#pancreatitis liver enzymes
Text
googling how to trust a ct scan
#again that scan (entire stomach area) was completely fine so i cannot have pancreatic cancer one of the most deadly cancers ever#that raises liver enzymes. HOWEVER. what if doctors mixed up results or it’s wrong or. or. HELP#romeo’s wretched rambles
4 notes
·
View notes
Text
I am sick. I feel like I am not being listened to or heard. I keep explaining everything including how I feel but its like it does not matter. I went to multiple different doctors for diagnoses but its like what is the point of it? I feel like they are not listening nor are trying to help me. They keep pushing medications after medications and it is not helping only making it worst. I have chronic pancreatitis that flares up occasionally and I have fatty liver disease.
The hospital would not do anything for my pancreas. They gave me IV and nausea medications and sent me home. I have been taking Physicians Choice Digestive enzymes and OX bile and it seems to be helping break down the foods that my body cannot due to a missing gallbladder that I had to get out. It also
is not causing pain as bad in my pancreas and I am less bloated than I was.
My liver and pancreas took over and was doing all the work and no one told me that it was going to be harder for the body. No one explained anything to me and it took me until now since I have a medical knowledge and went to college for parts of it that it is going to cause this.
I spent 3 years suffering with pain, nausea, vomiting, diarrhea and I am still suffering with the pain trying to get it diagnosed but its like everywhere I go, no one is listening and is only making assumptions and playing a guessing game so I decided to self treat.
#CHRONIC PANCERATITS#DIGESTIVE TRACT ENZYMES#GALLBLADDER SURGERY#LIPASE#LIVER#NO GALLBLADDER#OX BILES#PANCREATITIS#PROBIOTICS#digestive health products market#digestive health
0 notes
Text
“I’m exhausted, nauseous and hurting”
- @texasred43
@texasred43 is back in the hospital because she has been nauseous for days and days. She can’t keep any food down due to the symptoms of her pancreatic cancer. And her liver enzymes are elevated, which indicates she may need another stent because the tumor is growing.
I’ll keep the Tumblrverse and the #tribe updated as best I can. Please keep her in your prayers. And if you can, please contribute to her GoFundMe to help her pay for these ongoing and ever-growing medical expenses.
https://gofund.me/4d810a58
41 notes
·
View notes
Text

“According to Eastern medicine be it Indian, Chinese, Tibetan or Thai, the left side of the body is totally different from the right side. Even some Buddhist monastic traditions include within their precepts for monks to sleep on their left side. Although it sounds weird resting and sleeping on the left side has many health benefits.
The lymph drains to the left.
The left side of the body is the dominant side of the lymphatic system. Most of the lymph drains down to the thoracic duct which is located on the left side. In its path the lymph transports proteins, glucose metabolites and waste products that are purified by the lymph nodes to be drained to the left side.
Derived from the above it is common to deduct in Eastern medicine that the diseases of the left side of the body may be due to chronic congestion of the lymphatic system.
The priorities of the body.
According to ayurveda congestion occurs in the body following certain priorities. If the lymphatic system is digested, the liver and blood are subsequently saturated with toxic substances. Primary symptoms of congestion present on the left side of the body before moving to the right side where they make their later appearance.
Feeling bored after a meal?
The Indian suggestion is that if you take a break after eating, do it lying on your left side. The rest should not exceed 10 minutes and is different from the evening nap which is usually 20 minutes or more.
Stomach and pancreas hanging to the left side. When you lie on your left side both naturally hang allowing for optimal and efficient digestion. Food is driven to move naturally through the stomach and pancreatic enzymes are secreted in a paulatin way and not in a single stroke, which happens if you lie down on the right side.
Laying on your left side your liver and gallbladder hang from your right side. Resting on the left side allows them to hang and secret their precious enzymes into the digestive tract, emulsifying fats and neutralizing stomach acids.
When the digestive system is stimulated this way your digestive cycle is shorter and doesn't leave you stranded for the rest of the afternoon. Try resting 10 minutes on your left side after eating.
Feel energized and not tired after eating.
Try to eat in a relaxed way mid-day and don't forget to rest on your left side and check that you will feel more energized and with better digestion.
Sleeping magic from the left side.
Best elimination.
The small intestine flushes toxins through the ileocecal valve (VIC) on the right side of the body at the start of the large intestine. The large intestine travels down the right side of your body, crosses your stomach and descends down the left side.
Through the VIC, sleeping on the left side allows gravity to stimulate bodily waste into the large intestine from the small intestine more easily.
As the night passes and continue sleeping on your left side the debris moves more easily toward the downward column and morning removal will be easier.
Best cardiac function.
More than 80% of the heart is located on the left side of the body. If you sleep on the left side the lymph drained to the heart will be driven by gravity taking work out of your heart while you sleep.
The aorta, which is the largest artery in the body, comes out from the upper part of the heart and is arched left before going down to the abdomen. By sleeping on the left side, the heart pumps blood more easily into the downing aorta.
Sleeping on the left side allows the intestines to move away from the cava vein that brings blood back to the heart. Noticeably the cava vein rests on the right side of the thorn, so when you lie down on the left side the viscera move away from the cava veina. Again gravity makes the heart job easier.
The sparrow is on the left side.
The spleen is part of the lymphatic system and is also on the left side of the body. Its function is that of a large lymph node which filters the lymph and additionally filters the blood. When you lie on the left side the fluids return to the basin is easier and is more easily produced by gravity.
The lymphatic system drains all cells in the body through contractions and muscle movement and not by heart pumping. Helping the lymph drain into the pelvis and heart with gravity is a simple way to purify your body.
And while there are no scientific protocols on it, sleeping on the left side does make sense. Understanding ancestral wisdom based on knowledge of modern anatomy clears up many doubts about the reasons that exist in the east to sleep a certain way.”
Original article written by Dr. John Doull
[Leila L'Abate]
#sleep#Physiology#left side#Leila L'Abate#Dr. John Doull#quotes#articles#lymphatic system#Body Alive
25 notes
·
View notes
Note
I’M LATE BUT HAPPY VALENTINE’S DAY💜💜
Bio chem has been kicking my ass all day and I finally got a breather 😭
My Valentine’s Day gift to you

I can’t remember if I’ve sent this to you already but it’s okay because it’s ✨Rhys✨
Those thighs 🧎🏻♀️🧎🏻♀️
HIIIIIII!!!
Happy Valentines! OMGGG WHAT A HOTTIE!!!!
I'm sorry biochem is kicking ur booty! It is all about the pathways if I am being honest! Def make diagrams of the metabolic pathways and include the enzymes (and if they drive the reaction forward or backward or both) and you should be solid!
For some reason, we were also always tested on Vitamins and their deficiencies!
Vitamin C def = Scurvy = bleeding gums
Vitamin A def = night vision changes
Vitamin D def = rickets in kids; osteomalacia in adults
Vitamin B6 and B12 def = marcocytic anemia; methylmalonic acid increased in vitamin B12 def
Fat soluble vitamins = A, D, E, K = occurs with pancreatic insufficiency causing steatorrhea!
Vitamin K def = clotting disorder -> liver cant produce clotting factors: II, XII, IX, X - I remember as 1972 (10 - 9 - 7 - 2) AND protein C and S
Iron deficiency = microcytic hypochromic anemia + restless leg syndrome
Some med school factoids for you <3
Rhys would be very impressed with you for trying!!!
7 notes
·
View notes
Text
Malabsorption Syndrome Market To Grow At 6.8% Owing To Rising Prevalence Of Celiac Disease

The malabsorption syndrome market is comprised of various treatment products offered for celiac disease, Crohn's disease, short bowel syndrome, radiation injury, pancreatic insufficiency, bariatric surgeries, and liver disease. Malabsorption syndrome occurs when the small intestine is unable to absorb enough nutrients, vitamins, and minerals from food due to various diseases and conditions affecting the gastrointestinal tract. Treatments include enzyme replacement therapy, vitamin and mineral supplements, prebiotics and probiotics, dietary changes, and medication.
The Malabsorption Syndrome Market is estimated to be valued at US$ 3.42 Bn in 2024 and is expected to exhibit a CAGR of 6.8% over the forecast period 2024-2031.
Key Takeaways
Key players operating in the malabsorption syndrome market are AbbVie Inc., Immunogen X, LLC, Astra Zeneca, ImmusanT, Inc.,Ritter Pharmaceuticals. AbbVie Inc. holds a major share in the market and offers treatments such as Humira and Stelara.
