#hemimegalencephaly
Text
Happy disability pride month to people with brain malformations btw.
#I have a chairi malformation#no one ever talks abt us#disability pride month#ACC#septo-optic dysplasia#Holoprosencephaly#Lissencephaly#chiari malformation#schizencephaly#hemimegalencephaly#Rhomboencephalosynapsis#cripple punk
133 notes
·
View notes
Text
My friend's brand new baby girl, Vianney, who was born on Sept 1st, has been in the NICU since Thursday (Sept 14th) and has just been diagnosed with hemimegalencephaly. It's a rare, non-hereditary genetic mutation that caused a malformation of one side of her brain, causing seizures. She'll have to stay in the hospital for several more weeks while they try to get her seizures to slow down. She needs brain surgery but has to make it to 6 months before she can have it. Unless a miracle happens, she will need special care her whole life.
I work for the Little Sisters of the Poor and one of the sisters has suggested we start a novena asking for the intercession of the newly beatified Ulma Family, particularly asking for the special intercession of their unborn baby that was beatified with them, for a complete healing of Vianney.
I would greatly appreciate it if you could spread the word to everyone you know, asking them to help pray for a miracle for little Vianney and her family.
Parents are Jennifer & Shad, and Vianney has two older sisters, Cecilia & Zelie.
Prayer for the Intercession of the Ulma Family
Almighty and eternal God,
we thank You for the testimony of the heroic love of the spouses Józef and Wiktoria with their children, who gave their lives to save persecuted Jews.
May their prayers and example support families in Christian life and help everyone to follow the true path of holiness.
Lord, if it is in accordance with Your will, kindly grant the grace for the complete healing of little Vianney, for which we are asking You through their intercession and count them among the Blessed.
Through Christ Our Lord
Amen
Our Father..., Hail Mary..., Glory Be...

#prayers#prayer#prayer request#prayer requests#ulma family#catholic#catholic church#saints#tumblr catholic#tumblr catholics#christian#novena#novenas#miracle needed#catholic prayer#catholic prayers
211 notes
·
View notes
Text
**Epilepsy and the Role of Hemispherectomy**
Epilepsy is a chronic neurological disorder characterized by recurrent seizures, which are sudden bursts of electrical activity in the brain. While epilepsy can affect people of all ages, it is most common in children and young adults. In some cases, epilepsy can be effectively managed with medication, but for others, the seizures may be too severe or unresponsive to medication. For these individuals, surgery may be an option to control seizures.
One type of surgery that is sometimes used to treat severe epilepsy is a hemispherectomy. A hemispherectomy is a radical procedure that involves removing or disconnecting half of the brain. This is a major surgery, but it can be very effective in controlling seizures in carefully selected patients.
**Who is a candidate for a hemispherectomy?**
A hemispherectomy is typically considered for children who have severe epilepsy that is affecting only one hemisphere of the brain. The seizures may be severe enough to cause developmental delays, learning difficulties, and other disabilities.
Some of the conditions that may lead to a hemispherectomy include:
* **Hemimegalencephaly:** This is a rare condition in which one hemisphere of the brain is significantly larger than the other.
* **Sturge-Weber syndrome:** This is a syndrome that causes seizures, skin lesions, and eye problems.
* **Rasmussen's encephalitis:** This is a rare autoimmune disease that attacks the brain.
**How does a hemispherectomy work?**
The specific procedure of a hemispherectomy will vary depending on the patient's individual needs. However, the general steps are as follows:
* The surgeon will make an incision in the scalp and remove a piece of bone from the skull.
* The surgeon will then carefully remove or disconnect the diseased hemisphere of the brain.
* The surgeon will close the incision and the patient will be taken to the recovery room.
**What are the risks of a hemispherectomy?**
As with any major surgery, there are risks associated with a hemispherectomy. These risks include:
* Infection
* Bleeding
* Blood clots
* Damage to healthy brain tissue
* Learning difficulties
* Speech and language problems
* Motor problems
**What is the outcome of a hemispherectomy?**
The outcome of a hemispherectomy can vary depending on the patient's individual circumstances. However, in general, a hemispherectomy can be very effective in controlling seizures. Studies have shown that up to 80% of patients who undergo a hemispherectomy will experience complete seizure freedom.
