Link
In addition, the Doctors of asthma Bhawan suggest various other therapies which help in to cure asthma attacks. Hence, it’s necessary to consult recommendations from doctors for good respiration throughout the monsoon to manage an asthma attack. Make an appointment. Call us Tel: +0141-2235005 or Mob: +91-93529 345315 and get more information about How to Manage Asthma during Monsoon?
#what stands for asthma?#world health organization (who)#how omicron virus affect asthma patient?#How to Improve Asthma in Winter- Precautions and Treatment#How it is Dangerous for Asthma PatientsNeoCov#How to Improve Child Immunity During Covid-19?#what can protect your child against covid-19#what is tomato flu or tomato fever? know its symptoms | causes | prevention#what did asthma patients need to know during covid-19?#what is the risk factor for lung disease?#asthma treatment#Best Asthma Treatment in Rajasthan#asthma disease#ASTHMA and COVID-19#lung disease#Why COVID-19 vaccine is important?#What Are The Long-Term Lung Problems After Covid-19?#How to Manage Asthma during Monsoon?#Does Smoking Cause Lung Cancer?#How Does Dostarlimab Cancer Drug Work?#triggers and tips to manage asthma#best asthma treatment#Best Asthma Treatment in India#tips to manage asthma#allergy#allergy symptoms#allergy treatment#summer disease#Skin Problems during Summer and their Prevention#summer skin disease
0 notes
Text
Five Thousand Miles

Warning: Angst, descriptions of covid patients’ suffering, hospitals
A/n: I researched a lot about what covid patients go through in a hospital and their treatments but still took a couple creative liberties so I apologise if the descriptions aren’t accurate. Do tell me how you liked it!
Summary: Y/n tests positive for covid-19 and has to be hospitalised. Her boyfriend, Harry is five thousand miles away from her.
“Harry, I’m scared,” Y/n confessed as she readied herself, struggling with wearing her mask and gloves while also balancing her phone to continue talking to her boyfriend on FaceTime.
“It’ll be alright, you are taking every precaution you can. Plus, you have to get out of the house sometime, you can’t survive on air alone. Trust me, baby, you can do this.”
Harry’s voice was keeping her grounded, she wanted to continue talking to him but knew it would be impossible to shop and talk to him at the same time, so she nodded at him, “You’re right. Okay, I’ll call you when I get back. Safely.”
Taking a deep breath, she went out the door to a world of germs, people, and newly acquired viruses.
Being in the middle of a pandemic alone wasn’t her favourite situation to be in. It felt better when she had company, people who would help her buy the essentials. As soon as situations eased up a bit, her quarantine partners left New York to be with their families. She was all alone now.
Looking at all the empty streets, Y/n was left with a weird sensation. The city that never slept had never been quieter. She was so used to being woken up by car horns and car alarms in the morning that during the first few weeks of lockdown, she found it hard to wake before noon. This quiet was almost poetic, like the stuff of post-apocalyptic films. Y/n wasn’t sure if the silence comforted her or terrified her.
There were more people in the store than she had expected, though all in their masks, she breathed in relief. She went straight to the personal hygiene section, remembering the most important item on her list, only to find that the store was all out of toilet papers, the one thing films didn’t guess would be a big problem. She rolled her eyes at the selfish people who had panic-bought more stuff than they would have needed.
She tried every store near her neighbourhood, and eventually was able to get the last set in the final shop she visited. Tired from driving all over the city in search of toilet papers, she went to the check-out line to finally buy her stuff.
Standing in her place, Y/n noticed the people in the store, few whose foreheads were furrowed, their eyes darting around making sure they were maintaining the mandated distance from others, panic evident on their mask-covered faces. Some others appeared plain bored. Already used to the new routine and just wanting to get it over with.
She was so lost her observations, she almost didn’t hear it, the woman behind her in the line coughed loudly, making people jump farther apart than the required six feet.
“It’s just allergies,” the woman announced in a nasal voice, rolling her eyes at people’s reaction.
As Y/n’s turn came at the check-out counter, she found herself frozen to the ground, she didn’t know why but the cough threw her off. It felt weird to react the way she did, but she could not make herself move. She was nervous. She wanted to laugh at herself for feeling this way because of a measly cough, but it wasn’t so simple and right now all she felt was fear.
“Oh for god’s sake,” the woman moved forward, pushing her aside and placed her items at the counter. Even the employee there seemed wary, but knew he had to comply to keep his job.
It was only after the woman left, was Y/n finally able to move, she shook her head as if to shake the incident away from her mind and finally paid for her items.
She ran all the way home, even though she knew she shouldn’t have. She couldn’t help herself, she just wanted to move away from the public and into the safety of her home as soon as she could.
As she entered her house, Y/n felt her chest tighten, as though someone was sitting on it, she couldn’t breathe properly. It felt like she was breathing through a squished straw.
In between her wheezing, she searched around for her inhaler in her side bag. She felt her breath coming back a few seconds after she breathed in the medicine. She fell to her knees in exhaustion and took in a few more breaths to calm down.
She then picked herself up and embarked on an extensive set of tasks- Taking off her gloves and mask, removing her shoes at the entrance of her house, washing her hands. But, this somehow didn’t seem enough to her, so she went ahead and took another shower, just to be extra sure.
While in the shower, she cursed her asthma. It wasn’t usually a big hurdle in her life, but now, everything was a hundred times worse. This was the first time she had feared for her life. Her anxiety was at an all-time high and all she had to keep her sane was her daily FaceTime calls with Harry.
Opening her laptop to do her work, she checked the numbers again- seventy thousand new cases. She sighed and closed her laptop, not having the motivation to do any work. She scrolled through her social media to distract herself only to be shoved more news about the coronavirus, she let out a groan of frustration and switched off her phone, deciding to take a nap instead.
Only she couldn’t sleep. She thought back to all the plans she made with Harry, promising him to be there next to him while he toured the globe. She laughed at the situation and how no one in a million years could have guessed the current world state.
She didn’t know when she fell asleep, but she must have as she woke up with a jolt in her bed after a strange dream. She shook her head and looked out her window to see the sky dark. She switched on her phone, it was 8 pm. She cursed to see three missed calls from Harry and one from her friend, Sarah.
Preparing herself, she called Harry.
“Where were you, I called like three times?” His voice was deeper than usual, she guessed he had just woken up because of her call. She calculated it to be 4 am in London, where Harry was. She felt bad for waking him up like that.
“I know, I switched off my phone and fell asleep. Sorry,” she grimaced.
Harry hummed in acknowledgement, “how you doing?”
She could hear rustling on the other side and imagined a sleepy Harry sitting up in his bed, his hair messy from his sleep, “Just missing ya’.”
“I know, I hate that I had to leave you like that, wish you could come with me,” there was a hint of a whine in Harry’s voice which made Y/n smile.
“Wish I had a visa for England, I really wanted to come too,” and she meant that. At least that way, she wouldn’t have to be alone.
“I’ll video call you tomorrow, it’s late here, or rather early,” what he was saying next was obscured by his yawn. She sighed, she missed him too much.
“Yeah sure, see you tomorrow, bye.”
“Bye.”
When the call disconnected, she messaged Sarah to ask what the call was about, who didn’t respond. She shrugged her shoulders and went down to the kitchen to start preparing for dinner.
~
It started with a headache. She didn’t ponder much on it and instead only took medicine to curb the pain enough to continue working.
It was when she felt a certain roughness in her throat, did she pay attention. Her cough worsened within days, she was having a hard time breathing normally. It felt like a less severe but constant asthma attack. She took her temperature, which showed her to be having a fever at 101°F.
It took her some time to even process what was happening to her, she initially wondered if it could be the flu or something non-covid, but she knew she couldn’t take the chances. Harry was the first person she informed.
“What are you saying?!” Harry was frantic, his forehead creased as he ran his fingers through his hair, messing them up.
“I have a fever, a cough, and I’m having difficulty breathing,” counting the symptoms on her fingers, she informed him again.
“It could be the flu, Y/n you didn’t even go outside. How could it be anything else?”
“H, I did go out to buy supplies, didn’t I? Maybe I got infected there somehow. We shouldn’t be kidding ourselves. I have to at least get tested.” You didn’t want to show him just how scared you were, but it was hard to keep your voice from cracking.
“I am scared, H,” you let the tears out. Your shoulders shook while you tried to wipe your tears as they were leaking from your eyes.
Harry closed his eyes, not being able to see you sobbing, “I know baby, but I know you’ll be strong. I will take the next flight to LA. I’ll be there as soon as I can.” He promised, his mouth set in a hard line as a strong look of determination crossed his face.
She shook her head with as much strength she could muster, “No Harry, you shouldn’t keep travelling, plus, you can’t stay with me and I don’t want you staying at some hotel. It’s not safe.”
“Bu—”
“—I won’t hear another word about it. I have Sarah, and you have your work to take care of. I will be fine.”
She knew Harry wanted to say more, object to her claims, she would not be fine. But he knew it would be of no use, once she had made up her mind, it would be impossible to change it. So, he settled for a low nod.
“Keep me updated, I’ll also talk to Sarah. She better be there for it all. You should now call your doctor, see what’s the next step.”
Y/n nodded, smiling that Harry understood. She didn’t want to trouble him. She also wanted to pretend for a few more seconds that this was not a big deal.
She called Dr Gupta, her heart was beating at an all-time high and her energy was at an all-time low. She barely had enough breath to tell her doctor about her situation who booked an appointment for her to go to the nearest covid testing facility.
She took a deep breath, wore her protective gear and drove to the testing lab which was a ten-minute drive from her place. She was already out of breath by the time she reached the place.
When she was done with her test, she felt worse than she had before. Sarah called to check in on her, but Y/n didn’t have the energy to talk so Sarah video-called her, seeing Y/n’s face would have to be enough for her at that point.
Sarah’s eyes softened, seeing her best friend heaving, eyes shut and groaning due to her chest pain. But she knew, more than anything, her best friend was scared.
“I hope with everything that I am that the test comes back negative,” her voice was tinged with worry and genuine hope.
Y/n could only nod.
The call came two days later, Y/n sat up in her bed, she had been dreading this moment these past days, with Harry and Sarah to distract her.
The test came back positive.
She fell back into her bed, cushioned by her pillow and started shaking uncontrollably as she sobbed.
She felt insanely dehydrated by the time she stopped crying, she didn’t even get to call either of her friends. She stood up with a groan, and following one slow step after the other, she went to the bathroom to wash her now tear-stained face.
The call she made to Harry wasn’t an easy one. She knew he would take the news worse than she had, and her reaction was not a light one.
“I prayed. I promise I prayed Y/n,” his words were almost indecipherable in between his cries. His every tear followed the other with a ferocity never before noticed by Y/n.
Her own tears followed suite, she was so sure she had finished up all her tears, but she was proven wrong. Soon, the only conversation happening between the two was through their sobs.
She wanted to curse all the gods, she didn’t want to go through the pains of having this disease and she didn’t want to do it alone. Even though she had Harry and Sarah standing right beside her, knowing they would not be able to meet her in person, she had never felt more alone.
“I don’t feel good, H,” she confessed. Breathing was becoming difficult day by day, she would rather have an asthma attack twice a day than having this constant pressure on her chest and throat. She knew she had to tell him, “I have to get admitted to the hospital first thing in the morning tomorrow, they say my covid could be worsened because of my asthma,” she let out in between a series of coughs stopping her after every word.
Harry nodded, his heartbeat rising. He cursed himself for leaving his girlfriend alone in the country. If he hadn’t left, she would not be going through this, “I’ll tell Sarah, you go rest,” he promised, seeing it get increasingly difficult for her to even sit up in her bed.
If Y/n was scared before, then the hospital made it thousand times worse. It was a scary sight, the covid ward was in an isolated area of the hospital, the doctors and nurses were in full PPE kits, the patients were lined up next to each other separated by curtains. She passed a room with ICU written on the glass door. With what she could see, she noticed several other patients, some with masks covering their nose, probably providing oxygen. Others seemed in worse conditions, they were intubated via ventilators.
Seeing them facing the same crisis together, although away from their families, but forming a new family of sorts in solidarity to their conditions gave her little comfort. Those who wore the nasal masks and thus still had the ability to talk were speaking to each other, even reading something from their phones to those who were on ventilators. Covid had seemed like a situation she would have to go through alone, her initial views though were changing.
She was admitted to the regular covid ward, with the rest of the non-critical patients and would be observed overnight. She was assisted with oxygen through a nasal mask, just like the people around her, she had noticed.
“Hey, I’m Cecilia, call me Cece,” a thirty-something woman introduced herself from beside you. The curtain was partially open, allowing Y/n to see only her face.
“Y/n, nice to meet you,” she called back, smiling as much her energy would allow.
“Never guessed this is how I would be spending my lockdown,” she laughed lightly, pointing to her mask. She then followed it up with a cough, groaning with the strain.
Y/n felt bad for her, only to be subjected to the same.
These were going to be some long days. Though she did feel better knowing she would not be facing this alone. She looked around the room, at probably twenty patients around her, in the same situation as her, if not in worse conditions. She then thought back to the people in the ICU and what they must be subjected to.
Her phone brought her attention to itself, it was Harry FaceTiming her; putting on a smile, she picked up the call.
“Hey handsome,” she suggestively raised her eyebrows, not wanting to worry him any further.
Harry did not even notice her words, he was too busy gawking at her nasal mask, “what is that?” worry coating his voice.
“Oh just my new accessory, you like it?” although Y/n wanted to look nonchalant, the pain in her voice could not be hidden, she sighed, “They are giving me oxygen through this.”
Harry’s eyebrows were knitted together in worry, Y/n wanted to make him feel better. She could not rest knowing her love was out there worrying about her, “Look I made a friend,” she turned the camera to Cece laying next to her six feet apart, “Cece, say hi to my boyfriend, Harry.”
She had forgotten her boyfriend was a big deal but was reminded of it by Cece’s gasp, “Harry freaking Styles ohmigod ohmigod,” Cece squealed, making Y/n forget for a second that she was not a teenager.
“Hullo love,” Harry greeted her in his ‘fan voice’, a smile graced her lips. “Hope you beat covid and get better soon.” Cece’s smile made Y/n realise how long these people had gone without having a reason to smile and how desperately they needed it.
Cece’s squeal garnered the attention of the people around them. Noticing the pop icon on the phone screen, conversations started flowing between everybody. Introductions were made, friendships were formed and smiles were passed around, along with Y/n’s phone. So, she asked a nearby nurse if they could access a bigger screen so everyone could see and talk to her boyfriend.
When the staff hooked up a screen, Harry gave all the patients an impromptu concert. Y/n had not smiled in days the way this concert had made her. She expected fear, anxiety, deaths and instead got friends, laughter, and music.
When Harry was done performing for his audience, he gave her a brief look. “I love you,” she whispered to him, smiling when he returned the words.
The next day, she was woken up by the noises around her, she panicked for a moment, not recognising the place she was in; but calmed when she regained her senses and noticed the blue curtains of the hospital, several machines and the people they were attached to.
She made a short conversation with Cece but had to stop because she was getting out of breath. With every passing moment, her chest pain too was increasing. She did keep listening to people chat around her. Some were on calls with their family, others were busy reading books and listening to music. She kept getting shouts of gratitude from the people in the ward for Harry the previous night.
For the next two days, that kept her going. She learned about her fellow patients, Jonathan was 59 years old, his son was an engineer and he couldn’t have been more proud; Jaya was a 42-year-old woman with bronchitis and wanted to visit Paris at least once in her life. Marc was a 50-year-old diabetic who was in a band in the 80s, they were planning a reunion show. She met countless people, each with their own stories.
At about 10 am on a Thursday, her situation worsened. The doctors had come for a routine checkup, only to see that her oxygen levels were dropping steadily and she needed immediate assistance.
She was shifted to the ICU ward. She had to be intubated and thus was given a board and marker to write anything if she wanted.
“—Yes sir, she was shifted to the ICU this morning—”
“—We can’t say much right now, but we’ll inform you if anything changes—”
“—Okay, take care, Sir.”
Y/n heard bits and pieces of the conversation her doctor was having with Harry, although since she was on medication, she couldn’t register much of it. The nurses brought her phone to her, a silhouette moving on the screen.
“Hey baby, how are you feeling?”
Y/n pondered how to describe the immense pain burning through her respiratory passage and the lack of oxygen eating away her lungs and not give him nightmares. So, she offered him a tired thumbs up.
Harry watched his girlfriend cough, her face contorting in pain and could not control his tears, he didn’t want to think about the worst-case scenario but could not stop his mind from going there. He knew how low the chances were of people on ventilators coming back. But he had to remain positive, someone had to. She needed him to be strong for her. So, he wiped away his tears, put on his best brave face and talked to her.
He called her every three hours. Giving updates to her about his day, talking to her about whatever he could. He talked enough to compensate for the silence on her part. She smiled through every sentence, even though he could not see it, even though it wasn’t visible on her face, even though she didn’t have the power to, she smiled.
And she listened. So she didn’t have to focus on Josephine dying next to her or Augusta who was a hair length’s distance away from dying the previous day. Even though doctors told her that her situation was worsening, she listened because that became the only thing keeping her from giving up.
As her pains didn’t go away, and her condition worsened further, she was given sedatives and was thus mostly asleep. Which she was thankful for, for she couldn’t take it anymore, she just wanted to rest.
Dr Garcia came by routinely to check on her, talking to her about the outside world, gave her the gossips being passed around the hospital. Even though she was barely awake to listen to any of it, she was thankful for the kind doctor providing a calm lull while doing her job.
“Mr Styles, I’m afraid her condition isn’t getting any better. She should have shown atleast some improvements,” Dr Garcia informed Harry in a heavy voice.
On the other side of the line, Harry didn’t know what to do, it felt like someone was pulling away the floor under him. “What happens now?” He asked, praying for some hopeful news.
“We really can’t say much, each case is different, but it would be better uhm,” the doctor was thinking through her words, wanting to be as considerate as possible, “is there any family of hers that would want to talk to her?”
Harry almost let out a sob as he realised what the doctor was implying ‘is there anyone who would want to give her a final goodbye?’
“No, Y/n’s family passed away in an accident when she was 16, it’s just me and Sarah,” he explained, his voice on the verge of cracking, it was becoming harder to get words out of his mouth. He didn’t want to talk anymore, he just wanted to curl up in a ball and cry.
“Oh, I understand,” Dr Garcia nodded, feeling sorry for the young girl who had stolen the hearts of everyone in the ward. She was a sweet girl, who had dreams and still held love for life even after everything she had seen. “This is not the end, Harry, she can still recover, God, I pray she does, this is not the end.” She really believed the words she was saying and wanted Harry to feel the same.
He nodded, tears clouding his eyes. He too really wanted to believe that.
A beat of silence fell upon the conversation, both in deep thought, “Harry, she wrote something on her board when she was awake yesterday,” Harry’s ears pricked up, “she wrote and I quote ‘I will not give up’ with a smiley face at the end. She is a fighter, you remember that,” Dr Garcia gave her parting ways and went back to her work.
Y/n’s words were imprinted in Harry’s mind. After the call, he made himself more presentable, wiping his tears and drove up to the church near Y/n’s house. He had come back to LA after Y/n was admitted to the ICU. He couldn’t be five thousand miles away from her in that condition.
The church was almost empty, which was surprising to Harry, given the situation, but he wasn’t complaining. He walked up the aisle, his hand grazing each wooden bench as he reached the altar and kneeled. He didn’t what to pray or how to pray, but he tried anyway. He closed his eyes and called out to God; he prayed with every part in his body, with every bone, every muscle, every fibre of being for his love to get better. For her to keep fighting. And for him to gain enough strength to deal with it all.
All this time, he had been feeling so helpless, not being able to do anything to make her better. But he made peace with the fact that the only thing he could do right now was to have faith. To have faith in God to guide him and her, in Y/n to be the stubborn strong-willed woman that she was and continue fighting, he had faith in his faith and that it would not disappoint.
He stayed there, talking to God until the closing hours. He then went back to Y/n’s place and sat on the sofa, waiting by his mobile, ready for any phone call he might receive.
He was awoken the next day by his phone ringing on the coffee table next to him. He looked at the time, it was noon, he picked up.
“Congratulations Harry, she’s getting better,” the relief was evident in Dr Garcia’s voice.
Harry felt himself getting physically lighter.
“I mean there is still a long way to go, but her oxygen levels are rising, her lungs are recovering, she’ll be soon able to breathe on her own. Harry, she did it, she won,” Harry didn’t listen to the rest of what the doctor was saying, he was too busy falling in love with the love of his life. It felt like he himself had come back from the dead. He knew his faith could never disappoint.
“Thank you doctor, I’ll be waiting for the call when you tell me she’s tested negative,” he laughed, his lungs breathing in air after what felt like a lifetime.
Dr Garcia chuckled along with him and agreed, telling him Y/n would call him when she woke up.
~
“You know I love you right? My fighter,” Harry tightened his grip on her hand and kissed her knuckles.
Y/n’s head fell back as laughter bubbled out of her, “You just told me that like two minutes ago.”
“I know, but a few weeks ago I thought I would never get to say it to you ever again. So, I will keep reminding you every minute that I love you and that you are the strongest person I know,” he snaked his arms around her, placing his head on top of hers, “I really missed holding you.”
She breathed in Harry’s scent, slowly regaining her sense of smell, she had missed this too. She cupped his cheek with her right hand and gave him a light peck.
Harry grabbed the back of her head, keeping her lips on his, deepening the kiss. When they separated, he rested his forehead against hers, not wanting her to move even an inch away from him.
Noticing her deep breaths, he whispered in her ears, “This is the only reason I want you to be out of breath. This and well... the other one,” he smirked.
“Oh hush you,” Y/n blushed, she sucked in a breath through her teeth, “Shit man, I love you.”
#Harry Styles#harry styles fanfiction#harry styles fic#harry styles one shot#harry styles imagine#harry styles imagines#covid19#harry styles x reader#harry styles x y/n#harry styles angst#angst
289 notes
·
View notes
Note
If you ever want to write a full account of your hospital stay, I'm so here for it. I want it all: the farts, the grannies, the fighting over windows, the other weirdos, why you want to murder the doctor and how your fam will help you get away with it, the works. Start writing while I grab the popcorn! 🍿
Ok, don’t remember what I have said here already, so I’ll give a full story plus some flashbacks from my childhood.
-I got 4 grannies in my room, the average age: 65+
-granny number one: ultra Catholic, made a cross on my forehead (I was so shocked, I didn’t say a shit, aside of screaming in my head – woman?! Covid restrictions?! Keep your distance?!), a farmer woman (one day she just said that when she wants a chicken soup, she goes outside, catches the chicken, chops the head and make a soup – the faces of the other grannies - PRICELESS), praying in weird moments, instead of sweat pants, wearing dress shirts and dress pants (and you know, we were doing physical exercises there???), loving dirty jokes and making them A LOT,
-granny number two – tiny old sweet lady (she was like 80 something years old?), usually sitting in the corner or on the balcony and praying silently, she was like Catholic kamikaze, she sometimes was sitting on the balcony and praying for FIVE HOURS, oh, and once shitted her pants
-granny number three – ex school director, Miss Ooooow, Ooooow, came with 2 suitcases and occupied ½ of the wardrobe (for example, I managed to put all my things in my night stand), was very surprised I came with so little clothes and was washing them, was crying when she had to wash her hair because she always goes to hairdresser…
-granny number four – on a wheelchair, my best pal, making her own cigarettes at evenings on the canteen (a place where the meals were served, close to the balcony), as much done with the other ladies as I was,
-our room were filled with weird Turkish soap operas (the first time they turned the television on some Mahmud wanted to kill some Bahar and the dialogues were so cringy I had to check if it was a real show and surprisingly it was). Every day after I was evacuating my ass to the canteen or to the balcony where I was reading (I’ve finished 19 books and my ass still hurts because of the fucking hard chairs).
-if it was not a Turkish soap opera, it was Polish News on the public channel (Imagine FOX news), so every fucking day when it was played, the traitors of Polishness and Polish tradition and the only good ruling party like me, were gathering in the canteen. We were like a few folks (me, the granny number 4 and some dude doing crosswords and having super high blood pressure, mostly because all dudes from his room were watching the news and agreeing with everything what was said there)
-food, examples




