Text
Long COVID patients have similar brain activity to those with dementia, UK researchers find - Published Sept 10, 2024
By: Kendall Staton
Some patients with COVID see similar brain changes to people with such neurodegenerative disorders as Alzheimer’s, according to University of Kentucky researchers.
As the COVID pandemic raged across the world in 2020, researchers came together to start better understanding the new disease. At UK, Yang Jiang, a professor in the Department of Behavioral Science, led a study digging into the long-term effects of the virus.
“We’re together trying to understand how the COVID virus goes from getting into the nose and the lung, to somehow affecting the heart and the brain,” she said.
“We think there may be a long COVID, which we still don’t totally understand. It’s likely a risk factor for other neurodegenerative diseases.”
Looking at the effects of long COVID, Jiang sought help from the UK Sanders Brown Center on Aging to better understand the lingering mental effects of the virus.
“They understand some of the neuroinflammatory processes and how oxygen and blood will go through the blood brain barrier and interact with the virus, and how that alters brain functions,” she said. “So we began to sort of put two sides of evidence together.”
Chris Norris, a professor in the Department of Pharmacology and Nutritional Sciences and researcher at the Sanders Brown Center, said they were able to find brain cells, called astrocytes, in people diagnosed with COVID reacting similarly to brain cells of people with neurodecline.
“(Astrocytes) regulate blood flow to the brain, they regulate the shuttling of metabolites from the blood to the neurons, they support synaptic connections in the brain. When astrocytes become reactive and inflamed, like they do in COVID, all of those things – the metabolism, the blood flow, the synaptic communication – are adversely affected,” he said.
Those same cells also affect blood flow. Alzheimer’s patients and long COVID patients could both experience decreased blood flow in the brain, said Bob Simpol, an assistant professor in the Department of Pharmacology and Nutritional Sciences and researcher at the Sanders Brown institute.
He called COVID a “risk factor” that could contribute to long-term cognitive impairment or neurodegeneration.
People experiencing inflammation of astrocytes will see symptoms like brain fog, lapses in memory or forgetting the name of common items. Norris said these symptoms go beyond misplacing your keys, to something more serious – like forgetting you had your keys to begin with.
The research also showed that the brains of people with long COVID had similar electroencephalography (EEG) patterns to people with dementia.
Jiang said EEG’s measure “brain age” by looking at the activity of brain waves.
“Our brain is active all the time, even when you’re resting and when you sleep. EEG can capture the synchronized neural activity at the scalp. So what we observed, in COVID-19 patients, is the same pattern we see in dementia patients, which is the brain literally slows down,” Jiang said.
A COVID diagnosis does not mean you have dementia. Instead, people who have been diagnosed with COVID should have their brain function checked regularly, to catch signs of deterioration early and promote intervention.
With early intervention, 40-60% of neurodegeneration symptoms are reversible, Jiang said. With this research, the team is pushing for patients who have had a COVID diagnosis to get regular neurological check-ups.
“You can now look at brain function pretty easily and non invasively with EEG, just as easily as taking your blood pressure or listening to your lungs,” Norris said.
“After your symptomatic, it may be a good idea to have your brain activity assessed.”
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator#long covid
71 notes
·
View notes
Text
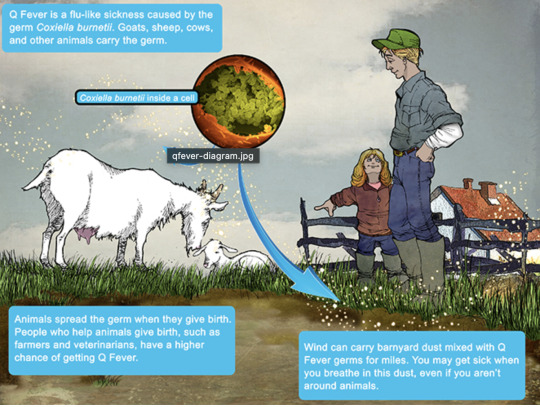
Q Fever
Aka, Query fever. What a weird name for a disease. Imagine telling people that's what you got.

in the 30s-40s, an Australian pathologist in QLD/Brisbane, came across an outbreak of the same or similar illness among abbatoir or slaughterhouse workers.
At the time, he called the disease "Q" fever or query as a temporary name until the pathogen could be identified. Unfortunately it stuck.
decades later, now nobel prize winner and virologist, MacFarlane Burnett isolated and identified the microbe responsible. I think this discovery contributed to his prize. i forget already.
Microbe responsible: Coxiella burnetti. Named for Burnett and HR Cox, the American bacteriologist who found the genus Coxiella where C burnetti falls under.
Initially they felt it was related to Rickettsia, responsible for Rocky Mountain Spotted Fever, but as science progressed, this was disproven.
Now for a Case Report
A 55 yo Italian man with a history of aortic valve replacement was diagnosed with pyrexia of unknown origin twice. Further signs included myalgias/splenomegaly/night sweats. The 2nd time he was admitted for PUO he deteriorated rather dramatically and was put on meropenem and teicoplanin.
A host of organisms was tested for on serological testing based on the man's travel and epidemiological history, all negative. Even a rheumatological panel was done, also less revealing. He also had a history of MGUS (a haem disoder), which is kind of a red herring here.
Cultures were negative, no vegetations were seen on a TTE - so they did consider IE. Which is an important differential for PUO.
Eventually a PET-CT was done (often favoured when investigations do not yield much for a sick patient with fevers), finally revealing a focus of infectious on his ascending aorta, where he'd also had previous surgery done. And in a round about way, they also further identified Coxiella Burnetti. He was treated doxycycline and hydroxychloroquine. As it's so rare in Italy, it wasn't really considered even though he mentioned rural travel.
Bottomline: Q Fever is an important consideration in the work up for culture negative IE. Further to this, always consider IE in the differentials for PUO particularly if they're at increased risk for IE (prosthetic valves, damaged valves, select congenital heart issues, previous IE). IE can present with night sweats, fevers, weight loss and splenomegaly. It can be insidious and chronic in nature. other risk factors can be more suggestive as we'll get into below.
Causative organism
Coxiella burnetti, it's a zoonoses - i.e. transmissible from animals. Special powers: very tough/hardy, can survive extreme environments (high temps and UV light etc.) over prolonged periods and is resistant to many common disinfectants/surface cleaners.
It's an intracellular pathogen and gram negative coccobacilli (PINK!)
name coccobaccili reminds me of cocopuffs.
it's mainly associated with farm animals, which the CDC so wholesomely displays on its website on Q fever (wtf).

goats, sheep, cattle typically (but many other animals, even birds, dogs and horses can be reservoirs)
in particular bodily fluids - amniotic fluid, placenta, faeces/urine, milk etc.
you can get it through unpasteurized milk and through inhaling it if it lands on dust in the area
ever visit a farm or petting zoo lately? OMG WASH YOU HANDS.

That said, it's typically inhaled in inorganic dust. You inhale it, it goes to the lungs, and then the bloodstream.
Increased risk for Coxiella burnetti (What to take on history of exposures and when to strongly consider it)
live on a farm or near one
exposure to a farm
work as a vet on a farm
farm worker, dairy workers, researchers on these animals/facilities
slaughterhouse/abbatoir
Also from CDC:
Clinical presentation
Most won't get sick after exposure and remain asymptomatic, a very small minority does. even though it is highly infectious.
incubation time is 2-3 weeks (consider this time in your history of exposure, did they work on the farm 2-3 weeks ago as opposed to yesterday).
