#Exocrined Gland
Text
Compound Multicellular Exocrine Glands

#medblr#studyblr#notes#my notes#anatomy and physiology#anatomy#physiology notes#physiology#anatomy notes#exocrine glands#exocrine glands notes#biology#biology notes#bio#bio notes#medblr notes#med notes#medical notes
2 notes
·
View notes
Text

Foie
Glande endocrine et exocrine digestive
26 x 16 x 10 cm
2.3 kg en moyenne (dont environ 0.8 kg de sang)
2 lobes séparés par le ligament falciforme

ligament falciforme : maintient le foie au diaphragme et à la paroi abdominale antérieure
ligament rond : reliquat fibreux de la veine ombilicale
ligament coronaire : ligne de réflexion du péritoine, permet de suspendre le foie au diaphragme
ligaments triangulaires : portions latérales du ligament coronaire
appendice fibreux : ligament associé au ligament triangulaire gauche dans la suspension du foie
vésicule biliaire : organe creux qui stocke la bile sécrétée par le foie
Bibliographie
Frank H Netter, Atlas d'anatomie humaine, 6e édition. Paris : Saunders Elsevier, 2014, 624p.
Casoli V, De Seze M, Midy D. Anatomie Appareil Digestif. Éditions Bergeret, 2014, 305p.
7 notes
·
View notes
Text
astro theory 2: organs/systems by ruler
everyone and their mother has their opinion on what body parts are ruled by which sign, including myself. maren altman described saturn in pisces as a time when one thing questioned would be bodily autonomy, so let's ring in this transit with a small anatomy lesson (if we have any activists here, i'd like to thank you in advance for the next 3 years, as they are going to be very important for you) on my opinions of what rules what.
the traditional western view (being general; not citing anyone specific in case of plagiarism accusations) was to 'slice' l'uomo vitruviano into 12 parts from top to bottom and label them like this:
aries: head/face/brain
taurus: neck/throat
gemini: hands, arms, shoulder area
cancer: chest, cervical spine area (of back), ribs
leo: heart, thoracic spine area
virgo: belly (under chest to navel/above hips), lumbar spine area
libra: navel until hip line
scorpio: genitals
sagittarius: thighs
capricorn: knees
aquarius: calves
pisces: feet
eastern astrology has a few interpretations but here's the one written by sanjay rath, based on traditional planets and organ systems:
sun: skeletal
moon: circulatory
mercury: nervous & integumentary
venus: reproductive
mars: muscular
jupiter: digestive
saturn: excretory

i disagree with both (eastern seems to fit my interpretation better though) as modern medicine has come a long way since then - while it may not be accurate for everything, as discoveries and advances will still and always will still be made, we can categorize some beliefs from the past as (generally) untrue.
i personally agree with putting signs as body part (if i say systems I'm talking about multiple body parts, rather than them working together) rulers and planets system rulers.
i'm starting with signs and then following with planets, as this seems like the more logical order. I can't list every body part, but it will be very detailed - comment/message and if i think it applies i will add it (cells/intracellular fluids do not have specific rulers).
aries/1st: skin, hair, nails, epithelial tissues
taurus/2nd: heart, veins/arteries
gemini/3rd: cerebellum, frontal lobe, occipital lobe, cns (including eyes)
cancer/4th: interstitial fluids (lymph, pus, spit, breast milk, etc.), eggs/sperm
leo/5th: blood (connective tissue)/intravascular fluid
virgo/6th: stomach hydrochloric acid, temporal lobe, parietal lobe, pns, ens
libra/7th: remaining connective (including osseous)
scorpio/8th: mesenchyme (connective) tissue, nephrons, cartilage, extracellular matrix
sagittarius/9th: enzymes, steroid/adrenal hormones*
capricorn/10th: joints, muscle tissues, protein (peptide/amine/glycoprotein) hormones
aquarius/11th: glands, lungs/airway, uterus, testes
pisces/12th: adipose tissues*
now for the slightly easier parts, planets in the modern order (why didn't i include rising? look in your first house - above in sign/degrees/house list with aries).
sun: fluid-based (lymphatic) immune**
moon: reproductive
mercury: nervous, digestive/excretory
venus: circulatory
mars: integumentary (exocrine)
jupiter: lipid structures/steroid-based endocrine*
saturn: musculoskeletal, protein-based endocrine*
uranus: respiratory
neptune: response-based immune* **
pluto: non-digestive excretory
*why are the jupiter signs not concrete? (aka i am preparied for the slander). jupiter and neptune are the 'expansive' and 'shadowy' planets (or as i like to say the 'overt/covert' planets) which means that unlike the other planets, there is not an easily decipherable concrete form (actually for the sake of technicality, there is a concrete form but its so large and made of so many parts that it is hard to see - think air molecules). jupiter being expansive is not the reason why it represents fats - jupiter's supportive nature (whether wanted or not) makes it the planet for fats. additionally, sagittarius which traditionally responds to gets tasks done quickly (whether correctly or not) represents every enzyme and steroid response. also saturn -> time -> growth.
**immune system is divided into: first the 'drainage' which is what the lymph picks up before being drained into lymph nodes, filtered and sent back to the bloodstream. 'but the sun is the outwards expression of personality' - hold on - the sun needs to 'take stock' of the other plants before expressing their desires in the 'sunny (lol) fashion' and it can only do this by passing through everyone else and collecting the inputs. the lymphatic network goes literally everywhere in the body and drains any 'extras' and doesn't make it waste - it eventually sends it back into the bloodstream. second the 'responses' - which is made of other parts of other systems working together. in the illusory nature of neptune (as described above) it makes sense to have the system that is not 'seen' but still works to defend from behind the scenes.

this is my theory but feel free to comment your questions and opinions if you have any - i'm interested in people's responses (and potential jupiter signs slander) - as I said, any input that I think applies may be added.
anyways,

~ Lala
43 notes
·
View notes
Note
So like- I've been wondering this after I found out about Runna... How did she and Donnie meet?
Also, when did they get married and decide to have their lil baby?I JUST WANNA KNOW MORE ABOUT THIS CUTE LIL FAM😭😭

AHHHHHHHHHHHHHHHHH THANK YOU THANK YOUU OMGGG‼️‼️‼️‼️BRO ALSO SORRY FOR NOT RESPONDING I SAVED IT AS A DRAFT AND FORGOT ABOUT IT 🙇🙇🙇VERY SORRY
okay so rn runa is going through a HUGE character redesign and species change because……….. impulsive behavior and also it was getting difficult to draw her, BUT‼️, i will answer those questions …
IINNNNN AN UPCOMING FIC— I’ve been planning on how they meet for a while but I can give you more information about Runa, like a wiki article or something 💀, I hope that helps a lil cause i cannot start answering questions or else I’ll spill the entire story line💔 (im sorry I’m so mean😔)
ANYWHO
Runa O’Crest comes from a powerful Yokai family that married into wealth, making her family name lower then royalty but still higher than a Duke/Duchess. She prides herself on her name and wealth, because that’s the core value that her mother, Princess Toriki, and her father, Prince Synson.
-They aren’t Queens and Kings yet, because Synson’s father hasn’t given him the throne yet; So Toriki isn’t a real princess (a fact she refuses to address), making her a princess consort.
Runa’s parents are overly protective of their youngest daughter and only heir after their eldest daughter, “Tawny Owl,” abdicated. This causes them to almost pressure Runa into being a “perfect” princess, she feels like her life revolves around trying to impress her parents. Still, Runa sees that her parents favor Tawny over her, which causes her to feel like she’s not good enough.
(I should say that I barely have a timeline scratched together so this is really funky💀 this, currently, isn’t my biggest priority atm, so I haven’t really put a lot of time into this💔)
After her parents decided that she’s finally ready to go to the outside world, they let her go to April O’Neil’s high school/college(???), and that’s where she meets the Turtles. The Ninjas were investigating a strange uprising of mystic mumbo-jumbo on school property and April called the experts.
Donnie was quick to jump on this opportunity as he investigated the mysterious happenings and quickly found the cause; Yokai taking the forms of humans and attending school!
But before the Mad Dogs came to the conclusion that there is more then one Yokai going to this school, Donnie tracks a trail of magic to the punk-rock girl, Tawny. And subsequently her sister, Runa.
April and Tawny have met before, just under harsh circumstances and thus ended up not really approving of each other.
Donnie followed the trail of mystical residue with his magic-seeking googles; and ends up at the feet of Tawny O’Crest, the “rebel with a plan.”
After a brief introduction, Runa stomps over to her sister and demands to know what April is doing talking to her sister.
“Hey, Runa,” April called, “Why don’t you make like a tree and leave?” April hissed, getting closer to the mean girl’s face trying to intimate her.
“Why don’t you make like an overactive sebaceous oil gland cell, and get out of my face.” Runa hissed back.
“Did you just… reference human biology down to its microscopic exocrine glands?” Donnie said, scooting April out of the way and behind him, “To insult me?” He asked, angry, but mostly confused fascination.
“Yeah, what about it? You’re just jealous because I won first place in the Science fair!” Runa pouted back.
At this point Donatello was stunned. This-This total wet towel had won over his brilliant and ground breaking tech?! He would not stand for this!
“Excuse me,” he said softly, “WHAT?!” He shouted so loudly that Jersey could hear him.
“That’s right, Grinchie,” Runa said, eyeing him up and down, “I won.”
“oKAY THAT’S IT!!” Donnie shouted, pulling a dramatic anime pose while pointing to the girl, “YOU. ME. RIVALS FROM NOW ON! Any objections?”
“Well, I think-.”
“GOOD!” Don shouted, “We are now rivals!!”