-so I was not eating too much, so granny number one made a cross on my forehead and blessed me, so I would eat more and have a strength to give birth to children – I shit you not
-when I said I don’t want children – they almost had a collective heart attack. I decided to not reveal my other social, religion and political opinions, because I would be strangled to death in my sleep by a rosary one night
-one day I was stupid too much and didn’t leave the room while they were watching Polish Fox News and while half listening to the bullshit I probably made a fuck-my-life-face. When they ask what I was thinking about, my, a fucking idiot, said that about the vanity of life. They almost got another collective heart attack and almost ran to the nurses, no idea why but whatever
-Granny number 3, was afraid of other people snoring, because she had problems with sleep. In the end she was the one who snored the loudest
-there was an opening/closing the windows war. Granny 1 had sick lungs and asthma and whatever so was always closing the window because she was getting pneumonia and oh my god, while Granny 3 had problems with breathing, was suffocating and oh my God, so she was always opening the window. Granny number 3 was always opening the window while other already left for the meals, while Granny number 1 was always returning first and complaining SOMEONE was trying to kill her with the cold air and closing the windows. HILAROUS stuff
-on the end of the first week I ACCIDENTALLY broke a small window that was situated on the top, a window that supposedly was not meant to be open, so for the next 2 weeks we had a window opened ALL the time. Don’t ask why no one called some dudes to fix it, I have no idea, but thanks to it I survived the nights full of symphonies of farts
-that one day they gave us beans for the dinner and boy, you can only imagine
-one day we got a meat chops with a crispy batter. If you added the batter on the bottom to the batter on the top of the meat, they were thicker than meat itself
-all soups tasted the same. One day they gave us a soup and I was SURE it was a pickled cucumber soup and I was AMAZED that they managed to make it without cucumbers. Then I have learnt it was a sorrel soup *sad music in the background*
-the grannies loved to motherhen me for some reason. For example, I was sitting politely in the canteen, reading another fucking book, when one of them came and said I should not read so much, it’s unhealthy and they are worried about me. I was blinking for 30 seconds, wondering if laughing like a mad hyena would make them having another collective heart attack. In the end I just mhm-ed and continued reading.
-later I have learnt they were behaving like that, because they thought I was in middle school…
-basically, I was the youngest person on the ward and some nurses and other patients felt sorry for me because I didn’t have anyone in my age to talk… and I was like… why the fuck I should have been feeling sad? I could read and NOT TALK??? Also, or reading or murdering the grannies with a plastic spoon in their sleep, so thank you very much, leave my ass alone.
-on one dinner I basically ate pasta with pepper, because the spinach, guys, the spinach was awful and I’m not going to traumatize you with the pic
-I had a deal with the crosswords dude during breakfasts and suppers – was giving him ham and cold meat, he was giving me jam
-the Granny number one was SLEEP SINGING one night
-two days per every week some farmer was coming and selling his vegetables and fruits. Guys, all patients were buying food there, for sure I was weeping while buying plums, apples and tomatoes.
-Granny number three was super annoying and acting like a bitch aka typical ex school director, because when she wanted to watch something in TV at night, she always did even if the others were upset, but when she wanted to go to sleep at 9 she owww owwww owwwwed and was turning the lights off. So, sometimes I was returning at 9 to the room and it was dark. And there were no night bedside lamps, so it meant you needed to go to sleep too. At fucking 9.
-the face of one dude who was eating with us on one table was always priceless every time when he was opening the boxes. It was a personification of a man who was done, crying inside and knowing he can’t escape
-the most traumatizing experience after my hip surgery was PEEING. The nurse brought me a bed pan and I needed to pee while laying on my back and it was weirdly difficult, maybe because the nurse was standing over me, talking to another patient. Also, I can’t imagine taking a shit while laying, but whatever. On one moment after like a minute me trying hard, she put a hand on my stomach and said, oh so hard. My face was probably a mix between: ==’ and O.O. But in the end I succeeded, yay…
-another traumatizing experience is measuring the temperature every morning around 6. You know, you are sleeping, but suddenly feel some movement, so you open your eyes and a nurse, wearing a mask is aiming a thermometer that looks like a gun at your forehead. Amazing feeling
-I talked with some dude who had the same surgery aka hip removal, but he was not sleeping so he herd everything, and said how blood was gushing all over the place and the surgeons and the nurse was bringing the artificial hips three times, because the surgeons were not sure if they are the good ones. FUN
-btw, the first time when I saw a dead body was in a hospital. There was a ward where one room was for children, the rest was for adults after accidents etc. Sometimes someone died and they were usually putting the dead body to the bathroom on the corridor (no toilets at the rooms, it was one of the two bathrooms for whole ward). They usually put an “out of service” paper on the door, but sometimes they forgot about it. So, one night, me, sleepy and yawning went to the toilet, opened the door and hellooooooooooo the end of my innocence.
-the most stressful experience from my childhood hospital stayings was “did you defecate yesterday”? Because if you didn’t for a few days an enema was waiting
3 notes
·
View notes
Text
I get a lot of flack from anti-vaxxers, anti-maskers, and other fuckwits about my words on the COVID-19 Pandemic and in particular the response to it in the US. I pull no punches about it, I believe firmly that the previous administration and ANYONE who enables them and their policies are complicit in the deaths of all of these people. They belong in prison.
I'm not going to fucking apologize for believing that. The fault for all of this belongs directly in the laps of the Republican Party. If you believe otherwise, you're WRONG. I can bring the receipts.
I've been pretty isolated during all of this. I went into lockdown on March 11, 2020 and I'm technically still there. I now work from home, and even though I've been fully vaccinated for two months now I still go out masked. I may never eat at a buffet again. Sorry Sizzler, but I've learned how to make your cheese bread.
I ripped a tendon in my left knee in May of 2020. I had to go to the hospital, but I was out in a few hours with crutches. I would joke with people that I'm now out of hinged joints to break.
But in July my cough returned with an attitude, and I picked up an infection. Not Covid, but it all made me pretty sick. So that you understand, I have what's called "Chronic Cough Syndrome". I've had it since I was 8. No one knows the cause or the cure. Believe me, we've looked. I just start coughing, and after a few months, I stop. It can be treated but I just have to live with it until someone comes up with something we haven't tried before.
Doctors have gotten into fistfights over whether or not I have Asthma. I don't, but sometimes Asthma medications work for a bit. To be honest, I've had this for so long that sometimes I don't even notice when I cough. It's just part of the wonder of being me.
I took the Pandemic seriously. I stayed home, I socially distanced, I got real familiar with teams, bluejeans, and zoom. I did a LOT of cooking. Started making bread. Watched the country fall apart at the seams and commented on it from my own little pocket of safety. I contributed a new song to a fund-raising effort for nurses. I did my part to stay safe, but my cough had other ideas.
Anyway, this time my coughing got pretty severe and I finally agreed to go to the hospital. As stated above, turns out I had picked up an infection. Combine that with my cough and I showed all of the symptoms of a severe case of COVID-19.
I'd been careful, but the hospital staff were all very cross with me. If I had COVID, I just exposed all of them, and the main nurse who tended to me had already been quarantined that same month for a different exposure. When the test came back negative the tension in the emergency ward calmed down immensely and everyone treated me kindly and professionally - I was a patient with something they knew what to do with and didn't bring plague into their house.
I spent 4 days in the hospital but the worst part, scariest part, was the wait to move from the Emergency Room to a private room. I came to the hospital in the late afternoon. I finally got my bed nearly 12 hours later, a good 8 hours after my test for COVID had come back negative.
I needed to be hospitalized, and needed a bed, and there weren't any. I had to wait for someone to either be discharged or to die.
I got my bed at 4 in the morning. Someone had died. Musical chairs was played and I was finally moved out of the Emergency Room.
It's really hard to understand how sobering that is without experiencing it. Many years ago, before we even knew about AIDS, I had the honor of donating blood and seeing it get used in a surgery mere minutes later. I became a regular blood donor at that moment - I felt so happy and alive that my blood had been used to save a life mere minutes after I had donated it (I'm O Negative) that I became a life-long believer. I donated every time I was eligible from that moment forward until a blood infection disqualified me from ever donating again 20 years later.
This was just the opposite. The guy with a cough and a treatable infection had to wait for someone on a ventilator to stop breathing. Someone with COVID died so that I could get a bed. They never knew this had happened, and I never learned who they were. Some random person died so that I could get better.
Try sleeping after that realization hits you. I couldn't. I barely slept the entire time I was there.
Despite the fact that I wasn't in the "COVID Ward" I got to see the effects first-hand. The newly disinfected bed and room I had was previously occupied by someone moved up to the Covid Ward. They in turn had moved up there after a ventilator was taken away from a patient who died. Staff rotated through different wards on different shifts. My first nurse was rotated into the Covid Ward. My next day nurse had just rotated out. I have never in my life seen a group of people look so haunted by their day to day lives.
A well-liked member of their staff was on a ventilator. So was a priest who worked in the hospital. I had never seen in person a "Code Blue". There were six of them my first day. There is also a "Code Black". It's much worse.
My wife and daughters weren't allowed to visit me. When your daily soundtrack is nothing but medical staff talking about the good and the bad, terrible television and the moaning/screaming of your new neighbors getting that visit from family is a huge stress relief. It wasn't available this time. I didn't see my family again until I was discharged. There was no outside world.
I admit that being in hospital during all of this, even though I myself didn't have COVID, shook me. When you're in hospital mostly what you deal with is yourself and your own condition, and getting the hell out of there as soon as you can. This time I was not only aware of the people around me, their conditions, their suffering and their recoveries, but I was also aware that a whole section of the building was dedicated to people who were going to die, and that the people who were treating me were also treating them.
This was as close as I got to the Pandemic. When I got home I fucking STAYED THERE. I went to the grocery store and the pharmacy and that was it. That was life for MONTHS.
Our grocery store was fantastic - they enforced social distancing and masks with gusto. They cleaned EVERYTHING. It had been a 24 hour store but converted to shorter hours so that the down time could be spent cleaning. Aisles were made one-way.
The first time I saw someone in the parking lot without a mask I have to admit that I lost it. I screamed at them (a white couple about my age), "PUT YOUR FUCKING MASKS ON YOU FUCKING MORONS!" Understand, I'm a fairly large man with a deep voice and have been a professional singer for decades and have played sax even longer. I'm loud and imposing. Everyone within 50 feet turned and stared at the couple. Okay, me first then the couple.
It's possible they didn't speak English. They exchanged a few words in Russian to each other and then masked up.
I've been known to let my temper show. I try not to because I know it's there and I know it's terrible. I've worked for decades to keep it in check and I just let it all out, screaming at a couple of rando Karens 20 feet away from anyone else who hadn't put their masks on yet. I had to acknowledge that this affected me profoundly. I'm dealing with that.
I've lost friends to COVID. One of my neighbors spent almost 3 months on a ventilator and survived it. Some of my friends have lost family. It hurts. It all hurts. It has changed me.
Some of you have noticed that I've been pretty productive in 2021 in terms of music, after not releasing material for over a decade. This whole experience has changed me, changed my perspective. I was already an angry liberal but I'm far angrier and much more liberal now than I was. The album I worked on forever essentially no longer exists. The person I am now couldn't make that album. I am excising demons and allowing the new to come in and take its place.
And you know what, so far, I'm okay. I'm still here. I intend to stay. In fact, what I intend to be the first song from my next album in its own way deals with the fact that I don't understand depression - I've never experienced it.
But I have to admit that I'm grateful to have family and friends in my life who accept me as I am, who provide unconditional love and support and I hope I do for them. I have the occasional doubt that I'm as good a friend/family member as I can be. I can be an ass sometimes.
(A couple of my long-time friends have just done spit-takes. "Sometimes????")
Because the scariest thing about what we've all been through - what I've been through - is that we have changed so much that I'm not sure that the people who know me best would be my friends if they met me as the person I am now. I am changed.
And the odds are pretty good that you have too. This is something we're all going to need to deal with, or we're lost.
Please, don't be lost.
And because it still needs doing, because the pandemic is still going strong as ever among the anti-vaxxers, the science deniers and the Republicans, please support our nurses. Here's the album I'm on that is still to this day, long after falling off the charts, raising money for them:
1 note
·
View note
Text
Obligatory Covid-19 related post (kinda)
So, as we all know, there is a pandemic at the moment. As someone with a chronic illness (and as someone whose partner has active asthma), I am concerned. I don't want to catch coronavirus and I certainly don't want my partner catching it. If we did, it would be extremely serious for us both.