**What is life after a hemispherectomy like?**
Patients who undergo a hemispherectomy will need to undergo rehabilitation to learn to cope with any new challenges they may face. This may include physiotherapy, speech therapy, and occupational therapy.
Despite the challenges, most patients who undergo a hemispherectomy go on to live fulfilling lives. They may experience some learning difficulties or motor problems, but they can still attend school, work, and participate in activities that they enjoy.
**Conclusion**
Epilepsy is a complex disorder that can have a significant impact on people's lives. While there is no cure, there are effective treatments available, including medication and surgery. A hemispherectomy is a major decision, but it can be a life-changing procedure for those with severe epilepsy.
My experience with:
In June 21st, 2018; I had my last seizure(day of my surgery). So after my surgery to this day I've yet to have a seizure(Nov 8 2023). Except, as previously stated; there can be some"after effects". To put it shortly I was left with "stroke-like side effects"meaning that I do have reduced motor abilities or low ROM (range of motion) sight problems and strength loss. Luckily, I do have more confidence, liberty, "authority" and responsibilities.
Disclaimer: for everyone's unique case it might be different because I have Rasmussen's encephalitis
#epilepsy#seizures#neuro#brain#neurology#seizure#after effects#hemispherectomy#storytime#cause#effect
2 notes
·
View notes
Text
Children's charity and Poundbakery give festive cheer to 12-year-old Olivia from Altrincham
Children’s charity Brainwave and Poundbakery, located on School Road in Sale, have joined forces this festive season to bring joy to 12-year-old Olivia (Liv) and her family by presenting them with a delightful hamper, filled with an assortment of her favourite bakery treats.
Liv was born with a rare brain condition called Hemimegalencephaly and a subsequent operation left her with hemiplegic…

View On WordPress
0 notes
Text
5 Unique Surgical Procedures - Weird or Wonderful?

Since the first human heart transplant in 1967, there are thousands of surgical procedures evolved, transforming people's lives every day.
Apart from those, we take a look at five of the most bizarre surgical procedures.
1) Ankle to knee Surgery
Rotationplasty is an extraordinary reconstructive surgery, where the ankle is used as a knee joint.
In this procedure, the bottom of the femur, the knee, and the upper tibia are surgically removed, and the lower part of the leg is then rotated 180 degrees and attached to the thigh.
In simple terms, the foot is attached to the knee backward.
After fitting the prosthesis, the ankle of the foot functions as a knee.
2) Tooth-in-eye surgery
Osteo-odonto-keratoprosthesis is just using the tooth to restore the sight of a patient.
OOKP is used for patients whose blindness is caused by irreversible damage to the cornea and for whom other treatment methods have failed. The patient's tooth is used as the body is unlikely to reject it.
The patient's canine or premolar tooth, and the surrounding bone is removed for the technique. Firstly, a hole is drilled in the tooth, and a plastic lens is inserted in the hole. To grow new blood vessels, the lens-tooth structure is implanted into the patient's cheek for a few months.
Finally, the structure is removed from the cheek and implanted into the eye. Light travels through the lens, thereby restoring the patient's vision.
3) Removing half of the brain
Hemispherectomy is the partial or total removal or disconnection of one of the two hemispheres of the brain. It seems beyond impossible that removing half of the brain can be a feasible, effective surgical solution for certain neurological conditions, but yes, in some cases, it is.
Hemispherectomy is considered a radical procedure, which can take as long as 12 hours to complete. It is usually performed on patients with neurological disorders that lead to seizures on one side of the brain.
Those neurological disorders include severe epilepsy, perinatal stroke, hemimegalencephaly, Sturge-Weber-Dimitri disease, and Rasmussen's encephalitis (inflammation of the cerebral cortex).
