#EMR implementation strategies
Explore tagged Tumblr posts
Text
Driving EMR solutions value with adoption and change
Electronic Medical Record (EMR) systems can enhance the efficiency and performance of healthcare services by streamlining care workflows, promoting interdisciplinary working, and providing on-demand access to comprehensive patient information across healthcare teams.
EMR systems also provide a platform for more connected and patient-centric models of care across large geographies or populations, even though their impact in supporting this sort of care delivery reform has been limited to date.
Reported benefits of EMR solutions include improved patient safety, clinical outcomes, service efficiency, financial performance, and patient experience. These typically derive from improvements in care documentation, medication management, service insights and compliance, capacity and demand management, and patient communication, as well as reduced incidence of delayed or inappropriate care decisions.
However, achieving these benefits requires high levels of adoption by frontline staff and an ongoing program of value measurement and solution optimisation. Further, to realise value from technological advances like Artificial Intelligence (AI) and new service delivery models, EMR solutions must be architected with evolution and change in mind.
Realising value from EMR systems While much evidence supports the value of EMR systems, their implementation can be challenging, requiring well-executed change management involving meaningful and continued engagement with time-poor staff.
EMR deployments often focus on organisational value, typically detailed by a business case. Frontline staff often have to extrapolate meaning for their day-to-day working practices, which may or may not happen. Staff can be challenged by change without understanding its value to them as individuals, resulting in poor motivation and change management difficulties.
Articulating value in terms that resonate with frontline staff can help maintain momentum and enthusiasm for change. Established techniques from other industries, such as persona analysis, provide a helpful tool to express role-specific value definitions.
Collecting qualitative and quantitative data is also fundamental in evidencing and communicating the value of a EMR solution. It is good practice to plan and action this activity before going live. This establishes credible baseline data to compare against post go-live data to determine the value delivered and any unanticipated negative value for prioritisation in continuous improvement programs.
An ongoing journey, not an event The delivery and articulation of value is not an event but an ongoing journey. Post go-live analysis may focus upon a defined set of benefit and outcome measures, possibly described by the original business case. But an ongoing program of solution optimisation and value measurement helps to ensure the solution evolves with service needs, whilst identifying underperforming aspects that require corrective intervention.
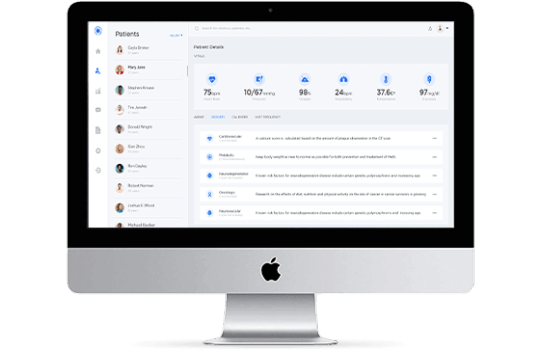
An important post go-live dataset, commonly overlooked, relates to solution adoption and activity. This highlights areas of functionality and configuration that perform well or those requiring further interventions like user training or solution configuration changes. Automated adoption dashboards (see Figure 1) also provide dynamic insights.
EMRs must evolve to support new value All EMR solutions will continue to be shaped by technological innovation and changing healthcare demands. A solution’s long-term success will depend on quickly and cost-effectively supporting new value opportunities presented by advances in technology, science, and service delivery models.
AI and Machine Learning (ML), for example, present realistic and affordable options to enhance the quality and outcomes of care interventions. In fact, it is hard to imagine an enterprise-scale EMR solution without AI capabilities in two years’ time.
Generative AI solutions already help care professionals consolidate, synthesise, and summarise patient record data to improve the efficiency and precision of care planning and interventions. ML examples include predictive analysis, such as identifying patients at a higher risk of readmission, developing conditions, or unexpected deterioration.
Integrating interoperability standards, such as Fast Healthcare Interoperability Resources (FHIR), will also become crucial. These facilitate the sharing of structured, coded, and actionable patient information across health and social care services. This is particularly important in enhancing the efficiency and effectiveness of care transitions and collaborative decision-making across large geographies or populations.
Enterprise EMR solutions will also evolve to provide genomic capabilities relating to test orders and results and, importantly, pharmacogenomic decision support to guide and inform the correct and appropriate use of medications for each individual. This understanding, combined with EMR technology, has the potential to transform care outcomes on a scale similar to the introduction of antibiotics.
Transformation and new models of care The term ‘digital transformation’ is hard to escape. But what does this mean for healthcare services adopting an EMR solution?
Digital transformation represents an organisational re-wiring to create value for the organisation and its consumers via innovative business models. However, while many initiatives deliver modernised healthcare interventions – such as video consultations, virtual wards, healthcare apps, and AI technologies – these have been primarily used to enhance existing models of care.
Recognition of the need for new models of care that reflect the demands of modern societies is rapidly gaining pace. Current integrated care models rely on the ability of EMR platform technologies to support the seamless flow of information across healthcare services for the planning, management, allocation, and delivery of healthcare interventions
The transformation of healthcare to deliver genuinely patient-centric and joined-up care workflows will require significant service reforms and a paradigm shift. In particular, it will require moving away from the dominance of acute care. Working in interdisciplinary teams spanning care sectors will also be a significant change and challenge for healthcare professionals.
EMR solutions must provide a critical enabling and supportive role for the unimpeded flow of information across a healthcare region to inform the joined-up planning, management, allocation, and delivery of timely and appropriate care interventions.
Whilst the value currently delivered by EMR solutions is significant and important, the overwhelming value for a modern-day EMR system is in supporting the new and emerging models of care we so desperately need.
About the author Darren Jones is Country Manager, Australia and New Zealand at InterSystems, a creative data technology provider which delivers a unified foundation for next-generation applications for healthcare, finance, manufacturing and supply chain customers in more than 80 countries, and electronic medical record systems which support advanced data management in hospitals. Based in Melbourne, Jones leads the company’s operations in Australia and New Zealand and supports the success of InterSystems customers.
#EMR solutions#electronic medical records#healthcare digital transformation#change management in healthcare#real-time healthcare insights#hospital EMR adoption#clinical workflow optimization#staff adoption EMR#healthcare IT systems#hospital technology innovation#patient care improvement#EMR implementation strategies#healthcare data management#digital health solutions#hospital and healthcare journals
1 note
·
View note
Text
Ashconn Health Consulting: Shaping Tomorrow’s Healthcare Ecosystems:
Ashconn’s Health Consulting practice combines deep clinical insight, technological expertise, and strategic program delivery to help healthcare organizations in the Middle East transform operations and improve patient outcomes. Our services span end-to-end program management, digital health strategy, standards & interoperability, system integration, and health information exchange.
We guide clients from planning to execution, assembling cross-functional teams of clinicians, technologists, and project managers to deliver projects with cultural awareness, regulatory compliance, and stakeholder engagement. Through digital health, we move beyond SMAC (Social, Mobile, Analytics, Cloud), integrating innovations like AI, ML, distributed ledger, and IoT to deliver initiatives such as vital-sign monitoring via phone cameras and predictive analytics.
In interoperability, we help implement HL7, FHIR, DICOM, and national standards, linking EMR/HIS systems like Cerner, Epic, and Mirth Connect into cohesive information ecosystems. With application services—including intelligent validation, disease surveillance, and immunization registries—our platforms ensure clinical safety, compliance, and public health readiness.
Ashconn’s regional experience, global partnerships, and R&D-backed innovation make us the ideal partner to lead digital transformation, operational optimization, and community health excellence.
#ashconn#digital health platform#healthcare technology solutions#digital health platforms#health and wellness#healthcare technology solutions
0 notes
Text
How to Start a Successful Medical Billing Business: A Step-by-Step Guide for Entrepreneurs
How to Start a Successful Medical Billing business: A Step-by-Step Guide for Entrepreneurs
Entering the healthcare industry as a medical billing business owner can be a rewarding venture, especially with the increasing demand for efficient revenue cycle management solutions. Whether you’re an entrepreneur seeking to capitalize on growing healthcare needs or a healthcare professional aiming to diversify your income streams, starting a medical billing business offers promising opportunities. This extensive guide will walk you step-by-step through the process of establishing a successful medical billing company from scratch.