Nonspecific acute infectious symptoms:
nonspecific systemic fevers/malaise/arthralgias/myalgias--> key is high fevers though and can be associated with headache and photophobia.
non specific GI - N/V/diarrhoea
respiratory ones - SOB or cough, consider it as atypical cause of community acquired pneumonia.
rare: hepatitis and jaundice (granulomatous) or encephalitis with neurological complications such as demyelinating disease or CN palsies, also haemolytic anaemia and HLH (yikes)

really it's the history of exposure that will lead you down the garden path to Q fever.
Chronic Q fever is perhaps worse, and can present as culture negative IE/PUO. Months/years later, as B symptoms as above above + LOW/LOA, night sweats. More likely to occur if you are predisposed for IE as above, have a weakened immune system for any reason, including pregnancy.
Chronic Q fever has a mortality of 10% if left untreated. About <5% of those with acute Q fever develop this if left untreated. Speculation is that it's more of an autoimmune process or abnormal immunological response to the bacteria.
To be honest, most who walk in the door with community acquired pneumonia get treated empirically for atypicals anyway, (standard course of doxycycline), so we hardly really ponder the question of Q fever in every patient. But if they present chronically and did not have atypical cover at the onset of acute symptoms, then it's something important to consider.
Other important conditions - can cause complications in pregnant women and 20% will get post Q fever syndrome. like chronic fatigue.
investigations
Serology! nice and easy. Look for IgG antibodies in the chronic presentation. Or PCR. Down side to serology - can take 2-3 days for the body to make said antibodies to the bacteria for detection. PCR can be done on any fluids/tissue sent.
Cultures useless, hence it fall under the umbrella of culture negative (hard to grow outside a host cell, it is an obligate intracellular pathogen).
Other hints on bloods (as serology/PCR takes time to return) - elevated or low platelet's, transaminitis with normal bili, opacities in CXR with hilar lymphadenopathy, CSF will show raised protein levels if done when encephalitis is suspected.
imaging can also support the diagnosis.. as illustrated by the case report.
Treatment
Acute disease - as standard for atypical bugs, doxycycline 100 mg BD for 14 days. Alternatives - TMP SMX or Clarithromycin.
Chronic Q fever or IE:
native valves: doxycycline and hydroxychloroquine (200 TDS) for 18 months
prosthetic: same but 24 months
why hydroxy: enhances the action of doxycycline (increases the pH of the phagolysosome)
Follow-up: look for 4 fold decrease in IGG
Sources:
CDC
Stat Pearls
Wiki as linked above
#australian history#medblr#medblrs#infectious disease#infectious diseases#q fever#coxiella#coxiella burnetti
73 notes
·
View notes
Text
STEVE PEOPLES and LAURAN NEERGAARD at AP:
WASHINGTON (AP) — If he wins next month’s election, Donald Trump would be the oldest person in U.S. history to be elected president. Yet the 78-year-old Republican nominee refuses to disclose new details about his physical or mental well-being, breaking decades of precedent. There have been limited snapshots of Trump’s health over the last year. After he survived an attempted assassination in July, Texas Rep. Ronny Jackson, a staunch supporter who served as his White House physician, wrote a memo describing a gunshot wound to Trump’s right ear. And last November, Trump’s personal physician, Dr. Bruce Aronwald, wrote a letter describing him as being in “excellent” health with “exceptional” cognitive exams. He noted that “cardiovascular studies are all normal and cancer screening tests” were negative. Trump had also “reduced his weight.” But those communications didn’t address more fundamental questions about Trump’s health, including his blood pressure, exact weight or whether he has continued using previously prescribed medication for high cholesterol — or even what testing he underwent. His campaign has also not disclosed whether Trump has been diagnosed with any diseases or received any mental health care after the assassination attempt.
That’s giving his political adversaries, including Democratic rival Kamala Harris, an opportunity to raise questions about his age and ability to execute the duties of the presidency into his 80s. “It makes you wonder: Why does his staff want him to hide away?” Harris asked recently as she needled Trump for withholding medical records, opting against another debate and skipping an interview with CBS’ “60 Minutes.” “One must question: Are they afraid that people will see that he is too weak and unstable to lead America? Is that what’s going on?” Trump’s doctors have long been opaque about his health, such as when his team at the White House initially downplayed the severity of his 2020 hospitalization for COVID-19.
[...]
Drawing a contrast with Trump
In an effort to draw a contrast with Trump, Harris released a letter from her doctor on Saturday that went into far more detail about her medical history, including a list of exams and the results. The letter said she has no heart, lung or neurological disorders, is at low risk for heart disease and up-to-date on cancer screenings. She takes medication for allergies and hives. She wears contact lenses, and her only surgery occurred at age 3, when her appendix was removed during an intestinal-related procedure. While the letter didn’t specify her weight, the 59-year-old vice president was declared to be in “excellent health” and to possess “the physical and mental resiliency” required to serve as president. Sensing an opportunity to put Trump on the defensive, the Harris campaign on Monday released a letter from more than 250 doctors and other medical professionals calling on Trump to release his medical records.
Still, it’s unclear that age will be a significant factor for voters. Polls found that voters were significantly less concerned about Trump’s mental capacity and physical health than they were about President Joe Biden’s when he was still in the race. Since Harris replaced Biden on the ticket, Trump’s advantage on the issue has diminished.
The AP bringing straight facts about Dementia Donald’s hiding of vital health details and how that would effect his 2nd term, which would effectively be a J.D. Vance Presidency.
A vote for Trump is essentially a vote to make Vance President, so vote Kamala Harris if you want a healthy leader in office.
5 notes
·
View notes
Text
i feel like i am going insane
this post was on my dash (screencapped bc don't go harass OP):
I'm not going to claim to be a TB expert, but any post talking about how we "have a cure" should be regarded as suspect. What happened in 1958 wrt TB treatment? I have no clue, and I just skimmed multiple reviews of the history of TB. If anyone knows, please tell me. In general the 1950s was the golden age of antibiotics, plus there was just a general better understanding of disease management in general, meaning fatalities from TB in Europe and North America tanked. But I could find no specific thing attributed to 1958.
What is the cure for TB? It's months of antibiotics, and even then clearance of the bacteria isn't going to be 100% of all patients. There's no specific miracle drug. There are vaccines (idk how effective, but they show up randomly in all sort of papers for having interesting and positive off-target effects, like improving blood glucose levels in diabetics), which is not a cure but IS a very important tool for stopping the spread and protecting people.
TB is tricky to manage. It can lay dormant in your lungs for decades. It's harder than the average bacteria to kill with antibiotics, and the course of antibiotics needed is so long that you end up with more logistical issues (what happens if you're in a remote area where you have limited supplies? how do you ensure patient compliance?). There are more and more antibiotic resistant strains appearing. A lot of effort and money and brilliant minds are dedicated researching TB and implementing strategies to manage it across the world. I'm sure there are ways to improve our approaches to managing and treating it, but TB is by no means a "neglected" disease. TB is not the example I would pick for how we have failed the world on a global level due to resource hoarding, unless you want to go into a much more nuanced discussion of why poverty is a huge risk factor for contracting it in the first place (due to things like overcrowding, poor living conditions, and poor access to healthcare, not because some specific miracle cure is being hoarded).
