#Case Reports in Otolaryngology Journal
Text
Insights and Innovations: The Importance of Case Reports in Otolaryngology
Case reports are an important part of medical research and education, providing valuable insights into the diagnosis, treatment, and management of a wide range of medical conditions. In the field of otolaryngology, case reports play a crucial role in advancing our understanding of the many conditions that affect the ear, nose, and throat.
What are case reports in otolaryngology?
A case report is a detailed description of a particular patient’s medical condition and treatment. In otolaryngology, case reports typically focus on conditions that affect the ear, nose, and throat, such as hearing loss, sinusitis, laryngeal cancer, and more.
Case reports provide valuable insights into the diagnostic process, treatment decisions, and patient outcomes, allowing other medical professionals to learn from real-world examples and apply that knowledge to their own practice.
Why are case reports important in otolaryngology?
There are several reasons why case reports are important in otolaryngology. First, they provide a unique opportunity to learn from real-world examples. By studying case reports, medical professionals can gain a better understanding of the many conditions that affect the ear, nose, and throat, including rare and unusual cases that may not be well-documented in the medical literature.
Second, case reports can help guide clinical decision-making. By analyzing the diagnostic process, treatment decisions, and patient outcomes in a particular case, medical professionals can learn what works and what doesn’t, and make more informed decisions in their own practice.
Finally, case reports can help advance our understanding of the underlying biology and mechanisms of disease in otolaryngology. By studying individual cases in detail, researchers can identify new avenues for investigation and develop new treatments and therapies.
What can we learn from case reports in otolaryngology?
There are many things that we can learn from case reports in otolaryngology. For example, case reports can help us:
Understand the diagnostic process for a particular condition
Learn about new or innovative treatments and therapies
Identify risk factors and potential complications associated with a particular condition or treatment
Gain insights into patient outcomes and quality of life
Identify areas for further research and investigation
Case reports also play an important role in medical education, providing valuable learning opportunities for medical students, residents, and practicing physicians. By studying case reports, medical professionals can gain a better understanding of the many conditions that affect the ear, nose, and throat, and develop the skills and knowledge they need to provide the best possible care for their patients.
Conclusion
Case reports are an important part of medical research and education, providing valuable insights into the diagnosis, treatment, and management of a wide range of medical conditions. In otolaryngology, case reports play a crucial role in advancing our understanding of the many conditions that affect the ear, nose, and throat, and helping medical professionals develop the skills and knowledge they need to provide the best possible care for their patients.
If you looking for Case Reports in Otolaryngology contact or visit us!
Contact us: +447588268983
Visit us: https://www.literaturepublishers.org/journal/case-report-in-otolaryngology-ent.html
#otolaryngology case reports#case reports in otolaryngology#casereportsinOtolaryngology#Case Reports in Otolaryngology Journal#Journal of Otolaryngology Case Reports
0 notes
Text
Lupine Publishers | The Optimal Pain Management Methods Post Thoracic Surgery: A Literature Review

Abstract
Post-operative pain control is one of the key factors that can aid in fast and safe recovery after any surgical interventions. Thoracic surgery can cause significant postoperative pain which can lead to delayed recovery, delayed hospital discharge and possibly increased risk of chest complications in the form of atelectasis and even lower respiratory infections. Therefore, appropriate pain management following thoracic surgery is mandatory to prevent development of such morbidities including chronic pain.
Keywords: Thoracic Surgery, Analgesia, VATS, Robotics, Thoracotomy
Introduction
Thoracic surgical procedures can result in severe pain which can present as a challenge to be appropriately managed postoperatively. In particular, thoracotomies are well known for their severity of pain due to the incision, manipulation of muscles and ligaments, retraction of the ribs with compression, stretching of the intercostal nerves, possible rib fractures, pleural irritation, and postoperative tube thoracotomy [1]. Recognition of this has contributed to the development of minimally invasive techniques such as video assisted thoracoscopic surgeries (VATS) and lately robotic surgery [1]. These techniques not only aim to produce better aesthetic results, but also reduce post-operative pain and enhance recovery without compromising the quality of treatment offered. Poor pain management can lead to several and serious complications such as lung atelectasis, hypostatic pneumonia due to avoidance of deep breathing in these patients as a result of pain and superimposed infection [1]. Pain management as a result, does not only lead to greater patient satisfaction, but it also reduces morbidity and mortality in patients undergoing thoracic surgery [2]. Historically, post-operative pain management for thoracic surgery involved the use of narcotics alongside parenteral or oral anti-inflammatory agents [2]. Post chest tube removal patients typically are transitioned to oral analgesia. Multiple additional pain control adjuncts were also implemented with differing levels of success [1]. Over time, intra-operative techniques have been developed which aims to target pain reduction postoperatively [2]. As our understanding of both pain management and the factors that play a role in the development of pain has increased, we have been able to target these and improve postoperative pulmonary morbidity and pain scores [1,2]. We aim to review different means of pain control in this paper in order to assess their effectiveness in achieving optimum results.
Thoracotomy
The mechanism of pain in thoracotomy involves the innervation of the intercostal, sympathetic, vagus and phrenic nerves [3]. Additionally, shoulder pain may result from stretching of the joints during the operation.
After a thoracotomy, pain can persist for two months or more, and in certain incidences it recurs after a period of cessation. The incidence of chronic pain post thoracotomy is reported to be 22-67% in the population [4]. Good surgical technique and effective acute post-operative pain treatment are evident means of preventing post-thoracotomy pain and consequent pulmonary complications [4]. Due to the multifactorial character of the pain, a multimodal approach to target pain is advised. Typically, both regional and systemic anaesthesia are administered. A combination of opioids such as fentanyl or morphine are typically used [5]. A variety of techniques for the administration of local anaesthetics are available at present, and the effectiveness of each is assessed in this paper.
a) Thoracic Epidural Analgesia (TEA)
TEA was the most widely used method of means of analgesia. It was the gold standard means of pain relief [6,7]. It is typically inserted prior to general anaesthesia, at the level of T5-T6, midway along the dermatomal distribution of the thoracotomy incision. A study by Tiippana et al. [8] measured the visual analogue scale (VAS) in order to assess the presence of pain during rest and at the time at which they coughed in 114 patients of whom 89 had TEA and 22 who had other methods of pain control. TEA was effective in alleviating pain at rest and during coughing. In TEA patients, the incidence of chronic pain of at least moderate severity was 11% and 12% at 3 and 6 months, respectively. The study found that at one week after discharge, 92% of all patients needed daily pain medication. The study advised for extended postoperative analgesia for up to the week post-discharge to be administered in order to manage this. The study however concluded overall, that TEA was effective in controlling evoked post-operative pain. However, the study did encounter problems of technical form in 24% of the epidural catheters. The incidence of chronic pain, however, was lower compared with previous studies where TEA was not used. Several other studies support that TEA is superior to less invasive methods. According to Shelley B. et al. [9] TEA was preferred by 62% of the respondents over paravertebral block (PVB) with 30% and other analgesic techniques with 8%. Limitations of this technique included hypotension and urinary retention. Certain patients with active infection and on anticoagulation are excluded from epidural placement.
b) Paravertebral Block (PVB)
PVB is considered an effective method for pain management and its use has been increased in the recent years. This technique involves injecting local anaesthetic into the paravertebral space and it is able to block unilateral multi-segmental spinal and sympathetic nerves. Previous studies have shown that it is effective in achieving analgesia and is associated with a lower incidence of side effects such as nausea, vomiting, hypotension and urinary retention [10,11]. As the lungs are collapsed, it is associated with a lower risk of pneumothorax.
In a study by Davies R.G. et al. [10] there was no significant difference in pain scores, morphine consumption and supplementary use of analgesia between TEA and PVB. The rate of failed technique was lower in PVB (OR =0.28, p=0.007). Respiratory function was improved at both 24 and 48 hours with PVB but only significantly improved at 24 hours.
c) Intercostal Nerve Block (ICNB)
ICNBs are generally administered as single injections at least two dermatomes above and below the thoracotomy incision [12]. It is performed percutaneously or under direct vision, using single injections or through placement of an intercostal catheter. It can also be formed using cryotherapy. It is associated with reduced post-operative pain scores; however, it is less effective than TEA in controlling chronic pain [12]. This was illustrated by a study by Sanjay et al. [12] which found that patients that underwent ICNB had higher pain scores 4 hours post-operatively, than those who received epidural anaesthesia using 0.25% bupivacaine (p<0.05). The study concluded that in the early post-operative period there was significant impact in pain relief for both techniques, but thereafter, epidural anaesthesia was proven to significantly reduce post thoracotomy pain over ICNB. Due to the multifactorial nature of post-thoracotomy pain, various approaches are required in order to target pain. ICNBs are useful in the blockade of intercostal nerves, whilst PVB and TEA appear to block the intercostal and sympathetic nerves. Due to the inability of regional anaesthesia to block the vagus and phrenic nerves which are implicated in the pathophysiology of pain, NSAIDs and opioids are required as adjuncts. TEA is proven to be the most effective means of treating pain alongside PVB; however, it is associated with more side effects than PVB. At present, there are a limited number of studies directly comparing pain control and post-operative outcomes between PVB and TEA. There is no conclusive evidence that either method is superior to the other regarding pain control.