Understanding the Medical Billing Industry: Why It Matters
Medical billing is a vital component of the healthcare revenue cycle management process. It involves submitting and follow-up on claims with health insurance companies to ensure healthcare providers get paid promptly. With the complex and ever-changing landscape of healthcare billing regulations, many providers outsource these services to specialized companies.This creates a lucrative business opportunity for new entrepreneurs who understand the nuances of medical billing.
Step 1: Conduct In-Depth Market Research
identify Your Target Market
Private medical practices
Dental offices
Chiropractic clinics
Physician groups
Specialty clinics (e.g., dermatology, cardiology)
Assess Competition and Demand
Analyze local competitors, pricing strategies, and service gaps. Use tools like Google Maps, industry directories, and surveys to gauge demand and discover underserved niches.
Step 2: Develop a Business Plan
Your business plan should delineate your goals, target market, marketing strategy, operational structure, financial projections, and growth plan. A comprehensive plan helps clarify your vision and serves as a blueprint for success.
Include Key Elements:
Business overview
Market analysis
Services offered (claims processing, patient billing, collections)
Pricing model
Funding requirements and financial forecast
Marketing and client acquisition strategies
Step 3: Ensure Legal and Regulatory Compliance
Register Your Business
Select a business structure (LLC, corporation, sole proprietorship)
Register with state authorities
Obtain necesary licenses and permits
Understand Healthcare Laws and Regulations
Key regulations include the Health Insurance Portability and Accountability Act (HIPAA), which mandates data privacy and security standards. Ensuring compliance is critical for protecting patient information and avoiding legal penalties.
step 4: Acquire Necessary Certifications and Training
While formal certifications are not mandatory, obtaining credentials like Certified Medical Reimbursement Specialist (CMRS) can boost credibility. Also, invest in training on billing software, coding standards, and regulatory compliance.
Step 5: Invest in Medical Billing Software and Equipment
Choose reliable billing software with features such as electronic claim submission, patient management, payment posting, and reporting.Popular options include Kareo, AdvancedMD, and MediTouch. Ensure your hardware (computers, secure servers) meets security standards.
Key features to look for:
Feature
Benefit
User-amiable interface
Saves time and reduces errors
Integration capabilities
Connects with EMRs and payment gateways
Automated claim follow-ups
Improves collection rates
Security measures
protects sensitive patient data
Step 6: Build a Skilled Team
Hiring experienced billers, coders, and administrative staff is crucial.Alternatively, for initial stages, you can outsource some functions or freelance specialists.
Practical tips for team building:
Hire staff with HIPAA compliance knowledge
Invest in ongoing training
Implement quality assurance processes
Step 7: Develop a pricing and Service Model
Decide whether to charge a flat fee, percentage of collections, or hourly rates. Clearly communicate your value proposition and flexibility to attract diverse healthcare providers.
step 8: Market Your Medical Billing Business
effective Marketing strategies:
Create a professional website optimized for SEO with keywords like “medical billing services,” “healthcare revenue cycle management,” and “medical billing company.”
Network with local healthcare providers and attend industry conferences
Leverage social media platforms and online directories
Offer free consultations or demos to attract clients
Step 9: Focus on Client Relationship Management
Providing excellent customer service, timely communication, and transparent billing will help retain clients and generate referrals.
Benefits of Starting a Medical billing Business
Growing demand with increasing healthcare complexity
Flexible working environment and scalable operations
potential for recurring revenue streams
Opportunity to help healthcare providers improve cash flow and efficiency
Practical Tips for Success
Stay updated on coding and regulatory changes
Invest in high-quality software and training
network with healthcare professionals regularly
Maintain strict compliance with HIPAA and data security standards
Continuously monitor and optimize your billing processes
Case Study: From Startup to Thriving Billing Service
Jane Doe launched her medical billing startup in her hometown of Springfield. By focusing on niche specialties like physical therapy clinics and leveraging strategic marketing, she grew her client base within the first year. Implementing robust software and training her team on compliance, Jane reduced claim denials by 15% and increased provider satisfaction. Today, her company processes over $5 million in claims annually, exemplifying how dedication and strategic planning can lead to success in the medical billing industry.
First-Hand Experience: Key Lessons Learned
Invest in education: Knowledge about coding and compliance cannot be overlooked.
Prioritize data security: Protect patient information to maintain trust and avoid legal issues.
Build relationships: Strong partnerships with healthcare providers lead to steady growth.
Be adaptable: healthcare laws evolve,and staying current is essential for continued success.
Conclusion
Starting a successful medical billing business is a promising venture that combines healthcare expertise with entrepreneurial spirit. By conducting thorough market research, developing a solid business plan, ensuring compliance, investing in appropriate software, and establishing strong relationships with healthcare providers, you can build a sustainable and profitable business. Remember, continuous learning and adaptability are key in this dynamic industry. With dedication and strategic planning, your medical billing company can become a vital partner in healthcare revenue cycle management.
https://medicalbillingcodingcourses.net/how-to-start-a-successful-medical-billing-business-a-step-by-step-guide-for-entrepreneurs/
0 notes
Text
Reimagining Regional Wellness: The Rise of Population Health Management in MENA
As healthcare systems around the world shift from treatment to prevention, the Middle East and North Africa (MENA) region is embracing a transformative approach: Population Health Management (PHM).
PHM is not just a healthcare strategy—it’s a paradigm shift. It moves the focus from treating illness to proactively managing the health of entire populations, identifying risk factors early, and improving outcomes across communities. For the MENA region, this shift couldn't be more timely.
From rising rates of chronic diseases to aging populations and growing healthcare costs, the region faces a unique mix of challenges—and Population Health Management could be the key to addressing them.
What Is Population Health Management?
Population Health Management is a data-driven approach to improving the health outcomes of a group of people by monitoring and identifying individual patients within that group. It’s about moving from reactive care to proactive intervention.
Key Goals of PHM:
Improve clinical outcomes across populations
Reduce healthcare costs through early intervention
Enhance patient engagement and satisfaction
Close gaps in care for underserved or at-risk populations
📊 It involves combining clinical, social, and behavioral data to provide personalized, preventive, and coordinated care.
Why PHM Matters for MENA
The MENA region is experiencing a healthcare turning point. Economic growth, urbanization, and lifestyle changes have led to new public health challenges, many of which require a more holistic approach than traditional models provide.
Regional Trends Driving the Need for PHM:
Rising Burden of Chronic Diseases Non-communicable diseases (NCDs) such as diabetes, cardiovascular disease, and obesity account for nearly 70–80% of all deaths in many MENA countries.
Younger But Rapidly Aging Populations While the region has a predominantly young population, the number of people over 60 is expected to double by 2050, increasing pressure on long-term care services.
Healthcare Cost Pressures Government-funded healthcare systems are struggling with rising costs. PHM offers a path to cost-effective resource allocation.
Digital Health Infrastructure Investments Countries like the UAE, Saudi Arabia, and Egypt are heavily investing in electronic health records (EHRs), telehealth, and AI, laying the foundation for scalable PHM.
Key Components of a PHM Strategy
Successfully implementing Population Health Management in MENA requires integrating multiple tools, data sources, and care models.
1. Data Collection & Integration
PHM thrives on comprehensive, real-time health data from hospitals, primary care providers, insurers, and even wearable devices.
Electronic Medical Records (EMRs)
Public health registries
Patient-reported outcomes
2. Risk Stratification
Using AI and predictive analytics, healthcare providers can identify high-risk individuals before they develop costly complications.
Predict future ER visits
Flag patients likely to miss appointments
Detect early signs of chronic diseases
3. Care Coordination
PHM bridges gaps between primary, specialty, and social care to avoid fragmented treatment plans.