And with that, the Mad Dogs left and the rest is history. As you can see, Runa was very prissy and quite obnoxious. But after meeting the turtles and challenging them, competing with them, and ever befriending them, she starts to let her inner self shine.
She becomes more helpful and affectionate towards the Mad Dogs, and realizes how messed up her relationship with her parents is. And the scheme that was running along just beneath the surface.
You see, Runa’s parents had invested a lot of money into the Battle Nexes, only to have their only source of income and entertainment slaughter by a creature they told her to get rid of.
“What a fitting end.” Toriki hissed, “She did always like to keep pets.”
So, Toriki was like, “oh shoot😨 we need more money🧐 how will this happen���� I know!🤩 the Battle Nexes 2: electric boogaloo 🤩🤩”
And Toriki sends her beloved children into the human world to get the best fighters they know of (this is a post-cannon fic btw so after the movie), and force them to fight in the Battle until they die or find a better fighter.
They have their sights set on Leo.
OKAY THIS IS RUNA’S NEW DESIGN AND I UH- IKD MAN TELL ME WHAT YOU THINK💖

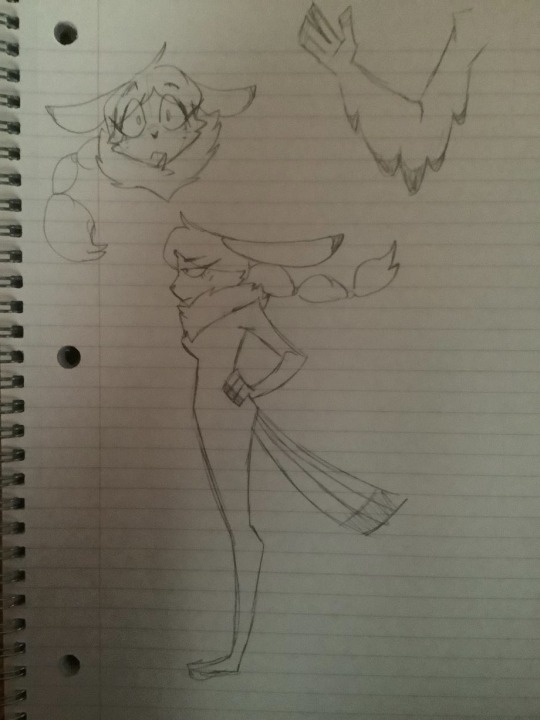

Owl and Rabbit hybrid because I’m indecisive af
NOW, ON TO ALEXANDER
tw/////dark subjects like sh and ed 🦋
SO; getting into Alexander’s trauma here, he’s very insecure about his plastron because it resembles Leo’s too much, making him feel kinda guilty for just,,,looking like donnie’s twin the slightest bit. He’s tried to smooth it out with filers (the nail things to sand your nails idk) and even sand paper, it’s kinda like self harm because it hurt really bad. And he was too scared to go to his parents so he went to April instead who told him that that wasn’t okay and his parents loved him no matter what. There’s still marks and scrapes but it’s mostly healed. (Originally drawing Alex with Leo’s plastron was a slight mistake but over time it kinda stuck and now you get lore)
he was also getting bullied at the Hidden City school for being half mutant and half yokai, something he still refuses to tell people until he has confirmation that they will accept him in any way, but as he grew up it only got worse. They wrote it on his lockers and backpacks, they even drew it on his face when he fell asleep in class once! He never told donnie, (but his father figured it out pretty quick), because he knew donnie would obliterate the school if he found out. So he told runa who,,,,handled it a-prop-et-ly. After that he trusts people more easily and gets betrayed yadah, yadah, yadah…
And Alex has always felt he was different from everyone else, mostly because of his strong mystic energy, but I digress.
He felt extremely thin with his plastron and resorted to eating a lot, so much so that he would get sick. He would just eat random shiz too, but that’s more of a inherited trait because he used to just eat random stuff as a baby.
But overall, he’s a happy kid, a little naïve, but mostly sweet.
NOW ON TO DONNIE
the only notes that I have on him are these ones ;
because donnie doesn’t like physical touch that much in his teen years and never really allowed himself to be all soft and affectionate towards his family and friends, when he’s an adult (future au with alex) he’s very cuddly and venerable. (not to his family but only to Runa and maybe alex if it calls for it)
and that’s why future donnie doesn’t really wear his battle shell around the house
And that’s about it for Donnie since his personality doesn’t change that much.👁👁
Anyway, here’s some fun trivia facts because I need some way to end this ;
-Runa and Donnie are very similar yet different at the same time. Runa is mean because everyone told her she cared too much so she stopped caring completely. Donnie was just born like that and he’s just naturally defensive as a safety precaution.
-They argue a lot over who’s right, sometimes they seem to argue for fun. But they will never admit if one of them is wrong until they’re proven right. Then neither of them will bring it up ever again. Sometimes Donnie will let Runa prove she’s right just to see her smile and laugh.
-When they game, don will let her win (rarely) just to see Runa’s dorky victory dance. Then it just turns into a dance party for everyone.
-When in her Yokai form, she accidentally hits people with her tail feathers.
-Runa listens to Shake Your Tail Feathers from Chicken Little unironically.
-Donnie makes dirty science jokes when he’s hormonal🫣. I.E. “Much like warm air molecules, I never stay on the bottom.”
-Donnie learns what every single coo, chirp, squak and screech means in owl language. Runa and Donnie usually talk to each other like that so Donnie doesn’t have to admit how mushy he can get around his brothers.
-They say a lot of things at the same time. Runa thinks a lot like donnie so she knows what a lot of complex abbreviations for blueprints are.
(I should mention the fun facts take place after they had Alex)
SO, that is all I have about this family!! Sorry if it’s long it’s just I have SO much to talk about with them, and don’t even get me started on NEXT GEN au (it’s future au with the kraang and Alex and his friends and all that stuff). I’m just SOOOOOOOOOOOOOOOOOOOOO SO, SO very happy you asked!!
Planning to write more in the future, so stay tuned ~~
#rottmnt#rise donnie#rottmnt alexander#rottmnt runa#rottmnt oc#rottmnt Runa O’Crest#rottmnt Donatello Hamato#rottmnt Alexander O’Crest Hamato#ask#thanks for the ask cherry!!^^#really enjoyed infodumping about thisssssss#makes me so SO happy
11 notes
·
View notes
Note
GAH i love the board!! i really needed this right now and i feel so relaxed looking at it :'}} thank you so much! also im glad to see youre back, and i 🖤 you too!! /p
and my day has gone okay, but its great now that ive seen that stimboard :D ive just slept most of the day lol, wnd i dont have a dog to send pics of but heres a random fact off the top of my head: did you know marine iguanas consume a lot of salt since they live near the sea, so to get rid of all the excess they filter the salt out and blow it out their nose like a sneeze? theyre able to do this because of the exocrine glands in their nostrils! another fact, did you know vultures (hehe) dont migrate? or that velociraptors couldnt turn their wrists due to their anatomy? okay sorry im done, this ask is long lol tell me how you are and i hope this finds you well!! thank you again for the board <33
-vulture𓅐
hihi vulture! good to hear from you <3
i’m so happy you liked the board! i’m glad i didn’t get rusty after me little break heheh
thank you for the facts! they are indeed fun! i had no idea that vultures don’t migrate, is there a reason for that??
i’m doing ok, thank you for asking! still feeling a bit rough, but i think i’m feeling a bit better! i hope so anyway :)
<3 u lots vulture! /p take care :)
2 notes
·
View notes
Text
“Sjogren Syndrome Antigen”, Victor McKusick, Mendelian Inheritance in Man, 1966.
Here I present: “Sjogren Syndrome Antigen”, Victor McKusick, Mendelian Inheritance in Man’, 1966.
INTRODUCTION.
Sjögren syndrome is an autoimmune disease that primarily affects the body’s exocrine glands, particularly the lacrimal and salivary glands. Common symptoms include: dry mouth, dry eyes and often seriously affects other organ systems, such as the lungs, kidneys, and nervous…
0 notes
Text
What is Sjogren's Syndrome? What are the Natural Remedies for its treatment?

WHAT IS SJOGREN’S SYNDROME ?
Sjogren's syndrome is a disease associated with the immune system. It is an autoimmune condition, which means that your immune system mistakenly attacks other parts of your body. This happens when white blood cells go to the salivary glands, tear glands and other exocrine tissues and affect them, which leads to a decrease in the production of tears and saliva in our body.
Due to this disease, there is dryness in the mouth, eyes, skin, nose, vagina or upper respiratory tract. Not only this, other parts of the body like joints, lungs, kidneys etc. are also damaged by this.
The problem of Sjogren's syndrome is more commonly seen in women and this disease starts only after the age of 40 years. The disease is sometimes associated with other diseases such as arthritis and lupus.
CAUSES OF SJOGREN’S SYNDROME :
The causes of Sjogren's syndrome are not known exactly. According to studies, viral or bacterial infection can be the cause of this disease.
However, its main causes are genetic and environmental. The nervous system, endocrine or hormone-producing systems may also be thought to cause Sjogren's syndrome.
An environmental factor can also alter the immune system and cause immune problems later, such as infection with hepatitis C or Epstein-Barr virus.
Women have more of this problem than men. It is believed that this is due to the hormones of women.
Menopause can also be a reason for this. Some studies suggest that estrogen protects against Sjogren's and that falling levels of the hormone may alter immune function and make the condition worse.
There is no cure for Sjogren's syndrome. But, by treating the dryness of the affected organs, the problems caused by this disease can be relieved.
