Don't wanna be here? Send us removal request.
Text
The Future of Lab Analyzers Interfacing: Trends and Innovations

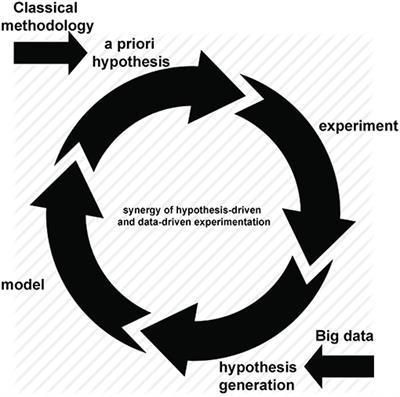
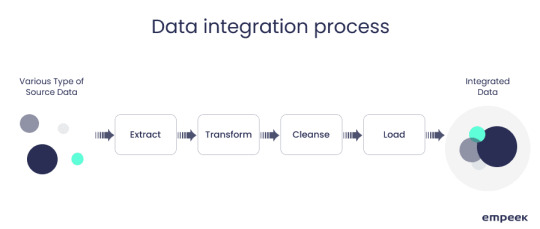
In the realm of laboratory technology, Lab Analyzers Interfacing stands as a cornerstone of efficiency and productivity. As the demand for faster, more accurate results grows, so too does the need for seamless connectivity and integration within laboratory environments. In this article, we'll delve into the latest trends and innovations shaping the future of Lab Analyzers Interfacing, exploring concepts such as Connectivity, Integration, Cloud Interfaces, Protocol Optimization, and Remote Monitoring. Connectivity lies at the heart of modern laboratory operations. Gone are the days of isolated instruments operating in silos. Today, laboratories are embracing interconnected systems that allow for real-time data sharing and collaboration. Lab Analyzers Interfacing solutions enable instruments to communicate with each other, streamlining workflows and enhancing overall efficiency. Whether it's through Ethernet, Wi-Fi, or Bluetooth, the ability to seamlessly connect lab analyzers is revolutionizing the way experiments are conducted and results are analyzed.
Integration takes Lab Analyzers Interfacing a step further by incorporating disparate instruments and software into a unified ecosystem. By integrating lab analyzers with Laboratory Information Management Systems (LIMS) or Electronic Health Records (EHR) platforms, laboratories can centralize data management and streamline reporting processes. This not only reduces the risk of errors but also provides researchers and clinicians with a comprehensive view of their data, facilitating informed decision-making. The emergence of Cloud Interfaces has further expanded the possibilities of Lab Analyzers Interfacing. By leveraging cloud-based solutions, laboratories can access and analyze data from anywhere in the world, breaking down geographical barriers and fostering collaboration on a global scale. Cloud interfaces also offer scalability and flexibility, allowing laboratories to adapt to changing needs without the hassle of traditional IT infrastructure.
Protocol Optimization is another area where Lab Analyzers Interfacing is driving innovation. By optimizing communication protocols between instruments, laboratories can minimize data transfer times and maximize throughput. This not only improves the speed and efficiency of experiments but also reduces the risk of errors associated with manual data entry. Remote Monitoring is perhaps one of the most exciting developments in Lab Analyzers Interfacing. With remote monitoring capabilities, laboratories can monitor and control instruments from anywhere with an internet connection. This not only frees up valuable time for laboratory staff but also enables round-the-clock operation, maximizing instrument uptime and productivity. In conclusion, the future of Lab Analyzers Interfacing is one of connectivity, integration, and innovation. By embracing trends such as Connectivity, Integration, Cloud Interfaces, Protocol Optimization, and Remote Monitoring, laboratories can unlock new levels of efficiency and productivity, paving the way for groundbreaking discoveries and advancements in science and healthcare.
0 notes
Text
The Role of Laboratory Management in Disease Diagnosis and Prevention

In the realm of healthcare, laboratory management stands as a pivotal force in the continuum of disease diagnosis and prevention. Behind every accurate diagnosis, every effective treatment plan, and every successful preventive measure lies the meticulous orchestration of laboratory processes, resources, and personnel.
Effective laboratory management strategies prioritize risk mitigation, implementing rigorous quality control measures to minimize the likelihood of errors or inaccuracies in testing processes. From specimen collection to result reporting, every step is scrutinized and optimized to uphold the highest standards of accuracy and reliability.
Moreover, laboratory management serves as the linchpin of interdisciplinary collaboration, fostering seamless communication and cooperation between laboratory staff, clinicians, and other healthcare stakeholders. Through interdisciplinary rounds, case conferences, and collaborative initiatives, laboratory management ensures that laboratory services are closely aligned with clinical priorities and patient needs.
Cost management is another crucial aspect of laboratory management. By leveraging strategic procurement practices, inventory optimization, and utilization management, laboratory management seeks to contain costs without compromising quality or accessibility of laboratory services.