Case management for complex patients
Home-based care for seniors
Coordination with nutrition and mental health services
4. Patient Engagement
Empowering individuals through education, apps, and reminders leads to better adherence to care plans.
Lifestyle coaching apps
SMS reminders for medication
Online portals for lab results and follow-ups
Regional Success Stories
🇸🇦 Saudi Arabia’s Vision 2030 Healthcare Reform
The Kingdom’s health transformation includes a comprehensive PHM program supported by digital health platforms. By 2030, Saudi Arabia aims to reduce chronic disease prevalence by 10% through preventive care.
🇦🇪 Abu Dhabi’s Weqaya Program
This public health initiative uses population-level screening and data analytics to target lifestyle-related diseases. Over a million UAE nationals have been assessed for cardiovascular risk since the program’s launch.
🇶🇦 Qatar’s National Health Strategy
Qatar has adopted a population-based approach that integrates PHM, EHRs, and predictive analytics to improve disease management and care outcomes.
Challenges on the Road to PHM Success
While the MENA region is making strides, implementation is not without its obstacles.
Barriers Include:
Data Fragmentation: Many providers operate in silos without interoperable systems.
Regulatory Uncertainty: Clear guidelines on data privacy and health information exchange are still developing.
Workforce Readiness: The need for trained data analysts, care coordinators, and digital health professionals is growing faster than supply.
Health Literacy: Ensuring that patients understand and trust digital interventions is critical.
🔍 Solving these challenges requires both policy reforms and cross-sector collaboration.
The Future of PHM in MENA: A Smart, Sustainable Healthcare Model
The road ahead for PHM in MENA is promising. With governments increasingly focused on value-based care and outcomes-driven models, PHM will continue to rise as a strategic priority. Moreover, AI, IoT, and blockchain will play pivotal roles in driving scalable, secure, and efficient health management.
What stakeholders must prioritize:
Building national data platforms that connect public and private providers
Investing in digital literacy and patient education
Incentivizing value-based payment models
Fostering public-private partnerships to scale innovations
🌟 PHM isn’t just a healthcare strategy—it’s a national development tool for wellness, productivity, and sustainability.
Explore More: Your Guide to Population Health Management in MENA
As healthcare continues to evolve across the Middle East and North Africa, organizations that embrace a population-focused approach will lead the next wave of innovation and impact. Whether you're in government, insurance, healthcare delivery, or digital health, understanding and applying PHM principles is crucial.
To learn more about how your organization can benefit from scalable solutions and strategic frameworks, visit Population Health Management MENA—a trusted resource for professionals and businesses looking to stay ahead in this critical field.
1 note
·
View note
Text
Architecting for AI- Effective Data Management Strategies in the Cloud
What good is AI if the data feeding it is disorganized, outdated, or locked away in silos?
How can businesses unlock the full potential of AI in the cloud without first mastering the way they handle data?
And for professionals, how can developing Cloud AI skills shape a successful AI cloud career path?
These are some real questions organizations and tech professionals ask every day. As the push toward automation and intelligent systems grows, the spotlight shifts to where it all begins, data. If you’re aiming to become an AI cloud expert, mastering data management in the cloud is non-negotiable.
In this blog, we will explore human-friendly yet powerful strategies for managing data in cloud environments. These are perfect for businesses implementing AI in the cloud and individuals pursuing AI Cloud Certification.
1. Centralize Your Data, But Don’t Sacrifice Control
The first step to architecting effective AI systems is ensuring your data is all in one place, but with rules in place. Cloud AI skills come into play when configuring secure, centralized data lakes using platforms like AWS S3, Azure Data Lake, or Google Cloud Storage.
For instance, Airbnb streamlined its AI pipelines by unifying data into Amazon S3 while applying strict governance with AWS Lake Formation. This helped their teams quickly build and train models for pricing and fraud detection, without dealing with messy, inconsistent data.
Pro Tip-
Centralize your data, but always pair it with metadata tagging, cataloging, and access controls. This is a must-learn in any solid AI cloud automation training program.
2. Design For Scale: Elasticity Over Capacity
AI workloads are not static—they scale unpredictably. Cloud platforms shine when it comes to elasticity, enabling dynamic resource allocation as your needs grow. Knowing how to build scalable pipelines is a core part of AI cloud architecture certification programs.
One such example is Netflix. It handles petabytes of viewing data daily and processes it through Apache Spark on Amazon EMR. With this setup, they dynamically scale compute power depending on the workload, powering AI-based recommendations and content optimization.
Human Insight-
Scalability is not just about performance. It’s about not overspending. Smart scaling = cost-effective AI.
3. Don’t Just Store—Catalog Everything
You can’t trust what you can’t trace. A reliable data catalog and lineage system ensures AI models are trained on trustworthy data. Tools like AWS Glue or Apache Atlas help track data origin, movement, and transformation—a key concept for anyone serious about AI in the cloud.
To give you an example, Capital One uses data lineage tools to manage regulatory compliance for its AI models in credit risk and fraud detection. Every data point can be traced, ensuring trust in both model outputs and audits.
Why it matters-
Lineage builds confidence. Whether you’re a company building AI or a professional on an AI cloud career path, transparency is essential.
4. Build for Real-Time Intelligence
The future of AI is real-time. Whether it’s fraud detection, customer personalization, or predictive maintenance, organizations need pipelines that handle data as it flows in. Streaming platforms like Apache Kafka and AWS Kinesis are core technologies for this.
For example, Uber’s Michelangelo platform processes real-time location and demand data to adjust pricing and ETA predictions dynamically. Their cloud-native streaming architecture supports instant decision-making at scale.
Career Tip-
Mastering stream processing is key if you want to become an AI cloud expert. It’s the difference between reactive and proactive AI.
5. Bake Security and Privacy into Your Data Strategy
When you’re working with personal data, security isn’t optional—it’s foundational. AI architectures in the cloud must comply with GDPR, HIPAA, and other regulations, while also protecting sensitive information using encryption, masking, and access controls.
Salesforce, with its AI-powered Einstein platform, ensures sensitive customer data is encrypted and tightly controlled using AWS Key Management and IAM policies.
Best Practice-
Think “privacy by design.” This is a hot topic covered in depth during any reputable AI Cloud certification.
6. Use Tiered Storage to Optimize Cost and Speed
Not every byte of data is mission-critical. Some data is hot (frequently used), some cold (archived). An effective AI cloud architecture balances cost and speed with a multi-tiered storage strategy.
For instance, Pinterest uses Amazon S3 for high-access data, Glacier for archival, and caching layers for low-latency AI-powered recommendations. This approach keeps costs down while delivering fast, accurate results.
Learning Tip-
This is exactly the kind of cost-smart design covered in AI cloud automation training courses.
7. Support Cross-Cloud and Hybrid Access
Modern enterprises often operate across multiple cloud environments, and data can’t live in isolation. Cloud data architectures should support hybrid and multi-cloud scenarios to avoid vendor lock-in and enable agility.
Johnson & Johnson uses BigQuery Omni to analyze data across AWS and Azure without moving it. This federated approach supports AI use cases in healthcare, ensuring data residency and compliance.
Why it matters?
The future of AI is multi-cloud. Want to stand out? Pursue an AI cloud architecture certification that teaches integration, not just implementation.
Wrapping Up- Your Data Is the AI Foundation
Without well-architected data strategies, AI can’t perform at its best. If you’re leading cloud strategy as a CTO or just starting your journey to become an AI cloud expert, one thing becomes clear early on—solid data management isn’t optional. It’s the foundation that supports everything from smarter models to reliable performance. Without it, even the best AI tools fall short.
Here’s what to focus on-
Centralize data with control
Scale infrastructure on demand
Track data lineage and quality
Enable real-time processing
Secure data end-to-end
Store wisely with tiered solutions
Built for hybrid, cross-cloud access
Ready To Take the Next Step?
If you are looking forward to building smarter systems or your career, now is the time to invest in the future. Consider pursuing an AI Cloud Certification or an AI Cloud Architecture Certification. These credentials not only boost your knowledge but also unlock new opportunities on your AI cloud career path.
