#Billing and coding in USA
Explore tagged Tumblr posts
Text
Best Medical Billing Services in USA: Enhancing Your Practice’s Efficiency

In today's rapidly evolving healthcare industry, efficient medical billing services are paramount to the success of any practice. The complexity of medical billing, coupled with the ever-changing regulations, makes it challenging for healthcare providers to manage billing processes internally. This is where professional medical billing companies come into play. By outsourcing to these experts, practices can streamline their operations, reduce errors, and enhance overall efficiency. In this article, we will explore the best medical billing services in USA and how they can significantly benefit your practice.
Understanding Medical Billing Services
Medical billing services are designed to manage the entire billing process for healthcare providers, from patient registration and insurance verification to claim submission and payment collection. These services ensure that healthcare providers receive timely and accurate payments for the services rendered. The primary goal is to minimize claim denials and rejections, thereby maximizing revenue.
Benefits of Outsourcing Medical Billing
Improved Efficiency: Outsourcing medical billing allows healthcare providers to focus on patient care rather than administrative tasks. Professional billing companies have the expertise and resources to handle billing processes efficiently, reducing the turnaround time for claims.
Reduced Errors: Medical billing companies employ trained professionals who are well-versed in coding and billing regulations. This reduces the likelihood of errors, which can lead to claim denials and delayed payments.
Cost Savings: Maintaining an in-house billing department can be costly due to the need for trained staff, software, and infrastructure. Outsourcing can significantly reduce these costs, as billing companies offer their services at competitive rates.
Compliance: The healthcare industry is heavily regulated, and staying compliant with the latest regulations can be challenging. Medical billing companies stay updated with the latest changes in regulations, ensuring that your practice remains compliant.
Enhanced Revenue Cycle Management: Professional billing services can optimize your revenue cycle by ensuring timely submission of claims and efficient follow-up on unpaid claims. This leads to improved cash flow and financial stability for your practice.
Top Medical Billing Companies in the USA
1. HRV Elite RCM: HRV Elite RCM offers comprehensive revenue cycle management services tailored to healthcare providers. Our expert team ensures efficient billing, coding, and claim management, maximizing your revenue and streamlining operations. Trust HRV Elite RCM for accuracy, compliance, and enhanced financial performance, allowing you to focus on patient care.
2. Kareo: Kareo is a leading medical billing company that offers comprehensive billing services for small practices. Their cloud-based platform is user-friendly and integrates seamlessly with electronic health records (EHR) systems. Kareo's team of experts ensures that claims are submitted accurately and on time, reducing the likelihood of denials.
3. AdvancedMD: AdvancedMD provides a robust medical billing solution that includes claims management, denial management, and patient billing. Their advanced analytics and reporting tools offer valuable insights into the financial health of your practice. AdvancedMD's billing services are designed to maximize revenue and improve efficiency.
4. DrChrono: DrChrono offers an all-in-one medical billing service that integrates with their EHR platform. Their billing team handles everything from coding and claim submission to follow-up on unpaid claims. DrChrono's transparent pricing model and excellent customer support make them a popular choice among healthcare providers.
5. Athenahealth: Athenahealth is a well-known name in the healthcare industry, offering comprehensive medical billing services. Their cloud-based platform automates many billing tasks, ensuring accuracy and efficiency. Athenahealth's team of experts handles claim submissions, follow-ups, and appeals, allowing healthcare providers to focus on patient care.
Choosing the Right Medical Billing Service
When selecting a medical billing service for your practice, it's essential to consider several factors:
Experience and Expertise: Look for a company with a proven track record and experience in your specialty. Experienced billing companies are more likely to understand the nuances of your practice and provide tailored solutions.
Technology and Integration: Ensure that the billing company uses advanced technology and integrates seamlessly with your existing EHR system. This will streamline the billing process and improve overall efficiency.
Transparency and Communication: Choose a billing company that offers transparent pricing and regular communication. Clear and open communication is crucial for addressing any issues that may arise during the billing process.
Customer Support: Excellent customer support is essential for a smooth billing process. Make sure the billing company provides reliable support and is responsive to your needs.
Compliance: Ensure that the billing company stays updated with the latest regulations and maintains compliance with industry standards. This will help protect your practice from potential legal issues.
Conclusion
Outsourcing medical billing services can significantly enhance the efficiency of your practice, allowing you to focus on providing quality patient care. By partnering with a reputable billing company, you can reduce errors, improve revenue cycle management, and stay compliant with industry regulations. The best medical billing companies in USA, such as Kareo, AdvancedMD, DrChrono, Athenahealth, and PracticeSuite, offer comprehensive solutions tailored to the unique needs of healthcare providers. Investing in professional medical billing services is a strategic decision that can lead to improved financial stability and overall success for your practice.
