#choriocarcinomas
Text
Super gostosa se masturbando em live
izy telo vavy
Become Neighbor Who Gets Rejected By Mina Moon, Calls In Favor & Has Mina Moon's Family Detained...
Asian Girl Gets Stuck and Fucked
Sirenita Fuentes - Caliente Navidad
Ebony wife has orgasm on sex machine
Morena gostosa debaixo da saia
Policial Pegando no Pau Dentro do Onibus
Guy finds out old mom toying his teen gf
Those tits want some Cum Compilation
#diactine#Brout#faculties#marshalled#rorschach#spademen#redia#unliberated#sulfuryls#plot's#choriocarcinoma#misdirecting#traffic#yester-year#undisgraced#derust#swerved#farmtown#Ruffi#wolfhound
0 notes
Text
Sex cancer does exist.
It's called Choriocarcinoma.
7 notes
·
View notes
Text
ABORTION RIGHTS
I’ve not told many but in 1966 I was a young mother expecting another child when something went wrong with the pregnancy. I was in my fifth month when I had what they then called “a partial miscarriage” but, because restrictive abortion laws were in place, I was told there was nothing I could do except “wait because you still could be pregnant.”
I’ll not go into detail but my doctor and I knew that there was no way that there would be a viable pregnancy but the law would not allow my doctor to do anything and I was forced to carry the dead fetus for two more months until I went into active labor and was admitted into the hospital.
A day or two later, when I was home, I received an urgent call from my OB asking that Ben and I "come to my office immediately” and I remembered thinking that something was seriously wrong.
Pathology reports had come back and I needed surgery – I had choriocarcinoma – a malignant fast growing cancer that has its origins from cells that would normally attach themselves to the uterus and form the placenta.
I had surgery the next afternoon and for almost a year after that I was checked monthly to make sure no cancer cells existed in my body.
And this is what this court and these pro-life people want us to go back to because “all life is precious.”
And so was mine.
28 notes
·
View notes
Text
Reasons to not have kids:
* Increased likelihood of autoimmune disease
* Pelvic floor dysfunction
* Diastasis recti
* Depression
* Anxiety
* Postpartum psychosis
* Choriocarcinoma
* Pregnancy is not representative of a woman!!
* Takes 7 years for your body to recover
P.s: the list goes on :)

#feminist#love#twitter#weird stuff#weirdcore#nahhhh#ew fanart#young royals#fandom#fanart#smut#new writer boost#new writers corner#new writerblr#new writers on tumblr#poems on tumblr#new writers society#dank memes#lol
1 note
·
View note
Text
Germ Cell Tumors - Causes, Symptoms, and Treatment Options - Dr. Mark Cabelin's Firewa ll
Germ cell tumors are a type of neoplasm that primarily originate from germ cells, which give rise to eggs in females and sperm in males. They can occur anywhere in the body but are most commonly found in the ovaries, testicles, and areas where germ cells usually don't reside, such as the chest, abdomen, or brain. Although germ cell tumors are relatively rare, they represent a significant proportion of cancers in adolescents and young adults.
Despite their potential severity, advancements in urology and oncology have led to effective treatment options, and the prognosis for patients with germ cell tumors has improved significantly over the past few decades. The key to successful treatment often lies in early detection and a comprehensive understanding of the tumor's nature and behavior,

Germ cell tumors arise from germ cells, unique cells involved in reproduction. They are the precursors to both egg and sperm cells. Unusual growth of these cells can lead to tumors, which can be benign (non-cancerous) or malignant (cancerous). Malignant germ cell tumors can be life-threatening if not treated promptly and effectively, Dr. Mark Cabelin.
Germ cell tumors are broadly categorized into two types: seminomas and non-seminomas. Seminomas are usually slower-growing and more responsive to radiation therapy. Non-seminomas are more aggressive and comprise several subtypes, including embryonal carcinoma, yolk sac carcinoma, choriocarcinoma, and teratoma. Each of these subtypes has its unique characteristics and requires specific treatment strategies.
In the field of urology, germ cell tumors, specifically testicular germ cell tumors, are of paramount importance. They constitute the majority of testicular cancers, making their understanding crucial for urologists. These tumors often present unique diagnostic and therapeutic challenges, necessitating a multidisciplinary approach involving urologists, oncologists, radiologists, and pathologists.
Their management extends beyond surgical intervention, encompassing chemotherapy, radiation therapy, and constant surveillance. Understanding germ cell tumors is thus critical for comprehensive patient care in urology. Understanding the causes of germ cell tumors is crucial for prevention and treatment.
While the exact cause is unknown, several factors are believed to contribute to their occurrence. Specific genetic abnormalities have been linked to the development of germ cell tumors. For instance, individuals with disorders of sex development (DSDs), who have unusual stories of sexual anatomy, are at a higher risk.
Additionally, carrying specific mutations in genes, such as the c-KIT gene, has been associated with an increased incidence of these tumors. Exposure to certain environmental factors may also increase the risk of developing germ cell tumors. These include exposure to chemicals, radiation, or certain drugs during pregnancy. Smoking and excessive alcohol use have also been implicated.
Research is ongoing to understand the complex interplay of genetic predisposition and environmental exposure in the development of germ cell tumors. The symptoms of germ cell tumors can vary greatly depending on their location and size. The most common sign of testicular germ cell tumors is a painless lump or swelling in the testes.
Other symptoms may include discomfort or pain in the testicle or scrotum, a feeling of heaviness in the scrotum, or a sudden collection of fluid in the scrotum. In females, ovarian germ cell tumors may cause abdominal pain or swelling. When germ cell tumors occur in other areas of the body, symptoms might include chest pain, cough, shortness of breath, or neurological symptoms if the cancer is in the brain.
It’s important to remember that these symptoms can also be caused by conditions other than germ cell tumors, so it’s essential to consult a healthcare professional for an accurate diagnosis. If left untreated, germ cell tumors can grow and spread to other body parts, leading to severe complications. Potential risks include metastasis, where the cancer spreads to other organs, which can significantly complicate treatment and worsen the prognosis, Dr. Mark Cabelin Urologist.