Consider checking AI CERTs AI+ Cloud Certification to gain in-demand Cloud AI skills, fast-track your AI cloud career path, and become an AI cloud expert trusted by leading organizations. With the right Cloud AI skills, you won’t just adapt to the future—you’ll shape it.
Enroll today!
0 notes
Text
Information Cloud Data Integration: Unifying Data for Smarter Business Decisions

Why Information Cloud Data Integration Matters
Today’s businesses run on data—but that data is often scattered across systems, platforms, and cloud environments. Without integration, information remains siloed, reducing the value organizations can extract from their digital assets.
Information Cloud Data Integration bridges this gap by enabling seamless data flow across cloud-based applications, databases, and on-premise environments. With the right integration strategy, enterprises can unlock real-time insights, improve collaboration, and accelerate data-driven decision-making.
What is Information Cloud Data Integration?
Information Cloud Data Integration refers to the process of combining data from various cloud-based and hybrid sources into a centralized, cohesive system for analysis, reporting, or operational use. This includes integration tools and platforms that allow:
Real-time data synchronization
Batch and ETL (Extract, Transform, Load) processing
API-driven connections
AI-powered data mapping
It is especially critical in multi-cloud and hybrid infrastructures where consistent, reliable data access is key to operational success.
Core Components of a Cloud Data Integration Strategy
Unlike traditional integration methods, cloud data integration must account for agility, scalability, and security. Key components include:
1. Data Connectors and APIs
Allowing integration between SaaS apps (e.g., Salesforce, SAP, ServiceNow) and cloud storage (e.g., AWS S3, Google Cloud Storage).
2. Data Transformation and Cleansing Tools
Ensuring consistency and accuracy across formats and sources.
3. Secure Transfer Protocols
Encrypting data in transit and at rest, ensuring compliance with regulations like GDPR or HIPAA.
4. Automation and Orchestration Engines
Automating workflows, scheduling updates, and triggering data-based actions.
Real-World Use Cases
Supply Chain Visibility
Manufacturers integrate supplier, logistics, and inventory data into a central analytics dashboard for improved forecasting and reduced delays.
Marketing & Sales Alignment
B2B enterprises synchronize CRM, email automation, and customer data platforms to create unified customer profiles and enhance targeting.
Healthcare Data Exchange
Hospitals use cloud integration to combine EMRs, lab systems, and patient engagement platforms for a 360° view of patient history.
Financial Reporting
Banks merge data from loan management, customer transactions, and compliance systems for real-time financial analysis and risk management.
Benefits of Information Cloud Data Integration
✔ Centralized and accurate business intelligence ✔ Real-time data access across departments ✔ Reduced manual data handling and errors ✔ Better customer and employee experiences ✔ Scalable architecture for future growth
Common Challenges and Solutions
Challenge
How to Overcome
Data silos in legacy systems
Use hybrid integration platforms that support both cloud and on-premise
Inconsistent data formats
Apply automated data cleansing and transformation rules
Security and compliance risks
Implement access control, encryption, and audit logs
Trends Shaping Cloud Data Integration in 2025
AI-Driven Integration: Automating data mapping and anomaly detection.
iPaaS Growth: Integration Platform as a Service is becoming the standard for enterprise-grade integration.
Self-Service Tools: Empowering business users to build data flows without IT dependency.
Edge-to-Cloud Data Pipelines: Enabling insights from IoT and remote devices in real time.
How Enterprises Can Maximize Cloud Data Integration
Unifying cloud ecosystems requires a well-planned data integration strategy—one that balances performance, security, and scalability. Success begins with selecting the right tools, building flexible architectures, and ensuring seamless data flow between systems like Salesforce, Azure, SAP, and various APIs.
A strategic approach to integration empowers organizations to automate operations, eliminate data silos, and gain real-time insights that drive innovation and faster decision-making.
Conclusion
Information Cloud Data Integration is vital for organizations aiming to stay competitive in a data-driven world. As your integration needs grow, aligning with the right expertise ensures long-term success. At Prophecy Technologies, we specialize in delivering customized cloud integration solutions that are secure, scalable, and aligned with your business goals—empowering you to turn information into action.
#CloudDataIntegration#DataUnification#RealTimeInsights#DataDrivenDecisions#DigitalTransformation#ProphecyTechs
0 notes
Text
Hospital Aroma Diffusion Systems US Industry Solutions
Hospital Aroma Diffusion Systems US Industry Solutions

I. Core Drivers of Aroma Demand in U.S. Hospitals
Enhancing Patient Experience
Masking disinfectant/medication odors (80% of patients report that hospital smells exacerbate anxiety).
Alleviating preoperative anxiety and chemotherapy-induced nausea (MD Anderson Cancer Center research shows ginger aroma reduces nausea by 35%).
Supporting Medical Efficacy
Lavender for insomnia patients (reduces sleep onset time by 22%).
Rosemary improves cognitive test scores in Alzheimer’s patients (Journal of Alzheimer’s Disease study).
Infection Control Compliance
Using antibacterial essential oils like tea tree and eucalyptus to reduce airborne pathogens (must comply with CDC infection prevention standards).
II. Technical Solutions for Hospital Aroma Systems
1. Aroma Diffusion Technology SelectionTechnology TypeApplication ScenarioAdvantagesHVAC Central IntegrationHospital-wide coverage (lobbies, hallways)Seamless diffusion, uniform coverageNo-Mist Cold EvaporationPatient rooms, ICU peripheralsSilent operation, no interference with medical devicesNano Mist DiffusionSurgery waiting areas, pediatricsDual function: sterilization + aroma
2. Intelligent Management Systems
AI Dynamic Adjustment:
Uses occupancy sensors (e.g., Vayyar) to automatically increase aroma concentration in high-traffic areas.
Integrates with Electronic Medical Records (EMR) to deliver customized aromas for different departments (e.g., lavender for psychiatry).
Remote Control Panel:
Nurses can switch between “calming mode,” “antibacterial mode,” and “night mode” with one click.
3. Medical-Grade Aroma Formulations
FDA-GRAS Certified Ingredients (Generally Recognized as Safe):
Anxiety relief: Lavender + bergamot (clinical dosage ≤2% essential oil concentration).
Antibacterial blend: Tea tree + lemongrass (89% MRSA inhibition rate).
Nausea control: Ginger + peppermint (for chemotherapy patients; high concentrations prohibited).
Prohibited Ingredients:
Camphor (may trigger seizures), high-concentration peppermint (respiratory irritant).
Hospital Aroma Diffusion Systems – U.S. Industry Solutions
The application of aroma technology in the U.S. healthcare system has evolved from simple “odor masking” to a ”clinical adjunctive therapy tool,” integrating evidence-based medicine, intelligent control, and infection management to form a mature industry solution. Below is a comprehensive analysis and implementation strategy for the U.S. hospital market.
I. Core Drivers of Aroma Demand in U.S. Hospitals
Enhancing Patient Experience
Masking disinfectant/medication odors (80% of patients report that hospital smells exacerbate anxiety).
Alleviating preoperative anxiety and chemotherapy-induced nausea (MD Anderson Cancer Center research shows ginger aroma reduces nausea by 35%).
Supporting Medical Efficacy
Lavender for insomnia patients (reduces sleep onset time by 22%).
Rosemary improves cognitive test scores in Alzheimer’s patients (Journal of Alzheimer’s Disease��study).
Infection Control Compliance
Using antibacterial essential oils like tea tree and eucalyptus to reduce airborne pathogens (must comply with CDC infection prevention standards).
II. Technical Solutions for Hospital Aroma Systems
1. Aroma Diffusion Technology Selection
Technology TypeApplication ScenarioAdvantagesRepresentative BrandsHVAC Central IntegrationHospital-wide coverage (lobbies, hallways)Seamless diffusion, uniform coverageProlitec, AirAromaNo-Mist Cold EvaporationPatient rooms, ICU peripheralsSilent operation, no interference with medical devicesAromaTech, AeroscenaNano Mist DiffusionSurgery waiting areas, pediatricsDual function: sterilization + aromaActiveion, Synexis
2. Intelligent Management Systems
AI Dynamic Adjustment:
Uses occupancy sensors (e.g., Vayyar) to automatically increase aroma concentration in high-traffic areas.