RISK FACTORS :
Age - The risk of developing Sjogren's syndrome is higher after the age of 40.
Gender - Women are more likely to have this problem than men.
Rheumatic disease - People who have rheumatic disease like arthritis. They also have a higher risk of getting this disease.
Family History - It is also believed that if someone in your family has this disease, then you are more likely to get this disease.
SYMPTOMS OF SJOGREN’S SYNDROME
The symptoms of Sjogren's syndrome are:
Dry eyes - There may be burning, itching in the eyes.
Dry mouth - It may feel like you have cotton in your mouth. Along with this, there is a problem in swallowing and even speaking.
Joint pain, swelling and stiffness
Swollen salivary glands – especially behind the jaw and in front of the ears
Skin rashes and dry skin
Vaginal dryness
Persistent dry cough
Chronic Fatigue Syndrome
Continue Reading
PREVENTION OF SJOGREN'S SYNDROME SYMPTOMS :
Drink more fluids, especially water.
Chew sugarless gum or use hard candies to moisten your mouth.
Use artificial tears and ointment regularly to keep your eyes moist
Use a saline spray for your nose.
Install a humidifier to help reduce dryness of the eyes, nose, mouth, and skin.
Don't smoke and don't drink alcohol.
AYURVEDIC MANAGEMENT OF SJOGREN’S SYNDROME
In Ayurveda symptoms of an eye disease known as 'Shushka Akshipaka' are similar to that of Sjogren’s syndrome. It can be broken into two words, 'Shushka' means 'Dry', and 'Paka' means 'inflammation' of eyes. It comes under the Sarvagata Netra Roga which is a Vata/Vata-Pitta dominant vyadhi. It also leads to derangement of metabolism and tissues of the body.
PANCHKARMA THERAPIES USEFUL IN SJOGREN’S SYNDROME :
Deepan pachana - Deepana-Pachana should be performed before any treatment to acquire niramavastha of doshas. It helps to eliminate Ama from the abdomen.
Virechan - Virechan is the process of eliminating vitiated doshas (mostly pitta) from the lower gastrointestinal tract via the anal pathway. This procedure provides clarity to mind, strengthens sense organs, stability to tissues, etc.
Basti - It is the process of administering medications in suspension form through the rectum using basti yantra. By virtue of the drug's virya, it draws the doshas or mala from all over the body, from the foot to the head.
Seka - In this application, the medication is poured continuously from four inches above the closed eye (on the eyelids) for a specified duration determined by the dosha.
Aschyotan - It is a process in which medicinal drops are delivered into the open eye from a height of two inches. It is the first-line therapy for all eye diseases.
Akshi tarpana - It is a treatment in which the eye is filled with medicinal oil or ghee for a set amount of time. It nourishes the eyes and treats the Vata-Pitta Vikara.
Nasya - It is a medicinal method in which medication is infused in the nostrils in the form of drops. This medication is quite successful in treating a variety of Urdhavjatrugata-related disorders.
Anjana - The anjana shalaka (rod) is used to apply medication to the inside surface of the lid margin from Kaneenaka sandhi (inner canthus of eye) to Apanga sandhi (outer canthus of eye).
CAC TREATMENT OF SJOGREN’S SYNDROME
SJOGREN’S SYNDROME CARE KIT
Chandigarh Ayurved Centre made the specialized kit that is very beneficial as it contains pure herbs that are free from side effects and cure this condition of its root cause. The kit has a total of 6 products – Ras raj ras, Kapha detox powder, Ekangveer rasa, Trikatu syrup, Pain-o-kill oil, and Vaat nashik vati.
ALL PRODUCTS DESCRIPTION IN DETAIL:
Cough go tablets:
CAC Cough Go Tablet is a herbo-mineral tablet of size 650 MG and is a purely ayurvedic formulation. CAC Cough Go tablets help in balancing the kapha dosha. It shows effective results in Chronic Cough, common cold, and all respiratory diseases along with Seasonal Allergy, Bronchitis, Bronchial Asthma. It helps to treat root cause and also increase immunity of the person. It’s not only symptomatic
treatment but heals your body naturally. It contains pure herbal ingredients like Sonth (Zingiber officinale), Mulethi (Glycyrrhiza glabra), Pippali (Piper longum), Kali mirch (Piper nigrum), Laxmi vilas rasa, Abhrak bhasam, Tankan bhasam etc. These ingredients contain natural Kapha doshahar properties and help in curing all respiratory diseases and symptoms like dry eyes and mouth.
DOSAGE: Take one tablet twice a day with normal water.
Nerve Up:
It is pure herbo-mineral formulation which helps to balance the vata dosha. It act as nervine stimulator and also reduces Kapha doshas. It mainly acts on central nervous system. It contains natural ingredients like Shudha kuchala, Shudha shilajeet, Praval pishti, Shankh bhasma etc. These contains natural Vatahar properties and helps in curing vata diseases. It speeds up physical and mental processes. It helps in painful joints, stiffness , inflammation, swelling and general weakness.
Dosage – Take 1 tablet twice daily with normal water after meal.
Trikatu syrup:
Trikatu syrup is pure ayurvedic formulation comprises of mainly three herbs such as Pippali (Piper longum), Shunthi (Zingiber officinale), &; Marich (Piper nigrum). the main function of trikatu syrup is that it removes excess of Kapha doshas and supports the respiratory system, help to reduce body weight and hence detoxifies the body. it has anti-inflammatory , analgesic and antioxidant properties. It boosts metabolism and helps to reduce inflammation of the body. Helps to fight against infections, and improve the body’s energy levels It is free from chemicals, additives, colors and fillers.
Dosage: 2 tsp twice daily before a meal.
Detox Premium Powder
The sachet includes all the natural ingredients which help to detoxify the body and maintain the natural luster and glow in the skin. This herbal sachet contain various ingredients mentioned below:
Parwal Pishti – It is an Ayurvedic medication based on Coral Calcium. Parwal pishti acts as an anti-inflammatory. It prevents from sunburn and pricking sensation in the skin after burning, etc.
Shukta Pishti – It is prepared from the pearl oyster shell. Shukta Pishti is used in acne and skin allergy. It mainly helps to remove the patches.
Giloy Satva – Giloy satva is ayurvedic preparation that reduces the signs of aging, dark spots, pimples, etc.
Tal Sindoor –It purifies the blood which in turns treats the skin disorders. Tal Sindoor shows an anti – allergic properties and also used in skin irritation, itching, and improves the health of the skin.
Gandhak Rasayana– This is a classical preparation used in itching, burning sensation, urticaria, eczema, scabies, pimples, etc.
Kamdudha Rasa – Kamdudha Ras is an herbal-mineral ayurvedic classical medicine having SHEETA VIRYA properties. It is used in burning sensation, excessive sweating, hot flashes, heat sensation, etc.
Sudh Yog Powder -It helps to remove patches, acne. Sudh Yog Powder helps in nourishing and moisturizing the skin. This powder promotes detoxification and rejuvenation. It helps in engender vibrant, which makes the skin healthy.
Jahar Mohra Pishti – Jahar mohra pishti is an Ayurvedic mineral based formulation. In Ayurveda, it mainly works on pitta dosha. The main work of Jahar Mohra Pishti is to detoxify the body and maintain the luster on the face.
Recommended Dosage –Take 1 Sachet twice a day with normal water.
Pain-o-kill syrup:
This is a herbal oil that helps in reducing pain, inflammation, stiffness, & swelling, tenderness of the joints. The oil is composed of Shunthi (Zingiber officinale), Erand (Ricinus communis), Kapoor (Camphora officinalis), Til taila (Sesame indicum), etc. The ingredients have anti-inflammatory, analgesic properties that are very effective to ease the signs and symptoms.
Method of application – Apply the oil over the affected area once or twice daily.
Rasayan Vati:
It is a pure herbal formulation which is free from chemicals, additives, colors, and fillers. It consist of Ashwagandha, Shilajeet, Amla, Kesar, Musli, Shatavari, Brahmi, Abhrak Bhasam, Swarn Makshik Bhasam, Yashad Bhasam, Mukta pisti, Praval pisti, Jaiphal, Vang Bhasam, Dalchini, Javitri, Gokhru, Kaunch Beej, Shilajeet, Saunth, Mirch, Pippali, Manjistha, Anant Mool, etc. It has anti-inflammatory, anti-oxidant, and immunomodulator properties. It helps to balance all three doshas and Brahmi present in it helps to increase brain functioning. Rasayan vati acts as a health tonic, memory tonic, and it is effective in general debility and nerve weakness.
Dosage: Take 1 tablet twice daily with normal water after meal.
Anu Tail:
Anu tail is herbo mineral and purely ayurvedic formulation. It is used for ayurvedic treatment procedure known as Nasya treatment in most of the disease involving Ear, Nose and Throat involving pain. It has Tridosha balancing properties but mainly help to balance your Kapha dosha that cause Headache, running Nose or Sinusitis. It strengthens Ear, Eyes, Nose, Tongue and Throat.
Dosage: Put 2 drops twice daily in nostril.
Kanth Sudharak Vati:
Kantha Sudharak Vati is a pure herbal formulation of CAC which provides a soothing effect and acts as an expectorant herb that gives relief in throat problems. It reduces the stickiness due to Kapha doshas in the oral cavity and removes bad breath. It is herbal combination without any added chemical, preservatives and fillers.Dosage: Take 1 tablet twice daily with normal water after meal.
0 notes
Text
Pancreatic Cancer Treatment In Delhi
Introduction
Pancreas is a vital organ and performs both the exocrine and endocrine functions. Pancreas may have several diseases. There are various causes of pancreatic diseases. Doctor advises to undergo several diagnostic tests to determine the type, cause, and extent of the disease.
