#LUMBAR FUSION
Text

Yup I'm cyborg.
5 notes
·
View notes
Text
CONSIDERING LUMBAR FUSION | DR. DILIP KIYAWAT
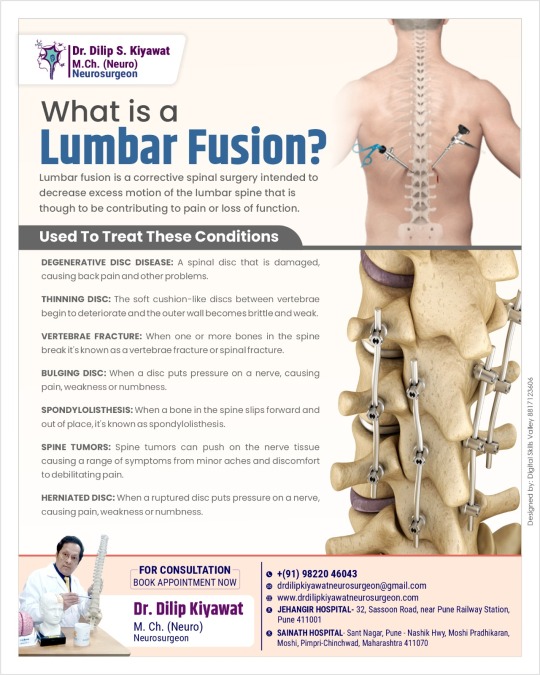
If you’re struggling with chronic back pain and reduced mobility, lumbar fusion might be the answer to your problems. This surgical procedure is designed to stabilize the spine and alleviate pain by reducing excessive movement in the lumbar region. Let’s explore what lumbar fusion is, the conditions it treats, and how you can benefit from a consultation with Dr. Dilip Kiyawat, a leading neurosurgeon specializing in lumbar fusion surgeries.
WHAT IS LUMBAR FUSION?
Lumbar fusion is a surgical procedure that aims to join two or more vertebrae in the lower back. By fusing these vertebrae together, the procedure eliminates the movement between them, which can significantly reduce pain and improve function. This is particularly beneficial for patients experiencing pain due to spinal instability or degenerative conditions.
CONDITIONS TREATED BY LUMBAR FUSION
Lumbar fusion is effective in treating a variety of spinal conditions, including:
Degenerative Disc Disease: Over time, the discs between vertebrae can deteriorate, causing pain and reduced flexibility.
Thinning Disc: Aging and other factors can lead to discs losing their cushioning ability, resulting in chronic back pain.
Vertebral Fracture: Fractures in the spine can cause instability and significant pain, often requiring surgical intervention to stabilize the spine.
Bulging Disc: When a disc protrudes beyond its normal boundary, it can press on spinal nerves, causing pain and numbness.
Spondylolisthesis: This condition occurs when one vertebra slips forward over the one below it, leading to pain and potential nerve damage.
Spine Tumors: Tumors in or around the spinal column can compromise the spine’s stability and function, necessitating surgical removal and stabilization.
Herniated Disc: A herniated disc happens when the inner gel-like core of a disc leaks out, irritating nearby nerves and causing significant pain.
EXPERT CONSULTATION WITH DR. DILIP KIYAWAT
Considering lumbar fusion surgery can be daunting, but with the right specialist, you can navigate this journey with confidence. Dr. Dilip Kiyawat is a distinguished neurosurgeon known for his expertise in lumbar fusion surgeries. Here’s why consulting with Dr. Dilip Kiyawat is a smart choice:
Expertise and Experience: With extensive experience in neurosurgery and spinal procedures, Dr. Dilip Kiyawat has successfully performed numerous lumbar fusion surgeries, helping patients regain their mobility and quality of life.
Personalized Care: Dr. Dilip Kiyawat believes in a patient-centric approach, taking the time to understand each patient’s unique condition and concerns. He tailors treatment plans to meet individual needs, ensuring the best possible outcomes.
Advanced Techniques: Staying abreast of the latest advancements in spinal surgery, Dr. Dilip Kiyawat employs cutting-edge techniques to enhance surgical precision and recovery times.
Comprehensive Support: From initial consultation to post-surgery recovery, Dr. Dilip Kiyawat and his team provide comprehensive support and guidance, ensuring a smooth and stress-free experience.
BOOK YOUR APPOINTMENT TODAY
Don’t let chronic back pain control your life. If you’re considering lumbar fusion, schedule a consultation with Dr. Dilip Kiyawat to explore your treatment options. With his expertise and compassionate care, you can look forward to a pain-free future and a return to your daily activities.
For More information:
Website: https://drdilipkiyawatneurosurgeon.com/
E mail: [email protected]
Mobile Number: 9822046043
Address: Railway Station, 32, Sasoon Rd, near Pune, Central Excise Colony, Sangamvadi, Pune, Maharashtra 411001
0 notes
Text
Continually toward Health
So, my A1C increased slightly, and I still don’t require any medication. My cholesterol is normal, and my blood pressure is superb. I believe I’m close to getting myself under control. I have even improved my diet somewhat.
Yesterday, I started physical therapy. I have been having pain in my hips. It turns out it isn’t my hips at all. As I understand it, because I have a lower lumbar fusion, the…

View On WordPress
1 note
·
View note
Text
#Vertiflex Superion Procedure#Dorsal Ganglion Root Stimulation#Pain Specialist Chicago#DRG Treatment#Chronic Pain Treatment in Chicago#Lumbar Spinal Stenosis Surgery Chicago#DRG Stimulation Procedure#Pain Management Specialists Chicago#DRG Stimulator Surgery#Spinal Cord Pain Treatment Chicago#Dorsal Root Ganglion Stimulation Therapy#Motor Vehicle Injuries Treatments#Sacroiliac Joint Fusion Treatment#Lower Back Pain Relief#Spinal Cord Stimulation Therapy#Lumbar Spinal Stenosis Treatment
0 notes
Text
Revolutionizing Lumbar Fusion Surgery: The MedSpine Experience in Chenna
Introduction:
In the bustling city of Chennai, finding the best lumbar fusion surgery specialist in Medavakkam can be a daunting task. However, MedSpine emerges as a beacon of excellence in spinal healthcare, offering top-tier services and unparalleled expertise in lumbar fusion surgery.
A Center of Repute: Lumbar Fusion Surgery in Perumbakkam
Located conveniently in Perumbakkam, MedSpine stands as a lumbar fusion surgery center of repute, catering to patients from across Chennai and beyond. With a commitment to excellence and patient-centric care, MedSpine has earned its reputation as the go-to destination for individuals seeking relief from chronic back pain and spinal instability.
