#Medical billing and coding strategies
Explore tagged Tumblr posts
Text
Finding Refuge.
Chapter two.
Surviving a Zombie Apocalypse with Terry Richmond

“I’m so sorry, Raelynn. The position has been filled.”
Raelynn Matthews looked into the eyes of the receptionist standing behind a sleek front desk. The stillness within that corporate building in Downtown Atlanta left an eerie feeling she was intensely familiar of.
“E–Excuse me?” Raelynn finally found the words to speak, “I–I–I–don’t understand.”
The nonchalant receptionist stared back at Raelynn with a cool expression and a slow blink.
“I received an email from your company for a job opportunity. You have an opening here,” Raelynn displayed the email to the receptionist, “So help me understand…”
The sunken, almost lifeless eyes of the receptionist flicked down to her iPhone and then back to her face.
“That email was sent two days ago. We don’t wait around for a response. If you wanted the job, you’d have shown up within the allotted timeframe.”
The even, condescending tone of the alabaster bitch sitting before her was about to bring the evil out of Raelynn.
“Are you being sarcastic? The date says March 25th. Today is March 25th—”
“I’m trying to be nice here. What would you rather me do? Go grab one of the big boys and have him tell you what I just told you?”
Emerald green eyes stared into Raelynn’s coffee brown orbs. The receptionist with a nameplate that reads: Monica Caudle, started packing her patchwork satchel, prepared to leave Raelynn standing there. The sound of dress shoes against polished, concrete floors echoed around her as her fingers covered in various silver rings twitched against the desk’s surface.
“You know your way out—AHHH! WHAT THE FUCK?!”
Somehow, Raelynn’s hand smacked against Monica’s Big Gulp cup and spilled the contents of a blue slurpie all over her white capris and black, pointed toe, ballet flats. Monica leaped up and almost tripped from the velocity of her sudden movements. The blue, icy-cold liquid drifted all over her desk, soaking very important documents and Monica’s AirPod Pro case.
“ARE YOU KIDDING ME?!” Monica screeched, “I OUTTA SLAP THE FUCK OUT OF YOU—”
Whoops,” Raelynn twisted her full lips and gave a single shoulder shrug, “My hand just…has a mind of its own.”
“I’m calling security—”
“Call them, I don’t care. You deserved it. I’m sure you’ve gotten by so far in your miserable life being nasty and rude to people. Today is the day you feel how it feels to be treated poorly. And it doesn’t help the fact that you’re so ugly on the outside. It matches that rotten core of yours.”
Raelynn beamed at Monica. Monica stared at her with her mouth agape.
“Think about what I’ve said. Really think on it, Monica. I could have done worse,” Raelynn placed her large, black, Telfar bag over her shoulder, “Have a good rest of your day!”
Turning, Raelynn walked away, ready to get so far away from that building. She refused to allow herself to cry over it. Maybe it was a sign for the heavens above that this job wasn’t for her. She was still in college working towards a certificate in medical billing and coding. Other opportunities were on the horizon.
Raelynn had a temper, one she couldn’t control when in situations. Slowing down, breathing deeply, and taking a break before responding were methods she tried to use to reduce her anger. Practicing relaxation skills and developing new anger-management strategies may also help. She just started therapy, so it was an adjustment for her.
A black girl from Decatur, apart of the 14.57 percent of African Americans within the eastern suburb. Her foster parents had her attend the best schools, put her in many clubs from ballet to karate, and made sure she got a full ride to Spelman.
You may have heard the expression “children are resilient,” promoting the idea that children can overcome and conquer hardship and trauma. While it may be comforting to believe in the rhetoric of childhood resilience — that children are immune to adverse experiences and won’t be damaged by trauma — it’s far from the truth. Raelynn suffered heavily from PTSD. She was neglected by her biological parents and abused by her mother’s boyfriend at the age of seven.
The cigarette burn in the center of her chest was a reminder. The sensation of piping hot water against her skin brought back memories of sitting in a hot tub after receiving a beating, the whelps on her skin so painful she couldn’t stand the heat against her skin. Nights without a meal because she ‘disrespected her mother’s man’. Going to school at the age of nine with a black eye was enough to have her 4th grade teacher call CPS.
“Take her, I can’t afford her anyway. One less thing to be concerned with.”
George and Tonya Williams adopted her. George was a Veteran and Tonya was a pediatric nurse. They drove all the way from Decatur to take her back with them. George was a very disciplined man. Very straight and very structured. He was like a drill sergeant. Tonya was loving and often times smothered Raelynn. They built a picture–perfect daughter to their liking, and Raelynn felt she didn’t have a say in the matter. Although she was forever grateful of them, she wished they could understand.
Raelynn became rebellious. She skipped school, got suspended multiple times, fought often, and stayed out way past curfew. It was a cry for help that fell on deaf ears. Eventually, George started to regret adopting Raelynn. And just like her mother’s boyfriend, he hit her. Slapped her in the face. Slapped her while her foster mother watched. Thankfully, she was of age to leave them both behind and figure out what she was going to do.
She left Decatur and moved to Atlanta where she worked two jobs to make ends meet, got her license, made poor dating choices, and partied till she couldn’t party anymore. It did nothing but numb the pain. She tried reaching out to her biological father, but discovered he had passed from colon cancer a year prior. Her mother was no longer with that abusive man but she was living in South Carolina with extended family until she got back on her feet.
Before stepping off the curb and into the street, Raelynn stopped herself, realizing what she was about to do. Was she about to…walk into incoming traffic? She took two wide steps back and closed her eyes. That wasn’t the answer. Raelynn noticed a bench and took a seat. She sat her bag down next to her and retrieved a small note pad and a pen with purple ink. Raelynn removed the top to the pen with her teeth and started jotting down what had just happened.
After what felt like an hour, Raelynn stood from the bench and walked safely across the street to her parked car and climbed inside. The drive back to her shared apartment with her roommate took longer than usual, cars bumper to bumper. Raelynn opened the door to their two bedroom apartment and dropped her shoes off where she stood. Walking inside, she spotted her roommate, Ashley, an art major with the beauty of a pageant girl and the body of an IG model. Ashley was wearing a matching, pale–pink pajama set with her honey blonde knotless braids cascading down her back.
“Raelynn? Did you see the news?” Ashley glanced over her shoulder at Raelynn with light–brown eyes, “look…”
This is a worldwide emergency broadcast; a viral outbreak has been reported and is spreading quickly. The virus is a fast acting strain and is passed through bodily fluids from the infected. Once bitten or contaminated in any way, it attacks your bloodstream and brain. The symptoms of the infected include profound sweating, fever and nausea.
Raelynn’s eyes were hooked to the screen. Ashley stood from the carpet and began ringing her shaky hands as fear rushed through her. Life was about to get interesting. So, a worldwide pandemic? Great. What else can go wrong? They were behind in rent, she couldn’t get another job after being fired from her job delivering packages from Amazon. With a pandemic, she’d have no way to pay bills and survive.
Call up George and Tonya. Move back home to Decatur, she thought.
“It’s probably one of those distractions, Ashley. Just like all of that Area 51 bullshit—”
“Shhhhh! Listen!”
Ashley turned the volume up on their wall—mounted flat screen.
The virus is fatal and there is no cure as we speak; we have reports coming in now that the infected that have passed are rising and attacking the non–infected. Please stay in your homes and do not get close to anyone sick, in severe cases that you need to protect yourself, the only way to stop them is damaging the brain. Do not try to come to emergency services or hospitals and wait for more information…
“Rae…”
Ashley was starting to have a panic attack right before Raelynn’s eyes. The intense fear and anxiety she was experiencing made her dizzy. Ashley almost lost her balance and fell face first against the carpet. Raelynn dropped her bag and rushed over, slowly lowering Ashley to the sofa. She wrapped her arms around her shaking body, rubbing her back in soothing circles. Ashley’s hyperventilating began to slow down.
“Ash, it’s okay…it’s okay—”
“I need to call my mom and my sister! I need to know that they’re okay!” Ashley shouted hysterically.
“Ash, Ash, please, calm down—”
“NO!”
Ashley shoved Raelynn, causing her to fall back against the couch while she stormed off down the hall. Raelynn shot up from the couch and followed Ashley, angered by her rage against her when she was only trying to help. She stood within the doorway of Ashley’s bedroom and watched her pack an overnight bag with random pieces of clothing.
“So, you’re just going to go out there when they just said to stay indoors—”
“I need to be with my family, Raelynn. They’re all I’ve got left. I don’t expect you to understand that—”
“HOLD ON,” Raelynn charged inside of Ashley’s room, “I was only trying to help you! If they’re saying it isn’t safe to go out, then why would you?—”
Raelynn wasn’t prepared for what just happened. Ashley bent over in front of her and vomited all over her bedroom floor. Raelynn rocked back on her heels to avoid it from getting on her. The putrid smell of her stomach contents filled the cramped space and Raelynn couldn’t stand there any longer.
Ashley looked up at her with a sweaty face and spit hanging from her bottom lip. They locked eyes and the silence between them was almost chilling.
The symptoms of the infected include profound sweating, fever and nausea.
“How long have you been feeling like this?” Raelynn questioned.
Ashley avoided Raelynn’s penetrating gaze.
“Ashley, how long?”
Ashley wiped her mouth with the back of her hand. She rushed past Raelynn and into their shared bathroom to grab cleaning supplies. Raelynn watched her scrub and clean, the scent of bleach mixed with vomit toxic to her senses.
“Do you think you were infected—”
“Shut up right now, Raelynn.”
“I need to ask these questions! Because if you are…if you are…”
Raelynn disappeared down the hall to her room. Fuck what that news anchor said on television. If Ashley was indeed infected, she would attack Raelynn and do the exact same to her. She packed an even bigger bag, grabbing all the important things she needed before heading back to Decatur.
Speaking of Decatur.
Incoming call…
“Tonya?”
Raelynn glanced down the hallway, the sound of Ashley scrubbing catching her ear.
“Raelynn, honey, is everything alright? Did you hear what’s happening? Are you safe?”
“Uh…” she lowered her voice and cracked her door, “I don’t think so…my roommate is sick…she just threw up everywhere.”
“You need to come home. Get out of there fast. I rushed home from work because the hospital is in an uproar. The things I’ve witnessed…come home, Rae.”
“How does George feel about all this?”
“…George wants you home too. Leave now and let me know when you’re on the way. I love you. Please be careful, Raelynn.”
Beep.
Raelynn started to feel her own sense of trepidation. She continued packing, and when she finished, she opened her door, silence ahead of her.
“Ashley?”
Nothing. Just an eerie silence.
Raelynn hated the unknown. She hated not knowing what she was walking into. That hallway was her only chance of leaving that apartment. Mustering courage, Raelynn gathered her things and began walking the hallway. Before she approached Ashley’s door. She stopped, reaching inside of her Telfar bag, gripping the handle of her licensed gun. She made sure to bring it with her if what the news was saying was true.
In severe cases that you need to protect yourself, the only way to stop them is damaging the brain.
Raelynn stepped in front of Ashley’s door and it was empty. She’d left. Raelynn exhaled, hoping that Ashley wasn’t infected. She was on her way to her mother and sister. If she’s infected, she would definitely do the same to them.
Not wasting anymore time, Raelynn left the apartment behind and as she exited the complex, her eyes moved back and forth, taking in the sight of people rushing and screaming and crying. She hadn’t been in her apartment for an hour and already there was mass hysteria. She jogged with her bags to her Honda Civic, popping the trunk and throwing her bags inside. Raelynn made sure to keep her eyes focused around her. She hopped in her car and slammed the door shut, thankful she was safe.