Germ cell tumors can also cause functional disturbances in the affected organ, such as infertility in men if the cancer is in the testes. In addition, treatments for germ cell tumors, like surgery, chemotherapy, and radiation therapy, can also have side effects and long-term health impacts. Regular follow-ups are necessary to monitor for potential complications and manage them promptly.
Diagnosing germ cell tumors usually involves a combination of physical examination, medical history review, and diagnostic tests. The first step often involves a thorough physical examination where the physician may check for lumps or abnormal growth. A detailed discussion about the patient's health history can also provide valuable insights, as certain genetic diseases or previous cancer treatments can increase the risk of germ cell tumors.
Imaging tests play a vital role in diagnosing and staging germ cell tumors. These can include ultrasound, often the first test for suspected testicular or ovarian tumors. It can determine whether a lump is solid (likely cancer) or filled with fluid (probably a cyst).
Computed Tomography (CT) scans, and Magnetic Resonance Imaging (MRI) can help detect tumors in other body parts and determine if cancer has spread. Positron Emission Tomography (PET) scans may also detect metastasis or evaluate the response to treatment. Pathological tests are essential for confirming the diagnosis and understanding the type and stage of the germ cell tumor.
These tests often involve a biopsy, where a tissue sample is removed from the tumor and examined under a microscope. A biopsy can reveal the presence of cancer cells and provide insights into the tumor's aggressiveness. Other pathological tests, such as serum tumor marker tests, measure the levels of certain substances in the blood that may increase when a germ cell tumor is present.
Pathological diagnosis is crucial in urology for the management of germ cell tumors. Treating germ cell tumors is typically a multidisciplinary effort involving urologists, oncologists, and other healthcare professionals.
Treatment decisions are based on factors such as the type and stage of the tumor, the patient's overall health, and personal preferences. Surgery is often the first line of treatment for germ cell tumors. The goal is to remove the cancer entirely.
In males, this may involve a radical inguinal orchiectomy, the surgical removal of the entire testicle. In females, surgery may include the removal of one or both ovaries. In some cases, lymph nodes in the abdomen may also need to be removed.
Radiation therapy uses high-energy rays to kill cancer cells. It's often used in conjunction with surgery, either before to shrink the tumor or after to kill any remaining cancer cells. Radiation therapy can also treat germ cell tumors that have spread to other body parts.
Chemotherapy is a systemic therapy that uses drugs to kill cancer cells throughout the body. It's often used when advanced germ cell tumors have spread to other body parts. Several chemotherapy regimens are used to treat germ cell tumors, and the choice of regimen depends on factors such as the type and stage of the tumor and the patient's overall health. Research is ongoing to develop more effective and less toxic treatments for germ cell tumors.
These emerging treatments include targeted therapies that aim to attack specific characteristics of cancer cells and immunotherapies that help the body's immune system fight cancer. Clinical trials are exploring the potential of these new treatments, and patients with germ cell tumors may have the opportunity to participate in these trials. Germ cell tumors, although rare, can have significant implications on a patient's health and quality of life.
Early detection and prompt treatment are crucial to improving the prognosis and reducing the risk of complications. Diagnosis involves comprehensive physical examinations, imaging tests, and pathological tests. Treatment is typically multidisciplinary, involving surgery, radiation therapy, and chemotherapy, often in combination.
Interestingly, the field of urology continues to explore new and innovative treatment methods, including targeted therapies and immunotherapies. Regular follow-ups, monitoring, and patient education are also integral to managing this condition effectively. Remember, each patient's journey is unique, and treatment should be personalized based on their specific circumstances and preferences.
Click Here-
https://www.linkedin.com/in/mark-cabelin-a544158
youtube
0 notes
Text
Gestational Trophoblastic Neoplasia
Understanding and Managing a Unique Pregnancy-Related Condition
Introduction:
Gestational Trophoblastic Neoplasia (GTN) is a rare group of tumors that develop from abnormal growth of cells in the uterus during pregnancy. While most pregnancies progress without any complications, GTN can occur in a small percentage of cases. Understanding GTN, its subtypes, causes, symptoms, diagnosis, and treatment options is crucial for early detection and effective management. In this blog, we will explore the world of Gestational Trophoblastic Neoplasia and shed light on this unique pregnancy-related condition.
Understanding Gestational Trophoblastic Neoplasia:
Gestational Trophoblastic Neoplasia refers to a group of tumors that arise from the placental trophoblast cells, which normally support the growth of the embryo during pregnancy. The different subtypes of GTN include Hydatidiform Mole (complete or partial), Invasive Mole, Choriocarcinoma, Placental Site Trophoblastic Tumor, and Epithelioid Trophoblastic Tumor. These tumors have distinct characteristics and can range from benign to malignant.
Causes and Risk Factors:
The exact cause of GTN is still not fully understood. However, certain factors can increase the risk of developing GTN:
Previous history of molar pregnancy: Women who have had a previous molar pregnancy are at a higher risk of developing GTN in subsequent pregnancies.
Age: Women younger than 20 or older than 40 years have a slightly higher risk of GTN.
Previous miscarriage or stillbirth: A history of recurrent miscarriages or stillbirths may slightly increase the risk of GTN.
Recognizing the Symptoms and Diagnosis:
The symptoms of GTN can vary depending on the subtype and stage of the tumor. Common symptoms may include:
Vaginal bleeding or spotting during or after pregnancy
Enlarged uterus or a rapidly growing abdomen
Severe nausea and vomiting (hyperemesis gravidarum)
Pelvic pain or discomfort
Anemia (low red blood cell count) or fatigue
If GTN is suspected, a series of diagnostic tests will be conducted, including:
Ultrasound: An ultrasound examination can help visualize the uterus and detect any abnormal growths or masses.
Beta-human chorionic gonadotropin (β-hCG) blood test: β-hCG levels are typically elevated in GTN. Serial measurements can help monitor the response to treatment and detect any recurrence.
Tissue biopsy: A biopsy of the suspected tumor may be performed to confirm the diagnosis and determine the subtype of GTN.