The growing prevalence of diseases causing malabsorption syndrome such as celiac disease and crohn's disease is a major factor driving the demand for malabsorption treatments. According to statistics, around 1% of the global population suffers from celiac disease.
Technological advancements have led to the development of targeted therapies, diagnostic tests, and personalized treatments. Companies are investing heavily in R&D to develop new drugs, enzymes, vaccines, and gene therapies to better manage malabsorption.
Market Trends
- Increasing adoption of enzyme replacement therapy: Enzyme supplements containing pancreatin, pancrelipase, etc. help breakdown proteins, carbs, and fats which people with pancreatic insufficiency cannot breakdown. Their use is steadily rising.
- Growth in demand for nutritional supplements: Products containing vitamins A, D, E, K, B12, iron, calcium, magnesium are widely used to meet nutritional needs of people with malabsorption. Tailored supplements address individual deficiencies.
Market Opportunities
- Developing new drug formulations: R&D in advanced drug delivery systems like nanoparticles, microspheres can offer improved treatment adherence and outcomes.
- Expanding into emerging markets: While North America and Europe dominate currently, focus on Asia Pacific and Latin America can tap high patient population and drive future growth.
Impact Of COVID-19 On Malabsorption Syndrome Market Growth
The COVID-19 pandemic has significantly impacted the growth trajectory of the malabsorption syndrome market. During the initial outbreak and peak of infections across regions, limited resources and concentrated efforts of healthcare systems towards COVID affected patients negatively impacted the diagnosis and management of malabsorption syndrome patients. Restrictions on non-essential medical visits and hospitalizations led to delays in consultations and treatments. However, with increasing availability of teleconsultation facilities, the impact was mitigated to some extent for stable patients requiring routine follow-ups.
As the pandemic spread, supply chain disruptions affected the production and distribution of important drugs and nutritional supplements used in malabsorption syndrome management. Shortage of raw materials and logistical challenges impacted the consistent supply to patients. This imbalance in demand-supply equilibrium affected patient compliance and clinical outcomes to a certain degree.
As vaccination drives progress and cases decline in many regions globally, healthcare services are rebuilding capacities. Patients are gradually resuming visits for malabsorption syndrome management. Drugmakers too have overcome early hurdles and restored production levels. With accelerated research on COVID therapies, the sector is expected to bounce back faster than anticipated earlier. Telehealth is also expected to continue complementing in-person care delivery, especially for rural populations.
Geographical Regions With Highest Malabsorption Syndrome Market Value
North America dominates the Malabsorption Syndrome Market in terms of value, given the high diagnosis and treatment rates supported by good healthcare infrastructure and reimbursement scenario. The United States accounts for the major share within the region owing to presence of key market players and large patient pool affected by different types of malabsorption disorders like celiac disease and tropical sprue.
Europe follows North America with a significant market presence led by countries such as Germany, United Kingdom and France where awareness levels are rising. Growing geriatric population prone to gastrointestinal issues also supports the regional market growth. However, Asia Pacific is emerging as the fastest growing regional market backed by improving access to healthcare in India and China along with rising incidences of intestinal diseases and gut dysbiosis ingeneral population.
Fastest Growing Region For Malabsorption Syndrome Market
Asia Pacific region holds immense opportunities for malabsorption syndrome market players and is expected to witness the fastest value growth during the forecast period. Factors such as increasing healthcare spending per capita, government focus on strengthening public healthcare through various programs, rising medical tourism and presence of contract manufacturing bases are attracting several global brands to expand in Asia Pacific markets.
At the same time, prevalence of tropical enteropathies, changes in dietary patterns exposing population to maldigestion and malabsorption risks, wider reach of new diagnostic technologies are enhancing the disease detection rates. With economic development, there is growing awareness among patients regarding available treatment options. This is supporting the demand for innovative drugs and supplemental nutrition products in Asia Pacific's malabsorption syndrome market.
Get more insights on this topic: https://www.trendingwebwire.com/malabsorption-syndrome-market-is-estimated-to-witness-high-growth-owing-to-advancements-in-immuno-absorption-therapies/
Author Bio:
Money Singh is a seasoned content writer with over four years of experience in the market research sector. Her expertise spans various industries, including food and beverages, biotechnology, chemical and materials, defense and aerospace, consumer goods, etc. (https://www.linkedin.com/in/money-singh-590844163 )
What Are The Key Data Covered In This Malabsorption Syndrome Market Report?
:- Market CAGR throughout the predicted period
:- Comprehensive information on the aspects that will drive the Malabsorption Syndrome Market's growth between 2024 and 2031.
:- Accurate calculation of the size of the Malabsorption Syndrome Market and its contribution to the market, with emphasis on the parent market
:- Realistic forecasts of future trends and changes in consumer behaviour
:- Malabsorption Syndrome Market Industry Growth in North America, APAC, Europe, South America, the Middle East, and Africa
:- A complete examination of the market's competitive landscape, as well as extensive information on vendors
:- Detailed examination of the factors that will impede the expansion of Malabsorption Syndrome Market vendors
FAQ’s
Q.1 What are the main factors influencing the Malabsorption Syndrome Market?
Q.2 Which companies are the major sources in this industry?
Q.3 What are the market’s opportunities, risks, and general structure?
Q.4 Which of the top Malabsorption Syndrome Market companies compare in terms of sales, revenue, and prices?
Q.5 Which businesses serve as the Malabsorption Syndrome Market’s distributors, traders, and dealers?
Q.6 How are market types and applications and deals, revenue, and value explored?
Q.7 What does a business area’s assessment of agreements, income, and value implicate?
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it
#Malabsorption Syndrome Market Trend#Malabsorption Syndrome Market Size#Malabsorption Syndrome Market Information#Malabsorption Syndrome Market Analysis#Malabsorption Syndrome Market Demand
0 notes
Text
Understanding Parenteral Nutrition (TPN): Components, Delivery Methods, and Applications
Definition and Purpose of Parenteral Nutrition
Parenteral nutrition, also known as total parenteral nutrition or TPN, refers to the delivery of nutrients directly into the bloodstream, bypassing the usual process of eating and digestion. It is used for patients who are unable to digest, absorb, or metabolize nutrients from foods or dietary supplements due to conditions like short bowel syndrome, impaired intestinal function, or other severe gastrointestinal issues. The goal of TPN is to provide patients with essential proteins, carbohydrates, fats, vitamins, minerals, and other nutrients necessary for growth and energy when oral or enteral feeding is not feasible or sufficient.
Components of Parenteral Nutrition
A typical TPN solution contains macronutrients like glucose, amino acids, fatty acids or lipid emulsions, and added micronutrients like vitamins, minerals, and trace elements. Glucose provides the main source of carbohydrate calories while amino acids, primarily from soy, dairy, or corn proteins, serve as the building blocks for the synthesis of new proteins and tissues in the body. Fatty acids provide concentrated calories to increase energy levels. Added vitamins and minerals ensure patients receive adequate levels of essential micronutrients their body needs but cannot obtain from the gut.Some solutions may also include supplementary hormones, fiber, or additional components depending on individual patient needs and medical conditions.
Delivery of Parenteral Nutrition
TPN is delivered through a central or peripheral venous access catheter, usually placed in large veins in the neck, chest, or groin. The most common type is a peripherally inserted central catheter (PICC line) which can remain in place for weeks or months to facilitate repeated TPN infusions. Parenteral Nutrition total nutrient fluids are administered continuously over 10-24 hours via an infusion pump to mimic physiological feeding and allow for proper digestion and absorption. Close monitoring under medical supervision is required as incorrect rates or mixtures can cause serious metabolic complications.
Conditions Treated with Parenteral Nutrition
Some of the most common clinical conditions requiring long-term TPN support include:
- Short bowel syndrome: When a large portion of the small intestine is surgically removed due to diseases like Crohn's, cancer, or vascular thrombosis.
- Bowel obstructions or fistulas: Blockages or abnormal connections between bowels that prevent normal nutrient passage and absorption.
- Motility disorders: Problems like intestinal neuronal dysplasia that affect proper bowel movement and emptying.
- Severe pancreatitis: Inflammation or damage to the pancreas gland that impairs digestive enzyme production.
- Radiation enteritis: Damage to the bowel lining from radiation therapy that causes severe malabsorption.