Video-Assisted Thoracoscopic Surgery (VATS)
Existing evidence supports the noninferiority of thoracic PVB when compared to TEA for postoperative analgesia [13]. PVB is versatile and may be applied both unilaterally or bilaterally. It can be used to avoid contralateral sympathectomy, consequently minimising hypotension. This is an apparent advantage it has over thoracic epidural. Furthermore, it offers a more favourable side effect profile when compared to epidural anaesthesia. At present, the factors taken into consideration when selecting a regional technique include tolerance of side effects associated with TEA, consensus on best practice/technique, and operator experience [13]. A randomised controlled trial by Kosiński et al. [14] compared the analgesic efficacy of continuous thoracic epidural block and percutaneous continuous PVB in 51 patients undergoing VATS lobectomy. The primary outcome measures were postoperative static (at rest) and dynamic (coughing) visual analogue pain scores (VAS), patient-controlled morphine use and side-effect profile. The study found that pain control (VAS) was superior in the PVB group at 24 hours, both at rest (1.7 vs3.3, p=0.01) and on coughing (5.8 vs 6.6, p=0.023), and control of pain at rest was also superior in the PVB group at 36 hours (3.0 vs 3.7 (p=0.025) and at 48 hours (1.2 vs 2.0, p=0.026). There were no significant differences in the postoperative morphine requirements. In regard to side-effect profile, the study showed that the incidence of postoperative urinary retention (defined as no spontaneous micturition for 8 hours or ultrasound-assessed volume of the urinary bladder >500ml) was greater in the epidural group (64.0% vs 34.6%, p=0.0036), as was the incidence of hypotension (32.0% vs 7.7%, p=0.0031). There was no significant difference in the incidence of atelectasis (4.0% vs 7.7%, p=0.0542). However, the incidence of pneumonia was significantly more frequent in the PVB group (3.8% vs 0%, p=0/0331). Kosiński et al. concluded that PVB is as effective as thoracic epidural block in regard to pain management as it offers a superior safety profile with minimal postoperative complications. A further randomised controlled trial by Okajima et al. [15] compared the requirements for postoperative supplemental analgesia in 90 patients who received wither a PVB or thoracic epidural infusion for VATS lobectomy, segmentectomy or wedge resection. The main outcome measures were pain scores at rest (verbal rating scale 0= none and 10=maximum pain), blood pressure, side effects and overall satisfaction scores relating to pain control (1=dissatisfied and 5=satisfied). The study found a similar frequency of supplemental analgesia (50mg diclofenac sodium suppository or 15mg pentazocine intramuscularly) for moderate pain in both groups, with 56% of those in the PVB group requiring ≥2 doses, compared to 48% in the epidural group (p=0.26). Hypotension, defined as a systolic blood pressure <90mmHg, occurred more frequently in the epidural group (21.2% vs 2.8%, p=0.02). There was no difference in the incidence of pruritus (3.0% vs 0%, p=0.29) and post-operative nausea and vomiting (30.3% vs 25.0%, p=0.62) between both groups. The study found no statistical difference between patient-reported satisfaction in pain control between epidural and PVB using the verbal rating scale (5.0 vs 4.5, p=0.36). The study concluded that PVB offered additional to equivalent analgesia to epidural, a lower incidence of haemodynamic instability postoperatively. A further study by Khoshbin et al. [16] performed an analysis on 81 patients undergoing VATS for pleural aspiration +/- pleurodesis, lung biopsies or bullectomy. The main outcome was postoperative pain levels, documented every 6 hours and scored against the Visual analogue Scale (0= no pain, 10= worst possible pain). In both PVB and epidural groups, bupivacaine 0.125% was the local anaesthetic of choice, with clonidine added to the epidural infusion at 300μg in 500ml. The study showed that there was no significant difference in mean pain scores between PVB or EP (2.1 vs 2.9, p=0.899), therefore concluding that PVB is as effective as epidural in controlling pain post-VATS.
Robotic Lung Surgery
Minimally invasive techniques are considered advantageous over open surgical approaches due to their shorter recovery times, reduced perceived levels of pain post-operatively and shorter postoperative length of stay in hospital [17-19]. Robotic surgery has become a popular method in recent years. Debate remains regarding whether robotic surgery is superior to VATS in regard with pain reduction. A case control study by Louie et al. [19] compared 45 robotic assisted lobectomies (RAL) to 34 VATS lobectomies. The study showed that both groups had a similar mean ICU stay (0.9 vs 0.6 days) and a mean total length of stay (4.0 vs 4.5 days). The study showed that patients that underwent robotic lobectomies had a shorter duration of analgesic use post-operatively (p=0.039) and a shorter time resuming to normal everyday activities (p=0.001). A limitation in this study was an inaccurate record of the amount of pain relief used by the patients, ultimately working as a confounding factor when interpreting the results. In a separate study by Jang et al. [18] 40 patients undergoing RAL were compared retrospectively to 80 VATS patients (40 initial patients and 40 most recent patients), all with resectable non-small cell lung cancer. The study showed that the post-operative median length of stay was significantly shorter in RAL patients compared to the initial VATS patients. The rate of post-operative complications was significantly lower in the RAL group (10%) compared to the initial VATS group (32.5%) and similar to the recent VATS group (17.5%). Post-operative recovery was easier for patients in both the RAL and VATS group due to earlier mobilisation, allowing them to return to their everyday activities quicker. In a retrospective review by Kwon et al. [17] 74 patients undergoing robotic surgery, 227 patients undergoing VATS and 201 patients undergoing anatomical pulmonary resection were assessed and compared with regard to acute (visual pain score) and chronic pain (Pain DETECT questionnaire). The study showed that there was no significant difference in acute or chronic pain between patients undergoing robotic assisted surgery and VATS. Despite no significant difference in pain scores, 69.2% of patients who underwent robotic-assisted surgery felt the approach affected their pain versus 44.2% of the patients who underwent VATS (p=0.0330). These results all support the superiority of robotic surgery over VATS and open approaches with regard to pain, length of hospital stay and recovery times. Both robotic surgery and VATS have their benefits i.e. two-versus three-dimensional view, instrument manoeuvrability, and reduced post-operative pain.
Conclusion
Since post-thoracotomy pain is multifactorial, a multimodal approach is required. In particular, ICNB blocks the intercostal nerves, and PVB and TEA appear to block the intercostal and sympathetic nerves. NSAIDs and opioids are required as valgus and phrenic nerve cannot be blocked by regional anaesthesia. TEA is evident to be the most effective in treating pain alongside with PVB. It is however associated with more side effects than PVB.
For more information about Surgery & Case Studies: Open Access Journal please click https://lupinepublishers.com/surgery-case-studies-journal/
For more Lupine Publishers please click on below link
https://lupinepublishers.com/
#lupine#lupine publishers#lupine publishers llc#SCSOAJ#clinical trials#Pharmacology and Physiology Case Reports#Cytology#otolaryngology#dermatology#anesthesia#Oral Investigations#Toxicology Case Reports#Surgery and case studies#open access journals#submission#manuscript
4 notes
·
View notes
Text
Journal of Clinical and Medical Images
Journal of Clinical and Medical Images illustrations is a peer-reviewed, high impact factor medical journal established Internationally which provides a platform to publish Clinical Images, Clinical Case Reports, Medical Case Reports, Case Series (series of 2 to 6 cases) and Clinical Videos pertaining to medical conditions.
Manuscript Submission
Authors are requested to submit their manuscript by using Online Manuscript Submission Portal:
(or) also invited to submit through the Journal E-mail Id: [email protected]
Journal of Clinical Imaging Science
Literature Publishers working for the growth of the researchers, scholars and students by publishing their valuable research work and case studies.
