processes and accuracy requirements. Healthcare providers must create a streamlined work procedure that lets the staff comprehend their work without handling the burden. Healthcare practices can investigate the productivity of each employee and prepare the team based on the information.
Enhanced strategies
Work techniques play a crucial role in healthcare revenue cycle management as all the functions are interdependent. Enhanced plans permit healthcare providers to battle unanticipated staff shortages without hindering operations. Devising work strategies can aid healthcare providers in preparing for impulsive registration.
Make endurable transformation
Denial trend analysis is vital for healthcare providers to run a profitable business. Knowing the root cause of denials aid healthcare providers in making the typical errors hampering revenue. It also boosts the billing staff to work more efficiently, as most of their claims bring revenue.
Believe in outsourcing
Outsourcing is an essential option for healthcare providers to fight the healthcare RCM talent shortage. Outsourcing RCM services boosts the productivity of healthcare providers at minimum cost. A Healthcare provider's RCM gets handled by trained professionals with experience and certification in the tasks assigned to them. RCM service providers efficiently manage account receivables and denials, increasing the FPAR for the healthcare provider.
RCM service providers use an excellent mix of technology and experience to offer superior results for healthcare practices. Besides revenue management, organizations can achieve patient and practice management benefits without constructing additional IT infrastructure.
Ways to choose the right revenue cycle management service provider
Keeping a fast and healthy cash flow is paramount for healthcare providers to stay strong in the market. Revenue authorities should handle all the pain points of healthcare providers and stop them from deficits and revenue leakage.
It is vital to select the correct revenue cycle service vendor. Healthcare providers' RCM process depends on the company they partner with. The right enterprise aligns with your objectives and provides answers that guarantee results.
You must partner with the RCM enterprise open to funding in the latest trends and technology. Plutus Health has the best resolutions for your practice to sustain and facilitate your revenue. We are a one-stop resolution for all your RCM needs.
Our trained professionals provide all the RCM services. They should be capable of giving outcomes without compromising grades. Schedule a call with our professionals to facilitate your revenue cycle management strategies.
#revenue cycle management healthcare#revenue cycle management in medical billing#revenue cycle management consulting#revenue cycle management solution#revenue cycle management process#revenue cycle management in healthcare
0 notes
Text
E/M Coding Changes 2023: All You Need to Know

Healthcare providers who understand how to code can significantly increase reimbursement and lower revenue concerns associated with stressful audits. AMA (American Medical Association) has presented a fresh set of revisions in E/M codes, conveying a substantial restructuring. The E/M coding modifications would be adequate from January 1, 2023, and will create coding streamlined for healthcare practices.
Evaluation and Management Codes (E/M) are utilized in general medical practices like hospital visits, office visits, preventive medicine services, or home care services by competent healthcare professionals (QHPs) or physicians. This blog will discuss all you must know about E/M coding changes in 2023.
What is E & M coding?
Evaluation and management codes comprehended as E/M are Current Procedure Terminology (CPT) codes from 99202 to 99499. These AMA codes are used for family physicians, general visits among emergency room physicians, and specialty care practitioners. These codes are based on the benefits given to the patients. E/M codes are used in every step of the patient expedition, from when they enter your practice to physical inspection and all procedures or medical evolution you conduct.
E/M codes Use
Comprehending E/M codes and understanding their care background and corresponding service type is vital to maintain practice efficiency, productivity, and financial health. E/M codes are not used for diagnostics, surgeries, testing, or radiology. These codes apply to the healthcare providers that evaluate or manage the patients. Multiple services fall beneath these codes, for instance, a patient seeing a provider for a general checkup. Here are the kinds of services that fall underneath E/M codes.
Hospital visits
General office visits
Home care services
Preventative medicine services
Components of E/M codes
There are three elements of E/M codes according to MCT (Medicine & Medicaid services) when determining the suitable level of E/M services delivered:
Patient history
Examination process
Medical decision making
Other factors clinch the selection of E/M codes, like the time spent giving a distinct service to the healthcare provider.