Personalized Care at Royapettah Clinic
At MedSpine's state-of-the-art clinic in Royapettah, patients receive comprehensive care and personalized attention from a team of skilled professionals. Whether it's a consultation with the best lumbar fusion surgery specialist in Medavakkam or a post-operative follow-up appointment, every aspect of the patient's journey is meticulously managed to ensure optimal outcomes.
Comprehensive Stability: 360-Degree Fusion Surgery
For those requiring more extensive intervention, MedSpine also specializes in 360-degree fusion surgery in Chennai. This comprehensive approach involves fusing together the entire circumference of the affected vertebrae, providing maximum stability and support to the spine. With MedSpine's expertise in this advanced procedure, patients can rest assured knowing that they are in capable hands.
Minimally Invasive Solutions: Lateral Lumbar Interbody Fusion Surgery
One of the key specialties offered at MedSpine is lateral lumbar interbody fusion surgery, a minimally invasive procedure that allows for the fusion of vertebrae from the side of the spine. This innovative approach reduces surgical trauma, minimizes blood loss, and promotes quicker recovery compared to traditional techniques, making it an attractive option for many patients.
Holistic Patient Care:
Furthermore, MedSpine's commitment to excellence extends beyond the operating room. The clinic's multidisciplinary team of specialists works collaboratively to provide holistic care, encompassing pre-operative education, surgical intervention, and post-operative rehabilitation. This comprehensive approach ensures that patients receive the support they need at every stage of their journey towards recovery.
Conclusion:
In conclusion, MedSpine stands as the best lumbar fusion surgery clinic in Royapettah, offering unparalleled expertise and compassionate care to patients in Chennai and beyond. Whether it's a lateral lumbar interbody fusion surgery or a 360-degree fusion procedure, patients can trust MedSpine to deliver exceptional results and help them reclaim their lives from chronic back pain and spinal instability.
0 notes
Text
0 notes
Text
Anterior-Lumbar-Interbody-Fusion
The procedure generally takes 2–3 hours total, not including a few hours after to rest and recovery while being monitored by the staff. Patients will usually spend a few nights in the hospital and will be able to walk within that time. Depending on the level of correction and the area, we may prescribe a back brace in order to support the spine. If you are suffering from any lumbar spine issues and would like to learn more about Anterior Lumbar Interbody Fusion, or ALIF, contact Dr. Vikas Varma today.

0 notes
Text
Anterior Lumbar Interbody Fusion (ALIF) Market – Industry Trends and Forecast to 2028
#Anterior Lumbar Interbody Fusion (ALIF) Markettrend#Anterior Lumbar Interbody Fusion (ALIF) Marketforcaste#Anterior Lumbar Interbody Fusion (ALIF) Marketsegment#Anterior Lumbar Interbody Fusion (ALIF) Marketoverview#Anterior Lumbar Interbody Fusion (ALIF) Marketgrowth#Anterior Lumbar Interbody Fusion (ALIF) Marketshare#Anterior Lumbar Interbody Fusion (ALIF) Marketdemand
0 notes
Text
Non Fusion Spine Surgery Tampa Florida
Are you experiencing severe neck pain? Cervical disk replacement surgery or Non Fusion Spine Surgery Tampa Florida is a newly FDA-approved treatment that involves the removal of a damaged cervical disk and its replacement with an artificial disk to alleviate pain. When compared to typical cervical disk surgery, this surgery is preferable because it allows for more range of motion and puts less strain on your surrounding vertebrae. Visit Total Spine & Brain Institute today for more info! Visit: https://totalspinebrain.com/
#Non Fusion Spine Surgery Tampa Florida#Thoracic & Lumbar Spine Tampa Florida#Brain Surgery Florida#Back Pain Doctor#Back Pain Clinic#Tampa Bay Neurosurgeon#Brandon Neurosurgeon#spine surgery#Neurosurgeon Tampa Florida#Neurosurgeon Near Me#neurosurgeon#spine specialist#spine surgeon
0 notes
Text
youtube
Post Spine Surgery Rehabilitation | exercises after lumbar fusion | Rehab After Spinal Fusion
A physical therapist will frequently use a number of techniques to assist a patient recover from a back injury and get back in outstanding physical condition.
#Back surgery rehab#Rehabilitation after spinal surgery#Rehabilitation after lumbar disc surgery#Rehabilitation after back surgery#Post spinal surgery physiotherapy#Physiotherapy after back surgery#Post spinal surgery rehabilitation#Rehabilitation after spinal fusion#Physiotherapy after lumbar spine surgery#Physical therapy after laminectomy#Youtube
0 notes
Link
0 notes
Text
Please Care to Read

hey guys, i’m alexa im a 23 yr old mentally/and physically disabled mexican/indigenous american now living in the balkans. as you know I’ve had a gofundme for my spinal operation running for several months now with not a lot of luck. I am suffering from a degenerative spinal cord due to an emergency spinal fusion I received after trying to commit suicide by jumping off a bridge onto a busy freeway. im in and out of wheelchairs/other mobility aids but most of the time I am admitted to full time bed rest. due to not being able to afford my surgery I have had to rely on opiates like tramadol, and palexia as well as arcoxia and morphine (all prescribed) just so im not in excruciating pain but these medications and the visits for my prescriptions refilled are very expensive and my only income in state disability (and u know how bullshit that is)
here’s some of my diagnoses (JUST FOR MY LUMBAR SPINE/PELVIC INJURY)

the more time that goes on, the more opiates I have to use to exist, are only weakening my body even more to the point where arthritis has grown throughout my entire body. it’s painful it sucks ! it sucks even more not being able to eat cus u can’t afford to, not being able to bathe yourself. my life has been spent in constant disability and as someone who is (legally) mentally disabled as well with bipolar 2, early onset schizophrenia, anorexia, autism, adhd, bpd, dpdr, ptsd, developmental disability, and a tonic clinic seizure disorder (seizures caused from stressed), it makes life EXTREMELY DIFFICULT.
We’ve only reached 13% of our goal in MONTHS now in my gofundme but hope still runs strong that me and my husband will get through this and do whatever we can we’re just reaching out for empathy, connection, and a helping hand in our darkest most difficult moment.