For more details do visit:
www.hrvelitercm.com
#Best medical billing companies in USA#Medical billing in USA#Revenue cycle management#billing and coding in USA
0 notes
Text
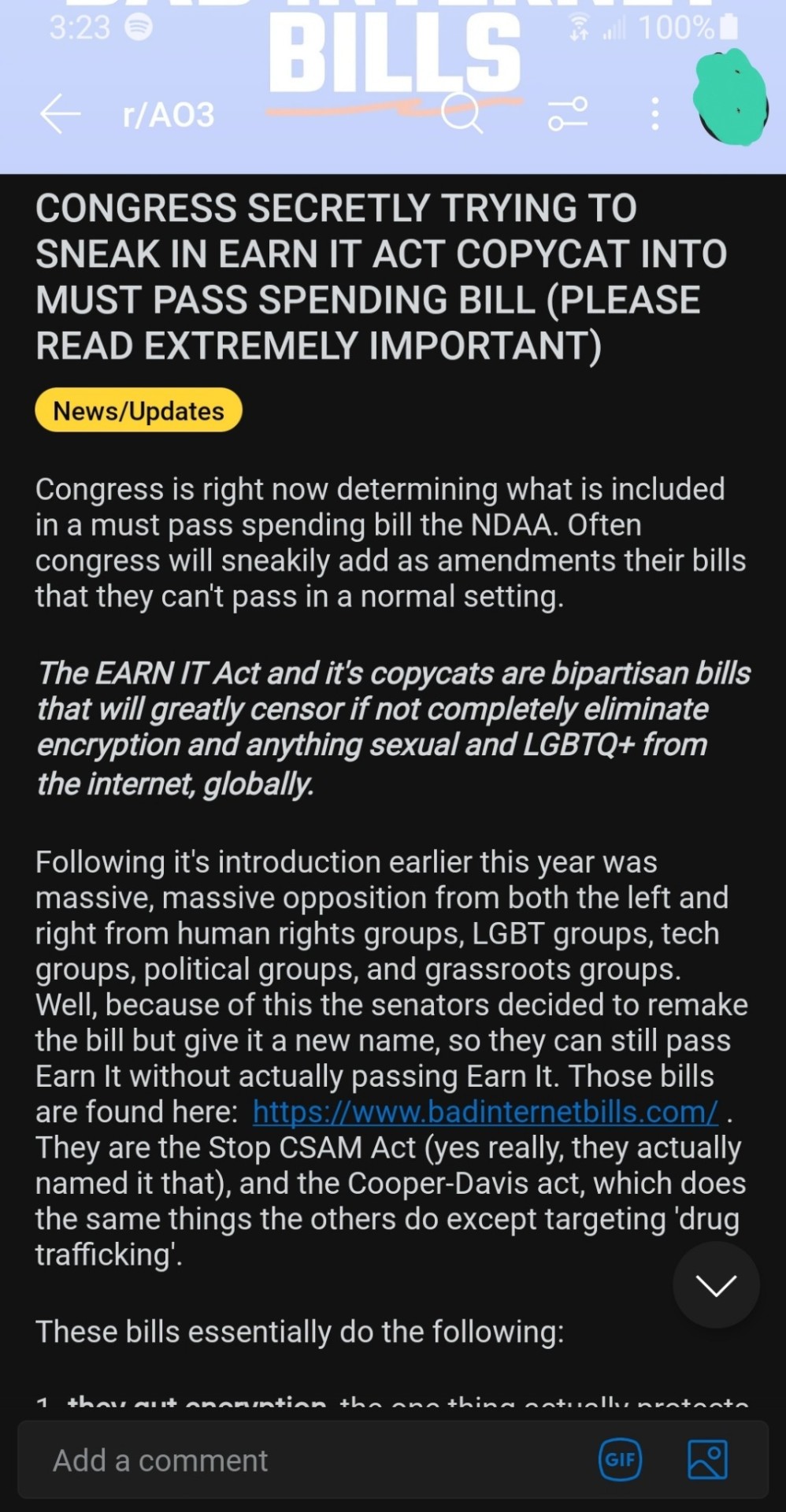

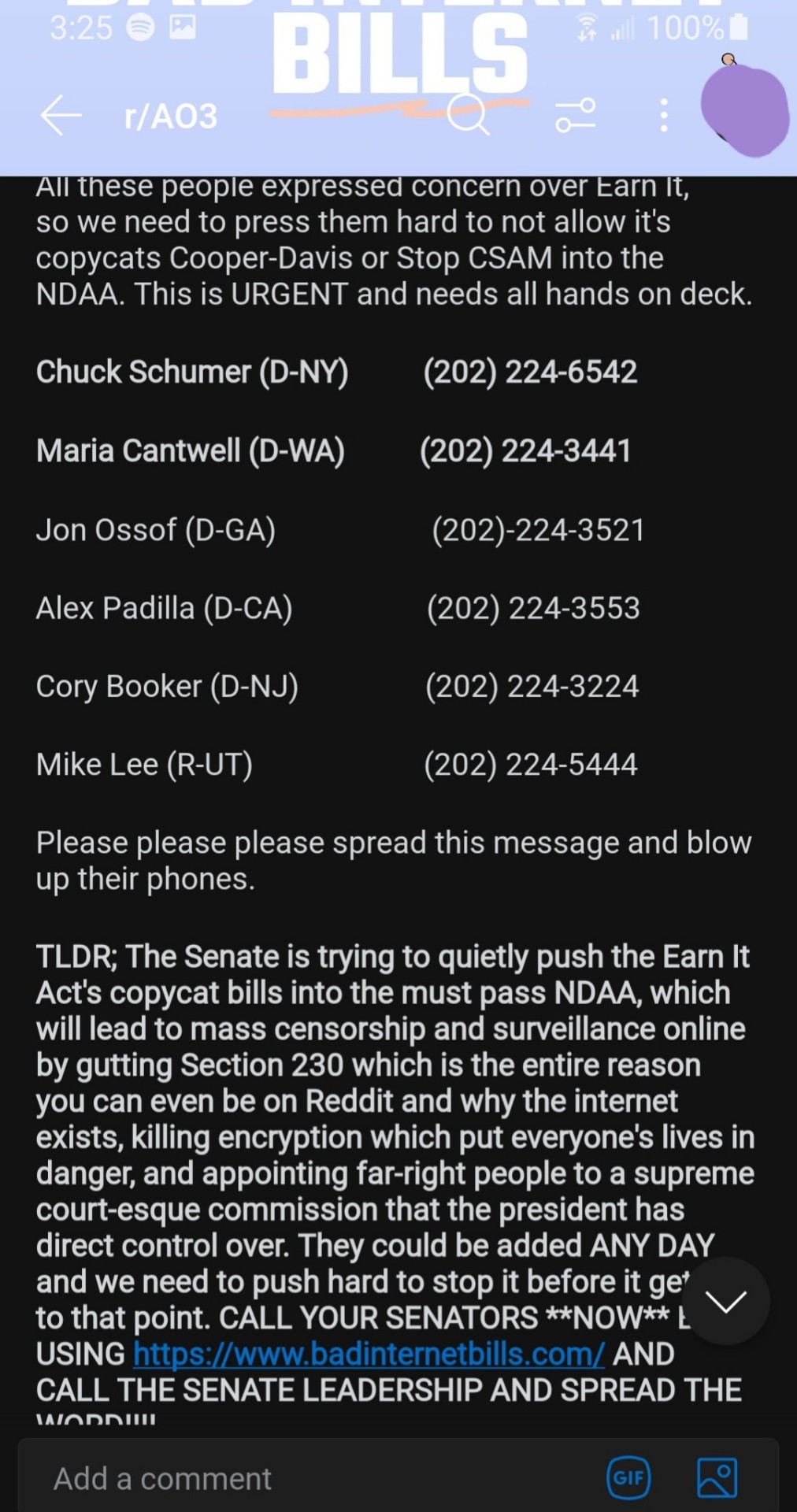
#ao3#archive of our own#earn it act#earn it bill#copycat earn it act#stop kosa#kosa act#stop bad internet bills#first amendment#censorship#CODE RED YOU GUYS#reddit#r/ao3#reddit news#fanfic#fanfiction#ao3 news#united states law#usa#american law#2023#online safety#online encryption#privacy#privacy rights#privacy regulations
253 notes
·
View notes
Text

Get expert medical coding services in USA and streamline your revenue cycle management.
#medical billing services#medical billing and coding#medical billing company#medical billing outsourcing#medical coding#medical billing specialist#usa#united states of america#united states#usa news#usa jobs#healthcare#health insurance
2 notes
·
View notes
Text
How Outsourcing DME Billing Improves Financial and Clinical Efficiency for Providers?

Are you a Durable Medical Equipment provider looking for financial viability and operational success?
If yes, adequate and correct DME billing is the key to such success.
Accurate DME billing and coding indicate timely and error-free claims processing. Such processing not only ensures timely healthcare reimbursements but also minimizes loss of revenue, keeping the practice financially sound.
But undertaking the DME billing and coding operations is extremely complicated and intricate. It requires stringent adherence to the constantly changing insurance policies and coding guidelines with little scope for error. Even a single mistake can result in denied claims and delayed payments.
Thereby, managing DME billing and coding in-house usually proves overwhelming for DME providers, requiring significant expertise, personnel, and constant training. This time-consuming process diverts attention from core clinical functions, eventually worsening the quality of patient care. Due to this, outsourcing DME billing services is still the only feasible solution to overcome these obstacles.