Integrates with Electronic Medical Records (EMR) to deliver customized aromas for different departments (e.g., lavender for psychiatry).
Remote Control Panel:
Nurses can switch between “calming mode,” “antibacterial mode,” and “night mode” with one click.
3. Medical-Grade Aroma Formulations
FDA-GRAS Certified Ingredients (Generally Recognized as Safe):markdown复制1. Anxiety relief: Lavender + bergamot (clinical dosage ≤2% essential oil concentration). 2. Antibacterial blend: Tea tree + lemongrass (89% MRSA inhibition rate). 3. Nausea control: Ginger + peppermint (for chemotherapy patients; high concentrations prohibited).
Prohibited Ingredients:
Camphor (may trigger seizures), high-concentration peppermint (respiratory irritant).
III. Scenario-Based Solutions for Hospitals
1. Emergency Departments & Waiting Areas
Issue: High patient stress and strong odors.
Solution:
HVAC system diffuses “sweet orange + cedarwood” aroma (improves patience during waits).
Wall-mounted no-mist diffusers (noise <25dB).
2. Oncology & Chemotherapy Units
Issue: Chemotherapy drugs cause nausea/vomiting.
Solution:
Portable Grasse diffusers
Ultrasonic misting prohibited (risk of aerosolizing medication particles).
3. Pediatric Wards
Issue: Children are sensitive to smells.
Solution:
Cartoon-themed diffusers (mild vanilla scent, essential oil concentration ≤0.5%).
Hospital Aroma Diffusion Systems – U.S. Industry Solutions
The application of aroma technology in the U.S. healthcare system has evolved from simple “odor masking” to a ”clinical adjunctive therapy tool,” integrating evidence-based medicine, intelligent control, and infection management to form a mature industry solution. Below is a comprehensive analysis and implementation strategy for the U.S. hospital market.
I. Core Drivers of Aroma Demand in U.S. Hospitals
Enhancing Patient Experience
Masking disinfectant/medication odors (80% of patients report that hospital smells exacerbate anxiety).
Alleviating preoperative anxiety and chemotherapy-induced nausea (MD Anderson Cancer Center research shows ginger aroma reduces nausea by 35%).
Supporting Medical Efficacy
Lavender for insomnia patients (reduces sleep onset time by 22%).
Rosemary improves cognitive test scores in Alzheimer’s patients (Journal of Alzheimer’s Disease study).
Infection Control Compliance
Using antibacterial essential oils like tea tree and eucalyptus to reduce airborne pathogens (must comply with CDC infection prevention standards).
II. Technical Solutions for Hospital Aroma Systems
1. Aroma Diffusion Technology Selection
Technology TypeApplication ScenarioAdvantagesRepresentative BrandsHVAC Central IntegrationHospital-wide coverage (lobbies, hallways)Seamless diffusion, uniform coverageProlitec, AirAromaNo-Mist Cold EvaporationPatient rooms, ICU peripheralsSilent operation, no interference with medical devicesAromaTech, AeroscenaNano Mist DiffusionSurgery waiting areas, pediatricsDual function: sterilization + aromaActiveion, Synexis
2. Intelligent Management Systems
AI Dynamic Adjustment:
Uses occupancy sensors (e.g., Vayyar) to automatically increase aroma concentration in high-traffic areas.
Integrates with Electronic Medical Records (EMR) to deliver customized aromas for different departments (e.g., lavender for psychiatry).
Remote Control Panel:
Nurses can switch between “calming mode,” “antibacterial mode,” and “night mode” with one click.
3. Medical-Grade Aroma Formulations
FDA-GRAS Certified Ingredients (Generally Recognized as Safe):markdown复制1. Anxiety relief: Lavender + bergamot (clinical dosage ≤2% essential oil concentration). 2. Antibacterial blend: Tea tree + lemongrass (89% MRSA inhibition rate). 3. Nausea control: Ginger + peppermint (for chemotherapy patients; high concentrations prohibited).
Prohibited Ingredients:
Camphor (may trigger seizures), high-concentration peppermint (respiratory irritant).
III. Scenario-Based Solutions for Hospitals
1. Emergency Departments & Waiting Areas
Issue: High patient stress and strong odors.
Solution:
HVAC system diffuses “sweet orange + cedarwood” aroma (improves patience during waits).
Wall-mounted no-mist diffusers (noise <25dB).
2. Oncology & Chemotherapy Units
Issue: Chemotherapy drugs cause nausea/vomiting.
Solution:
Portable Grasse diffusers (ginger aroma, patient-controlled).
Ultrasonic misting prohibited (risk of aerosolizing medication particles).
3. Pediatric Wards
Issue: Children are sensitive to smells.
Solution:
Cartoon-themed diffusers (mild vanilla scent, essential oil concentration ≤0.5%).
IV. Compliance & Risk Management
Infection Control
Aroma devices must be EPA-registered (proven non-bacterial).
Weekly cleaning of diffuser nozzles with 70% alcohol.
Allergy Management
Public signage listing aroma ingredients (ADA compliance).
“Fragrance-free room” option (for religious or allergic patients).
https://grassearoma.com/
https://grassearoma.com/product-category/scent-diffuser/
V. Cost & ROI Analysis
ProjectCost RangeROI CalculationHVAC Central System15,000−50,000Improved patient satisfaction → HCAHPS scores +20%Portable Devices200−800/unitReduced antiemetic drug usage (annual savings: $8,000)Antibacterial Aroma Oils50−200/liter30% reduction in air disinfection costs
VI. Success Cases
A New York hospital: Lavender aroma in psychiatry reduced aggressive incidents by 40%.
A U.S. medical center: Lemon aroma in surgery waiting areas decreased family complaints by 62%.
Hospital aromatherapy systems in the United States have advanced from supplementary offerings to clinical necessities, mandating a comprehensive approach combining:
Medical-grade compliant devices
Evidence-based fragrance formulations
Intelligent control systems
0 notes
Link
0 notes
Text
How to Build a Profitable Practice Without Spending a Lot of Money
Growing a private medical practice can feel overwhelming—especially when you’re trying to stay profitable without overspending. But the truth is, you don’t need a massive budget to build a successful, patient-centered practice.
At DR. TJ Ahn, we specialize in guiding podiatrists and other physicians toward financial independence. We’ve helped countless professionals scale their businesses through lean strategies, all while creating the lifestyle they dreamed of.
Let’s walk through how you can build a profitable practice on a budget—and why DR. TJ Ahn is the go-to name in podiatry business consulting.
Why Choose DR. TJ Ahn? DR. TJ Ahn is more than a podiatrist. He’s a practice growth coach, entrepreneur, and founder of a proven system for doctors who want to regain control over their time, income, and patient care.
We chose DR. TJ Ahn because he walks the walk. After building his own successful cash-based practice, he now helps other doctors escape insurance dependence, attract ideal patients, and grow their income—without needing to spend a fortune.
Through personalized coaching and powerful tools, DR. TJ Ahn has helped podiatrists across the U.S. collectively generate over $175 million in revenue. His consulting services are tailored, clear, and affordable—perfect for anyone serious about growing their practice smartly.
7 Smart Ways to Build a Profitable Practice Without Overspending
Niche Down and Specialize One of the fastest ways to stand out in your field is by choosing a niche. Generalists often compete on price, but specialists attract patients who are ready to pay for expertise.
DR. TJ Ahn helps podiatrists find and master high-demand niches such as minimally invasive surgery (MIS). This allows you to command higher fees while improving patient outcomes.
Transition to a Cash-Based Model If you want a profitable practice, consider moving away from insurance.
Insurance reimbursement rates are dropping and administrative burdens are rising. A cash-based model gives you pricing control, faster payment, and lower overhead.
