#Gamma-Glutamyl Transferase (GGT)
Text

Learn to interpret your liver function test results with our comprehensive guide. Understand commonly used liver tests and their implications for your health.
Do Visit: https://www.healixhospitals.com/blogs/reading-and-interpreting-your-liver-function-test-a-guide-to-commonly-used-liver-tests
#Liver Function Test#Liver Health#Diagnostic Tests#Liver Enzymes#Blood Tests#Hepatic Function#Liver Panel#Bilirubin Levels#Liver Disease#Alanine Aminotransferase (ALT)#Aspartate Aminotransferase (AST)#Alkaline Phosphatase (ALP)#Gamma-Glutamyl Transferase (GGT)#Liver Health Markers#Hepatobiliary Disorders#Serum Biomarkers#Hepatic Enzymes#Liver Damage#Medical Laboratory Tests#Hepatology
1 note
·
View note
Text
Aarogyam Advanced profile - Bookmytest
This is Basic Health Checkup Package Aarogyam Advanced profile which Consists of 74 Tests and Consists of fundamental tests for screening of the health status Like cardiac Risk Marker.Diabetics, Iron Deficiency Profile, Lipid Profile, Liver Profile, Kidney Profile, Vitamins,electrolytes. This package is ideal for People Aged 30 years and above. We at Bookmytest offers health checkup packages at a low price. We offer sample collection services at your home.
List of Profiles Included:
THYROID (TFT) (3 Tests)
THYROID STIMULATING HORMONE (TSH)
TOTAL THYROXINE (T4)
TOTAL TRIIODOTHYRONINE (T3)
DIABETES (4 Tests)
AVERAGE BLOOD GLUCOSE (ABG)
HbA1c
BLOOD KETONE (D3HB)
FRUCTOSAMINE
LIPID PROFILE (10 Tests)
TOTAL CHOLESTEROL
HDL CHOLESTEROL - DIRECT
LDL CHOLESTEROL - DIRECT
LDL / HDL RATIO
NON-HDL CHOLESTEROL
TC/ HDL CHOLESTEROL RATIO
TRIGLYCERIDES
VLDL CHOLESTEROL
TRIG / HDL RATIO
HDL / LDL RATIO
LIVER FUNCTION TESTS (12 Tests)
SERUM ALB/GLOBULIN RATIO
ALKALINE PHOSPHATASE
BILIRUBIN -DIRECT
BILIRUBIN (INDIRECT)
BILIRUBIN - TOTAL
GAMMA GLUTAMYL TRANSFERASE (GGT)
PROTEIN - TOTAL
ALBUMIN - SERUM
SERUM GLOBULIN
ASPARTATE AMINOTRANSFERASE (SGOT )
ALANINE TRANSAMINASE (SGPT)
SGOT / SGPT RATIO
CARDIAC RISK MARKERS (5 Tests)
APO B / APO A1 RATIO (APO B/A1)
APOLIPOPROTEIN - A1 (APO-A1)
APOLIPOPROTEIN - B (APO-B)
HIGH SENSITIVITY C-REACTIVE PROTEIN (HS-CRP)
LIPOPROTEIN (A) [LP(A)]
IRON DEFICIENCY PROFILE (4 Tests)
% TRANSFERRIN SATURATION
IRON
TOTAL IRON BINDING CAPACITY (TIBC)
UNSAT.IRON-BINDING CAPACITY(UIBC)
ELEMENTS (2 Tests)
SERUM COPPER
SERUM ZINC
VITAMINS (2 Tests)
VITAMIN B-12
25-OH VITAMIN D (TOTAL)
HORMONE (1 Tests)
TESTOSTERONE
RENAL (8 Tests)
BUN / SR.CREATININE RATIO
BLOOD UREA NITROGEN (BUN)
CREATININE - SERUM
URIC ACID
URI. ALBUMIN/CREATININE RATIO (UA/C)
CREATININE - URINE
CALCIUM
CYSTATIN C
HEMOGRAM (CBC) (24 Tests)
BASOPHILS - ABSOLUTE COUNT
EOSINOPHILS - ABSOLUTE COUNT
LYMPHOCYTES - ABSOLUTE COUNT
MONOCYTES - ABSOLUTE COUNT
NEUTROPHILS - ABSOLUTE COUNT
BASOPHILS
EOSINOPHILS
HEMOGLOBIN
IMMATURE GRANULOCYTE PERCENTAGE(IG%)
TOTAL LEUCOCYTES COUNT
LYMPHOCYTE PERCENTAGE
MEAN CORPUSCULAR HEMOGLOBIN(MCH)
MEAN CORP.HEMO.CONC(MCHC)
MEAN CORPUSCULAR VOLUME(MCV)
MONOCYTES
NEUTROPHILS
NUCLEATED RED BLOOD CELLS
NUCLEATED RED BLOOD CELLS %
HEMATOCRIT(PCV)
PLATELET COUNT
TOTAL RBC
RED CELL DISTRIBUTION WIDTH (RDW-CV)
RED CELL DISTRIBUTION WIDTH - SD(RDW-SD)
IMMATURE GRANULOCYTES(IG)
0 notes
Text
Liver Function Test Normal Range Chart
More Information: Liver Specialist in Kochi
Here is a general overview of the normal range for liver function tests. It's important to note that the specific reference ranges may vary slightly depending on the laboratory and the units of measurement used. Always consult with a healthcare professional for an accurate interpretation of your individual test results.
Alanine aminotransferase (ALT):
Normal range: 7-55 units per liter (U/L)
Aspartate aminotransferase (AST):
Normal range: 8-48 U/L
Alkaline phosphatase (ALP):
Normal range: 45-115 U/L
Total bilirubin:
Normal range: 0.1-1.2 milligrams per deciliter (mg/dL) or 1.71-20.5 micromoles per liter (µmol/L)
Direct bilirubin:
Normal range: 0-0.3 mg/dL or 0-5.1 µmol/L
Gamma-glutamyl transferase (GGT):
Normal range: 9-48 U/L
Albumin:
Normal range: 3.4-5.4 grams per deciliter (g/dL) or 34-54 grams per liter (g/L)
Total protein:
Normal range: 6.0-8.3 g/dL or 60-83 g/L
It's important to keep in mind that these values are general guidelines and may vary depending on factors such as age, sex, underlying medical conditions, and individual variations. Your healthcare provider will interpret your liver function test results in the context of your specific health situation and medical history.
If you have concerns about your liver function or specific test results, it is recommended to consult with a healthcare professional for a thorough evaluation and appropriate guidance.
0 notes
Text
John Korsah
ACCRA-Ghana
1. Liver Function tests, types, purpose, procedure and results.
2. Suggested ways of bringing the abnormalities to normal both in natural ways and the use of medicine.
🍁
1. Liver Function test
Liver function tests (LFTs) are a group of blood tests that are used to assess the health and function of the liver. These tests are often done as part of a routine health checkup or when a person is experiencing symptoms that may suggest liver disease.
The common liver function tests include:
▪️Alanine aminotransferase (ALT): This enzyme is found primarily in the liver and is released into the bloodstream when liver cells are damaged. High levels of ALT in the blood can indicate liver damage or disease.
▪️Aspartate aminotransferase (AST): Like ALT, AST is also found in the liver and is released into the bloodstream when liver cells are damaged. Elevated AST levels in the blood can also indicate liver damage or disease.
▪️Alkaline phosphatase (ALP): This enzyme is found in many tissues throughout the body, including the liver, bones, and intestines. Elevated levels of ALP in the blood can indicate liver disease, bone disease, or a problem with the intestines.