Patients who are undergoing hemispherectomy experience paralysis on the side of their body, opposite to their removed hemisphere. As the benefits of the surgery outweigh the risks and side effects, the procedure is opted in certain conditions.
4) Heterotopic heart transplant
The procedure is also known as "piggyback" heart transplantation. The surgical implantation of a healthy donor heart on the right side of the recipient's damaged heart where both the hearts are surgically attached is known as a heterotopic heart transplant.
The surgical connection between both hearts allows blood from the damaged heart to flow into the new heart, then the new heart can pumps blood around the body.
5) Head transplant
The procedure is named as HEAVEN-GEMINI will involve removing the heads of the recipient and a healthy donor using an "ultra-sharp blade," to avoid spinal cord damage.
The recipient's head and the donor body are placed into deep hypothermia for about 45 mins to reduce nerve damage. The recipient's head will then be attached to the donor body using spinal cord fusion.
The entire surgical procedure is expected to take around 36 hours, and it will require the skills of about 150 surgeons and nurses.
Later, the recipient is kept in a coma for 3-4 weeks to minimize movement and ensure the nerve connections between the neck and the spine have time to fuse.
0 notes
Text
Hypomelanosis of Ito with Partial Motor Seizure and Hemimegaloencephaly: Case Report

Authored by Amal Y. Kentab*
Abstract
The term hypomelanosis of Ito [HI] is applied to individuals with skin hypopigmentation along the lines of Blaschko. Even though originally described as a purely cutaneous disease, subsequent reports have included a 33% to 94% association with multiple extracutaneous manifestations mostly of the central nervous and musculoskeletal systems leading to frequent characterization as a neurocutaneous disorder. A boy with constellation of multiple congenital anomalies including facial dysmorphism, skin hypopigmentation, musculoskeletal, and nervous system abnormalities in the form of hypotonia and mild mental retardation suggestive of [HI] presented with partial motor seizures and found to have hemimegalencephaly [HME] on MRI of the brain.
Keywords: Hypomelanosis ito (HI); Cortical dysplasia; Neurocutaneous syndrome; Cerebral malformation.
Go to
Introduction
Hypomelanosis of I to [HI] or Incontinentia pigmenti achromians [OMIM no. 146150]. Ito first introduced the syndrome 1951 [1]. It is a rare neurocutaneous syndrome that involves mainly skin and nervous system symptoms in 75 % of cases and may be associated with multiple organ systems involvement including the head and face, eyes (microphthalmia, cataracts, optic atrophy, and retinal detachment), teeth, cleft lip and palate, heart (tetralogy of Fallot), kidneys, musculoskeletal (hemihypertrophy), and reproductive systems (precocious puberty) [2-4]. The incidence and prevalence of [HI] has been reported to be1/7540 births and 1/82,000 individuals, respectively [4]. McKusick`s catalogue of inherited diseases lists HI as an autosomal dominant disorder, although evidence for this mode of inheritance, or indeed for any genetic etiology, is inconclusive [2]. Frequency is equal among males and females. It is caused by Nonheritable mutation, and it have been reported frequently in association of various chromosomal abnormalities, including mosaicism for aneuploidy or unblanaced translocations, mosaic trisomy 18, ring chromosome 22, and translocations involving the X chromosome. There is no clear genotype - phenotype correlation [2]. Only a few cases of HI have been reported with partial motor seizures in association with hemimegalencephaly [HME]. In order to highlight on this rare neurocutaneous disorder, this report describes such association in a 10 year old boy with skin hypopigmentation, craniofacial and musculosketetal abnormalities.
Go to
Case Report
A 10 -year-old male, left handed, 6th grade student was evaluated in our tertiary care neurology clinic for afebrile complex partial motor seizure with 2nd generalization, started one month prior to presentation. He had frequent episodes of sudden left-sided eye deviation and facial twitching with secondary left-sided unilateral and generalized tonic-clonic seizures. Each episodes last for less than 3 minutes, preceded by dizziness, pain in the right eye with blurred vision and headache, end spontaneously after an episode of vomiting , headache , and postictal sleep without loss of sphincter control . Seizures were controlled with levetiracetam (Keppra). He was a product uneventful pregnancy delivered by spontaneous vaginal delivery at 36 weeks gestational age, readmitted on 2nd day, and operated for intestinal intussusception. Past history included a slower cognitive and language development in comparison to other siblings, skin hypopigmentation noted at 6 months of age, bronchial asthma, abnormal dentation with frequent dental caries, and tonsillectoy-adenectomy operation for frequent tonsillitis.