My gofundme link is currently not pasting to tumblr so I will attach it to this post but here’s what it looks like:
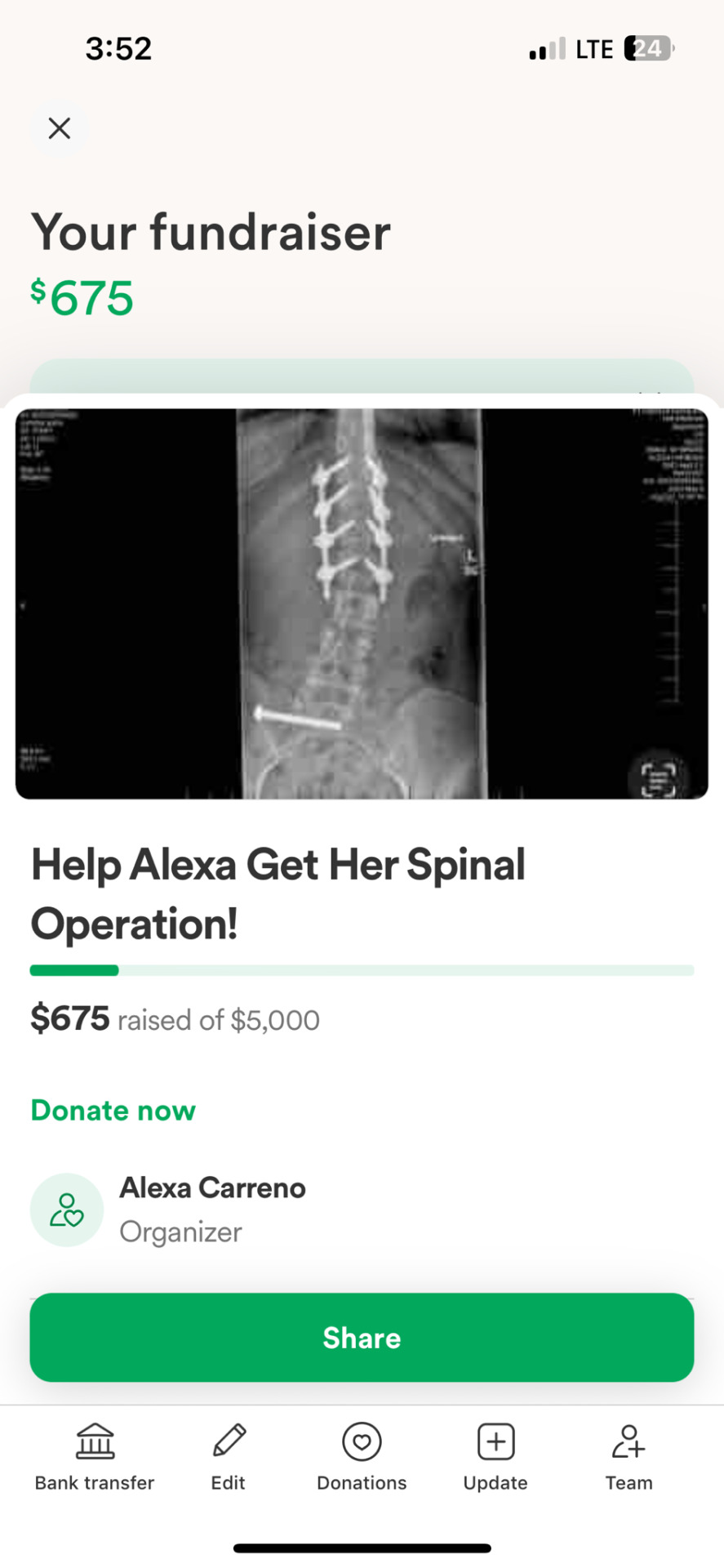
If you’d prefer not to use gofundme for any reason feel free to dm or my
PayPal - @gavinstrick
Venmo- @gavinstrick
Cashapp- $gavinstrick
Even if you could just spread the word , reblog this post, maybe you know someone who would like to help EVEN THE SMALLEST ACTIONS CAN CHANGE SOMEONES ENTIRE LIFE❤️
THANK YOU !!!💋❤️
550 notes
·
View notes
Text

The bones of your adult spine consist of 26 moveable joints. When these bones rub together or slip out of place, it causes pain and instability. If your back pain isn’t relieved by other forms of treatment, your doctor may recommend spinal fusion. During this procedure, your doctor attaches two or more vertebrae together to permanently stop movement between them, which prevents pain at the joint level.
To obtain the most effective back pain treatment, you must first obtain an accurate diagnosis of the cause of your pain so you can receive the best treatment.
Read more: https://premierspinenj.com/spinal-fusion/
#spinal fusion surgery#anterior lumbar fusion#minimally invasive sacroiliac joint fusion surgery#scoliosis spinal fusion
0 notes
Text
Risk Factor for Complex Regional Pain Syndrome - Juniper Publishers

Abstract
A narrative literature review of risk factor or predictor for Complex Regional Pain Syndrome (CRPS) or Reflex Sympathetic Dystrophy (RSD) was performed in the English language. Female sex, elderly people between the age of 45 and 65, pregnancy, intra-articular fracture, comminuted and displaced fracture, high energy trauma, severe fracture, strong pain after fracture, decreased sympathetic vasoconstrictor response after fracture, nerve and spinal cord injury, ankle dislocation, ankle fracture, injury in the extremities, treatment to the upper limb, motor nerve injury, decreased function before operation, poor physical functioning, higher median household income, economic compensation via work disability, social or psychological stress, good to excellent school performers, osteoporosis, hypertriglyceridemia, rheumatoid arthritis, musculoskeletal comorbidities, history of allergies, skin hypersensitivity, atopic background, asthma, trouble falling asleep, menstrual cycle-related problems, history of CRPS I, chronic pain, headache/migraine, first-degree family history of headache, fibromyalgia, multiple sclerosis, surgical or manipulative treatment, immobilization, plaster cast, longer duration of anaesthesia, barbiturates, angiotensin converting enzyme inhibitors, and specific gene are reported to be a risk factor for CRPS.
It is unknown whether smoking and diabetes are risk factors for CRPS. Obesity, hypothyroidism, anemia, and heart failure may be less likely to cause CRPS. I believe that depression and anxiety are consequence of CRPS. The incidence of CRPS varies greatly among studies. First, the concept of the disease changed, and the diagnostic criteria changed accordingly. Second, decision of abnormal right-left difference of each objective sign is based on a physician’s subjectivity. Third, discrimination between CRPS and the usual course of injury is based on a physician’s subjectivity. Identification of risk factor for CRPS provides some significance. First, it helps to find etiology of CRPS. Second, if a relative disease is found, treatment of the relative disease can be applied to CRPS. Third, it is helpful in the early detection of CRPS. Forth, it becomes helpful in an injury treatment such as fracture.
