#immunohistochemical staining
Text

immunohistochemistry cancer|IHC-PRS
#immunohistochemistry cancer#pathology slides#ihcstaining#digital pathology#immunohistochemical staining
0 notes
Text
Empowering Pathologists: NanoGene's Tech-Only Services
NanoGene Laboratory is at the forefront of advancing pathology through a comprehensive suite of tech-only services. For more details on their services, visit this link: https://nanogene.com/.
1 note
·
View note
Text
Day 2 of being back at work and I’m already done with everything. Having one person on staff to do an entire hospital’s load of IHC (immunohistochemical) staining is absurd. And everything is manual so the chance of error is much higher than I’m comfortable with.
4 notes
·
View notes
Text
The Crucial Role of Histochemical and Immunohistochemical Staining in Biomedical Research
Histochemical and immunohistochemical staining are indispensable techniques in biomedical research and diagnostic pathology. These methods enable scientists and clinicians to visualize and analyze the complex structures and functions within tissues, contributing significantly to our understanding of various diseases and conditions. This article delves into the importance of histochemical staining, immunohistochemical stains, and immunohistochemistry services, highlighting their applications and benefits.
Histochemical Staining
Histochemical staining involves the use of chemical reactions to identify and visualize specific components within tissue sections. This technique is essential for studying the structure, composition, and function of tissues at the microscopic level.
Histochemical stains can highlight various cellular components, such as carbohydrates, lipids, proteins, and nucleic acids. For instance, Hematoxylin and Eosin (H&E) staining is a widely used histochemical technique that provides detailed information about tissue morphology. Hematoxylin stains cell nuclei blue, while eosin stains the cytoplasm and extracellular matrix pink, creating a clear contrast that helps in identifying cellular structures and abnormalities.
Immunohistochemical Stains
Immunohistochemical (IHC) staining uses antibodies to detect specific antigens in tissue sections. This method combines histological and immunological techniques, making it possible to pinpoint the presence and location of proteins, pathogens, and other molecules within tissues.
The primary advantage of IHC staining is its specificity. By using antibodies that bind to particular antigens, researchers can identify and visualize the distribution and abundance of these targets within the tissue. This is especially valuable in cancer research, where IHC can detect tumor markers, helping to classify different types of cancer and guide treatment decisions.
Immunohistochemistry Staining
Immunohistochemistry (IHC) staining is a broader term that encompasses various techniques and applications of using antibodies for tissue analysis. IHC staining is crucial in both research and clinical settings, offering insights into the molecular mechanisms underlying diseases and aiding in the diagnosis and prognosis of various conditions.
IHC staining involves several steps: tissue preparation, antigen retrieval, antibody incubation, and visualization. Each step requires meticulous attention to detail to ensure accurate and reliable results. The choice of antibodies, detection systems, and visualization techniques can vary depending on the specific research or diagnostic question.
Immunohistochemistry Services
Professional immunohistochemistry services provide comprehensive support for researchers and clinicians who require high-quality IHC staining. These services often include antibody selection, tissue processing, staining, and analysis, ensuring that every aspect of the IHC process is expertly managed.
In San Diego, numerous laboratories and biotech companies offer specialized immunohistochemistry services, leveraging advanced technologies and expertise to deliver precise and reproducible results. These services are invaluable for researchers studying complex diseases, drug development, and biomarker discovery.
Histochemical and immunohistochemical staining are pivotal techniques in the field of biomedical research and pathology. They provide critical insights into the structure and function of tissues, enabling the detection and analysis of specific molecules within complex biological systems. With the availability of advanced immunohistochemistry services, researchers and clinicians can access high-quality staining and analysis, driving forward our understanding of diseases and improving diagnostic and therapeutic strategies. Whether through detailed histochemical staining or highly specific immunohistochemical stains, these techniques continue to be at the forefront of scientific discovery and medical innovation.
0 notes
Text
IHC Ancillaries
IHC ancillary products cover deparaffinators, retrievers and enzymes, washers and detergents, diluents and blockers, mounting media, counterstainers, and slide treatment solutions.
Immunohistochemical staining depends on many different factors, all of which can affect the result. CD BioSciences offer several reagents to ensure optimal conditions for high-quality staining and reliable and accurate results each time an antibody is applied to a tissue.
0 notes
Text
📆 Jan 2007 📰 The Effect of Toxoplasma gondii on Animal Behavior: Playing Cat and Mouse
As specified by the “manipulation hypothesis,” certain parasites can alter host behavior for their own selective benefit. Classic examples concern transmission through the food chain, where a parasite is immature in an intermediate host, that must be eaten by a predatory definitive host before the parasite can reach maturity and complete its life cycle. The parasite thus manipulates the behavior of its intermediate host so as to enhance its transmission to the definitive host. Toxoplasma gondii provides a convincing example of such a manipulatory parasite. Members of the cat family (Felidae) are the only definitive hosts, within which the parasites undergo full gametogenesis and mating within the intestinal epithelium.