Regulatory & coding changes of 2023
E/M code updates impact the guidelines on how these codes can be used. The current update released by AMA affects various types of healthcare providers. Here is the list of procedures and regulations that were deleted, modified, and retained.
Inpatient and observation care services
E/M codes 99217-99220 got deleted
E/M codes 99221-99223 & 99231-99239 got counted as observation and hospital inpatient care services
Consultations
E/M codes 99241 and 99251 got deleted
E/M codes 99242-99245 (Office or additional outpatient consultancies) & 99252-99255 (inpatient or observation consultation) got corrected
Emergency department services
E/M codes 99281-99285 (Emergency department visit) got corrected
Nursing facility services
E/M code 99318 got removed
E/M codes 99304-99310 and 99315 -99316 got revised
Custodial care, Rest home, or Domiciliary services
E/M codes 99324-99238, 99339-33340, and 99334- 99337 got deleted
Home and residency services
E/M code 99343 got deleted.
E/M codes 99341- 99342, 99344-99345, 99347- 99350, and guidelines are revised
Prolonged services
E/M codes 99354-99357 got deleted
E/M codes 99358 - 99359, and 99415 – 99416 (long face-to-face services in office or outpatient) got modified in the guidelines
E/M code 99417 (prolonged service with the direct patient) got revised in the service
E/M code 993X0 got counted in prolonged service codes
E/M coding changes were introduced to facilitate healthcare providers' lives and free their administrative burden.
Plutus Health has a team of certified coders who got corrected with the coding updates. We use the proper codes to get you paid what you merit. Connect with Plutus Health's coding professionals to learn more about the coding updates and steps you should pursue to aid them.
Register for the Webinar today to learn more about the changes to E/M coding in 2023.
Essential Takeaways:
E/M code modifications are likely to develop further in 2023.
E/M code changes energy disturbs your current workflow, but the benefits it brings to healthcare providers are far more significant.
E/M code updates got designed to facilitate uncovering the correct code.
Update your EHR system to organize and evaluate new coding changes
0 notes
Text
Advantages and Disadvantages of Outsourcing ASC Medical Billing
Medical billers need sounder dashboards, more leisurely reporting customizations, more virtual tools, enhanced capability to comprehend key billing metrics, and more. 50% of ASCs believe medical billing is complex and are often overwhelmed by the frequently varying rules & regulations. Payers have started requesting more from ASCs to chaperone the submitted claims.
ASCs must be on their toes to follow all the modifications in compliance and regulatory guidelines specific to them, as a tiny error can cost thousands of dollars and raise the risk of external audits. Even insurance companies keep reworking their platforms and are regularly altering their methodologies.
Medical billing firms are constantly updated with the most delinquent tools and software to oblige ASCs in billing and assure maximum reimbursements. As a result, most ASCs outsource their medical billing to sidestep all the intricate nuances enwrapping getting reimbursed for their helpful services. This blog discusses the advantages and disadvantages of outsourcing medical billing.
What precisely is outsourcing ASC billing imply?
ASC billing decrypts all the services, documents, and therapies offered to patients into a systematic structure that insurance payers can comprehend. ASCs get reimbursed only if all the data is suitably edited and documented according to the payer's guidelines. The ASC billing process is convoluted and full of slang that only a certified and adept professional can understand. The slimmest errors while proffering the documents or editing the patient treatment details result in a partisan payment or complete claim denial.
ASCs initially operated all the billing in-house with their team. It was and now is a tiresome process with plenty of documentation and terminology that takes a massive amount of time to understand and be able to complete. It also requires a lot of paperwork. Due to the upgrade in technology and increased awareness, ASCs have begun partnering with firms that provide end-to-end RCM services. Outsourcing billing services means that the ASC no longer has to worry about the complexities of the processes encircling getting compensated for their services from the payers. That responsibility now slips under the RCM service providers the ASC selects to handle their medical billing services. ASC billing service providers deliver outstanding services as they have a large squad of trained and certified specialists who work precisely to get full reimbursement for the ASCs. They utilize modern technologies, which count more value to the billing and help to streamline the RCM processes for ASCs.