Considering such a need, let us look in-depth at how DME billing outsourcing enhances financial and clinical effectiveness for medical providers.
Outsource DME Billing for Streamlining Care and Cash Flow
Providers can eliminate significant administrative work, lower costly mistakes, and speed up reimbursements by outsourcing billing activities to specialists. The following are the benefits of outsourcing DME billing and coding:
Clinical Benefits
Outsourcing billing services optimizes workflow and enables a better quality of care experience in the following ways:
Improved Patient Experience
Proper billing and clear communication regarding charges minimize patient confusion and financial anxiety. Outsourced DME billing and coding services guarantee correct billing from the beginning, resulting in fewer conflicts and delays. When DME billing is efficient, patients are more likely to be satisfied with their care and return for follow-up services.
Focus on Patient Care
When DME billing is outsourced, the medical providers are in a better position to focus all their attention on patient care instead of concentrating on the administrative functions. This leads to better healthcare treatment results and builds stronger provider-patient relationships. Therefore, an in-house team such as doctors, nurses, and alike will be able to manage their time more productively, generating a more responsive and compassionate care environment.
Enhanced Compliance
Billing experts are trained to comply with all the latest healthcare regulations and payer policies. In this way, the provider is continuously in alignment with shifting standards, thereby minimizing legal exposure. Compliance also enhances patient trust, demonstrating a concern for ethical practices and honest reporting of care and billing.
Improved Scalable Solutions
Outsourcing billing to experts indicates the scope for flexibility in adjusting billing and coding services as per the needs of DME providers. In fact, the billing services can be enhanced and tailored depending on whether you wish to open a new office, expand the services, or handle seasonal changes. This flexibility helps the DME providers to grow and makes sure that the billing process never becomes an obstacle during times of change.