Treatment Options for GTN:
The treatment approach for GTN depends on various factors, including the type and stage of the tumor, the patient's desire for future pregnancies, and overall health. The primary treatment options include:
Surgery: In cases of localized GTN, surgery may be performed to remove the tumor and surrounding affected tissues. This is often the preferred option for non-metastatic GTN.
Chemotherapy: Chemotherapy is the mainstay of treatment for GTN. It involves the use of drugs to kill cancer cells and prevent their spread. Chemotherapy is highly effective in treating GTN, even if it has spread to other organs or if the tumor is malignant.
Radiation therapy: In some cases, radiation therapy may be used to target and destroy cancer cells. It is typically used in combination with chemotherapy for advanced or persistent GTN.
Follow-up and monitoring: Regular follow-up visits, including β-hCG testing, are essential to monitor the response to treatment, detect any recurrence, and provide ongoing support and counseling.
Prognosis and Future Pregnancies:
The prognosis for GTN is generally good, especially when detected and treated early. The majority of women with GTN can be cured, and the chances of having a successful future pregnancy are usually excellent. However, close monitoring and appropriate follow-up are crucial to ensure the best possible outcomes.
Conclusion:
Gestational Trophoblastic Neoplasia is a unique group of tumors that can develop during pregnancy. Early detection and appropriate management are essential for a positive prognosis. By understanding the causes, recognizing the symptoms, and seeking timely medical attention, women and healthcare professionals can work together to effectively treat GTN and support future pregnancies. With advancements in diagnostic techniques and treatment options, the outlook for individuals affected by GTN continues to improve, offering hope and reassurance to those facing this rare pregnancy-related condition.
0 notes
Text
Molar Twin Deliveries with Coexisting Fetus at Term: Concerning Two Uncomplicated Cases of Gestational Trophoblastic Tumor, From 2015-2021, In Conakry, Guinea
Abstract
The coexistence of a molar pregnancy with a live fetus is a rare entity of difficult diagnosis and treatment. Continuation of the pregnancy until full-term delivery is possible. We report two cases of twin molar deliveries observed empirically from 2015-2021, in the gynecology-obstetrics department of the Donka national hospital and in the maternity ward of the Jean Paul II hospital in Conakry. The discovery was made on ultrasound of the first trimester of pregnancy and macroscopic examination of the placenta. One of the neonates was alive, a healthy female and the other was polymal formed with facial dysmorphism, omphalocele and sexual ambiguity, fresh stillborn. There was no maternal complication towards a gestational trophoblastic tumor (T.T.G) in both cases. Efforts must be made in the prevention of T.T.G. by screening for twin molar pregnancies with healthy fetuses on transvaginal ultrasound in the first trimester, the dosage of HCG in the face of unexplained metrorrhagia, macroscopic observation of the placenta after each delivery and biopsy sampling of any suspicious placenta.
Introduction
Complete moles with a coexisting fetus, evolving at term with spontaneous vaginal delivery, without fetal and maternal complications, are rare. Early diagnosis of this association leads in the majority of cases to termination of pregnancy on the one hand because of the frequency of triploidy and on the other hand because of the maternal risk and the possibility of progression to persistent trophoblastic disease [1]. We report two particular cases of twin molar deliveries at term without fetal complication and without progression to maternal gestational trophoblastic disease in the gynecology-obstetrics department of the Donka national hospital, the Teaching Hospital (C.H.U) of Conakry and in the maternity ward of the Jean Paul II hospital in Conakry.
Patients and Observations
Case 1
This was Mrs. D.F.B, aged 19, primigravida and primiparous, with no particular history, admitted while in labor at the gynecology- obstetrics department of Donka National Hospital, Conakry Teaching Hospital, with two results of ultrasound performed with a transparietal probe during her pregnancy. These results did not mention any notion of hydatidiform mole or associated congenital malformation. The pregnancy would have progressed normally until its term without maternal or fetal complications. It was only after the delivery of a fresh stillborn, polymalformed (with facial dysmorphism, omphalocele and sexual ambiguity) child, that the macroscopic examination of the placenta made it possible to make the diagnosis of presumptive mole twin by the presence of a normal placenta attached to a vesicular mass characteristic of a mole. The biopsy sample allowed the histological diagnosis of a complete mole. The post molar follow- up had been organized without maternal complication 61 days before the closure of the service for renovation, on October 5, 2015.
Case 2
This was Mrs. H.C, seamstress, 30 years old, gravidity of 5 and parity of 5 including a twin birth and a laparotomy for ruptured ectopic pregnancy (GEU), who came on her own for a consultation for incoercible vomiting, physical asthenia on a menorrhea of 3 three months, June 19, 2020. The clinical examination had objectified a uterine height greater than the age of amenorrhea and dating ultrasound had made it possible to observe, intrauterine, a normal eutrophic fetus of 13 weeks – Amenorrhea (W.A) and a poorly vascularized heterogeneous multicystic mass. The beta HCG serum marker level was 16000IU/l. We had concluded a twin molar pregnancy and animated counseling on the interest of a medical termination of pregnancy to avoid the risks associated with serious maternal complications of trophoblastic tumor including choriocarcinoma. The couple, after a delay of two weeks, had opted to continue the pregnancy until its term. A pregnancy monitoring and childbirth preparation plan had been drawn up with the pregnant woman, whose morphological ultrasound at the 23rd W.A of the second trimester carried out on 03/09/2020, which had objectified a mass of 81 x 97 mm, in previa position. The pregnancy had progressed, without fetal and maternal complications, at 40 WA 2 days and ended with a vaginal delivery of a normal female child, alive and weighing 2830 grams. The woman had benefited from active management of the third stage of labor (TSLM) and digital uterine dissection to confirm the uterine cavity. Macroscopic examination of the adnexa had confirmed the presence of two separate placentas, joined together (Figure 1), one of which appeared normal and linked to the umbilical cord and had a histologically confirmed vesicular mass of “complete mole”. The planned post-molar follow-up was regular with progressive regression of the beta HCG level until negativity on the fortieth day of delivery without any clinical particularity on the closing date of January 31, 2021.