But I guess "the problem is we're not DISTRIBUTING the CURE" is much easier take for people to pat themselves on the back for having. TBH I think a lot of people feel safer when they think complex problems are secretly very simple ones that can be fixed by overcoming one singular evil.
33 notes
·
View notes
Text
What do you know about CAP?
"In the United States, community-acquired pneumonia is one of the leading causes of hospitalization and death, with approximately 6 million cases reported each year.1-6 The annual incidence of hospitalization for community-acquired pneumonia in the United States is approximately 650 adults per 100,000 population, corresponding to 1.5 million unique hospitalizations for the disease each year.6 Factors that increase the risk of community-acquired pneumonia include advanced age, chronic lung disease, chronic heart disease, cardiovascular disease, diabetes mellitus, malnutrition, viral respiratory tract infections, immunocompromising conditions, and lifestyle factors such as smoking and excessive alcohol consumption." File & Ramirez, "Community-Acquired Pneumonia," NEJM (2023), DOI:10.1056/NEJMcp2303286
2 notes
·
View notes
Text
Is Green Mold Dangerous? Health Risks Explained
Mold is common in homes and offices. Green Mold can grow in many places, leading to potential health effects if not addressed. can also grow in damp areas and cause various health issues. is a type that worries many people. We'll look into if Black mold and green mold are both types of mold that can be dangerous to your health. is dangerous, its Being aware of the health risks associated with black mold is important., and how to get rid of it.

Key Takeaways
Green mold can be a serious health hazard, causing respiratory issues and allergic reactions.
Identifying the type of mold present is crucial, as green mold may indicate the presence of more dangerous species.
Controlling moisture is essential to prevent mold growth. moisture and ensuring proper ventilation are key to preventing green mold growth.
Proper removal and remediation of green mold should be handled by professional mold removal experts.
Understanding the risks and taking proactive measures can help protect your health and safety.
What is Green Mold?
Green mold is a type of fungus that can be found in many places at home. It can be a problem and might make you sick if you don't stop it. Knowing about the types of mold in your home is crucial. different kinds of green mold and where they live is key to stopping them at home.
Green Mold Varieties
There are many kinds of green mold In homes, mold can grow in various forms, like Cladosporium, Penicillium, and Aspergillus, which can pose health risks. These types of green mold can be particularly dangerous to your health. green mold types can make you sick and grow on many things, such as walls, wood, and food.
Where Green Mold Grows
Green mold likes damp, humid places and does well where air doesn't move much or where it's wet. You can find it in places like bathrooms, kitchens, basements, and where there's water damage or high humidity. You might need to test for mold to know what kind it is and how bad it is.

Knowing about the species of green mold and where they like to live is important for stopping them. If you have a lot of green mold, you might need a professional to help get rid of it and keep it away.
Is Green Mold Dangerous?
Many people worry about mold and if it's bad for their health. Green mold is one type that worries people. It's important to know if it's safe or not.
Green mold can make mycotoxins. These are bad for humans. Being around these toxins can cause breathing problems, allergies, and even worse health issues. Mold Type Potential Health Risks Aspergillus Respiratory problems, allergic reactions, and in severe cases, lung infections Penicillium Allergic reactions, asthma symptoms, and potential toxin production Trichoderma Respiratory problems, skin irritation, and potential toxin production can be caused by various species of mold.
The risks from green mold Mold infestations depend on many factors, including moisture levels. This includes how sensitive you are, how much mold there is, and how long you're exposed. People with weak immune systems might get sicker from it.
If you think there's green mold around, act fast. Get experts to check and fix it. This can keep you and others safe from health problems.

Health Risks of Green Mold Exposure
Green mold might look safe, but it's not good for your health. Being around green Mold spores can lead to a green mold infestation if not properly managed. can cause breathing problems and allergic reactions. These can really affect how you feel overall.
Respiratory Issues
Breathing in green mold can cause health issues. Mold spores are a common issue in homes, especially when dealing with green mold in your home. can make your lungs and airways upset. You might start coughing, wheezing, or feel short of breath. If you're around mold spores a lot, it could even lead to serious lung diseases like asthma or pneumonia due to exposure to mold.
People with weak immune systems or lung problems are especially at risk. They should be very careful around green mold.
Allergic Reactions
Green mold can make some people allergic. This can cause sneezing, a runny nose, itchy eyes, and skin rashes. In bad cases, it can make breathing hard or cause anaphylaxis, which is very serious and needs quick help from a doctor.
Don't ignore green mold if you see it. Fixing the problem quickly is key to keeping you and your family safe and healthy.

Identifying Green Mold
Green mold is a type of mold that looks green. It's often seen on plants, damp places, and where moisture builds up. Not all green molds are harmful, but knowing how to spot them is key.
Appearance and Characteristics
Green molds in homes and on plants look unique. They can be bright green or more like olive green. Their texture can be fuzzy or slimy, depending on the type and where it grows.
Green mold starts as small, round spots that can get bigger over time.
Some green molds look powdery or dusty, while others seem wet and gooey.
These molds love damp, humid places and can grow on wood, paper, fabrics, and even food.
Not all green molds are bad, but they can be a problem. It's good to deal with them quickly to stop them from getting worse.

Preventing Green Mold Growth
It's important to stop green mold from growing in your home. You can do this by controlling moisture and improving air flow. This way, you can prevent green mold, prevent green mold growth, and prevent future mold.
Moisture Control
Moisture makes green mold grow. To stop mold, fix leaks and improve drainage. Use a A dehumidifier can help prevent mold growth in your home by reducing moisture levels. to keep humidity levels right. Check for and fix any water damage quickly.
Proper Ventilation
Good air flow is key to stopping mold in your home from spreading. It keeps moisture levels down and stops mold from growing. You might need to install exhaust fans, open windows, or update your HVAC for better air flow.
By doing these things, you can greatly lower the chance of green mold. This keeps your family healthy and safe from mold growth in your home.
"Preventing green mold growth is a crucial step in maintaining a healthy, safe living environment."
Green Mold Removal and Remediation
Dealing with green mold is important. It's not just ugly; green mold can also grow and be harmful to your health. That's why getting it right with mold removal and remediation services is key.
Experts in professional mold remediation companies are best for green mold. They have the right tools and knowledge to prevent mold effectively. To remove green mold effectively, consider mold testing to identify the source. You can prevent mold growth by ensuring that the area is kept safely dry. Trying to do it yourself can spread the mold more.
The steps for professional mold remediation are:
They check to see how much mold there is and where it came from.
They make sure the mold doesn't spread by sealing off the area.
They use special ways to remove mold, like HEPA vacuuming and treatments.
They get rid of things that have mold on them.
They fix the moisture problem to stop more mold from coming back.