We’re gonna die!
It’s the apocalypse!
Those words stuck with her the entire ride to Decatur. She could only hope it wasn’t true. Maybe she was asleep. Maybe she needed to be woken up from this growing nightmare.
——
3:00 pm
The town of Senoia
located 45 minutes south of Atlanta. It was established in 1860 , the land was purchased by a Reverend. Cotton and Peaches where the agricultural products shipped from this area. There are still plenty of farms, now they have lots of honey farms and other fruits. The town was named after a captain's wife from the civil war.
Terry walked into that town with a shotgun flung across his body and a crossbow in his hand. He wore his favorite jeans, a grey T-shirt beneath a flannel shirt, and a beanie on his head. His hazel eyes took in the appearance of the charming little town, small shops surrounding him. The sound of shuffling feet startled him so he ducked low behind an abandoned, faded blue sedan.
It was a small group of zombies.
Terry silently watched while fixing his crossbow to shoot. He steadied his breathing, something he’d learned to do over the months. No use in making it known that he was highly anxious. His eyes peeked through the dusty window at the zombies moving along with weak attempts to stay on two feet.
It’s crazy to think that these were once everyday people. Waking up, going to work, driving, laughing, making love…
They stumbled around, moaning and groaning.
Rauuuhhh…guhhhhhhhh…
Another method that allowed Terry to keep the zombies away from where he hunkered down was to bait them. He’d tie dead animals to a wooden board and hang them in various locations within the forest to keep his scent away. It worked, because if they caught a whiff of him, they’d go crazy. He had to do it every several days. A lot of work, but worth your life.
When they were far enough away, Terry remained low, his eyes casing the area like a hawk. Solid back against a brick wall, Terry retrieved his walkie talkie from his back pocket. He’d made it to the first landmark Rae told him about.
“When you find the history museum, radio me and I’ll tell you what to do from there. Good luck, Terry.”
He was still unsure about Rae.
“Why are you helping me?” Terry questioned her hours prior.
“Because…I know what’s it’s like…and we have to have each other’s back, right?”
He’d like to believe that. Terry refused to travel in a pack. He refused to trust anyone else besides his cousin. But, with Mike gone, he had no choice but to let his guard down just a little. Only a little this time. As soon as he finds Mike, he’s leaving everyone behind. Including Rae.
“Rae, this is Terry, come in.”
Terry moved further away until he was hiding beside a dumpster, crouched low.
“Rae, what’s your 20?”
He couldn’t stay here any longer. What the fuck was she doing? His head snapped to the right when he thought he’d heard something.
Terry whispered a low “fuck,” before jogging as quickly and quietly as he could across to the other side.
“Rae, come in, I’m too exposed. You got me open out here.”
“Terry, Terry, I’m here, sorry…”
“What the fuck was that?” Terry whispered aggressively into the walkie talkie.
“Signal strength down. I’m trying here, Terry. Are you at the landmark?”
“Yes, yes. Now, where to go from here?”
“Travel north. You’ll notice train tracks straight away. Stick close to the trees. When you reach a tunnel, I’m waiting inside for you.”
“Will you? I need your word, Rae.”
“I promise. I wouldn’t lead you astray.”
Terry moved. He hadn’t been in this position for at least two months. His well, structured game plan to remain hidden most of the time was being tested. It took Terry about twenty minutes to find the tracks. He stepped over carefully and did as Rae suggested: sticking to the trees. Ignoring the twigs and pointy greenery scraping his skin, Terry could see the tunnel straight ahead.
“Argh!”
Terry dropped to his knees when the back of a gun collided with his head. He dropped his crossbow and turned around on his hands to see who had attempted to knock him out. He was resilient. it would take a lot to put Terry Richmond down. Not even a taser could subdue him for long. He’d withstood a bullet to his back. His bright eyes stared up into the eyes of a wild—looking white man with overgrown facial hair and thin, oily, dirty blonde hair.
“Who the fuck are you?!”
Terry wanted to kill this man with his bare hands. He was going to draw attention to them.
“Get that gun out my face.” Terry warned.
“I don’t recognize your face ‘round here. We don’t take kindly to outsiders in Woodsbury. You could be infected…”
“Yeah, well, I’m not. And you’re right, I’m not from around here. But I damn sure don’t owe you an explanation. After all, you don’t own this town.”
Click.
Terry acted quickly and charged the man into the bushes. They wrestled, rolling around in the dirt. Terry took his arm and pinned it back, causing the man with rancid breath to wail in agony. He wouldn’t keep still. Terry had to put him in a choking headlock with his bulging bicep.
He squeezed.
The man tapped his arm frantically.
“You wanna go to sleep? Drop the fuckin’ gun. Do it now, motherfucker.” Terry spoke through clenched teeth.
The man loosened his grip on the gun. Terry gave his throat one more painful squeeze to let him know he meant business before releasing him. Terry picked himself up from the ground while the man tried to catch his breath. He picked up the gun and placed it on his hip.
“This mine now.” Better move along before they come find you after making all that noise.”
Terry snatched up his crossbow and adjusted the shotgun around him as he walked, with one final look of pure hatred down at the man, he continued on his way and fast. Terry lifted his forearm and studied the bloody abrasion with fierce eyes.
He wanted to scream. He couldn’t afford to walk around with an open wound. If anything, that man he was fighting back there could be infected.
Terry took off running as fast as he could, darting between trees like a track runner. Up ahead, he came out onto the train tracks and sprinted into the dark tunnel. He slowed his footsteps and pressed his chest into the wall of the tunnel, exhausted breaths billowing from his mouth.
He didn’t have a second to gather himself before he had his crossbow aimed at the face of a woman.
Ebony skin a deep brown with a dewy appearance.
Heart shaped face with eyes coffee brown and a flared nose decorated with a hoop ring.
Lips full and lush.
Hair styled in thick, rope twists that reached her waist
She had her hands raised in surrender. Those entrancing eyes didn’t look away for a second.
Staring down the length of his crossbow, his eyes that appeared green drifted down her tiny frame. She was wearing a hoodie beneath a thick, utility jacket. Her lower half was dressed in a pair of skinny jeans and her feet were covered with dirty high–top Vans.
His eyes locked with hers again, and he slowly lowered his weapon. She released a shaky breath, the sound settling his nerves. He held the crossbow to his side and parted his dry lips to speak.
“Rae?”
She nodded her head, her own eyes taking him in from head to toe.
“Terry…”
She reached behind her and Terry’s eyes followed cautiously. Raelynn held up a hand to calm him down.
“I’m just grabbing the walkie talkie,” She displayed Mike’s walkie talkie, holding it out for him to take, “Here…figured you’d want this back—”
“Show me the worksite where you found it. Maybe there’s a clue there that’ll lead me to Mike—”
“That’s not a good idea…”
Terry tilted his head down at her short body. Rae had to crane her neck to look at him.
“That’s my family, Rae. And we had a deal. Did you forget that?”
Rae’s eyes darted down to her feet. Terry released a sigh.
“Fuck it, just point me in the direction and I can be out your way.” Terry said with a frustrated voice.
“It’s not that I don’t want to help you, Terry. It’s just…there’s guys from this group that are pretty dangerous…they’ve been on the hunt for anyone that could be infected and they’re killing them on the spot.”
“Hmm, is that so?” Terry looked left and right before his intimidating eyes fell on her again, “I just took down one of those guys not too far from here. I ended up with this,” Terry raised his arm to show her, “And I’m not tryna stick around to get infected. Got something on you to wrap me up?”
“Yes,” Rae started walking backwards towards a door, “This way—”
“Stop.”
Rae paused.
“What’s down there?”
“Our refuge. You coming or not?”
Terry hesitated. He looked around him one last time before following Rae through a door, darkness the only thing he could make out ahead.
@theereina @bombshellbre95 @planetblaque @trippyscotch @megamindsecretlair @thesweetestdrug @theblulife @blackerthings @deja-r@kanafunee @helloncrocs @kaylabuggggg06 @skyesthebomb @blyffe @gwenda-fav @beenathembo @blackpinup22 @novaniskye @melaninhawtie @urfavblackbimbo @avoidthings @rose-bliss @xo-goldengirl @kinginwithbreezy-blog @mysecertdiaryofableedingheart @sirenmouths @kokokonako @creartivefairy @soulfulbeauty19 @therealmrsrhodes @hrlzy @nayaesworld @gg-trini @brattyfics @flydotty @writingsbytee @shiania @browngirldominion @notapradagurl7 @madamzola @kismet83 @aristasworld @sl33p-deprived-princess @erynnnn @itssbrie @melaninangel @withoutmusiclifewouldbflat @sweettea-and-honeybutter
274 notes
·
View notes
Text
okay am i just going insane or does anyone else think that endocrine disorder is not like inherently a synonym for intersex. (in reference to this post and the discourse surrounding it). like at least when it comes to ICD coding, there's a million different endocrine disorder codes, and the code that specific doctor was most likely using was E34.9, which is for "endocrine disorder, unspecified" and doesn't automatically imply intersex variation and instead is so vague that it could mean any range of endocrine diagnoses from like thyroid disorders to diabetes to intersex variations. in the medical billing world i just do not think it is an automatic synonym for intersex variations and i don't think it's automatically treated that way by doctors!
because like as an intersex trans person who has been denied access to HRT because i'm intersex, yes, of course, i agree that it's a ridiculous idea to try to get intersex diagnoses added to your chart, and i'm pissed off by some of the posts I've seen denying the realities of intersex medical abuse and the current legal landscape for intersex people trying to access HRT. it would not help and it's honestly insulting + painful to see a few people suggesting that it would be beneficial to have an intersex diagnosis added to your chart--it shows me how some perisex people don't bother to listen to intersex people about what it's actually like to navigate this shit for us.
but i just don't think that's what people are talking about here, and i think it's honestly such a bad faith reading to assume that other trans people are instantly jumping to lying about being intersex. and i saw a lot of transphobic bullshit in the replies of that post from other intersex people. and i think i also just feel more suspicious about the motives of some people involved given like. the widespread transmisogyny + associated harassment campaigns in a lot of tumblr intersex spaces. like. i think it is completely reasonable for trans people to strategize about different ways to access HRT and i don't think we should be calling them intersexist if they haven't actually said any intersexist shit.
i don't know!!! i just think that it's always okay to lie to doctors and that it's valuable for us to discuss this shit and figure out strategies to try and what's going to be the most pragmatic! i also need people to educate themselves about what intersex healthcare actually looks like and intersex medical abuse and the way that gender affirming care bans also prevent a lot of intersex people from accessing hormones, because otherwise you get ridiculous shit where people were defending the hypothetical idea that doctors are helpful and support intersex people's bodily autonomy when it comes to our healthcare lmfao
like am i the only one feeling this way here like what is going onnnnnnnnn
sometimes being both trans and intersex online feels exhausting i have to say!!!
#personal#actuallyintersex#intersex#also i don't think billing specific encounters as endocrine disorder will actually work when it comes to#navigating HRT bans. if your insurance company is aware that you are trans and the rest of your chart says you're trans.#but i think if it does work for some people thats great i just am cynical
61 notes
·
View notes
Text

Character Information
Name: Vera Brooks Age: 42 Pronouns: she/her Face Claim: Christina Milian Occupation: Forgery specialist Neighborhood: Little Italy
Short Facts
Vera's forgery career kicked off not because she was feeling rebellious, but because her mom got cancer and Columbia College Chicago had to take a backseat.
Her first steps into illegal document creation were relatively innocent - making fake IDs for college students - before evolving into sophisticated document authentication and reproduction.