... Subsequent studies took the concept that T. gondii can alter innate behavior further by examining whether T. gondii affects a rat's perception of cat predation risk. The response to cat odor was chosen as a measure because this is known to elicit strong innate aversion, even among laboratory rodents following several hundred generations of passage. While uninfected rats showed a strong aversion to areas with cat odor (but not to, eg, rabbit odors), a proportion of infected rats showed not simply a reduction in their cat-aversion areas but actually a preference for cat-treated areas. These results suggested a significant divergence in the perceived response to cat predation, where uninfected rats show a significant and innate avoidance of cat-scented areas while infected rats show a significant, potentially suicidal, preference for cat-treated areas.

The next experiment drew on the demonstration that many antipsychotic drugs commonly used in the treatment of schizophrenia inhibit the replication of T. gondii tachyzoites in cell culture. Such observations provided support for the hypothesis that the antipsychotic and mood-stabilizing activity of some medications may be achieved, or at least augmented, through their inhibition of T. gondii replication and/or invasion in infected individuals. Moreover, they led to the prediction that such medications could also inhibit the behavioral effects of T. gondii in rats.
To test this, 4 groups of rats were infected with T. gondii and then treated, respectively, with haloperidol, valproic acid (both of which were shown to be highly effective inhibitors of T. gondii in cell culture), pyrimethamine with dapsone (a standard anti–T. gondii agent), and water. Without drug treatment, the infected rats demonstrated the same suicidal feline attraction and altered behavior described above. Following treatment, however, such behavior was significantly reduced, in order of decreasing efficacy, by haloperidol, pyrimethamine with dapsone, and valproic acid.
Moreover, fluorescence staining of tissue sections throughout the brains at postmortem indicated that the frequencies of T. gondii–exposed animals showing immunohistochemically positive neurons and glial cells were reduced following drug treatment, especially with haloperidol. Furthermore, certain T. gondii–exposed rats treated with haloperidol failed to seroconvert from IgM to IgG, while all the other treated rats did so.
1 note
·
View note
Text
Common Misdiagnoses in Lymphomas and Effective Strategies to Avoid Them
Lymphoma, a blood cancer that impacts the lymphatic system, plays a significant role in the body's immune defence. Lymphoma comprises two main types: Hodgkin lymphoma (also known as Hodgkin's disease) and non-Hodgkin lymphoma (NHL). While Hodgkin lymphoma is relatively easier to diagnose due to specific symptoms and the presence of Reed-Sternberg cells, NHL presents more complexity.
The immune system's compromised state in lymphoma patients makes it harder to combat other diseases and intensifies the challenge of fighting the lymphoma itself. Non-Hodgkin lymphomas develop from mutated white blood cells that multiply and spread rapidly through the lymph system, potentially affecting multiple areas of the body. Determining the causes of non-Hodgkin lymphoma remains unclear in most cases.

Diagnosing lymphoma involves various approaches. In suspected cases of NHL, physicians may perform a biopsy if a swollen lymph node persists or fails to regress. This procedure entails the removal of a small portion of the swollen lymph node for observation and testing. Biopsies provide the definitive diagnosis for non-Hodgkin lymphoma. In some instances, bone marrow biopsies are conducted to assess whether the lymphoma has reached the marrow.
On the other hand, diagnosing Hodgkin lymphoma typically involves blood tests and imaging techniques such as X-rays, CT scans, and MRIs. Blood tests can detect the presence of Reed-Sternberg cells, indicating Hodgkin lymphoma. Biopsies, including bone marrow biopsies, may also be performed to confirm the presence of Hodgkin lymphoma.
While these diagnostic methods are essential, pitfalls and misdiagnoses can occur. Understanding and addressing these common challenges in lymphoma diagnosis is vital to ensure accurate identification and appropriate treatment. In the following sections, we delve into the potential pitfalls and misdiagnoses associated with lymphoma. This will shed light on the complexities faced by healthcare professionals in accurately diagnosing this intricate disease.
Common Misdiagnoses & Pitfalls When Dealing with Lymphoma Cases
Here, we discuss the common misdiagnoses and pitfalls when dealing with lymphoma cases, the causes of these errors, and strategies to avoid inaccurate diagnoses.
Inadequate Material Including Insufficient Specimens & Sampling Errors
Insufficient samples and mistakes in how they are taken can make it hard to accurately diagnose a condition. When using ultrasound or CT-guided biopsies, it is best to use a specific needle size to ensure enough tissue is collected for testing. Sometimes the tissue sample does not accurately represent the problem, which can lead to the wrong diagnosis.
To prevent this, pathologists should communicate regularly with doctors and explain what kind of samples they need. Whenever possible, it is best to remove the entire affected area for testing. It is also important to train new pathologists on how to take proper tissue samples.
Insufficient Processing of Tissue
Processing tissue involves a series of steps to prepare it for examination, including fixing, dehydrating, embedding, sectioning, staining, and mounting. Each step is crucial to obtaining well-stained sections for an accurate diagnosis. Neglecting any part of this process can lead to diagnostic errors.