His parents were consanguineous and there was a history of seizure disorder in two sons of paternal uncle from twin pregnancy. Microophthalmia in two sisters of paternal ante. Reported multiple infantile deaths of both parental, and maternal side with obscured reasons. His mother had cafe`-au lit spot and hypopigmentation on her thighs. On examination, he had macrocephaly, short stature, dysmorphic features in the form of high prominent forehead, low set and posteriorly rotated prominent ears, orbital hypertelorism, epicanthal fold, depressed nasal bridge, anteverted nostrils, high arched palate, tooth spacing with abnormality in size and shape, micrognathia, broad fingers with archanodactyly, mild clinodatyly of 5th finger, broad nails, a gap between big toe and the second one, syndactly between the 2nd and the 3rd toes on the right foot, mild scoliosis (deviation to the left) with prominent lordosis, joint hyperlaxity and bilateral pes plans , with mild hemi hypertrophy of the right side of the body , involving mainly the face and upper extremity.
Hypopigmented areas (whorl-like and streaks) noted on the anterior and the lateral aspects of both legs extending to involve the left shine anteriorly and another similar one but with small size seen at the right shoulder (Figure 1). His neurological examination revealed poor short-term memory and cognitive delay, especially in terms of general knowledge, the ability to read and mathematical concepts and mild right hemiparesis. His initial basic laboratory work-up was normal apart from mild anemia, and low vitamin D 62 nmol/l (NR 75-120). Full metabolic screen thyroid function test, full chromosomal analysis, microarray CGH showed and Cardiac evaluation by electrocardiogram (ECG), echocardiogram (Echo) and Abdominal ultrasound were unrevealing. Ophthalmological evaluation showed mild sclerocornea, pigmented iris, and bilateral flat retinal astrocytoma with retinal pigmentary changes. Skeletal survey revealed mild osteoporosis and mildscoliosis.
Electroencephalogram (EEG) showed background asymmetry with slow theta wave activity noted on the left hemisphere with occasional sharp waves seen predominately on the left hemisphere. Computed tomographic (CT) scan of the brain showed no space occupying lesion, but left hemimegaloencephaly with dilated left ventricle. Magnetic resonance imaging scan of the brain (MRI) revealed similar findings with small arachnoid cyst at left middle fossa with no evidence of neuronal migration disorders or cortical dysplasia (Figure 2). Magnetic resonance angiography (MRA) was normal with no evidence of vessel stenosis or picture similar to moyamoya disease.
Go to
Discussion
The cutaneous features of HI include multiple hypopigmented streaks or patches that found in 100% of affected individuals and are either present at birth or emerge in infancy. These lesions follow Blaschko lines (skin lines that form specific patterns over the trunk and extremities, such as a V shape over the back and linear lines over the limbs and are best detected under ultraviolet light in light - skinned children. In contrary to incontinentiapigmenti, these lesions, are not preceded by inflammatory or degenerative changes. (Table 1) The extent of the skin lesions do not correlate strongly with neurologic involvement. An important differential diagnosis is Tuberus Sclerosis Complex, where the hypopigmented patch (ash leave spot which is usually oval in shape with regular border) appears during the 1st year of life mainly on trunk or extremities, and as the child approaching puberty other skin manifestations appear like adenoma sebaceum, on the face, shagreen patch on the back and periungual fibroma [3,4].