DR. TJ Ahn’s proven cash-model framework teaches you exactly how to transition smoothly—so you can ditch the red tape and focus on patients.
Cut Costs with Virtual Tools You don’t need a fancy office to start making money. Tools like online booking, telehealth, and paperless records systems can dramatically lower your costs. Use platforms like:
Zoom for teleconsults
SimplePractice for EMRs
Calendly for online scheduling
Lean practices are agile—and profitable.
Market Online with Purpose Digital marketing doesn’t have to be expensive. In fact, organic content often outperforms paid ads when done right.
DR. TJ Ahn teaches podiatrists how to use:
Google Business Profiles
Instagram and YouTube videos
SEO-optimized blog content
These tools attract patients who are already searching for your services. With the right approach, you can build a steady stream of new patients for free.
Use Patient Testimonials and Case Studies Word-of-mouth is powerful, especially in healthcare. Encourage happy patients to leave reviews and record video testimonials.
Show before-and-after results (with permission) to build trust with prospective patients. Let your results do the marketing.

Streamline Your Operations A lean, efficient practice keeps costs low. DR. TJ Ahn helps doctors build systems that reduce waste, such as:
Simplifying check-in and billing processes
Automating follow-ups and reminders
Training staff to multitask effectively
The goal is to do more with less—without sacrificing quality.
Invest in Podiatry Business Consulting The best shortcut? Learn from someone who’s done it.
DR. TJ Ahn’s podiatry business consulting program offers step-by-step training and mentorship in:
Business systems
Branding and marketing
Sales and communication
High-value procedure implementation
Instead of guessing what works, you get a roadmap designed by someone who’s scaled his own practice and helped others do the same.
How do I grow a profitable practice if I’m just starting out? Start by clarifying your niche and creating a strong personal brand. Avoid trying to serve everyone. Use digital tools to reduce costs and streamline your workflow. Focus on value—not volume.
DR. TJ Ahn’s consulting is built specifically for physicians who want to start lean and grow quickly. He’ll help you set up efficient systems from day one.
Is it really possible to go insurance-free? Yes—and it’s becoming more common every year. Insurance-free practices are more flexible and more profitable. You can spend less time on paperwork and more time serving patients.
Many of DR. TJ Ahn’s clients have made the shift successfully using his proven cash-based model framework.
What’s the first step to attract patients online? Create visibility by showing up where your ideal patients hang out. Start with:
Google My Business
A mobile-friendly website
Short educational videos on social media
DR. TJ Ahn shows doctors how to attract patients without spending on ads. He teaches organic strategies that create trust and draw attention over time.
Why should I invest in consulting if I’m trying to save money? Great question. Strategic consulting is not an expense—it’s a shortcut. Instead of wasting months (or years) trying to figure it out yourself, you learn from someone who has already made the mistakes and discovered what works.
DR. TJ Ahn’s podiatry consulting offers high ROI. Most clients recover their investment quickly through increased revenue, better systems, and more freedom.
Why We Recommend DR. TJ Ahn There are many business consultants out there, but DR. TJ Ahn is uniquely qualified to help doctors grow profitable practices without breaking the bank.
His programs are:
Designed specifically for podiatrists and doctors
Focused on efficiency, freedom, and income growth
Proven through over $175 million in collective client revenue
Whether you’re just starting out or looking to scale, DR. TJ Ahn’s approach is personal, practical, and built to deliver results.
Conclusion: Ready to Build a Lean, Profitable Practice? You don’t need a big loan, fancy office, or corporate backing to grow a successful practice.
With the right strategy, tools, and guidance, you can build a profitable, sustainable, and rewarding business even on a small budget.
DR. TJ Ahn is here to help. From podiatry business consulting to cash-based practice coaching, his team has everything you need to grow faster, smarter, and with less stress.
Start building the practice and life you deserve.
Contact us today to learn more about our podiatry business consulting services. Let’s turn your vision into a profitable reality.
0 notes
Text
Epic Integration: A Strategic Investment for Healthcare Efficiency
As healthcare systems evolve, the demand for reliable Epic integration services is growing rapidly. NHS trusts and private providers alike require seamless connectivity between electronic systems to improve patient care, streamline workflows, and ensure compliance. Whether you're implementing Epic for the first time or enhancing existing infrastructure, robust Epic integration solutions are essential.
What is Epic Integration?
Epic integration refers to the process of connecting the Epic Electronic Health Record (EHR) system with other healthcare applications and platforms. This ensures that data flows smoothly across systems, helping healthcare professionals access the right information at the right time. From diagnostics and imaging to billing and scheduling, integration eliminates data silos and enhances operational efficiency.
Benefits of Epic Systems Integration
Epic systems integration delivers tangible benefits for healthcare providers. These include:
Improved clinical workflows: Automatic data sharing reduces manual input, cutting errors and saving time.
Enhanced patient care: Real-time access to comprehensive patient records helps clinicians make better-informed decisions.
Regulatory compliance: Integrated systems simplify audit trails and support data governance.
Cost-efficiency: Integration reduces duplicate testing and administrative overheads.
Whether connecting with third-party software or internal systems, integration is vital for healthcare IT strategy.
Leveraging Epic API Integration
One of the key methods for connecting external applications to Epic is through Epic API integration. Epic provides a range of secure, standards-based APIs such as HL7, FHIR, and proprietary web services. These allow developers to build custom workflows and link apps that support clinicians, patients, and administrators.
From mobile apps that track patient recovery to analytics platforms that enhance population health management, API-driven integrations provide flexibility and innovation.
Epic EHR Integration: A Core Healthcare Priority
Epic EHR integration ensures that all health-related data is centralised and accessible. This is critical for multidisciplinary teams working across various departments. When done right, it enables faster diagnosis, improved treatment planning, and more personalised care.
It also supports nationwide health data initiatives by ensuring interoperability with NHS Digital systems and other healthcare providers.
Understanding Epic EMR Integration
The terms Epic EMR integration and EHR are often used interchangeably. However, EMR typically refers to a patient’s digital medical records within a single organisation. Integration at this level helps clinicians within the same hospital or trust share and update records without delay, leading to more efficient care delivery.
Conclusion:
Investing in expert Epic integration services is no longer optional—it's a strategic move for any healthcare organisation aiming for excellence. From Epic systems integration to Epic API integration, choosing the right partner ensures success in an increasingly connected digital health landscape.
0 notes
Text

Hospital & Healthcare Journals highlight how EMR solutions drive value through change management, real-time insights, and staff adoption for better care.
#EMR solutions#electronic medical records#healthcare digital transformation#change management in healthcare#real-time healthcare insights#hospital EMR adoption#clinical workflow optimization#staff adoption EMR#healthcare IT systems#hospital technology innovation#patient care improvement#EMR implementation strategies#healthcare data management#digital health solutions#hospital and healthcare journals
1 note
·
View note
Text
Reducing Hospital Operational Costs Without Compromising Care – SHPL’s Strategy
In today’s competitive healthcare landscape, hospitals must balance two critical goals: delivering high-quality care and maintaining financial sustainability. Rising costs—from equipment and technology to staffing and utilities—can strain even the most established institutions.
SHPL Management Consultancy helps hospitals streamline their operations, reduce waste, and improve efficiency—without compromising on patient care.
Why Operational Cost Control Matters
Excessive spending not only affects profitability but can also impact service delivery. Cost inefficiencies often lead to:
Overstaffing or resource underutilization
Equipment downtime or redundancy
Billing errors and revenue leakage
Longer patient wait times and reduced satisfaction
Controlling these factors requires more than short-term fixes. It calls for a strategic approach to hospital operations.