Advantages and disadvantages of outsourcing ASC medical billing
The advantages of outsourcing ASC medical billing comprise:
Fast insurance payment
A decrease in medical billing mistakes results in quicker payments and total reimbursement. ASC medical billing service providers employ a mix of advanced technology and knowledge to submit, track, and handle claims.
Outsourcing with a reputed RCM billing firm like Plutus Health can boost revenue, streamline workflow, and bring exponential enlargement for an ASC.
Fewer costs
Employing and sustaining in-house medical billing is an enormous expense for ASCs as it arrives with expenses like payroll, infrastructure, onboarding, insurance, and more. ASCs need to have disposable revenue or the time necessary to preserve an entire unit of in-house billers. They need help finding a fast solution if a critical employee intends to quit or walk out. Outsourcing medical billing services reduces overhead costs. ASCs can count on Plutus Health to handle all their billing needs, including staffing necessities, at a lower price.
Full transparency
A few ASCs believe outsourcing is like transferring control and decision-making authority to an exterior company. When ASCs associate with a third-party medical billing benefit provider, the outsourced medical billing firm is held accountable for and responsible for delivering positive outcomes based on pre-decided parameters. ASCs can peek at crucial performance indicators to assess the outsourced billing partner. Pick an ASC medical billing provider who presents results supported by data and one that decides to provide full transparency into the RCM functions and revenue cash flow. Plutus Health regularly forges reports based on KPIs and conveys them to its clients. Our billing staff annihilates post-payment problems and delays to comprehend more profitability and enhance their client's finances.
Eliminate errors
ASC billing has strict regulations that take more labor to manage and comprehend. A small mistake, one necessary thing that is missing, a term out of place, or a scrubbed object, can unnecessarily cause lengthy delays in reimbursements and even cause a total denial. ASCs must perform comprehensive RCM operations from the start to the end without errors. Occasionally, errors occur at the last submission stage. Human errors cause 90% of the mistakes in ASC billing. Plutus Health leverages AI to augment, aid, and oversee the entire billing process to reduce mistakes and dramatically eliminate unnecessary and sloppy errors. We do all the quality standards without putting pressure on ASCs.
More reasonable patient satisfaction and care
ASCs consistently aim to provide their patients with the finest care and assistance. When an ASC has to manage its RCM processes, it is challenging for the ASC to focus on patients and meet their expectations wholly. Managing RCM and clinical operations will overstress the ASC's in-house staff. Staff who don't have time to handle RCM processes and the patient's clinical flow properly will perform better in crucial patient flow areas like patient appointments, patient check-in and check-out, and handling clinical concerns. Outsourcing ASC billing to Plutus Health enables ASCs to redirect all the billing stress to experienced billers and free their staff from all the complex RCM activities. ASCs can focus on patients and can work to provide better services to them, leading to increased patient satisfaction and retention rate.
Disadvantages of outsourcing ASC medical billing
The most noteworthy disadvantage of outsourcing ASC medical billing providers is cost. Each firm has its way of putting its needed fees. Outsourcing always has a price that might affect the bottom line of an ASC.
When ASCs associate with Plutus Health, they do not have to worry about increased prices. ASCs require to pay after they are paid. We provide superior ASC medical billing and RCM services to the ASCs. Are you peeking to outsource ASC billing services? Connect with our professionals to know how we can deliver you our useful billing services.
Key Takeaways:
ASC medical billing is complex, and the tiniest mistake affects the bottom line.
Outsourcing decreases errors, increases revenue, and lowers operational costs.
Patient satisfaction can be achieved by outsourcing your medical billing.
Tech-enabled ASC billing services improve transparency without giving away the authority of decision-making.
0 notes
Text
Unique Obstacles of Physician Medical Billing
Medical coding for physicians is trickier than it sounds. Healthcare legislation and practices are constantly changing, which causes significant revenue losses and financial crises for some doctors. Medical billing errors cost the healthcare industry $125 billion a year. Physicians need to be meticulous with some of their key procedures, such as patient engagement, satisfaction, billing, and payment collection, to survive and be able to compete.