- Multiple organ failure: When several vital organs like liver or kidneys stop functioning temporarily or permanently.
- Gastrointestinal anomalies: Rare congenital defects in newborns that require bowel surgery or have abnormal gut structure.
Get more insights on Parenteral Nutrition
Get More Insights—Access the Report in the Language that Resonates with You
French
German
Italian
Russian
Japanese
Chinese
Korean
Portuguese
About Author:
Ravina Pandya, Content Writer, has a strong foothold in the market research industry. She specializes in writing well-researched articles from different industries, including food and beverages, information and technology, healthcare, chemical and materials, etc. (https://www.linkedin.com/in/ravina-pandya-1a3984191)
#Parenteral Nutrition#Intravenous Nutrition#TPN#Nutritional Support#IV Nutrition#Nutrient Delivery#Clinical Nutrition#Enteral vs. Parenteral Nutrition#Nutritional Therapy#Hospital Nutrition#Metabolic Support#Nutrient Infusion
0 notes
Text
Understanding Medical Conditions That Impact THC Processing in Edible Cannabis

Cannabis has gained popularity for its medicinal and recreational use, with various consumption methods available, including edibles. However, not everyone responds to cannabis in the same way, and certain medical conditions can affect how the body processes tetrahydrocannabinol (THC), the psychoactive compound in cannabis. In this article, we will explore medical conditions that may make it challenging for individuals to process THC when consuming cannabis in edible form.
Liver Enzyme Variations:
One crucial factor in THC metabolism is the liver’s involvement, where enzymes break down THC into its active and inactive metabolites. Individuals with variations in liver enzymes, such as those with liver diseases or genetic differences, may experience altered THC metabolism. This can result in unpredictable and potentially stronger effects when consuming cannabis edibles.
Gastrointestinal Disorders:
People with gastrointestinal disorders, such as Crohn’s disease or irritable bowel syndrome (IBS), may face challenges in absorbing THC through the digestive system. These conditions can affect the absorption rate, potentially leading to delayed onset or variable intensity of THC effects. Individuals with gastrointestinal disorders should approach edible cannabis cautiously and monitor their responses.
Pancreatic Issues:
The pancreas plays a role in regulating insulin and releasing digestive enzymes. Conditions affecting the pancreas, such as pancreatitis or pancreatic cancer, may impact the body’s ability to process THC efficiently. Edible cannabis, which undergoes digestion in the pancreas, might have different effects on individuals with pancreatic issues compared to those without.
Metabolic Disorders:
Metabolic disorders, including metabolic syndrome and diabetes, can influence the way the body metabolizes various substances, including THC. These conditions may lead to changes in the distribution and elimination of THC, potentially affecting the duration and intensity of its effects when consumed in edible form. Individuals with metabolic disorders should be aware of potential variations in their response to cannabis.
Medication Interactions:
Certain medications can interact with THC metabolism, affecting how the body processes and eliminates cannabis compounds. Individuals taking medications that impact liver enzymes, such as certain antibiotics or antifungal drugs, may experience altered THC effects when consuming edibles. It is crucial for individuals on medications to consult with healthcare professionals before incorporating cannabis into their routine.
While cannabis edibles offer an alternative consumption method for individuals seeking the therapeutic benefits of THC, it is essential to recognize that various medical conditions can influence how the body processes and responds to these compounds. Individuals with liver enzyme variations, gastrointestinal disorders, pancreatic issues, metabolic disorders, or those taking specific medications should exercise caution when consuming cannabis in edible form. Consulting with healthcare professionals and starting with low doses can help mitigate potential risks and ensure a more controlled and positive experience with edible cannabis.
ORIGINALLY FOUND ON-
Source: Shangri-La Dispensaries(https://shangriladispensaries.com/understanding-medical-conditions-that-impact-thc-processing-in-edible-cannabis/)

Our Dispensaries:
Missouri ------ Ohio ------ Connecticut ------ Illinois
1 note
·
View note
Text
Thoughts from Gastroenterologists on the Science: The basis of Digestive Health
Introduction:
Although digestive health is essential to overall wellbeing, it sometimes goes unnoticed until issues start to occur. Understanding the complex processes involved in digestion and absorption can help us make important improvements to our digestive systems and general health. These processes are essential to preserving health. This article explores the science of digestive health and provides tips from gastroenterologists on how to maintain the best possible health for your digestive system.
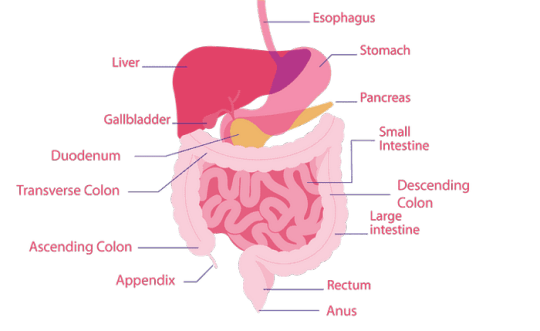
The Digestive System: A Complex Web
The digestive system is a multi-organ system with many moving parts and sophisticated functions. Here is a quick rundown of how it functions:
Ingestion and Mechanical Breakdown: Food is mechanically broken down by chewing and combined with saliva in the mouth, where digestion starts. Enzymes such as amylase found in saliva begin the breakdown of carbohydrates.
Chemical Breakdown: Food passes down the esophagus through a sequence of wave-like muscular contractions called peristalsis after it has been swallowed. When it gets to the stomach, dangerous germs are killed and proteins are further broken down by gastric acids and enzymes. The small intestine receives this combination, also referred to as chyme.
Nutrient Absorption: The main location for nutrient absorption is the small intestine. Digestion of lipids, proteins, and carbohydrates is aided by pancreatic enzymes and liver bile. Nutrients are absorbed into the bloodstream by the villi and microvilli that coat the lining of the small intestine.
Waste Formation: Any indigestible material that is still present travels to the large intestine, where it is absorbed together with water and electrolytes, eventually becoming feces. Some of the residual materials are fermented by beneficial bacteria in the colon, which improves general health.
Views from Gastroenterologists
Specialists in digestive health, gastroenterologists can provide valuable insights into how to keep the digestive system in good working order. Several important lessons from their experience are as follows:
The community of trillions of bacteria that reside in the digestive tract is known as the gut microbiome, and it is essential to immunological response, mental health, and digestion. A balanced microbiome is important, according to gastroenterologists. A balanced microbiome can be supported by a varied diet full of fruits, vegetables, fiber, and fermented foods. On the other hand, a diet rich in processed foods and overuse of antibiotics can upset the delicate balance of microorganisms.
Dietary Influence: Your diet has a big impact on the health of your digestive system. A high-fiber diet is advised by gastroenterologists to support regular digestion and ward off constipation. Foods that support intestinal health include veggies, legumes, and nutritious grains. Eating a range of fruits and vegetables also gives you vital vitamins and minerals that help your digestive system work better overall.
Hydration: Drinking enough water is essential for good gut health. Water facilitates food passage through the digestive tract and aids in digestion. Gastroenterologists recommend consuming enough water throughout the day and modifying consumption according to variables such as temperature and degree of physical activity.
Regular exercise is important because it helps maintain a healthy weight and stimulates the digestive system, both of which can help prevent illnesses like GERD and IBS (gastric reflux disorder). Frequent exercise helps reduce constipation symptoms and encourages regular bowel movements.
Handling Stress: Stress has a big effect on the health of the digestive system. Stress can make disorders like GERD and IBS worse by altering gastrointestinal motility and producing more acid, according to gastroenterologists. Stress reduction methods, mindfulness, and meditation are a few practices that can lessen these impacts.
The Treatment of Common Digestive Disorders
Many digestive diseases are often treated by gastroenterologists. A synopsis of several prevalent ailments and how they are treated is provided below:
Gastric reflux disease, also known as GERD, is characterized by regurgitation and heartburn brought on by stomach acid that frequently runs back into the esophagus. A basic approach to management is to make lifestyle adjustments such eating smaller meals, delaying sleeping right after meals, and avoiding trigger foods (such as fatty or spicy foods). Proton pump inhibitors (PPIs), among other medications, are prescribed to lower stomach acid.
Inflammatory Bowel Disease (IBD): This category comprises diseases that cause persistent inflammation of the digestive tract, such as ulcerative colitis and Crohn's disease. Anti-inflammatory drugs, immunosuppressants, and occasionally surgery are used in treatment. For the purpose of treating symptoms and avoiding malnutrition, dietary adjustments and nutritional support are also crucial.