SHPL’s Cost Optimization Framework
1. Department-Wise Cost Audit SHPL begins with a detailed audit of expenses across departments such as OPD, IPD, diagnostics, pharmacy, HR, and facility management. This reveals:
Areas of resource duplication
Non-performing services or units
Untracked inventory losses or billing issues
2. Resource Utilization Planning We help hospitals right-size their staffing, space, and equipment:
Optimizing shift patterns and manpower deployment
Scheduling diagnostics and procedures efficiently
Reducing idle time for expensive medical equipment
3. SOP-Driven Efficiency Standard Operating Procedures (SOPs) eliminate process variations that lead to time and cost wastage. SHPL implements SOPs in:
Admissions and discharge workflows
Lab and radiology reporting timelines
Pharmacy stock management
Billing and insurance processing
4. Technology Integration Digital tools reduce manual errors and save administrative time. SHPL assists in:
Selecting cost-effective EMR or HMS platforms
Automating inventory, billing, and scheduling systems
Implementing dashboards for real-time cost tracking
5. Vendor and Procurement Management SHPL helps hospitals save by:
Standardizing vendor contracts
Consolidating purchases for better pricing
Tracking supplier performance and delivery efficiency
6. Revenue Cycle Optimization From accurate coding to timely billing, SHPL ensures:
Clean claim submissions to insurers
Recovery of pending dues
Prevention of revenue leakage in outpatient and inpatient services
Real-World Impact
Hospitals that implemented SHPL’s cost-saving strategies achieved:
12–20% reduction in monthly operational costs
Improved patient turnaround time
Better staff productivity and morale
Sustained profitability without cutting essential services
Conclusion
Cutting costs doesn't mean cutting corners. With expert planning and system improvements, hospitals can reduce waste, increase efficiency, and maintain the highest standards of patient care. SHPL Management Consultancy delivers practical solutions that protect both your reputation and your bottom line.
#HospitalCostManagement#SHPLManagementConsultancy#HealthcareEfficiency#HospitalOperations#CostOptimization#HospitalSOPs#HealthcareConsultingIndia#MedicalFinance#HospitalWorkflow#RevenueCycleManagement
0 notes
Text
Ashconn Health Consulting: Shaping Tomorrow’s Healthcare Ecosystems
At Ashconn, we blend clinical expertise, technological innovation, and strategic vision to help healthcare institutions across the Middle East especially in Qatar, UAE, and India transform operations and elevate patient outcomes. As a trusted arm of Al Sulaiman Health Holdings, our Health Consulting practice ensures every initiative delivers quality, efficiency, and measurable impact.
Visionary Leadership & Healthcare Strategy:
Strategic Roadmapping: Engage our senior consultants and healthcare leaders to co-create long-term roadmaps tailored to each organization’s mission. Clinical
Service Line Optimization: Redesign service lines—like cardiology, oncology, or maternity care—to unlock productivity, eliminate bottlenecks, and enhance resource utilization.
Value-Based Care Readiness: Prepare providers for outcome-centric reimbursement models by assessing clinical quality, cost structures, and data performance.
Program & Project Management Excellence:
Full-lifecycle Delivery: We manage every stage—from needs assessment and vendor evaluation (EMR, PACS, HIE) to rollout, training, and post-production support.
Regulatory & Standards Governance: Ensure projects comply with local regulations (e.g. NHRA, MoH) and global benchmarks (JCI, ISO), along with data privacy frameworks.
Risk & Change Management: Mitigate implementation risks through proactive planning, operational impact analysis, stakeholder engagement, and structured communication.
Digital Health Strategy & Transformation:
Innovative Use Case Development: Identify priority digital initiatives—telehealth, remote monitoring, patient engagement—that align with organizational goals.
Technology Feasibility & ROI Analysis: Evaluate AI symptom-checkers, disease analytics tools, and remote vitals systems (e.g. FUTREX, ENHAPP) to validate impact and sustainability.
Interoperability & Standards Adoption: Architect integrated health information ecosystems using HL7, FHIR, DICOM, IHE, and national HIE frameworks.
Clinical Systems Integration & Interoperability:
Secure EMR/HIS Linking: Connect Cerner, Epic, Meditech, etc., with hospital systems to enable seamless data sharing and integrate clinical workflows.
Health Information Exchange (HIE): Design and implement HIE interfaces for data flow across hospital networks, regional health systems, and government registries.
Interface Engine & API Strategy: Build robust API layers that decouple applications, simplify integration, and pave the way for cloud-to-cloud deployments.
Clinical Validation, Testing & Go-Live Support:
In-depth Test Management: Design test plans covering unit, integration, performance, and user-acceptance testing for all clinical applications.
Data & Workflow Validation: Verify data integrity, user flows, and order-to-fulfillment processes to ensure clinical safety and operational readiness.
Go-Live Mobilization: Deploy on-site support teams or virtual war rooms during cutover—coordinating command centers, rapid issue resolution, and full stabilization.
Organizational & Operational Optimization:
Process Re-engineering: Map and redesign core processes—admissions, pharmacy, lab, billing—for operational excellence and cost reduction.
Lean & Six Sigma Tools: Apply continuous improvement methodologies (Kaizen, DMAIC) to systematically reduce waste and boost performance metrics.
Human Capital Development: Empower staff through role-based training, leadership coaching, and change readiness programs.
Population Health & Public Health Programs:
Disease Surveillance Platforms: Design systems like Qatar’s Surveillance and Vaccination Electronic System (SaVES) for real-time public health insights.
Immunization & Registry Management: Build registries for tracking vaccination campaigns and chronic disease cohorts—enabling broad, data-driven responses.
Analytics-driven Interventions: Leverage machine learning and predictive modeling to inform public health strategies and resource allocation.
Wellness & Consumer Health Initiatives:
Patient Engagement Platforms: Create portals and mobile apps for education, self-care, appointment scheduling, and online consultations.
Health Coaching & Behavior Tracking: Integrate Fitbit, wearables, IoT sensors, and NIR glucometer interfaces for continuous wellness monitoring.
Community Outreach & E-Learning: Launch tele-tutorials, community workshops, and digital content programs to foster preventive care and healthier lifestyles.
Innovation Lab & R&D:
Patent-backed AI/IoT Solutions: Drive innovation via our patent-strong units—FUTREX and ENHAPP—with 69+ U.S. patents in AI, IoT, and medical devices.
From Prototype to Scale: Use validated clinical pilots and regulatory frameworks to accelerate proof-of-concepts into full-scale, production-grade deployments.
Global Alliances: Collaborate with industry leaders—from NextGen and Clinisys to STChealth—to test frontier innovations in varied settings.
Governance, Compliance & Quality Assurance:
a. Holistic Governance Frameworks: Define clear roles, tools, policies, and oversight for large-scale digitalization programs. b. Data Protection & Cybersecurity: Embed HIPAA-style best practices, encryption, access controls, and incident response strategies. c. Quality & Accreditation Support: Assist in achieving JCI, HIMSS, ISO 9001, or equivalent quality certifications through continual performance audits and benchmarking.
Conclusion: Partnering with Ashconn Health Consulting means working with a future-focused team that delivers real-world excellence through robust digital, operational, and organizational revitalization. Whether your priorities lie in hospital optimization, EMR rollouts, public health systems, or patient engagement, our consultative approach, backed by technology and clinical insight, ensures each initiative delivers measurable, sustainable impact.
Contact us today to explore how we can co-create a healthier future for your institution and community.
#ashconn#Healthcare Consulting#Healthcare Management Consulting#Consulting and System Integration Services#System Integration Services#Staff Augmentation#Healthcare Consultants Qatar and Dubai#Healthcare Consultancy Qatar and Dubai
0 notes
Text
The Ultimate Guide to Finding a Trusted Ophthalmology Consultant in India
In today’s competitive healthcare environment, the success of your ophthalmology practice hinges not only on clinical expertise but also on strong business strategies, efficient operations, and patient-centered care. That’s why choosing a trusted ophthalmology consultant is one of the most important decisions you’ll make. At EyeForce Solutions, we specialize in guiding eye hospitals and clinics across India toward sustainable growth. Here's your ultimate guide to making the right choice.
1. Industry-Specific Expertise
Not all consultants understand the unique challenges of eye care—like equipment-intensive setups, OPD management, or specialty services such as LASIK, retina, or glaucoma care. A trusted ophthalmology consultant should bring deep experience in this niche. At EyeForce Solutions, we focus exclusively on eye care, which gives us the insights needed to help your practice thrive.