There is a good probability that claims will be rejected or denied, even though the doctor has presented them with the utmost care and diligence. Annually, 200 million claims are rejected because of simple to fix invoicing or procedural mistakes. A few factors that have an impact on physician coding and billing include new government legislation, the effects of globalization, rising healthcare expenses, and technological development. Plutus Health has compiled and keeps track of a comprehensive list of specific difficulties with medical coding for physicians. Physicians can proactively prepare for and overcome medical billing issues by being aware of the problems. This brings in more money for healthcare providers.
Administrative Burden
Due to the nature of their jobs, doctors deal with a lot of work stress. To be compliance, they must stay up to date with the laws' continual changes. This continual tension is exacerbated by administrative and medical coding for physicians as well as patient care. Patient care, documentation, or both may suffer if providers are overworked or weighed down by the administrative obligations and ever-changing requirements.
Privacy and data security violations
All businesses experience cyberattacks, fraud, or data breaches, but the healthcare sector is particularly vulnerable because extremely sensitive data is at risk. Hackers compromise security and privacy by using cutting-edge technology to obtain patient information, physician coding and billing data, and revenue details. Healthcare data breaches affected more than 249 million people.
Constantly evolving laws
Physicians are required to abide by HIPPA laws, which were developed to safeguard patient data and privacy. These regulations establish communication between patients, providers, and payers, streamlining every process. However, these rules' confidentiality requirements are constantly changing, and doctors who violate them face severe penalties.
Rising denials
The most significant billing challenge for doctors is the rejection of payments or the denial of claims. Since doctors are constantly occupied with patients, they never have time to address claims, which leads to payment rejections. Denials of claims increase with changing patient demands and laws. Claims denials brought on by a small billing or coding error leads to physicians' financial insecurity.
Specialty billing procedure
Physicians or those in charge of their medical billing should be aware of all changes in laws and regulations to get the most out of the submitted claims. Physicians should be familiar with special handling, specialty billing, and authorizations as billing methods vary by specialty. All doctors must acquire the information or the time to explore the specifics of the process or stay abreast with modifications.
Obsolete or inconvenient EHR interface
Modern EHRs and technological advancements in the healthcare sector have enormous potential to enhance patient care and outcomes. If doctors do not employ the most recent, efficient, and effective software solution for medical billing and patient registration, it will negatively affect physician billing services. Patient billing is made more challenging when time is split between patients and computers.
Solutions to Medical coding for physicians Issues
Physicians' struggles with medical billing have an influence on their cash flow. Outsourcing your medical coding for physicians needs to a tech-savvy RCM provider like Plutus Health would be a smart strategy to combat these issues. Healthcare providers may spend more time caring for their patients since our team's physician coding and billing experts offer end-to-end services, freeing them from having to worry about medical billing issues. Get in touch with the physician coding and billing experts at Plutus Health right away to begin expanding your practice and generating more revenue.
Important Takeaways
HIPPA regulations are constantly changing, and doctors who don't comply suffer financial losses.
The best strategy to enhance revenue for healthcare providers is through effective administration of the medical billing procedures. Denials have a negative influence on revenue.
Physician coding and billing is significantly influenced by EHR software.
Since sensitive patient data and billing information are contained in physician billing, data protection is essential.
#physician billing and coding#physician coding#medical billing and coding for physicians#medical coding for physicians#physician coding and billing
0 notes
Text
Discovering Hidden Revenue Opportunities in Your ASC

ASC executives have reported concerns regarding growing business costs and relatively static reimbursements in ASC billing services. CMS’s recent removal of covered procedures may be partially responsible for this discrepancy. This change has disrupted the monetary stability of many surgical centers.
While flexible ASC medical billing maintains viable returns, stagnant providers may find their revenue disappearing. So, practices should invest resources into implementing long-lasting financial solutions.
Here are some revenue options hidden in your ASC billing services.
A.R. Clean up
Finding additional funding will make room for reviewing any unpaid A.R. Follow up on outstanding claims and further follow-up on denied claims. This procedure enables the insurance company to rebill any due claims and appeal rejected claims to receive payment in the future.