Choosing professional mold remediation services is the best way to get rid of green mold. This way, you keep your family or workers safe and protect your property from green mold. Service Description Benefits Mold remediation is essential to prevent a green mold infestation in your home. This process gets rid of mold and stops it from coming back. It makes your indoor space safe and healthy again. It also keeps your property's value up. Green Mold Removal They use special methods to remove green mold and stop it from spreading. It deals with the special problems of green mold. It makes sure everything is clean and free from harmful mold spores. Expert Mold Removal Experts with lots of training and experience do this work to prevent mold infestations. It means you get the best results. They follow the best safety and practice rules.
Working with a professional mold remediation company means your green mold removal and mold remediation will be done right. You'll get a safe and healthy place for you and your family.
Conclusion
Green mold can be a big health risk. It can cause breathing problems and allergies. Knowing about the The dangers of green mold can include health effects that you should know about green mold. is key.
If you find mold at home, work, or elsewhere, act fast. Identify, prevent, and remove it to keep safe.
Learn about different green molds and how they grow. Know the health issues they can cause. This way, you can watch out and act early.
Use good moisture control and keep air flowing well. Get help from experts for mold removal. These steps help keep your places safe from green mold.
Knowing how to deal with green mold is powerful. Stay informed and take action to keep your space mold-free. Your health is important, especially when considering the health effects of mold exposure.
Q: What is green mold and is it dangerous?
A: Green mold refers to various types of mold that appear green in color, including some that can be harmful. While not all green mold is dangerous, certain types can cause health problems, especially in individuals with respiratory issues or weakened immune systems.
Q: How can I identify green mold in my home?
A: To find green mold in your home, look for patches of green growth on damp surfaces, such as walls, ceilings, and floors. Signs of mold can include a musty odor and visible discoloration, particularly on spoiled food or wet materials.
Q: What causes green mold to grow in my home?
A: The causes of green mold often include excess moisture, humidity, or water damage in your home. It can thrive in damp environments, which may arise from leaks, poor ventilation, or condensation.
Q: How can I remove green mold safely?
A: To remove green mold, you can use a mixture of water and detergent or specialized mold removal products. However, for extensive mold problems, it’s best to consult with an expert mold removal service to address any mold growth effectively and safely.
Q: Are there different types of green mold?
A: Yes, there are various types of green mold, including species like Cladosporium and Penicillium. Each type of mold can vary in its characteristics and potential health risks, so it’s essential to identify the specific type of mold growth.
Q: How do green mold spores affect health?
A: Green mold spores can affect health by triggering allergic reactions, respiratory issues, and other health problems, particularly in those who are exposed to mold or have sensitivities. Prolonged exposure to mold can lead to more serious health concerns.
Q: Can black mold be mistaken for green mold?
A: Yes, black mold and green mold can sometimes be confused due to their appearance. However, black mold is typically more dangerous and associated with more significant health risks compared to some types of green mold.
Q: What are the risks associated with green mold in my home?
A: The risks associated with green mold include potential health problems for occupants, particularly respiratory issues, allergies, and other complications. It’s important to address any mold growth promptly to minimize these risks.
Q: What should I do if I see green mold on my food?
A: If you see green mold on your food, it’s advisable to discard it, as mold can produce mycotoxins that may be harmful if ingested. Always inspect food for signs of mold and err on the side of caution.
2 notes
·
View notes
Text
Understanding Heart Disease: What is Heart Disease
What is Heart Disease?
Heart disease, also known as cardiovascular disease (CVD), encompasses a range of conditions affecting the heart and blood vessels. It is the leading cause of death worldwide, causing significant morbidity and mortality. The term "heart disease" is often used interchangeably with "cardiovascular disease," although technically, cardiovascular disease includes all diseases of the heart and blood vessels, while heart disease specifically refers to conditions affecting the heart itself.
Types of Heart Disease
Coronary Artery Disease (CAD): CAD is the most common type of heart disease and occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to plaque buildup (atherosclerosis). This can lead to chest pain (angina), heart attacks, and other complications.
Heart Failure: Heart failure, or congestive heart failure, happens when the heart muscle is unable to pump blood efficiently, leading to a buildup of fluid in the lungs and other tissues. Causes include CAD, hypertension, and cardiomyopathy.
Arrhythmias: These are disorders of the heart's rhythm, which can be too fast (tachycardia), too slow (bradycardia), or irregular. Common arrhythmias include atrial fibrillation and ventricular fibrillation, which can significantly impact heart function.
Heart Valve Disease: Heart valve disease involves damage to one or more of the heart's valves, affecting blood flow within the heart. Conditions include stenosis (narrowing of the valve), regurgitation (leakage of the valve), and prolapse (improper closure of the valve).
Congenital Heart Defects: These are heart abnormalities present at birth, ranging from simple defects like a hole in the heart's walls (septal defects) to more complex malformations. They can affect how blood flows through the heart and to the rest of the body.
Cardiomyopathy: Cardiomyopathy refers to diseases of the heart muscle. The heart muscle becomes enlarged, thickened, or rigid, which can lead to heart failure or arrhythmias. Types include dilated, hypertrophic, and restrictive cardiomyopathy.
Pericarditis: Pericarditis is inflammation of the pericardium, the thin sac surrounding the heart. It can cause chest pain and fluid buildup around the heart, affecting its function.
Causes and Risk Factors
Heart disease is influenced by a combination of genetic, environmental, and lifestyle factors. Major risk factors include:
High Blood Pressure (Hypertension): Hypertension forces the heart to work harder to pump blood, leading to the thickening of the heart muscle and potential heart failure.
High Cholesterol: Elevated levels of cholesterol, particularly low-density lipoprotein (LDL), contribute to the formation of plaque in the arteries, leading to atherosclerosis.
Smoking: Smoking damages the lining of blood vessels, increases blood pressure, reduces oxygen to the heart, and raises the risk of heart disease.
Diabetes: Diabetes significantly increases the risk of heart disease. High blood sugar levels can damage blood vessels and the nerves that control the heart.
Obesity: Excess body weight strains the heart, raises blood pressure, and increases the likelihood of diabetes and cholesterol problems.
Physical Inactivity: A sedentary lifestyle contributes to obesity, hypertension, and other heart disease risk factors.
Unhealthy Diet: Diets high in saturated fats, trans fats, cholesterol, sodium, and sugar can lead to heart disease by raising cholesterol levels, blood pressure, and weight.
Family History: A family history of heart disease increases one's risk, suggesting a genetic predisposition.
Age and Gender: Risk increases with age, and men are generally at higher risk earlier in life than women, although women's risk increases and can surpass men's post-menopause.
Symptoms
Symptoms of heart disease vary by condition but may include:
Chest pain or discomfort (angina)
Shortness of breath
Pain, numbness, or coldness in the legs or arms
Fatigue
Lightheadedness or dizziness
Palpitations (irregular heartbeats)
Swelling in the legs, ankles, and feet
Diagnosis and Treatment
Diagnosing heart disease often involves a combination of medical history review, physical examination, and diagnostic tests such as:
Electrocardiogram (ECG or EKG)
Echocardiogram
Stress tests
Blood tests
Cardiac catheterization
CT or MRI scans
Treatment strategies vary based on the specific type of heart disease and its severity and may include:
Lifestyle Modifications: Healthy diet, regular exercise, smoking cessation, and weight management are crucial for preventing and managing heart disease.
Medications: Medications can control risk factors such as hypertension, high cholesterol, and diabetes, or treat specific heart conditions like arrhythmias and heart failure.