In addition to this, patient-centered care is integral to laboratory management. From ensuring prompt turnaround times to enhancing the clarity and comprehensibility of result reports, laboratory management endeavors to enhance the patient experience at every touchpoint.
Efficient allocation and utilization of resources are fundamental to the success of any healthcare enterprise, and laboratory management is no exception. Through resource optimization, laboratory management strives to maximize the productivity and value of laboratory assets, whether human, financial, or technological.
In conclusion, laboratory management plays a multifaceted and indispensable role in disease diagnosis and prevention. By embracing innovation, collaboration, and a steadfast commitment to excellence, laboratory management paves the way for improved healthcare outcomes and a healthier future for all.
#Risk Mitigation#Interdisciplinary Collaboration#Cost Management#Patient-Centered Care#Resource Optimization
0 notes
Text
Hospital Management Software Demystified: Understanding the Basics

In the intricate world of healthcare, the efficient management of hospital operations is paramount to ensuring quality care delivery. Hospital management software serves as the backbone of modern healthcare institutions, streamlining processes, and enhancing overall efficiency. In this blog, we will delve into the fundamental aspects of hospital management software, shedding light on its key components and functionalities.
Patient Data: At the heart of any healthcare institution lies the comprehensive patient data management system facilitated by hospital management software. From admission to discharge, every interaction and medical record pertaining to a patient is meticulously documented and stored electronically. This not only ensures easy access to patient information but also facilitates seamless communication among healthcare providers.
E-Records: Gone are the days of paper-based record-keeping systems. With the advent of hospital management software, the transition to electronic health records (EHRs) has revolutionized the way patient data is managed. E-records not only minimize the risk of errors associated with manual documentation but also enable healthcare professionals to retrieve vital information swiftly, thereby enhancing the quality and efficiency of patient care.
Admin Efficiency: Efficient administration is the cornerstone of effective hospital management. Hospital management software plays a pivotal role in optimizing administrative tasks, ranging from appointment scheduling and inventory management to billing and invoicing. By automating these processes, administrative staff can allocate their time and resources more effectively, thereby improving overall productivity and service delivery.

Staff Management: Proper allocation and management of human resources are essential for the smooth functioning of any healthcare institution. Hospital management software offers robust tools for staff scheduling, task assignment, and performance tracking. By centralizing staff management processes, healthcare administrators can ensure adequate staffing levels and optimize workforce utilization, leading to improved patient outcomes and staff satisfaction.
Analytics & Reporting: In the era of data-driven decision-making, hospital management software provides invaluable insights through advanced analytics and reporting capabilities. By analyzing key performance metrics and trends, healthcare administrators can identify areas for improvement, streamline operations, and enhance the overall quality of care. Moreover, comprehensive reporting functionalities enable institutions to meet regulatory requirements and demonstrate compliance with industry standards.
In conclusion, hospital management software serves as a cornerstone of modern healthcare delivery, revolutionizing the way institutions manage patient data, streamline operations, and optimize resource utilization. By leveraging the power of hospital management software, healthcare institutions can enhance efficiency, improve patient outcomes, and stay ahead in an ever-evolving healthcare landscape.
0 notes
Text
The Value Proposition of Healthcare Consulting Services

In the ever-evolving landscape of healthcare, organizations continually seek ways to navigate complex challenges and optimize their operations. This is where Healthcare Consulting Services emerge as invaluable partners, offering advisory support and strategic guidance to drive sustainable success.
At the core of Healthcare Consulting Services lies industry expertise—a deep understanding of the unique dynamics and intricacies of the healthcare sector. Leveraging this expertise, consulting firms bring a wealth of knowledge and insights to the table, enabling organizations to make informed decisions and navigate industry-specific challenges effectively.
One of the primary offerings of Healthcare Consulting Services is healthcare analysis. Through comprehensive assessments and data-driven insights, consultants delve into various facets of healthcare organizations, identifying areas for improvement and opportunities for growth. This rigorous analysis forms the foundation for strategic planning and informed decision-making.
Moreover, consulting solutions are tailored to address the specific needs and objectives of each healthcare organization. Whether it's optimizing operational efficiency, enhancing patient care delivery, or navigating regulatory compliance, consulting firms offer bespoke solutions designed to deliver tangible results.

Advisory support is another key component of Healthcare Consulting Services. Consultants serve as trusted advisors, guiding organizations through strategic initiatives, change management processes, and organizational transformations. Their objective perspective and seasoned guidance help organizations navigate complexities and achieve their strategic goals.
In summary, the value proposition of Healthcare Consulting Services is multifaceted and impactful. By leveraging industry expertise, offering strategic guidance, conducting rigorous healthcare analysis, providing tailored consulting solutions, and offering advisory support, consulting firms empower healthcare organizations to thrive in an ever-changing landscape. As healthcare continues to evolve, the partnership between organizations and consulting firms will remain instrumental in driving innovation and excellence in patient care.
0 notes
Text
Hospitality Trends Transforming the Healthcare Landscape

In today's dynamic healthcare landscape, the integration of user-friendly hospitality practices is revolutionizing the way patients experience care. From improved accessibility to cutting-edge facility design trends, healthcare providers are embracing hospitality principles to enhance guest satisfaction, empower staff through training, and foster meaningful patient engagement.
Improved accessibility lies at the heart of user-friendly healthcare hospitality. By prioritizing accessibility in facility design, healthcare providers ensure that patients of all abilities can navigate their environments with ease. From wheelchair ramps to digital wayfinding systems, these efforts aim to create an inclusive and welcoming atmosphere for all patients and visitors.
Meanwhile, staying abreast of facility design trends is crucial for healthcare organizations aiming to provide a modern and inviting environment. From soothing color schemes to comfortable seating areas, thoughtful design elements can significantly impact the overall patient experience. By incorporating hospitality-inspired design concepts, healthcare facilities can create spaces that promote healing, relaxation, and comfort.
Central to the success of user-friendly healthcare hospitality is guest satisfaction. Healthcare providers are increasingly adopting strategies from the hospitality industry to prioritize patient comfort and convenience. This includes offering amenities such as complimentary Wi-Fi, room service options, and concierge services to enhance the overall patient experience.