Beyond just forgery, she developed a unique specialty in recreating historical documents and artwork provenance papers, serving both legitimate museums and shadowy collectors.
Her 2021 move to Devil's Junction wasn't random - she timed her relocation during a period of heightened tension between crime families, positioning herself as a valuable neutral resource.
Her art restoration business isn't just a cover - she actively maintained it as a legitimate operation, showcasing real conservation work alongside her covert activities.
Even in her not-so-legal career, Vera kept her moral compass firmly in her pocket. Identity theft was a hard pass - she wasn't about to start messing with innocent people's lives just because she could.
She's developed a risk management strategy by maintaining strict professional discretion and balanced relationships with all crime families in Devil's Junction.
She gives back to the community through youth art programs, seeing herself in disadvantaged kids who need creative outlets like she once did.
Biography
Vera Brooks didn’t choose to enter the world of document forgery - necessity led her there. Born on June 18, 1982, in Chicago’s South Side to a single mother working multiple jobs, she learned early that survival sometimes required creative solutions. Her artistic talents emerged in high school, where she excelled in graphic design and fine arts, earning a partial scholarship to Columbia College Chicago. However, mounting medical bills from her mother’s cancer diagnosis forced her to drop out during her junior year. What started as a side hustle creating fake IDs for college students evolved into a sophisticated operation. Her attention to detail and steady hands earned her a reputation as a master document authenticator and reproduction specialist. She developed a particular expertise in recreating historical documents and artwork provenance papers, skills that attracted high-end collectors and museums - some legitimate, others less so. When heat from Chicago law enforcement intensified in 2021, Vera strategically relocated to Devil’s Junction. Her arrival matched the growing feud between the city’s crime families. Setting up shop in Little Italy, she carefully positioned herself as a neutral party, providing services to all while maintaining strict professional discretion. Her art restoration business is a front for her other work. The gallery showcases her art conservation, but her secret, illegal projects happen in her high-tech studio. She handles the city’s power struggles in a practical way, carefully balancing relationships to stay safe. Despite her chosen profession, Vera holds to a personal code. She refuses jobs involving identity theft that could harm innocent people and maintains a policy of destroying any work that she discovers might be used for violent purposes. This ethical framework, while sometimes costly, has helped her maintain respect among both the traditional families and the aggressive newcomers. In her rare downtime, she volunteers at a youth art program, believing in giving disadvantaged kids the creative outlets she once cherished.
3 notes
·
View notes
Text
By: Christina Buttons
Published: Feb 21, 2024
The Arizona Mirror published an article earlier this month titled "The latest GOP anti-trans strategy: Requiring ‘detransition’ services," arguing that legislation aimed at providing healthcare and insurance coverage for detransitioners is unnecessary—it is merely a tactic by Republicans to hassle people who currently identify as transgender. The article was republished under the same title in the Phoenix New Times.
The article focuses on an Arizona senate bill that would make the pathway of detransition easier for those who are struggling to get the healthcare they need. Currently, there are no billing codes for detransitioning, nor is there anything resembling a standard of care for this growing population. Additionally, some insurance companies explicitly exclude gender-reversal procedures.
But you wouldn’t learn any of this from reading the Arizona Mirror. It appears that the author, Gloria Gomez, only writes about the bill in an attempt to discredit it. The articles’ premise is that detransitioners face no difficulties in accessing healthcare and this bill is merely a scheme designed to inconvenience people who currently identify as transgender.
Gomez does not speak to a single detransitioner, opting instead to quote gender activists who argue the bill is “unnecessary” and not a “real issue” because detransitioners’ “medical needs are already covered by insurance.”
The first half of this article will debunk these misleading claims and clarify the purpose and necessity of detransition healthcare bills, offering a new contribution to the discourse. The latter half will counter several common misleading claims about detransition and "gender-affirming care" made by Gomez. For those familiar with my work, I often address these claims, so some of the content may be drawn from earlier writings.

Gomez quotes two representatives from the Human Rights Campaign (HRC), the largest LGBTQ political lobbying organization in the United States, which received $50 million in donations in 2023. The HRC regularly protests the New York Times' coverage of detransitioners and the inadequacies of the "gender affirming" model of care.
-
Misleading Claim #1: Detransitioners’ medical needs are “already covered by health insurance”
An emailed statement by Cathryn Oakley, the senior director of legal policy for the Human Rights Campaign (HRC) said:
“This bill is an unnecessary and gratuitous excuse to talk about detransition in an effort to shift the focus from the actual health care that transgender people receive, which is supported by every mainstream American medical health organization, to the care of a very small number of folks whose medical needs are already covered by health insurance.”
For many detransitioners, this is false.
There is significant variability among insurance policies regarding what is covered, leading to disparities in access to care. While some insurers may cover detransition care under certain conditions, others may not, deeming the care not medically necessary.
Had Gomez done any research she’d know some insurance companies explicitly exclude detransition healthcare—like Capital Blue, which has a stipulation in its plans stating gender-reversal surgery is “considered not medically necessary and, therefore, not covered.”
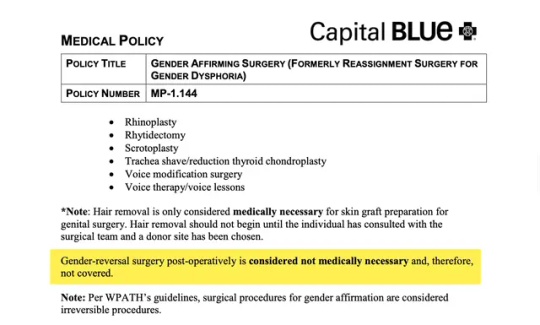
[ Capital Blue ]
…or United Healthcare Community Plan, which excludes “reversal of genital surgery or reversal of surgery to revise secondary sex characteristics.”
[ United Health Community Plan ]
Others evaluate on a case-by-case basis (California Health & Wellness) or if certain criteria are met (Wellmark), and thankfully, some health insurance companies do cover detransition healthcare (Aetna). These are just a few examples and by no means an exhaustive list. I plan to conduct a much larger overview of insurance providers’ coverage of detransition care in a future investigative article.
-
Misleading Claim #2: Detransitioners receive the same care as those seeking to transition
Bridget Sharpe, the director of HRC's Arizona branch, who responded to the Arizona Mirror's request for comment, said:
“The care for people who detransition is the same as the care for transgender people. Any medical service that affirms someone’s gender includes someone who decides to detransition. If they decide to detransition they are affirming their gender.”
This is not accurate.
Under the current system, when someone transitions, they receive a diagnosis code indicating gender dysphoria. When someone detransitions, they no longer meet the criteria for a gender dysphoria diagnosis. Without a specific diagnosis like gender dysphoria to justify “medical necessity,” obtaining coverage for detransition procedures can be complicated, demonstrating the need for legislation that ensures detransition is covered.
Legislation like SB 1511, which mandates that doctors, health care institutions, or any other licensed health care providers in Arizona offering gender transition procedures must also provide gender detransition procedures. Furthermore, if an insurance policy covers gender transition, it will be required to "provide or pay" for detransition procedures.
A third provision aims to collect information on how many people are requesting detransition procedures by requiring insurance companies to submit a report. Currently, there is no method for tracking detransition, so we don't know how many people are detransitioning.
Gathering more data on detransitioners would aid in the process of acquiring new billing codes from coding authorities. Nine months ago, FAIR in Medicine submitted an application to the Centers for Disease Control and Prevention (CDC) for International Classification of Disease (ICD) diagnosis codes specific to detransition. This application is currently under review. The process to review and approve new ICD diagnosis codes can take over a year and involves several steps, including gathering data, public comment, and revision.
The absence of dedicated medical billing codes for detransition procedures creates a significant barrier for healthcare providers seeking reimbursement for these services. Consequently, they may resort to using inaccurate billing codes.
In practice, healthcare professionals apply their discretion to navigate these challenges. For example, a detransitioned woman who underwent a hysterectomy as part of her transgender experience might be classified similarly to a postmenopausal woman for the purposes of accessing hormone replacement therapy.
An important article by Drs. Aida Cerundolo and Carrie Mendoza on detransition billing codes highlights a case like this: A woman named Katie began taking testosterone at 19, underwent a double mastectomy at 20, and had a hysterectomy at 24. Shortly after, she realized transitioning was a mistake.
Now at 25, Katie is experiencing early menopause and has had significant difficulty obtaining the correct hormone dosage. Even after numerous phone calls, she was prescribed estrogen at a dose typically given to males seeking to become transgender women, which was not suitable for her needs. For obvious reasons, this is not a sustainable solution. We need detransition billing codes.
-
Misleading Claim #3: Detransition healthcare is not a “real issue”
The director of HRC's Arizona branch, Bridget Sharpe, continued her statement by saying:
Instead of resolving a real issue, Sharpe said, the Republican legislation instead seeks to weaponize detransitioning against transgender health care.
It is insulting to dismiss detransitioners’ healthcare needs as not a “real issue.”
Had Gomez interviewed any detransitioners or reviewed research on them, she would understand that many encounter challenges in finding information on detransition or healthcare professionals equipped to address their specific needs.
A 2021 international survey of 237 detransitioners found the support available to detransitioners to meet their medical needs is currently inadequate.
49% seek accurate information on stopping or changing hormonal treatment.
24% require assistance for complications from surgeries or hormonal treatments.
15% need information on and access to reversal surgeries or procedures.
7% provided other responses not listed, such as the need for tests to assess current reproductive health, information on the long-term effects of cross-sex hormones, the health consequences of undergoing a full hysterectomy, and issues related to pain from chest binding.
My preliminary survey of 94 detransitioners and desisters (pending publication) revealed that 72% of those seeking medical assistance faced significant challenges, and 78% of those who sought insurance coverage for detransition services had difficulty accessing it.
I've interviewed several detransitioners who have had immense difficulty in getting insurance coverage for detransition-related needs. One male detransitioner had to wait a full year to have his breast implants removed. Others have turned to crowdfunding to finance their detransition-related procedures.
However, one detransitioner I recently spoke with had no issues in getting insurance coverage for breast reconstruction surgery, which I believe is due to a growing awareness of detransitioners' needs in the last year.
-
Activist-journalism
In the last decade, influential activist organizations, including HRC, GLAAD, ACLU, and SPLC, have collaborated closely to shape the narrative on transgender issues. They provide news outlets with a range of media reference guides, stylebooks, fact sheets, and other resources, equipping mainstream journalists—most of whom are not well-informed on the debate surrounding youth medical transition—with the materials needed to present a biased perspective and label any valid concerns as bigotry. This approach effectively transforms journalists into activists.
Activists rely on propaganda tactics like the illusory truth effect—the tendency for people to believe things that are false after repeated exposure. This strategy of creating a semblance of public agreement benefits from the support of progressive platforms like the Arizona Mirror, which claims to be “an independent, nonprofit news organization” yet serves as an example of political activism masquerading as journalism. Their reporting standards neglect objectivity and thorough research, delivering a skewed narrative that deceives the public.
It seems ironic that progressives who champion “healthcare for all” would try to undermine bills aimed at ensuring a vulnerable group has access to healthcare. And like Pamela Paul pointed out in her recent New York Times op-ed, “These are people who were once the trans-identified kids that so many organizations say they’re trying to protect.”
Activist organizations frequently ignore or downplay the experiences of individuals who have detransitioned, despite these being the same individuals they pledge to support. This neglect is a significant departure from their stated principles. For many, a transgender identity is not a lifelong experience — they need support too.