I work for the NHS and so am classified as a key worker (as is my partner). Where he can work from home, I can not. I am currently at home due to an IBD flare-up (which I'll get into in a bit), but I will eventually need to go back to work. The thing is, even though my work’s Occupational Health has advised I stay away from patient interaction, my job is patient-facing, so I'm not sure what I'll be able to do when I do go back. And on top of that, what if I pick up coronavirus on my way home or from an asymptomatic colleague? There's not a lot I can do other than opt to self-isolate. This will have to be something I discuss with my manager when I return to work.
As for the flare-up, it started about three weeks ago. We had just got back from the Netherlands and I was starting to experience stomach cramps. I put this down to having tensed during the flights as I dislike flying, namely take-off and turbulence. I thought they'd go away after a bit but no, they kept getting worse. Two weeks ago, it got to a point where I was having to sit down because I would get nauseous if I was stood for too long. That's when the fatigue began to set in, to a point that my colleagues were starting to notice. They would tell me that I didn't look well and that I should go home. I didn't want to. The fact is, I haven't been at this job for a year yet and my probation period had already been extended due to two instances of sickness (both of which I was hospitalised). If I called in sick, that would be three instances within the first nine months of my employment and I didn't want to risk losing my job (despite all the reassurances from my colleagues to the contrary).
Come Friday of that week, and I am feeling awful. Thankfully, Friday afternoons are quiet for me at work so I didn't have to do a lot. I decided I would use the weekend to rest and evaluate my condition Monday morning. I think they saw it coming as my manager was not surprised when I called in. I was signed off for two weeks. That two weeks is almost up and, unfortunately, I am not feeling much better. If anything, the pain is worse. I'll be speaking to my GP again Monday to extend my sick note. It sucks but I have been advised by my GI to stay at home if I am experiencing flare symptoms. Hopefully, things will settle down soon and I'll feel well enough to return to work.
Anyway, to everyone who reads this, whether you have a chronic illness or not, stay safe.
#ulcerative colitis#colitis#Inflammatory Bowel Disease#ibd#working#wokring with ibd#flare#flare up#flare-up#coronavirus#covid-19#work#nhs
6 notes
·
View notes
Text
The Actual Coronavirus diet…according to HealthMessenger
On March 23, the World Food Programme issued guidelines on the “do’s” and “dont’s” of eating while on quarantine. In last week’s article, I gave my take on each of the 7 tips on keeping a healthy diet in the face of coronavirus…according to the WFP…
Some of you subsequently reached out to ask what my guidelines would be. Even though I have not personally contracted the virus…yet…and havent had to quarantine, I did preventatively tweak my diet;
Full Disclosure…
As some of you already know, I strongly advocate for low carb diets, especially when tackling auto-immune diseases such as type-2 diabetes, high blood pressure, asthma, etc… . I myself have recently adopted a modified Ketogenic diet in an attempt to rebalance my macros to boost my immune system. The “modified” part comes with the addition of low GI fruits(strawberries, raspberries, kiwi, apples, pears, apricots, tomatoes) and low GI starches(sweet potatoes) around workouts in order to maintain a high metabolic rate. I have also started supplementing with Vitamin D in order offset the lack of sun exposure. That’s enough about me though… . Let’s see what the science has to say…
Low-carb nutrition and immune function
On Number 15, 2019 a study published in ScienceImmunology showed that mice fed a Ketogenic diet for seven days were protected from a lethal flu virus by increasing the number of specialised immune cells in their lungs. But interestingly, this protection only came once the mice had metabolically adapted to the high-fat diet. Giving exogenous ketones without the metabolic adaptation did not confer the same benefit. Obviously, that’s a far cry from saying a keto diet will do the same for influenza in humans or for COVID-19, simply because 1)Humans are not mice and 2)something tells me we can’t do the same study where we purposely infect people with a lethal influenza strain. To be completely honest, the paper is incredibly dense with detailed discussion of the immunologic and genetic responses, but I think the basic conclusion is good enough. The metabolic adaptation to a ketogenic diet can affect the function of the immune system to the point where it can prevent a lethal infection. But one question we should ask is, if we follow a diet that is proven to help with weight loss and metabolic health and may also beneficially affect immune function, wouldn’t it be worth trying? What do we have to lose?
Quality, quality, quality…
So, now more than ever, you might want to jump on a low-carb diet. I am not going to debate which LCHF diet is the best, simply because there is no clear cut answer to that question and also because I have partially answered that question in a previous article. Having said that, the quality (nutritional density) of the food you choose must prevail over the underlying food category (fruits vs vegetables vs meat vs etc…) promoted by the diet you eventually decide to pick. I don’t care wether you are vegan, carnivore or anything in between, the quality of the ingredients/foods you pick must be of the highest quality possible. That is as organically grown as available in your area. You are better off eating a grass-fed, grass finished steak over an “enhanced” apple(genetically modified with added sugar). Vice versa, you are better off eating an organically grown apple from your grandmothers’ apple tree over an antibiotic treated piece of meat. The same rule of thumb applies across food categories. Simply pay a bit more attention to the labels and do not hesitate to ask your well-intentioned butcher/gardener.
Cook your Food
France’s health and safety agency (ANSES) convened an expert group to investigate whether the COVID-19 disease can be potentially transmitted via contaminated food.
In light of the scientific knowledge available, ANSES has suggested transmission through food could occur if a person infected with the virus prepares or handles food with dirty hands – and contaminates it.
“This could concern all types of food (animal or plant products),” noted the agency. “Furthermore, while there is no evidence to suggest that consumption of contaminated food can lead to infection of the digestive tract, the possibility of the respiratory tract becoming infecting during chewing cannot be completely ruled out.”
As with other known coronaviruses, the novel coronavirus is sensitive to cooking temperatures, ANSES continued. “Heat treatment at 63°C for four minutes (temperature used when preparing hot food in mass catering) can therefore reduce contamination of a food product by a factor of 1,000.”
ANSES has reiterated that cooking food and observing good hygiene practices when handling and preparing food are effective at preventing contamination of the novel coronavirus.
Load up on fruits, vegetables, nuts and seeds
This one sounds like a no brainer…until you adopt a low-carb diet. Studies after studies have shown that the consumption of fruits, vegetables, nuts and seeds is obviously a common recommendation when it comes to strengthening ones immunity. I would recommend 2-3 pieces of low GI fruits(below 50) per day and at least 5 vegetables(below 30) a day. As far as nuts and seeds are concern, choose raw over salted. Portions will vary on an individual basis. A hand full per day is good rule of thumb though. Forget about the rainbow
Stay the hell away from refined carbs and sugars
I know how tempting it can be to reach out to cookies whilst binging on the latest Netflix series, awaiting for the quarantine to end …but please…dont… .
Laboratory evidence suggests sugar impairs white blood cell function and triggers acute rises in blood sugar, leading to an increased risk of infections and complications. Therefore, it would make sense that we want to limit these blood sugar elevations. Refined carbohydrates and simple sugars are two of the biggest offenders for blood sugar spikes and should therefore be eliminated.
This is not to say that studies show avoiding these foods results in fewer infections. (We don’t have that clear evidence.)
However, one simple solution is to use the measurement of your own blood sugar as a guide. If higher blood sugar is associated with more complications, it makes sense we want to limit that. I suggest measuring your blood sugar either with a regular glucometer or, even better, with a continuous glucometer (CGM) if you have access to one. If the foods you eat cause your blood sugar to rise above 140mg/dl (7.8mmol/L), consider eating something different.
Again studies show that a low-carb, moderate protein, higher fat diet effectively reduces blood sugar and can even reverse type 2 diabetes. We don’t have proof that this will “boost your immune system,” but it may help keep blood sugars in check which may be associated with decreased infectious risk.
Chicken soup/bone broth
Treating colds and the flu with chicken soup may be the most popular urban myth of all time. Surprisingly, it may not be 100% a myth. One study showed chicken soup “inhibited neutrophil migration,” which the authors suggest could improve our ability to recover from infections. However, this is one of those instances where laboratory findings may not translate to clinical improvements such as fewer or less serious infections. But it’s hard to argue with a tasty homemade soup with chicken(grass-fed), a few low-carb veggies, and plenty of real salt. Immune booster or not, it sounds like a great meal for a period in self-isolation.
Herbs and Spices
Turmeric
Turmeric is a spice commonly used in Indian and Asian cuisine, including curries. It contains a bright-yellow compound known as curcumin, which emerging research suggests might enhance immune function. However, there isn’t any convincing evidence showing that it helps fight viral infections yet. On the other hand, adding turmeric to your food adds flavour, and taking a curcumin supplement is unlikely to cause any harm in otherwise healthy people. If you have any medical conditions — especially if you take blood thinners — check with your doctor before supplementing with curcumin.
Echinacea
Echinacea is an herb that can reportedly help prevent the common cold. But is this reputation well-deserved? A recent systematic review of randomised trials found that echinacea may possibly have a mild protective effect against upper-respiratory infections but doesn’t appear to reduce the length or severity of illness. While it’s impossible to say whether it might offer any protection against COVID-19, it appears to be safe to take on a short-term basis. If you’re at high risk, you may consider taking it for the next several weeks.
Garlic
Garlic, a popular and pungent herb with a characteristic aroma, is widely believed to have antibacterial and antiviral effects, including helping to fight the common cold. A 2014 randomised controlled trial did find that people who took a garlic supplement had fewer colds and recovered more quickly from colds than people who didn’t take garlic. Although this is encouraging, this is just one study. Other high-quality trials are needed to confirm whether garlic is truly beneficial for the common cold or other upper-respiratory infections. For now, enjoy garlic for its zesty flavour and unmistakable aroma rather than counting on it to boost your immunity during the coronavirus pandemic.
Supplements
Vitamin C
For decades, Vitamin C has been used to help prevent the common cold. Among other functions, this vitamin can help maintain healthy skin that provides a barrier to germs and other harmful invaders. In addition, some — but not all — studies suggest it may improve the function of certain white blood cells that fight infection. In addition, there is conflicting evidence about the potential mortality benefits of high dose Vitamin C for patients with sepsis, the most severe form of systemic infections. While it’s unclear whether taking a Vitamin C supplement is beneficial for COVID-19, for most people there’s no harm in taking up to 2,000 mg per day (the upper limit set by the National Academy of Medicine).
For smokers and high-risk individuals, it’s definitely worth considering. Vitamin C is water-soluble, so your body will excrete whatever you don’t need into your urine. However, at very high doses, Vitamin C may cause diarrheas or increase the risk of kidney stones (especially in men), so be sure not to exceed 2,000 mg daily.
Vitamin D
As both a hormone and a vitamin, Vitamin D plays a number of important roles in health. In recent years, people have taken very high doses of Vitamin D with the intention of boosting immunity. But is this an effective tactic? A 2017 systematic review of 25 randomised trials found that taking a Vitamin D supplement seemed to have a mild protective effect against respiratory-tract infections in most people, but provided much greater protection in those who were very deficient in Vitamin D. If your Vitamin D levels are low, you may have a better chance of staying well if you supplement with 2,000 IU per day (or more, with medical supervision). Many — perhaps even most — people are deficient in vitamin D. So it’s probably wise to take a Vitamin D supplement right now, especially if you’re at increased risk for COVID-19. Of course, your body can make Vitamin D on its own when your skin is exposed to sunlight, so try to get some sun whenever you can. How much sun depends on the time of year and your location. A good starting point is 15 minutes of exposure to a large body part (such as the torso or back). Just remember to avoid sunburns, as excess sun exposure carries its own risks
Zinc
Zinc is a mineral involved in the white blood cell response to infection. Because of this, people who are deficient in zinc are more susceptible to cold, flu, and other viruses. One meta-analysis of seven trials found that supplementing with zinc reduced the length of the common cold by an average of 33%. Whether it could have a similar effect on COVID-19 isn’t yet known. Taking supplementary zinc may be a good strategy for older people and others at increased risk. If you decide to take zinc, make sure to stay below the upper limit of 40 mg per day, and avoid administering nasally, due to the risk of olfactory complications.
Fasting
With all the focus on how certain foods affect your immune system, you may also wonder, what about fasting? As counterintuitive as this one may sound, fasting protocoles are proving more and more effective at boosting immune functions..
One study in mice showed that fasting, or more specifically refeeding after a fast, restored immune function that had been suppressed by chemotherapy. During the fasting period itself, however, fasting appeared to impair the immune system, especially in the elderly. This is a very important caveat to keep in mind, especially if yo have already been infected by COVI-19. Fasting should only be used a a preventative tool.
Over the long term, intermittent fasting and refeeding will boost the immune system. Keep this in mind in preparation for the next pandemic. Sorry but yes, we will likely face other, more or less severe, pandemics in the coming years/decades. Better be safe than sorry. However, during an acute pandemic, where the immediate risk of infection is higher than usual, it may not be a good time to try fasting, given the potential for a temporary decrease in immunity.