Equally important is investing in comprehensive staff training programs to ensure that healthcare professionals deliver service with warmth, empathy, and efficiency. By equipping staff with the necessary skills and knowledge, healthcare organizations can elevate the level of care they provide and create positive interactions that leave a lasting impression on patients.
Lastly, fostering meaningful patient engagement is essential for building trust and fostering loyalty. Healthcare providers are leveraging technology and communication tools to engage patients in their care journey, solicit feedback, and address concerns promptly. By actively involving patients in decision-making and care planning, healthcare organizations can cultivate a sense of partnership and empowerment.
In conclusion, the integration of user-friendly hospitality practices is transforming the healthcare landscape, reshaping the way patients experience care. From prioritizing improved accessibility and embracing facility design trends to enhancing guest satisfaction, investing in staff training, and fostering patient engagement, these efforts aim to create a healthcare environment that is welcoming, inclusive, and centered around the needs of the individual. As healthcare providers continue to prioritize hospitality principles, they can forge deeper connections with patients, improve outcomes, and drive overall satisfaction.
0 notes
Text
Achieving Excellence: Implementing Healthcare Standards in Practice

In the realm of healthcare, adherence to healthcare standards is paramount for ensuring quality care delivery and patient safety. From patient safety protocols to industry best practices, healthcare organizations strive to implement and maintain rigorous standards that uphold the highest levels of excellence in patient care.
Healthcare standards encompass a wide array of guidelines, protocols, and best practices aimed at standardizing processes, procedures, and protocols across healthcare settings. These standards serve as benchmarks for quality assurance and regulatory compliance, guiding healthcare professionals in delivering safe, effective, and consistent care to patients.
One of the cornerstones of healthcare standards is the implementation of patient safety protocols. These protocols are designed to minimize the risk of adverse events, medical errors, and preventable harm to patients. By adhering to established safety protocols, healthcare providers can create a culture of safety, mitigate risks, and enhance patient outcomes.
Furthermore, industry best practices play a crucial role in shaping healthcare standards and driving continuous improvement in patient care. These practices represent the collective wisdom and experience of healthcare professionals and organizations, offering proven strategies and methodologies for delivering high-quality, patient-centered care.
Standardization initiatives also play a significant role in advancing healthcare standards. These initiatives aim to harmonize processes, terminology, and technologies across healthcare systems, promoting interoperability, efficiency, and consistency in care delivery. By embracing standardization efforts, healthcare organizations can streamline operations, reduce errors, and improve care coordination.

Clinical guidelines are another essential component of healthcare standards, providing evidence-based recommendations for diagnosis, treatment, and management of various medical conditions. These guidelines serve as valuable tools for healthcare professionals, offering authoritative guidance on best practices and protocols for delivering optimal patient care.
Moreover, continuous quality improvement is integral to maintaining and enhancing healthcare standards over time. By systematically monitoring performance, identifying areas for improvement, and implementing evidence-based interventions, healthcare organizations can drive ongoing improvements in care quality, patient outcomes, and organizational efficiency.
In conclusion, achieving excellence in healthcare requires a steadfast commitment to implementing and upholding healthcare standards in practice. From patient safety protocols and industry best practices to standardization initiatives, clinical guidelines, and continuous quality improvement, these standards serve as guiding principles for delivering safe, effective, and patient-centered care. By embracing and adhering to these standards, healthcare organizations can foster a culture of excellence, promote patient safety, and drive continuous improvement in the delivery of healthcare services.
#Patient Safety Protocols#Industry Best Practices#Standardization Initiatives#Clinical Guidelines#Continuous Quality Improvement
0 notes
Text
The Future of Radiology: Innovations in Machines Interfacing and PACS

In the rapidly evolving landscape of healthcare, radiology machines interfacing and PACS (Picture Archiving and Communication Systems) play pivotal roles in enhancing diagnostic accuracy and workflow efficiency. As technology continues to advance, the future of radiology is poised for groundbreaking innovations in these crucial areas.
Radiology Automation stands at the forefront of this revolution, revolutionizing how medical images are processed, analyzed, and interpreted. By harnessing the power of artificial intelligence (AI) and machine learning algorithms, radiologists can streamline repetitive tasks, accelerate image interpretation, and prioritize critical cases for immediate attention. This not only reduces human error but also optimizes resource utilization, ultimately leading to improved patient outcomes.
PACS Integration is another key aspect driving the future of radiology. Seamlessly integrating PACS with other healthcare IT systems enables healthcare providers to access and share medical images and patient data across disparate platforms with ease. This interoperability fosters collaboration among multidisciplinary care teams, facilitates remote consultations, and expedites treatment decisions, thereby enhancing the quality and efficiency of patient care.
Seamless Data Exchange further enhances the interoperability of radiology systems, enabling the seamless transmission of imaging data between different healthcare facilities, departments, and imaging modalities. By standardizing data formats and communication protocols, healthcare organizations can overcome barriers to information exchange, improve care coordination, and reduce redundant imaging studies, ultimately driving down costs and enhancing patient satisfaction.