For instance, lymph nodes need to be promptly fixed and sliced before fixation because their outer protective layer hinders the penetration of the fixing agent. Insufficient or improper fixation can alter the tissue's appearance and affect immunohistochemical results.

When lymph nodes are not properly fixed and cut, the outer part may look preserved, but the centre may show shrunken lymphocytes that resemble plasma cells. This can result in misdiagnosing plasmacytoma instead of diffuse large B-cell lymphoma. In addition, there can be misdiagnoses of T-cell lymphoma instead of Epstein-Barr virus (EBV)-positive large B-cell lymphoma.
Another issue in tissue processing is "dry-mounting," which occurs when a slide is dried with a hairdryer without using xylene to make it clear. This causes the nuclei of lymphocytes to shrink into dark dots without any discernible details, making accurate diagnosis challenging. Researchers have highlighted these problems and provided solutions to address them.
Inadequate Clinical Information
To make a precise diagnosis of lymphoma, it is crucial to have sufficient clinical information alongside the pathology findings. The World Health Organization (WHO) highlights the importance of combining clinical details, physical appearance, immunophenotyping, and genetic data to reach an accurate diagnosis for these types of diseases.
Therefore, regular discussions among a team of specialists from various fields (known as multidisciplinary discussions) are significant in diagnosing complex cases like lymphomas and other challenging diseases. These discussions help ensure a comprehensive approach and improve diagnostic accuracy.
Errors Due to Personal Subjectivity
Even though advanced techniques are used in diagnosing diseases, the final diagnosis ultimately relies on the personal judgment of the pathologist. Because different pathologists may have different training and experience, they may interpret the same specimen in different ways.
These differences in interpretation can lead to delays in providing appropriate treatment for patients and, in rare cases, even legal complications. To address this issue, pathologists can specialize in specific diseases and seek opinions from experts with extensive experience in that area. This collaboration helps minimize subjective errors and improve the accuracy of diagnoses.
Inaccuracy Relating to Immunohistochemistry
Errors in immunohistochemistry can occur for several reasons:
Insufficient knowledge of antibody reactions
Improper use of positive and negative controls
Changes in sensitivity caused by variations in reagents or equipment
Limited range of tests conducted due to cost concerns
Performance degradation of reagents if not used and replaced adequately
One common error is not conducting a comprehensive range of antibody tests, which can result in a lack of diagnostic accuracy. For example, a lymphoma initially misdiagnosed as marginal zone lymphoma was later identified as mantle cell lymphoma when the patient developed cervical lymph node enlargement. This misdiagnosis could have been avoided if CD5 and Cyclin D1 expressions were initially examined.
Using an insufficient panel of immunostains can also lead to a misdiagnosis. For instance, an ALK-positive lymphoma might be mistakenly identified as Hodgkin lymphoma or reactive lymphoid proliferation if ALK is not included in the initial panel of antibodies.
Pathologists need to understand the specificity of antibodies. Monoclonal antibodies target specific epitopes on antigens but may not recognize the entire cell expressing that antigen. Some antibodies can exhibit cross-lineage expressions, such as CD20 in T and NK cell lymphomas or CD3 in non-T cell lymphomas. Additionally, certain antibodies may have lower sensitivity than expected, and their staining can vary with fixation, potentially resulting in missed true positive cells.
Errors Relating to Molecular Genetic Tests
In the pathological field, along with immunohistochemistry, molecular and cytogenetic techniques are becoming increasingly important. These methods serve as supplementary tools and involve analyzing specific genetic changes.
Some of the examples include analyzing rearrangements in genes like IGH, IGK, IGL, TCR-B, and TCR-G, as well as fusion genes like IGH-BCL2, CCND-IGH, BCL6, MALT1, and MYC. However, interpreting the results of these techniques requires specialized training due to their complexity.
It is essential to understand the specificity and limitations of each test when analyzing the molecular and cytogenetic results. It is also important to note that the presence of a monoclonal result does not always indicate malignancy, and the results must be considered in conjunction with clinical information, physical appearance, immunohistochemistry, and other findings. In some cases, small biopsies can show a pseudo-monoclonal result, which reflects normal immune reactions rather than malignancy.
Fortunately, advancements in immunohistochemistry now allow for the detection of many molecular changes through protein expression analysis. For instance, the protein expression of ALK, MYC, and mutations in the epidermal growth factor receptor (EGFR) at specific locations (exons 19 and 21) can be assessed. It is predicted that in the near future, no more than 5% of lymphoma diagnoses will rely solely on molecular and cytogenetic tests.
Accurate diagnosis of lymphomas is crucial for effective treatment. Healthcare professionals should identify the early signs of lymphoma. They should also know the common misdiagnoses, including inadequate samples, errors in tissue processing, a lack of clinical information, subjective interpretation, and errors in immunohistochemistry and molecular genetic tests. By addressing these challenges through proper training, collaboration, and attention to detail, we can improve diagnostic accuracy and enhance patient care.