This may sound surprising for those who have heard the phrase, “starve a fever.” The theory is that humans have evolved to not feel hungry and purposely avoid food during an acute illness as a protective mechanism, which may in turn limit nutrients the virus needs to replicate. To be clear, this is all conjecture without any quality supporting evidence.
Other evidence suggests that ketones are beneficial for immune function, and perhaps that could be why some recommend fasting. But considering all of the data together, if that were the case, you are better off adopting a keto diet and not fasting. Based on the limited data available, I suggest not fasting longer than 36 hours during the outbreak of the coronavirus, especially if you are older than 60 years old. It’s logical that you can continue with shorter-duration time-restricted eating, although there is no data on this either.
There you go…my official guidelines on keeping a healthy diet in the face of coronavirus…
Coming up next: Why you cannot “catch” a virus
Until then…take care of you and your loved ones.
To Your Health
The Health Messenger
5 notes
·
View notes
Text
Surviving Covid 19
Close friends, family, and some people who follow me as a musician on social media are aware that I was recently very ill with Covid 19. I live alone which presented a few challenges, and am still recuperating, well over a month later.
I haven’t said too much about it online, apart from trying to battle the disinformation about the disease out there, and privately providing information and moral support to those who have become ill more recently than I, and who felt lost and confused by the system in place.
However, I feel that it’s time that I spoke about this publicly, in the hope of helping others and perhaps saving a few lives.
The biggest problem we face right now is a lack of easily accessible information. I have research experience, which helped me a great deal to understand what was happening to me, but not everyone has that skill set and therefore I hope my experience will be useful.
In the UK they have three symptoms listed on the NHS website, just three. This is wholly inaccurate and has cost lives. I am a member of a number of Covid survivors groups, and most of those in these groups share similar experiences to myself, and are still in recovery.
Symptoms of Covid 19 include, but are not limited to the following -
1. Fever ( I had this on the 1st night, but didn’t get another one until week 2, when I was hit with fevers, cold sweats and teeth chattering chills which came and went for the next 2 weeks. They do come and go intermittently for longer than that while you recuperate but they aren’t the same)
2. Dry Cough ( I personally only had this on the first night, I never really had a cough for the rest of the illness)
3. Anosmia ( I personally didn’t experience this, I did however experience a severe change in taste and smell in week 2. Everything smelled and tasted of chemicals which was extremely unpleasant. I would have preferred a complete loss than the experience that I had. Thankfully it passed after a few days, though I still occasionally detect that chemical taste momentarily)
4. Fatigue (This is a hard one to explain as I’ve never really experienced anything like it. That seems to be the opinion of all others who have had it too. On Wk1 I just felt exhausted, on Wk 2 it hit me like a sledgehammer. I now understand this was silent hypoxia. I could barely get out of my chair to walk 6 feet to the kettle. Just picking something up off the floor was like climbing Mount Everest. Just because you are not in bed doesn’t mean you aren’t seriously ill. I am now on week 10 and am still experiencing fatigue after mild exercise, and this is something most Covid survivors are reporting. My advice would be to get an oximeter and call the paramedics if it drops below 95. I didn’t have one but they suspect it was probably very low)
5. Shortness of breath/tight chest ( I didn’t really notice this but I wasn’t able to move around much with the fatigue)
6. Fainting/blacking out (This happened to me on week 2. I probably needed oxygen support and could also have been low blood pressure due to the blood rushing to my organs in defence against the virus, but either way I should have had medical support. I have been told since that I could have died. 111 symptom checker was still not advising anything other than staying at home, and didn’t have the option to add any of these symptoms)
7. Gastric problems ( Many people contract the gastric version of Covid 19/ This is not something that 111 has much information about, and is potentially as lethal as the mainly respiratory version. I was eating relatively normally but lost my appetite on week 2 with the change in taste and smell. I personally started with the gastric symptoms in week 3, vomiting and diarrhoea on day 21, diarrhoea for the next few days, and morning gastric issues for the next 2 weeks. Stomach is still iffy on and off)
8. Reduced lung capacity ( This seems to be very common. My local pharmacy is reporting a huge increase in the number of inhalers being prescribed, and I’m aware of many people globally with the same issue. I’m a professional saxophonist and singer, and despite having the gastric version, have currently got the lung capacity of an 85 year old woman with asthma.)
I have no idea if my condition will improve, chest X-rays have shown nothing, which I understand is quite common. Fibrosis may only show up via CT, and needs early treatment, but my GP is not allowed to refer anyone for CT scans, or to the respiratory clinic in my area, as they are only dealing with cancer patients currently. There is no post Covid treatment in place, my GP and others I have spoken to, are angry at the lack of information being fed to them from NHS England. They are being left to wing it, and do their own research. This very important stage, dealing with the long and sometimes complicated recovery from this disease has not been considered by this government. I find this unsurprising given that they chose to adopt a fire fighting approach to the outbreak. This needs action now though, to prevent long term health damage which could be avoided if dealt with early in recovery.
Other symptoms include rashes, headaches, ear and eye problems, dehydration, dizziness. brain fog and confusion. Also feet can develop purple lesions on the soles which then disappear. I experienced that very briefly, plus a very short period where the soles of my feet turned black, which I believe relates to low blood pressure, but it did frighten me when it occurred.
I personally felt quite dizzy, was inhaling large volumes of water during the illness and am still experiencing brain fog and blurred vision at times, something that others are also reporting. I began craving fresh fruit and ice-cream, probably Vitamin C and Potassium at the end of the illness. This disease lowers potassium levels and I’ve been following my body’s wishes by eating a lot more fresh fruit, especially bananas, for potassium.
During the period of fevers I was avoiding using paracetamol except at night, as fever is important for making your body a hostile environment for the virus. I’m also on other medication for long term medical issues, including blood thinners, which may have protected me against the blood clots that seem to be a big problem with this disease, but I can’t be certain of that, so I’ll leave those studies to the scientists.
I also found that baths helped me feel a lot better but I did find it very hard to get in and out of the bath during the second week, so it probably wasn’t that good an idea, as I was living alone.
Many people may have mild symptoms for a few days, fever, cough etc. and then feel absolutely fine, others may show no symptoms at all.
You also hear about the tragic deaths, and people who can’t breathe so need to be supported with oxygen and/or ventilators.
What they aren’t telling you is that there are a large number of people, yet to be counted in the official figures, and/or tested, that have a serious form of the disease, but don’t end up in hospital, due to the incorrect list of symptoms.
111 in the UK have failed to identify people with dangerously low 02 levels, who suffer from what is being called ‘happy hypoxia’, due to the woefully inadequate symptom checking system.
Most of the people I know that have had the virus, and there are many, have gone through this horrific illness without help, or recognition, because of the flawed symptom check and lack of testing. I have only been offered a test this week, long after I would have tested positive, but even then the site wouldn’t allow me to order one. I now need an antibody test, but can’t get one of those at present either.
We deserve better.
1 note
·
View note
Text
To my 19 years old self,
Get ready. There is a lot to unpack in this letter. If you think you already faced the worst during your childhood and adolescence, well, you are wrong. You will face or even climb a mountain starting on your 21st birthday. Your ideal perspective of the world will be shattered as you enter the corporate world.
As tiring as it can be in your last term of your college year, you started to apply to different companies to start off your career in the corporate world as early as it can be with the thought of this will be just a gap year before you enter medschool. Spoiler alert: you’re still not in medschool at 23 years old, but let's save it for later. The lack of rest or gap between the academe and corporate world plus the tumultuous responsibility you had in your first job ate you away. You were the only HR personnel in your first job, anomalies went around the company from the unstable finance team, fraud, team leads taking part in agents’ issues, lack of benefits and permit to operate, and an operation manager who is having an affair with another agent. You faced it alone and tried to make things right, but the corporate world does not work that way. You chose to stay for 6 months to show that you are strong and not easily swayed, but you realized is it worth representing the company who doesn’t have your back. However, it was too late. You are slowly withering. This is the first lesson I would like you to know, learn to say no. It is hard, but you need to draw boundaries so you will not lose yourself in the name of pleasing other people. Get out of your box. Dye your hair. Wear the clothes you always wanted to try, but couldn’t because of “rules”.
You found yourself working in a stable company 2 weeks after you resigned. Your colleagues are amiable and easy to work with, your boss is patient and knows how to recognize your strength. However, the fear of making mistakes is back. As a newbie, it is normal to make mistakes, but you are so scared that someone will shout at you in the office or slap you when you make mistakes. Your cough gets worse, you need to take medical leaves to be confined. As you go back to the office, you will find yourself having a hard time breathing while travelling to the office. You thought it was your bronchitis or asthma so you decided to resign to recuperate despite having medical clearance, and also, to avoid making mistakes in the office. I want you to know that it is not your lungs acting up while you are travelling to the office, you are having an anxiety attack.
Before anything else, I would like you to know that before you leave the company, a certain virus started to spread around the world. As the world stops because of the virus, your own world becomes darker. Remember your 1st breakdown, you were 15? It took a year before it happened again, but your breakdown that year happened twice. Until yearly, it became worse and worse. The intervals between your breakdown become shorter. Remember when you were so proud of not being able to sleep or still being lively even with a short amount of sleep? As your birthday comes nearer, you are slowly, completely losing yourself. Paranoia and delusions that everyone hates you or will hate you because you did not reach their expectation. 2 weeks before your birthday, the stress is at the all time high. You cried while asking yourself what you did wrong for everyone else to think that you are such a bad person. The emotional pain and voices were getting louder. That was the first time you ever hit yourself to the headboard of the bed. It was painful, but felt good. Finally your pain makes sense, because you felt it physically. On the day of your birthday, it isn’t good as well. You see you went back to your grandmother’s house to cut the expenses, but your mental health got worse there. You heard your step-grandfather and grandmother fighting about her giving money to you as a gift. A day after that you will try to commit suicide, thinking that everything else will be solved when you are dead. You always think that if you weren’t born your parents will have a better life. If you weren’t born, you will never feel the pain. The only person who stopped you from committing suicide was Mama Rhea. She will tell you that you will smell bad once you drown in the Marikina river. As funny as it could be, somehow, I am thankful for my kaartehan. The next day you will punch your cousin. You hate hurting people, because you know how it feels. You hate disappointing them, but all the pent up anger and bitterness will finally surface. Honestly, it felt good. You started laughing hysterically while crying when your grandmother said she can’t take anymore of you and called papa to report what you did. You are conscious, but cannot move. It didn’t take a while for your grandmother to realise, they lost you. You are not sane anymore. You sat there for hours without moving, until papa arrived. You went to the CR convincing yourself to drink the muriatic acid like tea, but your father caught you. He slapped you and kicked you, because he said he knows that it will help you communicate and wake you up. The 2nd lesson I would like you to know is you can forgive, but also you have a choice not to reconnect with the person who brought you so much pain. Days will pass by and you are still not yourself. Forcing you to read a bible, confessing to your sins, and attempting to exorcise you, but none of that work. It was not until you were able to use your phone, when Mama and you decided to have you checked with a neuropsychiatrist.
Newsflash: You have Bipolar type 2 disorder. You cannot carry the baggage of physical, mental, and verbal abuses anymore. It pulled you down to the bottom. It is irreversible. A psych graduate who got a psychological disorder? It will take for a while to finally accept the knowledge of having a disorder. Your journey of healing will take a while. Weekly therapy, side effects of your 7 medications, and lots of crying and convincing yourself that the fire in your eyes will be back. There will be doubts and attempts to let go of your dreams, but please don’t let that side win. It’s just a disorder, not a death sentence. There are people who will invalidate you or will make you feel they are an ally, but in the end they will get fed up with you. Telling you to learn how to fight and stand on your feet. They will never understand that we cannot control our episodes. Just to let you know, I still get episodes. There are breakdowns and hump on the roads, but we need to keep on walking in this path of healing for ourselves, not for others. You are on your own.
At 23, you will have a failed business and relationship. On top of that, you will get afflicted with COVID-19. It will be revealed to you on who are the people that are willing to stay with you despite your sufferings and emotional high. It will show you that no matter what happens or your relationship with them, you are not their priority. Painful? Yes. But you need to rise above from this experience. You will make plans ahead. You are still ambitious. You just had a detour, not a dead-end. You will still be great, Dei.