-
Additional reading:
Misleading Claim #4: Detransition is rare
Gomez states that people who detransition "represent an extreme minority of the transgender experience." To support this statement, she cites the U.S. Transgender Survey of 2015, which is a deeply flawed sample consisting primarily of older adults who transitioned under a medical model vastly different from the current gender-affirmation model concerning youth and young adults.
The study included only those who identified as transgender at the time they took the survey, which, by definition, excludes detransitioners. Gomez overlooks more recent, robust, and representative studies that challenge the notion that detransition is rare, such as a 2022 comprehensive review of medical records that found 30% of teens and young adults discontinued cross-sex hormones after 4 years.
A 2021 study found that 75% of detransitioners did not inform their doctors about their decision to detransition. The rate of detransition remains unknown and is difficult to track, partly due to the absence of specific medical billing codes for detransition procedures.
-
Misleading Claim #5: Youth medical transition is backed by major medical organizations
Gomez relies on an appeal to authority fallacy by stating that puberty blockers and cross-sex hormones for minors are “backed by major medical associations as safe and necessary for the well-being of transgender people.” But these US-based medical organizations are not basing their recommendations on the best available evidence.
Systematic evidence reviews—widely recognized as the gold standard in evidence-based medicine (EBM)—have found that the risks of youth medical transition outweigh any purported benefits.
Public health agencies in Finland, Sweden, England, Denmark and soon Norway have aligned their guidelines with systematic evidence reviews, and have adopted a far more restrictive and cautious approach, one that prioritizes psychotherapy.
Medical authorities in several other countries including France, Ireland, Italy, the Netherlands, Australia, and New Zealand, have begun expressing concerns or are in the process of reevaluating their stance on transitioning minors.
US-based medical organizations in favor of youth medical transition have not aligned their guidelines with systematic evidence reviews, actively resisting such calls for many years. However, just last year, the American Academy of Pediatrics (AAP) finally announced it will be conducting its own systematic evidence review.
The unfortunate reality is that a small, ideologically-motivated group of individuals in charge of US-based medical organizations are acting as political entities that represent specific interest groups and invest heavily in lobbying.
Last year, international experts publicly weighed in on the American debate over "gender-affirming care" for the first time. 21 leading experts on pediatric gender medicine from eight countries wrote a letter expressing disagreement with US-based medical organizations over the treatment of gender dysphoria in youth, urging them to align their recommendations with unbiased evidence “rather than exaggerating the benefits and minimizing the risks.”
Dr. Gordon Guyatt, a clinical epidemiologist at McMaster University and founder of the evidence-based medicine (EBM) movement, who is a highly respected figure in the field of medical research methods and evidence evaluation, has stated that the current guidelines in the US for managing gender dysphoria in adolescents are "untrustworthy" and should not be considered evidence-based.
Guyatt adds that the guidelines fail to offer cautious and conditional recommendations appropriate for the low-quality evidence, highlighting that European policies are ”much more aligned with the evidence than are the Americans.”
-
Misleading Claim #6: Bills aimed at safeguarding youth and vulnerable adults are “anti trans”
Gomez refers to detransitioner Chloe Cole, who transitioned as a minor and spoke in favor of SB 1511, as “a frequent supporter of anti trans legislation.”
Activists and activist-journalists rely heavily on the label “anti-trans,” a strategy referred to as poisoning the well. By branding anyone or anything critical of youth medical transition as motivated by bigotry, they skew the audience’s perception, making them less receptive to other viewpoints.
Legislation aimed at protecting youth (and sometimes vulnerable young adults with psychiatric comorbidities) from a reckless model of care is not “anti-trans,” it is pro-safeguarding. Gender activists have spent years lobbying to remove these protective measures, which they call “gatekeeping.”
Many states that have placed restrictions on medical transition services have not included provisions for detransition or gender-reversal procedures, which is why some are doing so now. Earlier this month, the Tennessee House filed a bill requiring gender clinics to perform detransition procedures.
Do No Harm, an organization dedicated to scientific integrity and ethics in medicine, introduced model legislation last year called the Detransitioner Bill of Rights, which has already been used in several states.
-
Misleading Claim #7: Republicans are the sole proponents of age restrictions on medical transition services
Throughout the article, Gomez repeatedly identifies Republican lawmakers as proponents of "anti-trans legislation," stating, "far-right politicians have latched onto detransitioners to justify their calls to curtail gender-affirming care."
This perspective overlooks the broader context and the international consensus among European countries, arguably more progressive than the United States, that have drastically scaled back on youth medical transition. It also ignores the bipartisan support that opposition to youth transition policies is now receiving in the United States, as groups of Democrats in four states (Louisiana, Maine, New Hampshire, and Texas) have voted against them.
There's also a new organization called Democrats for an Informed Approach to Gender (DIAG), which seeks to organize initiatives for left-leaning individuals that oppose youth transition. Additionally, organizations like Genspect, the Society for Evidence-Based Gender Medicine (SEGM), the LGBT Courage Coalition, the Gender Dysphoria Alliance, and others are non-partisan but primarily consist of healthcare professionals and researchers who identify as liberal or left-leaning, or at least did at some point in time.
Age restrictions on youth medical transition reflect broader public opinion across the political spectrum. A 2023 Washington Post-KFF poll found a majority of adults (nearly 7 out of 10) oppose allowing children aged 10 to 14 access to puberty-blocking drugs, and a similar majority (6 out of 10) opposes cross-sex hormones for 15- to 17-year-olds.
It's regrettable that legislative intervention has become necessary, but as medical organizations continue to let ideologues dictate policies and silence more moderate voices within the profession, lawmakers are left with little choice but to step in.
==
If you haven't already spotted the moral-religious overtones in this ideology, I don't know what more to show you.
The people who insist that "Gender Affirming Treatment" is "healthcare" and "not about you, it's about us and our survival," also want you to believe that care for detransitioners is all about them and attacking them. The narcissism and sociopathy are completely off the charts.
What they're actually afraid of is the scale of this medical scandal. At present, there's no insurance coverage, no billing codes, and limited doctor accountability, which will change as lawsuits proceed. Activists can claim that detransition is "rare" because the medical system doesn't track it. Detransitioners frequently do not return to the same doctor-activist who drugged or carved them up in the first place and are forced to simply "make do." Legal coverage of detransition isn't just a recognition of the phenomenon of detransition and the flaws of simply "affirming" everyone but will also reveal in fine grain detail the extent of it, in a way activists will be unable to continue lie about.
Meanwhile...
#Christina Buttons#detrans#detransition#gender ideology#gender identity ideology#queer theory#medical corruption#medical malpractice#medical scandal#gender affirming care#gender affirming healthcare#gender affirmation#affirmation model#religion is a mental illness
12 notes
·
View notes
Text
Learning Medical Billing Management: Strategies to Boost Efficiency and profits
Mastering Medical Billing Management: Strategies to Boost Efficiency and Revenue
in today’s competitive healthcare landscape, effective medical billing management is vital for optimizing practice revenue and ensuring smooth operations. Whether you run a small clinic or a large hospital, mastering the art of billing management can substantially impact your bottom line. This extensive guide explores proven strategies, practical tips, and technological innovations to **boost billing efficiency**, **maximize revenue**, and streamline your medical billing processes.
Why Is Medical Billing Management Critical for Healthcare Practices?
Medical billing is more than just submitting claims; it encompasses a broad spectrum of activities including patient data management,coding accuracy,claim submission,payment processing,and compliance adherence. Poor billing management can lead to delayed reimbursements, increased denials, and revenue loss. Conversely, a well-organized billing system enhances cash flow, improves patient satisfaction, and reduces administrative burdens.
Key Challenges in Medical Billing
Complex Coding and Documentation: Ensuring accurate coding is critical to avoid claim denials.
Insurance billing Complications: Navigating different insurer requirements can slow down reimbursements.
High Claim Rejection Rate: repeated rejections reduce revenue and increase operational costs.
Delayed Payments: Inefficient follow-up leads to cash flow issues.
Regulatory Compliance: Staying compliant with HIPAA and other regulations is a constant challenge.
Strategies to Master Medical Billing Management
1. Implement an Advanced Medical Billing Software
Leverage technological solutions such as electronic health record (EHR) integrated billing software.Features to look for include automated claim generation, real-time eligibility verification, denial management tools, and secure payment portals. The right software reduces manual errors and accelerates the billing cycle.
2. Prioritize Staff Training and Education
Constantly train your billing staff on the latest coding updates, payer policies, and compliance protocols. Knowledgeable staff are more efficient at reducing errors, avoiding denials, and managing appeals.
3. Standardize Billing Procedures
Develop clear, standardized billing workflows to ensure consistency. Regular audits and process reviews can identify bottlenecks and areas for advancement.
4. Ensure Accurate and Complete Documentation
Accurate clinical documentation supports proper coding and claim accuracy. Encourage providers to document thoroughly and clearly to minimize claim rejections due to insufficient information.
5. Conduct Regular Reconciliation and Follow-Up
implement daily reconciliation of payments and claims. Use automated alerts for overdue claims and promptly follow-up on unpaid or denied submissions to recover revenue faster.
6. Focus on Compliance and Security
Stay updated with healthcare regulations such as HIPAA, and use secure, encrypted platforms for billing data. Compliance reduces legal risks and potential fines.
7. Analyze and Monitor Billing Metrics
Regularly review key performance indicators (KPIs) such as claim acceptance rate, average days in accounts receivable (A/R), and denial rates. Use these insights to adapt your strategies effectively.
Benefits of Optimized Medical Billing Management
Benefit
Description
Increased Revenue
Reduce claim denials and accelerate reimbursements for improved cash flow.
Reduced Administrative Costs
Automation minimizes manual work and errors, saving time and money.
Enhanced Patient Satisfaction
Clear billing processes and quick responses improve patient experiences.
Better Compliance
Staying aligned with healthcare regulations minimizes legal risks.
Operational Efficiency
Streamlined workflows lead to faster processing and less stress on staff.
Practical Tips to Improve Medical Billing Efficiency
Use integrated EHR and billing software for seamless data flow.
Verify patient insurance eligibility prior to services to prevent rejections.
Automate recurring billing tasks where possible.
Implement denial tracking and appeals management systems.
Schedule periodic staff training sessions on coding updates.
Maintain detailed documentation to support claims and audits.
Set clear KPIs and regularly review billing performance metrics.
Case Study: How a Private Clinic Boosted Revenue by 30%
Background: A growing private clinic faced frequent claim denials and cash flow issues. They decided to overhaul their billing system using advanced software and staff training.
Implementation: They adopted an integrated EHR and billing platform, conducted regular coding workshops, and established daily reconciliation routines.
Results: Within six months, claim rejection rates dropped by 25%, and overall revenue increased by 30%. Patient satisfaction scores improved due to transparent billing processes.
Conclusion
Mastering medical billing management is essential for healthcare providers aiming to optimize revenue and operational efficiency. By investing in the right technology, training staff, standardizing procedures, and monitoring key metrics, practices can significantly reduce errors, accelerate reimbursements, and enhance patient satisfaction. Embracing these strategies will ensure your practice remains financially healthy and compliant in an increasingly complex healthcare environment.
Remember, efficient medical billing management is a continual process of improvement. stay informed about industry changes,leverage automation,and prioritize accuracy to achieve long-term success in your healthcare practice.
https://medicalcodingandbillingclasses.net/learning-medical-billing-management-strategies-to-boost-efficiency-and-profits/
0 notes
Text
Leading 10 Must-Read Books on Medical Billing to Boost Your Healthcare Career
Top 10 Must-Read Books on Medical Billing to Boost your Healthcare Career
Embarking on a career in medical billing can be both rewarding and challenging.As the healthcare industry evolves rapidly with new coding standards, regulations, and billing practices, staying well-informed is crucial for success. Whether you’re just starting out or looking to enhance your existing skills, reading the right books on medical billing can provide valuable insights, practical knowledge, and a competitive edge. In this comprehensive guide, we present the top 10 must-read books on medical billing that can help elevate your healthcare career to new heights.