Discussion
The diagnosis of the association of a live fetus with a normal karyotype with a hydatidiform mole is often difficult, especially in the absence of revealing clinical signs [2,3]. The diagnostic modalities of molar twin pregnancy associating a complete mole with a healthy fetus were different due to the early ultrasound detection in the first trimester and the observation of the placenta. The lack of diagnosis of the coexisting mole during pregnancy despite the two ultrasound examinations in the first case would be linked to the age of the ultrasound scanners, which are often second-hand, the technique used (endovaginal in the first trimester or transparietal) and of the operator’s experience in the first observation. Early ultrasound detection made it possible to develop a follow-up plan for pregnancy, childbirth and postpartum in the second case. In the event of a twin pregnancy associating a live fetus and a molar pregnancy, the pregnancy can be continued until term if the patient wishes after having been informed of the risks and the most frequently reported complications (hemorrhages, late miscarriage, fetal death in utero and preeclampsia) [3]. Evacuation of the pregnancy is required only in cases of fetal anomalies or deterioration of the maternal condition [4]. The probability of obtaining a live birth varies between 16 and 56% [5] or 16 and 60% [4] deliveries. The continuation of the pregnancy is against payment given the risks of immediate and distant maternal complications. Close monitoring of the mother and fetus can help achieve a favorable outcome [4]. We accepted monitoring despite the maternal risks for one of our two pregnant women. The two pregnancies resulted spontaneously in the normal delivery at term of a healthy living fetus and another which would have succumbed to its multiple malformations per partum. The most feared complication is progression to gestational trophoblastic disease [1]. The diagnosis of postmolar Gestational Trophoblastic Tumor (G.G.T.) can be made according to criteria such as the persistence of h.C.G detectable more than 6 months after uterine evacuation and the histological diagnosis of choriocarcinoma [5]. According to Ikram Boubess et al., who adopted termination of two of these pregnancies, one remotely progressed to an invasive mole [6]. Regular monitoring of h.C.G levels throughout pregnancy and the postpartum period is necessary to detect GTN [7]. For Suksai M et al., a pregnancy with an initial serum h.C.G level of less than 400,000m.U.I/ml is a good candidate for the continuation of the pregnancy and the achievement of fetal viability [8]. The incidence of post-molar GTN is higher in twin pregnancies combining a complete hydatidiform mole (CHM) and a normal fetus than in single CHM [9].
Conclusion
Spontaneous evolution of the association of molar pregnancy with a live-to-term fetus, without immediate fetal and maternal complications, is possible. The most formidable complication, gestational trophoblastic tumor, choriocarcinoma, was not observed during the study period. The prevention of this complication requires the training of providers in endovaginal ultrasound, its systematic practice in the first trimester of pregnancy, ultrasound and biological monitoring of suspected cases during pregnancy, systematic macroscopic examination of the placenta with biopsy of cases suspect for histological confirmation.
0 notes
Text
DRUG OF CHOICE SERIES
ANTICANCER DRUGS
▪️Drug of choice for breast cancer - Tamoxifen
▪️Drug of choice for glioma - Nitrosourea
▪️Drug of choice for colorectal cancer - 5 Fluorouracil
▪️Drug of choice for choriocarcinoma - Methotrexate
▪️Drug of choice for pancreatic carcinoma - Gemcitabine
▪️First line chemotherapy for cervix carcinoma - Cisplatin
▪️Drug of choice for the brain tumor - Lomustine
▪️Drug of choice for prostate carcinoma - Flutamide
▪️Drug of choice for insulinoma - Streptozotocin
▪️Drug of choice for polycythemia vera - Busulphan or Chlorambucil
▪️Drug of choice for carcinoma of endometrium - Progestins
▪️Drug of choice for kaposi sarcome - IF2 alpha
▪️Drug of choice for CLL - Chlorambucil or Fludarabine
▪️Drug of choice for acute myelocytic leukemia - Cytarabine with Mitoxantrone
▪️Drug of choice for wilm's tumor - Vincristine with Danctinomycin
▪️Drug of choice for acute promyeloblastic leukemia - Retinoic acid
▪️Drug of choice for hairy cell leukemia - Cladarabine
▪️Drug of choice for thyroid carcinoma-1-131 with Doxarubicin and cisplatin
▪️Drug of choice for stomach cancer - Fluorouracil with Cisplatin
▪️Drug of choice for CML-Imatinib or Busulfan
▪️Drug of choice for acute lymphocytic leukemia (ALL) - Vincristine +Prednisolone +Mercaptopurine + Cyclophosphamide +Methotrexate
▪️Drug of choice for ovarian cancer - Cisplatin with Paclitaxel
▪️Drug of choice for lung cancer - Cisplatin with Taxane
▪️Drug of choice for malignant melanoma - Dacarbazine
▪️Drug of choice for testicular cancer - Bleomycin+ Etoposide + Cisplatin

0 notes
Text
Ung thư nhau thai
Phụ nữ có thể mắc ung thư nhau thai nếu có thai trứng, từng sẩy thai, phá thai… với triệu chứng như chảy máu âm đạo nặng, đau vùng chậu dữ dội.
Ung thư nhau thai (choriocarcinoma) do mô bất thường phát triển sau khi tinh trùng thụ tinh với trứng bên trong tử cung. Có nhiều trường hợp mắc ung thư nhau thai nhưng có thể mang thai bình thường và sinh con khỏe mạnh.
Theo Hiệp hội Ung thư lâm sàng Mỹ, di truyền không ảnh hưởng đến khả năng mắc ung thư nhau thai. Các nhà nghiên cứu đã không tìm thấy mối liên hệ trực tiếp giữa các gene hoặc đột biến cụ thể với loại ung thư này. Tuy nhiên, tiền sử gia đình mang thai bất thường có thể làm tăng nguy cơ phát triển ung thư nhau thai.