I will write to you again before you turn 25. Maybe, no, hopefully, it will be on a lighter note.
Cheering you always,
23 years old Deiriz

0 notes
Link
Does Smoking Cause Lung Cancer? The answers is yes. It is vital risk for lung cancer. Know the Symptoms and Prevention of Lung Cancer at Asthma Bhawna. Make an Appointment at Department of Pulmonary Medicine at Asthma Bhawan or call us on +91-9352934531
#what is the risk factor for lung disease?#Does Smoking Cause Lung Cancer?#Symptoms and Prevention of Lung Cancer#Best Lung Cancer Treatment Center in Jaipur | Best Lungs Cancer Diagnosis in Rajasthan#lung disease#treatment of lung cancer in india#Best Lungs Cancer Diagnosis in Rajasthan#Best Lungs Cancer Diagnosis in India#lung#Lung Cancer Diagnosis Centre in Jaipur|Ebus#Lung disease treatment in Inida#Lung Cancer Diagnosis Centre in RajasthanEbus#child health#Childhood Asthma: Symptoms Diagnosis and Treatment | Asthma and Lung Cancer Treatment Center#Symptoms and Precautions of Covid-19 XE Variant in Children#what can protect your child against covid-19#asthma treatment#Asthma and Lung Cancer Treatment Center#what did asthma patients need to know during covid-19?#asthmaBhawan
0 notes
Text
I’m pregnant… should I get the Covid-19 vaccine?
There’s enough to worry about during pregnancy, even without a pandemic. As the vaccine rollout continues, there’s still concern over its impact on pregnancy. Covid-19 has added an entirely new layer of health anxiety for anyone expecting a child. That’s why one of the biggest questions on many pregnant women’s minds is if the Covid-19 vaccine is safe for them.
One drugmaker, Pfizer, will attempt to answer that question with a clinical trial of its coronavirus vaccine on pregnant women, the company announced last week. The results are not expected for months.In the meantime, how can pregnant women decide whether they should get the Covid-19 vaccine? What about those trying to become pregnant or those who are nursing?We asked CNN Medical Analyst Dr. Leana Wen for her advice. Wen is not only an emergency physician and public health expert; she’s also a mother to a 3-year-old son and a 10-month-old baby girl who was born during the pandemic.
CNN: Is the coronavirus vaccine approved for pregnant women?
Dr. Leana Wen: Technically, it’s not, but it is an option for pregnant women. Here’s why: The initial clinical trials did not include anyone who was pregnant or breastfeeding. Some women did become pregnant over the course of the trials, but because the research wasn’t intended to study the vaccine’s effect on pregnancy, there wasn’t enough data for the Food and Drug Administration to authorize the shot for pregnant individuals.Thousands of pregnant women have decided to take the coronavirus vaccine anyway. There have been no significant safety issues reported for these women. The US Centers for Disease Control and Prevention, the FDA, and other experts have stated clearly that all pregnant individuals who are eligible should have the choice to receive the vaccine.
CNN: If the vaccine is not specifically tested in pregnancy, why would pregnant women take it?
Wen: Pregnant women are at higher risk for severe complications from Covid-19. There is a higher risk of being hospitalized and ending up in the ICU for pregnant women compared to non-pregnant women. The risk is further increased for pregnant patients with underlying medical conditions.
Many pregnant women have decided to take the coronavirus vaccine.This is why medical organizations of OB-GYNs recommend that pregnant women are presented with the option of receiving the vaccine. The American College of Obstetricians and Gynecologists and the Society of Maternal and Fetal Medicine say that “given clear evidence of the dangers of Covid-19 in pregnancy, an absence of data demonstrating adverse effects associated with the vaccine in pregnancy, and in the interest of patient autonomy, ACOG and SMFM recommend that pregnant individuals be free to make their own informed decisions regarding Covid-19 vaccination.”
CNN: So how do you recommend a pregnant woman make this decision?
Wen: Here are the two things I’d urge my patients to consider. First, what’s your risk of exposure to Covid-19? Let’s say that my patient is a nurse or respiratory therapist who is treating Covid-19 patients. That person has significant occupational exposure and getting the vaccine could protect her substantially during her pregnancy. Perhaps she has a spouse who is in a high-risk profession, or she lives in a household where she cannot keep physical distance from a family member with exposure risk. That would weigh in favor of getting the vaccine now.Second, what’s your risk of having a severe outcome if you were to contract Covid-19? Pregnancy alone already predisposes a person to more severe illness, and if you have other underlying medical conditions, you are at even higher risk, because the risk is additive. Conditions like chronic lung, kidney, or heart problems; diabetes; high blood pressure; and sickle cell disease could worsen the effects of coronavirus. Patients who are pregnant and with these underlying medical conditions could substantially benefit from the vaccine.
The bottom line is that any risk of an adverse effect from the Covid-19 vaccine is theoretical and the risks of Covid-19 infection are not. Based on what we know of the vaccine, there is no reason to believe that it will have a detrimental effect on the pregnancy or the long-term health of either the mother or baby. Lack of evidence doesn’t mean it can’t exist, but this kind of theoretical very low risk needs to be weighed against the real and potentially very high risk of a severe outcome from Covid-19.This is the reason why many health care professionals who are pregnant have received the vaccine.
CNN: What about breastfeeding women?
Wen: We don’t have data to say unequivocally that the vaccine is absolutely safe for breastfeeding people. However, there’s no physiological reason as to why it would not be safe. Vaccines deemed to be of concern are those that contain live viruses. The Covid-19 vaccines currently authorized in the United States — and those that are in clinical trials here — do not contain any live virus. In fact, if anything, the vaccines could have additional benefits to the baby. Some recent research suggests protective antibodies might be transferred to the baby via breastmilk.
CNN: You were pregnant at this time last year. Would you have gotten the vaccine if it were available to you when you were pregnant or breastfeeding?
Wen: I’m a health care worker seeing patients, with high-risk occupational exposure, and I also have asthma. So yes, I would have received the vaccine if it were available when I was pregnant. By the time the vaccines became approved, I had stopped nursing. As soon as I stopped nursing, I joined a vaccine trial. If I were still nursing and had the opportunity to get the vaccine, I would have no hesitation to take it.
CNN: What would you say to people who want to wait until there are clinical trials that prove the vaccine is safe for pregnant and breastfeeding women?
Wen: I’d say that’s a reasonable choice, too. Everyone needs to make the best decision for themselves. A lot has been written about the ethics of vaccines in pregnancy. On the one hand, it makes sense to not include pregnant women in initial vaccine trials out of concern for them and their babies. On the other hand, it’s not fair to deny an entire group of people the benefit of vaccines. The majority of health care workers are women of reproductive age, for example.A lot of other vaccines actually have not specifically been tested in pregnancy but are routinely given because the proven benefits outweigh any theoretical risk. I think every patient needs to make the right decision for themselves and their family, in consultation with their health care provider.
It’s important to note that pregnant and nursing women aren’t in priority vaccination groups just by virtue of being pregnant or post-partum. If they are otherwise not prioritized to be vaccinated (for reasons such as a high-risk occupation or preexisting health condition), they need to wait their turn to be in the eligible groups, just like everyone else.
CNN: There’s some misinformation out there about the vaccine and fertility. Can you clear this up?
Wen: Yes. There’s absolutely no link between the coronavirus vaccine and fertility. This has been thoroughly debunked, and multiple medical societies around the world have come out with statements to this effect.
CNN: What would you say to women who are thinking of getting pregnant or trying to get pregnant? Should they get the vaccine?
Wen: If they are in priority groups to receive the vaccine and are able to, I’d say that they should. There’s no reason to hold off. Of course, they should always consult with their health care provider, especially if they have medical procedures planned. For example, if they are planning IVF procedures — maybe they don’t want to time their vaccines for exactly the same day as their procedures to avoid simultaneous side effects.Remember that the vaccines are very effective at preventing illness — especially severe illness — from Covid-19, but they are not 100% effective, and we still don’t fully understand if those who have received the vaccine can transmit the virus. Even after receiving the vaccine, people should still use caution.For pregnant patients, that means they can breathe a bit easier when going to their prenatal visits, but they should definitely still wear masks and abide by physical distancing guidelines in public places.Breastfeeding women, will have good immunity, but they won’t know whether their babies do, so keeping up good physical distancing for their babies will still be important. And for everyone, an abundance of caution is a good idea until more people can be vaccinated and we are closer to reaching herd immunity.Source: CNN
0 notes
Link
Mucous membranes line your nose, mouth, and eyes. The virus comes in contact with healthy cells and multiplies within them. It reaches and infects nearby cells. The lining of the respiratory tract gets inflamed. Hence, the infection and inflammation can even extend up to the lungs.
#what did asthma patients need to know during covid-19?#treatment of lung cancer in india#Best Lungs Cancer Diagnosis in Rajasthan#Lung disease#Best Lung Cancer Treatment Center in Jaipur | Best Lungs Cancer Diagnosis in Rajasthan#Lung disease treatment in Inida#Long-Term Lung Problems After Covid-19?#Covid Care Center in Jaipur#What Are The Long-Term Lung Problems After Covid-19?#lung complications.#coronavirus#covidー19#COVID-19 vaccine#best rehabilitation Centre based in Jaipur#omicron virus#how omicron virus affect asthma patient?#Omicron BA.4 and BA.5 detected in India#BA.4 and BA.5 sub-variants of Omicron#How Omicron Variants lead to a COVID surge in India?#Summer Allergy Symptoms That Similar Coronavirus Infection#lung complications
0 notes
Photo
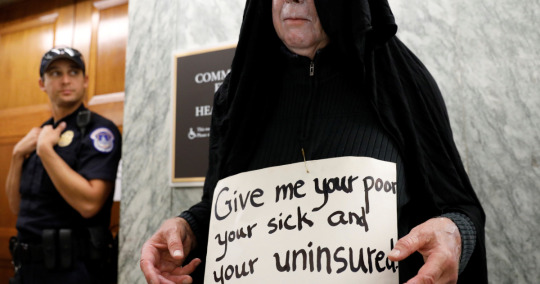
What is at stake when the US Supreme Court takes on Obamacare?
On November 10, the Supreme Court of the United States will hear a new case against the Affordable Care Act (ACA), the signature legislation of Barack Obama’s two-term presidency.
It will be heard by a court that is more conservative than Americans have known for generations, with its newest judge Amy Coney Barrett rushed into a vacant seat just days before the divisive presidential election. This tipped the balance of the already conservative-leaning nine-member court to a much more weighted 6-3 split in their favour.
The case, California v Texas, which deals with the constitutionality of the 2010 ACA (commonly known as “Obamacare”), is the latest salvo against a complex, intricate law that is loved, hated and misunderstood in the US, and that touches the lives of almost everyone in it.
The hearing comes just in the wake of Donald Trump losing the presidential election – even as he refuses to concede – while nearly a quarter of a million people have died from COVID-19, and as millions of American citizens have lost their jobs and their health coverage.

