#and us getting used to a new baseline so the symptoms we were previously used to feel worse and more alarming now
Text
our mum's boyfriend has been telling her to avoid going to a doctor about her asthma symptoms for as long as possible because "once you start on an inhaler it's really hard to stop taking it again because you can't breathe when you stop taking it" and like??? yeah no shit, if you stop taking the meds that help you breathe you're gonna start struggling to breathe
#personal#thoughts#🍬 post#vent post#see the thing is I know before we got diagnosed we thought our breathing wasn't too bad#other than that we got out of breath really easily and regularly noticed a whistling noise when we breathed#and now if we stop taking our inhaler we very quickly start struggling to breathe and it's very obvious that something's wrong#as in we ran out of meds twice and couldn't get more when we needed to and almost had to call an ambulance#and I can see why that would look like ''oh so now your breathing is worse when you don't take the meds than before you started them''#but no it's a combination of us not realising how bad our symptoms were until we experienced them not being that bad#and us getting used to a new baseline so the symptoms we were previously used to feel worse and more alarming now#and like... if we stop taking the maintenance meds suddenly it makes sense that our body's gonna flip its shit and have a bad time#and we're gonna get an especially bad flare up of symptoms#but the thing about putting off getting diagnosed and getting treatment#is that the longer you go without getting treatment the more your lungs are gonna get fucked up and you risk permanent damage from that#it's called airway remodelling and it can fuck up your lungs pretty badly
8 notes
·
View notes
Text
Emotional Abuse and ADHD
Ok, first real post on the ADHD sideblog, so lets dive straight into the heavy stuff. TW/CW for emotional abuse, gaslighting, and probably some other things too (please feel free to let me know if I should add additional tags).
I had trouble sleeping last night because my brain kept insisting I needed to start this blog, like immediately, despite it being clearly not an opportune time to do anything of the sort. Or at least, it insisted, I needed to jot down all the essay/ramble/whatever topic ideas I had complicated thoughts on so I could start the blog today. I managed to resist doing both of those things, and get to sleep eventually, but here I am. The first topic that brought this on was wanting to talk about my experience in an emotionally abusive relationship and how many aspects of that were exacerbated by various symptoms of my (then undiagnosed) ADHD.
I’m going to assume a certain amount of baseline familiarity with some terminology and whatnot here, if you’re confused by any of the ADHD terms I use here I recommend heading over to theadhdmanual.com and reading their very helpful “three pillars” articles which do a great job of explaining Rejection Sensitive Dysphoria (RSD) and emotional hyperarrousal (also elsewhere called emotional disregulation, I’ll be using both terms interchangably but won’t be abbreviating the latter for hopefully obvious reasons). On the emotional abuse terminology front, there’s a couple great articles on gaslighting on everydayfeminism.com that I recommend seeking out.
It is possible I am slightly stalling here by providing all this context.
At this point damn near ten years ago, for most of my senior year of college and for a good few months afterwards (I don’t remember how long exactly since adhd brains suck at timelines and I don’t feel like logicing it out right now) I was in what I later realized (with help from the aforementioned everydayfeminism articles) was an emotionally abusive relationship. My then-boyfriend, who I will call Al, was insecure and jealous. I had more sexual experience than him going into the relationship, and he used that as an excuse to guilt-trip, manipulate, and ultimately control me. I realize now, that the primary weapon he would use against me was my own RSD.
Whenever I did something that upset Al, (typical infractions included things like accidentally mentioning one of my exes, correcting him about something, “flirting with” --read: talking to-- any of my friends who were more my friend than his, or singing along to music) he would generally make his displeasure known by ignoring me--withdrawing all physical affection, coupled with the silent treatment. If you’re familiar with RSD, you can already guess how effective this was. If you’re not, then for comparison you should know that ADHD people can spiral very quickly into completely irrational “they hate me, don’t they?” thought spiral from something as small as a delayed text. Al would almost never tell me what I did to upset him, and in my guilt-spiral I would usually tearfully beg forgiveness for everything I could think of until I guessed correctly and/or he arbitrarily decided I’d had enough.
As an aside, he would often do this silent treatment toward me in public while being perfectly cheerful and whatnot with our other friends, often making it seem to others like he was just joking or messing with me. On one memorable occasion he refused to say anything to me but the word “spoon” with varying inflections for the better part of a day--a pretty skillful gaslight because to everyone else around this just seemed like goofy ol’ Al being his silly self, but from context I knew this was part of a punishment, and I couldn’t express any kind of being upset about this, even annoyance, without looking like I was overreacting to a dumb joke.
Ultimately much of what he actually did (or didn’t do) in public didn’t look like much to an outside observer, but he knew my (RSD fueled) insecurity would make it hurt, especially when I wouldn’t be able to address anything with him until we were in private later.
Also (and I intend to write a whole different post about this later) my particular brand of emotional disregulation takes the form of crying extremely easily. I cry when I’m sad, when I’m tired, when I’m happy, when I see something too cute to handle, and (most importantly, in this instance) when I’m angry. Because of this, every time I tried to address some relationship concern I had with him, whenever I tried to call out some of his shitty behavior or bring attention to my own emotional needs, it was extremely difficult--nigh impossible--to do so without crying. This gave him a massive amount of gaslighting ammunition--it made it very easy for him to say I was overreacting, overemotional, irrational, trying to manipulate him, et cetera. And it was hard to defend myself against that, even to myself. After all, lacking the ADHD diagnosis and resources about emotional disregulation that I have now, I had pretty much internalized the idea that I’m just “oversensitive” when it comes to crying, so I rationalized that I was also being oversensitive about whatever concern I started with in the first place. So every time a conversation started with me telling him he hurt me some way, it inevitably ended with me apologizing to him instead of the other way around.
Just to add to the already nasty cycle, Al also considered crying over something he didn’t deem worth crying over a punishable offense, so it often triggered the previously discussed silent treatment.
A third aspect of ADHD I haven’t discussed yet also played a major part in how I was abused--Memory. I don’t have a good resource to link on this one (I’m pretty sure there are some good howtoadhd videos on it on youtube but I’m not going to go dig for them right now), but ADHD people, on the whole, have terrible memories, especially short term/working memory. Mine in particular might be even worse for some kinds of things for unrelated reasons (aphantasia, which I might write about later but this is already really long and it’s not actually that relevant here).
Al was perpetually convinced that I was cheating on him, and any time we were apart he would quiz me afterwards on where exactly I was, what I did, for how long, and in what order. Any inconsistency in my account, or any “I don’t remember”s would mean he would accuse me of lying about the whole thing. I am pretty sure I have in common with most ADHD people that between time blindness and bad working memories, giving a consistent and accurate account like that is basically impossible, so this rarely went well for me. Just to further complicate matters, being accused of lying when I’m not is practically guaranteed to make me cry, and trying to keep from crying (to avoid angering him further) means I swallow a lot, and somewhere Al had heard that excessive swallowing is a sign that someone is lying, so again these various ADHD symptoms would combine to just make everything worse.
I eventually got out of that relationship, and not too long afterwards got together with my now-husband, who is wonderful, so that’s a happy ending. Getting diagnosed with ADHD a few months ago, learning about these symptoms, and figuring all this out has made this make much more sense to me than before. But in addition to my ADHD symptoms making me more vulnerable to these emotional abuse tactics, I’m pretty sure the leftover baggage from the emotional abuse may have made those very same ADHD symptoms worse, and while my new meds seem to help immensely with the executive disfunction aspects of ADHD, they don’t do a damn thing about RSD spirals or emotional disregulation. Healing and processing it all is slow going, but it has gotten a lot better over the years, and knowing now that even another aspect of this isn’t my fault helps too. And taking my meds today did help me motivate myself to write all this out, so maybe that will help as well.
I’m not sure what the takeaway is here, other than I strongly suggest everyone learn what gaslighting and emotional abuse in general looks like, but especially if you have ADHD or suspect you might have ADHD because we might be more vulnerable to being on the receiving end of it than most people. If anything I talked about here sounds a little too familiar, I strongly recommend reading up on gaslighting, and consider getting the heck away from anyone who sounds too much like Al. Maybe us ADHDers will inevitably get into some nasty thought-spirals or bad emotional places sometimes, maybe we’ll cry over nothing or worry too much that something we said will make everyone hate us, but if anyone tries to use any of that against you, uses it to get you to do what they want, or intentionally makes you feel worse, they’re not someone worth being around, and I promise you deserve better.
Not sure if anyone will read this, much less any fellow ADHDers because yeah, it’s a big ol’ wall of text and I get that can be hard, but if you made it this far, thanks for listening and I’ll try to go not quite so heavy with my next post, (assuming, of course, that I have a next post and this blog doesn’t become yet another started-and-abandoned project).
That’s all for now.
#adhd#actuallyadhd#rsd problems#emotional abuse#tw emotional abuse#tw emotional manipulation#gaslighting#tw gaslighting
6 notes
·
View notes
Text
on origins [part ii]
december 1981
moscow
a week later
[npc faceclaims used: sophia lillis, ryan hurst, anthony stewart head]
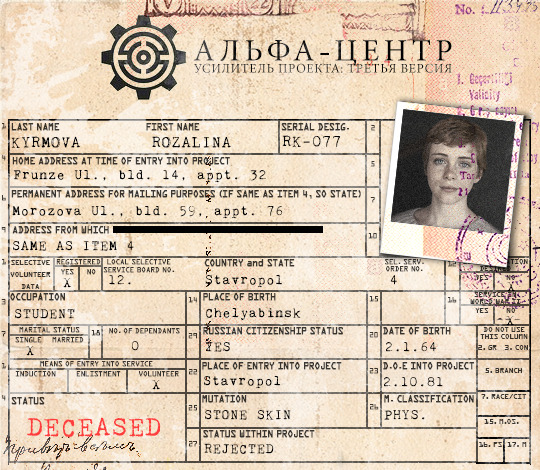
Rozalina’s in the middle of telling a knock knock joke when Kazimir gives her the injection.
“Who’s there?” he replies dutifully, distracted.
“Interrupting sloth,” she prompts, swinging her legs back and forth where they hang over the edge of the examination table she’s sitting on. She can’t help the grin that’s creeping over her lips, anticipation of the joke she’s about to tell.
Kazimir withdraws the needle, swabs over the site of injection with a cotton ball, sighs, and asks, “Interrupting sloth wh--”
He doesn’t get to finish, because Rozalina’s raising her arm -- slowly, so slowly, like she’s reaching toward a doorbell but doomed to never get there in time. Kazimir blinks, takes a second to get the joke, and snorts an unwilling laugh. “Terrible,” he concludes.
“Pfft. Made you laugh, it can’t have been that bad.” Rozalina chortles, glancing down at her arm. “So, let’s get this shit going. What do I do?”
“Just try to change your skin as you normally would,” Kazimir directs. “I theorize that amplifying this ability will allow you to turn your entire body to stone; muscle, bone and all, which should greatly increase your strength and defense. Bear in mind, it will also greatly increase your weight, so... if you could hop off the table before we begin, that’d be much appreciated. Thank you.”
She does, tossing Kazimir a jaunty salute and a wink.
CAUSE OF DEATH: Auto-decapitation
SUMMARY: Subject received serum, and was given time to adjust. When the subject initiated her ability, the change started at the crown of her head, with her hair turning to stone. Subject paused change to remark upon how cool that was, as that had never happened before.
Subject’s stone transformation was descending, and stopped suddenly when it reached her eyes. Subject’s stone cranium -- from crown to cheekbone -- separated from the rest of her body.
Autopsy concluded that the serum had amplified the subject’s ability so thoroughly that it allowed her to turn her brain to stone, but as the material is not conductive, it was no longer able to function neurologically. At the moment of the subject’s death, her mutation’s ability to hold cohesive tension between stone and skin cells during transformation was lost, resulting in auto-decapitation due to weight of the cranium.
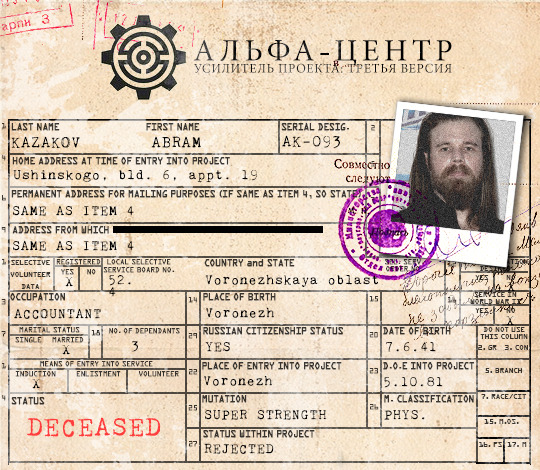
“So, how much stronger am I gonna get, Doc?”
Abram is unaware of the horror that had happened in this very room not six hours ago. The lab cleaners were efficient, methodical, but Kazimir can still see a fleck of blood on the concrete floor. Nobody else would see it -- one has to know where to look.
Numbness has begun to set in. Theorizing that one may be the cause of death is very different from witnessing it, and all Kazimir can do is picture his children. Annika’s dimpled smile and blonde curls, Katina’s serious dark eyes and studious frown. Chebrikov is not a man to make idle threats.
“At least twice your current levels, though we’re hoping for five times that,” Kazimir finally answers, busying himself with readying the serum.
“Five times?” Abram blinks, astonished. “Shit, Doc, I can already lift a car over my head. What the hell am I gonna be able to lift up after the serum?”
Kazimir flicks the side of the hypodermic. “Mother Russia, Abram. If this works, you will be able to hold all of us on your shoulders.”
CAUSE OF DEATH: Severe auto-immune response
SUMMARY: Subject’s initial injection was routine. After a small adjustment period, the subject was taken to the gym room of the Alpha Centre facility, to test his new strength capacity. Subject reported ease in lifting twice his previous baseline.
While working up to heavier weights, subject started to report slight shortness of breath, but pressed on. Other symptoms were reported over the next ten minutes: fever, increasing trouble breathing, lethargy, muscle ache. Half an hour later, subject collapsed, and was transported to the medical wing to be placed on a ventilator, but died shortly after.
Scans of the subject’s lungs reveal severe inflammation scarring not previously seen. Autopsy concluded that a severe and sudden onset of an auto-immune response was to blame: it seems the serum made everything about him stronger, including his immune system, which kicked into overdrive and started attacking itself.
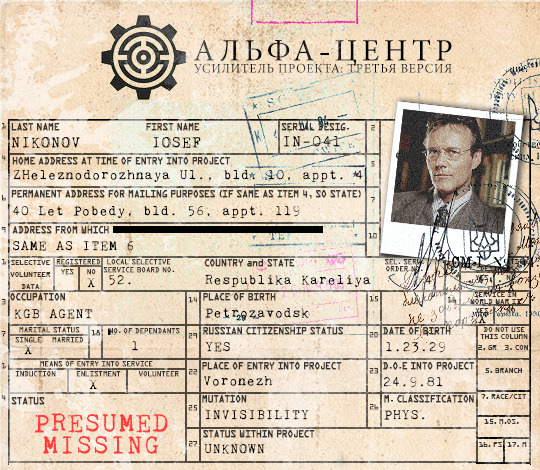
Iosef knows something is wrong.
He seems to be able to tell the moment he walks into the room -- his sharp gaze rakes over Kazimir’s slumped shoulders, and the way he is studiously avoiding walking over a particular spot of the lab floor.
“I’m number three, yes? Let me guess. The first two attempts were failures,” Iosef drawls. He doesn’t look concerned.
“I-- yes,” Kazimir admits. There’s no point lying. Iosef is KGB, though god knows why he’s here in this project. Is this a punishment for him? Did he volunteer?
Iosef strolls over to the examination table, already rolling up one of his shirt sleeves. “And you’re going to tell me that you don’t want to test this serum on me, because you’re fairly certain it will kill me,” he continues, downright mild, “but that you have no choice, because Chebrikov has something on you, something you value much more than a stranger’s life. You don’t want to, but you will. Because you’re that sort of man, Doctor.”
Kazimir’s heart cannot possibly plunge any further, cannot possibly feel any heavier. Because Iosef is right; he hates this, he hates knowing that he’s about to kill yet another fellow mutant.
But he loves his children more.
“I’m sorry,” he tries.
“Yes. I’m sure you are.” Iosef’s voice is almost gentle, but his predator’s eyes take any softness out of his words. “But that doesn’t help anybody, does it?”
STATUS: Presumed missing
SUMMARY: Subject had no issues with initial injection. Upon being prompted to test his ability, subject turned invisible.
Subject did not answer questions. Subject did not respond when asked to reveal himself again. Subject was clearly not in the same place he was when he turned invisible, verified by the Dr. attempting to find him by physical contact. A similar search of the rest of the room yielded the same result.
Both doors to the room were shut and locked as a precaution, pre-injection. Subject was unable to be located.
#[ FLASHBACK ]#tw: gore#i lied when i said it would be three parts#this got so long it'll have to be four#WHOOPS
1 note
·
View note
Text
two articles on psychiatric medication
I'm planning on writing a bigger psychiatry-critical piece soon about how the overwhelming majority of both leftists and trans people that I know believe themselves to be necessarily reliant on either psychiatric medication or therapy or both, and permit themselves (rather, semi-deliberately evacuate themselves of agency in identification with those harming them, I do not wish to victim blame) to be extensively abused by the psychological-psychiatric medical system in a fruitless search of validation for their malaise in some horrible cycle of iatrogenic dependence.
In particular, I know at least two transgender people personally (one male, one female) who are so heavily medicated that I have few compunctions about calling what is being done to them a kind of chemical lobotomy. They have both been left minimally functional and dramatically changed in personality by their "treatments", but both still seek out psychiatry to endorse their transgender interpretation of themselves, despite the fact their doctors are brutally and with little humanity "re-adjusting" them out of inconvenient behavior through repeated hospitalization, high and probably inappropriate doses of lithium alongside multiple other medications, and of course their whole gender treatment paradigm.
So I am continually startled by not only the distinct lack of modern leftist criticism of psychiatric medical institutions but outright collaboration with these institutions. Many people in the broader community-- whether radical queers or lesbian feminists-- purport to value self-reliance and peer support networks, distrusting well-funded and politically undermining officially-sanctioned institutions, but I am not sure I know a single gay person in my everyday life who is not regularly attending counseling sessions of some variety or another or who is not taking psychiatric medications-- prescribed by a psychiatrist that they see monthly or sooner-- that they believe they cannot live without.
One of the reasons I am so critical is that I was once one of these people: I have been on at least fourteen different psychiatric medications in various combinations throughout my life, and both I and many of my doctors believed that I was so critically ill that I could not live a meaningful or even minimally functional life without them. I, or my depression-- we were coextensive, inseparable, my personhood was inconvenient to assessment, I suppose-- was considered so deeply treatment resistant that I had multiple psychiatrists tell me to my face that it might not be possible to help me (of course, while still holding the prescription pad). I was lucky to never have been on lithium or Lamictal, nor subjected to electroshock, but all were floated as an unfortunate but potentially necessary part of my treatment plan. I was indeed considered such a hopeless case that I was actually approved for disability payments for mental illness, without appeal, an extreme rarity in the United States, especially at such a young age (23). I do not know for sure or not whether I could have set the grounds to get my shit together without the intervention of psychiatry-- I did survive long enough to leave an abusive home, after all-- but I do not consider it a coincidence that I did not get my shit together until I stopped having a therapist whispering in my ear and stopped having these substances in my body.
I don't think you can understand the modern transgender movement-- whether the push to identify various gender-distressed people as having a disorder or just niche lifestyle in need of medicalized affirmation, or the ideology that demands we believe that gender identity is an essential characteristic of human beings-- without understanding the history of psychiatry as a coercive practice attempting to normalize the socially abnormal, often in service to extremely oppressive interests, and the history of therapy as inherently individualizing and anti-political, an authority-laden substitute for discernment and appropriate and healthy social feedback.
In any case, I want to keep it short today, and it's with this context I want to share with you two articles, one from the New Yorker and the other from NPR.
The first article, by the amazing writer Rachel Aviv, who has previously covered dense and thorny ethical issues regarding psychiatric treatment and the construction of mental illness, is a critical article about how many modern psychiatric patients come to take consecutive strings of multiple psychiatric medications, coming to have and then losing faith in their doctors and medications to fix their ills. It follows a woman who decided to withdraw from her medications and the people she meets as she must build her own support network during her process of withdrawal, given her unhealthy dependence on the psychiatric network treating her and the psychiatric industry's public denial that medication discontinuation symptoms even occur, nonetheless can have severe and life-disrupting effects. Aviv gives a contextual history and science of the use of several classes of modern psychiatric medications, including their incredible limitations given psychiatry's practice and value system; in a description that will read eerily familiar to any detransitioned woman, she states that "there are almost no studies on how or when to go off psychiatric medications, a situation that has created what he [Allen Frances, chair of the DSM-4 committee] calls a 'national public-health experiment.'"
An important excerpt relevant to both general psychiatry and the practice of transgender medicine and health care:
A decade after the invention of antidepressants, randomized clinical studies emerged as the most trusted form of medical knowledge, supplanting the authority of individual case studies. By necessity, clinical studies cannot capture fluctuations in mood that may be meaningful to the patient but do not fit into the study’s categories. This methodology has led to a far more reliable body of evidence, but it also subtly changed our conception of mental health, which has become synonymous with the absence of symptoms, rather than with a return to a patient’s baseline of functioning, her mood or personality before and between episodes of illness. “Once you abandon the idea of the personal baseline, it becomes possible to think of emotional suffering as relapse—instead of something to be expected from an individual’s way of being in the world,” Deshauer told me. For adolescents who go on medications when they are still trying to define themselves, they may never know if they have a baseline, or what it is. “It’s not so much a question of Does the technology deliver?” Deshauer said. “It’s a question of What are we asking of it?”
The second article, which also contains a longer-form audio interview with the author, is about a new book by Harvard historian of science Anne Harrington called Mind Fixers: Psychiatry's Troubled Search for the Biology of Mental Illness. What I found particularly striking about her interview is Harrington's assertions about the state of psychiatry and psychiatric pharmaceutical research now-- she claims that the psychiatric medication market has stalled because of research finding that many common antidepressant medications work no better than placebo versions, and that pharmaceutical companies therefore are de-investing from psychiatric medication research and development because they can no longer use their previous strategy of slightly tweaking the chemical components of previously monetizeable drugs. She states there have been very few innovations in finding new classes of antidepressant medications in particular (the most easily marketed psychiatric drugs, for whom the target population can easily be expanded).
I think her points here are crucial to understanding exactly why pharmaceutical companies and psychiatry have become increasingly invested in transgender health care and in expanding the market for hormones and transgender-related surgeries through promoting interventions like HRT and "top surgery" as elective procedures suggested as ways to "affirm a patient's identity" rather than "treat a disorder". The gender critical blogger Brie Jontry, a mother of a formerly trans-identified female teen, calls this practice and ideology "identity medicine", a term I find useful to describe the unholy conglomeration that is the individualized medicalization of gender-related distress and the advertising of medical treatments (particularly those provided by cosmetic surgeons) as ways to facilitate self-expression and authenticity.
Given increasing attempts by gender doctors to create patients permanently dependent on exogenous hormones (those children left with non-functional gonads after treatment with GnRH agonists like Lupron and cross-sex hormones, or those transgender people who have had theirs removed) or to convince patients that gender dysphoria is a life-long, inescapable condition that they had already failed in not treating/affirming earlier (because you Always Were A Boy), I have to note parallels with psychiatric medicine's anti-recovery, anti-patient-autonomy assertions about other recently marketed drugs such as atypical antipsychotics, on which patients are also purportedly permanently dependent, or antidepressants (as above) where withdrawal symptoms purportedly prove that a patient is doomed to relapse should she cease psychiatric treatment. "Informed consent" and the formation of transgender resources outside a "gatekeeping" paradigm, where patients need not seek insurance approval nor the opinions of several doctors of different specialties for transgender medical interventions, nor wait a set period of time prior to transitioning, is often lauded as progressive and anti-institution by radical transgender activists, who can rightly see issue with a psychiatry put in charge of policing the intimate personal beliefs, coping mechanisms for misogyny or homophobia, and individual gender expression of its patients.
However, I can't but see this as part of a new and terrifying medical strategy regarding transgenderism, where a loss of patient agency is replaced with the false sense of consumer choice; we have seen this in other realms of psychiatry, where forms of psychiatric incarceration were rebranded as the choice to take a break or "finally" seek help after self-negatingly denying it for so long, where tranquilizing drugs were rebranded as assistive devices for women struggling to have it all, and where high-risk, heavily sedating antipsychotic medications were rebranded as ways to give other psychiatric medications a "boost" should you still experience unhelpful emotions after complying with psychiatric treatment. "Gender dysphoria" is increasingly nebulous, something you might have had all along if you experienced various forms of generic malaise or failed to have your suffering sufficiently validated and thereby dissipated by psychiatry; funny that we've seen this before with other conditions and their treatments, and psychiatry somehow always comes up with a money-making solution for its own problems.