Keywords: Complex regional pain syndrome, Reflex sympathetic dystrophy, Algodystrophy, Subdeck’s atrophy, Causalgia, Risk factor, Predictor
Introduction
Complex Regional Pain Syndrome (CRPS), which was previously referred to as Reflex Regional Dystrophy (RSD), usually occurs after injury and/or surgery. CRPS is a disease that the orthopedic surgeons would like to ignore. Risk factors for CRPS were examined with a narrative review
Methods
A narrative literature review of risk factor or predictor for CRPS or RSD was performed in the English language. Some literatures that show risk factor or predictor for CRPS or RSD do not include the term of “risk factor” or “predictor” in the title, abstract, or key words, therefore, a systematic review is not useful to show risk factor or predictor for CRPS or RSD. I read all abstract of literatures of CRPS, RSD, causalgia between April 2003 and April 2018 using MEDLINE. In addition, in case of important literatures, I read the full text. Important old literatures before March 2003 about risk factor or predictor for CRPS or RSD are included in this review. Strictly speaking, the reported risk factors for occurrence of CRPS after stroke are often early symptoms of CRPS. In addition, orthopedic surgeons rarely treat CRPS after stroke. Therefore, risk factor for occurrence of CRPS after stroke is excluded from this review.
Results
Demographic information
Female sex: A population based retrospective study with all Mayo Clinic and Olmsted Medical Group medical records showed that gender specific incidence rates per 100,000-person years at risk were 8.57 and 2.16 for women and men, respectively [1]. Prevalence was 35.33 vs. 5.06 per 100,000 persons years for women and men, respectively [1]. A retrospective cohort study was conducted with electronic patient record data from 600,000 patients throughout The Netherlands [2]. Females were affected at least three times more often than males (ratio: 3.4) [2]. A total of 90 patients with distal radius fracture (DRF) was prospectively treated by closed reduction and casting and CRPS I occurred in 29 patients (32.2%) [3]. Logistic regression showed that risk for CRPS I was higher in cases of women (odds ratio [OR] 5.774: 95% Confidence Interval [CI] 1.391-23.966) [3].
Thirty-nine patients were diagnosed with CRPS immediately after Open Reduction and Internal Fixation (ORIF) for limb fracture from a cohort of 185,378 in patients treated with ORIF [4]. A comparable number of male and female patients suffered from CRPS [4]. Pons et al. [5] conducted a systematic search of the literature focused on determining the potential risk factors for the onset of CRPS 1 [5]. Female, particularly postmenopausal female was one of risk factors for the onset of CRPS 1 [5]. It is not possible to draw definite conclusions as this evidence is heterogeneous and of mixed quality, relevance, and weighting strength against bias and has not been confirmed across multiple trials or in homogenous studies [5].
Retrospective analysis of the Nationwide Inpatient Sample database from 2007 to 2011 in the United States [6]. There were 22,533 patients with the discharge diagnosis of CRPS type 1 of an inpatient sample of 33,406,123 [6]. Female gender was associated with higher rate of CRPS type 1 [6]. Using the Danish Patient Compensation Association’s database, Petersen et al. [7] identified 647 patients claiming CRPS following orthopedic treatment. The following ratios were found: women: men was 4:1 [7]. Multivariate logistic regressions were performed. Female gender was one of risk factors associated with posttreatment development of CRPS [7]. Database queries yielded 853,186 patients diagnosed or treated for DRF [8]. Multivariable logistic regression showed that female gender was positively associated with CRPS [8]. Of 165 patients who had suffered a mechanical traumatic injury isolated to their hand or forearm, 84 patients were diagnosed with CRPS [9] A logistic regression showed that risk for CRPS was higher in females [9].
A cross-sectional study in patients with distal tibial fracture showed that among the 488 patients RSD occurred in 45 patients, of whom 28 (62.22%) were female and 17 (37.77%) were male; there was thus a significant difference in the prevalence of RSD in terms of gender (P = 0.00; chi square test) [10]. Crijns et al. [11] identified 59,765 patients treated for a DRF, of whom 114 (0.19%) were diagnosed with CRPS [11]. Gender (women at greater risk, OR 3.86: 95% CI 1.99-7.49; p < 0.001) was independently associated with a diagnosis of CRPS [11]. A prospective observational study with 477 patients with a DRF who had been treated surgically reported that according to the multivariate analysis, female patients was significantly more likely to develop CRPS I (p = 0.02) [12].
Age: A retrospective cohort study was conducted with electronic patient record data from 600,000 patients throughout the Netherlands [2]. The highest incidence occurred in females in the age category of 61-70 years [2]. Retrospective analysis of the Nationwide Inpatient Sample database from 2007 to 2011 in the United States [6]. There were 22,533 patients with the discharge diagnosis of CRPS type 1 of an inpatient sample of 33,406,123 [6]. It peaks between age 45 and 55 [6]. Database queries yielded 853,186 patients diagnosed or treated for DRF [8]. Multivariable logistic regression showed that age >65 was negatively with CRPS [8]. Crijns et al. [11] identified 59,765 patients treated for a DRF, of whom 114 (0.19%) were diagnosed with CRPS [11]. Older age (OR 1.029; 95% CI 1.011-1.048; p = 0.002) was independently associated with a diagnosis of CRPS [11]. A case-control study using 249 patients with DRF who underwent surgical treatment (4% developed CRPS) showed that >60 years of age (OR 9.38: 95% CI 1.170-75.233) was a higher risk of developing CRPS [13].
Pregnancy: A population-based case-control study was conducted [14]. CRPS onset was increased during the first 6 months after pregnancy (OR 5.6: 95% CI 1.0-32.4), although based on small numbers (143 cases and 1493 controls) [14].
Condition of injury
Severity of injury: A total of 90 patients with DRF was prospectively treated by closed reduction and casting and CRPS I occurred in 29 patients (32.2%) [3]. Logistic regression showed that risk for CRPS I was higher in cases of medium and low energy trauma patients (OR 7.718: 95% CI 1.136-52.44) [3]. A prospective cohort study using 291 patients with traumatic hand injuries showed that patients with crush injuries were more likely to develop CRPS (OR 4.74: 95% CI 2.29-9.80) [15].
Severity of fracture: Pons et al. [5] conducted a systematic search of the literature focused on determining the potential risk factors for the onset of CRPS 1 [5]. Intra-articular fracture was one of risk factors for the onset of CRPS 1 [5]. Zyluk published a review about risk factors of CRPS and reported that patients with comminuted and displaced DRF (suggesting more severe trauma) showed higher incidence of CRPS than in those with minimally displaced fractures [16]. However, many studies are small and heavily biased towards DRF [16]. A prospective multicenter cohort study of 596 patients with a single fracture of the wrist, scaphoid, ankle, or the fifth metatarsal showed that dislocation and an intra-articular fracture contributed significantly to the prediction of the development of CRPS1 [17].
A cross-sectional study in patients with distal tibial fracture showed that the OR for RSD was 1.100 (95% CI 0.795-1.531) in patients with an injury severity score higher than the calculated mean score in patients without RSD [10]. Crijns et al. [11] identified 59,765 patients treated for a DRF, of whom 114 (0.19%) were diagnosed with CRPS. Concomitant fracture of the distal ulna (OR 1.54: 95% CI 1.05-2.23; p = 0.029) and open fracture (OR 0.414: 95% CI 0.192-0.895; p = 0.025) were independently associated with a diagnosis of CRPS [11].