Financial Benefits
Outsourcing DME billing and coding allows healthcare providers to comply with regulations from payers and ensures financial operations are accurate and efficient in the following manner:
Reduced Audit Risk
Professional DME billers and coders remain up-to-date on the most recent healthcare regulations and payer policies. They confirm that all claims are compliant and complete, reducing the likelihood of errors leading to audits. Their compliance-oriented procedures also preserve precise documentation and coding, safeguarding the provider from financial and legal penalties.
Increased Revenue
Professional DME billing companies guarantee precise coding and prompt claim submission, eliminating rejections and denials. As a result, DME providers enjoy the benefits of faster payments with maximized revenue collection. They also track payer trends and refine billing strategies to reap every dollar due. This regular revenue stream makes the practice's financial health more robust.
Cost Savings
DME billing outsourcing lowers the cost of hiring, training, and keeping in-house billing personnel. It also avoids the need to purchase expensive billing software and IT infrastructure. The money saved can then be channelized into enhancing clinical services or expanding patient programs. As a result, this approach makes the practice financially stronger in the long term.
Access to Advanced Technology
The majority of outsourced DME billing companies utilize advanced billing software and analytic tools. These tools enable tracking of performance, identification of revenue trends, and better accuracy. Real-time reporting also gives visibility to the billing cycle and reveals bottlenecks. Furthermore, providers gain benefits through tools that assist in forecasting and financial planning.
The Future of DME Billing Outsourcing
The future of outsourcing DME billing and coding services to experts is very promising, with increased demand due to the need for quicker and more precise billing. Healthcare providers will increasingly depend on outsourcing partners that provide end-to-end revenue cycle management and advanced tools, such as real-time tracking and reporting.
Not only this but automation (including artificial intelligence) will also be used to quicken billing, minimize errors, and enhance reimbursements. Simultaneously, changing healthcare rules will make working with billing experts who stay updated and ensure compliance even more critical. Outsourcing will save providers time and money and allow them to concentrate on caring for patients.
Outsourcing DME billing and coding services companies, such as 24/7 Medical Billing Services, are at the forefront of this transformation. With a team of committed certified billing experts and innovative technology, 24/7 MBS ensures providers' compliance, increased claim approvals, and maximum revenue. Their scalable, flexible solutions make them the go-to partner for handling the future of DME billing.
FAQs
Q1. How quickly can I switch to an outsourced DME billing service?
Most implementations take 1–4 weeks, depending on practice size and existing systems.
Q2. Will I lose billing control by outsourcing it?
You can maintain complete control and transparency through detailed reporting and performance monitoring.
Q3. Will outsourcing impact my existing EHR or billing software?
Our billing partners can integrate with your existing software systems seamlessly.
Q4. Is staff training still needed if I outsource billing?
Minimum training is required, primarily for coordination and workflow understanding.
Q5. What KPIs should I monitor when outsourcing billing?
It is important to track AR aging, claim acceptance rates, denial trends, and reimbursement timelines.
Content Source: [https://www.247medicalbillingservices.com/blog/how-outsourcing-dme-billing-improves-financial-and-clinical-efficiency-for-providers]
For More Information:
Call us at 888-502-0537 or Sales: [email protected]
Support: [email protected]
Visit at https://www.247medicalbillingservices...
Our Office Locations:
Ohio: 28405 Osborn Road, Cleveland, OH, 44140
Texas: 2028 E Ben White Blvd, #240-1030 Austin TX, 78741
Subscribe @247medicalbillingservices
Follow us on social media channels-
Facebook: https://www.facebook.com/247MBS
Twitter: https://x.com/247MBServices
Instagram: https://www.instagram.com/247mbs/
LinkedIn: https://www.linkedin.com/company/24-7-medical-billing-services/
#DME Billing#Durable Medical Equipment Billing#Durable Medical Equipment Coding#Durable Medical Equipment Insurance Billing#Durable Medical Equipment#DME Billing New York#DME Billing services#Durable Medical Equipment Billing services USA#Durable Medical Equipment Billing Massachusetts#top Durable Medical Equipment Billing company#Durable Medical Equipment Billing Services California#Durable Medical Equipment Billing Services Rhode Island#DME Medical Services Connecticut#Durable Medical Equipment Billing Agency Delaware#DME Billing Agency Florida#Durable Medical Equipment Billing Company Georgia#DME Billing Company New Jersey#Best DME Billing Company Oklahoma#Top DME Billing Company Texas#Top DME Billing Company Ohio#Professional DME Billing Company USA#Cheap DME Billing Company Virginia#Outsourcing DME Billing Oregon#Outsourcing DME Billing Services Connecticut#Outsourcing DME Billing Services Florida#Durable Medical Equipment Billing Services Company#DME Billing Services Company Georgia#Best DME Billing Services providers USA#Best DME Coding Services Company#Leading DME Billing and Coding Services Company
0 notes
Text
How Can Clean Claims Transform Your Practice Success Today?

In today's complex healthcare environment, the submission of clean claims stands as a cornerstone of successful medical billing and coding services. Healthcare providers increasingly recognize that professional medical billing services are essential for maintaining financial stability and operational efficiency.
Understanding Clean Claims Significance
For healthcare practitioners, from primary care physicians to specialized surgeons, clean claims represent more than just paperwork—they're essential for practice sustainability. Professional medical billing and coding services focus primarily on ensuring claims are submitted correctly the first time, reducing delays and optimizing cash flow.