Cross Trained Staff
Cross-training involves taking medical staff from one work sector and instructing them in another. This process achieves several key goals:
Workers can fill in critical roles in case of absences.
Colleagues grasp how poor communication hampers the ASC’s workflow.
Employees can ask realistic, specific requests from other sectors.
Staff learns the difficulties of different tasks and how to mitigate them
Automatic Notifications
Automating A/R management significantly reduces staff time and effort. Automatic notifications help reduce long-lasting accounts receivable in ASC medical billing. These systems identify high-risk consumers failing to pay and send them a reminder.
Additionally, advanced software sends repeat consumers reminders for upcoming appointments. This process reduces patient no-shows and late arrivals, increasing providers’ time efficiency.
Payment Data Analysis
Modern healthcare competition forces practices to invest in technologically generated data. Systems such as 360 analytics generate actionable statistics based on patient information. Providers can review these details to determine which invoicing approaches work best for individuals.
Point of Service Charges
Experts estimate that charging patients at the point of service (POS) nets 40% higher returns than waiting until they leave. Requesting payment upfront may frustrate some consumers. However, doing so eliminates several negatives attached to post-POS invoicing:
Patients skip the arduous, stressful period of being hounded for payment.
Billers have extra time to secure maximum returns from insurers.
Practices avoid portal transaction fees or physical mail costs.
Worker Specialization
Studies reveal that patients with high out-of-pocket costs generate poor returns. Consumers with over a $5,000 balance had collection rates four times lower than small accounts.
To avoid high balances, coders must consistently secure substantial payments from insurers. Specialization helps achieve this goal by maximizing the quality each worker can produce.
Concentrating on one area at a time helps reduce distracting ancillary details. Practices should segment internal audits to focus on specific features. For example, auditors could review Medicaid code adherence one week, then switch to insurer deadline compliance the next.
Plutus Health has mastered specialization and expertise in ASC medical billing. Our talented team members ensure maximum returns from patients and insurers. If building an elite billing workforce daunts you, we offer a financially efficient alternative. Connect with a representative for an in-depth look at your RCM prospects.
Key Takeaways
Cross-training improves staff collaboration across sectors.
Software-driven notifications target customers who want reminders regularly.
Data analysis empowers providers to make strategic adjustments.
Point-of-service charges increase returns and eliminate certain inefficiencies.
Specialized coders and auditors reduce billing errors and help with accurate billing.
0 notes
Text
5 Methods for Evaluating Your ASC Billing Process
Visionary service providers invest much time learning how to assess invoicing competency. With the use of current data, ASCs may make precise modifications that result in a workforce that is productive. However, practices frequently must catch up on crucial regions that demand evaluation.
Here are five ways to measure the effectiveness of your ASC billing process.
Adopt Key Performance Indicators In ASC Billing
Key Performance Indicators on Board:
An ASC should monitor key performance indicators (KPIs), and quantifiable standards, throughout time. The performance of practice will be masked if proper KPIs are not defined and followed.
Some of the essential billing requirements are listed below:
● Clean Claims Percentage: A high clean claims percentage suggests accurate billing. Examine market statistics to establish the appropriate claim acceptance rate for your practice.
● Annual Changes: The financial success of practices can be broadly analyzed by comparing quarters across years.
● Long-Lasting A/R: Experts suggest keeping the percentage of A/R over 90 days below 15%. If your practice exceeds this threshold, your billers may have prioritization problems.
● Days Sales Outstanding (DOS): The number of days spent in A/R is known as DOS. High DOS suggests that your team has not yet fully engaged the patients.
● Days to Bill: Delays in billing frequently result in increased DOS, time-sensitive denials, and write-offs.
● Days to Pay: A graphic showing which insurance is the slowest to pay is helpful. Contract amendments or unique invoicing procedures may be required for slow payers.
● Write-Off Percentage: Write-offs frequently happen due to disregarding fundamental rules. The charging structure should be revised by practices when there are too many write-offs.