Yếu tố rủi ro lớn nhất có thể mắc ung thư nhau thai là có một khối hiếm phát triển trong tử cung khi bắt đầu mang thai. Tình trạng này được gọi là thai trứng. Khối này trông giống như một chiếc túi chứa đầy chất lỏng, có thể biến thành khối u và trở thành ung thư.
Các yếu tố nguy cơ khác có thể khiến phụ nữ phát triển ung thư nhau thai như có tiền sử thai trứng, từng sảy thai hoặc phá thai, từng mang thai ngoài tử cung, mang thai dưới 20 tuổi hoặc trên 35 tuổi, có tiền sử gia đình hoặc bản thân mắc u lành trong tử cung, có khối u âm đạo.
Người có nồng độ hormone gonadotropin màng đệm ở người (HCG) cao, có hàm lượng caroten và vitamin A thấp, nhóm máu A hoặc AB, hút thuốc cũng có khả năng mắc ung thư này. Hầu hết các yếu tố gây ung thư nhau thai đều nằm ngoài tầm kiểm soát nhưng nếu bạn đang mang thai hoặc dự định có thai nên tránh hút thuốc để không làm tăng nguy cơ mắc bệnh.
Bồn nôn và nôn mửa nặng khi mang thai là dấu hiệu có thể cảnh báo ung thư nhau thai. Ảnh: Freepik.
Bồn nôn và nôn mửa nặng khi mang thai là dấu hiệu cảnh báo có thể mắc ung thư nhau thai. Ảnh: Freepik.
Các triệu chứng ung thư nhau thai khác nhau ở từng người. Nhiều triệu chứng của ung thư này tương tự như một số triệu chứng mang thai bình thường nên việc chẩn đoán thường khó khăn. Các triệu chứng phổ biến có thể cảnh báo ung thư nhau thai như chảy máu âm đạo bất thường, áp lực ở vùng chậu, buồng trứng và tử cung mở rộng bất thường, u nang hoặc nốt sần hình thành bên trong buồng trứng, buồn nôn và nôn nặng trong thời kỳ mang thai, thiếu máu (số lượng hồng cầu thấp). Bạn cũng có thể xuất hiện các triệu chứng hiếm gặp gồm chóng mặt, nhức đầu, co giật, tức ngực, ho, khó thở và đau bụng.
Ung thư nhau thai có thể gây ra các biến chứng nếu không được phát hiện và điều trị kịp thời gồm nhiễm trùng tử cung, nhiễm trùng huyết, sốc xuất huyết (phản ứng đe dọa tính mạng do mất máu nghiêm trọng), cường giáp (tuyến giáp hoạt động quá mức), tiền sản giật (huyết áp cao). Ung thư có thể lây lan qua máu đến các cơ quan khác và gây ra các biến chứng tại nơi ảnh hưởng. Nếu ung thư lan đến não có thể gây ra các vấn đề về thần kinh, lan đến vùng ngực có thể ảnh hưởng đến hô hấp.
Vì một số triệu chứng ung thư nhau thai khó phân biệt với tình trạng mang thai bình thường và các tình trạng khác, phụ nữ nên khám sàng lọc trước khi muốn thụ thai và trước sinh để loại trừ khả năng mắc ung thư này.
Trong thai kỳ, nếu mẹ bầu có các dấu hiệu cho thấy nhiều khả mắc ung thư nhau thai nên đến ngay bệnh viện để kiểm tra và điều trị. Các dấu hiệu này có thể gồm chảy máu âm đạo nặng hoặc đột ngột, phát triển mô trong âm đạo và rò rỉ dịch từ âm đạo, nôn mửa và buồn nôn nghiêm trọng, đau bụng hoặc đau vùng chậu dữ dội, đau lưng dưới nặng, tức ngực, co giật.
0 notes
Text
Gynecological Cancer In Ahmedabad, Gujarat , India | Dr. Nitin Singhal

Cancers affecting the female reproductive organs are classified under gynecological cancers. Cancers that are included in gynecological cancers include cervical cancer, vaginal cancer, ovarian cancer, vulvar cancer and uterine cancer. gynecological cancer diagnosis Symptoms commonly associated with gynecological cancer include vaginal bleeding that is not normal, bloating or swelling that persists in the abdominal area, weight gain or loss, persistent diarrhea or constipation. Gynecological cancer is diagnosed only after thorough gynecological and examination. Imaging techniques such as ultrasound, CT and PET/CT scan are also used for accurate diagnosis. Biopsy may or may not be used in the diagnostic process. Gynecological Cancer treatment in Ahmedabad Treatment is also based on the extent of the cancer's spread and the type of cancer present.
Treatment is usually a combination of surgery, chemotherapy, and may or may not use radiotherapy. Surgery involves removing cancer cells from the affected area. Chemotherapy is the use of drugs to stop or control the growth of cancer cells in the affected area. The drugs are administered into the body either in the form of tablets, or intravenously, or through IV injection. Radiotherapy involves the use of high-energy radiation beams to kill cancer cells or stop them from spreading further. Gynecological cancer in Ahmedabad, Gujarat that impair fertility have been successfully treated. Ovarian choriocarcinoma that was in stage IV has been successfully treated by reducing fertility using a combination of surgery and chemotherapy. Services and treatments patients can expect from cancer hospitals for gynecological cancer include: Diagnostic services such as hysteroscopy, biopsy, laparoscopy, colposcopy, and so forth, Ultra-radical and radical surgeries such as Wertheim hysterectomy, radical vaginal-abdominal surgery to treat cervical cancer and Japanese radical surgery for cancer in stage II B. Para-aortic and pelvic lymphadenectomy are also performed as part of the procedure.