Why Reading books on Medical Billing Is Essential for Your Healthcare Career
Understanding the complexities of medical billing requires continuous learning. The healthcare billing landscape is constantly changing with updates in coding systems like ICD-10, CPT, and HCPCS, as well as new compliance regulations and billing software advancements. Reading authoritative books offers several benefits:
Enhanced Knowledge: Master the fundamentals and advanced concepts of medical billing.
Stay Updated: Learn about latest industry changes, code updates, and compliance standards.
Improve Practical Skills: Gain tips and strategies to handle real-world billing challenges effectively.
Career Advancement: Position yourself as a informed professional,increasing job opportunities.
Practical Tips for Maximizing Your Learning from Medical Billing Books
Create a Reading Schedule: Dedicate regular time slots to study and review.
Take Notes: Highlight crucial concepts, coding tips, and regulatory updates.
Implement Knowledge: Practice by applying what you’ve learned using billing software or simulated exercises.
Engage with Professional Communities: Join forums and discussion groups for insights and peer support.
Overview of the Top 10 Must-Read Books on Medical Billing
Below is a curated list of essential books that cover foundational knowledge, advanced billing strategies, coding updates, and practical insights into medical billing and coding. These books are highly recommended for healthcare professionals, billing specialists, and students aiming to excel in this field.
Rank
Book Title
Author
Key Focus
1
Medical Billing & coding for Dummies
Ana Heilmann
Introductory guide, coding basics, billing procedures
2
Coding Fundamentals for Prosperous Medical Billing
Carol J. Buck
In-depth coding techniques, compliance, and updates
3
The Medical Billing company’s Guide to Coding and Compliance
Sharon hanson
Billing company operations, legal compliance
4
Understanding Healthcare Coding: ICD-10-CM and CPT
Barbara L. Danney
Medical coding fundamentals with practical examples
5
Medical Billing & Coding Handbook
Cengage Learning
Comprehensive reference, billing workflows, coding standards
6
Medical Insurance: Text & Procedures
elam & Sager
insurance procedures, claims processing
7
Mastering Medical Billing & Coding
Morleys Learning
Practical insights, billing software skills
8
Healthcare Billing and Reimbursement
June M. Reinardy
Billing forms, reimbursement strategies
9
The Complete Medical Billing and Coding Exam Guide
Daniel Favreau
Exam planning, certification insights
10
Billing and Coding Made Easy
Judy Capko
Simplified explanations, practical tips
Deep Dive: Highlights of Some Essential Books
1. Medical Billing & Coding for Dummies by Ana Heilmann
This beginner-friendly book provides a straightforward introduction to the world of medical billing and coding. It covers basic terminology, billing procedures, and key coding concepts, making it a perfect starting point for newcomers.
2. Coding Fundamentals for Successful Medical Billing by Carol J. buck
Designed for those seeking in-depth understanding, this book offers comprehensive insights into coding techniques, including CPT, ICD-10, and HCPCS. It emphasizes compliance and updates essential for staying current in the industry.
Real-Life Case Studies and Practical Applications
Integrating case studies into your learning process can substantially enhance understanding. Here are examples of how these books can help in real-world scenarios:
Resolving Billing Disputes: Apply coding accuracy principles learned from “Coding Fundamentals” to minimize claim denials.
Updating to Current Coding Standards: Use insights from “Understanding Healthcare Coding” to adapt to new ICD-10 updates.
Efficient Claim Submission: Leverage practical tips from “Mastering Medical Billing & Coding” to streamline workflows.
Conclusion: Invest in Your Healthcare Future with the Right books
In today’s competitive healthcare environment, staying ahead in medical billing knowledge is vital. The books listed above serve as valuable resources to deepen your understanding, enhance your practical skills, and keep you updated on the latest trends and regulatory changes.Whether you’re an aspiring billing specialist, a seasoned professional, or a healthcare administrator, investing time in reading these essential books will undoubtedly boost your career prospects and professional competency.
Start Your Learning Journey Today
Don’t wait to elevate your healthcare career. Dive into these top-rated medical billing books, implement your new knowledge, and watch your confidence and expertise grow. Remember, effective billing not only ensures compliance and revenue but also contributes significantly to excellent patient care and healthcare management.
© 2024 Your Healthcare Resources | All Rights Reserved
https://medicalbillingcertificationprograms.org/leading-10-must-read-books-on-medical-billing-to-boost-your-healthcare-career/
0 notes
Text
Learning Medical Services Billing: Essential Tips to Boost Revenue and Ensure Accuracy
Mastering Medical Services Billing: Essential Tips to Boost Revenue and Ensure accuracy
Effective medical services billing is crucial for healthcare providers aiming to maximize revenue,maintain compliance,and provide quality patient care. As the healthcare industry becomes increasingly complex, mastering the nuances of medical billing can differentiate accomplished practices from those facing financial challenges. This complete guide offers essential tips and practical insights to help healthcare professionals optimize their billing processes, boost revenue, and ensure billing accuracy.
Understanding the Importance of Accurate Medical Billing
Medical billing is the backbone of revenue cycle management. Accurate and efficient billing ensures that providers receive appropriate compensation for services rendered. mistakes or delays can lead to denied claims, delayed payments, and lost revenue. Besides financial implications, correct billing also ensures compliance with insurance policies and regulations, avoiding potential legal issues and penalties.
Key Benefits of Mastering Medical Services Billing
Increased Revenue: Minimize denied claims and optimize reimbursements.
Improved Cash Flow: Faster claim submission leads to quicker payments.
Enhanced Patient Satisfaction: Obvious billing reduces confusion and disputes.
Regulatory Compliance: Reduce risk of penalties through adherence to billing standards.
Operational Efficiency: Streamlined billing process saves time and resources.
Practical Tips to Master Medical Services Billing
1. Invest in Robust Billing Software
Choosing the right billing software can considerably streamline your billing process.Look for solutions with features like insurance verification,automatic claim generation,real-time tracking,and compliance checks.Cloud-based platforms offer flexibility and scalability, essential for growing practices.
2. Ensure Detailed and Accurate Documentation
Complete documentation of patient encounters is vital. Double-check that all procedures, diagnoses, and modifiers are correctly recorded to match billing codes. Incomplete or inaccurate documentation leads to claim denials and delays.
3. Use Correct and Up-to-Date Coding
Stay current with the latest CPT (Current Procedural Terminology), ICD-10, and HCPCS coding updates. Proper coding ensures accurate reimbursement and reduces the risk of audits or penalties.
4. Conduct Regular Staff Training
Continuous education for billing staff keeps them updated on industry changes,compliance requirements,and best practices. Well-trained staff are less likely to make costly errors.
5. Verify Patient Insurance Details
Pre-authorization and insurance verification prevent claim rejections. Confirm coverage details before the appointment to avoid surprises and delays.
6. Implement Quality Checks and Audits
Regular audits of submitted claims help identify common errors, improve accuracy, and reduce denials. Establish a checklist for review before submission.
7. Follow Up on denied or Rejected Claims Promptly
Timely follow-up with payers ensures issues are resolved quickly, optimizing cash flow and reducing outstanding receivables.
Case Study: Improving Revenue Through Better Billing Practices
Practice Type
Previous Monthly Revenue
After Implementing New Billing Strategies
Revenue Increase
Primary care Clinic
$150,000
$180,000
20%
Specialty Practice
$200,000
$240,000
20%
By adopting advanced billing software, staff training, and rigorous auditing, healthcare practices have seen a noteworthy increase in revenue and reduced claim denial rates.
Tools and Resources for Medical Billing Success
Billing Software: Kareo, AdvancedMD, PracticeSuite
Coding Resources: American Medical Association (AMA), AAPC
Compliance guidelines: HIPAA, CMS policies
Training Platforms: Healthcare Billing and Coding Certifications, webinars
First-Hand Experience: My Journey in Medical Billing Optimization
Having worked with diverse healthcare providers, I’ve seen firsthand how effective billing strategies transform a practice’s financial health. When I implemented strict documentation protocols,updated coding practices,and staff training,my clients experienced a notable reduction in claim rejections and a smoother revenue cycle. It’s clear that mastering medical billing is an ongoing process-it requires vigilance, education, and process improvement.
Conclusion
Mastering medical services billing is essential for healthcare practices striving to boost revenue and maintain billing accuracy. By investing in the right tools, ensuring detailed documentation, staying current with coding updates, and fostering continuous staff education, practices can greatly reduce claim denials, improve cash flow, and enhance patient satisfaction. Remember, a proactive approach to billing not only safeguards your revenue but also promotes compliance and operational efficiency. Embrace these best practices today to make your billing process a powerful asset for your healthcare organization!
https://medicalbillingcodingcourses.net/learning-medical-services-billing-essential-tips-to-boost-revenue-and-ensure-accuracy/
0 notes
Text
Reducing Hospital Operational Costs Without Compromising Care – SHPL’s Strategy
In today’s competitive healthcare landscape, hospitals must balance two critical goals: delivering high-quality care and maintaining financial sustainability. Rising costs—from equipment and technology to staffing and utilities—can strain even the most established institutions.
SHPL Management Consultancy helps hospitals streamline their operations, reduce waste, and improve efficiency—without compromising on patient care.
Why Operational Cost Control Matters
Excessive spending not only affects profitability but can also impact service delivery. Cost inefficiencies often lead to:
Overstaffing or resource underutilization
Equipment downtime or redundancy
Billing errors and revenue leakage
Longer patient wait times and reduced satisfaction
Controlling these factors requires more than short-term fixes. It calls for a strategic approach to hospital operations.
SHPL’s Cost Optimization Framework
1. Department-Wise Cost Audit SHPL begins with a detailed audit of expenses across departments such as OPD, IPD, diagnostics, pharmacy, HR, and facility management. This reveals:
Areas of resource duplication
Non-performing services or units
Untracked inventory losses or billing issues
2. Resource Utilization Planning We help hospitals right-size their staffing, space, and equipment:
Optimizing shift patterns and manpower deployment
Scheduling diagnostics and procedures efficiently
Reducing idle time for expensive medical equipment
3. SOP-Driven Efficiency Standard Operating Procedures (SOPs) eliminate process variations that lead to time and cost wastage. SHPL implements SOPs in:
Admissions and discharge workflows
Lab and radiology reporting timelines
Pharmacy stock management
Billing and insurance processing
4. Technology Integration Digital tools reduce manual errors and save administrative time. SHPL assists in:
Selecting cost-effective EMR or HMS platforms
Automating inventory, billing, and scheduling systems
Implementing dashboards for real-time cost tracking
5. Vendor and Procurement Management SHPL helps hospitals save by:
Standardizing vendor contracts
Consolidating purchases for better pricing
Tracking supplier performance and delivery efficiency
6. Revenue Cycle Optimization From accurate coding to timely billing, SHPL ensures:
Clean claim submissions to insurers
Recovery of pending dues
Prevention of revenue leakage in outpatient and inpatient services
Real-World Impact
Hospitals that implemented SHPL’s cost-saving strategies achieved:
12–20% reduction in monthly operational costs
Improved patient turnaround time
Better staff productivity and morale
Sustained profitability without cutting essential services
Conclusion
Cutting costs doesn't mean cutting corners. With expert planning and system improvements, hospitals can reduce waste, increase efficiency, and maintain the highest standards of patient care. SHPL Management Consultancy delivers practical solutions that protect both your reputation and your bottom line.