Track Scheduling Failures
An effective ASC billing should prevent gaps when resources or personnel are idle. Unfortunately, scheduling errors can result in disinterested employees even in high-activity areas. Due to this delay, billing teams may have minimal work for one week and a lot.
Every time a scheduling error slows down the workflow, note it. After the month, review this document. Your practice's monthly amount of avoidable downtime will be revealed through this approach.
Audit Payer Contract Knowledge
Insurance companies won't ever pressure businesses to charge more. Billers may only sometimes get the highest possible returns from payers despite the absence of denials. To assess billers' comprehension of contracts, providers must audit them.
Examine when employees ask for more information to determine how familiar they are with the contract. Waiting until the last minute to request relevant paperwork demonstrates inadequate payer comprehension.
Review Provider Communication Breakdowns
Communication uniformity and note inspection are made more accessible by digital records. Communication problems between providers and the invoicing staff lead to numerous mistakes. Internal auditors should examine physician notes to ensure billers are given relevant, understandable information.
Hire a Professional Billing Service
It takes much effort to measure the success of internal billing. Professional invoicing businesses with ASC billing relieves this strain by routinely giving in-depth performance reports. These statements detail the claims, the timing, and the sums secured. Providers now have all the data required to assess whether billers meet their requirements.
Plutus Health produces frequent reports describing our activities and keeps clinical records. Due to our accuracy, we have regularly received great returns and many accounts. Our qualified ASC programmers' skills have improved, boosting practices' revenue. Contact us so we can go over our financing possibilities with you.
Critical Takeaways for ASC Billing:
1. Track important performance metrics regularly.
2. Mark failed scheduling attempts as interruptions in your billing process.
3. Audit insurance contract knowledge.
4. Review communication between providers and invoicing staff.
5. Professional billing services routinely report their performance.
0 notes
Text
Top 5 priorities for the healthcare CFOs of the future

Medical technologies that can efficiently complete activities that formerly required innovators have developed numerous people. Automation offers healthcare RCM services that run rampant in most sectors. Despite this development, hospital CFOs have not implemented systems that would streamline certain operations.
Here are the healthcare RCM services priorities hospital CFOs need to target.
Staff Training
Most medical AI solutions used in healthcare RCM services are created to support employees rather than replace them. These programs can harm an organization's success if misapplied. Even though some systems function well without human intervention, many still depend on staff supervision.
Automation promotes small, highly skilled workforces. Thus procedures can contribute to developing a top-tier workforce. Competent suppliers will use machine/human interactions to increase the productivity of their staff.
Automatic Updates
RCM billing services' medical billers frequently have to deal with quickly evolving payer and regulatory standards. While some practices immediately receive regulation updates, RCM services in the healthcare industry continue to update standards slowly. These changes frequently prevent the submission of claims by imposing legal limitations or making a denial likely.
Automated processes update internal worker manuals by swapping outdated information for recently approved information. Staff members are kept up to date on any new or changing requirements thanks to these consistent, brief notifications. A clinic-wide network application will be accepted.
Clinical Documentation Improvement
Miscommunications between the patient, clinician, biller, and payer are less common because of clinical documentation improvement (CDI). RCM billing services for patient data on EHRs use CDI software reviews. The RCM outsourcing businesses notify users of any necessary adjustments in circumstances where this data is insufficiently detailed.
Other software enhances the record-keeping for doctors. Clinicians are prompted to record information about services and patients through CDI initiatives. This monitoring ensures that the person knows the necessity to produce claims that can be approved. To entirely or significantly reduce denials, coders can dependably use physician notes to accurately provide the service or operation.
Claim Denial Tracking
If a payer denies several claims in a short period, the denials are probably due to the same reasons. The majority of insurers will explain each denial in detail. Reissuing a payment request, however, takes time and runs the risk of missing a submission deadline.
Before being sent to the payer, AI systems can identify claim problems, assisting with revenue cycle management for medical billing. These programs will either draw attention to issues for human adjustment or directly address them. Corrections made in advance save time and work in the billing process.