Dr. Nitin Singhal is the World’s No.1 Gynecological Cancer Doctor, Surgeon in Ahmedabad, Gujarat. For More Information Visit Us : https://www.drnitinsinghal.com
#gynecological cancer#best cancer surgeon in ahmedabad#best cancer surgeon in gujarat#onco surgeon in ahmedabad#cancer doctor in ahmedabad#cancer doctor#Gynecological Cancer In Ahmedabad
0 notes
Photo
Can you answer today’s question 🙋♀️?! Q: What’s the most common site of metastasis of choriocarcinoma?! 🤔…#medicine #obgyn #neet #pathology #nclex #usmle #doctor #cancer https://www.instagram.com/p/CiDJn2eOYg6/?igshid=NGJjMDIxMWI=
0 notes
Text
Basic safety and also Performance involving Ixazomib Dose-escalating Strategy inside Ixazomib-Afatinib-Dexamethasone Strategy for Relapsed/Refractory Several Myeloma
Approaches. Tissues as well as sera have been gathered through females going through treatment for GTD inside a tertiary proper care school clinic. We all examined partial and handle hydatidiform most individuals, invasive most individuals along with choriocarcinoma, d Is equal to 07. Trophoblast individuals ended up looked at by a fresh designed IHC set-up with regard to hGH-V together with gross morphologic and also histopathological evaluation. Serum trials had been assessed by way of a very hypersensitive hGH-V distinct immunoassay. Results. hGH-V was local in most agencies of GTD on the syncytiotrophoblast through immunohistochemistry. Serum hGH-V ended up being recognized the first time inside GTD and it was contained in a top number of almost all analyzed agencies. Results. hGH-V might be found in all of the organizations associated with GTD simply by IHC in addition to through serum analysis and may even for that reason be the story biomarker to the ailment. Its scientific electricity throughout carried out GTD along with keeping track of surgical or hospital treatment needs to be identified inside even more research. (Chemical) This year Elsevier Inc. Just about all rights set aside.History. Sunitinib is really a multitargeted tyrosine kinase inhibitor utilized in the management of metastatic renal cellular carcinoma (RCC) and also intestinal stromal growth (Idea), along with going through assessment with regard to other malignancy. Blood pressure is just one of it's significant negative effects using a significant alternative from the noted frequency amid clinical tests. Many of us the following performed a deliberate evaluation and also meta-analysis associated with printed many studies to find out it's overall risk. Approaches. Related research ended up looked along with determined throughout MEDLINE (OVID 1966 for you to July, 3 years ago), Web regarding Technology, and abstracts presented with the American Community of #Link# Medical Oncology annual conferences via 2004 through '07. Entitled studies were possible many studies that have defined era of high blood pressure levels for individuals that obtained one agent sunitinib. The incidence regarding high blood pressure and also comparative #Link# threat (RR) were determined while using random-effects or even the fixed-effects product. Results. A total of 4, 999 individuals using RCC as well as other malignancies via 12 clinical trials have been incorporated pertaining to investigation. Amid individuals acquiring sunitinib, the particular occurrence of all-grade as well as high-grade hypertensions have been 21.6% (95% CI: Eighteen.7-24.8%) and also 6.8% (95% CI: Five.3-8.8%) respectively. The danger can vary using cancer sort as well as the dosing timetable of sunitinib. Sunitinib was associated with a substantially increased likelihood of high-grade high blood pressure (Three quarter's Is equal to 22.Seventy two, 95% CI: Four.Twenty four for you to 115.29, s < 3.001) and also kidney problems (Three quarter: One particular.Thirty five, 95% CI: A single.Something like 20 to a single.54, r < 0.001) in comparison to settings. Conclusions. You will find there's important probability of establishing blood pressure and renal problems #Link# amid individuals getting sunitinib. Enough checking and also treatment of high blood pressure levels is mandatory.
0 notes
Text
Comprehensive Guide to Choriocarcinoma Treatment: Dr. Chandrakanta Sulaniya
Introduction:
Welcome to Dr. Chandrakanta’s Gynae-Oncology Center, your premier destination for advanced care in gynecologic cancers, including choriocarcinoma. Led by Dr. Chandrakanta, a renowned Gynae Oncologist in Jaipur, our center is dedicated to providing compassionate, personalized care to patients battling gynecologic malignancies. In this blog post, we will delve into the intricacies of choriocarcinoma treatment, exploring its causes, available options, and the hope that accompanies modern advancements in oncology.
Understanding Choriocarcinoma:
Choriocarcinoma is a rare but aggressive form of cancer that develops from trophoblastic cells, which are responsible for forming the placenta during pregnancy. While choriocarcinoma most commonly occurs in the uterus following a molar pregnancy (an abnormal pregnancy characterized by a nonviable fertilized egg), it can also arise from normal pregnancies, ectopic pregnancies, or even without a preceding pregnancy. This makes it crucial for women of childbearing age to remain vigilant about their reproductive health and seek prompt medical attention if they experience concerning symptoms.
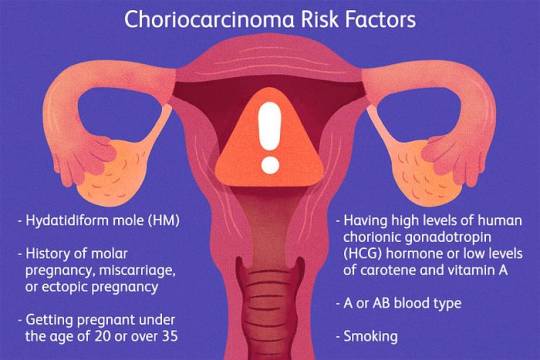
Causes of Choriocarcinoma:
The exact causes of choriocarcinoma remain elusive, but several risk factors have been identified, including:
1. Molar Pregnancy: Choriocarcinoma often arises following a molar pregnancy, wherein abnormal growth of placental tissue occurs instead of a viable fetus.
2. Previous Gestational Trophoblastic Disease (GTD): Women with a history of GTD, which includes molar pregnancies, are at increased risk of developing choriocarcinoma.
3. Age: Choriocarcinoma primarily affects women of reproductive age, with peak incidence occurring between the ages of 20 and 40.