Procedures and Surgeries: Angioplasty, stent placement, bypass surgery, valve repair or replacement, and implantable devices like pacemakers or defibrillators may be necessary for severe cases.
Prevention
Preventing heart disease involves managing risk factors through:
Maintaining a healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats
Regular physical activity
Avoiding tobacco use
Controlling blood pressure, cholesterol, and blood sugar levels
Regular health screenings
Stress management techniques
Understanding and addressing heart disease through lifestyle changes, medical management, and preventive measures is crucial in reducing its impact and improving overall heart health.
2 notes
·
View notes
Text
Yahoo News: Research uncovers stunning factor behind nearly 200,000 cases of dementia each year: ‘Toxins for the brain’
For years, health issues, like heart attacks, respiratory problems, and decreased lung function, have been linked to air pollution.
Now, new research has added another disease to the laundry list of health issues that may be caused by dirty air: dementia.
What happened?
CBS News reported that new estimates from researchers published in the journal JAMA Internal Medicine showed that annually nearly 188,000 dementia cases in the U.S. may have been caused by air pollution.
The study, one of the latest to spotlight health risks from air pollution, looked at how specific causes of air pollution seem to be more strongly tied to dementia than others.
It indicated exposure to pollution from wildfires and agriculture as having the strongest links to increasing a person’s risk of Alzheimer’s disease and other types of dementia later in life.
Research findings were based on survey data that spanned decades and is backed by the National Institutes of Health. The data was then combined with air quality modeling, according to CBS.
“They model all sources at once: coal-fired power plants, agriculture, wildfires, traffic — all these different emission sources — and then they turn off the source in the model one at a time. And then they can see the difference in what levels are there with the emissions sources and what are there without them,” Sara Adar, associate chair of epidemiology at the University of Michigan’s School of Public Health, told CBS News.
Researchers focused on particulate matter with diameters that are generally 2.5 micrometers and smaller in air pollution that is breathable and found that direct emissions aren’t the only concern.
In addition to the smoke directly from wildfires, other toxic molecules travel with the smoke as fires burn through communities. Farming was also found to worsen serious air pollution.
“Farms will release a lot of ammonia gas,” Adar said, “and then in the air with the sunlight and other pollutants out there, they’ll react to make particles, and those particles are what we see are likely toxins for the brain.”
Why are these findings concerning?
With wildfires and agriculture being the leading causes, if we don’t change our habits, we will likely see even more cases of dementia apparently caused by air pollution.
Agriculture is another significant contributor to air pollution, with livestock accounting for 14.5% of human-made planet-heating pollution, according to the United Nations. Overall, agriculture makes up over 11% of this type of pollution, per the Center for Climate and Energy Solutions.
Further, extreme temperatures and less rainfall — both becoming increasingly common, at least in some places, as our planet heats up — make for longer and worse fire seasons, meaning air pollution from wildfires will only worsen as well.
What can I do to help?
To protect ourselves and others from this risk, we must all work to reduce the amount of pollution released into the air.
“Unlike many other common risk factors for dementia (e.g., hypertension, stroke, and diabetes),” the study’s authors wrote, “exposures to air pollution can be modified at the population level, making it a prime target for large-scale prevention efforts.”
We can do this by moving away from single-use plastics, switching from gas-powered cars to electric vehicles, and utilizing clean energy sources whenever possible.
#dementia#brain toxins#pfos#pfas#toxic chemicals#Research uncovers stunning factor behind nearly 200#000 cases of dementia each year: ‘Toxins for the brain’
4 notes
·
View notes
Text
The Myth of Normal: Trauma, Illness and Healing in a Toxic Culture (Gabor Maté, 2022)
“The gender gap in health is real, if underappreciated.
Women are more subject to chronic disease even long before old age, and they have more years of poor health and disability.
“Women have it worse,” a leading U.S. physician wrote recently, pointing out that women are at much higher risk of suffering chronic pain, migraines, fibromyalgia, irritable bowel syndrome, and autoimmune conditions like rheumatoid arthritis.
As noted in chapter 4, rheumatoid arthritis strikes women three times more often than it does men, lupus afflicts women by a disproportionate factor of nine, and the female-to-male ratio of multiple sclerosis has been rising for decades.
Women also have a higher incidence of non-smoking-related malignancies. Even when it comes to lung cancer, a woman who smokes has double the chance of developing the disease.
Women also have double men’s incidence of anxiety, depression, and PTSD. (…)
Early childhood mechanisms of self-suppression are reinforced by persistent, gendered social conditioning.
Many women end up self-silencing, defined as “the tendency to silence one’s thoughts and feelings to maintain safe relationships, particularly intimate relationships.” This chronic negation of one’s authentic experience can be fatal.
In a study that followed nearly two thousand women over ten years, those “who reported that, in conflict with their spouses, they usually or always kept their feelings to themselves, had over four times the risk of dying during the follow-up compared with women who always showed their feelings.”
As at home, so on the job. Another study showed that for women with non-supportive bosses, the squashing of anger—a natural adaptation to an environment in which to self-express would be to risk the loss of employment—increased the risk of heart disease.
Recall from chapters 5 and 7 this array of self-abnegating traits that predispose to disease: a compulsive and self-sacrificing doing for others, suppression of anger, and an excessive concern about social acceptability.
These personality features, found across all autoimmune conditions, are precisely the ones inculcated into women in a patriarchal culture.
“I was denying myself as a person, denying my own desires, my wants,” the first responder Liz said.
“I was not paying attention to what I needed. Everyone else was far more important. My job was way more important than any concern that I had. I wasn’t listening to myself in any regard.”
That “not listening to self” in order to prioritize others’ needs is a significant source of the health-impairing roles women assume.”
18 notes
·
View notes
Text
A few weeks ago several people I hang out with all got COVID around the same time. My partner and I were clearly exposed. But we didn't manifest normal 'sick' symptoms: no fever, no runny nose, no cough, no shortness of breath.
However my partner noticed she overheated more than normal when doing a more strenuous task on a cool morning. Similarly, I was doing heavy garden work on a cool morning and felt overly warm and tired, and took longer than normal to feel rested and bounce back.
I noticed repeatedly I had more trouble than normal, thermoregulating, over the next few days. It resolved quickly, I'm now back to normal in the thermoregulation department.
The last time we both had COVID, we noticed this same phenomenon during our recovery, even though that time we had a fever and she tested positive (I never did.) We each experienced unexpected episodes of heat exhaustion, she at work, and I on a walk on a hot afternoon.
I think trouble thermoregulating can be a symptom of COVID even in the absence of fever or other classic symptoms.
I wish people were studying this or talking about it. I searched and found nothing.
It seems plausible that what is going on is that COVID stresses the vascular system, which, among other things, is used to thermoregulate. You can have these symptoms even with no lung symptoms. People talk as if COVID is primarily a respiratory disease but for many people it primarily has cardiovascular manifestations. This may be why asthma is not a risk factor for death by COVID whereas heart disease is.
Our experience suggests that you can have very mild cases, borderline asymptomatic even, and never test positive, yet still have stress on your cardiovascular system.
Pay attention to this stuff. Check weather, and listen to your body. If you feel hot and others don't, or you're feeling hot and cold at the same time, especially if these reactions are not normal for you, especially if you may have been exposed to COVID, maybe take it easy. You may be more vulnerable to heat exhaustion or worse, during a brief recovery window, and you may also be contagious, who knows?