Radiology Equipment Connectivity plays a vital role in ensuring the seamless integration of imaging devices within the healthcare ecosystem. By establishing secure connections between radiology machines and PACS, healthcare providers can efficiently capture, store, and retrieve medical images, regardless of the vendor or model. This interoperability not only enhances workflow efficiency but also ensures the accessibility and integrity of imaging data throughout its lifecycle.
Advanced Imaging Interfaces represent the future of radiology, offering intuitive user interfaces and advanced visualization tools that empower radiologists to extract actionable insights from complex medical images. From 3D reconstruction and virtual reality to augmented reality and deep learning-based image analysis, these cutting-edge interfaces enable radiologists to navigate through vast amounts of imaging data with unprecedented speed and precision, unlocking new diagnostic capabilities and enhancing clinical decision-making.
In conclusion, the future of radiology is marked by continuous innovation in machines interfacing and PACS. From radiology automation and PACS integration to seamless data exchange, radiology equipment connectivity, and advanced imaging interfaces, these advancements are poised to revolutionize healthcare delivery, improve patient outcomes, and shape the future of medicine. As technology continues to evolve, embracing these innovations will be essential for healthcare organizations striving to stay ahead in the ever-changing landscape of radiology.
#Radiology Automation#PACS Integration#Seamless Data Exchange#Radiology Equipment Connectivity#Advanced Imaging Interfaces
0 notes
Text
Blood Bank Management: From Donor to Recipient

In the intricate network of blood bank management, ensuring the safety and availability of blood products from donor to recipient is paramount. Key aspects such as cold chain management, blood typing, quality assurance, emergency preparedness, and transfusion safety are critical components in this process.
Cold chain management is crucial for preserving the integrity of blood products throughout their journey. Proper temperature control and monitoring at every stage, from collection to transfusion, are essential to prevent spoilage and maintain the efficacy of blood components. By adhering to stringent cold chain protocols, blood banks can ensure the safety and viability of blood products for patients in need.
Blood typing is a fundamental step in matching donors with compatible recipients to prevent adverse transfusion reactions. Accurate and timely blood typing ensures that recipients receive blood products that are compatible with their blood type, minimizing the risk of hemolytic reactions and other complications. Through meticulous blood typing procedures, blood banks can uphold the highest standards of patient safety and care.
Quality assurance measures are integral to maintaining the highest standards of safety and efficacy in blood banking operations. From stringent testing protocols to comprehensive quality control processes, quality assurance efforts encompass every aspect of blood collection, processing, storage, and distribution. By implementing robust quality assurance programs, blood banks can instill confidence in donors, recipients, and healthcare providers alike.
Emergency preparedness is essential for blood banks to respond swiftly and effectively to crises and disasters. By developing comprehensive emergency response plans and conducting regular drills and exercises, blood banks can ensure continuity of operations and timely access to life-saving blood products during emergencies. Emergency preparedness efforts are essential for safeguarding public health and supporting communities in times of need.
Transfusion safety is the cornerstone of blood bank management, encompassing measures to minimize the risk of adverse transfusion reactions and transfusion-transmitted infections. From donor screening and testing to proper blood product labeling and verification, every step in the transfusion process is designed to prioritize patient safety. Through rigorous transfusion safety protocols, blood banks uphold their commitment to providing safe and effective blood products to patients in need.
In conclusion, blood bank management encompasses a comprehensive array of practices and protocols aimed at ensuring the safety, efficacy, and availability of blood products for patients in need. By prioritizing cold chain management, blood typing, quality assurance, emergency preparedness, and transfusion safety, blood banks can fulfill their vital mission of saving lives and supporting healthcare delivery.
0 notes
Text
Lab Analyzers Interface Solutions: Enhancing Efficiency and Accuracy

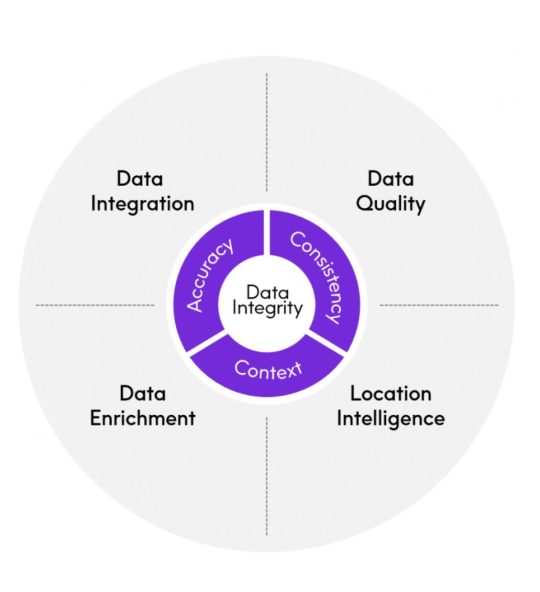
In the ever-evolving landscape of laboratory operations, lab analyzers interfacing plays a crucial role in streamlining workflows and ensuring accuracy. As laboratories seek to optimize their processes, system integration, laboratory efficiency, instrument interface, analytical instruments, and automated reporting emerge as key components of successful interface solutions.
System integration is essential for seamlessly connecting various laboratory instruments and systems, allowing for efficient data exchange and workflow automation. By integrating disparate systems, laboratories can eliminate manual data entry errors, reduce turnaround times, and improve overall efficiency.
Achieving laboratory efficiency requires optimizing every aspect of laboratory operations, from sample processing to result reporting. Through effective analyzers interfacing, laboratories can automate repetitive tasks, minimize downtime, and allocate resources more effectively, ultimately enhancing productivity and reducing costs.
The instrument interface is a critical component of lab analyzers interfacing, facilitating communication between analytical instruments and laboratory information systems (LIS). By implementing standardized interfaces, laboratories can ensure compatibility between instruments, streamline data transfer, and enhance interoperability.