▪️Total bilirubin: This is a waste product that is produced when red blood cells are broken down in the liver. High levels of bilirubin in the blood can indicate liver disease or a problem with the gallbladder.
▪️Albumin: This is a protein that is produced by the liver. Low levels of albumin in the blood can indicate liver disease or malnutrition.
▪️Prothrombin time (PT): This test measures the time it takes for the blood to clot. The liver produces many of the proteins needed for blood clotting, so changes in PT can indicate liver disease.
It is important to note that LFTs are not a definitive diagnosis of liver disease, and further testing may be needed to confirm a diagnosis.
🔳Types
There are several types of liver function tests that can be used to assess liver health and function. Some of the most common types include:
▪️Alanine aminotransferase (ALT): This test measures the level of ALT in the blood, which is an enzyme that is primarily found in liver cells. Elevated levels of ALT in the blood can indicate liver damage or disease.
▪️Aspartate aminotransferase (AST): Like ALT, AST is also found in liver cells and is released into the bloodstream when liver cells are damaged. Elevated levels of AST in the blood can indicate liver damage or disease.
▪️Alkaline phosphatase (ALP): This test measures the level of ALP in the blood, which is an enzyme that is found in many tissues throughout the body, including the liver. Elevated levels of ALP in the blood can indicate liver disease, bone disease, or a problem with the intestines.
▪️Total bilirubin: This test measures the level of bilirubin in the blood, which is a waste product that is produced when red blood cells are broken down in the liver. High levels of bilirubin in the blood can indicate liver disease or a problem with the gallbladder.
▪️Albumin: This test measures the level of albumin in the blood, which is a protein that is produced by the liver. Low levels of albumin in the blood can indicate liver disease or malnutrition.
▪️Prothrombin time (PT): This test measures the time it takes for the blood to clot. The liver produces many of the proteins needed for blood clotting, so changes in PT can indicate liver disease.
▪️Gamma-glutamyl transferase (GGT): This test measures the level of GGT in the blood, which is an enzyme that is found in liver cells and other tissues. Elevated levels of GGT in the blood can indicate liver disease or heavy alcohol consumption.
▪️Lactate dehydrogenase (LDH): This test measures the level of LDH in the blood, which is an enzyme that is found in many tissues throughout the body, including the liver. Elevated levels of LDH in the blood can indicate liver disease or damage to other tissues in the body.
These tests are often done together as part of a liver function panel to provide a comprehensive assessment of liver health and function.
🔳Purpose
The purpose of liver function tests (LFTs) is to assess the health and function of the liver. The liver is a vital organ that performs many important functions in the body, including:
▪️Filtering and removing toxins from the blood
▪️Producing bile, which helps with the digestion of fats
▪️Regulating the body's metabolism of carbohydrates, proteins, and fats
▪️Storing vitamins and minerals, such as iron and vitamin D
▪️Producing proteins that are essential for blood clotting
▪️LFTs are used to detect liver damage, inflammation, or disease by measuring the levels of enzymes, proteins, and other substances in the blood that are produced by or indicative of liver cells. Abnormal results from LFTs can help identify liver problems early on and guide further testing and treatment.
🔳Some common reasons for ordering LFTs include:
▪️Monitoring liver function in people with liver disease, such as hepatitis or cirrhosis
▪️Assessing liver function in people who are taking medications that can damage the liver
Screening for liver disease in people who have risk factors, such as heavy alcohol use or a family history of liver disease
▪️Evaluating abnormal liver function tests found incidentally during routine blood testing
Investigating the cause of symptoms that may suggest liver disease, such as jaundice, abdominal pain, or unexplained fatigue
Overall, the purpose of liver function tests is to help assess liver health and function, detect liver disease or damage, and guide further testing and treatment.
🔳Procedure
Liver function tests are a blood test that can be performed at a doctor's office, hospital or laboratory.
The procedure for liver function tests is typically as follows:
▪️Preparation: There is no specific preparation required for liver function tests. However, it is important to inform your doctor of any medications or supplements you are taking, as some can affect liver function test results.
▪️Blood collection: A healthcare professional will collect a blood sample from a vein in your arm using a sterile needle. The procedure is quick and usually involves minimal discomfort.
▪️Results: The blood sample is sent to a laboratory for analysis. Results are typically available within a few days, and your doctor will discuss the results with you and any further action needed.
It is important to note that liver function tests are just one tool used to assess liver health and function, and abnormal results do not necessarily mean that you have liver disease.
Further testing and evaluation may be needed to determine the cause of abnormal results and guide appropriate treatment.
Additional information: Some people may experience mild discomfort, bruising, or bleeding at the site of the blood draw. If you experience severe pain, swelling, or bleeding, contact your doctor or healthcare provider immediately.
🔳Results
Interpretation of liver function test results can vary depending on the specific test being performed, the individual's age, sex, and medical history, and other factors.
However, some general guidelines for interpreting common liver function test results are as follows:
▪️Alanine aminotransferase (ALT): Normal levels of ALT are generally between 7 and 55 units per liter (U/L) for men and between 7 and 45 U/L for women. Elevated levels of ALT may indicate liver damage, such as hepatitis or cirrhosis.
▪️Aspartate aminotransferase (AST): Normal levels of AST are generally between 8 and 48 U/L for men and between 7 and 35 U/L for women. Elevated levels of AST may indicate liver damage or other conditions, such as muscle damage or heart disease.
▪️Alkaline phosphatase (ALP): Normal levels of ALP are generally between 44 and 147 U/L for adults. Elevated levels of ALP may indicate liver disease, bone disease, or other conditions, such as pregnancy.
▪️Total bilirubin: Normal levels of bilirubin are generally between 0.1 and 1.2 milligrams per deciliter (mg/dL) for adults. Elevated levels of bilirubin may indicate liver disease, such as hepatitis or cirrhosis, or other conditions, such as gallbladder disease.
▪️Albumin: Normal levels of albumin are generally between 3.5 and 5.0 grams per deciliter (g/dL) for adults. Low levels of albumin may indicate liver disease or malnutrition.
▪️Prothrombin time (PT): Normal PT values range from 9.5 to 13.8 seconds, depending on the laboratory. Prolonged PT can indicate liver disease or a deficiency of clotting factors.
▪️Gamma-glutamyl transferase (GGT): Normal levels of GGT are generally between 9 and 48 U/L for men and between 9 and 33 U/L for women. Elevated levels of GGT may indicate liver disease or heavy alcohol consumption.
▪️Lactate dehydrogenase (LDH): Normal levels of LDH are generally between 140 and 280 U/L for adults. Elevated levels of LDH may indicate liver disease or damage to other tissues in the body.
It is important to note that these are general guidelines, and interpretation of liver function test results should always be done by a healthcare professional who can take into account individual factors and medical history.
🔳 Suggested ways of bringing the abnormalities to normal both in natural ways and the use of medicine.
The treatment of abnormal liver function test results depends on the underlying cause. In some cases, lifestyle changes, natural remedies, or medications may be used to help bring the abnormalities back to normal.
Here are some suggested ways to manage abnormal liver function test results:
▪️Lifestyle changes: Making healthy lifestyle choices can improve liver function and help prevent liver damage. These changes may include:
▪️Limiting alcohol consumption or avoiding alcohol altogether, especially if you have liver disease.
▪️Maintaining a healthy weight through diet and exercise.
▪️Eating a balanced diet that is low in saturated fat, sugar, and salt.
▪️Avoiding exposure to toxins, such as pesticides and industrial chemicals.
▪️Quitting smoking.
Natural remedies: Some natural remedies may help support liver function, such as:
▪️Milk thistle: This herb has been shown to help protect the liver from damage and improve liver function. It can be taken in capsule or tea form.