Gluten consumption causes the autoimmune disease celiac disease, which damages the small intestine. Strict gluten-free diet followed for the duration of the treatment helps heal the intestinal lining and reduce symptoms.
Peptic Ulcer Disease: Peptic ulcers are sores that develop on the lining of the stomach or small intestine due to excess stomach acid or infection with Helicobacter pylori. Treatment typically involves medications to reduce acid production and, if necessary, antibiotics to clear the infection.
The Future for Digestive Health
The future of digestive health is constantly being shaped by developments in gastroenterology. We are approaching innovations like personalized medicine, in which a patient's regimen is customized based on their microbiome and genetic profile. Furthermore, current studies on the gut-brain axis, which investigates the communication between the stomach and the brain, may offer fresh perspectives on treating illnesses like anxiety and depression by promoting digestive health.
In Conclusion
Maintaining general health requires an understanding of the science underlying gut health. A balanced diet, adequate hydration, frequent exercise, and stress reduction are all crucial for maintaining a healthy digestive system, according to gastroenterologists' insights. You can take proactive measures to ensure your gut health is optimal, which will improve your general health and quality of life, by keeping an eye on these aspects and getting medical guidance when needed.
0 notes
Text
What are the Process and Functions of the Human Digestive System?
The human alimentary canal is one of the most clearly defined systems in the body. It consists of a long passageway called the digestive tract and other associated glands. This digestive tract is also called the gastrointestinal (GI) tract. The organs of the digestive system contain the pharynx, esophagus, stomach, and small and large intestines. The mouth is also an essential aspect of the digestive system and is the first of the human digestive system parts. The liver, pancreas, and gallbladder are also part of the gastrointestinal tract.
Food enters through the mouth and passes through the anus through the various organs of the digestive system. It is important to understand the digestive system’s function as it breaks down the consumed food into various nutrients that are required by the body for energy, growth, and cell repair. Food eventually gets converted into carbohydrates, proteins, fats, and vitamins which in turn aids the body to function at its optimal best.
The Structure of the human digestive system
The human digestive system is an intricate network of organs and glands working together in a harmonious tandem to facilitate the journey of food and drink through the body. Understanding the human digestive system function and structure is important to appreciate the beauty of this biological marvel.
The Process of the human digestive system
The functioning of the human digestive system involves the propulsion of food along the gastrointestinal (GI) tract. The process of digestion initiates in the mouth through the act of chewing and culminates in the small intestine. Throughout the journey along the GI tract, food undergoes mixing with digestive juices, leading to the breakdown of large food molecules into smaller ones. Subsequently, the body absorbs these diminished molecules through the walls of the small intestine, facilitating their entry into the bloodstream. The bloodstream then transports these nutrients to various parts of the body. Waste materials from the digestion process travel through the large intestine and are expelled from the body as solid waste known as stool.
Functions of the human digestive system
Understanding the multifaceted functions of the digestive system is crucial for appreciating its role in maintaining overall health and well-being.
Understanding each stage of digestion – from ingestion to elimination – is crucial for comprehending the intricate processes that sustain human life and well-being. These processes work in tandem to ensure the body receives essential nutrients while efficiently eliminating waste.
Ingestion
The process of taking in food into the body initiates the digestive cascade.
Mechanical Breakdown: Ingestion involves the mechanical breakdown of food by chewing, facilitated by the teeth. This initial step increases the surface area of the food particles, making it easier for enzymes to act on them during later stages of digestion.
Saliva, produced by salivary glands, contains enzymes like amylase that initiate the chemical breakdown of carbohydrates in the mouth. This process transforms complex carbohydrates into simpler sugars. After a mechanical and chemical breakdown in the mouth, the partially digested food is formed into a bolus and swallowed. The swallowing reflex is a coordinated muscular action that propels the bolus down the esophagus.
Digestion
Mechanical and chemical breakdown of food into smaller, absorbable components. Digestion is the process of breaking down ingested food into simpler, absorbable substances.
In the stomach, gastric juices containing hydrochloric acid and pepsin help break down proteins into smaller peptides. The stomach also mechanically churns the food, creating a semi-liquid mixture known as chyme. The small intestine is the primary site of digestion. Pancreatic enzymes (lipase, protease, and amylase) and bile from the liver further break down fats, proteins, and carbohydrates, respectively. Digestion results in the breakdown of complex molecules into simpler forms. Proteins are broken into amino acids, fats into fatty acids and glycerol, and carbohydrates into simple sugars.
Absorption
The absorption of nutrients, such as carbohydrates, proteins, fats, vitamins, and minerals, into the bloodstream for distribution to cells.The majority of nutrient absorption occurs in the small intestine. The inner surface of the small intestine is lined with villi, tiny finger-like projections that increase the surface area for absorption. Nutrients, including amino acids, fatty acids, glucose, vitamins, and minerals, are transported across the intestinal wall into the bloodstream. Some fats and fat-soluble vitamins are absorbed into the lymphatic system before entering the bloodstream.
Assimilation
The utilization of absorbed nutrients by cells for various physiological functions, including energy production and cellular maintenance.
After absorption, nutrients are transported to cells throughout the body. Amino acids are used for protein synthesis, glucose for energy production, and fats for various cellular functions. Different nutrients play specific roles in various tissues and organs. For example, calcium is crucial for bone health, iron for oxygen transport in blood, and vitamins for various biochemical processes.
Elimination
The removal of indigestible waste material as feces, ensures the body’s efficient waste management.
In the large intestine, water is absorbed from the remaining chyme, forming solid feces. Feces are stored in the rectum until they reach a sufficient volume, triggering the urge to defecate. The expulsion of feces through the anus completes the process of elimination, ensuring the removal of indigestible waste from the body.
Safeguarding a robust and well-functioning digestive system is of utmost significance for one’s comprehensive state of well-being. The achievement of optimal digestive health involves a combination of various factors, including adequate hydration, a judiciously balanced diet with a focus on fiber-rich foods, and the incorporation of regular physical activity into one’s lifestyle. These elements collectively contribute to the seamless operation of the digestive processes, promoting not only the efficient breakdown and absorption of nutrients but also fostering overall bodily health.
Knowledge of the functions of each component within the digestive system empowers individuals to make informed choices regarding their dietary and lifestyle habits. Awareness of how the mouth, stomach, small intestine, and large intestine work in harmony allows individuals to appreciate the importance of nutrient breakdown, absorption, and waste elimination. This understanding fosters a mindful approach to eating and lifestyle choices that positively impact digestive health.
By intertwining these elements – hydration, a fiber-rich diet, regular physical activity, and a comprehensive understanding of digestive functions – individuals can proactively contribute to maintaining a healthy digestive system. This, in turn, ensures the efficient processing of nutrients for bodily functions and plays a pivotal role in supporting overall vitality and wellness.llness. If you want to try our online tuition, you can enroll with our exclusive FREE DEMO session with Tutoroot from an expert faculty. Click here to BOOK FREE DEMO.
0 notes
Text
The Science Behind the Health Benefits of Indian Spices

Indian food is well known worldwide for its robust and nuanced flavors. A variety of spices that have been prized for millennia for their culinary skills and extraordinary health benefits are at the core of these flavor experiences. Let’s know some benefits of Indian spices.
Turmeric: The Golden Elixir of Nature
Turmeric powder sometimes known as the "golden spice," has attracted considerable scientific interest. Its vivid color is a reflection of the powerful chemical curcumin, which has shown strong antioxidant and anti-inflammatory effects. Due to these qualities, turmeric is a promising addition to foods that boost immune system function, promote joint health, and may lower the risk of chronic illnesses, including cancer and heart disease.
2. Cumin: An Intestinal Powerhouse
An essential ingredient in Indian cooking, cumin is prized for its hearty, earthy taste. Beyond its use in cooking, cumin has several health advantages. It helps digestion by boosting the pancreatic enzymes, allowing food to be digested more easily. The antibacterial properties of cumin also support general health and gut wellness.
3. The Natural Cooling Agent, Coriander
In Indian cooking, coriander leaves and seeds are fundamental ingredients. Coriander is well known for its calming effects and is frequently used to counterbalance the spiciness of other spices. By reducing bloating and gas, it aids in digestion. Additionally, coriander is a helpful complement to a balanced diet because it has demonstrated promise in controlling blood sugar levels.