Advanced analytical instruments offer enhanced capabilities for laboratory testing, allowing for more accurate and precise analysis of patient samples. Leveraging the latest analytical technologies, laboratories can improve diagnostic accuracy, expand testing capabilities, and deliver better patient care.
Automated reporting capabilities streamline the generation and delivery of test results, ensuring timely access to critical information for healthcare providers. By automating reporting processes, laboratories can reduce turnaround times, improve result accuracy, and enhance communication with clinicians and patients.
In conclusion, lab analyzers interface solutions play a vital role in enhancing efficiency and accuracy in laboratory operations. Through system integration, laboratory efficiency, instrument interface, analytical instruments, and automated reporting, laboratories can optimize workflows, improve diagnostic capabilities, and ultimately deliver better patient care.
#System Integration#Laboratory Efficiency#Instrument Interface#Analytical Instruments#Automated Reporting
1 note
·
View note
Text
Laboratory Management in the Age of Precision Medicine

In the fast-paced realm of healthcare, laboratory management plays a critical role in supporting the delivery of precise and personalized care. As the healthcare landscape continues to evolve towards precision medicine, laboratories must adapt by leveraging advancements in test automation, sample tracking, result analysis, personnel training, and turnaround time.
Test automation is revolutionizing laboratory workflows by streamlining repetitive tasks and enhancing efficiency. By automating routine laboratory processes, such as specimen handling and analysis, laboratories can minimize human error, improve accuracy, and accelerate turnaround times, ultimately enhancing the quality of patient care.
Effective sample tracking is essential for ensuring the integrity and traceability of specimens throughout the testing process. Leveraging advanced sample tracking systems, laboratories can monitor the movement of specimens in real-time, reduce the risk of misidentification or loss, and maintain compliance with regulatory standards.
Result analysis is at the heart of laboratory diagnostics, providing valuable insights into patient health and informing clinical decision-making. With advanced analytics tools, laboratories can analyze test results more efficiently, identify trends or anomalies, and generate actionable insights to support precision medicine initiatives.
Investing in personnel training is crucial for equipping laboratory staff with the knowledge and skills needed to perform their roles effectively in the era of precision medicine. Through ongoing education and professional development programs, laboratories can ensure that their personnel stay abreast of emerging technologies, best practices, and regulatory requirements, ultimately enhancing the quality and reliability of laboratory services.
Turnaround time is a key performance metric for laboratory efficiency and patient satisfaction. By optimizing workflows, streamlining processes, and implementing priority testing protocols, laboratories can reduce turnaround times, expedite diagnosis, and improve patient outcomes, aligning with the principles of precision medicine.
In conclusion, as healthcare embraces precision medicine, laboratory management must evolve to meet the demands of this transformative approach to patient care. By harnessing the power of test automation, sample tracking, result analysis, personnel training, and turnaround time, laboratories can position themselves as essential partners in delivering precise, personalized, and timely healthcare solutions.
0 notes
Text
Seamless Integration: The Key to Successful Hospital Management Systems

In today's rapidly evolving healthcare landscape, the effective implementation of hospital management system/software is essential for optimizing operations and enhancing patient care. A critical aspect of this implementation is seamless integration, ensuring that various components such as billing solutions, appointment scheduling, analytics dashboard, interoperability solutions, and user interface design work together harmoniously to meet the needs of healthcare providers and patients alike.
Billing solutions are integral to the financial health of hospitals, facilitating accurate and timely billing processes. By seamlessly integrating billing functionalities within the hospital management system, healthcare organizations can streamline revenue cycle management, reduce billing errors, and improve reimbursement rates.
Efficient appointment scheduling is crucial for maximizing resource utilization and minimizing patient wait times. Hospital management systems with robust scheduling modules enable healthcare providers to manage appointments effectively, optimize clinician schedules, and enhance patient access to care.
An analytics dashboard provides actionable insights into key performance metrics, allowing hospital administrators to make informed decisions and drive continuous improvement. By integrating an analytics dashboard within the hospital management system, stakeholders can monitor operational performance, identify trends, and implement data-driven strategies to enhance efficiency and quality of care.
Interoperability solutions facilitate seamless data exchange between disparate systems and healthcare providers, ensuring that patient information is readily accessible whenever and wherever it's needed. By integrating interoperability functionalities within the hospital management system, healthcare organizations can improve care coordination, enhance communication, and promote continuity of care across the healthcare continuum.
A user-friendly user interface design is essential for ensuring adoption and usability of the hospital management system among healthcare professionals. By prioritizing intuitive navigation, responsive design, and personalized user experiences, hospital management systems can enhance user satisfaction, productivity, and overall system effectiveness.
In conclusion, seamless integration of hospital management system/software components such as billing solutions, appointment scheduling, analytics dashboard, interoperability solutions, and user interface design is essential for optimizing hospital operations and improving patient care delivery. By embracing integration as a key principle, healthcare organizations can unlock the full potential of their management systems and achieve sustainable success in today's healthcare environment.
#Billing Solutions#Appointment Scheduling#Analytics Dashboard#Interoperability Solutions#User Interface Design
0 notes
Text
Navigating Change: The Role of Healthcare Consulting Services