Pancreatic Cancer Treatment In Delhi

What Is Pancreas?
Pancreas is situated in the abdominal cavity and helps in food metabolism. It is a gland and performs both exocrine and endocrine functions. Due to its exocrine function, it helps in digestion, while its endocrine ability helps in regulating the optimum blood sugar level. The length of the pancreas is about six to eight inches and the shape is like an extended pear. Several organs such as liver, small intestine, and spleen surrounds the pancreas.
Pancreas secretes chymotrypsin and trypsin for the digestion of proteins, amylase for the digestion of carbohydrates, and lipase for the digestion of fats. The pancreatic duct carries the enzymes from the pancreas to the stomach when the food enters the digestive tract. A part of the pancreas, islets of Langerhans, synthesizes the hormones and secretes them directly into the blood stream. The main hormones secreted by the pancreas are insulin and glucagon.
What Are The Diseases Of Pancreas?
Different diseases may affect the pancreas. The symptoms of the diseases depend upon the type and severity. Some of the diseases of pancreas are:
Acute Pancreatitis : The acute pancreatitis is the condition in which there is a sudden inflammation in the pancreas. The patient with this condition experiences severe abdominal pain. Patient may also have nausea, vomiting, and diarrhea. There are several causes of acute pancreatitis. The treatment depends upon the underlying causes of the disease. Most patients with acute pancreatitis completely recover.
Chronic Pancreatitis : Chronic pancreatitis is a long-term disease and may result in damage to the pancreas. The condition most commonly occur in people with the age between 30 years to 40 years. Men are at increased risk for developing this condition. The symptoms, along with the disease, progresses from mild to severe. In case of complete pancreatic damage, the patient is unable to maintain optimum blood sugar level and may suffer from diabetes mellitus.
Hereditary Pancreatitis : Pancreatitis may also occur due to hereditary alterations in the pancreas and intestine. The patient may have pancreatitis early in the life and then progress tochronic pancreatitis. Cystic fibrosis, a hereditary disease, also cause pancreatitis. The condition progresses and result in permanent damage to the pancreas. The treatment for hereditary pancreatitis is almost like chronic pancreatitis.
Pancreatic Cancer : Malignant cells in the pancreatic tissues result in pancreatic cancer. Patients do not experience any symptoms of pancreatic cancer in the initial stage. However, as the diseases progresses, symptoms began to appear. Painless jaundice is usually the first sign of pancreatic cancer.
What Are The Symptoms Of Pancreatic Diseases?
Most patients do not experience any symptoms during the initial stage of the pancreatic disease, except in acute pancreatitis. Some of the general symptoms in pancreatic diseases are:
Fever
Fatigue and weakness
Diarrhea, nausea and vomiting
Pain in the abdomen
Weight loss
Upset stomach
Malnutrition
Diabetes
Bloating
What Are The Causes Of Pancratic Diseases?
Some of the causes of pancreatic disorder are:
Underlying medical conditions : Several underlying medical conditions result in pancreatic diseases. The patients with infection, gallstones, high level of triglycerides, and metabolic disorders are at increased risk of developing pancreatic diseases.
Medications: There are several drugs that causes pancreatic diseases as their side effects. Some of them are estrogen, corticosteroids, antibiotics, diuretics, and medicines for autoimmune diseases.
Trauma : A trauma to the pancreas causes pancreatic injury and may cause pancreatic dysfunction. Trauma may occur during vehicle collision or when hit by a blunt object.
Surgery : In some cases, the post-operative complications may result in hemorrhagic pancreatitis.
Hereditary disease: Certain hereditary diseases, such as cystic fibrosis, may result in pancreatic diseases.
Prolonged consumption of alcohol: People who consume excessive alcohol for a prolong period are at high risk for developing pancreatic disease.
Family history : People with the family history of pancreatic disease are more vulnerable to developing the pancreatic disease.
How The Doctor Diagnoses Pancreatic Diseases?
There are several methods to diagnose the pancreatic disease. Some of the methods are:
Physical evaluation : The doctor perform comprehensive examination and seek information about your symptoms.
Blood tests: The doctor may advise you to undergo blood test. Through the blood test, your doctor may evaluate the functional status of the pancreas. Blood test includes determining the level of amylase and lipase.
Imaging techniques: The doctor may also advise you to undergo imaging techniques to determine the presence and severity of the pancreatic disease. The imaging techniques include MRI, Ultrasound, and CT scan.
Stool tests : Stool tests may also be performed to analyze the level of fat present in the stools. It will provide information about the nutrient absorption status.
What Are The Options For Treating Pancreatic Disease In Delhi?
There are several options for the treatment of pancreatic diseases in Delhi. The type of treatment depends upon the pancreatic disease and its severity. Some of the treatment for pancreatic diseases are:
Medications: The medications may help to manage the underlying causes of pancreatitis. For example, if the pancreatitis is due to infection, the doctor may prescribe antibiotics. The doctor may also prescribe pain relievers to manage pain.
Fasting: The doctor may also advise you to stop eating for one to two days to allow the pancreas to recover. Once the inflammation is stable, the doctor may allow you to drink liquid. After some time, you may return to your normal diet.
Surgery: The doctor may also recommend surgery in case the medications did not provide any relief. The surgery depends upon the cause of pancreatic diseases. You should consult with the best GI surgeon in Delhi for surgery for your pancreatic disease.
What Is The Cost Of Pancreatic Disease Treatment In Delhi?
The cost of pancreatic disease treatment in Delhi depends upon several factors. It depends upon the type of hospital, experience of the doctor, type of treatment (whether medicines or surgery) and severity of the disease (as more severe disease may require longer hospital stay or longer treatment).
From Where I Can Get More Information About The Pancreatic Disease And Treatment?
For more information about the pancreatic disease and treatment options, you may fill the form and write your symptoms in more detail.
To schedule an appointment With Dr. Neeraj Goel for Cancer Surgeon in Delhi, please contact:
Name: Dr. Neeraj Goel (Cancer Surgeon in Delhi)
Address: D-1, Hakikat Rai Rd, Block D, Adarsh Nagar, Delhi, 110033
Phone: +91–9667365169, +91–9599294453
Website: www.gastrodelhi.com
1 note
·
View note
Text
16th May 2024
CC: A&P - T, Epithelial Tissue Terminology
Epithelial Tissue - The kind of tissue that forms coverings and linings in the body, and also forms glands that secrete hormones.
Connective Tissue - The kind of tissue deep to all epithelial membranes, and that provides support and a blood supply to those membranes.
Cell Shape & The Number of Layers of Cells - We classify epithelial tissues based on these two characteristics.
Squamous - Short, wide epithelial cells, in which even the nucleus appears flattemed.
Squamous - The shape of epithelial cells good for forming thin permeable membranes or for making multi-layered abrasion resistant surfaces where each cell is inexpensive to replace.
Columnar - Tall, narrow epithelial cells, sometimes with a vertically stretched nucleus.
Columnar - The shape of epithelial cells found in the stomach and intestinal linings, where they must secrete mucus and form an active and thick membrane.
Cuboidal - Epithelial cells that are aboust as tall as they are wide with a circular nucleus.
Cuboidal - The shape of epithelial cells found in sweat glands and kidney tubules, where materials are being secreted or actively transported across a membrane, respectively.
Stratified - The type of epithelial tissue made up of two or more layers of cells.
Simple - The type of epithelial tissue made up of a single layer of cells - where every cell reaches from the tissue's apical surface to its basal surface.
Pseudostratified - The type of epithelial tissue where some cells reach from the apical or basal surface in a single layer but other cells are stratified or multilayered.
Simple Squamous - The name for a single layer of flattened cells in an epithelial membrane, like the lining of the lungs
Stratified Cuboidal - The name for a tissue with multiple layers of square-like cells in an epithelial membrane, like the linings of ducts to our salivary glands.
Selectively Permeable - Many epithelial membranes, because they allow some level of absorption, filtration or excretion of specific types of molecules, are described as this.
Apical - The exposed surface of an epithelial membrane that is not attached to the connective tissue.
Polar - A word that describes something, like epithelial tissue, the Earth and water molecules, as having two distinct sides or ends.
Basal - The side of an epithelial membrane that is attached to the underlying connective tissue and basement membrane, opposite the exposed surface.
Exocrine Glands - The type of glands that secrete chemicals destined for the outside of the body, or for the inside of your digestive and respiratory tubes that connect to the outside of the body.
Endocrine Glands - The type of glands, made of epithelial tissue, that secrete chemicals into the bloodstream.
All epithelial tissues are avascular, meaning that those tissue... don't have their own blood vessels.
When naming epithelial tissues, the first word describes... number of cell layers.
When naming epithelial tissues, the second word describes... shape of the cells.
0 notes
Note
Castoreum /kæsˈtɔːriəm/ is a yellowish exudate from the castor sacs of mature beavers. Beavers use castoreum in combination with urine to scent mark their territory. Both beaver sexes have a pair of castor sacs and a pair of anal glands, located in two cavities under the skin between the pelvis and the base of the tail. The castor sacs are not true glands (endocrine or exocrine) on a cellular level. Hence, references to these structures as preputial glands, castor glands, or scent glands are misnomers. It is used as a tincture in some perfumes and, rarely, as a food additive.
Sorry, Lovebug heard "sac," "sexes," and "anal" and got so horny they left front. So.
1 note
·
View note
Text

Sparks of Life Electrical Activity in Glands?
introduction
Have you ever wondered about the mysterious workings of your body? We often hear about organs like the heart, lungs, and brain, but there's a whole other set of important players called glands that work behind the scenes to keep everything running smoothly. In this article, we'll explore the fascinating world of glands, what they are, how they function, and their crucial role in maintaining our health and well-being.