A prospective observational study with 477 patients with a DRF who had been treated surgically reported that according to the multivariate analysis, those with a high energy trauma or severe fracture type were significantly more likely to develop CRPS I (p = 0.01 and 0.01, respectively) [12]. A case-control study using 249 patients with DRF who underwent surgical treatment (4% developed CRPS) showed that associated fracture (OR 12.95: 95%CI 1.614-103.861) and level of impact (OR 6.47: 95% CI 1.751-23.872) were higher risks of developing CRPS [13].
Pain due to fracture: A total of 90 patients with DRF was prospectively treated by closed reduction and casting and CRPS I occurred in 29 patients (32.2%) [3]. Logistic regression showed that risk for CRPS I was higher in cases of patients with Patient- Rated Wrist Evaluation pain subscale score >16 (OR 12.192: 95% CI 4.484-43.478) [3]. Pons et al. [5] conducted a systematic search of the literature focused on determining the potential risk factors for the onset of CRPS 1 [5] A report of higher than usual levels of pain in the early phases of trauma was one of risk factors for the onset of CRPS 1 [5]. A prospective multicenter cohort study of 596 patients with a single fracture of the wrist, scaphoid, ankle, or the fifth metatarsal showed at baseline, patients with CRPS 1 had significantly more pain than patients without CRPS 1 (P < .001) [17].
A prospective cohort study using 291 patients with traumatic hand injuries showed that patients with pain scores ≥ 5 three days after surgery had a high risk of developing CRPS compared with patients with pain scores <5 (OR 3.61: 95% CI 1.94-6.70) [15]. A prospective cohort study with 1,549 patients with wrist fracture who were managed non-surgically showed that a pain score of ≥5 in the first week after fracture should be considered a “red flag” for CRPS [18].
Decreased sympathetic vasoconstrictor response after fracture: A prospective study with 27 patients with DRF showed that the sympathetic vasoconstrictor response was diminished or absent from the first posttraumatic day to 2 weeks later in CRPS I patients and ‘borderline patients’, whereas the normal fracture patients revealed slightly impaired sympathetic nervous function on the first posttraumatic day and normal results for 2 weeks [19]. With regard to the unaffected contralateral hand, CRPS I patients also showed impaired sympathetic nervous function [19].
Location and type of injury
Type of injury: A nationwide population-based case-control study showed as follows: Injury was a risk factor for CRPS (OR 2.96: 95% CI, 2.18-4.02) [20]. In adjusted models, open wound on the upper limbs (OR 1.25: 95% CI 1.02-1.54) conferred higher CRPS risk [20]. Injury mechanisms including nerve and spinal cord injury (OR 2.42: 95% CI 1.44-4.08), muscle and joint sprain and strain (OR 1.69: 95% CI 1.40-2.03), superficial injury (OR 1.23: 95% CI 1.00-1.51), and contusion (OR 1.44: 95% CI 1.20- 1.74), but not fracture, increased the risk of CRPS [20].
Location of injury: Pons et al. [5] conducted a systematic search of the literature focused on determining the potential risk factors for the onset of CRPS 1 [5]. Ankle dislocation was one of risk factors for the onset of CRPS 1 [5] A prospective multicenter cohort study of 596 patients with a single fracture of the wrist, scaphoid, ankle, or the fifth metatarsal showed that an ankle fracture contributed significantly to the prediction of the development of CRPS1 [17]. A nationwide population-based case-control study showed that injury in the extremities rather than the trunk was an important risk factor for CRPS [20].
Treatment of the upper limb: Using the Danish Patient Compensation Association’s database, Petersen et al. [7] identified 647 patients claiming CRPS following orthopedic treatment [7]. The following ratios were found: primary diagnosis to the upper limb: lower limb was 2.5:1 [7]. Multivariate logistic regressions were performed. Treatment to the upper limb was one of risk factors associated with post-treatment development of CRPS [7].
Motor nerve injury:Of 165 patients who had suffered a mechanical traumatic injury isolated to their hand or forearm, 84 patients were diagnosed with CRPS [9]. A logistic regression showed that risk for CRPS was higher in patients with motor nerve injury [9].
Decreased function before operation:A retrospective study showed as follows: Results of multivariate analysis demonstrated that decreased function in the Japanese Orthopedic Association score for the shoulder joint before surgery was a risk factor for the development of CRPS after arthroscopic rotator cuff repair [21].
Pathological condition and stress of patient
Health condition of patient: A total of 90 patients with DRF was prospectively treated by closed reduction and casting and CRPS I occurred in 29 patients (32.2%) [3]. Logistic regression showed that risk for CRPS I was higher in cases of Medical Outcomes Study 36-Item Short-Form Health Survey physical functioning score <40 (OR 4.931: 95% CI 1.428-17.025) [3].
Social circumstances of patient:Retrospective analysis of the Nationwide Inpatient Sample database from 2007 to 2011 in the United States [6]. There were 22,533 patients with the discharge diagnosis of CRPS type 1 of an inpatient sample of 33,406,123 [6]. Higher median household income was associated with higher rate of CRPS type 1 [6].
Psychological abnormality (depression, anxiety, etc.):A cross-sectional study with 88 CRPS patients and 88 low back pain patients showed that disability and pain severity were more strongly associated with psychological factors (depression, anxiety, and kinesiophobia) in CRPS than they were in low back pain [22]. Cause and effect relationships could not be established by this cross-sectional study [22]. Retrospective analysis of the Nationwide Inpatient Sample database from 2007 to 2011 in the United States [6]. There were 22,533 patients with the discharge diagnosis of CRPS type 1 of an inpatient sample of 33,406,123 [6]. Depression and drug abuse were associated with higher rate of CRPS type 1 [6].
Database queries yielded 853,186 patients diagnosed or treated for DRF [8]. Multivariable logistic regression showed that anxiety was positively associated with CRPS [8]. Bayle- Iniguez et al. [23] performed a case-control study and reported that multivariate analysis showed a strong association with being anxious (OR 44.9: 95% CI 7.4-273) [23]. A case-control study showed that psychological factors were not associated with CRPS onset [24]. A prospective study showed that the psychological context (anxio-depressive state) showed a (subsignificant) tendency to increase the risk of CRPS I (relative risk [RR] 2.6) [25]. A systematic review reported that in summary, studies with a higher methodological quality suggested no relationship between psychological factors and CRPS1 in adults [26].