74 notes
·
View notes
Text
Why Doctors Keep Monitoring Kids Who Recover From Mysterious COVID-Linked Illness
Israel Shippy doesn’t remember much about having COVID-19 — or the unusual auto-immune disease it triggered — other than being groggy and uncomfortable for a bunch of days. He’s a 5-year-old, and would much rather talk about cartoons, or the ideas for inventions that constantly pop into his head.
“Hold your horses, I think I know what I’m gonna make,” he said, holding up a finger in the middle of a conversation. “I’m gonna make something that lights up and attaches to things with glue, so if you don’t have a flashlight, you can just use it!”
In New York, at least 237 kids, including Israel, appear to have Multisystem Inflammatory Syndrome in Children, or MIS-C. And state officials continue to track the syndrome, but the Centers for Disease Control and Prevention did not respond to repeated requests for information on how many children nationwide have been diagnosed so far with MIS-C.
A study published June 29 in the New England Journal of Medicine reported on 186 patients in 26 states who had been diagnosed with MIS-C. A researcher writing in the same issue added reports from other countries, finding that about 1,000 children worldwide have been diagnosed with MIS-C.
Tracking the Long-Term Health Effects of MIS-C
Israel is friendly and energetic, but he’s also really good at sitting still. During a recent checkup at Children’s Hospital at Montefiore, in the Bronx, he had no complaints about all the stickers and wires a health aide attached to him for an EKG. And when Dr. Marc Foca, an infectious disease specialist, came by to listen to his heart and lungs, and prod his abdomen, Israel barely seemed to notice.
There were still some tests pending, but overall, Foca said, “Israel looks like a totally healthy 5-year-old.”
“Stay safe!” Israel called out, as Foca left. It’s his new signoff, instead of goodbye. His mother, Janelle Moholland, explained Israel came up with it himself.
And she’s also hoping that after a harrowing couple of weeks in early May, Israel himself will “stay safe.”
That’s why they’ve been returning to Montefiore for the periodic checkups, even though Israel seems to have recovered fully from both COVID-19 and MIS-C.
MIS-C is relatively rare, and it apparently responds well to treatment, but it is new enough — and mysterious enough — that doctors here want to make sure the children who recover don’t experience any related health complications in the future.
“We’ve seen these kids get really sick, and get better and recover and go home, yet we don’t know what the long-term outcomes are,” said Dr. Nadine Choueiter, a pediatric cardiologist at Montefiore. “So that’s why we will be seeing them.”
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
When Israel first got sick at the end of April, his illness didn’t exactly look like COVID-19. He had persistent high fevers, with his temperature reaching 104 degrees — but no problems breathing. He wasn’t eating. He was barely drinking. He wasn’t using the bathroom. He had abdominal pains. His eyes were red.
They went to the emergency room a couple of times and visited an urgent care center, but the doctors sent them home without testing him for the coronavirus. Moholland, 29, said she felt powerless.
“There was nothing I could do but make him comfortable,” she said. “I literally had to just trust in a higher power and just hope that He would come through for us. It taught me a lot about patience and faith.”
As Israel grew sicker, and they still had no answers, Moholland grew frustrated. “I wish his pediatrician and [the emergency room and urgent care staff] had done what they were supposed to do and given him a test” when Israel first got sick, Moholland said. “What harm would it have done? He suffered for about 10 or 11 days that could have been avoided.”
In a later interview, she talked with NPR about how COVID-19 has disproportionately affected the African American community, due to a combination of underlying health conditions and lack of access to good health care. She said she felt she, too, had fallen victim to those disparities.
“It affects me, personally, because I am African American, but you just never know,” she said. “It’s hard. We’re living in uncertain times — very uncertain times.”
Finally, Children’s Hospital at Montefiore admitted Israel — and the test she’d been trying to get for days confirmed he had the virus.
“I was literally in tears, like begging them not to discharge me because I knew he was not fine,” she recalled.
Israel was in shock, and by the time he got to the hospital, doctors were on the lookout for MIS-C, so they recognized his symptoms — which were distinct from most people with COVID-19.
Doctors gave Israel fluids and intravenous immune globulin, a substance obtained from donated human plasma, which is used to treat deficiencies in the immune system.
Immune globulin has been effective in children like Israel because MIS-C appears to be caused by an immune overreaction to the initial coronavirus infection, according to Choueiter, the Montefiore pediatric cardiologist.
“The immune system starts attacking the body itself, including the arteries of the heart,” she said.
In some MIS-C cases — though not Israel’s — the attack occurs in the coronary arteries, inflaming and dilating them. That also happens in a different syndrome affecting children, Kawasaki disease. About 5% of Kawasaki patients experience aneurysms — which can fatally rupture blood vessels — after the initial condition subsides.
Choueiter and her colleagues want to make sure MIS-C patients don’t face similar risks. So far, they’re cautiously optimistic.
“We have not seen any new decrease in heart function or any new coronary artery dilations,” she said. “When we check their blood, their inflammatory markers are back to normal. For the parents, the child is back to baseline, and it’s as if this illness is a nightmare that’s long gone.”
For a Pennsylvania Teen, the MIS-C Diagnosis Came Much Later
Not every child who develops MIS-C tests positive for the coronavirus, though many will test positive for antibodies to the coronavirus, indicating they had been infected previously. That was the case with Andrew Lis, a boy from Pennsylvania who was the first MIS-C patient seen at the Nemours/Alfred I. duPont Hospital for Children in Wilmington, Delaware.
Andrew had been a healthy 14-year-old before he got sick. He and his twin brother love sports and video games. He said the first symptom was a bad headache. He developed a fever the next day, then constipation and intense stomach pain.
“It was terrible,” Andrew said. “It was unbearable. I couldn’t really move a lot.”
His mother, Ingrid Lis, said they were thinking appendicitis, not coronavirus, at first. In fact, she hesitated to take Andrew to the hospital, for fear of exposing him to the virus. But after Andrew stopped eating because of his headache and stomach discomfort, “I knew I couldn’t keep him home anymore,” Lis said.
Andrew was admitted to the hospital April 12, but that was before reports of the mysterious syndrome had started trickling out of Europe.
Over about five days in the pediatric intensive care unit, Andrew’s condition deteriorated rapidly, as doctors struggled to figure out what was wrong. Puzzled, they tried treatments for scarlet fever, strep throat and toxic shock syndrome. Andrew’s body broke out in rashes, then his heart began failing and he was put on a ventilator. Andrew’s father, Ed Lis, said doctors told the family to brace for the worst: “We’ve got a healthy kid who a few days ago was just having these sort of strange symptoms. And now they’re telling us that we could lose him.”
Though Andrew’s symptoms were atypical for Kawasaki disease, doctors decided to give him the standard treatment for that condition — administering intravenous immune globulin, the same treatment Israel Shippy received.
“Within the 24 hours of the infusion, he was a different person,” Ingrid Lis said. Andrew was removed from the ventilator, and his appetite eventually returned. “That’s when we knew that we had turned that corner.”
It wasn’t until after Andrew’s discharge that his doctors learned about MIS-C from colleagues in Europe. They recommended the whole family be tested for antibodies to the coronavirus. Although Andrew tested positive, the rest of the family — both parents, Andrew’s twin brother and two older siblings — all tested negative. Andrew’s mother is still not sure how he was exposed since the family had been observing a strict lockdown since mid-March. Both she and her husband were working remotely from home, and she says they all wore masks and were conscientious about hand-washing when they ventured out for groceries. She thinks Andrew must have been exposed at least a month before his illness began.
And she’s puzzled why the rest of her close-knit family wasn’t infected as well. “We are a Latino family,” Ingrid Lis said. “We are very used to being together, clustering in the same room.” Even when Andrew was sick, she says, all six of them huddled in his bedroom to comfort him.
Meanwhile, Andrew has made a quick recovery. Not long after his discharge in April, he turned 15 and resumed an exercise routine involving running, pushups and situps. A few weeks later, an echocardiogram showed Andrew’s heart was “perfect,” Ed Lis said. Still, doctors have asked Andrew to follow up with a cardiologist every three months.
An Eye on the Long-Term Effects
The medical team at Montefiore is tracking the 40 children they have already treated and discharged. With kids showing few symptoms in the immediate aftermath, Chouetier hopes the long-term trajectory after MIS-C will be similar to what happens after Kawasaki disease.
“Usually children who have had coronary artery dilations [from Kawasaki disease] that have resolved within the first six weeks of the illness do well long-term,” said Choueiter, who runs the Kawasaki disease program at Montefiore.
The Montefiore team is asking patients affected by MIS-C to return for a checkup one week after discharge, then after one month, three months, six months and a year. They will be evaluated by pediatric cardiologists, hematologists, rheumatologists and infectious disease specialists.
Montefiore and other children’s hospitals around the country are sharing information. Choueiter wants to establish an even longer-term monitoring program for MIS-C, comparable to registries that exist for other diseases.
Moholland is glad the hospital is being vigilant.
“The uncertainty of not knowing whether it could come back in his future is a little unsettling,” she said. “But I am hopeful.”
This story is part of a partnership that includes WNYC, NPR and Kaiser Health News.
Why Doctors Keep Monitoring Kids Who Recover From Mysterious COVID-Linked Illness published first on https://smartdrinkingweb.weebly.com/
0 notes
Text
Why Doctors Keep Monitoring Kids Who Recover From Mysterious COVID-Linked Illness
Israel Shippy doesn’t remember much about having COVID-19 — or the unusual auto-immune disease it triggered — other than being groggy and uncomfortable for a bunch of days. He’s a 5-year-old, and would much rather talk about cartoons, or the ideas for inventions that constantly pop into his head.
“Hold your horses, I think I know what I’m gonna make,” he said, holding up a finger in the middle of a conversation. “I’m gonna make something that lights up and attaches to things with glue, so if you don’t have a flashlight, you can just use it!”
In New York, at least 237 kids, including Israel, appear to have Multisystem Inflammatory Syndrome in Children, or MIS-C. And state officials continue to track the syndrome, but the Centers for Disease Control and Prevention did not respond to repeated requests for information on how many children nationwide have been diagnosed so far with MIS-C.
A study published June 29 in the New England Journal of Medicine reported on 186 patients in 26 states who had been diagnosed with MIS-C. A researcher writing in the same issue added reports from other countries, finding that about 1,000 children worldwide have been diagnosed with MIS-C.
Tracking the Long-Term Health Effects of MIS-C
Israel is friendly and energetic, but he’s also really good at sitting still. During a recent checkup at Children’s Hospital at Montefiore, in the Bronx, he had no complaints about all the stickers and wires a health aide attached to him for an EKG. And when Dr. Marc Foca, an infectious disease specialist, came by to listen to his heart and lungs, and prod his abdomen, Israel barely seemed to notice.
There were still some tests pending, but overall, Foca said, “Israel looks like a totally healthy 5-year-old.”
“Stay safe!” Israel called out, as Foca left. It’s his new signoff, instead of goodbye. His mother, Janelle Moholland, explained Israel came up with it himself.
And she’s also hoping that after a harrowing couple of weeks in early May, Israel himself will “stay safe.”
That’s why they’ve been returning to Montefiore for the periodic checkups, even though Israel seems to have recovered fully from both COVID-19 and MIS-C.
MIS-C is relatively rare, and it apparently responds well to treatment, but it is new enough — and mysterious enough — that doctors here want to make sure the children who recover don’t experience any related health complications in the future.
“We’ve seen these kids get really sick, and get better and recover and go home, yet we don’t know what the long-term outcomes are,” said Dr. Nadine Choueiter, a pediatric cardiologist at Montefiore. “So that’s why we will be seeing them.”
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
When Israel first got sick at the end of April, his illness didn’t exactly look like COVID-19. He had persistent high fevers, with his temperature reaching 104 degrees — but no problems breathing. He wasn’t eating. He was barely drinking. He wasn’t using the bathroom. He had abdominal pains. His eyes were red.
They went to the emergency room a couple of times and visited an urgent care center, but the doctors sent them home without testing him for the coronavirus. Moholland, 29, said she felt powerless.
“There was nothing I could do but make him comfortable,” she said. “I literally had to just trust in a higher power and just hope that He would come through for us. It taught me a lot about patience and faith.”
As Israel grew sicker, and they still had no answers, Moholland grew frustrated. “I wish his pediatrician and [the emergency room and urgent care staff] had done what they were supposed to do and given him a test” when Israel first got sick, Moholland said. “What harm would it have done? He suffered for about 10 or 11 days that could have been avoided.”
In a later interview, she talked with NPR about how COVID-19 has disproportionately affected the African American community, due to a combination of underlying health conditions and lack of access to good health care. She said she felt she, too, had fallen victim to those disparities.
“It affects me, personally, because I am African American, but you just never know,” she said. “It’s hard. We’re living in uncertain times — very uncertain times.”
Finally, Children’s Hospital at Montefiore admitted Israel — and the test she’d been trying to get for days confirmed he had the virus.
“I was literally in tears, like begging them not to discharge me because I knew he was not fine,” she recalled.
Israel was in shock, and by the time he got to the hospital, doctors were on the lookout for MIS-C, so they recognized his symptoms — which were distinct from most people with COVID-19.
Doctors gave Israel fluids and intravenous immune globulin, a substance obtained from donated human plasma, which is used to treat deficiencies in the immune system.
Immune globulin has been effective in children like Israel because MIS-C appears to be caused by an immune overreaction to the initial coronavirus infection, according to Choueiter, the Montefiore pediatric cardiologist.
“The immune system starts attacking the body itself, including the arteries of the heart,” she said.
In some MIS-C cases — though not Israel’s — the attack occurs in the coronary arteries, inflaming and dilating them. That also happens in a different syndrome affecting children, Kawasaki disease. About 5% of Kawasaki patients experience aneurysms — which can fatally rupture blood vessels — after the initial condition subsides.
Choueiter and her colleagues want to make sure MIS-C patients don’t face similar risks. So far, they’re cautiously optimistic.
“We have not seen any new decrease in heart function or any new coronary artery dilations,” she said. “When we check their blood, their inflammatory markers are back to normal. For the parents, the child is back to baseline, and it’s as if this illness is a nightmare that’s long gone.”
For a Pennsylvania Teen, the MIS-C Diagnosis Came Much Later
Not every child who develops MIS-C tests positive for the coronavirus, though many will test positive for antibodies to the coronavirus, indicating they had been infected previously. That was the case with Andrew Lis, a boy from Pennsylvania who was the first MIS-C patient seen at the Nemours/Alfred I. duPont Hospital for Children in Wilmington, Delaware.
Andrew had been a healthy 14-year-old before he got sick. He and his twin brother love sports and video games. He said the first symptom was a bad headache. He developed a fever the next day, then constipation and intense stomach pain.
“It was terrible,” Andrew said. “It was unbearable. I couldn’t really move a lot.”
His mother, Ingrid Lis, said they were thinking appendicitis, not coronavirus, at first. In fact, she hesitated to take Andrew to the hospital, for fear of exposing him to the virus. But after Andrew stopped eating because of his headache and stomach discomfort, “I knew I couldn’t keep him home anymore,” Lis said.
Andrew was admitted to the hospital April 12, but that was before reports of the mysterious syndrome had started trickling out of Europe.
Over about five days in the pediatric intensive care unit, Andrew’s condition deteriorated rapidly, as doctors struggled to figure out what was wrong. Puzzled, they tried treatments for scarlet fever, strep throat and toxic shock syndrome. Andrew’s body broke out in rashes, then his heart began failing and he was put on a ventilator. Andrew’s father, Ed Lis, said doctors told the family to brace for the worst: “We’ve got a healthy kid who a few days ago was just having these sort of strange symptoms. And now they’re telling us that we could lose him.”
Though Andrew’s symptoms were atypical for Kawasaki disease, doctors decided to give him the standard treatment for that condition — administering intravenous immune globulin, the same treatment Israel Shippy received.
“Within the 24 hours of the infusion, he was a different person,” Ingrid Lis said. Andrew was removed from the ventilator, and his appetite eventually returned. “That’s when we knew that we had turned that corner.”
It wasn’t until after Andrew’s discharge that his doctors learned about MIS-C from colleagues in Europe. They recommended the whole family be tested for antibodies to the coronavirus. Although Andrew tested positive, the rest of the family — both parents, Andrew’s twin brother and two older siblings — all tested negative. Andrew’s mother is still not sure how he was exposed since the family had been observing a strict lockdown since mid-March. Both she and her husband were working remotely from home, and she says they all wore masks and were conscientious about hand-washing when they ventured out for groceries. She thinks Andrew must have been exposed at least a month before his illness began.
And she’s puzzled why the rest of her close-knit family wasn’t infected as well. “We are a Latino family,” Ingrid Lis said. “We are very used to being together, clustering in the same room.” Even when Andrew was sick, she says, all six of them huddled in his bedroom to comfort him.
Meanwhile, Andrew has made a quick recovery. Not long after his discharge in April, he turned 15 and resumed an exercise routine involving running, pushups and situps. A few weeks later, an echocardiogram showed Andrew’s heart was “perfect,” Ed Lis said. Still, doctors have asked Andrew to follow up with a cardiologist every three months.
An Eye on the Long-Term Effects
The medical team at Montefiore is tracking the 40 children they have already treated and discharged. With kids showing few symptoms in the immediate aftermath, Chouetier hopes the long-term trajectory after MIS-C will be similar to what happens after Kawasaki disease.
“Usually children who have had coronary artery dilations [from Kawasaki disease] that have resolved within the first six weeks of the illness do well long-term,” said Choueiter, who runs the Kawasaki disease program at Montefiore.
The Montefiore team is asking patients affected by MIS-C to return for a checkup one week after discharge, then after one month, three months, six months and a year. They will be evaluated by pediatric cardiologists, hematologists, rheumatologists and infectious disease specialists.
Montefiore and other children’s hospitals around the country are sharing information. Choueiter wants to establish an even longer-term monitoring program for MIS-C, comparable to registries that exist for other diseases.
Moholland is glad the hospital is being vigilant.
“The uncertainty of not knowing whether it could come back in his future is a little unsettling,” she said. “But I am hopeful.”
This story is part of a partnership that includes WNYC, NPR and Kaiser Health News.
Why Doctors Keep Monitoring Kids Who Recover From Mysterious COVID-Linked Illness published first on https://nootropicspowdersupplier.tumblr.com/
0 notes
Text
Why Doctors Keep Monitoring Kids Who Recover From Mysterious COVID-Linked Illness
Israel Shippy doesn’t remember much about having COVID-19 — or the unusual auto-immune disease it triggered — other than being groggy and uncomfortable for a bunch of days. He’s a 5-year-old, and would much rather talk about cartoons, or the ideas for inventions that constantly pop into his head.
“Hold your horses, I think I know what I’m gonna make,” he said, holding up a finger in the middle of a conversation. “I’m gonna make something that lights up and attaches to things with glue, so if you don’t have a flashlight, you can just use it!”
In New York, at least 237 kids, including Israel, appear to have Multisystem Inflammatory Syndrome in Children, or MIS-C. And state officials continue to track the syndrome, but the Centers for Disease Control and Prevention did not respond to repeated requests for information on how many children nationwide have been diagnosed so far with MIS-C.
A study published June 29 in the New England Journal of Medicine reported on 186 patients in 26 states who had been diagnosed with MIS-C. A researcher writing in the same issue added reports from other countries, finding that about 1,000 children worldwide have been diagnosed with MIS-C.
Tracking the Long-Term Health Effects of MIS-C
Israel is friendly and energetic, but he’s also really good at sitting still. During a recent checkup at Children’s Hospital at Montefiore, in the Bronx, he had no complaints about all the stickers and wires a health aide attached to him for an EKG. And when Dr. Marc Foca, an infectious disease specialist, came by to listen to his heart and lungs, and prod his abdomen, Israel barely seemed to notice.
There were still some tests pending, but overall, Foca said, “Israel looks like a totally healthy 5-year-old.”
“Stay safe!” Israel called out, as Foca left. It’s his new signoff, instead of goodbye. His mother, Janelle Moholland, explained Israel came up with it himself.
And she’s also hoping that after a harrowing couple of weeks in early May, Israel himself will “stay safe.”
That’s why they’ve been returning to Montefiore for the periodic checkups, even though Israel seems to have recovered fully from both COVID-19 and MIS-C.
MIS-C is relatively rare, and it apparently responds well to treatment, but it is new enough — and mysterious enough — that doctors here want to make sure the children who recover don’t experience any related health complications in the future.
“We’ve seen these kids get really sick, and get better and recover and go home, yet we don’t know what the long-term outcomes are,” said Dr. Nadine Choueiter, a pediatric cardiologist at Montefiore. “So that’s why we will be seeing them.”
Email Sign-Up
Subscribe to KHN’s free Morning Briefing.
Sign Up
Please confirm your email address below:
Sign Up
When Israel first got sick at the end of April, his illness didn’t exactly look like COVID-19. He had persistent high fevers, with his temperature reaching 104 degrees — but no problems breathing. He wasn’t eating. He was barely drinking. He wasn’t using the bathroom. He had abdominal pains. His eyes were red.
They went to the emergency room a couple of times and visited an urgent care center, but the doctors sent them home without testing him for the coronavirus. Moholland, 29, said she felt powerless.
“There was nothing I could do but make him comfortable,” she said. “I literally had to just trust in a higher power and just hope that He would come through for us. It taught me a lot about patience and faith.”
As Israel grew sicker, and they still had no answers, Moholland grew frustrated. “I wish his pediatrician and [the emergency room and urgent care staff] had done what they were supposed to do and given him a test” when Israel first got sick, Moholland said. “What harm would it have done? He suffered for about 10 or 11 days that could have been avoided.”
In a later interview, she talked with NPR about how COVID-19 has disproportionately affected the African American community, due to a combination of underlying health conditions and lack of access to good health care. She said she felt she, too, had fallen victim to those disparities.
“It affects me, personally, because I am African American, but you just never know,” she said. “It’s hard. We’re living in uncertain times — very uncertain times.”
Finally, Children’s Hospital at Montefiore admitted Israel — and the test she’d been trying to get for days confirmed he had the virus.
“I was literally in tears, like begging them not to discharge me because I knew he was not fine,” she recalled.
Israel was in shock, and by the time he got to the hospital, doctors were on the lookout for MIS-C, so they recognized his symptoms — which were distinct from most people with COVID-19.
Doctors gave Israel fluids and intravenous immune globulin, a substance obtained from donated human plasma, which is used to treat deficiencies in the immune system.
Immune globulin has been effective in children like Israel because MIS-C appears to be caused by an immune overreaction to the initial coronavirus infection, according to Choueiter, the Montefiore pediatric cardiologist.
“The immune system starts attacking the body itself, including the arteries of the heart,” she said.
In some MIS-C cases — though not Israel’s — the attack occurs in the coronary arteries, inflaming and dilating them. That also happens in a different syndrome affecting children, Kawasaki disease. About 5% of Kawasaki patients experience aneurysms — which can fatally rupture blood vessels — after the initial condition subsides.
Choueiter and her colleagues want to make sure MIS-C patients don’t face similar risks. So far, they’re cautiously optimistic.
“We have not seen any new decrease in heart function or any new coronary artery dilations,” she said. “When we check their blood, their inflammatory markers are back to normal. For the parents, the child is back to baseline, and it’s as if this illness is a nightmare that’s long gone.”
For a Pennsylvania Teen, the MIS-C Diagnosis Came Much Later
Not every child who develops MIS-C tests positive for the coronavirus, though many will test positive for antibodies to the coronavirus, indicating they had been infected previously. That was the case with Andrew Lis, a boy from Pennsylvania who was the first MIS-C patient seen at the Nemours/Alfred I. duPont Hospital for Children in Wilmington, Delaware.
Andrew had been a healthy 14-year-old before he got sick. He and his twin brother love sports and video games. He said the first symptom was a bad headache. He developed a fever the next day, then constipation and intense stomach pain.
“It was terrible,” Andrew said. “It was unbearable. I couldn’t really move a lot.”
His mother, Ingrid Lis, said they were thinking appendicitis, not coronavirus, at first. In fact, she hesitated to take Andrew to the hospital, for fear of exposing him to the virus. But after Andrew stopped eating because of his headache and stomach discomfort, “I knew I couldn’t keep him home anymore,” Lis said.
Andrew was admitted to the hospital April 12, but that was before reports of the mysterious syndrome had started trickling out of Europe.