Scope of Clinical & Medical Images Journal
International journal of medical case reports, hematology images, images in hematology, journals that accept case reports, case reports in hepatology, archives of clinical and medical case reports, journal of clinical case reports impact factor, clinical case reports journal impact factor, journal of otolaryngology head and neck surgery, journals accepting clinical images, journal of dental case reports, gastroenterology journal case report, ophthalmology case report journals, case reports in nephrology and dialysis, gi case report journals, clinical imaging journal impact factor, orthopedic surgery case reports, international journal of clinical case reports, journal of medical diagnostic methods, international journal of dental case reports, eye case reports, clinical case reports international impact factor, scholars journal of medical case reports, journal of invasive cardiology case report, dental case reports journal, journal of medical imaging and case reports impact factor, journal of oral health case reports, journal of clinical images and case reports impact factor, international journal of medical and dental case reports, journal of clinical images and case reports, journal of surgical technique and case report, journal of clinical and medical images impact factor, journal of case reports and medical images, journal of case reports and images in surgery, ophthalmology case studies, clinical journal of gastroenterology and hepatology, Journal of cardiology and cardiovascular medicine, clinical images journal, clinical and medical case reports, International medical case reports journal, case report journal impact factor, clinical images, journal of cardiology cases, clinical case reports journal, surgery case reports, case reports in endocrinology, case reports in orthopedics, journal of clinical case reports, journal of cardiology case reports, journal of laryngology and otology, scholars journal of medical case reports impact factor, case reports ophthalmology, case reports in dentistry, journal of medical cases, cardiology case reports journal, case reports in orthopedic research, journal of clinical imaging science impact factor, gastroenterology case reports, international journal of clinical cardiology impact factor, ophthalmology case reports, impact factor journals of medical case reports, neuro ophthalmology case reports, case reports in hematology, international journal of medical case reports impact factor, clinical case report impact factor, case reports in otolaryngology, clinical case reports journals, endocrinology case reports.
0 notes
Text
Journal of Clinical and Medical Case Reports

Journal of Clinical and Medical Case Reports publishes clinical case reports, medical case series, medical case studies, medical case reports and clinical images for publication that fall under the scope of all clinical and medical studies. Journal of Clinical and Medical Case Reports mainly focuses on symptoms, signs, diagnosis, treatment, and follow-up of patient disease in different areas of the journal in diagnostic case report and treatment.
Journal Homepage: https://www.literaturepublishers.org/
Journal of Clinical and Medical Case Reports is a peer-reviewed open access high impact factor indexed Journal that publishes highly cited research work conducted as case reports in the medical field on various types of diseases, covering their respective clinical journal case reports, medical journal case report, clinical reports, medical case reports, clinical images, clinical case reports, journal of medical case reports and diagnosis issues.
Scope and Keywords: Journal of Clinical and Medical Case Reports, Open Journal of Clinical and Medical Case Reports, Journal of Medical Case Reports, Clinical and Medical Case Reports, Journal of Clinical Images and Medical Case Reports, Journal of Clinical Studies & Medical Case Reports, Journal of Clinical and Medical Case Studies, International Journal of Clinical and Medical Cases, Journal of Clinical Medicine, Clinical Case Reports, International Medical Case Reports Journal, Archives of Clinical and Medical Case Reports, Case Reports - A journal for medical case reports, International Journal of Clinical Case Reports and Reviews, Japanese Journal of Clinical and Medical Case Reports etc.
Journal of Clinical and Medical Case Reports
Journal publishes only high quality articles from all over the world. Journal of Clinical and Medical Case Reports follows double blinded peer review process. All Editors are active and Editorial Board Members belonging to reputed institutions from abroad. They are senior faculty members, doctors, scientist and research fellows etc. Journal regularly releasing issues with good number of articles in the form of clinical images and case reports.
Scope of Clinical and Medical Case Reports Journal
Authors can also find this journal in their scope on the basis these keywords: medical case reports journals, journal of medical case reports, clinical image, cardiology case reports, case reports cardiology, case reports in cardiology, case reports pediatrics, pediatrics case reports, ent journal, case reports hematology, hematology case reports, journal of otolaryngology head and neck surgery, orthopaedics & traumatology, case reports gastroenterology, case reports in gastroenterology, gastroenterology case report, clinical case report journal, International journal of surgery case reports, case images, dermatology case reports, case report in ophthalmology, case report ophthalmology, case reports in surgery, clinical image journal, journal of surgical case reports, ophthalmology case report, journal of clinical imaging science, literature publishers, cardiology case report journals, journal of traumatology, case reports in nephrology, case reports nephrology, nephrology case reports, clinical images in medicine, journal of pediatric surgery case reports, medical image analysis journals, journal of medical case reports impact factor, otolaryngology case reports, clinical case reports impact factor, case reports otolaryngology, surgical case reports, journal of orthopedic case reports, case reports in neurological medicine, best case report journals, journal of otology and laryngology and, clinical imaging impact factor etc.
Medical Case Report Journal scope also includes medical advancements with an aim towards special techniques that are implementing in all aspects of the human anatomy journal. The body image journal is running with a strong desire to provide knowledge on recent scientific research and advances in the field of Clinical and Medical Studies. The aim of the clinical imaging journal is to collect an article in the Journal of Clinical and Medical Case Reports across all clinical imaging science, medical imaging science and clinical fields, thereby integrating international medical case reports and clinical knowledge.
We feel honored to associate with and invite scientists and researchers to submit their original research/ medical case report journal/ body imaging journal/ clinical imaging journal/ clinical imaging science in International journal of clinical and medical images and case reports work for publication in literature publishers: journal of clinical and medical case studies and reports. This journal considers articles in the form of a research article, review article, short communication, opinion, Image, Case reports and commentary.
Journal of Clinical and Medical Case Reports covers all the areas of Medical Science Journal that includes: case reports in oncology, oncology case reports journal, case reports in cardiology, journal of cardiology case reports, international journal of surgery case reports, case reports in surgery, journal of surgery case reports, general surgery case report, surgical case reports journal, surgery case reports journal, journal of dermatological case reports, case reports in dermatology, case reports in endocrinology, case reports endocrinology, case reports in gastroenterology, gastroenterology case report journals, case reports in hematology, case reports in nephrology, orthopedic surgery case reports, journal of orthopedic case reports, case reports in pediatrics, journal of pediatric surgery case reports, case reports in microbiology, clinical microbiology case reports, case reports in genetics, case reports in toxicity, case reports in neuroscience, case reports in ophthalmology, case reports in andrology and gynecology, case reports in dentistry, case reports in odontology, case reports in otolaryngology, case reports in ENT, case report in head and neck surgery etc.
Journal of Clinical and Medical Case Reports encourages authors and scientists all over the world to submit their work related to various diseases, clinical trials, radiology, surgery, basic research, epidemiology, and palliative care. At a time when the research on drug delivery is taking place at a tremendous phase.
Manuscript Submission
Authors are requested to submit their manuscript by using Online Manuscript Submission Portal:
(or) also invited to submit through the Journal E-mail Id: [email protected]
0 notes
Text
Horrifying video reveals molting spider rustling in woman's ear

The spider in the woman's ear was making continuous, weird clicking and rustling noises that were so bad, she couldn't sleep.
Scared of spiders? You might want to look away now.
In a bizarre medical case, a woman in Taiwan got a nasty shock when doctors discovered a spider about 0.1 inch (0.25 centimeters) long crawling in her left ear canal. At first glance, it looks like there are two spiders scuttling around in there, but the second arachnid is actually just the spider's molted hard outer shell, or exoskeleton.
The 64-year-old woman had visited an ear, nose and throat clinic at the Tainan Municipal Hospital in Taiwan after spending four days hearing weird sounds in her left ear.
The day her symptoms started, she was woken up to a strange feeling that a creature was moving inside her ear. She then began to hear incessant beating, clicking and rustling sounds that were so bad, she struggled to sleep.
At the hospital, doctors discovered that a small spider with bulging, brown eyes was moving within the ear's external auditory canal, the passageway that links the outside of the ear to the eardrum. They also saw that the spider had molted its ghostly white exoskeleton — something that spiders normally do when they grow so that it can be replaced with a new one.
"She didn't feel pain because the spider was very small. It's just about 2 to 3 millimeters [0.07 to 0.12 inch]," Dr. Tengchin Wang, co-author of the report and director of the otolaryngology department at Tainan Municipal Hospital, told NBC News.