▪️Turmeric: This spice has anti-inflammatory properties and may help reduce liver inflammation. It can be added to food or taken in supplement form.
▪️Dandelion root: This herb has diuretic properties and may help reduce liver congestion. It can be taken in capsule or tea form.
It is important to note that natural remedies should be used with caution and under the guidance of a healthcare professional, as they may interact with other medications or have side effects.
Medications
Depending on the underlying cause of abnormal liver function test results, medications may be prescribed to help manage symptoms or treat the underlying condition.
For example:
▪️Antiviral medications may be used to treat hepatitis B or C.
▪️Corticosteroids may be used to reduce liver inflammation in autoimmune hepatitis.
▪️Medications may be used to manage symptoms of liver disease, such as itching or fatigue.
It is important to work closely with a healthcare professional to determine the best treatment plan for abnormal liver function test results, as untreated liver disease can lead to serious complications.

0 notes
Link
1. Xét nghiệm Gamma GT là gì?Gamma GT cùng với AST và ALT là ba loại men gan quan trọng trong cơ thể chúng ta. Ngoài xuất hiện ở gan thì GGT còn có thể xuất hiện ở thận, lá lách, ruột non,...Xét nghiệm Gamma GT giúp đo men ganGGT là một loại enzym có tác dụng trong việc chẩn đoán hiện tượng gan bị ứ mật, do loại enzym này phản ứng rất nhạy với tình trạng trên. Ngoài ra giá trị GGT tăng còn giúp trong việc chẩn đoán các bệnh về gan như viêm gan mạn, viêm gan virus, tổn thương gan do rượu bia.Xét nghiệm Gamma GT còn giúp xác định nguyên nhân gây nên sự tăng ALP, nhờ đó mà đánh giá được các bệnh về xương. Nếu người xét nghiệm có chỉ số GGT bình thường mà ALP tăng thì rất có thể bạn bị các bệnh lý về xương.2. Khi nào bạn cần xét nghiệm Gamma GT và cần lưu ý gì?Khi bạn gặp phải những triệu chứng sau thì bác sĩ sẽ yêu cầu bạn thực hiện xét nghiệm Gamma GT : Các biểu hiện: chán ăn, sụt cân, buồn nôn và chướng bụng.Vàng mắt, vàng da, da nổi rõ mạch máu, nước tiểu sẫm màu.Sử dụng rượu bia các chất kích thích trong một thời gian dài.Trước khi thực hiện xét nghiệm bạn nên lưu ý một số yếu tố sau:Không sử dụng các thuốc có tác dụng tăng chỉ số Gamma GT như phenytoin, phenobarbital,... trong vòng 24h trước xét nghiệm.Không sử dụng rượu bia thuốc lá trong vòng 24h trước xét nghiệm. Chỉ cần một lượng nhỏ cũng đủ thay đổi và ảnh hưởng đến kết quả xét nghiệm.Không sử dụng rượu bia trước khi thực hiện xét nghiệm Gamma GT3. Nguyên nhân khiến chỉ số Gamma GT tăng cao và tăng bao nhiêu là gây hại?Những nguyên chính gây nên tình trạng tăng chỉ số Gamma GT Nghiện rượu bia và các thức uống kích thích khác.Chế độ dinh dưỡng không khoa học, ăn quá nhiều đồ chiên dầu mỡ và chất béo, ăn ít rau củ quả.Thức khuya, làm việc quá sức và stress trong một thời gian dài.Mắc các bệnh viêm gan A, B, C, D, E.Mặc bệnh lý như xơ gan, gan nhiễm mỡ hoặc có khối u ở gan.Bị các bệnh như đái tháo đường, các bệnh lý tim mạch, viêm tụy.Chỉ số Gamma GT tăng bao nhiêu là đáng lo ngại?Ở người bình thường chỉ số Gamma GT luôn nhỏ hơn 60UI/L. Cụ thể ở từng giới tính như sau:Ở nam giới : 11 đến 50 UI/L.Ở nữ giới : 7 đến 32 UI/L.Chỉ số Gamma GT tăng theo từng mức độ và độ nguy hiểm như sau:Chỉ số Gamma GT tăng cao 1 đến 2 lần thì tình trạng ở mức độ nhẹ.Tăng cao 2 đến 5 lần là mức độ trung bình.Tăng trên 5 lần là tình trạng của bạn ở mức độ nặng.Nếu chỉ số Gamma GT của bạn lớn hơn 5000 UI/L thì rất có thể bạn bị ung thư gan hoặc bị gan mật cấp.Chỉ số men gan Gamma GT cao gấp 5 lần bình thường là rất nguy hiểm4. Cách kiểm soát giá trị Gamma GT trong ngưỡng an toànMột số lời khuyên mà MEDLATEC đưa ra cho bạn đọc để có thể kiểm soát giá trị Gamma GT của bản thân ở ngưỡng an toàn nhất có thể.Thực hiện các xét nghiệm viêm gan B hoặc viêm gan C. Đối với viêm gan B thực hiện đầy đủ các xét nghiệm sau : HBsAg, HbeAg, anti HBsAg và HBsAb.Xét nghiệm viêm BNếu chỉ số Gamma GT tăng do nguyên nhân viêm tắc đường mật thì cần có sự hỗ trợ và điều trị của bác sĩ để chữa một cách dứt điểm.Hạn chế sử dụng đồ uống có cồn có ga như rượu bia, nước giải khát.Thực hiện chế độ ăn uống khoa học lành mạnh để tăng sức khỏe cho “gan” của mình. Hạn chế đồ ăn nhanh, đồ ăn nhiều dầu mỡ, đồ ăn không đảm bảo an toàn vệ sinh thực phẩm. Nếu chế độ ăn uống không lành mạnh duy trì lâu dài sẽ khiến suy giảm chức năng gan dẫn đến các bệnh sau này.Bổ sung các đồ ăn tốt cho gan như súp lơ xanh, bơ, táo, nghệ, bưởi,...Không nên sử dụng các loại thuốc Nam hay Đông Y truyền miệng hoặc không có nguồn gốc rõ ràng để tự ý uống. Bởi những loại thuốc này chưa có bằng chứng khoa học nào xác nhận độ tin cậy sẽ dẫn đến hậu quả nghiêm trọng, gây tổn hại đến gan của người sử dụngNgoài chế độ ăn uống thì chúng ta cũng nên có kế hoạch sinh hoạt hợp lý, nghỉ ngơi đầy đủ và tránh căng thẳng trong một thời gian dài.5. Xét nghiệm Gamma GT ở đâu và mất bao nhiêu tiền.Việc xét nghiệm Gamma GT bạn nên thực hiện ở các cơ sở y tế lớn và có uy tín để có được kết quả chính xác nhất. Ngoài ra sau khi xét nghiệm Gamma GT nếu cần xét nghiệm bổ sung để xác định tình trạng bệnh thì có thể tiến hành ngay một cách dễ dàng. Bệnh viện Đa khoa MEDLATEC có hệ thống máy móc và Trung tâm xét nghiệm đạt tiêu chuẩn ISO 15189:2012, chúng tôi hỗ trợ hơn 500 loại xét nghiệm trong đó bao gồm các xét nghiệm về gan như xét nghiệm Gamma GT. Với đội ngũ y bác sĩ có trình độ chuyên môn cao, nhất định sẽ chẩn đoán chính xác tình trạng của bệnh nhân, nhờ đó nâng cao hiệu quả trong điều trị bệnh.Chi phí xét nghiệm Gamma GT cũng là một trong những yếu tố mà khách hàng quan tâm. Thông thường xét nghiệm Gamma GT có giá dao động trong khoảng 50.000 VNĐ đến 100.000 VNĐ tùy từng vào đối tượng bệnh nhân.Ngoài ra, hiện nay, MEDLATEC còn hỗ trợ lấy mẫu xét nghiệm tại nhà, rất phù hợp cho người bận rộn và người già yếu, giúp tiết kiệm tối đa thời gian và chi phí đi lại, được sự ủng hộ rất lớn từ phía bệnh nhân.Nếu còn vấn đề gì thắc mắc về xét nghiệm Gamma GT thì hãy liên hệ với MEDLATEC qua tổng đài tư vấn miễn phí: 1900565656 để được giải đáp cụ thể và chính xác nhất.Theo: Medlatec
0 notes
Text
0 notes
Text
Best Liver Function Test In Delhi
Liver function tests (also known as a liver panel) are blood tests that measure different enzymes, proteins, and other substances made by the liver. These tests check the overall health of your liver. The different substances are often tested at the same time on a single blood sample and may include the following: Albumin, Total protein, ALP (alkaline phosphatase), ALT (alanine transaminase), AST (aspartate aminotransferase), and gamma-glutamyl transferase (GGT), Bilirubin, Lactate dehydrogenase (LD), Prothrombin time (PT).