4. Ethnicity: Certain ethnic groups, such as women of Asian descent, have a higher prevalence of choriocarcinoma.
Treatment Options for Choriocarcinoma:
Choriocarcinoma treatment typically involves a multidisciplinary approach tailored to each patient’s unique circumstances. The primary goals of treatment are to eradicate the cancer, preserve fertility when possible, and minimize the risk of recurrence. Treatment modalities may include:
1. Chemotherapy: Chemotherapy is the cornerstone of choriocarcinoma treatment and is highly effective in killing cancer cells. Various chemotherapy regimens, such as EMA-CO (etoposide, methotrexate, actinomycin D, cyclophosphamide, and vincristine), are used either alone or in combination depending on the stage and severity of the disease.
2. Surgery: In cases where the tumor is confined to the uterus or has spread locally, surgical intervention may be recommended. This may involve a hysterectomy (removal of the uterus) or more conservative surgeries aimed at preserving fertility for women desiring future pregnancies.
3. Radiation Therapy: Radiation therapy may be used in conjunction with chemotherapy to target and destroy cancer cells, particularly in cases where the disease has spread to other organs or tissues.
4. Follow-up Care: After completing primary treatment, close monitoring and surveillance are essential to detect any signs of recurrence early. This typically involves regular imaging studies, blood tests, and clinical examinations.
Hope and Support:
While a diagnosis of choriocarcinoma can be overwhelming, it’s important for patients to remember that they are not alone in their journey. At Dr. Chandrakanta’s Gynae-Oncology Center, we offer comprehensive support services, including counseling, nutritional guidance, and access to support groups, to help patients navigate through diagnosis, treatment, and survivorship.
Conclusion:
Choriocarcinoma is a rare but treatable gynecologic cancer that requires prompt diagnosis and aggressive treatment. With advancements in medical science and a multidisciplinary approach to care, patients can find hope in the journey towards remission and recovery. If you or a loved one are facing choriocarcinoma, don’t hesitate to reach out to Dr. Chandrakanta’s Gynae-Oncology Center for expert care and compassionate support. Your journey to healing starts here.
#choriocarcinomatreatment in jaipur#dr chandrakanta gynae oncology in jaipur#cervical cancer treatment in jaipur#gynae oncologist in jaipur#endometrial cancer treatment in jaipur#gynae cancer doctor in jaipur#gynaecological cancer in jaipur#gynaecological surgeries in jaipur#gynaecological oncologist near me
0 notes
Text
Persistent Embryo-Larval Direct exposure involving Fathead Minnows for the Pharmaceutical Drug Osimertinib: Survival, Expansion, and Microbiome Responses
Findings from our examine established that triple-phase CT is often a great tool regarding preoperative distinction of hepatocellular carcinoma, nodular hyperplasia, and also hepatic metastatic cancers in dogs. (Chemical) 2013 American University of Vet Radiology.The actual cytotoxicity regarding 8 perfluorinated chemicals (PFCs), namely, perfluorobutanoic acid (PFBA), perfluorohexanoic acidity (PFHxA), perfluorooctanoic acid solution (PFOA), perfluorononanoic acid solution (PFNA), perfluorododecanoic chemical p (PFDoA), perfluorobutanesulfonate (PFBS), perfluorohexanesulfonate (PFHxS) as well as perfluorooctanesulfonate (PFOS) ended up being examined from the man placental choriocarcinoma mobile line JEG-3. Only the prolonged string PFCs -- PFOS, PFDoA, PFNA, PFOA -- confirmed important cytotoxicity in JEG-3 tissue with EC50 valuations inside the selection of 107 for you to 647 mu Mirielle. The particular witnessed cytotoxicity would have been to some amount linked to a better uptake from the longer chain #Link# PFCs simply by cells (PFDoA bigger when compared with PFOS bigger when compared with bigger compared to PFNA bigger than PFOA bigger than PFHxA). Furthermore, the project evidences a top potential of PFOS, PFOA and also PFBS to do something because aromatase inhibitors in placental cellular material with 1C5Os in the variety of 57-80 mu Mirielle, your inhibitory effect of PFBS being particularly important regardless of the rather lower subscriber base from the chemical substance by simply tissues. Last but not least, coverage regarding JEG-3 cellular material with a mix of the actual ten PFCs (2.Some mu Mirielle every) resulted in a family member enhance (around 3.4-fold) of varied lipid classes, which includes phosphatidylcholines (Computers #Link# ), plasmalogen PC as well as lyso plasmalogen PC, this means a great disturbance of PFCs with membrane lipids. Overall, this work shows ale the PFC blend to alter cellular fat routine in concentrations properly down below people who generate toxicity, and the probable from the quick chain PFBS, typically deemed a safe and secure exchange regarding PFOS, to be able to substantially inhibit aromatase action in placental tissue. (c) This year Elsevier Incorporated. Just about all legal rights earmarked.Bevacizumab is often a recombinant humanized monoclonal antibody that will precisely hindrances the adventure regarding vascular endothelial growth aspect (VEGF) receptor which is found in metastatic digestive tract people. All of us existing the following a case of lethal necrotizing fasciitis in the patient through bevacizumab strategy for digestive tract cancer malignancy. Within our review of the materials, necrotizing fasciitis has not been noted ahead of or perhaps throughout bevacizumab treatment method.Amphiphilic dextran-b-poly(epsilon-caprolactone) diblock copolymers were synthesized using the purpose of organizing nanocarriers with regard to doxorubicin (DOX), the anticancer substance. Your Dex-b-PCL diblock copolymers have been created simply by end-to-end direction regarding amino-terminated dextran and also aldehyde-terminated poly(epsilon-caprolactone) and also seen as a H-1 NMR spectra along with teeth whitening gel permeation chromatography. The particular DOX-loaded Dex-b-PCL nanoparticles were cooked by an improved nanoprecipitation method and seen as transmission electron microscopy along with powerful lighting scattering. Throughout vitro discharge of DOX via DOX-Dex-b-PCL nanoparticles revealed any #Link# continual discharge manner with certain quantity regarding broke launch within the very first Nine h. Throughout vitro cytotoxicity analyze of DOX-Dex-b-PCL nanoparticles versus SH-SY5Y tissue demonstrated that DOX is still pharmacologically productive following drug launching.
1 note
·
View note
Text
A “new normal?” I don’t think so...(?)