Over about five days in the pediatric intensive care unit, Andrew’s condition deteriorated rapidly, as doctors struggled to figure out what was wrong. Puzzled, they tried treatments for scarlet fever, strep throat and toxic shock syndrome. Andrew’s body broke out in rashes, then his heart began failing and he was put on a ventilator. Andrew’s father, Ed Lis, said doctors told the family to brace for the worst: “We’ve got a healthy kid who a few days ago was just having these sort of strange symptoms. And now they’re telling us that we could lose him.”
Though Andrew’s symptoms were atypical for Kawasaki disease, doctors decided to give him the standard treatment for that condition — administering intravenous immune globulin, the same treatment Israel Shippy received.
“Within the 24 hours of the infusion, he was a different person,” Ingrid Lis said. Andrew was removed from the ventilator, and his appetite eventually returned. “That’s when we knew that we had turned that corner.”
It wasn’t until after Andrew’s discharge that his doctors learned about MIS-C from colleagues in Europe. They recommended the whole family be tested for antibodies to the coronavirus. Although Andrew tested positive, the rest of the family — both parents, Andrew’s twin brother and two older siblings — all tested negative. Andrew’s mother is still not sure how he was exposed since the family had been observing a strict lockdown since mid-March. Both she and her husband were working remotely from home, and she says they all wore masks and were conscientious about hand-washing when they ventured out for groceries. She thinks Andrew must have been exposed at least a month before his illness began.
And she’s puzzled why the rest of her close-knit family wasn’t infected as well. “We are a Latino family,” Ingrid Lis said. “We are very used to being together, clustering in the same room.” Even when Andrew was sick, she says, all six of them huddled in his bedroom to comfort him.
Meanwhile, Andrew has made a quick recovery. Not long after his discharge in April, he turned 15 and resumed an exercise routine involving running, pushups and situps. A few weeks later, an echocardiogram showed Andrew’s heart was “perfect,” Ed Lis said. Still, doctors have asked Andrew to follow up with a cardiologist every three months.
An Eye on the Long-Term Effects
The medical team at Montefiore is tracking the 40 children they have already treated and discharged. With kids showing few symptoms in the immediate aftermath, Chouetier hopes the long-term trajectory after MIS-C will be similar to what happens after Kawasaki disease.
“Usually children who have had coronary artery dilations [from Kawasaki disease] that have resolved within the first six weeks of the illness do well long-term,” said Choueiter, who runs the Kawasaki disease program at Montefiore.
The Montefiore team is asking patients affected by MIS-C to return for a checkup one week after discharge, then after one month, three months, six months and a year. They will be evaluated by pediatric cardiologists, hematologists, rheumatologists and infectious disease specialists.
Montefiore and other children’s hospitals around the country are sharing information. Choueiter wants to establish an even longer-term monitoring program for MIS-C, comparable to registries that exist for other diseases.
Moholland is glad the hospital is being vigilant.
“The uncertainty of not knowing whether it could come back in his future is a little unsettling,” she said. “But I am hopeful.”
This story is part of a partnership that includes WNYC, NPR and Kaiser Health News.
from Updates By Dina https://khn.org/news/why-doctors-keep-monitoring-kids-who-recover-from-mysterious-covid-linked-illness/
0 notes
Text
Men’s Health Month: Busting The Myths Surrounding Testosterone Replacement Therapy
Not so shockingly, men are less likely than women to visit a healthcare provider when they’re not feeling 100%. And often they wait until a medical issue has become serious before they do anything about it. Some of this tendency may be because men are less likely to ask for help in general (hence their often-joked-about difficulty with asking for directions). And some of it may be because, like most adults of working age these days, men often feel that they’re too busy to look for health solutions.
When it comes to hormonal issues, we have come across a whole new reason why men sometimes hesitate to get the help they need – misinformation about negative side effects of hormone replacement therapy. With the rise in chronic conditions and disease, we at Alpha Hormones Inc. strongly believe that men need to be more proactive about their health. This November for Men’s Health Month, we’re going to help you put any fears you have about testosterone therapy to rest.
This information doesn’t replace the need to see your doctor – in fact, we hope that it will encourage more men to take their health seriously and visit their healthcare practitioners.
Low Testosterone Is One Of The Most Common Health Concerns For Men
Many signs of “low T” develop slowly over time. As a result, men often ascribe their symptoms to simply growing older. However, a reduction in testosterone levels doesn’t have to be a normal consequence of aging. Although your hormone levels do begin to drop as early as your 30’s for a variety of reasons, there are a number of steps you can take to help protect them.
What Are The Symptoms Of Low Testosterone?
How can you tell if you have low testosterone levels? Only your healthcare practitioner can make a definitive diagnosis, but the following signs could indicate it’s time to schedule an appointment.
Lagging libido
Unexplained fatigue
Depression
Irritability
Increased body fat
Male breast tissue growth
Loss of muscle tone
Natural Ways To Protect Your Testosterone Levels
1. Sleep
Missing a few hours can quickly cause your levels of testosterone to drop. Try to maintain a consistent sleep schedule, and practise good “sleep hygiene” by ensuring your bedroom is dark and switching off any electronics for one hour before bedtime.
2. Exercise
Working out is one of the more direct ways to give your testosterone levels a boost- there’s a reason many men feel “pumped up” after a workout. Weights are the most effective activity for raising testosterone levels, and recent studies found high-intensity interval training High Intensity Interval Training (HIIT) workouts productive in this regard.
3. Eat a balanced diet
Include plenty of good quality protein, unrefined carbohydrates, and healthy fats.
4. Keep stress levels in check.
When you’re stressed, your levels of the hormone cortisol rise. And when cortisol rises, testosterone drops. So avoid chronic, long-term stress. And if you’re feeling overwhelmed, schedule some mini-breaks for yourself. Calling a time out on a hectic schedule to meditate or simply go for a short walk can pay off in the long run.
5. Watch your vitamin D levels
Spending time in the sun, or taking vitamin D supplements during the winter, can give your body a key component needed to raise your testosterone levels if they are low.
6. Avoid estrogen-mimicking materials
Many compounds found in daily life can affect your hormones because they mimic estrogen in your body. In particular, avoid materials made with BPA, parabens, and phthalates. That means not using things like plastic water bottles, air fresheners, and scented grooming products.
Consider Bioidentical Testosterone Replacement Therapy (TRT)
If you are experiencing the uncomfortable symptoms listed above, consider coming in to discuss whether TRT is the right choice for you. When you meet with us, we’ll take a blood sample and analyze it to determine what your hormonal baseline should be, what you’re lacking, and the best way to move forward. Then we will design a personalized health regimen that’s all about increased energy, mood, and looking and feeling younger, healthier and optimal.
Wait – Should You Be Concerned About Bioidentical Testosterone Replacement Therapy?
If you have been reading mixed information about TRT, you’re not alone. That’s why in October 2015, a group of respected experts in endocrinology, diabetology, internal medicine and science research from around the world, including Harvard Medical School and Johns Hopkins University School of Medicine, got together to discuss Testosterone Deficiency.
All of the experts volunteered their time as they debated the top considerations and treatment issues surrounding Testosterone Replacement Therapy based on the best available scientific evidence, and drafted the following resolutions.
Expert Resolutions On Low T Following The 2015 Conference
– Low testosterone should be taken seriously
– Low T symptoms benefit from treatment
– Testosterone Deficiency is a global public health concern
– Testosterone replacement is an evidence-based therapy
– Even mild cases can benefit
– Men of any age can benefit
– T Therapy does not increase heart risk
– T Therapy does not increase Prostate Cancer risk
– T Therapy shows promise in certain chronic conditions such as Diabetes
Now, I know that for many of the men who are hesitant to come in and discuss testing and treatment for low testosterone, there are a couple of issues they are most concerned about. So let’s dig a little deeper into two key areas: Does TRT actually affect your risk of heart disease or prostate issues?
The History OF The T Therapy Controversy
Testosterone Therapy has been in use since the 1940s, however, until the turn of the century, it was exclusively prescribed for men with severe testosterone insufficiency such as after treatment for pituitary cancer. The primary concern in the early days was that it may be associated with an increased risk of prostate cancer.
The Rise of T Supplements In Sports
In the past 20 years, the use of Testosterone supplements has grown and it has become controversially associated with illicit athletic performance enhancement and its use as an anabolic steroid in bodybuilding.
The Media Effect
Negative media stories peaked in 2013 when a retrospective study was published in a top medical journal reporting increased cardiovascular risks. A second retrospective data analysis in 2014 reported an increase in nonfatal myocardial infarction (heart attack) rates following a T prescription compared with the rate before the prescription.
Following the negative press, Health Canada and the FDA added warnings to T products in 2014 stating that there was a risk of cardiovascular issues. The FDA also limited the prescription of Testosterone products to men with identified underlying Testosterone issues, and rejected the concept of age-related testosterone decline. In contrast, the European Medicines Agency (EMA) reviewed the same evidence but decided not to add any warnings to T products in Europe.
Studies Lose Credibility
While the damage had already been done to the reputation of TRT, subsequent analysis showed that neither of the 2013/14 studies provided credible evidence of an increased risk to the heart.
The first study underwent 2 official corrections: one for misreporting its results, which actually showed an approximately 50% lower rate of adverse cardiovascular events in men who received a T prescription compared with untreated men, and the second for large data errors, including that nearly 10% of its all-male database was comprised of women.
The second study had no control group, so it is unknown whether cardiovascular events (nonfatal heart attacks in that study) differed between treated and untreated men with testosterone deficiency.
Does Bioidentical TRT Cause Heart issues?
Looking at the origins of this question, we know that two observational studies received intense media attention after reporting increased cardiovascular risks, however both studies had major flaws. One misreported results, the other had no control group. The 2015 conference highlighted the following facts:
Subsequent research tells us that low testosterone levels are associated with increased atherosclerosis, coronary artery disease, obesity, diabetes, and mortality.
Several randomized controlled studies in men with known heart disease (angina, heart failure) showed better blood flow and exercise capacity in those supplemented with testosterone versus the placebo group.
The largest meta-analysis showed no increased risk with T therapy, in fact, reduced risk was noted in men with metabolic conditions such as diabetes.
There is no evidence of an increased risk of blood clots (aka thrombosis, including an increased risk of stroke) with T therapy.
Does Bioidentical Testosterone Replacement Therapy Cause Prostate Cancer?
Medically, the greatest concern for the first 70 years of TRT was the fear that it may cause prostate cancer. The 2015 conference addressed this concern and these were their findings:
Upon reviewing all available evidence they found that the evidence does not support the theory that T therapy is associated with an increased risk of prostate cancer.
Androgen (male hormone) levels in the general (non-supplemented) public are not associated with any increased risk of prostate cancer nor aggressive disease.
Study participants taking Testosterone therapy had no greater risk of prostate cancer than the placebo groups
Aggressive/high-grade prostate cancer is in fact associated with low serum testosterone levels.
Early data suggests that there is no increased risk of recurrence or progression of prostate cancer in men who have been previously treated for prostate cancer when taking TRT.
0 notes
Text
Gum Disease: Stages, Prevention, and Treatment
From a simple case of bleeding gums to painful gum recession, gum disease is a problem that you need to deal with as soon as possible.
Here, we’ll discuss the hierarchy of gum disease and what happens at each stage. You’ll also learn what you can do at home in your daily routine to prevent this from happening and protect your dental health.
If all else fails, fear not. Your dentist can help you with a treatment plan to manage gum disease at any stage of gum disease (officially dubbed “periodontitis”).
Gum Disease Signs and Symptoms
There are a few very common signs of periodontal disease to look for in your daily routine. These signs of gum disease may be signals that your gum health isn’t where it needs to be.
Red, swollen gums
Receding gums
Bleeding on brushing or flossing
Visible pus
Teeth feel loose and moveable
A change in your bite
Heightened sensitivity to hot or cold foods
Pain when chewing
A bad taste in your mouth
Persistent bad breath
A note of caution: Even if you do not have any of these symptoms, it is possible you still have gum disease.
Always go to your routine dental visits for check-ups—gum disease diagnosis is one reason you should stick to these appointments.
How Your Dentist Will Diagnose Gum Disease
When you show up for a dental appointment, you may not realize your dentist and hygienist are looking for gum disease symptoms. Here are some of what happens at your dental cleanings that can help recognize periodontitis.
1. Medical History
You may be thinking, “Did I come to the doctor’s office, or the dentist’s?” This is a common notion many people have when a dentist asks about certain diseases that run in their family, or if they’ve recently been diagnosed with any systemic conditions.
One reason for this is that any medication you may have been prescribed by your physician could cause severe consequences for your oral health.
For example, medications that have the side effect of causing a dry mouth, or “xerostomia,” can lead to tooth decay.
The saliva in our mouths helps us wash away food and other debris to rid of plaque. Plaque naturally forms a biofilm on the surface of our teeth after we eat or drink anything with carbohydrates or sugars.
Over time, if plaque is not removed regularly by brushing and flossing, it can lead to tartar buildup. Tartar is also called “calculus,” and it forms a yellow, brown deposit after plaque hardens. Unlike plaque, you cannot safely remove tartar on your own. This can only be done professionally by a dentist or dental hygienist.
2. Pocket Depth Measurement
This part of your dental exam and teeth cleaning is called “perio probing.” Here, dentists use an instrument called a periodontal probe with markings in millimeters used to measure the pocket depths around each and every tooth.
With firm and gentle pressure, the perio probe is inserted into your gingival sulcus, which is the space between your tooth and the gum surrounding it.
Healthy measurements are between 1-3mm of pocket depth.
Generally, anything deeper than that indicates gum inflammation that is making the pocket deeper. The deeper the pocket, the looser the gums surrounding your tooth, and the higher the degree of inflammation.
Another sign that your dentist or dental hygienist will look for when measuring pocket depth is bleeding upon probing. We may be poking at you, but a periodontal probe is blunted at the end, so it shouldn’t cause any bleeding in a healthy mouth. Bleeding upon probing is not considered normal and is one of the significant signs of gum inflammation.
It is really important that you don’t miss your regular check-ups and cleanings, or reschedule as soon as you can if something pops up. That way, anything out of the ordinary will be caught on early and promptly treated.
3. Dental X-Rays
The purpose of taking an x-ray (radiograph) is help your dentist examine everything in your mouth that is not visible to the naked eye.
The most commonly taken x-rays to evaluate gum disease are “bitewings.” There are four bitewings that are taken, one for each quadrant. Your dentist will be able to see everything from the top of your tooth to its roots, as well as the height of the bone around it.
The periodontal ligament, or PDL, serves as the supporting structure between the tooth and the bone. Bacteria can build up in deep periodontal pockets and cause destruction to the PDL, leading to bone loss and eventual tooth loss.
Taking bitewing x-rays will help your dentist assess if there are any changes to your jawbone as a result of gum disease.
Radiographs are not “one size fits all.” Your dentist will determine your oral profile risk and the frequency of x-rays needed. It may be as recent as every 6 months or only every couple of years.
The Stages of Gum Disease
There are four stages of gum disease, although the lines between these are a bit blurred.
Stage I: Gingivitis
This first stage of gum disease refers to inflammation of the gums.
Bacteria and plaque build up gradually over time along your gingival sulcus. Toxins released from this bacteria may cause deeper periodontal pockets due to damage of the PDL fibers that support the teeth and gums.
As mentioned previously, healthy gums have a probing depth of 1-3 mm. At the gingivitis stage, probing depths will be about 2-4 mm. (1)
You may also have other gingivitis symptoms, like:
Redness and swelling of the gums
Bleeding upon flossing
Bad breath
This is the mildest form of gum disease and therefore does not result in any bone loss or connective tissue loss. The good news is this stage is completely reversible and you can usually correct it at home! We’ll learn more about that later.
Stage II – III: Slight to Moderate Periodontal Disease
These two stages are grouped together because their effects are similar but gradual in strength.
The infection has now penetrated deep into your gums rather than along your gums. You will have:
Increased redness in your gums
More bleeding upon brushing
Worsening bad breath.
For slight periodontal disease, your dentist will observe 4-5 mm in probing depth. As for moderate periodontal disease, we will see probing depths at about 6-7 mm.
The deeper the infection gets into the gums, the greater the destruction of the PDL fibers, and the higher the probing depth.
At this point, the bacteria gets so entrenched into your gums that it actually begins to enter your bloodstream. This can compromise your immune system and might lead to or heighten your risk of other diseases (thanks, mouth-body connection!).
The main distinction from these stages in contrast to gingivitis is the start of bone loss. Bone loss here can range from 20-50%.
At this point, you cannot just cure gum disease at home. Treatment will require a consultation with your dentist.
Stage IV: Advanced Periodontal Disease
As you enter this stage of periodontal disease, bacteria has become more virulent.
You have pocket depths greater than 7 mm and the roots of your teeth may be exposed. Tooth mobility has increased significantly and tooth loss becomes very probable. This changes your overall bite and makes chewing more of a challenge.
Something else your dentist will see are pus-filled abscesses in and around your gums. These abscesses form in because immune system is trying to fight off the infection and keep it from spreading.
Bone loss at this stage is between 50-90%. Due to the severe infiltration of bacteria and the destruction it has caused to the integrity of your teeth, this final stage is only manageable with treatment, not reversible.
Types of Gum Disease
Gum disease happens for a number of reasons, and depending on the cause, it can progress more or less rapidly. The four types of gum disease can help your dentist determine the best course of treatment and help you with expectations for recovery. (2)
Chronic: Most common of the four types, chronic periodontitis is the gradual progression of inflammation in and around the gums. This typically happens slowly but can worsen rapidly at different points of the condition.
Aggressive: Typically seen in families, aggressive periodontitis often happens in healthy people and progresses faster than chronic periodontitis. There’s a likely genetic component to this type of gum disease.
Related to systemic disease: Certain diseases can manifest as gum disease. Periodontitis as a manifestation of systemic disease occurs most often in children with issues like diabetes, respiratory disease, or cardiovascular disease.
Necrotizing: In necrotizing periodontal disease, lesions cause necrosis (tissue death) of gingival tissue, periodontal ligament, and alveolar bone. People with these kinds of lesions are typically those with compromised immune systems, like patients with HIV, malnutrition, or other immune-compromising conditions.
Options for Gum Disease Treatment at Each Stage
Whether you’re struggling with advanced gum disease or the beginning stages of gingivitis, there are things you can do to keep your gums healthy.
In 1965, Dr. Harald Löe and his colleagues conducted a study called “Experimental Gingivitis in Man.”
Dr. Löe asked eleven healthy male dental students to be experimental subjects. The participants had their teeth cleaned and scaled to provide a baseline of their gingival health. They were then asked to cease all oral hygiene measures. That means no brushing, flossing, or mouth rinsing.
I imagine this might have been hard for their girlfriends. But, I digress.
As oral hygiene measures were withdrawn, plaque accumulated and the subjects developed gingivitis in a range of 9-21 days. They were then asked to begin oral hygiene measures again.
Although some men took a longer time to develop gingivitis, all the men returned to their normal, healthy status in about 7-11 days. They did this on their own, with no professional help, but only consistent oral care and hygiene. (3) Clearly, there’s something important in that daily routine!
Let’s look at the treatment options for each stage of gum disease.
1. Treatment for Gingivitis
The purpose of Dr. Harald Löe’s experiment (though this type of research is considered unethical in today’s research guidelines) was to prove that the mildest form of gum disease, gingivitis, is completely reversible.
Your dentist or hygienist will give you a dental prophylaxis, or “prophy.” This is what is known as a professional cleaning. (4) It will consist of supragingival (above the gum line) and subgingival (below the gum line) removal of plaque, calculus, and staining.
However, your provider can only do so much. The only way of reversing gingivitis at this stage is good oral hygiene on your part. Brushing twice a day for two minutes at a time, flossing at least once, and regular dental check-ups will get you back to a healthy smile.
If you notice bleeding gums more regularly than you’d like but your dentist hasn’t seen signs of more advanced gum disease, try some of the treatments for gingivitis Dr. Burhenne outlines here.
2. Treatment for Slight to Moderate Periodontal Disease
At this stage, the infection has gotten deep enough into your tissues that a prophy, brushing, or flossing just won’t cut it. Here, your dentist will introduce a non-surgical procedure called scaling and root planing procedure (SRP for short).
“Scaling” is when your provider cleans out the toxins in your periodontal pockets. “Root planing” is when he or she smooths out the surfaces of your roots to help your gums reattach. (5) Generally, this procedure causes very little discomfort. If you have sensitive teeth, your dentist may numb your gums with a local anesthetic.
An SRP can be done in a single visit, but it is usually broken up into appointments per quadrant (¼ of the mouth) or by halves, depending on the severity. After an SRP, your gums may feel tender and sensitive.
If you are consistent with a proper oral hygiene regimen after the procedure, your gums should turn back to their smooth texture and natural pink color within a few weeks.
Other ways to handle this stage of gum disease at home include a gum disease diet, using knotted floss to dislodge stubborn food particles, and trying mouth tape to cut down on mouth breathing at night.
3. Treatment for Advanced Periodontal Disease
Flap Surgery
At this stage, your bone and surrounding supporting tissue have been significantly destroyed. The objective of flap surgery is to reduce the depth of the periodontal pockets and regenerate the PDL fibers.
After numbing the area with local anesthetic, your dentist will make a flap-like incision around the gum tissue. The gums are lifted back, which allows a thorough cleaning of all the diseased tissue that has infiltrated. The flap is then sealed tightly so the gums fit snugly around the teeth and the healing process takes place.
After the procedure, you will have reduced pockets, which makes it easier to maintain your oral health. A combination of professional maintenance and consistent home care of your teeth will help prevent recurrence of this disease. (6)
Bone Graft
If you have teeth lost to gum disease, the bone around those teeth will also be lost. Since there is no support in that area, your skin will droop and it will give you an older-looking appearance.
Fortunately, bone grafting helps regenerate any bone that was lost to periodontal disease.
Essentially, what your dentist is doing is placing natural or synthetic bone that works with your body to help build new bone. Tissue-stimulating growth factor proteins may also be used to help your body regrow bone.
In cases with exposed tooth roots, your dentist may suggest a soft tissue graft. Recovery following the bone big graft procedure varies with each patient, but the entire healing process can take between 4-6 months.
Pinhole Surgery
This particular surgery hasn’t been around long, but some clinicians claim that pinhole surgery can help gum tissue grow back. (7) This would be revolutionary, and the preliminary results are good. However, this procedure is in its infancy and it’s not yet proven to be a long-term solution.
Causes and Risk Factors of Gum Disease
Depending on your individual genetics, lifestyle, diet, and other factors, you may be at a higher or lower risk of gum disease. Let’s look at what science tells us are the most common risk factors. (8, 9)
Smoking & Tobacco Use
This one is no surprise. Studies have shown that smoking causes an increase in gum recession and in bone loss.
If you are a current smoker, you have four times the chance of developing periodontal disease in relation to non-smokers.
Research also shows that periodontal therapy is less effective in smokers than it is in non-smokers. Be above the influence, friends.
Genetics
There has been research done in twins that suggest “50% of susceptibility to [gum] disease is due to host factors.” This could be because twins share very similar environmental and behavioral exposures.
Stress
Everybody suffers from chronic stress in his or her own way. People with higher levels of stress have a greater incidence of developing periodontal disease.
Stress depresses our immune system and causes an imbalance in our homeostasis. When you are stressed out, you release a higher number of inflammatory cells, which can promote tissue damage.
Another reason stress is associated with poor oral hygiene is sometimes, you have other things preoccupying your mind. You may not be giving your oral hygiene the attention it needs in times of emotional stress.
The key takeaway here is: we all need a good massage or a spa day every once in a while. Grab some friends and try to unwind; your mouth will thank you.
Medication
Some medications decrease your salivary flow, which impacts its ability to wash away plaque and debris. This is important because saliva helps prevent plaque buildup and gum inflammation.
These medications include but are not limited to:
Antihistamines
Antihypertensives
Anticonvulsants
Sedatives
Ask your physician if any of the medications you’ve been prescribed causes dry mouth, or “xerostomia.” If so, perhaps your dentist and physician can work together to find another alternative.
Orthodontic Treatment
Some types of partial dentures, braces, or other orthodontic devices can make it hard to remove all the tartar and calculus buildup common to gum disease.
Diet
Studies in adolescents aged 11-18 have shown that kids in this age group do not eat many fruits and vegetables, which are sources high in vitamin C. Moreover, calcium-rich beverages such as milk have decreased while sugary beverages such as sport-drinks have increased.
A decrease in calcium and vitamin C have been associated with an increased risk of periodontal disease.
In general, a diet heavy on carbohydrates (breads, pastas, crackers, sugary treats, etc.) is going to be bad for oral health, particularly when you aren’t keeping up with dental hygiene as well. Keep in mind that your mouth and body as a whole need healthful, whole foods to function well.
Age
There is a caveat to this one: the risk of gum disease doesn’t just go up because a person merely gets older; it’s tied in to various other factors.