0 notes
Text
Gamma-Glutamyl Transferase from Bovine Kidney
Gamma-Glutamyl Transferase from Bovine Kidney
Gamma-Glutamyl Transferase from Bovine Kidney
Catalog number: B2012156
Lot number: Batch Dependent
Expiration Date: Batch dependent
Amount: 1 kU
Molecular Weight or Concentration: na
Supplied as: Lyophilized
Applications: molecular tool for various biochemical applications
Storage: -20 °C
Keywords: Gamma-Glutamyltranspeptidase, Gamma-Glutamyl Transpeptidase, gGT, gamma-GT, GGTP
Grade:…

View On WordPress
0 notes
Text
Reading And Interpreting Your Liver Function Test - A Guide To Commonly Used Liver Tests

The liver is a vital organ responsible for numerous metabolic functions in the body, including detoxification, protein synthesis, and bile production. Monitoring liver health is crucial for early detection and management of liver diseases. One of the primary tools for assessing liver function is the Liver Function Test (LFT). In this guide, we will delve into the commonly used liver tests, how to interpret the results, and what they indicate about your liver health.
Understanding Liver Function Tests
Liver Function Tests (LFTs) are a group of blood tests that provide valuable insights into the health and function of the liver. These tests measure various enzymes, proteins, and substances in the blood that are indicative of liver health.
Key components of Liver Function Tests
Alanine Aminotransferase (ALT): Elevated levels suggest liver damage, commonly caused by conditions like hepatitis or fatty liver disease.
Aspartate Aminotransferase (AST): Similar to ALT, elevated AST levels indicate liver damage but may also be elevated in conditions affecting the heart or muscles.
Alkaline Phosphatase (ALP): Elevated ALP levels may suggest liver or bone disease.
Total Bilirubin: Increased levels may indicate liver dysfunction or obstruction of bile ducts.
Albumin and Total Protein: These are measures of liver synthetic function; decreased levels may suggest liver disease.
What are the causes of abnormal liver function test results?
Causes of abnormal liver function test results can vary and may indicate different underlying conditions. Some common causes include:
1. Build-up of Fat in the Liver:
* Non-alcoholic fatty liver disease (NAFLD) can lead to abnormal liver function tests, especially in overweight or obese individuals.
2. Liver Inflammation and Damage:
* Infections, toxic substances like alcohol or certain medications, and immune conditions can cause liver inflammation and subsequent abnormal test results.
3. Liver Overworking:
* When the liver is under stress from processing medicines or toxic substances like alcohol or paracetamol, it can result in abnormal liver function tests.
4. Bile Duct Blockage:
* Blockages in the bile ducts, such as by gallstones, can lead to abnormal liver function test results.
5. Liver Conditions and Diseases:
* Underlying conditions like Wilson's disease, haemochromatosis, or Gilbert's syndrome can affect liver function and result in abnormal test values.
6. Liver Injury:
* Physical injury to the liver, trauma, or presence of abscesses or tumors within the liver can cause abnormal liver function tests.
7. Medications and Supplements:
* Certain medications, over-the-counter drugs, herbal remedies, and traditional medicines can also impact liver function test results.
8. Other Factors:
* Factors like high alcohol intake, viral infections, autoimmune conditions, metabolic liver diseases, heart problems, and tumors in the liver can contribute to abnormal liver function tests.
Continue Reading: https://www.healixhospitals.com/blogs/reading-and-interpreting-your-liver-function-test-a-guide-to-commonly-used-liver-tests
#Liver Function Test#Liver Health#Diagnostic Tests#Liver Enzymes#Blood Tests#Hepatic Function#Liver Panel#Bilirubin Levels#Liver Disease#Alanine Aminotransferase (ALT)#Aspartate Aminotransferase (AST)#Alkaline Phosphatase (ALP)#Gamma-Glutamyl Transferase (GGT)#Liver Health Markers#Hepatobiliary Disorders#Serum Biomarkers#Hepatic Enzymes#Liver Damage#Medical Laboratory Tests#Hepatology
1 note
·
View note
Text
Best Liver Function Test in Delhi
Liver function tests (also known as a liver panel) are blood tests that measure different enzymes, proteins, and other substances made by the liver. These tests check the overall health of your liver. The different substances are often tested at the same time on a single blood sample, and may include the following: Albumin, Total protein, ALP (alkaline phosphatase), ALT (alanine transaminase), AST (aspartate aminotransferase), and gamma-glutamyl transferase (GGT), Bilirubin, Lactate dehydrogenase (LD), Prothrombin time (PT).
0 notes
Text
Xét nghiệm chức năng gan đánh giá tình trạng bệnh
Xét nghiệm chức năng gan đo lường các chỉ số men gan, protein đặc trưng, bilirubin trong máu để đánh giá tình trạng hoạt động của gan.
Xét nghiệm chức năng gan là xét nghiệm máu để đo một số enzym và protein. Chúng có thể bao gồm phosphatase kiềm (ALP), aspartate transaminase (AST), bilirubin và gamma glutamyl transferase (GGT)... Các chỉ số xét nghiệm phản ánh mức độ hoạt động của gan và được sử dụng để chẩn đoán, theo dõi bệnh tật, nhiễm trùng và tổn thương gan.
Bạn có thể được kiểm tra chức năng gan nếu có các triệu chứng như vàng da, đau bụng, buồn nôn, ói mửa, sưng bụng, nước tiểu sẫm màu. Ngoài ra, các tình trạng còn có thể gặp như chảy máu hoặc bầm tím bất thường, ngứa quá mức nhưng không phát ban, chán ăn, mệt mỏi, giảm cân không thể giải thích.
Bạn đã chụp X-quang bụng, siêu âm, chụp cắt lớp vi tính (CT) hoặc chụp cộng hưởng từ (MRI) và có phát hiện bất thường. Xét nghiệm chức năng gan có thể được thực hiện nếu đánh giá thêm. Người có tiền sử viêm gan, ung thư gan, ghép gan, xơ gan (bệnh gan giai đoạn cuối) sẽ cần tái khám định kỳ để đánh giá những thay đổi trong chức năng của cơ quan này. Dưới đây là một số xét nghiệm thường sử dụng.