(Table 1) Neurologic manifestations include intellectual impairment with mild to severe mental deficiency (IQ<70) that is usually seen in 57% while only 20% of patients have an IQ above 85% with reported poor school performance in (40-60%). Seizures that include generalized tonic or tonic-clonic, complex partial, myoclonic seizures or infantile spasm with onset early in the first year of life, with variable response to anticonvulsant drugs . Behavior disorders that include autism, Asperger`s syndrome, self-injurious behavior and severe sleep problems especially in the first 3-5 years of age [3,4]. Macrocephaly or microcephaly may be seen, with the former being more common. Other associated findings include, a non-progressive speech delay, muscular hypotonia or hypertonia, hyperkinesias, nystagmus, ataxia, and neurosensory deafness. MRI in more than half of patients may show either cerebral or cerebellar hypoplasia and various other malformations of cortical development including hemimegalencephaly, lissencephaly, pachygyria, and heterotopia. White matter abnormalities of either cystic like lesions or delayed myelination. Other brain abnormalities include, focal or generalized brain atrophy, basal ganglia lesion, or intracranial vascular abnormalities such as A-V malformation, Moyamoya disease, leptomeningeal angioma [2]. The patient in this report had clinical picture suggestive of HI (skin hypopigmentation, facial dysmorphism, eye and dental abnormalities, joint hypermobility, skeletal abnormalities ie. short stature, scoliosis, osteoporosis, mild learning disability, partial motor seizures), mild right hemiparesis and HME with no other associated neuronal migration disorder on brain MRI which has been previously reported [5-9].
Hemimegalencephaly is a major, but rare congenital hamartomatous malformation of the brain [10], characterized by enlargement of all or parts of a cerebral hemisphere and frequently associated with cortical focal or diffuse neuronal migration defects, such as polymicrogyria, pachygyria, or heterotopias. HEM affects all ethnic groups and both genders equally.
Its etiology remains unknown. It has been suggested that it results from some type of acquired unilateral hemispheric insult in the mid to late second trimester of pregnancy [11] that affect the genetically programmed process that establishes symmetry as well as the development of neuroepithelial lineage and cellular growth occurring at an earlier stage of neuroblast migration [12]. It does not follow a Mendelian pattern of inheritance and usually occurs sporadically. It is widely believed that a single or multiple gene mutations contribute to this process.
It typically presents with a triad of intractable epilepsy, psychomotor delay and hemiparesis. Some patients show entire brain asymmetry, hemifacial hypertrophy, or hemicorporal hypertrophy. Other associated features may include macrocephaly with cranial asymmetry, and behavioral disabilities. Epilepsy is usually of early onset and intractable. Those with later-onset epilepsy are more likely to have mild motor deficit like the patient in this report, or normal motor function. The EEG is abnormal in all cases of HME. In the neonatal period, suppression burst pattern, followed by hypsarrhythmia and later, focal seizure activity may be seen. Functional or anatomical hemispherectomyis recommended for early - onset pharmacoresistant epilepsy as improvement of either the motor function level or intellectual development was seen in most patients post-surgery [13,14].
It is often an isolated disorder, but may be syndromic associated with several diseases or neurocutaneous syndromes, such as epidermal nevus syndrome, tuberous sclerosis complex (TSC), linear sebaceous nevus syndrome, Klippel - Trenaunay syndrome (KTS), Proteus syndrome (PS), hypomelanosis of ito (HI), neurofibromatosis , Sotos syndrome and Alexander [10,15]. It is worthy to mentioned that usually there is no differences in clinical symptoms in regards to the laterality (Right or left) or the type (isolated or syndromic) of hemimegalencephaly [16].
MR Imaging is the investigation of choice for diagnosis, though ultrasound and CT will show the abnormalities. As in our patient, increased size and altered shape of the ventricle is usual. The cortex is broader (dysplastic) than normal, neuroblast migratory anomalies are frequently seen, the most common being heterotopias. [11], as well as white-matter abnormalities (high signal intensity in T2W image) [17]. Since the disease does not follow a Mendelian pattern of inheritance, chances of recurrence are rare and there is usually no family history of other affected individuals. Prenatal diagnosis may be suspected on the basis of fetal ultrasound [18] or MRI (diffusion - weighted images) [19].