The case report, published Oct. 21 in The New England Journal of Medicine, didn't note the species of spider or how the critter might have gotten into the woman's ear. Although these instances are rare, there have been documented cases of spiders crawling into people's ears, and it happens with insects, too: Live insects account for about 14% to 18% of cases of the foreign objects that doctors find in the external auditory canal. This is likely because the area is warm and dark, so it provides a welcoming space for these critters.
Dr. David Kasle, an otolaryngologist at ENT Sinus and Allergy of South Florida who was not involved in the woman's case, told NBC News that the average ear, nose and throat specialist will see "tens, if not more, of bugs or some sort of arthropod" in ear canals throughout their career. However, he said this particular case was "unusual and disturbing."
Wang had seen insects — such as ants, moths and cockroaches — in people's ears before, but he'd never come across a spider that had shed its exoskeleton inside a person's ear canal, NBC News reported.
Wang and his team successfully removed the spider and its exoskeleton from the woman's ear by sucking it out with a thin tube, called a cannula, placed through an otoscope, a tool doctors use to look into the ear. The woman's symptoms vanished after the arachnid was removed. For bigger spiders or insects, a local anesthetic should be used to kill the critter before it's removed to "prevent excessive movements and subsequent damage to the structures of the ear," the case report authors wrote.
However, liquids should never be used if the eardrum has been pierced and has holes in it, the authors cautioned; this wasn't the case for women in Taiwan. Wang told NBC News that, to be on the safe side, anyone who experiences any of these symptoms should see a doctor even if they think the bug or spider has exited their ear, just in case an antenna or exoskeleton got left behind.
This article is for informational purposes only and is not meant to offer medical advice.
1 note
·
View note
Text
Negative Pathology Report Following Salivary Gland
Surgery for Suspected Primary Tumor– What Went
Wrong?

Abstract
Objective: For patients undergoing an oncologic surgery, postoperative pathological diagnosis negative for a tumor is a confusing outcome. Additionally, it may carry clinical and medicolegal consequences. The study defines the causes of such discrepancies in order to prevent such instances in the future.
Methods: A retrospective cohort study of patients who had undergone resection of a major salivary gland for a suspected or diagnosed primary tumor but had no tumor on surgical pathology.
Results: Eight patients (2.5%) had negative pathology. Causes for negative pathology were A) Surgical pathology error (n=3) B) Surgical management error (n=1) C) Surgery for definite diagnosis (n=2) D) Unexplained (n=2).
Conclusions: Negative pathology in salivary gland surgery is not rare. Negative pathology should raise the suspicions of both the surgeon and the pathologist. An immediate multidisciplinary review of all data will find the cause in most cases Keywords: Negative pathology; no tumor on pathology; salivary gland tumor; parotid gland tumor
Read More About This Article Click on Below Link:
https://lupinepublishers.com/otolaryngology-journal/fulltext/negative-pathology-report-following-salivary-gland-surgery-for-suspected-primary-tumor.ID.000262.php
Read More about Lupine Publishers Google Scholar Articles:
https://scholar.google.com/citations?view_op=view_citation&hl=en&user=dMOUw-wAAAAJ&https://scholar.google.com/citations?view_op=view_citation&hl=en&user=dMOUw-wAAAAJ&cstart=100&pagesize=100&citation_for_view=dMOUw-wAAAAJ:vD2iS2Kej30C
#lupine publishers#lupine publishers group#scholarly journal of otolaryngology#journal of otolaryngology#sjo
0 notes
Text
Case Reports in Clinical Medicine Journal and Images
Case Reports in Clinical Medicine Journal and Images accepting Clinical Medicine articles, journal of Clinical Medicine case reports, journal publishing Clinical Medicine case reports, images in Clinical Medicine journal, image journal in Clinical Medicine, journal of Clinical Medicine images etc. Case Reports in Clinical Medicine Journal and Images is an International, open access journal which considers case reports in all areas of clinical medicine which advance general medical knowledge. Of particular but not exclusive interest are case reports in the areas of arthritis and musculoskeletal disorders, cardiology, circulatory, respiratory and pulmonary medicine, dermatology, ear, nose and throat and otolaryngology, endocrinology, ethics, health services and epidemiology, gastroenterology, geriatrics, obstetrics and gynaecology, reproduction, women’s health, oncology, pathology, psychiatry, neurology, psychology, and trauma and intensive medicine.
Journal Homepage: https://www.literaturepublishers.org/
Case Reports in Clinical Medicine Journal and Images: Visual images are a rich source of the information we use in clinical medicine, yet we expend little effort to enhance our perception and recognition of these images. A new feature introduced in this issue of the Journal, Case Reports in Clinical Medicine Journal and Images, will present a broad representation of useful and clinically important visual images. We believe that exposure to these photographs will help sharpen the reader's ability to identify common forms. As doctors we encounter an enormous variety of images from day to day, including skin lesions, funduscopic views, blood smears, bone marrow smears, urine sediments, microbiologic specimens, joint etc.
Manuscript Submission
Authors may submit their manuscripts through the journal's online submission portal: https://www.literaturepublishers.org/submit.html
(or) Send an e-mail attachment to the Editorial Office E-mail Id: [email protected]
0 notes
Text
Case Reports in Dentistry - Salford Publishers
Dentistry is the diagnosis, treatment, and prevention of disorders of the teeth, gums, mouth and jaw. Often considered essential for overall oral health, dentistry can affect the health of your entire body.
The Journal of Clinical Images and Case Reports in Dentistry Journal Friend Check, Open Access Journal Case Journal which distributes case reports and case management, case report documents in dental journals over the entire field of dentistry, including dental or case reports odontology, Case Reports in Dentistry, journals, dental Pathology, reported only as oral and maxillofacial medical procedures.
Submit your Case Reports in Dentistry Journal via Online Submission at: https://www.salfordpublishers.org/publisher/submission/Japanese-Journal-of-Dentistry-Case-Reports
Or as an e-mail attachment to the Editorial Office at E-mail id:- [email protected]
For More Details Visit:- https://www.salfordpublishers.org/publisher/Japanese-Journal-of-Dentistry-Case-Reports
#pulmonology case reports#case reports in dentistry journal#case reports in dentistry#otolaryngology case reports#case reports in otolaryngology
0 notes
Text
Juniper Publishers- Open Access Journal of Case Studies

Symptomatic Pulmonary Embolism after Achilles Tendon Repair
Authored by Naoki Yoshida
Abstract
The incidence of symptomatic pulmonary embolism (PE) following treatment for Achilles tendon rupture is rare. Here we present a case of a 40-year-old man with symptomatic PE, who was operated 24 days ago for Achilles tendon rupture. Computed tomography angiography (CTA) showed numerous pulmonary emboli in the bilateral pulmonary artery from the main pulmonary artery and a thrombus in the inferior vena cava (IVC) from the left iliac vein. The patient was treated using an anticoagulant and IVC filter and showed a good functional outcome at the five-month follow-up. It is important to examine and treat Achilles tendon rupture, keeping in mind PE.
Background
Achilles tendon rupture is common in orthopedic practice [1]. In both operative and conservative treatments, cast immobilization is necessary to protect the repaired tendon [2]. There are a few reports on the incidence of symptomatic PE following treatment for Achilles tendon rupture [3,4]. This current report underscores the possibility of acute PE in cases of Achilles tendon rupture.
Case Presentatıon
A 40-year-old man presented to the emergency department with a painful left heel. The pain was suddenly brought on during aerobics, but he was able to walk despite the pain. He had no past medical history and was not on any medication at that time. On physical examination, there were a palpable gap in the left Achilles tendon, and Thompson test was positive. We diagnosed left Achilles tendon rupture and discussed the treatment with the patient. He agreed to have surgical repair and was operated upon nine days post injury. The tendon was sutured using the Kessler technique (Figure 1) and was subsequently protected by a below-the-knee cast in a plantar-flexed position. The patient was permitted to walk on crutches. He was discharged from our hospital, and he returned to work with no complications.