Xét nghiệm ALT, AST
Các xét nghiệm này đo hàm lượng enzym được giải phóng từ các tế bào gan bị tổn thương. Bất kỳ những tác nhân nào làm tổn thương gan đều có thể dẫn đến mức enzym cao. Điều tương tự cũng xảy ra đối với các yếu tố làm giảm lưu lượng oxy hoặc máu đến gan. Mức ALT bình thường là 8-37 IU/L. Trong khi AST 10-34 IU/L là bình thường.
Xét nghiệm máu thường được dùng để kiểm tra tình trạng gan. Ảnh: Shutterstock
Xét nghiệm máu thường được dùng để kiểm tra tình trạng gan. Ảnh: Shutterstock
Xét nghiệm Albumin
Albumin là mloại protein được tạo ra bởi gan. Nếu gan bị tổn thương mạn tính hoặc cấp tính, mức albumin trong máu thường sẽ dưới mức bình thường 3,9-5,0g/dL.
Xét nghiệm ALP
Enzym Alkaline Phosphatase (ALP) tăng cao thường là có vấn đề trong các ống dẫn dẫn mật từ các tế bào bên trong gan vào và ra túi mật đến tá tràng (phần đầu tiên của ruột non). Xương và một số mô khác tự tạo ra phosphatase kiềm cũng có thể dẫn đến ALP cao, ngay cả khi gan hoạt động bình thường. Lượng enzyme này cao cũng có thể liên quan đến các bệnh xương khớp. Mức bình thường là 44-147 IU/L.
Xét nghiệm Bilirubin
Bilirubin được tạo ra khi cơ thể phá vỡ các tế bào hồng cầu. Mức độ cao có thể chỉ ra tình trạng sức khỏe như thiếu máu, vàng da hoặc bệnh gan. Xét nghiệm này giúp đo tổng lượng bilirubin trong máu. Rối loạn chức năng gan dẫn đến sự tích tụ của bilirubin trong máu. Do bilirubin có màu vàng nên bạn có thể nghi ngờ bị vàng da, vàng mắt dù chưa thực hiện xét nghiệm này. Tuy nhiên, tổng mức bilirubin có thể tăng lên trước khi vàng da trở nên rõ ràng. Mức bình thường là 0,2-1,9 mg/dL.
Xét nghiệm GGT
Gamma-GDướilutamyl Transferase (GGT) là một loại enzym được tìm thấy khắp cơ thể, nhưng chủ yếu ở gan. GGT có thể tăng cao trong bệnh gan giai đoạn đầu. Mức GGT của bạn có thể tăng cao khi suy tim sung huyết. Nó cũng có thể tăng lên sau khi sử dụng rượu nặng. Mức bình thường khoảng 8-61 U/L.
Bạn có thể cần kiêng ăn và uống từ 6-8 giờ, một số loại thuốc trước khi xét nghiệm máu. Theo Verywell Health, vì chức năng gan được kiểm tra bằng xét nghiệm máu định kỳ nên có rất ít rủi ro và không có chống chỉ định.
Bạn cũng có thể cần thực hiện các xét nghiệm chức năng gan tại một số thời điểm. Ví dụ, nếu bạn bị bệnh gan do rượu có thể cần phải kiểm tra theo dõi trong 6 tháng để xem các chỉ số có được cải thiện sau khi ngừng uống rượu hay không. Trường hợp người bệnh đã bị tắc nghẽn ống mật có thể cần điều trị can thiệp hoặc phẫu thuật. Bạn nên thực hiện lại các xét nghiệm trong vòng vài tuần để theo dõi chức năng gan. Trường hợp bệnh nặng, bạn có thể cần kiểm tra men gan thường xuyên. Nếu kết quả cho thấy khả năng bị ung thư, bạn có thể cần sinh thiết hoặc xét nghiệm khác.
0 notes
Text
Marked and early elevations of alkaline phosphatase is the earliest marker of metastatic liver cancers. Bilirubin and gamma glutamyl transferase (GGT) are the other two early indicators. Alkaline phosphatase provides for the most reliable liver function testing for demonstrating primary or metastatic tumors to the liver. Please note that increased levels of transaminases (AST or ALT) are the most sensitive markers for the liver cancers, but their levels do not rise as early or as abruptly as alkaline phosphatase.
3 notes
·
View notes
Text
Lupine Publishers | Nanotechnology in Phytotherapy: The Effect of Noni’s Nanoemulsion on Bacterial Translocation Induced By Experimental Model of Intestinal Ischemia and Reperfusion
Lupine Publishers | Journal of Health Research and Reviews
Abstract
Background: The study evaluated nano structured extract Morinda citrifolia L. (Noni) conveyed in enteral form, in an experimental model of intestinal ischemia/reperfusion (I/R), as well as in the prevention of bacterial translocation.
Purpose: Observe the protective and repairing effect of Noni’s nanoemulsified extract in the presence of induced bacterial translocation, by an experimental model of intestinal ischemia/reperfusion.
Methods and Findings: The study consisted of 2 groups of 7 animals, where the Controls were treated with 0.9% saline solution (I/R + S) and Experimental group (I/R + Noni) treated with 5 mg/ml/Kg Noni nanoemulsion, orally by gavage 12h and 2h before the experiment. In the groups, the superior mesenteric artery was occluded with a vascular micro clamp and the laparotomy reopened 60min. after for pull back the clamp. Treatment response was assessed by blood count, inflammatory markers and biochemical dosages, including a sample of the terminal ileum and hepatic of each animal was harvested, fixed in formalin 10% and included in paraffin and stained with hematoxylin-eosin for morphometric measurement. Measurement of TNF-α, IL-1β, IL-6, and IL-10 was done. One gram of spleen, liver, and mesenteric lymph nodes were harvested for culture by selective means for Gram (-) and Gram (+) bacteria. ANOVA and the post-hoc Turkey and Student´s t test were used, considering p<0, 05 as significant.
Conclusion: Noni´s nanoemulsion positively influenced the organic reactions in the presence of intestinal ischemia/reperfusion, reducing the production of pro inflammatory cytokines, bacterial translocation, preventing tissue injury and attenuating the systemic inflammatory response against the experimental model used
Keywords: Noni: Ischemia-reperfusion injury; Bacterial translocation; Biotechnology; Nanotechnology; phytotherapy
Abbreviations: GGT: Gamma-glutamyl Transferase; ECUA: Ethics Committee on the Use of Animals; NCCAE: National Council for Control of Animal Experimentation; NO: Nitric oxide; AST: glutamic-oxalacetic transaminase; ALT: glutamic-pyruvic transaminase; HSV: total bilirubin and fractions, erythrocyte sedimentation rate; SMA: Superior Mesenteric Artery
Mammography
Intestinal ischemia-reperfusion (I-R) injury is a severe condition resulting from acute mesenteric ischemia, small bowel transplantation, abdominal aortic aneurysm, hemorrhage, trauma, septic shock, or severe burns. Various chemical and cellular mediators have been implicated in the pathogenesis of intestinal ischemia/reperfusion, such as reactive oxygen, cytokines, endotoxins, and neutrophils [1]. Following adhesive interactions among neutrophils and endothelial cells, neutrophil accumulation in the intestinal mucosa contributes to intestinal ischemia/ reperfusion injury via production of reactive oxygen metabolites and proteases. Leukocyte accumulation is a complex phenomenon that also involves endothelium-based adhesion molecules as well as leukocyte chemotaxis factors such as interleukin-8 (IL-8) [2,3]. Intercellular adhesion molecules are normally expressed at a low basal level, but their expression can be enhanced by several inflammatory cytokines such as IL-1β and tumour necrosis factor-α (TNF-α). A variety of cytokines, including TNF-α, interferon-γ, and IL-1β, are released from post-ischemic tissues [4].