Key Provider Concerns
Healthcare professionals commonly express several concerns:
Delayed reimbursements affecting practice viability
Complex coding requirements and frequent updates
Staff overwhelm from claim corrections
Rising administrative costs
Compliance challenges
Strategic Goals for Healthcare Practices
Implementing comprehensive medical billing services helps achieve several critical objectives:
Maximize First-Pass Claim Rates Professional medical billing and coding services aim to achieve clean claims rates above 95%, significantly reducing resubmission needs.
Optimize Revenue Collection Efficient claims processing ensures faster payments and improved cash flow management.
Reduce Administrative Burden Healthcare practitioners can focus more on patient care when supported by effective medical billing services.
Technology Implementation
Modern medical billing and coding services leverage advanced technologies for:
Automated claim scrubbing
Real-time eligibility verification
Electronic remittance processing
Integrated coding validation
Staff Training Excellence
Healthcare practices must ensure their teams master:
Current coding guidelines
Insurance requirements
Documentation standards
Regulatory updates
Quality Assurance Processes
Effective medical billing services include:
Regular claim audits
Performance monitoring
Process improvement initiatives
Compliance checks
Best Practices for Clean Claims
Pre-submission Verification Essential checks include:
Patient demographic accuracy
Insurance verification
Authorization requirements
Coding precision
Documentation Standards Maintain comprehensive documentation supporting:
Medical necessity
Service delivery
Time requirements
Treatment plans
Regular Updates and Training Keep staff current on:
Coding changes
Payer policies
Regulatory requirements
Best practices
Performance Analytics Track crucial metrics including:
Clean claims percentages
Denial patterns
Processing timeframes
Collection rates
Impact on Practice Success
When healthcare providers implement effective medical billing and coding services, they experience:
Improved financial performance
Reduced administrative costs
Enhanced operational efficiency
Better patient satisfaction
Increased profitability
Future Trends in Claims Management
As healthcare evolves, billing practices must adapt to:
Value-based care models
New payment systems
Technological advances
Changing regulations
Solutions for Common Challenges
Complex Coding Requirements Professional medical billing services provide:
Certified coding expertise
Regular updates training
Quality assurance reviews
Compliance monitoring
Payer Policy Changes Effective medical billing and coding services include:
Policy update monitoring
Staff training programs
Process adaptation
Communication systems
Technology Integration Modern solutions offer:
Integrated platforms
Automated workflows
Real-time reporting
Analytics capabilities
Maximizing Practice Revenue
Healthcare practitioners can optimize revenue through:
Accurate charge capture
Timely submission
Proper documentation
Effective follow-up
Keys to Sustainable Success
Long-term success requires:
Consistent processes
Ongoing training
Regular audits
Performance monitoring
The Role of Technology
Advanced medical billing and coding services utilize:
AI-powered coding assistance
Cloud-based platforms
Mobile accessibility
Integrated analytics
Ensuring Compliance
Healthcare practices must focus on:
Documentation accuracy
Coding precision
Regulatory adherence
Regular updates
Building Better Workflows
Successful practices implement:
Streamlined processes
Quality checks
Team coordination
Performance tracking
Conclusion
In today's healthcare environment, clean claims submission represents a crucial element of practice success. By partnering with experienced medical billing services providers, healthcare practitioners can ensure financial stability while focusing on delivering quality patient care.
Contact Us
For seamless billing solutions and expert assistance, reach out to P3 Healthcare Solutions today!
Call us at: (844) 557–3227
Address: 3200 E Guasti Rd Suite 100, Ontario, CA 91761, United States
Read more: Transforming Healthcare Revenue: The Role of Comprehensive Medical Billing Services
1 note
·
View note
Text

VOCIS is a premier medical practice service provider in New York
We are specialized in comprehensive healthcare services designed to optimize your practice’s efficiency and profitability. Our primary offerings include Revenue Cycle Management, Medical Credentialing, Medical Billing Coding, Collections, Transcription, Medical Marketing, IT support, Virtual Receptionist, and Virtual Medical Scribe services, Medical Search Engines Optimization. We also provide specialized practice setup services for independent NPs, PTs, and MDs, ensuring a seamless start for healthcare professionals looking to establish or expand their practices.
Why choose VOCIS ?
We are dedicated to enhancing your practice’s financial performance, reducing administrative burdens, and ensuring compliance with the latest healthcare regulations. Our expert team delivers accurate and efficient services that streamline operations, improve cash flow, and boost patient satisfaction.
Partner with VOCIS to benefit from our personalized approach, cutting-edge technology, and commitment to your practice’s success, allowing you to focus on delivering exceptional patient care without the hassle of managing complex administrative tasks. With VOCIS, your practice is in capable hands.
Contact us today and experience the difference in efficiency, revenue and peace of mind.
End-to-End Healthcare service provider in New York
#Medical Marketing#Medical SEO#Local SEO#digital marketing#Google SEO#Digital medical marketing#Medical Billing#Medical Coding#Internet Marketing#Marketing for Physicans#USA
0 notes
Text
0 notes
Text
Best Medical Billing services
Our Medical Billing Services provide a comprehensive solution to streamline your practice’s revenue cycle, maximize reimbursements & improve cash flow. From accurate claims submission to timely follow-up and denial management, our expert team ensures each claim is processed efficiently to reduce payment delays. We handle complex billing, coding & compliance issues, allowing healthcare providers to focus on patient care. Trust our customized, secure services to optimize your practice’s financial health.