Go to
Conclusion
Combination of a triad of intractable epilepsy, psychomotor delay and hemiparesis in the presence of macrocephaly and / or skin hypopigmentation should prompt consideration of HEM . MRI is the imaging of choice for diagnosis of HEM. HEM should prompt a search for other syndromic diagnosis such as HI.
Go to
Acknowledgment
This work was supported by the College of Medicine Research Center, Deanship of Scientific Research, King Saud University.
For more open access journals in juniper publishers please click https://juniperpublishers.com/
For more articles on Open Access Journal of Neurology & Neurosurgery Please click on https://juniperpublishers.com/oajnn/
Open Access Journal of Neurology & Neurosurgery in Full text in Juniper Publishers
https://juniperpublishers.com/oajnn/OAJNN.MS.ID.555585.php
#Juniper Publishers#Juniper Publishers in USA#Juniper Publishers reviews#Juniper Publishers Peer review journals
0 notes
Text

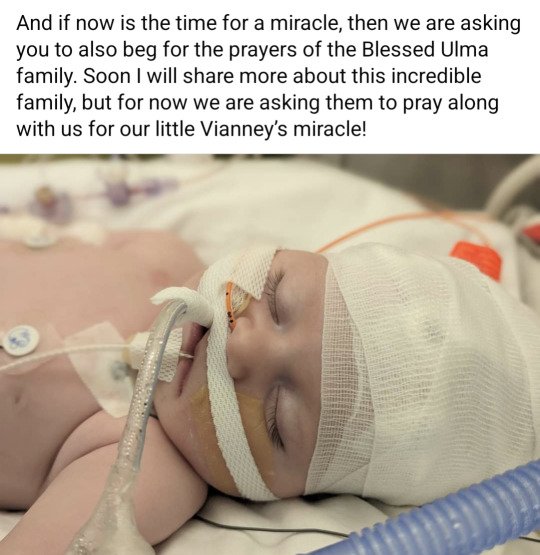
[Image Text:
Please, please, please, if you even so much as glance at this post - share it for us and help us storm heaven!!! Our little girl needs a miracle and I beg any and every one of you to pray, pray, pray! Even if you don't know how to pray, please just ask God to heal Vianney’s brain. Now is the time for her miracle.
We are devastated. Ever since we first found out about her diagnosis of left hemimegalencephaly, we have been praying and asking you all to pray that her right brain be spared. And you have shown up and helped us pray for this intention! All along the doctors have told us how strong and beautiful her right brain looked.
However, this all changed sometime in the night between Friday and Saturday. At a time when we thought we were in the clear and were actually making plans to go home in a couple of weeks (!), something happened. The doctors can't explain it, they are looking into every avenue, as this was completely unexpected and unexplainable. She was awake. She was breathing on her own. She was moving. Shad was with her Friday night and video chatted me and I could not wait to see her the next day, finally alert! But suddenly very early that morning she took a turn and stopped responding. That's when her seizures started and they were indeed coming from the right side this time, due to whatever injury the right side sustained. They said her injury looks consistent with hypoxic-ischemic encephalopathy but none of her vitals ever changed and her labs have remained great. There is truly no explanation at this time.
My heart is broken. I cry out to God to understand why, in this final moment, when we were so close to her recovery, did this happen? I am trusting in Him with all my might and KNOW in my heart and soul that He is loving her far greater than I, but oh man I am absolutely broken.
She has lost 40-60% of function in her right brain. Even typing it out and reading it in this post is too cruel to bear. They don't expect that she is in dire life threatening circumstances yet but they also can't say that her brain won't be injured further - since we still don't have a cause. Even if she survives all of this and is able to come home, we don't yet know what kind of life our little, beautiful perfect girl will have with only 25% of her brain. At this point, the most basic expectation is that she will not be able to walk or talk along with many other difficulties.
She is outside of what they can do (other than trying to prevent more damage) and is truly in God's hands now. I told our priest yesterday before we got the full news - perhaps God is giving us the most dire of circumstances to give us the most miraculous of recoveries. In a world that needs to witness a miracle more than ever, I am praying to God that He show us one now. Please, please, please, keep praying for our Vianney - that her brain is completely healed and she can defy all medical expectations.