For example, as we get older, we lose some of our manual dexterity and thus cannot brush as well as we used to. You may become more forgetful and forget to practice as oral hygiene on a daily routine.
People are also living longer! As we’re retaining our teeth for a longer period of time, they need to be maintained for a longer period of time. This can be hard to do since as we age, we naturally develop many other systemic diseases that negatively impact our oral health.
This brings us to the next point.
Periodontitis and Other Diseases
When you think about gum disease, you shouldn’t think only of your oral health. There are connections between gum disease and other health problems, including diabetes, heart disease, Alzheimer’s, pneumonia, and even cancer.
Diabetes
Poor glycemic control has been associated with higher rates of periodontal disease. (10) The good news is that patients with controlled diabetes respond favorably to periodontal treatment. Check your HbA1c count regularly to make sure your blood sugar is in the target range.
You may also want to consider natural diabetes treatment options, like dietary alteration. These have a great track record of effectively managing blood sugar and A1c levels.
Heart Disease
There has been a lot of research done on the association between cardiovascular disease and periodontitis. High cholesterol and atherosclerotic plaque together may increase the risk for chronic periodontitis. (11)
We have many different inflammatory markers in our bodies that serve a variety of functions. Generally, they are increased when there is injury somewhere in your body and your immune system is trying to defend you.
Both periodontitis and heart disease are associated with the same increase in inflammatory markers, C-reactive protein (CRP) and Interleukin-6 (IL-6). (12)
The only confirmed causal link between oral disease and systemic infection is that of infective endocarditis, an inflammation in the lining of the heart. (13)
Bacteria are more likely to escape into the bloodstream when the biological width, the seal of gums to teeth that serves to protect the alveolar bone, isn’t healthy, like in gum disease. These bacteria can then collect on the heart to cause endocarditis—which is most likely after a root scaling and planing.
Alzheimer’s Disease
There are two mechanisms by which association Alzheimer’s and gum disease are explained.
One theory is that the bacteria in gum disease that seeps into your bloodstream increases inflammatory markers, which leads to systemic inflammation. These markers are capable of crossing into the brain and leading to neuronal damage.
The second mechanism is explained by the bacteria from your plaque crossing into the brain. Dental plaque enters the brain via the bloodstream or peripheral nerves. This organisms then cause and inflammatory response in your central nervous system (CNS), which leads to cognitive impairment. (14)
A team of researchers released a compelling study in 2019 introducing a possible causation between gum disease and Alzheimer’s. (15) While this hasn’t been confirmed by other studies or human trials, it’s enough to consider being more diligent treating gum disease.
Hematologic Disorders (Leukemia)
Gingival hyperplasia, which is overgrowth of gum tissue around the teeth, can be an early symptom of acute leukemia. (16)
Chemotherapy or bone marrow transplantation can also negatively affect gingival health. Some of the symptoms are abscesses, inflamed gums, or severe redness.
Pneumonia
The same people at risk for pneumonia are typically those at risk for gum disease. Although it’s not clear if one causes or contributes to the other, they are closely connected.
One proposed reason for this connection is that patients in hospitals and nursing homes that frequently contract pneumonia also can’t keep up with good oral care. This may upset the oral microbiome and set the stage for other immune system-compromising infection. (13)
How to Prevent Gum Disease
There are several things you can do regularly if you notice warning signs of gum disease—or to prevent these from ever happening.
Brush twice a day for 2 minutes. Use your smartphone or a brush timer as a measurement of time to how long you’ve been brushing.
Floss at least once a day to remove plaque from places your toothbrush can’t get access to. You know when your mom tells you to clean your room, and you think it’s clean, but then she goes in and finds areas that aren’t really clean? It’s basically the same concept, but with flossing.
Avoid smoking (anything) and all forms of tobacco. This includes cigarettes, cigars, “dip” or chewing tobacco, and hookah. Being healthy is the new cool.
Maintain a healthy diet. Now, I’m not telling you to go vegan, but I am telling you that it’s important to add fruits and vegetables to get your daily dose of vitamin C and calcium.
Ask your physician if any of your medications cause dry mouth, or “xerostomia.” If they do, ask if there are any other alternatives available. It’s important for different healthcare providers to be in contact so we can provide you with the best possible care.
Tape your mouth shut at night. Weird habit, but great results. Mouth taping cuts down on mouth breathing while you sleep. This, in turn, can help resolve dry mouth.
Don’t use conventional mouthwash. I know what you’re thinking. This is the stuff that’s supposed to give me a cleaner mouth and me have kissable breath! But it’s just not good for your oral health.
So many mouthwashes have a high alcohol content, which dries your mouth and disrupts your oral microbiome. Dry mouth and an imbalance of bacteria are both risks for plaque retention. You can read more about other DIY mouthwash alternatives here.
Try natural methods of gum disease prevention. These may include using turmeric in a lot of your recipes, oil pulling, and taking oral probiotics to support a healthy oral microbiome.
Into DIY-ing? Dr. B created a great DIY recipe for toothpaste specifically for healthier gums. You can check it out and try it for yourself by reading this article.
Always, always schedule regular check-ups and professional cleanings. You will have a much less chance of developing anything suspicious if your dentist is monitoring your health. Remember, preventative is always better than constructive!
Common Questions About Gum Disease
Q:
What’s the difference between gingivitis and gum disease?
A: Gingivitis is the early, reversible stage of gum disease. The main difference here is that in gingivitis, there is no loss of bone or loss of connective tissue. Not all cases of gingivitis result in gum disease, but it can if left untreated.
Once bacteria have seeped deep below your gum line, it starts to destroy gum tissue, your periodontal pockets deepen, and some of your bone is lost. Your teeth become mobile and loose because it doesn’t have as much support from bone anymore. This is when you have advanced into Stages II-IV of periodontitis.
Q:
How common is gum disease?
A: Very common! In a study titled “Prevalence of Periodontitis in Adults in the United States” found that 47.2% or roughly 64.7 million American adults have either mild, moderate, or severe periodontal disease. This is even higher in adults aged 65 and older, at about 70.1%.
On a greater scale, we are looking at 743 million people afflicted, according to the FDI World Dental Federation. I would classify this as sort of an epidemic, wouldn’t you? It’s quite a shocking number, but the severity and prevalence is real, and we need to take more measures in preventing it.
Q:
Can you die from gum disease?
A: You cannot die from gum disease, per se. Keep in mind that your mouth is linked to your systemic health, rather than an isolated ecosystem on its own. This means that gum disease can lead to or heighten other diseases related to your overall health.
As mentioned earlier, there is an inflammatory marker called C-reactive protein (CRP) that increases when infection triggers your immune system. This inflammatory marker has also been linked to cardiovascular disease. Periodontal treatment has shown to decrease inflammation and thus decrease CRP.
Gum disease has also been associated with complications such as diabetes, Alzheimer’s, and cancer to name a few.
Q:
Can I get rid of gum disease without a dentist?
A: The only stage you can get rid of without a dentist is Stage I, gingivitis. At this stage, a daily brushing and flossing regimen can reverse your gingival inflammation. As mentioned in the study conducted by Harald Loe, you can reverse your gingivitis in an average of 9-21 days if you are consistent (which you should always be).
However, if you surpass that stage and progress into advanced stages of gum disease, you will need the intervention of your dentist or hygienist. The reason for this being so is gingival recession, bone loss, and deep pocket depths cannot be reversed by simply brushing and flossing.
Depending on your symptoms and clinical manifestations, your dentist or periodontist will suggest a scaling-and-root planing procedure, flap surgery, or bone graft. Be open with your dentist about any questions or concerns you have with a procedure.
Q:
Does gum disease go away when teeth are removed?
A: In addition to cavities, gum disease is one of the major reasons for tooth extraction. Tooth extraction may be a treatment option to prevent infections from spreading and additional tooth loss. Extracting a tooth can lead to changes in your dietary habits, your bite, and your overall quality of life.
There are several elements that come into play here, such as the function of the specific tooth being extracted, how it will affect your mastication (chewing) after it is removed, and how deep the lesion is on that tooth. (18)
Ideally, dentists do not want to extract your teeth; our goal is to be as minimally invasive as reasonably possible. Unfortunately, the disease becomes so advanced in certain situations that the tooth has to come out to prevent further destruction.
Q:
How can I fix loose teeth from gum disease?
A: You definitely can’t go to a steakhouse with loose teeth. If your tooth is loose, but still in its socket, just keep it in place until you see a dentist. Until then, it is important you keep the area clean as it is now a risk for potential infection.
One way a dentist can tighten that loose tooth is through a process called “splinting.” The adjacent teeth are “splinted,” or attached together. This stabilizes any loose teeth and prevents them from moving.
Other treatments for loose teeth were discussed earlier such as deep professional cleanings, scaling-and-root planing, and bone grafting.
Key Takeaways: Gum Disease
Prevention is of utmost importance in your oral health as well as your systemic health. As we have seen, gum disease has been associated with a plethora of other problems. If you treat gum disease at an early stage, that will decrease your probability in treating other diseases.
If you make small, conscious decisions every day, you can save your oral health.
There are so many things you can do in your everyday routine to prevent you from getting gum disease. The types of foods you eat (or don’t eat), smoking cessation, daily brushing and flossing, and keeping up with dental checkups will go a long way.
You can reverse the beginning stage of gum disease. Gingivitis can be reversed completely by you, but you won’t know when it advances to a point where you can’t control it anymore.
Regular cleanings by your dentist or hygienist can prevent gingivitis from developing. Your routine check-ups will also allow your dentist to screen for anything that may or may not be suspicious, but if so, address and treat it promptly.
Got more questions about gum disease? Send a message to Dr. Burhenne and he can hook you up with whatever you need!
18 References
Tolmie, P., DDS, Rasenberger, K., DMD, & Van Kesteren, C., DDS. The Four Levels of Periodontal Disease. Retrieved from https://www.northstateperio.com/pdfs/newsletters/4%20Levels%20of%20Perio%20Dz.pdf
American Academy of Periodontology. Types of gum disease. Retrieved from: https://www.perio.org/consumer/types-gum-disease.html
Theilade, E., Wright, W. H., Jensen, S. B., & Löe, H. (1966). Experimental gingivitis in man: II. A longitudinal clinical and bacteriological investigation. Journal of periodontal research, 1(1), 1-13. Abstract: https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1600-0765.1966.tb01842.x
Pihlstrom, B. L., Michalowicz, B. S., & Johnson, N. W. (2005). Periodontal diseases. The lancet, 366(9499), 1809-1820. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/16298220
American Dental Hygienists’ Association. (1998). American Dental Hygienists’ Association Position Paper on the Oral Prophylaxis. Retrieved from: https://www.adha.org/resources-docs/7115_Prophylaxis_Postion_Paper.pdf
National Institutes of Health. (2008). Periodontal (Gum) Disease: Causes, Symptoms, and Treatments. Retrieved from https://www.nidcr.nih.gov/sites/default/files/2017-09/periodontal-disease_0.pdf
Chao, J. C. (2012). A novel approach to root coverage: the pinhole surgical technique. International Journal of Periodontics & Restorative Dentistry, 32(5). Abstract: https://www.ncbi.nlm.nih.gov/pubmed/22754900
Van Dyke, T. E., & Dave, S. (2005). Risk factors for periodontitis. Journal of the International Academy of Periodontology, 7(1), 3. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1351013/
AlJehani, Y. A. (2014). Risk factors of periodontal disease: review of the literature. International journal of dentistry, 2014. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4055151/
Taylor, G. W., Manz, M. C., & Borgnakke, W. S. (2004). Diabetes, periodontal diseases, dental caries, and tooth loss: a review of the literature. Compendium of continuing education in dentistry (Jamesburg, NJ: 1995), 25(3), 179-84. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/15641324
Bahekar, A. A., Singh, S., Saha, S., Molnar, J., & Arora, R. (2007). The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. American heart journal, 154(5), 830-837. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/17967586
Loos, B. G., Craandijk, J., Hoek, F. J., Dillen, P. M. W. V., & Van Der Velden, U. (2000). Elevation of systemic markers related to cardiovascular diseases in the peripheral blood of periodontitis patients. Journal of periodontology, 71(10), 1528-1534. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/11063384
Li, X., Kolltveit, K. M., Tronstad, L., & Olsen, I. (2000). Systemic diseases caused by oral infection. Clinical microbiology reviews, 13(4), 547-558. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC88948/
Abbayya, K., Puthanakar, N. Y., Naduwinmani, S., & Chidambar, Y. S. (2015). Association between periodontitis and Alzheimer’s disease. North American journal of medical sciences, 7(6), 241. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4488989/
Dominy, S. S., Lynch, C., Ermini, F., Benedyk, M., Marczyk, A., Konradi, A., … & Holsinger, L. J. (2019). Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Science advances, 5(1), eaau3333. Full text: https://advances.sciencemag.org/content/5/1/eaau3333
Demirer, S., Özdemir, H., Şencan, M., & Marakoḡlu, I. (2007). Gingival hyperplasia as an early diagnostic oral manifestation in acute monocytic leukemia: a case report. European journal of dentistry, 1(2), 111. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2609944/
American Academy of Periodontology. (2012). Retrieved from: https://www.perio.org/consumer/cdc-study.htm
Chrysanthakopoulos, N. A. (2011). Periodontal reasons for tooth extraction in a group of greek army personnel. Journal of dental research, dental clinics, dental prospects, 5(2), 55. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3429994/
The post Gum Disease: Stages, Prevention, and Treatment appeared first on Ask the Dentist.
Gum Disease: Stages, Prevention, and Treatment published first on https://wittooth.tumblr.com/
0 notes
Link
From a simple case of bleeding gums to painful gum recession, gum disease is a problem that you need to deal with as soon as possible.
Here, we’ll discuss the hierarchy of gum disease and what happens at each stage. You’ll also learn what you can do at home in your daily routine to prevent this from happening and protect your dental health.
If all else fails, fear not. Your dentist can help you with a treatment plan to manage gum disease at any stage of gum disease (officially dubbed “periodontitis”).
Gum Disease Signs and Symptoms
There are a few very common signs of periodontal disease to look for in your daily routine. These signs of gum disease may be signals that your gum health isn’t where it needs to be.
Red, swollen gums
Receding gums
Bleeding on brushing or flossing
Visible pus
Teeth feel loose and moveable
A change in your bite
Heightened sensitivity to hot or cold foods
Pain when chewing
A bad taste in your mouth
Persistent bad breath
A note of caution: Even if you do not have any of these symptoms, it is possible you still have gum disease.
Always go to your routine dental visits for check-ups—gum disease diagnosis is one reason you should stick to these appointments.
How Your Dentist Will Diagnose Gum Disease
When you show up for a dental appointment, you may not realize your dentist and hygienist are looking for gum disease symptoms. Here are some of what happens at your dental cleanings that can help recognize periodontitis.
1. Medical History
You may be thinking, “Did I come to the doctor’s office, or the dentist’s?” This is a common notion many people have when a dentist asks about certain diseases that run in their family, or if they’ve recently been diagnosed with any systemic conditions.
One reason for this is that any medication you may have been prescribed by your physician could cause severe consequences for your oral health.
For example, medications that have the side effect of causing a dry mouth, or “xerostomia,” can lead to tooth decay.
The saliva in our mouths helps us wash away food and other debris to rid of plaque. Plaque naturally forms a biofilm on the surface of our teeth after we eat or drink anything with carbohydrates or sugars.
Over time, if plaque is not removed regularly by brushing and flossing, it can lead to tartar buildup. Tartar is also called “calculus,” and it forms a yellow, brown deposit after plaque hardens. Unlike plaque, you cannot safely remove tartar on your own. This can only be done professionally by a dentist or dental hygienist.
2. Pocket Depth Measurement
This part of your dental exam and teeth cleaning is called “perio probing.” Here, dentists use an instrument called a periodontal probe with markings in millimeters used to measure the pocket depths around each and every tooth.
With firm and gentle pressure, the perio probe is inserted into your gingival sulcus, which is the space between your tooth and the gum surrounding it.
Healthy measurements are between 1-3mm of pocket depth.
Generally, anything deeper than that indicates gum inflammation that is making the pocket deeper. The deeper the pocket, the looser the gums surrounding your tooth, and the higher the degree of inflammation.
Another sign that your dentist or dental hygienist will look for when measuring pocket depth is bleeding upon probing. We may be poking at you, but a periodontal probe is blunted at the end, so it shouldn’t cause any bleeding in a healthy mouth. Bleeding upon probing is not considered normal and is one of the significant signs of gum inflammation.
It is really important that you don’t miss your regular check-ups and cleanings, or reschedule as soon as you can if something pops up. That way, anything out of the ordinary will be caught on early and promptly treated.
3. Dental X-Rays
The purpose of taking an x-ray (radiograph) is help your dentist examine everything in your mouth that is not visible to the naked eye.
The most commonly taken x-rays to evaluate gum disease are “bitewings.” There are four bitewings that are taken, one for each quadrant. Your dentist will be able to see everything from the top of your tooth to its roots, as well as the height of the bone around it.
The periodontal ligament, or PDL, serves as the supporting structure between the tooth and the bone. Bacteria can build up in deep periodontal pockets and cause destruction to the PDL, leading to bone loss and eventual tooth loss.
Taking bitewing x-rays will help your dentist assess if there are any changes to your jawbone as a result of gum disease.
Radiographs are not “one size fits all.” Your dentist will determine your oral profile risk and the frequency of x-rays needed. It may be as recent as every 6 months or only every couple of years.
The Stages of Gum Disease
There are four stages of gum disease, although the lines between these are a bit blurred.
Stage I: Gingivitis
This first stage of gum disease refers to inflammation of the gums.
Bacteria and plaque build up gradually over time along your gingival sulcus. Toxins released from this bacteria may cause deeper periodontal pockets due to damage of the PDL fibers that support the teeth and gums.
As mentioned previously, healthy gums have a probing depth of 1-3 mm. At the gingivitis stage, probing depths will be about 2-4 mm. (1)
You may also have other gingivitis symptoms, like:
Redness and swelling of the gums
Bleeding upon flossing
Bad breath
This is the mildest form of gum disease and therefore does not result in any bone loss or connective tissue loss. The good news is this stage is completely reversible and you can usually correct it at home! We’ll learn more about that later.
Stage II – III: Slight to Moderate Periodontal Disease
These two stages are grouped together because their effects are similar but gradual in strength.
The infection has now penetrated deep into your gums rather than along your gums. You will have:
Increased redness in your gums
More bleeding upon brushing
Worsening bad breath.
For slight periodontal disease, your dentist will observe 4-5 mm in probing depth. As for moderate periodontal disease, we will see probing depths at about 6-7 mm.
The deeper the infection gets into the gums, the greater the destruction of the PDL fibers, and the higher the probing depth.
At this point, the bacteria gets so entrenched into your gums that it actually begins to enter your bloodstream. This can compromise your immune system and might lead to or heighten your risk of other diseases (thanks, mouth-body connection!).
The main distinction from these stages in contrast to gingivitis is the start of bone loss. Bone loss here can range from 20-50%.
At this point, you cannot just cure gum disease at home. Treatment will require a consultation with your dentist.
Stage IV: Advanced Periodontal Disease
As you enter this stage of periodontal disease, bacteria has become more virulent.
You have pocket depths greater than 7 mm and the roots of your teeth may be exposed. Tooth mobility has increased significantly and tooth loss becomes very probable. This changes your overall bite and makes chewing more of a challenge.
Something else your dentist will see are pus-filled abscesses in and around your gums. These abscesses form in because immune system is trying to fight off the infection and keep it from spreading.
Bone loss at this stage is between 50-90%. Due to the severe infiltration of bacteria and the destruction it has caused to the integrity of your teeth, this final stage is only manageable with treatment, not reversible.
Types of Gum Disease
Gum disease happens for a number of reasons, and depending on the cause, it can progress more or less rapidly. The four types of gum disease can help your dentist determine the best course of treatment and help you with expectations for recovery. (2)
Chronic: Most common of the four types, chronic periodontitis is the gradual progression of inflammation in and around the gums. This typically happens slowly but can worsen rapidly at different points of the condition.
Aggressive: Typically seen in families, aggressive periodontitis often happens in healthy people and progresses faster than chronic periodontitis. There’s a likely genetic component to this type of gum disease.
Related to systemic disease: Certain diseases can manifest as gum disease. Periodontitis as a manifestation of systemic disease occurs most often in children with issues like diabetes, respiratory disease, or cardiovascular disease.
Necrotizing: In necrotizing periodontal disease, lesions cause necrosis (tissue death) of gingival tissue, periodontal ligament, and alveolar bone. People with these kinds of lesions are typically those with compromised immune systems, like patients with HIV, malnutrition, or other immune-compromising conditions.
Options for Gum Disease Treatment at Each Stage
Whether you’re struggling with advanced gum disease or the beginning stages of gingivitis, there are things you can do to keep your gums healthy.
In 1965, Dr. Harald Löe and his colleagues conducted a study called “Experimental Gingivitis in Man.”
Dr. Löe asked eleven healthy male dental students to be experimental subjects. The participants had their teeth cleaned and scaled to provide a baseline of their gingival health. They were then asked to cease all oral hygiene measures. That means no brushing, flossing, or mouth rinsing.
I imagine this might have been hard for their girlfriends. But, I digress.
As oral hygiene measures were withdrawn, plaque accumulated and the subjects developed gingivitis in a range of 9-21 days. They were then asked to begin oral hygiene measures again.
Although some men took a longer time to develop gingivitis, all the men returned to their normal, healthy status in about 7-11 days. They did this on their own, with no professional help, but only consistent oral care and hygiene. (3) Clearly, there’s something important in that daily routine!
Let’s look at the treatment options for each stage of gum disease.
1. Treatment for Gingivitis
The purpose of Dr. Harald Löe’s experiment (though this type of research is considered unethical in today’s research guidelines) was to prove that the mildest form of gum disease, gingivitis, is completely reversible.
Your dentist or hygienist will give you a dental prophylaxis, or “prophy.” This is what is known as a professional cleaning. (4) It will consist of supragingival (above the gum line) and subgingival (below the gum line) removal of plaque, calculus, and staining.
However, your provider can only do so much. The only way of reversing gingivitis at this stage is good oral hygiene on your part. Brushing twice a day for two minutes at a time, flossing at least once, and regular dental check-ups will get you back to a healthy smile.
If you notice bleeding gums more regularly than you’d like but your dentist hasn’t seen signs of more advanced gum disease, try some of the treatments for gingivitis Dr. Burhenne outlines here.
2. Treatment for Slight to Moderate Periodontal Disease
At this stage, the infection has gotten deep enough into your tissues that a prophy, brushing, or flossing just won’t cut it. Here, your dentist will introduce a non-surgical procedure called scaling and root planing procedure (SRP for short).
“Scaling” is when your provider cleans out the toxins in your periodontal pockets. “Root planing” is when he or she smooths out the surfaces of your roots to help your gums reattach. (5) Generally, this procedure causes very little discomfort. If you have sensitive teeth, your dentist may numb your gums with a local anesthetic.
An SRP can be done in a single visit, but it is usually broken up into appointments per quadrant (¼ of the mouth) or by halves, depending on the severity. After an SRP, your gums may feel tender and sensitive.
If you are consistent with a proper oral hygiene regimen after the procedure, your gums should turn back to their smooth texture and natural pink color within a few weeks.
Other ways to handle this stage of gum disease at home include a gum disease diet, using knotted floss to dislodge stubborn food particles, and trying mouth tape to cut down on mouth breathing at night.
3. Treatment for Advanced Periodontal Disease
Flap Surgery
At this stage, your bone and surrounding supporting tissue have been significantly destroyed. The objective of flap surgery is to reduce the depth of the periodontal pockets and regenerate the PDL fibers.
After numbing the area with local anesthetic, your dentist will make a flap-like incision around the gum tissue. The gums are lifted back, which allows a thorough cleaning of all the diseased tissue that has infiltrated. The flap is then sealed tightly so the gums fit snugly around the teeth and the healing process takes place.
After the procedure, you will have reduced pockets, which makes it easier to maintain your oral health. A combination of professional maintenance and consistent home care of your teeth will help prevent recurrence of this disease. (6)
Bone Graft
If you have teeth lost to gum disease, the bone around those teeth will also be lost. Since there is no support in that area, your skin will droop and it will give you an older-looking appearance.
Fortunately, bone grafting helps regenerate any bone that was lost to periodontal disease.
Essentially, what your dentist is doing is placing natural or synthetic bone that works with your body to help build new bone. Tissue-stimulating growth factor proteins may also be used to help your body regrow bone.
In cases with exposed tooth roots, your dentist may suggest a soft tissue graft. Recovery following the bone big graft procedure varies with each patient, but the entire healing process can take between 4-6 months.