#HospitalCostManagement#SHPLManagementConsultancy#HealthcareEfficiency#HospitalOperations#CostOptimization#HospitalSOPs#HealthcareConsultingIndia#MedicalFinance#HospitalWorkflow#RevenueCycleManagement
0 notes
Text
Why Medical Billing Audit Services Are Essential for RCM Success

In the ever-evolving landscape of healthcare, revenue cycle management (RCM) plays a pivotal role in ensuring financial sustainability for healthcare providers. One of the most crucial yet often overlooked components of RCM is medical billing audit services. With rising regulatory scrutiny, coding complexities, and payer challenges, conducting regular billing audits has become essential for mitigating revenue leakage and maintaining compliance.
In this blog, we’ll explore what medical billing audit services entail, why they matter, and how healthcare organizations can benefit from integrating them into their RCM strategies.
What Are Medical Billing Audit Services?
Medical billing audit services involve a comprehensive review and analysis of a healthcare provider's billing processes, coding accuracy, claim submissions, and reimbursement patterns. These audits are designed to identify discrepancies, detect potential fraud or abuse, and ensure compliance with federal and payer-specific regulations.
There are two primary types of billing audits:
Internal Audits: Conducted by the provider’s own billing or compliance team.
External Audits: Performed by third-party experts who bring an unbiased and specialized perspective.
Both types play a critical role in helping healthcare providers ensure the accuracy and integrity of their billing processes.
Why Are Medical Billing Audit Services Important?
1. Reduce Revenue Leakage
Revenue leakage is one of the biggest threats to a healthcare organization’s financial health. Whether it’s due to coding errors, missed charges, or claim denials, even small oversights can cost millions over time. Medical billing audit services help uncover these issues early, enabling providers to take corrective actions before they impact the bottom line.
2. Ensure Regulatory Compliance
The healthcare industry is heavily regulated, and failing to comply with coding and billing guidelines from CMS, HIPAA, and private insurers can result in hefty fines or even audits by regulatory bodies. Regular audits ensure that your practice stays compliant, reducing the risk of legal repercussions.
3. Improve Coding Accuracy
Inaccurate coding not only leads to claim denials but also delays reimbursements. Through detailed audits, providers can assess their coding accuracy, identify undercoding or upcoding trends, and train staff accordingly. This is especially vital for specialties like cardiology, oncology, and orthopedics, where coding complexity is high.
4. Enhance Operational Efficiency
By identifying gaps in the billing cycle, audits provide actionable insights that can streamline workflows, reduce claim rework, and minimize administrative burdens. This results in faster reimbursements and fewer rejections.
5. Protect Against Payer Audits
Insurance payers are increasingly conducting their own audits. If your billing processes are not airtight, you may be subject to clawbacks or penalties. Engaging a third-party for medical billing audit services helps you proactively identify and fix vulnerabilities before the payers do.
Key Areas Covered in a Medical Billing Audit
When you engage a service provider for medical billing audit services, the audit typically covers the following areas:
Charge capture analysis
CPT/ICD-10 coding accuracy
Medical necessity and documentation review
Modifier usage validation
Claim submission timelines
Denial patterns and trends
Reimbursement discrepancies
Patient balance and collections process
Each of these components plays a vital role in the RCM process and directly impacts your revenue cycle efficiency.
When Should You Perform a Billing Audit?
There’s no one-size-fits-all answer, but here are some triggers that indicate it might be time for an audit:
Sudden increase in claim denials or rejections
Significant drop in revenue or reimbursement rates
Changes in coding or billing staff
EHR system migration or upgrade
Preparing for external payer audits or accreditations
Regulatory updates or compliance changes
Ideally, healthcare organizations should conduct medical billing audit services at least once a year, and more frequently for high-volume or high-risk specialties.
Benefits of Outsourcing Medical Billing Audit Services
While some practices have in-house teams to perform audits, many benefit from outsourcing to RCM experts who specialize in this area. Here’s why:
✅ Expertise and Accuracy
Third-party auditors bring years of experience, updated compliance knowledge, and industry-specific insights that in-house teams may lack.
✅ Objectivity
An external team offers a fresh, unbiased perspective and is more likely to catch errors overlooked internally.
✅ Cost-Effective
Outsourcing eliminates the need to hire, train, and retain a dedicated internal audit team—resulting in lower operational costs.
✅ Faster Turnaround
Experienced vendors use advanced auditing tools and proven methodologies to complete audits quickly and efficiently, helping you act on insights faster.
How to Choose the Right Medical Billing Audit Partner
Not all audit service providers are created equal. Here are key factors to consider before selecting a vendor:
Industry expertise and certifications (e.g., AAPC, AHIMA)
Experience in your medical specialty
Comprehensive reporting capabilities
Customizable audit scope and frequency
Data security and HIPAA compliance
Client references and success stories
A reliable partner not only helps you optimize billing processes but also becomes a long-term advisor in your revenue cycle strategy.
Final Thoughts
In today’s challenging healthcare environment, medical billing is more than just a back-office function—it’s the lifeline of your revenue. Medical billing audit services act as a safeguard to ensure that every dollar earned is captured and collected efficiently. They not only protect your practice from compliance risks but also empower you to make data-driven decisions that drive long-term financial success.
Whether you’re a small clinic or a multi-specialty group practice, integrating regular billing audits into your RCM process is no longer optional—it’s essential. Start auditing today to stay ahead of the curve, improve your bottom line, and deliver better care without the financial stress.
0 notes
Text
Global Electronic Health Records EHR Market driven by regulatory push to sustain 5–6% CAGR 2029
The electronic health records (EHR) market is experiencing steady growth, with a CAGR projected at around 5-6% during the forecast period. The increasing adoption of digital health solutions, driven by the need for efficient healthcare management and regulatory mandates, is fuelling this growth. However, high implementation costs and data privacy concerns are barriers, slowing down the rapid expansion of EHR systems in some regions.
Electronic health records (EHR) refer to digital versions of a patient's medical history, maintained over time by healthcare providers. These records contain essential data like diagnoses, treatment plans, medications, immunization dates, allergies, and test results. EHRs are designed to streamline the sharing of patient information between authorized healthcare professionals, enabling more coordinated and efficient care. With a focus on enhancing healthcare delivery, EHR systems aim to reduce medical errors, improve patient outcomes, and support evidence-based decisions.
Download a free sample report for in-depth market insights https://meditechinsights.com/electronic-health-records-market/request-sample/
Regulatory Compliance and Government Support Driving Demand
One of the most influential factors driving the demand for electronic health records is the global push for regulatory compliance and the increasing involvement of government support. Governments around the world are adopting stringent regulations to standardize healthcare processes and ensure the digitization of health records. These regulations are designed to improve patient safety, reduce medical errors, and promote better quality of care through accessible and shared data. In the United States, the Health Information Technology for Economic and Clinical Health (HITECH) Act has played a pivotal role in encouraging the use of EHRs by offering financial incentives to healthcare providers. Similar initiatives can be seen across Europe, Asia, and other regions, where governments incentivize healthcare organizations to transition to digital records. This regulatory pressure and financial aid have accelerated EHR adoption, making compliance an essential driver in the market’s expansion.
AI Integration and Predictive Analytics Boosting Market Trends
An exciting trend fuelling the growth of the EHR market is the increasing integration of AI and predictive analytics These advanced technologies are enhancing the functionality of EHR systems, transforming them into more dynamic tools for healthcare professionals. AI-driven systems automate time-consuming administrative tasks such as data entry, coding, and billing, allowing physicians to spend more time on patient care. Furthermore, predictive analytics embedded in EHRs can analyze patient data to identify patterns, predict disease risks, and recommend personalized treatment plans. This trend is particularly beneficial for managing chronic conditions, as it allows for earlier interventions and more precise monitoring. By making EHR systems smarter and more intuitive, AI and predictive analytics are not only boosting operational efficiency but also contributing to improved clinical outcomes, thus increasing the overall value and appeal of these systems in the healthcare market.
Unlock key data with a sample report for competitive analysis: https://meditechinsights.com/electronic-health-records-market/request-sample/
Competitive Landscape Analysis
The global EHR market is marked by the presence of established and emerging market players such as Cerner Corporation (Oracle); Veradigm LLC (Allscripts Healthcare, LLC); Epic Systems Corporation; eClinicalWorks; Greenway Health LLC; NextGen Healthcare; Inc.; Medical Information Technology, Inc. (Meditech); TruBridge, Inc. (CPSI); AdvancedMD, Inc.; CureMD Healthcare; CareCloud, Inc. and McKesson Corporation among others. Some of the key strategies adopted by market players include product innovation and development, strategic partnerships and collaborations, and geographic expansion.
About Medi-Tech Insights
Medi-Tech Insights is a healthcare-focused business research & insights firm. Our clients include Fortune 500 companies, blue-chip investors & hyper-growth start-ups. We have completed 100+ projects in Digital Health, Healthcare IT, Medical Technology, Medical Devices & Pharma Services in the areas of market assessments, due diligence, competitive intelligence, market sizing and forecasting, pricing analysis & go-to-market strategy. Our methodology includes rigorous secondary research combined with deep-dive interviews with industry-leading CXO, VPs, and key demand/supply side decision-makers.
Contact:
Ruta Halde Associate, Medi-Tech Insights +32 498 86 80 79 [email protected]
0 notes
Text
Enhancing Physician Efficiency with Behavioral Health Revenue Cycle Management

In today’s complex healthcare environment, managing revenue streams efficiently is crucial for sustaining profitability especially in specialized fields like behavioral health. Behavioral Health Revenue Cycle Management (RCM) plays a pivotal role in ensuring timely reimbursements, accurate billing, and streamlined operations. For physicians working in behavioral health, a strong RCM strategy can not only minimize administrative burdens but also improve clinical focus, financial outcomes, and patient satisfaction.
In this blog, we’ll explore how behavioral health revenue cycle management supports physicians and why investing in specialized RCM practices is essential for long-term success.
What is Behavioral Health Revenue Cycle Management?
Behavioral Health Revenue Cycle Management refers to the end-to-end process of managing the financial aspects of patient care in behavioral health services—from patient registration and eligibility verification to claims processing, payment posting, and accounts receivable follow-up. Given the sensitive nature of mental health and substance use services, billing complexities, and frequent changes in payer regulations, RCM in this area demands a more specialized approach.
Unique Challenges in Behavioral Health RCM
Behavioral health practices face a distinct set of RCM challenges that can overwhelm physicians if not managed properly:
Variable session lengths and codes: Unlike standard medical visits, behavioral health services may involve individual therapy, group therapy, evaluations, and crisis interventions all requiring accurate coding.
Prior authorizations: Mental health services often require additional documentation and approvals, delaying care and reimbursement.
Coverage limitations: Insurers may restrict the number of sessions, therapy types, or treatment durations, affecting reimbursement potential.
Compliance regulations: HIPAA, HITECH, and payer-specific rules are especially stringent for behavioral health providers.
Without a robust behavioral health revenue cycle management system, physicians risk revenue leakage, denied claims, and patient dissatisfaction.
How Behavioral Health RCM Benefits Physicians
1. Reduces Administrative Overload
Physicians in behavioral health often juggle both clinical and administrative tasks. A dedicated RCM system automates tasks such as eligibility checks, coding accuracy, and claims submission. This reduces the manual workload, allowing physicians to focus more on patient care.