In the ever-evolving landscape of healthcare, organizations face numerous challenges as they strive to adapt to changing regulations, technological advancements, and patient expectations. This is where healthcare consulting services play a pivotal role, offering expertise and guidance in areas such as operational efficiency, financial management, quality improvement, process improvement, and market analysis.
Operational efficiency is essential for healthcare organizations to deliver high-quality care while optimizing resources. Healthcare consulting services can assess current workflows, identify inefficiencies, and implement strategies to streamline operations, reduce costs, and enhance overall efficiency.
Effective financial management is critical for the long-term sustainability of healthcare organizations. Consultants specializing in financial management can analyze revenue streams, control expenses, and develop strategies to improve financial performance, ensuring stability and growth in an increasingly competitive healthcare market.
Quality improvement is central to delivering safe, effective, and patient-centered care. Healthcare consulting services can assist organizations in implementing quality improvement initiatives, such as performance measurement, evidence-based practice, and patient satisfaction surveys, to drive continuous improvement and enhance outcomes.
Process improvement initiatives focus on optimizing clinical and administrative processes to increase productivity and efficiency. Consultants can conduct process assessments, identify bottlenecks, and redesign workflows to streamline operations, reduce errors, and improve patient care delivery.
Market analysis provides valuable insights into the competitive landscape and emerging trends in healthcare. Healthcare consulting services can conduct market assessments, analyze consumer preferences, and develop strategies to help organizations adapt to changing market dynamics and seize growth opportunities.
In conclusion, healthcare consulting services play a vital role in helping organizations navigate change and overcome challenges in today's complex healthcare environment. By addressing areas such as operational efficiency, financial management, quality improvement, process improvement, and market analysis, consultants empower healthcare organizations to thrive amidst change and deliver exceptional care to their patients.
#Operational Efficiency#Financial Management#Quality Improvement#Process Improvement#Market Analysis
0 notes
Text
Radiology Machines Interfacing: Streamlining Imaging Processes

In the fast-paced world of radiology, efficient Radiology Machines Interfacing and PACS (Picture Archiving and Communication System) are essential for streamlining imaging processes and improving diagnostic outcomes. Let's delve into how these technologies facilitate seamless integration, optimize workflow, and enhance diagnostic efficiency.
Seamless Integration: The integration of radiology machines with PACS enables seamless integration of imaging data into a centralized system. This integration eliminates the need for manual data entry and facilitates the automatic transfer of images and patient information, reducing the risk of errors and ensuring data accuracy. With seamless integration, radiologists can access patient images and data from any location within the healthcare facility, enhancing collaboration and efficiency.
Image Management: Effective image management is crucial for organizing and storing large volumes of medical images generated by radiology machines. PACS provides robust tools for storing, retrieving, and managing images, allowing radiologists to quickly access relevant patient data during diagnosis and treatment planning. Advanced image management capabilities ensure that images are securely archived and readily accessible when needed, improving workflow efficiency and patient care.
Workflow Optimization: Radiology Machines Interfacing and PACS streamline imaging processes by optimizing workflow and reducing manual tasks. With automated workflows and intelligent routing, radiology images are routed to the appropriate radiologist for interpretation, ensuring timely diagnosis and treatment planning. Workflow optimization also minimizes unnecessary delays and bottlenecks, allowing healthcare providers to deliver prompt and efficient care to patients.

Real-time Access: PACS enables real-time access to radiology images and patient data, empowering healthcare providers to make informed decisions quickly. Radiologists can access images instantly from any location, enabling remote interpretation and consultation, particularly beneficial in emergency situations or when expert opinions are required. Real-time access to imaging data enhances diagnostic accuracy and facilitates timely interventions, ultimately improving patient outcomes.
Diagnostic Efficiency: By streamlining imaging processes and providing rapid access to radiology images, Radiology Machines Interfacing and PACS contribute to diagnostic efficiency. Radiologists can efficiently review and interpret images, leading to faster diagnoses and treatment decisions. Additionally, advanced features such as image enhancement and 3D reconstruction tools further enhance diagnostic accuracy, enabling radiologists to detect and analyze abnormalities with precision.
In conclusion, Radiology Machines Interfacing and PACS play a vital role in streamlining imaging processes and enhancing diagnostic efficiency in radiology departments. Through seamless integration, robust image management, workflow optimization, real-time access, and improved diagnostic efficiency, these technologies empower healthcare providers to deliver high-quality care and improve patient outcomes.
0 notes
Text
The Role of Technology in Modern Blood Bank Management