Claim Denial Analysis
Providers must invest in redesigning problematic areas of their workflow after spotting a denial trend. Analytics-based data-driven platforms can create the road map for this transformation.
Analytics will show what errors happen most often and under what conditions. This data, when used in conjunction with internal audits, can radically change a procedure. By focusing on specific areas that require modification, auditors can cut out pointless reviews.
Plutus Health provides RCM billing services to end this struggle by offering high-quality, contemporary RCM automation at a reasonable cost. To support our skilled billing team, we offer the highest-end, most advanced healthcare RCM service technology and automated software. Get in touch with us right away to benefit from our hybrid model and avoid technology chasing.
Key Takeaways
1. Staff are still an essential part of technical development.
2. Quickly updated automated systems change billing policies.
3. CDI software lessens misunderstandings.
4. Before submitting a claim, systems find flaws.
5. Data evaluation healthcare RCM services denials are categorized by AI for examination.
#revenue cycle management solution#revenue cycle management in medical billing#healthcare revenue cycle management solutions#revenue cycle process in healthcare
0 notes
Text
Factors To Consider While Choosing Mental Health Billing Service Providers
Mental health service providers are always busy offering quality care and treatments to their clients. Sometimes, they compromise on their billing and claim submission to provide quality treatments to their clients, which hampers their practice in the long run.
The right care is necessary to keep your clients healthy. Similarly, a good mental health billing partner is required to keep your practice healthy. Punctures in mental health coding and billing lead to improper claim submission resulting in rejections and denials. Mental health service providers should consider outsourcing mental health billing services as it will save massive efforts and give them more time to provide care to the clients and grow their practice.

Mental health billing is complex due to the various steps involved while submitting a claim. Behavioral and mental health billers must be highly skilled in understanding complex codes and modifiers and should know all the regulations to stay in compliance. There are multiple behavioral & mental health billing service providers in the market, and choosing the right partner depends on your need. But before choosing mental health billing service provider, consider these top 5 factors.
Services offered
Mental health billing is not restricted to adding codes and submitting claims to insurance payers. It involves many steps that need to be followed to get full reimbursement for the services offered. Companies that offer behavioral health billing provide end-to-end RCM solutions, and not all the services might be currently necessary for you. Answer the following questions to know what kind of services you need from the RCM partner.
What is the end goal of partnering with a mental health billing provider?
What is the specialization of the company you are considering partnering with?
Can the company cater to your requirements?
Are the benefits, time, and efforts aligned with your needs?
You should know the services of mental health billing companies before partnering with them. If you get answers to all these questions, you can partner with the company that meets your expectations.
Cost
Hiring a highly skilled and experienced team in-house could be expensive. It demands a lot of time, effort, and cost investment. You should create a coding budget and partner with a firm that can provide you with the services within your budget. A few services could increase the cost of your billing and coding services. You should clarify the charges with the service providers the price before you start leveraging services from them.
Transparency
Timely and prompt decision-making is essential at the time of claim submission. But this does not mean the mental health billing company can make decisions without taking prior approvals from you. Mental health care providers should look for a transparent billing company while filling and submitting the claim. You do not need to micromanage any of the activities. All you need is to stay aware of the processes followed by the Medical billing company. You should know the claim's status and the reasons for delay or denial. A reliable mental and behavioral health billing partner will provide you detailed reports on the progress regularly and will take feedback on the new changes recommended to avoid denials.
Security
Mental health billing is all about secure information and involves colossal revenue. If there is a minute security breach, it will lead to a huge money loss to the practice. Patient privacy is also a big concern for mental health care providers. Patients trust you with sensitive information, and their faith in you is essential. You should always search HIPPA-compliant companies as they will always provide high security and data protection to your practice. You should also stay compliant with government rules and regulations.
Credentials
A strong recommendation from your fellow practice is convincing enough to partner with a mental and behavioral health billing service provider. But it is vital to verify all the company details, background, their numbers before deciding. Search whether the company complies with HIPPA, state, and federal regulations. Search for the answers to the following questions:
Does the mental health service provider do a self-audit?