What are Glands?
Let's start with the basics: what exactly are glands? In simple terms, glands are specialized organs in our bodies that produce and release substances necessary for various bodily functions. These substances, known as secretions, Glands electrical can include hormones, enzymes, oils, sweat, and saliva, among others. Glands are found throughout the body, from the head to the toes, and they come in different shapes and sizes.
Types of Glands
Glands are broadly classified into two main categories: exocrine glands and endocrine glands.
Exocrine Glands: These glands secrete their substances directly into ducts, which then carry the secretions to specific locations within the body or to the body's surface. Examples of exocrine glands include sweat glands, salivary glands, and oil glands (sebaceous glands).
Endocrine Glands: Unlike exocrine glands, endocrine glands release their secretions, such as hormones, directly into the bloodstream. These hormones then travel throughout the body, affecting various organs and tissues to regulate processes like metabolism, growth, and reproduction. Major endocrine glands include the pituitary gland, thyroid gland, adrenal glands, and pancreas.
How Glands Work
Now that we know the types of glands, let's delve into how they work, particularly focusing on the electrical aspect, as per the remember keyword.
Glands function through a complex interplay of chemical and electrical signals within the body. While many glandular secretions are primarily regulated by chemical signals, such as hormones, the process itself often involves electrical impulses.
In the case of endocrine glands, for instance, the secretion of hormones is triggered by electrical signals originating from the nervous system. These signals prompt the gland to release specific hormones into the bloodstream in response to various stimuli, such as stress, changes in the environment, or the body's internal needs.
Similarly, exocrine glands may also be influenced by electrical signals, particularly in processes involving muscle contractions or nerve stimulation. glands electrical For example, when you eat food, your salivary glands receive electrical signals from nerves in your mouth, prompting them to release saliva to aid in digestion.
Importance of Glands
Glands play a vital role in maintaining homeostasis, which is the body's ability to regulate its internal environment despite external changes. Whether it's regulating body temperature through sweat glands, Glands electrical aiding in digestion through the secretion of digestive enzymes, or controlling metabolism through hormone release, glands are indispensable for overall health and well-being.
Common Glandular Disorders
When glands malfunction or become imbalanced, it can lead to various health problems. Some common glandular disorders include:
Hypothyroidism: A condition where the thyroid gland doesn't produce enough thyroid hormone, resulting in symptoms like fatigue, weight gain, and cold intolerance.
Diabetes: A disorder characterized by high blood sugar levels due to insufficient insulin production (Type 1) or the body's inability to use insulin effectively (Type 2).
Hyperhidrosis: Excessive sweating beyond what is necessary to regulate body temperature, often due to overactive sweat glands.
Cushing's Syndrome: Caused by prolonged exposure to high levels of cortisol, a hormone produced by the adrenal glands, leading to symptoms such as weight gain, high blood pressure, and fatigue.
Conclusion
In conclusion, glands are remarkable organs that play a crucial role in maintaining the body's overall function and balance. glands electrical From regulating metabolism and growth to facilitating digestion and temperature regulation, glands are involved in almost every aspect of our health. Understanding how glands work, including their electrical aspects, can help us appreciate the intricate mechanisms that keep our bodies functioning optimally. So, the next time you marvel at the wonders of the human body, remember the unsung heroes working tirelessly behind the scenes – the glands.
0 notes
Text
If your face tends to resemble a grease-slicked pan by midday, you’re not alone. Excessively oily skin afflicts millions, causing embarrassing shine, large pores, acne breakouts and constant need to blot. But what causes faces to overproduce sebum, t...
#Mirari #MirariDoctor #MirariColdPlasma #ColdPlasma
0 notes
Text

Pancréas
Glande endocrine et exocrine digestive qui s'abouche dans le duodénum. Divisée en plusieurs portions :
tête : enchâssée dans le duodénum
processus unciné (uncinatus) : prolongement inféro-gauche de la tête du pancréas, excavé en regard des vaisseaux mésentériques supérieurs
tubercule omental (épiploïque) : région de la tête du pancréas
col (isthme) : jonction entre la tête et le corps en regard du tronc porte
corps : portion horizontale, triangulaire à la coupe, en regard des vertèbres lombaires
queue : prolongement du pancréas, en regard des vertèbres T11-T12
Bibliographie
Frank H Netter, Atlas d'anatomie humaine, 6e édition. Paris : Saunders Elsevier, 2014, 624p.
Casoli V, De Seze M, Midy D. Anatomie Appareil Digestif. Éditions Bergeret, 2014, 305p.
4 notes
·
View notes
Note
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e., it has both an endocrine and a digestive exocrine function.[2] 99% of the pancreas is exocrine and 1% is endocrine.[3][4][5][6] As an endocrine gland, it functions mostly to regulate blood sugar levels, secreting the hormones insulin, glucagon, somatostatin and pancreatic polypeptide. As a part of the digestive system, it functions as an exocrine gland secreting pancreatic juice into the duodenum through the pancreatic duct. This juice contains bicarbonate, which neutralizes acid entering the duodenum from the stomach; and digestive enzymes, which break down carbohydrates, proteins and fats in food entering the duodenum from the stomach.
Pancreas
Anatomy of the pancreas
Details
Pronunciation
/ˈpæŋkriəs/
Precursor
Pancreatic buds
System
Digestive system and endocrine system
Artery
Inferior pancreaticoduodenal artery, anterior superior pancreaticoduodenal artery, posterior superior pancreaticoduodenal artery, splenic artery
Vein
Pancreaticoduodenal veins, pancreatic veins
Nerve
Pancreatic plexus, celiac ganglia, vagus nerve[1]
Lymph
Splenic lymph nodes, celiac lymph nodes and superior mesenteric lymph nodes
Identifiers
Latin
pancreas
Greek
Πάνκρεας (Pánkreas)
MeSH
D010179
TA98
A05.9.01.001
TA2
3114
FMA
7198
Anatomical terminology
[edit on Wikidata]
Inflammation of the pancreas is known as pancreatitis, with common causes including chronic alcohol use and gallstones. Because of its role in the regulation of blood sugar, the pancreas is also a key organ in diabetes mellitus. Pancreatic cancer can arise following chronic pancreatitis or due to other reasons, and carries a very poor prognosis, as it is often only identified after it has spread to other areas of the body.
The word pancreas comes from the Greek πᾶν (pân, "all") & κρέας (kréas, "flesh"). The function of the pancreas in diabetes has been known since at least 1889, with its role in insulin production identified in 1921.
Structure
edit
The pancreas (shown here in pink) sits behind the stomach, with the body near the curvature of the duodenum, and the tail stretching to touch the spleen.
The pancreas is an organ that in humans lies in the abdomen, stretching from behind the stomach to the left upper abdomen near the spleen. In adults, it is about 12–15 centimetres (4.7–5.9 in) long, lobulated, and salmon-coloured in appearance.[7]
Anatomically, the pancreas is divided into a head, neck, body, and tail. The pancreas stretches from the inner curvature of the duodenum, where the head surrounds two blood vessels: the superior mesenteric artery and vein. The longest part of the pancreas, the body, stretches across behind the stomach, and the tail of the pancreas ends adjacent to the spleen.[7]
Two ducts, the main pancreatic duct and a smaller accessory pancreatic duct run through the body of the pancreas. The main pancreatic duct joins with the common bile duct forming a small ballooning called the ampulla of Vater (hepatopancreatic ampulla). This ampulla is surrounded by a muscle, the sphincter of Oddi. This ampulla opens into the descending part of the duodenum. The opening of the common bile duct into main pancreatic duct is controlled by sphincter of Boyden. The accessory pancreatic duct opens into duodenum with separate openings located above the opening of the main pancreatic duct.[7]
Parts
edit
The head of the pancreas sits within the curvature of the duodenum, and wraps around the superior mesenteric artery and vein. To the right sits the descending part of the duodenum, and between these travel the superior and inferior pancreaticoduodenal arteries. Behind rests the inferior vena cava, and the common bile duct. In front sits the peritoneal membrane and the transverse colon.[7] A small uncinate process emerges from below the head, situated behind the superior mesenteric vein and sometimes artery.[7]
The neck of the pancreas separates the head of the pancreas, located in the curvature of the duodenum, from the body. The neck is about 2 cm (0.79 in) wide, and sits in front of where the portal vein is formed. The neck lies mostly behind the pylorus of the stomach, and is covered with peritoneum. The anterior superior pancreaticoduodenal artery travels in front of the neck of the pancreas.[7]
The body is the largest part of the pancreas, and mostly lies behind the stomach, tapering along its length. The peritoneum sits on top of the body of the pancreas, and the transverse colon in front of the peritoneum.[7] Behind the pancreas are several blood vessels, including the aorta, the splenic vein, and the left renal vein, as well as the beginning of the superior mesenteric artery.[7] Below the body of the pancreas sits some of the small intestine, specifically the last part of the duodenum and the jejunum to which it connects, as well as the suspensory ligament of the duodenum which falls between these two. In front of the pancreas sits the transverse colon.[8]
The pancreas narrows towards the tail, which sits near to the spleen.[7] It is usually between 1.3–3.5 cm (0.51–1.38 in) long, and sits between the layers of the ligament between the spleen and the left kidney. The splenic artery and vein, which also passes behind the body of the pancreas, pass behind the tail of the pancreas.[7]
Blood supply
edit
The pancreas has a rich blood supply, with vessels originating as branches of both the coeliac artery and superior mesenteric artery.[7] The splenic artery, the largest branch of the celiac trunk, runs along the top of the pancreas, and supplies the left part of the body and the tail of the pancreas through its pancreatic branches, the largest of which is called the greater pancreatic artery.[7] The superior and inferior pancreaticoduodenal arteries run along the back and front surfaces of the head of the pancreas adjacent to the duodenum. These supply the head of the pancreas. These vessels join together (anastamose) in the middle.[7]
The body and neck of the pancreas drain into the splenic vein, which sits behind the pancreas.[7] The head drains into, and wraps around, the superior mesenteric and portal veins, via the pancreaticoduodenal veins.[7]
The pancreas drains into lymphatic vessels that travel alongside its arteries, and has a rich lymphatic supply.[7] The lymphatic vessels of the body and tail drain into splenic lymph nodes, and eventually into lymph nodes that lie in front of the aorta, between the coeliac and superior mesenteric arteries. The lymphatic vessels of the head and neck drain into intermediate lymphatic vessels around the pancreaticoduodenal, mesenteric and hepatic arteries, and from there into the lymph nodes that lie in front of the aorta.[7]
Microanatomy
edit
This image shows a pancreatic islet when pancreatic tissue is stained and viewed under a microscope. Parts of the digestive ("exocrine") pancreas can be seen around the islet, more darkly. These contain hazy dark purple granules of inactive digestive enzymes (zymogens).