In the realm of Blood Bank Management, technology plays a pivotal role in enhancing efficiency, accuracy, and patient safety. Let's explore how various technological advancements are revolutionizing blood bank operations:
Inventory Optimization: Effective inventory optimization is essential for ensuring that blood banks have an adequate supply of blood products to meet patient needs while minimizing wastage. Advanced inventory management systems utilize real-time data and predictive analytics to forecast demand, track inventory levels, and automate replenishment processes, ensuring optimal stock levels at all times.
Donor Recruitment: Leveraging technology for donor recruitment has transformed the process of blood collection. Online donor portals, mobile applications, and social media campaigns enable blood banks to reach a broader donor pool, streamline appointment scheduling, and provide convenient donation options. By harnessing technology, blood banks can engage donors more effectively and maintain a consistent blood supply.
Blood Component Tracking: Accurate blood component tracking is critical for ensuring the traceability and safety of blood products throughout the supply chain. Barcode and RFID (Radio-Frequency Identification) technology enable blood banks to track each blood component from collection to transfusion, ensuring proper handling, storage, and distribution. This level of traceability enhances blood product quality and patient safety.

Expiry Monitoring: Technology-enabled expiry monitoring systems help blood banks prevent the wastage of blood products by tracking expiration dates and facilitating timely usage or disposal of nearing-expiry units. Automated alerts and notifications ensure that blood bank staff are promptly notified of expiring products, allowing for proactive management and optimization of inventory.
Automated Matching: Automated matching algorithms utilize advanced computational techniques to match donor blood with recipient blood, ensuring compatibility and reducing the risk of adverse transfusion reactions. These algorithms analyze donor and recipient characteristics, such as blood type and antigen compatibility, to identify suitable matches quickly and accurately, enhancing patient safety during transfusions.
In conclusion, technology plays a transformative role in modern Blood Bank Management, revolutionizing inventory optimization, donor recruitment, blood component tracking, expiry monitoring, and automated matching processes. By embracing technological innovations, blood banks can enhance operational efficiency, ensure blood product quality, and ultimately improve patient outcomes.
#Inventory Optimization#Donor Recruitment#Blood Component Tracking#Expiry Monitoring#Automated Matching
0 notes
Text
Lab Analyzers Interfacing: Bridging the Gap Between Data and Action
In the dynamic landscape of laboratory operations, the seamless integration of Lab Analyzers Interfacing plays a pivotal role in transforming raw data into actionable insights. By bridging the gap between data generation and actionable outcomes, these interfaces facilitate efficient decision-making and enhance overall laboratory performance.
Seamless Data Integration: Seamless data integration is the cornerstone of effective lab analyzer interfacing. It enables disparate laboratory instruments and systems to communicate seamlessly, ensuring that data flows seamlessly throughout the laboratory ecosystem. With seamless data integration, laboratories can consolidate data from various sources, such as analyzers, LIS (Laboratory Information Systems), and EMR (Electronic Medical Records), enabling comprehensive analysis and reporting.
Real-time Analytics: Leveraging real-time analytics, laboratories can gain immediate insights into test results and performance metrics. By analyzing data as it is generated, laboratory professionals can identify trends, anomalies, and potential issues in real time, enabling proactive decision-making and intervention. Real-time analytics empower laboratories to optimize workflows, prioritize tasks, and deliver timely results to healthcare providers and patients.
Workflow Automation: Workflow automation streamlines laboratory processes by automating routine tasks and optimizing resource utilization. Through workflow automation, tasks such as sample handling, testing, and result reporting can be automated, reducing manual errors and accelerating turnaround times. By automating repetitive tasks, laboratories can enhance efficiency, improve throughput, and allocate resources more effectively.

Quality Assurance Measures: Maintaining quality assurance is paramount in laboratory operations to ensure the accuracy and reliability of test results. Lab analyzer interfacing enables the implementation of robust quality assurance measures, including instrument calibration, proficiency testing, and result validation. By enforcing stringent quality control protocols, laboratories can uphold the highest standards of accuracy and reliability in diagnostic testing.
Decision Support Systems: Integrated decision support systems empower laboratory professionals with actionable insights and recommendations based on data analysis. These systems leverage advanced algorithms and machine learning techniques to assist in result interpretation, diagnosis, and treatment planning. By providing evidence-based guidance, decision support systems enable laboratories to deliver more informed and personalized care to patients.
In conclusion, Lab Analyzers Interfacing plays a crucial role in bridging the gap between data generation and actionable outcomes in laboratory settings. Through seamless data integration, real-time analytics, workflow automation, quality assurance measures, and decision support systems, laboratories can enhance efficiency, accuracy, and overall performance, ultimately improving patient care and outcomes.
#Seamless Data Integration#Real-time Analytics#Workflow Automation#Quality Assurance Measures#Decision Support Systems
0 notes
Text
The Art of Hospitality in Modern Healthcare Settings