0 notes
Text
Variable Outcome of Immunotherapy in Advanced Multiple Cutaneous Squamous Cell Carcinomas in Two Patients with Recessive Dystrophic Epidermolysis Bullosa
Cutaneous squamous cell carcinoma (cSCC) is a major complication of recessive dystrophic epidermolysis bullosa (RDEB) that has high morbidity and mortality rates and unmet therapeutic needs. The aim of this study was to evaluate the molecular pattern of cSCC and the clinical course of immunotherapy in 2 RDEB patients with multiple advanced cSCC. Clinical course and disease staging were evaluated retrospectively. The tumour tissues were subjected to immunohistochemical staining. DNA from the... http://dlvr.it/Sr1FtR
0 notes
Text
Localised Cutaneous Amyloidosis of the Glans Penis: A Case Report and Review of the Literature by Victoria Hyett in International Journal of Clinical Images and Medical Reviews
Abstract
Amyloidosis represents a notable cause of morbidity within the developed world. Urological presentations of systemic or localised amyloidosis are rare, with penile amyloidosis being poorly reported. We performed a literature review investigating cases of penile cutaneous amyloidosis via the PubMed database during March 2020, in conjunction with clinical review of a local patient presenting with a penile lesion. Our patient is a 60-year-old uncircumcised, caucasian male presenting with a longstanding history of 2 irregular lesions affecting his glans penis and a further 2 lesions affecting the inner surface of his prepuce. He underwent excision biopsy of the largest lesion which represented cutaneous amyloid deposits. He underwent immunological testing for systemic disease which was negative.
In current literature, there are 13 cases of cutaneous amyloidosis affecting the glans penis, with 1 of those having evidence of extra genitourinary amyloid deposits. All the documented cases were treated with local excision and investigation for systemic disease. It is important to recognise alternative diagnoses in patients presenting with penile lesions. Despite cutaneous amyloidosis mimicking malignancy macroscopically, the morbidity and mortality is lower in comparison to penile cancer. Treatment remains surgical excision of the lesion and further investigations to exclude systemic disease.
Introduction
Amyloidosis is a notable cause of morbidity, and in some cases mortality within the developed world. Urological presentations of systemic or localised amyloidosis are rare, with primary penile amyloidosis being poorly reported in the literature. It can commonly mimic malignancy on imaging and macroscopically, thus representing an important differential diagnosis to be aware of when examining and investigating a penile lesion.
Case Presentation
A 60-year-old uncircumcised, Caucasian male was referred with multiple longstanding granular lesions of his penis. His past medical history included hypertension and insulin dependent type 2 diabetes. On initial assessment there were two irregular granular lesions on his glans penis and two further similar lesions on the inner prepuce. These were initially thought to be malignant and an excision biopsy of the largest one was performed.
The histopathological examination showed an abundance of relatively amorphous pink material in the superficial to mid dermis with positive Congo red staining and mild apple-green birefringence in keeping with cutaneous amyloidosis. Further analysis with immunohistochemical staining of the sample by the National Amyloidosis Centre confirmed this result and determined this to be of the AL Kappa subtype.
Following investigation under the care of the haematology department with serum free serum light chains, electrophoresis and Bence Jones’ protein, there was no evidence of systemic amyloidosis or multiple myeloma. A diagnosis of cutaneous AL amyloidosis of Kappa subtype affecting the glans penis and prepuce was made.
The patient underwent a circumcision for localised treatment of the remaining preputial lesions. The remaining glandular one was deemed high risk for meatal stenosis due to its proximity to the urethral meatus and therefore not excised.
The patient remains well under yearly review from the National Amyloidosis Centre.
Discussion
The term ‘Amyloid’ was first coined by Virchow in the 19th century to describe a macroscopic tissue abnormality characterised by a positive iodine staining reaction. Subsequent technological advancements in light microscopy furthered Virchow’s description to include distinct birefringence of the amyloid deposits when stained with Congo red dye [1].
The pathophysiology of amyloidosis stems from a failure of proteolysis of misfolded proteins resulting in oligomeric conglomerates referred to as amyloid fibrils. As amyloidosis is caused by misfolded proteins, there are multiple classifications of the disease specifically related to the original protein involved. All of the involved proteins may form extracellular deposits and lead to subsequent organ dysfunction [2]. The most common subtypes of amyloidosis include amyloid light chain (AL), the origin of which is an immunoglobulin arising from plasma cells, and amyloid associated (AA), arising from a non-immunoglobulin synthesised by the liver. Further classification can be made by the clinical presentation of the proteinaceous deposit; whether it be systemic or localised, and the clinical syndrome it produces.
The amyloid Light Chain (AL) subtype is characterized by clonal plasma cell dyscrasia, similarly to multiple myeloma [3]. This results in a failure to produce the classical alpha-helix configuration of either kappa or lambda light chains, instead producing a beta-pleated sheet which is inherently insoluble. Classically there is involvement of the kidneys, heart or nervous system however involvement of many organ systems has been documented.