And if now is the time for a miracle, then we are asking you to also beg for the prayers of the Blessed Ulma family. Soon I will share more about this incredible family, but for now we are asking them to pray along with us for our little Vianney’s miracle!]
Please storm heaven for my friend's little girl! 🙏
You can follow their GiveSendGo for updates
Prayer for the Intercession of the Ulma Family
Almighty and eternal God,
We thank You for the testimony of the heroic love of the spouses Józef and Wiktoria with their children, who gave their lives to save persecuted Jews.
May their prayers and example support families in Christian life and help everyone to follow the true path of holiness.
Lord, if it is in accordance with Your will, kindly grant the grace for the complete healing of little Vianney, for which we are asking You through their intercession and count them among the Blessed.
Through Christ Our Lord
Amen
Our Father…, Hail Mary…, Glory Be…

#prayer request#prayer#prayers needed#blessed ulma family#catholic#tumblr catholics#yes i have permission to share all of this#jennifer's fb is public due to her A Love So Strong ministry
82 notes
·
View notes
Link
Accepted dogma holds that—although every cell in the body contains its own DNA—the genetic instructions in each cell nucleus are identical. But new research has now proved this assumption wrong. There are actually several sources of spontaneous mutation in somatic (nonsex) cells, resulting in every individual containing a multitude of genomes—a situation researchers term somatic mosaicism. “The idea is something that 10 years ago would have been science fiction,” says biochemist James Eberwine of the University of Pennsylvania. “We were taught that every cell has the same DNA, but that's not true.” There are reasons to think somatic mosaicism may be particularly important in the brain, not least because neural genes are very active.
[...]
A 2012 study found somatic mutations in the brains of children with hemimegalencephaly, a developmental disorder in which one hemisphere is enlarged, causing epilepsy and intellectual disability. The mutations were found in brain tissue, but not always in blood nor in cells from unaffected brain areas, and only in a fraction (around 8 to 35 percent) of cells from affected areas. Such studies, showing somatic mutations can cause specific populations of cells to proliferate, leading to cortical malformations, has researchers wondering whether somatic mutations may also play roles in more complex conditions.
Mature neurons stop dividing and are among the longest-living cells in the body, so mutations will stick around in the brain. “In the skin or gut, cells turn over in a month or week so somatic mutations aren’t likely to hang around unless they form cancer,” McConnell says. “These mutations are going to be in your brain forever.” This could alter neural circuits, thereby contributing to the risk of developing neuropsychiatric disorders. “In psychiatric disease we don't know that much yet, and that’s largely the goal [to find an answer],” McConnell says. “It’s a good hypothesis but it’s going to require this big, multi-team effort to really address it.”
[...]
One question to be explored is whether genes associated with a brain disorder may harbor somatic mutations. The fact specific genes only explain a small proportion of cases may be because researchers have only been looking in the germ line (sex cells), McConnell says. “Maybe the person doesn’t have the mutation in their germ line, but some percentage of their neurons have it.” Somatic mosaicism may also contribute to neural diversity in general. “It might explain why everybody’s different—it’s not all about the environment or genome. There’s something else,” says neuroscientist Alysson Muotri of the University of California, San Diego, who is not part of the consortium. “As we understand more about somatic mosaicism, I think the contribution to individuality as well as the spectrum [of symptoms] you find in, for example, autism, will become clear.”