Two weeks postoperatively, his cast was converted into an Achilles tendonitis brace. However, 24 days postoperatively, he presented to the emergency department with sudden severe dyspnea. On examination, his blood pressure was 88/59mmHg, pulse 98/min, and respiratory rate 26/min, with an O2 saturation of 93% in room air. CTA showed numerous pulmonary emboli in the bilateral pulmonary artery from the main pulmonary artery (Figure 2A). CTA also showed a vein thrombus in the IVC (Figure 2B) from the left iliac vein (Figure 2C). There was no thrombus in the right iliac vein. The patient was administered an anticoagulant and IVC filter as treatment for acute PE. The side of the Achilles tendon surgery coinciding with the side of the thrombus strongly suggested the Achilles tendon repair was the cause of PE. One month later, angioplasty revealed the thrombus had disappeared, so the IVC filter was removed. The patient showed a good functional outcome and returned to work at the six-month follow-up.
Discussion
The Achilles tendon is the largest tendon in the body, but it often ruptures, mostly during sports activities [5]. Injury is caused by a sudden pushing off from the weight-bearing forefoot with the knee in extension, unexpected ankle dorsiflexion, and violent dorsiflexion of a plantar-flexed foot [6]. Achilles tendon rupture can be managed by both operative and nonoperative strategies. It is generally accepted that surgery should be performed for athletes and young and fit patients and that conservative treatment may be suitable for the elderly [7]. Both treatments include a period of immobilization, which is a welldocumented risk factor for deep vein thrombosis (DVT) [2]. In the current literature, the reported incidence of DVT after Achilles tendon rupture is highly variable, ranging from less than 1% to 34% [8]. Common symptoms and signs of DVT are unilateral or asymmetric swelling, leg edema, pain, erythema, fever, and leg warmth [9]. Actually, most DVT patients are asymptomatic, and only 9%–17% of them show clinical manifestation [9]. However, silent DVT can progress to a PE, a significant source of mortality [10].
There are several controversies surrounding thromboprophylaxis for Achilles tendon rupture. Several authors have recommended that the use of milder forms of prophylaxis, such as aspirin, also be explored [11]. Others have recommended that prophylactic anticoagulation not be routinely administered [12]. It is important to examine and treat Achilles tendon rupture, keeping in mind DVT and PE.
For more articles in Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php
#juniper publishers journals#Juniper Publishers Contact#Surgical case reports#Maxillo-facial Surgery#Obstetrics and Gynaecology#Otolaryngology
0 notes
Text
How Marijuana Accelerates Growth of HPV-related Head and Neck Cancer Identified

University of California San Diego School of Medicine researchers have identified the molecular mechanism activated by the presence of tetrahydrocannabinol (THC) — the ingredient that causes people to feel the euphoria or “high” associated with cannabis — in the bloodstream that accelerates cancer growth in patients with human papillomavirus (HPV)-positive head and neck squamous cell carcinoma.
“HPV-related head and neck cancer is one of the fastest growing cancers in the United States. While at the same time, exposure to marijuana is accelerating. This is a huge public health problem,” said Joseph A. Califano III, MD, senior author and professor and vice chief of the Division of Otolaryngology in the Department of Surgery at UC San Diego School of Medicine.
Head and neck squamous cell carcinoma is the sixth most common cancer worldwide. These cancers begin in the cells that line the mucous membranes inside the mouth, nose and throat. Approximately 30 percent of cases of this disease are related to HPV infection, and it is these cases, in particular that are on the rise. Califano suggested increased marijuana use may be a driving factor.
Previous studies have linked daily marijuana exposure to an increased prevalence of HPV-related throat cancer. However, a mechanism linking cannabis exposure to increased growth of the cancer was unknown.
Reporting in the January 13, 2020 online edition of Clinical Cancer Research, a journal of the American Association for Cancer Research, researchers outline how the presence of THC in the bloodstream activates the p38 MAPK pathway, which controls programed cell death called apoptosis. When activated, p38 MAPK prevents apoptosis from occurring, thus allowing cancer cells to grow uncontrollably.
Working with Chao Liu, MD, visiting scientist at UC San Diego and a physician at China’s Central South University, and other colleagues, Califano and team used animal and human cell lines to show that THC turns p38 MAPK on and were able to stop the growth of HPV-positive head and neck cancer by turning off the pathway.
The team then analyzed blood samples from patients with HPV-related throat cancer who had their genomes comprehensively mapped to define activated gene pathways. Similar to the cell lines, the blood samples showed p38 MAPK activation and loss of apoptosis in tumors from patients with THC in their blood.
The authors said studies and public opinion suggestions that THC and other cannabis products have cancer-fighting properties need additional, more critical evaluation. Past studies showing anticancer effects of THC and other cannabinoids often used levels of THC higher than those found with recreational use, but doses used recreationally clearly activate a cancer-causing pathway, said Califano.
“We now have convincing scientific evidence that daily marijuana use can drive tumor growth in HPV-related head and neck cancer,” said Califano. “Marijuana and other cannabis products are often considered benign, but it is important to note that all drugs that have benefits can also have drawbacks. This is a cautionary tale.”
“How Marijuana Accelerates Growth of HPV-related Head and Neck Cancer Identified“
#science#medicine#hpv#hpv related cancers#head and neck cancer#sex-related conditions#infectious disease#marijuana#thc#cannabis#recreational marijuana#public health#academic medicine#ucsd#uc san diego
38 notes
·
View notes
Link
#otolaryngology case reports#case reports in otolaryngology#casereportsinOtolaryngology#Case Reports in Otolaryngology Journal#Journal of Otolaryngology Case Reports
0 notes
Text
Numb Chin Syndrome Secondary to Vestibular Schwannoma | Lupine Publishers
Lupine Publishers | Journal of Otolaryngology

Abstract
Numb chin syndrome (NCS) or mental neuropathy is a sensory neuropathy. It can present as trivial finding of hypoesthesia/ paraesthesia or pain over the chin and area supplied by the mandibular nerve. The etiology can vary from dental pathogenesis to malignancy and neurological disorders. Here we present a case report of 18 year old female patient, who presented with numb chin syndrome and on further investigation was detected with a large vestibular schwannoma.
Introduction
Parasthesia or Numbness over the chin is common symptom in dental practice. It is generally seen as adverse effect of peripheral neurectomy that may occur during oral surgical procedures involving inferior alveolar nerve. However, in certain instances it may be symptom of serious underlying disorder such as malignancy or neurological pathology. In this case report we highlight one such case of a young patient presenting with a trivial symptom of numbness over the chin which was the only manifestation of a large intracranial Schwannoma.
Case Report
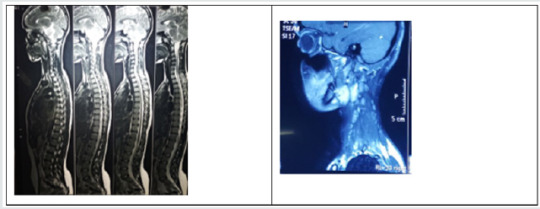
An 18 year old female patient reported with chief complaint of numbness in the left lower side of the face for 2 months. Her medical and dental history was not significant. She was well built and nourished, conscious and cooperative during the examination. On extra oral examination there was no facial a symmetry. Temporomandibular examination was normal. A single jugulodigastric lymph node was enlarged and tender on the left side. It was firm in consistency and not fixed. On intraoral examination, two ulcers spherical in shape and less than 1cm in diameter with peri inflammatory halo were noticed on the left lower labial mucosa. Tongue was coated with mild erythematous changes on the left lateral aspect, soft palate and tonsillar pillars on the left side were also erythematous. We performed cranial nerve examination and found deficit on the mandibular division of trigeminal nerve. Pulp vitality testing was done and all the teeth on the lower left quadrant did not respond. OPG showed widening of the mandibular foramen. A provisional diagnosis of numb chin syndrome was made, and patient was advised for a complete blood count and MRI of head and neck. Blood reports were within normal limits. The MRI detected a well-defined encapsulated heterogenous signal intensity in the left cerebellopontine angle (CP) which had solid and cystic components and measured 4.7 X 4.3cm with intracanalicular extension causing widening of internal carotid artery. Compression on the 4th ventricle, pons and left cerebellar hemisphere. Similar intensity lesion was noticed in carotid space in the left side of neck measuring 5 X 3.7cm (Figures 1 & 2). Patient was referred to neurologist and was diagnosed as schwannoma associated with neurofibromatosis type 2. She was referred to neurosurgeon, who has kept her under observation.
Figure 1: MRI Axial View.
Figure 2: MRI Sagittal View.