Pinhole Surgery
This particular surgery hasn’t been around long, but some clinicians claim that pinhole surgery can help gum tissue grow back. (7) This would be revolutionary, and the preliminary results are good. However, this procedure is in its infancy and it’s not yet proven to be a long-term solution.
Causes and Risk Factors of Gum Disease
Depending on your individual genetics, lifestyle, diet, and other factors, you may be at a higher or lower risk of gum disease. Let’s look at what science tells us are the most common risk factors. (8, 9)
Smoking & Tobacco Use
This one is no surprise. Studies have shown that smoking causes an increase in gum recession and in bone loss.
If you are a current smoker, you have four times the chance of developing periodontal disease in relation to non-smokers.
Research also shows that periodontal therapy is less effective in smokers than it is in non-smokers. Be above the influence, friends.
Genetics
There has been research done in twins that suggest “50% of susceptibility to [gum] disease is due to host factors.” This could be because twins share very similar environmental and behavioral exposures.
Stress
Everybody suffers from chronic stress in his or her own way. People with higher levels of stress have a greater incidence of developing periodontal disease.
Stress depresses our immune system and causes an imbalance in our homeostasis. When you are stressed out, you release a higher number of inflammatory cells, which can promote tissue damage.
Another reason stress is associated with poor oral hygiene is sometimes, you have other things preoccupying your mind. You may not be giving your oral hygiene the attention it needs in times of emotional stress.
The key takeaway here is: we all need a good massage or a spa day every once in a while. Grab some friends and try to unwind; your mouth will thank you.
Medication
Some medications decrease your salivary flow, which impacts its ability to wash away plaque and debris. This is important because saliva helps prevent plaque buildup and gum inflammation.
These medications include but are not limited to:
Antihistamines
Antihypertensives
Anticonvulsants
Sedatives
Ask your physician if any of the medications you’ve been prescribed causes dry mouth, or “xerostomia.” If so, perhaps your dentist and physician can work together to find another alternative.
Orthodontic Treatment
Some types of partial dentures, braces, or other orthodontic devices can make it hard to remove all the tartar and calculus buildup common to gum disease.
Diet
Studies in adolescents aged 11-18 have shown that kids in this age group do not eat many fruits and vegetables, which are sources high in vitamin C. Moreover, calcium-rich beverages such as milk have decreased while sugary beverages such as sport-drinks have increased.
A decrease in calcium and vitamin C have been associated with an increased risk of periodontal disease.
In general, a diet heavy on carbohydrates (breads, pastas, crackers, sugary treats, etc.) is going to be bad for oral health, particularly when you aren’t keeping up with dental hygiene as well. Keep in mind that your mouth and body as a whole need healthful, whole foods to function well.
Age
There is a caveat to this one: the risk of gum disease doesn’t just go up because a person merely gets older; it’s tied in to various other factors.
For example, as we get older, we lose some of our manual dexterity and thus cannot brush as well as we used to. You may become more forgetful and forget to practice as oral hygiene on a daily routine.
People are also living longer! As we’re retaining our teeth for a longer period of time, they need to be maintained for a longer period of time. This can be hard to do since as we age, we naturally develop many other systemic diseases that negatively impact our oral health.
This brings us to the next point.
Periodontitis and Other Diseases
When you think about gum disease, you shouldn’t think only of your oral health. There are connections between gum disease and other health problems, including diabetes, heart disease, Alzheimer’s, pneumonia, and even cancer.
Diabetes
Poor glycemic control has been associated with higher rates of periodontal disease. (10) The good news is that patients with controlled diabetes respond favorably to periodontal treatment. Check your HbA1c count regularly to make sure your blood sugar is in the target range.
You may also want to consider natural diabetes treatment options, like dietary alteration. These have a great track record of effectively managing blood sugar and A1c levels.
Heart Disease
There has been a lot of research done on the association between cardiovascular disease and periodontitis. High cholesterol and atherosclerotic plaque together may increase the risk for chronic periodontitis. (11)
We have many different inflammatory markers in our bodies that serve a variety of functions. Generally, they are increased when there is injury somewhere in your body and your immune system is trying to defend you.
Both periodontitis and heart disease are associated with the same increase in inflammatory markers, C-reactive protein (CRP) and Interleukin-6 (IL-6). (12)
The only confirmed causal link between oral disease and systemic infection is that of infective endocarditis, an inflammation in the lining of the heart. (13)
Bacteria are more likely to escape into the bloodstream when the biological width, the seal of gums to teeth that serves to protect the alveolar bone, isn’t healthy, like in gum disease. These bacteria can then collect on the heart to cause endocarditis—which is most likely after a root scaling and planing.
Alzheimer’s Disease
There are two mechanisms by which association Alzheimer’s and gum disease are explained.
One theory is that the bacteria in gum disease that seeps into your bloodstream increases inflammatory markers, which leads to systemic inflammation. These markers are capable of crossing into the brain and leading to neuronal damage.
The second mechanism is explained by the bacteria from your plaque crossing into the brain. Dental plaque enters the brain via the bloodstream or peripheral nerves. This organisms then cause and inflammatory response in your central nervous system (CNS), which leads to cognitive impairment. (14)
A team of researchers released a compelling study in 2019 introducing a possible causation between gum disease and Alzheimer’s. (15) While this hasn’t been confirmed by other studies or human trials, it’s enough to consider being more diligent treating gum disease.
Hematologic Disorders (Leukemia)
Gingival hyperplasia, which is overgrowth of gum tissue around the teeth, can be an early symptom of acute leukemia. (16)
Chemotherapy or bone marrow transplantation can also negatively affect gingival health. Some of the symptoms are abscesses, inflamed gums, or severe redness.
Pneumonia
The same people at risk for pneumonia are typically those at risk for gum disease. Although it’s not clear if one causes or contributes to the other, they are closely connected.
One proposed reason for this connection is that patients in hospitals and nursing homes that frequently contract pneumonia also can’t keep up with good oral care. This may upset the oral microbiome and set the stage for other immune system-compromising infection. (13)
How to Prevent Gum Disease
There are several things you can do regularly if you notice warning signs of gum disease—or to prevent these from ever happening.
Brush twice a day for 2 minutes. Use your smartphone or a brush timer as a measurement of time to how long you’ve been brushing.
Floss at least once a day to remove plaque from places your toothbrush can’t get access to. You know when your mom tells you to clean your room, and you think it’s clean, but then she goes in and finds areas that aren’t really clean? It’s basically the same concept, but with flossing.
Avoid smoking (anything) and all forms of tobacco. This includes cigarettes, cigars, “dip” or chewing tobacco, and hookah. Being healthy is the new cool.
Maintain a healthy diet. Now, I’m not telling you to go vegan, but I am telling you that it’s important to add fruits and vegetables to get your daily dose of vitamin C and calcium.
Ask your physician if any of your medications cause dry mouth, or “xerostomia.” If they do, ask if there are any other alternatives available. It’s important for different healthcare providers to be in contact so we can provide you with the best possible care.
Tape your mouth shut at night. Weird habit, but great results. Mouth taping cuts down on mouth breathing while you sleep. This, in turn, can help resolve dry mouth.
Don’t use conventional mouthwash. I know what you’re thinking. This is the stuff that’s supposed to give me a cleaner mouth and me have kissable breath! But it’s just not good for your oral health.
So many mouthwashes have a high alcohol content, which dries your mouth and disrupts your oral microbiome. Dry mouth and an imbalance of bacteria are both risks for plaque retention. You can read more about other DIY mouthwash alternatives here.
Try natural methods of gum disease prevention. These may include using turmeric in a lot of your recipes, oil pulling, and taking oral probiotics to support a healthy oral microbiome.
Into DIY-ing? Dr. B created a great DIY recipe for toothpaste specifically for healthier gums. You can check it out and try it for yourself by reading this article.
Always, always schedule regular check-ups and professional cleanings. You will have a much less chance of developing anything suspicious if your dentist is monitoring your health. Remember, preventative is always better than constructive!
Common Questions About Gum Disease
Q:
What’s the difference between gingivitis and gum disease?
A: Gingivitis is the early, reversible stage of gum disease. The main difference here is that in gingivitis, there is no loss of bone or loss of connective tissue. Not all cases of gingivitis result in gum disease, but it can if left untreated.
Once bacteria have seeped deep below your gum line, it starts to destroy gum tissue, your periodontal pockets deepen, and some of your bone is lost. Your teeth become mobile and loose because it doesn’t have as much support from bone anymore. This is when you have advanced into Stages II-IV of periodontitis.
Q:
How common is gum disease?
A: Very common! In a study titled “Prevalence of Periodontitis in Adults in the United States” found that 47.2% or roughly 64.7 million American adults have either mild, moderate, or severe periodontal disease. This is even higher in adults aged 65 and older, at about 70.1%.
On a greater scale, we are looking at 743 million people afflicted, according to the FDI World Dental Federation. I would classify this as sort of an epidemic, wouldn’t you? It’s quite a shocking number, but the severity and prevalence is real, and we need to take more measures in preventing it.
Q:
Can you die from gum disease?
A: You cannot die from gum disease, per se. Keep in mind that your mouth is linked to your systemic health, rather than an isolated ecosystem on its own. This means that gum disease can lead to or heighten other diseases related to your overall health.
As mentioned earlier, there is an inflammatory marker called C-reactive protein (CRP) that increases when infection triggers your immune system. This inflammatory marker has also been linked to cardiovascular disease. Periodontal treatment has shown to decrease inflammation and thus decrease CRP.
Gum disease has also been associated with complications such as diabetes, Alzheimer’s, and cancer to name a few.
Q:
Can I get rid of gum disease without a dentist?
A: The only stage you can get rid of without a dentist is Stage I, gingivitis. At this stage, a daily brushing and flossing regimen can reverse your gingival inflammation. As mentioned in the study conducted by Harald Loe, you can reverse your gingivitis in an average of 9-21 days if you are consistent (which you should always be).
However, if you surpass that stage and progress into advanced stages of gum disease, you will need the intervention of your dentist or hygienist. The reason for this being so is gingival recession, bone loss, and deep pocket depths cannot be reversed by simply brushing and flossing.
Depending on your symptoms and clinical manifestations, your dentist or periodontist will suggest a scaling-and-root planing procedure, flap surgery, or bone graft. Be open with your dentist about any questions or concerns you have with a procedure.
Q:
Does gum disease go away when teeth are removed?
A: In addition to cavities, gum disease is one of the major reasons for tooth extraction. Tooth extraction may be a treatment option to prevent infections from spreading and additional tooth loss. Extracting a tooth can lead to changes in your dietary habits, your bite, and your overall quality of life.
There are several elements that come into play here, such as the function of the specific tooth being extracted, how it will affect your mastication (chewing) after it is removed, and how deep the lesion is on that tooth. (18)
Ideally, dentists do not want to extract your teeth; our goal is to be as minimally invasive as reasonably possible. Unfortunately, the disease becomes so advanced in certain situations that the tooth has to come out to prevent further destruction.
Q:
How can I fix loose teeth from gum disease?
A: You definitely can’t go to a steakhouse with loose teeth. If your tooth is loose, but still in its socket, just keep it in place until you see a dentist. Until then, it is important you keep the area clean as it is now a risk for potential infection.
One way a dentist can tighten that loose tooth is through a process called “splinting.” The adjacent teeth are “splinted,” or attached together. This stabilizes any loose teeth and prevents them from moving.
Other treatments for loose teeth were discussed earlier such as deep professional cleanings, scaling-and-root planing, and bone grafting.
Key Takeaways: Gum Disease
Prevention is of utmost importance in your oral health as well as your systemic health. As we have seen, gum disease has been associated with a plethora of other problems. If you treat gum disease at an early stage, that will decrease your probability in treating other diseases.
If you make small, conscious decisions every day, you can save your oral health.
There are so many things you can do in your everyday routine to prevent you from getting gum disease. The types of foods you eat (or don’t eat), smoking cessation, daily brushing and flossing, and keeping up with dental checkups will go a long way.
You can reverse the beginning stage of gum disease. Gingivitis can be reversed completely by you, but you won’t know when it advances to a point where you can’t control it anymore.
Regular cleanings by your dentist or hygienist can prevent gingivitis from developing. Your routine check-ups will also allow your dentist to screen for anything that may or may not be suspicious, but if so, address and treat it promptly.
Got more questions about gum disease? Send a message to Dr. Burhenne and he can hook you up with whatever you need!
18 References
Tolmie, P., DDS, Rasenberger, K., DMD, & Van Kesteren, C., DDS. The Four Levels of Periodontal Disease. Retrieved from https://www.northstateperio.com/pdfs/newsletters/4%20Levels%20of%20Perio%20Dz.pdf
American Academy of Periodontology. Types of gum disease. Retrieved from: https://www.perio.org/consumer/types-gum-disease.html
Theilade, E., Wright, W. H., Jensen, S. B., & Löe, H. (1966). Experimental gingivitis in man: II. A longitudinal clinical and bacteriological investigation. Journal of periodontal research, 1(1), 1-13. Abstract: https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1600-0765.1966.tb01842.x
Pihlstrom, B. L., Michalowicz, B. S., & Johnson, N. W. (2005). Periodontal diseases. The lancet, 366(9499), 1809-1820. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/16298220
American Dental Hygienists’ Association. (1998). American Dental Hygienists’ Association Position Paper on the Oral Prophylaxis. Retrieved from: https://www.adha.org/resources-docs/7115_Prophylaxis_Postion_Paper.pdf
National Institutes of Health. (2008). Periodontal (Gum) Disease: Causes, Symptoms, and Treatments. Retrieved from https://www.nidcr.nih.gov/sites/default/files/2017-09/periodontal-disease_0.pdf
Chao, J. C. (2012). A novel approach to root coverage: the pinhole surgical technique. International Journal of Periodontics & Restorative Dentistry, 32(5). Abstract: https://www.ncbi.nlm.nih.gov/pubmed/22754900
Van Dyke, T. E., & Dave, S. (2005). Risk factors for periodontitis. Journal of the International Academy of Periodontology, 7(1), 3. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1351013/
AlJehani, Y. A. (2014). Risk factors of periodontal disease: review of the literature. International journal of dentistry, 2014. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4055151/
Taylor, G. W., Manz, M. C., & Borgnakke, W. S. (2004). Diabetes, periodontal diseases, dental caries, and tooth loss: a review of the literature. Compendium of continuing education in dentistry (Jamesburg, NJ: 1995), 25(3), 179-84. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/15641324
Bahekar, A. A., Singh, S., Saha, S., Molnar, J., & Arora, R. (2007). The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. American heart journal, 154(5), 830-837. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/17967586
Loos, B. G., Craandijk, J., Hoek, F. J., Dillen, P. M. W. V., & Van Der Velden, U. (2000). Elevation of systemic markers related to cardiovascular diseases in the peripheral blood of periodontitis patients. Journal of periodontology, 71(10), 1528-1534. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/11063384
Li, X., Kolltveit, K. M., Tronstad, L., & Olsen, I. (2000). Systemic diseases caused by oral infection. Clinical microbiology reviews, 13(4), 547-558. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC88948/
Abbayya, K., Puthanakar, N. Y., Naduwinmani, S., & Chidambar, Y. S. (2015). Association between periodontitis and Alzheimer’s disease. North American journal of medical sciences, 7(6), 241. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4488989/
Dominy, S. S., Lynch, C., Ermini, F., Benedyk, M., Marczyk, A., Konradi, A., … & Holsinger, L. J. (2019). Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Science advances, 5(1), eaau3333. Full text: https://advances.sciencemag.org/content/5/1/eaau3333
Demirer, S., Özdemir, H., Şencan, M., & Marakoḡlu, I. (2007). Gingival hyperplasia as an early diagnostic oral manifestation in acute monocytic leukemia: a case report. European journal of dentistry, 1(2), 111. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2609944/
American Academy of Periodontology. (2012). Retrieved from: https://www.perio.org/consumer/cdc-study.htm
Chrysanthakopoulos, N. A. (2011). Periodontal reasons for tooth extraction in a group of greek army personnel. Journal of dental research, dental clinics, dental prospects, 5(2), 55. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3429994/
The post Gum Disease: Stages, Prevention, and Treatment appeared first on Ask the Dentist.
from Ask the Dentist https://askthedentist.com/gum-disease-stages-prevention-treatment/
0 notes
Text
I Did The Keto Diet Where I Ate All Fat And No Carbs & It Went Better Than You’d Expect
Welcome to the fourth installment of the Fad Diet Diaries: a series of experiments, where I willingly put myself through diets that range from challenging to questionable to downright abhorred by the medical community and then record my experience so that other people can learn from my mistakes. Both my doctor and my metabolism are thrilled.
While in the past I’ve tested out crash cleanses, obscure 90s fad diets, and completely arbitrary food challenges, set by people at , this round of dieting was a truly unique experience. Why? Because it was kind of healthy.
For the past two weeks I have been living the ketogenic lifestyle, which I’ve been describing to people as Atkins on Crisco. It entails cutting out essentially all carbs and sugars and sustaining yourself on a diet of high-fat foods. If this sounds like a dream to you, it’s because it kind of is. For instance, if you’ve ever found yourself in bed at 10pm on a Thursday night, wishing you had a bowl of sour cream and carnitas in front of you, you’ll want to keep reading.
The purpose of this diet is to put yourself into a metabolic state called ketosis, which is a natural process that your body initiates when carb intake is low. Essentially, instead of burning carbs for energy, your body is burning fats. You are quite literally eating fats to burn and lose weight, and it sounds fake until you suddenly fit into a pair of pants you haven’t been able to wear since junior year of college.
This website will explain the scientific side of this better than I will ever be able to and serves as a really great introduction for people who are looking to dive into a keto lifestyle.
While keto is more of a lifestyle than a fad diet, I’ve decided it falls into the realm of this series, because people won’t stop talking about it. Originally promoted as a way to help regulate epilepsy and diabetes, keto is receiving a seal of approval from fitness fanatics, professional athletes, and people who just really like high-maintenance diets. On the other end of the spectrum, you have your usual skeptics and assorted doctors who really wish that people would stop creating fad diets so that their patients will stop coming in quoting Dr. Oz. This sounded like an argument that I wanted to drop myself directly into the middle of.
The diet breakout looks something like this: 70% fat, 25% protein, and 5% carbs. You can get your own specific macros calculated on any number of online keto calculators, which make you do inhumane things like try and figure out your body fat percentage. My requirements were 1,531 calories a day, 119g of fat, 95g of protein, and a mere 20g of carbs.
For reference, there are 48g of carbs in one bagel. Half a bagel would max out my entire carb intake for one day and likely destroy any ketosis that I had established. I know most of you likely just checked out, but stay with me here.
And the thing is, the allowed 20g of carbs aren’t fun carbs like bread or apple cider donuts that a girl in your office had shipped fresh from New York on day two of your diet. They’re hidden carbs that live in foods you thought were safe, like arugula and mushrooms. What I began to refer to as “sleeper carbs” were nearly my downfall and the cause of one of the most dread-filled Sunday nights of my entire life. Don’t worry, we’ll get there.
In order to ensure that you’ve reached ketosis, you get to pee on these little strips that tell you if your body is expelling high levels of ketones with a color scale that quite easily allows you to mistake one level for another, and will have you sitting and examining a strip of paper, covered in your own urine, for longer than you’d like to admit it. Accept this as your new normal.
The test strips are a bit controversial in that they don’t work for everyone, and for some, are less of a measure of your level of ketone creation and more of a litmus test for simply whether you’re in ketosis or not. If you’re a die-hard follower and want the truest measurement, the best route is a blood test, for which you can buy a handy gadget and perform at home. My needle-phobic ass will stick to examining my own pee, thanks.
Other things that will become your new normal: consuming 100+ grams of fat a day, drinking butter, having meltdowns at 8:30pm when you realize you’re still 60 grams of fat short of your daily goal, being that asshole at a restaurant who orders deconstructed burgers with every imaginable sauce removed, and in a moment of weakness, spending $30 on the most pretentious ingredients you can find at your nearest New Seasons, so you can splurge on a keto-safe cookie dough concoction that you’re really going to hate yourself for eating.
The hardest part of this diet wasn’t necessarily following it, but getting into the mindset that not only is it okay to be eating fats, but that you have to do it to keep yourself going.
I, like most women, have grown up in a body-shaming, lady-hating, diet-purporting society that has conditioned me to avoid fats like my life depended on it. In fact, we’ve been taught that our lives do actually depend on it, lest we fall victim to such horrors as high blood pressure, bad cholesterol, or, God forbid, being bigger than a size 6.
But I just spent the last two weeks indulging in eggs fried in butter, bacon, cream cheese, and all the avocado my heart desired, and guess what? I lost nine pounds, went down an entire pant size, and suffered what can only be described as an existential crisis, when I realized that I don’t know how the fuck food or my body works.
If this sounds equal parts enjoyable, eye-opening, and entirely overwhelming, that’s because it was. I know I’ve painted the whole experience as a dream come true, but there were considerable downsides as well. For one, in order to live as true to the lifestyle as possible, I committed to tracking my macros to ensure I was meeting my daily requirements (spoiler alert: I rarely did). This entailed painstakingly measuring out—or in my case, wildly estimating—the exact amount of each individual ingredient I was consuming and putting it into an app that would tell me whether or not I was failing.
Is failing the right word to use, considering I still lost weight and reaped the benefits of a keto diet? Probably not, but that’s certainly what it felt like. While the food was enjoyable, and I’m pleasantly surprised by the end results, a diet shouldn’t make me feel the way that AP Tests and the SAT did; I shouldn’t be having stress dreams about eating an entire cake and immediately throwing my body out of ketosis.
A regular diet is stressful in its own right, but one that makes you meticulously track everything you put into your mouth is a giant undertaking. There were times that I just opted not to eat, because the thought of recording a meal sounded exhausting.
Other negative side effects that one could experience include: muscle cramps due to lack of magnesium (check), sudden drop-offs in energy while your body adapts to this new reality (check), the keto flu—a period of during the induction phase where one might suffer flu-like symptoms due to a lack of electrolytes (thankfully avoided), and zero tolerance for any bullshit from anyone (potentially just me).
What was shocking was how quickly I adapted to this new way of life. Unlike most of my diets where each day brought a new hurdle, either physical or emotional, the reality of keto set in quickly. The second half of the journey moved along smoothly, and I didn’t even find myself wishing for it to end, but that first week was a whirlwind of discovery.
Day One
This first day was exciting in the way these experiments always are in the beginning. I’m out here trying something entirely new and haven’t stooped to the point of hating myself for it yet. Everything is still a novelty, and I haven’t had to embarrass myself at a restaurant by asking for the sugar content of the house Bloody Mary Mix. Everything was bright and shiny.
I learned a couple things really quickly, both through the way I felt and the sage wisdom of my keto coach, a friend who willingly lives like this as an actual preference and not just so she can publish a bunch of jokes about it online. Some people are just enlightened, I guess.
The first lesson: Bodies in ketosis require almost double the amount of water as normal, because your liver is doing a lot more work than usual. This was rough to hear, considering that, on a good day, I drink about half as much water as an adult human should. In light of this news, I downloaded an app to remind me to drink water, because I’m the kind of person that needs technology to remind her to meet the baseline requirements for survival. All in all, things were off to a good start.
Day Two
On day two, I discovered butter coffee, which is exactly what it sounds like: a tablespoon of grass-fed butter and sixteen ounces of black coffee, thrown into a blender. What comes out tastes more like a latte than anything else, and drinking it for the first time felt like what I would imagine it’s like to live life in all caps. I don’t think I’ll ever again reach the level of euphoria that I experienced that first buttery morning, but I’ll dream of it for the rest of my days, chasing that butter coffee dragon.
To be clear, there’s a method behind the madness of drinking a tablespoon of butter first thing every morning. First and foremost, as previously mentioned, I had a hard time squeezing all recommended 119g of fat into my diet, so starting out my day with a steaming cup of butter was actually really helpful. Beyond that, your body takes longer to metabolize fats, which means butter coffee is supposed to keep you energized longer, rather than offering a spike of caffeine in the morning and dropping off by lunch. I found this to be true, because I no longer required my usually mandatory 2pm cup of coffee to make it through the work day.
If a 7am butter coffee was the high of day two, then you could say the low was a mere 12.5 hours later, when I found myself sitting on my patio in the dark, eating rotisserie chicken directly out of the bag, an event spurned by the fact that I had finally checked my macros for the day, and found I was insufficient in just about everything but carbs, which I’d already maxed out at 20g.
It was at this point that I realized that this diet had a definite learning curve, something that I really wasn’t accustomed to. Rather than depriving myself and accepting the suffering, I needed to plan my entire day around meeting dietary requirements that I couldn’t really even fathom. Luckily, there are hundreds of forums, Facebook groups, and Pinterest pages dedicated to this very idea. Did I check any of those? Absolutely not, but it probably would have been a good idea.