It is now considered that these mediators bring about the systemic microcirculatory injury which is thought to be the main mechanism responsible for damage in sepsis. The host defence responses to sepsis may promote the generalized increase in leukocyte recruitment and accumulation in the tissues, which may lead to subsequent endothelial damage, leaky capillaries, and organ dysfunction and failure [5,6]. The organic lesion begins in the lungs, progressing to the anguish respiratory syndrome, followed by kidney and liver failure because of damage caused by the architecture of these organs. Heart failure occurs in late-stage sepsis [7]. The pathophysiology of intestinal ischemia/reperfusion (I/R) in rats with induction of bacterial translocation is widely used in animal models and well established in the literature, and is a viable way of analyzing therapeutic options [8].
The technique will result in a bacterial translocation, generating an ideal model for the therapeutic trial with Noni. Medicinal plants influence the health conditions of the people, in part due to the increase of studies with phytotherapeutics, leading to a confirmation of the therapeutic action of several popular plants, a fact that proves Phytotherapy as part of the culture of the population, being used and widespread for many generations[9-11]. In Brazil, the use of medicinal herbs has its bases in the indigenous practice, which influenced by the African and Portuguese culture, generated a vast popular culture. With the technological advances in allopathic medicine and the pharmaceutical industry in recent years, herbal medicines have been placed in the background, being something allied to popular belief and without scientific bases [12]. However, due to side effects and the high cost of medicines, Phytotherapy is again highlighted and scientific studies with medicinal plants are being resumed [13].
Among the species for herbal treatment highlights the Morinda citrifolia L. (Rubiaceae), popularly known as Noni. Information on its therapeutic benefits has gone through the world causing great demand as a medicinal product [14-16]. Morinda citrifolia L (Noni) has the phytotherapeutic activity of analgesic, antimicrobial, antitumor, anti-inflammatory and antioxidant effects. In scientific studies conducted for the isolation of fixed compounds of the plant, about 200 active substances have already been isolated, where the presence of anthraquinones, triterpenes, iridoids, among others [7- 9]. The anti-inflammatory activity of Noni has been studied in vivo and in vitro by inhibiting the activity of COX-1 enzymes and COX- 2, and the release of chemical mediators from macrophages (nitric oxide (NO) and prostaglandin E2 - PGE-2)[10].
In this sense, products using biotechnology in the form of nanoparticles or nanostructured compounds, can have excellent results, since, due to their reduced diameter, the substance can be used in smaller doses, avoiding the toxic effect of the plant and maintaining its phytotherapic action [11-13]. Thus, the objective of the present study was to evaluate the protective and repairing effect of Noni’s nanoemulsified extract in the presence of induced bacterial translocation, by an experimental model of intestinal ischemia/ reperfusion (I/R) in rats, using the dosage and subsequent blood count, inflammatory markers and biochemical measurements, including histopathological analysis of the compared to the control group treated with 0.9% saline solution.
Material and Methods
Ethical Principles
The experimental protocol was approved by the Ethics Committee on the Use of Animals - ECUA, number 012/2016, Brazil. Animals were handled in accordance with the Guide for the Care and Use of Laboratory Animals, US National Research Council, 1996. The Institutional Committee on Ethics in the Use of Animals approved the research project under the protocol. The care with the use of the animals followed the standards of the Brazilian legislation for the scientific use of animals (Law 11.794 / 2008 National Council for Control of Animal Experimentation - NCCAE / Brazilian Government).
Preparation of vegetable extract hydroalcoholic extract of Morinda citrifolia L: (Noni)
The hydroalcoholic extract of Morinda citrifolia L. was prepared from the aerial parts (stem, leaves, and fruits) of fresh adult plants. The collected material was placed for drying at room temperature; then comminuted with a knife and placed for 24h in an oven at a temperature between 45ºC and 50ºC to remove moisture. It was then subjected to a grinding process to obtain the powder. This material was weighed and deposited in a glass vessel with the addition of 70% hydroalcoholic solution in the ratio of 1:3 of the powder. The resulting mixture was stirred for 12h and stirred for five minutes every two hours under two simple filtration procedures under reduced pressure to give the crude extract, which was concentrated in a rotary evaporator under reduced pressure, at a temperature between 55°C and 60°C, for total solvent elimination. The product obtained after concentration was in the form of a paste which was diluted in distilled water until a hydroalcoholic extract at the concentration of 5mg/ml was obtained, being kept in a refrigerator at 10ºC until it was used.
Obtaining Nanoemulsified Systems
Nanoemulsion systems were obtained by maceration in a mixture of ethanol: water (8:2/800mL of alcohol 70° INPM + 200mL of distilled water) according to the previously described methodology. The study of phase diagrams of the oil, water and surfactant mixture formed a nanoemulsified (SN) system with a self-emulsifying characteristic. The SN system was considered O/W of the autoemulsifying type due to the unchanging of its appearance after successive dilutions in water. The vegetable oil used contains the following chemical components: vitamin E, oleic, linoleic and linolenic acid, low saturated fat and high content of polyunsaturated components [17,18]. The procedure used to obtain the nano emulsion regions is based on the method involving the determination of the maximum solubility points of active matter (surfactant) in the aqueous and oily phases, by means of mass titrations. The structure is composed of vegetable oil in the range of 0.5% to 6.0%; a surfactant in the range of 8.0% to 20% and distilled water in the range of 75% to 90% (Figure 1).
Figure 1: Phase Diagram (Maciel 2009).
Description of Nanoemulsion Preparation: Initially, industrialized vegetable oil was weighed on a precision digital scale (model: FA-2104N / 2008; Brand: BIOPRECISA-->) in the preferred range (1% to 5%), the surfactant in the preferred range (8% to 20%), and distilled water in the preferred range (75% to 90%) mixed and heated the components of the formulated SME - Nanoemulsion System, in magnetic stirrer with heating - stirring range 100-2200rpm and temperature controlled in the preferred range between 40°C to 70°C (Model NI1103P/2009: Mark: NOVAINSTRUMENTS-->). Thereafter, centrifuged at a constant speed, between 550rpm and 650rpm, for a preferential time of 15 minutes. (Model TDL80-2B, Mark Centribio-->).
Analysis Characterization: Performed through the refractive index, droplet diameter, rheological behavior and surface tension. To obtain the refractive index, an analog bench refractometer (ABBE, Model: 2waj; Mark: BioBrix-->) was used at a temperature in the range of 20°C-30°C.
Determination of droplet diameter: The diameter of the nanoemulsion droplets was determined by measurements in triplicates and with the refractive index of 1.4715 with a light beam of 659nm wavelength and angle of incidence of 90°. The diameter of the droplets (ranged from 50nm-75nm).
Rheology: The evaluation made from the graph generated by shear stress versus shear rate using a greenhouse thermometer (HG - Brazil, No.1876/11-->), in the range of 20°C-30°C, with variation for the shear rate (1s-1-1000s-1), resulted in a linear behaviour, with r2 = 0.91058.
Fluid Classification: The fluid under analysis was classified as Newtonian and the viscosity was determined to be 2mPa.s - 6mPa.s (2cP - 5cP).
Maximum Dilution Analysis: The evaluation was performed by experimental data of surface tension. Assays were performed using the SensaDyne Tensiometer apparatus (model QC-600, Chem-Dyne Research Corp. - USA). The description of the method consisted of measuring the maximum bubble pressure using two capillaries with holes of different diameters, where an inert gas (N2) was pumped at a certain constant pressure (200-595kPa). The larger capillary measured the effect of the immersion depth and the smaller the surface tension. For each measurement, the samples were diluted in distilled water, with concentrations varying until the values of surface tension close to the water (γH2O = 72.1mN/m) and temperature in the range of 20°C to 30°C were reached.