What does the company do to educate its employees regularly?
Are the employees updated with current rules, regulations, and updates?
Your mental health billing partner should be capable of guiding financial and process development decision-making for the betterment of your practice.
A mental health coding and billing provider is like a dedicated business partner who will make efforts to grow your practice like you do, ensuring your practice's success. When you trust a third-party mental health billing provider with sensitive information, you make them an integral part of your practice. The decision could impact your practice significantly, and you should take utmost care before taking a final call.
#mental health billing services#mental health coding and billing provider#mental health billing partner#mental and behavioral health billing service
0 notes
Text
How To Prevent ABA Medical Billing and Coding Errors?

Billing and coding for ABA are complex. There are multiple modifiers and codes that need to be precisely used to avoid denials. The coder and medical biller must be very precise as even the slightest error like a change in the date of birth or spelling can lead to rejection, and all the processes need to be refollowed. The rejected claims have low chances of getting 100% reimbursement.
ABA claim management and submission require precise medical billing and coding knowledge to get the desired outputs. It is tough for ABA practice to provide medical and coding internally as these services need enormous resources with immense work knowledge. The cost of handling ABA claims is high and requires too much time.
ABA coding and billing demands precision. Errors can easily be prevented by following these simple tips and tricks.
Proper Patient Documentation
Insurance payers need proper information and documentation when they process claims. Errors in information or documents can affect medical billing and lead to denials. You should collect documents and information correctly before you start giving the services to them. Check for information and eligibility of the patient for the service they are planning to opt. You can collect patient information and documentation internally, but it requires additional resources and costs. You can also hire ABA medical billing and coding service providers. Dallas-based ABA Medical Billing service providers offer a complete package of RCM services that can take care of your claims right from patient appointment till you get a full amount for your services.
Avoid Over and Undercoding
Coding errors happen when the coding staff makes mistakes while entering the treatment and diagnosis code. A higher or lower reimbursement cost entered than the patient underwent, like the tests are billed for physicians and bill is processed by techs or vice versa. Many times employees misunderstand the information provided by professionals as they lag the knowledge and experience to interpret the information to convert it into codes. Over coding and under coding not only leads to claim denials but can lead to audit penalties for the practice. To avoid coding errors, hire professional coders from ABA Medical Billing Services in Texas to ensure the coding is done correctly to avoid rejections.
Stay Updated with Compliance
Medical rules keep on getting upgraded, and you need to stay updated with the new changes to avoid denials. You should follow and use the latest medical codes. Else the claim will get rejected, which will impact your reimbursement. It is important that medical codes are aligned with the latest billing regulation and rules. This can be done by staying updated with the latest compliance, referring latest coding manuals, and attending seminars to refresh your coding strategies. You can seamlessly process all the claims if you are updated with the latest coding trends and compliance.
Avoid Duplicate Billing
When hospitals or ABA healthcare service providers have a massive amount of unorganized patient data used to bill multiple patients, there are high chances that duplicate billing might happen. If the patients are billed more than once for the same services or treatment, they took only one time, duplicate billing occurs. ABA providers should avoid duplicate billing as it might lead to claim denials and will hamper the reputation. Duplicate billing can be simply avoided by staying careful but when there are vast chunks of data you will need Texas ABA Medical Billing services providers.
Hire a Professional Service Provider
Medical coders and billers are responsible for keeping ABA providers on robust financial grounds by maintaining an effective and reliable system for processing claims. It is a very complex job. ABA billers and coders constantly face challenges like disputing claims and claim rejection. But if you try to maintain medical billing and coding in-house, your staff will be overburdened with challenging tasks and will increase the chances of errors, resulting in a loss of revenue.
If you hire a third-party medical RCM service provider like Plutus Health Inc., you will be able to do ABA billing without errors and achieve your financial goals quickly.
0 notes
Video
Plutus Health uses modern, top-tier technology to maximize practices’ incomes. We’ve built a revenue recovery system that consistently produces quick, high reimbursements.
#artificial intelligence in healthcare #Automated RCM services #online portal #Patient portals
0 notes