Day Three
Day three was when the reality of what macro tracking meant really set in. I am but a simple American, who barely has a grasp on our standard system of measurement, let alone the metric one. Keto does not care about my mathematical inadequacies. This diet is out here asking me to estimate the number of grams of salmon I’m consuming in a single day.
“Idk, like a handful of spinach” isn’t an option on my tracking app, and my kitchen is sorely lacking in basic measurement tools, which left me frequently Googling conversion calculators and trying to rationalize amounts of food by comparing them to items that had their weights listed. In short, it was a fucking train wreck.
After the great rotisserie chicken debacle of the night before, I vowed to never fall victim to macro deficiency again and grabbed a pack of bacon on the way home from work. The second major hurdle of this diet was the fact that I had to spend a substantial amount of time cooking every night. Although it’s been covered in every installment of this series, it probably bears importance in repeating that I am not a cook by any stretch of the word, and any meal that takes more than 15 minutes to prepare just seems exorbitant.
And yet, I found myself that night spending 45 minutes frying up an entire pack of bacon. Should it take that long to cook bacon? Probably not. But things like logic and cook times have never applied to me, and they weren’t about to start this week.
My next lesson was in sleeper carbs and the fact that even if you’re positive you haven’t touched a single carbohydrate all day, you can still rack up about 12g too many of them. The culprit? Vegetables, whom I’d always considered to be a safe and reliable friend, were secretly carrying carbs and betraying any trust established between us. Et tu, arugula?
Day Four
Day four was a turning point, one of the first times I thought to myself, “Maybe this should be something I just do all the time.” What could possibly drive me to consider a lifetime without carbs and sugar? It’s simple really: natural energy, something this body hasn’t experienced since the tender age of 12.
On this momentous day, I woke up on my very first alarm. To some, this is just a mundane requirement of being an adult and making it to work on time, but for me? Unheard of. I am a five alarm girl, set at five-minute intervals for optimal suffering. I usually drag my lifeless body out of bed about 10 minutes after that fifth alarm and proceed to caveman around the house until I’ve deemed myself presentable enough to wander into work and directly to the coffee machine.
But on day four, I sprang out of bed at a chill 6:40am with a sizable craving for butter coffee and the drive to get out of the house as soon as humanly possible.
Improved energy is, in fact, a side effect of this diet. Fat is the body’s largest and most efficient source of energy, and you’ve just about doubled your intake of it. The result is that you aren’t spending time working through heavy carbs anymore, just burning through these high-energy molecules, which are making you feel truly awake for the first time in your cursed life.
In my case, it was also making me second-guess a lot of things that I had never questioned before. For instance, I am now almost 99% sure that I’ve spent my entire life mistaking the signs of dehydration for anything but that. On my way to work that morning, I thought, “Hm, I’d really love another cup of coffee,” and then stopped myself, because that wasn’t actually what I wanted at all. I was thirsty and finally recognizing it for what it was. Natural selection is truly slacking in my case.
You might be asking yourself how I’ve made it a full 25 years without being able to tell if my body was in need of water or not, and I’m here to tell you that I have no idea. But now that I’m drinking 2.5 liters of water a day, I’ve finally begun to understand what a baseline craving for hydration feels like. Let me tell you, it’s wild.
Day Five
I had made it to Friday and had done pretty well for myself, so on day five, I decided it was time for a treat: professional butter coffee. It’s actually called Bulletproof Coffee, and it’s basically butter coffee with the addition of MCT oil, a naturally occurring oil that is supposed to boost energy and burn fat like crazy.
Was it weird at first? For sure. I had grown accustomed to my butter lattes, and this was less of a soothing morning ritual and more so on par with what I would expect it’s like to do angel dust for the first time. I didn’t really know how to process it until I was about a third of the way through and my body took over. Suddenly, I needed to drink the rest of it, and it needed to happen as quickly as humanly possible.
It was like I had transcended mundane things like taste buds in favor of becoming omnipotent. I could see new colors. Conversations around me slowed down. I got more work done on that single day than I had all week, and it was all due to this $6 oily, buttery, bitter concoction that I will never stop thinking about. I was riding on an absolute high, ready to adopt a keto diet for life, until suddenly I wasn’t.
There was a flurry of reasons for that abrupt turn of events that all culminated in one thing: alcohol. Naturally.
Maybe it was the Bulletproof coffee, or my intense focus, but I didn’t drink nearly as much water as I should have on Friday. Realizing this around 4pm was the first red flag that put me off-kilter. A work happy hour led to a birthday party, which led to a bar, which led to another bar, which ultimately led to me standing in front of a Mediterranean food cart at 2am trying to rack up the 1,000 calories I was supposed to have consumed throughout the day, while explaining to a confused, bemused, but accommodating Middle Eastern man what exactly ketogenic diets entail.
All week I had been shaping my plans and schedule so specifically around this diet, but day five was the first day that life intervened. Sometimes, you’re going to be out and about and won’t be able to find a high-fat, moderate protein meal that adheres exactly to your needs. Sometimes you’re going to fall off the wagon, because you’ve had a shitty day and you need to. Sometimes you’re going to accidentally get super drunk on a Friday, because you would have been racked with FOMO if you hadn’t gone to the cool rooftop happy hour.
And all of that is okay! You can have those off days, as long you wake up the next morning and rededicate yourself to your goals.
Let me tell you, that is exactly what I did.
Day Six
I don’t know how to explain the way I felt Saturday morning. I woke up… energized?
The three tequila Diet Cokes (it pains me to write that) and two vodka sodas I consumed the night before? Gone.
Any exhaustion that may have stemmed from the fact that I went to bed at 3am and woke up naturally at 8am? Gone.
A sudden need to grocery shop, clean my room, do the dishes, buy a wall calendar to map out the rest of these diets, and just generally get my life together ARRIVED.
Here I was, making the most of a Saturday morning, planning for my week ahead and feeling slightly guilty for consuming alcohol. It wasn’t even the “I blacked out and embarrassed myself” guilt but a completely foreign “I didn’t really need to drink alcohol at all last night” kind. It was during those abundantly productive hours that I first questioned whether this diet was turning me into a functional adult. Or at the very least, someone who could pass for one. I bought a relaxing nighttime tea, for God’s sake. What next? Learning how to make sous vide eggs?
Day Seven
All the serenity of Saturday was completely spent by the time Sunday rolled around. I was coming up on one week of this diet, and the only thing I really felt was stressed out. Well, skinny and stressed out. I had yet to figure out a solution to sleeper carbs and was on the verge of a nervous breakdown, trying to reconcile this newfound, entirely one-sided feud with vegetables that I was harboring.
I hadn’t experienced a Sunday night woe like this since high school, at which point I consulted my keto coach who encouraged me to throw caution to the wind and indulge in a meal consisting solely of eggs, butter and meat. Decadent doesn’t begin to describe the way I felt.
Sunday night was a true breakthrough in both keto and probably just my adult life: I had finally allowed myself to eat something that a past me would have deemed wildly unacceptable. I’d dismantled the mental block that told me a meal wasn’t complete if it wasn’t 50% green and leafy. I wasn’t “treating myself” or “having a cheat meal.” I was eating fucking dinner, and it was glorious and liberating, and I was evolving my relation with food.
From that moment forward, I was a new person. I no longer shied away from the high-fat foods, that I was supposed to be embracing. I committed to drinking water, not just for the diet, but also for myself. I slowly began to relax my meal planning, allowing myself to eat out and not slave over tracking nuances. I ate a shit ton of bacon. And come the two-week mark, I’d lost nine pounds.
Every diet in this series has taught me something about myself: that I am capable of superhuman levels of self-control when I need to be, that I can eat an inhumane amount of ice cream and still kind of function, and that I can accomplish just about anything that I set my mind to, even if my body is begging me not to.
But this is the first diet to show me that maybe my regular habits aren’t all that much better than the ones I force upon myself, for the sake of these articles. Eating healthy is all well and good, but not if you’re punishing yourself after a moment of weakness. Hell, maybe they shouldn’t be called moments of weakness, but moments where I really wanted a muffin, and so I ate a goddamn muffin.
Does this mean I’m fully committed to a keto lifestyle from here on out? Not necessarily. Lazy keto, a diet that still follows ketogenic rules but doesn’t force you to track your macros or panic over vegetable carbs, seems more up my alley and is something I could see myself adopting between diet ventures. But I’m also acutely aware that fall is here and with it the great love of my life: kettle corn. I won’t deprive myself of that, and I also won’t gorge myself with it. I’ll enjoy a responsible amount and determinedly not feel bad about it.
In the end, the ultimate irony is that a high-fat, indulgent diet has brought a sense of balance to my life that I hadn’t realized I was missing. Somehow, on this never-ending quest to test every possible limit my body possesses, I’ve managed to stumble upon something worthwhile.
No promises that it will ever happen again, but I’m pretty happy with myself in the meantime.
Read more: http://ift.tt/2wpLDdj
from Viral News HQ http://ift.tt/2xqXs3i
via Viral News HQ
0 notes
Link

Welcome to the fourth installment of the Fad Diet Diaries: a series of experiments, where I willingly put myself through diets that range from challenging to questionable to downright abhorred by the medical community and then record my experience so that other people can learn from my mistakes. Both my doctor and my metabolism are thrilled.
While in the past I’ve tested out crash cleanses, obscure 90s fad diets, and completely arbitrary food challenges, set by people at , this round of dieting was a truly unique experience. Why? Because it was kind of healthy.
For the past two weeks I have been living the ketogenic lifestyle, which I’ve been describing to people as Atkins on Crisco. It entails cutting out essentially all carbs and sugars and sustaining yourself on a diet of high-fat foods. If this sounds like a dream to you, it’s because it kind of is. For instance, if you’ve ever found yourself in bed at 10pm on a Thursday night, wishing you had a bowl of sour cream and carnitas in front of you, you’ll want to keep reading.

The purpose of this diet is to put yourself into a metabolic state called ketosis, which is a natural process that your body initiates when carb intake is low. Essentially, instead of burning carbs for energy, your body is burning fats. You are quite literally eating fats to burn and lose weight, and it sounds fake until you suddenly fit into a pair of pants you haven’t been able to wear since junior year of college.
This website will explain the scientific side of this better than I will ever be able to and serves as a really great introduction for people who are looking to dive into a keto lifestyle.
While keto is more of a lifestyle than a fad diet, I’ve decided it falls into the realm of this series, because people won’t stop talking about it. Originally promoted as a way to help regulate epilepsy and diabetes, keto is receiving a seal of approval from fitness fanatics, professional athletes, and people who just really like high-maintenance diets. On the other end of the spectrum, you have your usual skeptics and assorted doctors who really wish that people would stop creating fad diets so that their patients will stop coming in quoting Dr. Oz. This sounded like an argument that I wanted to drop myself directly into the middle of.
The diet breakout looks something like this: 70% fat, 25% protein, and 5% carbs. You can get your own specific macros calculated on any number of online keto calculators, which make you do inhumane things like try and figure out your body fat percentage. My requirements were 1,531 calories a day, 119g of fat, 95g of protein, and a mere 20g of carbs.
For reference, there are 48g of carbs in one bagel. Half a bagel would max out my entire carb intake for one day and likely destroy any ketosis that I had established. I know most of you likely just checked out, but stay with me here.
And the thing is, the allowed 20g of carbs aren’t fun carbs like bread or apple cider donuts that a girl in your office had shipped fresh from New York on day two of your diet. They’re hidden carbs that live in foods you thought were safe, like arugula and mushrooms. What I began to refer to as “sleeper carbs” were nearly my downfall and the cause of one of the most dread-filled Sunday nights of my entire life. Don’t worry, we’ll get there.
In order to ensure that you’ve reached ketosis, you get to pee on these little strips that tell you if your body is expelling high levels of ketones with a color scale that quite easily allows you to mistake one level for another, and will have you sitting and examining a strip of paper, covered in your own urine, for longer than you’d like to admit it. Accept this as your new normal.
The test strips are a bit controversial in that they don’t work for everyone, and for some, are less of a measure of your level of ketone creation and more of a litmus test for simply whether you’re in ketosis or not. If you’re a die-hard follower and want the truest measurement, the best route is a blood test, for which you can buy a handy gadget and perform at home. My needle-phobic ass will stick to examining my own pee, thanks.

Other things that will become your new normal: consuming 100+ grams of fat a day, drinking butter, having meltdowns at 8:30pm when you realize you’re still 60 grams of fat short of your daily goal, being that asshole at a restaurant who orders deconstructed burgers with every imaginable sauce removed, and in a moment of weakness, spending $30 on the most pretentious ingredients you can find at your nearest New Seasons, so you can splurge on a keto-safe cookie dough concoction that you’re really going to hate yourself for eating.
The hardest part of this diet wasn’t necessarily following it, but getting into the mindset that not only is it okay to be eating fats, but that you have to do it to keep yourself going.
I, like most women, have grown up in a body-shaming, lady-hating, diet-purporting society that has conditioned me to avoid fats like my life depended on it. In fact, we’ve been taught that our lives do actually depend on it, lest we fall victim to such horrors as high blood pressure, bad cholesterol, or, God forbid, being bigger than a size 6.
But I just spent the last two weeks indulging in eggs fried in butter, bacon, cream cheese, and all the avocado my heart desired, and guess what? I lost nine pounds, went down an entire pant size, and suffered what can only be described as an existential crisis, when I realized that I don’t know how the fuck food or my body works.

If this sounds equal parts enjoyable, eye-opening, and entirely overwhelming, that’s because it was. I know I’ve painted the whole experience as a dream come true, but there were considerable downsides as well. For one, in order to live as true to the lifestyle as possible, I committed to tracking my macros to ensure I was meeting my daily requirements (spoiler alert: I rarely did). This entailed painstakingly measuring out—or in my case, wildly estimating—the exact amount of each individual ingredient I was consuming and putting it into an app that would tell me whether or not I was failing.
Is failing the right word to use, considering I still lost weight and reaped the benefits of a keto diet? Probably not, but that’s certainly what it felt like. While the food was enjoyable, and I’m pleasantly surprised by the end results, a diet shouldn’t make me feel the way that AP Tests and the SAT did; I shouldn’t be having stress dreams about eating an entire cake and immediately throwing my body out of ketosis.
A regular diet is stressful in its own right, but one that makes you meticulously track everything you put into your mouth is a giant undertaking. There were times that I just opted not to eat, because the thought of recording a meal sounded exhausting.
Other negative side effects that one could experience include: muscle cramps due to lack of magnesium (check), sudden drop-offs in energy while your body adapts to this new reality (check), the keto flu—a period of during the induction phase where one might suffer flu-like symptoms due to a lack of electrolytes (thankfully avoided), and zero tolerance for any bullshit from anyone (potentially just me).
What was shocking was how quickly I adapted to this new way of life. Unlike most of my diets where each day brought a new hurdle, either physical or emotional, the reality of keto set in quickly. The second half of the journey moved along smoothly, and I didn’t even find myself wishing for it to end, but that first week was a whirlwind of discovery.
Day One
This first day was exciting in the way these experiments always are in the beginning. I’m out here trying something entirely new and haven’t stooped to the point of hating myself for it yet. Everything is still a novelty, and I haven’t had to embarrass myself at a restaurant by asking for the sugar content of the house Bloody Mary Mix. Everything was bright and shiny.

I learned a couple things really quickly, both through the way I felt and the sage wisdom of my keto coach, a friend who willingly lives like this as an actual preference and not just so she can publish a bunch of jokes about it online. Some people are just enlightened, I guess.
The first lesson: Bodies in ketosis require almost double the amount of water as normal, because your liver is doing a lot more work than usual. This was rough to hear, considering that, on a good day, I drink about half as much water as an adult human should. In light of this news, I downloaded an app to remind me to drink water, because I’m the kind of person that needs technology to remind her to meet the baseline requirements for survival. All in all, things were off to a good start.
Day Two
On day two, I discovered butter coffee, which is exactly what it sounds like: a tablespoon of grass-fed butter and sixteen ounces of black coffee, thrown into a blender. What comes out tastes more like a latte than anything else, and drinking it for the first time felt like what I would imagine it’s like to live life in all caps. I don’t think I’ll ever again reach the level of euphoria that I experienced that first buttery morning, but I’ll dream of it for the rest of my days, chasing that butter coffee dragon.

To be clear, there’s a method behind the madness of drinking a tablespoon of butter first thing every morning. First and foremost, as previously mentioned, I had a hard time squeezing all recommended 119g of fat into my diet, so starting out my day with a steaming cup of butter was actually really helpful. Beyond that, your body takes longer to metabolize fats, which means butter coffee is supposed to keep you energized longer, rather than offering a spike of caffeine in the morning and dropping off by lunch. I found this to be true, because I no longer required my usually mandatory 2pm cup of coffee to make it through the work day.
If a 7am butter coffee was the high of day two, then you could say the low was a mere 12.5 hours later, when I found myself sitting on my patio in the dark, eating rotisserie chicken directly out of the bag, an event spurned by the fact that I had finally checked my macros for the day, and found I was insufficient in just about everything but carbs, which I’d already maxed out at 20g.
It was at this point that I realized that this diet had a definite learning curve, something that I really wasn’t accustomed to. Rather than depriving myself and accepting the suffering, I needed to plan my entire day around meeting dietary requirements that I couldn’t really even fathom. Luckily, there are hundreds of forums, Facebook groups, and Pinterest pages dedicated to this very idea. Did I check any of those? Absolutely not, but it probably would have been a good idea.
Day Three
Day three was when the reality of what macro tracking meant really set in. I am but a simple American, who barely has a grasp on our standard system of measurement, let alone the metric one. Keto does not care about my mathematical inadequacies. This diet is out here asking me to estimate the number of grams of salmon I’m consuming in a single day.
“Idk, like a handful of spinach” isn’t an option on my tracking app, and my kitchen is sorely lacking in basic measurement tools, which left me frequently Googling conversion calculators and trying to rationalize amounts of food by comparing them to items that had their weights listed. In short, it was a fucking train wreck.
After the great rotisserie chicken debacle of the night before, I vowed to never fall victim to macro deficiency again and grabbed a pack of bacon on the way home from work. The second major hurdle of this diet was the fact that I had to spend a substantial amount of time cooking every night. Although it’s been covered in every installment of this series, it probably bears importance in repeating that I am not a cook by any stretch of the word, and any meal that takes more than 15 minutes to prepare just seems exorbitant.
And yet, I found myself that night spending 45 minutes frying up an entire pack of bacon. Should it take that long to cook bacon? Probably not. But things like logic and cook times have never applied to me, and they weren’t about to start this week.
My next lesson was in sleeper carbs and the fact that even if you’re positive you haven’t touched a single carbohydrate all day, you can still rack up about 12g too many of them. The culprit? Vegetables, whom I’d always considered to be a safe and reliable friend, were secretly carrying carbs and betraying any trust established between us. Et tu, arugula?
Day Four
Day four was a turning point, one of the first times I thought to myself, “Maybe this should be something I just do all the time.” What could possibly drive me to consider a lifetime without carbs and sugar? It’s simple really: natural energy, something this body hasn’t experienced since the tender age of 12.
On this momentous day, I woke up on my very first alarm. To some, this is just a mundane requirement of being an adult and making it to work on time, but for me? Unheard of. I am a five alarm girl, set at five-minute intervals for optimal suffering. I usually drag my lifeless body out of bed about 10 minutes after that fifth alarm and proceed to caveman around the house until I’ve deemed myself presentable enough to wander into work and directly to the coffee machine.
But on day four, I sprang out of bed at a chill 6:40am with a sizable craving for butter coffee and the drive to get out of the house as soon as humanly possible.
Improved energy is, in fact, a side effect of this diet. Fat is the body’s largest and most efficient source of energy, and you’ve just about doubled your intake of it. The result is that you aren’t spending time working through heavy carbs anymore, just burning through these high-energy molecules, which are making you feel truly awake for the first time in your cursed life.
In my case, it was also making me second-guess a lot of things that I had never questioned before. For instance, I am now almost 99% sure that I’ve spent my entire life mistaking the signs of dehydration for anything but that. On my way to work that morning, I thought, “Hm, I’d really love another cup of coffee,” and then stopped myself, because that wasn’t actually what I wanted at all. I was thirsty and finally recognizing it for what it was. Natural selection is truly slacking in my case.
You might be asking yourself how I’ve made it a full 25 years without being able to tell if my body was in need of water or not, and I’m here to tell you that I have no idea. But now that I’m drinking 2.5 liters of water a day, I’ve finally begun to understand what a baseline craving for hydration feels like. Let me tell you, it’s wild.
Day Five
I had made it to Friday and had done pretty well for myself, so on day five, I decided it was time for a treat: professional butter coffee. It’s actually called Bulletproof Coffee, and it’s basically butter coffee with the addition of MCT oil, a naturally occurring oil that is supposed to boost energy and burn fat like crazy.
Was it weird at first? For sure. I had grown accustomed to my butter lattes, and this was less of a soothing morning ritual and more so on par with what I would expect it’s like to do angel dust for the first time. I didn’t really know how to process it until I was about a third of the way through and my body took over. Suddenly, I needed to drink the rest of it, and it needed to happen as quickly as humanly possible.
It was like I had transcended mundane things like taste buds in favor of becoming omnipotent. I could see new colors. Conversations around me slowed down. I got more work done on that single day than I had all week, and it was all due to this $6 oily, buttery, bitter concoction that I will never stop thinking about. I was riding on an absolute high, ready to adopt a keto diet for life, until suddenly I wasn’t.

There was a flurry of reasons for that abrupt turn of events that all culminated in one thing: alcohol. Naturally.
Maybe it was the Bulletproof coffee, or my intense focus, but I didn’t drink nearly as much water as I should have on Friday. Realizing this around 4pm was the first red flag that put me off-kilter. A work happy hour led to a birthday party, which led to a bar, which led to another bar, which ultimately led to me standing in front of a Mediterranean food cart at 2am trying to rack up the 1,000 calories I was supposed to have consumed throughout the day, while explaining to a confused, bemused, but accommodating Middle Eastern man what exactly ketogenic diets entail.
All week I had been shaping my plans and schedule so specifically around this diet, but day five was the first day that life intervened. Sometimes, you’re going to be out and about and won’t be able to find a high-fat, moderate protein meal that adheres exactly to your needs. Sometimes you’re going to fall off the wagon, because you’ve had a shitty day and you need to. Sometimes you’re going to accidentally get super drunk on a Friday, because you would have been racked with FOMO if you hadn’t gone to the cool rooftop happy hour.
And all of that is okay! You can have those off days, as long you wake up the next morning and rededicate yourself to your goals.
Let me tell you, that is exactly what I did.
Day Six
I don’t know how to explain the way I felt Saturday morning. I woke up... energized?
The three tequila Diet Cokes (it pains me to write that) and two vodka sodas I consumed the night before? Gone.
Any exhaustion that may have stemmed from the fact that I went to bed at 3am and woke up naturally at 8am? Gone.
A sudden need to grocery shop, clean my room, do the dishes, buy a wall calendar to map out the rest of these diets, and just generally get my life together ARRIVED.
Here I was, making the most of a Saturday morning, planning for my week ahead and feeling slightly guilty for consuming alcohol. It wasn’t even the “I blacked out and embarrassed myself” guilt but a completely foreign “I didn’t really need to drink alcohol at all last night” kind. It was during those abundantly productive hours that I first questioned whether this diet was turning me into a functional adult. Or at the very least, someone who could pass for one. I bought a relaxing nighttime tea, for God’s sake. What next? Learning how to make sous vide eggs?
Day Seven
All the serenity of Saturday was completely spent by the time Sunday rolled around. I was coming up on one week of this diet, and the only thing I really felt was stressed out. Well, skinny and stressed out. I had yet to figure out a solution to sleeper carbs and was on the verge of a nervous breakdown, trying to reconcile this newfound, entirely one-sided feud with vegetables that I was harboring.
I hadn’t experienced a Sunday night woe like this since high school, at which point I consulted my keto coach who encouraged me to throw caution to the wind and indulge in a meal consisting solely of eggs, butter and meat. Decadent doesn’t begin to describe the way I felt.
Sunday night was a true breakthrough in both keto and probably just my adult life: I had finally allowed myself to eat something that a past me would have deemed wildly unacceptable. I’d dismantled the mental block that told me a meal wasn’t complete if it wasn’t 50% green and leafy. I wasn’t “treating myself” or “having a cheat meal.” I was eating fucking dinner, and it was glorious and liberating, and I was evolving my relation with food.

From that moment forward, I was a new person. I no longer shied away from the high-fat foods, that I was supposed to be embracing. I committed to drinking water, not just for the diet, but also for myself. I slowly began to relax my meal planning, allowing myself to eat out and not slave over tracking nuances. I ate a shit ton of bacon. And come the two-week mark, I’d lost nine pounds.