3 notes
·
View notes
Text
EXTRA; ABOUT COPD

disclaimer: i‘m no medical professional. this is based on research alone. please contact me if the information provided is untrue.

what is copd?
copd, short for chronic obstructive pulmonary disease, is a progressive type of lung disease, with the two most common contributors being emphysema (condition in which the alveoli at the end of the smallest air passages (bronchioles) of the lungs are destroyed) and chronic bronchitis (inflammation of the lining of the bronchial tubes, which carry air to and from the air sacs (alveoli) of the lungs). even thought it is a progressive disease which gets worse over time, it is treatable, allowing people to still achieve symptom control and a good quality of life.
sign and symptoms
signs and symptoms include shortness of breath, cough and exacerbations.
copd often also occurs alongside other conditions like cvd, skeletal muscle dysfunction, metabolic syndrome, osteoporosis, depression, anxiety and lung cancer.
complications
copd can cause various complications including respiratory failure, pulmonary heart disease, lung cancer, depression, anxiety and pneumothorax
risk factors
risk factors include exposure to tobacco smoke, exposure to dust and chemicals, exposure to fumes from burning fuel, pollution, asthma and genetics, the major genetic risk factor being aat deficiency.
diagnosis
the most common way to diagnose copd is through spirometry. doctors can also assess their patients through the mrc breathlessness scale and the copd assessment test.
treatment
many people with copd have rather mild forms and therefore only requiring little therapy.
copd can be treated by medication taken on regular basis such as bronchodilators, inhaled steroids, combination inhalers, oral steroids, phosphodiesterase-4 inhibitors, antibiotics and theophylline. further therapies are lung therapies like oxygen therapy and a pulmonary rehabilitation program. for people with severe emphysema surgery is also an option, like a lung transplant. lung volume reduction surgery or a bullectomy.
statistics
copd is the third leading cause of death worldwide. the five year mortality rate ranges from 40-70%, depending on the severity.
men are more likely to suffer from copd.
it is estimated that between 7-19% of the world population suffers from mild to severe copd.
most people are over 40 years old when their first symptoms develop. younger people developing copd are often linked to aat deficiency
smoking accounts for up to 8/10 copd-related deaths.

evanescent
/ɛvəˈnɛs(ə)nt,iːvəˈnɛs(ə)nt/ — “soon passing out of sight, memory, or existence; quickly fading or disappearing.”
mlist
#₊❏❜ ⋮evanescent#iwaizumi x reader#haikyuu x reader#haikyuu smau#haikyuu angst#hq smau#iwaizumi x you#iwaizumi hajime#haikyuu social media au#haikyuu imagines#hq x you#hq x reader
13 notes
·
View notes
Text
Also preserved on our archive
Another perfect example of how masking to help prevent covid keeps us *all* safer from *all* airborne illness.
by Tamara Schneider
Lingering respiratory viruses set the stage for chronic lung disease, mouse study shows
Doctors have long known that children who become seriously ill with certain respiratory viruses such as respiratory syncytial virus (RSV) are at elevated risk of developing asthma later in life. What they haven’t known is why.
A new study by researchers at Washington University School of Medicine in St. Louis may have solved the mystery. The study, in mice, shows that respiratory viruses can hide out in immune cells in the lungs long after the initial symptoms of an infection have resolved, creating a persistently inflammatory environment that promotes the development of lung disease. Further, they showed that eliminating the infected cells reduces signs of chronic lung damage before they progress to a full-blown chronic respiratory illness.
The findings, published Oct. 2 in Nature Microbiology, point to a potential new approach to preventing asthma, chronic obstructive pulmonary disease (COPD) and other chronic lung diseases by eradicating the persistent respiratory viruses that fuel these conditions.
“Right now, children who have been hospitalized for a respiratory infection such as RSV are sent home once their symptoms resolve,” said senior author Carolina B. López, PhD, a professor of molecular microbiology and a BJC Investigator at WashU Medicine. “To reduce the risk that these children will go on to develop asthma, maybe in the future we will be able to check if all of the virus is truly gone from the lung, and eliminate all lingering virus, before we send them home.”
About 27 million people in the U.S. are living with asthma. Many factors influence a person’s likelihood of developing the chronic breathing illness, including living in a neighborhood with poor air quality, having exposure to cigarette smoke and being hospitalized for viral pneumonia or bronchitis while young. Some researchers — López included — suspected that the link between serious lung infection and subsequent asthma diagnosis was due to lingering virus in the lungs that causes ongoing damage, but a direct link between the ongoing presence of virus and chronic lung disease has not been previously shown.
López and first author Ítalo Araújo Castro, PhD, a postdoctoral researcher in her lab, developed a unique system involving a natural mouse virus known as Sendai virus, and fluorescent markers of infection. Sendai is related to human parainfluenza virus, a common respiratory virus that, like RSV, has been linked to asthma in children. Sendai behaves in mice in very much the same way that human parainfluenza virus behaves in people, making it an excellent model of the kinds of infections that could lead to chronic lung disease.
Using the fluorescent trackers, the researchers could observe signs of the virus throughout infection. After about two weeks, the mice recovered, but viral RNA and protein were still detectable several weeks later in their lungs, hidden away in immune cells.
“Finding persistent virus in immune cells was unexpected,” López said. “I think that’s why it had been missed before. Everyone had been looking for viral products in the epithelial cells that line the surface of the respiratory system, because that’s where these viruses primarily replicate. But they were in the immune cells.”
Moreover, the presence of the virus changed the behavior of the infected immune cells, causing them to become more inflammatory than the uninfected immune cells. Persistent inflammation sets the stage for chronic lung disease to arise, the researchers said. Indeed, seven weeks after infection, the mice’s lungs exhibited inflammation of air sacs and blood vessels, abnormal development of lung cells and excess immune tissue — all signs of chronic inflammatory lung damage, even though the mice appeared outwardly to have recovered. Once the infected immune cells were eliminated, the signs of damage diminished.
“We use a perfectly matched virus-host pairing to prove that a common respiratory virus can be maintained in immunocompetent hosts for way longer than the acute phase of the infection, and that this viral persistence can result in chronic lung conditions,” Castro said. “Probably the long-term health effects we see in people who are supposed to be recovered from an acute infection are actually due to persistence of virus in their lungs.”
The findings point to new ways to think about preventing chronic lung diseases, the researchers said.
“Pretty much every single child gets infected with these viruses before the age of 3, and maybe 5% get serious enough disease that they could potentially develop persistent infection,” López said. “We’re not going to be able to prevent children from getting infected in the first place. But if we understand how these viruses persist and the effects that persistence has on the lungs, we may be able to reduce the risk of serious long-term problems.”
Study: Castro IA, Yang Y, Gnazzo V, Kim DH, Van Dyken SJ, López CB. Murine parainfluenza virus persists in lung innate immune cells sustaining chronic lung pathology. Nature Microbiology. Oct. 2, 2024. DOI: 10.1038/s41564-024-01805-8
www.nature.com/articles/s41564-024-01805-8 (PAYWALLED)
#mask up#covid#pandemic#covid 19#wear a mask#public health#sars cov 2#coronavirus#still coviding#wear a respirator#flu#influenza#RSV#respiratory syncytial virus
43 notes
·
View notes
Note
disability pride ask!!