A prospective study showed that those who developed algodystrophy did not show increased distress before the onset of the condition in patients with Colles’ fractures [27]. Another prospective study showed that there were no significant differences in scores on any of the personality and depression scales between CRPS Type 1 and non-CRPS Type 1 patients after DRF [28]. A review published by Feliu et al. [29] concluded there was no evidence to support a linear relationship that established a psychologic predisposition to develop CRPS [29]. A review reported that the observed modifications in behaviour and personality of CRPS patients, in particular depression and anxiety, were a consequence of the persisting pain disease and its considerable resistance towards treatment and not the cause [30].
A prospective study using 50 patients with a DRF reported that the risk of CRPS type I was significantly increased in patients with high trait anxiety scores (P = 0.038), indicating that after DRF, patients who have an anxious personality have a higher risk of developing CRPS type I [31]. A prospective multicenter cohort study using 596 patients indicated that there was no association between psychological factors and CRPS1 [32]. A systematic review did not reveal support for specific personality or psychopathology predictors of CRPS [33]. In a retrospective cohort study of 390 patients who had undergone elective foot and/or ankle surgery, 8 (47.06%) had had a pre-existing diagnosis of anxiety and/or depression of the 17 patients with CRPS [34].
A case-control study using 249 patients with DRF who underwent surgical treatment (4% developed CRPS) showed that psychiatric history (OR 7.22: 95% CI 1.315-39.606) was a higher risk of developing CRPS [13]. Speck et al. [35] collected data from 152 patients with CRPS, 55 control patients and 55 age- and sex-matched healthy individuals [35]. Fifty-eight CRPS patients (38%), six non-CRPS pain patients (10%) and two healthy individuals (4%) met diagnostic criteria for posttraumatic stress disorder (PTSD) [35]. Initial PTSD symptom onset was prior to CRPS in 50 CRPS patients (86%) and during the course of CRPS in eight patients [35]. A logistic regression revealed that the PTSD severity score was associated with CRPS (p < 0.0001) [35].
Economic compensation:A case-control study using 249 patients with DRF who underwent surgical treatment (4% developed CRPS) showed that economic compensation via work disability (OR 14.4: 95%CI 1.79-115.38) was a higher risk of developing CRPS [13].
Smoking:A case-control study showed that cigarette smoking was strikingly increased in patient frequency in RSD (68% versus 37% of hospitalized controls, p less than 0.0001) [36] Pawelka et al. reported that there were 37 women and 27 men; 32% of the female and 48% of the male patients were smokers and in the general population of Vienna, these percentages are 30 and 46, respectively [37]. In a retrospective cohort study of 390 patients who had undergone elective foot and/or ankle surgery, 5 patients (29.41%) were smokers of the 17 patients with CRPS [34]. Of 301 patients who underwent carpal tunnel release (CTR), 25 patients developed CRPS and smoking did not show a relationship with the development of post-CTR CRPS [38].
Social or psychological stress:Eighty percent of all dystrophy patients had a recent life-event while only 20% of the control group members reported such an event [39]. Of 145 patients (122 patients with CRPS I and 23 patients with CRPS II), 61 patients (42.1%) reported stressful life events in a close relationship to the onset of CRPS [40]. Most frequent were conflicts within the family (n=30; 20.7%), death of relatives (n=13; 9%) or serious job-related problems (n=12; 8.3%) [40]. A systematic review reported that patients who experienced more life events appeared to have a greater chance of developing CRPS1 [26].
Good to excellent school performers:Bayle-Iniguez et al [23]. performed a case-control study and reported that multivariate analysis showed a strong association with being good to excellent school performers (OR 8.4: 95% CI 1.3-52.1) [23].
Diseases
Osteoporosis:A case-control study showed that a medical history of osteoporosis (OR 2.44: 95% CI 1.17-5.14) was associated with CRPS [24].
Diabetes:Retrospective analysis of the Nationwide Inpatient Sample database from 2007 to 2011 in the United States [6]. There were 22,533 patients with the discharge diagnosis of CRPS type 1 of an inpatient sample of 33,406,123 [6]. Diabetes was associated with a lower rate of CRPS type 1 [6]. Database queries yielded 853,186 patients diagnosed or treated for DRF [8]. Multivariable logistic regression showed that diabetes was negatively with CRPS [8]. A retrospective study showed that of the 200 stroke patients with Type 2 Diabetes Mellitus (T2DM), 108 were in the CRPS group and 92 were in the non-CRPS group [41]. There were significant differences in HbA1c (p<0.05) between the two groups [41]. Across the five HbA1c groups, there were significant differences in CRPS prevalence (p<0.01); specifically, it increased as HbA1c increased [41].
Hypertriglyceridemia:Disease analysis using a retrospective series of nine cases and a review of the literature of RSD in pregnancy reported that hypertriglyceridemia appeared to be a risk factor for RSD [42].
Rheumatoid arthritis:A prospective multicenter cohort study of 596 patients with a single fracture of the wrist, scaphoid, ankle, or the fifth metatarsal showed that patients who developed CRPS1 at a later time more often had rheumatoid arthritis (14.3% vs 5.3% non-CRPS 1) [17].
Musculoskeletal comorbidities:A prospective multicenter cohort study of 596 patients with a single fracture of the wrist, scaphoid, ankle, or the fifth metatarsal showed that patients who developed CRPS1 at a later time more often had musculoskeletal comorbidities (54.8% vs 27.6% non-CRPS 1) [17].
Allergy/hypersensitivity reactions:A case-control study showed that of the patients with CRPS I, 78 (67.8%) reported a statistically significant history of allergies compared with the 39 (33.9%) patients in the control group (P<.0001) and skin hypersensitivity testing yielded an 83.3% positive predictive value with an accuracy of 76.9% [43]. Bayle-Iniguez et al [23] performed a case-control study and reported that multivariate analysis showed a strong association with presence of an atopic background (OR 25.0: 95% CI 4.6-135) [23]. A case-control study showed that asthma (OR 3.0: 95% CI 1.3-6.9) and CRPS were related [24].
Trouble falling asleep:Bayle-Iniguez et al [23]. performed a case-control study and reported that multivariate analysis showed a strong association with having trouble falling asleep (OR 5.3: 95% CI 1.6-17.0) [23].
Diseases hard to cause CRPS:Retrospective analysis of the Nationwide Inpatient Sample database [6] from 2007 to 2011 in the United States [6]. There were 22,533 patients with the discharge diagnosis of CRPS type 1 of an inpatient sample of 33,406,123 [6]. Obesity, hypothyroidism, and anemia were associated with a lower rate of CRPS type 1 [6] Database queries yielded 853,186 patients diagnosed or treated for DRF [8]. Multivariable logistic regression showed that heart failure was negatively with CRPS [8].