Every diet in this series has taught me something about myself: that I am capable of superhuman levels of self-control when I need to be, that I can eat an inhumane amount of ice cream and still kind of function, and that I can accomplish just about anything that I set my mind to, even if my body is begging me not to.
But this is the first diet to show me that maybe my regular habits aren’t all that much better than the ones I force upon myself, for the sake of these articles. Eating healthy is all well and good, but not if you’re punishing yourself after a moment of weakness. Hell, maybe they shouldn’t be called moments of weakness, but moments where I really wanted a muffin, and so I ate a goddamn muffin.
Does this mean I’m fully committed to a keto lifestyle from here on out? Not necessarily. Lazy keto, a diet that still follows ketogenic rules but doesn’t force you to track your macros or panic over vegetable carbs, seems more up my alley and is something I could see myself adopting between diet ventures. But I’m also acutely aware that fall is here and with it the great love of my life: kettle corn. I won’t deprive myself of that, and I also won’t gorge myself with it. I’ll enjoy a responsible amount and determinedly not feel bad about it.
In the end, the ultimate irony is that a high-fat, indulgent diet has brought a sense of balance to my life that I hadn’t realized I was missing. Somehow, on this never-ending quest to test every possible limit my body possesses, I’ve managed to stumble upon something worthwhile.
No promises that it will ever happen again, but I’m pretty happy with myself in the meantime.
Read more: http://www.betches.com/fad-diet-diaries-ketogenic-diet
0 notes
Link
Study Reveals Previously Unknown Mechanism Behind Acupuncture’s Ability to Reduce Pain Dr. Mercola By Dr. Mercola When it comes to treating ailments such as chronic pain, I definitely prefer nontoxic options to drugs and surgery. Americans use 80 percent of all the opioids sold worldwide1 — a testament to the pervasiveness of pain in this country — and with drug overdoses now being the ninth leading cause of death in the U.S., we clearly need safer alternatives. Acupuncture is one such alternative. Research shows it can be an effective option for a number of health problems, but pain in particular. Contrary to allopathic, symptom-based medicine, acupuncture aims to eliminate the root cause of your problem, which is said to originate in a dysfunction in your body's energetic meridian system. Basic Principles of Acupuncture Traditional Chinese medicine (TCM) views the body as a cohesive system where everything within it is interconnected. In other words, it recognizes that each part of your body has the ability to affect all other parts. There are 14 major energy channels called meridians that flow through your body. An energy called qi (or chi) circulates along the meridians to all parts of your body, including the internal organs and every cell. This qi is the vital force that literally keeps us alive. Vibrant health is a result of balanced, unimpeded flow of energy through your body. According to TCM, illness and pain are the byproducts of energy blockages somewhere along one or more meridians. Each acupuncture point along the meridian acts like a pass-through or gate. Energy can get "bottlenecked" in these points, slowing down the flow, sometimes to the point of standstill. This is the precursor to pain and illness. By inserting a thin needle into the congested or "clogged" area, it opens the gate and allows the energy to flow again. With qi flowing smoothly, your body can re-regulate the flow of energy, repair itself and maintain its own optimal level of health. Herbs and other therapies such as guacha, cupping and moxibustion — the burning of herbs on or over the skin — can be used to support the healing. Acupuncture May Offer Drug-Free Pain Relief In a 2012 analysis2,3 of 29 published studies involving more than 17,900 participants, researchers concluded that acupuncture has a definite effect in reducing chronic pain — more so than standard pain treatment. Real acupuncture also produced slightly better results than using sham needles, which suggests the benefits of needling are due to more than the placebo effect. By going the extra mile and retrieving the raw data on self-reported pain, and standardizing the various study participants' responses, they were also able to more accurately assess and compare them as a whole. Overall, the team discovered a "clear and robust" effect of acupuncture in the treatment of back pain, neck pain, shoulder pain, osteoarthritis and headaches. On a scale of zero to 100, participants who started out with a pain rating of 60 experienced an average 30-point drop (a 50 percent reduction) in response to the real acupuncture treatments (using needles); a 25-point drop when receiving sham acupuncture; and a mere 17-point drop when receiving "standard pain care" that did not include acupuncture. According to the lead author:4 "The effects of acupuncture are statistically significant and different from those of sham or placebo treatments ... So we conclude that the effects aren't due merely to the placebo effect." Acupuncture Cuts Pain by Boosting Nitric Oxide While there's been a great deal of controversy as to whether or not acupuncture works "for real," and if so, how, new research presents an answer to this question. The study5,6,7,8,9 in question was conducted by researchers at LA BioMed.10 The research laboratory has developed a noninvasive device capable of sampling biomolecules over specific skin regions. Using this device, they were able to determine that when acupuncture is properly administered, nitric oxide (NO) is released at the "acupoints" — the acupuncture sites into which the needles are inserted. NO is a soluble gas that is continually produced from the amino acid L-arginine inside your cells. This gas plays an important role in supporting normal endothelial function and protecting your cells' powerhouses, the mitochondria. It's also a potent vasodilator. By relaxing and dilating your blood vessels, NO improves blood flow and lowers blood pressure. NO also encourages release of natural analgesics (pain relieving chemicals) in your body. Together, this helps explain why and how acupuncture works to reduce pain. A number of acupuncture studies have produced negative results. The reason for this may have to do with the way the acupuncture is done. In order for NO release to occur, "de qi" had to be elicited. De qi feels a bit like an electric shock. Westerners are not accustomed to this sensation, which is why many Western acupuncturists won't do it. De qi is elicited by twisting the inserted needle. In this study, they twisted the needle for two minutes or until de qi was elicited. They then manipulated the needles for two minutes every five minutes, for a total of 20 minutes each treatment. Heat can also amplify the effectiveness of the treatment and, here, the application of heat also increased NO release at the acupoints. Acupuncture Reduces Osteoarthritis Pain A number of studies support the use of acupuncture for pain. A large, landmark study11,12 published in 2004, which assessed whether acupuncture might work for osteoarthritis pain, produced remarkably positive results. A total of 570 patients diagnosed with osteoarthritis of the knee were enrolled for this 26-week-long trial — the longest and largest randomized, controlled phase III clinical trial of acupuncture ever conducted. None of the participants had tried acupuncture before, and none had had knee surgery in the previous six months. Nor had they used steroid injections. The participants were randomly assigned to receive one of three treatments: acupuncture, sham acupuncture or self-help strategies recommended by the Arthritis Foundation (the latter served as a control group). Significant differences in response was seen by week eight and 14, and at the end of the trial, the group receiving real acupuncture had a 40 percent decrease in pain and a nearly 40 percent improvement in function compared to baseline assessments — a 33 percent difference in improvement over the sham group. According to the late Dr. Stephen E. Straus, who served as the first director of the National Center for Complementary and Alternative Medicine (NCCAM), which is a part of the National Institutes of Health:13 "For the first time, a clinical trial with sufficient rigor, size and duration has shown that acupuncture reduces the pain and functional impairment of osteoarthritis of the knee. These results also indicate that acupuncture can serve as an effective addition to a standard regimen of care and improve quality of life for knee osteoarthritis sufferers. NCCAM has been building a portfolio of basic and clinical research that is now revealing the power and promise of applying stringent research methods to ancient practices like acupuncture." Other Evidence Showing What Acupuncture 'Does' Boosting NO release isn't the only mechanism by which acupuncture reduces pain. Previous research suggests acupuncture stimulates your central nervous system to release natural chemicals that alter bodily systems, pain and other biological processes. In 2003, the World Health Organization (WHO) conducted an extensive review and analysis of clinical trials involving acupuncture.14 According to this report,15 acupuncture: Stimulates the conduction of electromagnetic signals, which may release immune system cells or painkilling chemicals Activates your body's natural opioid system, which may help reduce pain or induce sleep Stimulates your hypothalamus and pituitary gland, which modulate numerous body systems Alters secretion of neurotransmitters and neurohormones, which may positively influence brain chemistry According to the WHO's analysis, "Some of these studies have provided incontrovertible scientific evidence that acupuncture is more successful than placebo treatments in certain conditions." The report again confirmed its benefits for pain, saying: "The proportion of chronic pain relieved by acupuncture is generally in the range 55–85 percent, which compares favorably with that of potent drugs (morphine helps in 70 percent of cases) and far outweighs the placebo effect (30–35 percent)" Acupuncture Reduces Pain by Shutting Down Certain Brain Regions In the BBC documentary, "The Science of Acupuncture," which originally aired in 2015, a team of researchers conducted an experiment that had never been done before. Using high-tech MRI imaging, they visually demonstrated that acupuncture has a very real effect on the brain. Acupuncture, it turns out, does something completely unexpected — it deactivates certain parts of the brain, particularly in the limbic system, decreasing neuronal activity, opposed to having an activating impact. Their experiment also clearly showed that superficial sham needling does not have this effect. Your limbic system is associated with the experience of pain, adding further evidence that something unique happens during acupuncture. It quite literally alters your experience of pain by shutting down these deeper brain regions. Another Simple Way to Boost NO Production As mentioned, NO can help reduce pain, and a simple way to boost your body's NO production is by performing high intensity exercises. In the video above, I demonstrate an updated version of the "nitric oxide dump" exercise developed by Dr. Zach Bush. If you have previously watched this video, please review it again as I recently updated it to correct a couple of errors and omissions that sneaked into my previous video. You don't need any weights, and all it takes is three minutes, two to three times a day, with at least two hours between sessions. A key component I forgot in my earlier video is to make sure you're breathing through your nose and not your mouth. I am convinced that this gentler strategy — although it has not been evaluated or compared to other high intensity interval training protocols (HIIT) — is a far healthier strategy to obtain the benefits of HIIT without any of the downsides. I only wish I had known about this more effective approach earlier. Depending on the type of pain you're struggling with, you might conceivably be able to control it through this natural NO boosting exercise. Other Nondrug Solutions for Pain Relief There are many other ways to address pain beside acupuncture. Below is a long list of suggestions. Clearly, there are times when pain is so severe that a narcotic pain reliever may be warranted. But even in those instances, the options that follow may allow you to at least reduce the amount you take, or the frequency at which you need to take them. If you need an acute pain reliever, you can consider an over-the-counter (OTC) option. Research16 shows prescription-strength naproxen (Naprosyn, sold OTC in lower dosages as Aleve) provides the same pain relief as more dangerous narcotic painkillers. However, while naproxen may be a better alternative to narcotic painkillers, it still comes with a very long list of potential side effects,17 and the risks increase with frequency of use, which is why I discourage anyone from taking them, especially long term. It would be far better to try some of the nontoxic options below. ✓ Eliminate or radically reduce most grains and sugars from your diet Avoiding grains and sugars will lower your insulin and leptin levels and decrease insulin and leptin resistance, which is one of the most important reasons why inflammatory prostaglandins are produced. That is why stopping sugar and sweets is so important to controlling your pain and other types of chronic illnesses. ✓ Take a high-quality, animal-based omega-3 fat Omega-3 fats are precursors to mediators of inflammation called prostaglandins. (In fact, that is how anti-inflammatory painkillers work, by manipulating prostaglandins.) Good sources include wild caught Alaskan salmon, sardines and anchovies, which are all high in healthy omega-3s while being low in contaminants such as mercury. As for supplements, my favorite is krill oil, as it has a number of benefits superior to fish oil. ✓ Optimize your sun exposure and production of vitamin D Optimize your vitamin D by getting regular, appropriate sun exposure, which will work through a variety of different mechanisms to reduce your pain. Sun exposure also has anti-inflammatory and pain relieving effects that are unrelated to vitamin D production, and these benefits cannot be obtained from a vitamin D supplement. Red, near-, mid- and far-infrared light therapy (photobiology) and/or infrared saunas may also be quite helpful as it promotes and speeds tissue healing, even deep inside the body. ✓ Medical cannabis Medical marijuana has a long history as a natural analgesic and is now legal in 29 states including Washington DC. You can learn more about the laws in your state on medicalmarijuana.procon.org.18 ✓ Kratom Kratom (Mitragyna speciosa) is another plant remedy that has become a popular opioid substitute.19 In August 2016, the U.S. Drug Enforcement Administration issued a notice saying it was planning to ban kratom, listing it as a Schedule 1 controlled substance. However, following massive outrage from kratom users who say opioids are their only alternative, the agency reversed its decision.20 Kratom is likely safer than an opioid for someone in serious and chronic pain. However, it's important to recognize that it is a psychoactive substance and should not be used carelessly. There's very little research showing how to use it safely and effectively, and it may have a very different effect from one person to the next. Also, while it may be useful for weaning people off opioids, kratom is in itself addictive. So, while it appears to be a far safer alternative to opioids, it's still a powerful and potentially addictive substance. So please, do your own research before trying it. ✓ Emotional Freedom Techniques (EFT) EFT is a drug-free approach for pain management of all kinds. EFT borrows from the principles of acupuncture in that it helps you balance out your subtle energy system. It helps resolve underlying, often subconscious, and negative emotions that may be exacerbating your physical pain. By stimulating (tapping) well-established acupuncture points with your fingertips, you rebalance your energy system, which tends to dissipate pain ✓ Meditation and Mindfulness Training Among volunteers who had never meditated before, those who attended four 20-minute classes to learn a meditation technique called focused attention (a form of mindfulness meditation) experienced significant pain relief — a 40 percent reduction in pain intensity and a 57 percent reduction in pain unpleasantness.21 ✓ K-Laser, Class 4 Laser Therapy If you suffer pain from an injury, arthritis or other inflammation-based pain, I'd strongly encourage you to try K-Laser therapy. It can be an excellent choice for many painful conditions, including acute injuries. By addressing the underlying cause of the pain, you will no longer need to rely on painkillers. K-Laser is a class 4 infrared laser therapy treatment that helps reduce pain, reduce inflammation and enhance tissue healing — both in hard and soft tissues, including muscles, ligaments or even bones. The infrared wavelengths used in the K-Laser allow for targeting specific areas of your body and can penetrate deeply into the body to reach areas such as your spine and hip. ✓ Chiropractic Many studies have confirmed that chiropractic management is much safer and less expensive than allopathic medical treatments, especially when used for pain such as low back pain. Qualified chiropractic, osteopathic and naturopathic physicians are reliable, as they have received extensive training in the management of musculoskeletal disorders during their course of graduate health care training, which lasts between four to six years. These health experts have comprehensive training in musculoskeletal management. ✓ Physical therapy Physical therapy has been shown to be as good as surgery for painful conditions such as torn cartilage and arthritis. ✓ Foundation Training Foundation training is an innovative method developed by Dr. Eric Goodman to treat his own chronic low back pain. It's an excellent alternative to painkillers and surgery, as it actually addresses the cause of the problem. ✓ Massage A systematic review and meta-analysis published in the journal Pain Medicine included 60 high-quality and seven low-quality studies that looked into the use of massage for various types of pain, including muscle and bone pain, headaches, deep internal pain, fibromyalgia pain and spinal cord pain.22 The review revealed massage therapy relieves pain better than getting no treatment at all. When compared to other pain treatments like acupuncture and physical therapy, massage therapy still proved beneficial and had few side effects. In addition to relieving pain, massage therapy also improved anxiety and health-related quality of life. ✓ Astaxanthin Astaxanthin is one of the most effective fat-soluble antioxidants known. It has very potent anti-inflammatory properties and in many cases works far more effectively than anti-inflammatory drugs. Higher doses are typically required and you may need 8 milligrams (mg) or more per day to achieve this benefit. ✓ Ginger This herb has potent anti-inflammatory activity and offers pain relief and stomach-settling properties. Fresh ginger works well steeped in boiling water as a tea or grated into vegetable juice. ✓ Curcumin In a study of osteoarthritis patients, those who added 200 mg of curcumin a day to their treatment plan had reduced pain and increased mobility. A past study also found that a turmeric extract composed of curcuminoids blocked inflammatory pathways, effectively preventing the overproduction of a protein that triggers swelling and pain.23 ✓ Boswellia Also known as boswellin or "Indian frankincense," this herb contains specific active anti-inflammatory ingredients. ✓ Bromelain This enzyme, found in pineapples, is a natural anti-inflammatory. It can be taken in supplement form but eating fresh pineapple, including some of the bromelain-rich stem, may also be helpful. ✓ Cetyl Myristoleate (CMO) This oil, found in fish and dairy butter, acts as a joint lubricant and anti-inflammatory. I have used this for myself to relieve ganglion cysts and carpal tunnel syndrome. I used a topical preparation for this. ✓ Evening Primrose, Black Currant and Borage Oils These contain the essential fatty acid gamma-linolenic acid (GLA), which is particularly useful for treating arthritic pain. ✓ Cayenne Cream Also called capsaicin cream, this spice comes from dried hot peppers. It alleviates pain by depleting the body's supply of substance P, a chemical component of nerve cells that transmits pain signals to your brain. ✓ Mind-Body Therapies Methods such as hot and cold packs, aquatic therapy, yoga, various mind-body techniques and cognitive behavioral therapy24 can also result in astonishing pain relief without drugs. ✓ Grounding Walking barefoot on the earth may also provide a certain measure of pain relief by combating inflammation. ✓ Low-Dose Naltrexone (LDN) Naltrexone is an opiate antagonist, originally developed in the early 1960s for the treatment of opioid addiction. When taken at very low doses (LDN, available only by prescription), it triggers endorphin production, which can boost your immune function and ease pain.
0 notes
Text
Dale Earnhardt Jr. paves the way for concussion awareness and a safer NASCAR
Admitting injury used to be a NASCAR no-no, but Dale Jr. helped change that for the better.
Editor’s note: Dale Earnhardt Jr. received medically clearance to resume racing in December 2016 and returned to competition at the beginning of the 2017 season. On Tuesday, citing that he wanted to walk away on his own terms, Earnhardt announced he is retiring from fulltime NASCAR competition effective at the end of the current season. The story that follows was originally published in July 2016.
Dale Earnhardt Jr. is far more than NASCAR's most popular driver, an award he's won a record-tying 13 years running. He's also the sport's primary ambassador, a crossover star whose name resonates with those who cannot differentiate a lug nut from a tie rod yet are still drawn to the 41-year-old's down-home country charm and thoughtful genuineness.
In recent years, however, Earnhardt has taken on a far more important role: NASCAR's No.1 head injury advocate.
It has long been part of NASCAR's fabric that drivers were expected to race hurt. If you could find a way to get yourself in the car, you were expected to do so. No excuses. Just grit it out and strap yourself behind the wheel.
NASCAR's national championship was even constructed to reward those willing to "tough it out," as points were awarded just for starting a race. And with the consequences for sitting out an event too detrimental to their title aspirations, drivers who often had no business being on the track felt compelled to race with injuries that otherwise would have had them sidelined.
This rudimentary way of thinking prompted Richard Petty to race with a broken neck, for Davey Allison to race with a broken right wrist requiring his team to Velcro his hand to the gear shifter and so on and so forth. Even Earnhardt fell victim to this culture of playing hurt when in 2002 he purposely hid a concussion for months out of fear he wouldn't be allowed to race.
It was a ridiculous mindset desperately needing to evolve, but a leader was needed to spur the revolution to eradicate the tough guy ethos permeating within the sport.
Enter Earnhardt.
Ten years after refusing to say publicly he had a concussion, Earnhardt suffered a pair of concussions within a six-week span. After the second, which occurred in a multi-car crash during a race at Talladega Superspeedway, Earnhardt was medically cleared onsite. But still not feeling healthy, he took it upon himself to seek additional medical opinions.
What he learned changed not only his way of thinking, but also NASCAR's entire approach to dealing with head injuries.
Following the diagnosis, Earnhardt disclosed the news and sat out two races to recuperate. That he did so on his own volition went against the essence of how drivers were supposed to act, especially those who were racing for a championship, as Earnhardt was that season.
However, instead of being disparaged for his decision, Earnhardt rightly received overwhelming praise. It takes a big man to admit something is wrong, and Earnhardt did just that. His health was too important, and by ignoring the signs he was not only endangering himself but other drivers.
Not coincidentally, NASCAR shortly thereafter overhauled how it handled concussions. Drivers were required to submit a baseline ImPACT test as a gauge to determine whether they could resume competing following a crash. Although some disagreed with NASCAR's methods, its most popular figure was an unwavering staunch supporter.
I appreciate everyone's support and prayers and will miss my team terribly this weekend. I'm working with some great doctors to get well.
— Dale Earnhardt Jr. (@DaleJr) July 15, 2016
Another major step to protect drivers from themselves was taken when NASCAR overhauled its Chase playoff format prior to the 2014 season. Incorporating a once unheard measure, officials now had the power to grant waivers to drivers needing to miss a race for medical reasons, thereby allowing them to maintain championship eligibility. Immediately the practice of drivers sacrificing the well-being of themselves and others just to win a title was discontinued.
In the years since, multiple drivers have received exemptions for injuries that previously may not have been reported lest they keep them from racing. In 2015, Kyle Busch received such a measure after breaking his leg in a crash, and after letting his body heal properly he used that second chance to go on and win the championship. Tony Stewart, who broke his back in a January all-terrain vehicle accident, finds himself in a similar situation this season, with a chance he wouldn't have had just a few years ago.
Busch and Stewart wouldn't have likely raced anyway because their injuries were too serious, but we cannot definitively say what desperate steps they may have taken in the name of competition.
It is not hyperbole to say that, without Earnhardt at the forefront, NASCAR may not have been as quick to modify its longstanding policies. In March, he went a step further by pledging his brain to science for concussion research.
But it is also due to Earnhardt's awareness of the long-term effects head injuries can have on his health, as well as his advocacy on the topic, that there is the very real possibility the 41-year-old may not return this season. He announced on Thursday that he'll sit out Sunday's race at New Hampshire because he's suffering from concussion-like symptoms following two accidents in a three-race stretch from June 12 to July 2.
Neither Earnhardt nor Hendrick Motorsports have laid out any timetable for a possible return, and with Earnhardt's history he understands as well as anyone what the ramifications are if he were to continue subjecting himself to additional concussions.
Many injuries can be overcome or outright ignored. Head injuries simply aren't one of them. That's a fact Earnhardt unfortunately knows all too well.
0 notes
Text
Gum Disease: Stages, Prevention, and Treatment
From a simple case of bleeding gums to painful gum recession, gum disease is a problem that you need to deal with as soon as possible.
Here, we’ll discuss the hierarchy of gum disease and what happens at each stage. You’ll also learn what you can do at home in your daily routine to prevent this from happening and protect your dental health.
If all else fails, fear not. Your dentist can help you with a treatment plan to manage gum disease at any stage of gum disease (officially dubbed “periodontitis”).
Gum Disease Signs and Symptoms
There are a few very common signs of periodontal disease to look for in your daily routine. These signs of gum disease may be signals that your gum health isn’t where it needs to be.
Red, swollen gums
Receding gums
Bleeding on brushing or flossing
Visible pus
Teeth feel loose and moveable
A change in your bite
Heightened sensitivity to hot or cold foods
Pain when chewing
A bad taste in your mouth
Persistent bad breath
A note of caution: Even if you do not have any of these symptoms, it is possible you still have gum disease.
Always go to your routine dental visits for check-ups—gum disease diagnosis is one reason you should stick to these appointments.
How Your Dentist Will Diagnose Gum Disease
When you show up for a dental appointment, you may not realize your dentist and hygienist are looking for gum disease symptoms. Here are some of what happens at your dental cleanings that can help recognize periodontitis.
1. Medical History
You may be thinking, “Did I come to the doctor’s office, or the dentist’s?” This is a common notion many people have when a dentist asks about certain diseases that run in their family, or if they’ve recently been diagnosed with any systemic conditions.
One reason for this is that any medication you may have been prescribed by your physician could cause severe consequences for your oral health.
For example, medications that have the side effect of causing a dry mouth, or “xerostomia,” can lead to tooth decay.
The saliva in our mouths helps us wash away food and other debris to rid of plaque. Plaque naturally forms a biofilm on the surface of our teeth after we eat or drink anything with carbohydrates or sugars.
Over time, if plaque is not removed regularly by brushing and flossing, it can lead to tartar buildup. Tartar is also called “calculus,” and it forms a yellow, brown deposit after plaque hardens. Unlike plaque, you cannot safely remove tartar on your own. This can only be done professionally by a dentist or dental hygienist.
2. Pocket Depth Measurement
This part of your dental exam and teeth cleaning is called “perio probing.” Here, dentists use an instrument called a periodontal probe with markings in millimeters used to measure the pocket depths around each and every tooth.
With firm and gentle pressure, the perio probe is inserted into your gingival sulcus, which is the space between your tooth and the gum surrounding it.
Healthy measurements are between 1-3mm of pocket depth.
Generally, anything deeper than that indicates gum inflammation that is making the pocket deeper. The deeper the pocket, the looser the gums surrounding your tooth, and the higher the degree of inflammation.