Discussion
Numb chin syndrome (NCS) or mental neuropathy is a sensory neuropathy. It was first described by Charles Bell IN 1830 [1] (BELL C On the nerve of the face, in nervous system and human body: embracing the pears delivered to the royal society subject of the nerves 1833, Duff Green: Washington p65. Google Scholar). It can present as trivial finding of hypoesthesia/paraesthesia or pain over the chin and area supplied by the mandibular nerve. The etiologies of this condition can be grouped as [2,3]:
a) Dental: Iatrogenic trauma during oral surgical procedure (Most common cause).
b) Malignancy/Systemic Disease: In the absence of any trauma due to dental/oral surgical procedures NCS has been reported as the first sign of Primary malignancy like osteosarcoma of the mandible and oral squamous cell carcinoma metastatic malignanciesof the breast, lung, thyroid etc. or hematological malignancies such as lymphoma, leukemia, multiple myeloma. It has also been reported to have presented initially as numbness over the chin. This could be considered as herald sign of relapse in patients with history of malignancy (Rogers sign).
c) Neurological: Tumors of the inferior alveolar nerve and the sheaths and compression at the base of the skull by tumor mass may also cause NCS (Figure 3).
Figure 3: MRI Coronal View.
In the presence of metastatic disease NCS is an advanced symptom. This symptom is often overlooked or not urgently investigated. It is one of the symptoms with poor prognosis, only 15% of patients are known to survive more than nine months. NCS has better prognosis if it has leptomeningeal involvement. Hence the role of dentists, ENT specialists and physicians is to consider malignancies and neurological disorders in patients with NCS in the absence of local causes. Patients need investigation to rule out malignancies and neurological disorder. This involves blood examination and radiographs which include OPG, brain MRI and targeted imaging such as CT scan and scintigraphy [4]. The trigeminal nerve root originates from the lateral aspect of the pons and extends superiorly, laterally and anteriorly towards the petrous apex entering the Meckel’s cave. The first segment which extends from the brainstem to the Meckel’s cave is referred to as cisternal or cerebellopontine angle segment. The cerebellopontine angle is a triangular space located posterior to the pyramid inferior to the tentorium, lateral to pons and ventral to cerebellum.
The most common mass found in this location is vestibular schwannoma, commonly referred to as acoustic neuroma, followed by meningioma and epidermoid tumors and rarely metastases [5]. Nerve sheath tumors can be dividing into schwannoma, neurofibroma and malignant nerve sheath tumors. Schwannoma/ neurilemmomas are encapsulated, benign slowly growing neoplasms arising from Schwann cells of central, spinal, peripheral nerves, oligodendrocytes of the myelin in the brain. Primary intracranial nerve sheath neoplasm are mostly schwannomas and they do not have malignant potential. 5- 20% of these cases are associated with type 2 neurofibromatosis [6]. Type 2 neurofibromatosis is an inherited autosomal dominant syndrome with a propensity for developing multiple schwannomas, meningiomas and gliomas [7,8]. A mutation in the tumor suppressor gene NF2 located on chromosome 22 is identified as the reason for this syndrome. Neurofibroma in contrast, have propensity for malignant transformation. Spinal neurofibroma is sporadic tumor and is usually sign of von Recklinghausen disease i.e., type 1 neurofibramatosis. There are 3 types of neurofibromatosis.
a) Type 1 NF1: Skin and bony changes present early usually in childhood.
b) Type 2 NF2: Associated with Hearing loss and poor balance.
c) Type 3 NF3/Schwannomatosis: Congenital neurilemmoma characterized by multiple peripheral nerve tumors without the involvement of vestibular nerve.
Intracranial nerve schwannomas are benign tumors that are slow growing [9]. Most of them arise from cranial nerves, the most common being the vestibular schwannoma. Clinical signs are: Progressive unilateral sensorineural dysacusis, Intermittent hearing loss, Tinnitus and sensation of fullness in the ear, Vertigo, difficulty in walking, Visual blurring, Trigeminal neuralgia and headaches. All these signs were absent in our patient. Trigeminal schwannomas account to only about 0.2% - 0.8 % of the total intracranial nerve schwannomas it is also associated with neurofibromatosis -2. Their clinical presentation can vary from neuralgia, neurasthenia or numbness as in our case. It has female predilection. Jefferson has classified trigeminal schwannomas based on their location into four types [10].
CT imaging displays it as is dense regions difficult to differentiate. Areas within large tumors are hypodense. On administration of contrast it shows moderate enhancement. MRI is the investigation of choice for these lesions. T1- weighted image, it appears as isointense and cystic areas appears hypointense. T2 images it appears as hyperintense to brain and cystic areas appear hyperintense [11]. Treatment is directed at symptomatic control. Surgical resection of intracranial tumors carries a risk of significant morbidity such as hydrocephalus and meningitis. Microsurgical techniques have better outcome with preservation of neurologic function. Malignant nerve sheath tumors have poor prognosis [11]. After the neurological evaluation, our patient has been kept under observation, it was considered best not to perform any intervention. Patient has been under continuous follow up and during the preparation of this manuscript she has been found to be stable.
Conclusion
It is important that symptoms of parathesia over the chin are never overlooked as trivial in patients. Investigations such as MRI of brain may reveal an underlying pathology that may be detrimental.
For more Lupine Publishers Open Access Journals Please visit our website: h
https://lupinepublishersgroup.com/
For more Journal of Otolaryngology articles Please Click Here:
https://lupinepublishers.com/otolaryngology-journal/
To Know More About Open Access Publishers Please Click on Lupine Publishers
#Lupine Publishers#Lupine Publishers Group#Lupine Publishers Indexing Journals#Journal of Otolaryngology#ENT Research Journal
42 notes
·
View notes
Text

A woman wearing a protective mask smells a rose as she wanders through the Paris streets. Photograph By Myriam Tirler, Hans Lucas Via Redux
How COVID-19 Can Damage All Five Senses
The virus that causes the disease disrupts not just smell and taste, but all the ways humans perceive the world. For some, the loss may be permanent.
— By Stacey Colino | September 28, 2021
Considering how sick he was, Michael Goldsmith seemed like one of the lucky ones, because he survived. After becoming severely ill with COVID-19 in March 2020, he spent 22 days on a ventilator in the ICU. Fortunately, Goldsmith’s condition improved, and he was moved to an intermediate level of care in the hospital as he recovered. That’s when he began to realize he had lost most of his hearing in his left ear.
“Anything I did hear had to be loud, and then it sounded like Charlie Brown’s teacher,” says Goldsmith, now 35, referencing the nonsensical noises the teacher made in the popular cartoon show.
He also had a static sound in that ear that turned out to be tinnitus. After he fully recovered from the infection and went back to his home in Bergenfield, New Jersey, the IT security analyst and father of two saw one doctor after another, seeking relief for his hearing problems. He tried several different prescription medicines, and still he was no better off.
It’s easy to take our senses for granted—until there’s a problem with one of them. This is something many people who suffered from COVID-19 discovered when they unexpectedly lost their senses of smell and taste. More recently, though, it has become apparent that a COVID-19 infection can also affect sight, hearing, and touch.
In the short term and the long run, this virus can affect all the ways we perceive and interact with the world.
Though not life-threatening, “it’s disarming to lose any of these senses, especially as suddenly as happens in the context of this infection,” says Jennifer Frontera, a professor of neurology at the NYU Grossman School of Medicine.
Diminished Hearing
Like Goldsmith, many people who recovered from COVID-19 continued to experience some auditory loss. In the March issue of the International Journal of Audiology, researchers reviewed published case studies and other reports of COVID-19 symptoms, and they estimate that hearing loss has occurred in about 8 percent of patients who had COVID, while about 15 percent developed tinnitus.
The mechanisms aren’t completely understood, but experts suspect the disease may affect the eustachian tube, which connects the middle ear with the throat. “With any viral infection, you can have eustachian tube dysfunction, which can lead to fluid build-up in the middle ear—this acts as a mechanical dampener on the ear drum,” explains Elias Michaelides, an associate professor of otolaryngology at Rush University Medical Center in Chicago.
Once someone recovers from the illness, the eustachian tube drains and hearing returns to normal in most cases, though it can take a couple of weeks, he says. In the meantime, taking an oral decongestant and using a nasal steroid spray may help hasten drainage, says Michaelides.
But if the virus damages the sensory neurons in the inner ear or cochlea, sudden hearing loss may occur, and it may be permanent. Exactly how this nerve damage happens isn’t clear, though it may have to do with COVID-19’s ability to trigger a cascade of inflammatory effects and small blood vessel damage.