Painful disorders
Chronic pain:Of 145 patients (122 patients with CRPS I and 23 patients with CRPS II), 60 patients (41.4%) had a history of chronic pain before CRPS [40]. The majority suffered from chronic low back pain (n=20; 13.7%), chronic headache (n=17; 11.7%), multiple chronic pains (n=6; 4%) or different other pains (n=17; 11.7%) [40]. A case-control study showed that in a recent history (1-year before CRPS), cases had more menstrual cyclerelated problems (OR 2.60: 95% CI 1.16-5.83) and neuropathies (OR 5.7: 95% CI 1.8-18.7) [24]. A prospective study showed that history of CRPS I was a significantly correlated factor (RR 10.4) [25]. A retrospective analysis using 190 patients with CRPS and additional 26 patients with CRPS NOS (not otherwise specified) showed that a third had already experienced other than everyday pains in the now CRPS-affected limb before the CRPS incident trigger [44]. A total of 21 patients (11.1%) experienced widespread pain in clinic [44]. Additional patients reported CRPS-concomitant regional pains, most commonly headaches/ migraines, lower back pain, and irritable bowel syndrome [44].
Headache:Retrospective analysis of the Nationwide Inpatient Sample database from 2007 to 2011 in the United States [6]. There were 22,533 patients with the discharge diagnosis of CRPS type 1 of an inpatient sample of 33,406,123 [6]. Headache was associated with higher rate of CRPS type 1 [6]. Of 145 patients (122 patients with CRPS I and 23 patients with CRPS II), 60 patients (41.4%) had a history of chronic pain before CRPS [6]. The majority suffered from chronic low back pain (n=20; 13.7%), chronic headache (n=17; 11.7%), multiple chronic pains (n=6; 4%) or different other pains (n=17; 11.7%) [40]. A case-control study reported that headache and a firstdegree family history of headache were risk factors for CRPS [45]. A case-control study showed that a medical history of migraine (OR 2.43: 95% CI 1.18-5.02) was associated with CRPS [24].
Age and gender-adjusted standardized morbidity ratios (SMR) showed that those with CRPS were 3.6 times more likely to have migraine and nearly twice as likely to have chronic daily headache (CDH) as the general population [46]. Of those CRPS sufferers with migraine, 61.2% (41/67) reported the onset of severe headaches before the onset of CRPS symptoms [46]. More extremities were affected by CRPS in participants with migraine (median of four extremities) compared with the combined group of those CRPS sufferers with no headaches or tension-type headache (TTH) (median 2.0 extremities), P < 0.05 [46]. Migraine may be a risk factor for CRPS and the presence of migraine may be associated with a more severe form of CRPS [46].
Fibromyalgia:Database queries yielded 853,186 patients diagnosed or treated for DRF [8]. Multivariable logistic regression supported the association between fibromyalgia and the development of CRPS, with estimated OR of 2.0 (P < .001) [8]. Crijns et al. [11] identified 59,765 patients treated for a DRF, of whom 114 (0.19%) were diagnosed with CRPS [11]. Comorbid fibromyalgia (OR 16.0: 95% CI 4.92-51.8; p < 0.001) was independently associated with a diagnosis of CRPS [11].
Multiple sclerosis:Schwartzman et al. [47] reported that multiple sclerosis patients (4 cases per 205 patients) were at a higher risk of developing CRPS than the general population (expected prevalence: 0.078 cases per 205 persons) [47].
Difference due to treatment
Surgery:Using the Danish Patient Compensation Association’s database, Petersen et al. identified 647 patients claiming CRPS following orthopedic treatment [7]. The following ratios were found: surgical: nonsurgical treatment was 3:1 [7]. Multivariate logistic regressions were performed. Surgical treatment was one of risk factors associated with post-treatment development of CRPS [7]. Database queries yielded 853,186 patients diagnosed or treated for DRF [8]. Multivariable logistic regression showed that surgical or manipulative treatment was positively associated with CRPS [8].
Difference of incidence due to difference of treatment for distal radius fracture:network meta-analysis showed that compared with bridging external fixation, K-wire fixation, dorsal plating, volar plating, dorsal and volar plating, plaster fixation and non-bridging external fixation might be the better treatment methods to reduce the risk of CRPS in DRF patients [48]. A total of 77 postmenopausal female patients with DRF were divided into three subgroups: 1. closed reduction and immobilisation in a plaster cast; 2. closed reduction and percutaneous fixation with K wires; 3. open reduction and fixation with a locking plate [49]. Open reduction with locking plate fixation produced better functional outcomes in the early postoperative period and reduced the risk of development of CRPS [49]. A meta-analysis compared showed that the overall incidence of complications, including CRPS, was higher with pinning/wiring in patients with unstable DRF, though the incidence of carpal tunnel syndrome and nerve defects was not different [50].
Fixation:Pons et al. [5] conducted a systematic search of the literature focused on determining the potential risk factors for the onset of CRPS 1 [5]. Immobilisation was one of risk factors for the onset of CRPS 1 [5]. Field et al. [51] reported that in patients who had objective signs of algodystrophy the plaster cast was significantly tighter during the first three weeks than in patients who did not develop algodystrophy [51].
Perioperative factors:Thirty-nine patients were diagnosed with CRPS immediately after Open Reduction and Internal Fixation (ORIF) for limb fracture from a cohort of 185,378 in patients treated with ORIF [4]. A longer duration of anaesthesia, but not regional anaesthesia, was significantly associated with a higher incidence of CRPS [4].
A total of 301 patients who underwent carpal tunnel release were randomly distributed to undergo one of the following techniques: general anesthesia, regional intravenous anesthesia with lidocaine, regional intravenous anesthesia with lidocaine and clonidine, or axillary plexus block [38]. Twenty-five of them developed CRPS [38]. Predominance was not observed among the anesthetic techniques used [38].
Medicine
A total of 126 neurosurgical patients was treated with barbiturates, and 108 control patients were treated with carbamazepine or phenytoin [52]. A total of 25 barbituratestreated patients (27.6%) experienced shoulder-hand syndrome (SHS) and none of the patients in the control group developed SHS [52]. A retrospective case-control study (186 cases and 697 controls) showed that current use of Angiotensin Converting Enzyme (ACE) inhibitors was associated with an increased risk of CRPS (adjusted OR 2.7: 95% CI 1.1-6.8) [53]. The association was stronger if ACE inhibitors were used for a longer time period (adjusted OR 3.0: 95% CI 1.1-8.1) and in higher dosages (adjusted OR 4.3: 95% CI 1.4-13.7) [53]. None of the other antihypertensive drug classes was significantly associated with CRPS [53]. Forty-seven patients with metastatic renal cell carcinoma were treated with Everolimus and 3 developed unilateral leg pain related to RSD [54].