Surgical model / experimental design: We used 14 Wistar male Wistar rats weighing 265±32g (from Nucleus of Experimental Surgery, Potigura Universty - LAUREATE INTERNATIONAL UNIVERSITIES - UnP/Natal/Rio Grande do Norte State/ Brazil), randomly divided into 2 groups, kept in individual cages with food and water standard (Labina-Purina-->) is rodents, ad libitum. In the experimental group (n=7) rats received 5mg/mL/Kg (EMS-FC5) Noni nanoemulsion via the probe/gavage 18 and 2 hours prior to clamping of the superior mesenteric artery (I/R), the remainder rats (n=7) were treated with oral saline solution at 0.9%, 18 and 2h prior to (I/R). After 12h of fasting, the rats were anesthetized with for the induction of anesthesia general, the solution of Zoletil--> 50, the anesthetic dissociative, will be used in the dose of 0.3mL/100mg intramuscularly in the region of the quadriceps, with disposable syringes of 1mL of insulin and needle 27F and operated under aseptic conditions. In groups I/R + Saline and I/R + Noni, under sterile conditions.
Measurement of bacterial translocation: After shaving, the abdominal skin was disinfected with 0.2% chlorhexidine. All procedures were performed under sterile conditions. A laparotomy was performed and the superior mesenteric artery (SMA) was occluded with a microvascular clamp for 60 minutes. In order to block any collateral blood supply, the right colic and proximal jejunal arteries were also clamped. The laparotomy incision was then closed, to be opened later for removal of the clamps after 60 minutes of ischemia. Reperfusion was confirmed by the return of the mesenteric arcade pulsation. The incision was closed again and the animals were killed by anesthetic overdose (thiopental 100mg/ Kg) after 120 minutes of reperfusion. They breathed spontaneously throughout the procedures.
Measurement of bacterial translocation: At the end of the procedures (time = 180 minutes), a midline laparotomy was performed under aseptic conditions and biopsies were aseptically obtained for bacterial colony counts. One gram of mesenteric lymph node complex, blood, liver, and lung were removed for culture. Tissues were homogenized and aseptically solubilized after addition of 0.5mL of 0.9% saline. Aliquots of 0.2mL were processed and cultured on selective MacConkey’s agar and Blood Agar for detection of gram-negative and gram-positive bacteria, respectively. The agar plates were incubated at 37oC and examined for growth after 24 and 48h. Any growth in the plates of bacteria of the same biotype as cultured was considered positive and expressed as colony-forming units per gram of tissue (CFU/g).
Laboratory analysis/ Cytokine Assays: After 24h of a conclusion of the procedures under anesthesia and aseptic conditions, blood was collected by cardiac puncture to measure the hemogram, hepatogram, cytokines, and albumin. Samples of blood were treated with EDTA and the plasma was separated by centrifugation at 2000rpm and stored in -80°C for later measurement of tumor necrosis factor (TNF-a) interleukin-6 (IL-6) and interleukin- 1b (IL-1b) by the ELISA (enzyme-linked all immunoassay kits from PeproTech--> (Rocky Hill, NJ, USA) according to the manufacturer’s recommended protocols. The fluorescence was measured by a Bio-Tec--> Instruments EL808 ultra microplate reader, using KC4-V3.0 analysis software. The sensitivity of detection was 30pg/mL for all cytokines. For counting leukocytes and red cells using an automated cell counter (Abbott Cell-Dyn 3500R CD--> 5L-3500, USA). For albumin, alkaline phosphatase, gamma-glutamyl transferase (GGT), glutamic-oxalacetic transaminase (AST), glutamic-pyruvic transaminase (ALT), total bilirubin and fractions, erythrocyte sedimentation rate (HSV) blood was treated with EDTA.
Histological study: Terminal ileum and liver specimens were fixed in 10% buffered formalin and embedded in paraffin. Sections cut at a thickness of 4μm were stained with hematoxylin and eosin for morphometric measurements using an image analyzer (Image- Pro Plus, Media Cyber-->)[19-21]. The damage of the intestinal specimens was assessed in a blinded manner by an experienced pathologist according to microscopic criteria for degree of damage based on a grading system previously described: normal mucosa, 0; subepithelial space at the villus tip, 1; more extended subepithelial space, 2; epithelial lifting along villus, 3; denuded villi, 4; loss of villus tissue, 5; crypt layer infarction, 6; transmucosal infarction, 7; transmural infarction, 8.
Statistics: Data analysis was performed using the BioEstat--> 2.0 program. Differences between the microbiological samples as measured by positive cultures were evaluated by a test for differences between proportions. The results were tabulated and compared by ANOVA using post hoc analysis with Tukey and Student’s t test. P<0.05 was considered significant. Data on continuous quantitative variables are the mean ± expresso standard deviation. In the variables that did not present normal distribution, the logarithmtransformation method was adopted. These variables are represented by their respective logarithms. To verify if the differences between the Experimental (Noni nanoemulsion) and Control groups were statistically significant, the Student’s t-test for independent samples was used. The statistical package SPSS-->21 was used.
Results
We observed bacterial translocation to mesenteric lymph nodes, liver, lung, and blood in all animals subjected to I / R. However, in I/R group rats treated with Noni nanoemulsion, translocation to these organs and blood was significantly lower than in I/R untreated (Table 1). Cytokines had lower levels of proinflammatory cytokines in group I/R+Noni (TNF-α, IL-1β, IL-6) and a higher level of antiinflammatory-cytokine (IL-10), when compared with I/R + Saline (C) (Table 2). In I/R + Saline (Control) group rats, the levels of pro-inflammatory cytokines were significantly higher when compared to I/R+Noni. This group had the highest values of IL-10 when compared with (Control) group (p<0.05). Noni was able to maintain and modulate the inflammatory reaction in the experimental group, which was proven through normality in the hematological dosages. There was also a significant reduction in the number of total leukocytes, which did not generate immune suppression in experimental animals, but control the systemic inflammatory response in the presence of induced bacterial translocation for intestinal ischemia and reperfusion.
Table 1: Bacterial Translocation in groups treated and not treated with Noni nanoemulsion (colony-forming units per gram of tissue - CFU/g).
*p < 0.01 compared with groups I/R + Saline (C) and I/R + Noni nanoemulsion.
Table 2: Serum levels of cytokines in groups with and without Noni nanoemulsion treatment.
*p< 0.01 compared with groups I/R + Saline (C) and I/R + Noni nanoemulsion.
Table 3: Descriptive and inferential statistics of hemograma results.
Figure 2: The mucosa is injured, and leukocyte infiltration of lamina propria and mucosa are shown (group I/R), 100x. 2: Hemorrhage and inflammation of mucosa (group I/R), 100x.
A trend towards normality was observed in the other cellular parameters measured in relation to the control group (Table 3). Macroscopically, the segments of the organs studied presented intramural dilation and hemorrhage, with greater intensity in rats of the I / R group, compared to the experimental group (Noni). Microscopic findings revealed marked mucosal lesion after ischemia and reperfusion injury; we observed more intense lesions in the rats of the I / R group compared to the other groups. The most frequent lesions were: disorganization of the normal tissue structure, transmural infarction, infiltration of leukocytes in the lamina propria and mucosa, alveoli and hepatic sinusoids. In the group that used the nanoemulsion of Noni, there was protection and preservation of the tissue structure, with reduced or absent infiltrating inflammatory reaction (Figures 2-4).