Because Goldsmith’s hearing didn’t improve in his left ear after he fully recovered and tried various prescription medications, he went to see J. Thomas Roland, Jr., chair of the department of otolaryngology-head and neck surgery at NYU Langone Health. Roland told him he was a good candidate for a cochlear implant, a small electronic device that can directly stimulate the auditory nerve and generate signals that the brain registers as sound.
“The inner ear is a very delicate organ and very susceptible to microvascular problems and inflammation, so I’m not surprised people have experienced hearing loss or tinnitus related to COVID,” says Roland.
In September 2020, Goldsmith had a cochlear implant surgically placed in his left ear. It has made a world of difference, he says. “I now have 80 percent recognition of single words, and it’s even higher with full sentences in my left ear.” And when the device is on, his tinnitus disappears completely. “I wish I didn’t need this,” Goldsmith says, “but I’m glad I had it.”
Blurred Sight
Other people who’ve had COVID-19 have reported problems with their vision. A study published last year in BMJ Open Ophthalmology found that light sensitivity, sore eyes, and blurred vision are among the more common eye disorders experienced by patients. And in a study involving 400 COVID-19 patients who were hospitalized, researchers found that 10 percent had eye disorders, including conjunctivitis, vision changes, and eye irritation.
“There is definitely a viral load in the eye that causes symptoms, but that doesn’t mean it necessarily causes long-term diseases in the eye,” says study co-author Shahzad I. Mian, a professor of ophthalmology and visual sciences at the University of Michigan Medical School.
Still, some doctors are finding that the SARS-CoV-2 virus can increase the risk of blood clots throughout the body, including in blood vessels in the retina, which can cause blurry vision or some degree of vision loss, explains Julia A. Haller, ophthalmologist-in-chief at the Wills Eye Hospital in Philadelphia.
If someone experiences any vision changes possibly related to COVID-19, it’s important for them to see an ophthalmologist as soon as possible, the experts say. “Some forms of vision loss are treatable with medications, depending on how much damage has occurred,” Haller says.
Tingling and Numbness
A person’s sense of touch also can be affected by a COVID-19 infection, since the disease has been shown to cause persistent neurologic symptoms.
In a study published in May 2021, researchers evaluated 100 people who weren’t hospitalized for COVID-19 but had ongoing symptoms. They found that 60 percent had numbness and tingling six to nine months after the onset of their illness. Sometimes these symptoms were widespread throughout the body; in other instances, they were localized to the hands and feet.
The exact mechanisms behind these stubborn symptoms aren’t well understood, but they most likely relate to local inflammation and local infection with COVID-19 virus in the nerves, explains Igor Koralnik, a professor of neurology at the Northwestern Feinberg School of Medicine and chief of the division of neuroinfectious diseases and global neurology at Northwestern Memorial Hospital in Chicago.
“In most cases, [the numbness and tingling] improves over time,” he says. “Everybody goes at their own pace.” And in some cases, tingling and other symptoms of neuropathy can be treated with medications like gabapentin, a drug that is used to prevent seizures and relieve nerve pain.
Loss of Smell and Taste
Perhaps the most recognizable effect COVID-19 has on the senses is the one-two punch of lost smell and taste. Elizabeth DeFranco, a medical sales rep in Cleveland, Ohio, experienced both sensory changes shortly after developing a mild COVID-19 infection in June 2020.
“I was eating salt and vinegar potato chips, and I couldn’t taste anything,” recalls DeFranco, 58. Then she realized she couldn’t smell anything, either. These losses remain with her to this day, though once in a while she gets a brief whiff of an odor like freshly cut grass.
Viral-induced smell loss existed before anyone had ever heard of COVID-19, but the percentage of people who experience smell dysfunction or loss is much higher with this virus than with other types of infections, experts say. A review of studies published in 2020 found that of 8,000 subjects with confirmed COVID-19, 41 percent experienced problems with smell and 38 percent reported problems with taste. When people who contract COVID-19 lose their sense of smell, a condition called anosmia, they lose it across the board, not just with one type of scent.
Generally speaking, there are two major types of smell loss. Conductive smell loss can occur when nasal congestion or obstruction prevents odor molecules from passing into the nasal cavity. Sensorineural smell loss involves damage or dysfunction to the olfactory neurons, which seems to be what’s happening with COVID-19.
“With COVID-19, most people don’t have a lot of nasal symptoms, and yet smell loss can be fairly severe,” says Justin Turner, an associate professor of otolaryngology-head and neck surgery at Vanderbilt University Medical Center and director of the Vanderbilt Smell and Taste Center. “We believe this stems from damage to sustentacular cells that live way up in the nose and are particularly susceptible to infection by the virus.”
As people recover from COVID-19, regenerating cells can spring into action and make new functional neurons, Turner explains. This allows most people to regain their sense of smell six to eight weeks after infection—but not everyone does. At that point, doctors may prescribe systemic or topical steroids and sometimes smell conditioning, which involves repeated exposure to essential oils that have different scents. It’s like the olfactory equivalent of physical therapy.
“What you’re doing is exposing the olfactory system to these odorants and helping the brain form new connections,” Turner explains. “Once the damage [to neurons] has been done, we’re relying on regenerative capacity in the olfactory system to help people regain their sense of smell.”
Losing the sense of taste usually goes hand in hand with the loss of smell, says Michael Benninger, professor and chair of the department of otolaryngology-head and neck surgery at the Cleveland Clinic Lerner College of Medicine.
“We are not seeing people who have truly lost their sense of taste [with COVID-19 infection]. When people lose their sense of smell, their taste is diminished”—meaning, their ability to discriminate between different flavors is lost. “If the sense of smell comes back, taste comes back, too,” Benninger says.
Since she recovered from COVID-19, DeFranco has tried numerous interventions—including steroid medications, antibiotics, cryotherapy, craniosacral therapy, supplements, homeopathic remedies, and smell retraining. Nothing has helped. So she has found ways to work around these limitations to protect her safety. She installed additional smoke detectors in her home because she wouldn’t be able to smell smoke. She throws all her food out by the “best by” date and often has a neighbor smell food from her fridge to make sure it hasn’t spoiled.
The worst part: “It is very depressing to think that this anosmia could be forever. I have no enjoyment of food,” she says. “I may never be able to appreciate the taste of wine or chocolate or the smell of a barbecue or cookies baking in the oven or the salt in the air when I go to the ocean. No one can really empathize unless it happens to them.”
1 note
·
View note
Text
Journal of Clinical Images

Clinical Image Journal: Journal of Clinical Images accepting articles in the form of images, image case, clinical images journal, image of journal, clinical image illustrations journal, clinical research image journal, clinical research imaging journal etc. Journal paves a great platform to access the recent developments of the clinical and medical world and is employed for publishing the varied case reports & clinical images that pertains to many clinical and medical conditions. Clinical Image Journal: Journal of Clinical Images is an international peer reviewed open access journal focused on publishing the most complete, reliable source of research information, current developments, and clinically interesting, trainees and researchers in all surgical subspecialties, as well as clinicians in related fields. Clinical Image Journal: Journal of Clinical Images is internationally peer reviewed and provides major understanding of diagnosis of many diseases, their management and their therapeutic strategies that aims in improving health outcomes globally. Case reports and clinical images are required altogether areas of medicine and involves research using the human volunteers who are intended to contribute to the clinical and medical knowledge.
Journal Homepage: https://www.literaturepublishers.org/
Manuscript Submission
Authors are requested to submit their manuscript by using Online Manuscript Submission Portal:
(or) also invited to submit through the Journal E-mail Id: [email protected]
The mission of Clinical Image Journal: Journal of Clinical Images is to publish, in a timely manner, the very best clinical research around the world with special attention to the impact of medical imaging on patient care. Clinical Image Journal: Journal of Clinical Images publications cover all imaging modalities, radiology issues related to patients, policy and practice improvements, and clinically-oriented imaging physics and informatics. Clinical Image Journal: Journal of Clinical Images is a valuable resource for practicing radiologists, radiologists-in-training and other clinicians with an interest in imaging.
Papers are carefully peer-reviewed and selected by our experienced subject editors who are leading experts spanning the range of imaging sub-specialties, which include: Body Imaging- Breast Imaging- Cardiothoracic Imaging- Imaging Physics and Informatics- Molecular Imaging and Nuclear Medicine- Musculoskeletal and Emergency Imaging- Neuroradiology- Practice, Policy & Education- Pediatric Imaging- Vascular and Interventional Radiology.