Cutaneous amyloid deposits can be seen in both systemic and localized disease. Commonly up to 40% of systemic AL amyloidosis sufferers complain of epidermal disease, which reflects amyloid deposition within the capillaries of the skin involved. Cutaneous disease typically presents as petechiae or purpuric lesions, yellow macular or nodular lesions. There are also macular and lichen subtypes which can be associated with systemic connective tissue diseases.
Statistically, within the UK the age-adjusted prevalence of amyloidosis is between 5.1 and 12.8 per 1 million per year*. Approximately 10-20% of cases remain localised, with the remainder of cases being classified as systemic disease. Although the localised form is rarer, it carries a better prognosis [5]. Rarer still is localised penile amyloidosis, with only 14 documented cases, including ours, on literature review.
Merika et al. comments on the low prevalence of systemic disease in those presenting with cutaneous penile amyloid lesions as the primary presenting complaint. Their study also highlights the increased rate of primary nodular amyloidosis amongst those with penile cutaneous lesions [4]. Of the confirmed cases of cutaneous amyloidosis of the glans penis, only one reported a second site affected, namely the trachea. This was subsequently found to be a lone deposit, with no further evidence of widespread disease identified; however, this does not exclude the possibility of this representing systemic amyloidosis [16].
Of the cases identified, most were diagnosed on a serological and histological basis, more in depth modalities such as serum amyloid protein component (SAP) scintigraphy and genetic testing were not performed routinely. SAP scintigraphy is highly sensitive for AL and AA amyloidosis (90% for both subtypes), with a specificity of 93%. The use of SAP scintigraphy may give a more definitive answer regarding the presence of systemic disease however the modiality itself is often not available in local centres [17,18].
Treatment of the lesions remains case dependent and requires a multi-disciplinary approach [19]. The underlying amyloid subtype also greatly influences management. In systemic AL amyloidosis, treatment aims to suppress plasma cell production of amyloid which predominantly involves using dexamethasone and mephalan, an oral chemotherapeutic agent, alongside supportive care for the underlying organs involved. Similarly, AA amyloidosis requires management of the underlying disease process often involving immunomodulation [19]. Localised cutaneous amyloidosis is typically managed by surgical excision, or laser ablation, systemic chemotherapeutic agents are usually not employed due to their side effect profile [16]. The majority of cases reported were treated with local excision as in our case.
Conclusion
These cases highlight the importance of consideration of alternative diagnoses in patients presenting with cutaneous penile lesions. Fortunately, despite penile cutaneous amyloidosis mimicking malignancy, the morbidity and mortality are low due to the low incidence of systemic amyloidosis in patients who present with a penile lesion. Treatment remains local excision of the lesion, histological and immunochemical confirmation of the amyloid subtype and further investigations to exclude systemic disease. Consideration could be made for the introduction of SAP scintigraphy in these cases, however the benefit of this remains unclear with such a small demographic to review.
For more details: https://ijcimr.org/editorial-board/
#Amyloidosis#Urological#poorly#immunological#genitourinary#macroscopically#amorphous pink#Victoria Hyett#ijcimr
0 notes
Text
New study suggests a promising therapeutic target for sepsis
PLK1 promotes intestinal epithelial autophagy in intestinal epithelia in cecal ligation and puncture (CLP) mice. CAG-PLK1 mice were intraperitoneally injected with chloroquine (CQ; 60 mg/kg bodyweight) or rapamycin (Rapa; 10 mg/kg bodyweight) 1 hour after the CLP operation; the mice were then sacrificed 24 hours after CLP. A: Representative images of LC3-II and P62 immunohistochemical staining in…

View On WordPress
0 notes
Text
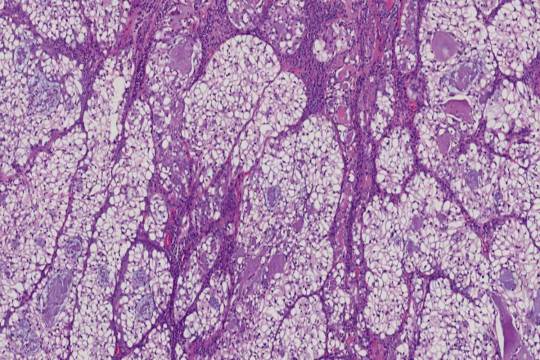
Unlocking the Power of Immunohistochemical Staining: A Deep Dive into Pathology Slides
Immunohistochemical staining (IHC) is a crucial technique in the field of pathology, offering invaluable insights through pathology slides. This method allows for the detection and visualization of specific proteins within tissue samples, providing a detailed understanding of disease mechanisms.

IHC involves using antibodies to target specific antigens in tissue sections. When these antibodies bind to their targets, they produce a detectable signal, usually visualized under a microscope. Pathology slides treated with Immunohistochemical Staining can reveal the presence, localization, and concentration of proteins, which is critical for accurate diagnosis and treatment planning.