A 2018 group portrait of the justices of the US Supreme Court, including the now-late Ruth Bader Ginsburg who passed away in September 2020. Amy Coney Barrett was confirmed as her replacement in October, bolstering the conservatives on the bench [File: AP]
Healthcare in the US: A short history
Since the second world war, most Americans have known that good health insurance is tied to a good job.
But in the 1960s, two government options were created by the Lyndon Johnson administration: For Americans over 65, there was Medicare, a programme that has long been popular and difficult to cut due to its wide bi-partisan reach (everyone gets old).
And for the poor, there was Medicaid, which is administered individually by states, resulting in wide variations in who is eligible. In some states, for example, children were only covered by Medicaid if their parents earned less than half of what would put a family of three on the federal poverty line (approximately $9,000 a year at the time), while in other states, with more progressive policies, children would be covered if their family’s income was $55,000 for a family of three.
Despite these limited government options, health insurance was understood as a private enterprise, and across the insurance market, plans were shaped by the demands of hospital networks and providers.

In a photo from 2012, a woman opposed to healthcare reform, rallies in front of the Supreme Court in Washington [File: AP]
By the 2000s most insured Americans were covered by a private healthcare plan they chose through their workplace. In 2008, a family would, on average, pay $12,300 per year just to own a plan through their workplace, with additional co-payments for services, medicines, and therapies on top of that. That average premium also varied widely between states.
For those who wanted something else, or for the wealthy, self-funded private medical plans were available. In 2009, someone buying individual non-employer health insurance would pay about $3,600, or $7,000 if it also covered their family, but pay much higher deductibles for medical services. Many of these plans were not as comprehensive as employer-backed options.
For most insured people (59 percent of employee plans and nearly 90 percent of individual plans) there were lifetime caps on how much total coverage a provider would pay for. After that cap – sometimes one or two million dollars – was reached, insurers would stop covering, even if the treatment continued.
Hitting such a maximum might seem unlikely, but for someone receiving specialised treatments, or managing the care of a very sick premature baby, those costs could be exceeded within a few years or less, and the patient would be left to cover the remaining costs. A long-term stay in the ICU could leave a family in financial ruin.
Insurance companies considered future health complications liabilities, and charged higher costs or did not sell policies to people with so-called pre-existing conditions, affecting more than 100 million Americans in 2010. A pre-existing condition could be asthma, a family tendency towards high blood pressure, or a likelihood the patient would develop cancer.
Women are statistically more likely to develop diabetes and cancer than men and were disproportionately uninsured, in part due to the pre-existing conditions loophole. In 2010, 20 percent of women aged 18 to 65 did not own health insurance.

In a 2017 photo, a man walks by a healthcare insurance office in Florida [File: AP]
Black and Hispanic Americans were also insured at lower rates. In 2010, 13 percent of white working-age Americans, 20 percent of Black Americans and 33 percent of Hispanic Americans were uninsured. Among those who did have a plan, higher numbers of Black and Hispanic Americans were receiving Medicaid, which often delivered lower-quality care options. People of colour in the US are more likely to live in low-income families without access to an employer-sponsored option, and most private plans were out of reach. As a result of this lack of health insurance – along with other barriers to care – these groups are also less likely to receive preventive care, diminishing overall health outcomes.
For the uninsured patient walking into a clinic, price vertigo could quickly strike. With most doctors and nurses unable to tell a patient how much the eventual cost of a medical service would be, they would have to decide whether to receive treatment before knowing if they could afford it.
Typically for an insured patient, a medical provider would submit documentation of a medical service – a physical exam, a blood test, an MRI, for example. The insurance company negotiates reimbursement with the health network and the patient gets the bill after treatment has been delivered. Depending on how much their plan covers, the patient may pay a portion.
Meanwhile, medical interventions in the US have become more state-of-the-art, more expensive, and more common.
By the early 2000s, health spending accounted for roughly one-sixth of the US economy, the largest share in the world, but only about 85 percent of Americans had health insurance. Many of the millions of families left out were an injury or illness away from dire financial consequences.
The cost of care
Marleny, who prefers that Al Jazeera use only her first name, was one of the millions of uninsured. She lives in Framingham, Massachusetts, and is a single mother of 9-year-old twin girls and a 20-year-old daughter. She is an immigrant from Guatemala and used to live in California, where she had a basic insurance plan sponsored by her employer while she was pregnant. In addition to her premium, she paid $30 for a doctor’s visit and $500 for each birth.
When she moved to the Boston area in the cold winter of 2014, all of her daughters fell ill with bronchitis. She was scared to take them to the hospital.
“I waited a week to take them to the hospital. My daughters had a lot of fever and coughing, and I noted they were losing weight. My mother said, ‘You need to take them’,” Marleny explained in a phone interview.
The family of four was living in a single rented room and their car had not yet arrived from the west coast. But with her daughters’ conditions worsening, Marleny knew she had to do something. She borrowed a car from someone she knew, packed the twins, then two years old, and her older daughter into it and drove.
There were two things Marleny did not know when she walked into the Emergency Room at Metrowest Medical Center: that Massachusetts did have some state coverage plans available for low-income people, and that the first provisions of the ACA were just coming into effect. She thought of walking back out into the cold.
“I was scared that I might get a high bill. I told them I don’t have health insurance here, and I don’t know how much this will be.”
Her story mirrored others playing out in ERs across the US. She would soon discover that a reform bitterly fought on the national level was at that moment becoming available. Too concerned about her girls’ health to leave, she decided to stay.