16 notes
·
View notes
Photo

Энцефалит Расмуссена/ #Rasmussen's #Encephalitis является прогрессивной атрофией одной гемисферы у детей. У пациента развивается возрастающая частота эриприступов и прогрессивная гемиплегия. #мрт#кт#мскт#рентген#mri#CT#xray#head#spine#knee#abdomen#muskuloskeletal#neuroradiology#teacher#radiology#neurosurgery#neurology##medizin#невролог#педиатр#педиатрия By radiologyassistant.nl Rasmussen's encephalitis is a progressive hemispheric atrophy of unknown origin. Patient develop an increasing frequency of seizures and progressive hemiplegia. Notice that, opposed to hemimegalencephaly, the smaller hemisphere is the site of abnormality, and the lateral ventricle is larger in the smaller hemisphere
#muskuloskeletal#невролог#мскт#neuroradiology#педиатрия#мрт#knee#mri#teacher#ct#педиатр#кт#xray#neurology#spine#radiology#rasmussen#abdomen#рентген#medizin#encephalitis#neurosurgery#head
0 notes
Text
Aberrant Midsagittal Fiber Tracts in Patients with Hemimegalencephaly
#Figureskate #NorikoSato [ajnr.org]d Department of Diagnostic Imaging and Nuclear Medicine, Kyoto University School of Medicine, Kyoto, Japan e Department of Radiology, Tokyo University School of Medicine, Bunkyo-ku, Tokyo, Japan Please address correspondence to Noriko Sato, MD, PhD …
0 notes
Text
Aberrant Midsagittal Fiber Tracts in Patients with Hemimegalencephaly
#Figureskate #NorikoSato [ajnr.org]d Department of Diagnostic Imaging and Nuclear Medicine, Kyoto University School of Medicine, Kyoto, Japan e Department of Radiology, Tokyo University School of Medicine, Bunkyo-ku, Tokyo, Japan Please address correspondence to Noriko Sato, MD, PhD ...
0 notes
Link
Joss is in the News Again!
#Dr. Ki Lee#Epilepsy#Florida Hospital for Children#hemimegalencephaly#hemispherectomy#Joscelyn Dempsey
0 notes
Photo

Essential Brains
Our brain is the control centre for everything we do, think and feel. Malformations in the brain can be disastrous and leave the sufferer incapacitated. Hemimegalencephaly is a rare brain malformation in which one side of the brain is abnormally large, seen here highlighted by the dashed line on the left, and causes severe epileptic seizures. The deformity is caused by mutations in the genome of individual brain cells during development. Currently surgery is the most successful treatment for severe symptoms, but for some patients this can mean having the entire affected half of their brain removed. While the remaining healthy side of the brain may gradually take over functions that have been lost, the procedure is immensely invasive. Scientists are now investigating the gene mutations sustained by the developing brain cells in the hope of uncovering better ways to treat such debilitating conditions in the future.
Written by Mary-Clare Hallsworth
--
Christopher Walsh
Harvard Medical School, USA
Copyright Elsevier 2012
Published in Cell 151(3): 483-396
15 notes
·
View notes
Text
Hemimegalencephaly
Its my condition. I can't even pronounce it but give me time. It means that my left side of my brain is larger than the right side of my brain, and it was oddly developed.
I'm called one the lucky ones. It's because my abnormality is more subtle then most. I actually have decent motor functions and have developed normally. So technically, i'm an anomaly. Cool huh? Well they thought it was a tumour, so thank god its just this.
I still have an MRI to go through, by my neurologist I really have nothing to worry about.
Now I can make big brain jokes or "if I had that tumour jokes" ...
0 notes
Text
Aberrant Midsagittal Fiber Tracts in Patients with Hemimegalencephaly
#Figureskate #NorikoSato [ajnr.org]d Department of Diagnostic Imaging and Nuclear Medicine, Kyoto University School of Medicine, Kyoto, Japan e Department of Radiology, Tokyo University School of Medicine, Bunkyo-ku, Tokyo, Japan Please address correspondence to Noriko Sato, MD, PhD …
0 notes
Text
Aberrant Midsagittal Fiber Tracts in Patients with Hemimegalencephaly
#Figureskate #NorikoSato [ajnr.org]d Department of Diagnostic Imaging and Nuclear Medicine, Kyoto University School of Medicine, Kyoto, Japan e Department of Radiology, Tokyo University School of Medicine, Bunkyo-ku, Tokyo, Japan Please address correspondence to Noriko Sato, MD, PhD ...
0 notes