The application of IHC-PRS (Immunohistochemical Staining - Pathology Slide) is particularly significant in oncology, where it helps identify tumor markers and guide therapeutic decisions. By analyzing pathology slides with IHC, pathologists can differentiate between various types of cancers, assess their aggressiveness, and predict patient outcomes.

Moreover, immunohistochemical staining is not limited to oncology; it is also instrumental in research and diagnostics across various medical fields. It provides a deeper understanding of cellular processes and disease pathology, aiding in the development of targeted therapies.
In summary, immunohistochemical staining of Pathology Slides, or IHC-PRS, is an indispensable tool in modern medicine. Its ability to provide precise information at the molecular level enhances diagnostic accuracy and contributes to more effective patient management. Embracing IHC-PRS in pathology ensures a more detailed and informed approach to diagnosing and treating diseases.
#immunohistochemical staining#pathology slides#immunohistochemistry protocol#digital pathology scanner#ihc staining
0 notes
Text
Medicina, Vol. 59, Pages 190: Sevoflurane Exposure of Clinical Doses in Pregnant Rats Induces Vcan Changes without Significant Neural Apoptosis in the Offspring
Background and Objectives: Sevoflurane is a commonly used inhalational anaesthetic in clinics. Prolonged exposure to sevoflurane can induce significant changes in lipid metabolism and neuronal damage in the developing brain. However, the effect of exposure of pregnant rats to clinical doses of sevoflurane remains unclear. Materials and Methods: Twenty-eight pregnant rats were randomly and equally divided into sevoflurane exposure(S) group, control (C) and a blank group at gestational day (G)18; Rats in S group received 2% sevoflurane with 98% oxygen for 6 h in an anesthetizing chamber,while C group received 100% oxygen at an identical flow rate for 6 h in an identical chamber. Partial least squares discriminant analysis (PLS-DA), ultra performance liquid chromatography/time-of-flight mass spectrometry(UPLC/TOF-MS) and MetaboAnalyst were used to analysis acquire metabolomics profiles, and immunohistochemical changes of neuronalapoptosis in hippocampus and cortex of neonatal rats were also analyzed. Results: This study aimed to explore lipidomics and transcriptomics changes related to 2% sevoflurane exposure for 6 h in the developing brains of newborn offspring rats. Ultra-performance liquid chromatography/time-of-flight mass spectrometry (UPLC/TOF–MS) and #RNA sequencing (#RNA-seq) analyses were used to acquire metabolomics and transcriptomics profiles. We used #RNA-seq to analyse the expression of the coding and non-coding transcripts in neural cells of the cerebral cortex. No significant differences in arterial oxygen tension (PaO2), arterial carbon dioxide tension (PaCO2), or arterial blood gas were found between the groups. The relative standard deviation (RSD) of retention times was <1.53%, and the RSDs of peak areas ranged from 2.13% to 8.51%. Base peak chromatogram (BPC) profiles showed no differences between the groups. We evaluated the partial least square-discriminant analysis (PLS-DA) model. In negative ion mode, R2X was over 70%, R2Y was over 93%, and Q2 (cum) was over 80%. Cell apoptosis was not remarkably enhanced by TUNEL and haematoxylin and eosin (HE) staining in the sevoflurane-exposed group compared to the control group (p > 0.05). Glycerophospholipid (GP) and sphingolipid metabolism disturbances might adversely influence neurodevelopment in offspring. The expression of #mRNAs (Vcan gene, related to neuronal development, function and repair) of the sevoflurane group was significantly increased in the differential genes by qRT-PCR verification. Conclusions: GP and sphingolipid metabolism homeostasis may be potential therapeutic approaches against inhalational anaesthetic-induced neurodegenerative disorders. Meanwhile, sevoflurane-induced Vcan changes indicated some lipidomic and transcriptomic changes, even if neural cell apoptosis was not significantly changed in the usual clinical dose of sevoflurane exposure. https://www.mdpi.com/1648-9144/59/2/190?utm_source=dlvr.it&utm_medium=tumblr
0 notes
Text
Spindle cell sarcoma

They comprise less than 1% of all adult malignancies but are relatively common in the pediatric population, with an estimated incidence of 4 per 100,000 cases per year . Sarcomas are a very rare and heterogenous group of human malignant tumors of mesenchymal cells. Immunohistochemical stain (IHC) results were as follows: The histopathology results showed malignant spindle and epithelioid neoplasm with necrosis consistent with high-grade sarcoma. The differentials of the pelvic mass included lymphoma and STSs, and core needle biopsy was performed. To better identify the mass and its extent for possible surgical debulking, magnetic resonance imaging (MRI) of the abdomen and pelvis with contrast was also performed, which was remarkable for large pelvic mass fistulizing with the rectum (Figures 2, 3). A urinary catheter was placed, and broad-spectrum antibiotics including ciprofloxacin and metronidazole for bloody diarrhea was initiated, and he was admitted for further medical optimization. Stool