Benefit: More time for clinical services, less burnout from paperwork.
2. Improves Cash Flow and Reimbursement Rates
With correct coding, timely claim submission, and efficient denial management, physicians can ensure faster reimbursements and fewer rejected claims. Behavioral health RCM teams specialize in understanding payer nuances, ensuring clean claim rates are consistently high.
Benefit: Predictable revenue streams and better financial planning.
3. Ensures Regulatory Compliance
Behavioral health practices must stay updated with constantly changing billing codes (like CPT/HCPCS), state mandates, and payer-specific rules. Professional RCM services ensure compliance to avoid penalties and audits.
Benefit: Peace of mind and reduced legal risk for providers.
4. Enhances Patient Satisfaction
Efficient RCM improves billing transparency and ensures patients receive accurate statements. Automated reminders, co-pay collections, and insurance communication improve the patient financial experience.
Benefit: Happier patients and reduced billing disputes.
5. Scalable Growth Support
As behavioral health demand rises, practices need systems that scale. RCM providers offer technology and expertise to handle increased volumes without disrupting care delivery.
Benefit: Smooth expansion of services or locations without revenue bottlenecks.
Key Components of a Successful Behavioral Health RCM Strategy
To truly reap the benefits, physicians must ensure their RCM process includes:
a) Accurate Clinical Documentation
Proper documentation is the foundation of clean claims. Training clinicians to document thoroughly and consistently is key for reducing denials.
b) Specialized Coding for Behavioral Health
Behavioral health coding includes unique CPT codes, modifiers, and time-based billing rules. Certified coders familiar with the niche can make a significant difference.
c) Patient Eligibility and Authorization Checks
Automating eligibility verification ensures that services rendered are covered, reducing the chances of uncompensated care.
d) Claims Scrubbing and Denial Management
Using claims scrubbing software or experts to pre-check claims before submission boosts the first-pass acceptance rate. A dedicated denial management team can appeal and resolve rejections swiftly.
e) Robust Analytics and Reporting
Real-time dashboards and revenue cycle KPIs (like Days in AR, denial rate, and collection rate) help physicians make data-driven decisions and identify bottlenecks.
Should You Outsource Behavioral Health RCM?
For smaller practices or busy clinicians, outsourcing RCM to a specialized behavioral health billing company can be a game-changer. Outsourced partners bring:
Industry-certified coders
Real-time reporting
Scalable infrastructure
Ongoing compliance monitoring
This not only reduces internal staffing burdens but also improves collections and accuracy.
However, it’s important to choose a partner with proven experience in behavioral health revenue cycle management, not just general medical billing.
Technology’s Role in Behavioral Health RCM
Modern RCM solutions leverage AI, automation, and EHR integration to improve efficiency. Physicians benefit from:
Automated appointment reminders
Electronic claim submission and tracking
Patient portals for easier payment
Real-time coding suggestions
By integrating RCM with clinical workflows, technology enhances productivity and reduces revenue leakage.
Final Thoughts
In a field as critical and nuanced as behavioral health, revenue cycle management isn’t just a financial necessity it’s a strategic asset. For physicians, effective behavioral health RCM means more than getting paid on time. It translates into reduced stress, greater focus on patient outcomes, and sustainable practice growth.
As behavioral health services continue to grow in demand, practices that invest in specialized RCM systems or partners will be better equipped to serve patients while maintaining financial health.
0 notes
Text
Navigating Medical Debt and Your Credit Score: What Texas Residents Need to Know

Medical debt can disrupt your finances, lower your credit score, and leave you feeling powerless—especially in Texas, where unexpected hospital bills and billing errors are all too common. Understanding your rights and recent policy shifts is essential to regaining control of your financial health. In this blog, we explore the Consumer Financial Protection Bureau’s evolving stance on medical‑debt reporting and offer practical strategies to dispute or remove hospital bills from your credit report. Our goal is to guide you toward clear paths for effective credit repair.
CFPB’s Changing Position on Medical‑Debt Reporting
In early 2025, the CFPB introduced a rule to remove most medical debts from consumer credit reports, aiming to protect millions of Americans from unfair score damage. Soon after, legal challenges prompted the CFPB to reverse its position and seek to vacate the rule, creating uncertainty for consumers. As a Texas resident, staying informed about these developments is critical, since shifts in federal policy directly affect how medical debts impact your report.
Five Strategies to Dispute or Remove Hospital Bills in Texas
1. Verify and Itemize Your Charges
Start by requesting an itemized statement from your healthcare provider and compare it to your insurance Explanation of Benefits (EOB). Discrepancies in billing codes or duplicate charges are common. If you find errors, submit a written request for verification or correction before the debt moves to collections.
2. Explore Charity Care and Financial Assistance
Many Texas hospitals offer charity care programs or sliding‑scale payment options for low‑income patients. Hospitals that receive federal funds are required to publicize their assistance policies. Contact the billing department early to apply for discounts or deferments, which can eliminate or reduce your obligation before it appears on your credit report.
3. Dispute for quick credit repair
If an account has already been reported, file disputes with TransUnion, Experian, and Equifax within 30 days of seeing the entry. Clearly state that you are challenging the validity of the debt and provide copies of supporting documents, such as itemized bills and EOBs. Each bureau must investigate and remove unverifiable items, helping you achieve fast credit repair.
4. Escalate to the CFPB
If the credit bureaus or debt collectors do not resolve your disputes, submit a formal complaint to the CFPB. The bureau issues a response timeline and often accelerates corrections when a company’s practices are questioned publicly. This step adds extra pressure for compliance under federal consumer protection laws.
5. Leverage Texas‑Specific Consumer Resources
Utilize guides from the Texas State Law Library and TexasLawHelp.org, which provide templates for dispute letters and instructions on sending certified mail. These resources are tailored to Texas law and ensure you follow best practices when challenging inaccuracies on your credit report.
Taking Control of Your Financial Future
Facing medical debt can feel overwhelming, but you have the tools and rights to contest unfair practices. By verifying charges, seeking assistance programs, and aggressively disputing errors, you can prevent unjust hospital bills from damaging your credit. If disputes stall, escalation to the CFPB and use of Texas‑specific resources offer additional support. At 700 Plus Credit, we understand the challenges Texas residents face when dealing with medical collections and credit setbacks. Our team specializes in personalized strategies that remove erroneous debts, negotiate with providers, and optimize credit profiles. With our expert guidance, you can navigate medical debt disputes confidently and achieve lasting improvement. Let us partner with you on your journey to financial wellness and stronger credit through comprehensive credit repair solutions.
0 notes
Text

Ambulance Medical Billing Services | GetMax Healthcare Solutions
Managing medical billing for ambulance services requires precision, compliance, and expertise. At [Your Company Name], we specialize in providing comprehensive Ambulance Medical Billing Services designed to maximize reimbursement, ensure accuracy, and streamline your financial operations.
Why Choose Our Services?
Expertise in Ambulance Billing: Our team understands the complexities of ambulance billing codes, payer requirements, and regulatory compliance, ensuring claims are processed quickly and accurately.
Claim Denial Management: We actively address denials and rejections, reducing delays and improving cash flow.
Customized Solutions: Tailored billing strategies to fit your unique needs, whether for emergency transport or non-emergency medical services.
Advanced Technology: Utilizing cutting-edge billing software and analytics, we ensure efficiency and transparency in all processes.
HIPAA Compliance: Safeguarding patient data is our top priority, adhering to all privacy and security standards.
Our Services Include:
Verification of patient eligibility and benefits
Accurate coding of ambulance services
Submission of clean claims to payers
Appeals for denied claims
Detailed reporting and analytics
Benefits of Partnering with Us:
Increased revenue collection
Reduced operational burden on your staff
Improved claim acceptance rates
Transparent communication and real-time updates
Transform your ambulance billing process with GetMax Healthcare Solutions. Let us handle the complexities while you focus on delivering lifesaving care.
Contact us today to learn more! Phone: +91-867-891-0338 Email: [email protected]
0 notes
Text
Ace Your Medical Billing Certification Exam: Essential Tips & Insights to Boost Your Career
Ace Your Medical Billing Certification Exam: Essential Tips & Insights to boost Your Career
Embarking on a career in medical billing is a rewarding path that combines healthcare knowledge with administrative skills. Obtaining a reputable medical billing certification can significantly enhance your credibility, job prospects, adn earning potential. But, successfully passing the medical billing certification exam requires strategic readiness, a clear understanding of key concepts, and confidence in your abilities. In this extensive guide, we’ll share valuable tips, practical insights, and proven strategies to help you ace your exam and elevate your health data management career.
Understanding the Importance of Medical Billing Certification
A medical billing certification not only validates your expertise in medical billing and coding but also demonstrates your commitment to professional growth. Certifications like the certified Professional Biller (CPB) from the American Medical billing Association (AMBA) or Certified Medical Reimbursement Specialist (CMRS) from the National Healthcareer Association (NHA) are recognized industry standards that can differentiate you in a competitive job market.
Key benefits of earning a medical billing certification include:
Enhanced job opportunities and salary potential
Increased professional credibility
Better understanding of insurance processes, coding systems, and compliance regulations
Preparation for complex billing scenarios
Essential Tips to Prepare for Your Medical Billing Certification Exam
1. Understand the Exam Format and Content
Before diving into study materials, familiarize yourself with the exam structure and core topics. Most certification exams cover areas such as medical terminology, insurance claims, coding procedures, and regulatory guidelines.
Take advantage of official exam outlines provided by certification bodies like AMBA or NHA to pinpoint key areas to focus on.
2. Develop a Focused Study Plan
A structured study plan is crucial to cover all exam topics efficiently.Allocate time for each section based on your familiarity and difficulty level. Consistency beats last-minute cramming!
Sample Study Schedule:
Week 1-2: Medical Terminology and Anatomy
Week 3-4: Coding Procedures and Disease Classification
Week 5-6: insurance policies & Billing Software
Week 7: Practice exams and review
3. Use Quality Study Resources
Invest in reputable textbooks, online courses, and practice exams. Some trusted resources include:
Official certification preparation guides
Online practice tests
Educational webinars and tutorials
Joining study groups or forums can also provide support, shared insights, and motivation.
4. Master Medical Coding & Billing Software
Hands-on practice with popular billing software enhances your understanding of actual workflows. Many providers offer free trial versions or simulation tools for learners.
This experience not only prepares you for exam questions but also boosts your confidence in real-world scenarios.
5. Focus on Key Exam Strategies
Read each question carefully-attention to detail is vital.
Answer easier questions first to secure marks early on.
Manage your time effectively-allocate specific minutes to each section.
Watch out for qualifiers like “most likely,” “best match,” or “all of the above.”
Practical Tips & Common Pitfalls to Avoid
don’t ignore the fundamentals: A strong grasp of basic medical terminology and coding is essential.
Avoid reliance solely on memorization: Focus on understanding concepts rather than rote learning.
Stay updated on regulatory changes: follow updates from CMS, HIPAA, and other relevant bodies.
Take regular breaks: Prevent burnout and maintain focus during study sessions.
Practice timed exams: Mimic real exam conditions to build stamina and time management skills.
case Study: from novice to Certified Medical Biller
Consider Sarah’s story. A healthcare administrative assistant, Sarah decided to pursue a medical billing certification to advance her career. She followed a structured study plan, invested time in online tutorials, and practiced extensively with billing software. Within three months, she scored above the passing mark on her exam and secured a higher-paying billing specialist position. Her journey highlights how dedication, strategic preparation, and resourcefulness can lead to professional success.