Another sign that your dentist or dental hygienist will look for when measuring pocket depth is bleeding upon probing. We may be poking at you, but a periodontal probe is blunted at the end, so it shouldn’t cause any bleeding in a healthy mouth. Bleeding upon probing is not considered normal and is one of the significant signs of gum inflammation.
It is really important that you don’t miss your regular check-ups and cleanings, or reschedule as soon as you can if something pops up. That way, anything out of the ordinary will be caught on early and promptly treated.
3. Dental X-Rays
The purpose of taking an x-ray (radiograph) is help your dentist examine everything in your mouth that is not visible to the naked eye.
The most commonly taken x-rays to evaluate gum disease are “bitewings.” There are four bitewings that are taken, one for each quadrant. Your dentist will be able to see everything from the top of your tooth to its roots, as well as the height of the bone around it.
The periodontal ligament, or PDL, serves as the supporting structure between the tooth and the bone. Bacteria can build up in deep periodontal pockets and cause destruction to the PDL, leading to bone loss and eventual tooth loss.
Taking bitewing x-rays will help your dentist assess if there are any changes to your jawbone as a result of gum disease.
Radiographs are not “one size fits all.” Your dentist will determine your oral profile risk and the frequency of x-rays needed. It may be as recent as every 6 months or only every couple of years.
The Stages of Gum Disease
There are four stages of gum disease, although the lines between these are a bit blurred.
Stage I: Gingivitis
This first stage of gum disease refers to inflammation of the gums.
Bacteria and plaque build up gradually over time along your gingival sulcus. Toxins released from this bacteria may cause deeper periodontal pockets due to damage of the PDL fibers that support the teeth and gums.
As mentioned previously, healthy gums have a probing depth of 1-3 mm. At the gingivitis stage, probing depths will be about 2-4 mm. (1)
You may also have other gingivitis symptoms, like:
Redness and swelling of the gums
Bleeding upon flossing
Bad breath
This is the mildest form of gum disease and therefore does not result in any bone loss or connective tissue loss. The good news is this stage is completely reversible and you can usually correct it at home! We’ll learn more about that later.
Stage II – III: Slight to Moderate Periodontal Disease
These two stages are grouped together because their effects are similar but gradual in strength.
The infection has now penetrated deep into your gums rather than along your gums. You will have:
Increased redness in your gums
More bleeding upon brushing
Worsening bad breath.
For slight periodontal disease, your dentist will observe 4-5 mm in probing depth. As for moderate periodontal disease, we will see probing depths at about 6-7 mm.
The deeper the infection gets into the gums, the greater the destruction of the PDL fibers, and the higher the probing depth.
At this point, the bacteria gets so entrenched into your gums that it actually begins to enter your bloodstream. This can compromise your immune system and might lead to or heighten your risk of other diseases (thanks, mouth-body connection!).
The main distinction from these stages in contrast to gingivitis is the start of bone loss. Bone loss here can range from 20-50%.
At this point, you cannot just cure gum disease at home. Treatment will require a consultation with your dentist.
Stage IV: Advanced Periodontal Disease
As you enter this stage of periodontal disease, bacteria has become more virulent.
You have pocket depths greater than 7 mm and the roots of your teeth may be exposed. Tooth mobility has increased significantly and tooth loss becomes very probable. This changes your overall bite and makes chewing more of a challenge.
Something else your dentist will see are pus-filled abscesses in and around your gums. These abscesses form in because immune system is trying to fight off the infection and keep it from spreading.
Bone loss at this stage is between 50-90%. Due to the severe infiltration of bacteria and the destruction it has caused to the integrity of your teeth, this final stage is only manageable with treatment, not reversible.
Types of Gum Disease
Gum disease happens for a number of reasons, and depending on the cause, it can progress more or less rapidly. The four types of gum disease can help your dentist determine the best course of treatment and help you with expectations for recovery. (2)
Chronic: Most common of the four types, chronic periodontitis is the gradual progression of inflammation in and around the gums. This typically happens slowly but can worsen rapidly at different points of the condition.
Aggressive: Typically seen in families, aggressive periodontitis often happens in healthy people and progresses faster than chronic periodontitis. There’s a likely genetic component to this type of gum disease.
Related to systemic disease: Certain diseases can manifest as gum disease. Periodontitis as a manifestation of systemic disease occurs most often in children with issues like diabetes, respiratory disease, or cardiovascular disease.
Necrotizing: In necrotizing periodontal disease, lesions cause necrosis (tissue death) of gingival tissue, periodontal ligament, and alveolar bone. People with these kinds of lesions are typically those with compromised immune systems, like patients with HIV, malnutrition, or other immune-compromising conditions.
Options for Gum Disease Treatment at Each Stage
Whether you’re struggling with advanced gum disease or the beginning stages of gingivitis, there are things you can do to keep your gums healthy.
In 1965, Dr. Harald Löe and his colleagues conducted a study called “Experimental Gingivitis in Man.”
Dr. Löe asked eleven healthy male dental students to be experimental subjects. The participants had their teeth cleaned and scaled to provide a baseline of their gingival health. They were then asked to cease all oral hygiene measures. That means no brushing, flossing, or mouth rinsing.
I imagine this might have been hard for their girlfriends. But, I digress.
As oral hygiene measures were withdrawn, plaque accumulated and the subjects developed gingivitis in a range of 9-21 days. They were then asked to begin oral hygiene measures again.
Although some men took a longer time to develop gingivitis, all the men returned to their normal, healthy status in about 7-11 days. They did this on their own, with no professional help, but only consistent oral care and hygiene. (3) Clearly, there’s something important in that daily routine!
Let’s look at the treatment options for each stage of gum disease.
1. Treatment for Gingivitis
The purpose of Dr. Harald Löe’s experiment (though this type of research is considered unethical in today’s research guidelines) was to prove that the mildest form of gum disease, gingivitis, is completely reversible.
Your dentist or hygienist will give you a dental prophylaxis, or “prophy.” This is what is known as a professional cleaning. (4) It will consist of supragingival (above the gum line) and subgingival (below the gum line) removal of plaque, calculus, and staining.
However, your provider can only do so much. The only way of reversing gingivitis at this stage is good oral hygiene on your part. Brushing twice a day for two minutes at a time, flossing at least once, and regular dental check-ups will get you back to a healthy smile.
If you notice bleeding gums more regularly than you’d like but your dentist hasn’t seen signs of more advanced gum disease, try some of the treatments for gingivitis Dr. Burhenne outlines here.
2. Treatment for Slight to Moderate Periodontal Disease
At this stage, the infection has gotten deep enough into your tissues that a prophy, brushing, or flossing just won’t cut it. Here, your dentist will introduce a non-surgical procedure called scaling and root planing procedure (SRP for short).
“Scaling” is when your provider cleans out the toxins in your periodontal pockets. “Root planing” is when he or she smooths out the surfaces of your roots to help your gums reattach. (5) Generally, this procedure causes very little discomfort. If you have sensitive teeth, your dentist may numb your gums with a local anesthetic.
An SRP can be done in a single visit, but it is usually broken up into appointments per quadrant (¼ of the mouth) or by halves, depending on the severity. After an SRP, your gums may feel tender and sensitive.
If you are consistent with a proper oral hygiene regimen after the procedure, your gums should turn back to their smooth texture and natural pink color within a few weeks.
Other ways to handle this stage of gum disease at home include a gum disease diet, using knotted floss to dislodge stubborn food particles, and trying mouth tape to cut down on mouth breathing at night.
3. Treatment for Advanced Periodontal Disease
Flap Surgery
At this stage, your bone and surrounding supporting tissue have been significantly destroyed. The objective of flap surgery is to reduce the depth of the periodontal pockets and regenerate the PDL fibers.
After numbing the area with local anesthetic, your dentist will make a flap-like incision around the gum tissue. The gums are lifted back, which allows a thorough cleaning of all the diseased tissue that has infiltrated. The flap is then sealed tightly so the gums fit snugly around the teeth and the healing process takes place.
After the procedure, you will have reduced pockets, which makes it easier to maintain your oral health. A combination of professional maintenance and consistent home care of your teeth will help prevent recurrence of this disease. (6)
Bone Graft
If you have teeth lost to gum disease, the bone around those teeth will also be lost. Since there is no support in that area, your skin will droop and it will give you an older-looking appearance.
Fortunately, bone grafting helps regenerate any bone that was lost to periodontal disease.
Essentially, what your dentist is doing is placing natural or synthetic bone that works with your body to help build new bone. Tissue-stimulating growth factor proteins may also be used to help your body regrow bone.
In cases with exposed tooth roots, your dentist may suggest a soft tissue graft. Recovery following the bone big graft procedure varies with each patient, but the entire healing process can take between 4-6 months.
Pinhole Surgery
This particular surgery hasn’t been around long, but some clinicians claim that pinhole surgery can help gum tissue grow back. (7) This would be revolutionary, and the preliminary results are good. However, this procedure is in its infancy and it’s not yet proven to be a long-term solution.
Causes and Risk Factors of Gum Disease
Depending on your individual genetics, lifestyle, diet, and other factors, you may be at a higher or lower risk of gum disease. Let’s look at what science tells us are the most common risk factors. (8, 9)
Smoking & Tobacco Use
This one is no surprise. Studies have shown that smoking causes an increase in gum recession and in bone loss.
If you are a current smoker, you have four times the chance of developing periodontal disease in relation to non-smokers.
Research also shows that periodontal therapy is less effective in smokers than it is in non-smokers. Be above the influence, friends.
Genetics
There has been research done in twins that suggest “50% of susceptibility to [gum] disease is due to host factors.” This could be because twins share very similar environmental and behavioral exposures.
Stress
Everybody suffers from chronic stress in his or her own way. People with higher levels of stress have a greater incidence of developing periodontal disease.
Stress depresses our immune system and causes an imbalance in our homeostasis. When you are stressed out, you release a higher number of inflammatory cells, which can promote tissue damage.
Another reason stress is associated with poor oral hygiene is sometimes, you have other things preoccupying your mind. You may not be giving your oral hygiene the attention it needs in times of emotional stress.
The key takeaway here is: we all need a good massage or a spa day every once in a while. Grab some friends and try to unwind; your mouth will thank you.
Medication
Some medications decrease your salivary flow, which impacts its ability to wash away plaque and debris. This is important because saliva helps prevent plaque buildup and gum inflammation.
These medications include but are not limited to:
Antihistamines
Antihypertensives
Anticonvulsants
Sedatives
Ask your physician if any of the medications you’ve been prescribed causes dry mouth, or “xerostomia.” If so, perhaps your dentist and physician can work together to find another alternative.
Orthodontic Treatment
Some types of partial dentures, braces, or other orthodontic devices can make it hard to remove all the tartar and calculus buildup common to gum disease.
Diet
Studies in adolescents aged 11-18 have shown that kids in this age group do not eat many fruits and vegetables, which are sources high in vitamin C. Moreover, calcium-rich beverages such as milk have decreased while sugary beverages such as sport-drinks have increased.
A decrease in calcium and vitamin C have been associated with an increased risk of periodontal disease.
In general, a diet heavy on carbohydrates (breads, pastas, crackers, sugary treats, etc.) is going to be bad for oral health, particularly when you aren’t keeping up with dental hygiene as well. Keep in mind that your mouth and body as a whole need healthful, whole foods to function well.
Age
There is a caveat to this one: the risk of gum disease doesn’t just go up because a person merely gets older; it’s tied in to various other factors.
For example, as we get older, we lose some of our manual dexterity and thus cannot brush as well as we used to. You may become more forgetful and forget to practice as oral hygiene on a daily routine.
People are also living longer! As we’re retaining our teeth for a longer period of time, they need to be maintained for a longer period of time. This can be hard to do since as we age, we naturally develop many other systemic diseases that negatively impact our oral health.
This brings us to the next point.
Periodontitis and Other Diseases
When you think about gum disease, you shouldn’t think only of your oral health. There are connections between gum disease and other health problems, including diabetes, heart disease, Alzheimer’s, pneumonia, and even cancer.
Diabetes
Poor glycemic control has been associated with higher rates of periodontal disease. (10) The good news is that patients with controlled diabetes respond favorably to periodontal treatment. Check your HbA1c count regularly to make sure your blood sugar is in the target range.
You may also want to consider natural diabetes treatment options, like dietary alteration. These have a great track record of effectively managing blood sugar and A1c levels.
Heart Disease
There has been a lot of research done on the association between cardiovascular disease and periodontitis. High cholesterol and atherosclerotic plaque together may increase the risk for chronic periodontitis. (11)
We have many different inflammatory markers in our bodies that serve a variety of functions. Generally, they are increased when there is injury somewhere in your body and your immune system is trying to defend you.
Both periodontitis and heart disease are associated with the same increase in inflammatory markers, C-reactive protein (CRP) and Interleukin-6 (IL-6). (12)
The only confirmed causal link between oral disease and systemic infection is that of infective endocarditis, an inflammation in the lining of the heart. (13)
Bacteria are more likely to escape into the bloodstream when the biological width, the seal of gums to teeth that serves to protect the alveolar bone, isn’t healthy, like in gum disease. These bacteria can then collect on the heart to cause endocarditis—which is most likely after a root scaling and planing.
Alzheimer’s Disease
There are two mechanisms by which association Alzheimer’s and gum disease are explained.
One theory is that the bacteria in gum disease that seeps into your bloodstream increases inflammatory markers, which leads to systemic inflammation. These markers are capable of crossing into the brain and leading to neuronal damage.
The second mechanism is explained by the bacteria from your plaque crossing into the brain. Dental plaque enters the brain via the bloodstream or peripheral nerves. This organisms then cause and inflammatory response in your central nervous system (CNS), which leads to cognitive impairment. (14)
A team of researchers released a compelling study in 2019 introducing a possible causation between gum disease and Alzheimer’s. (15) While this hasn’t been confirmed by other studies or human trials, it’s enough to consider being more diligent treating gum disease.
Hematologic Disorders (Leukemia)
Gingival hyperplasia, which is overgrowth of gum tissue around the teeth, can be an early symptom of acute leukemia. (16)
Chemotherapy or bone marrow transplantation can also negatively affect gingival health. Some of the symptoms are abscesses, inflamed gums, or severe redness.
Pneumonia
The same people at risk for pneumonia are typically those at risk for gum disease. Although it’s not clear if one causes or contributes to the other, they are closely connected.
One proposed reason for this connection is that patients in hospitals and nursing homes that frequently contract pneumonia also can’t keep up with good oral care. This may upset the oral microbiome and set the stage for other immune system-compromising infection. (13)
How to Prevent Gum Disease
There are several things you can do regularly if you notice warning signs of gum disease—or to prevent these from ever happening.
Brush twice a day for 2 minutes. Use your smartphone or a brush timer as a measurement of time to how long you’ve been brushing.
Floss at least once a day to remove plaque from places your toothbrush can’t get access to. You know when your mom tells you to clean your room, and you think it’s clean, but then she goes in and finds areas that aren’t really clean? It’s basically the same concept, but with flossing.
Avoid smoking (anything) and all forms of tobacco. This includes cigarettes, cigars, “dip” or chewing tobacco, and hookah. Being healthy is the new cool.
Maintain a healthy diet. Now, I’m not telling you to go vegan, but I am telling you that it’s important to add fruits and vegetables to get your daily dose of vitamin C and calcium.
Ask your physician if any of your medications cause dry mouth, or “xerostomia.” If they do, ask if there are any other alternatives available. It’s important for different healthcare providers to be in contact so we can provide you with the best possible care.
Tape your mouth shut at night. Weird habit, but great results. Mouth taping cuts down on mouth breathing while you sleep. This, in turn, can help resolve dry mouth.
Don’t use conventional mouthwash. I know what you’re thinking. This is the stuff that’s supposed to give me a cleaner mouth and me have kissable breath! But it’s just not good for your oral health.
So many mouthwashes have a high alcohol content, which dries your mouth and disrupts your oral microbiome. Dry mouth and an imbalance of bacteria are both risks for plaque retention. You can read more about other DIY mouthwash alternatives here.
Try natural methods of gum disease prevention. These may include using turmeric in a lot of your recipes, oil pulling, and taking oral probiotics to support a healthy oral microbiome.
Into DIY-ing? Dr. B created a great DIY recipe for toothpaste specifically for healthier gums. You can check it out and try it for yourself by reading this article.
Always, always schedule regular check-ups and professional cleanings. You will have a much less chance of developing anything suspicious if your dentist is monitoring your health. Remember, preventative is always better than constructive!
Common Questions About Gum Disease
Q:
What’s the difference between gingivitis and gum disease?
A: Gingivitis is the early, reversible stage of gum disease. The main difference here is that in gingivitis, there is no loss of bone or loss of connective tissue. Not all cases of gingivitis result in gum disease, but it can if left untreated.
Once bacteria have seeped deep below your gum line, it starts to destroy gum tissue, your periodontal pockets deepen, and some of your bone is lost. Your teeth become mobile and loose because it doesn’t have as much support from bone anymore. This is when you have advanced into Stages II-IV of periodontitis.
Q:
How common is gum disease?
A: Very common! In a study titled “Prevalence of Periodontitis in Adults in the United States” found that 47.2% or roughly 64.7 million American adults have either mild, moderate, or severe periodontal disease. This is even higher in adults aged 65 and older, at about 70.1%.
On a greater scale, we are looking at 743 million people afflicted, according to the FDI World Dental Federation. I would classify this as sort of an epidemic, wouldn’t you? It’s quite a shocking number, but the severity and prevalence is real, and we need to take more measures in preventing it.
Q:
Can you die from gum disease?
A: You cannot die from gum disease, per se. Keep in mind that your mouth is linked to your systemic health, rather than an isolated ecosystem on its own. This means that gum disease can lead to or heighten other diseases related to your overall health.
As mentioned earlier, there is an inflammatory marker called C-reactive protein (CRP) that increases when infection triggers your immune system. This inflammatory marker has also been linked to cardiovascular disease. Periodontal treatment has shown to decrease inflammation and thus decrease CRP.
Gum disease has also been associated with complications such as diabetes, Alzheimer’s, and cancer to name a few.
Q:
Can I get rid of gum disease without a dentist?
A: The only stage you can get rid of without a dentist is Stage I, gingivitis. At this stage, a daily brushing and flossing regimen can reverse your gingival inflammation. As mentioned in the study conducted by Harald Loe, you can reverse your gingivitis in an average of 9-21 days if you are consistent (which you should always be).
However, if you surpass that stage and progress into advanced stages of gum disease, you will need the intervention of your dentist or hygienist. The reason for this being so is gingival recession, bone loss, and deep pocket depths cannot be reversed by simply brushing and flossing.
Depending on your symptoms and clinical manifestations, your dentist or periodontist will suggest a scaling-and-root planing procedure, flap surgery, or bone graft. Be open with your dentist about any questions or concerns you have with a procedure.
Q:
Does gum disease go away when teeth are removed?
A: In addition to cavities, gum disease is one of the major reasons for tooth extraction. Tooth extraction may be a treatment option to prevent infections from spreading and additional tooth loss. Extracting a tooth can lead to changes in your dietary habits, your bite, and your overall quality of life.
There are several elements that come into play here, such as the function of the specific tooth being extracted, how it will affect your mastication (chewing) after it is removed, and how deep the lesion is on that tooth. (18)
Ideally, dentists do not want to extract your teeth; our goal is to be as minimally invasive as reasonably possible. Unfortunately, the disease becomes so advanced in certain situations that the tooth has to come out to prevent further destruction.
Q:
How can I fix loose teeth from gum disease?
A: You definitely can’t go to a steakhouse with loose teeth. If your tooth is loose, but still in its socket, just keep it in place until you see a dentist. Until then, it is important you keep the area clean as it is now a risk for potential infection.
One way a dentist can tighten that loose tooth is through a process called “splinting.” The adjacent teeth are “splinted,” or attached together. This stabilizes any loose teeth and prevents them from moving.
Other treatments for loose teeth were discussed earlier such as deep professional cleanings, scaling-and-root planing, and bone grafting.
Key Takeaways: Gum Disease
Prevention is of utmost importance in your oral health as well as your systemic health. As we have seen, gum disease has been associated with a plethora of other problems. If you treat gum disease at an early stage, that will decrease your probability in treating other diseases.
If you make small, conscious decisions every day, you can save your oral health.
There are so many things you can do in your everyday routine to prevent you from getting gum disease. The types of foods you eat (or don’t eat), smoking cessation, daily brushing and flossing, and keeping up with dental checkups will go a long way.
You can reverse the beginning stage of gum disease. Gingivitis can be reversed completely by you, but you won’t know when it advances to a point where you can’t control it anymore.
Regular cleanings by your dentist or hygienist can prevent gingivitis from developing. Your routine check-ups will also allow your dentist to screen for anything that may or may not be suspicious, but if so, address and treat it promptly.
Got more questions about gum disease? Send a message to Dr. Burhenne and he can hook you up with whatever you need!
18 References
Tolmie, P., DDS, Rasenberger, K., DMD, & Van Kesteren, C., DDS. The Four Levels of Periodontal Disease. Retrieved from https://www.northstateperio.com/pdfs/newsletters/4%20Levels%20of%20Perio%20Dz.pdf
American Academy of Periodontology. Types of gum disease. Retrieved from: https://www.perio.org/consumer/types-gum-disease.html
Theilade, E., Wright, W. H., Jensen, S. B., & Löe, H. (1966). Experimental gingivitis in man: II. A longitudinal clinical and bacteriological investigation. Journal of periodontal research, 1(1), 1-13. Abstract: https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1600-0765.1966.tb01842.x
Pihlstrom, B. L., Michalowicz, B. S., & Johnson, N. W. (2005). Periodontal diseases. The lancet, 366(9499), 1809-1820. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/16298220
American Dental Hygienists’ Association. (1998). American Dental Hygienists’ Association Position Paper on the Oral Prophylaxis. Retrieved from: https://www.adha.org/resources-docs/7115_Prophylaxis_Postion_Paper.pdf
National Institutes of Health. (2008). Periodontal (Gum) Disease: Causes, Symptoms, and Treatments. Retrieved from https://www.nidcr.nih.gov/sites/default/files/2017-09/periodontal-disease_0.pdf
Chao, J. C. (2012). A novel approach to root coverage: the pinhole surgical technique. International Journal of Periodontics & Restorative Dentistry, 32(5). Abstract: https://www.ncbi.nlm.nih.gov/pubmed/22754900
Van Dyke, T. E., & Dave, S. (2005). Risk factors for periodontitis. Journal of the International Academy of Periodontology, 7(1), 3. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1351013/
AlJehani, Y. A. (2014). Risk factors of periodontal disease: review of the literature. International journal of dentistry, 2014. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4055151/
Taylor, G. W., Manz, M. C., & Borgnakke, W. S. (2004). Diabetes, periodontal diseases, dental caries, and tooth loss: a review of the literature. Compendium of continuing education in dentistry (Jamesburg, NJ: 1995), 25(3), 179-84. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/15641324
Bahekar, A. A., Singh, S., Saha, S., Molnar, J., & Arora, R. (2007). The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. American heart journal, 154(5), 830-837. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/17967586
Loos, B. G., Craandijk, J., Hoek, F. J., Dillen, P. M. W. V., & Van Der Velden, U. (2000). Elevation of systemic markers related to cardiovascular diseases in the peripheral blood of periodontitis patients. Journal of periodontology, 71(10), 1528-1534. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/11063384
Li, X., Kolltveit, K. M., Tronstad, L., & Olsen, I. (2000). Systemic diseases caused by oral infection. Clinical microbiology reviews, 13(4), 547-558. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC88948/
Abbayya, K., Puthanakar, N. Y., Naduwinmani, S., & Chidambar, Y. S. (2015). Association between periodontitis and Alzheimer’s disease. North American journal of medical sciences, 7(6), 241. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4488989/
Dominy, S. S., Lynch, C., Ermini, F., Benedyk, M., Marczyk, A., Konradi, A., … & Holsinger, L. J. (2019). Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Science advances, 5(1), eaau3333. Full text: https://advances.sciencemag.org/content/5/1/eaau3333
Demirer, S., Özdemir, H., Şencan, M., & Marakoḡlu, I. (2007). Gingival hyperplasia as an early diagnostic oral manifestation in acute monocytic leukemia: a case report. European journal of dentistry, 1(2), 111. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2609944/
American Academy of Periodontology. (2012). Retrieved from: https://www.perio.org/consumer/cdc-study.htm
Chrysanthakopoulos, N. A. (2011). Periodontal reasons for tooth extraction in a group of greek army personnel. Journal of dental research, dental clinics, dental prospects, 5(2), 55. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3429994/
The post Gum Disease: Stages, Prevention, and Treatment appeared first on Ask the Dentist.
Gum Disease: Stages, Prevention, and Treatment published first on https://wittooth.tumblr.com/
0 notes