Figure 3: Preserved intestinal mucosa, demonstrating normal villi and intestinal epitelial cells of uniform pattern, normal to histological examination, 100x
Figure 4: A) Normal liver structures are demonstrated. B) A hepatic section from a septic rat with vehicle (normal saline) treatment. Patches of hepatocytes show necrosis with eosinophilic cytoplasm nuclei that are condensed and intensely stained with hematoxylin. C: A section from a septic rat with Morinda citrifolia L (Noni) treatment. Liver structures appear normal. (HE.50;100 x /100 μm).
Discussion
The present study used an experimental model of ischemia and reperfusion, to verify the effect of nanostructured extract Morinda citrifolia L. (Noni) on intestinal injury and bacterial translocation. Some authors consider the bacterial factor, crucial in the pathogenesis of sepsis and multiple organ failures [22]. In surgery and intensive care, intestinal obstruction and intestinal ischemia are the most associated pathological conditions [23]. The use of medicinal plants for the treatment of diseases has been occurring since the dawn of civilization. The development of methodologies for the isolation of active substances has made it possible to identify substances in complex samples such as plant extracts. In this way, the interest for compounds of vegetal origin that could be used as prototypes for the development of new drugs resurfaced [24]. Medicinal plants represent the main raw material used for the synthesis of medicinal products, besides being used as therapeutic agents. Plant consumption is overvalued in traditional use based on it medicinal benefits [25].
Noni (Morinda citrifolia L.) has become a promise of the cure for a variety of diseases, ranging from simple hypertension to malignant tumors; even provokes the cure of syndromes, still incurable such as AIDS and other viral diseases [26]. However, The popular use and wellbeing attributed to Noni make the industry commercially explore Morinda citrifolia L products, often without scientific evidence [15].In this context, the use of biotechnology transforming Noni into a nanostructured compound, has the advantage of using the plant’s medicinal properties, reducing its toxicity, keeping its bioactive principles beneficial to health [27,28]. Antimicrobial activity of Noni has already been reported in the literature. Studies have shown that noni inhibited growth in vivo and in-vitro bacterial strains such as Staphylococcus aureus, Pseudomonas aeruginous, Bacillus subtilis, Escherichia coli, Helicobacter pylori, Salmonella and Shigella.
In addition, Noni has already been studied on its effect against Plasmodium falciparum, believed to be due to the presence of anthraquinones, acubin, L-asperuloside, alizarin, scopoletin, among other substances [29,30]. It has also been found that ethanol and hexane extracts of noni have an antitubercular effect since they inhibit by 89-95% the growth of Mycobacterium tuberculosis. The major components identified in the hexane extract were E-phytol, cycloartenol, stigmasterol, b-sitosterol, campesta-5,7,22-trien-3-bol, and the ketosteroids, stigmasta-4-en-3-one and stigmasta-4-22- dien-3-one[18-20]. Moreover, they showed that the anti-microbial effect is highly dependent on the stage of ripeness and on processing, being greater when the fruit is ripe, without drying [23-25]. The limiting factor for the use of Noni as an herbal remedy is that most of the studies previously found in the literature, administer the extract in the alcoholic or hydro-alcoholic form, which may, through prolonged use, mainly cause hepatotoxicity [24].
With this in mind, the present study makes its scientific contribution to demonstrate that with the use of biotechnology in the formulation of a nanostructured extract of Noni, such undesirable side effects were abolished, maintaining the active principles of the vegetable under analysis [31]. Recent studies have demonstrated, respectively, the efficiency of Noni´s nanoemulsion in experimental models of healing of infected wounds in the skin of rats as well as in abdominal sepsis induced by cecum ligation and puncture [32,33]. This phenomenon was confirmed in the present study, where a reduction in the total leukocytes and polymorphonuclear levels was observed, maintaining normal hemoglobin and hematocrit levels in the experimental group, which used Noni in the presence of an experimental model of intestinal ischemia/reperfusion (I/R) in rats with induction of bacterial translocation.
Conclusion
In conclusion, the present study demonstrated that Noni’s nanoemulsified extract acted as an immune modulatory agent in the presence of an experimental model of intestinal ischemia/ reperfusion (I/R) in rats with induction of bacterial translocation, reducing the systemic inflammatory response, stimulating the immunity of experimental group animals, preserving liver function and maintaining its bioactive principles beneficial to the experimental model used
For more Lupine Publishers Open Access Journals Please visit our website: h
http://www.lupinepublishers.us/
For more Journal of Research and Reviews on Healthcare Research articles Please Click Here:
https://lupinepublishers.com/research-and-reviews-journal/
To Know More About Open Access Publishers Please Click on Lupine Publishers
#Lupine publishers#Lupinepublishers#Lupine Publishers Group#journal of research and review#open access publishers
4 notes
·
View notes
Photo
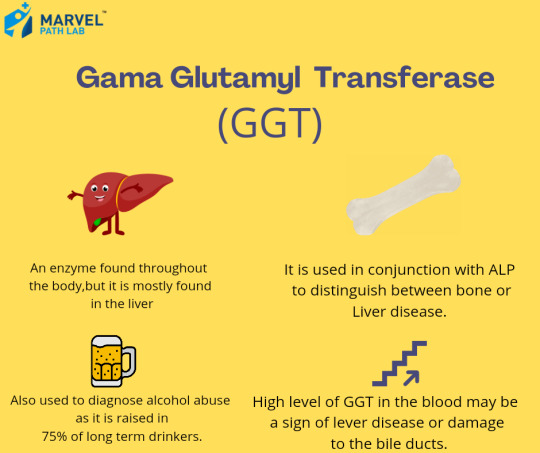
Gamma GT, also known as Gamma-Glutamyl Transferase (GGT), is an enzyme found throughout the body, but it is mostly found in the liver. Levels of GGT typically rise after heavy alcohol intake that has continued for several weeks, which is why it is often used to diagnose alcohol abuse (as 75% of long-term drinkers have raised levels). Prolonged, continuous, heavy alcohol intake can lead to liver damage. When the liver is damaged, GGT may leak into the bloodstream🩸. High levels of GGT in the blood may be a sign of liver disease or damage to the bile ducts. Check your liver function today with our at-home Liver Blood Test. CALL US AT 8222999888 FOR BOOK A TEST. #marvelpathlab #marvellab #health #liver #livercare #ggt bloodtest #homecollection #medical
0 notes
Text
Thyrocare Aarogyam Male Profile
Thyrocare Aarogyam Male Profile
Includes 93 Test Parameters | Price: 2400/- Only | Fasting Needed | Sample Type: Blood
IRON DEFICIENCY [3]
% TRANSFERRIN SATURATION
IRON
TOTAL IRON BINDING CAPACITY (TIBC)
LIVER [11]
SERUM ALB/GLOBULIN RATIO
ALKALINE PHOSPHATASE
BILIRUBIN -DIRECT
BILIRUBIN (INDIRECT)
BILIRUBIN – TOTAL
GAMMA GLUTAMYL TRANSFERASE (GGT)
PROTEIN – TOTAL
ALBUMIN – SERUM
SERUM GLOBULIN
ASPARTATE AMINOTRANSFERASE…
View On WordPress
0 notes
Text
Liver Function Test In Delhi
The liver has a significant role in metabolism, regulation of red blood cells (RBCs), and glucose synthesis and storage. The liver function tests typically include alanine transaminase (ALT) and aspartate transaminase (AST), alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), serum bilirubin, prothrombin time (PT), the international normalized ratio (INR) and albumin. These tests can be helpful in determining an area of the liver where damage may be taking place and depending on the pattern of elevation can help organize a differential diagnosis.
0 notes