1. 5. and 9.
Thanks! mentions of disability down below cw vomit
1. what disability/ies do you have? (and are they mental, physical, or both?) I do have a whole catalogue of different kinds of disability - I call them my main three. Heart, Lungs, Esophagus. I have esophageal atresia. Basically my esophagus was disconnected from my stomach and was also connected to my windpipe instead. Had to be artifically stretched and widened. Nearly doesnt bother me anymore but i have slight problems eating and a scar on my stomach from the feeding tube i used to have. I have 3rd degree asthma and only one side of my lung working proberly; also caused through the first disabilty and a lung collapse i had. Also have a chronic cough. Heart is well the main thing. I have 4 different kinds of heart diseases. They cause low blood pressure, circulatory problems and an underdeveloped heart muscle. I at times have problems moving my arms to a certain extend without them hurting. Because of one of those heart diseases i am at high risk for strokes and brain bleeding. And well on top of that depression and dermatillomania. 5. if you have multiple disabilities: do they affect each other? how? People with esophageal atresia have commonly heart diseases so this goes hand in hand. My lungs are shit thanks to it as well and complications during the operation. Everything is connected. When i have circulation problems I am very often nearly throwing up as well. Aka exhaustions makes me vomit 9. how do you measure your energy? (spoons, battery, something else?) I dont have a fancy name for it. My energy levels changes from day to day and also are influenced by weather and temperature and other factors. But i think its more like a battery for me - but some that can be recharged.
5 notes
·
View notes
Text
Content warning: weight and fitness related talk as they pertain to medicine.
Got another Medscape email which was about this. Basically an article describing some research study linking VO2max to cancer risk and mortality (specifically: colon cancer risk, and lung and prostate cancer mortality- also specifically only in men)
Okay, cool, it’s fun knowledge to have but imo i can’t see the Curbsiders calling this research particularly practice changing. Overall help messaging too- cardio exercise is in fact good!! And thankfully they did factor in other variables (although using self report for some of them) like additional disease/comorbidities, smoking (self report based on a categorical # of cigs a day), dietary habits (self report of general good/poor rating, not standardized), and somehow they added BMI in there too.
But here is something I really dislike… they use vo2max which is based on weight but then also say they adjusted for BMI in the models.
The fact is, BMI - and body fat - play a role in vo2max. I’m not joking; fat mass is actually a better predictor of vo2max than your physical performance on a cardio test.
Admittedly I haven’t looked into HOW they adjusted for BMI (like, I’d need to more about the math behind the adjustments), but it seems extra silly to make your main “risk groups” something that is weight dependent and then say you adjusted for a variable that is also weight dependent later on.
I need to do more reading about the topic of maximal oxygen uptake and fitness- but atm I’m curious what would happen if we ran studies not based on vo2max per body mass but per “fat free” or lean body mass. Otherwise I feel like we always have some strong lurking variables that hide in the vo2max measurement itself.
(It’s kind of like how when body fat% ranges were being set, some researchers set values not based on health criteria, but based on correlation with BMI…. And then we ran with those numbers… and then we claim body fat% is a better indicator of health than BMI. It’s recursive)
2 notes
·
View notes
Photo










National Take the Stairs Day
National Take the Stairs Day is celebrated every second Wednesday in January. You know what that means: celebrate the day by hitting the stairs. Elevator? What elevator? If you’re interested in taking things up a notch, run around the block or cycle to work. It doesn’t matter what you do, as long as you keep that heart rate up.
Lung health is more important now than ever before. Did you know that over 3.7 million Americans live with chronic lung diseases like asthma or lung cancer? We’re not moving as much as we should. To top it, the air we breathe gets increasingly unhealthy. Some factors may be beyond our control, but staying fit and healthy is entirely in our hands. Take the first steps towards a healthier life today. What matters eventually are the choices we make.
History of National Take the Stairs Day
The first mention of Take the Stairs Day was in 2016. A dedicated stair-running group likely organized it, although there’s not much documentation on the event.
On the other hand, National Take the Stairs Day is a recent initiative by the American Lung Association. The goal is to improve our lung health by choosing a life of movement over convenience.
Stair walking is excellent exercise and one of the easiest things to do. It’s gentler on our joints and muscles compared to HIIT or gym workouts, with almost similar benefits. It’s an activity to seriously consider if you’re looking to lose weight, tone muscle, and enhance overall cardiovascular health.
Taking charge of our health can sometimes feel daunting. Where does one begin? The good news is you don’t need to make drastic alterations to your lifestyle, unless medically advised. The key lies in little but consistent steps each day. They really do go a long way. Small changes such as choosing to take the stairs instead of an elevator can significantly reduce the risk of chronic diseases.
National Take the Stairs Day hopes to encourage Americans to make changes to their lifestyle. By taking part, you also show support for the millions of people who live with debilitating lung disease. If a few minutes of climbing stairs can make your lungs explode, imagine what it’s like for those with chronic pulmonary disease. It can be a humbling reminder of how lucky we are to be alive. We hope everyone takes the stairs today and every other day.
National Take the Stairs Day timeline
8000 B.C. - 2000 B.C. The First Ornate Staircases
As human civilization progresses, the people of ancient Mesopotamia build magnificent staircases in their homes.
2016 A Day For Taking Stairs
The internet first hears of Take the Stairs Day.
2019 Backed By Science
Researchers at McMaster University find that short bursts of stair climbing throughout the day can boost cardiovascular health.
2020 A Guinness Record For Stair Climbing
On November 18, Ryoji Watanabe from Japan breaks the world record for the fastest vertical mile stair climbing, at one hour, six minutes, and 58 seconds.
National Take the Stairs Day FAQs
When is National Take the Stairs Day?
Organized by the American Lung Association, National Take the Stairs Day takes place on the second Wednesday in January each year. The association encourages Americans to improve their lung health by taking the stairs instead of an elevator.
What are the benefits of stair climbing?
Stair climbing comes with tremendous health benefits. A few minutes of stair climbing throughout the day improves lung capacity, heart function, and blood circulation. It also reduces the risks of developing chronic heart diseases, cancer, diabetes, and hypertension.
How many stairs should I climb for a good workout?
Try climbing up and downstairs on 10 to 12 steps for about 30 minutes. Climb one step at a time and progress to skipping steps once you’re comfortable. For intense calorie burn, climb up and down a 10-story building five times.
National Take the Stairs Day Activities
Take the stairs
Design a stairs-climbing challenge
Climb stairs for a killer cardio burn
Wherever you can, choose to take the stairs today. Find opportunities throughout the day: on a lunch break, coffee run, or en route to the break room.
The good thing about stairs is you’ll find them everywhere. Gather everyone for a stairs-climbing challenge at the office or apartment complex. It can be a surprising way to bond. Take care to offer support to anyone who may be struggling.
Start incorporating stair climbing into your workout. Jog up a few flights each day, increasing the pace as you go along. Level up by skipping one step or carrying a heavy backpack on your way up.