Clinical Image Journal: Journal of Clinical Images Scope
Case reports / Clinical Images can be prospective or retrospective and examine the effects of an intervention in more than one patient. All case reports and clinical Images submitted need to comply with the relevant reporting criteria. It is dedicated to publishing Medical Case Reports, Clinical Images, Case Series and Clinical Videos. The following classifications and topics related to it will be considered for publication in the Journal but not limited to the following fields.
Neurology Image Journal, Oncology Image Journal, Dentistry Image Journal, Surgery Image Journal, Cardiology Image Journal, Nutrition and Dietetics Image Journal, Ophthalmology Image Journal, Gastroenterology Image Journal, Internal Medicine Image Journal, Nephrology Image Journal, Palliative Care Image Journal, Physiotherapy Image Journal, Radiation Oncology Image Journal, Sleep Disorders Image Journal & Sleep Studies Image Journal, Anesthesiology Image Journal, Emergency Medicine Image Journal and Critical, Forensic Image Journal and Legal Medicine Image Journal, Infectious Disease Image Journal, Infertility Case reports, Neurological Surgery Image Journal, Obstetrics Image Journal and Gynecology Image Journal, Otolaryngology Image Journal, Pharmacology Image Journal and Therapeutics Image Journal, Physical Medicine Image Journal & Rehabilitation Image Journal, Radiology Image Journal, Dermatology Image Journal, Endocrinology Image Journal, Diabetes Image Journal & Metabolism Image Journal, Orthopedics Image Journal & Rheumatology Image Journal, Pathology- Anatomic & Clinical Image Journal, Pulmonary Image Journal Disease, Preventive Medicine Image Journal, Respiratory Medicine Image Journal, Urology Image Journal, Oral Medicine Image Journal, ENT Image Journal, Geriatric Medicine Image Journal, Maxillofacial Surgery Image Journal, Neonatology Image Journal, Nuclear Medicine Image Journal, Pain Management Image Journal, Pediatrics Image Journal, Psychiatry Image Journal, Sexual Health Image Journal, Vascular Medicine Image Journal, Family Medicine Image Journal and Public Health Image Journal, Allergy Image Journal & Immunology Image Journal, Diabetology Image Journal, Hematology Image Journal.
0 notes
Text
Journal of Clinical and Medical Images
Clinical Images and Case Reports Journal (CICRJ) is a peer-reviewed, high impact factor journal established Internationally which provides a platform to publish Clinical Images, Clinical Case Reports, Medical Case Reports, Case Series (series of 2 to 6 cases) and Clinical Videos pertaining to medical conditions.
Journal Homepage: https://www.literaturepublishers.org/
Journal of Clinical Imaging Science
Literature Publishers working for the growth of the researchers, scholars and students by publishing their valuable research work and case studies.
Scope of Clinical & Medical Images Journal
International journal of medical case reports, hematology images, images in hematology, journals that accept case reports, case reports in hepatology, archives of clinical and medical case reports, journal of clinical case reports impact factor, clinical case reports journal impact factor, journal of otolaryngology head and neck surgery, journals accepting clinical images, journal of dental case reports, gastroenterology journal case report, ophthalmology case report journals, case reports in nephrology and dialysis, gi case report journals, clinical imaging journal impact factor, orthopedic surgery case reports, international journal of clinical case reports, journal of medical diagnostic methods, international journal of dental case reports, eye case reports, clinical case reports international impact factor, scholars journal of medical case reports, journal of invasive cardiology case report, dental case reports journal, journal of medical imaging and case reports impact factor, journal of oral health case reports, journal of clinical images and case reports impact factor, international journal of medical and dental case reports, journal of clinical images and case reports, journal of surgical technique and case report, journal of clinical and medical images impact factor, journal of case reports and medical images, journal of case reports and images in surgery, ophthalmology case studies, clinical journal of gastroenterology and hepatology, journal of cardiology and cardiovascular medicine, clinical images journal, clinical and medical case reports, international medical case reports journal, case report journal impact factor, clinical images, journal of cardiology cases, clinical case reports journal, surgery case reports, case reports in endocrinology, case reports in orthopedics, journal of clinical case reports, journal of cardiology case reports, journal of laryngology and otology, scholars journal of medical case reports impact factor, case reports ophthalmology, case reports in dentistry, journal of medical cases, cardiology case reports journal, case reports in orthopedic research, journal of clinical imaging science impact factor, gastroenterology case reports, international journal of clinical cardiology impact factor, ophthalmology case reports, impact factor journals of medical case reports, neuro ophthalmology case reports, case reports in hematology, international journal of medical case reports impact factor, clinical case report impact factor, case reports in otolaryngology, clinical case reports journals, endocrinology case reports.
The mission of Clinical Image Journal is to publish, in a timely manner, the very best Clinical and Medical Images from all over the world with special attention to the impact of medical imaging on patient care. The journal's publications cover all imaging modalities, health issues related to patients. The International Journal of biomedical imaging is valuable for medical image analysis journal resources for practicing in medical science journals and other clinicians with an interest in imaging journals. Papers are carefully peer-reviewed and selected by our experienced subject editors who are leading experts spanning the range of imaging sub-specialties.
Clinical and Medical Images is being published by Literature Publishers with the aim of publishing the Clinical Images and International journal of clinical & medical images that are related to all the areas of clinical science and Medicine. The purpose of this journal is to spread the knowledge of novel discoveries, journal of medical imaging and interventions in various fields of health science & medicine.
Clinical and Medical Images is a peer-reviewed International Journal that has got immense scholarly significance and responsible to do medical image analysis. This journal is being dedicated to clinical images from various areas of medicine. All the latest updates are being included in this journal.
Clinical Images and Case Reports Journal committed to publishing high-quality articles in the vast field of Clinical and Medical Imaging science with special attention to the impact of medical imaging on patient care. The journal aims to present imaging science and relevant clinical information in an understandable and useful format.
The objective of this health science journal is to serve the associated scientific community and the relevant readers with the latest scientific information and aid in further development and understanding of the subject in Image Journal/ Clinical Image Journal or Medical Image Journal.
Medical image analysis and International Journal of Clinical & Medical Images/ Journal of Medical Imaging in medical and clinical case report journal offer an open access platform to share their research and reviews journal outcome on drug delivery approaches, formulations, technologies, and systems that would deliver medicines in the body to safely achieve the desired therapeutic effect.
Manuscript Submission
Authors are requested to submit their manuscript by using Online Manuscript Submission Portal:
https://www.literaturepublishers.org/submit.html
(or) also invited to submit through the Journal E-mail Id: [email protected]
0 notes
Text
Orbital Ameloblastic Carcinoma – Unusual Presentation in A Non-Odontogenic Location

Abstract
Ameloblastic carcinoma has been described as an ameloblastoma in which there is histological evidence of carcinoma in a primary or recurrent ameloblastoma. The frequency of the lesion is estimated to be less than 1% of all ameloblastomas occurring in the mandible and maxilla.1 We present a case of a 30-year-old woman who presented with painless swelling of left upper face and recurrent upper respiratory tract infections. She was evaluated with CECT, MRI and PET-CT which showed 3.6 x 3.5 x 3.3 cm mass arising from the inferomedial wall of left orbit with sunburst periosteal reaction and cloudy osteoid matrix which was thought to be an osteosarcoma. She underwent a transorbital and trans nasal endoscopic wide local excision of the lesion which was then diagnosed as ameloblastic carcinoma on histopathology. Imaging features and pathological findings of the tumor along with novel treatment strategies and differential diagnosis are discussed in this case report.
Keywords: MRI; orbital tumor; ameloblastic carcinoma; osteosarcoma; CECT; PET
Abbreviations: 18F-FDG-PET: 18F-fluorodeoxyglucose–Positron Emission Tomography; CECT: Contrast Enhanced Computed Tomography; FLAIR: Fluid Attenuated Inversion Recovery; MRI: Magnetic Resonance Imaging; WHO: World Health Organization
Read More About This Article Click on Below Link:
https://lupinepublishers.com/otolaryngology-journal/fulltext/orbital-ameloblastic-carcinoma-unusual-presentation-in-a-non-odontogenic-location.ID.000260.php
Read More about Lupine Publishers Google Scholar Articles:
https://scholar.google.com/citations?view_op=view_citation&hl=en&user=dMOUw-wAAAAJ&cstart=100&pagesize=100&citation_for_view=dMOUw-wAAAAJ:v_xunPV0uK0C
#lupine publishers#lupine publishers group#scholarly journal of otolaryngology#journal of otolaryngology#sjo
0 notes