4. The Queen of Spices is cardamom.
Cardamom, sometimes referred to as the "queen of spices," is prized for its fragrant, sweet taste. Cardamom has been used traditionally to treat respiratory problems, digestive pain, and dental health. Its diuretic actions can promote heart health, while its antioxidant qualities fight oxidative stress.
The diverse range of tastes and health advantages present in Indian cooking are perfectly embodied by these three spices. Including them in everyday meals helps support a healthy, colorful palette and general wellbeing.
5. Cloves: The Natural Protector of Oral Health
Cloves are little, fragrant flower buds that have a significant impact on dental health. For millennia, people have used their antimicrobial and antiseptic qualities to treat gum disease and toothaches. Cloves are high in antioxidants, which promote liver health and general wellbeing in addition to dental health.
6. Mustard Seeds: Little Giants
Be not deceived by their diminutive size; mustard seeds are nutrient-dense superfoods. Rich in omega-3 fatty acids, magnesium, and selenium, they support heart health. They are advantageous in the treatment of respiratory discomfort and muscle soreness due to their anti-inflammatory qualities.
7. Fenugreek: An Adaptable Health Benefit
A multipurpose plant that may be used in savory and sweet recipes, fenugreek has many health advantages. It is a useful tool for managing diabetes because of its capacity to control blood sugar levels. Fenugreek seeds are high in antioxidants and fiber, and it also lowers inflammation and promotes digestive health.
8. The spice of life (and health), cinnamon
Loved for its cozy, sugary taste, cinnamon is also a superfood. It has a well-established history of controlling blood sugar levels and improving insulin sensitivity. Cinnamon is a powerful anti-inflammatory and antioxidant that promotes general health and well-being.
These four spices are good examples of the amazing health benefits that can be found in Indian food. Including them in your diet can be a tasty method to promote general wellbeing.
9. Spices' Underappreciated Hero: Black Pepper
Black pepper is the hidden star of the spice world, frequently overshadowed by its more showy counterparts. Justly dubbed the "king of spices," it is a mainstay in many cuisines across the globe. Black pepper contains a chemical called piperine, which is a potent enhancer that increases the absorption of essential nutrients like turmeric curcumin. Beyond its culinary abilities, black pepper has a wealth of health advantages, including antibacterial, anti-inflammatory, and antioxidant qualities.
A Wellness Path Infused with Spice
A trip through the world of Indian spices offers a mosaic of tastes and wellbeing advantages. These spices provide a comprehensive approach to well-being, from the digestive abilities of cumin and coriander to the anti-inflammatory qualities of turmeric and ginger. The wisdom of including these natural miracles in our diets is ageless, even as scientific research continues to unlock their complexity.Accepting the rich history of Indian spices opens doors to a tasty and healthy world.
#indian spice mixes#indian spices online#indian spice#indian spices online australia#indian spices in australia#indian spices in new zealand
0 notes
Text
Pancreatic Cancer: Symptoms, Causes, Diagnosis, Treatment & More

Pancreatic cancer cases, although not very common, still persist in India. According to recent surveys, there are approximately 0.5–2.4 cases per 100,000 men and around 0.2–1.8 cases of pancreatic cancer for every 100,000 women. To effectively combat this issue, early detection is crucial. We’re here to guide you through understanding, recognizing, and managing this serious health concern. Read on to stay informed about its types, stages, symptoms, and prevention.
What is Pancreatic Cancer?

Types of Pancreatic Cancer
Pancreatic cancer can be classified into several types:
Adenocarcinoma: The most common type, developing in the cells that line the pancreatic duct. Early detection is difficult, and it tends to grow rapidly, making timely intervention crucial.
Neuroendocrine Tumors (NETs): Less common, these tumors can either produce hormones (functional) or not (non-functional). They typically grow slower than adenocarcinomas.
Cystic Lesions: Fluid-filled sacs in the pancreas, which are mostly harmless but some can turn cancerous. Regular check-ups are essential to monitor their development.
Acinar Cell Carcinoma: A rare type, starting in the cells responsible for producing digestive enzymes. Its behavior differs from the more common adenocarcinoma.
Stages of Pancreatic Cancer
Stage I: Cancer is confined to the pancreas. Surgery is often an option for effective removal.
Stage II: Cancer may reach nearby tissues but not major blood vessels. Treatment options like surgery are considered effective.
Stage III: Cancer has progressed to major blood vessels. A comprehensive approach with surgery, chemotherapy, and radiation may be recommended.
Stage IV: In this advanced stage, cancer has spread to distant organs. The focus shifts to improving the patient’s quality of life and managing symptoms.
Symptoms of Pancreatic Cancer
Digestive Issues: Changes in bowel habits, such as light-colored stools or dark urine.
Jaundice: Yellowing of the skin and eyes due to bile duct blockage.
Unintended Weight Loss: Losing weight without trying.
Abdominal Pain: Persistent pain in the abdomen or back.
Loss of Appetite: A decrease in the desire to eat.
New-Onset Diabetes: Development of diabetes without a clear explanation.
Fatigue: Feeling unusually tired or weak.
These symptoms, especially when persistent, should prompt consultation with a healthcare professional for further evaluation and diagnosis. Early detection is crucial for effective management.
Causes of Pancreatic Cancer
Smoking
Family History of pancreatic cancer
Chronic Pancreatitis: Long-term inflammation of the pancreas
Age: More common in older adults
Overweight or Obesity
Uncontrolled Diabetes
Dietary Factors: High in red and processed meats
Occupational Exposure: Chemicals and petroleum industries
Complications Associated with Pancreatic Cancer
As pancreatic cancer grows, it can cause complications such as:
Spread to Nearby Organs: Complicating treatment.
Blockage of the Digestive System: Affecting nutrient absorption.
Jaundice: Yellowing of skin due to bile duct blockage.
Blood Vessel Involvement: Posing additional challenges for treatment.
Diabetes Development: Leading to new-onset diabetes.
Pain and Discomfort: Persistent abdominal pain impacting quality of life.
Diagnostic Tests for Pancreatic Cancer
Imaging Tests: CT Scan, MRI, Ultrasound
Blood Tests: CA 19–9, Liver Function
Biopsy: Fine Needle Aspiration (FNA)
Endoscopic Tests: EUS, ERCP
Laparoscopy: Direct Visualization
These tests aid in diagnosing pancreatic cancer and guiding appropriate treatment approaches. If symptoms arise, prompt medical attention ensures timely intervention.
Prevention of Pancreatic Cancer
Prevention is better than cure. Follow these tips:
Quit Smoking
Maintain a Healthy Weight
Eat a Balanced Diet
Limit Alcohol Consumption
Stay Active
Manage Diabetes
Know Your Family History
Protect Against Occupational Risks
Consider Genetic Counseling in cases of a family history of pancreatic cancer
Treatment of Pancreatic Cancer
Diagnosis: Initial tests like CT scans and biopsies confirm the presence of pancreatic cancer.
Surgery: Depending on the stage, surgical procedures may remove the pancreatic cancer tumor, partially or entirely.
Chemotherapy: Powerful drugs eliminate cancer cells, administered before or after surgery.
Radiation Therapy: High-energy rays target and destroy cancer cells.
Targeted Therapy: Medications specifically target molecules involved in cancer growth.
Immunotherapy: Enhances the body’s immune system to combat cancer cells.
Palliative Care: Focuses on alleviating symptoms and improving the overall quality of life.
Clinical Trials: Participation in research studies exploring new treatments.
Conclusion
Recognizing symptoms, staying healthy, and seeking early treatment are key steps in effectively fighting pancreatic cancer. Personalized approaches like surgery and innovative treatments aim for better outcomes. Palliative care and keeping patients motivated are effective ways to enhance the quality of life. Making informed choices and staying proactive are vital in the fight against pancreatic cancer. For expert care and comprehensive treatment options, consider Arvachin Hospital, known for its dedication to patient well-being.
0 notes
Text
Zieve’s syndrome is a complication of chronically high alcohol consumption and often develops after periods of drinking a lot of alcohol in a short period of time. It’s characterized by three signs.
Zieve’s syndrome was first described by Dr. Leslie Zieve in the 1950s. It’s a collection of three signs that develop in people with alcohol-induced liver injuries. These signs include:
jaundice
hemolytic anemia (a low red blood cell count)
hyperlipidemia (high levels of fat in your blood)
People with Zieve’s syndrome often have an improvement in their symptoms after completely stopping their alcohol consumption.