cytology revealed numerous malignant spindle cells. Computed tomography (CT) of the abdomen and pelvis with contrast performed in the emergency department was remarkable for a 14.0 x 9.1 cm heterogenous solid mass fistulizing into the rectum (Figure 1), distension of the small bowel, and bilateral moderate hydronephrosis with possible hydroureter. Stool studies were unremarkable, and urine culture did not grow any microorganism. Initial laboratory workup including blood urea nitrogen, serum creatinine, electrolytes, hemoglobin, white blood cell count, platelet count, and lactic acid were all within normal limits. Subsequently, straight urinary catheterization was performed, which retrieved 900 mL of urine, with remarkable improvement in his symptoms. Emergent bladder scan showed that approximately 800 mL of urine was retained in the bladder. In the subsequent days, his symptoms worsened and he presented to the emergency department with severe lower abdominal pain, inability to void, and bloody diarrhea. His symptoms were attributed to enlarged prostate gland, and he was sent home on tamsulosin. His past medical history was significant for hypertension only. This is a very rare presentation of STS, and, to the best of our knowledge, only few similar cases have been reported thus far.Ī 68-year-old male presented to the primary care physician with difficulty in passing urine for two days. Core needle biopsy of the mass was performed, which showed malignant spindle and epithelioid neoplasm with necrosis consistent with high-grade sarcoma. To better identify the extent of disease, magnetic resonance imaging (MRI) with contrast was performed, which also revealed a similar large pelvic mass fistulizing into the rectum. All laboratory workup including complete blood count, complete metabolic panel, and urinalysis were within normal limits, but computed tomography (CT) of the abdomen and pelvis with contrast was remarkable for bilateral moderate hydronephrosis and a large 14 x 9.1 cm pelvic mass fistulizing into the rectum. Straight urinary catheterization retrieved 900 mL of urine, and a Foley catheter was placed. A 68-year-old male presented to the emergency department with abdominal pain, inability to void urine, and bloody diarrhea. We present a very interesting case of high-grade spindle cell sarcoma of the pelvis manifested as urinary retention and bloody diarrhea. Extremities are the most commonly affected anatomical sites, and majority of them present as a painless mass. Soft tissue sarcomas (STSs) are rare malignant tumors originating from mesenchymal cells.

0 notes
Link
To the Editor:
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has been associated with the development of autoimmune processes.[1], [2], [3], [4] Molecular mimicry has been suggested as a potential mechanism for these associations.1 In an in vitro study, Vojdani et al. 5 showed that antibodies against the spike protein S1 of SARS-CoV-2 had high affinity against the following human tissue proteins: transglutaminase 3, transglutaminase 2, anti-extractable nuclear antigen, nuclear antigen, and myelin basic protein. As this is the same viral protein that the vaccine mRNA codes for, it is plausible that these vaccines may unmask autoimmune diseases in predisposed patients. Recently, several cases of immune thrombocytopenia (ITP) developing days after COVID-19 vaccination, have been reported to the Vaccine Adverse Event Reporting System (VAERS), reinforcing the possibility of vaccine-induced autoimmunity.6
We have recently treated a 35-year-old Caucasian female in her third month postpartum, who developed autoimmune hepatitis after COVID-19 vaccination. During pregnancy, she was diagnosed with gestational hypertension and started on labetalol 100 mg bid. C-section was performed without any complications, and patient was discharged from the hospital on labetalol for blood pressure control. She resumed her job as a healthcare provider in mid-December, and received her first dose of Pfizer-BioNTech COVID-19 vaccine on January 4th. After 1 week, she started developing generalized pruritus, then choluria, and finally noticed jaundice, presenting to the emergency room on day +13 after COVID-19 vaccination.
She had a normal physical exam, except for scleral icterus, jaundice and palpable hepatomegaly. In the emergency room, laboratories were significant for: bilirubin 4.8 mg/dl, AST 754 U/L, ALT 2,001 U/L, alkaline phosphatase 170 U/L, and ammonium 61 mg/dl. Laboratory results were negative for hepatitis A, B, and C, Epstein-Barr virus (EBV), cytomegalovirus (CMV), herpes simplex virus (HSV) type 1 and 2, and HIV. At the time of submission, HEV had not been tested. Antinuclear antibody (ANA) was positive (1:1,280; homogeneous pattern). Double-stranded DNA antibodies were also positive (1:80). Other antibodies (i.e. anti-mitochondrial, anti-smooth muscle, liver-kidney microsomal, antineutrophil cytoplasmic antibodies) were negative. Total IgG was 1,081 mg/dl (normal range: 694–1,618 mg/dl). Ceruloplasmin, transferrin saturation, alpha-1-antitrypsin, TSH, and serum protein electrophoresis were all normal. Abdominal ultrasound with Doppler reported hepatomegaly without cirrhotic morphology, and no intra- or extra-hepatic biliary dilation.