In a photo from 2017, protesters gather across from Trump Tower to rally against the repeal of the Affordable Care Act in Chicago [File: AP]
Attempts at health reform
During his term, President Bill Clinton tried to reform the healthcare system – but failed.
Then, in 2006, Republican (then-governor) Mitt Romney succeeded in delivering Massachusetts, a wealthy liberal-leaning state, a form of universal coverage in which everyone was obligated to buy insurance. State-funded options were available to those making up to 300 percent of the figure that would put someone on the federal poverty line, and at-cost individual plans were regulated and sold in streamlined marketplaces. The reform was seen as radical as until that point no state had passed a plan compelling people to buy health insurance.
When Obama debated John McCain on national television ahead of the election in 2008, he said healthcare spending was a burden on the American people and vowed to tackle it. At the time, millions were out of work and hence health insurance, due to the “Great Recession”. McCain said he would solve the problem by sending a $5,000 tax credit to the average family, which they could use to pay for health costs (at that point, the average yearly premium for a family was more than $10,000). McCain said Obama’s plan would be so limiting that it would leave “Joe the plumber”, a made-up potential user, without any plan at all.
Obama was swept into the White House with a strong mandate, and his team set out to invest their political capital directly in the divisive issue.
“Both the politics and the substance of health care were mind-numbingly complicated,” the former president writes in his new memoir, excerpted by the New Yorker on October 26, 2020. “When I think back to those early conversations, it’s hard to deny my overconfidence,” he recalled.

In a March 23, 2010 photo, President Barack Obama signs the Affordable Care Act in the East Room of the White House in Washington [File: AP]
Democratic lawmakers drafted a 900-page bill containing hundreds of provisions. They hosted dozens of bipartisan meetings and held hours of public hearings with 200 witnesses. Senators from the Finance Committee grilled representatives from the health insurance industry, conservative think-tanks, interest groups for retired Americans and state regulators.
“A single provision tucked inside the bill could translate to billions of dollars in gains or losses for some sector of the health-care industry,” Obama reflected. It was early 2010 and the White House, the House of Representatives, and Senate were all controlled by Democrats. When it was clear that no Republican would support any law that reformed the health sector, the politicians pushed it through in a rare late-night holiday vote on December 24.
Obamacare’s bold approach
The ACA’s bold idea was to get more healthy Americans to own health insurance. This, the administration believed, would put more money into the insurance market and lower costs for everyone. The authors did it by introducing the “individual mandate”, a penalty for those who stayed uninsured, administered by Congress. Anyone who did not purchase a private plan would have to pay a fee to the Internal Revenue Service. Critics raged that the federal government was forcing them to buy something they did not want.
The ACA then clamped down on insurers by making them offer better individual plans for those without employer-sponsored options. It stopped the pre-existing condition loophole. It required insurers to include basic essentials such as emergency services, pregnancy and maternal care, and substance abuse treatment, many of which had been out-of-pocket extras before.
The law required these new individual plans to be sold in transparent marketplaces run by states, which would only offer plans that were vetted. Separately, the law dramatically expanded the free health coverage programmes for the poor and the elderly – Medicaid and Medicare – which had always missed millions who did not qualify according to their state’s criteria.
Lastly, the law invested billions in research for innovations to improve how health is paid for, and quality of delivery.
Don Berwick, a Harvard-educated paediatrician, had studied the quality of care for 30 years when he was appointed by Obama to lead this particular expansion in 2010.
“I told my staff three questions for any proposal: How would this improve care? How would this improve people in dire straights? How would this help reduce costs overall?” he told Al Jazeera.
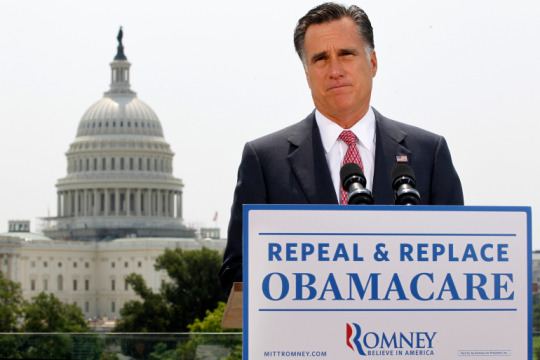
In a 2012 photo, Republican Mitt Romney spoke about the Supreme Court’s healthcare ruling in Washington [File: AP]
Berwick developed plans to expand the free services and prepare the state marketplaces for launch, before resigning 18 months later due to his recess appointment. He had been criticised by Republicans after saying Britain’s NHS, a government-paid system, could be an example for the US. Opponents, like the Republican senator from Wyoming, said his approach would ration care. Dr Berwick vigorously refuted that accusation. Berwick, who has long argued for healthcare delivery to be a government responsibility, is now president emeritus of the Institute for Healthcare Improvement.
“We don’t have evidence that market forces yield improvements that we’re after. Market induces competition instead of cooperation … The market system will not encourage [knowledge sharing] … Market systems tend to lead to behaviours that favour providing services to people with more money and not people with less money. We need exactly the opposite approach,” he told Al Jazeera.
Republican lawmakers and judges took aim at the ACA from multiple angles and, in 2012, Obamacare was challenged in the Supreme Court. The National Federation for Independent Businesses (NFIB) and 26 states argued the ACA forced small business owners to buy insurance for their employees, hurting the businesses. The court did not agree, but it did transform the ACA by declaring the individual mandate was a tax, not a fine. The change was subtle but would open an opportunity for that tax to be reduced by Congress.
The justices also ruled that the decision to expand Medicaid would be left to individual states. A dozen mostly southern states immediately stopped the expansion, leaving millions without promised insurance options. The NFIB said the “constitution has been undone”.
After more than three years of preparation, the ACA became active in 2014.
More than just crisis care
Sitting in the emergency room that January, Marleny knew her girls were too sick to leave untreated. A member of the staff told her not to worry, there were plans for her. One of the new advantages of the ACA was same-day enrollment, shrinking a process that had previously taken up to 45 days. The girls were prescribed antibiotics and sent home. Her family would need emergency services several more times that winter, but Marleny was now covered, as were her daughters.
She started to think of healthcare as more than something for a crisis. Marleny began visiting her own doctor regularly, going for mammograms and other preventive services, which were free.
“Thank God we have this programme,” she said. “If not, I don’t know what we are going to do. A lot of families like mine don’t have the money to pay for health insurance.”
Marleny is not unemployed. She works as an administrative assistant at an NGO that provides housing help to people in Massachusetts, making about $2,500 each month. She says her employer-provided plan costs $600 a month for the premiums alone, too expensive for her to afford. Her income, near the poverty line, makes her eligible for the subsidised plans Don Berwick helped expand. Her ACA-insurance costs just $45 per month; a visit to the doctor costs $18, medicine for the children costs her a few dollars.

A woman in Florida holds a sign in support of Obamacare in October 2020, ahead of the US election [AP]
Marleny’s insurance is available because Massachusetts receives federal money for people in her situation. Health Care for All, an NGO in the state, helps her navigate the process. For many years Hannah Frigand, the NGO’s director of education and enrollment services, received phone calls from people eager or desperate to secure a coverage plan.
“We hit a peak when the ACA was implemented,” she told Al Jazeera. Calls nearly doubled as the law was passed, and again when it was implemented four years later. Thousands of people had been waiting for better coverage.
Trump and the case against Obamacare
Donald Trump criticised the ACA in his very first speech as a candidate, calling Obamacare “a disaster”. He claimed, citing anecdotes, that patients would lose their health coverage, doctors would quit, and the health consumer would be stuck with ballooning payments. When he spoke in 2015, about 17 million new working-age Americans were insured who previously had not been before the law. The average family premium for employer-sponsored insurance had indeed gone up, as it had every year before and continues to today, but the cost of individual plans was falling. In his first day as president, Trump issued a broad executive order for government agencies to scale back as many parts of the ACA they could.
With control of both Houses of Congress in 2017, Republican lawmakers pushed forward bills to repeal and replace Obamacare. Their “skinny” version lowered the individual mandate to zero dollars, leaving the rule with no penalty. But their replacement preserved much of the ACA’s popular parts like coverage for pre-existing conditions, for children up to 26 years old under their parents’ plans, and the expansion of Medicare.
In an after-midnight vote on July 28, 2017, Republican Senator John McCain, who had been facing months of aggressive criticism from President Trump and who had just been diagnosed with a brain tumour that would take his life a year later, walked to the podium and held his thumb down for the cameras to see. The ACA would continue.

In a July 2017 photo, now-late Republican Senator John McCain looks on during a press conference about his resistance to the so-called “Skinny Repeal” of the ACA [File: Reuters]
Nisha Kurani studies the law and its effects at the Kaiser Family Fund (KFF), an organisation that tracks the medical insurance industries. In a phone interview, she said the loss of the individual mandate has, paradoxically, not had the impact many feared.
“Early on there were concerns that the market would destabilise. But that hasn’t happened. Premiums in the past years have gone down. Healthy people have not left the market as was predicted. And the financial health of insurers has dramatically improved since the early years of the ACA. We’ve seen that the marketplace has stabilised.”
At the start of the Trump presidency, 20 million new Americans were insured by the expanded programmes. The gap between uninsured Black and white Americans fell by four percent, and that between uninsured Hispanic and white Americans fell by over nine percent. The number of uninsured women halved in two years.
The White House under Trump pushed for many parts of the ACA to be undone. Obamacare blocked a type of short-term insurance option sold across states that had often driven consumers into medical debt: The user would buy one, undergo a treatment, and find it was not actually covered. The ACA limited these plans to 30 days, the Trump administration extended that to a full year with the option of renewal.
Watchdog organisations have documented how the websites for state marketplaces have been closed for hours or days during enrollment periods, due to “maintenance”, preventing people from finding health plans. Funding for public messaging about health insurance has been reduced. States have seen their waivers for innovation programmes cut. Some states have imposed work requirements for Medicaid, demanding that people who receive the subsidised coverage for the poor prove that they are employed, even though studies have shown that most on the programme already are working or have a good reason such as disability not to.
In one stirring example, money intended for medical research and other services was moved by the White House’s Health and Human Services director to pay for the detention of migrant children. These cuts have made a difference: the uninsured rate has been growing slowly since its 2016 low, creeping up by a few million people.

Democratic Senator Chris Coons spoke during the Supreme Court confirmation hearing for Amy Coney Barrett in Washington in October, ahead of the US election and court hearing on the ACA [AP]
The new challenge
This Tuesday, November 10, the ACA will again be challenged at the Supreme Court.
Texas, 18 other – traditionally Republican-led – states, two individuals and the White House say the whole law must be thrown out because the individual mandate is zero, “a law that does nothing”, the case says. The justices will first decide whether the two sides have what is called “standing”, they will ask whether the individual business owners have been injured by the ACA. It will be a difficult argument, as there is no penalty for not buying insurance. If the plaintiffs do not have standing, the case will be rejected.
The justices will then decide whether the ACA would have been written and passed had it been known at the time that the individual mandate would be unconstitutional. If the answer is yes, the individual mandate could be sliced off the law, or severed, leaving the rest intact. The court could rule that both the individual mandate and the protections for pre-existing conditions are unlawful, but leave states to decide which subsidies and other parts to preserve.
If the court agrees with the federal decision made in Texas and strikes down the law, the impact would be profound. It is estimated that 23 million people could lose their health coverage (20 million who gained it plus another 3 million who have had to find new plans since the start of the pandemic). States that have taken full advantage of the subsidies of the ACA would lose those funds in their budgets. Massachusetts may have to cut programmes that prevent Marleny from worrying whether rent, food or health costs come first.
“Pulling away the ACA would be, I think, a disaster for millions of people in this country,” Berwick told Al Jazeera. “They would be left high and dry, angry, their costs would soar … it’s hard to imagine the ACA being pulled away at this point without severe dislocations.”