A pancreatic islet that uses fluorescent antibodies to show the location of different cell types in the pancreatic islet. Antibodies against glucagon, secreted by alpha cells, show their peripheral position. Antibodies against insulin, secreted by beta cells, show the more widespread and central position that these cells tend to have.[9]
The pancreas contains tissue with an endocrine and exocrine role, and this division is also visible when the pancreas is viewed under a microscope.[10]
The majority of pancreatic tissue has a digestive role. The cells with this role form clusters (Latin: acini) around small ducts, and are arranged in lobes that have thin fibrous walls. The cells of each acinus secrete inactive digestive enzymes called zymogens into the small intercalated ducts which they surround. In each acinus, the cells are pyramid-shaped and situated around the intercalated ducts, with the nuclei resting on the basement membrane, a large endoplasmic reticulum, and a number of zymogen granules visible within the cytoplasm. The intercalated ducts drain into larger intralobular ducts within the lobule, and finally interlobular ducts. The ducts are lined by a single layer of column-shaped cells. There is more than one layer of cells as the diameter of the ducts increases.[10]
The tissues with an endocrine role within the pancreas exist as clusters of cells called pancreatic islets (also called islets of Langerhans) that are distributed throughout the pancreas.[9] Pancreatic islets contain alpha cells, beta cells, and delta cells, each of which releases a different hormone. These cells have characteristic positions, with alpha cells (secreting glucagon) tending to be situated around the periphery of the islet, and beta cells (secreting insulin) more numerous and found throughout the islet.[9] Enterochromaffin cells are also scattered throughout the islets.[9] Islets are composed of up to 3,000 secretory cells, and contain several small arterioles to receive blood, and venules that allow the hormones secreted by the cells to enter the systemic circulation.[9]
Variation
edit
The size of the pancreas varies considerably.[7] Several anatomical variations exist, relating to the embryological development of the two pancreatic buds. The pancreas develops from these buds on either side of the duodenum. The ventral bud rotates to lie next to the dorsal bud, eventually fusing. In about 10% of adults, an accessory pancreatic duct may be present if the main duct of the dorsal bud of the pancreas does not regress; this duct opens into the minor duodenal papilla.[11] If the two buds themselves, each having a duct, do not fuse, a pancreas may exist with two separate ducts, a condition known as a pancreas divisum. This condition has no physiologic consequence.[12] If the ventral bud does not fully rotate, an annular pancreas may exist, where part or all of the duodenum is encircled by the pancreas. This may be associated with duodenal atresia.[13]
Gene and protein expression
edit
Further information: Bioinformatics § Gene and protein expression
10,000 protein coding genes (~50% of all human genes) are expressed in the normal human pancreas.[14][15] Less than 100 of these genes are specifically expressed in the pancreas. Similar to the salivary glands, most pancreas-specific genes encode for secreted proteins. Corresponding pancreas-specific proteins are either expressed in the exocrine cellular compartment and have functions related to digestion or food uptake such as digestive chymotrypsinogen enzymes and pancreatic lipase PNLIP, or are expressed in the various cells of the endocrine pancreatic islets and have functions related to secreted hormones such as insulin, glucagon, somatostatin and pancreatic polypeptide.[16]
Development
edit
The pancreas originates from the foregut, a precursor tube to part of the digestive tract, as a dorsal and ventral bud. As it develops, the ventral bud rotates to the other side and the two buds fuse together.
The pancreas forms during development from two buds that arise from the duodenal part of the foregut, an embryonic tube that is a precursor to the gastrointestinal tract.[11] It is of endodermal origin.[11] Pancreatic development begins with the formation of a dorsal and ventral pancreatic bud. Each joins with the foregut through a duct. The dorsal pancreatic bud forms the neck, body, and tail of the developed pancreas, and the ventral pancreatic bud forms the head and uncinate process.[11]
The definitive pancreas results from rotation of the ventral bud and the fusion of the two buds.[11] During development, the duodenum rotates to the right, and the ventral bud rotates with it, moving to a position that becomes more dorsal. Upon reaching its final destination, the ventral pancreatic bud is below the larger dorsal bud, and eventually fuses with it. At this point of fusion, the main ducts of the ventral and dorsal pancreatic buds fuse, forming the main pancreatic duct. Usually, the duct of the dorsal bud regresses, leaving the main pancreatic duct.[11]
Cellular development
edit
Pancreatic progenitor cells are precursor cells that differentiate into the functional pancreatic cells, including exocrine acinar cells, endocrine islet cells, and ductal cells.[17] These progenitor cells are characterised by the co-expression of the transcription factors PDX1 and NKX6-1.[17]
The cells of the exocrine pancreas differentiate through molecules that induce differentiation including follistatin, fibroblast growth factors, and activation of the Notch receptor system.[17] Development of the exocrine acini progresses through three successive stages. These are the predifferentiated, protodifferentiated, and differentiated stages, which correspond to undetectable, low, and high levels of digestive enzyme activity, respectively.[17]
Pancreatic progenitor cells differentiate into endocrine islet cells under the influence of neurogenin-3 and ISL1, but only in the absence of notch receptor signaling. Under the direction of a Pax gene, the endocrine precursor cells differentiate to form alpha and gamma cells. Under the direction of Pax-6, the endocrine precursor cells differentiate to form beta and delta cells.[17] The pancreatic islets form as the endocrine cells migrate from the duct system to form small clusters around capillaries.[9] This occurs around the third month of development,[11] and insulin and glucagon can be detected in the human fetal circulation by the fourth or fifth month of development.[17]
Function
edit
The pancreas is involved in blood sugar control and metabolism within the body, and also in the secretion of substances (collectively pancreatic juice) that help digestion. These are divided into an "endocrine" role, relating to the secretion of insulin and other substances within pancreatic islets that help control blood sugar levels and metabolism within the body, and an "exocrine" role, relating to the secretion of enzymes involved in digesting substances in the digestive tract.[10]
Blood glucose regulation
edit
See also: Pancreatic islets
The pancreas maintains constant blood glucose levels (shown as the waving line). When the blood glucose level is too high, the pancreas secretes insulin and when the level is too low, the pancreas secretes glucagon.
Cells within the pancreas help to maintain blood glucose levels (homeostasis). The cells that do this are located within the pancreatic islets that are present throughout the pancreas. When blood glucose levels are low, alpha cells secrete glucagon, which increases blood glucose levels. When blood glucose levels are high beta cells secrete insulin to decrease glucose in blood. Delta cells in the islet also secrete somatostatin which decreases the release of insulin and glucagon.[9]
Glucagon acts to increase glucose levels by promoting the creation of glucose and the breakdown of glycogen to glucose in the liver. It also decreases the uptake of glucose in fat and muscle. Glucagon release is stimulated by low blood glucose or insulin levels, and during exercise.[18] Insulin acts to decrease blood glucose levels by facilitating uptake by cells (particularly skeletal muscle), and promoting its use in the creation of proteins, fats and carbohydrates. Insulin is initially created as a precursor form called preproinsulin. This is converted to proinsulin and cleaved by C-peptide to insulin which is then stored in granules in beta cells. Glucose is taken into the beta cells and degraded. The end effect of this is to cause depolarisation of the cell membrane which stimulates the release of the insulin.[18]
The main factor influencing the secretion of insulin and glucagon are the levels of glucose in blood plasma.[19] Low blood sugar stimulates glucagon release, and high blood sugar stimulates insulin release. Other factors also influence the secretion of these hormones. Some amino acids, that are byproducts of the digestion of protein, stimulate insulin and glucagon release. Somatostatin acts as an inhibitor of both insulin and glucagon. The autonomic nervous system also plays a role. Activation of Beta-2 receptors of the sympathetic nervous system by catecholamines secreted from sympathetic nerves stimulates secretion of insulin and glucagon,[19][20] whereas activation of Alpha-1 receptors inhibits secretion.[19] M3 receptors of the parasympathetic nervous system act when stimulated by the right vagus nerve to stimulate release of insulin from beta cells.[19]
Digestion
edit
The pancreas has a role in digestion, highlighted here. Ducts in the pancreas (green) conduct digestive enzymes into the duodenum. This image also shows a pancreatic islet, part of the endocrine pancreas, which contains cells responsible for secretion of insulin and glucagon.