5 Facts About Exercising That Will Blow Your Mind
Let the music take control
Exercising is good for the brain
Bring on the muscles
Slows down aging
Variety is super important
Listening to music during a workout can improve performance by 15%.
Cardio-intensive exercises help create new brain cells, improving brain power and memory.
People with more muscle mass burn more fat amounts while resting.
Those who exercise for 45 minutes, three times a week can significantly reduce signs of aging.
Compared to those who cross-train, people who don’t switch up their workouts are more susceptible to injury.
Why We Love National Take the Stairs Day
It challenges us
Gratitude for our lungs
A community endeavor
The comfort of familiar things lulls most of us into complacency. When was the last time you challenged your body and mind? It’s time today to get up and move. If not now, when?
Breath is life, but we don’t notice it at all. When we take the stairs, we are reminded of how hard our heart and lungs work. That exploding sensation in the chest? It means we’re alive.
Staying fit and healthy can be a lonesome road. National Take the Stairs Day recognizes the importance of the community's rallying around better health. It’s easier when everyone’s in it together.
Source
#Sonoma State Historic Park#Denver#California#Colorado State Capitol#USA#summer 2022#architecture#cityscape#Domaine Carneros#travel#North Window Arch#Arches National Park#landscape#Utah#Earthquake Fault#Mammoth Lakes#Freemark Abbey Winery#St. Helena#Hess Collection Winery#National Take the Stairs Day#11 January#NationalTaketheStairsDay#original photography
3 notes
·
View notes
Text
Interview by Stephanie Desmon
Until now, people who suffered mild or asymptomatic COVID-19 were thought to have dodged the brunt of the virus’s brutal side effects. But new evidence has revealed that anyone infected with COVID is at higher risk for heart issues—including clots, inflammation, and arrhythmias—a risk that persists even in relatively healthy people long after the illness has passed.
In this Q&A, adapted from the March 9 episode of Public Health On Call, Ziyad Al-Aly, director of the Clinical Epidemiology Center and chief of Research and Education Service at Veterans Affairs St. Louis Health Care System, talks with Stephanie Desmon about COVID-19 and the heart, including his recent study, which found a significant risk of heart problems in people a year after being diagnosed with COVID.
You just published a study that says that in some people who’ve had COVID, heart issues can persist for a year or more. What does this mean and what did you study?
We've known for a while that during the acute phase—the first 30 days of COVID-19—people who have severe disease and need to be admitted to the hospital or ICU may develop heart complications. We didn't know what happened to people's hearts in the long term—six months to a year out—or what happened to people who had mild disease and did not need hospitalization or ICU care.
We did this study to evaluate the one-year risk of heart problems in people who got COVID-19, compared to nearly 11 million controls of people who did not.
What did you find?
The major finding was that people with COVID-19 have a higher risk of all sorts of heart problems at one year. That included arrhythmias (irregular heart beats or the heart beating too fast or too slow) and atrial fibrillation (a fast heart rhythm in a particular pattern). We found evidence of an increased risk of stroke, of blood clots in the legs and the lungs, and of heart failure and heart attacks. The increased risk of a broad spectrum of heart problems was evident.
I went into it thinking that [the risk] was going to be most pronounced and evident in people who smoked a lot or had diabetes, heart disease, kidney disease, or some [other] risk factors. What we found is that even in people who did not have any heart problems start with, were athletic, did not have a high BMI, were not obese, did not smoke, did not have kidney disease or diabetes—even in people who were previously healthy and had no risk factors or problems with the heart—COVID-19 affected them in such a way that manifested the higher risk of heart problems than people who did not get COVID-19.
It was really eye-opening that the risk was also evident in people who did not have severe COVID-19 that necessitated hospitalization or ICU care. People who got COVID-19 and were asymptomatic, or got COVID-19 that was so mild that they were able to nurse it at home, without going to the doctor still developed an increased risk of heart problems a year out.
What's going on in the body?
A lot of different things could be happening. It's possible that the virus itself and the immune response to it cause an intense inflammation that subsequently hits the heart and results in some of the manifestations we've seen here. It's possible that COVID-19 may attack the endothelial cells that line the vessels of the heart. Some of these cells might die and eventually facilitate the formation of blood clots and blockages of the arteries or vessels of the heart.
There are several other mechanisms that revolve around something called the ACE receptor. The virus has something called a spike protein, which is like a key that engages a lock—the ACE receptor. That allows the virus into cells, including heart cells.
Why would SARS-CoV-2, the virus that causes COVID 19, which we all thought about as a respiratory virus, attack the heart up to a year down the road? That’s likely one of the explanations.
This study was done before vaccination was widely available. Is there any indication that, for example, breakthrough infections would have a different result long term?
Yes. We are [studying] this, but I think the jury is still out. We're certainly very interested in addressing that publicly as soon as we can.
You studied Veterans Administration records, and that population is mostly men, white, and older. Do you feel that [the findings] apply to the entire population?
Yes and no. I think we have to be cognizant that this study comes from one system, the VA system, but that needs to be put into a larger context. This is a study of nearly more than 11 million people. People tell me most vets are males, but 10% are females—meaning our study has more than 1 million females. Similarly, 20% [of study participants] are Black—more than 2 million people.
In addition to this, we did subgroup analyses to see what would happen in only women, only men, only Black people or white people, people younger than a certain age or older than a certain age. Across the board we saw an increased risk of heart problems. This tells us that it doesn't matter if you are a female or male, Black or white, older or younger, diabetic, a smoker, have chronic kidney disease or other cardiovascular risk factors, or not. The risk was across the board, and it’s driven by COVID-19. It really spared no one.
The jury's still out on all of the things that long COVID might encompass. Would this fit into that category?
Absolutely. Long COVID is the umbrella term that describes all the post-acute manifestations that happen as a result of COVID-19. It could be things that started in the acute phase that lingered and persisted into the long term, or it could be new things attributable to SARS-CoV-2 that have happened three, four, or five months out. When you have that definition in mind, it's very clear that the heart manifestations we described in our report are part and parcel of the broader picture of long COVID.
Long COVID can give you fatigue and brain fog and result in new-onset diabetes, kidney problems, and heart problems. All of that collectively forms a multilayered, multifaceted long COVID. That's not to say one patient will have all of these things.
Are we going to have a lot of people who have some form of long COVID and are chronically ill? Will it be a strain on government resources? What do you see as the future?
I think that's why talking about it is very important. We think long COVID can affect anywhere between 4% and 7% of people. That seems really small, but it’s not if you multiply that number by the huge number of people infected with COVID in the U.S., more than 80 million people and counting. We think that will translate into millions of people with long COVID in need of care, and broadly speaking, our health systems need to be prepared. People running health systems or clinics need to start preparing for the tide of patients that are going to hit our doors with heart problems and other long COVID problems.
On a government level, I think we definitely need to be prepared for this. We cannot move on from the pandemic and disregard its long-term consequences. Arguably the long-term consequences are going to be even more profound and stick with us and scar a lot of people around us for generations.
A lot of the manifestations we're describing in this report are chronic conditions that will [affect] people for a lifetime. For example, heart failure isn't something that you wake up tomorrow and all of a sudden don't have. That's not how it works. We're no longer talking about things that might improve tomorrow—we're seeing chronic conditions that will require care for a long time. People, health systems, and governments need to be prepared for that.
1 note
·
View note