•••••••••••••••••••••••••••••••••••••••••••••••
I remember the day like the back of my hand. I had just been admitted to the Johns Hopkins hospital, hooked up to oxygen and IV fluids. I was meeting with my new team of oncology doctors.
They went over my plan of treatment and what to expect. Naturally, as many would also probably respond as, I blacked out. I’m sure it was the lack of oxygen and the mix of pain killers, but I honestly don’t remember any of it. The room went dark, I could hear them— feel their pressence, but my mind had basically burst into a million pieces. So much information given to me in...in what, maybe 30 minutes, tops?
Chemo was a drag, as most would expect. I handled it well, quite honestly. I got sick maybe once or twice my first round, but it was smooth sailing the rest of the way. Fatigue and the emotional sobbing was my biggest problem. It would come out of nowhere. I became sensitive to everything. The sun, the moon, and the stars would pop out and I’d be sobbing. I’d watch my 600lb life... and sob. I’d sit down for morning coffee, and sob. I didn’t fight the tears anymore.
Chemo does weird things to your body and your mind— you’re literally morphing into this lifeless, non-recognizable body. My hair fell out everywhere. My beard fell out. Christmas Day I was in the shower and globs of hairs were just falling out. A few days later I said fuck it, took my clippers, and pulled a 2007 Brittney Spears.
I began to look like my pubescent 11 year old self. It was weird. Just totally taboo.
I was facing a huge challenge now. This really hadn’t hit me yet.
But in all honesty, it wasn’t until my eyelashes, my eyebrows, and the hairs on my legs and arms began to fall out. It wasn’t really until I began to puff up like a fish from all the steroids; and gain the “Freshman 15” that I never did in college. That’s when it really hit me.
•••••••••••••••••••••••••••••••••••••••••••••••
“Holy shit, I have cancer.”
•••••••••••••••••••••••••••••••••••••••••••••••
This “new normal” mentality was brought up so many times to me by so many people in the last year that I have learned to just ignore it...or at least try to.
Uh...Yeah, of course my life is going to change. I was just diagnosed with late stage metastatic ball cancer. I’m 24 fuckin years old, are you kidding me?
I was pissed, so mad at the world. What did I do to deserve this? Everything was finally falling into place for me. My career was taking off, I began to work on my masters degree. I was eating healthy and taking numbers. I had what I wanted. I had security.
I might have struggled financially, but I had begun to get my life together one step at a time.
•••••••••••••••••••••••••••••••••••••••••••••••
I tried and tried to get back to my old self after finishing chemo, going through all these surgeries and getting back to my daily work life and weekend fun.
I was fighting this “new normal” mentality.
•••••••••••••••••••••••••••••••••••••••••••••••
As of recently, I think I’m starting to get what they meant.
I was doing so well, health related. Tumor markers were returning to a normal range, lung mets were still shrinking. I wasn’t worried.
But as I look back from the last few months, I see it now. Something was wrong. My mood fluctuated, my emotions were all over the place. I emailed my urologist to ask for bloodwork for T levels. My hormones went through quite a bit over the last few months— a lot of hormonal changes. T levels came back normal. I started working out again, getting my ass into shape at kickboxing. (What a great stress relief, by the way. I highly recommend.)
•••••••••••••••••••••••••••••••••••••••••••••••
I mean, yeah, I knew I was sorta depressed, but I was back to at least a little bit of what we say ~thriving~ nowadays.
“Living my best life.”
Or so I thought I was...
But then I began to run myself into the ground. I started drinking a lot, being reckless, putting my roommate and my friends through hell. There would be times she would come home and I’d be passed out on the floor from having too much bubbly by myself on a Sunday morning. It wasn’t healthy— for me or for her. I had to get my shit together or I was out. Never did either of us even imagine I’d be struck with cancer. The tension was high. We both knew it, but, at least for myself, I’m not afraid to say I like to avoid conflict.
I was self medicating because thats what seemed what was best for me. In reality, I was self-destructing. And a steady decline I was taking.
•••••••••••••••••••••••••••••••••••••••••••••••
For the last couple days I’ve had a lot of time to think. (Maybe too much time, to be honest.)
I guess what I’m trying to say is.. I can sorta admit that I’m learning to accept these changes— this “new normal” mentality. I didn’t want to at first, but I think it’s ok. Instead of fighting to try to find the old me, maybe this “new normal” is a change that I needed.
A life style change? A new outlook? A restart button? Shut down, and reload.
•••••••••••••••••••••••••••••••••••••••••••••••
Two and a half weeks ago, I had a brain tumor removed. Yeah, the cancer came back. Six months post chemo, six months post surgeries, six months getting back to work, getting healthy— a brain tumor. Surgery went well. They got it all out and I’ll meet with oncology next week for further details and a plan of more treatment if need be. (I’ll be sure to update.)

•••••••••••••••••••••••••••••••••••••••••••••••
What...What I’m trying to say is that this brain tumor and this brain surgery and all that has opened my eyes even more to the “new normal.” The depression seems to have subsided, although I’m not afraid to admit I’m on antidepressants and anti-anxiety meds and sometimes I feel like maybe we all should just be on them. I truly feel happier. Everyone wants to be happy— and I can honestly say that I’m getting there. I’m working on it. I have my days. We all do. So I don’t let it bother me.
It’s made me wonder— this latest occurance— to think of it as a learning experience. Some higher power put me in this situation to really challenge me...again. And I’m succeeding.
I refuse to lose. I never was a loser. My competitve side really comes out sometimes, catching people off guard. I’m usually the sarcastic wise-ass in the corner cracking jokes.
•••••••••••••••••••••••••••••••••••••••••••••••
I need to start setting life goals. I want to travel more, I want to experience life like there’s no tomorrow. It’s easier said than done, I know, but it’s turning in a necessity now for me. Tomorrow is not promised. As cliches as it sounds, I want to carpe dium.
And that’s my plan. Carpe the shit out of that dium.
•••••••••••••••••••••••••••••••••••••••••••••••
Enjoy your day, my lovely friends ❤️
4 notes
·
View notes