#Medical Billing Services#Best Medical Billing Services#Medical Billing#Medical Billing Company#Best Medical Billing Company#Medical Billing Company In USA#Top Medical Billing Company#Best Medical Billing Company in the USA#Best Medical Billing and Coding Company
0 notes
Text

Medical coding is a critical aspect of the healthcare industry, translating patient care into standardized codes for billing and documentation. However, errors in medical coding can lead to significant problems, including denied claims and compliance issues. Here are some common medical coding errors and tips on how to avoid them. CrosLinks, the best medical coding service company in USA offers comprehensive medical coding services to help healthcare providers achieve coding accuracy and maximize reimbursement. Our team of experienced coders stays up-to-date with the latest coding guidelines and utilizes advanced coding software to ensure optimal results. Trust CrosLinks for reliable medical coding solutions and expert assistance in managing your healthcare administration.
#best medical coding service company in USA#healthcare administration.#healthcare billing and coding#Medical billing and medical coding
0 notes
Text
Certified Clinical Medical Assistant: Bridging the Gap Between Doctors and Patients

In the intricate ecosystem of healthcare, the Certified Clinical Medical Assistant (CCMA) stands as a crucial linchpin, ensuring seamless communication and efficient operation within medical facilities. These professionals are uniquely positioned to bridge the gap between doctors and patients, providing essential support that enhances both patient care and the functionality of healthcare services.
The Role of a CCMA
Certified Clinical Medical Assistants wear many hats, balancing clinical duties with administrative tasks. This dual role makes them indispensable in healthcare settings, as they ensure both the smooth operation of the medical office and the delivery of quality patient care.
Clinical Responsibilities:
Patient Interaction: CCMAs often serve as the first point of contact for patients. They greet patients, take medical histories, and record vital signs. This initial interaction is crucial as it sets the tone for the patient's visit and provides the physician with essential information.
Assisting Physicians: During examinations and procedures, CCMAs assist physicians by preparing patients, handling instruments, and ensuring that the physician has everything needed for a successful exam. Their support allows physicians to focus more on diagnosing and treating patients.
Performing Tests: CCMAs are trained to perform routine laboratory tests, such as drawing blood and conducting urine analyses. They ensure that specimens are properly collected and processed, contributing to accurate and timely diagnosis.
Administrative Responsibilities:
Managing Patient Records: Accurate and up-to-date patient records are vital for effective healthcare. CCMAs are responsible for maintaining these records, ensuring that all information is accurately documented and readily accessible.
Scheduling and Coordination: CCMAs schedule appointments, manage patient flow, and coordinate with other healthcare providers. Their organizational skills help reduce wait times and improve the overall efficiency of the medical practice.
Insurance and Billing: Navigating insurance claims and billing can be complex. CCMAs assist patients with understanding their insurance coverage, handling billing inquiries, and resolving any issues that may arise. This support is essential for both patients and the financial health of the medical practice.
Enhancing Patient Care
CCMAs play a pivotal role in enhancing patient care through personalized attention and effective communication. Their ability to connect with patients on a personal level improves patient satisfaction and contributes to better health outcomes.
Personalized Care:
By addressing patient concerns, explaining procedures, and offering emotional support, CCMAs create a more comfortable and reassuring environment for patients. This personalized care is particularly important for patients who may feel anxious or uncertain about their medical visit.
Efficient Operations:
CCMAs ensure that medical facilities operate efficiently. Their ability to multitask and handle both clinical and administrative duties reduces bottlenecks, leading to shorter wait times and a more streamlined patient experience.
Effective Communication:
CCMAs serve as a critical communication link between patients and physicians. They relay important information, clarify instructions, and ensure that patients understand their treatment plans. This effective communication helps prevent misunderstandings and ensures that patients receive the care they need.
Supporting the Medical Team
CCMAs provide essential support to the entire medical team, enhancing the overall effectiveness of healthcare delivery.
Physician Support:
By handling routine tasks, CCMAs free up physicians to focus on more complex aspects of patient care. This support is invaluable in busy medical settings, where time and resources are often limited.
Team Coordination:
CCMAs coordinate with other healthcare professionals, including nurses, lab technicians, and specialists, to provide comprehensive care. Their ability to manage these interactions ensures that all members of the healthcare team are on the same page.
Training and Supervision:
Experienced CCMAs often take on roles in training and supervising new medical assistants. By sharing their knowledge and expertise, they help maintain high standards of care and ensure that new staff members are well-prepared for their roles.
The Importance of Certification
Certification Clinical Medical Assistant is a testament to a professional’s competence and commitment to excellence. Certified CCMAs have met rigorous educational and practical standards, which enhances their credibility and job prospects.
Quality Assurance:
Certification provides assurance to employers and patients that the CCMA has the necessary knowledge and skills to perform their duties effectively. It serves as a benchmark for quality in the profession.
Career Advancement:
Certified CCMAs often have more opportunities for career advancement and higher earning potential compared to their non-certified counterparts. Certification opens doors to specialized roles and leadership positions within the healthcare industry.
Conclusion
Certified Clinical Medical Assistants are integral to the healthcare system, bridging the gap between doctors and patients with their diverse skills and unwavering dedication. Their ability to perform both clinical and administrative tasks ensures that medical practices run efficiently and patients receive the highest quality of care. As the healthcare landscape continues to evolve, the demand for skilled and certified CCMAs will undoubtedly grow, further highlighting their essential role in the industry. Through their commitment to excellence and patient-centered care, CCMAs continue to make a significant impact on the lives of patients and the effectiveness of healthcare delivery.