In the realm of modern healthcare, user-friendly hospitality isn't just a luxury—it's a necessity. Patients and their families seek not only effective treatment but also a comforting experience that puts them at ease during what can often be stressful times. This demand has led healthcare providers to recognize the importance of incorporating elements of hospitality into their services, creating environments that prioritize personalization, communication, comfort, experience, and integration.
One of the key aspects of user-friendly hospitality in healthcare is personalization. Gone are the days of one-size-fits-all approaches to patient care. Today, healthcare providers strive to tailor their services to meet the unique needs and preferences of each individual. From personalized treatment plans to customized amenities in hospital rooms, the focus is on making patients feel seen and valued.
Effective communication is another essential component of user-friendly hospitality in healthcare settings. Clear and open lines of communication between patients, their families, and healthcare providers are crucial for building trust and ensuring that everyone is on the same page regarding treatment plans and expectations. Whether it's through face-to-face conversations, digital platforms, or informational materials, healthcare institutions are finding innovative ways to keep everyone informed and involved.
Creating a comfortable environment is also paramount in delivering user-friendly hospitality in healthcare. Patients who feel relaxed and at ease are more likely to have positive experiences and outcomes. This goes beyond just physical comfort—although that's important too—and extends to creating spaces that feel welcoming and calming. From soothing decor to amenities like adjustable beds and temperature controls, every detail counts.

A positive experience is what sets exceptional healthcare providers apart from the rest. Beyond just addressing medical needs, these providers go the extra mile to ensure that every interaction leaves a lasting impression. This could involve small gestures like offering a warm blanket or a friendly smile, or larger initiatives such as patient-centered care programs that focus on holistic well-being.
Finally, successful integration of hospitality principles into healthcare requires a coordinated effort across all levels of an organization. It's not enough for individual departments to excel in isolation; rather, there must be a cohesive approach that ensures consistency and continuity of care. This might involve training staff in hospitality techniques, implementing technology solutions to streamline processes, or fostering partnerships with external service providers.
In conclusion, the art of hospitality has found a new home in modern healthcare settings, where user-friendly hospitality is now a fundamental part of the patient experience. By prioritizing personalization, communication, comfort, experience, and integration, healthcare providers can create environments that not only heal bodies but also nurture spirits.
0 notes
Text
The Future is Now: Embracing Technological Advancements in Healthcare

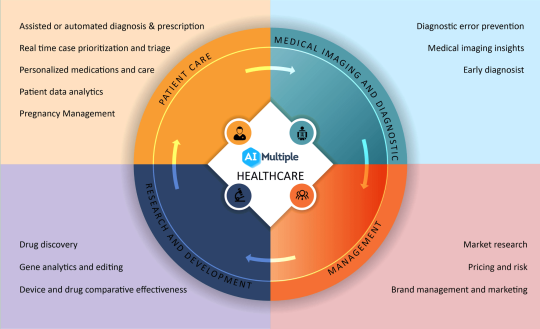
In the dynamic realm of healthcare, the journey towards progress and innovation is propelled by the embrace of technology. As we stand at the threshold of a new era in healthcare, the convergence of groundbreaking advancements promises to revolutionize the way we deliver and experience medical care. From AI in Healthcare to Telemedicine, Wearable Devices, Blockchain in Healthcare, and Robotics & Automation, let's explore how these transformative technologies are shaping the future of healthcare.
AI in Healthcare: Artificial Intelligence (AI) holds immense potential to revolutionize healthcare delivery. By harnessing the power of machine learning algorithms and data analytics, AI enables healthcare providers to make more accurate diagnoses, personalize treatment plans, and optimize clinical workflows. From predictive analytics to virtual health assistants, AI is transforming every facet of healthcare delivery, driving efficiency, and improving patient outcomes.
Telemedicine: Telemedicine has emerged as a game-changer in healthcare delivery, especially in light of recent global events. Through telemedicine, patients can access medical care remotely, eliminating barriers to healthcare access and enhancing convenience. From virtual consultations to remote monitoring, telemedicine offers patients greater flexibility and accessibility while enabling healthcare providers to deliver timely and efficient care.
Wearable Devices: Wearable devices are empowering individuals to take control of their health and well-being like never before. From fitness trackers to smartwatches equipped with health monitoring capabilities, wearable devices enable continuous tracking of vital signs, activity levels, and other health metrics. By providing real-time health insights, wearable devices empower users to make informed decisions about their health and lifestyle choices.

Blockchain in Healthcare: Blockchain technology has the potential to revolutionize healthcare by providing a secure and immutable platform for storing and sharing health data. By leveraging blockchain, healthcare organizations can enhance data security, interoperability, and patient privacy. From electronic health records to supply chain management, blockchain holds the promise of transforming every aspect of healthcare delivery and administration.
Robotics & Automation: Robotics and automation are reshaping healthcare delivery by augmenting the capabilities of healthcare providers and improving operational efficiency. From surgical robots that enhance precision and minimize invasiveness to automated systems that streamline administrative tasks, robotics & automation are driving innovation and transforming the way healthcare is delivered.
In conclusion, the future of healthcare is being shaped by the bold embrace of technology. By embracing technology and harnessing the power of AI in Healthcare, Telemedicine, Wearable Devices, Blockchain in Healthcare, and Robotics & Automation, we can unlock new possibilities, improve patient outcomes, and build a healthier future for all. Let us embark on this transformative journey together, as we embrace the future of healthcare today.
0 notes