Let’s look at Zieve’s syndrome in more detail, including what causes it, symptoms, and treatments.
What causes Zieve’s syndrome?
A syndrome is a collection of signs and symptoms that commonly occur together. The development of Zieve’s syndrome is associated with alcohol-induced liver injury and cirrhosis. It often develops after periods of heavy drinking. Cirrhosis is scarring of your liver that prevents it from functioning properly.
It’s not clear why hemolytic anemia and hyperlipidemia develop in people with Zieve’s syndrome.
Some research suggests that changes to the membrane of your red blood cells due to vitamin E and polyunsaturated fatty acid deficiency may contribute. Additionally, alcohol breaks down in your liver into a chemical called acetaldehyde. Acetaldehyde may inhibit red blood cell enzymes and make your blood cells more susceptible to injury.
Hyperlipidemia may occur due to fat molecules moving from your liver to your bloodstream.
Zieve’s syndrome risk factors
Zieve’s syndrome is associated with alcohol-related liver disease. Risk factors for alcohol-related liver disease include:
consuming more than 14 drinks per week for males or having more than 4 drinks at a time
consuming more than 7 drinks per week for females and people over 65, or having more than 3 drinks at a time
Daily consumption of 30–50 grams per day for over 5 years can lead to alcohol-related liver disease. One standard drink contains roughly 14 grams of alcohol.
Cirrhosis occurs in 30% of people with a long history of consuming more than 40 grams of alcohol per day.
Zieve’s syndrome symptoms
Zieve’s syndrome is characterized by:
hyperlipidemia
jaundice
hemolytic anemia
People with Zieve’s syndrome may initially have symptoms such as:
abdominal pain
nausea
vomiting
malaise
low grade fever
Hyperlipidemia often doesn’t cause noticeable symptoms.
Jaundice is characterized by:
yellow skin and eye whites
dark or brown urine
pale or clay-colored stools
itchy skin
Hemolytic anemia might cause:
paleness
fever
weakness
dizziness
confusion
spleen or liver enlargement
increased heart rate
Most cases are also associated with acute pancreatitis, which can cause:
sudden and severe pain in your abdomen
fever
jaundice
diarrhea
Potential complications of Zieve’s syndrome
Developing Zieve’s syndrome is a potential warning sign that you’re at risk for severe cirrhosis and liver disease. Cirrhosis can lead to liver failure, which is when your liver can no longer perform its normal functions adequately.
A liver transplant is often the only cure for chronic liver failure.
When to contact a doctor
It’s important to contact a healthcare professional right away if you develop signs of jaundice like yellowing of your skin and eyes. Jaundice is often a sign of liver disease.
Other signs that should prompt an immediate visit to a doctor include:
unexplained fatigue
abdominal pain
atypical paleness
itchy skin
Diagnosing Zieve’s syndrome
More than 200 cases of Zieve’s syndrome have been reported since it was first described in the 1950s. Most of these cases have been initially misdiagnosed. Its true prevalence isn’t known.
Doctors can usually establish a diagnosis with:
a review of your personal and family medical history
a review of your symptoms
the results of a physical exam
blood tests to look for elevated markers in your blood, such as:
bilirubin
alkaline phosphatase
gamma-glutamyl
lactate dehydrogenase
reticulocytes (immature red blood cells)
A bone marrow biopsy may be performed in some cases.
Zieve’s syndrome treatment
Zieve’s syndrome is primarily treated by completely stopping alcohol consumption.
When Dr. Zieve first described the condition in the 1950s, he noticed people had spontaneous resolution of their symptoms when they quit alcohol.
You may also receive repeated blood transfusions to help increase your red blood cell count.
Plasmapheresis may be considered if you have a high chance of intracerebral hemorrhage and a history of pancreatitis. This procedure involves removing plasma from your blood.
Living with Zieve’s syndrome
Most people with Zieve’s syndrome seem to recover completely within 4–6 weeks if they completely stop drinking alcohol. It’s thought that quitting alcohol allows fat to move from your blood back to your liver and reduces your red blood cells’ susceptibility to injury.
If you don’t quit drinking, you may have a chance of severe liver damage that can be life threatening. Quitting is often difficult, but a doctor can help build a cessation plan that works for you.
Can you prevent Zieve’s syndrome?
The best way to prevent Zieve’s syndrome is by consuming alcohol only in moderation and avoiding overconsumption.
To reduce the risk of alcohol-related disease, the Centers for Disease Control and Prevention (CDC) recommend that on days you consume alcohol:
males consume no more than 2 drinks per day
females consume no more than 1 drink per day
They also don’t recommend starting to consume alcohol if you don’t currently drink. Their stance is that drinking less is always better for your health than drinking more.
Learn more about how to stop drinking.
Takeaway
Zieve’s syndrome is characterized by three signs: jaundice, hemolytic anemia, and hyperlipemia. It usually improves once you quit drinking alcohol. Continuing to drink may put you at risk of severe liver disease that can be life threatening.
0 notes
Text
Your Digestive Health Ally: A Comprehensive Guide to Gastroenterologists
The digestive system, a complex network of organs from your mouth to your rectum, plays a crucial role in processing food, absorbing nutrients, and eliminating waste. When things go wrong in this intricate system, it can lead to a range of uncomfortable and potentially debilitating conditions. This is where gastroenterologists, the guardians of your digestive health, come in.
This blog post delves into the world of gastroenterology, exploring what a gastroenterologist does, the conditions they treat, diagnostic procedures, treatment options, and how to find a Best Gastroenterologist Dubai.
Who is a Gastroenterologist?
A gastroenterologist is a specialized physician with expertise in diagnosing and treating diseases of the digestive system. This includes organs like the oesophagus, stomach, small intestine, large intestine (colon), rectum, liver, pancreas, and gallbladder. After completing medical school, gastroenterologists undergo several years of additional training, including an internal medicine residency and a gastroenterology fellowship.
What Conditions Do Gastroenterologists Treat?
Gastroenterologists manage a wide spectrum of digestive conditions, including:
Gastroesophageal Reflux Disease (GERD): Also known as heartburn, GERD is a condition where stomach acid backs up into the esophagus, causing discomfort and irritation.
Peptic Ulcers: These are sores that develop on the lining of the stomach or duodenum (the first part of the small intestine).
Irritable Bowel Syndrome (IBS): A chronic condition characterized by abdominal pain, cramping, bloating, diarrhea, or constipation.
Inflammatory Bowel Disease (IBD): This encompasses two chronic conditions, Crohn's disease and ulcerative colitis, that cause inflammation in the digestive tract.
Celiac Disease: An autoimmune disorder triggered by gluten, a protein found in wheat, barley, and rye.
Liver Disease: Gastroenterologists diagnose and treat various liver diseases like hepatitis, cirrhosis, and fatty liver disease.
Gallbladder Disease: This includes conditions like gallstones and inflammation of the gallbladder.
Pancreatitis: Inflammation of the pancreas, an organ behind the stomach that produces digestive enzymes and hormones.
Colorectal Cancer: Gastroenterologists play a crucial role in colorectal cancer screening, diagnosis, and treatment.
Diagnostic Tools Employed by Gastroenterologists
To diagnose digestive issues, gastroenterologists utilize a range of diagnostic tools, including:
Detailed Medical History and Physical Examination: A comprehensive review of your symptoms, medical history, and family history is crucial for initial assessment.
Blood Tests: Blood tests can reveal signs of infection, inflammation, or nutritional deficiencies.
Stool Tests: These tests can help diagnose infections, parasites, or hidden blood in the stool.
Imaging Techniques: X-rays, CT scans, MRIs, and ultrasounds can visualize the digestive organs and identify abnormalities.
Endoscopy: This procedure uses a thin, flexible tube with a camera to examine the inside of the digestive tract.
Upper Endoscopy: Examines the esophagus, stomach, and duodenum.
Colonoscopy: Examines the entire colon and rectum.
Biopsy: During endoscopy, a small tissue sample can be taken for further analysis under a microscope.
Treatment Options Offered by Gastroenterologists
Depending on the diagnosis, gastroenterologists offer a variety of treatment options, including:
Lifestyle Modifications: Dietary changes, managing stress, and getting enough sleep can significantly improve digestive health.
Medication: Medications are prescribed for various conditions, such as antacids for heartburn, antibiotics for infections, and anti-inflammatory drugs for IBD.