More details do visit:
www.hrvelitercm.com
#Certification Clinical Medical Assistant#revenue cycle management#Medical billing in USA#medical records software#billing and coding in usa
0 notes
Text
Best Medical Billing & Revenue Cycle Management Services
Discover the best medical billing and exceptional revenue cycle management (RCM) services in Maryland, USA with Prime Med Billing. Whether you are looking for medical billing or medical codding, need a credentialing services or looking for virtual practice management services. Look, no further than Prime Med Billing that provides tailored solutions, expert coding, and technology-driven processes to maximize revenue and improve efficiency. Choose Prime Med Billing for improve your revenue in Medical World! Click now to read full article:
1 note
·
View note
Text
🩺📋 Tired of Insurance Headaches in Healthcare? We’ve Got You. 📋🩺
Ever had a claim denied because of eligibility issues? Or watched your front desk team drown in insurance verification chaos?
At RevMax Healthcare, we take the stress out of insurance eligibility and verification—so you can focus on patients, not paperwork. 💼✨
💡 Here's why our service matters: ✔️ Faster patient onboarding ✔️ Fewer claim denials ✔️ Real-time verification ✔️ 100% HIPAA compliant ✔️ Increased revenue & trust
Whether you're a clinic, hospital, or private practice, accurate insurance checks can make all the difference in how smoothly your operations run.
🔗 Learn more: revmaxhealthcare.com →
Because in healthcare, every detail matters. 🧾✅
#medical billing specialist#healthcare#medical billing services#insurance#medical billing and coding#medical billing company#health insurance#medical billing outsourcing#medical coding#insurance eligibility verification#usa#united states of america#united states
0 notes
Text
How Outsourcing DME Billing Improves Financial and Clinical Efficiency for Providers?
Discover how outsourcing DME billing to 24/7 Medical Billing Services increases revenue, decreases errors, and increases clinical efficiency for medical providers.
#DME Billing#Durable Medical Equipment Billing#Durable Medical Equipment Coding#Durable Medical Equipment Insurance Billing#Durable Medical Equipment#DME Billing New York#DME Billing services#Durable Medical Equipment Billing services USA#Durable Medical Equipment Billing Massachusetts#top Durable Medical Equipment Billing company#Durable Medical Equipment Billing Services California#Durable Medical Equipment Billing Services Rhode Island#DME Medical Services Connecticut#Durable Medical Equipment Billing Agency Delaware#DME Billing Agency Florida#Durable Medical Equipment Billing Company Georgia#DME Billing Company New Jersey#Best DME Billing Company Oklahoma#Top DME Billing Company Texas#Top DME Billing Company Ohio#Professional DME Billing Company USA#Cheap DME Billing Company Virginia#Outsourcing DME Billing Oregon#Outsourcing DME Billing Services Connecticut#Outsourcing DME Billing Services Florida#Durable Medical Equipment Billing Services Company#DME Billing Services Company Georgia#Best DME Billing Services providers USA#Best DME Coding Services Company#Leading DME Billing and Coding Services Company
0 notes
Text
Discover top-notch medical billing service in Florida with MedUSA Healthcare Services. We offer tailored billing solutions to meet the unique needs of healthcare providers. Our services are designed to improve accuracy and efficiency in your billing processes.
#medical billing service in Florida#medical billing services florida#medical billing companies in florida#medical billing services in florida#coding & consulting south windsor#medical billing services#best medical billing services#billing services in florida#medical billing service#healthcare billing service#medical billing companies in usa
0 notes
Text
Transforming Healthcare Billing with Medical Billing and Coding Services

Healthcare billing is a complex process that plays a critical role in ensuring smooth revenue cycles and patient care. Submitting clean claims is a pivotal aspect of this process, requiring meticulous attention to detail and compliance with regulations.
At P3 Healthcare Solutions, we excel in providing top-notch medical billing and coding services to healthcare practitioners, including doctors, nurses, and surgeons, helping them overcome challenges and achieve their goals. Our expertise also extends to MIPS reporting and consulting services, ensuring our clients stay compliant and financially secure.
Challenges Faced by Healthcare Practitioners
1. Frequent Claim Denials
Claim denials are among the most pressing issues for healthcare providers. Errors in documentation or coding can lead to rejected claims, impacting the financial stability of medical practices.
Our Solution:P3 Healthcare Solutions employs experienced professionals and advanced systems to ensure accurate claim submissions. Our medical billing and coding services focus on minimizing errors, reducing the risk of denials.
2. Navigating Regulatory Requirements
Keeping up with ever-changing regulations, such as those related to MIPS, can be daunting for healthcare practitioners. Non-compliance can lead to financial penalties and reputational harm.
Our Solution:Our MIPS reporting and consulting services ensure that your practice remains compliant with all relevant standards, relieving you of the burden of regulatory updates.
3. Managing Revenue Cycles
Healthcare providers often struggle to maintain a steady cash flow due to delayed reimbursements and complex billing systems.
Our Solution:We streamline your revenue cycle management by providing efficient and accurate medical billing and coding services, ensuring timely reimbursements and financial stability.
4. Administrative Overload
The administrative demands of billing and compliance can detract from the primary goal of delivering quality patient care.