2. Customized Solutions for Every Practice
Your hospital is different from the one down the road. A reliable consultant should provide tailored strategies based on your clinic size, patient demographics, budget, and long-term vision. Whether you’re launching a new practice or upgrading an existing one, EyeForce Solutions delivers personalized roadmaps for success.
3. Results-Driven Approach
Talk is easy—results matter. A trusted consultant should show a proven track record of increasing patient footfall, improving operational efficiency, and enhancing profitability. EyeForce Solutions is proud to have partnered with dozens of top-performing eye hospitals in India, helping them optimize services and achieve scalable growth.
4. 360° Support – From Setup to Marketing
The best ophthalmology consultants offer end-to-end support: from location planning and staff training to branding, digital marketing, and patient engagement strategies. At EyeForce Solutions, we offer a complete suite of services so you don’t have to juggle multiple vendors.
5. Long-Term Partnership
Eye care is evolving fast. Whether it’s adopting advanced technology like phacoemulsification or implementing EMR systems, you need a consultant who stays ahead of the curve. EyeForce Solutions isn’t just a service provider—we’re your long-term strategic partner in success.
Conclusion
When you choose EyeForce Solutions as your ophthalmology consultant in India, you’re choosing expertise, commitment, and growth-focused results. Let us help you build a future-ready, patient-centric eye care practice that stands out in today’s dynamic market.
Visit -
1 note
·
View note
Text
Do you provide workplace safety training to prevent workers’ comp injuries?
Yes, I provide comprehensive workplace safety training to prevent workers’ comp injuries, a critical strategy for reducing claims and premiums. My process begins with a workplace risk assessment, identifying hazards specific to your industry—e.g., repetitive strain in offices, falls in construction, or equipment risks in manufacturing. I then design OSHA-compliant safety training programs tailored to your workforce, covering topics like proper equipment use, ergonomic practices, and emergency protocols. Training is delivered through interactive sessions, videos, and written guides, ensuring accessibility for all employees. For example, a manufacturing client reduced incidents by 30% after implementing my machine safety training. I also develop injury prevention protocols, such as regular safety audits and hazard reporting systems, to maintain a proactive culture. These programs align with OSHA standards and state workers’ comp requirements, reducing the risk of fines. To sustain impact, I train supervisors to reinforce safety practices and monitor compliance. My deliverables include customized training materials, safety checklists, and performance metrics to track incident reductions. By lowering injury rates, these programs directly reduce workers’ comp claims and experience modification rates (EMR), often saving clients thousands in premiums. A construction firm I worked with saw their EMR drop from 1.3 to 0.9 over two years, cutting costs significantly. Ongoing support, including quarterly safety reviews, ensures long-term effectiveness, making your workplace safer and more cost-efficient.
0 notes
Text
What Steps Should I Take for OpenEMR Installation Issues?
Introduction
The installation process of OpenEMR presents difficulties due to its power as an open-source Electronic Medical Records (EMR) system. The following section presents known OpenEMR installation issues with corresponding step-by-step solutions.
Common Installation Errors and Solutions
1.PHP Compatibility Issues
Error: OpenEMR installation fails due to compatibility issues with PHP version.
Solution: The installation process requires using PHP version 7.4 or newer versions. The php.ini file requires PHP configuration updates that match OpenEMR settings. Proper error prevention involves enabling Off for short_open_tag while setting the memory_limit to 512M in your php.ini file.
2.Database Connection Failure
Error: “Cannot connect to the MySQL database.”
Cause: This error arises when the OpenEMR installer cannot establish a connection to the MySQL database.
Solution:
· Ensure the MySQL service is running: sudo service mysql start.
· Verify that the credentials in the sqlconf.php file are correct:
Php: $host = 'localhost'; $port = '3306'; $login = 'your_username'; $pass = 'your_password'; $dbase = 'openemr';
3. Blank Page After Installation
Error: A blank screen is displayed after installing OpenEMR.
Cause: Typically caused by a missing PHP module or a permissions issue.
Solution:
· Check for missing PHP modules using php -m | grep -i <missing_module>.
· Install missing modules with sudo apt-get install php-<module_name>.
· Ensure correct file permissions: sudo chmod -R 755 /var/www/openemr.
4. Locale Errors
Error: “PHP Warning: Failed to setlocale��”
Cause: The locale settings on the server are not configured correctly.
Solution:
· Install the appropriate locales: sudo locale-gen en_US.UTF-8.
· Reconfigure locales: sudo dpkg-reconfigure locales.
5. SQL Error in OpenEMR Usage
Error: A fatal error occurred that showed “Uncaught Error: SQLSTATE[42S02]: Base table or view not found…”
Cause: The missing database table or improper database table creation process causes this error to appear.
Solution:
· Re-execute the SQL upgrade script through the command: mysql -u root -p openemr < sql/upgrade.sql.
· All database tables need to be imported correctly.
6. PDF Generation Failure
Error: The error message reads, “FPDF error: Unable to create output file.”
Cause: The file system write permissions create a cause that prevents OpenEMR from generating output files.
Solution:
· Users need write permissions in the sites/default/documents directory because of this command: sudo chmod -R777/var/www/openemr/sites/default/documents.
Common Mistakes During Setup
1.Inadequate System Requirements Assessment
· Performance problems emerge because organizations underestimate their hardware requirements along with their software needs.
· System requirements assessment needs to become a complete process done before any installation begins.
2.Neglecting Data Backup and Recovery Planning
· Failing to plan backup procedures and recovery strategies remains one of the main setup challenges.
· Planning for data backup becomes essential since the absence of planning may cause complete loss of information.
· Regular backups should be conducted either through OpenEMR’s tools or third-party scripting solutions.
3.Improper Configuration
· Incorrectly implemented settings result in both performance issues and system errors.
· Users should verify that both database and PHP settings align correctly with OpenEMR’s necessary requirements.
Real-World Examples and Case Studies
Cloud Success Story: Through OpenEMR Cloud on AWS, this Vermont clinic cut their server maintenance expenses by 70% and also gained better peak-season system capabilities.
On-Premises Example: A large Texas hospital chose on-premises deployment of OpenEMR to sustain whole authority over security standards while maintaining easy integration with current hospital information infrastructure.
Troubleshooting Tips for Windows Installation
· Check PHP settings because you must enable all required PHP extensions while following the correct settings in the php.ini configuration file.
· Check MySQL Connection by verifying the correct running of MySQL and sqlconf.php credentials.
· During installation, use a temporary disable of antivirus software to prevent interruptions.
· You should check OpenEMR directory permissions to stop unauthorized access to its files.
Future Trends in OpenEMR
OpenEMR will continue integrating modern features into its system as healthcare technology advances forward.
AI and Machine Learning
· OpenEMR will incorporate artificial intelligence-based clinical decision support systems and predictive analytics technology for patient care in future updates.
Telehealth Enhancements
· The telehealth system will receive updated modules that enable remote consultation access while offering better healthcare access to patients.
Interoperability Standards
· Additional FHIR technology support in the system will help different healthcare systems communicate their data more efficiently.
Conclusion
The resolution of OpenEMR installation problems requires a careful approach together with expertise in frequent installation barriers. Healthcare providers who focus on PHP compatibility along with database connections and permissions will establish a successful OpenEMR setup while maximizing its functionality. Continuous updates about the latest OpenEMR advancements enable healthcare professionals to achieve maximum performance and efficiency for their management tasks.
FAQs
What are the most common installation errors in OpenEMR?
During OpenEMR installation, you might encounter three major issues that include PHP version conflicts as well as database connection problems and unexplained blank pages showing up because of either missing components or access permission problems.
How do I troubleshoot a blank page error after OpenEMR installation?
Review both PHP module's presence and verify correct permissions for the OpenEMR directory files.
What are some common mistakes during OpenEMR setup?
The integration of insufficient system assessment with poor data backup and recovery planning along with unsuitable configuration represents the main mistakes that cause performance degradation and data loss.
0 notes