President Donald Trump with Amy Coney Barrett, who was confirmed to be a Supreme Court justice in October 2020 [AP]
All eyes are now on Amy Coney Barrett, the newest justice. She was clerk to the court’s most famous recent conservative justice, Antonin Scalia, who dissented both previous healthcare rulings. Justices are not often public speakers, so Barrett’s verbal record has been combed over looking for clues as to how she could rule. She has said she supported the dissent in a previous case against the ACA – but as a law professor, not a judge.
In her confirmation hearings, she said the Supreme Court tends to rule in favour of severability, keeping most of a law if a part can be chopped off. Whether or not California v Texas prevails, this is unlikely to be the final case to challenge the ACA.
In 2020, the Affordable Care Act is still (mostly) law, and it is as popular as it is divisive. Most Americans want the whole ACA to stand, though most Republicans want to see it repealed. More than 90 percent of Democrats and two-thirds of Republicans do not want to see protections for pre-existing conditions disappear. Critics like the Cato Institute and Heritage Foundation write that the law is too expensive for both the government and for beneficiaries, and too limiting for the American consumer.
Under the ACA, more people are insured. Costs for individual insurance buyers have fallen, but costs for insurance through work have grown. Expanded Medicaid services are credited with saving tens of thousands of lives, protecting essential workers during the pandemic, and even slowing eviction rates in high-enrollment areas (one study suggested that low-income users were less frequently forced to choose between paying rent and paying for health costs).
The US is a country that has incredible health resources, but mixed outcomes. Measured against comparable nations, the US has better outcomes for its cancer patients and worse outcomes for maternal mortality, according to Kurani at KFF. Healthcare is a work in progress.
Berwick advocates taking a long view.
“If we can take a breath as a country and depoliticise this, there’s a lot to be learned. ACA is not a perfect law. It has many elements that could be better.
“I think the ACA, even as weakened now, can and should survive … Then we have to remember – it still left 30 million uninsured, so there’s work yet to do.”
. #world Read full article: https://expatimes.com/?p=13665&feed_id=15577
0 notes
Text
Reiterating Our Bullish Long-Term View on Stocks

Image: The NASDAQ 100 Index remains resilient, bouncing off support, after breaking out to new highs recently. Some of our best ideas are included in the NASDAQ 100, and our favorite concentrations include exposure to big cap tech and large cap growth. We continue to be bullish on equities for the long run.
By Brian Nelson, CFA
Hi everyone,
Hope you are doing great! First, I wanted to let you know that we're still working to get the second release of the survey out to you. Your participation in the survey will determine whether we launch a new business, so please do fill it out and keep a watchful eye out for it. I will let you know shortly after it's sent out so you may be able to find the email easier.
As for the markets, the good news keeps coming in. Supporting our thesis that the Fed/Treasury have your back (April 29), the Fed all but telegraphed yesterday that it is watching the equity markets closely (and will do anything to support them), as after just a small sell-off last week, it reiterated that it is going to start buying " a broad and diversified portfolio of corporate bonds to support market liquidity and the availability of credit for large employers," in addition to the investment-grade and junk bond ETFs it is already buying. With credit and liquidity concerns continuing to be off the table for the vast majority of the equity markets, more optimistic fair value scenarios can now be weighted more heavily within valuation models, and this sent the markets rallying heartily off the intra-day lows June 15.
In addition to unlimited quantitative easing and "whatever it takes, squared" Fed policy, today, June 16, the Trump administration announced that it is weighing a $1 trillion stimulus bill to help support the economy. While uncertainties remain regarding specifics of the bill (it might include state assistance, extension of unemployment benefits, etc.), the move is consistent with the outsize spending we expect to further bolster the bull case, "ICYMI -- Stay Optimistic. Stay Bullish. I Am." We continue to emphasize that, in light of unlimited QE and runaway fiscal stimulus, the longer-duration components of intrinsic values are expanding considerably, and as a result, fair values, themselves, are actually rising during this recession and pandemic [a good estimate of the value of the S&P 500 today may be between 3,530-3,920, as outlined in the following: "Scribbles and More Newsletter Portfolio Changes.]."
What's more, in addition to the large number of "shots on goal" to develop a vaccine, "Excited By COVID-19 Vaccine Candidates (May 18)," health professionals are also making tremendous progress on therapies, too. Just today, for example, it was reported that "low doses of dexamethasone, a generic drug used to lower inflammation for other illnesses, decreased death rates (among people with severe cases of COVID-19) by nearly a third in patients on ventilators and by one-fifth in other patients receiving oxygen." It is clear that the healthcare community is making huge strides in fighting COVID-19, and it now has a life-saving drug to combat the disease as the new standard care in severe cases. From where we stand, things are looking much, much better than they did in February/March. Here's the current situation with COVID-19,per BBC (nowhere near as bleak as it was a few months ago):
About 19 out of 20 patients with coronavirus recover without being admitted to hospital. Of those who are admitted, most also recover but some may need oxygen or mechanical ventilation. And these are the high-risk patients dexamethasone appears to help. The drug is already used to reduce inflammation in a range of other conditions, including arthritis, asthma and skin some conditions. And it appears to help stop some of the damage that can happen when the body's immune system goes into overdrive as it tries to fight off coronavirus.
From calling the top in February, to dollar cost averaging near the bottom in March, to "going fully invested" ahead of the market's surge, to staying positive on the markets as COVID-19 worries subside, we are again reiterating today our long-term bullish take on the equity markets. In our view, investors have yet to fully factor in the incremental value generation corresponding to the increased long-duration aspect of intrinsic value composition (see here, also see page 74-83 of Value Trap). For your convenience, the updated simulated Best Ideas Newsletter portfolio can be accessed here (login required), and the updated simulated Dividend Growth Newsletter portfolio can be accessed here (login required). Contact us at [email protected] if you may have forgotten your password.
All things considered, we remain excited about the newsletter portfolios, the track record of the Exclusive publication, and we continue to monitor the High Yield Dividend Newsletter portfolio closely, as we scour the markets for new options ideas. In case you missed it, we released the June edition of the Best Ideas Newsletter, which can be accessed here (pdf) yesterday. We remain bullish on the markets for the long run, and we continue to prefer exposure to big cap tech and large cap growth, arbitrary buckets that today capture many of the Valuentum stocks we include in the simulated newsletter portfolios. Many thanks again for your interest, and we're available for any questions. We sincerely hope you are enjoying your membership!
----------
Valuentum members have access to our 16-page stock reports, Valuentum Buying Index ratings, Dividend Cushion ratios, fair value estimates and ranges, dividend reports and more. Not a member? Subscribe today. The first 14 days are free.
Brian Nelson owns shares in SPY and SCHG. Some of the other securities written about in this article may be included in Valuentum's simulated newsletter portfolios. Contact Valuentum for more information about its editorial policies.
0 notes
Text
May 2020 Learning Network Resources
May is National Asthma and Allergy Awareness Month. Check out the Choosing Wisely Clinician Lists – Allergy & Immunology.
Blogs, Issue Briefs, Opinion Pieces and More…
Guidelines on Neuroimaging for Migraine. Physician’s Weekly. May 2020 “Determining when and how to use neuroimaging for migraine is an important issue that physicians face when seeing the 40 million Americans with migraine. Neuroimaging for suspected migraine is used for many reasons, including exclusion of secondary conditions that mimic migraine. Other reasons include medicolegal issues, busy practice conditions in which tests are ordered as a shortcut, providing neuroimaging to appease patient requests, and addressing concerns and expectations of referring clinicians.”
Pandemic effect: All other health care visits can wait. MDedge. May 2020 “A majority of adults are reluctant to visit health care providers unless the visit is related to COVID-19, according to survey conducted at the end of April.”
Reduced cancer screenings in Covid-19. Lown Institute. May 2020 “The authors of the EPIC report make it clear what is at stake–lives lost due to reduced screening. However, it is very likely this number is overestimated, given the high rates of inappropriate screening in the real world, and the potential negative effects of screening on overall mortality. While the true impact of the sudden halt in screening due to Covid-19 remains unknown, we have the opportunity to find out in the future. Such a drastic change in screening is unusual, so we should track the results of this historical experiment to better understand the actual health effects–both beneficial and harmful–of cancer screening.”
Soong C, Cho HJ, Shojania KG. Choosing quality problems wisely: identifying improvements worth developing and sustaining. BMJ Quality & Safety. April 2020 “In this issue of BMJ Quality and Safety, Ambasta and colleagues examined the impact of a social comparison and education intervention on routine blood test utilization at a single academic medical centre. Trainees and attending physicians each received their own performance feedback in comparison with a group aggregate. Compared with controls, the intervention groups ordered fewer routine laboratory tests (incidence rate ratio 0.89; 95% CI 0.79 to 1.00; p=0.048) with an associated cost savings of $68 877 in Canadian dollars (p=0.020).”
Journals
Prachand, VN. Medically Necessary, Time-Sensitive Procedures: Scoring System to Ethically and Efficiently Manage Resource Scarcity and Provider Risk During the COVID-19 Pandemic. American College of Surgeons. April 2020 “Hospitals have severely curtailed the performance of nonurgent surgical procedures in anticipation of the need to redeploy healthcare resources to meet the projected massive medical needs of patients with coronavirus disease 2019 (COVID-19). Surgical treatment of non-COVID-19 related disease during this period, however, still remains necessary. The decision to proceed with medically necessary, time-sensitive (MeNTS) procedures in the setting of the COVID-19 pandemic requires incorporation of factors (resource limitations, COVID-19 transmission risk to providers and patients) heretofore not overtly considered by surgeons in the already complicated processes of clinical judgment and shared decision-making. We describe a scoring system that systematically integrates these factors to facilitate decision-making and triage for MeNTS procedures, and appropriately weighs individual patient risks with the ethical necessity of optimizing public health concerns. This approach is applicable across a broad range of hospital settings (academic and community, urban and rural) in the midst of the pandemic and may be able to inform case triage as operating room capacity resumes once the acute phase of the pandemic subsides.”
Bonafide CP. Prevalence of Continuous Pulse Oximetry Monitoring in Hospitalized Children With Bronchiolitis Not Requiring Supplemental Oxygen. JAMA. April 2020 “In a convenience sample of children hospitalized with bronchiolitis who were not receiving active supplemental oxygen administration, monitoring with continuous pulse oximetry was frequent and varied widely among hospitals. Because of the apparent absence of a guideline- or evidence-based indication for continuous monitoring in this population, this practice may represent overuse.”
Siddaiah H, et alt. Preoperative Laboratory Testing: Review of “Choosing Wisely” Guidelines. Best Practice & Research Clinical Anesthesiology. April 2020 “Healthcare providers, primarily anesthesiologists, should remain cost-conscious when ordering specific laboratory or imaging tests prior to surgery based on available literature. We review the overall evidence and key points from the Choosing Wisely guidelines, identification of potential wasteful practices, possible harms of testing, and key clinical findings associated with preoperative laboratory testing.”
Mark TL, Parish WJ, Zarkin GA. Association of Formulary Prior Authorization Policies With Buprenorphine-Naloxone Prescriptions and Hospital and Emergency Department Use Among Medicare Beneficiaries. JAMA Network. April 2020 “Prior authorization is commonly used for buprenorphine-naloxone because of concerns regarding costs and diversion. These findings suggest that these concerns may be unfounded and that requiring prior authorization before one can access a buprenorphine-naloxone product may be more harmful than beneficial.”
Clark SD, Reuland DS, Enyioha C, Jonas DE. Assessment of Lung Cancer Screening Program Websites. JAMA Internal Medicine. April 2020 “Information on public-facing websites of US lung cancer screening programs appears to lack balance with respect to portrayal of potential benefits and harms of screening. Important harms, such as overdiagnosis, were commonly ignored in the sites evaluated, and most of the centers did not explicitly guide individuals toward a guideline-recommended, shared decision-making discussion of harms and benefits.”
Gupta A, et alt. Physician Practice Variability in the Use of Extended-Fraction Radiation Therapy for Bone Metastases: Are We Choosing Wisely? JCO Oncology Practice. April 2020 “Routine use of extended-fraction (> 10 fractions) radiation therapy (RT) for palliation of bone metastases is recognized as a low-value intervention by the American Society for Radiation Oncology. We examined contemporary practice patterns of, and physician characteristics associated with extended-fraction RT use. In this study, almost one fourth of patients received extended-fraction RT, and one third of physicians had an extended-fraction RT use rate of > 30%. Personalized feedback of performance data, clinical pathways and peer review, and updated reimbursement models are potential mechanisms to address this low-value care.”
Schrag D, Hershman DL, Basch E. Oncology Practice During the COVID-19 Pandemic. JAMA. April 2020 “In the space of a month, approaches and accepted norms of cancer care delivery have been transformed of necessity. Most of these changes would not have occurred without the pandemic. Although the immediate priority is to save lives, in the aftermath and recovery phase, evaluating the effects of COVID-19 on cancer mortality will be a priority. Planning for resuming cancer treatment and screening to mitigate harms is already underway. It is also likely that some changes provoked by the crisis will permanently transform how to treat cancer, in some cases perhaps for the benefit of both patients and their physicians.”
Media Coverage
Column: An opportunity to reimagine health care after COVID-19. Quad City Times. May 2020 “Fourth, the healthcare system will reassess low-value procedures and tests. The U.S. healthcare system spends more than $200 billion on low-value healthcare every year.”
How To Get The Most Out Of Your Virtual Medical Appointment. NPR. April 2020 “It may be frustrating to be told you’ll have to wait for an in-person appointment, but please know that when we say that, it’s done with your health in mind. I certainly miss seeing my patients in person. Telemedicine has plenty of limitations. But I also hope that we doctors can learn from this experience, and start using technology, in some cases, to offer our patients more convenient care. Especially now, when so much of daily life has been upended, “it’s gratifying to be able to offer this additional service to our patients,’ LeRoy says. ‘We can interact with them. They feel connected, and not marginalized or forgotten.’”






https://feeds.feedblitz.com/~/625425210/0/catherinemccracken~May-Learning-Network-Resources/
0 notes