Our Solution:Outsourcing your billing needs to P3 Healthcare Solutions allows you to focus on patient care while we handle the complexities of the billing process.
Goals of Clean Claim Submission
1. Faster Reimbursements
Timely payments are essential for maintaining operational efficiency in healthcare practices.
How We Help:Our meticulous billing processes ensure that claims are submitted accurately and promptly, leading to faster reimbursements.
2. Enhanced Compliance
Staying compliant with regulatory standards is crucial to avoid penalties and maintain credibility.
How We Help:With our MIPS reporting and consulting services, we ensure that your practice adheres to all applicable regulations, mitigating risks.
3. Improved Patient Trust
Patients value transparent and accurate billing processes, which enhance their overall experience and trust in your practice.
How We Help:We eliminate billing errors, ensuring that patients are charged accurately, fostering trust and long-term relationships.
4. Optimized Revenue
Accurate billing and coding directly impact the financial health of healthcare practices.
How We Help:Our medical billing and coding services focus on maximizing revenue through error-free submissions and efficient claim management.
How P3 Healthcare Solutions Leads the Way
Cutting-Edge Technology
We utilize advanced tools to ensure precision in billing and coding, reducing errors and speeding up the claims process.
Expert Team
Our team of certified coders and billing professionals is well-versed in industry standards, ensuring the highest level of accuracy and compliance.
Customized Services
We understand that each practice is unique. Our services are tailored to meet the specific needs of your practice, whether you require comprehensive medical billing and coding services or specialized MIPS reporting and consulting services.
Proven Results
With a track record of reducing denial rates and improving cash flow, P3 Healthcare Solutions is a trusted partner for healthcare providers.
The Impact of Clean Claims
Submitting clean claims isn’t just about avoiding errors—it’s about creating a system that supports better patient care, financial stability, and compliance. By prioritizing clean claim submissions, healthcare providers can:
Reduce administrative costs
Enhance operational efficiency
Improve patient satisfaction
Ensure financial growth
Contact Us
For seamless billing solutions and expert assistance, reach out to P3 Healthcare Solutions today!
Call us at: (844) 557–3227
Address: 3200 E Guasti Rd Suite 100, Ontario, CA 91761, United States
Read more: Transforming Healthcare Revenue: The Role of Comprehensive Medical Billing Services
0 notes
Text
Streamline Your Revenue Cycle with Effective Eligibility Verification

Eligibility verification is a critical process in the medical billing cycle, ensuring that healthcare providers receive payment for their services. It involves confirming a patient's insurance coverage and benefits before services are rendered. This step helps to prevent claim denials and delays, which can significantly impact a healthcare provider's revenue cycle. By verifying eligibility upfront, providers can identify potential issues early, communicate with patients about their financial responsibilities, and streamline the billing process. As a result, eligibility verification is a fundamental practice for maintaining a healthy financial operation in healthcare.
Benefits of Eligibility Verification
Implementing effective eligibility verification offers numerous benefits to healthcare providers. First, it reduces the likelihood of claim denials by ensuring that patients have active insurance coverage and that the services provided are covered under their plans. This proactive approach minimizes the administrative burden of reworking denied claims. Second, it enhances patient satisfaction by providing clarity about their insurance benefits and out-of-pocket costs, preventing unexpected bills. Third, eligibility verification improves cash flow by ensuring timely payments from insurers and patients, contributing to a more predictable and stable revenue stream.
Importance of Eligibility Verification
The importance of eligibility verification in medical billing cannot be overstated. It serves as the first line of defense against revenue loss, allowing providers to catch issues that could lead to denied or delayed payments. By verifying insurance details, providers can avoid the costly and time-consuming process of chasing unpaid claims. Additionally, eligibility verification helps maintain compliance with insurance requirements and reduces the risk of fraud. It ensures that only eligible patients receive services covered by their insurance, thus safeguarding the provider’s financial health and contributing to overall operational efficiency.
Cost of Eligibility Verification in the USA
While eligibility verification is essential, it does come with associated costs. These costs can vary based on the size of the healthcare practice and the complexity of their billing processes. Smaller practices may rely on manual verification methods, which can be time-consuming and labor-intensive. Larger practices often invest in automated verification systems or third-party services, which can be costly but offer greater efficiency and accuracy. Despite the initial investment, the long-term savings from reduced claim denials, improved RCM services, and enhanced patient satisfaction often outweigh the costs. Ultimately, the investment in eligibility verification is a strategic decision that can lead to significant financial benefits for healthcare providers in the USA.
The best Medical Coding Services for your businessAre you looking for effective eligibility verification service for your business? Mediclaim Management is the answer to your question. Medi Claim Management provides comprehensive medical coding services to ensure accurate and compliant coding practices. Our certified professionals use their expertise in major coding systems to maximize legitimate reimbursements and minimize compliance risks. The services include revenue integrity, denial prevention, and increased collections, all delivered by a team with decades of experience. Medi Claim Management handles various coding complexities, including HCPCS Level I/II and other intricate procedures, to keep reimbursements on track while healthcare providers focus on patient care. For more information, visit here.
#medical billing agency#medical billing and coding#medical billing outsourcing#medical billing and credentialing services#medical billing company#medical billing providers#medical billing appointment#medical billing for dermatology#medical billing call answering#eligibility verification service#us billing services#medical billing companies in USA#RCM services in boston#rcm providers in usa
0 notes