Key Certification Programs & Their Requirements
Certification
Prerequisites
Exam Focus
Validity
CPB (Certified Professional Biller)
High school diploma or equivalent
Billing procedures, insurance, coding
2 years
CMRS (Certified Medical Reimbursement Specialist)
Medical background preferred
Reimbursement, compliance, coding
3 years
CCB (Certified Coding Biller)
Basic coding knowledge
Coding, billing, insurance rules
3 years
First-Hand Experience & Additional Insights
Many successful certified billers emphasize the importance of on-the-job experience. Internships or volunteer positions provide practical exposure and deepen your understanding of day-to-day operations. Also, staying current with industry trends through webinars, workshops, and professional associations keeps your skills sharp and relevant.
Conclusion: Your Path to Success in Medical Billing Certification
Passing your medical billing certification exam is a significant milestone that can open doors to rewarding career opportunities. By understanding the exam format, creating a detailed study plan, utilizing quality resources, and practicing diligently, you increase your chances of success. Remember,preparation,perseverance,and practical experience are your best allies in achieving certification and boosting your healthcare career.
Stay motivated, keep learning, and aim high-your certified future as a skilled medical billing professional awaits!
https://medicalcodingandbillingclasses.net/ace-your-medical-billing-certification-exam-essential-tips-insights-to-boost-your-career/
0 notes
Text
Top Medical Billing Companies in NJ: Your Guide to Streamlined Healthcare Revenue Management
Top Medical Billing Companies in NJ: Your Guide to Streamlined healthcare Revenue Management
In the rapidly evolving healthcare landscape of New Jersey, managing medical billing efficiently is crucial for ensuring steady revenue flow and compliance. Healthcare providers-from small clinics to large hospitals-must navigate complex insurance policies, coding standards, and billing regulations.Partnering with a top medical billing company in NJ can transform your revenue cycle, reduce administrative burdens, and improve cash flow.
Understanding the Importance of Medical Billing Services in NJ
Medical billing is more than just submitting claims; it’s a comprehensive process that involves coding, bill submission, payment follow-up, and compliance management. Effective medical billing services streamline this process, minimize errors, and maximize reimbursement rates.In new Jersey,where healthcare demand is high and regulations are stringent,choosing the right billing partner is essential.
What to Look for in the Best Medical Billing Companies in NJ
Experience and Industry Reputation: Look for companies with a proven track record in NJ.
Comprehensive Services: Ensure they handle coding, claims submission, denial management, and reporting.
Technology and Security: Use of advanced billing software ensuring HIPAA compliance and data security.
Customized Solutions: Tailored billing strategies to fit your practice size and specialty.
Transparent Pricing: Clear,upfront billing service costs without hidden fees.
Top Medical Billing Companies in New Jersey
Based on industry reputation, client reviews, service offerings, and technological capabilities, here are some of the leading medical billing companies serving healthcare providers in NJ:
Company Name
Specialties
Key Features
Average Client Satisfaction
Elite Medical Billing NJ
Primary Care, specialty Clinics
End-to-end billing, denial management, real-time analytics
4.8/5
Precision Revenue Solutions
Physicians,Hospitals
Advanced AI-driven coding,compliance assurance
4.7/5
NJ Billing experts
Urgent Care, Surgical Practices
Dedicated account managers, transparent pricing
4.6/5
Healthcare Revenue Partners
Specialty practices, Multi-specialty clinics
Custom solutions, comprehensive reporting
4.8/5
BrightBilling NJ
Pediatric, Family Medicine
Cloud-based platform, customer support
4.5/5
Benefits of Hiring a Top Medical Billing Company in NJ
Maximized Revenue and Faster Payments
Professional billing companies optimize claim submission and follow-up processes, leading to quicker reimbursements and reduced outstanding payments.
reduced Administrative Burden
Delegating billing tasks frees up your staff, allowing focus on patient care and practice growth.
Enhanced Compliance and Reduced Errors
Expert billing services stay updated with NJ and federal regulations, reducing the risk of audits and penalties.
Access to Advanced Technology
Most top billing companies use state-of-the-art software for reporting, analytics, and secure data management.
Practical Tips for Choosing the Right Medical Billing Partner in NJ
Assess your Practice Needs: Determine your volume, specialties, and specific requirements.
Check References and Reviews: Ask for client testimonials and review case studies.
Verify Technology Compatibility: Ensure their software integrates with your EHR system.
Understand Pricing Models: Clarify billing fees-percentage-based, flat rate, or hybrid models.
Evaluate Customer Support: Responsive and informed support team is essential.
Case Study: How Precision Revenue Solutions Transformed a NJ Clinic’s Billing Process
Dr. Smith’s dermatology practice in Newark faced frequent claim denials and delayed payments. Partnering with Precision Revenue Solutions revolutionized their revenue cycle. Through the implementation of AI-driven coding and intensive denial management,Dr. Smith’s practice saw a 30% increase in collections within the first six months. The clinic appreciated real-time dashboards and dedicated support, highlighting the value of choosing the right billing partner in NJ.
First-Hand Experience: Why NJ Healthcare Providers Trust These Companies
Many healthcare providers in New Jersey testify to the importance of a reliable medical billing partner. An effective billing company doesn’t just improve profitability; it enhances operational efficiency and allows providers to focus on delivering quality patient care. Trust is built through openness, expertise, and cutting-edge technology.
Conclusion
Choosing the top medical billing company in NJ is a strategic decision that can significantly impact your healthcare practice’s financial health. The right partner will streamline your revenue cycle, ensure compliance, and maximize your reimbursements, ultimately allowing you to focus on what you do best-caring for your patients. With the comprehensive insights provided in this guide, you are better equipped to select a billing service that aligns with your practice’s unique needs and goals.
investing in expert medical billing services in New Jersey is a smart move toward a more efficient, profitable, and compliant healthcare operation. Take the time to evaluate your options and partner with a reputable NJ-based billing company for a future of steady growth and exceptional patient service.
https://medicalbillingcertificationprograms.org/top-medical-billing-companies-in-nj-your-guide-to-streamlined-healthcare-revenue-management/
0 notes
Text
Top Medical Billing Practices to Boost Revenue & Ensure Compliance in Healthcare
Top Medical Billing Practices to Boost Revenue & Ensure Compliance in Healthcare
Introduction
in the ever-evolving landscape of healthcare, a robust medical billing process is vital for ensuring financial stability, maximizing revenue, and maintaining regulatory compliance. Proper medical billing practices not only streamline cash flow but also help avoid costly audits and penalties. Whether you’re a healthcare provider, billing specialist, or practise manager, understanding the top strategies for effective medical billing is essential. This comprehensive guide explores proven practices, practical tips, benefits, real-world case studies, and expert insights to help you optimize your billing workflow and achieve enduring growth.
why Effective Medical Billing Practices Matter
Efficient medical billing is the backbone of a profitable healthcare practice. It directly impacts revenue cycle management,patient satisfaction,and compliance with federal and state regulations. Poor billing practices can result in delayed payments, denied claims, revenue loss, and legal complications. Thus, adopting best practices is crucial for fiscal health and operational excellence.
Key Medical billing Practices to Boost Revenue & Ensure Compliance
1. Accurate Data Entry & Documentation
One of the most foundational aspects of successful medical billing is ensuring accuracy in patient data and documentation. Mistakes in demographic info, insurance details, or clinical documentation can lead to claim rejections.
Double-check patient information during registration
Ensure thorough and precise clinical documentation
use integrated electronic health records (EHR) systems for automatic data syncing
2. Staying Updated with Coding & Regulations
Medical coding standards-such as ICD-10, CPT, and HCPCS-stand at the core of insurance reimbursements. Outdated or incorrect codes can cause claim denials or audits.
Regularly train billing staff on coding updates
Utilize coding software with built-in guidelines
stay informed about healthcare billing regulations like HIPAA and Medicare policies
3. Robust Claim Submission & Follow-up Process
Automating claim submission and implementing diligent follow-up procedures enhance the chances of timely reimbursement. Use electronic claim submission (EDI) systems to reduce errors and accelerate processing.
Step
Action
Benefits
1
Automatic claim submission via EHR
Faster processing
2
Regular claim status review
Early detection of issues
3
Prompt appeal of denied claims
Increased revenue recovery
4. Effective Denial Management
Handling claim denials proactively can save considerable revenue and prevent cash flow disruptions.Establish a denial management team ��or process for rapid resolution.
Analyze denial reasons systematically
Correct errors promptly and resubmit claims
Implement denial tracking tools for continuous enhancement
5. Regular Staff Training & Education
Healthcare billing regulations and coding standards evolve frequently. Continuous education ensures your team remains compliant and efficient.
Schedule quarterly training sessions
Leverage online courses and certifications
Promote a culture of compliance and accuracy
6. Integrate Revenue cycle Management (RCM) Technology
Investing in comprehensive RCM software can automate many billing tasks, from patient registration to collections. This integration leads to reduced errors and faster reimbursements.
Popular tools include:
Automated claim scrubbing
Real-time eligibility verification
Advanced analytics dashboards
Benefits of Implementing Top Medical Billing Practices
Benefit
Description
Increased Revenue
Faster and accurate reimbursements boost your practice’s cash flow.
Improved Compliance
Minimize legal risks by adhering to regulations and standards.
Reduced Claim Denials
Efficient processes lead to fewer rejected claims, saving time and resources.
Enhanced Patient Satisfaction
Clear billing processes and obvious interaction improve patient trust.
Operational Efficiency
Automation and staff training streamline workflows for better productivity.
Practical Tips for Optimizing Your Medical Billing Process
Use Technology: Invest in reliable billing and practice management software that integrates with EHR systems.
Monitor KPIs: Track metrics such as days in accounts receivable, claim rejection rate, and denial reasons for continuous improvement.
Establish Clear policies: Develop standardized procedures for billing,denials,and collections to ensure consistency.
Maintain Open Communication: Foster collaboration between clinical, administrative, and billing teams for seamless workflows.
Perform Regular Audits: Conduct periodic audits to identify vulnerabilities and rectify inconsistencies early.
Case Study: Transforming Billing Efficiency at HealthyCare Clinic
Background: HealthyCare Clinic faced recurring claim rejections and delayed reimbursements, impacting their revenue cycle. They decided to overhaul their billing practices.
Approach: By implementing automated billing software, retraining staff, and establishing a denial management team, HealthyCare substantially enhanced their billing operations.
Aspect
Before
After
Claim Rejection Rate
15%
4%
Average Days in Accounts Receivable
45 days
25 days
Revenue Growth
Flat
15% increase annually
Result: Streamlined billing led to faster collections, fewer rejected claims, and increased revenue-highlighting the power of adopting top medical billing practices.
First-Hand Experience: My Recommendations
Having worked with various healthcare providers, I recommend prioritizing technological integration and staff training. Align billing practices with evolving regulations to stay compliant and optimize revenue. Consistent review and improvement ensure your practice remains resilient against common billing pitfalls.
Conclusion
Implementing top medical billing practices is key to boosting revenue,ensuring compliance,and fostering a smooth healthcare operation. From accurate documentation and staying current with coding standards to leveraging automation and continuous staff education, these strategies can transform your billing process into a powerful tool for growth.Remember, proactive denial management and regular audits are essential for maintaining financial health. By adopting these proven practices, healthcare providers can achieve operational excellence, enhance patient satisfaction, and secure long-term success.
Ready to revolutionize your medical billing? Contact us today for expert guidance and tailored solutions to maximize your healthcare practice’s revenue and compliance!
https://medicalbillingcodingcourses.net/top-medical-billing-practices-to-boost-revenue-ensure-compliance-in-healthcare/
0 notes