Endoscopic Procedures: Minimally invasive procedures like polyp removal or stricture dilation can be performed during endoscopy.
Surgery: In some cases, surgery might be necessary to treat certain conditions like gallstones or advanced cancers.
Finding the Best Gastroenterologist Dubai
If you're experiencing digestive problems, finding a qualified and Best Gastroenterologist Dubai is crucial. Here are some factors to consider:
Qualifications and Experience: Choose a board-certified gastroenterologist with extensive experience in treating your specific condition.
Hospital Affiliation: Consider the hospital or clinic where the gastroenterologist practices and ensure it has a good reputation and advanced facilities.
Communication Style: Look for a doctor who listens attentively to your concerns and explains things in a clear and understandable manner.
Location and Appointment Availability: Choose a gastroenterologist conveniently located and with appointment scheduling that suits your needs.
Insurance Coverage: Verify if the gastroenterologist accepts your health insurance plan to avoid out-of-pocket costs.
Patient Reviews: Reading online reviews from other patients can offer valuable insights into the doctor's bedside manner, communication skills, and overall patient experience.
Beyond Finding the Best: Building a Relationship with Your Gastroenterologist
Having an open and trusting relationship with your gastroenterologist is vital for optimal digestive health management. Here are some tips for building a strong patient-doctor relationship:
Be Prepared for Your Appointment: Make a list of your symptoms, medical history, and any questions you have for the doctor.
Be Honest and Open: Don't hesitate to discuss all your symptoms, even if they seem embarrassing. The more information you provide, the better your doctor can diagnose and treat your condition.
Ask Questions and Seek Clarification: Don't be afraid to ask questions and ensure you understand your diagnosis and treatment plan.
Follow Through with Treatment Recommendations: Adherence to your doctor's recommendations, whether it's medication, dietary changes, or lifestyle modifications, is crucial for successful treatment.
Schedule Regular Follow-up Appointments: Regular checkups allow your gastroenterologist to monitor your progress and adjust your treatment plan as needed.
The Importance of Preventive Care for Digestive Health
While gastroenterologists excel in treating digestive problems, prevention is always better than cure. Here are some tips for maintaining good digestive health:
Eat a Healthy Diet: Focus on a balanced diet rich in fruits, vegetables, whole grains, and lean protein.
Stay Hydrated: Drinking plenty of water throughout the day keeps your digestive system functioning smoothly.
Manage Stress: Chronic stress can wreak havoc on your digestive health. Practice stress-management techniques like yoga, meditation, or deep breathing.
Maintain a Healthy Weight: Being overweight or obese can increase your risk of certain digestive disorders.
Limit Alcohol and Smoking: Excessive alcohol consumption and smoking can irritate the digestive tract and contribute to digestive problems.
Get Regular Exercise: Regular physical activity can improve gut health and overall well-being.
Schedule Regular Screenings: Regular screenings for conditions like colorectal cancer are crucial for early detection and treatment.
The Future of Gastroenterology: Innovations for a Healthier Digestive System
The field of gastroenterology is constantly evolving, with exciting new technologies and treatment options emerging. Here's a glimpse into what the future might hold:
Advanced Imaging Techniques: Enhanced imaging technologies like capsule endoscopy and stool DNA testing might revolutionize diagnosis.
Personalized Medicine: Understanding individual gut microbiomes could pave the way for personalized treatment plans for digestive disorders.
Minimally Invasive Procedures: Advancements in endoscopic techniques and robotic surgery might lead to less invasive and more precise procedures.
Microbial Therapy: Research on the gut microbiome suggests potential for using probiotics and fecal microbiota transplants to treat digestive diseases.
Investing in Your Digestive Health: A Partnership with Your Gastroenterologist
Digestive health is a cornerstone of overall well-being. By prioritizing preventive care, finding a qualified Best Gastroenterologist Dubai, and building a strong patient-doctor relationship, you can navigate any digestive challenges effectively. Remember, open communication, adherence to treatment plans, and a commitment to a healthy lifestyle are your allies in maintaining a healthy digestive system. Cornerstone Clinic is also designed for everyday family health from leading UK Family Doctors to dentist to cosmetic surgeons to vascular treatments. To get the best out of our team, it’s important to discuss your needs with our practitioners so a program can be designed for your schedule especially for our longevity and rejuvenation programs. For example, many of our families will send children to the dentist, whilst mum has a botox and dad is receiving a health check at the same time.
#family clinic dubai#blepharoplasty dubai#invisalign dubai#menopause dubai#eyelid bag surgery dubai#breast augmentation dubai#family doctor dubai#veneers dubai#mini tummy tuck dubai#liposuction dubai
0 notes
Text
When To See a Gastroenterologist in Westchester County and Yonkers
Experiencing stomach problems and digestive difficulties may prompt one to consult a general physician initially. Sure, the medical professional will take time to examine the patient carefully and ask many questions to identify the source of discomfort. The problem may be minor, such as acid reflux or bloating. Feeling nauseous is a common complaint among patients diagnosed with gastrointestinal problems. The general doctor may think that the patient needs more specialized care and refer the patient to an experienced hepatologist in Westchester County and Yonkers.
Inquiring or checking the facts about such a specialty and the specialist is essential. It suffices to know that a hepatologist is often called a liver doctor who treats diseases related to the liver and the biliary system. A sub-specialty of gastroenterology, the concerned doctor must undergo specialized and extensive training. The American Board of Internal Medicine awards a certificate to successful professionals.
Role of a hepatologist
This specialty doctor is equipped to diagnose and treat all liver diseases and gallbladder problems. Additionally, pancreatic disorders may be treated by them too. The most common treatments done by such a specialist include the following:-
· Hepatitis
· Hepatic encephalopathy
· Nonalcoholic fatty liver disease
· Nonalcoholic steatohepatitis
· Cirrhosis of the liver
· Other types of liver damage
· Liver cancer
· Fatty liver disease
· Metabolic liver diseases
Moreover, the specialist is also trained to treat other complaints of the biliary system, i.e., the gall bladder, bile duct, and the liver. The patient can thus expect the best possible treatment from the hepatologist for the following conditions:-
· Primary biliary cholangitis
· Primary sclerosing cholangitis
· Removal of gallstones
· Gallbladder cancer
· Pancreatitis
· Pancreatic cancer
· Gallbladder inflammation
· Bile duct stones
· Noncancerous tumors of the gallbladder, liver, or bile duct
· Bile duct cancer
Some of the other responsibilities handled by the hepatologist include:-
· Performing diagnostic tests
· Explaining the treatment options to the patient's family
· Providing treatment as required
· Monitoring patients scheduled for liver surgery or liver transplant
· Refer the patient to other specialists for further assessment and treatment
· Working together with other medical experts to ensure the best care
Reasons to consult a hepatologist
A layperson is not aware of this specialty. The primary care doctor may refer the patient to a liver specialist when any of the following problems are noticed:
· Abnormal liver function test results
· Gastrointestinal bleeding
· Jaundice
· Ascites
· Enzyme problems
· Drug overdose
Where is a hepatologist found?
The hepatologist may examine patients in clinics, hospitals, and other healthcare facilities. Other specialist doctors often consult them about other patients diagnosed with liver problems, too. Patients seeking a quality hepatologist may also inquire at high-dependency units, intensive care units, or liver specialist centers.
An individual who experiences several stomach and digestive issues will surely obtain the proper treatment from a reputed gastroenterologist in Westchester County and Yonkers.
#gastroenterologist in Westchester County and Yonkers#hepatologist in Westchester County and Yonkers
0 notes
Text
Digestive System
The digestive system is a marvel of biological engineering, orchestrating the journey of food through the body, from the moment it enters the mouth to its exit through the anus. This complex process involves a network of organs, each playing a crucial role in breaking down food, absorbing nutrients, and eliminating waste. In this detailed exploration, we delve into the anatomy, functions, common conditions, care practices, and the importance of seeking medical attention for digestive system issues.
Anatomy of the Digestive System

Gastrointestinal (GI) Tract:
1.Mouth:
Initiating Digestion: Salivary glands activate as the sight and scent of food trigger the digestive process.
Chewing and Mixing: Food is chewed into digestible pieces, mixed with saliva to facilitate breakdown.
Swallowing: The tongue propels the food into the throat and esophagus.
2. Esophagus:
Transportation: A muscular tube conducting food to the stomach through peristalsis.