The pancreas plays a vital role in the digestive system. It does this by secreting a fluid that contains digestive enzymes into the duodenum, the first part of the small intestine that receives food from the stomach. These enzymes help to break down carbohydrates, proteins and lipids (fats). This role is called the "exocrine" role of the pancreas. The cells that do this are arranged in clusters called acini. Secretions into the middle of the acinus accumulate in intralobular ducts, which drain to the main pancreatic duct, which drains directly into the duodenum. About 1.5 - 3 liters of fluid are secreted in this manner every day.[8][21]
The cells in each acinus are filled with granules containing the digestive enzymes. These are secreted in an inactive form termed zymogens or proenzymes. When released into the duodenum, they are activated by the enzyme enterokinase present in the lining of the duodenum. The proenzymes are cleaved, creating a cascade of activating enzymes.[21]
Enzymes that break down proteins begin with activation of trypsinogen to trypsin. The free trypsin then cleaves the rest of the trypsinogen, as well as chymotrypsinogen to its active form chymotrypsin.[21]
Enzymes secreted involved in the digestion of fats include lipase, phospholipase A2, lysophospholipase, and cholesterol esterase.[21]
Enzymes that break down starch and other carbohydrates include amylase.[21]
These enzymes are secreted in a fluid rich in bicarbonate. Bicarbonate helps maintain an alkaline pH for the fluid, a pH in which most of the enzymes act most efficiently, and also helps to neutralise the stomach acids that enter the duodenum.[21] Secretion is influenced by hormones including secretin, cholecystokinin, and VIP, as well as acetylcholine stimulation from the vagus nerve. Secretin is released from the S cells which form part of the lining of the duodenum in response to stimulation by gastric acid. Along with VIP, it increases the secretion of enzymes and bicarbonate. Cholecystokinin is released from Ito cells of the lining of the duodenum and jejunum mostly in response to long chain fatty acids, and increases the effects of secretin.[21] At a cellular level, bicarbonate is secreted from centroacinar and ductal cells through a sodium and bicarbonate cotransporter that acts because of membrane depolarisation caused by the cystic fibrosis transmembrane conductance regulator. Secretin and VIP act to increase the opening of the cystic fibrosis transmembrane conductance regulator, which leads to more membrane depolarisation and more secretion of bicarbonate.[22][23][24]
A variety of mechanisms act to ensure that the digestive action of the pancreas does not act to digest pancreatic tissue itself. These include the secretion of inactive enzymes (zymogens), the secretion of the protective enzyme trypsin inhibitor, which inactivates trypsin, the changes in pH that occur with bicarbonate secretion that stimulate digestion only when the pancreas is stimulated, and the fact that the low calcium within cells causes inactivation of trypsin.[21]
Additional functions
edit
The pancreas also secretes vasoactive intestinal peptide and pancreatic polypeptide. Enterochromaffin cells of the pancreas secrete the hormones motilin, serotonin, and substance P.[9]
Clinical significance
edit
Main article: Pancreatic disease
Inflammation
edit
Main article: Pancreatitis
Inflammation of the pancreas is known as pancreatitis. Pancreatitis is most often associated with recurrent gallstones or chronic alcohol use, with other common causes including traumatic damage, damage following an ERCP, some medications, infections such as mumps and very high blood triglyceride levels. Acute pancreatitis is likely to cause intense pain in the central abdomen, that often radiates to the back, and may be associated with nausea or vomiting. Severe pancreatitis may lead to bleeding or perforation of the pancreas resulting in shock or a systemic inflammatory response syndrome, bruising of the flanks or the region around the belly button. These severe complications are often managed in an intensive care unit.[25]
In pancreatitis, enzymes of the exocrine pancreas damage the structure and tissue of the pancreas. Detection of some of these enzymes, such as amylase and lipase in the blood, along with symptoms and findings on medical imaging such as ultrasound or a CT scan, are often used to indicate that a person has pancreatitis. Pancreatitis is often managed medically with pain reliefs, and monitoring to prevent or manage shock, and management of any identified underlying causes. This may include removal of gallstones, lowering of blood triglyceride or glucose levels, the use of corticosteroids for autoimmune pancreatitis, and the cessation of any medication triggers.[25]
Chronic pancreatitis refers to the development of pancreatitis over time. It shares many similar causes, with the most common being chronic alcohol use, with other causes including recurrent acute episodes and cystic fibrosis. Abdominal pain, characteristically relieved by sitting forward or drinking alcohol, is the most common symptom. When the digestive function of the pancreas is severely affected, this may lead to problems with fat digestion and the development of steatorrhoea; when the endocrine function is affected, this may lead to diabetes. Chronic pancreatitis is investigated in a similar way to acute pancreatitis. In addition to management of pain and nausea, and management of any identified causes (which may include alcohol cessation), because of the digestive role of the pancreas, enzyme replacement may be needed to prevent malabsorption.[25]
Cancer
edit
Main article: Pancreatic cancer
Pancreatic cancer, shown here, most commonly occurs as an adenocarcinoma in the head of the pancreas. Because symptoms (such as skin yellowing, pain, or itch) do not occur until later in the disease, it often presents at a later stage and has limited treatment options.
Relative incidences of various pancreatic neoplasms, with pancreatic cancers in red/pink color.[26]
Pancreatic cancers, particularly the most common type, pancreatic adenocarcinoma, remain very difficult to treat, and are mostly diagnosed only at a stage that is too late for surgery, which is the only curative treatment. Pancreatic cancer is rare in people younger than 40 and the median age of diagnosis is 71.[27] Risk factors include chronic pancreatitis, older age, smoking, obesity, diabetes, and certain rare genetic conditions including multiple endocrine neoplasia type 1, hereditary nonpolyposis colon cancer and dysplastic nevus syndrome among others.[25][28] About 25% of cases are attributable to tobacco smoking,[29] while 5–10% of cases are linked to inherited genes.[27]
Pancreatic adenocarcinoma is the most common form of pancreatic cancer, and is cancer arising from the exocrine digestive part of the pancreas. Most occur in the head of the pancreas.[25] Symptoms tend to arise late in the course of the cancer, when it causes abdominal pain, weight loss, or yellowing of the skin (jaundice). Jaundice occurs when the outflow of bile is blocked by the cancer. Other less common symptoms include nausea, vomiting, pancreatitis, diabetes or recurrent venous thrombosis.[25] Pancreatic cancer is usually diagnosed by medical imaging in the form of an ultrasound or CT scan with contrast enhancement. An endoscopic ultrasound may be used if a tumour is being considered for surgical removal, and biopsy guided by ERCP or ultrasound can be used to confirm an uncertain diagnosis.[25]
Because of the late development of symptoms, most cancer presents at an advanced stage.[25] Only 10 to 15% of tumours are suitable for surgical resection.[25] As of 2018, when chemotherapy is given the FOLFIRINOX regimen containing fluorouracil, irinotecan, oxaliplatin and leucovorin has been shown to extend survival beyond traditional gemcitabine regimens.[25] For the most part, treatment is palliative, focus on the management of symptoms that develop. This may include management of itch, a choledochojejunostomy or the insertion of stents with ERCP to facilitate the drainage of bile, and medications to help control pain.[25] In the United States pancreatic cancer is the fourth most common cause of deaths due to cancer.[30] The disease occurs more often in the developed world, which had 68% of new cases in 2012.[31] Pancreatic adenocarcinoma typically has poor outcomes with the average percentage alive for at least one and five years after diagnosis being 25% and 5% respectively.[31][32] In localized disease where the cancer is small (< 2 cm) the number alive at five years is approximately 20%.[33]
There are several types of pancreatic cancer, involving both the endocrine and exocrine tissue. The many types of pancreatic endocrine tumors are all uncommon or rare, and have varied outlooks. However the incidence of these cancers has been rising sharply; it is not clear to what extent this reflects increased detection, especially through medical imaging, of tumors that would be very slow to develop. Insulinomas (largely benign) and gastrinomas are the most common types.[34] For those with neuroendocrine cancers the number alive after five years is much better at 65%, varying considerably with type.[31]
A solid pseudopapillary tumour is a low-grade malignant tumour of the pancreas of papillary architecture that typically afflicts young women.[35]
Diabetes mellitus
edit
Type 1 diabetes
edit
Main article: Diabetes mellitus type 1
Diabetes mellitus type 1 is a chronic autoimmune disease in which the immune system attacks the insulin-secreting beta cells of the pancreas.[36] Insulin is needed to keep blood sugar levels within optimal ranges, and its lack can lead to high blood sugar. As an untreated chronic condition, complications including accelerated vascular disease, diabetic retinopathy, kidney disease and neuropathy can result.[36] In addition, if there is not enough insulin for glucose to be used within cells, the medical emergency diabetic ketoacidosis, which is often the first symptom that a person with type 1 diabetes may have, can result.[37] Type 1 diabetes can develop at any age but is most often diagnosed before age 40.[36] For people living with type 1 diabetes, insulin injections are critical for survival.[36] An experimental procedure to treat type 1 diabetes is pancreas transplantation or isolated transplantation of islet cells to supply a person with functioning beta cells.[36]
Type 2 diabetes
edit
Main article: Diabetes mellitus type 2
Diabetes mellitus type 2 is the most common form of diabetes.[36] The causes for high blood sugar in this form of diabetes usually are a combination of insulin resistance and impaired insulin secretion, with both genetic and environmental factors playing a role in the development of the disease.[38] Over time, pancreatic beta cells may become "exhausted" and less functional.[36] The management of type 2 diabetes involves a combination of lifestyle measures, medications if required and potentially insulin.[39] With relevance to the pancreas, several medications act to enhance the secretion of insulin from beta cells, particularly sulphonylureas, which act directly on beta cells; incretins which replicate the action of the hormones glucagon-like peptide 1, increasing the secretion of insulin from beta cells after meals, and are more resistant to breakdown; and DPP-4 inhibitors, which slow the breakdown of incretins.[39]