Gene
Huehne et al. [56] reported that particular ACE gene polymorphism is unlikely to be a predisposing factor for CRPS I [54]. Huehne et al. [56] tested a GT-repeat polymorphism in the Neutral Endopeptidase (NEP) promoter region as well as 18 tag Single Nucleotide Polymorphisms (SNPs) in six linkage disequilibrium blocks in the NEP gene region in 320 CRPS patients and 376 controls [56]. No significant genetic association was observed. Thus, Huehne et al. [56] concluded that the NEP gene did not seem to be a major risk factor for CRPS [56]. Fifteen of 163 patients with DRF were diagnosed with CRPS I and significant association was detected for the rs1048101 polymorphism of the alpha1a-adrenoceptor [57].
All other tested variants were not associated with CRPS I. This study suggests the rs1048101 single nucleotide polymorphism within the alpha1a-adrenoceptor as one risk factor for the development of CRPS I after DRF [57]. Smith theorizes that genetic alterations including functional polymorphisms of Nrf2 (a master regulator of the transcription of multiple antioxidants) may render certain subjects more or less susceptible to developing CRPS after surgery or trauma [57].
Discussion
>Difference of incidence
The incidence of CRPS varies greatly among studies. Three factors explain it. First, the concept of the disease changed, and the diagnostic criteria changed accordingly. Second, decision of abnormal right-left difference of each objective sign is based on a physician’s subjectivity. Third, we have to distinguish between CRPS and the usual course of injury. CRPS has many aliases. RSD, the former major disease name, was renamed CRPS. The concept of CRPS (or RSD) changed, and the diagnostic criteria changed accordingly. Even if the identical patients are diagnosed by the identical physician, the incidence of CRPS depends to a large extent on the diagnostic criteria used [17]. Of the 596 participants after a single fracture, 42 (7.0%) were diagnosed with CRPS1 according to the Harden and Bruehl criteria [59], 289 (48.5%) according to the International Association for the Study of Pain criteria [60] and 127 (21.3%) according to the criteria of Veldman [61]. The problem of right-left difference is serious. Almost all CRPS occur in the extremities. There are many diagnostic criteria for CRPS (or RSD), however, all criteria are combinations of right-left difference of some subjective symptoms and right-left difference of some objective signs.
The difference between right-left difference corresponding to diagnostic criteria and right-left difference not corresponding to diagnostic criteria, in other words, the difference between abnormal range right-left difference and normal range rightleft difference, is unclear. The decision is made based on a physician’s subjectivity. Therefore, even if the identical patients are diagnosed with the identical criteria, the diagnosis depends on physicians. Operators are not more likely to diagnose the patients who were operated by himself/herself as having CRPS. CRPS usually occurs after injury and operation. Naturally, there is right-left difference in pain, skin temperature, and skin color of the both limbs after injury and operation. A physician’s subjectivity decides whether these right-left differences are natural course or abnormal. It is similar to afore mentioned right-left difference.
Is CRPS-associated factor cause of CRPS or consequence of CRPS?
Is CRPS-associated factor that was found with case-control studies cause of CRPS or consequence of CRPS? In case of age, certain age is never consequence of CRPS, but cause (or risk factor) of CRPS. In case of depression and anxiety, they cause a chicken-and-egg situation. Many case-control studies or retrospective studies showed that depression and/or anxiety were positively associated with CRPS [6,8,13,23,24]. Of five prospective studies, three studies showed no association between psychological factors and CRPS [27,28,32]. One study showed a (sub-significant) tendency to increase the risk of CRPS [25]. One study showed that patients who have an anxious personality have a higher risk of developing CRPS [31]. Systematic review and/or meta-analysis of prospective studies alone were not published; however, I believe that depression and anxiety are consequence of CRPS at the moment.
Significance or risk factor
Identification of risk factor for CRPS provides some significance. First, it helps to find etiology of CRPS. Second, if a relative disease is found, treatment of the relative disease can be applied to CRPS. Third, it is helpful in the early detection of CRPS. Forth, it becomes helpful in an injury treatment such as fracture. Menstrual cycle-related problems [24]. headaches/ migraines [6,40,44,45], lower back pain [44], irritable bowel syndrome [44], fibromyalgia [6,11], widespread pain [44] are risk factors for CRPS. And female sex is also a risk factor for CRPS [1-7]. These indicate that CRPS may be included in central sensitivity syndrome.
Steroids are effective to some extent in the early stage of CRPS [62-72]. however, these are not effective in a chronic stage of CRPS. There are few evidence-based effective treatments for CRPS. There are many evidence-based effective treatments for FM or headache, therefore, it is possible to use them as treatments for CRPS. In some patients with a chronic stage of CRPS, objective signs such as swelling, local heat, redness disappear, and pain alone persists on the affected limb, further pain spreads to the trunk and/or other limbs. In such a patient, it is almost impossible to distinguish between chronic stage of CRPS and FM or chronic widespread pain (incomplete form of FM). If we know risk factors for CRPS, it is useful to detect CRPS early. If CRPS occurs after operation, treatment outcomes are decreased. Knowledge of risk factors for CRPS is important to decrease occurrence of CRPS. Cowell et al. [72] reported that simple practice changes (a patient information leaflet, a local gold standard for care of DRF, education for staff regarding risk factors and early warning signs of CRPS, and simple patient and staff visual aids) reduced the incidence of CRPS from 25% to 1% after DRF [73].
A severe pain after injury may be a risk factor of CRPS, however, it may be an early symptom of CRPS. In any case, a severe pain after injury should be alleviated as soon as possible in some way. Until only recently, in Japan, almost all physicians did not know FM and some physicians consider FM equivalent to Piltdown Man (fabricated Homo sapiens). Therefore, physicians who treat FM is very rare like Nippon Nippon, endangered bird. Knowledge of FM has spread in Japanese orthopedic surgeons in an unfortunate state. Some Japanese orthopedic surgeons do not want to operate patients with FM. One of the reasons is that FM is a risk factor for CRPS. An patient with comminuted and displaced DRF underwent a conservative treatment and suffered from serious malunion. Initially, surgery was planned, however, treatment suddenly changed to a conservative therapy immediately after she explained that she suffered from FM. It is an inappropriate use of knowledge of FM or risk factor for CRPS.
For More Open Access Journals in Juniper Publishers Please Click on https://juniperpublishers.com/journals.php
For more articles, Please click on Juniper Online Journal of Orthopedic & Orthoplastic Surgery
https://juniperpublishers.com/jojoos/JOJOOS.MS.ID.555579.php
#Surgical Orthopedics#Traumatic Surgery#Plastic Surgery#Knee arthroscopy#Hip replacement#Lumbar spinal fusion
1 note
·
View note
Text
0 notes