Sphincter Function: The lower esophageal sphincter relaxes to allow food entry and contracts to prevent stomach content reflux.
3.Stomach:
Container and Mixer: A hollow organ holding and mixing food with stomach enzymes for further breakdown.
Acid Secretion: Cells in the stomach lining secrete powerful acids and enzymes crucial for digestion.
Release to Small Intestine: Processed stomach contents move to the small intestine for further digestion.
4.Small Intestine:
Segments and Functions: Comprising the duodenum, jejunum, and ileum, each segment has distinct roles in digestion and nutrient absorption.
Enzymatic Breakdown: Pancreatic enzymes and bile from the liver aid in breaking down food.
Nutrient Absorption: The jejunum and ileum absorb nutrients into the bloodstream.
Consistency Changes: Contents transition from semi-solid to liquid as water, bile, enzymes, and mucus contribute to the process.
Biliary System
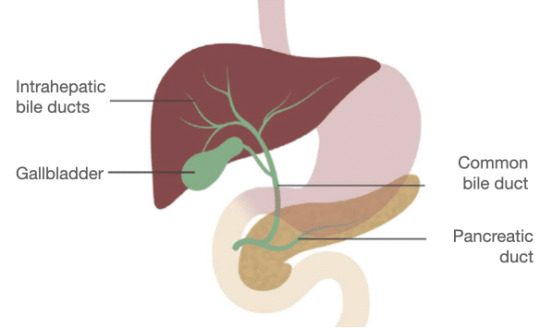
a. pancreas:
Enzyme Secretion: Releases digestive enzymes into the duodenum to break down proteins, fats, and carbohydrates.
Insulin Production: The pancreas produces insulin, a key hormone for sugar metabolism.
b. Liver:
Nutrient Processing: Processes nutrients absorbed by the small intestine.
Bile Production: Secretes bile into the small intestine, aiding in fat digestion and vitamin absorption.
Detoxification: Acts as the body’s chemical “factory,” detoxifying harmful substances.
c. Gallbladder:
Bile Storage: Stores and concentrates bile from the liver.
Release into Duodenum: Releases bile into the duodenum to assist in fat absorption.
Large Intestine (Colon):
Colon:
Waste Processing: Responsible for transforming waste into a convenient form for bowel movements.
Peristalsis: Propels stool through the colon, removing water and transitioning it from a liquid to a solid state.
Storage and Elimination: Stool is stored in the sigmoid colon until mass movements propel it into the rectum for elimination.
Rectum:
Chamber Function: A straight chamber connecting the colon to the anus.
Signaling and Holding: Signals the brain about stool presence and holds stool until evacuation.
Anus:
Final Elimination: The last part of the digestive tract, consisting of pelvic floor muscles and sphincters.
Sphincter Control: Surrounding sphincter muscles control stool release, preventing involuntary bowel movements.
Conditions and Disorders
Digestive system health can be affected by a spectrum of conditions, ranging from temporary issues to chronic diseases:
Temporary Conditions:
Constipation:
Frequency and Characteristics: Reduced bowel movements with dry and hard stool.
Difficulty and Pain: Straining during bowel movements, leading to discomfort.
2.Diarrhea:
Loose and Watery Stool: Abnormal stool consistency often caused by various factors.
Potential Causes: Bacterial infections, dietary issues, or unknown triggers.
3.Heartburn:
Misleading Name: Despite the name, heartburn is a digestive issue.
Acidic Backflow: Occurs when stomach acids move up the esophagus, causing discomfort in the chest.
4.Hemorrhoids:
Swollen Veins: Enlarged veins inside and outside the anus and rectum.
Symptoms: Pain, discomfort, and rectal bleeding.
5.Stomach Flu (Gastroenteritis):
Viral Infection: Infection of the stomach and upper part of the small intestine.
Duration: Typically lasts less than a week.
6.Ulcers:
Sore Development: Sores on the lining of the esophagus, stomach, or small intestine.
Causes: Helicobacter pylori infection and prolonged use of anti-inflammatory drugs.
7.Gallstones:
Solid Material Formation: Small pieces formed from digestive fluid in the gallbladder.
Chronic Diseases:
GERD (Chronic Acid Reflux):
Frequent Acid Backflow: Acid-containing contents in the stomach frequently leak into the esophagus.
Symptoms: Persistent heartburn and regurgitation.
2,Irritable Bowel Syndrome (IBS):
Colon Muscle Dysfunction: Irregular contractions leading to excessive gas, abdominal pain, and cramps.
Chronic Nature: A long-term condition affecting bowel function.
3.Lactose Intolerance:
Inability to Digest Lactose: Results in digestive discomfort after consuming milk and dairy products.
Common Symptoms: Bloating, gas, and diarrhea.
4.Diverticulosis and Diverticulitis:
Colon Pockets Formation: Diverticula (pockets) in the wall of the colon.
Complications: Inflammation (diverticulitis) can occur, causing pain and infection.
5.Gastrointestinal (GI) Cancers:
Tissue and Organ Affliction: Cancers affecting the digestive system, including esophageal, gastric, colorectal, pancreatic, and liver cancers.
6.Crohn’s Disease:
Inflammatory Bowel Disease (IBD): A lifelong condition causing inflammation in the digestive tract.
7.Celiac Disease:
Autoimmune Disorder: Gluten consumption damages the small intestine.
Trigger: Found in wheat, barley, and rye.
Care Practices for Digestive Health

Maintaining a healthy digestive system involves adopting proactive lifestyle and dietary habits:
1.Hydration:
Importance of Water: Drinking water facilitates smooth food flow, preventing dehydration-related constipation.
Dehydration Consequences: Insufficient water intake can lead to dry and hard stool.
2.Fiber-Rich Diet:
Benefits of Fiber: Supports digestion and regular bowel movements.
Soluble and Insoluble Fiber: Both types contribute to digestive health.
3.Balanced Nutrition:
Fruits and Vegetables: Multiple servings daily for essential vitamins and minerals.
Whole Grains: Choosing whole grains over processed grains.
Limiting Processed Foods: Reducing intake of processed and sugary foods.
4.Probiotics:
Role of Probiotics: Supporting a healthy gut microbiome.
Post-Antibiotic Use: Especially beneficial after antibiotic treatments.
5.Mindful Eating:
Chewing and Digestion: Thorough chewing aids in proper digestion.
Eating Pace: Slower eating allows the body to signal fullness.
6.Physical Activity:
Exercise and Digestion: Physical activity and gravity aid in moving food through the digestive system.
Post-Meal Walks: Taking a walk after meals can enhance digestion.
7.Avoiding Harmful Habits:
Alcohol and Smoking: Limiting alcohol intake to prevent acid-related issues.
Smoking Cessation: Quitting smoking improves digestive symptoms.
8.Stress Management:
Stress and Digestive Issues: Association between stress and conditions like constipation, diarrhea, and IBS.
Stress Reduction Techniques: Incorporating stress-relief practices into daily life.
Seeking Medical Attention
While occasional digestive issues are common, persistent symptoms warrant attention:
When to Contact a Healthcare Provider:
Frequent Symptoms: Constipation, diarrhea, vomiting, stomach pain, excessive gas, or heartburn.
Potential Underlying Issues: Frequent occurrences may indicate a more serious digestive system problem.
2.Importance of Medical Evaluation:
Diagnostic Assessment: Identifying the cause of persistent symptoms.
Early Intervention: Timely treatment prevents potential complications.
3.Collaborative Approach:
Healthcare Professional Guidance: Seeking advice on managing and preventing digestive issues.
Individualized Care: Tailoring interventions based on the individual’s health status and conditions.
Conclusion
In conclusion, understanding the details of the digestive system provides a foundation for promoting digestive health. The collaboration of organs in the GI tract and the biliary system highlights the complexity of the digestive process. Awareness of common conditions, care practices, and the significance of seeking medical attention empowers individuals to prioritize their digestive well-being. Adopting a holistic approach that combines a healthy lifestyle, balanced nutrition, and regular medical check-ups ensures a resilient and well-functioning digestive system, contributing to overall health and vitality.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at [email protected] for professional assistance.
#medical students#nursing student#nursing school#healthcare#medicine#medical help#university student#medical university#assignment help#student life#study blog#study inspiration#studyblr community#studyblr#aesthetic#academic assignments#student#study motivation#case study#online writing#writers on tumblr#writeblr#writing
0 notes