Removal
edit
It is possible for a person to live without a pancreas, provided that the person takes insulin for proper regulation of blood glucose concentration and pancreatic enzyme supplements to aid digestion.[40]
History
edit
The pancreas was first identified by Herophilus (335–280 BC), a Greek anatomist and surgeon.[41] A few hundred years later, Rufus of Ephesus, another Greek anatomist, gave the pancreas its name. Etymologically, the term "pancreas", a modern Latin adaptation of Greek πάγκρεας,[42] [πᾶν ("all", "whole"), and κρέας ("flesh")],[43] originally means sweetbread,[44] although literally meaning all-flesh, presumably because of its fleshy consistency. It was only in 1889 when Oskar Minkowski discovered that removing the pancreas from a dog caused it to become diabetic.[45] Insulin was later isolated from pancreatic islets by Frederick Banting and Charles Best in 1921.[45]
The way the tissue of the pancreas has been viewed has also changed. Previously, it was viewed using simple staining methods such as H&E stains. Now, immunohistochemistry can be used to more easily differentiate cell types. This involves visible antibodies to the products of certain cell types, and helps identify with greater ease cell types such as alpha and beta cells.[9]
Other animals
edit
Pancreatic tissue is present in all vertebrates, but its precise form and arrangement varies widely. There may be up to three separate pancreases, two of which arise from the pancreatic bud, and the other dorsally. In most species (including humans), these "fuse" in the adult, but there are several exceptions. Even when a single pancreas is present, two or three pancreatic ducts may persist, each draining separately into the duodenum (or equivalent part of the foregut). Birds, for example, typically have three such ducts.[46]
In teleost fish, and a few other species (such as rabbits), there is no discrete pancreas at all, with pancreatic tissue being distributed diffusely across the mesentery and even within other nearby organs, such as the liver or spleen. In a few teleost species, the endocrine tissue has fused to form a distinct gland within the abdominal cavity, but otherwise it is distributed among the exocrine components. The most primitive arrangement, however, appears to be that of lampreys and lungfish, in which pancreatic tissue is found as a number of discrete nodules within the wall of the gut itself, with the exocrine portions being little different from other glandular structures of the intestine.[46]
Cuisine
edit
The pancreas of calf (ris de veau) or lamb (ris d'agneau), and, less commonly, of beef or pork, are used as food under the culinary name of sweetbread.[47][48]
Oh my, that information is very nutritious. Thank you! :D
0 notes
Text
Homeopathy Treatment For Diabetes
Home | Diabetes | Homeopathy Treatment For Diabetes

Diabetes mellitus known commonly as “Diabetes” and also “sugar” is a disease which includes a group of metabolic disorders that feature increase in blood sugar levels, hyperglycaemia.
What causes Diabetes?
Diabetes is caused due to the factors which contribute to hyperglycemia , factors are ;
Reduced insulin secretion
Decreased glucose utilization
Increased glucose production
What happens in Diabetes?
Reduced Insulin Secretion : Insulin is secreted by the pancreas which is both an exocrine and endocrine gland located in the abdomen. The function of Insulin facilitates the body to utilise glucose for metabolic activities and growth. Any metabolic disorder which causes reduced insulin secretion leads to hyperglycemia condition as the glucose is left unutilised by the body.
Decreased glucose utilization : This factor is self-explanatory. Whenever the glucose in the body is not utilised, it leads to hyperglycemia. This could be due to either reduced insulin secretion and release or due to faulty lifestyle activities such as sedentary life, obesity, lack of physical exercise, improper diet etc.
Increased glucose production : Sometimes, glucose is produced within the body by the breakdown of glycogen by the process of glycogenolysis,which is stored in certain organs. And way which causes increase in glucose production is by the gluconeogenesis, conversion of non-carbohydrates such as fatty acids and proteins into glucose.
What are the symptoms of Diabetes?
Diabetes is a disease which includes a group of metabolic disorders. It is not a single disease or a syndrome but a group of disorders which cause increase in blood sugar levels. Therefore, it should be understood that in a patient with diabetes, not one system of the body is affected but there different reasons for hyperglycemia which need to be attended. This clearly implies, constitutional treatment is the way to treat diabetes which includes all the characters of the patient , from physical appearance to medical history, from hereditary factors to the lifestyle modifications, from mind to body.
What is the treatment for Diabetes?
Homeopathy is a system of medicine which has remedies for diabetes treatment with proven efficacy on human beings. A homeopathic doctor follows constitutional mode of treatment in their profession which enables recovery of health in patients with diabetes. At Positive Homeopathy, complete emphasis is given to orthodox and constitutional methods by experienced doctors so as to provide best homeopathic treatment for diabetes and its complications.
Along with quality treatment for diabetes, management of patients with diabetes is stressed upon by expert doctors at Positive Homeopathic clinics. The importance of lifestyle changes in the control of blood sugar levels is communicated to the patients by our doctors. Lifestyle changes such as regular physical exercise, proper diet regimen, avoidance of undue stress, etc are needed to followed by the diabetic patients.
Finally, it should be understood by the patients with diabetes that the treatment plan for diabetes includes a long-term approach for a healthy life. This is definitely attainable and is seen happening in many satisfied diabetic patients of Positive Homeopathy. Patients should follow the treatment for the duration recommended by the doctors along with the homeopathic management protocol.
**Results may vary from patient to patient
Frequently Asked Questions
What health problems can people with diabetes develop?
Over time, high blood glucose leads to problems such as
heart disease stroke, kidney disease, eye problems, dental disease, nerve damage, foot problems
You can take steps to lower your chances of developing these diabetes-related health problems.
What is the cause of type 1 diabetes?
Type 1 diabetes develops because the body’s immune system destroys beta cells in a part of the pancreas called the islet tissue. These beta cells produce glucose. So people with type 1 diabetes can’t make their own glucose. The pancreas normally adjusts the amount of glucose it makes based on your changing blood sugar.
0 notes
Text
The Submandibular Gland: Structure, Function, and Clinical Significance
Introduction
The submandibular gland is one of the major salivary glands located in the human oral cavity. It plays a vital role in the process of digestion and maintaining oral health. This article provides an overview of the submandibular gland, discussing its structure, function, and clinical significance, including treatment options available in Warangal, Hanumakonda, Kukatpally, and Hyderabad.
Anatomy of the Submandibular Gland
The submandibular gland, also known as the submaxillary gland, is a paired exocrine gland located beneath the floor of the mouth, on either side of the mandible, hence its name. It is the second-largest salivary gland in the human body, following the parotid gland. The gland has a roughly almond-shaped structure and is composed of both serous and mucous acini (secretory units). It is connected to the oral cavity through a duct called Wharton's duct.
Function of the Submandibular Gland
Saliva Production: The primary function of the submandibular gland is to produce saliva. Saliva is essential for various processes in the oral cavity, including digestion, speech, and maintaining oral hygiene.
Enzyme Secretion: The serous acini of the submandibular gland secrete saliva rich in enzymes, such as amylase, which helps break down starches in food during the initial stages of digestion.
Lubrication: Saliva produced by the submandibular gland aids in the lubrication of food, making it easier to swallow.
Antibacterial Properties: Saliva contains enzymes and antimicrobial proteins that help protect the oral cavity from harmful bacteria.
Clinical Significance and Treatment Options
Salivary Stones: One common issue associated with the submandibular gland is the formation of salivary stones, also known as sialolithiasis. These stones can block the duct, causing pain and swelling in the gland. Treatment, including submandibular gland swelling treatment in Warangal and Hanumakonda, may involve removal of the stone or managing symptoms.
Infections: Infections of the submandibular gland can occur, resulting in conditions like sialadenitis. These infections may be bacterial or viral in origin and require appropriate antibiotic treatment. Seek submandibular gland swelling treatment in Warangal for prompt care.
Tumors: Tumors, both benign and malignant, can develop in the submandibular gland. These can lead to swelling, pain, and changes in saliva production. Diagnosis and submandibular gland surgery in Hanumakonda or Kukatpally may be necessary, and further treatment options like salivary gland removal surgery in Kukatpally and Hyderabad may be considered based on the type and stage of the tumor.
Sjögren's Syndrome: This autoimmune disorder can affect the submandibular gland and other salivary glands, leading to reduced saliva production and dry mouth. Management may involve medications and submandibular gland removal in Hyderabad in severe cases.
Conclusion
The submandibular gland is a crucial component of the human oral cavity, responsible for saliva production, enzyme secretion, and maintaining oral health. Understanding its anatomy and functions is essential for diagnosing and managing various clinical conditions associated with this gland. If you are in Warangal, Hanumakonda, Kukatpally, or Hyderabad and require treatment for submandibular gland-related issues, it is important to consult with a qualified healthcare professional who can provide appropriate care and guidance tailored to your specific needs.
About
Dr. Gouda Ramesh is a seasoned ENT surgeon in Hyderabad with more than 18 years of experience. He is an expert in performing complex ENT surgeries and adept in coblator assisted adeo- tonsillectomy, endoscopic laser tympano-mastoidectomy, micro-debrider assisted sinus surgeries (FESS), radiofrequency, laser micro-laryngeal surgeries, and thyroid surgeries, bronchoscopy. He has successfully performed more than 10000 surgeries and treated more than 200000 patient. Gouda ENT is the best ENT hospital in hyderabad.
0 notes