Endoscopic ultrasound showed no evidence of biliary lithiasis or biliary dilation, and transduodenal liver biopsies were obtained. In Fig. 1 A–D we have included the slides of her liver biopsy and a full description of the histology. Liver biopsy was consistent with drug/toxin related liver injury, autoimmune hepatitis or infectious related etiologies. A PAS-D stain, CMV & HSV 1/2 immunohistochemical stains, EBV by in situ hybridization (EBER-ISH) and Grocott methenamine special stain for fungi were all negative. Other than the COVID-19 vaccine and labetalol, no other drugs, herbal supplements or toxins were reported by the patient. The Revised Original Score for autoimmune hepatitis pretreatment was 18 (results >15 suggest definite autoimmune hepatitis). Fig. 1E summarizes plasma ALT, AST, and total bilirubin over time, before and after treatment with prednisone 20 mg daily.
Fig. 1
Histological (H&E stain) and biochemical findings.
(A) Low-magnification (40x) shows pan-lobular hepatitis (black arrows: portal inflammation and yellow arrows: lobular inflammation). (B) Medium-magnification images (200x) show a portal tract with an intense lymphoplasmacytic infiltrate effacing the interface with rosette formation and (C) lobular activity with scattered hepatocyte necrosis (Black circle: acidophilic bodies). (D) At high magnification (600x), the inflammation consists primarily of lymphocytes with plasma cells (black arrowheads) and eosinophils (yellow arrowheads). (E) Trends of plasma ALT, AST and total bilirubin over time.
To our knowledge, this is the first reported episode of autoimmune hepatitis developing post-COVID-19 vaccination, raising concern regarding the possibility of vaccine-induced autoimmunity. As causality cannot be proven, it is possible that this association is just coincidental. However, severe cases of SARS-CoV-2 infection are characterized by an autoinflammatory dysregulation that contributes to tissue damage.1 As the viral spike protein appears to be responsible for this,1 , 5 it is plausible that spike-directed antibodies induced by vaccination may also trigger autoimmune conditions in predisposed individuals. In support of this, several cases of ITP have been reported days after COVID-19 vaccination.6
Several atypical features of her presentation deserve further discussion. First, immunoglobulin G levels were not elevated as typically reported for autoimmune hepatitis. However, Hartl et al. recently reported that ~10% of patients with autoimmune hepatitis had normal immunoglobulin G levels at presentation.7Second, histology revealed the presence of eosinophils, which are more commonly seen with drug or toxin induced liver injury. However, they can be found in cases of autoimmune hepatitis.8 It is also possible that we could be in the presence of a vaccine-related drug-induced liver injury with features of autoimmune hepatitis, as previously described for nitrofurantoin or minocycline.9 In line with this, the patient has already started a prednisone taper, as patients with well documented drug-induced AIH do not typically show relapses after steroid discontinuation.10 Finally, symptoms developed 6 days after vaccination, which instinctively appears as a short period of time. However, latency periods after vaccination of just days have been observed in prior reports.6 , 11
In summary, autoimmune hepatitis developed in a healthy 35-year-old female in her third month postpartum. Whether there exists a causal relationship between COVID-19 vaccination and the development of autoimmune hepatitis remains to be determined. We are hopeful that this manuscript will not discourage healthcare providers from getting and prescribing COVID-19 vaccines, but that it will raise awareness about potential side effects that will likely emerge as we continue to vaccinate more people. Only long-term follow-up of large cohorts of patients receiving the vaccine will answer the question as to whether it increases the risk of autoimmune conditions. Until then, healthcare providers are encouraged to remain vigilant.
3 notes
·
View notes
Text

immunohistochemical staining|IHC-PRS
#immunohistochemical staining#ihc staining#digital pathology scanner#digital pathology#immunohistochemistry antibodies
0 notes
Text
Biomolecules, Vol. 13, Pages 1260: Transcriptomics Reveals Molecular Features of the Bilateral Pelvic Nerve Injury Rat Model of Detrusor Underactivity
The pathogenesis of detrusor underactivity (DU) is unclear, and the available therapeutic effects are unsatisfactory. We propose to find key molecules and pathways related to DU based on transcriptome sequencing. A rat model of bilateral pelvic nerve injury (BPNI) was established. Bladder tissues from the sham-operated group, 3 and 28 days after BPNI mapping, were taken for urodynamics, histopathology, and #RNA-seq. An enrichment analysis of the screened differential expression genes was performed. Three days after BPNI, the results showed urodynamic features of overflow incontinence, while there was a recovery at 28 days after the operation. Masson staining revealed collagen deposition accompanied by progressive thickening of the smooth muscle layer as DU progressed. #RNA-seq results suggested that a total of 1808 differentially expressed genes (DEGs) differed among the groups. #RNA-seq and subsequent analysis confirmed that the cell cycle and immune response were significantly activated 3 days after BPNI, while extracellular matrix remodeling occurred 28 days after BPNI. Partial DEGs and pathways were verified by qRT-PCR. Validation of key proteins involved in cell cycle, inflammation, and fibrosis was performed by immunohistochemical staining and western blot, respectively. These molecular expression patterns at different time points after BPNI injury provide valuable insights into the search for therapeutic targets for DU. https://www.mdpi.com/2218-273X/13/8/1260?utm_source=dlvr.it&utm_medium=tumblr
0 notes